hea th magazine
Women's health
THE BABY BLUES: WHAT IT IS - AND ISN'T WOMEN AND AUTOIMMUNE DISORDERS
RUSHING WOMAN'S SYNDROME: HOW TO SLOW DOWN
ENDOMETRIOSIS: MUCH MISUNDERSTOOD
SPECIAL EDITION 2023




2 Try Ferrogen Modified Release Iron Supplements for the prevention & treatment of iron deficiency Always read the label and follow the directions for use. When iron deficiency anaemia has been diagnosed by a doctor and a therapeutic oral iron supplement has been recommended. Choose Pink. Choose * Women aged 19-50. Australian Health Survey: Usual Nutrient Intakes 2011-12 financial year. el in your element OF AUSTRALIAN WOMEN % DON’T GET ENOUGH IRON.* 38 ARE YOU ONE OF THEM?
Your health is your most important asset. It allows you to live your life to the fullest, and guides your life no matter your age, background or ambitions. Investing in your heath and learning more about it could enrich your understanding of yourself, and help not just your physical health but your overall wellbeing.



On page 6, we look at just how important mental health is for new and expectant parents. Learn all about slowing down with Rushing woman's syndrome on page 20. If you've heard of endometriosis and want to know more, see page 18 as we look at it's causes, treatments, and how it affects women across the world.
All material included in Health Check magazine is provided as general information and is not intended, nor may it be construed, as medical advice or instruction. Information and opinions expressed are believed to be correct and accurate to the best knowledge and judgement of the authors. Readers should consult their appropriately qualified health care professional prior to taking any action or inaction in relation to the content contained herein.
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 3 CONTENTS 14 FINDING BALANCE: HOW TO PRIORITISE YOUR HEALTH AND AVOID EXTREME EATING HABITS 16 FROM PILLS TO PATCHES: EXPLORING THE RANGE OF CONTRACEPTIVE CHOICES 18 ENDOMETRIOSIS 20 RUSHING WOMAN’S SYNDROME 22 GETTING ENOUGH SLEEP 25 WHAT IS OSTEOPOROSIS? 28 UNDERSTANDING OUR REPRODUCTIVE HORMONES 32 RETURNING TO WORK 35 MENOPAUSAL HORMONE THERAPY FACTSHEET 38 LOOKING AFTER YOUR ACLS 39 WHAT’S
BLOOMS THE CHEMIST
CHECK MAGAZINE | WOMENS'S EDITION 2023 4 ASK A PHARMACIST: HIGH BLOOD PRESSURE 6 PERINATAL MENTAL HEALTH IN AUSTRALIA 8 STRONGER THINGS 10 WOMEN AND AUTOIMMUNE DISORDERS
ON AT YOUR
Disclaimer:
HEALTH
HIGH BLOOD PRESSURE

 by Aurelia Captari
by Aurelia Captari
4
Ask a Pharmacist
What is blood pressure?
Blood pressure is the force of blood pushing against the walls of your arteries as your heart beats. When the pressure is too high, it can damage your arteries and put you at risk of serious health problems such as heart disease and stroke.1 Normal blood pressure is usually considered to be below 120/80 mmHg, and it’s considered high when it consistently measures at 140/90 mmHg or above. In those readings, the first digit is the systolic reading, when the blood is first heard pulsing through the artery, and the second is the diastolic reading, when that sound disappears.
Different for women and men
Women often experience different symptoms and complications. They are more likely to develop high blood pressure during and after menopause, for example.2
High blood pressure in pregnancy can be a sign of pre-eclampsia, a serious condition which can have short- and long-term effects for both mother and baby. Also, women who have high blood pressure during pregnancy are more likely to have it again in later life.3
Symptoms in women
High blood pressure may have no noticeable symptoms, which is why it is often referred to as the ‘silent killer’.4 This means it’s crucial for women to have their blood pressure tested. You can get this done at your nearest Blooms The Chemist pharmacy or most medical centres.
Noticeable symptoms may include:
• Headaches
• Dizziness
• Shortness of breath
• Chest pain
• Vision problems
• Fatigue
• Irregular heartbeat
If you experience any of these symptoms, it is important to speak with your healthcare provider and get your blood pressure checked.4
Complications in women
If left untreated, high blood pressure can lead to a range of serious health complications, for example:5
• Heart disease: There is a risk of damage to the arteries which supply blood to the heart, which can lead to heart disease, heart attacks and other problems.
• Stroke: High blood pressure can interrupt or block blood flow to the brain, causing stroke.
• Kidney disease: Over time, hypertension can cause damage leading to kidney disease and even kidney failure.
• Eye damage: Damage to blood vessels in the eyes can result in vision problems and even blindness.
• Pregnancy complications: Women are at a higher risk of developing pre-eclampsia, which can cause serious problems for both the baby and mother.2
Prevention and management
A healthy lifestyle, following your healthcare provider's recommendations, and monitoring your blood pressure regularly can help you to reduce your risk of serious health complications:5
• Maintain a healthy weight: Being overweight or obese can increase your risk of developing high blood pressure. If you are overweight, losing even a small amount of weight can help lower your blood pressure.
• Eat a healthy diet: Eating a diet rich in fruits, vegetables, whole grains and lean protein can help lower your blood pressure, as will limiting your intake of salty and processed foods.
• Exercise regularly: Regular physical activity can help lower your blood pressure. This can also support the effects of managing weight and stress.
• Quit smoking: Smoking can damage your blood vessels and increase your risk of developing high blood pressure.
• Limit alcohol: Even small adjustments to lower your alcohol intake can prove beneficial for your blood pressure.
• Take medication as prescribed: If you’re on medication to manage high blood pressure, it is important to take it as directed. Follow the instructions and make it known if you experience any side effects or have trouble sticking to your medication regimen.
• Manage stress: Finding ways to manage stress can help lower your blood pressure. Techniques such as deep breathing, meditation, mindfulness, yoga and exercise can all help reduce stress.
• Regularly check your blood pressure: This can help you make adjustments to your lifestyle or medication as needed. It can also inform progress, and help you understand what changes do and don’t work for you.
Medical treatment
Your healthcare provider may recommend medication to help lower your blood pressure.6 Several types are available, including:
• Diuretics: These help the kidneys to remove excess water and salt from the body, which can help lower blood pressure.
• ACE inhibitors (angiotensin-converting enzyme inhibitors): These block the action of a hormone called angiotensin, which can cause blood vessels to narrow, in turn raising your blood pressure.
• ARBs (angiotensin receptor blockers): ARBs work by blocking the receptors that the hormone angiotensin acts on. This helps to lower the blood pressure and to prevent damage to the heart and kidneys.6
• Calcium channel blockers: These help relax and open the blood vessels, which can lower blood pressure.
• Beta blockers: These slow the heart rate and reduce the workload on the heart, which can help lower blood pressure.
It is important to take your medication exactly as prescribed, and to follow up with your healthcare provider regularly to monitor your blood pressure and make any necessary adjustments to your treatment plan.7
1High blood pressure (hypertension): https://www.healthdirect.gov.au/high-bloodpressure-hypertension
2What are the symptoms of high blood pressure in women?: https://www.healthline. com/health/high-blood-pressure-symptoms-women
3Pregnancy – preeclampsia: https://www.betterhealth.vic.gov.au/health/healthyliving /pregnancy-preeclampsia
4High blood pressure and heart disease in women: https://www.goredforwomen.org/ en/know-your-risk/risk-factors/high-blood-pressure-and-heart-disease
5Highbloodpressuresymptomsandcauses:https://www.cdc.gov/bloodpressure/about.htm
6Angiotensin receptor blockers (ARBs): https://www.bhf.org.uk/informationsupport/ heart-matters-magazine/medical/drug-cabinet/arbs
7Bloodpressuremedication:https://www.healthdirect.gov.au/blood-pressure-medication
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 5
HIGH BLOOD PRESSURE, ALSO KNOWN AS HYPERTENSION, IS A COMMON CONDITION THAT AFFECTS OVER A BILLION PEOPLE WORLDWIDE. IT MAY HAVE DIFFERENT EFFECTS ON WOMEN THAN ON MEN, WHICH COULD CHANGE WHAT CAN HELP TO PREVENT AND MANAGE THIS CONDITION.
Perinatal mental health in Australia
by Gidget Foundation Australia
DEPRESSION IS A SERIOUS CONDITION THAT AFFECTS PHYSICAL AND MNETAL HEALTH AND IT'S NOT JUST LOW MOOD
Perinatal Depression and Anxiety
1 in 5 mothers and 1 in 10 fathers will experience perinatal depression and anxiety
50% of new parents will experience adjustment disorders
PNDA is treatable and temporary PNDA is when the number of bad days outnumber the good Anxiety can develop gradually and can be hard to detect
Risk factors for developing PNDA1
100,000 Australians are affected by PNDA each year, with maternal suicide being a leading cause of death amongst expectant and new mothers
Postnatal psychosis affects 1 or 2 new mums in every 1,000. This is marked by thought distortions and altered sense of reality
• Psychological: e.g. birth trauma, grief and loss.
• Social: e.g. isolation, lack of access to safe and culturally responsive support.
• Biological: e.g. mental health history, baby-related factors, physical health issues.
Women experience baby blues and this is not depression. It occurs between days 3-10 after birth and goes away by itself with supportive care. Women can experience mood swings, teariness, feeling overwhelmed and anxiety. It’s a reaction to hormonal shifts3 and adjustment to being a mum.

Protective Factors2
Supportive partner
Other social supports
Resilience
Quality of partner relationship
Women showing more positive feelings towards pregnancy
The first weeks after childbirth are the most critical2 and emphasise the need for early assessment and care. Early intervention reduces the impact and severity of PNDA for all involved5
6
Depression
• Feelings of hopelessness, inadequacy, failure, anger.
• Guilt or teariness.
• Loss of appetite and sleep issues not related to baby.
• Lack of motivation.
• Sad, persistent low mood.
• Thoughts of self-harm or suicide.
Anxiety
• Panic attacks.
• Physical sensation e.g. tight chest, heart palpitations, tense muscle sensations.
• Intrusive, scary thoughts.
• Fear that stops you going out, or checking baby constantly.
• Irritability.
• Finding it hard to relax.
• Agitation.
"My psychologist from Gidget House was my life saviour through this hard time. She was there for myself and for my family and I will always have a special place in my heart for her. The assistance Gidget House offers to families that are struggling is priceless." (Sally)
How Gidget Foundation Australia helps
• Emotional Wellbeing screening program.
• Gidget House.
• Start Talking telehealth.
• Gidget Village group treatment.
• Gidget Virtual Village Facebook group.
TERMINOLOGY
Perinatal – During pregnancy and up to 1 year after birth PPD – (postpartum depression) has been replaced by the term PNDA (perinatal depression and anxiety) as we recognise anxiety and depression systems often occur together and can begin during prgnancy.
THE COST OF PERINATAL DEPRESSION & ANXIETY IN AUSTRALIA IN 1 YEAR IS:
= $877m6
IMPACT OF PNDA
$227m health cost
$643m economic cost
$7m wellbeing cost
Society – increases in sick leave, absenteeism and presenteeism
Family – stesses, health issues, family breakdown, partner having mental health concerns
Individual – pregnancy complications, less self-care, attachment difficulties, attempts to dull pain resulting in overuse of drugs and alcohol, suicide
Baby – prematurity, low birth weight, cognitive, behavioural and emotional difficulties,7 attachment issues, infanticide5
Men's testosterone levels go down after a baby is born, whilst their levels of oxytocin go up. This helps attachment.

Women also have a biological response when babies are born and the release of various hormones aid attachment.
Steps in recovery
Despite the fact that the majority of women are engaged in regular health appointments in the perinatal period, most women with perinatal mental health issues are not identified by care providers.
Acknowledgments and diagnosis
Activities at home: self-care, time out, mindfulness, daily exercise, focus on healthy eating and gut health, re-working sleep habits, kindness to self, re-adjusting expectations.
Social supports: friends, family, groups – online or in person, health professionals, helplines.
Seek more targeted assistance including professional counselling and medication or alternate therapies e.g. acupuncture if needed, from perinatal specialists.
What needs to happen?
• Increase awareness of PNDA in the community and with healthcare providers.
• Provide specific support to partners of new mums.
• Develop online support resources and networks as well as the more traditional face-to-face counselling.
• Development of and access to free in-patient hospital mother and baby units across Australia.
• Screening in perinatal care with specific mental health questions in conjunction with referral and access to timely perinatal support services.
• Specific training of perinatal mental wellbeing to health professionals and students in tertiary education.
• Being more culturally aware in our service delivery.
• Building a workforce supportive of the perinatal period.
Gidget Foundation Australia is a not-for-profit organisation that exists to support the emotional wellbeing of expectant and new parents to ensure they receive timely, appropriate and specialist care. Visit gidgetfoundation.org.au to learn more.
1A comprehensive analysis of post-partum depression risk factors: The role of sociodemographic, individual, relational, and delivery characteristics. Frontiers in public health.
2Risk and protective factors for antepartum and postpartum depression:a prospective study Journal of Psychosomatic Obstetrics & Gynecology 37(4).
3‘Healthy families: https://healthyfamilies.beyondblue.org.au/
4‘FactCheck: Is suicide one of the leading causes of maternal death in Australia?: https://theconversation.com/factcheck-is-suicide-one-of-the-leading-causes-ofmaternal-death-in-australia-65336
5PANDA submission to the productivity commission mental health inquiry April 2019.
6PNDA cost evaluation undertaken by Price waterhouse Coopers Consulting (Australia) Pty Limited in November 2019.
7Risks of untreated depression in pregnancy, Can Fam Physician. 2014 Mar; 60(3).
8Seeking help forchildbirth and depression after childbirth: results of Maternal mental health Study, Arch Women’s Mental Health, 2009.
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 7
Signs and symptoms
From a Gidget Angel
Stronger things
STRENGTH TRAINING, ALSO CALLED RESISTANCE OR MUSCLE TRAINING, IS THE PRACTICE OF BUILDING MUSCLE STRENGTH BY MAKING OUR MUSCLES WORK AGAINST A FORCE. IT’S AN ESSENTIAL PART OF ANY FITNESS ROUTINE, BUT ONLY ONE IN FOUR AUSTRALIAN ADULTS DO THE RECOMMENDED AMOUNT IN A WEEK, AND MANY OF THOSE MISSING OUT ARE WOMEN OR OLDER FOLKS.1

8
Strength training involves lifting weights or using resistance bands to work the muscles in the body. When you lift weights, you create microscopic tears in the muscle fibres, which then repair and grow stronger during the recovery period.2 Over time, this process leads to increased muscle mass and strength. Strength training is often overlooked by women, perhaps due to fears of noticeably bulking up or thinking that cardio is enough.3 However, strength training has numerous benefits for women, both physical and mental, and it's a crucial component of a healthy lifestyle.
Improved muscle mass
Strength training is the most effective way to build and maintain muscle mass, which is essential for women of all ages. As we age, our muscle mass decreases, and this loss is linked to a variety of health problems such as decreased mobility and increased risk of falls. Strength training can counteract this muscle loss and even increase muscle mass, leading to improved strength, balance, and overall physical function.2
Improved bone density
Osteoporosis, a condition characterised by weak and brittle bones, is a common problem among women, especially after menopause. Strength training has been shown to increase bone density and reduce the risk of osteoporosis.4 This is because the stress of resistance training stimulates the bones to build more bone tissue, making them stronger and more resistant to fractures.
Speeds up the metabolism
Many women are concerned about their weight and body composition and may turn to cardio exercise as a way to burn calories and lose fat. While cardio exercise can be effective for that purpose and improving heart health, strength training has the added benefit of increasing the metabolism, which can lead to higher calorie burn, even at rest.2
This is because muscle tissue is more metabolically active than fat tissue, meaning it burns more calories just to maintain itself. By increasing muscle mass through strength training, women can increase their resting metabolic rate, which can lead to long-term weight loss and improved body composition.5
Enhances mental health
Strength training can also have a positive impact on mental health. Exercise has been shown to be an effective way to reduce stress, anxiety and depression, and strength training is no exception.3 It can boost mood by releasing endorphins, the body's natural feelgood chemicals. It can also increase self-esteem and confidence by improving physical appearance and ability. Additionally, strength training provides a sense of accomplishment and empowerment, and may even become a long-term hobby if you enjoy it enough!
Reduces the risk of chronic disease
Chronic diseases like heart disease, diabetes, and cancer are major health concerns for women. Fortunately, strength training has been shown to reduce the risk of these and other chronic diseases. For example, strength training can improve insulin sensitivity, which can reduce the risk of type 2 diabetes.6 It can also lower blood pressure and cholesterol levels, which can reduce the risk of heart disease. Additionally, strength training has been shown to reduce the risk of certain cancers, including breast and colon cancer.
Reduces pain
Many women experience pain and discomfort in their backs, necks, and shoulders. This can be due to poor posture, but it can also be affected by pregnancy and lifting or carrying children. Strength training can help to correct posture by strengthening the muscles that support the spine and improving overall body alignment.6 This can alleviate pain and discomfort, and even prevent future injuries. Additionally, strength training can help to reduce the risk of falls, which can be especially important for older women at a higher risk of falls and associated injuries.
Customisable to individual needs
One of the great things about strength training is that it can be tailored for the individual. Women can choose from a variety of equipment and exercises, including free weights, machines, resistance bands, bodyweight exercises, and more. They can also adjust the weight and intensity of their workouts to match their fitness level and goals.
Strength training can be done at home, at a gym, or even outside, making it a flexible and convenient option for women with busy schedules or limited access to exercise facilities.
Conceptions of strength training
A common concern among women is the fear of developing an overly muscular physique.1 However, this fear is often unfounded. Women typically don’t have enough testosterone to build large amounts of muscle mass naturally, and it takes years of dedicated training and a specialised diet to achieve a bodybuilder's physique. Instead, strength training can help women achieve a healthy, strong body that supports their wellbeing.7 Furthermore, strength training can improve body confidence and self-esteem by focussing on strength and function rather than appearance.
Getting started
Beginning strength training can seem daunting, but everyone has to start somewhere! It's essential to begin with a proper warm-up and to use proper form (techniques) during exercise, to prevent injury. Talking to a certified personal trainer or fitness professional can be helpful in designing a safe and effective strength training program. If you're looking to improve your health and well-being, consider adding strength training to your fitness routine and to help you achieve a strong and healthy body that supports your overall health and wellbeing.
1Muscle strengthening activities among Australian adults: https://www.aihw.gov.au/ getmedia/2f8e0603-5055-4018-9a7d-4960d17e1d40/aihw-phe-275.pdf.aspx 2Resistance training – health benefits: https://www.betterhealth.vic.gov.au/health/ healthyliving/resistance-training-health-benefits
3Physical activity and exercise guidelines for all Australians: https://www.health.gov. au/topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-forall-australians
4Effects of resistance exercise on bone health: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC6279907/
5Strength training for women as a vehicle for health promotion at work: https://www. ncbi.nlm.nih.gov/pmc/articles/PMC5523796/
6Why resistance training is essential for women at every age: https://www.hcf.com. au/health-agenda/women/strong/resistance-training
7The effect of resistance training in women on dynamic strength and muscular hypertrophy: https://pubmed.ncbi.nlm.nih.gov/31820374/
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 9
Women and autoimmune disorders
WHILE BOTH MEN AND WOMEN CAN DEVELOP AUTOIMMUNE DISEASES, THEY ARE MORE PREVALENT IN WOMEN. THEY AFFECT UP TO 8% OF THE FEMALE POPULATION, COMPARED TO 5% OF MEN.1

10
Autoimmune diseases are a group of disorders which occur when the immune system mistakenly attacks healthy cells in the body. These disorders can affect any part of the body, including the joints, skin, and internal organs.
There are more than 80 autoimmune diseases, and they can vary in their severity and symptoms. Common autoimmune diseases affecting women include rheumatoid arthritis, lupus, multiple sclerosis, and thyroid disorders.1
These diseases can be difficult to diagnose, as their symptoms can mimic other illnesses. Common symptoms include fatigue, joint pain, fever, skin rashes, and digestive problems.2 Depending on the type of autoimmune disease, other symptoms may also be present, such as hair loss, vision problems, and breathing difficulties.
Why are women more affected?
Autoimmune diseases may be more prevalent in women due to hormonal differences. Oestrogen, a hormone more abundant in women, can play a role. Studies have shown that oestrogen can influence the immune system by increasing the production of antibodies and inflammatory cytokines (proteins which control the growth and activity of immune system cells), which can trigger autoimmune responses.3
Genetics may be another factor. Women with a family history of autoimmune diseases are at a higher risk of developing these disorders themselves.3 Exposure to toxins and infections may also trigger autoimmune responses in susceptible individuals.
Chromosomes are another possible factor. Women have two X chromosomes compared to men who typically have an X and a Y, and the X contains over double the amount of genetic material of the Y chromosome. As a foetus with two X chromosomes develops, it undergoes ‘X inactivation’ whereby X chromosomes in some cells are inactivated. This varies between foetuses, and the variance is thought to cause an immune response that can cause the body to attack itself, creating an autoimmune disorder.3
Common autoimmune disorders
One autoimmune disease which is particularly common in women is rheumatoid arthritis. This is a chronic inflammatory disorder affecting the joints, which causes pain, stiffness and swelling. Women are two to three times more likely to develop it than men, often during the reproductive years.
Another autoimmune disease more prevalent in women is lupus, or systemic lupus erythematosus. Lupus can affect multiple organs including the skin, kidneys, and lungs.4 Women are nine times more likely to develop lupus than men, and the disease often develops during the childbearing years.
Multiple sclerosis (MS) is also seen more often in women. MS is a chronic inflammatory disorder that affects the central nervous system, causing symptoms such as fatigue, muscle weakness, and vision problems. Women are twice as likely to develop MS as men, often during the fertile years.
Thyroid disorders, such as Hashimoto's thyroiditis and Graves' disease, are more prevalent in women. These occur when the immune system attacks the thyroid gland, causing either an underactive or overactive thyroid.5 Women are up to eight times more likely to develop thyroid disorders than men, and the risk increases with age.
Impact of autoimmune diseases
Autoimmune diseases can seriously affect women's health. Many are chronic conditions requiring ongoing medical management, which can be emotionally and financially draining. Women with autoimmune diseases may also experience social isolation, as their symptoms can make it difficult to participate in social activities or work 6
Pregnancy can also be a concern, as these autoimmune conditions can increase the risk of complications. Women may be at a higher risk of miscarriage, pre-term birth, and pre-eclampsia. Some medications may also be harmful to the foetus, so women with these conditions should work closely with their healthcare providers to manage their symptoms and minimise risks during pregnancy.
Treatment
Treatment typically involves medications to suppress the immune system and reduce inflammation. In some cases, lifestyle changes such as a healthy diet and regular exercise may also help manage symptoms. Individualised treatment plans can address personal symptoms and needs but may change depending on the type of autoimmune condition. For instance, someone suffering from a condition that affects their skin would receive advice on bathing, creams, and the sun. However, someone with coeliac disease would follow a gluten-free diet.
Self-care is an important aspect of managing autoimmune diseases, too. This may include dealing with stress, getting enough sleep, and avoiding triggers which can worsen symptoms. Women with autoimmune diseases may also benefit from support groups, which can provide emotional help along with resources for managing their condition. Some people with an autoimmune condition may find managing symptoms very effective and be able to lead typical lives that are hardly affected by illness.
The outlook
While there is currently no cure for autoimmune diseases, ongoing research is exploring new treatments and potential causes. Advances in genetics and immunology may help to improve our understanding of autoimmune diseases and lead to more effective treatments in future.7
In the meantime, it is important for women to be aware of the signs and symptoms and to seek medical attention if they suspect they may have one of these disorders. Early diagnosis and treatment can help prevent long-term damage and improve quality of life.8
1Autoimmune disease in women: https://www.frontiersin.org/articles/10.3389/ fendo.2019.00265/full
2What are common symptoms of autoimmune disease?: https://www. hopkinsmedicine.org/health/wellness-and-prevention/what-are-common-symptomsof-autoimmune-disease
3The prevalence of autoimmune disorders in women: https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC7292717/
4Autoimmune diseases: https://www.womenshealth.gov/a-z-topics/autoimmunediseases
5Autoimmune disorders: https://w ww.betterhealth.vic.gov.au/health/ conditionsandtreatments/autoimmune-disorders
6Social isolation stress exacerbates autoimmune disease in MRL/lpr mice: https:// pubmed.ncbi.nlm.nih.gov/15589047/
7Treating human autoimmunity: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC4061980/
8Autoimmune diseases: https://www.healthdirect.gov.au/autoimmune-diseases
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 11







Arma Yourself with immune system support
Protect
ArmaForce ® Daily Protect contains vitamin C, D and zinc to proactively support your immune system health.

Relieve
ArmaForce ® is a comprehensive formula containing Andrographis to relieve symptoms of common colds and flu.
Recover
ArmaForce ® Recover is specially formulated with Siberian ginseng to assist in recovery from illness and astragalus traditionally used in Chinese medicine to promote immune defence.

Always read the label and follow the directions for use.
Scan to find out more
Found exclusively behind the counter. Speak to your Pharmacist for specially formulated relief.
Finding balance:
how to prioritise your health and avoid extreme eating habits

EATING A NUTRITIOUS, NOURISHING DIET IS CRITICAL TO KEEPING HEALTHY, HOWEVER, IT CAN BE CONFUSING KNOWING EXACTLY WHAT CONSTITUTES HEALTHY EATING AND WHAT DOESN’T, PARTICULARLY WHEN IT COMES TO DIETING. DIETING IS OFTEN SEEN AS A QUICK FIX FOR WEIGHT LOSS AND IMPROVED HEALTH, AND WHILE SOME CAN BE EFFECTIVE, OTHER DIETS CAN DO MORE HARM THAN GOOD TO YOUR HEALTH. UNDERSTANDING THE DIFFERENCE BETWEEN UNSAFE DIETING, AND SAFE, SUSTAINABLE EATING, CAN HELP YOU STAY NUTRITIONALLY BALANCED AND NOURISHED.
WARNING
PLEASE BE AWARE THIS ARTICLE DISCUSSES EATING DISORDERS WHICH SOME READERS MAY FIND UPSETTING.
14
Be aware of the risks
Nutrient deficiencies: Many diets are very restrictive, eliminating entire food groups or severely limiting calorie intake. While this may lead to weight loss in the short term, it can also result in nutrient deficiencies over time.1 For example, a low-carbohydrate diet may limit fruits, whole grains and other carbohydrate-rich foods which are important sources of vitamins, minerals, and fibre. A low-fat diet may limit healthy fats which are important for brain function, hormone production and other bodily functions.
Slowed metabolism: When you drastically reduce calorie intake or eliminate entire food groups, your body may respond by slowing down its metabolism to conserve energy. This can make it more difficult to lose weight over time and may lead to weight gain if you return to your previous eating habits.2
Disordered eating: Some diets can trigger disordered eating patterns, such as yo-yo dieting, or obsessing over food and weight.3 This may increase the risk of developing eating disorders as it can lead to binge eating and purging, which are symptoms of conditions such as anorexia and bulimia, or orthorexia which is diagnosed obsession with the quality of food.
Negative body image: When you focus on weight loss as the goal, you may start to view your body as a problem which needs to be fixed rather than appreciating it for what it is.3 This can lead to feelings of shame, guilt, lack of self-esteem, and anxiety around food.
Weight cycling: Yo-yo dieting, or weight cycling, is a common result of fad diets or other extreme weight loss methods. When you lose weight quickly, you may also regain it quickly once you return to your previous eating habits.2 This cycle of weight loss and gain can be harmful to your physical and mental health and could even increase the risk of chronic diseases such as heart disease and diabetes.
Managing your weight safely
Dieting may not be the best approach for managing your weight sustainably or improving your health. Here are some alternative ways to help you achieve your goals safely and effectively:
Focus on whole foods: Rather than eliminating entire food groups or severely restricting your calorie intake, focus on eating a variety of whole foods that provide essential nutrients and satisfy hunger. Choose fruits, vegetables, whole grains, lean proteins, and healthy fats to nourish your body and provide sustained energy throughout the day.4 Keeping these foods available in your home, if possible, makes it even easier to create nourishing meals. These meals provide a more nutritious platform on which to manage food intake and manage weight.
Practice mindful eating: Rather than obsessing over calorie counts or food restrictions, practise mindful eating techniques such as paying attention to hunger and fullness cues, eating slowly and without distraction, and savouring each bite.4 This can help with weight loss by helping you tune into your body's needs and avoiding overeating or binge-eating.
Be active: Regular physical activity is essential for weight loss and improved health. Find activities that you enjoy, such as walking, swimming, or cycling, and aim for at least four hours of moderateintensity physical activity each week.5
Embrace self-care: Rather than focussing solely on weight loss, think about taking care of your whole self. Make sure you get enough sleep, manage any stress, and do things which bring you joy and fulfillment.5 This can help you cultivate a positive relationship with food and your body, and can contribute to improved mental and physical health.
Avoid quick fixes: Quick-fix or rapid-weight-loss diets are often unsustainable, can lead to nutrient deficiencies, and may contribute to a cycle of weight loss and gain. Instead, focus on making gradual, sustainable changes to your eating and exercise habits which you can maintain over the long term.6
Dieting red flags include those that promise rapid weight loss, eliminate entire food groups, or encourage extreme calorie restriction. If a diet or weight loss program sounds too good to be true, it probably is. Additionally, diets that promote detox or cleansing regimens can be dangerous and may lead to nutrient deficiencies or other health problems.
Listen to your body: Your body is designed to tell you when you’re hungry or full, so give yourself permission to follow those cues. This can promote self-care and self-acceptance, contributing to improved mental and physical health. By encouraging a more positive relationship with food, it can help people to break free from disordered eating patterns.
Seek help: Rather than going it alone, ask friends, family, or healthcare professionals for help. This can keep you motivated and on track with your goals and can provide a source of accountability and encouragement.7 A therapist or registered dietitian can help you develop a healthier relationship with both food and your body, and provide guidance and support for achieving your goals.
Be aware of societal pressure: We’re all under pressure from the influence of diet culture and society’s prevailing body ideals. Media and advertising often promote unrealistic beauty standards, leading many individuals to believe that they must diet to achieve a certain body shape or size.8 This can lead to disordered eating patterns and negative body image, perpetuating a cycle of harmful dieting behaviours.
Consider other factors: While diet and exercise are important factors in weight management and overall health, it's important to acknowledge that genetics and environmental factors also play a role. Some individuals may have a genetic predisposition to certain health conditions or a particular body type, making weight loss more challenging.9 Environmental factors or economic factors, such as lack of access to healthy food options or opportunities for physical activity, can also affect the ability to adopt certain health habits.
1Micronutrients: https://www.who.int/health-topics/micronutrients#tab=tab_1
2How dieting might make some fatter: https://pubmed.ncbi.nlm.nih.gov/32099104/
3Disordered eating & dieting: https://nedc.com.au/eating-disorders/eating-disordersexplained/disordered-eating-and-dieting/
4Weight loss – a healthy approach: https://www.betterhealth.vic.gov.au/health/ healthyliving/weight-loss-a-healthy-approach
5How to lose weight safely; https://www.nhsinform.scot/healthy-living/food-andnutrition/healthy-eating-and-weight-loss/how-to-lose-weight-safely
6Weight loss and dieting; https://www.healthdirect.gov.au/weight-loss-and-dieting
7Weight management services; https://www.betterhealth.vic.gov.au/health/ healthyliving/weight-management-services
8Recognizing and resisting diet culture; https://www.nationaleatingdisorders.org/blog/ recognizing-and-resisting-diet-culture
9Genetic predictors of weight loss in overweight and obese subjects: https://www. ncbi.nlm.nih.gov/pmc/articles/PMC6656717/
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 15
From
pills to patches: exploring the range of contraceptive choices
CHOOSING THE RIGHT CONTRACEPTIVE METHOD IS AN ESSENTIAL ASPECT OF WOMEN'S REPRODUCTIVE HEALTH. WITH SEVERAL OPTIONS AVAILABLE, IT CAN BE CHALLENGING TO MAKE THE RIGHT DECISION, OR TO KNOW THE BENEFITS AND DRAWBACKS OF EACH OPTION. BELOW ARE SOME OF THE CONTRACEPTIVE OPTIONS YOU MAY CHOOSE, WITH INFORMATION ON HOW THEY MAY IMPACT YOUR HEALTH, AND HOW THEY MAY DIFFER.

16
It's important for women to understand the different types of contraception methods available, how they work, and their effectiveness. This will help to ensure that decisions are wellinformed and right for each individual.
Barrier methods
This method prevents pregnancy by physically blocking the sperm from reaching the egg. Examples of barrier methods include condoms, diaphragms, and cervical caps.
Condoms are an effective and affordable way to prevent both pregnancy and sexually transmitted infections.1 They are made of latex, polyurethane, or polyisoprene, and are available in both male and female versions. Used correctly, they can be up to 98% effective in preventing pregnancy and infections.
Diaphragms and cervical caps are placed inside the vagina and cover the cervix to prevent sperm from entering the uterus. They are not as effective as condoms and can be difficult to use correctly; they require fitting by a healthcare professional, and must be used with spermicide.2 A cervical cap is smaller than a diaphragm and can be left in place longer (around 72 hours, compared to about 30 hours for the diaphragm).
Hormonal methods
These release synthetic hormones which prevent ovulation, thus preventing the release of an egg from the ovaries. They also thicken cervical mucus, making it difficult for sperm to enter the uterus. Options include birth control pills, patches, injections, vaginal rings, and hormonal intrauterine devices (IUDs).
Birth control pills are a popular and effective method of contraception, but they must be taken at the same time every day. Some women experience side effects such as nausea, headaches, mood changes, and weight gain.1
Patches are thin beige stickers applied to the skin once a week. While easy to use, some women may experience skin irritation or other side effects. It can also be easy to make an error in applying the patch, and application error makes the patch significantly less effective.
The contraceptive injection is administered every three months. It is a convenient option for women who don't want to worry about daily or weekly contraceptive methods, but it may cause irregular periods and weight gain.
Vaginal rings are flexible and transparent and are inserted into the vagina once a month. They are easy to use, but some women experience vaginal irritation or other side effects.
Hormonal IUDs are small, T-shaped devices which are inserted into the uterus by a healthcare professional. They offer a long-lasting and effective method of contraception, and brands can last up to five years. Hormonal IUDs may also reduce menstrual bleeding and cramping, but some women experience side effects such as irregular bleeding, cramping, or infection.
Intrauterine devices (IUDs)
These are sometimes also called ‘the coil’. In addition to the hormone-releasing version, other versions stop the sperm and egg from surviving in the womb or fallopian tubes, or stop a fertilised egg from implanting. Copper IUDs release copper ions which alter the way sperm move and prevent them swimming towards an egg. An IUD requires a prescription and is put in place by a doctor or nurse. They are effective and long-lasting, with some brands lasting up to 10 years.3 However, some women experience heavier periods or cramping.
Sterilisation
This is a permanent way to prevent pregnancy, involving either surgery to cut or seal the fallopian tubes, or a non-surgical method which uses a device to block the fallopian tubes. Sterilisation is highly effective, with a failure rate of less than 1%.4 However, it is important to note that it cannot easily be reversed.
Fertility awareness
This involves tracking the menstrual cycle to identify the fertile window when a woman is most likely to conceive. Methods include checking the basal body temperature, cervical mucus observation, or a combination of both.5 These methods require careful monitoring and education to be effective, and may not be suitable for women with irregular cycles or those who struggle to accurately track their cycle.5
Non-tracking methods include withdrawal, where a man removes (withdraws/pulls out) his penis from a woman’s vagina before he ejaculates. Withdrawal can be ineffective due to the presence of sperm in pre-ejaculate, which is not stopped with this method. Another method is lactational amenorrhoea method (LAM), which refers to using breastfeeding as a natural hormone disruptor. This can be highly effective if used correctly but due to the variance in instances of breastfeeding and post-partum hormone levels, this is far less effective six months after giving birth.
Emergency contraception
Emergency contraception (EC), sometimes referred to casually as ‘the morning-after pill’, is a form of contraception that can be used after unprotected sex to prevent pregnancy. The morning-after pill is most effective when taken within 72 hours, but it can be taken up to five days afterwards.1 Because it uses a large amount of hormones to prevent pregnancy, it’s not advised to use often, and should be relied upon as a last resort compared to other methods of contraception. This pill can be obtained from your local Blooms
The Chemist and doesn’t require a prescription.
Choosing the right contraceptive method is a personal decision which depends on individual preferences, health status, and lifestyle Your healthcare provider can talk to you about the benefits and risks of each method. It’s good to be able to make informed decisions and take control of your own reproductive health – although no contraceptive method is 100% effective.
1Contraception – choices: https://www.betterhealth.vic.gov.au/health/healthyliving/ contraception-choices
2Contraception: https://www.thewomens.org.au/health-information/contraception/ condoms-diaphragms
3Your contraception choices: https://www.thewomens.org.au/health-information/ contraception/your-contraception-choices
4Contraception options: https://www.healthdirect.gov.au/contraception-options
5Fertility awareness based methods of contraception, lactational amenorrhoea and withdrawal: https://www.fpnsw.org.au/health-information/contraception/fertilityawareness-based-methods-contraception-lactational
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 17
Endometriosis
ENDOMETRIOSIS IS A COMMON BUT OFTEN MISUNDERSTOOD CONDITION. UNDERSTANDING ITS CAUSES, SYMPTOMS, DIAGNOSIS AND TREATMENT IS VITAL FOR WOMEN’S HEALTH, AND HELPS TO IMPROVE PUBLIC AWARENESS – ESPECIALLY FOR SUPPORT IN THE WORKPLACE.

Endometriosis is a severe condition that affects up to 10% of reproductive-age women; around 190 million women worldwide and at least one in nine Australian girls, women and those assigned female at birth. Endometriosis occurs when tissue similar to the lining of the uterus, called the endometrium, grows outside of the uterus. This may lead to chronic, often extreme pain, discomfort and sometimes infertility. Management of the condition may include medical treatments, surgical treatments and complementary
treatments.3 The Australian government has recently acknowledged the historical lack of awareness, education, diagnosis, research, and treatment into endometriosis, with the ‘National Action Plan for Endometriosis’ released in 2023. The plan highlights the need to develop a more robust response to the management and treatment of the condition, with an emphasis on improving the quality of life for those affected by endometriosis.3
18
Causes
The exact cause of endometriosis remains unclear, and it is likely that genetic, biological, and environmental factors may influence the development of the condition.4 Some factors may increase the risk of developing endometriosis, including:
• ‘Retrograde menstruation’: If menstrual blood flows back through the fallopian tubes and into the pelvis, this can lead to the growth of endometrial tissue in the wrong places.4
• Movement of endometrial stem cells: If these cells move through the bloodstream or lymphatic system to other parts of the body, these parts could begin to grow and form endometrial tissue.4
• Cellular metaplasia: This refers to the ability of cells to change from one form to another, e.g., cells outside the uterus of change into endometrial-like cells and begin to grow.4
Symptoms
The symptoms of endometriosis can vary widely; some people may experience no symptoms at all. Common symptoms include:5
• Pelvic pain: This is the most common symptom and may occur before, during and/or after menstruation. The pain may be mild or severe and may worsen over time. Pain can also be present in the lower back or legs.
• Painful and/or heavy periods: Many women will experience pain during their period, which may be so debilitating they cannot participate in day-to-day activities including education, work or sport. Heavy bleeding or clotting, irregular bleeding, or bleeding for longer than ‘normal’ may also signal endometriosis.
• Pain during intercourse: Experiencing pain during intercourse, especially during deep penetration, can be another common symptom of endometriosis.
• Painful bowel movements or urination: Endometrial tissue may grow on the bowel or bladder, causing pain or changes to urination or bowel movements.
• Infertility: Endometriosis can cause scarring and adhesions in the pelvic area, which can make it difficult to conceive.
• Fatigue: Many women with endometriosis experience extreme tiredness with low energy levels.
Diagnosis
On average, it takes over seven years to get a diagnosis.6 Before that, 58% of sufferers will visit their GP at least 10 times, and over a quarter will go to the emergency room with severe symptoms. Unfortunately, many of those affected by endometriosis will not receive adequate support from their GP or gynaecologist.7
The diagnosis of endometriosis typically involves a combination of a physical exam, imaging tests, and possibly laparoscopy (keyhole surgery in the abdomen). If you suspect endometriosis, you will need to visit a GP to receive a diagnosis.
During the physical exam, the doctor will ask about your symptoms and medical history and may feel for any lumps or abnormalities in your pelvic area. Imaging tests such as an ultrasound or MRI may be used to detect the presence of endometrial tissue outside of the uterus.8
If the diagnosis is still unclear, a laparoscopy may be performed in a hospital setting. Under general anaesthetic, a small camera will be inserted through a small incision in your abdomen to examine your pelvic organs. A biopsy may also be taken to confirm the presence of endometrial tissue beyond the uterus.
Treatments
Treatment for endometriosis depends on the severity of the symptoms and the desire for fertility. Mild cases may be managed with pain relievers and hormone therapy to suppress the menstrual cycle.8 More severe cases may require surgery to remove the endometrial tissue and any adhesions.
These surgical procedures can include laparoscopy, laparotomy (a larger incision), and/or hysterectomy (removal of the uterus).9 Unfortunately, even the removal of the uterus means the condition may still return, as endometrial tissue can continue to grow in other parts of the body.
Managing endometriosis
In addition to medical treatments, there are several steps that may manage symptoms and improve overall health and well-being. These include:4
• A healthy diet: Inflammation can exacerbate the symptoms of endometriosis. A diet that is rich in fruits, vegetables and whole grains can help to reduce inflammation in the body.
• Regular exercise: This can help to reduce stress, manage your symptoms, and improve your overall health.
• Stress management: Stress can exacerbate endometriosis symptoms, so practices such as meditation, mindfulness or yoga can be helpful.
• Pain management: Over-the-counter pain relief, such as ibuprofen or acetaminophen, can be helpful. In more severe cases, prescription pain medication may be necessary.
• Hormonal birth control: This can regulate your menstrual cycle and reduce the growth of endometrial tissue.
• Alternative therapies: Acupuncture, massage or herbal remedies can provide some relief for some, but you should always consult your healthcare provider before trying any alternative therapies.10
Living with endometriosis
Endometriosis can be a challenging condition to live with, but resources are available to help those affected manage their symptoms and improve their quality of life. The Endometriosis Association and the National Endometriosis Society offer information and support groups.
Additionally, many healthcare providers specialise in the treatment of endometriosis and can provide guidance and support in managing the condition. There are also several government programs designed to make life easier for those suffering with endometriosis through increasing awareness and developing potential treatments.2 These programs include over $87 million in funding, allocated as part of the ‘National Action Plan for Endometriosis’.
While endometriosis remains a severe condition, there are increasing resources dedicated to awareness and education. With advancements in research and technology, the aim is to develop better support and assistance and improve the quality of life for those affected by endometriosis.
1Endometriosis: https://www.who.int/news-room/fact-sheets/detail/endometriosis
2What we’re doing about endometriosis: https://www.health.gov.au/topics/chronicconditions/what-were-doing-about-chronic-conditions/what-were-doing-aboutendometriosis
3What is endometriosis: https://www.endometriosisaustralia.org/about-endo 4Montgomery et al, “The search for genes contributing to endometriosis risk,” Human Reproduction Update 14.5 (2008): 447-57.
5Endometriosis: https://www.healthdirect.gov.au/endometriosis
6Endometriosis: https://www.bbc.com/news/health-49897873
7Satisfaction with medical support in women with endometriosis: https://www.ncbi. nlm.nih.gov/pmc/articles/PMC6264517/
8Endometriosis: https://www.hopkinsmedicine.org/health/conditions-and-diseases/ endometriosis
9Treating endometriosis: https://www.thewomens.org.au/health-information/periods/ endometriosis/treating-endometriosis
10Endometriosis & natural therapies: https://www.jeanhailes.org.au/health-a-z/ natural-therapies-supplements/endometriosis-natural-therapies
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 19
Rushing woman’s syndrome
IN TODAY’S FAST-PACED WORLD, IT CAN BE CHALLENGING TO KEEP UP WITH THE DEMANDS OF WORK, FAMILY, AND PERSONAL LIFE. WOMEN, IN PARTICULAR, ARE OFTEN EXPECTED TO BALANCE MULTIPLE ROLES AND RESPONSIBILITIES, WHICH CAN LEAD TO A STATE OF CONSTANT STRESS AND ANXIETY.

20
Women typically bear the brunt of managing the household and family commitments, along with their own personal and work lives. All this juggling can lead to ‘rushing woman’s syndrome’, a term coined by Dr Libby Weaver, a nutritional biochemist and author. It can have a significant impact on women’s physical and mental health, including a state of chronic stress.1
Women who suffer from this condition often feel like they’re in a constant rush, with little time for self-care or relaxation. They may also experience physical symptoms such as fatigue, weight variance, and disrupted sleep patterns.
It’s important to note that rushing woman’s syndrome is not a medical diagnosis, but rather a term used to describe a collection of symptoms.1
The causes
Many factors contribute to rushing woman’s syndrome. One of the primary drivers is societal expectations around work, family, and personal appearance. Women are often expected to excel in their careers while also maintaining a happy home life and perfect appearance. This pressure can lead to a sense of being overwhelmed and not being able to keep up.2
Another factor is the pace of modern life. With smartphones, social media, and other technologies, it can be challenging to switch off from work and personal demands.2 This constant stimulation can lead to a state of hyper-vigilance, where women feel like they need to be ‘on’ all the time.3
The impact of hormones
Hormones can play a significant role in the development of rushing woman’s syndrome. Women may have imbalances of cortisol, oestrogen, progesterone, and thyroid hormones, for example.3
Cortisol is a hormone released by the adrenal glands in response to stress. When cortisol levels are constantly elevated, it can lead to a range of negative health outcomes, including weight gain, mood swings, and disrupted sleep patterns.4
Low levels of oestrogen can lead to a decrease in bone density, while imbalances in progesterone can lead to mood swings and anxiety. Thyroid hormones play a crucial role in regulating metabolism, energy levels, and mood. Imbalances can lead to fatigue, weight gain, and mood swings.5
These hormones are designed to help us cope with acute stress, but when they are constantly elevated, they can lead to a range of negative health outcomes.
The effects
One of the most common symptoms of rushing woman’s syndrome is fatigue. Women who are always in a rush may not be getting enough sleep or expending too much energy throughout the day. This can lead to exhaustion, which can make it challenging to perform well at work, feel energised or supported in their family life, or engage in enjoyable activities outside of work.6
Weight gain is another common symptom, especially around the midsection. When stress hormones are constantly elevated, they can lead to an increase in appetite and a decrease in metabolism.6
The syndrome can also cause physical symptoms such as headaches, muscle tension and gastrointestinal issues. Women may also feel less able to concentrate, and like they are constantly in a state of mental fog.3
Mood swings and irritability may also occur as a result of rushing woman’s syndrome. When stress hormones are elevated, they can impact our emotional regulation, leading to feelings of anxiety, anger, or depression. Women may find themselves snapping at loved ones or feeling like they are on an emotional rollercoaster. Finally, there’s the effect on women’s sexual health. When stress hormones are elevated, they can impact libido and sexual function, leading to decreased desire and difficulty achieving orgasm.
Managing the syndrome
Fortunately, there are steps that women can take to manage rushing woman’s syndrome and improve their overall health and wellbeing. One of the most important of these is prioritising selfcare. This means taking time each day to engage in activities that promote relaxation and stress reduction, such as meditation, yoga, or deep-breathing exercises.6
Another important step is to set boundaries around work and personal time. This means being intentional about when you check your email or respond to work-related messages, and setting aside time each day for activities that bring you joy and relaxation.3
Women may also benefit from speaking to a mental health professional. Therapy can help identify patterns of thought and behaviour which contribute to stress and anxiety, and help us develop strategies for managing those patterns in a healthy and productive way.
In addition to these individual steps, there are also broader societal changes that could help support women who feel overwhelmed. This includes promoting flexible work arrangements for a better work/life balance and reducing the stigma around mental health issues.
For more information on rushing woman’s syndrome, visit drlibby.com
1Rushing woman’s syndrome: https://shop.drlibby.com/product/rushing-womanssyndrome?v=13b249c5dfa9
2Gender role perspectives and job burnout: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC8375289/
3Do you have rushing woman’s syndrome?: https://www.womenshealth.com.au/doyou-have-rushing-womans-syndrome/
4High cortisol levels in women and negative effects on the body: https://www. womenshealthnetwork.com/adrenal-fatigue-and-stress/negative-effects-of-highcortisol/
5Thyroid gland: https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/ thyroid-gland
6Don’t dismiss rushing woman’s syndrome; https://www.smh.com.au/lifestyle/dontdismiss-rushing-womans-syndrome-20140617-zsaqb.html
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 21
Getting enough sleep
SLEEP IS AN ESSENTIAL MARKER OF HEALTH FOR EVERYONE, HOWEVER, RESEARCH HAS SHOWN THAT SLEEP DIFFERS BETWEEN MEN AND WOMEN. WE ALL NEED ENOUGH REST FOR OPTIMAL HEALTH, BUT THERE ARE SEVERAL SIGNIFICANT DIFFERENCES BETWEEN HOW MEN AND WOMEN SLEEP.

22
One of the most notable differences in sleep between men and women is the amount of time they spend sleeping. Women generally require slightly more sleep than men, requiring an average of around 11 minutes more sleep per night because they tend to have more complex brain activity during sleep.1
Additionally, women are more likely to have their sleep disrupted:
• During the menstrual cycle, progesterone levels rise and can make women feel sleepier than usual. On the other hand, before their period, oestrogen levels will drop – leading to difficulty falling or staying asleep.2
• Pregnancy can cause difficulty sleeping during the later stages due to discomfort and the need to urinate frequently.3
• Breastfeeding, or ongoing primary responsibility for childcare, can lead to late nights, frequent awakening and a lack of control over sleep.
• During menopause, significant drops in oestrogen levels can lead to night sweats and other sleep disturbances. These can continue for several years after menopause.2
Disrupted sleep
Women are also more likely to suffer from sleep disorders than men. One of the most common sleep disorders in women is insomnia. This is characterised by difficulty falling or staying asleep, and is often associated with anxiety, stress, or depression. Women are twice as likely as men to suffer from insomnia, and it tends to be more severe among women.4
Restless leg syndrome is a neurological disorder that causes uncomfortable sensations in the legs, which can make it difficult to fall or stay asleep. Women are twice as likely as men to develop it, and the condition is more common during pregnancy.3
One significant factor that contributes to differences in sleep between men and women is hormonal fluctuations. Hormones such as oestrogen and progesterone can affect sleep patterns, particularly in women.5
In addition to hormonal fluctuations and sleep disorders, women's sleep can also be affected by lifestyle choices.5 For example, women who smoke or consume alcohol are more likely to experience sleep disturbances than men who do the same. Additionally, women who work night shifts or irregular hours are at an increased risk of developing sleep problems.
Cultural and societal expectations can affect how men and women sleep. For example, women are often expected to be caregivers for their families, which can lead to a lack of time for self-care and adequate sleep.6 Similarly, societal expectations for men to be breadwinners or to work long hours can contribute to sleep disruptions and a lack of restful sleep.
Different types of sleep
While women may need more sleep than men, men tend to experience a different type of sleep. Men spend more time in deep sleep, which is essential for physical recovery and regeneration and is therefore typically more restorative. Men also tend to wake less often during the night, so they feel more rested in the morning. However, men are twice as likely to develop sleep apnoea, a disorder which causes breathing to stop and start repeatedly during sleep. It can lead to snoring, daytime sleepiness, and other health problems if left untreated. It is more common in older men who are overweight or obese.7 This may also impact the sleep of women who share a bedroom with a snoring partner,
What can you do to improve your sleep?
• Stick to a regular sleep schedule: Try to go to bed and wake up at the same time every day, even on weekends.
• Create a relaxing bedtime routine: Take a warm bath, read a book, or listen to calming music to help your body and mind relax before bedtime.
• Create a sleep-positive environment: Make sure your bedroom is dark, temperature-adjusted, and quiet.
• Avoid stimulating activities before bedtime: Don’t use electronic devices such as phones or tablets, exercise, or eat a large meal.
• Avoid caffeine and alcohol: Caffeine and alcohol can disrupt sleep, so it's best to avoid them in the lead up to bedtime.
• Get regular exercise: This can promote better sleep by decreasing the time it takes to fall asleep, potentially lowering your time spent lying awake at night, and reducing the risk of sleep apnoea. However, be careful if you’re planning to complete vigorous exercise right before you go to bed; post-exercise adrenaline may prevent you from falling asleep easily.
• Manage stress: Finding ways to manage stress, such as meditation, yoga, or deep breathing, can help improve sleep quality.
• Seek treatment: If you suspect you have a sleep disorder, such as insomnia, sleep apnoea or restless leg syndrome, seek medical attention for confirmation and treatment.
• Prioritise sleep: Recognise the importance of sleep and prioritise it in your daily routine. Avoid sacrificing sleep for work or other activities, as chronic sleep deprivation can have serious health consequences.
If you have concerns about your sleep quality, or suspect you or someone close to you may have sleep apnoea, chat to your local Blooms The Chemist Pharmacist about improving your sleep health.
1Do women need more sleep than men?: https://www.sleepfoundation.org/womensleep/do-women-need-more-sleep-than-men#references-175668
2Sleep and women’s health: https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC4327930/
3How is sleep different for men and women?: https://www.sleepfoundation.org/howsleep-works/how-is-sleep-different-for-men-and-women
4Insomnia and women: https://www.sleepfoundation.org/insomnia/insomnia-women
5Exploring sex and gender differences in sleep health: https://pubmed.ncbi.nlm.nih. gov/24956068/
6Menstrual cycle and sleep: https://www.sleephealthfoundation.org.au/pdfs/ Menstrual-Cycle-and-Sleep.pdf
7How to get better sleep, according to science: https://www.healthdirect.gov.au/blog/ how-to-get-a-good-nights-sleep
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 23
Put mindyour at ease

Herbs of Gold Mind Ease contains KSM-66®, a clinically trialled Ashwagandha extract to relieve symptoms of mild anxiety.*
Always read the label and follow the directions for use.

24
*Chandrasekhar, K. et al.
Indian J Psychol Med, 34(3), 255-62. Life’s golden formula With KSM-66® Ashwagandha
(2012).
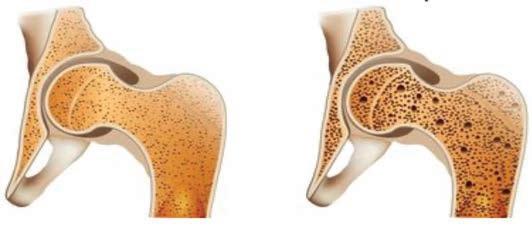
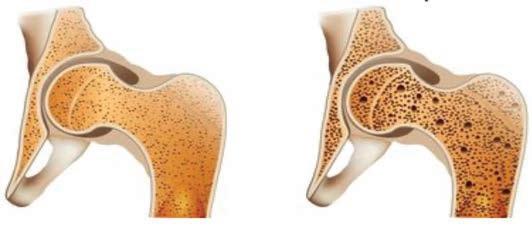
What is osteoporosis?
OSTEOPOROSIS IS LOSS OF BONE STRENGTH, MAKING BONES MORE FRAGILE AND MORE PRONE TO FRACTURE. LEARN MORE ABOUT OSTEOPOROSIS, OSTEOPENIA, COMMON PLACES IN THE BODY FOR FRACTURE, AND RATES OF OSTEOPOROSIS IN AUSTRALIA.
Reproduced with permission from Jean Hailes.
About bone strength
Normal bone is made up of a mixture of calcium and other minerals including magnesium and phosphate. Normal bone also contains collagen, a protein that forms the physical framework of bone. Bone is constantly being broken down and renewed. During childhood more bone is made than broken down. Just after puberty (about 15-17 years) 90% of bone growth is complete and there is only a small increase in bone strength after this age until the age of 30. From our mid 30s onwards, more bone is broken down than made. This results in a gradual decrease in bone strength as we age. Hormones such as oestrogen play a role in maintaining bone strength. When women go through menopause there is a significant fall in oestrogen (up to 90%). This means there is rapid bone loss in the years immediately after menopause. However, the rate of loss slows 4-8 years after menopause.
With osteoporosis bones become thinner, and in severe cases even a minor bump can cause a fracture (break or crack). Any bone can be affected by osteoporosis, but the most common sites are the:
• hip
• spine
• wrist
• ribs
• pelvis
• upper arm.
Often, there are no signs or symptoms of osteoporosis until a fracture occurs.
Some women develop osteoporosis early because of illness or hormonal deficiencies.
What is osteopenia?
Osteopenia is essentially lower bone density, where bones have lost some mass and strength. In osteopenia the bone density is between normal bone density and osteoporosis. A woman with osteopenia has a risk of broken bones that is higher than normal, but not as high as with the more severe effects of osteoporosis.
Osteoporosis in Australia
Nearly two million Australians (approximately 10% of the population) currently have an osteoporosis-related condition, and three quarters of these are women:


• After age 60, 1 in 2 Australian women will have a fracture related to osteoporosis
• Of all osteoporotic fractures in Australia, almost half are vertebral (bones in the spinal column) followed by fractures of the hip and wrist

Hip fractures are a particular problem, with evidence showing a decline in health after a hip fracture:
• 50% of elderly people will need long term nursing care
• The risk of mortality increases with hip fractures with up to 15% leading to death within 4 months of the fracture1
Osteoporosis
Osteoporosis is a condition that results in loss of bone strength, making bones more fragile and more prone to fracture. It occurs when bones lose minerals, like calcium, more quickly than the body can replace them. This leads to loss of bone thickness (also called bone mass or density). This is a normal part of ageing for everyone.
With our increasing life expectancy the rate of osteoporosis is likely to increase over the next few years, and up to 13% of the Australian population will be affected by osteoporosis.
To find out more and understand what you can do to optimise your bone health, visit jeanhailes.org.au/health-a-z/bone-health.
We also recommending speaking to your GP if you have any questions or concerns about osteoporosis and osteopenia.
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 25
Childhood to puberty is a critical time for developing peak bone mass By early 20s peak bone mass is reached After our 20s more bone is lost than made In menopause
is a
decline in
mass As
there
rapid
bone
we age we continue to lose bone mass and strength
Normal bone
Osteoporosis



26 make a positive difference for you & your baby PRE POST DURING Always read the label and follow the directions for use. Natalis is a proud supporter and in a paid partnership with Australian College of Midwives. Arrotex Pharmaceuticals, 15-17 Chapel St, Cremorne VIC 3121. ABN 30 605 552 234. The Arrotex and Natalis trade marks are used under licence. Copyright@May 2023. All rights reserved. CON-0038 NEW LOOK
Brauer’s Calm & Sleep Range




A range of convenient stress relief products to suit your lifestyle
Calm Range
Contains ingredients traditionally used in Homeopathic medicine to relieve symptoms of stress & mild anxiety

A range of convenient bedtime products to suit your lifestyle
Ingredients to help you own the night
Easy-to-take liquid, oral sprays, and tablets for a no-fuss night-time ritual
Non-drowsy formulas, so you can get on with your day

Easy-to-take liquid, oral spray, and tablets for on-the-go stress relief
Sleep Range
Contains ingredients traditionally used in Homeopathic medicine to relieve sleeplessness & restless sleep


Always read the label and follow the directions for use.

HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 27
3 3 3 3 3 3
Understanding our reproductive hormones
HORMONES ARE CHEMICALS WHICH CONTROL AND REGULATE OUR BIOLOGICAL PROCESSES – AND THEREFORE MANY ASPECTS OF OUR HEALTH. THIS ARTICLE EXPLORES THE KEY FEMALE REPRODUCTIVE HORMONES: WHAT THEY DO, AND THE EXTENT TO WHICH THEY CAN IMPACT ON OUR PHYSICAL, MENTAL, AND EMOTIONAL HEALTH.

28
Hormones are chemical messengers produced by glands and organs in the endocrine system. They manage growth and development, metabolism, mood, and reproduction, and are therefore critical to the functioning of our bodies.
There are over 50 hormones; you may have heard of insulin, adrenaline, melatonin, and thyroxine, for example. But quite a few are involved in reproduction, and the main female hormones are oestrogen, progesterone, and testosterone.1
Female reproductive hormones
Oestrogen is produced primarily in the ovaries and plays a key role in the development and regulation of the reproductive organs and secondary sex characteristics (such as pubic hair).2 It also helps maintain healthy bones and regulates cholesterol levels. Oestrogen has three major forms:3
• Oestrone, which is made after menopause4
• Oestradiol, the most potent form, which is made during the reproductive years
• Oestriol, the primary form during pregnancy
Progesterone is produced mainly in the ovaries and the adrenal glands, and is essential for maintaining menstruation and healthy pregnancy.5 Testosterone is not an exclusively male hormone. In women, it is produced in the ovaries, adrenal glands and peripheral tissues and is responsible for maintaining muscle mass, bone density and libido.6
The menstrual cycle
This is a complex process, regulated by reproductive hormones. It is divided into four phases,7 each characterised by different hormone levels and physical changes in the body:
• The follicular phase begins on the first day of menstruation. The pituitary gland produces follicle-stimulating hormone (FSH), which stimulates the growth of follicles and eggs in the ovaries. As they grow, they in turn produce increasing amounts of oestrogen. This oestrogen causes the lining of the uterus (the endometrium) to thicken and become blood-rich, so that any fertilised egg could implant there and develop. The oestrogen also triggers the release of luteinising hormone, which is needed in the next phase. This follicular phase lasts around 14 days.
• The ovulatory phase lasts one day. Luteinising hormone causes the biggest follicle to release its egg – this is called ovulation. The egg travels down the fallopian tube towards the uterus. If it is fertilised by a sperm, the egg implants in the thickened uterine wall and pregnancy begins. If fertilisation doesn't occur, then both the egg and the uterine lining are shed during the final menstrual phase.
• The luteal phase begins after ovulation and lasts around 14 days. The follicle which released the egg transforms into a corpus luteum, a small temporary cyst which produces progesterone. Like oestrogen, progesterone helps thicken the uterine wall in preparation for pregnancy, but it also inhibits contractions – thereby preventing miscarriage – and stops the body’s immune system from rejecting the foetus as a perceived foreign body. If pregnancy doesn’t occur, the corpus luteum disintegrates and hormone levels drop, triggering the start of the next phase.
• The menstrual phase is the shedding of the uterine lining and occurs approximately every 28 days. It lasts anywhere from three to seven days and involves the discharge of blood and other materials from the uterus. During this phase, hormone levels are low, and the body is beginning to prepare for the whole cycle to repeat.
Hormonal imbalances
Hormone imbalances can cause a variety of health problems in women:
Low oestrogen can lead to irregular periods, hot flushes, and vaginal dryness.2 It can also increase the risk of osteoporosis, where bones
become weak and brittle. High levels of oestrogen, on the other hand, can increase the risk of breast and uterine cancer.8
Low progesterone can cause irregular periods, heavy bleeding, and mood swings, as well as increased risk of miscarriage and pre-term birth.9
Low testosterone can lead to decreased sex drive, irregular periods, acne, and unwanted hair growth.6
High follicle-stimulating hormone can damage the ovaries and reduce the chances of getting pregnant.10
Low luteinising hormone can also cause fertility problems.10
Hormone imbalances can have various underlying causes, from stress and poor nutrition to certain medical conditions. While oestrogen levels fluctuate throughout life, particularly during puberty, pregnancy, and menopause, you should consult your healthcare provider if you experience any of the above symptoms.11
Common reproductive hormone therapies
Birth control pills: These contain synthetic versions of oestrogen and progesterone, and they can prevent ovulation (thus avoiding pregnancy) and regulate the menstrual cycle. They can also improve acne and reduce the risk of ovarian and endometrial (uterine) cancer. However, they can have side effects such as nausea, headaches and mood changes.12 You should discuss the risks and benefits with a healthcare provider, such as your local Blooms The Chemist Pharmacist.
Menopausal hormone therapy: This is used to alleviate symptoms of menopause, the process by which a woman’s fertility and reproductive cycle come to an end, typically between the ages of 45 and 55. During menopause, oestrogen and progesterone levels decrease, leading to over 30 symptoms – common ones include hot flushes, night sweats, dry skin and mood changes.3 MHT contains synthetic versions of oestrogen and/or progesterone to relieve these symptoms. However, MHT may not be appropriate for everyone, such as those with a family history of breast or ovarian cancer, a history of blood clots, or those with hypotension. Consult your doctor to learn if this may be appropriate for you.
Lifestyle changes can also help to regulate hormones and improve overall health. A balanced diet rich in fruits, vegetables, whole grains, and lean protein can help to regulate hormone levels and prevent chronic diseases such as heart disease and diabetes. Regular exercise can also help, along with stress management techniques such as yoga, meditation, and getting enough sleep.13
1How do female sex hormones affect menstruation, pregnancy, and other functions?: https://www.healthline.com/health/female-sex-hormones
2Oestrogen: https://www.healthdirect.gov.au/oestrogen
3Estrogen: https://my.clevelandclinic.org/health/body/22353-estrogen
4Oestrone: https://www.yourhormones.info/hormones/oestrone/
5Physiology, progesterone: https://www.ncbi.nlm.nih.gov/books/NBK558960/
6Testosterone and women; https://www.menopause.org.au/health-info/resources/ testosterone-and-women
7The normal menstrual cycle and the control of ovulation: https://www.ncbi.nlm.nih. gov/books/NBK279054/
8Breast cancer and oestrogen: https://www.betterhealth.vic.gov.au/health/ conditionsandtreatments/breast-cancer-and-oestrogen
9Everything you need to know about progesterone: https://www.healthline.com/health/ progesterone-function
1010 warning signs you may have a hormonal imbalance : https://hormonehealth. co.uk/10-warning-signs-you-may-have-a-hormonal-imbalance-and-what-to-do-about-it
11Hormones: a balancing act?; https://www.jeanhailes.org.au/news/hormones-abalancing-act
12Contraceptive pills: https://www.thewomens.org.au/health-information/ contraception/contraceptive-pills
13Effect of physical activity on sex hormones in women: https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC4635995/
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 29
shake up how you live
Active skin protection

Odour neutraliser
For light to moderate bladder weakness



30
MoliCareAustralia
BUY NOW
BRING BACK YOUR BAJINGO!
BRING IT BACK
SAY BYE-BYE TO VAGINAL
DRYNESS AND DISCOMFORT

KEEP IT THERE
MAINTAIN YOUR VAGINAL PH
Available at your local pharmacy

ALWAYS READ THE LABEL AND FOLLOW THE DIRECTIONS FOR USE
Returning to work
WITH MANY WOMEN TAKING BREAKS IN THEIR CAREER TO CARE FOR LOVED ONES, SPEND TIME TRAVELLING OR SIMPLY TAKING TIME TO REASSESS THEIR CHOSEN CAREER OR PRIORITIES, RETURNING TO THE WORKPLACE AFTER AN EXTENDED PERIOD CAN BE A SOURCE OF ANXIETY AND STRESS. WE OUTLINE SOME STRATEGIES THAT MAY HELP EASE THE TRANSITION BACK TO WORK.

32
Some people may experience challenges when returning to the workplace, including feeling less confident in their abilities, worry about taking time away, and physically adapting to traditional working hours.1
Finding a new job
Looking for a new job after taking time off from your career can be intimidating but is becoming increasingly normal. Workplace customs become more flexible due to virtual technologies and the growth in working from home.2 Even so, there are ways to help boost your confidence and help your return to work.
Update your skills: Even if you've been away from work for a while, don't underestimate the value of your experience. Take charge of your career and assess your current skillset to identify any areas where you can grow. Read industry journals and publications to get a feel for market trends, and try to attend inspiring conferences or training events, or enrol in online courses to ensure your skillsets and qualifications align to current industry preferences. By investing in yourself and your skills, you'll not only become a more desirable candidate to potential employers, but you'll increase your confidence and competence in your field.
Update your CV and cover letter: Showcase your unique story, express your enthusiasm for a job and demonstrate how your skills and experiences align with the role by ensuring your CV and cover letter reflect your current experience. It’s advisable to tailor your application materials to each job you’re applying for, and remember, honesty is key, so don't be afraid to share how your time off has helped you develop new skills or perspectives. Highlight any relevant experiences, such as volunteering or caregiving, to show potential employers the value of your time away. Remember, you bring a wealth of knowledge and expertise to the table, and your individual story can set you apart from other candidates.
Prepare for interviews: Whether it's been a while since your last interview or you're feeling nervous, you can take charge of the situation by preparing ahead of time. Start by researching the company and the role and familiarise yourself with common interview questions. Then, showcase your skills and accomplishments by preparing examples of your past work. Recalling past interviews where you were successful can help to quiet any negative or anxious thoughts about the outcome. If you're doing a virtual interview, test your technology beforehand and find a quiet, distraction-free space to conduct the interview.
Network: It can be an introvert’s worst nightmare, but networking is a crucial aspect of job hunting, regardless of your background or circumstances. By reaching out to former colleagues, mentors, and friends in your industry, you can expand your network and potentially find new career opportunities. Consider attending industry events, joining professional organisations, and participating in online forums and groups to connect with like-minded individuals and stay up-todate on the latest industry trends. Building a network can also provide valuable insights and advice from individuals who have been in your shoes. Remember, networking is a powerful tool that can open doors and help you achieve your career goals. Take control of your job search and build connections that will support your success.
Ask for what you are worth: Negotiating your salary is a crucial step in advocating for fair pay and advancing your career. Women, in particular, may face challenges in securing equal pay for equal work.3 Returning to work after a break can also add complexity to the negotiation process. However, it's essential to advocate for yourself and negotiate a salary that accurately reflects your skills and experience. Start by researching typical salaries for your role and industry and be prepared to articulate why you deserve a certain salary based on your expertise. Remember, negotiating your salary is a sign of confidence and self-respect. By speaking up and asserting your value, you'll not only benefit yourself, but also help pave the way for greater equality in the workplace.
Returning to a previous role
Returning to the same workplace after an extended period can be just as stressful as searching for a new role. By making adjustments both in and out of the workplace, you can ease this transition and help manage this new stage of your career.
Be flexible: If you’re juggling new responsibilities and routines at home, you may need to adjust your working hours or negotiate flexible working arrangements, such as working from home or parttime hours. Being open to different options may lessen any anxiety and result in a solution that works for both you and your employer. This may require some compromise and negotiation, but ensure you find a work-life balance that suits you and your needs.
Prioritise self-care: It's normal to feel overwhelmed or anxious during this transition, so ensure you prioritise your own health. When possible, take breaks throughout the day to reset, practise mindfulness or meditation, and make time for activities that bring you joy and relaxation. Remember, self-care is not selfish – it's essential for your overall wellbeing, as well as your work performance.4
If you feel the need to talk to someone about your experiences, don't hesitate to seek support from a therapist or support group. By taking care of yourself and seeking support when needed, you can navigate this transition with greater ease and confidence.
Build a support system: Having a supportive network can be incredibly helpful in your career success. Returning to work can sometimes feel isolating, especially if you're the only one in your workplace who has taken a break.5 This can be heightened by work-from-home environments. Building a network of family, friends, and colleagues who understand your journey and can offer guidance, encouragement, and support can make a significant difference. Consider joining a women's professional network or a career support group for women returning to work as another great option. Surrounding yourself with a supportive community can help you overcome obstacles and achieve your goals.
Set realistic goals: Encouraging yourself with realistic goals can help you maintain motivation and build momentum as you return to work. Break down your role and career goals into smaller, achievable steps, focussing on one step at a time. Celebrate each accomplishment, no matter how small it may seem. Setting achievable goals can help you feel a sense of accomplishment and progress, and help you stay positive and continue to develop in your career. Remember that your goals can extend beyond work and may include personal or family priorities.
It’s important to be kind to yourself and maintain a positive attitude during your return-to-work journey. Remember that finding the right job or adjusting to a new routine may take time, but with persistence and patience, you'll get there. Don't forget to celebrate small successes along the way, such as reconnecting with colleagues or receiving positive feedback on your work. It's important to avoid comparing your current achievements to those from before your break, as this can lead to unnecessary pressure and self-criticism. Embrace the journey, stay focussed on your goals, and take pride in your progress.
1Returning to work: https://www.womeninresearch.org.au/returning-to-work
2The future of flexible work: https://www.hrpartners.com.au/career-advice/archives/ the-future-of-flexible-work_950/
3Gender pay gap data: https://www.wgea.gov.au/pay-and-gender/gender-pay-gap-data
4Self-care at work matters: https://journals.copmadrid.org/jwop/art/jwop2022a15
5Lost connections: https://newscentre.vodafone.co.uk/app/uploads/2021/05/LostConnections-2021-180521-Pages-Web-1-1.pdf
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 33








34
hormoneMenopausaltherapy factsheet
A JEAN HAILES ARTICLE
IF MENOPAUSAL SYMPTOMS ARE AFFECTING YOUR QUALITY OF LIFE, IT’S IMPORTANT TO GET HELP. SYMPTOMS MAY INCLUDE HOT FLUSHES, NIGHT SWEATS, ACHES AND PAINS, VAGINAL DRYNESS AND MOOD CHANGES. THERE ARE MANY WAYS TO MANAGE YOUR SYMPTOMS, BUT NO OTHER TREATMENT HAS BEEN SHOWN TO BE AS EFFECTIVE AS MENOPAUSAL HORMONE THERAPY (MHT).


What is MHT and how does it help?
MHT is the replacement of female hormones oestrogen and progesterone, and sometimes testosterone. This hormone therapy must be prescribed by your doctor. MHT helps to reduce menopausal symptoms that are caused by lower levels of oestrogen hormones before and after menopause. MHT may also help to reduce health risks such as osteoporosis and heart disease.
Is MHT safe?
A recent review of evidence on MHT found it is a safe and effective treatment for the relief of menopausal symptoms for healthy women. The data showed that MHT had low risks for women aged between 50 and 60 years, or when used within 10 years of their final period. There may be some risks associated with MHT, depending on your individual situation. For example, your age, medical history, family history, when the medication is started, how long you use it, and the type and dose of medication taken.
The risk of blood clots, stroke or breast cancer due to taking MHT is small but may increase if you have other risk factors, such as smoking or being overweight.
Possible side effects
Everyone responds differently to MHT. Some women may not experience any side effects, while others might have symptoms such as nausea, fluid retention, vaginal bleeding or sore breasts. Most symptoms settle within the first three months.
Who should not use MHT?
It’s recommended you do not start MHT if you are older than 60 years old or if you’ve been postmenopausal for 10 years or more. MHT is not recommended if you have had hormone-dependent cancer. Your doctor may also advise you not to use MHT if it could increase your health risks, for example, if you have undiagnosed vaginal bleeding or heart disease.
TYPES OF MHT Oestrogen and progesterone
Oestrogen is the main hormone prescribed to relieve menopausal symptoms. If you’ve had a hysterectomy, oestrogen may be all you need. If you haven’t had a hysterectomy, oestrogen and progesterone are used together, as progesterone reduces the risk of endometrial cancer (cancer of the uterus). Your doctor may also recommend different combinations of oestrogen and progestogen (including progesterone and other progesterone-like hormones).
Vaginal oestrogen can be used in the form of a cream, pessary or tablet to help treat vulvovaginal atrophy (changes to the vaginal and vulval tissue), dry vagina and pain during sex.
Tibolone
Tibolone is a synthetic hormone that has oestrogen, progesterone and testosterone effects. Some women find Tibolone helps with menopausal symptoms and mood. It may also help with libido (sexual desire), due to improved vaginal secretions and elevated mood.
Testosterone
Testosterone therapy is only recommended for postmenopausal women who are distressed by their loss of libido. This condition is known as hypoactive sexual desire disorder (HSDD). A testosterone 1% cream (specifically for women) is now available and approved for use in Australia.
There is no evidence to support using testosterone in premenopausal women for low libido or any other condition, such as low mood or depression.
How do you take MHT?
MHT can be taken in various forms, including pills, patches, gels, vaginal pessaries, creams and tablets. Types and doses vary according to individual needs and responses to MHT.
How long do you need to take MHT?
It can take some time to find the right type and dose of MHT. Once you’ve found an effective MHT, you can take it for as long as you need. Many women have symptoms for around eight years and one in four women have symptoms into their 60s and 70s.
When to see your doctor
It’s important to review your need for therapy, and potential risks, with your doctor each year.
Jean Hailes forWomen's Health is a national not-for-profit organisation dedicated to improving women's health across Australia through every life stage.
For more information, visit jeanhailes.org.au/health-a-z/menopause
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 35
Nourish dry skin with Bio-Oil Body Lotion.




Discover the power of oil - but not as you know it. Introducing Bio-Oil Body Lotion. An ultra-light yet high-oil formula that provides sheer, long-lasting moisturisation. Instantly absorbed, it leaves your skin nourished and feeling silky smooth. Shake-up your skincare routine with Bio-Oil Body Lotion.
Discover the power of oil - but not as you know it. Introducing Bio-Oil Body Lotion. An ultra-light yet high-oil formula that provides sheer, long-lasting moisturisation. Instantly absorbed, it leaves your skin nourished and feeling silky smooth. Shake-up your skincare routine with Bio-Oil Body Lotion.

36
Trademarks are owned by or licensed to the Aspen Group of companies.© 2022 Aspen Group of companies or its licensor. All rights reserved. 6849-091024
Ultra-light, yet powerful.
Trademarks are owned by or licensed to the Aspen Group of companies.© 2022 Aspen Group of companies or its licensor. All rights reserved. 6849-091024 NEW







Supporting you and your baby’s healthy development Most trusted, brand* No. 1 Always read the label and follow the directions for use. If you have had a baby with a neural tube defect /spina bifida, seek specific medical advice. *Elevit is Australia’s most trusted pregnancy brand, based on Kantar Research, Sept 2021. 1. Elevit has supported an estimated 2 million pregnancies since its launch 20 years ago. Based on ABS Births 2001-2019, FiftyFive5 Brand Penetration research 2018 and Fiftyfive5 Green Cross 2 Research 2021. 1 CH-20220719-17 SCAN HERE FOR MORE INFORMATION
Looking after your ACLs
THE ANTERIOR CRUCIATE LIGAMENT (ACL) IS ONE OF THE MOST IMPORTANT LIGAMENTS IN EACH KNEE. DAMAGING IT CAN BE A DEVASTATING INJURY, OFTEN REQUIRING SURGERY AND A LENGTHY RECOVERY PERIOD. WOMEN ARE MORE LIKELY TO SUFFER THAN MEN – FOR EXAMPLE, FEMALE ATHLETES CAN FACE TWO TO EIGHT TIMES HIGHER RISK.
The ACL is responsible for stabilising the knee joint and preventing it from moving excessively, so you really don’t want to tear it. But why are more women at risk?

Anatomy
Women naturally have wider hips than men, which creates a greater angle between the thigh bone and the shin bone.1 This angle, known as the Q angle, can put more stress on the knee joint and increases the risk of an ACL tear. Additionally, women tend to have smaller ACLs and narrower knee tendons, which can make the ligament more vulnerable to injury.1
Hormones
Research has shown that oestrogen can weaken the ACL and make it more susceptible to injury.2 Of course, women have higher levels of oestrogen than men, and particularly so during their menstrual cycle, which may explain why they are more likely to experience ACL tears during this time.
Biomechanics
Female athletes often move differently from male athletes, which can increase their risk.1 For example, females tend to land from jumps with their knees straighter and their hips rotated inward, which puts more stress on the knee joint.3 They also tend to rely more on their quadriceps muscles, at the front of the thighs, which can cause the shin bone to move forward and puts the ACL at risk of tearing.3
Training and conditioning
Female athletes often receive less training in strength and conditioning than their male counterparts, which can put them at a disadvantage in terms of muscular strength and control.2 This can lead to compensatory movements and an increased risk of ACL injury. Sports such as soccer and basketball have higher rates of ACL tears among females, possibly due to differences in playing style and rule enforcement.
How do we tackle this?
Preventing ACL tears in women requires a comprehensive approach which addresses these multiple factors. Strength and conditioning programs that focus on the muscles surrounding the knee joint can help to improve control and stability and reduce the risk of compensatory movements that can lead to injury.4
Teaching women proper landing techniques, and how to change direction at speed, could also help them to avoid putting unnecessary stress on their knees.4 Additionally, a better understanding of hormonal factors in future could mean timing training and competition schedules, especially individual sports, to avoid high-risk periods during the menstrual cycle – or possibly hormone therapy, in certain cases.
If you tear an ACL
In the event of an ACL tear, prompt and appropriate treatment is crucial. Surgery may be necessary to repair the ligament, followed by a rehabilitation program that includes physical therapy and a gradual return to activity.5 To ensure the best possible outcome, it's important to work with a healthcare provider who has experience in treating ACL injuries.
1The female ACL: Why is it more prone to injury?: https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4805849/
2Anterior cruciate ligament injury: https://bjsm.bmj.com/content/55/17/984
3Female football players are at much higher risk of career-ending ACL injuries – the science on why: https://theconversation.com/female-football-players-are-at-muchhigher-risk-of-career-ending-acl-injuries-the-science-on-why-198121
4Why female athletes injure their ACLs more frequently: https://www.ncbi.nlm.nih.gov/ pmc/articles/PMC8329328/
5Evidence-based recommendations for the management of anterior cruciate ligament (ACL) rupture: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6723618/
38
What’s on at your Blooms The Chemist
Iron screening
Your iron levels have a big impact on how you function day-to-day. If you have too little you could experience fatigue, breathlessness, decreased immunity or even be anaemic (insufficient red blood cells). If you have too much, it can be toxic – it’s all about balance.
Low iron affects around 5% of Australia’s population.
At Blooms The Chemist you can check your total iron levels with a quick iron screening check.
Blood glucose monitoring
Blood glucose monitoring helps to manage your risk of diabetes, a condition in which your body has trouble converting glucose (sugar) into energy. With 1.5 million people in Australia living with diabetes, it's important to check your blood glucose levels and see if you are at risk of being diagnosed.
It can assist those recently diagnosed, or those with higher risk of developing Type 2 diabetes. However, this test may not confirm if you have diabetes, as a high blood glucose reading only indicates that there may be an issue.
Stroke risk sssessment
Stroke is one of Australia’s biggest killers and a leading cause of disability. Stroke kills more women than breast cancer and more men than prostate cancer. The good news is that more than 80% of strokes can be prevented. At Blooms The Chemist, we offer a free and quick stroke risk assessment service. This involves a short list of questions about your age, gender, lifestyle, and familial history to assess your risk of developing a stroke over the next five years.
For professional advice, products and to book your vaccinations this flu season, visit bloomsthechemist.com.au
HEALTH CHECK MAGAZINE | WOMEN'S EDITION 2023 39
.com.au
bloomsthechemist








 by Aurelia Captari
by Aurelia Captari