Birmingham Hospitalist in Iraq






































 By laura FreeMan
By laura FreeMan
The 20-year mark is when most military personnel think of retiring to civilian life. After 21 years in the Air Force, Ronald Roan, MD returned to the Army with the goal of completing another 20 years where his dual careers in medicine and the military began as a medic in 1990. As chief of staff at the Baghdad Diplomatic Support Center’s Level I Trauma Center, Roan’s latest deployment was in Iraq.

CARDIOLOGY
Dogs are heroes too.
“We cared for both American and coalition forces serving in the region. In addition to patients from Iraq, we saw cases flown in from Syria and Jordan. After the war, most of the cases we see have been either medical or non-combat trauma,” Roan said.

“In addition to patients from the U.S., many

(CONTINUED ON PAGE 4)
UAB Cardiogenomics Clinic Helps Patients with Inherited Heart Disease
By SteVe SPenCer
Back in the early 2000s when Pankaj Arora, MD was training in population genomics at the Massachusetts Institute of Technology’s Broad Institute, he got his first inkling of the possibilities that genetic testing could do for medicine. “Those were the early days of genome-wide association studies, where we realized that we could scan through the genomes of individuals in an unbiased fashion to look at genetic variations contributing to a disease,” he said.
Years later, he put his vision to work with the founding of the UAB Cardioge-
nomics Clinic in 2021. The clinic, which is just one of two in the southeast, provides patients with a cardiovascular assessment that includes genetic testing, genomic counseling, and a personalized treatment plan for patients who are at risk of inherited cardiovascular diseases.

“Inherited cardiovascular conditions include abnormally high cholesterol, cardiomyopathy and arrhythmias. Many of these conditions can be managed through screenings, follow-ups, prevention and other treatment options,” said Arora, who serves as director of the Cardiogenomics Clinic.
The clinic sees referral patients from
(CONTINUED ON PAGE 4)
FOCUS TOPIC CARDIOLOGY SERVING A 24 COUNTY AREA, INCLUDING BIRMINGHAM, HUNTSVILLE, MONTGOMERY & TUSCALOOSA FEBRUARY 2023 / $5 www.birminghammedicalnews.com FOLLOW US STOP EXPLAINING HEALTHCARE TO YOUR IT EXCLUSIVETOHEALTHCARE|ENTERPRISEIT&CLINICALIT|TEAM-BASEDAPPROACH SIMPLIFIEDMED.COM 205.366.3565
Ronald Roan, MD in Iraq.
Pankaj Arora, MD confers with a patient.






2 • FEBRUARY 2023 Birmingham Medical News Our firm works with all types of health care clients on business, regulatory, and litigation matters, covering every aspect of the industry. Burr & Forman’s regional health care group includes over 40 attorneys across the southeast. No representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. 350 Attorneys. 19 Offices. Results matter. We care about you. Burr.com Howard E. Bogard Richard J. Brockman Kelli Carpenter Fleming James A. Hoover Catherine “Cat” Kirkland Robin B. Mark Lindsey Phillips Angie C. Smith 420 North 20th Street, Suite 3400, Birmingham, AL (800) GET-BURR No representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. Alabama Health Care Team Birmingham, Mobile, Montgomery
Value Based Care Model is Reinventing Primary Care










 By Jane ehrhardt
By Jane ehrhardt

By 2030, CMS aims to change most Medicare fee-for-service beneficiaries to a value-based care (VBC) program. That means Medicare will reimburse providers and insurers based on the benefits of the care given to the patient rather than the volume of services provided. “Value-based care is kind of a misnomer. It’s really about better care for the patient,” says John Farley, MD, medical director with Complete Health.

The primary care group’s VBC model centers on the 27 million or so people in the nation enrolled in Medicare Advantage plans. At their 16 practices, Complete Health works with the commercial insurers who offer the plans, such as Viva, United and Cigna, to take over the risk of managing the cost of care for those patient. For each patient, Complete Health receives 85 percent of the lump sum from Medicare designated toward healthcare. The insurers keep the other 15 percent.
Whatever monies remain after care, Complete Health can keep. If costs go over that 85 percent, it comes out of the company’s pocket. “The only way to have money left over is to take better care of the
patients,” Farley says, because Medicare also pays based on whether parameters indicate better outcomes, such as hospital readmission rates, star ratings, and ordering preventive tests.

The extra monies are shared with all their providers and to pay for the additional services to keep the patients healthier. Those services focus on engagement and convenience for the patient. “We want to keep them out of the hospital,” Farley says. The nine Birmingham locations open at 8:00 a.m. with one offering Saturday hours along with an urgent care clinic in Pell City open on the weekends. All promote same-day and next-day appointments, with walk-ins at the urgent care clinic.
“You keep patients out of the hospital and emergency room by being available,” Farley says. “So we employ 45 care management nurses in Birmingham to engage with our sickest patients as frequently as they need to by calling or checking in on them. Patients seen in the clinics receive a call 24 hours after a visit to be sure they’re feeling better and have their prescriptions at-hand.
“Our motto is, see us first and we’ll get you seen, whether it’s virtual, personal, or a home visit. We send someone on house visits to












The journey to mend his heart led






certain patients every week, not only for their health, but so they don’t feel the need to visit the ER to seek companionship.

When specialists are needed, patients are referred to Complete Health’s preferred network of specialists. The network helps mitigate costs that have become a mainstay of the feefor-service model specialists rely on for revenue. “For instance, do all patients need a chest x-ray before surgery? Science says no,” Farley says. “So we do less of those.
“All the money we earn comes from fixing the broken system. If a patient calls with UTI symptoms, they’re not sent to the ER because no appointments are available. We see them that day and dispense their medicine in the clinic or we have two nurse practitioners who can come to their house and see them. It’s about being proactive.”
Farley, who works out of the Florida headquarters, did a ride-along for a home visit in the west end of Birmingham. “The patients were so grateful to not have to come to the office,” he says. The company also perform mobile labs, ultrasounds, and x-rays.
The model has worked, and the resulting profits have created an additional revenue stream for their providers. “Our doctors typically make more than they did before they joined us, because we’re sharing the money






with them that typically goes to the insurance company,” Farley says.



Three weeks ago, he distributed $1.5 million made by following their VBC model to their 25 providers in Daytona and 89 in Birmingham, including nurse practitioners. “Some doctors can make an additional $45,000 twice a year,” Farley says. “If you want to slow down, get paid better and focus on taking better care of the patients you already have, then you can do that.”


Between their Daytona and Birmingham locations, Complete Health now cares for more than 100,000 patients, of which 20,000 are enrolled in a Medicare Advantage plan with 6,500 of those under varied ACOs. The remainder are on traditional Medicare, Medicaid or are commercially insured patients. “Since we have these extra services, all of our patients benefit from them,” Farley says.
A fourth generation physician, Farley sees this value-based care model as a way to reinvent primary care. With its new revenue stream increasing income without increasing volume, it could help to end the primary care physicians shortage and lessen burnout. “Because we can pay our providers more based on managing a patient population well rather than on how many patients they see every day,” he says. “This is an evolution.”
Qua was born with tricuspid atresia that required a series of open heart surgeries as an infant. But as a teen, his health took a dramatic turn. Qua’s pediatrician and cardiologist recognized something wasn’t right with his heart and sent him to Children’s of Alabama. Our team was standing by when he arrived by helicopter, and within two weeks he received a new heart. He rebounded quickly and was back at home a few weeks later, thanks to the expert heart team here at Children’s of Alabama.


Birmingham Medical News FEBRUARY 2023 • 3
Qua Heart Transplant Survivor Learn more at ChildrensAL.org/heart
John Farley, MD
in our care were coalition soldiers from Spain and Poland. We also helped with medical care of local residents when we could.
“On this deployment, I also learned something new—how to treat canine soldiers who are ill or injured. The Malinois Belgian shepherds are beautiful dogs and have a very important role. In addition to guard duty and searching for explosives, they are often first in when dangerous situations arise. A great deal of training and a major investment in time and money is required to prepare the dogs for the essential work they do. There are also strong bonds between the dogs and their handlers. When a dog needs
care, we do everything possible to save it and get it healthy again. That includes learning to do transfusions from dog to dog.”
Roan came home from deployment in Iraq just before Christmas and returned to his role as a hospitalist the day after.
“I work through Southern Anesthesia Management’s Intensivist Division,” he said.












“The team there has been great about covering for me while I’m deployed. Although I’m board certified in anesthesia, critical care, neurocritical care and other areas, my primary interest is critical care. When I’m home, I work as an ICU hospitalist in Birmingham area medical centers.
“I’ve always found critical care interesting and challenging. When I was a medic, I realized that helping others through medicine was what I was meant to do. I used my education benefits first to become a nurse. As I worked, I wanted to learn and do more. Medical school was the next step. I enlisted in the Air Force since the educational benefits were great. The military gave me the opportunity to pursue a career I loved while seeing interesting places around the world.”
After medical school and a fellowship at UAB, Roan served as an Air Force flight surgeon. He worked as a member of the Critical Care Transport Team (CCAP) in air evacuation of high acuity patients and has been an instructor in medical training at US air bases.
Back at home, Roan’s work as an ICU hospitalist has him fighting to save lives in a daily battle with critical illnesses and injuries.
“The job of a hospitalist is overwatch, maintaining a constant presence and rounding frequently so we can respond quickly to changes in the patient’s condition,” he said.
“Since I’m trained in neurocritical care, some of my patients have brain trauma. Sepsis takes so many patients is sepsis. We have to stay vigilant to prevent it and make sure we give every patient the best chance for recovery.”
Between his military duties and long hours working as a physician, finding time for a personal life could be a challenge.
“My wife Sara has been the anchor that held us all together through raising five children and moving from one base to the next. We both love to fly. She’s better than I am right now and getting more practice. My oldest son is considering going into the Air Force. I’m all for it. I tell him the Air Force offers great opportunities.”
Meanwhile, Roan has another nine years ahead of him to achieve his goal of 20 years in the Army in addition to more than that in the Air Force. His next assignment will take him to Fort Bragg as an instructor where he’ll teach advanced medical training to Army medics. Sometimes life really does have a way of going full circle.
CARDIOLOGY

UAB Cardiogenomics Clinic,


across the southeast, particularly with people who have family histories of heart disease. In many cases, patients receive whole genome sequencing to seek out critical spelling mistakes inside their DNA code, using gene panels to look for specific genetic variations.

“There is a gene panel for heart failure and arrhythmias, for early heart attack, and for diseases of the blood vessels,” Arora said.
High blood pressure is determined by a composite of common genetic variations summarized as a polygenic risk score. These genetic risk scores help accurately predict the risk of cardiovascular events in the future which allows the clinic team to tailor the patient’s treatment plan.
Genetic results can lead to other types of treatments, as well. “One common consequence of congenital cardiovascular defects is aortopathy, or dilation of the aorta, when the big vessel coming out of the heart is enlarged,” Arora said. “My surgical colleague Kyle Eudailey, MD and others are interested in us letting them know when this condition in a patient is genetic in etiology so they can operate before it grows too large and leads to fatal outcomes.”
Once the results of the genetic tests are in, the next step is to help patients understand what this means for their cardiac care and help them create a plan. For that, the clinic has two genetic counselors on staff who specialize in translating the complex vocabulary of genetic testing and disease into a language everyone can understand. “We want to help them understand what to do if they have a genetic variation, and how it impacts them, their children, and their sig-
continued from page 1
nificant others,” said Taylor McClinchey, one of the counselors.
Research by the Cardiogenomics Clinic team has uncovered some information that sheds light on different cardiac vulnerabilities between population groups. In a paper published last year in the Journal of the American Medical Association, Arora and co-authors reported that people carrying the Val122lle variation in the transthyretin gene were at significantly higher risk of heart failure and death. Notably, this Val122lle genetic variant is more common among those of African ancestry. Those carrying this genetic variation had a nearly 2.5-fold higher risk of heart failure and a 40 percent higher risk of death from any cause than non-carriers.
In addition to caring for patients, Arora and Vibhu Parcha, MD lead the UAB Cardiovascular Clinical and Translational Research Program, which has created a biobanking effort known as UAB CARBON (for Cardiovascular Research Biobank) that is building a database of de-identified samples to help researchers uncover new connections between genetic variations and heart conditions. Advancing research and bettering the lives of patients and their families is central to the work being done in the UAB Cardiogenomics Clinic. As advances in genetic medicine continue leading to more gene-based therapeutics, the clinic’s value to the community will grow, hopefully leading to better quality of life for people with inherited cardiovascular conditions.

4 • FEBRUARY 2023 Birmingham Medical News
Birmingham Hospitalist in Iraq, continued from page 1 It makes all the difference. That’s how we make a difference in your debt collection. After 25 years, we know the best way to recover overdue balances is hands-on. No automation, no robots, just a personal outreach and connection. DiRecManagement.com WE USE THE PERSONAL TOUCH. Call Nathan Ryan today and discover how we can help improve your bottom line 251.344.6660 x298 ENDORSED BY JEFFCO MEDICAL SOCIETY Come visit our booth at the MGMA CONFERENCE MARCH 1-3 We are here for you You are our focus. 205.838.3888 52 Medical Park Dr. E., Suite 401, Birmingham, AL 35235 We bring you easy access to high-quality care by board-certified specialists and a host of compassionate sta . No parking fees. Close to home.













Birmingham Medical News FEBRUARY 2023 • 5 F
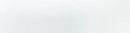
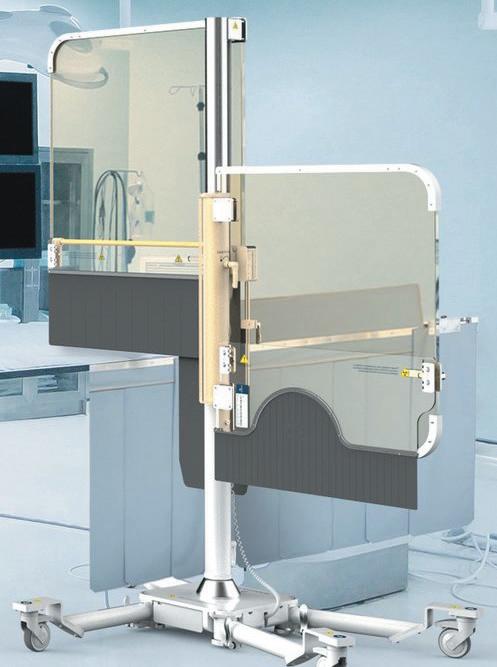
Efstathia Andrikopoulou, MD on the New, Growing Field of Cardio Oncology
This January, Efstathia Andrikopoulou, MD, a cardiologist in the UAB Cardiovascular Institute, sat down with the Birmingham Medical News to talk about Cardio Oncology.


What is Cardio Oncology?







Cardio Oncology is a new field that sits at the intersection of cardiology and oncology. It involves cardiologists who specialize in caring for people who are either currently diagnosed with cancer and undergoing treatment ,whether it be chemotherapy or radiation treatment, or people who have survived cancer and had these treatments in the past.
This field, which is about 10 to 15 years old, is growing at a dramatic pace because, as our diagnosis of cancer gets more accurate and we develop novel treatments, more and more cancer patients survive. This, of course, is great. The problem, however, is that we are recognizing that chemotherapy and radiation therapy can damage the heart muscle both in the near term and in the long run.
There could be heart-related complications like heart attacks, high blood pressure, or inflammation of the heart muscle,












known as myocarditis. The most common condition is heart failure, which is weakness of the heart muscle. These could manifest while patients get chemotherapy or months or years later.
Who do you see?
In our clinics we see patients who have been diagnosed with any type of cancer. It could be breast cancer, colon cancer, kidney cancer, head and neck cancers, bone cancers, or blood cancers like Leukemia or Lymphoma.
If a patient has already had heart issues, like high blood pressure, elevated cholesterol, or a past heart attack or stroke, they are at higher than average risk for developing or worsening heart disease as a result of chemotherapy or radiation treatment.
6 • FEBRUARY 2023 Birmingham Medical News
Expect more from your lab 205-918-7156 • southeastlabs.com • Local testing • Accurate billing • Industry-leading turnaround times • EMR/EHR connectivity • Lower cost to your patients Let us create a customized laboratory solution for your practice At Southeast Clinical Lab, we give you more— CARDIOLOGY
Efstathia Andrikopoulou, MD
(CONTINUED ON PAGE 7)
The UAB Cardio Oncology team with Andrikopoulou first row, far right.
Efstathia Andrikopoulou, MD on the New, Growing Field of Cardio Oncology,




We definitely want to see these people in our clinic, even before they start chemotherapy, and our oncology colleagues are good at identifying them. We want to see the state of their heart muscle. Is there good blood flow to the walls of their heart? Is the heart muscle pumping strongly on both the left and the right side? Are the valves opening and closing nicely?
For example, yesterday I saw a man who was diagnosed with sarcoma a few weeks ago. The UAB oncologist did an echocardiogram of his heart to make sure his heart was in good shape, and even though he was young and active, the oncologist found that his heart muscle was weak.
We want to help him get the strongest chemo that has been shown to work best for him, while at the same time, ensuring that we keep his heart healthy. Before starting chemo, we got him on medications that are proven to help the heart muscle stay strong, but also recover its strength when its weakened.

Are there some types of chemotherapy that are more risky for the heart than others?

Yes. One chemo medication that is one of the highest risk in causing heart failure is anthracycline. These are drugs like Doxorubicin, Daunorubicin, and Epirubicin, to name a few. With these drugs, the heart problems can manifest years later.
Another class of agents is Tyrosine Kinase inhibitors, which can be used for various types of blood cancers or organ cancers. Others include new types of agents that are coming out now – immunotherapies – things like immune check point inhibitors (ICI). The other new kid on the block is car-t cell therapies. We are starting to recognize that they may also cause heart disease.
The most fearful complication from ICI is myocarditis, in which the heart inflammation can range from mild to life-threatening and manifests soon after they get the medication. We have started to recognize that a small percentage of people can get this medication and then go into acute heart failure where the heart muscle can’t pump and they were at risk of dying. We’ve had to give them
strong treatment like high doses of steroids to reverse the inflammation.

The potential for cardiac harm is worsened if a patient has to take a combination of these drugs, which is not uncommon in the case of breast cancer. So we are more aggressive in keeping a close eye on these patients, doing frequent tests with ultrasounds of the heart, electrocardiogram, echocardiograms, as well as blood tests that can show early signs of abnormal function of the heart muscle.
What about patients who don’t have heart problems in advance?

There is some standardization of who needs to be seen. But at the same time, we also want to personalize our approach. Let me add that not all heart disease causes symptoms. A diabetes sufferer might get a heart attack without any pain, which we call silent heart attacks.
There are things we have to look out for to try to uncover heart disease when there are no symptoms. For example: let’s say a doctor sends us a patient who is going to have chemo, but who doesn’t show any signs of heart trouble. She is a 50 year old woman with breast cancer. We will start by checking her blood pressure and her heart to make sure there is no undiagnosed high blood pressure. If there is, we want to control the high blood pressure with a heart healthy diet and more exercise. We also get an EKG to make sure the electrical activity in her heart is good. Then we ask about her family’s heart history.
Is your clinic involved in any innovations in the field?


Yes, actually. At the beginning of February, we’ve started the first of its kind artificial intelligence driven cardiology program. We’ll use AI to screen through all our ECG reports to identify certain features that will put people at risk of getting or worsening heart disease when they receive chemo. This will help us ensure that no patients fall through the cracks and that everyone gets high-quality cardiac care.
Jefferson County Medical Foundation Trust



















Answering Service
Birmingham Medical News FEBRUARY 2023 • 7 Aggressively Pursuing Victory Over Injury SPECIALTIES Elbow | Foot & Ankle | General Orthopaedics | Hand & Wrist | Hip | Joint Replacement | Knee Shoulder | Spine & Neck | Sports Medicine | Non-Surgical Sports Medicine for Adults & Children BIRMINGHAM | Ascension St. Vincent’s Birmingham 805 St. Vincent’s Dr, Ste 100 | Birmingham AL 35205 CULLMAN | 1301-A Bridge Creek Dr NE | Cullman, AL 35055 CROSSROADS AT GREYSTONE | 5406 US Hwy 280 East, Ste D106 | Hoover, AL 35242 GARDENDALE | 323 Fieldstown Road, Ste 105 | Gardendale, AL 35071 PELHAM | 3143 Pelham Pkwy | Pelham AL 35124 TRUSSVILLE | Ascension St. Vincent’s Trussville | 7201 Happy Hollow Road | Trussville, AL 35173 (205) 939-3699 AndrewsSportsMedicine.com
continued from page 6 CONTACT MARY WHITEHEAD 205-933-8601
Exclusively for medical professionals, The Service has provided reliable, caring service to physicians and their patients for over 30 years. • Change your schedule from computer, tablet or smartphone • Operator follow-ups with patient to confirm calls are returned • All calls recorded • Messages delivered via pager, text, phone, fax or email • HIPAA-compliant secure messaging After 6 months of scrutiny by trade industry judges, the Service beat call centers throughout North America & the U.K. with our distinguished customer service rapport, accuracy, & response time.
of Excellence! Winner of the International ATSI 2018 – 2022
Award
David Sibley, MD Began His Career with a Diagnostic Breakthrough













 By Marti WeBB Slay
By Marti WeBB Slay
Significant medical developments are the result of creative thinking, attention to scientific data and good teamwork. Sometimes, they are also the result of a dose of good luck.
For David Sibley, MD, chief of the Division of Cardiology and director of the Cardiac Catheterization Lab Interventional Cardiology at Princeton Baptist Medical Center, a chance encounter in 1984 gave him insight into a new and more effective way to determine if coronary artery disease was slowing delivery of oxygen to a patient’s heart.
Performed during a heart catheterization, instantaneous wave-free ratio, or iFR, is a way to assess stenosis and the degree to which it limits blood flow to the heart. It helps cardiologists determine when surgical or percutaneous intervention is necessary.





But the road to today’s standard procedure has its roots in 1984, when Sibley ran late and missed a bus to the American Heart Association meeting.
“I was a first-year fellow at UAB’s cardiovascular department when this odyssey started for me,” he said. He was learning how to do coronary angiograms to determine if someone had significant coronary disease and needed surgical intervention or

percutaneous coronary intervention (PCI). Balloon angioplasty was very new, and stents were not yet being used. He was one of the first interventional fellows in cardiology at UAB.
That American Heart Association meeting in Miami was his first big cardiac meeting. He ran late his first day, missed the bus, and when he arrived by taxi, he was unsure where to go. After taking a wrong turn, he ended up in the poster section, where he met Dr. Mal Marcus from the University of Iowa.
they listen.
That’s the difference in having the attorneys at Cloud Willis & Ellis represent your medical practice in managing your accounts receivables. We provide the complete services of an agency and a law firm or anywhere in between — you choose. We will collaborate with you to design a collection strategy that helps limit unpaid invoices and medical bills. Then we will implement that strategy in our office, and help you implement the strategy in yours. We have the experience and know-how in medical collections to make it better for you.



Instead of angiograms, Marcus was investigating a whole new method to measure coronary disease. “He was measuring coronary blood flow in the coronary arteries with a Doppler device attached to the outside of the vessel while the CV surgeons were performing open heart surgery,” Sibley said. “He was measuring actual blood flow and comparing the results to angiograms and showing how the two correlated. The angiogram showed anatomy and the Doppler crystal showed physiology. Physiology was the more accurate predictor of measuring the importance of the patient’s coronary artery disease.
“His findings fascinated me. I had just spent months learning about coronary angiograms, and here was an expert telling me it wasn’t the best way to determine how we should treat a patient.”
As Sibley mused over this new insight, he asked himself how to apply this information in a way that would help diagnose how a patient should be treated, whether by intervention or medical therapy. He came up with the idea of putting a Doppler-tipped 1mm catheter over the guidewire to measure coronary blood flow during a heart cath. “Can the patient increase blood flow in the coronaries to meet the demands of the heart? That was the major issue. It was assumed if there were a 50 percent blockage,
that reduced coronary blood flow. But that was a leap,” he said.







Sibley discussed his idea with Huntley Millar, who was well known for developing high fidelity catheters, and Millar designed the requested catheter within a few months. In the meantime, Sibley found an advisor at UAB for the project and received $25,000 funding, a lab and a technician for the research.
The testing had to begin with animals. “We were talking about taking an instrument and putting it inside a coronary artery on the surface of the heart and then hooking the other end of it to the AC adaptor in the wall,” Sibley said. “I don’t think that had ever been done.”
The animal research was successful, and the next step was to perform the test on a patient. “We did it on our first patient in UAB’s Quarterback Tower, and for the first time that I know of, we had online in the cath lab, blood pressure, EKG and coronary blood flow on the ocilloscope in front of us on a live patient. I’ll never forget it. There were a lot of people watching us. You could also hear it on the audio, how the flow would increase as we stimulated coronary flow in the coronary arteries,” he said.
When Sibley had data on 10 patients, he was able to present at the American Heart Association meeting in 1985, as a second-year fellow, and in December 1986, he was published in the Journal of the American College of Cardiology. He also travelled extensively around the world to lecture on the procedure.
Today’s iFR measurement, which is a standard of care in cardiology, is a direct follow-up to Sibley’s efforts as a UAB fellow.
“I can’t take all the credit for this,” Sibley said. “Dr. Robert Wilson at the University of Iowa was working on it too, with Mal Marcus, but the side-mounted blunt probe they were using made it difficult to obtain consistent results.” Sibley’s idea to put the Doppler technology on the end of the catheter and over a guidewire moved the technology forward.
Despite his success in research and the development of this technology, Sibley’s interest was in working in private practice, and when he was invited to develop the interventional cardiology department at Princeton, he decided to make the move. The department had completed only three angioplasties before his arrival, and he performed 250 in his first year.
“It was a very exciting time for me, and also a lot of work,” Sibley said. “I can’t say enough about Drs. Harriet Dustin and Suzanne Oparil at UAB for giving me, a first year fellow, $25,000 in funding, a lab and a tech. It was a stretch.”
And one that paid off for the field of interventional cardiology.
8 • FEBRUARY 2023 Birmingham Medical News
When people receive a communication from a law firm,
No Representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. 205.322.6060 • CLOUDWILLIS.COM BIRMINGHAM • MOBILE • NASHVILLE Willis & Ellis ATTORNEYS AT LAW Cloud CALL TODAY FOR A FREE CONSULTATION. CARDIOLOGY
David Sibley, MD
At Medical West, we understand how important it is to return to normal life after experiencing a heart-related event. That’s why we’re proud to offer an outpatient Cardiac Rehabilitation program. Our Cardiac Rehab clinicians create personalized treatment plans approved by our team of cardiologists. These plans combine exercise and education and are designed to help patients adopt heart-healthy lifestyle changes that will improve their overall health and quality of life. By focusing on exercise training, stress reduction and nutritional counseling, patients can return to their normal lives faster and healthier.


To learn more about the outpatient Cardiac Rehabilitation program at Medical West, scan the QR Code or call (205) 481-7202.


Birmingham Medical News FEBRUARY 2023 • 9
It doesn’t get easier. You just get stronger.
MEDICAL WEST Our outpatient Cardiac Rehabilitation program is designed to help get you back on your feet after recovering from a heart-related condition.
Medical West Cardiac Rehabilitation 950 Medical Center Drive | Bessemer, AL 35022 P: (205) 481.7202
Options for Coronary Chronic Total Occlusion
 By Jane ehrhardt
By Jane ehrhardt



“There are patients with angina who are told they have a 100-percent blockage in a coronary artery and that nothing can be done about it. But, in fact, things can be done,” says Matthew Sample, MD, interventional cardiologist with Cardiovascular Associates in Birmingham.

Advances in interventional cardiology have produced multiple solutions for inserting stents in patients with chronic total occlusion (CTO). “In the early days, we didn’t have the skill-set or the appropriate equipment to handle 100-percent blockages,” Sample says. “Now we’ve advanced our abilities to the point where we know how to deal with these lesions better.”

Specialty coronary wires have been developed, such as micro catheters that are less than a millimeter in diameter, which help the coronary wires be more aggressive. “Typically a coronary wire has about a gram of tip load pushability,” Sample says. “But if you reinforce that wire by putting a catheter over it all the way to the tip, you dramatically increase the tip load and can push through more challenging lesions.”
Some wires offer greater torque ability, allowing the operator to turn the wire a quarter turn outside the catheter translating to a




true quarter turn inside the coronary, which older wires could not do. Other wires come polymer-jacketed to increase or decrease friction. A thinner, stronger, stiffer and more responsive array of wires and sheaths has led to more options for treating CTO.
“Traditionally, in terms of a routine stent, we’d antegrade down the artery from the beginning to end,” Sample says. “But we have techniques now that allow us to go retrograde to the artery through the opposite coronary artery and use collateral branches to get wires into the distal end of the artery.”
For example, if a blockage in the midright coronary artery could not be reached antegrade, the operator can go in through the left anterior descending artery and use small con-
necting collateral branches to reach the right coronary and go backwards through that vessel to increase the likelihood of success.
The algorithms that determine the potential for routes have also grown more sophisticated. The algorithms are like a flow chart, mapping out the optimal option in a “if this, then do that” fashion based on variables for that patient. Factors can include the length of the blockage, the amount of calcium, the area of the total occlusion, and whether it involves side branches. That generates a difficulty score, called a J-CTO score.
Based on the score, the physician can determine how best to start the procedure to open the occlusion. The four options include using either the antegrade or retrograde approach of wire escalation or dissection reentry, in which it purposely enters the subintimal space to get past the blockage and reenter beyond it, then using a stent to connect true lumen to true lumen.
The algorithm also presents hard stopping points for when an operator should switch strategies. “These lesions used to fail opening because we would get stuck trying one strategy over and over,” Sample says. “But now we have better algorithms informing us when to give up on a strategy and adopt a new one. That keeps the procedure moving much quicker and provides better results.”
Not every patient with chronic total occlusion (CTO) qualifies for the procedure. “This is for patients with uncontrolled symptoms despite good medical therapy,” Sample says. “If patients with total occlusion don’t have symptoms like angina or shortness of breath day to day and they get around fine, they absolutely do not need that artery opened because the risks exceed the benefits.”
The risks run about five percent versus one percent for a standard stent procedure. “That’s pretty high in my occupation,” Sample says. “But if the patients understand the risks and what they stand to gain from it, it’s perfectly reasonable to move forward.”
Sample makes it clear to patients that the procedure is about relieving their lifelimiting symptoms. Opening the vessels does not prolong life or prevent heart attacks. “We can do help patients who can’t enjoy their day-to-day lives because they’re limited by angina,” he says.
Most importantly, CTO patients need to know there is something that can be done. “If a patient had 90-percent blockage and was having angina, you’d probably recommend getting stented. The 100-percent blockage is no different,” Sample says. “Times have changed. If it’s indicated for the 95-percent blockage, it’s indicated for the 100-percent.”

10 • FEBRUARY 2023 Birmingham Medical News TOTALON1ST.COM 1927 1ST AVE N, WOODWARD BUILDING, 1ST FLOOR Healthy
we should all indulge. Discover a renewed definition of skin care in a lavish, immersive environment. After all, health is a hard thing to overdo.
is a fee ling
CARDIOLOGY
Matthew Sample, MD
Ascension St. Vincent’s East Opens New Cardiology Unit
 By laura FreeMan
By laura FreeMan
For years, the cardiologists of Ascension St. Vincent’s East have dreamed of a central unit where all their patients admitted for cardiovascular conditions could receive specialized care in one dedicated space. Now they are seeing that reality take shape with the new cardiology unit in place, equipped and recruiting staff to begin welcoming its first patients this month.
“Having heart patients in a central location is going to be a game changer in helping us deliver the best possible patient experience and even better care,” cardiologist Jason Thompson, MD, PhD, of Birmingham Heart Clinic said. “Instead of having to walk all over the hospital, we will be able to spend more time with each patient. We can check on patients more often and do rounds with the entire care team so we can exchange information and respond to changes there and then.”
While the heart surgery unit continues to care for patients undergoing major cardiovascular surgery, those admitted primarily for a diagnosis like heart failure, a rhythm disturbance, a cardiac event and those needing follow up after stent placement, a transcatheter aortic valve replacement, or similar heart procedure will be cared for in the new unit on the 7th floor of the North Tower.
Nursing Manager Nicole Arnold, RN, sees the dedicated unit as a win for both patients and the care team. “It’s a great opportunity to add to the depth of our skills and professional knowledge,” she said. “While nurses work to be proficient in all our duties, performing specialized care every day will allow us to become particularly adept with new skills. We also gain a greater understanding of heart disease processes and interventions as we work with top professionals. Frequent in-service training on key topics in cardiovascular care will allow us to
continue growing professionally.

“Patients benefit from caregivers with a greater depth of expertise. So do we. Continuing to learn and expand our skills keeps our work interesting and challenging. The new unit is beautiful and well-designed and equipped. It’s going to be a great place to work. Our nurses are so excited.”
The 23-bed unit will have both telemetry beds and several intermediate beds offering a level of care between standard and CICU. The unit is fully equipped with the latest cardiovascular technology.

“Cardiology is an imaging-intensive field,” Thomas said. “If a scan comes in while we are on rounds, we can just step over to the reader to view the latest update and make decisions in real time. In addition to saving time, having a central unit for heart patients also means we will be working with a team that has a skills set geared to caring for people with those conditions.”
In a dedicated centralized unit with shared knowledge, communication becomes seamless and the care team can better support each other as they learn to anticipate what is likely to come next. When heart patients are spread out on different units, the skills of the support team may be geared to orthopedics, oncology or something else completely different.
“Providing quality care for patients with a condition like heart failure can be much more effective when someone can check on them,” Thompson said. “Either I can round again to see how a patient is doing, or one of the unit’s cardiology nurse practitioners who is always on duty can check back and notice when medication needs to be increased. The order can be changed immediately instead of waiting for notes and change orders to get to the right people.”

Having grown up in Trussville, Thompson feels very close to the people in the area who are served by Ascension St. Vincent’s East.
“When I care for teachers from high school or friends of my parents, it feels good to help. The new cardiology unit is going to make such a difference in caring for the people who live here,” he said.

Ascension St. Vincent’s East is now re-


cruiting nurses, nurse practitioners, hospitalists and a full range of support staff for the new cardiology unit. Anyone interested in applying for one of these positions can go to Ascention.org/careers.

Birmingham Medical News FEBRUARY 2023 • 11 Birmingham Bessemer We’ve made referring easy! Don’t LOVE the referral process? • Patients are scheduled within 24 hours. • Patients are seen in clinic within 2-4 weeks of referral. • We keep you informed about the patient’s treatment plan. • We make sure the loop is closed on your referral. CARDIOLOGY
A nurse checks equipment in a patient room at the new cardiology unit.
Nurse’s station at Ascension St. Vincent’s East cardiology unit.
Gain the Security and Advantage of a Healthcare IT Strategic Partner


Your Practice and Telemedicine
Patient care generates a large amount of data that must remain accessible 24/7/365 to keep your doors open. Our team takes that seriously. Our engineers work around the clock to ensure your network is consistently monitored and downtime is minimized. And should concerns arise, our Healthcare IT is just a phone call away—any time, every day.
866.951.7676 | DYNAMICQUEST.COM
By Catherine (Cat) KirKland
The COVID-19 pandemic gave way to a rapid increase in virtual care for patients. Now nearly three years on, the American Medical Association found in a recent study that eighty-five percent (85%) of physicians continue to offer telehealth visits. Further, Doximity, a telemedicine platform, found that the Birmingham metropolitan area possessed the sixth highest telemedicine adoption rate in the United States. The trends are clear: telemedicine is here to stay. Whether your practice has currently implemented a telemedicine program or is interested in implementing a program in the future, physicians should be aware of several important legal considerations.
Alabama Specific Considerations:
In line with Alabama’s July 2022 telemedicine practice law, the Alabama Board of Medical Examiners requires the following related to physician licenses for the practice of telemedicine in the state:
• If the patient is located in Alabama, the physician must possess a full and active license to practice medicine in Alabama.
• The location of the medical services provided is controlled by the physical location of the patient, rather than the location of the physician.
• Certain telehealth services do not require an Alabama license, these include:


o When a physician is licensed in another state or D.C.; and services are irregular or infrequent; or





o Services are provided in consultation with an Alabama licensed physician, limited to ten days in a calendar year, or necessary medical care is provided to a patient being transported into Alabama.

In addition to these requirements, the Board also sets forth a variety of physician

responsibilities and requirements related to telemedicine. For example, while Alabama law allows a physician-patient relationship to be formed virtually without an in-person exam, if “a physician or practice group provides telehealth services more than four times in a 12-month period to the same patient for the same medical condition without resolution, the physician shall either: see the patient in person within a reasonable amount of time, which shall not exceed 12 months; or appropriately refer the patient to a physician who can provide the in-person care within a reasonable amount of time, which shall not exceed 12 months.”
To ensure compliance with the Alabama rules, physicians should:





• Review Alabama Acts No. 2022-302 and regularly monitor Board telehealth requirements.

• Establish procedures to ensure compliance. For example, a practice may want to set alerts for patients who regularly receive telehealth visits to ensure that after four visits for the same condition, that patient sees the doctor in-person.


• Keep careful documentation evidencing how the patient encounter occurred.
It is also important to note that these rules are Alabama specific. Unfortunately, there is not a uniform rule for telemedicine practice around the United States. If an Alabama-licensed physician desires to treat a patient physically located outside of Alabama, that physician must review and ensure compliance with the laws and rules of where that patient is physically located before proceeding.
Other Legal Considerations:
Beyond licensing and state law requirements, physicians also need to be aware of various other considerations, including the treatment of patient information, changes to



(CONTINUED ON PAGE 15)
12 • FEBRUARY 2023 Birmingham Medical News
BIRMINGHAM
MOBILE
| HUNTSVILLE | MONTGOMERY |












Birmingham Medical News FEBRUARY 2023 • 13 VIBRANT COMMUNITY. GROWING HEALTH SYSTEM. You work every day to improve quality of life for your patients. Now it’s time to improve yours. – Modern, updated hospital – Advanced robotics technology – Full vesting of 403b match after 90 days – Immediate time off accrual – Tuition reimbursement, education starter loans and education partnerships – Free, convenient parking Scan the QR code to learn more about career opportunities at Cullman Regional.
The No Surprises Act is Full of Surprises
Legislation had problems from the get-go
By lynne Jeter

The No Surprises Act (NSA), which went into effect January 1, 2022, to protect patients from an estimated 12 million surprise bills annually, has been fraught with challenges, with medical professionals calling at least one of its processes flawed and ineffective.
“While the goals of consumer protection and price transparency are important, the legislation is starting to present real challenges to medical practices’ financial stability,” said Dan D’Orazio, CEO of Sage Growth Partners, a national consulting firm for healthcare organizations.
The NSA applies to employer-sponsored health plans for certain emergency services and those received from out-ofnetwork providers at in-network facilities regarding balanced billing. The act doesn’t apply to out-of-network providers at out-ofnetwork facilities. Providers risk a penalty of up to $10,000 per violation.
“If a patient requests it, even physician offices are required to provide a good faith estimate,” said Matt Clements, CFO of Sage Infusion. “One day soon, upfront pricing may be required for all practices.”
The Benefit Claim Process
The benefit claim process is time-sensitive and consuming. When negotiation doesn’t resolve the dispute, the NSA provides for an arbitration process, Independent Dispute Resolutions (IDR).
The Centers for Medicare and Medicaid Services (CMS) anticipated 22,000 IDR appeals in 2022. Yet within the first six months of the law going into effect, more than 90,000 IDR appeals were initiated. What’s more, only 3,500 determinations had been made by midDecember.



The Trouble with IDRs
Under the IDR process, a strictly controlled baseball-style arbitration for disputing unreasonable reimbursement amounts with insurers, a provider must initiate open negotiations within 30 days of receipt of the payment or notice of denial.

“If open negotiations fail, then the IDR process is initiated within four days of the end of the 30-day open negotiation period,” said Michael Lowe, an attorney at Lowe & Evander in Florida. “IDR is started by issuing notice to the other party and the HHS
Secretary. The parties have three business days from the initiation of the IDR to jointly select the arbitrator. If the parties fail to agree on an arbitrator, then the HHS Secretary will select one within six business days from the start of the process. After the arbitrator is selected, within 10 days from the selection, the parties must submit their offer, along with any supporting evidence or documentation. After the submission, the IDR arbitrator must choose one of the two offer amounts.”
Here’s the rub: “There are only 13 IDR arbitrators (entities) and only 11 accepting new disputes, which is simply not enough,” said Christine Cooper, co-managing member of Koehler Fitzgerald, a law firm with a national practice. “The IDR process is also occurring piecemeal. Appeals are initiated in the federal portal. Every other step is managed by the IDR entity. Each IDR entity manages the process differently, some by email, some by their own portal. Progress is difficult to track, and some IDR entities have failed to follow deadlines. Rather, they pause the acceptance of offers upon receipt of new disputes. It’s been very difficult to communicate with the IDR entities, as most don’t
respond to phone calls or emails.”
“Physicians will not only need to become savvy at submitting bids to receive more favorable reimbursements, but also because the loser in the arbitration may be required to cover fees for both parties,” D’Orazio said.
“To add to the uncertainty, the IDR rules keep changing. Early in 2022, several state medical associations and air ambulance companies filed suits about the interim final rule that bases appropriate reimbursements on insurers’ qualifying payment amounts (QPA). In April, CMS retracted its stance on just how much weight QPAs should carry in arbitrators’ decision-making.”
More Legal Woes
Last February, Eastern District of Texas Judge Jeremy Kernodle agreed with the Texas Medical Association that the HHS interim final rule governing the IDR process conflicted with the NSA statute when it created a rebuttable presumption that the QPA was the correct out-of-network rate for purposes of the IDR process.

In September, the Tennessee Advisory Commission on Intergovernmental Relations revealed that it was studying the overall effect
(CONTINUED ON PAGE 15)
14 • FEBRUARY 2023 Birmingham Medical News (CONTINUED ON PAGE 14) (CONTINUED ON PAGE 16) We’re di erent & proud of it! Our professional sta will help you lower your cost, lower your stress, and treat you like family! (plus they’re kinda cute!) Celebrating 12 years of the only family-owned medical waste company in Alabama • Medical waste removal • Secure document shredding • Pharmaceutical waste removal • Hazardous waste removal • Online compliance & training portal CONTACT US TODAY FOR A QUOTE 205.938.3333 | WESTMEDDISPOSAL.COM
Christine Cooper
The No Surprises Act is Full of Surprises,
continued from page 14
on health insurance prices when referencebased pricing is used. Tennessee may be the latest state to adopt reference-based pricing to control healthcare costs. (The final report had not been presented by press time.)
“Several other states have adopted reference-based pricing and are successfully using it,” Cooper said. “The most wellknown is Montana, which became the first state to use reference-based pricing for all of its employees’ health benefits. Other states that have adopted reference-based pricing include California, Oregon, Colorado, and Washington. Each of these states was armed with the experience of Montana.
“Reference-based pricing is a way to avoid the uncertainty the NSA is creating. We anticipate seeing a broader adoption of reference-based pricing plan design both for public entities and private corporations. It’s a true cost control mechanism that brings uncertainty to the plans and the providers.”
Woes Before NSA Became Law
“In November 2021, congressional doctors, their medical associations and members of Congress led the charge that the rule released by the Biden Administration two months earlier for implementing the law, favored insurers and didn’t follow the spirit of the legislation,” wrote Michael McAuliff for Kaiser Health News.
“The Administration’s recently proposed regulation to begin implementing the law doesn’t uphold Congressional intent and could incentivize insurance companies to set artificially low payment rates, which would narrow provider networks and potentially force small practices to close, thus limiting patients’ access to care,” wrote Rep. Larry Bucshon (R-Indiana). Roughly half of the 152 lawmakers who signed the letter were Democrats.
“The doctors in Congress are furious about this,” a staff member told McAuliff.
Cooper said it was clear that providers would take issue with the language in the Rule creating a rebuttable presumption that the payor’s median contracted rate is the proper reimbursement rate for claims governed by the NSA, ignoring the other factors listed in the NSA.
“The median contracted rate is solely within control of the payors and it stripped the providers of any say,” Cooper said. “In addition, the providers likely understood that the IDR entities would naturally select the offer closest to the median contracted rate because they’re on a tight timeline and couldn’t reasonably process the number of claims they would be receiving if they had to evaluate each factor listed in the NSA and provide a written opinion as to why they deviated from the median contracted rate.”
Your Practice and Telemedicine
, continued from page 12
telemedicine once the public health emergency (PHE) ends, and physician liability concerns.
Ensure Liability Coverage
Most physician liability coverage policies include telemedicine coverage, but some do not. As a practical consideration, every physician providing telemedicine services should ensure that they have appropriate coverage and that this coverage extends to wherever the physician provides telehealth services (for example, if the physician virtually treats patients physically located outside of Alabama).
Protection of Patient Information
From a patient information perspective, physicians must ensure appropriate cybersecurity is in place and that The Health Insurance Portability and Accountability Act of 1996 (HIPAA) and any other state-specific patient information laws are followed. Regarding state specific rules in particular, if you are located in Alabama, but are treating a patient located elsewhere, you may be legally required to comply with privacy rules from the patient’s home state.
What Happens When the PHE Ends
HHS currently affords a fair amount of flexibility and leniency to telemedi -
cine services as a result of the COVID-19 pandemic. Once the PHE expires, many of these flexibilities will expire within 151 days—barring agency or Congressional action. It is widely expected for Congress to permanently extend some of these practices, but it is impossible to predict what will happen. For example, barring Congressional action after the PHE 151-day grace period, Medicare may no longer reimburse telehealth services that occur at a patient’s home (as opposed to a patient located in a hospital /nursing home setting). Medicare will also cease reimbursement for telehealth visits furnished by physician therapists, occupational therapists, speech language pathologists, and audiologists. Medicare will also no longer cover audio-only visits for physical health encounters. HHS currently maintains a webpage outlining telehealth policy changes that will occur after the COVID-19 PHE ends. Physicians providing telehealth services should 1) pay attention to when the PHE ends, 2) monitor HHS’ telehealth policies and potential permanent changes, and 3) update and change telemedicine policies as needed.
Birmingham Medical News FEBRUARY 2023 • 15 205.447.1642 | V oltz P rofessional r isk . com We work for YOU, not the insurance company. A M O P R O B OS VOLTZ PROFESSIONAL RISK ADVISORS Put our 35 years of professional liability experience to work for you. Take advantage of our complimentary consultation to explore your medical professional liability options. With VOLTZ PROFESSIONAL RISK, you get all five! What’s important to you in your Medical Malpractice coverage? A superior (A-Excellent) or better rated company? Excellent defense attorneys with proven defense results? Competitive rates? A “mutual” company versus a “stockholder-owned” company? Superior service from a personal, independent agent?
Catherine (Cat) Kirkland is a Partner at Burr & Forman LLP practicing exclusively in the firm’s Health Care Practice Group. Cat may be reached at (251)-340-7271 or ckirkland@burr.com.
FTC Proposes an End to Employee Non-Compete Agreements
 By Beth VeSSel
By Beth VeSSel
In a dramatic departure from longstanding practice, the Federal Trade Commission hopes to put an end to the use of non-compete agreements by employers. A Proposed Rule from the FTC would prohibit employers from entering into non-compete agreements or representing to workers that they are covered by non-compete agreements. Additionally, employers would be required to nullify existing non-competes and notify workers within 45 days of nullification that the restrictions will not be enforced. The Proposed Rule – which would apply to both employees and independent contractors, whether paid or unpaid – is based on a preliminary finding by the FTC that non-compete agreements constitute an unfair method of competition and violate Section 5 of the Federal Trade Commission Act. Historically, the enforceability of such agreements was predicated on state law.
The Proposed Rule specifically states that it is an unfair method of competition for an employer to enter into or attempt to enter into a non-compete clause with a worker, maintain such a clause or represent to a worker that the worker is subject to such a clause if
the employer has no good faith basis for such representation. The Proposed Rule does not nullify non-solicitation, non-disclosure and other confidentiality agreements, unless they are so broad that they effectively function as non-competes. The FTC notes that the term “non-solicitation agreement,” for purposes of the Proposed Rule, is intended to refer to contractual provisions prohibiting workers from soliciting clients or customers of the employer, not agreements not to solicit employees. Nonsolicitation agreements with respect to employees may therefore still be viewed as problematic and potentially subject to challenge.


Physician Non-Competes

Physician non-competes would likely be included unless subject to an exception.

In the Notice of Proposed Rulemaking, the FTC lists examples of non-compete clauses and includes a case involving a contractual term between a medical services firm and an ophthalmologist which provided that, for two years after employment termination, the physician was not allowed to engage in the practice of medicine in two Idaho counties unless the physician paid the firm a practice fee.

Detailing the estimated benefits of the Proposed Rule, the FTC includes a section on physicians, as one of four broad classes of workers meriting specific attention as a sector for which researchers have generated empirical estimates of the effects of noncompete clause enforceability. One cited study indicated that for a physician with 10
years of experience in the state which enforces non-compete clauses most readily, a prohibition on non-compete clauses and removing such physician’s non-compete clause would lead to a 12.7 percent increase in earnings. For a physician with just one year of experience, the study indicated that the increase in earnings would be 37.4 percent.

The FTC argues that non-compete clauses reduce competition in labor markets, suppressing employee earnings and benefits and reducing innovation and competition in product and service markets by decreasing the flow of information and knowledge among firms. If the Proposed Rule were enacted as written, many employers would no longer be able to rely on non-competes to deter workforce attrition. In an already tight labor mark, competition between employers to attract and retain talent would rise and result in increased costs to businesses. It may also make it easier for competitors to enter a market because they will be able to attract talent more easily, but they will face the same challenges with respect to retention of such talent.
The Proposed Rule represents a major departure from legal precedent that has often


(CONTINUED ON PAGE 18)

16 • FEBRUARY 2023 Birmingham Medical News Having a professional with the touch and skill to keep all the components of your business in just the right motion is what produces reliable, satisfying results. That’s our role. No matter your needs — large or small — with our flexible, a la carte menu of services, you get what you want, the way you want it. All provided by sta based right here in Alabama. With MBCS, you have a convenient contact to wait on you with answers and empowered to find you solutions. The right ingredients produce the most satisfying outcomes 1-888-441-380 MEDBCS.COM DENIAL MANAGEMENT REPORTING CODING SERVICES CLAIMS PREPARATION CLAIMS SUBMISSION PAYMENT POSTING
Beth Vessel







Birmingham Medical News FEBRUARY 2023 • 17 SpineCare. Better Together. Call 205-221-5374 to make an appointment or visit PrecisionSportsOrtho.com Life can be so much better with less pain. Dr. Mark Prevost II and his spinal surgery team offer advanced, minimally invasive spine care treatment options that maximize outcomes and reduce recovery time. We help get you back in motion for the life you want to lead. Common conditions we treat include: Get back on track with local, advanced spine care. • Disc herniation • Lumbar disc disease • Myelopathy • Pinched nerves • Scoliosis • Spinal cancer • Spinal cord compression • Spinal instability • Spinal stenosis
End to Employee Non-Compete Agreements,
continued from page 16
allowed such agreements, as long as not unreasonable in duration and scope, if there are appropriate business justifications. Only three states currently prohibit such restrictions entirely. In the M&A context, it would likely reduce transaction values if buyers are unable to ensure that key employees will remain after an acquisition. There may also be reduced incentives for employers to invest in personnel development.
The public has been given 60 days (after the date of publication of the Notice of Proposed Rulemaking in the Federal Register) to provide comments to the Proposed Rule. Challenges to the FTC’s authority to issue the Rule seem inevitable. The FTC has stated that Sections 6(g) and 18 of the FTC Act enable it to make rules to carry out the FTC Act’s provisions and that the FTC has the explicit authority to prescribe rules with respect to unfair methods of competition in or affecting commerce. As noted in the Dissenting Statement of Commissioner Christine S. Wilson, however, the Notice of Proposed Rulemaking is vulnerable to challenges that the FTC lacks authority to engage in substantive rulemaking with respect to competition. In addition, citing West Virginia vs. EPA, if the Proposed Rule presents a major question (which would include the power to resolve a matter of great political significance, regulate a significant portion of the American economy or intrude in an area that is the particular domain of state law), the FTC would be required to identify clear Congressional authorization to impose a regulation banning non-compete clauses. The final rule will almost certainly be subject to significant legal hurdles.
Beth Vessel is a partner with Waller where she focuses on mergers, acquisitions, divestitures and joint ventures in the healthcare industry.
GRAND ROUNDS Khanal is First UAB faculty to receive National AAO Career Development Award
Safal Khanal, OD, PhD, assistant professor at the UAB School of Optometry, has received the 2022 Career Development Award from the American Academy of Optometry. Khanal is the first UAB faculty member to receive this honor since its inception in 2015.

This national award is designed for educators and scientists and provides funding for innovative investigator-driven projects. Through this award, Khanal will receive $200,000 in grant funds over two years to pursue a clinical research project that investigates why myopia, commonly known as nearsightedness, develops and progresses in humans.

Over two billion people worldwide suffer from myopia and are at risk of losing sight due to myopia-related complications. “Without a mass implementation of preventive and curative strategies, myopia will soon become the leading cause of blindness and visual impairment worldwide,” Khanal said. “I hope that our research will contribute to the development of effective myopia control strategies.
Alabama Department of Public Health Offers Free Radon Test Kits for Households
Radon is the number one leading cause of lung cancer among non-smokers. The Alabama Department of Public Health (ADPH) is offering one free radon test kit per Alabama household as part of an initiative to cut down on dangerous radon exposure.
Radon is a radioactive gas that cannot be seen or smelled. It is produced when uranium breaks down in soil and water. Radon is harmlessly dispersed in outdoor air, but it can increase the risk of lung cancer when trapped in buildings. Symptoms of dangerous radon exposure include persistent coughing, shortness of breath, and chest pain.
According to the U.S. Department of Housing and Urban Development, one in 15 homes has a radon problem. In Alabama, 15 counties have been identified as having the highest potential for elevated radon levels: Calhoun, Clay, Cleburne, Colbert, Coosa, Franklin, Jackson, Jefferson, Lauderdale, Lawrence, Limestone, Madison, Morgan, Shelby, and Talladega.
The only way to tell if a home has a radon problem is to check with a radon testing kit. Alabama households can order one free radon test kit online via ADPH. Recipients are only responsible for paying a return shipping fee.
Citizens Baptist Medical Center Installs 3D Mammography Technology
Citizens Baptist Medical Center has installed a 3D Mammography machine, an imaging test that combines multiple breast X-rays to create a three-dimensional picture of the breast. When utilized for breast cancer screening, a 3D Mammography machines create three- dimensional images in addition to standard two-dimensional mammogram images.
Studies show that combining 3D mammograms with standard mammograms can reduce the need for additional imaging and may increase the number of cancers detected during screening.
“We’re thrilled to have this technology,” said Frank Thomas, CEO. “This will have a transformative impact on our hospital, our medical staff and the patients we serve.”
BlueCross BlueShield of Alabama’s Blue Advantage Plan Receives 4.5 Star Rating
BlueCross BlueShield of Alabama’s Blue Advantage Plan received a 4.5 star rating from the Centers for Medicare and Medicaid Services (CMS).

CMS uses a five-star system to measure the quality and experience of Medicare Advantage health and prescription drug plans. The rating is based on information from member satisfaction surveys, plan operations and healthcare providers.
Blue Advantage plans will continue to offer a variety of extra services at no additional cost, including:
• Comprehensive Dental Allowance
• SilverSneakers® Fitness Program
• Healthy Rewards Program
• AirMed Transport Services
• 24-hour Nurse Line
• In-home Support (for Blue Advantage Premier only)
Alabama Children’s Hospital Foundation Coke Matthews, III to Retire; Chandler Bibb to Replace
Children’s of Alabama Senior Vice President and Chief Development Officer (CDO) Coke S. Matthews, III is retiring in March.
Chandler Bibb has been appointed to succeed Matthews. Bibb joined Children’s in 2013, serving most recently as director of development. She came to Children’s from Birmingham’s McWane Science Center where she was Vice President of Marketing and Development.

Bibb is a graduate of the University of Georgia. She received a Master of Management in Health Care from Vanderbilt and completed the Executive Certificate in Nonprofit Leadership program at the Harvard Kennedy School. She has also received several other professional designations and honors, including the 2020 Association of Healthcare Philanthropy’s 40 Under 40 winner, a graduate of the 2014 class of Leadership UAB, and the Certified Fundraising Executive (CFRE) designation.
Our
Matthews, who has served as CDO at Children’s since 2002, led the successful $100 million Keeping Promises Capital Campaign to support major expansion at Children’s. Under his leadership, the development program at Children’s helped to provide funding support not only for the transformation of the downtown Russell Campus, but also for the expansion of many pediatric clinical programs, as well as myriad family-centered care services for patients and their families.
18 • FEBRUARY 2023 Birmingham Medical News
Safal Khanal, OD, PhD
BIRMINGHAM (near Super Target) Grandview Medical Center 4600 Hwy 280, Ste 230 Medhelp 280 Bldg, 2nd floor ALABASTER (formerly Shelby Ob-Gyn) 408 1st Street North 205.664.9995 | CWCALABAMA.COM
Providing Services at Grandview Medical Center
professional team of doctors, nurses, and staff look forward to seeing you.
SAME DAY APPOINTMENTS AVAILABLE
Kara Conti, MD | Ashley Duke Gooding, MD | James Head, MD | Jessica Rodriguez, MD Malcolm Simmons, MD | David L. Spangler, MD | George Zaharias, MD
Chandler Bibb Coke Matthews, III
UAB Heersink School of Medicine Granted Full LCME Accreditation at the Highest Level
The University of Alabama at Birmingham Marnix E. Heersink School of Medicine has achieved the highest level of accreditation available to a medical school in the United States by the Liaison Committee on Medical Education after a rigorous self-study.


Accreditation demonstrates that the Heersink School of Medicine has met and is maintaining high standards set by the LCME, the nationally recognized authority for accrediting medical education programs leading to the MD degree in the United States and Canada.
The process toward reaccreditation began in 2020 with the gathering of information for the school’s Data Collection Instrument, a database that was divided and read by members of the Self-Study Task Force. The task force was charged to highlight institutional strengths, identify challenges and put forth solutions to address those challenges.
Student leaders also conducted the Independent Student Analysis, an assessment of the medical school’s learn-
ing environment, educational program, resources, administration and services. The process concluded with a virtual site visit from an LCME review team.
The next full survey for reaccredita-

Rampart IC Expands Global Distribution Network





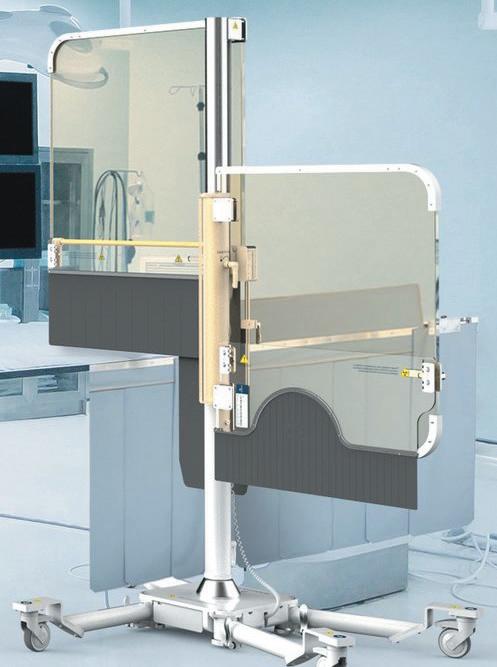
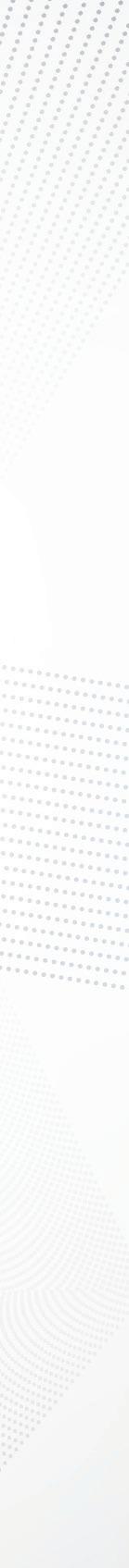
Birmingham-based Rampart IC, a medical device company specializing in radiation shielding, has signed agreements that expand its distribution to Israel, Hong Kong, United Arab Emirates, Qatar, Kuwait, Oman, Egypt, and Canada. The company has existing agreements with distributors throughout Europe, Australia, New Zealand, and Japan. Rampart manages direct sales in the United States.

The Rampart M1128 is a radiation shielding device for interventionalists. It is an adjustable, mobile structure that supports transparent lead acrylic panels
to create a protective wall between the medical team and the radiation source, which allows interventionalists to work without the heavy lead aprons that can cause orthopedic injuries.
Although the Rampart M1128 device was originally developed for interventional cardiologists because of the extended time they spend in catheterization labs, resulting in one of the highest levels of radiation exposure in the world, the device is beginning to be used by several interventional specialties.
tion for the School of Medicine will take place in the 2029-2030 academic year.
Birmingham Medical News FEBRUARY 2023 • 19 EDITOR & PUBLISHER Steve Spencer VICE PRESiDENT OF OPERATIONS Jason Irvin CREATIVE DIRECTOR Katy Barrett-Alley CONTRIBUTING WRITERS Jane Ehrhardt, Laura Freeman, Lynne Jeter, Marti Slay Birmingham Medical News 270 Doug Baker Boulevard, Suite 700-400, 35242 205.215.7110 AD SALES: Jason Irvin, 205.249.7244 All editorial submissions should be mailed to: Birmingham Medical News 270 Doug Baker Boulevard, Suite 700-400 Birmingham, AL 35242 or e-mailed to: editor@birminghammedicalnews.com All Subscription requests or address changes should be mailed to: Birmingham Medical News Attn: Subscription Department 270 Doug Baker Boulevard, Suite 700-400 Birmingham, AL 35242 or e-mailed to: steve@birminghammedicalnews.com Birmingham Medical News is published monthly by Steve Spencer ©2021 Birmingham Medical News, all rights reserved. Reproduction in whole or in part without written permission is prohibited. Birmingham Medial News will assume no reponsibilities for unsolicited materials. All letters sent to Medical News will be considered Medical News property and therefore unconditionally assigned to Medical News for publication and copyright purposes. birminghammedicalnews.com FOLLOW US GRAND ROUNDS ARMSA is administered by the Alabama Office of Primary Care and Rural Health and is supported by the Office for Family Health Education & Research, UAB Marnix E. Heersink School of Medicine For details visit https://aohw.org/2022-armsa or email ARMSA@uabmc.edu Apply for ARMSA today! Answer the call to practice in rural Alabama The Alabama Rural Medical Service Award (ARMSA) incentivizes primary care physicians and NPs to practice in rural, medically-underserved areas in Alabama. Eligible PCPs receive $50,000 a year and NPs receive $30,000 a year for up to 3 years as a service loan payable by years of service. PCP and NP must not have practiced in the rural area within 3 years of October 1, 2022. We’re looking for NPs in family medicine and for physicians in the primary care fields of: • family medicine • internal medicine • general pediatrics • internal medicine/pediatrics Earn $50,000 a year! ARMSA
The Rampart M1128.
Danielle Powell, MD (right), associate professor in the UAB Heersink School of Medicine, Dept of Physical Medicine, works with a student.
NOTE: if this is too long under the picture, we can go with : Danielle Powell, MD (right), associate professor in the UAB Heersink School of Medicine, works with a student.
No representation is made that the quality of the legal services to be performed is greater than the quality of legal services performed by other lawyers. Contact: Colin Luke 205-226-5717.



wallerlaw.com













 By laura FreeMan
By laura FreeMan





















 By Jane ehrhardt
By Jane ehrhardt











































































































 By Marti WeBB Slay
By Marti WeBB Slay




















 By Jane ehrhardt
By Jane ehrhardt










 By laura FreeMan
By laura FreeMan















































 By Beth VeSSel
By Beth VeSSel