Cullman Regional First to Use BrainScope Technology
 By Jane eHrHarDt
By Jane eHrHarDt

A new diagnostic tool opens the door for physicians to identify minor brain injuries and concussions in minutes. “It gets patients the answers faster and gets them home quicker. They love that,” says Mark Christensen, MD, emergency department medical director at Cullman Regional Medical Center.
Cullman is the first hospital in the Southeast to use the BrainScope. They were part of the pilot program,
An Alternative for Sleep Apnea Sufferers Who Can’t Use CPAP
By SteVe SpenCer
The American Medical Association estimates that obstructive sleep apnea (OSA) affects up to 30 million people. The condition, in which a person’s airway completely or partially closes during the night, can lead to a number of comorbidities. Poor sleep may be associated with an increase in insulin resistance, a precursor of diabetes. And because people with sleep apnea get less oxygen, it can elevate the possibility of heart attacks or stroke, as well as potential neurocognitive deficits.
The gold standard for treating OSA is continuous positive airway pressure

(CPAP) in which the patient wears a mask that is connected through a hose to a motorized machine that delivers a continuous stream of pressurized air that acts like a stent to keep the airway open.
The problem is that although the CPAP works well, compliance is very low. A study of over 20 years of data shows that, even with advances in the CPAP like quieter pumps and softer masks, only around 30 to 50 percent of patients use the machine regularly, if at all.
“I’ve had patients who don’t wear their CPAP for a number of reasons,” said John Stafford, MD with ENT Associates of Alabama. “Some can’t wear it because of claustrophobia, while oth-

Celebrating 25 Years of Orthopaedic



ers are affected by PTSD. Sometimes people fall asleep before they’ve had a chance to put it on. And people might not take it when they go out of town. CPAP tolerance is so low that technical compliance for insurance purposes means that the patient is using it at least four days a week for four hours a night. That's very low.” Unfortunately, there was no effective alternative for CPAP until the Inspire was introduced a few years ago. Currently, potential candidates for Inspire are patients who have moderate to severe OSA shown on a sleep study within the

FOCUS TOPIC AUTOIMMUNE DISORDERS SERVING A 24 COUNTY AREA, INCLUDING BIRMINGHAM, HUNTSVILLE, MONTGOMERY & TUSCALOOSA OCTOBER 2022 / $5 www.birminghammedicalnews.com FOLLOW US 205.985.4111 SouthlakeOrthopaedics.com
Excellence Medplex Medical Building Hoover | Grandview Physicians Plaza Birmingham
(CONTINUED ON PAGE 4)
Patient wears the BrainScope while Nurse reads the results on handheld device.
John Stafford, MD implants the Inspire.
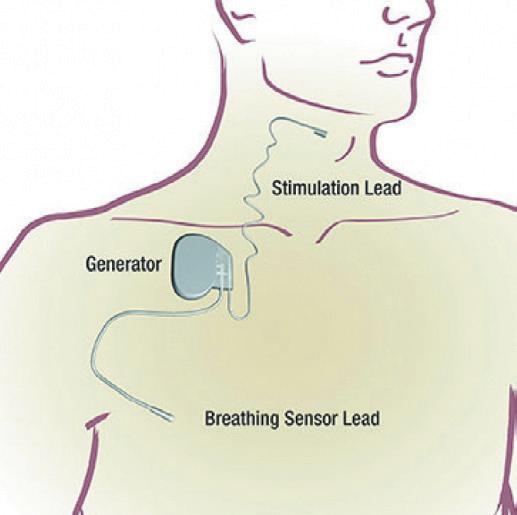
Inspire device with breathing and stimulator leads.
(CONTINUED ON PAGE 5)
We care about you.
Our firm works with all types of health care clients on business, regulatory, and litigation matters, covering every aspect of the industry. Burr & Forman’s regional health care group includes over 40 attorneys across the southeast.






Alabama Health Care Team Birmingham, Mobile, Montgomery
Howard E. Bogard
J. Brockman
2 • OCTOBER 2022 Birmingham Medical News
No representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. 350 Attorneys. 19 Offices. Results matter.
Burr.com
Richard
Kelli Carpenter Fleming
James
A.
Hoover
Catherine
“Cat” Kirkland
Robin B. Mark
Lindsey Phillips Angie C. Smith
420 North 20th Street, Suite 3400, Birmingham, AL (800) GET-BURR No representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers.
Brookwood Father/Daughter Team Delivers Healthy Babies Together
By Marti WeBB Slay
When ob/gyn Greg Banks, MD welcomed his newborn daughter, Amy, at Brookwood in 1990, he knew he’d be joining the staff the next day. What he didn’t anticipate, however, was that 32 years later he would be working side by side with her as a colleague.

Amy Freeman, MD was born into the Brookwood family, grew up watching her father bring new babies into that fam ily, and then rejoined it recently in a new role: as a neonatologist on staff.
“It’s amazing,” Freeman said. “It’s a dream that I’ve had since I started pursu ing neonatology. I love the field and when I chose that path, I always thought about a scenario where my dad was there in a delivery, and he would need to come to us and hand that baby off to me.”
That event has already occurred, within weeks of Freeman beginning her new role. “We counseled the mother together before delivery and worked to gether through that case,” she said.
“It was amazing to see her transi tion from daughter to fellow physician,” Banks said. “She took over the situation



and did what she was trained to do. She was calm and cool.”
Growing up as a physician’s daugh ter, Freeman knew the stakes of a career in medicine, but she also saw the rewards. “I witnessed my dad’s effect on people with his kindness and empathy,” she said. “We never went out to dinner without someone stopping to say, ‘you delivered
EXPERIENCED FIRM, FOCUSED




Why entrust your practice to a generalist when you could have an advisor that understands your specific needs and the challenges of the healthcare industry?


Warren Averett is uniquely equipped with experts who have dedicated their careers to helping medical practices thrive. We help physicians make smart personal and business decisions. We’re here for you.







my child,’ or ‘you saved my life.’ It made me want to have that effect on people.”
Freeman’s mother was a NICU nurse, and her brother is completing his residency in vascular surgery at UAB. “I would love to have him at Brookwood, too,” she said. “We often discuss our cases. It’s nice to consult with him about difficult cases that might affect us emotionally.”
“I love what I do,” Banks said. “When I asked my son if he was sure he wanted to go into medicine, he said that it was a calling, not a choice. Amy said she couldn’t think of anything else she’d want to do. That makes me feel good about their career choices. Medicine takes a lot of time, sometimes from family. It’s a bal ance, and I can love both. My patients become part of the family when I’m at work. My kids have seen that.”
“We’ve always been close, and he has advised and counseled me to get through medical school, residency and fellow ship,” Freeman said.
She started medical school planning to be a surgeon, but during her rotations, she found her passion in the NICU. “I fell in love with it, and I did a general pediat rics residency, primarily to go into the field of neonatology,” she said. “What drew me was the relationships you build with fami lies. Whether it’s a term baby who is there a short period of time or a 23-weeker who’s there for months or up to a year, it’s the relationships you build with the fami lies and getting them through the happiest times and the hardest times.
Birmingham Medical News OCTOBER 2022 • 3
ON HEALTHCARE
Alabama | Florida | Georgia | 205.979.4100 | www.warrenaverett.com
Daughter and father, Amy Freeman, MD and Greg Banks, MD.
(CONTINUED ON PAGE 4)
Relax. Recover. Regain.
Alternative for Sleep Apnea Sufferers Who Can’t Use
last two years, have a BMI of less than 35 for Medicare or 32 for private insurance, and cannot tolerate CPAP.

In order to see if patients who fit within these parameters are candidate for the Inspire, Stafford and the team at ENT Associates perform a drug induced sleep endoscopy in which the patient is given anesthesia to achieve a level of se dation that is similar to natural sleep. “At that time, I use a scope camera to exam ine their airway,” Stafford said. “With sleep apnea, your airway can close ei ther by the tongue falling back to cause the blockage or by the sides collapsing. The tongue falling back, which we call an anterior to posterior collapse, is the type that is best suited for Inspire. The device stimulates the hypoglossal nerve during sleep, which keeps the tongue in a non-obstructive position.”
Let our luxurious surroundings soften your road to recovery



The resort-like amenities at Aspire will create a soothing environment for your rehab stay. Our licensed physical therapists will work with you personally to restore your strength and ability.



Our facility boasts the latest in rehabilitation options, including two state-of-the-art gyms with specialized equipment to get you back in action. Our ceiling-mounted Zero Gravity System suspends patients for secure guidance to get you on your feet faster. Our therapists utilize the latest Omni Virtual Reality System to stimulate progressive therapy through walking, jogging, and other movements. We also have recovery services for hip and knee replacements, plus strength and conditioning programs following rheumatologic conditions.
Let Aspire’s resort-like atmosphere be a partof your rehab experience.
The Inspire is implanted during an outpatient surgery that usually lasts two to three hours. It consists of a small impulse generator that is implanted be neath the clavicle, along with a tunneled breathing sensing lead placed between the external and intercostal muscles, and a tunneled stimulation lead attached to the branch of the hypoglossal nerve that produces tongue protrusion.
“Originally this was performed as a surgery with three incisions, but as of this













from page 1
year we perform this through two inci sions: one on the right neck and one of the right chest,” Stafford said. “The chest location holds the device and the neck incision is where the hypoglossal nerve is located. We dissect the hypoglossal to identify only the branches of the nerve that help keep the airway open. Then we place the stimulation lead around this portion of the nerve. We can test the de vice in real time and verify that the de sired tongue motion has been achieved. While the device is immediately func tional, the patient usually won’t fully acti vate it for use until about one month after surgery to allow for healing.”
The patient can turn on the therapy on before they go to sleep and turn it off when they wake up. They can also pause the therapy, if needed. Typically, patients feel a tingling sensation or mild contraction in their tongue muscles. The stimulation should not be painful or un comfortable and the level is adjustable.
“I've had patients who had dif ficulty wearing their CPAP, and once they started on inspire, they’ve told me they couldn't be happier,” Stafford said. “They have restorative sleep. They wake up in the morning feeling much better than they’ve felt in years. It's great to fi nally be able to help those patients.
Father/Daughter Team Delivers
Healthy Babies
Together, continued from page 3
“Neonatology is also a great mixture of procedures and medicine. I enjoy doing procedures, and I also enjoy the physiology aspect of it. The physiology and changes that happen before and after delivery are fascinating. I am also amazed at the resil ience of babies. They fight their hardest every day. They fight harder than many adult patients I’ve taken care of. I’ve seen so many miracles during my training.”
Freeman said she has had no trouble being fully accepted as a professional among her new peers, despite their hav

ing known her as a child. “It’s fun to reminisce with them, but I’m definitely treated as a colleague,” she said.
For his part, Banks is a proud father.
“I can’t tell you the feeling, watching my kids over the years as they’ve grown from children to friends in college, and now as work companions. It means so much when you hear patients and staff talk about them as professionals and as the type of person they are. For a parent, it’s one of the greatest things in the world.”
you manage or
practice?
4 • OCTOBER 2022 Birmingham Medical News Conveniently located off Hwy 31 in Hoover 575 Southland Dr | Hoover AL 35226 Contact Kathy Maynor at 721-6200 for more information Medicare, Medicare Advantage Plans and other insurances accepted.
CPAP, continued
Do
supervise
in a
healthcare
Discover fresh ideas, project support, and solutions. Consider joining today. For meeting info or to join: bhmgma.com or email bhmgma@gmail.com Your local MGMA chapter is here for you
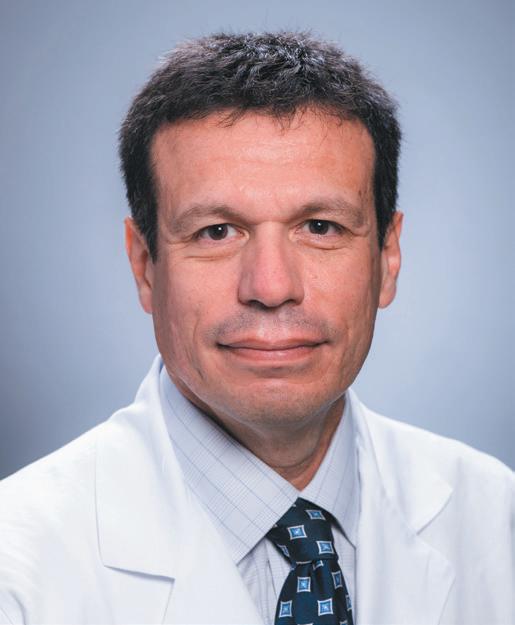
Cullman Regional First to Use
but during the pandemic head injuries became less common in the emergency room with the end of sports and group activities. Now their ER sees several cases a week with that number growing as word spreads about this unique diagnostic tool.



“This is the first of its kind,” Chris tensen says. “It’s is a modification on the electroencephalogram (EEG). Certain brainwave patterns present if there’s in ternal injury to the brain, like a bleed or skull fracture, which is why we did CT scans on patients anyway.”
On this device, a lightweight dispos able headset lined with seven plastic elec trodes attaches to the forehead, temples, and each earlobe. The manufacturer says the reading takes up to 20 minutes, but Christensen says it’s closer to five and as low as three minutes. An EEG, on the other hand, would usually take 45 minutes and require a neurologist to interpret the results. CT scans can take hours of waiting and then waiting again for the radiologist to study the data. And neither diagnoses a concussion.
BrainScope delivers the results on a handheld device in a straightforward manner any healthcare worker could understand. The screen displays positive or negative for each of the available con ditions: internal injury and concussion.










A positive result for internal injury means the brainwave pattern signaled the likelihood of bleeding in the brain. “BrainScope can detect as little as 1cc of blood in the brain, which is as sensitive as a CT scan with a proven 99 percent accuracy,” Christensen says.
The device diagnoses concussion the same way. The brainwaves run through Brainscope’s artificial intelligence utiliz ing multiple algorithms to compare the patient’s brain patterns to a database of over 10,000 cases. The comparison takes into account biomarkers as well, includ ing gender, age, type of injury, loss of consciousness, and whether the incident was witnessed.
For concussions, the device presents additional insights into the condition be yond positive or negative. A brain func tion index scale displays a percentile reflecting a range from normal to abnor mal. A third screen presents a concussion index (CI) ranking up to 100. “Lower is more severe,” Christensen says. “Physi cians can also track that CI over time by retesting to monitor how the patient is progressing and their readiness to return to work, sports or other activities.”
Recovering from a concussion can be a tough road. Some people struggle with insomnia keeping them up for days at a time, while others face panic attacks, brain fog, and headaches. Full recovery can take 24 hours or several months. “Concussion is not just a mild thing. It’s about time we have a tool to identify it now in the emergency rooms,” Chris tensen says. “We’re really excited.”
Cullman’s data mirrored Brain Scope’s national results to show a 30 percent reduction in the use of head CT scans in ERs after using the device to tri age head injuries initiating, which saved those patients from unnecessary radia tion exposure as well. That reduction also equated to a 40 percent decrease in the length of stay in the ER for those patients with mild head injuries. “And the patients are much happier, because we can show them results,” Christensen says.
Before BrainScope, no diagnostic tool existed for concussion. CAT scans only look for injuries like skull fractures or bleeds. So ER physicians would ex amine the patient and report to the wor ried parents or patients that no CAT scan was needed but that they likely had a concussion, and then discharge them.


“Patients are not often happy with that,” Christensen says. “They want something concrete to tell them they do or don’t have a concussion.”
Currently, the device holds FDA ap proval for 13 to 85 year olds. BrainScope is working toward its acceptance for use in any age, but there has not been a large enough sample size of those age extremes in the clinical trials to qualify yet.


Christensen is also excited at the potential for the device to be used in diagnosing strokes. EMTs being able to accurately identify a stroke at the scene means saving precious time by taking the person right to a stroke center for treat ment. “Your own brain wave is all that’s read for that to happen,” Christensen says. “So simple, and yet what it does is so significant.”
Mark Christensen, MD








Birmingham Medical News OCTOBER 2022 • 5 CARING FOR ALL YOUR ORTHOPEDIC NEEDS Loy Vaughan, M.D.S. Evan Carstensen M.D Daryl Dykes, M.D. Michael C. Gerhardt, M.D. Lloyd Johnson Ill, M.D. Winston Capel, M.D. Alabama Bone & Joint is committed to medical excellence and pledges the highest quality of orthopedic care available. Our physicians and support staff provide all of our patients with professional orthopedic care delivered efficiently and on a personal level. Workers’ Compensation • Fracture Care • Joint Replacement• Sports Medicine • Digital Imaging Arthroscopy & Minimally Invasive Procedures • Orthopedic Spine • Physical and Occupational Therapy Hand, Wrist & Upper Extremity • Foot, Ankle & Lower Extremity • General Orthopedics • Osteoporosis Care Available For Same-Day Appointments CALL 205-621-3778 FAX 205-621-4835 VISIT ALABAMABONEANDJOINT.COM 120 Cahaba Valley Pkwy, Suite 100 Pelham, AL 35124 MRI - MRA || ULTRASOUND || CT || VASCULAR STUDIES GENERAL X-RAY || DEXA || MAMMOGRAPHY NUCLEAR MEDICINE || ECHOGRAPHY || NERVE CONDUCTION Same-day imaging appointments. All insurance precertifications done in-house.
BrainScope, continued from page 1
OrthoGrid Navigation System Offers a Clearer Picture of Hip Surgeries
By laura FreeMan
Michael K. Ryan, MD of Andrews Sports Medicine is a rare orthopedic surgeon.


In addition to the anterior approach hip replacements he performs at Ascen sion St. Vincent’s Medical Center, he is one of the few surgeons in the country who also does complex osteotomies for conditions like hip dysplasia, as well as arthroscopies to relieve symptoms with out the need for a total hip replacement.
“The OrthoGrid application helps me perform all three to the very best of my abilities,” Ryan said. “In hip sur geries, we are guided by intraoperative x-rays projected on a screen. However, these images tend to have distortions that can make precise measurements more challenging.
“The OrthoGrid software takes the original x-ray and corrects the distor tions. It sets up an overlay on a second screen with a virtual guidewire. I can use touch screen tools to easily measure pa rameters like distance and angles.”
One of the world’s first intraopera tive hip surgery navigation systems, the OrthoGrid platform improves the ef ficiency, accuracy and reproducibility of hip surgeries. The newest release of the application uses AI and machine learning capabilities for even greater precision, functionality and seamless integration into the OR workflow. The navigation system can be used in surgi cal planning and through each step of the procedure.
“Every patient who comes to us has a unique anatomy with bones and joints that differ in size and how they fit together. The nature and location of the hip makes us more dependent on im aging for it, compared to joints like the knee that is easier to visualize. That’s why these capabilities can make such a difference,” Ryan said.
Michael K. Ryan, MD

The Orthogrid technology auto matically registers the patient’s anatomy and retains it in the surgical file. It iden tifies instruments and implants, and it processes data through the surgery in accordance with the surgeon’s workflow.
Ryan’s expertise is in hip preserva tion and improving function in congeni tal hip disorders. When Ascension Saint Vincent’s was looking at acquiring a hip surgery navigation system, Ryan consid ered other systems but only the Orthogrid application offered tools that he could use across a broader range of hip surgeries.
“If I’m doing an arthroscopy or oste otomy to correct hip dysplasia, I can see exactly how much bone I need to trim and how I need to position the joint for optimal function,” he said. “For a hip replacement, I know where to cut and how to place the new joint to avoid stress and wear. This helps us give the patient more years of functional use and may help to avoid the need for a second replacement later.”
Designer OrthoGrid Systems, Inc., has also been working on an augmented reality program to assist surgeons in re pairing injuries from trauma. It is ex pected to offer many similar advantages as the OrthoGrid navigation platform and to help physicians and surgeons work quickly and efficiently in emer gency situations.
“I found the OrthoGrid platform very intuitive and easy to learn,” Ryan said. “A company rep shadowed me for a couple of days, showing me the nuances of how the system works and some of its special features. I was soon using it in most of my hip surgeries. Some sur geons use it with robotic systems, but I work with it hands-on. It gives me better data so I can make the best decisions.
“At the end of the day, it’s all about outcomes. The precision, efficiency and consistency the OrthoGrid application helps me achieve gives my patients the best possible surgery for a good outcome.”
6 • OCTOBER 2022 Birmingham Medical News
Welcome Our Newest Provider


Interventional Neurology Chike Ilorah, MD, MPH

Brookwood Baptist Health Specialty Care Network is proud to welcome Dr. Chike Ilorah. Dr. Ilorah is a practicing interventional neurologist and is affiliated with Brookwood Baptist Medical Center, a Joint Commission certified Primary Stroke Center and a 2021 GWTG Gold Plus Target: Stroke Honor Roll Elite Plus Advanced Therapy. He and the team at Brookwood Baptist Health Specialty Care Network – Neurology are dedicated to 24/7 care for all stroke patients.

Dr. Ilorah is board certified by the American Board of Psychiatry & Neurology. He attended medical school at Nnamdi Azikinwe University in Nigeria. He served his residency at the University of Illinois-Peoria and earned his fellowship at Saint Louis University School of Medicine. He earned his Vascular Neurology and Endovascular Surgical Neuroradiology Fellowships at Saint Louis University School of Medicine.
Brookwood Baptist Health Specialty Care Network - Neurology 513 Brookwood Blvd., Ste. 372 Birmingham, AL 35209




Dr. Ilorah’s areas of interest include:

■ Mechanical thrombectomy for acute stroke
■ Brain aneurysms with a minimally invasive focus including flow diverter device, endovascular coiling, WEB device, etc.
■ Carotid stent placement for severe carotid artery stenosis
■ Vertebral stent placement for severe vertebral artery stenosis
■ Intracranial stent placement
■ Diagnostic cerebral angiogram
■ Diagnostic spinal angiogram
■ Tumor embolization
■ Middle meningeal artery embolization for chronic subdural hemorrhage
■ Embolization for severe nose bleeding

Birmingham Medical News OCTOBER 2022 • 7
Call 205-802-6595 to make an appointment with Dr. Ilorah. BBHCareNetwork.com
Pediatric Urgent Care is on the Rise
By Jane eHrHarDt
“Children don’t get sick on a schedule, and it’s unreasonable to expect pediatricians to be open 24/7. That’s where we come in. We serve as an extension to their team,” says Allury Arora-Lal, MD, the founder and Chief Medical Officer of Urgent Care for Children.
Urgent care clinics fill a gap in America’s healthcare system by providing convenient, on-demand care without the high cost of an emergency room visit. Started in the U.S. in the 1970s, many were opened by emergency medicine doctors responding to the need for walk-in care for minor illnesses, fractures, sprains, and wounds during the off-hours of traditional primary care practices. The centers, most of which cater to all ages, have taken off in the last decade, especially in suburban areas, growing to almost 10,000 throughout the country.
More recently, pediatric urgent cares have sprung up to focus only on children. Urgent Care for Children, which started in 2017 on Highway 280 was designed with children in mind. Waiting areas offer coloring books, cartoons, and QR codes for parents to download books for contactless reading. “We offer snacks, popsicles, and drinks to our patients because most come
after school or right after evening activities. They’re hungry. And hungry kids can get cranky,” Arora-Lal says.
Serving patients from newborns to young adults up to 21 years old, the centers are open evenings, holidays, and weekends every day of the year and are staffed with pediatric-trained healthcare staff. “It can take a special heart and specific training to know how to handle children.” Arora-Lal says. “They are coming into a new, overwhelming environment feeling sick. Our staff is trained to not just support the children, but also the guardians and parents who accompany them.”
Some traditional urgent care centers will not treat very young children or infants, automatically sending them on to ERs. “Pediatric physiology and the way children’s bodies process pharmacology is unique, and you need to be proficient to safely treat children, even with such common medications as steroids and antibiotics,” Arora-Lal says.

Everything is offered under one roof at the clinics, including labs and x-rays. “We also have a pharmacy so parents don’t have to run around town to pick up prescriptions,” Arora-Lal says. About 45 percent fill their prescriptions at the centers.
Around 50 percent of their patients return for treatment at some point, but the clinics do not serve as a source for primary care. “I see pediatric urgent care as a partner to our patients’ primary care, which is their medical home,” Arora-Lal says. “With strong communications, we can create a seamless process of care.”
To keep the patients tied into their primary care physician, the urgent care sends detailed notes of the patient’s visit to their PCP by the next day. The centers also do not offer any well-child visits, such as immunizations (except Covid), vision and hearing testing, milestone visits, and growth plotting. “They go to their family care doctor for that,” Arora-Lal says.
About 10 percent of the almost 100,000 Alabama children and young adults seen annually by their centers arrive with no primary care provider connection.
“In that case, we act as the entry point into the medical care system for them,” AroraLal says, and refer them to area pediatricians for continued care.
Urgent care also brings a unique value proposition to the healthcare industry.

“Getting patients into the appropriate setting has the potential to save billions of dollars,” Arora-Lal says. The average urgent care visit runs about $160. For the same treatment, the patient would spend $2,000 at the emergency room, according to a 2016 study in the Annals of Emergency Medicine. “We are the option for these families who don’t have pay the expensive ER copay for reasons like rashes, urinary infections, sore throats, and fevers.”
Besides lower out-of-pocket costs, urgent cares tend to be more accessible than hospitals, with twice the expansion in suburban areas than in urban ones. They also see patients very quickly. Almost 97 percent of urgent care patient interactions lasted an hour or less, and 92 percent saw a provider within 30 minutes, according to the Urgent Care Association 2019 benchmarking report.
OUR DOCTORS
Nicholas Izor, MD
Dr. Nicholas Izor grew up in Birmingham and graduated from the University of Alabama with a degree in Chemistry. After receiving his medical degree from the University of Alabama School of Medicine, he completed his residency in Internal Medicine at Saint Louis University followed by his nephrology fellowship at Yale University.

Thomas Ozbirn, D.O. Roman Brantley, M.D. • James Lewis, M.D. John Brouillette, M.D. • Jeffrey Glaze, M.D. Harold Giles, M.D. • Agata Przekwas, M.D. Thomas Watson, M.D. • William Lyndon, M.D. Michael Hovater, M.D. • Benjamin Broome, M.D. Phillip Madonia, M.D. • Timothy Williams, M.D. Theodore Feely, M.D. • James Harms, M.D.
David Tharpe, M.D.
OFFICE LOCATIONS
Alabaster
Anniston
Bessemer Birmingham
Clanton
Gadsden
Gardendale Greystone
Pell City
Homewood
Trussville
Winfield
Jasper Oneonta
NEPHROLOGY ANEMIA CLINICS
Alabaster
Homewood
Birmingham
Greystone
Bessemer
NEPHROLOGY VASCULAR LAB Birmingham





HOSPITAL AFFILIATIONS
Brookwood Baptist Medical Center
Grandview Medical Center
Princeton Baptist Medical Center Shelby Baptist Medical Center
Vincent’s Birmingham
Vincent’s East
Medical West
Lakeshore Rehabilitation Center
Shelby Rehabilitation Center
8 • OCTOBER 2022 Birmingham Medical News
205.226.5900 NEPHROLOGYPC.COM Kidney Care Close to Home
St.
St.
UAB
HealthSouth
Encompass
•
•
•
•
•
•
•
•
•
•
•
•
•
•
WELCOMES
Allury Arora-Lal, MD
(CONTINUED ON PAGE 10)
Amanda Tapley McGriff, MD Has Always Found Creative Solutions
From Raising Money for Sick Children to Paying for Medical School
By laura FreeMan
Throughout her life, when Amanda Tapley McGriff, MD has faced ob stacles, she has come up with creative solutions, beginning with the use of her musical talents.
“My grandfather, Dr. Witold W. Turkiewicz, was a piano virtuoso who taught music at Samford University,” Tapley McGriff said. “He also taught the children in our family to play and he showed us that we had to put in the work if we wanted to perform on a stage someday.
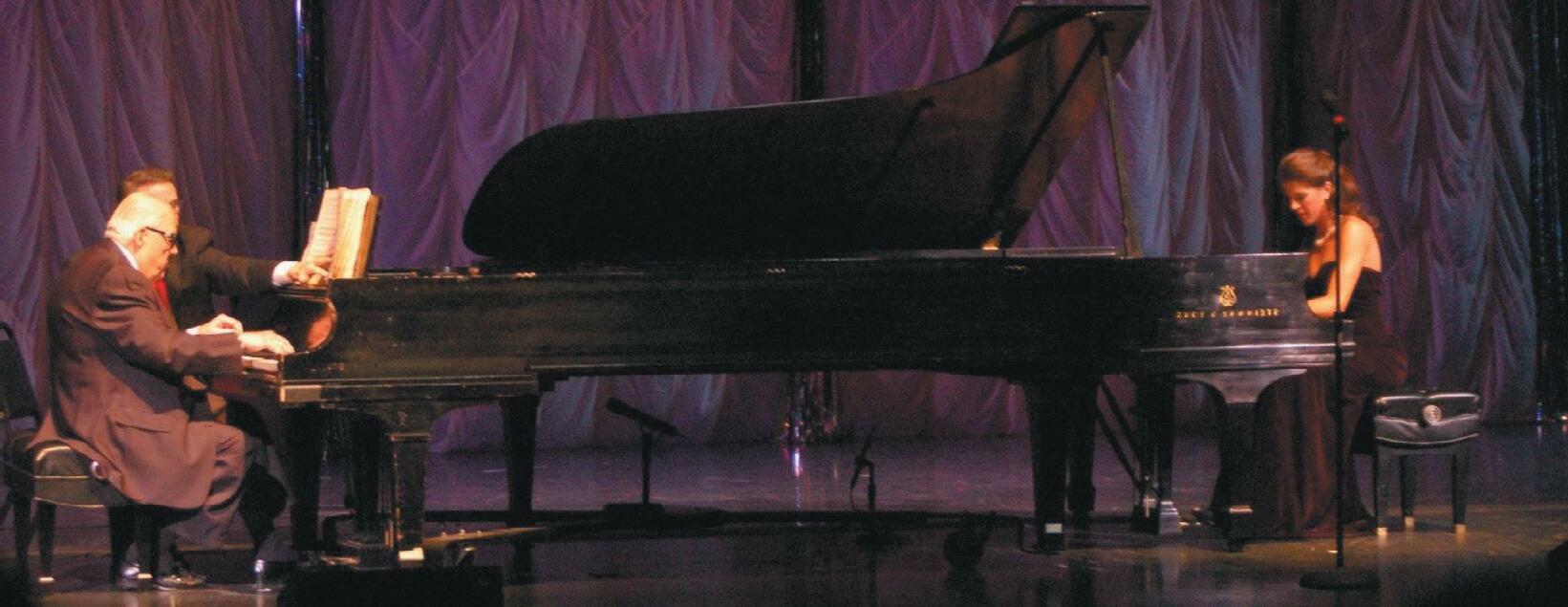
“My brother and I loved music and playing the piano. We decided we wanted to raise money to help sick chil dren. But how could a couple of teenag ers raise enough to make a difference? Someone suggested that we put on a concert and sell tickets. By that time, we had developed our music to the point that we had the confidence to go for it. We also recorded the classical pieces and sold CDs. When we added up the proceeds, we were surprised to find we
had raised almost $50,000, which we donated to Children’s of Alabama and St. Jude’s in Memphis.”
Her next challenge was the cost of medical school. She had dreamed of becoming a doctor since childhood, but while paying for college was doable, she was concerned about taking on massive
Banking for what’s
student loans needed to pay for medical school.

When she learned that the Miss Alabama pageant awarded scholarship money, she decided to give it a try, even though she didn’t really see herself be coming Miss Alabama. And while she didn’t win the first year, she learned
that a good deal of scholarship money was available, even for contestants who didn’t come in number one.
“The next year, I worked as hard as I could, getting everything as perfect as possible, memorizing every note of the music for the talent competition,” she
Birmingham Medical News OCTOBER 2022 • 9
next. 600 Luckie Drive, Ste. 200 • Birmingham, AL 205.313.8100 • SouthStateBank com
(CONTINUED ON PAGE 10)
Amanda Tapley McGriff, MD performed with her grandfather, Dr. Witold W. Turkiewicz.
Alexander, CEO
McGriff, MD Has Always Found
Clark, CEO

said. “I became Miss Alabama 2008 and went on to the Miss America pageant. I didn’t win first place there, but I did bring home enough scholarship money to bring my dream of paying for medical school within reach.”
On the stage at Samford where the Miss Alabama pageant was held, Tapley McGriff also created a memory she will cherish forever.
“I played a piano duet with my grandfather,” she said. “Since he taught at Samford, he had played duets on that stage with the boys in our family. That year, he had been diagnosed with cancer and knew he didn’t have a long time left. As we left the stage he smiled and said, ‘I played on this stage with my boys, and I got to play my swan song on this stage with my granddaughter.’”
After medical school and a residency in emergency medicine at UAB, Tapley McGriff is now a physician with credentials at multiple emergency departments in the Birmingham area.
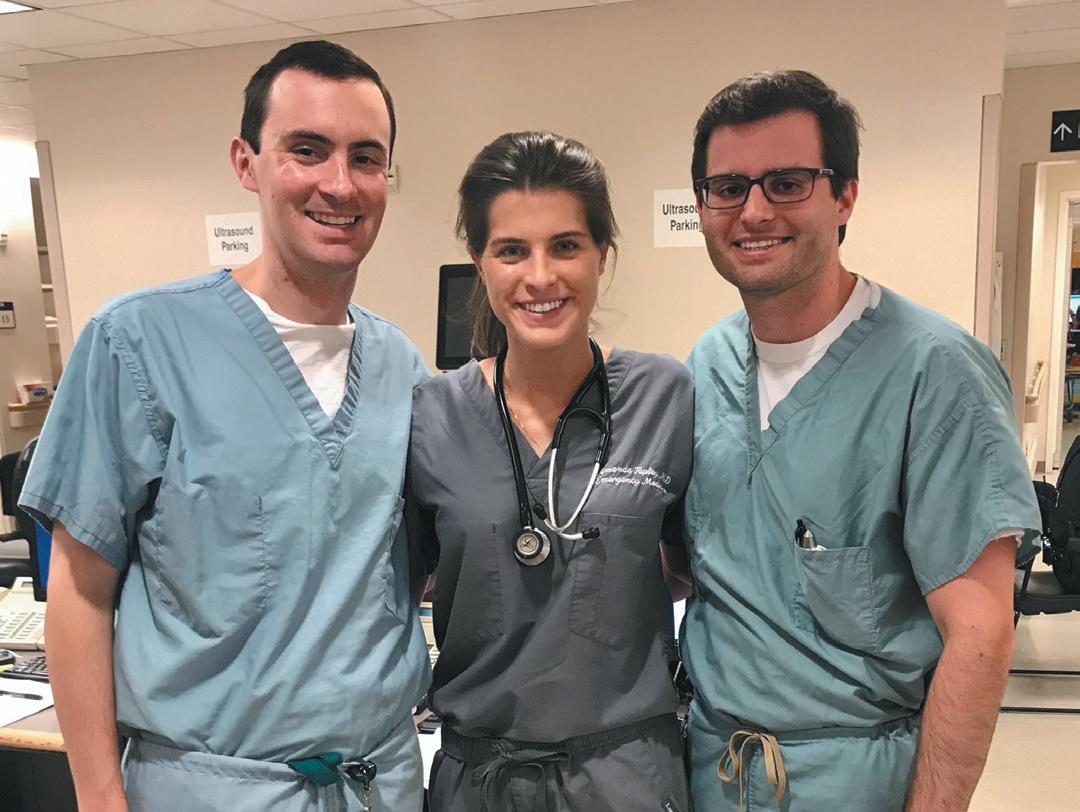



“Working shifts at Brookwood, Princeton and other ER’s in the area gives me the flexibility for one of my biggest dreams, which is to start a family and raise children,” she said.
She married Army Captain Bronson McGriff in the fall of 2019. Two months later he was deployed, she found out she was pregnant, and she became a newly minted ER doctor just in time for the COVID-19 pandemic.
“It was a hard time for everyone,” she said. “We saw so many people coming in the ER who were so very sick. We didn’t know who was going to make it and who wasn’t. I didn’t know if a mask would keep me safe or protect my baby, but I had to help as many people as I could. It was lonely going home and only being able to talk with my husband by phone or video chat.
“Finally the world is getting a bit more back to normal. My husband is home. We had a baby girl, Amelia. I’ve been working as an ER doctor and really enjoying it. In a couple of months, I’ll be taking some time off when Amelia’s baby brother is born.
“After that, I’ll be going back to ER medicine. I went into that specialty because there’s always something new. You never know what will be coming through those doors next. Every patient has a story.”
Pediatric Urgent Care is on the Rise,



from page 8
This convenience of walk-in appointments, cost savings, and accessibility to quality care is why urgent care centers continue to sprout up. As of this year, 78 percent of the U.S. population is within a 10-minute drive to an urgent care center, according to the Urgent Care Association. Urgent Care for Children has quickly expanded in the last five years to 11 locations in Alabama with nine more in Tennessee and Louisiana.
Arora-Lal foresees pediatric urgent care experiencing growth, not only because of consumer demand, but also to fill the shortage of primary care physicians, making same-day visits even harder to obtain. “When you have a sick child, you don’t have time to wait for another day,” she says. “We are the solution to many issues in healthcare continuity.”
10 • OCTOBER 2022 Birmingham Medical News NOVEMBER 16 AT THE CLUB 11:30 AM - 1:00PM Daniel McKinney, CEO Grandview Medical Center Jeremy
Brookwood Baptist Health and Brookwood Baptist Medical Center Jason
Ascension St. Vincent’s For meeting info or to join: bhmgma.com or email bhmgma@gmail.com Hospital Executive Roundtable To reserve your spot, visit BHMGMA.COM SPONSORED BY
Creative Solutions , continued from page 9
Pictured with cousin (left), Darryl Outlaw, Jr., MD & brother (right) Jeffrey Tapley, Jr., MD.
continued
Progress Slow with Hospital Price Transparency


 By Carrie DouglaS anD ZaCHary trotter
By Carrie DouglaS anD ZaCHary trotter
gross charges and discounted cash prices for 300 “shoppable services.” CMS has announced 70 mandatory “shoppable” services which must be reported by hospitals. These services include:
• Psychotherapy Consultations











• Preventive Medicine Services
A patient rights organization recently reported that only 16 percent of the 2,000 U.S. hospitals it reviewed were in compliance with the federal Hospital Price Transparency Rule. Back in June, the Journal of the American Medical Association published a study that also showed that progress on price transparency was slow. To date, CMS has imposed two fines totaling more than $1 million for failure to comply with the Rule and issued more than 350 warning notices to hospitals with more surely to come.
The federal Hospital Price Transparency Final Rule took effect on January 1, 2021 with the goal of increasing healthcare price transparency and facilitating patient price shopping online. Hospitals are required to post machinereadable, consumer-friendly files of the rates they negotiate with payers,
• Routine Labs
• CT/MRI Services
• Mammography Services
• Obstetrical Care
• Surgical Services
Hospitals possess more discretion, however, in selecting what services are identified in the remaining 230 disclosures. Notably, the 230 services must be services that are commonly provided to the hospital’s patient population and selected from the following categories of “shoppable” services:
• Evaluation and management


• Laboratory and pathology
• Radiology
• Medicine/surgery services
Under the Rule, for hospitals with 30 or fewer beds, the minimum civil monetary penalty for failure to comply is $300 per day. For hospitals with more
than 30 beds, the minimum civil monetary penalty for failure to comply is $10 per bed per day, capped at $5,500 per day. Thus, yearly noncompliance penalties can range from $109,500 to more than $2,000,000.
For purposes of complying with the Price Transparency Rule, hospitals must include five types of standard charges for the 300 “shoppable services.”
A hospital may meet the requirements of displaying its shoppable services by means of a price estimator tool if it provides estimates for shoppable

services provided by the hospital, allows healthcare consumers to obtain an estimate of what they will pay for the shoppable services, and allows consumers to search for shoppable services by service description, billing code, and payor.
If a hospital does not use a price estimator tool, it may meet the Rule’s requirement by disclosing its Standard Charge information, which requires a hospital to make public the Standard Charges for as many of the 70 CMS-specified shoppable services that are provided by the hospital, a description of each shoppable service, the billing code for those services, and more.

Regulators have pledged to increase the penalties and have sent hospitals warning letters and corrective action mandates, but fines have only just begun. To promote further compliance, commentators expect CMS to aggressively issue fines and to increase the amount of the fines to a point where they are too large to ignore.


Centers of Alabama is pleased to announce
Meagan Cramer will be joining UCA Women’s Center
October 3,
Cramer is a urogynecologist who offers surgical and non-surgical treatment for women with pelvic floor disorders. Common pelvic floor disorders that she treats include pelvic organ prolapse, urinary incontinence, urinary tract infections, overactive bladder, accidental bowel leakage, difficulty emptying the bladder or rectum, pelvic and bladder pain, and fistulas.


Birmingham Medical News OCTOBER 2022 • 11 Alabama DDS Needs Part-time Medical Consultants If interested, please contact: DDS Medical Section Supervisor (205) 989-2234 or write to: PO Box 830300, Birmingham AL 35283-0300 The Alabama Disability Determination Service (DDS) invites letters of interest from physicians wanting to work part-time as a medical consultant. The work involves reviewing disability claims in the Birmingham or Mobile offices. An Alabama medical license is required. The DDS is committed to maintaining a diverse workforce; and therefore, the DDS encourages minority applications. Welcome Dr. Meagan Cramer UROGYNECOLOGIST 205.930.0920 | UCAWOMENSCENTER.COM To refer a patient, our easy-to-use Referral Form can be found at UrologyCentersAlabama.com/referral. Urology
that Dr.
beginning
2022. Dr.
(CONTINUED ON PAGE 14)
Understanding Guidelines for Diagnosing Celiac Diseas
 By Marti WeBB Slay
By Marti WeBB Slay
If as a physician, you think celiac disease always presents with gastrointes tinal symptoms – and only gastrointesti nal symptoms – UAB gastroenterologist Amanda Cartee MD wants to refresh your awareness of the condition and what the symptoms can include.

“We used to think of celiac disease as presenting with diarrhea, abdominal bloating, weight loss, and what’s some times called failure to thrive or vitamin deficiencies in school age children of mid-European ancestry,” Cartee said. “We now know that’s not the only way it can present. Actually, more people have constipation than diarrhea. People can have nausea and heartburn. And even aside from the gastrointestinal symp toms, they can have fatigue, headaches, joint pain and skin rashes. Some people have bone loss, or osteoporosis. Often people aren’t diagnosed because we don’t realize they can have so many dif ferent types of symptoms.”
Symptoms can be quite mild for some patients. “I have some patients who have had two to three bowel move






ments a day for most of their life,” Car tee said. “That changed with their celiac diagnosis, but it was so mild that they never went to a doctor. In fact, some people don’t have any symptoms. There are still consequences to having the dis ease, however, including anemia, osteo porosis and liver problems.
“Many times physicians don’t con sider a possible celiac disease diagno sis because of the patient’s heritage or

because they think the disease is rare. While it was once considered a disease of people of Irish or Nordic descent, it’s now clear that people from India or China, or their descendants, can also de velop celiac disease. I estimate that one percent of US citizens have it, which counts as common.”
Routinely screening everyone for celiac disease is considered controversial. The United States Preventive Services
Task Force concluded in 2017 that “the current evidence is insufficient to assess the balance of benefits and harms of screening for celiac disease in asymptom atic persons.” But Cartee said there are certain patients who wouldn’t have been screened in the past that now should be tested, based on current knowledge.

“We recommend that there are certain types of people who should be




Nurse
Alabama Pain Physicians,
have a highly skilled team of Nurse Practitioners. With over 50 years of experience at











practice between them, our team
hard to provide the best pain care to
patients.
Pain Physicians,
refer
New x-ray project?

to

12 • OCTOBER 2022 Birmingham Medical News BamaPain.com | 205.332.3160 Meet Our
Practitioners! At
we
our
works
their
When you
to Alabama
you can rest assured that your patients are in great hands. Serina Bourassa, CRNP Anna Turner, CRNP Mickey Brown, CRNP Jessi Barthelemy, CRNP Vanessa Daniel, CRNP Sara Byars, CRNP David Lee, CRNP Heather Lee, CRNP Lauren Windsor, CRNP 3 Generations of Experience at Your Service ALABASTER AL | 205-283-0704 | SALES@HOLTZMANXRAY.COM holtzmanxray.com HOLTZMAN X-RAY & IMAGING XRAY SALES, SERVICE & DIGITAL IMAGING • conventional & digital x-ray equipment • x-ray machines • ultrasound • x-ray accessories • consumable x-ray supplies • all diagnostic equipment Let us help you avoid costly mistakes and time-consuming research.
Wanting
expand? • initial planning • radiation regulatory guidance • facility design • equipment selection & installation • applications training • various support services AUTOIMMUNE DISORDERS
Amanda Cartee MD
(CONTINUED ON PAGE 14)
Early Diagnosis Key to Treating Vasculitis
By Marti WeBB Slay
When Angelo Gaffo, MD from the UAB Division of Clinical Immunology and Rheumatology works with resi dents, he always goes over the signs of vasculitis with them.

“They will probably only see a few cases a year of this,” he said. “My mes sage to them is, ‘you’ll see 100 times more cases of diabetes than this, but when a patient comes in with vasculitis, you don’t want to miss it.’
“Vasculitis diseases are character ized by inflammation of the blood ves sels of different sizes and locations in the body, which leads to damage in a num ber of internal organs, so early identifi cation and treatment is important.
“I’ve seen many patients who were not referred early enough. Usually there has already been, for example, kidney damage or peripheral nerve damage or lung damage. We can treat them, and we can get them better, but then we have to deal with the consequences of delayed diagnosis.”
He believes that because primary care doctors see vasculitis so rarely, it is not the first diagnosis to come to mind, and it can be missed while other possi bilities are checked. Likewise, a shortage
Angelo Gaffo, MD
of rheumatologists and long waits to get appointments can result in delayed di agnosis and treatment. “Sometimes we find these patients in the hospital, be cause they are already so sick,” he said.
Gaffo said the key is to recognize the patterns and understand how the different forms of vasculitis can pres ent. The most common form in the US Southeast is ANCA associated vascu litis. These diseases include granulo matosis with polyangiitis, microscopic polyangiitis, and the more rare eosino
philic granulomatosis with polyangiitis.
“The patterns can be a specific form of kidney disease, glomerulone phritis, diagnosed with a kidney biopsy,” Gaffo said. “This may occur with swell ing, with hypertension and sometimes concurrently with a purpuric rash. Sometimes there is recurring sinusitis with crusting and bleeding, or recurring ear infections. Otitis media is common in children, but should not be common in adults. So we should ask if this some thing else. We should then explore if
this person has a systemic illness.”


Nerve damage is another symptom that can be a red flag. “Nerve damage is very common in diabetes, so in that context, you may miss somebody who is not diabetic and has unexplained nerve damage,” he said.
Another form of vasculitis is giant cell arteritis, which is the most com mon form of vasculitis in general, but less common among African Americans and Latinos. It involves large blood ves sels around the head and neck. “This can cause chronic head discomfort, headaches and painful and tired jaw, known as jaw claudication,” Gaffo said.
“These patients can have incidents of blurry vision or double vision. These vi sion changes can herald the complica tion of vision loss that can happen in patients with giant cell arteritis. This is almost universally in patients over 50, and most commonly over the age of 60. A pattern of headache, fatigue and quite often shoulder and neck pain with jaw claudication and episodes of vision loss can indicate giant cell arteritis.
“When vasculitis is suspected, you should start with basic labs including inflammation markers. For ANCA as sociated vasculitis, you can run ANCA
a banker

as a
Practice Executive. Justin Truelove,

understands healthcare and its
different facets, from financial to HR,
and governance. That unique knowledge in a financial partner means we can integrate
solutions to help you evolve your practice to navigate patient payables and receivables










evaluate lease and real estate purchase benefits, and ensure access to reporting to speed up your revenue cycle.

financing solutions for medical practices during Mergers and Acquisitions, buy-ins, buy-outs, expansion, equipment finance, real estate acquisition, practice
and new clinic

Birmingham Medical News OCTOBER 2022 • 13 When people receive a communication from a law firm, they listen. No Representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. 205.322.6060 • CLOUDWILLIS.COM BIRMINGHAM • MOBILE • NASHVILLE That’s the difference in having the attorneys at Cloud Willis & Ellis represent your medical practice in managing your accounts receivables. We provide the complete services of an agency and a law firm or anywhere in between — you choose. We will collaborate with you to design a collection strategy that helps limit unpaid invoices and medical bills. Then we will implement that strategy in our office, and help you implement the strategy in yours. We have the experience and know-how in medical collections to make it better for you. Call today for a free consultation. Wish Your Banker Understood How to Run a Medical Practice? Wish granted. expansive resources • expertise • strong customer commitment • credibility Colony Bank brings you the exceptional financial experience of
certified
Medical
CMPE, truly
many
IT,
our
challenges,
Unique
renovation,
construction. WWW.COLONY.BANK | 205.909.7220 INVESTORS.COLONYBANK.COM | JUSTIN.TRUELOVE@COLONYBANK.COM 2100 SOUTHBRIDGE PKWY SUITE 650 | BIRMINGHAM, AL 35209 AUTOIMMUNE DISORDERS
(CONTINUED ON PAGE 14)
Y O U R I T C O M P A N Y H E A L T H C A R E T O S T O P E X P L A I N I N G


Progress Slow with Hospital Price
Transparency , continued from page 11
Currently, hospitals’ non-compliance may reflect hospital executives’ concerns about the administrative work required to set up the price transparency database, their rivals undercutting them on publicly disclosed prices and the legal ramifica tions if a patient bill doesn’t match the disclosed data. Given the fine limitations, there are also relatively small conse quences for hospitals that ignore or only partially comply with the Rule. These consequences include allowing CMS to publish a list of hospitals that are penal ized by CMS for failure to comply.

Right now, hospital executives, in con
junction with their legal counsel, should proactively plan how to achieve their goals, the legal ramifications of any failure to comply with the Rule, and, if needed, how to challenge any asserted penalties.


Zachary Trotter is a partner at Waller in Birmingham, Ala. where he assists hospitals, health systems, physicians and other providers with a broad range of transactional, compliance and operational issues.
Carrie Douglas is a partner at Waller where her legal practice focuses on assisting healthcare providers resolve reimbursement disputes with commercial payors.
Understanding Guidelines for Diagnosing Celiac Diseas,
tested,” she said. “That would be any body with the symptoms [discussed above], anyone with elevated liver tests and anybody with ongoing anemia. Peo ple with other autoimmune conditions can be at higher risks of it, so if they are having symptoms, they should be tested. We pretty strongly recommend anyone with a first degree relative be tested. That’s how we catch up to 25 percent of people who have it: if they have a child or a sibling or a parent who is diagnosed.
“Celiac disease can develop at any age. It’s hard to know if some people have had it for a long time and it just hasn’t been recognized, but I meet people in their 60s and 70s who have never had symptoms before and all of a sudden get symptoms, and then we diagnose them.”
When celiac disease is considered as a possible diagnosis, the first step is a blood test. This test has a 98 percent sen sitivity, so if a patient tests positive, they likely have celiac, but those with only a mildly elevated result could get a false
page

positive. Cartee recommends a biopsy before implementing an expensive and difficult gluten-free diet. It’s important for patients to get their tests while they are eating gluten because that is the only way to tell if it’s celiac disease.
She recommends a referral to a gas troenterologist for anyone with a new di agnosis, so they can be connected with a nutritionist and get appropriate follow-up tests. “A gluten-free diet is easier said than done,” she said. “It takes a while for the intestine to get back to normal and the patient needs regular blood tests and pos sibly a repeat biopsy.”
While recovery may vary following the necessary dietary changes, it is usually weeks or even months before improve ment can be seen. Recovery from fatigue and brain fog can take up to a year.
In addition, Cartee said that celiac pa tients are at a higher risk for flu and pneu monia complications, so patients should be urged to get all necessary vaccines.
Early Diagnosis Key to Treating
Vasculitis, continued from page 13

antibodies. That can increase your sus picions if it comes back positive, but use clinical judgment. A biopsy of an affected organ is always preferable. If you really suspect vasculitis, you should refer to a rheumatologist, even while labs are being collected. It is even more important with suspected giant cell arteritis. The rheu matologist should get involved very soon.
“When talking about vasculitis, we are considering more than six or seven different diseases. For some, the referral should be prompt and early.”
There is no cure for vasculitis. Physicians control the underlying au toimmune process with the available treatments. The first line of treatment is often a steroid to rapidly shut down
inflammation and damage, concurrent with another medicine that is tailored to address the process that is driving that condition, which allows physicians to cut the steroids in the future.
Patients are generally followed by a rheumatologist for several years. In some cases, they may go into remission, but that is less common.
Gaffo is aware that referrals to rheumatologists can sometimes result in a significant wait time for a first ap pointment, but he stresses the need for prompt attention when vasculitis is sus pected. “Don’t be shy about prompt re ferral,” he said. “When it is flagged as possible vasculitis, we try to rush these cases. It’s very important.”
14 • OCTOBER 2022 Birmingham Medical News SimplifiedMed.Com (205) 366-3565 | info@simplifiedmed.com C O M P R E H E N S I V E T E C H N O L O G Y S O L U T I O N S F O R H E A L T H C A R E O R G A N I Z A T I O N S You handle Healthcare. We handle Healthcare Technology. W e o f f e r a T e a m - B a s e d A p p r o a c h f o r C o m p l e t e M a n a g e d I T S e r v i c e s . S i m p l e P r i c i n g , C o m p r e h e n s i v e S o l u t i o n s .
continued from
12
Maximize Your Health with your benefits.





Now is the time to check your insurance deductible.











If you’re close to or have met your annual insurance deductible, your out-of-pocket costs could be significantly reduced. Now could be the ideal time to schedule any appointments or procedures you’ve been putting off. Why wait to start feeling better? Make an appointment today.


Appointments tend to fill up quickly as the year closes. We opened additional time through December so you can book early.


Birmingham Medical News OCTOBER 2022 • 15
To find a specialist near you, visit BBHCareNetwork.com/Deductible Learn More
By Kelli Carpenter FleMing
Providers often ask how long they need to retain certain types of medi cal information. While there are some general rules regarding the timeframes for retaining medical information, the specific answer varies depending on what type of information is involved and what type of healthcare provider is inquiring. For example, a ten (10) year retention period would typically cover most legal requirements, but the time frame may be extended depending on the age of the patient or the specific type of information involved. Further, if the medical information is the subject of an investigation or dispute, the information should be retained at least until resolu tion of the investigation or dispute.
However, how long to retain medi cal information is only one piece of the puzzle. Once you decide you have satis fied the retention timeframes and can destroy the information, you have to also make sure that the destruction and disposal process is compliant with appli cable HIPAA requirements. The destruc tion and disposal process may also vary

depending on what format the health information takes, which can range from paper records to electronic information to information included on certain medi cal supplies. Regardless, a recent Office for Civil Rights (“OCR”) settlement re minds providers of the importance of ensuring that a proper destruction and disposal process is followed.
OCR recently announced a $300,000 settlement involving the im proper disposal of protected health information by a physician practice. A

dermatology prac
tice filed a voluntary breach report with OCR when empty specimen containers with labels containing patient identifi able information were placed in the gar bage for disposal. The information was not destroyed or rendered unreadable prior to being placed in the trash. The information contained on each label included patient name, patient date of birth, date of collection, and provider
name. Interestingly, the information did not include diagnosis, detailed clinical information, social security numbers or billing information. In connection with the investigation, OCR determined that proper disposal safeguards were not fol lowed by the dermatology practice and resolved the case with a $300,000 settle ment.

In announcing the settlement, OCR took the opportunity to remind providers of its guidance on the proper destruction and disposal of protected health information. In that regard, OCR reminds covered entities to have policies and procedures in place address ing the destruction and disposal process for the various forms of medical infor mation they receive or maintain. OCR also reminds covered entities to train in dividuals involved in the destruction and disposal of medical information on such processes and procedures.
While HIPAA does not dictate a certain destruction method, reason able methods of destruction should be utilized based on the form, type, and amount of health information to be de stroyed. OCR provides a few examples


16 • OCTOBER 2022 Birmingham Medical News
Grandview Physicians Plaza II is a state-ofthe-art outpatient companion to the nationally ranked Grandview Medical Center PHYSICIAN OFFICE SPACE AVAILABLE FOR LEASE 3680 GRANDVIEW PARKWAY | BIRMINGHAM, ALABAMA • PREMIER LOCATION Excellent visibility and accessibility on the campus of Grandview Medical Center • CUSTOMIZABLE OFFICE SPACE New Construction. Suites may be specifically designed for the unique requirements of each physician practice. • DESIGNED FOR CONVENIENCE Enclosed crosswalks provide easy access to and from Grandview Physicians Plaza I and Grandview Medical Center. Convenient parking immediately beneath the building for physicians; convenient surface parking for patients and staff. JIM ADAMS JADAMS@DANIELCORP.COM 205.443.4522 (OFFICE) | 205.515.3402 (CELL) II Disposal of Medical Information— It’s More Than Just Shredding (CONTINUED ON PAGE 18)
The Medical Assistant Dilemma
Staffing Shortages Require New Workforce Solutions
 By lynne Jeter
By lynne Jeter
Cone Medical Group reduced its turnover rate from 20 to 10 percent by starting its own program for certified medical assistants (CMAs). HealthPoint Medical Care shifted their medical assis tant (MA) responsibilities to nurse prac titioners (NPs).
Spurred by the COVID-19 pan demic, practices across the country are having to be resourceful to fill MA posi tions, with solutions varying from cutting clinic hours to building schools and focus ing on other roles. Part of the problem: candidates are demanding higher wages or don’t have the requisite experience.
“We’ve had many MA candidates ask for up to $30 per hour with little to no experience in healthcare, much less our particular specialty,” a practice man ager in Georgia said. “Since 2019, more than 70 percent of our candidates are failing to keep their interview appoint ment or even failing to submit a resume. And when we find suitable candidates, they often want to work four days a week at a higher pay rate.”
In a July poll by Medical Group
Management Association, 44 percent of practices noted that MA positions were the most difficult to fill, while 52 percent of medical groups are hiring alternative staff to cover MA roles: namely nonclinical staff, certified nursing assistants (CNAs), licensed practical nurses (LPNs) and registered nurses (RNs). Nearly half of respondents hire a combination of the four designations, and even EMTs and pre-med students.
With fewer providers and staff, some practices are forced to cut back
on scheduling patients, especially for extended hours and weekends. “There have been days that we’ve had to close the office early or block out certain pro viders due to being short-staffed,” said a Colorado practice manager.
Burnout because of the problem has led practices to cut corners else where. A practice manager in Louisiana just started letting the phone go to an answering service during the lunch hour. “That way, everyone can get a few min utes to decompress and have lunch,” she
said. “We also started closing the doors a couple of hours early on Fridays to lessen the strain on providers and staff. Lunches being brought in, ice cream parties, and gift cards only go so far.”
Cone Health Medical Group found a niche with its CMA academy, started in part because nearby community colleges and technical schools weren’t providing the clinical training CMAs require. “We were very blessed to be in a health system,” said Sally Hammond,

What’s important to you
Excellent defense
rates?
A “mutual”
“stockholder-owned”
Superior service from a personal, independent agent?
Birmingham Medical News OCTOBER 2022 • 17 205.447.1642 | V oltz P rofessional r isk . com We work for YOU, not the insurance company. A M O P R O B OS VOLTZ PROFESSIONAL RISK ADVISORS Put our 35 years of professional liability experience to work for you. Take advantage of our complimentary consultation to explore your medical professional liability options. With VOLTZ PROFESSIONAL RISK, you get all five!
in your Medical Malpractice coverage? A superior (A-Excellent) or better rated company?
attorneys with proven defense results? Competitive
company versus a
company?
(CONTINUED ON PAGE 18)
Disposal of Medical

proper destruction methods. Shred ding,
be ap propriate for paper records. Clearing or purging electronic media would be appropriate for electronic information. However, when it comes to disposal, OCR makes it clear that disposing health information in dumpsters, recy cle containers, or other trash bins that are accessible to the public is not an acceptable form of disposal when such information has not been rendered un readable or indecipherable.
In some instances, it may make sense to hire a third-party business as sociate to handle the destruction and disposal of the information. Using a third-party is acceptable, as long as you enter into a Business Associate Agree ment with the third-party and contrac tually agree to the destruction terms (e.g., that the vendor will destroy the in formation in accordance with applicable legal requirements).
In light of the most recent action by OCR, it would be wise to re-visit your
policies and procedures regarding not only the retention of medical information, but also the destruction and disposal of such information. Take this opportunity to train your employees on acceptable procedures for destroying and disposing of medical information in various forms. Otherwise, you could find yourself facing a similar $300,000 settlement with OCR.
Kelli Fleming is a Partner at Burr & Forman LLP practicing exclusively in the firm’s Health Care Practice Group. Kelli may be reached at (205) 458-5429 or kfleming@burr.com.
The
Assistant Dilemma,
assistant director of Cone Health Medi cal Group. “We probably had more of an opportunity to find folks who would like to do this kind of work.”
Meanwhile, a practice in Louisiana was experiencing something similar. The local community college was the gold standard for CMAs four years ago, producing top-level personnel. However, enrollment in the two-year program de clined and the community college lost its accreditation. Now administrators of the community college are reducing the length of the program to seven to nine months. What’s more, the practice has only been able to retain one new hire in the last year.
“I felt there must be a problem with our pay, our mission, our facilities, any thing that would explain why we are no longer able to staff this clinic,” the prac tice manager said. “But what I found out other colleagues were facing the same dilemma.”
HealthPoint Family Care has moved completely away from hiring MAs, fo cusing instead on NPs. Last September, the group initiated a formal program, providing an annual stipend for NPs as an incentive, while also extending ap pointment times to account for tasks MAs would have done.
A Leader in Healthcare Accounting





TOP 25
“NPs have the training and expe rience to do the work of MAs, such as administering immunizations and point of care testing,” said practice CEO Sally Jordan, adding that 80 percent of the group’s NPs are participating in the program. “When surveyed about going back to working with clinical sup port staff when the hiring challenges are gone, 100 percent of the integrated NPs said they would choose to continue to work without support staff. Many state they are more efficient working alone and the benefit of the additional income as reasons.”
HealthPoint also started a hybrid NP position for recent graduates, allow ing them to practice as an NP three days a week, while also training with a physi cian in a support role the other two days. The NPs involved in this program report high satisfaction rates. Within a year of starting in the hybrid model, NPs are ex pected to be fully blended into the new NP program, with added MA-type re sponsibilities, said Jordan.
Regardless of various solutions, the problem still lies in the lack of professional MAs, which impacts the bottom line.
“We all feel that we’re falling short of the high level of patient care and ser vice that we had before COVID,” said the Louisiana practice manager. “There simply is not enough support to perform at the standard that we’ve set for our clinic for years.”

18 • OCTOBER 2022 Birmingham Medical News 40 years of state-of-the-art surgical excellence performed with world-class skill. Specializing in Minimally Invasive Laparoscopic & Robotic Surgery 52 Medical Park Drive East #308 | Birmingham Al 35235 150 Gilbreath Drive | Oneonta Al 35121 74 Plaza Drive | Pell City Al 35125 3 LOCATIONS TO SERVE YOU 205.838.3025 | FAX 205-838-0411 | EASTERNSURGICAL.COM of
burning, or pulping would
Information, continued from page 16
Medical
continued from page 17
HEALTHCARE@CRICPA.COM | CRICPA.COM TRY
CPA FIRM
Questions to Ask When Considering Outsourcing Billing
By Bill CoCKrell
Having been involved in medical practice management for almost 40 years, I’ve seen the move from the old pegboard financial tracking system to today’s computerized patient account management systems. To attempt to manage the patient accounting and in surance claims systems of today’s world by paper would be a monumental task that would prove costly from both in direct and direct cost standpoints. The move to the electronic world of patient accounts management has opened the door to in-house or outsourced (full or partial) billing departments.
The decision to outsource the bill ing functions of a medical practice should be made only after carefully con sidering all the needs of the practice and the capabilities of any independent bill ing organization. It’s not for all medical practices and is affected in large part by the complexity of the practice in ques tion. If a practice is going to consider this step, here are some considerations:
• How does a practice keep from “losing control” of its billing department? In considering outsourcing a practice
should be sure that billing service has a convenient contact who can answer detailed questions and who is empowered to find solutions to problems. The practice should never feel that it has lost control of this function. The outside provider must offer services according to the guidelines of a practice.
• How will a practice know how well the outsourced service is performing? The servicing company should provide you with detailed reports on an ongoing basis as needed and should also review reports and results in a face-to-face manner. That might include in person (preferred) or
Civic Center Health & Rehabilitation
remote video contact.
• How is staffing handled? If a practice has an internal billing department, what happens to the staff? Will the billing company hire them, taking their cost and related benefits and H/R issues of the hands of the practice, or will the practice be responsible for transferring or outplacing staff?
• Where will the billing staff work? In today’s world remote work is feasible and cost-effective. However, that means there needs to be appropriate network security in place. In addition, when patients call with questions, can they have ready access to individuals who will communicate with them clearly and accurately?

• What services will be provided by the billing company and what services might be maintained internally? It is easy for an outside provide to handle claims filing and payment posting. However, who will enter charge, precertify testing and answer the phone when patients call with questions?
• What billing system will be used? Does the third party have a separate system that must be interfaced with or are the able to access, and understand,
the practice’s billing system?
• What are the follow-up services provided? It is easy to take electronic remittances and automatically post payments. However, doing that without a careful review of payment rejections might lead to unnecessary write offs of collectible money. In addition, feedback to the practice of why a payment is rejected so the practice can take corrective action, is critical to the success of any patient accounting process. Indeed, through economies of scale, an outside billing service may be able to provide high quality coders, billers and follow-up staff that exceeds the capabilities of an in-house department.
Outsourced billing can be of great value to a practice by improving pro cesses and saving staffing costs. The ques tions above are just some of the questions to be asked. Again, while work may be outsourced, the practice should never feel that it has lost control of this function.
Bill Cockrell is the Co-Founder and Chief Ad ministrative Officer at Medical Billing and Con sulting Services, LLC.

CaringFamilyforYours
Birmingham Medical News OCTOBER 2022 • 19 1201 N. 22nd St. Birmingham, AL 35234 205-251-5271 | Call us today for a tour! • Long-term care • Short-term care • 24/7 admissions • In-patient physical, occupational & speech therapies Serving the Birmingham Community for over 38 Years Our
Bill Cockrell



20 • OCTOBER 2022 Birmingham Medical News We’re di erent & proud of it! Celebrating 12 years of the only family-owned medical waste company in Alabama WESTMEDDISPOSAL.COM Our professional sta will help you lower your cost, lower your stress, and treat you like family! (plus they’re kinda cute!) • Medical waste removal • Secure document shredding • Pharmaceutical waste removal • Hazardous waste removal • Online compliance & training portal Contact us today for a quote 205.938.3333
Cheri Canon, MD is Honored
Cheri Canon, MD, pro fessor and department chair in the UAB Marnix E. Heersink School of Medicine’s Department of Radiology, has been named 2022 Ashbel Smith Dis tinguished Alumni Award recipient by the University of Texas Medical Branch at Galveston John Sealy School of Medi cine Alumni Association Board of Trust ees.

“It is such an honor to receive this award, to visit my alma mater, to recon nect with friends and colleagues, and to be surrounded by my family,” Canon said.
The ASDA Awards are the highest alumni honor given by the university’s John Sealy School of Medicine Alumni Association. Winners for this award were determined after an in-depth review by the ASDA committee based on recog nized contributions to the medical field and support for the high standards of excellence within the profession.
Ascension St. Vincent’s Birmingham and UAB Hospital Earn National Consumer Loyalty Award
Ascension St. Vincent’s Birmingham and UAB Hospital were among the na tion’s top 100 hospitals to receive the national Consumer Loyalty Award from NRC Health. Both organizations are the only in Alabama to receive the award. NRC Health’s loyalty-based hospital ranking recognizes the top 100 health care facilities that are working to cul tivate long-lasting loyalty among their patient populations.
“Ascension St. Vincent’s Birmingham is both humbled and honored to receive this national recognition. Our unique brand of healthcare is made possible by our people,” said Andrew Gnann, Ascen sion St. Vincent’s Birmingham President.
NRC Health used results from its na tional market insights study, which polled more than 310,000 consumers across the U.S. from April 2021 to March 2022. To qualify for the list, an organization had to secure at least 150 top-of-mind men tions from customers in the survey.
Cardiologists Join Alabama Cardiovascular Group



Longleaf, a new partnership between Birmingham Recovery Center and LIV Ventures, has broken ground on a pri mary mental health facility in Hoover. The new facility, Longleaf Wellness Cen ter, will be a partial hospitalization and intensive outpatient program with a ca pacity of 60 clients. The facility will be located next to Birmingham Recovery Center in the International Park off Ac ton Road.
2021. And prescriptions of naloxone to treat patients at risk of an opioid over dose rose 851 percent between 2012 to 2021 and 35.4 percent from 2020 to 2021.
UAB to Lead National Study in Trauma Patients
Alabama Cardiovascular Group, an af filiate of Grandview Health, has added three cardiologists.


Francis Benn, MD, cardiac electro physiology, earned his medical degree from the American University of Antigua – College of Medicine. He completed his internal medicine residency train ing at New York-Presbyterian Brook lyn Methodist Hospital / Weill Cornell Medical College. Benn completed his cardiovascular fellowship training at the University of Kentucky and his clini cal cardiac electrophysiology fellowship training at Ochsner Clinic Foundation.

William Black, MD, cardiovascular dis ease, earned his medical degree from the University of South Alabama College of Medicine. He completed his inter nal medicine training with Brookwood Baptist Health. After serving as chief resident Brookwood Baptist Health, he completed general cardiology and in terventional cardiology fellowships at the University of Tennessee.
Judson Colley, III, MD, MPH, cardiac electrophysiology, earned his medical degree from the University of Alabama at Birmingham (UAB) where he also completed his internal medicine resi dency. Colley completed both his car diovascular medicine fellowship training and cardiac electrophysiology fellow ship at the Medical University of South Carolina in Charleston.
Longleaf Breaks Ground on Mental Health Outpatient Facility
Birmingham Recovery Center, an outpatient drug and alcohol addiction treatment program, opened its doors summer 2021 and quickly identified ad ditional need for outpatient mental well ness services.
“Mental health and substance use disorder treatment options have been extremely limited in our state for too long,” said Thomas Harris, chairman of the Birmingham Recovery Center. Ac cording to Mental Health America’s 2022 State of Mental Health in America, Alabama ranked 50th out of 51 states on access.
Opioid Prescriptions
Continue to Decline in Alabama
It appears that increased awareness of the dangers of opioid misuse has made a difference in Alabama. The Medical Association of the State of Alabama was one of the first medical associations in the country to offer a continuing educa tion course to train physicians on safely and effectively prescribing opioids. Since 2009, more than 8,000 prescribers in Alabama have completed the course.
Opioid prescriptions in Alabama have decreased 41.6 percent from 2012 to 2021. From 2020 to 2021, opioid pre scriptions in the state declined 1.6 per cent, marking the eighth consecutive year the number of opioid prescriptions in Alabama has dropped. Likewise, the dosage strength of opioid prescriptions fell 52.7 percent from 2012 to 2021 and dropped 6.5 percent between 2020 to
& Vascular
to
The Center for Injury Science at UAB (CIS), together with the School of Public Health at the University of Texas Health Science Center at Hous ton, has been awarded $8.8 million by the National Institutes of Health to con duct a clinical trial in trauma patients.
The Trauma Resuscitation with Group O Whole Blood or Products, or TROOP trial, will compare two resuscitation strategies — one using whole blood, the other using component therapy — in trauma patients predicted to require large-volume blood transfusions.
Bleeding is the most common cause of preventable death following injury.
The traditional approach for treating injured patients who are bleeding is to transfuse multiple separate units of red blood cells, plasma and platelets — known as component therapy. However, recent evidence suggests outcomes are better when patients receive whole blood, instead of previously separated blood products.
TROOP is the first large-scale clinical trial evaluating whole blood in injured patients. The design of the trial was sup ported by a U34 planning grant from the National Heart, Lung and Blood Insti tute. The TROOP trial’s Clinical Coordi nating Center is based in the Center for Injury Science at UAB, and the Data Co ordinating Center is based in the School of Public Health, at UT Health.
The CCC’s principal investigators are Jan Jansen, MBBS, PhD, the director of CIS, and a professor in the UAB Division of Trauma and Acute Care Surgery and John Holcomb, MD, a CIS senior scientist.
Clinic
Birmingham Medical News OCTOBER 2022 • 21 Trust your Heart
Needs
Birmingham Heart
LEADERS SPECIALIZING IN Chest Pain & Hypertension • Cutting-Edge Minimally Invasive Therapies Watchman & Treatment of AFIB • Varithena Without Incision For Varicose Veins BHC Trussville 100 Pilot Medical Dr, Ste 300 | Birmingham 205.856.2284 BHC at Northside Medical Home 74 Plaza Dr, Ste 2B | Pell City 205.815.4818 BHC at St. Vincent’s Blount 150 Gilbreath Dr | Oneonta 205.274.3323 BHC Vein Center 100 Pilot Medical Dr Ste 185 | Birmingham 205.815.4800 BHC at St. Vincent’s Gardendale 2217 Decatur Hwy | Gardendale 205.518.7660 CALL TODAY TO SCHEDULE AN APPOINTMENT • BIRMINGHAMHEART.COM GRAND ROUNDS Cheri Canon, MD
Judson Colley, III, MD, MPH William Black, MD Francis Benn, MD
Jan Jansen, MBBS, PhD
Every Monday and Thursday, we’ll feature healthcare professionals discussing important medical topics. BirminghamMedicalNews.com In right sidebar, click on blog CHECK OUT OUR BLOG
Every spectrum of eye care.

At UAB Callahan Eye, we’re focused on providing vision-saving care at every level — from the only 24/7 eye emergency room in Alabama to daily primary care from expert physicians.
See the di erence at uabcallahaneye.org.
UAB Callahan Eye Opens New Clinic in Tuscaloosa
UAB Callahan Eye has opened a new clinic in Tuscaloosa, which is Callahan’s 18th clinic location in Alabama. Serving at the new clinic are providers Eric Sputh, MD and Michelle Langkawel, OD who have practiced in the Tuscaloosa area for several years.

The Tuscaloosa clinic offers comprehen sive eye care specialists with an on-site optical store. Patients will receive services
including family eye care, eye exams, cata ract evaluations, glaucoma screenings, cornea diagnosis and treatment, and con tact lens evaluations. All Callahan Eye pa tients are eligible to receive a 15 percent discount on all sunglasses and eyeglasses.
To schedule an appointment, patients can call or text 844-UAB-EYES. Same-day appointments are available. For more in formation, go to uabcallahaneye.org.
New Cooper Green Gains Final Approval to Begin Construction

The Cooper Green Mercy Health Ser vices Authority has received final approv al to move forward with plans to replace the current building with a state-of-theart medical clinic. With construction starting this winter, it will be built on the site of the former Cooper Green parking deck. The new five-story building will be 207,000 square feet with an estimated cost of $120 million.
The building will feature new equip ment along with an MRI. The amenities include an expanded rehabilitation suite with a covered outdoor section for devel oping outdoor skills such as navigating curbs and different ground surfaces.
A separate phlebotomy and injection
clinic will streamline laboratory visits and improve the vaccination process. The clinic areas will be designed to support team-based, multidisciplinary care, mak ing clinic visits more centralized for the comfort of the patients.
The facility will also incorporate natu ral light throughout the building. Oncol ogy infusion suites will feature windows in each treatment room.
The new building will have a gift shop, and food service options are being ex plored. It will house several other profes sional services, including Cahaba Den tal, the Recovery Resource Crisis Center, UAB Community Psychiatry and the UAB School of Nursing PATH clinic.
22 • OCTOBER 2022 Birmingham Medical News
24/ 7 EYE EMERGENCY ROOM GRAND ROUNDS
The new building will be 207,000 square feet.
The clinic is located at 1030 Fairfax Park in Tuscaloosa.
EDITOR & PUBLISHER Steve Spencer VICE PRESiDENT OF OPERATIONS Jason Irvin
CREATIVE DIRECTOR Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Laura Freeman, Lynne Jeter, Marti Slay
Birmingham Medical News
270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES:
Jason Irvin, 205.249.7244
All editorial submissions should be mailed to:
Birmingham Medical News
270 Doug Baker Boulevard, Suite 700-400 Birmingham, AL 35242 or e-mailed to: editor@birminghammedicalnews.com


All Subscription requests or address changes should be mailed to: Birmingham Medical News
Attn: Subscription Department 270 Doug Baker Boulevard, Suite 700-400 Birmingham, AL 35242 or e-mailed to: steve@birminghammedicalnews.com
Ascension St. Vincent’s Blount Opens Outpatient Wound Care Center
The new Ascension St. Vincent’s Blount Wound Center opened in September. The wound center treats patients with nonhealing wounds that require an advanced level of expertise, including wounds such as diabetic, venous and pressure ulcers.

Eric DuBois, MD, a general surgeon at Ascension St. Vincent’s, is overseeing the program. He and the staff of clinicians will develop an individualized care plan for each patient.
“The treatment of hard-to-heal wounds requires the unique care plan that comes from a dedicated wound center,” DuBois Said.
To make an appointment with a wound care specialist, call 205-274-3030.
Medical Association Awards $5,000 Minority Scholarship
The Medical Association of the State of Alabama awarded a $5,000 scholarship to Madison Hogans, a student at the Universi ty of South Alabama College of Medicine, to help pay the cost of medical school.

The Underwood Minority Scholarship Award is named in honor of Dr. Jefferson Underwood, III, a Montgomery physician who was the first African American man to serve as the Association’s president. Afri can American students who are already attending medical and osteopathic school or who have been accepted to school are eligible to apply for the scholarship.
Hogans was selected for her leadership, academic achievement, and desire to give back to her community.
“We are honored to present this scholar ship to Madison,” said Julia Boothe, MD, President of the Medical Association. “Af rican Americans are underrepresented in Alabama’s medical schools and the state’s physician workforce. The Underwood
Minority Scholarship aims to help diver sify that workforce to meet the health care needs of all Alabamians.”
Hogans graduated with a Bachelor of Science Degree from Auburn University.
A native of Dothan, she hopes to become a physician to serve her community. “ My goal is to make an impact on this world and make a valuable contribution to what the world needs,” she said.
Birmingham Medical News is published monthly by Steve Spencer ©2021 Birmingham Medical News, all rights reserved. Reproduction in whole or in part without written permission is prohibited. Birmingham Medial News will assume no reponsibilities for unsolicited materials.

All letters sent to Medical News will be considered Medical News property and therefore unconditionally assigned to Medical News for publication and copyright purposes.
Earn
a year!
Birmingham Medical News OCTOBER 2022 • 23
birminghammedicalnews.com FOLLOW US GRAND ROUNDS
Ascension St. Vincent’s Blount
ARMSA is administered by the Alabama Office of Primary Care and Rural Health and is supported by the Office for Family Health Education & Research, UAB Marnix E. Heersink School of Medicine For details visit https://aohw.org/2021-armsa or email ARMSA@uabmc.edu Apply for ARMSA today! Answer the call to practice in rural Alabama The Alabama Rural Medical Service Award (ARMSA) incentivizes primary care physicians and NPs to practice in rural, medically-underserved areas in Alabama. Eligible PCPs receive $50,000 a year and NPs receive $30,000 a year for up to 3 years as a service loan payable by years of service. PCP and NP must not have practiced in the rural area within 3 years of October 1, 2021. We’re looking for NPs in family medicine and for physicians in the primary care fields of: • family medicine • internal medicine • general pediatrics • general medicine/pediatrics
$50,000
(L to r): Jill Smith, Houston
County Medical Society who nominated Hogans; Hogans’ parents; Madison Hogans; Julia Boothe, MD
KNOWS
ANGLES



Driving business, practicing law. wallerlaw.com A partner in healthcare law that
all the
No representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. Contact: Colin Luke 205-226-5717. Waller is proud to be recognized as #1 in the South region in the ABA Health Law Section’s 2019 Law Firm Recognition List.
 By Jane eHrHarDt
By Jane eHrHarDt


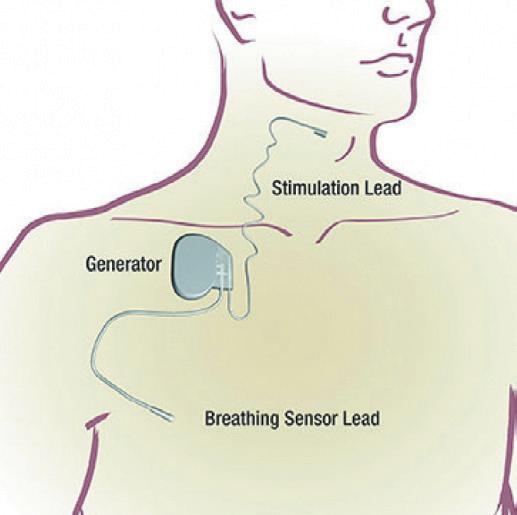
























































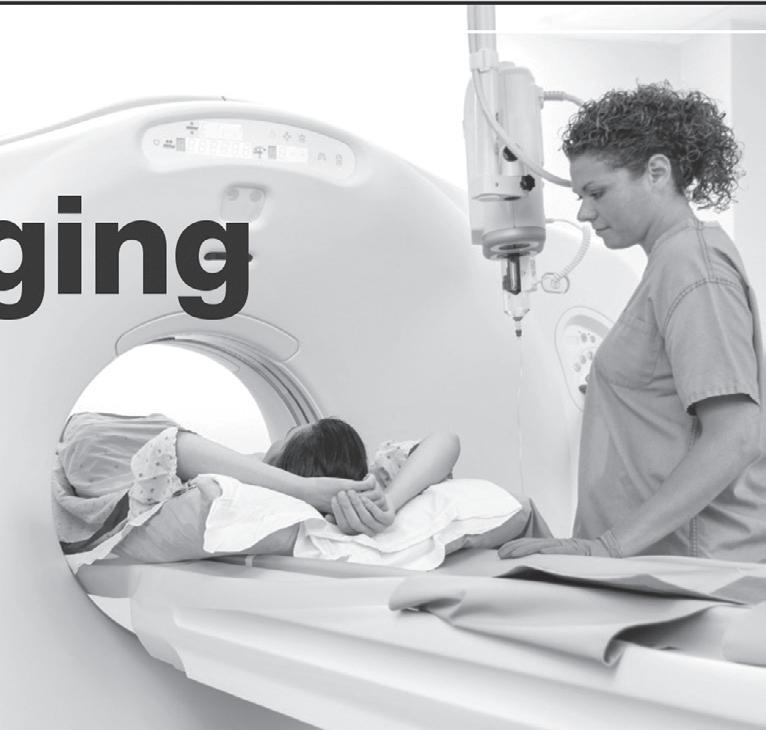































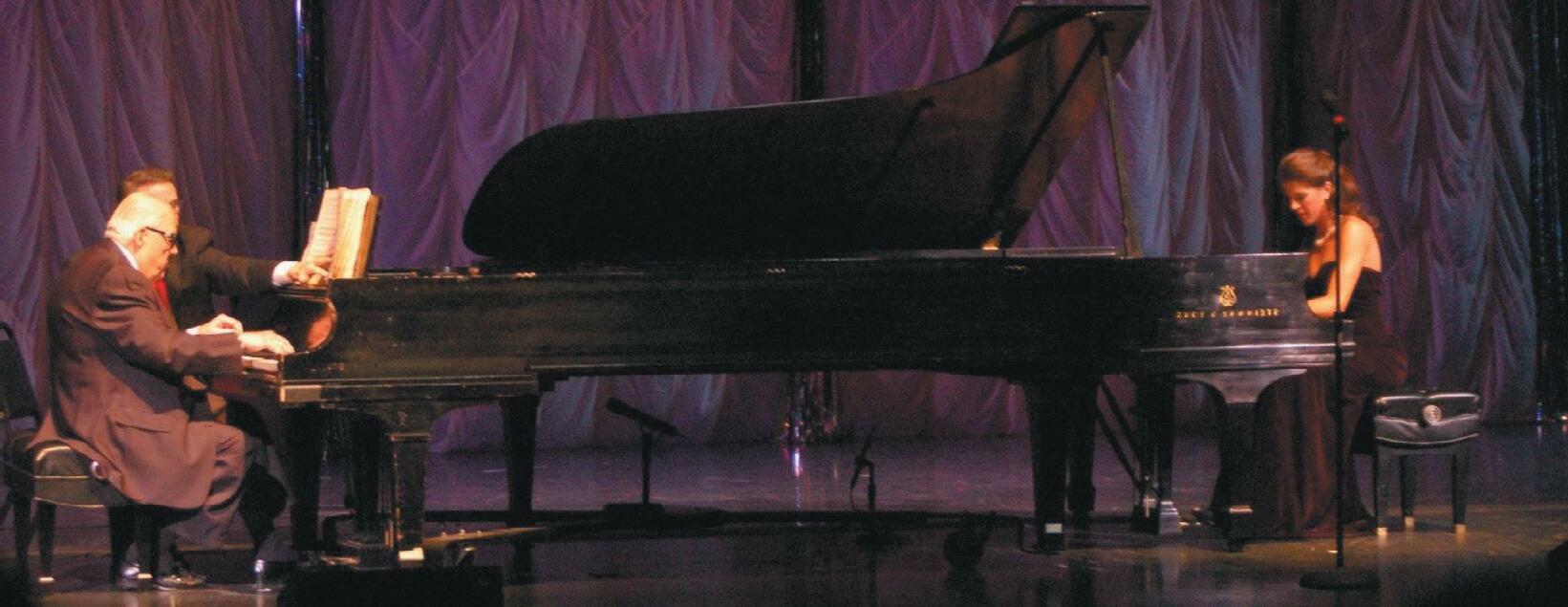


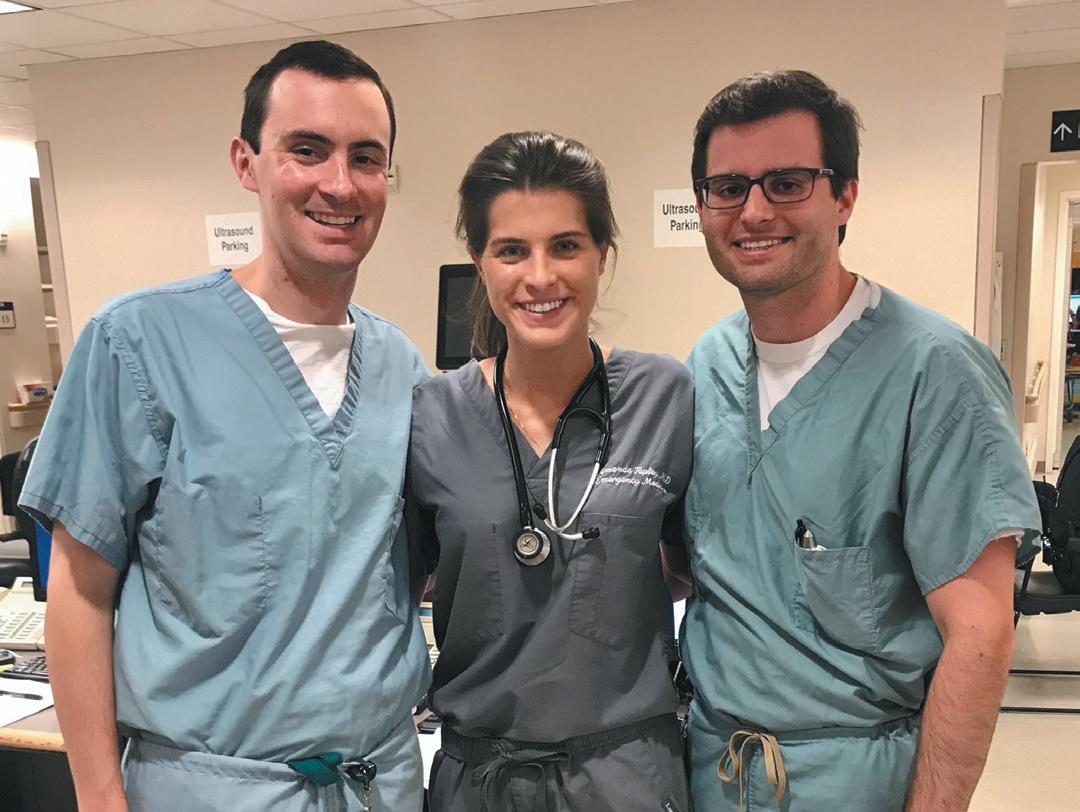








 By Carrie DouglaS anD ZaCHary trotter
By Carrie DouglaS anD ZaCHary trotter










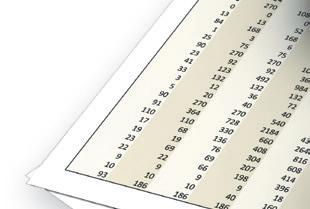







 By Marti WeBB Slay
By Marti WeBB Slay

























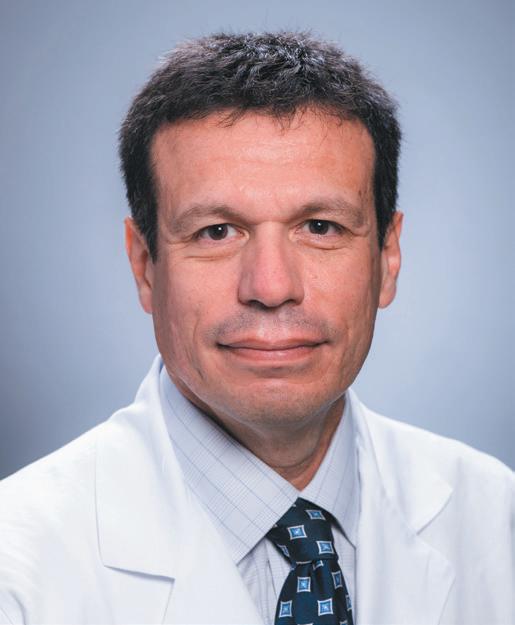













































 By lynne Jeter
By lynne Jeter