Bereavement Support Book
Written by bereaved families and
midwives


Parents' names:
Baby’s name(s):
Date of birth:
Time of birth:
Weight:
Length:

Written by bereaved families and


Parents' names:
Baby’s name(s):
Date of birth:
Time of birth:
Weight:
Length:


Bereavement Midwife
T. 07971 939709
maternity.bereavement@nhs.net
Hereford Hospital Switchboard
T. 01432 355444
Maternity Triage
T. 07990 986517
Delivery Suite
T. 01432 364070
Maternity Governance Team
T. 01432 372963
Registry Office
T. 01432 260565
Maternity Screening Team
T. 07917 000102
Special Care Baby Unit (SCBU)
T. 01432 364162

Let us start by offering our deepest condolences following the loss of your precious baby/babies. Every single baby and the situation you find yourself in are unique. But the loss of a baby during any stage of pregnancy, birth or early after birth, is deeply sad and upsetting.
According to Sands, around 13 babies die before, during or soon after birth, every day in the UK. These are not just numbers, these babies belonged to families and every one of them are important. We have included these statistics to show you that sadly, you are not alone.
This booklet aims to provide you with the general information you will need immediately following the loss of your baby(s) and to help guide you in the longer term too.
In Hereford Hospital we use the symbol of a purple butterfly to help recognise and signal baby loss. You may see this butterfly on paperwork, door signs or equipment to help signal to staff that extra sensitivity is needed.

We have also introduced a butterfly lanyard for the same purpose. Bereaved mums are welcomed to wear these lanyards when attending the hospital for a follow up appointment hospital wide.
To ease some of the stress at this difficult time, free car parking is provided for the duration of your stay. Please ask your midwife for a ‘Forget-me-not car parking pass’. The ticket can be taken to the parking office where they will issue you with free parking for one vehicle.

We recognise that it is very important for you to be well supported by your friends or family. Visiting for friends, family and children, before and after labour is flexible and ultimately at the discretion of the midwife in charge. In labour we would encourage that you have a maximum of 2 consistent and supportive birth partners. You are likely to be physically and emotionally exhausted so please look after yourself and ensure that you get the rest that you need.
It is natural to have lots of thoughts and questions going around your head and during this time of great sadness families often find themselves desperately searching for answers. Please feel free to ask any questions, no matter how simple or strange they may seem.
Initial questions:

If your baby has not already been born, then the baby will need to be delivered. This may be by inducing a vaginal delivery or by an operation called a caesarean section.
Deciding how your baby is born is very individual, however the doctors and midwives can help you make an informed choice based on both your physical and mental health.
Choosing to birth your baby by caesarean section is a very individual decision and will be influenced by several things, including if you have had a caesarean section before, the gestation of your baby and your medical history.
When you are moved to theatre for your operation, you will be supported by a midwife. In theatre there will be an anaesthetist, obstetrician and the theatre team. We will try to keep the people around you to a minimum. To complete the caesarean, it is likely that you will have a spinal anaesthetic which will numb feeling from your waist to your toes; the feeling usually returns after a few hours.
In theatre, the environment can be adapted to make things as calm and sensitive as possible. You can still choose to play music and have a family member or friend with you.
Recovering from a caesarean section is likely to be more painful and intense than a normal delivery, therefore it is important to discuss the pain relief available to you. The wound from the operation will usually heal within 6 weeks, however will leave a scar, usually in your lower abdomen. Although it may be difficult to think about at the moment, it is important to know that a caesarean section will have an impact should you go on to have another pregnancy.

“Our initial reaction when we were told that our son had died was that we wanted to have a caesarean section. The thought of giving birth to a dead baby was almost unbearable. But of course this wasn’t just a dead baby this was our precious son and I am so glad that I was persuaded to give birth to him naturally. I feel proud of going through that for him. I held him within a minute of being born, after the midwife had dried him a little and wrapped him in a blanket – what a wonderful feeling that was to finally meet him.”
Kathryn, who lost her son Arthur.
If you decide that a vaginal birth is right for you, unless you are already in labour a course of tablets will be given to help bring on contractions. They are split into 2 stages.
The first stage involves taking a medicine called mifepristone, which is given orally as a tablet. This medication blocks the action of the natural hormone progesterone and can cause the cervix neck of the womb to start to open. Most women do not experience side effects from mifepristone. However, as with all medicines, these can occur and vary from person to person but may include:
• vaginal bleeding
• cramps/period type pains
• nausea (feeling sick) and vomiting (being sick)
• headaches
• skin rashes
Very occasionally, after taking the Mifepristone you may get worsening period or contraction-type pains, increasing bleeding, or lose fluid from your vagina before your next visit to hospital. These could be signs that the process is starting. If vaginal loss is heavy or pain is worsening, we advise you call triage or the delivery suite at Hereford County Hospital.
After around 24-48 hours you will attend the delivery suite at Hereford County Hospital, where we advise you are admitted until the baby is born.
Once settled onto Delivery Suite, you will be given a medication every 4-6 hours called Misoprostol; this may be given as an oral tablet or given vaginally. Misoprostol medication causes contractions which helps your body deliver the baby and placenta. Side effects from Misoprostol are rare but can include:
• abdominal pain
• diarrhoea
• nausea and vomiting
Sometimes getting labour started can take some time, please ask if you are unsure what may happen. Labour is different for everyone, for some it will be quick and likened to a bad period while others will find the pain difficult to manage and it may feel like it’s taking a long time. It will be difficult to predict how your body will react but the staff will guide you through the process and answer your questions.
You will be offered pain relief options to suit your needs and supported throughout the process. We recommend you discuss your pain relief options with your midwife and the anaesthetist who is caring for you.
Occasionally the placenta may be born at the same time as the baby but usually once the baby is born the placenta will need to be birthed. It is your decision whether you would like to wait for contractions to restart naturally to help birth the placenta or the midwife may offer you an injection containing a medication called Syntocinon. Syntocinon medication can help to speed up this process, this is known as ‘active management’. In most cases, active management is recommended as this helps to minimise bleeding however we encourage you to discuss this with your midwife or doctor.

Thinking about your baby’s birth and preparing for your stay in hospital can be really daunting. Below are a few things that you may want to think about and gather together to bring with you. We understand that there are a lot of choices and decisions to make at this time, so please remember to take your time and think what is right for you and your family. The items on the lists below are only a suggestion.
The Blossom room is well stocked with refreshments, tissues and has clothes and baby supplies for babies of all sizes and gestation. There is also a television, telephone and radio should you wish to use these.
Comfortable clothes, such as pyjamas
Items that brings you comfort - e.g., a teddy bear, pillow or blanket
Any medication you are currently taking
Dressing gown
Toiletries - e.g., Shampoo, conditioner, shower gel, toothbrush and toothpaste, hair brush, hair ties, deodorant
Towel
Phone charger
Breast pads
Maternity pads / padded underwear
Small snacks and isotonic drinks
Water bottle
Items to help keep you occupied - e.g., Books, magazines, a playlist on a phone or speaker, download films or TV series on a laptop or iPad
Comforting fragrance - e.g., Body spray, moisturiser or essential oils
A special outfit
A blanket and teddy
Re-sealable bags to help contain your baby's smell on fabric items
A story book
Precious items for photographs - e.g.,Wedding rings or special jewellery
You may have some preferences on how you would like to give birth. You can fill out the form below and let us know of these:
My birth preferences:
Room environment:
Dimming the lights natural light no preference
Music playlist:
Use of familiar smells:
I’d like my baby to be called:
Fetus Baby their nickname official name
People present:
Pain relief:
Alternative coping techniques I’d like to try:
Birthing the placenta:
Religious considerations:

At Hereford Hospital we have a dedicated family room called the Blossom Room, which leads in from the delivery suite and the main corridor. It has an ensuite, large bed, sofa, chairs, television and fridge.
The room was designed by bereaved families and looks a little different from other rooms in the hospital. We hope the facilities can offer you privacy and comfort during your stay.
When you give birth, you will be temporarily moved to another room to make sure we can keep you safe during this process, the delivery room will be adapted to your needs. You can spend time with your baby in either room.
If you decide to see your baby again after you’ve been discharged; this can also be arranged in the Blossom Room.
If you are invited to the hospital for a follow up appointment or to meet any member of the team, consultations can take place in the Lavender Room.
The Lavender Room is at the very end of the 2nd floor corridor. You should not need to go into Women’s Health or the maternity department.




Occasionally there may be complications during the process of inducing the birth of your baby(s). If you feel you need to discuss these further, please do ask your doctor.
Possible problems:
• The placenta being retained in the womb after the baby is delivered. Medication may help your body deliver the placenta, but if this is not successful then you will need a short operation. This is done through the vagina. You would have a spinal anaesthetic (an injection in your back to remove pain) or a general anaesthetic.
• Excessive bleeding. You may require medication to stop the bleeding, and sometimes a blood transfusion.
• Damage to the womb, such as rupture. This is very rare, an operation would be required under general anaesthetic to repair.

Unfortunately, some pregnancies do not progress as planned and some babies are found to have serious anomalies. Anomalies may be found on an ultrasound scan or on diagnostic testing during pregnancy but are not always picked up. If anomalies are found, depending on the extent of an anomaly parents could be faced with very difficult decisions and options about ending the pregnancy.
When the baby is not known to have any anomalies, one of the most common questions asked by parents is ‘What happened to my baby?’ Previous scans or the medical history may shed some light on why a baby has died. But, sadly, even after a post mortem, we do not always know exactly why a baby has died.
Haemorrhage
Umbilical cord problems
Placental problems
Genetic conditions
disorders
If not clear in your pregnancy, the midwives may offer you different tests to help investigate if there was anything that contributed to the death of your baby. You are welcome to ask for more information or to decline these investigations.
• The midwife can very gently examine your baby and will take extra caution to note anything during the birth, such as any differences with the cord or placenta.
• You may also be offered blood tests, these can be taken before or after birth. The blood tests you might be offered will include: looking for any evidence of bleeding between your blood and the baby’s, evidence of diabetes, blood clotting concerns, lupus, common virus (cytomegaly virus, parvovirus, syphilis, toxoplasmosis, herpes simplex virus), evidence of infection and to check your liver and kidney function.
• The midwife can also offer to take swabs from you and your baby to check for signs of infection. They are likely to include a vaginal swab from yourself, a swab from the placenta and a ear, nose and groin swab from your baby.
• Your placenta can be examined firstly by your midwife to look at the basic structure of your placenta and for obvious differences.
It is likely that your placenta will then be sent for further testing to Birmingham Women’s Hospital (BWH). Please ask your midwife if this will happen.
At BWH they will look very closely under a microscope to see if there is anything else that can be picked up which can’t be seen by the naked eye. The results of this examination can take around 10 months to return. Once the results are received a follow up appointment is arranged by your bereavement midwife.
• A post-mortem examination of your baby may help to find out why your baby has died. Although it does not always find a definite cause of death, it may still answer some questions and rule out some possible causes of death. If you already know the immediate cause of your baby’s death, a post-mortem might confirm this or highlight additional problems that might be useful for you to know for a possible future pregnancy.
If you would like to discuss a post mortem further, please let your midwife know. They can provide further information and ask a senior doctor or the bereavement midwife to discuss this with you.
• If a problem is suspected in your pregnancy you may be offered genetic testing whilst you are still pregnant. Genetic testing may also be offered after birth alongside a post mortem investigation.

The doctor looking after your baby must, by law, refer the case to a coroner if:
• The death is sudden and unexpected
• The cause of death is not known
• The death occurred as the result of an accident or unnatural cause
• The death occurred after surgery
It is their job to ascertain where and when the baby died. They can establish the cause of death and determine whether it is thought to be “unnatural”.
If the coroner is concerned about the circumstances of the baby’s death being suspicious, they will open an investigation and then possibly an inquest. The coroner may then write a report about any specific concerns. As parents, you will be given the details of when and where the inquest will take place. You may be called in as a witness, in which case you must attend the inquest. You can ask any questions you have at the inquest. There may be other professionals who are asked to be witnesses.
It is not common for a coroner to open an inquest into the death of a newborn baby in hospital, but if they do, they may require a post-mortem.
In this instance, parents are not asked for their consent, but the coroner’s office will keep them informed about any decisions that are made.
Once the coroner or procurator fiscal decides that no further examinations are required, they will inform the registrar. You will then be able to obtain the certificates that you need to organise your baby’s funeral.

It is important to understand as much as we can about what happened and why your baby died. The team at Hereford Hospital will start to review your care, this may take a number of months to complete. The type of review will depend on the circumstances around your baby’s death.
The review team discussing your care may include doctors who care for women in pregnancy (obstetricians), doctors who look after new-born babies (neonatologists) and senior midwives. If there are any other health professionals specific to your care we will invite them also. The aim of the review is to try to understand as much as possible about what happened and why your baby died.
The team will:
• look at medical records, tests and results, including post mortem results if you have consented to this
• answer any questions you may have and address any concerns
• talk to staff involved
• look at guidance and policies to ensure the care you received was appropriate.
The review may tell us that we need to change the way we do things or that good and appropriate care was given to your family.
The care of every bereaved family is reviewed. If you made the difficult decision to end the pregnancy for medical reasons the bereavement midwife will review the bereavement care you received and work with the Governance team if there were any other concerns or issues that arose.
For all other families, your care is reviewed using a national system called InPhase where the case will be presented to a multi-disciplinary team before any actions are taken and the review closed.
The PMRT is used to notify and investigate cases of:
• All late miscarriages 22+0 weeks to 23+6 weeks
• All stillbirths
• All neonatal deaths from 20+0 weeks to 28 days after birth
• All post-natal deaths where the baby is born alive from 20+0 weeks but dies after 28 days following care in a neonatal unit
If your circumstances meet those listed above, you will be informed that a review will take place.
Your views are important and it would be helpful if you could share your feelings and thoughts about your care before we carry out the review. The bereavement midwife will send you a feedback form that will help prompt your thoughts.
We will address any questions or concerns you have in the hospital team review meeting. You will not be asked to attend the meeting in person. It may take some time to gather all the information required for a review meeting. We understand that this is a long time to wait and if you would like to meet with a consultant before the review takes place, you can arrange this through the bereavement midwife. We may, however, not have any further information about what happened and why your baby died by then.
The review meeting will take place with health professionals from another hospital to ensure that the review isn’t biased. Every aspect of your care from booking to beyond birth will be considered. The review will use the PMRT to help the health professionals to be objective and thorough.
Once the review report is completed, a consultant can discuss its findings with you. We can also send you the review report by post or email if you prefer. Similarly, if you do not wish to know the outcome of the review, this is okay.
If you would like to know more please go to: www.npeu.ox.ac.uk/pmrt/information-for-bereaved-parents
If your baby was born alive, your care will be independently reviewed by a local CDOP. The panel do not investigate the cause of an individual child’s death but they look at all child deaths to understand if there is any learning that could help improve care and prevent children dying in the future.
Following a local review meeting, a report is not made for each child. Instead, the CDOP make recommendations about the lessons learned to those responsible at a local level and an annual report is written; this is a public document. Anyone can read the annual report, but it does not contain any details that could identify an individual child or their family.
The CDOP will submit data to be collected on a National Child Mortality Database, this is a legal requirement. Collecting this information will ensure that deaths are learned from, that learning is widely shared, and that actions are taken, locally and nationally, to reduce preventable child deaths in the future.
The MNSI investigates cases of:
• Early neonatal death (born after 37 weeks gestation)
• Stillbirths during labour
• Severe brain injury in babies
• Maternal deaths in England
If your circumstances meet those above, it will be offered that the MNSI conduct an independent review of your care.
If you consent to participate in the investigation, you will be contacted by a named investigator who will explain more about the investigation process and keep you informed throughout. MNSI aim to complete all investigations within six months however every investigation is different. All other case reviews will be paused whilst this review takes place.
If you would like to know more please go to: www.mnsi.org.uk/for-families/

Some parents wish to see and hold their baby straight away and others choose not to. Many parents are anxious about seeing their baby as they are unsure of how they will feel and how the baby will look. It is normal to feel this way and the midwives will be at hand to talk through any concerns, answer any questions and talk to you about what your baby looks like. Your baby can be wrapped in a blanket and wear a hat and you may wish to have these as keepsakes later. You will be able to hold your baby and talk to them if you would like to. Everyone is different, and it is important that you do not feel pressured into making an immediate decision.
In the hospital, you can spend as much time with your baby as you wish. You may be given the opportunity to bath and dress your baby, with or without the support of midwives. You may decide to bring in outfits for your baby to wear. Your midwife or consultant should be able to give you an idea of what size clothing you will need before the birth.
Some specialist shops include:
www.little-mouse.co.uk
www.superdinky.co.uk
www.cheekychumsonline.co.uk
The hospital also have a range of clothing carefully picked by bereaved families that you are very welcome to use.
The stage of pregnancy when you experienced your loss may determine how you choose to remember your baby. Sensitive guidance will be first given to you by the midwife. They will help you to make choices which will enable you to make precious memories, following the delivery of your baby. How you feel before, during and after the delivery may change, so please keep talking to the staff that are looking after you.
All memory making supplies given to you by the hospital are free of charge.
If you are unsure about wanting any of these, the midwives can put them in an envelope for you to take home and you can look at them in your own time.
You will also be offered a special memory box that includes small mementoes which are aimed to provide comfort. The boxes can be tailored to include what you would like and you can add your own cards, letters from parents and/or siblings, photos, drawings, teddies etc.
Some families shared that having two identical copies of some items was useful so one could be left with baby and one can be kept by you.
Some other memory making ideas can include keepsakes such as:
• A lock of hair
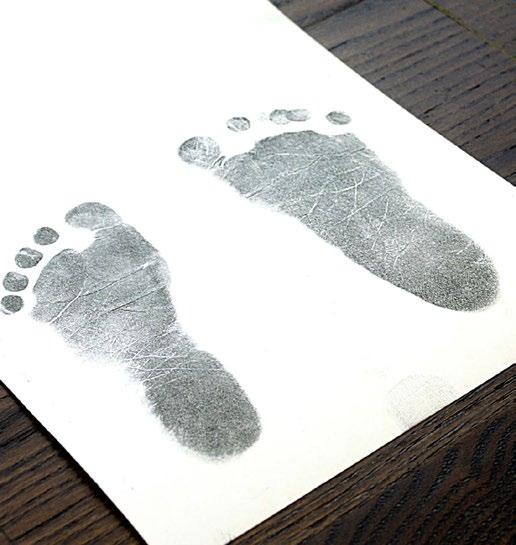
• Hand and footprints
• Hospital tags and bracelets
• Photographs
• Special blankets

• Scan pictures
• Pregnancy notes
• Baby clothes and hat
• Special teddies

“Having Reuben’s footprints means that we could go to the jewellers that made our wedding rings and have something made personal to us, that we can keep forever”.
- Sarah, Reuben’s Mum
“Because Penny was not full term, I was really worried that she may not be very well developed and have some deformities or that her skin would be too fragile for us to hold her. I felt guilty that I had these concerns, but I was also scared of how I would feel about seeing her. I asked Sam the midwife to clean her up after she was delivered and let me know if there were any abnormalities for me so that I could prepare myself. Sam cleaned up Penny, put her in a woolly hat and wrapped her in a blanket. When she passed her to me, she looked like she was sleeping. Her skin was fragile around her hands and feet, but she was otherwise perfect and I loved holding her.
I’m so glad we had the opportunity.”
- Laura, Penelope’s Mum

‘Remember My Baby’ is a non-profit registered charity created by professional photographers for the benefit of bereaved parents across the UK. Their goal is to have baby remembrance photography offered as a choice in every hospital across the UK.
Photographs are one of the most tangible mementoes that parents can have. These portraits will honour a tiny life that is always loved and cherished and never forgotten.
A RMB Volunteer Photographer will come to the hospital or birth centre and carry out a sensitive, portrait session for a family in need. Parents are provided with professionally edited black and white images on a USB memory drive free of charge.
Please note that in general, 24 weeks gestation is the minimum gestational age that an RMB photographer will attend. However, it will be at the discretion of the individual RMB photographer whether they attend an earlier loss.

You are welcome to take your own photos whether RMB attend or not. Hereford Hospital have a camera that you are welcome to use.
If you think that this is something that you think you would like, please ask the midwife caring for you for more information.
“I decided that it would be better to have a photo I might never look at than to want a photo that I do not have”
- A bereaved father




If you wish to be supported by one of the hospital chaplains please let your midwife know.
The chaplaincy team are able to offer a blessing and a naming ceremony if you would like.
You may prefer for your own religious leader to attend. They are welcome to visit to support you.
If there are any religious or cultural practices that you would like to carry out for your baby please let us know and we will try our best to ensure that everything is done as you wish.
At Hereford Hospital we stock ‘Ibraheem’s Gift’; this gift pack was designed by 4Louis in close consultation with a hospital Imam and contains the immediate necessities that allow parents to prepare for their baby's muslim burial.
The pack includes white cotton burial shrouds, a memory blanket and hat, attar bottle (scented oil), Tasbih (prayer beads) and a book ‘Remedy for grief from the Islamic perspective’.
We also have memory boxes that are specifically designed for Muslim families.


Your body will react physically in the same way as if your baby had been born alive or deceased.
If you experience any of the following, please seek medical help immediately. Depending on the severity, either an ambulance on 999 or maternity triage on 079 9098 6517.
• Experiencing chest pain or shortness of breath (call 999)
• Bleeding heavily, filling a large sanitary pad in 1 to 2 hours or if you are passing blood clots larger than the palm of your hand or size of an apricot/plum
• Experiencing thoughts of harming or killing yourself
• Experiencing pain, redness or swelling in one leg
• Feeling unwell with flu-like symptoms
• Experiencing a persistent headache and have blurred vision
Your body will naturally start making milk around the 16th week of pregnancy. After birth your body will undergo hormone changes that lead to milk production.
Some parents find this experience very upsetting and may want to stop their milk production as quickly as possible. Others may find the idea of making and expressing their milk comforting. There is no right or wrong way to feel.
It is possible to reduce the symptoms of you milk ‘coming in’ and gradually the amount of milk you produce naturally; this process may take several weeks.
You will need to reduce your supply slowly to avoid discomfort and reduce the risk of breast inflammation. You may find it helpful to wear breast pads for the first few days if you find you’re leaking milk.
You may like to try:
• Using a cold compress for 15- 20 minutes
• Wearing a well-fitting bra
• Putting chilled cabbage leaves on your breasts to reduce the pain and swelling (there isn’t a lot of evidence that this works but helps some people)
• Using pain relief, such as ibuprofen or paracetamol (please read the instructions and discuss with your GP if you are unsure)
• Expressing small amounts by hand, just enough to ease the pain, otherwise you will encourage the production of more milk
You may prefer the support of medication. The medication is called Cabergoline. If the medication is taken within the first 24 hours after birth you should only need to take one tablet. Like all medicines, there may be side effects and it may not be suitable for all parents, so please ask your midwife for support.
Some parents find that expressing their milk for donation can be comforting. Occasionally parents will have already expressed milk in preparation for their baby. You may wish to consider donating your breast milk to a UK Milk Bank for use in research or for another baby in need. When a mother is unable to give any or enough of her own breastmilk for premature and sick babies, donor breastmilk is preferred to infant formula as it contains antibodies to fight infection.
If this is something you think you would like to know more about, please speak to the Bereavement midwife or visit www.milkbankchester.org.uk/donationafterloss
Most women experience tenderness and ‘after pains’ (cramping) following birth which is easily managed with simple pain killers such as paracetamol and ibuprofen (please read the instructions and discuss with your GP if you are unsure).
In the initial period following your loss you are likely to experience a mixture of emotions and your mental health may be impacted. These feelings are a natural response to loss. In addition to grief, some mothers may experience normal postnatal blues a few days after the birth as pregnancy hormones regulate.
Initially you may experience:
• Difficulty completing everyday tasks e.g., cooking, cleaning
• Reduction in self-care, such as washing and bathing
• Under or over eating
• Over sleeping or not being able to sleep
• Difficulty in leaving your home
• Reliving your experience (flashbacks)
• Nightmares
• Intrusive thoughts
Many of the symptoms listed above will subside, however if you are noticing these symptoms are lasting for longer please contact the bereavement midwife.
Occasionally losing a baby can have a more severe impact on your mental health. In this case you may experience:
• Inability to leave your home
• Consistent intrusive or uncontrollable thoughts
• Inflicting pain or harm on yourself
• Thoughts and plans to end your life
If you experience any of the above please attend A&E, contact maternity triage on 07990 986517 and the bereavement midwife for immediate support.
Hygiene and comfort are important after birth. It is a good to change your pads frequently to help prevent infection, avoid using tampons, wear cotton underwear, and wash your hands before and after using the toilet. It can help to have a jug of water on hand (in the toilet) so you can clean and cool the area after having a wee. Stitches usually dissolve by the time a cut or tear has healed.
After the birth, you will bleed through the vagina. This is called lochia and it is your body getting rid of the lining of your womb and blood from where your placenta was attached. Everyone is different, but for most it will be heaviest for around 2 weeks and then will be lighter until around 6 weeks after the birth. At the start, it may have some lumps or small clots in it. It changes colour from red, to pink, to brown. The flow of this blood loss can increase and decrease, so don’t worry if your bleeding was easing off, but then looks heavier the next day; this is normal.
It can be worrying going to the toilet after giving birth because of fear of the pain, worry about the stitches breaking and the lack of sensation, or control.
Avoid constipation by eating a high fibre diet and drink plenty of fluid, especially water. It might give you confidence to hold a clean pad of tissues over the stitches while you do a poo. But try not to worry, it’s very unlikely that going to the toilet will affect your stitches. If you are having difficulty opening your bowels please contact your midwife or GP for advice.
During pregnancy and following birth your blood is thicker and sticky; this happens naturally to help your blood clot following the birth and delivery of the placenta, but means that blood clots in the legs and lungs are more common.
We would encourage you to make sure you keep well hydrated and mobilise gently but often. You may also be sent home with some injections that will help to prevent bloods clots, you should be taught how to use these before you are sent home.
Pelvic floor exercises
Pelvic floor exercises help to strengthen the muscles of the pelvic floor, which come under great strain in pregnancy and childbirth. The pelvic floor consists of layers of muscles that stretch like a supportive hammock from the pubic bone (in front) to the end of the backbone (spine). Pelvic floor exercises should be started as soon as you feel able.
How to do pelvic floor exercises:
1. Close up your bottom, as if you're trying to stop yourself going to the toilet
2. At the same time, draw in your vagina as if you're gripping a tampon, and your urethra as if to stop the flow of urine
3. At first, do this exercise quickly, tightening and releasing the muscles immediately
4. Then do it slowly, holding the contractions for as long as you can before you relax: try to count to 10
5. Try to do 3 sets of 8 squeezes every day: to help you remember, you could do a set at each meal
As well as these exercises, practice tightening the pelvic floor muscles before and during coughing and sneezing.
Avoid heavy lifting for four to six weeks after the birth. Always bend your knees and keep your back straight when you lift things. Hold heavy objects close to you and avoid twisting as you lift. You should always take care of your back but remember it is especially vulnerable for 3-4 months after your baby’s birth.
Listen to your body, go at your own pace and stop if it hurts. Swimming is an excellent way to regain overall fitness and to tone up muscles, but ensure that any wounds have healed first.
This will vary from woman to woman depending on the healing process and when you feel comfortable enough to be able to consider trying. It may be helpful to use a non-perfumed lubricant jelly. If intercourse continues to be painful or if you feel ‘things aren’t right’ since your baby’s birth, please see your GP. Further information can be found in the SANDs booklet.

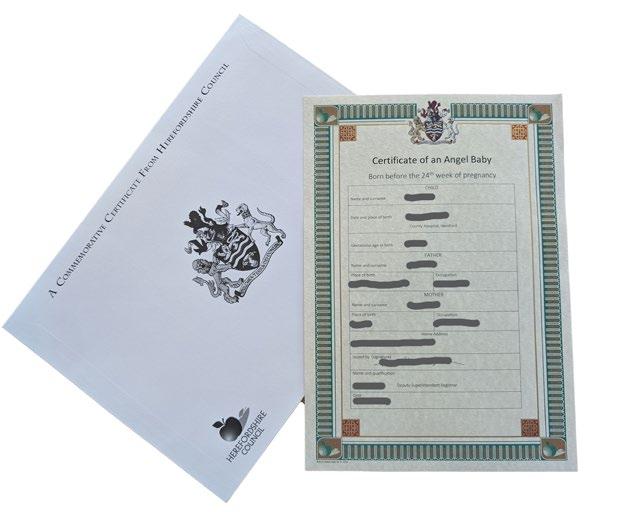
Babies born before 24 weeks do not receive a lawful death certificate. However, the county of Herefordshire acknowledges that every baby is extremely precious and offer an official Certificate of Acknowledgement for babies born before 24 weeks gestation; this is known as an ‘Angel Certificate’. Your midwife should offer this to you, however please don’t be afraid to ask if they haven’t managed yet.
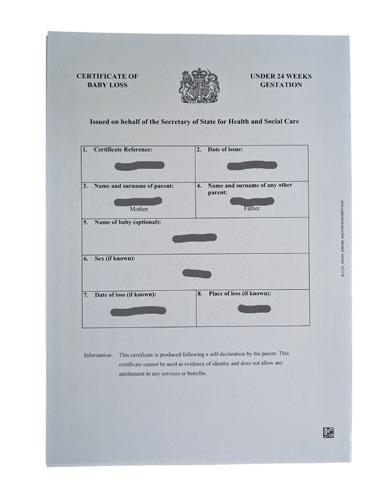
Alternatively, a ‘Baby loss certificate’ can be requested by parents directly from the Government website at www.gov.uk/request-baby-loss-certificate
The Births and Deaths Registration Act 1953 defines babies that are born, without signs of life, over 24 weeks gestation as ‘stillborn’. A stillborn baby must be registered in the Stillborn Register within 42 days from birth.
When a baby is born alive and later sadly dies, the birth must be legally registered, whatever the length of the completed pregnancy, within 42 days. The death must be registered in the same way as any other death within five days.
Your midwife will complete a hospital certificate which will be sent to the registry office by the bereavement midwife. Once the registry office receive the certificate, they will contact you to arrange an appointment to register your baby. We encourage you to make sure you have identification (ID) with you. Parents who are not married at the time of their baby’s birth and wish for both parents to be on the certificate must be present during the appointment. A funeral can only go ahead once your baby has been registered.
The address of the registry office is: Town Hall, St Owen’s Street, Hereford, HR1 2PJ Tel: 01432 260565

Once you leave the hospital, your baby will rest in the hospital mortuary. If you consent to further investigations planned, your baby will be transferred to another department or hospital and will return to the mortuary in preparation of being laid to rest according to your wishes – should you wish, the bereavement midwife can keep you informed where your baby is.
It may be the first time you have had to think about organising a funeral, it is natural to feel overwhelming and difficult to know where to start. Funerals can be a way of acknowledging your baby’s death and can be helpful in the stages of grieving.
You can opt for a non-religious ceremony or you may wish to organise a church service in your local parish. It may be that you decide to have very few people in attendance, or you may wish to have all your family and friends.
It is important that you take your time and choose what is right for you and your family. Afterwards, most parents feel comforted that their baby was laid to rest with dignity and respect.
By law, all live born or stillborn babies are required to be buried or cremated, however this does not mean you are obliged to have a funeral service. If you would prefer not to take part in the decision about how your baby is laid to rest, the bereavement midwife can arrange a shared cremation on your behalf. You will need to sign a consent form with your chosen wishes or to let us know you’d like more time.
Please note, if we do not hear from you and arrangements aren’t made within 6 weeks of your loss, your baby will laid to rest by shared cremation.
Funeral directors will provide a basic funeral for free, however there is often a charge for additional services such as; order of services, carriages, flowers and headstones. If the hospital chaplain or any other religious leader of the family’s choice officiates at the service, this is usually free of charge. Church fees are also generally free, but there may be a charge for an organist. You can also apply to Rocky Lees Little Feet for financial relief to assist with memorial headstones or plaques for stillborn babies.
A shared cremation is where your baby would be cremated alongside other babies and pregnancy tissue. All babies and pregnancy tissue are blessed by the hospital chaplain prior to being transferred to Hereford crematorium. At the crematorium there will not be an officiated service, however you are very welcome to attend to spend a moment of quiet before the cremation takes place.
The ashes will be scattered in the forget-me-not garden according to the season - spring, summer, autumn or winter. There is no financial charge for the service of a shared cremation.
An individual cremation is where your baby would be cremated on their own. The bereavement midwife will work closely with you and the hospital's contracted funeral director to make these arrangements. It cannot be guaranteed that there are ashes available after the cremation but this is rare. The ashes can be collected by yourself, or scattered on your behalf at the crematorium.
You can choose to have a service and if you wish, you can attend along with other family members. The hospital chaplain or your local religious leader can be involved. Ashes can be turned into beautiful jewellery and keepsakes, be kept at home or scattered in a special place.
An individual burial is where your baby would be buried on their own, usually in a graveyard or natural burial ground. The bereavement midwife will work closely with you and the hospital's contracted funeral director to make these arrangements. You can choose to have a service and if you wish, you can attend along with other family members. The hospital chaplain or your local religious leader can be involved. If your baby is buried, this may offer you a place to visit, and comfort that they are with family or other babies nearby.
Private arrangements is when you choose to make arrangements with a funeral director of your choice; this may be a company that family or friends have used or is more convenient for you. Families can choose a funeral director to arrange a cremation or burial within a cemetery, churchyard or crematorium.
Careful thought must be given when considering burial in a garden, taking into account what would happen if you were to move house or the land is used for new purposes in the future.
It is acceptable for parents to bury their pregnancy remains in their own garden/land if they choose to.
The law supports this choice as long as:
• It does not cause any danger to others
• It must not interfere with any rights other people may have on the land
• There must be no danger to water supplies or watercourses
• There must be no chance of bodily fluids leaking into or onto adjoining land
• The pregnancy remains must be buried at a depth of at least 18 inches.
• Permission must be obtained from the landowner if the parents do not own the land
Funeral notes:
Type of funeral: cremation burial
Funeral Directors:
Type of service: Religious Non-religious No service
Guests:
Dress code:
Order of service:
Hymn/song choice:
Readings/poems: You may find some relevant poems at lilymaefoundation.org/poems
Flowers: .............................................................................................................................................................................................
Donations:
Wake location:

There are many decisions to be made at this sad time, and one may be that you are considering taking your baby home.
A majority of families who chose to take their baby home, tell us this is something they are glad they did, and looking back, are thankful for the time they had with their baby.
Reasons families take their baby home include:
• Spending more time with their baby in the comfort and privacy of their own home
• More time to create memories with their baby, and gather keepsakes away from the hospital setting
• An opportunity for any siblings, extended family or friends to meet their baby
• Time together as a family to say goodbye to their baby
It is important your baby is transported home in a safe and dignified manner. You can transport your baby home in your own car or arrange for a family member or friend to drive you home in their car. You may want to use a car seat or a moses basket so you can safely secure your baby in the vehicle.
It is not advisable to take your baby home using public transport. If you wish to take your baby home in a taxi, we advise you check first with the company that the driver is happy to do so.
Once at home, it is important to keep your baby cool. We do not recommend opening windows or having fresh flowers in the room, to minimise the risk of exposure to insects. We would also advise any pets are kept in a separate room to your baby.
We would encourage you to borrow one of our Flexmort CuddleCots™ home with you, your midwife will show you how to set up the cool cot before you leave the hospital. Ideally, your baby should be kept in contact with the cool cot mat as much as possible. It will quietly cool your baby, to slow down the expected physical changes which happen following death. This can include changes to your baby’s skin colour and lips, their skin may become more fragile, and you may notice some pink fluid leaking from their nose, mouth or skin. All these changes are normal.
You may care for your baby as you wish at home, including bathing (with cool water) and dressing, however over handling may increase the rate of the changes outlined above. If your baby’s skin is particularly fragile, it may be advisable to place your baby on a pillow and hold the pillow when giving them cuddles.
If you have other children at home, let them be involved as much as they or you think is enough for them. Talking to your children to explain how your baby looks and that they feel cold to touch, can be helpful.
You may want to take your baby home for a few hours or a few days. The national guidance is to take your baby home for a maximum of 3 days, however the length of time your baby is at home with you will depend on your wishes.
When you are ready, you can bring your baby back to the hospital or arrange for your chosen funeral director to collect your baby from your home; this will be arranged with you prior to you leaving the hospital.

Some parents may wish to return to the hospital to visit their baby. It is preferred if this is arranged in advance with the bereavement midwife to ensure that we can support you appropriately, however we understand that this is not always possible.
Visiting is likely to take place in the Blossom Room, however can also take place in the Lavender Room or mortuary viewing room. During your visit, dependent on how long you want to spend with your baby, a cold cot can be set up to allow you more time.
If you have chosen for your baby to have a post-mortem, you are able to visit your baby at the hospital before and after they are transferred. However, the earlier the examination is held, the more likely it will provide useful information.
We sadly know that the condition of the baby gradually deteriorates over time, and whilst we try everything we can to prevent this, it is a natural process that we only have so much control over. It is a good idea to think if you wish the bereavement midwife to visit the baby first to describe how your baby looks now and if their condition has changed significantly. For some parents the change in their baby’s condition doesn’t matter, however other parents prefer to remember their baby as they were when they were first born.
We kindly ask for you to bring ID when you return to visit your baby. It may be useful to decide if you would like anyone with you to support you.
If the mother doesn’t wish to visit baby again and other family members and friends do, this is okay as long as permission is granted by the mother.

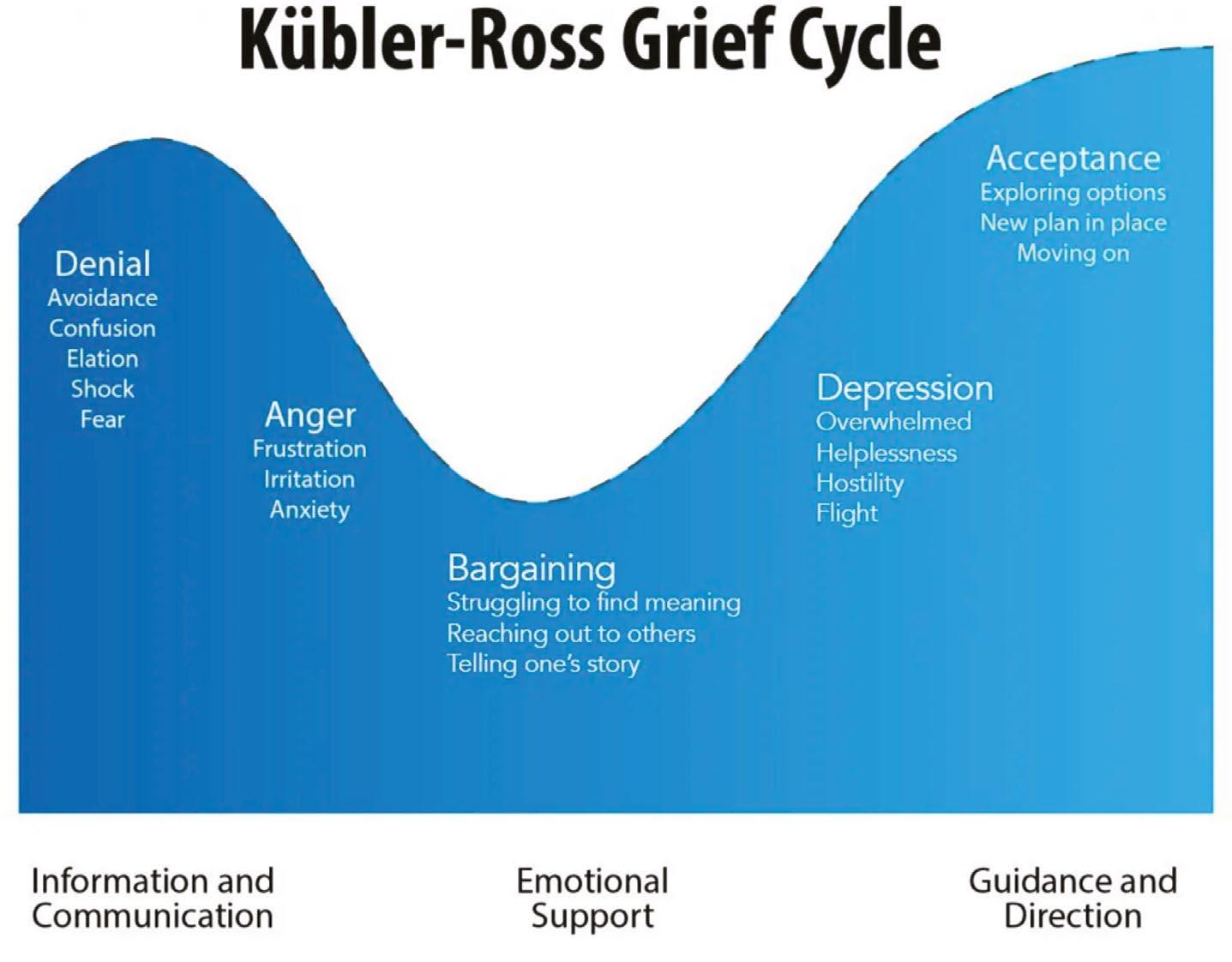
There are various theories of grief. We have chosen two that are likely to help you understand that your feelings are valid both now and in the future.
The idea is there are 5 basic stages of grief that in reality will be experienced in a random and unexpected order as grief is a very individual process. You are likely to feel a wide range of emotions and physical reactions, such as altered sleeping and eating habits. These feelings can be both frightening and confusing but are very normal whilst grieving. It is important to be kind to yourself and allow time to follow a natural grieving process.
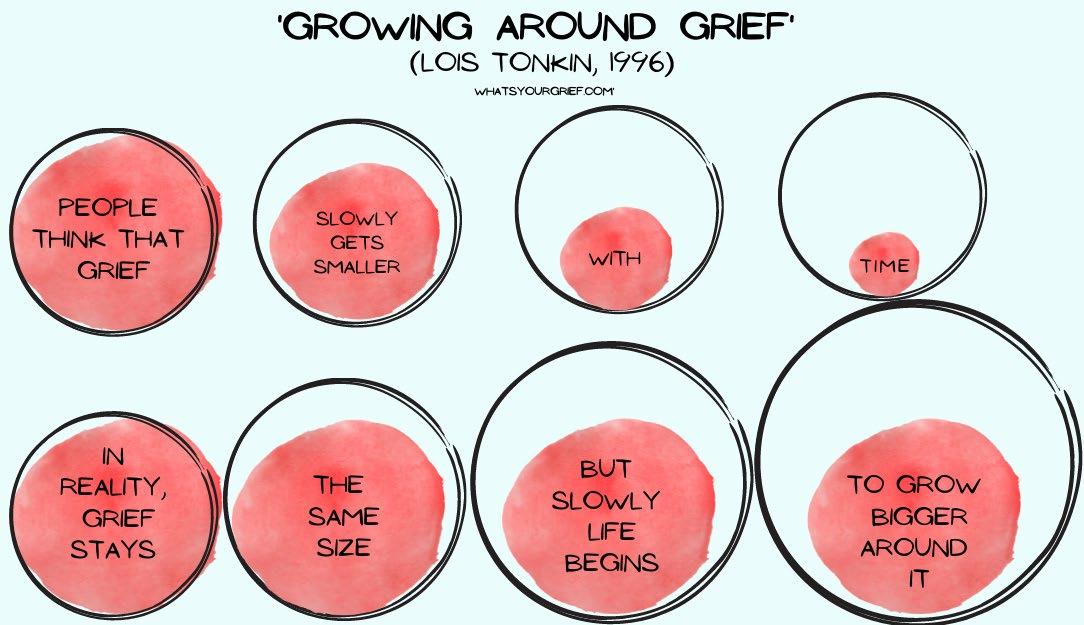
The idea is that your grief remains intact and that your life grows around it. The grief of losing your baby initially takes up almost every part of you, but as time goes on, and with support, your grief does not diminish but other aspects of life grow around it, enabling you to find a new kind of normal.
This view of grief does not tell someone that their grief will go away in time. You will never be ‘over it’. The model acknowledges that there will be some days where you feel grief as strongly as you did when the person first died. But there will also be days when you are able to move forward with other parts of your life.

Some people like to read about those who have undergone similar experiences to themselves. The following books can be picked up and put down in your own time, at your own pace. Sometimes just dipping into a chapter can be helpful.
In the Blossom Room we have a bookshelf filled with books that have been recommended by other bereaved parents.
Please feel free to take these books home and either pass them on when you have finished or bring them back to the hospital for another family to use.
“I’ve just read Ask Me His Name. It was lovely, very different from my experience but also very relatable in other ways. I found it helpful having something to read while I waited to collect my son from school.”
- Amy, Joshua’s Mum

Many people agree that there are positive and negative aspects to social media. Posts can help spread news and be a means of expressing feelings. However, some people may find social media full of triggers, such as pregnancy or birth announcements and can leave them feeling alone or isolated. Some people turn to social media in search of like-minded people who may understand their experiences. There are many groups that can provide a forum of support. These may be specifically for parents, mothers, fathers, or anybody who has suffered a bereavement.
After a baby loss, it can be very upsetting and frustrating to continue to receive promotional coupons and information for baby related items through your email.
You may find it helpful to contact the Baby MPS (Mailing preference service) and register to stop these communications.
Please go to: www.bmpsonline.org.uk
Locally we use The Real Birth Studio to help deliver antenatal care. You may have already signed up to receive communication and education from this company, to cancel this please scan the QR code.



To avoid well-intentioned, but potentially hurtful questions about your pregnancy in the weeks and months to come, you may want to post an announcement about your loss.
Ultimately, how you communicate the loss of your baby is up to you. So, don't feel pressured to handle things in a specific way.
Alternatively, you may wish for a close friend or family member to do this on your behalf.
Below, you’ll find some suggested wordings for loss announcements of many kinds.
We lovingly honour the memory of our son/daughter, (name).
It is with heavy hearts we announce we are no longer expecting a child. Our son/daughter was born sleeping on (date). Thank you for your care and support during this difficult time.
We would like to announce the birth and death of our sweet son/ daughter (name), on (date). He/she was a beautiful baby who will always live on in our hearts. We take comfort in knowing (name) is now watching over us from beyond.
Thank you for all your well wishes on my pregnancy. I’m deeply saddened to tell you I’ve miscarried. There will be a small memorial service on (date) at (location). We’d love to have you with us as we honour the memory of our baby.

During your journey you will meet a bereavement midwife who will be your key contact at the hospital. If the bereavement midwife hasn’t met you during your inpatient stay, they will be in contact shortly after you return home to offer further support and guidance.
The Maternity Bereavement Team contact details are: Mobile: 07971 939709
Email: maternity.bereavement@nhs.net
The bereavement midwife can support you by:
• Providing immediate bereavement support, including birth planning and memory making
• Communicating and co-ordinating your care amongst the wider hospital team
• Providing long term bereavement support; this may be via phone call, text, meetings in the hospital or in the community
• Keeping you informed of where your baby is resting
• Supporting you and your family in organising a funeral for your baby
• Advising and signposting if you have any concerns or questions
• Advocating for you and ensure your voice is heard during case reviews and ongoing care
• Organising debrief and follow up appointments with your named consultant and supporting in the process of feeding back the results from clinical investigations
• Continually developing the bereavement service to ensure it is the best it can be for bereaved parents
• Referring you for further support, such as specialist counselling or mental health services
• Supporting you should you decide to have another baby
Proudly funded by The Born Sleeping Appeal, Hereford Hospital has partnered with PETALS – a specialist baby loss counselling charity. The counselling programme is unique and specifically designed to meet the needs of parents who have suffered pregnancy loss complications.
Usually following referral, you will be contacted to arrange a triage assessment to hear more about your story and to help match you with your counsellor. From there you will be offered up to 5 virtual sessions and signposted after these if further support is required.
If you feel that counselling would be useful, please let the bereavement midwife know to organise the referral. Occasionally, the bereavement midwife may suggest another service based on your individual needs.

The baby loss counselling charity - Petals Charity

Email: info@achingarms.co.uk
Tel: 07826 067801
www.achingarms.co.uk
Aching arms offer beautiful comfort bears to fill your arms and a community to support you as you grieve via a dedicated ‘Supporting Arms’ service.

ARC
Email: info@arc-uk.org
Tel: 020 7713 7356
Helpline: 0845 077 2290 or 0207 713 7486
(Monday - Friday, 10.00am-5.30pm)
www.arc-uk.org
ARC is the only national charity helping parents and healthcare professionals through antenatal screening and its consequences.
Bliss
Email: hello@bliss.org.uk
Helpline: 0808 801 0322
www.bliss.org.uk
Bliss champion the right for every baby born premature or sick to receive the best care by supporting families, campaigning for change and supporting professionals, and enabling lifechanging research.

Email: support@childbereavementuk.org
Helpline: 0800 0288840 www.childbereavementuk.org
Supports families and educates professionals when a baby or child of any age dies or is dying, or when a child is facing bereavement.
Email: support@lullabytrust.org.uk
Helpline: 0808 802 6868 www.lullabytrust.org.uk
Provides specialist support for bereaved families and anyone affected by a sudden infant death.
Email: info@miscarriageassociation.org.uk
Helpline: 01924 200799 (Monday - Friday, 9am-4pm) www.miscarriageassociation.org.uk
Providing support and information to anyone affected by miscarriage, molar pregnancy or ectopic pregnancy.

Email: rockyleesfund@gmail.com www.rockyleeslittlefeet.co.uk
Provide financial support to people in the UK who are struggling to afford a memorial headstone or plaque for their baby.

Helpline: 0808 164 3332
Email: helpline@sands.org.uk
Befrienders email: support.hereford@sandsvolunteer.org.uk
Local enquiries: hereford@sandsvolunterr.org.uk www.sands.org.uk
Stillbirth and neonatal death charity, supporting anyone affected by the death of a baby and promote research to reduce the loss of babies’ lives.
Hereford has their own dedicated befrienders and monthly support group.

Email: mailbox@tommys.org Tel: 0800 0147 800 www.tommys.org
Tommy's is the largest UK pregnancy and baby loss charity, funding research into stillbirth, premature birth and miscarriage and providing trusted pregnancy advice and support.

Email: helpline@tcf.org.uk
Helpline: 0345 123 2304 www.tcf.org.uk
The Compassionate Friends have a wealth of helpful leaflets and run support groups and retreats.


Please reach them via their contact form www.theteddyrosefoundation.org
Provide support to bereaved families through various platforms and support groups in Solihull.
They also provide special cuddle blanket, care packages and heart in their hand keyrings.
The Lodge, Balsall Street East, Balsall Common, Coventry West Midlands, CV7 7FR
Please reach them via their contact form www.lilymaefoundation.org
Provide extensive support options for bereaved families across the West Midlands including:
• Memory boxes
• 1:1 counselling
• Podcasts for dads
• Sibling support
• Pregnancy after loss support
• Health professionals support

There is no wrong or right way of dealing with grief, nor a typical way to commemorate a baby. A baby will always remain in the hearts of those that wanted and loved them.
Below are some ideas of how you may wish to remember your baby:




Copies of your baby’s hand and/or footprints can be put onto bracelets, necklaces, cufflinks, keyrings etc.
Planting a tree or plant that flowers and/or produces fruit, every year


Naming a star in your baby’s name
Lighting a candle
Placing a bench where you like to sit and think.
- You can add a memorial plaque too.



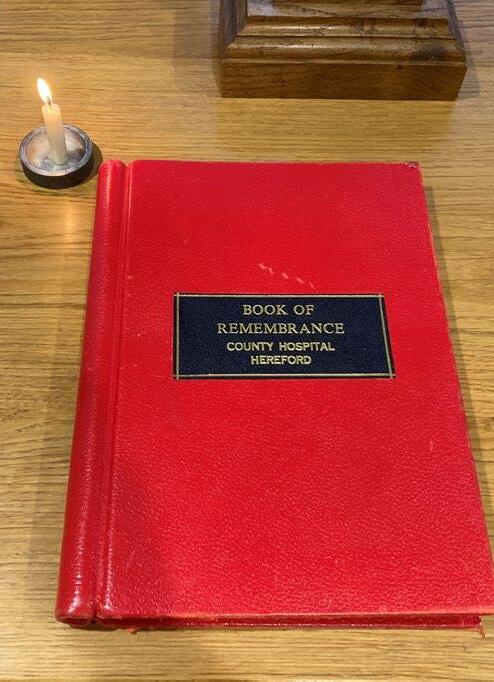
In the hospital chapel, there is a book of remembrance which lies open on the current month. If you decided to name your baby, their name will be added to the book along with their date of birth. If you decide not to name your baby, they will be entered as Baby Surname.
If you would prefer for your baby not to be entered in this book, please let your midwife or the bereavement midwife know as soon as possible.
Across the UK, every year in October is Baby Loss Awareness Week and lots of different events are held to raise awareness. For many years Hereford Hospital and the local SANDs group have also organised events during this week which usually include a Ribbon Run, lighting up the hospital in pink and blue, ribbon tying and a lantern walk concluding with a memorial service at Hereford Cathedral.
Each year slightly different events are held, if you would like to be involved please look out for posters around the hospital and information shared via social media.



The Annual Memorial Service for bereaved parents is on the

The Annual Memorial Service for bereaved parents is on the
First Tuesday evening in July at 7.30pm in the hospital Chapel
First Tuesday evening in July at 7.30pm in the hospital Chapel
Invitations are sent via the post to families that have lost a baby within the twelve months prior to the service.
Invitations are sent via the post to families that have lost a baby within the twelve months prior to the service.

This is a lovely service which involves lighting candles.
This is a lovely service which involves lighting candles.



The service is open to all, regardless of when they lost their baby
The service is open to all, regardless of when they lost their baby

Many families find that fundraising in their baby’s memory is very therapeutic and helps maintain a connection with their baby in the weeks, months and years following their loss.
We are lucky to have lots of different baby loss charities support us in Hereford, however to make sure we can provide extra resources to support our bereaved families the hospital have a dedicated charity fund called ‘The Born Sleeping Appeal’. This fund has been used to help provide families with specialised counselling, buy resources for the bereavement suite, support staff training, build a memorial garden and much more.
If you would like to support and donate to The Born Sleeping Appeal we would be very grateful.
To donate you can:



Provide cash to the bereavement midwife or reception desk at Hereford County Hospital
Transfer money to Bank Name: Barclays Bank
Account Name: Wye Valley National Health Service Trust
Sort Code: 20-39-72
Account Number: 50214299
Reference: CF30 Born Sleeping Appeal
Via the Go Fund Me page: www.justgiving.com/campaign/bornsleepingmemorialgarden
Alternatively if you would prefer to donate via our Amazon Wish list you can do so via: www.amazon.co.uk/hz/wishlist/ls/36H5Q3F431CJP

We recognise it is important that the support and care doesn’t stop after you go home. You will be offered different options of follow up options depending on your situation, which may include telephone appointments or face to face.
You should be offered a visit by the community midwife within the first few days of returning home. This is mainly to assess your physical and psychological wellbeing. We will try to get your named midwife to visit you, however this can’t always be guaranteed.
You will also be offered the opportunity to meet with your named consultant. In this appointment you will have the opportunity to discuss:
• Any questions or concerns you may have
• Reviewing your existing plan of care
• Debriefing on events and the care you received in hospital
• The results of any clinical investigations, such as blood tests, post mortem and placental histology reports
• Any further investigations, such as genetics
• Any further referrals, such as counselling, mental health support and support groups
• The reports from relevant case investigations and reviews
• If you are ready, what care in a future pregnancy might look like
Following this appointment the consultant will write a letter summarising what was discussed. If you would prefer to see a different consultant, please discuss this with the bereavement midwife.

Following your care in maternity service, we would like to offer you the opportunity to give us feedback about your experience. In order to do this a national questionnaire has been developed with the support of bereaved parents. Any feedback on your experience would be extremely valuable to us. We will use this feedback to ultimately improve the care bereavement families receive here in Hereford.
All information given will remain anonymous unless you wish to share your details when prompted. You can scan the QR Code or visit

https://forms.office.com/e/RN9kTdqbDu
At Wye Valley NHS Trust, we offer a Patient Advice Liaison Service (PALS). This is a confidential service for patients, relatives and carers to help with any questions or concerns. We aim to provide an honest and thorough procedure when reviewing concerns and complaints in order to resolve each one.
The Trust will acknowledge when things have gone wrong and will endeavour to make service improvements. It is important that you make your complaint as soon as possible after the event.
Under the NHS Complaints Procedure a complaint must be made no later than 12 months after:
• The date of the event which is subject of the complaint; or
• The date on which you realised you had something to complain about.
The above time limit will not apply if the Trust is satisfied that you have good reasons for not making the complaint within the time limit.
You can contact PALS via: 01432 372986 Pals@wvt.nhs.uk & Complaints@wvt.nhs.uk
The PALS office is located at the main reception of Hereford County Hospital and is open between 8:30am until 4:30pm Monday to Friday.

There is no ‘right’ time to have off from work. Everybody and their situation are different. It is important you talk to a few key people at work to let them know what has happened and sort paperwork on your behalf.
Dependent on the gestation that your baby was born and if they were born alive, your rights to maternity leave and financial support will be different.
We advise that for more detailed advice you look at:
Website: maternityaction.org.uk/advice/miscarriage-stillbirth-andneonatal-death-rights-to-time-off-and-pay-for-parents/
Returning to work after pregnancy and baby loss can be a time filled with fear and anxiety. Before returning we recommend you have a meeting with your manager and occupational health department to try and make this transition smoother.
Here are some tips to help prepare you for your return to work:
• Know in advance what you are going to say to colleagues. Have a few ‘banked’ answers prepared
• Ask for a phased return so as not to be overwhelmed physically and emotionally
• Have an ‘escape plan’, is there somewhere you can go if you become upset or need some time out?
• Utilise breaks fully and go outside if possible
• Do speak to employers about your feelings and allow them to support you in the way that is most helpful to you
When you come back to see your consultant if you would like, you can talk about what the future holds and what is likely to happen in another pregnancy. They can tell you what can be done to help reduce the risk of something similar happening again and how they would plan to look after you in the future. If or when you decide to try for another baby is up to you. Pregnancy following a loss can be very emotional and you will have constant reminders of previous pregnancies. However, you will be fully supported by the bereavement team, midwives, doctors and charities such as SANDs.
Whether through choice, circumstance or due to medical reasons, some families opt to adopt children or babies. First4Adoption is the national information service for people interested in adopting a child in England. They give clear and impartial information about adopting and can put you in touch with adoption agencies in your area. www.first4adoption.org.uk
First Steps is a free online resource, designed by experts, to help you understand the rewards and challenges of adoptive parenting.
The adoption information helpline is 0300 222 0022
For people living in Wales, you can search the National Adoption Service for help and support www.adoptcymru.com/contact
Please go to www.herefordshire.gov.uk and search ‘adoption’ for more details of the process involved in adopting babies and children for those living in Herefordshire and the surrounding counties. There are adoption information events throughout the year, so you can talk to the members of the adoption team and see whether this may be a suitable option for you and your family.

A baby that has been lost during pregnancy, died at birth or shortly afterwards
Miscarriage:
A baby that died before 24 weeks gestation
Stillbirth:
A baby that died after 24 weeks gestation, with no signs of independent existence following the delivery
Neonatal death:
A child born alive but dies within the first 28 days of life
Infant death:
Any death before 1 year
Perinatal Death:
Death after 24 weeks gestation (including still births) and any child born alive but dies within the first 7 days
Rainbow baby:
A baby born after an Angel baby
Sunshine baby:
A baby born before an Angel baby
Placenta: The afterbirth