




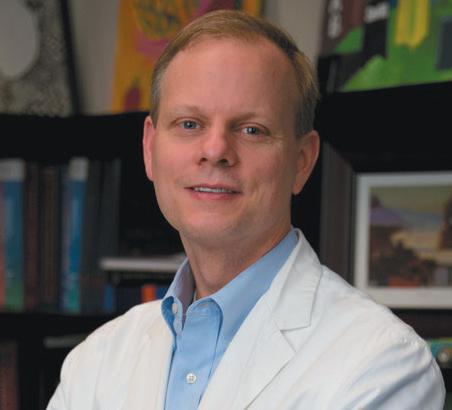
“We’re getting data on things we’ve never been able to measure before,” said Scott Appell, MD, the joint replacement surgeon who performed Birmingham’s first smart total knee replacement (TKR) in Birmingham at Surgical Institute of Alabama.
basis is significant,” Appell said. The device collects measurements throughout the day, producing a wellspring of data for surgeons versus reliance on observed data during physical therapy for a few hours a week.
Starting the second day after surgery, the device begins sending the readings. Using Bluetooth, it transmits the data to its home
The world’s first smart knee implant, the
The world’s first smart knee implant, the Persona IQ, is embedded with sensors and a telemetry system to allow for remote patient monitoring. Produced by Zimmer Biomet, the device automatically measures step count, average walking speed, stride length, and tibial range of motion.
Bluetooth, it transmits the data to its home base, which is about the
(CONTINUED ON PAGE 3)
“How much a patient is doing and what kind of progress they’re making on a daily
“How much a patient is doing




































 By Lauren Johnson
By Lauren Johnson
In March, Grandview Medical Center became the first hospital in Alabama to treat patients with brain tumors using Surgically Targeted Radiation Therapy (STaRT). This targeted therapy is for patients with newly diagnosed malignant brain tumors and recurrent brain tumors, including gliomas, glioblastomas, meningiomas, and brain metastases.
Through this radiation therapy, a GammaTile is implanted into the operative cavity within the last five minutes of brain tumor removal surgery, provid-
ing direct radiation that will delay brain tumor regrowth while protecting healthy brain tissue.
The GammaTile is a small white tablet, about the size of a postage stamp, that has titanium bars that will be radioactive for about 60 days. Over time, the white portion of the tile will resorb naturally, leaving the tiny pieces of titanium behind. Surgeons will typically implant one to four of these tiles in the operative cavity.
Usually, patients would need to wait two to four weeks before receiving traditional radiation after surgery, and they





At the heart of one of the most highly regulated industries in the nation, health care facilities and providers face challenges that draw attention and resources away from their mission to provide quality patient care.
Burr & Forman’s health care team works alongside you to address and anticipate your needs by providing preventative guidance and pragmatic solutions, enabling you to focus on providing care and achieving healthy outcomes.
Jessie Bekker
Howard Bogard
Richard Brockman
Kelli Carpenter Fleming
Jim Hoover
Catherine “Cat” Kirkland
Angie Cameron Smith

size of a modem stationed in the patient’s home. That securely routes the information to a HIPAA-compliant, cloud-based platform. It does not collect patient locations. The patient’s orthopedic surgeon can then securely access its objective, real-time data. Patients can view everything via a phone app, as well.
The device also sends alerts. “Most of the early alerts so far among my 15 implants are about an abnormally low range of motion,” said Appell, who practices at Grandview Medical Center. “Generally, the cause points to swelling or pain impeding their therapy. We can intervene then to help get the pain level and swelling down so they can get better motion, which is imperative in the early stages of recovery.
“Viewing their own daily metrics has stimulated patients to be more involved in their recovery. We’re a society of instant information, and this is instantaneous. People are fascinated with it. When some of my patients received an alert about their cadence or motion being suboptimal, they said it made them work harder to catch up and keep within the data norms. That early mobilization and early rehabilitation leads to better results, and that’s what this implant allows us to do.”
Early interventions can also help quickly reset the motor pattern that dictates a patient’s gait. “Our brain has a motor pattern it uses for the least painful, most efficient way to walk,” Appell said. “That gait becomes the default setting.”
So as the damaged knee becomes painful, that healthy default setting warps into a limping gait. Post-surgical recovery then requires the patient to consciously reactivate the healthy motor pattern to reestablish their normal gait.
The sensor’s consistent measurements based on actual movement can play an integral role in that recovery. “If we reestablish that default early on—and consistently—then that normal gait happens much sooner,” Appell said. “Intervening early allows you to get back to your normal walking a lot sooner, and
from page 1
that’s where the most benefit is.”
Another advantage to the flow of data straight to the patient’s orthopedic surgeon can mean fewer office visits. “Now you do not have to come to the office to check motion, so visits may not be required for simple things,” Appell said. That can be quite a boon, since most of the 1,500,000 knee-replacement patients each year are not able to drive for about a month. It also spares patients from missing work, finding child care, or having to travel longer stretches to reach their surgeon’s office.
The data flow does not continue forever, though. Daily transmissions last through the first year. The next year, it only sends the metrics for 36 consecutive days every quarter, which drops to annually during the next 10 years or until the battery wears out. That timeline totals slightly over two years’ worth of data.
Appell sees that data becoming even more useful once artificial intelligence becomes part of the assessments. “In 10 years, I think it will look completely different with the millions of data points that can be analyzed in milliseconds with AI,” he said. With the right algorithms, information could be generated about weight-bearing, pain, decay, and positioning, which could advance not just the devices themselves, but the guidance for successfully implanting them for greater patient satisfaction.
“The most unexpected thing about the smart knee replacement has been the verification through fact-based numbers,” Appell said. “Before surgery, the impeded walk and the painful limps are obvious. The view after the implant is a gamechanger. To me, it’s how people start walking better almost immediately, and that improvement in the first two weeks postsurgery. I could always see that difference, but now we have numbers. And numbers make everyone more comfortable.”



Hutton Brantley, DO | Raghuram Chava, MD Kristen Brown, MD (coming this fall)



“Year ago, when Radiofrequency Ablation Therapy (RF) was introduced, it was a major advance over trying to manage atrial fibrillation with only medications and the few other treatments we had,” UAB Chief of Cardiac Electrophysiology Tom McElderry, MD said. “However, it wasn’t perfect. Targeting the right tissue took skill, and there was always a risk of serious damage to the esophagus and nerves. Today, there is still a place for RF and other thermal tech in some applications, but now that the pulse field option is broadly available, I think it will become the treatment of choice in most cases.
“Around a decade ago, I began looking into alternatives to thermal energy ablation and became interested in research using pulse field technology. The big advantage was that it could be tuned to specifically target heart muscle tissue without risk to the esophagus and other tissue.”
In addition to participating in research as the pulse field technology was being developed, once it was ready to go

into clinical trials, McElderry performed the first procedure using the technology in in a human patient in Paraguay.
“As researchers studied atrial fibrillation and more was known about how it occurs, we saw that the electrical impulses that cause fibrillation often arise around the pulmonary vein and are conducted along it to the heart,” he said. “A key strategy in pulse field ablation is to isolate the area so there is no longer a pathway for impulses to travel. It’s a bit like the insulation around a power cord that lets you use it without getting shocked.”
Instead of the thermal energy used
in RF ablation, pulse field technology uses a series of high powered, short duration electrical pulses specifically tuned to disrupt the cells along the pulmonary vein.
“The targeted cells burst and empty into the surrounding area, which kills adjoining cells and starts to form an insulating barrier that will help to block fibrillation impulses,” McElderry said. Like thermal ablation, pulse field equipment works through a catheter. However, the system allows us to work faster than with RF. Procedures are usually same day and patients are ready to go home in the evening or before. Best of all, we don’t

We can change that.
We put you in touch with A.M. Best A-rated mutual companies at competitive rates. Then YOU get the dividend at the end of the year, not a stockholder. Put our 35 years of professional liability experience to work for you. Start today with a complimentary consultation to explore your options.
have to worry about an esophageal fistula or ulcer, or phrenic nerve injuries. In Europe, some procedures are done with conscious sedation, which allows patients to recover even faster. They can leave the hospital sooner, have something to eat and go home to rest and recover.”
The underlying causes of atrial fibrillation can be related to genetics, aging, hypertension, sleep apnea, obesity and other factors. What may start as a mild symptom can quickly become serious, interfering with the heart’s pumping ability and encouraging the development of clots that can travel to the brain and (CONTINUED ON PAGE 14)

med-mal Company





















As a combined EHR and PM system, Systemedx solutions and services optimize your practice’s effi ciency and accuracy with proven workfl ows and custom templates

Maximize Coding with Artificial Intelligence
Using Systemedx with AI for surgical coding stops those rogue surgeries from going unpaid. Proven to grow revenue more than $50,000 annually per surgeon through greater accuracy and fewer hassles for your coders.


Heighten Collections
Tap into our more than 20 years of billing experience to sharpen your collections process for the greatest possible outcomes.


Automate the Surgical Admin
Reduce mix ups, avoid oversights, and get paid faster through automatic tracking of every surgical process from the moment it hits the schedule until every payment is collected. Using the Systemedx Surgical Pathways solution, each device, piece of paperwork, person involved, and all the nitty-gritty details in between are tracked and validated for each procedure.

If your orthopedic practice is looking for optimal practice outcomes and revenue, call Systemedx today for a demonstration.




If you suffer from allergies or other ear, nose, throat or hearing problems, we don’t want you to treat your healthcare lightly or ignore symptoms that could lead to more serious issues. Call us now for a complete evaluation with one of our 15 board certified physicians, 4 highly trained and licensed PAs, or 16 clinical audiologists — all available to serve your needs at any of our 10 locations.

continued from page 1

could be required to have up to 30 treatments over a span of several weeks. The GammaTile gives patients another option.
“It’s more convenient for the patient,” said Henry Ennis, MD, a radiation oncologist at Grandview. “We generally have to hold off on radiation until the patient heals after surgery, which could allow some of the tumor to start growing back. If you’re able to put a radioactive source directly into the operative cavity at the time of surgery, then you don’t have that four-week delay.”
Ennis performed treatment for the first patient in Birmingham alongside neurosurgeon Elizabeth Kuhn, MD who was the first in the state to perform this surgery. Ennis also treated the second patient alongside neurosurgeon Phillip Cezayirli.
“One of the exciting aspects of this is that Glioblastoma Multiforme (GBM), which is a very aggressive tumor, is typically treated with surgery, then radiation, followed by chemotherapy,” Ennis said. “These tumors try to grow back in the area where the tumor resection was. Using GammaTile may be more effective because you’re getting a good radiation dose right where it needs to go, and you’re able to get that radiation started quicker. We’re also able to increase access for patients in rural parts of the state that don’t have a radiation machine in their backyard.”
A release from Grandview Medical Center stated, “Over 200,000 patients are diagnosed with an aggressive brain tumor in the U.S. each year. Aggressive brain tumors tend to be resistant to current treatments and have a high likelihood of recurrence.”
This therapy is shown to improve local tumor control, providing hope for patients battling aggressive tumors and extending their life. Patients are able to go to rehab sooner and can get on with their lives without worrying about more
treatment. Most patients also avoid losing their hair during treatment.
“This type of targeted therapy is not new to medicine, but it is relatively new to neurosurgery,” Cezayirli said. For brain metastatic disease, we don’t have to do any radiation after the GammaTile, necessarily, because we’re delivering all of the radiation there. For glioblastomas, we’re able to reduce the amount of radiation and the number of sessions required.”
Trials for upfront GBM haven’t been completed, but Cezayirli believes the outcome will be positive just like the first clinical trial was for recurrent brain metastases.
“The hypothesis is that delivering radiation immediately is better than waiting because the tumors aren’t waiting for your skin to heal,” he said. “Although the trial isn’t completed for GBM, I think that’s the most promising. It’s the most aggressive tumor that we have in neurosurgery where the average survival rate is two years or less.”
Studies have shown that the side effects from the GammaTiles are about the same as the traditional radiation treatment. “There was no statistically significant change in overall complications or side effects from the surgeries with GammaTiles or without,” Cezayirli said.
GammaTiles are a type of brachytherapy, meaning it’s delivering radiation through an implanted device, which is common for prostate cancer treatment. While GammaTiles were designed for neurosurgery, there are discussions going on about using them for spine and spinal cord tumors.
“Conceptually, it could certainly be used in other places. There’s no reason it has to be used for only neurosurgery,” Cezayirli said. “The limitation to how we use the GammaTiles is making sure we understand the physics of it in that location.”


The U.S. Department of Health and Human Services (HHS) Office of Inspector General (OIG), a top federal watchdog tasked with overseeing Medicare, Medicaid and other HHS programs, announced earlier this year that it will audit the Centers for Medicare & Medicaid Services' (CMS) nursing home survey practices, with a report expected to be issued in 2025. In its announcement, OIG recognized that prior OIG reviews of nursing homes "identified multiple issues related to the backlog of required nursing home surveys conducted by state survey agencies."
Federal standard survey requirements call for a skilled nursing facility (SNF) to receive a routine survey at least every 15 months. While CMS is responsible for the certification and oversight of most of America's nearly 16,000 nursing homes, including compliance with requirements for participation in Medicare and Medicaid, CMS has entered into agreements with states under Section 1864 of the Social Security Act, referred to as "1864 Agreements," which include delegating survey responsibilities to individual states.
Annual surveys are a key tool in evaluating nursing home quality of care, including fire and safety policies, distribution of medications, patient care, nursing home records, infection control, environmental conditions, dietary practices in the nursing home and more. Surveyor work is guided by a complex set of regulations that requires significant training. Survey teams are required to arrive
unannounced, and a typical survey will be conducted over three to five days, depending on the size of the facility. The survey team may conduct an extended survey if substandard quality of care is suspected and additional information is required to confirm or refute that finding.
Despite the 15-month requirement, survey backlogs have plagued the skilled nursing sector for years. A May 2023 report (2023 Report) from the U.S. Senate Special Committee on Aging confirmed that nursing home inspection agencies are "severely understaffed," noting that 32 state survey agencies report job vacancy rates of 20 percent or more. High turnover rates, driven largely by the inability to offer competitive salaries, present another major hurdle, especially given the significant time required to train a new surveyor.
According to the 2023 Report, "[m]ultiple states have noted it can take one to two years for surveyors to become fully independent." The survey backlog was further exacerbated by the COVID-19 pandemic, which included shutdowns as well as a temporary shift toward Focused Infection Control (FIC) surveys over standard routine surveys. Data from 2021 indicated that more than 70 percent of U.S. nursing homes went at least 16 months without a standard survey, with additional 2022 data indicating that more than 34 percent of facilities had gone more than two years without a standard survey.

The implications of missed surveys are far-reaching. Operators rely on regular surveys to help identify and correct potential issues at their facilities. Operators also count on a timely resurvey to show that identified problems have been
(CONTINUED ON PAGE 14)



HERE Join us as we face down those fears, uncover the harrowing truths, and keep you up with the ever-shifting threats and challenges being thrown at you by hackers and HIPAA.
















•
•
•

Our new podcast brings you straight talk in simple terms from an arsenal of experts who’ve faced the danger. Tune in to our YouTube channel and subscribe to get alerts as new episodes drop.







Surgeons at UAB are finding that the LINX® (Laparoscopic magnetic sphincter augmentation) is giving patients an option besides medication or laparoscopic fundoplication to treat reflux.
LINX is a magnetic device that is similar to a beaded bracelet that stretches apart and then, using the magnets, goes back into place around the esophagus. “Prior devices were fixed so they didn’t expand,” said Britney Corey MD MACM FACS, General Surgery Residency Program Director, Minimally Invasive GI Surgery in the Department of Surgery at UAB. “Over time, there was too much erosion into the esophagus or too much scar tissue. The idea of having magnetic beads was developed so that the beads could pop apart with pressure to let food pass and then come back together. That would protect you from reflux and keep that valve closed. Similarly, if you need to belch or vomit, your stomach can generate the pressure to pop open the beads.”
That ability to belch or vomit is one of the ways LINX can be preferable to the more traditional fundoplication sur-

gery in which the stomach is wrapped around the esophagus. Many patients have difficulty or the inability to belch or vomit following fundoplication which can cause bloating and discomfort. The tissue can also come unwrapped, causing the need for a return to reflux medicine in time.
The LINX device is inserted as an outpatient procedure, and patients must follow a diet of soft food, eating every

few hours, for several weeks after surgery. “Any time you put a foreign body into the body, it has a reaction and forms scar tissue,” Corey said. “Scar tissue will form around the LINX, and you don’t want that scar to get tight around the device. So it’s really important for those first few weeks that you regularly open the device. That means you are going to try and eat every two hours while you are awake. Often it’s just one or two tablespoons of food. And we want it to be soft, easyto-pass-through food. We aren’t confident liquid is enough, so it needs to be applesauce, yogurt, mashed potatoes, or scrambled eggs.
“It’s not necessary to wake every two hours to eat. You don’t have to set an alarm, but if you get up during the night


Our team of 15 board-certified physicians specializes in minimally invasive procedures to capture the latest in treatments with the most e ective outcomes for each patient.
WE ARE LEADERS SPECIALIZING IN:
• Chest pain & hypertension
• Peripheral Artery Disease
• Cutting-edge therapies
• Watchman & treatment of AFIB
• Venous disease & procedures
• Interventional cardiology including TVAR, TCAR, and EVAR procedures


to go to the bathroom, stop by the refrigerator and have a couple of spoonful’s of something. It’s physical therapy for the esophagus, exercising that opening.
“The scar formation is usually heaviest around the two-week mark. That’s when some patients have difficulty swallowing, and they have to work through that. They have to keep eating anyway and keep opening the device. Over time, the scar tissue will start to soften. Oftentimes we will prescribe a steroid dose pack to soften up the scar tissue.”
In order to be a candidate for the LINX procedure, patients cannot have an MRI over 1.5 Tesla. Most patients who qualify see an immediate improvement in reflux. “Sometimes it’s hard to appreciate that right away because you
(CONTINUED ON PAGE 14)


















































Three additional mental health facilities are opening in Alabama this year to provide alternatives for individuals who don’t require admission to a hospital psychiatric unit or infrequent psychiatrist visits.
According to a 2023 Forbes article, Alabama has the third-lowest number of mental health treatment centers nationwide and the second-highest percentage of uninsured adults with mental illness. With this in mind, leaders at Longleaf Recovery and Wellness want to make a positive change in Alabama’s mental health care community.
“I’ve only found one intensive outpatient program in the state for people with commercial insurance,” said John Giannetto, Founder and Chief Development Officer at Longleaf. “Once someone gets stabilized in the psych unit, they have limited options on where to go for aftercare. Because of this, they will often find themselves back in the hospital.
“There are a fair number of options for the lower frequency of care, and there are options for the much higher, intense level of care in, for example, a psych

stabilization unit,” Ian Henyon, Chief Operating Officer at Longleaf, said. “But there are no options in that middle tier, which we recognized a few years ago. So that started the idea to open this mental health wellness program.”
Longleaf was founded through a partnership between the Birmingham Recovery Center (BRC), which offers drug and alcohol addiction treatment programs, and LIV Ventures. The purpose is to bring additional outpatient
addiction and mental health treatment options to Alabama.
“From day one, our thought was we want to be more than just a treatment center,” Giannetto said. “We want to be part of the Birmingham community. So anybody struggling with mental health issues can call Longleaf and feel like they’re being heard, and taken care of.”
For patients outside Birmingham, BRC works with sober living facilities
around the state that provide transportation to the center Monday through Friday. Clients have also commuted to BRC from Tuscaloosa and Huntsville.
To address the shortage of mental health facilities in Alabama, Longleaf is opening new recovery centers in Madison and Baldwin County and a wellness center in Birmingham. The recovery centers will focus on substance use treatment by offering day and evening treatment, medication management and group/individual therapy. The Madison location will also include relapse prevention and withdrawal management services. The Birmingham wellness center will target mental health treatment.
“Madison County and Baldwin County are both growing rapidly,” Colin Harris, Founder and Chief Executive Officer at Longleaf, said. “And there was already a need in those communities before this growth was taking place. So there is a significant need in both locations.
“Each facility has a warm and welcoming environment, all the way down to the lighting. Our facilities don’t give off a clinical or sterile vibe. The goal is creating a place where our clients feel safe, that
(CONTINUED ON PAGE 15)

No matter your needs — large or small — with our a la carte, flexible menu of services, you get what you want, the way you want it. All provided by sta based right here in Alabama.
With MBCS, you have a convenient contact to wait on you with answers to your detailed questions and empowered to find you solutions. A local company, in your own time zone. We’re here to serve you, following your protocols, so you stay in control while we do the work. So you end up happy and satisfied.














Patients with chronic, non-surgical low back pain now have access to a minimally invasive outpatient procedure that can bring relief and rehabilitate the muscles of the lower back. The treatment stimulates the multifidus muscle using an implanted neurostimulator.
“Primarily this is for patients with axial back pain without significant radicular complaints. It’s for the patient who typically would have been treated with lumbar radiofrequency ablation,” said Christopher Paul MD, assistant professor in the UAB Department of Anesthesiology and Perioperative Medicine and medical director of the UAB Pain Treatment Clinic. “We’ve found an element of muscular dysfunction in the low back, specifically with multifidus muscles, which provide a lot of microstability to the spine.”
Paul distinguishes between surgical instability and microstability. Patients who experience low back pain while brushing their teeth, doing dishes or sim

deemed to not be a surgical candidate, this device could be an option for them,” Paul said. “The device is implanted in a 30 to 45 minute outpatient procedure under general anesthesia. There are two small incisions, and the device sits on top of the spine. It doesn’t go into the spinal canal, so the risk is less than with other implantable devices.”
While the device is relatively new in the US, it has been tested here and used in Europe long enough to publish three-to-
pain score at three years, and 67 percent had what is statistically considered resolution of back pain, less than 2.5 on that scale,” Paul said. “Also, about 71 percent of the people in that data study were able to eliminate or reduce their opioid use.
“There is nothing else out there that will restore or regenerate muscular function. Most devices are for palliation after surgery. Instead of covering up the pain, this aims to regenerate the muscle that has been atrophied so it’s a unique indication.
“It’s important for patients to realize they have to do their part following the surgery. An internal battery powers the system, and patients use a remote control to initiate a session that feels like a deep tissue massage. This is a therapy that requires active participation from the patient. They have to use it for two 30 minute sessions a day. It causes contractions in these atrophied muscles that have been disused. They must set time aside to run the programming.
“The treatment sessions are done at home. People are doing this at home, watching the TV, drinking their coffee.
there is an improvement in function. Fine motor movements start to come back as the muscle regenerates, but the pain relief tends to lag a little behind that. But over time the data would suggest the patients use this less and less as time goes on.
“Most patients when they hit the 12 to 18 month mark are using it maybe every other day or once a week or not using it at all, because they regenerate the muscle and they are able to use the muscle again. It’s patient driven. There’s a decrease in patient usage because they are getting better.”
UAB was one of the first hospitals in Alabama to perform this procedure, although other hospitals are now offering it as well. UAB has completed 10 procedures so far. “We did the first ones in October and those are having considerable success and doing well,” Paul said.
Paul expects the procedure will be more prevalent in future. “It’s really a matter of educating our referring physicians, particularly neurosurgical and orthopedic spine colleagues, that this is an option,” he said. “We want to work with our col












































At Cloud Willis, we analyze your legal issues using an add-value approach with an eye fixed on results. We combine seasoned legal advice with practical solutions to get you the best outcomes in an everchanging healthcare landscape.














Medical technology continues to evolve, and Brookwood Baptist Medical Center is walking in lockstep with that evolution. Our hospital is actively investing in robotics across multiple specialties, including gynecology, urology, general surgery, orthopedics and neurosurgery.
We have seen these investments lead to successful recruiting outcomes, as more and more physicians have come to Brookwood recently, eager to utilize our fleet of advanced medical technology. In early 2024, our hospital surpassed the mark of 15,000 robotic-assisted surgeries completed on the da Vinci Surgical System. In fact, Brookwood has completed more gynecological robotic-assisted surgeries on the da Vinci than any other hospital in Alabama.
Strong investment and utilization of robotic systems is a necessity for practice growth, and Brookwood is dedicated to that goal. New physicians who have joined the medical staff are already witnessing this effect.
Currently, the Mako Robotic Surgery System for hip and knee replacements, the da Vinci Xi Surgical System for gynecological and additional procedures, and the Mazor x Stealth System for spine procedures are all available to Brookwood patients. As the year continues, Brookwood is actively exploring ways to add to its robotics fleet.
In da Vinci robotic-assisted surgeries, small incisions are used to insert miniaturized instruments and a high-definition camera. A certified surgeon then views a magnified, high-resolution 3D image of the surgical site inside the patient. Computer and robotic technologies seamlessly translate the surgeon’s hand movements into steady, precise micro-movements of the instruments. Safety mechanisms ensure that the robot only moves under the control of a surgeon.

The Mako system is designed to enhance surgical accuracy when removing diseased bone and cartilage from a damaged joint, as well as when guiding the implant into place during hip and knee replacements.
Feedback generated by the Mako system helps the surgeon stay within clearly defined boundaries so that no healthy bone or tissue is inadvertently removed. Preserving healthy bone or tissue can result in minimal blood loss, faster post-operation recovery times, and less post-operation pain.
The Mazor X Stealth System is robotic technology that allows surgeons to perform procedures like general spine or brain surgery using several small incisions, instead of making a larger cut typically seen in traditional surgeries. It features a specialized guidance system for safe and accurate surgery no matter the complexity of the procedure performed.
Typical spine surgeries performed using the Mazor robot include treating complex spinal deformities, such as scoliosis. These procedures are completed by implanting pedicle, transfacet or translaminar-facet screws to provide stability in between bones during healing, osteotomies or surgical bone removal and biopsy, or extracting sample cells from patients for further examination.








The robotic instruments have a greater range of motion than the human wrist does, allowing surgeons more precision in making placements at the correct angle. Robotic systems can also hold instruments more steadily than the human hand. The systems arms can help surgeons get to areas of the body that are harder to reach than in traditional surgeries.
All of these factors can lead to patient benefits such as less blood loss, less postoperative pain and discomfort, and lower risks of infection.
Robotics-assisted procedures offered at Brookwood currently include hip and knee replacements, clolecystectomy, prostatectomy, hysterectomy, adrenalectomy, hemicolectomy, lobectomy, nephrectomy, hernia repair, gastrectomy, and appendectomy.
There can be some level of hesitation in patients, particularly when they are presented with the term robotic surgery. However, candidates for these procedures can rest assured the surgeon is in complete control, and is simply being assisted by the
(CONTINUED ON PAGE 15)


Edward Ferguson, MD, is double board-certified in general and cardiothoracic surgery with over 35 years of surgical experience. He graduated from LSU School of Medicine and completed a general surgery residency including a NIH cardiovascular surgery research fellowship at the University of Alabama at Birmingham followed by a cardiothoracic surgery residency at Baylor College of Medicine.


Dr. Ferguson’s areas of interest include:
• Structural heart disease
• Complex mitral valve repairs and replacements
• Transcatheter aortic valve replacement (TAVR)
• Coronary artery bypass surgery
• Atrial fibrillation surgery
• Lung surgery including lung cancer
• Video-assisted thoracoscopy
• Lung, pleural and pericardial disease


Dr. Ferguson is very pleased to return to the Birmingham area and is accepting new patients.




continued from page 4
cause a stroke, or move into the lungs and heart.
“Patients recently diagnosed with atrial fib are usually prescribed blood thinners to reduce the risk of clots. Testing usually follows and may include a halter monitor to determine the frequency and intensity of symptoms. As symptoms become worse, ablation becomes a consideration to discuss with the patient,” McElderry said.
Follow-up studies have shown that the effectiveness of the new option in both paroxysmal and persistent atrial fibrillation is comparable to thermal ablations when patients are checked 90 days post procedure after their bodies have had time to settle into what will be their normal rhythms.
The pulse field option has been released relatively recently, but it is generally
available in most areas and more cardiac electrophysiologists are being trained to use the new technology. Equipment used in performing the procedure is available from two different companies. As of now, costs for ablations done using the new option are slightly higher than those using older technologies, but there are also advantages in efficiency and safety. Insurance coverage should be reviewed and approved prior to the procedure.
“In some cases with other complexities to consider or unusual trigger areas, it’s possible that RF ablation may still have a role. However, the advantages of pulse field ablation are clear, offering an equivalent likelihood of successfully relieving symptoms without the risk of complications from a thermal injury to other tissues,” McElderry said.
continued from page 7 corrected. Consumers rely on regular surveys when making decisions about where they or a loved one might receive care, and lenders rely on surveys as part of underwriting financing transactions. Finally, providers that are unable to get resurveyed after making necessary facility corrections could face higher financing costs while waiting for updated survey results.
To combat the survey backlog, state agencies have increasingly relied on thirdparty contractors to conduct surveys. CMS itself uses contractors to conduct




its comparative state surveys to ensure compliance with the 1864 Agreements. The new OIG report questions whether CMS provides adequate oversight of the third-party contractors used by states in conducting these surveys in accordance with federal requirements. Although the report does not go into further detail, it is expected that OIG will be looking at third-party surveyors' training and qualifications, among other factors.
continued from page 9 are dealing with other side effects from the surgery like swelling or difficulty swallowing, but if you are going to have success, you are typically going to have it almost immediately,” Corey said.
The device is new enough to make it difficult to determine long-term results for LINX, but all the studies thus far have been promising. “In general, I still think it’s a very good option for the right patient,” Corey said. “The tricky thing is to define who is the right patient. We’ve had great success with patients who have small hiatal hernias, whose most persistent symptom is reflux, and who have normal esophageal function.”


LINX has proven overall to be better than medicines to treat reflux, and about the same for fundoplication, but without the side effects of that more traditional surgery.
“Since some patients with reflux will eventually develop esophageal cancer, having an additional treatment option is important,” Corey said. “Reflux is a big problem, and surgical therapy should never be the first-line treatment, but in patients who have failed medical therapy and made all the lifestyle modifications and are still having reflux, it can really improve their quality of life. It’s always helpful to have options for patients, and that’s what excites us about this.”




















continued from page 10 they enjoy being at, a place that makes them feel worthy.”
To become a client, a person would call the number on the website, where someone from the admissions team will ask questions about basic demographics, collect insurance and perform an overthe-phone assessment. Giannetto said there are no hidden costs throughout the entire process at Longleaf. If the individual is a good fit for Longleaf, their goal is to get them into treatment the following day. The center has working relationships with other training facilities, so if Longleaf is not the right fit for a potential client, they will find somewhere that is.
“There’s a big customer service orientation. Making sure that people have all of the information that they need in order to feel comfortable with treatment,” Henyon said. “We want to make sure our staff
approaches them in an empathetic manner. Another piece is our medical component. We’ve invested heavily. These pieces are not inexpensive to maintain, but our clients deserve this, and it’s needed.”
The Birmingham Wellness Center is slated opened in April with the Madison County opening scheduled for May 15. Finally, Longleaf Baldwin will open at the beginning of July.
For Henyon, Harris, and Giannetto, this project is driven by passion, stemming from their shared experiences of undergoing treatment in Alabama and other states, where limited in-state options made them seek help elsewhere.
“The options that we have had historically has not been the highest quality. We want to raise the bar not just in Alabama but across the industry as a whole,” Harris said.
continued from page 11
“There is a little correlation between the degree of atrophy and how fast they respond to the therapy, but subset analyses of the study groups do not show any benefits to younger patients vs. older patients. The Medicare population per-
formed equally as well on this.
“The data is very encouraging, and I am very excited about this in terms of improving long-term outcomes of our patients.”
continued from page 12
advanced medical technology at his or her disposal. Like all surgeries, there are risks to robotic-assisted procedures, but the minimization of incisions, coupled with improved accuracy provided by the machines, can make it easier to identify bleeding or other complications earlier than in traditional surgery.
All in all, robotic surgery has been an extremely positive development in healthcare, and Brookwood is committed to furthering our investment in these exciting technologies.
Recent and future planned investments in the robotics field represent
Brookwood’s continued commitment to utilizing advanced medical technology. We’re proud to offer these procedures to our community and look forward to many more successful procedures going forward.
For more information on roboticassisted surgeries at Brookwood Baptist Medical Center, please visit www. brookwoodbaptisthealth.com/services/ general-surgery/robotic-surgery
Jeremy Clark is the Chief Executive Officer of Brookwood Baptist Health and Brookwood Baptist Medical Center.
We have two clinic locations, in Birmingham and Bessemer, so patients have the option to choose the closest location for them.
We’ve made referring easy by contacting and scheduling patients quickly and keeping you informed on their treatment plan.
We provide a comprehensive treatment plan for patients, offering the most up-to-date and innovative treatment options.
•
•
reimburses about $60 per patient per month for 20 minutes of staff time of chronic care management on patients with 2 or more high risk conditions. Tasks your staff already performs qualify for that reimbursement, such as PAs, prescription re lls, referrals, arranging home health/DME, and more. These can add up to 20 minutes of staff time per month, with no of ce visit required, which could mean—


Even better, the bulk messaging feature of our software allows your staff to engage with hundreds of patients simultaneously versus spending hours on the phone with one patient at a time.
CCM can be used in Internal Medicine, Primary Care, Cardiology, Psychiatry, Nephrology, and many more.

Under certain circumstances, Medicare allows physician practices to bill eligible non-physician practitioners (NPPs) under a supervising physician’s provider number and at 100 percent of the supervising physician’s allowable rate. This sort of arrangement is known as “incident to” billing in the Medicare world because the NPP’s services are “incidental” to the physician’s diagnosis and treatment plan for the patient. “Incident to” arrangements help promote productivity within a practice and reduce wait times for appointments. However, because “incident to” arrangements enable a higher reimbursement rate for NPPs, the arrangements can be fraught with compliance risks.
Generally, Medicare requires the following be met for compliant “incident to” billing:
• The physician must initiate treatment and diagnose a patient first.
• The physician must continue to participate and manage the patient being treated by the NPP.
• The NPP’s service must be an integral, though incidental, part of the service of a physician (or other practitioner) in the course of diagnosis or treatment of an injury or illness.

• The NPP’s service must be commonly rendered without charge or included in the physician’s bill. For example, if a service has its own benefit category under Medicare, the service should be billed under that benefit category, not under an “incident to” arrangement.
• The NPP’s service must be the type commonly furnished in a physician’s office or clinic.
• Services must be furnished under the “direct supervision” of the physician. Direct supervision requires that the supervising physician be physically present in the same office suite as the NPP at the same time the services are being provided (i.e. the physician could immediately come assist if needed). Beyond immediate availability and physical presence, direct supervision
also requires the physician to actively participate in and manage the course of treatment for the patient. As of 2023, certain behavioral health services may be provided under the “general supervision” of a physician, which does not require the physician’s physical presence while the behavioral health service is being provided by the NPP. This flexibility is limited to only a select number of behavioral health services.
• NPPs must provide services within the scope of their license under state law and the NPP must be employed or contracted.
When a practice believes it may have inadvertently violated “incident to” regulations, that practice should seek legal guidance and as appropriate, self-report the conduct to the Office of Inspector General (OIG). The OIG publishes its self-disclosure settlements online and several recent “incident to” cases stand out as examples of the potential penalties involved with “incident to” violations.
In February 2024, a gastroenterology and hepatology practice agreed to pay nearly $400,000 after the practice self-disclosed that it had billed services provided by advanced care practitioners as “incident to” the practice’s physician services, but those services failed to meet the requisite requirements. Spe-
cifically, the practice’s advanced care practitioners provided initial diagnostic and treatment services for new patients. Similarly, in November 2023, a primary care group in California agreed to pay over $1 million dollars after the OIG discovered the practice billed claims as “incident to” a physician’s services, but the physician did not remain actively involved in the course of treatment. In yet another example, a California gastroenterology practice agreed to pay nearly $1.8 million dollars in June 2023 because its NPPs billing under an “incident to” arrangement were not properly credentialed with Medicare, Medicaid, and Tricare.



On the other end of the spectrum, purposefully violating “incident to” requirements can lead to federal criminal charges. In early April 2024, an Arizona physician plead guilty in federal court to healthcare fraud. In this case, the physician operated a mobile medical practice that treated patients in their homes. The physician dispatched NPPs to the homes of his patients and billed those services as “incident to” his own. As the physician was not physically present or immediately available for the home-based services, the Department of Justice (DOJ) alleged the use of an “incident to” billing arrangement was inappropriate. The DOJ also determined that the physician had purposefully disregarded written advice from auditors and thirdparty commercial payors about his improper billing practices.
The above cases and regulations center on Medicare-related billing issues, but physician practices must also be aware that “incident to” billing requirements may vary from payor-to-payor. Some payors do not allow “incident to” billing at all. Some payors allow “incident to” billing, but only for very limited NPPs. Assuming that every commercial plan follows Medicare guidelines is illadvised. The best practice is to ask each payor for their “incident to” guidelines and craft billing policies (including clear policies on supervision documentation) accordingly.
Catherine (Cat) Kirkland is a Partner at Burr & Forman LLP practicing exclusively in the firm’s Health Care Practice Group. Cat may be reached at (251) 340-7272 or ckirkland@burr.com.






You deserve results. Not headaches.


Warmer weather isn’t the only gift summer brings. Along with the buzz of summer break comes a rush of graduating providers and physicians who are eager to start the next phase of their career.

Summertime is when many healthcare organizations hire a new resource to join their busy team, and physician and provider enrollment with insurance payers is an essential component of the onboarding process. Kassouf’s credentialing specialists can manage the credentialing and enrollment process from start to finish, helping you avoid the headaches this time-consuming project can cause. Our team of experts leverages years of experience to make the process as efficient as possible, while our advanced credentialing software efficiently and accurately completes applications.
Let us manage the enrollment process for you so you can focus on your practice. Contact us today to schedule a software demo and discuss how we can help you with your provider enrollment needs.
“I brag all the time on the great job you all did. To get up and running as quick as we did was truly remarkable, and I believe that was because you guys cared and appreciated our sense of urgency. Honestly, I don’t see how we could have done this on our own. We are truly grateful for you all.”
–Owner & Physician, Obstetrics & Gynecology


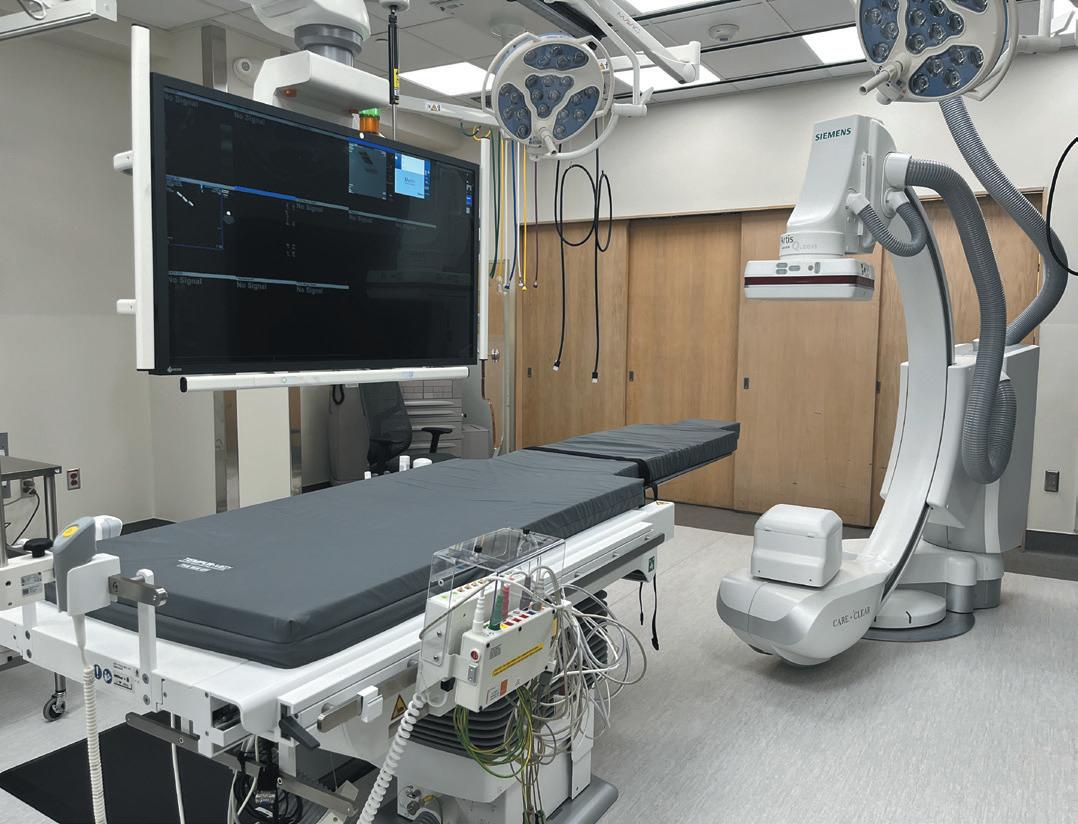
In April, Ascension St. Vincent’s Birmingham opened a new electrophysiology (EP) lab, a $3.2 million renovation project that is part of a $13.4 million investment in cardiology enhancements across the system. This is the second EP lab at the Birmingham campus.
“This space was designed with the focus of delivering the safest, most effective arrhythmia care for our patients,” said Ibrahim Hanna, MD, electrophysiologist at St. Vincent’s Birmingham.
Hanna joined St. Vincent’s in Fall 2023 as the second interventional cardiologist specializing in electrophysiology. Since his arrival, the hospital has doubled the amount of EP related procedures, to roughly 90 a month, making the completion of a second lab important to meet the needs of the community.
Kassouf Healthcare Solutions is celebrating their 25th anniversary this month. While the official anniversary is 25 years, the company became Kassouf Healthcare Solutions in 2014 when it acquired the former Retina & Vitreous Associates (RVAA).
“Reaching this milestone is a testament to our team’s client-centered mindset, and their trust in our services. We look forward to continuing to serve our clients for many years to come,” said Kassouf Healthcare Solutions Executive Director Jeff Dance.
Kassouf Healthcare Solutions was created to enhance the business side of medicine, allowing doctors time to focus on their patients. Services include accounting, human resources, management

and consulting, revenue cycle management (RCM), and information technology.
The organization was nationally recognized as a Top Revenue Cycle Management Provider by HealthcareTech Outlook. Kassouf Healthcare Solutions was also honored as one of the best Alabamabased human resources companies by BestStartup.
Kassouf Healthcare Solutions is part

of the Kassouf Family of Companies; all are tied to Kassouf CPAs and Advisors, which was founded in 1931.
“It has been amazing to witness Kassouf Healthcare Solutions’ success. Kassouf’s niche services for healthcare providers complement KHS’s offerings so well, allowing both companies to offer exceptional client service,” said Kassouf Managing Partner Jonathan Kassouf.

Our professional team of doctors, nurses, and staff look forward

The American College of Radiation Oncology (ACRO) has created a new scientific journal, and named Christopher Jahraus, MD, physician at Generations Radiotherapy & Oncology PC in Alabaster, to help lead the editorial team. Jahraus will work with senior editor, Jessica Schuster, MD from the University of Wisconsin. The two editors have begun to identify individuals from a range of universities and private practices throughout the U.S. and Canada to lead teams with oversight of manuscript publication. The journal will focus on clinical cancer care, and other aspects of practice in radiation oncology.
“I hope my involvement with the ACRO journal for up-to-the-minute cancer research brings useful data to my colleagues, along with a new sense of confidence in the quality of care community oncologists bring our patients every day,” Jahraus said. Jahraus has been in practice in Alabaster for 15 years, and acquired Generations Radiotherapy & Oncology PC in 2012.

Noland Health Services has named Barbara Estep as the new president and chief executive officer. She has been with the company since 1987 and most recently served as Vice President over administration. She replaces Carol Knight, who had served as CEO since 2018 and retired as of March 31.
Noland Health operates across Alabama with five long-term acute care hospitals and nine senior living communities that include facilities for skilled nursing, assisted living and specialty care assisted living, as well as independent living apartments and a long-term care pharmacy.

Steve
Katy Barrett-Alley
CONTRIBUTING WRITERS
Jane Ehrhardt, Ashley Franco, Laura Freeman, Lynne Jeter, Marti Slay
Birmingham Medical News
270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110
AD SALES: Jason Irvin, 205.249.7244
editorial submissions should be e-mailed to: editor@birminghammedicalnews.com
Brookwood Baptist Medical has received delivery of its fifth da Vinci Xi Surgical System, a robotic system for gynecological and additional procedures.
Installation of this latest system adds to Brookwood’s existing robotic surgery fleet, which in addition to four l da Vinci Xi systems includes a Mako Robotic Surgery System for hip and knee replacements and a Mazor x Stealth System for spine procedures.



The Alabama State Board of Medical Examiners has new leadership and two new members.
Max Rogers, MD of Mobile was elected as the new Chair of the Board and Hernando Carter, MD was elected Vice Chair on Saturday.
Rogers was commissioned into the Marine Corps after graduating from the Virginia Military Institute and became a fighter pilot. He then graduated from the University of Alabama School of Medicine, and returned to Mobile in 1998, entering private practice in Obstetrics and Gynecology.
Carter practices Internal Medicine in Birmingham. He also founded Prescription for Better Living, a non-profit that promotes health careers to those from underrepresented backgrounds. He received his undergraduate degree from Morehouse College and his Medical Degree from the University of Alabama School of Medicine.
In addition, two new members were elected to the Board: Adam Harrison, DO and William Schneider, MD. Harrison received his Doctor of Osteopathy in 2010 and completed his residency in Family Medicine at Huntsville Hospital through UAB. He is a partner at Cullman Internal Medicine.
Schneider joined the Huntsville Cardiovascular Clinic in 2011. He attended medical school at Case Western Reserve University and completed an Internal Medicine residency at Barnes-Jewish Hospital.

At Pulmonary Associates of the Southeast, we get your patients in sooner. Because sooner is better when someone is struggling with lung function, sleep, asthma, or other critical care conditions. That’s why we make referrals as easy as possible to get your patients in and on their way to feeling better.

With the largest healthcare practice in the country, Holland & Knight has more than 400 experienced attorneys covering virtually every segment of the healthcare industry, from transactional matters, regulatory compliance and real estate to litigation, government enforcement and public policy issues.
Our dedicated healthcare attorneys and professionals – in Birmingham and throughout the country – have the insight, experience, depth and resources to help promote and protect your interests.