BC Doctors of Optometry 121 –10551 Shellbridge Way, Richmond B.C, V6X 2W8


BC Doctors of Optometry 121 –10551 Shellbridge Way, Richmond B.C, V6X 2W8

Holiday Greetings from BCDO 3
Independence Through Interdependence 5
Earn COPE CE Credit Anywhere-Anytime ....................................................................... 7
From Basics to Biologics: Selecting Drops for Every Dry Eye Patient 8
The Scotia Profession Plan for Optometrists
............................................................... 15
Photobiomodulation: A “Photoceutical” Approach to Treating Ocular Conditions and Diseases 16
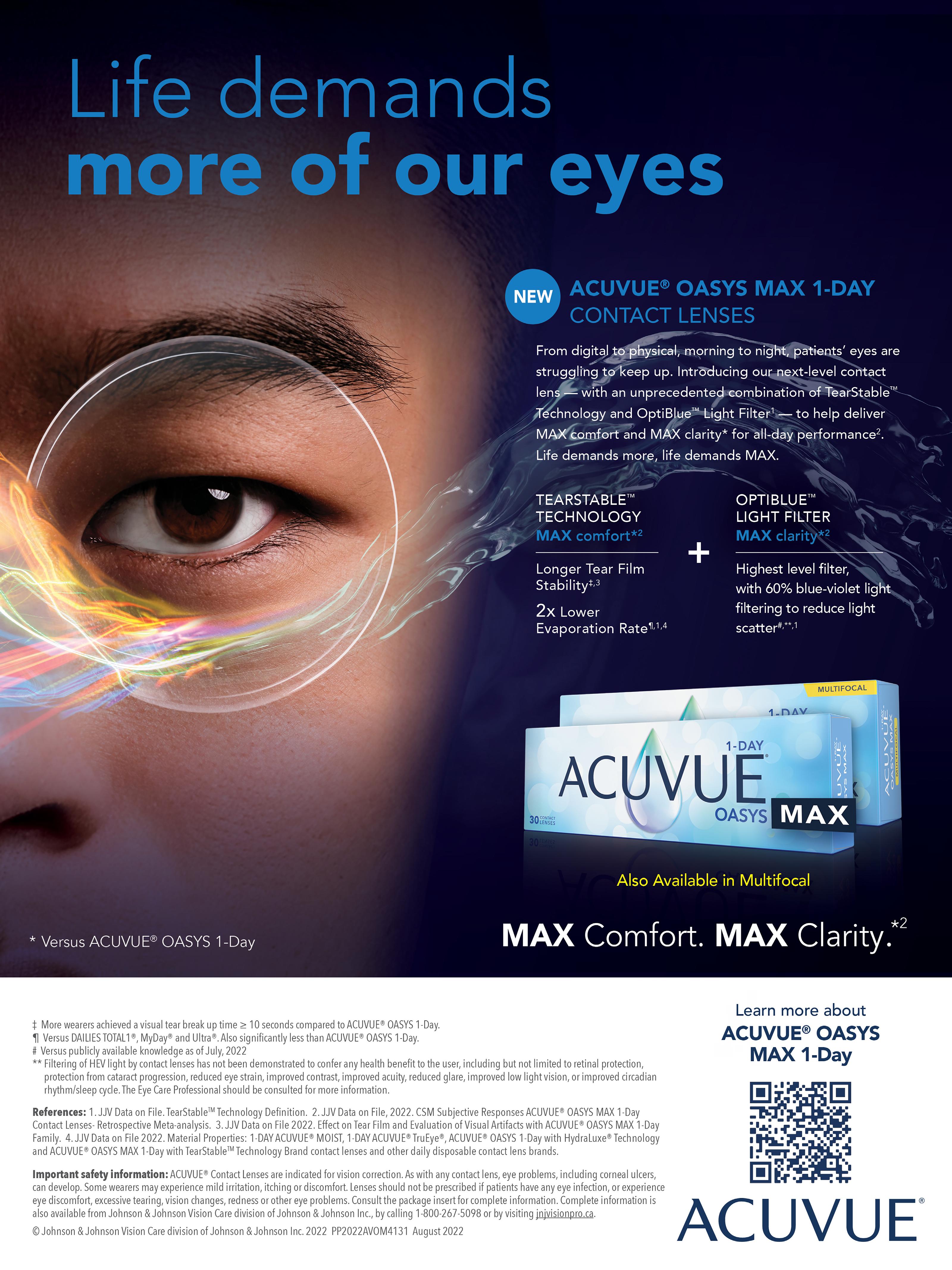
Acuvue Oasys Max ................................................................................................................. 18
BCDO PR Collateral Form 19
Trigeminal Dysphoria and Dry Eye Symptoms .......................................................... 20
Neurolens: Unlock their Lives ........................................................................................... 22
Save the Date: 2023 BCDO Annual Conference & Optofair 23
Private Member’s Bill Calls for National Eye Care Strategy .................................. 25
Acuvue: Life Demands More of Our Eyes 27
Can emulating the dental model improve how we treat OSD? 28
Online VA Tool Can Screen Post-Op Cataract Patients
.......................................... 30
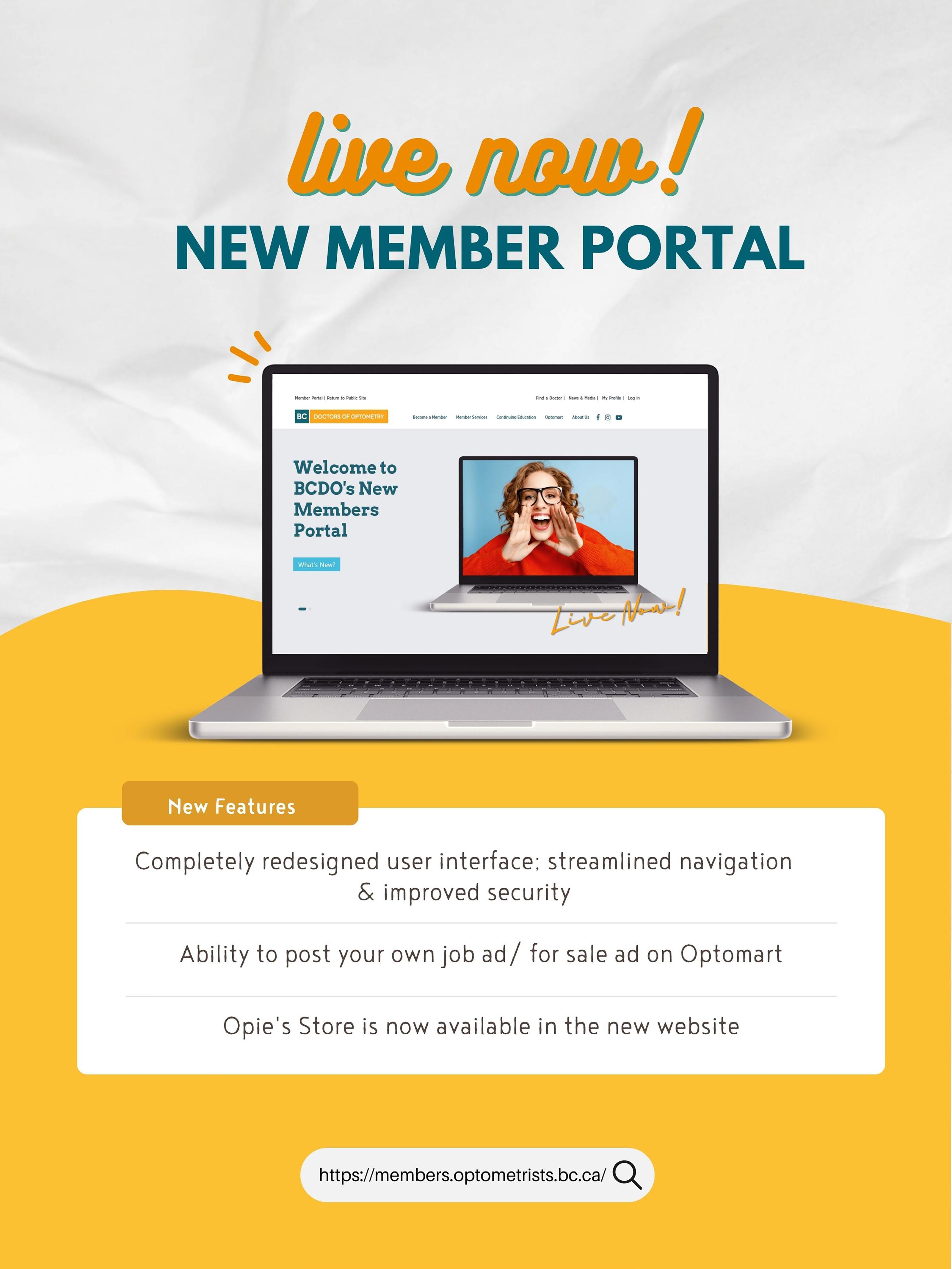
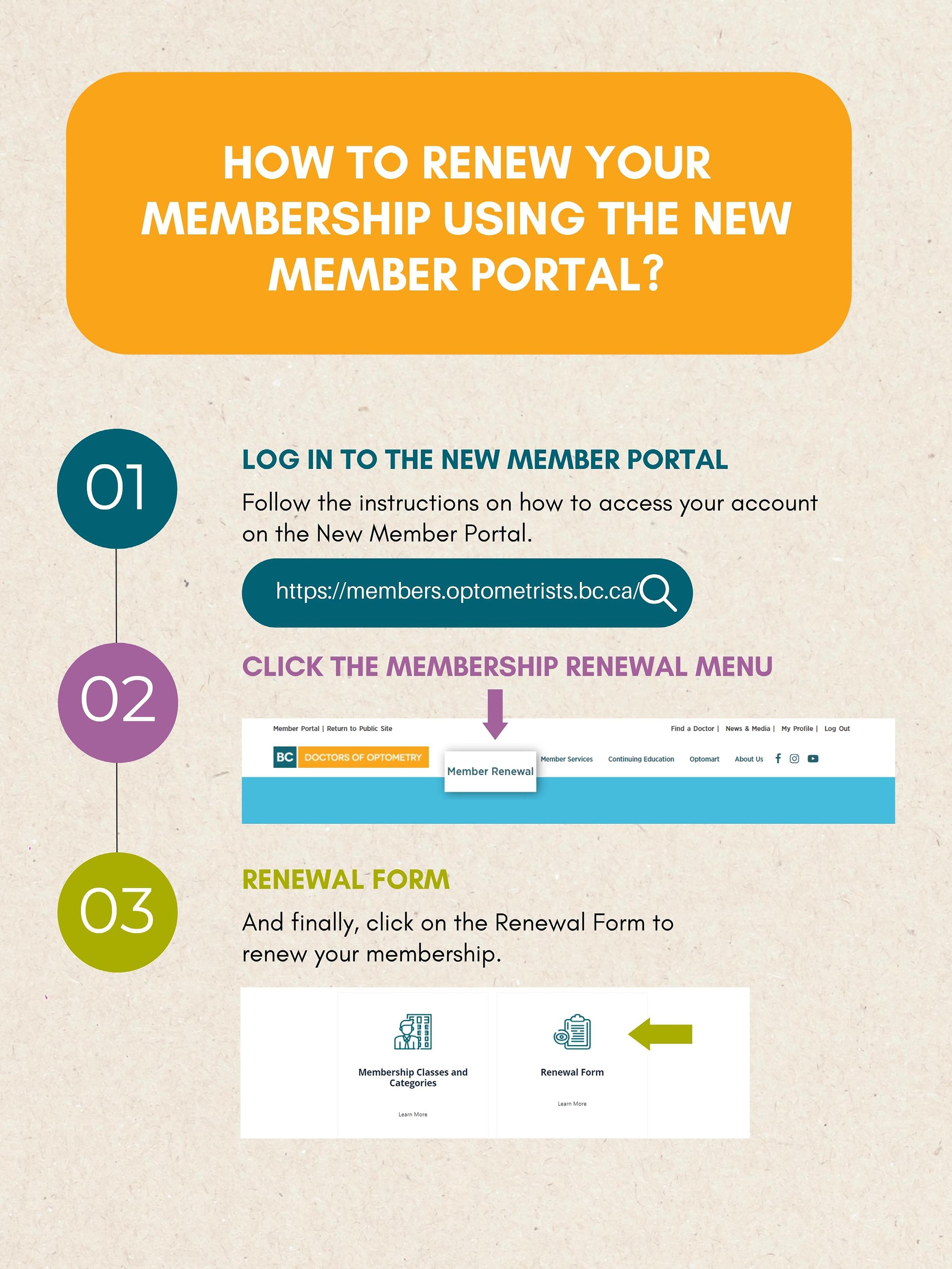
BCDO New Member Portal 32
Alcon: Total 1 ............................................................................................................................ 35
Alcon: Precision1 41
Alcon: Fitscan 56
2023 Membership Renewal & Benefits ......................................................................... 34
Why Every Practice Owner Needs a Shareholder Agreement 36
Optomart 40
Member Spotlight – Dr. Mindy Blumberg ..................................................................... 42
Alcon: Precision1 48
Alcon: New Systane Complete ......................................................................................... 49
HR Help Desk 50
Perkopolis 52
BCDO 2022 Public Education Campaign ...................................................................... 54
Are You Interested in Locum Work? Let Us Know! 58


Today’s term “Independent Optometrist” has been hijacked by almost every form of practice.

Practitioners next to Lenscrafters, inside of big box stores and practicing in solo and group practices all have seized the phrase “independent optometrist” to describe their mode of practice. I would like to think I am an independent optometrist. Free to practice how I see fit with the equipment, products, staff, fees, and culture that I feel suits my practice preferences.
What does it mean to be “independent”? What are the benefits and risks of being truly independent?
As a parent of three adult children, my goal has always been to raise independent kids. Today's world is intricate and complex, full of nuanced relationships and global challenges. Might it be a better goal to raise children that are capable of independence through interdependence? By this, I mean being stronger as an individual by learning and collaborating with others.
Can we apply the same goal to our optometric
professional careers? Learning, collaborating, and networking are basic tenets of excellence. In my career, I have learned processes and skills from those practitioners that have consistently shown excellence in their practice and personal lives. Learning is important but implementation is even more important to benefit from the learnings.
There are many ways to collaborate within the profession. Join your provincial and national professional associations. Be an active member and take on committee chair or Board positions. Join a buying/training network - I am part of Eye Recommend and have consistently gleaned practice management nuggets from my peers during an ER conference or get-togethers. Join a small business optometric group - I am part of a “mastermind” type group called Quantum where we share professional and personal challenges and collaborate with best practices and share the "group mind". I am also part of our regional "BIG" (Business Influence Group). This group discusses all matters of optometry from HR and staffing issues to tricks and tips to maximize opportunities and practice enjoyment.
Today's uber-competitive retail environment requires independent practitioners to collaborate with manufacturer suppliers. Choosing such partners requires careful consideration. Does an independent optometrist fit all contact lenses?
Does the clinic deal with multiple spectacle lens companies? Does joining a buying group reduce the cost of goods and improve choices? These questions need to be answered but the most important question is what is best for the patient?
It has always amazed me when one clinic can sell one brand of glasses and a clinic across the street feels like that frame line "doesn't sell".
Even at the same store, different opticians may have a bias towards certain products which can result in vastly different styles and designs of optical products that are sold.
Most professional sales personnel don't usually have such a wide choice of similar products to choose from. For instance, a car salesperson for Lexus has a limited product offering and must understand and highlight the features and benefits of Lexus, not Mercedes.
Limiting the product offering to excellent products and allowing very occasional “off menu” choices in exceptional circumstances can improve staff product knowledge, increase supplier investment in your clinic and reduce costs in shipping and reduce costs of goods.
Choose your contact lens, spectacle lens and frame manufacturers carefully. Which companies support your independent practice ideals? Do these companies compete with your clinic at a retail level? Do they have products available online at a retail level? Do they help keep repeat orders through your independent OD channels?
The interdependence of suppliers and independent optometrists relies on careful consideration on choosing your supplier partners. Every purchase you make from a supplier is a proxy for your future success.
I recommend picking two suppliers in each category and deepening your partnerships. This existential dilemma will only increase as manufacturers continue to supply optometrists on the wholesale side while attempting to compete for our patients on the retail side.
Might the future survival of truly independent practices rely on cross-equity partnerships where independent clinics own pieces of other independent clinics? Might this joint ownership model allow for better pricing through a master account so independents can compete on a level playing field with corporate accounts to lower product acquisition costs?
I am a big believer in the future of independent optometry. Independents can truly keep the patient's best interests at the top of the pyramid while curating partnerships with industry and partnerships with other like-minded clinics. Independence through interdependence!

Mahnia Madan, OD, FAAO

President BC Doctors of Optometry www.vancouvereyedr.ca
Financial disclosure: Labtician Thea, Lumenis, Sun Pharma, Santen, MYE Drop
Mark Eltis, OD, FAAO, Dipl. ABO Toronto, ON www.drmarkeltis.com
Financial disclosure: Labtician Thea, Sun Pharma, Volk, Heine, Cooper Vision, Zocular, Aequus Pharma
Article republished from Review of Optometry https://www.reviewofcontactlenses.com/article/from-basics-to-biologics-selecting-drops-for-every-dry-eye-patient

Addressing meibomian gland dysfunction, and blepharitis in general, is the key to suppressing the inflammatory nature of dry eye disease (DED). However, artificial tears (ATs) still play a pivotal role in managing the condition. They are particularly effective at providing symptomatic relief to patients, especially during flare-ups. Advise DED patients to use tears regularly “like a lip balm” and not wait until their ocular surface is compromised and symptomatic. DED can’t easily be categorized in a binary classification of evaporative or aqueous deficient: TFOS DEWS II found up to 70% of suffer-
ers have a mix of the two. Aside from symptomatic relief, artificial tears can reduce inflammation and help prevent epithelial cell death. When chosen carefully, eye drops can play a significant role in the management of dryness.
The amount of eye drops available can make selection overwhelming for a doctor (let alone a patient). Let’s explore some favorites and clarify when they are most appropriate. We will also simplify when it makes sense to turn to biological drops in the management of DED.
Dropping In
Preservatives in multi-dose bottles are considered a necessary evil to contain bacterial replication and minimize contamination risk. However, they are counterproductive: an irritant is being introduced to an already compromised tear film and ocular surface. Preservative-free formulations are always superior but should be highly recommended for those using drops more than four times a day. Benzalkonium chloride and thimerosal formulations should be avoided at all costs.
Tear osmolarity can be used as a guideline for selecting AT viscosity. Moderate to severe DED often necessitates a thicker drop. Generally speaking, as viscosity increases the duration of effect of the drop increases—but so does the potential for blurred vision.


A relatively inexpensive and effective option for mild to moderate DED is Systane Ultra Hydration (Alcon). It’s a moderately viscous drop that contains hyaluronate. Another ingredient, hydroxypropyl-guar (HP-Guar), interacts with the blinking motion to prolong on-eye contact time. HP-guar molecules bind preferentially to dried or compromised hydrophobic areas of the cornea, containing further damage while epithelial cells regenerate. It forms a gel layer (acting as a mucomimetic), compensating for a compromised tear layer and reducing friction during blinks.1
Systane Ultra also comes in a single dose non-preserved option, which is substantially more

expensive but highly recommended if using drops more than four times a day.
A top-shelf multi-dose preservative-free option for more advanced dry eye is Hylo Dual Intense (Candorvison). It combines ectoine (a natural anti-allergy and anti-inflammatory agent) with a higher viscosity level (produced by a high concentration of heavier molecular weight sodium hyaluronate) that does not blur vision. Ectoine has been found effective in DED and allergic conjunctivitis. It has even been shown to accelerate wound healing post-op.2 The unique multi-dose pump does not allow air to penetrate the interior, keeping it safe for its six-month lifespan (once opened). When compared head-to-head with single-dose non-preserved options, this product’s cost becomes more defensible.
Thealoz Duo Gel (Labtician-Thea), a single unit preservative-free thicker gel, is an excellent bedtime option. It does not blur vision and is not oily. Trehalose (also found in Refresh Optive Mega 3) is an osmoprotectant designed to guard dried epithelial cells and stabilize their membranes. Simply put, trehalose protects against the destructive inflammatory cascade of DED. Sodium hyaluronate (as a glycosaminoglycan) enhances viscosity. Carbomer (a water-soluble polymeric resin) increases viscosity and maintains the hyaluronic acid and trehalose together in contact with the ocular surface for six hours without being sticky.3-5 The single-unit dose does make it a more expensive option among the nighttime alternatives.
A unique product for MGD is preservative-free Calmo spray (CandorVision). It is used with the eyes closed, which allows it to seep into the eye slowly, replicating meibomian gland secretions. It’s also an excellent option for people who hate putting drops into their eyes. The product contains liposomes to replicate the oil-deficient layer in MGD sufferers and dexpanthenol (pro-vitamin B5), which moisturizes the eye and surrounding
skin.
Optase Hylo Night (Scope Health) is a nighttime ointment that uses vitamin A to speed up epithelial healing.6 It is preservative-free and good for mild to moderate dry eye. It is also phosphate free and good for six months once opened.
Refresh Lacri-Lube ointment (Allergan) is the go-to for very thick overnight coverage. It uses mineral oil as an ointment base that allows melting at body temperature and white petroleum as a lubricant.7 If inserting the ointment in both eyes, patients need to be warned that it will blur them out for a sustained period. Ideally, they should already be in bed when inserting it, for safety.
The Liposic (Bausch + Lomb) line has been a reasonably priced option for decades. While MGD patients don’t always respond to oil replenishment drops, this particular product has endured in both drop and ointment form (for nighttime use). The drops contain carbomer, sorbitol, medium-chain triglycerides and cetrimide preservative. Liposic gel has sodium hydroxide, which closely mirrors tear pH, and attempts to replicate all three tear layers.
Refresh Optive Mega-3 (Allergan) is a single-dose preservative-free drop. As the name suggests, it contains omega-3 from flaxseed oil. Studies show that eye drops using emollients can increase lipid layer thickness for a short duration.8 Omega-3 fatty acids are actually found in the normal tear film. Refresh Optive Mega-3 is formulated to minimize blur and does not require shaking. It is designed to replenish all three tear layers and is targeted towards MGD patients (like Systane complete and Retaine). Its lubricants include glycerin 1%, carboxymethylcellulose sodium 0.5% and polysorbate 80 (0.5%). These drops may be most helpful for patients with prolonged screen time, a lifestyle that decreases blinking and meibum secretion.8
There are many other excellent products on the market for DED. While there is no magic formula or perfect drop for every patient, a careful case history and an understanding (by both doctor and patient) that there will be some trial and error in finding the right products is key.
Another benefit of punctal occlusion: it can increase the effectiveness of other medications used in the dry eye treatment, as it allows the drug to stay on the ocular surface longer. In one study, punctal plugs used with the cyclosporine group had longer symptom relief than either group treated separately.11
Before reaching for punctal plugs, though, manage ocular inflammation first with other methods. Punctal plugs are contraindicated when there are signs of active infection or allergies present (Figures 1a and 1b). Plugs are also not ideal in patients with blepharitis or meibomianitis, as they need management of their lid disease first.
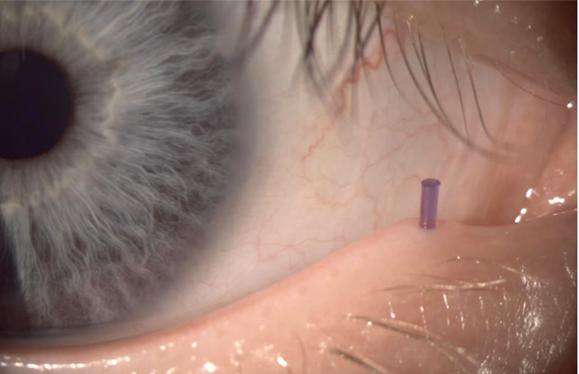
Options range from dissolvable collagen inserts to more permanent silicone-type plugs. Temporary plugs can be used diagnostically to see if patients will benefit from longer plug use. Collagen plugs have a design advantage, too, as they lack the cap that is found in silicon plugs and can sometimes be irritating for patients (Figure 2).
Fig. 2. Placing punctal plug in a lagophthalmos patient to increase tear volume.

Punctal occlusion to preserve tear volume was a more popular option when we thought DED was effectively an absence of tears. We now know inflammation is the root cause. Recent years have seen a reduction in punctal occlusion—the thought is that occlusion keeps inflammatory mediators in the eye.9 However, the procedure should not be dismissed outright. It is still a key player in patients who have neurotrophic components, aqueous-deficient dry eye or non-resolving persistent epithelial defects (as in lagophthalmos patients). Increasing the tear volume can be extremely beneficial in these patients.10
Typically, plugs are placed in the lower puncta; however, all four can be plugged if needed. Punctal plugs may not have a significant impact when used alone in the treatment algorithm, but when combined with other treatment modalities, patients are likely to benefit. Current manufacturers include: Odyssey, Katena, Lacrimedics and others.
In the not so far future, we will be seeing punctal plug-based drug delivery systems for glaucoma, allergies and even dry eye. These will address compliance issues and are more convenient for patients. They also have the potential to reduce ocular surface and systemic side effects of drugs.
For more severe dry eye sufferers, artificial lubricating drops are simply not enough. TFOS DEWS II reported that our natural tear film is a complex structure containing over 1,800 molecules that
work together to not only form the most perfect lubricant, but the tear film also protects and nourishes the ocular surface. Our natural tears are epitheliotropic, which means they can support the proliferation, migration and differentiation of corneal and conjunctival cells.12 This is not something over-the-counter lubricating drops have been able to replicate.
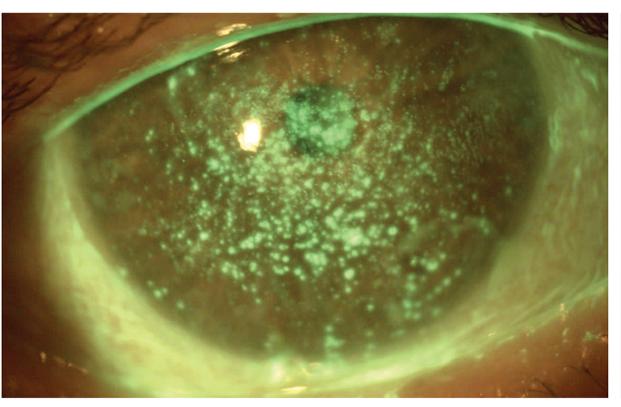
When patients present with moderate to severe dry eyes with significant punctate keratitis, we can turn to blood biologics to help rescue and rehabilitate the ocular surface. The two common options are autologous serum eye drops (ASED) and platelet-rich plasma (PRP) eye drops.
Both have been successfully used in the treatment of moderate to severe DED; however, research suggests that PRP is superior in restoring the ocular surface.13 This is because PRP contains platelets, which are considered the powerhouses

for healing. Platelets are the first cells to arrive at the wound site; they adhere to damaged tissue and initiate a healing reaction that includes the release of a variety of cytokines and growth factors. Similar to the natural tear film, growth factors released by platelets have epitheliotropic properties and are responsible for cell growth, collagen production, cell adhesion and healing of corneal and conjunctival cells, thus improving signs and symptoms of DED.13,14
Platelets are eliminated in the production of ASED, decreasing its potency. ASEDs are often diluted before dispensing, which further reduces the growth factors (Figure 3).
Both ASED and PRP drops are particularly helpful in recalcitrant dry eye (e.g., neuropathic and neurotrophic). PRP can help increase corneal nerve density lost in chronic DED.15 It is beneficial in multiple conditions, including recurrent corneal erosions, persistent epithelial defects, post-LASIK dry eye and Sjögren’s syndrome (Figure 4).13,14
Contraindications to ASED and PRP drops are few but barriers to availability are many. Both require regular blood draw and processing of blood, which may not be feasible for everyone. Typical blood draw yields a three-month supply of ASED or PRP eye drops, which are often used four to six times per day. They also require refrigeration. Once improvement in ocular surface disease is noted, frequency can be tapered and patients can be maintained on other therapies.
Optometrists can produce blood biologics in their practice (subject to state law) or work with local compounding pharmacies. Vital Tears (vitaltears. org) is another option for ODs looking to access ASED.
If drawing the patient’s blood is not an option, practitioners can also consider biological eye drops derived from donor human amniotic fluid
Fig. 4. Resolution of persistent epithelial defects with PRP and lid hygiene for three months. Click image to enlarge.
or placenta. These are indicated for mild to severe DED and can be a good option for patients looking for lubricants from natural sources. One study found that topical application of amniotic membrane extract eye drops reduced pain and inflammation and promoted re-epithelialization in ocular chemical burns.16
Options here include StimulEyes (M2 Biologics) and Regener-Eyes (Regener-Eyes) eye drops. Both are preservative-free and contain cytokines, chemokines and growth factors to aid ocular surface healing.17
When neurotrophic keratitis (NK) is suspected, cenegermin eye drops may also be used. Cenegermin is a recombinant nerve growth factor (rhNGF), produced in Escherichia coli, can promote corneal healing in a neurotrophic

cornea.18,19 Oxervate (cenegermin-bkbj 0.002%, Dompé) is a sterile, preservative-free eye drop. It is aouvailable in seven multi-dose vials (1.0mL) intended to be used six times a day for eight weeks.
NGFs are known to regulate sensitivity in a normal cornea, which is important for epithelial healing. When persistent corneal staining or non healing epithelial defects are present and corneal sensitivity is reduced, neurotrophic keratitis should be suspected. Although rare, when it does occur NK is challenging to manage, as patients can develop non-healing corneal ulcers and even perforation due to the cornea’s inability to heal.20
In the current clinical studies, significant improvement in corneal healing was noted in the cengermin treatment group vs. the placebo group.21,22 However, whether there is improvement in corneal sensitivity in patients of the treatment groups is still debatable.18 Interestingly, use of bandage contact lenses along with cenergemin drops improved corneal sensation in 79% of the eyes in a recent retrospective study.23 Most common side effects of this therapy include hyperemia and eye pain, and it’s important to note that patients can relapse when drops are discontinued, suggesting the need for ongoing treatment and additional therapies.18
Just like with artificial tears, biologics and advanced alternatives are not a silver bullet. Every patient is best served through an individualized treatment plan that matches their experience in the DED spectrum. As eyecare providers, we must be well-informed on all options available to make that proper connection between a patient condition and appropriate care.
View Foonotes

The utilization of light to heal goes back thousands of years but is now evolving into a significant treatment modality with applications for a host of eye conditions. Photobiomodulation (PBM), also known as low-level light therapy (LLLT), is an emerging treatment modality with immense benefits for patients and eye care professionals.
Photobiomodulation is the application of low power Red to Near Infrared light to “recharge” aging and diseased mitochondria to restore cell function. Mitochondria are the primary source of Adenosine 5’-triphosphate, or ATP which is the principal molecule for storing and transferring energy in cells. Aging and disease reduce ATP production and increase Reactive Oxygen Species (ROS), which drives oxidative stress, inflammation, and cell loss.
Extensive research in both the scientific and clinical communities has shown immense benefits to this form of treatment without any concerning side effects associated with traditional pharmaceutical or surgical interventions. With more energy available, new cells can do their work more efficiently such as repairing skin, boosting new cell growth, and enhancing blood flow.
Our team, composed of Physicians, Ophthalmologists and Optometrists, has been at the forefront of clinical research and evaluation of PBM as it relates to eye conditions for the last ten years. Our primary focus has been the use of PBM on dry age-related macular degeneration, a significant burden to patients and society and an enormous and costly unmet need.
Evaluation of PBM in dry AMD started with small IRB open pilot studies and evolved due to the success of these trials to multi-centred, worldwide sham-controlled clinical trials. Results have been very positive, and this safe, non-invasive treatment has shown improvements in visual outcomes
and reduction of disease immediately following a short three-week course of treatments, with benefits generally lasting more than six months.
With this in mind we have developed a truly innovative, wearable, red (670nm) LED home use device called Arunalight. Arunalight closely resembles predicate devices that have been proven in clinical trials and treatments and would be readily available to patients at an affordable price, to use as needed in the comfort of their own homes. We anticipate the Arunalight will be available for purchase in 2023 and enable the greatest number of patients to benefit from PBM therapy for dry AMD.
Not only could PBM significantly impact outcomes for dry AMD patients but is also being investigated as an adjunct to anti-VEGF injections for wet AMD. Anti-VEGF injections are good at reducing subretinal fluid, however visual acuity still declines in these patients over time. PBM may improve functional outcomes by maintaining any initial VA improvement and reducing the frequency of injections.
We believe Arunalight will not only provide an impactful treatment option for dry AMD but that its scope of use will expand as researchers look for opportunities to utilize PBM for other eye diseases and conditions including diabetic retinopathy, amblyopia, glaucoma, Leber’s hereditary optic neuropathy, retinopathy of prematurity, retinitis pigmentosa, amblyopia, dry eye disease, and progressive myopia.
For more information, please contact Bright Optical at 877-870-0105 or sales@brightoptical.com



I am very excited about the prospect of helping patients see and feel better! When I can help a patient with a long-standing issue whose cause has not been previously identified, it is especially satisfying. Let’s face it, there is a lot of “new technology” to wade through these days. What will really make a difference to the lives of our patients? What will be a technology that can be seamlessly integrated into our clinical workflow and give measurable results that create raving fans out of our patients. Drumroll please…. Neurolens!
We have a bustling full-scope practice that includes all the latest dry eye treatment technologies: Lipiflow, Radio Frequency, IPL and Photobiomodulation included. What really amazed and delighted me was when we added Neurolens testing our Dry Eye patient protocols.
Testing on the Neurolens Measurement Device (NMD) takes less than two minutes and provides accurate and repeatable phoria and fixation disparity measurements at near and far. The test recommends a Neurolens value when indicated, which is the amount of prism required to properly align and fuse the images to improve binocular dysfunction. The Neurolens value is used
to prescribe Neurolenses, which incorporate a “contoured” prism that allows for better binocularity at distance as well as near focus. The result is a decrease in symptoms related to a proprioceptive conflict between misaligned eyes and the trigeminal nerve—sometimes referred to as “Trigeminal Dysphoria”. The interesting part for our Dry Eye clinic is that Trigeminal Dysphoria can manifest symptoms very similar to dry eye disease such as dry eyes, headache, neck pain and fatigue.
Some of our patients that were suffering from “Dry Eye” type symptoms were completely relieved when fit with Neurolenses. Be aware of those pain with no stain patients and ensure you get a Neurolens test to rule out Trigeminal Dysphoria. In our primary care clinic Neurolens has started to evolve from a problem solver for patients not adapting to traditional progressive lenses to a problem predictor. We have started using the Lifestyle Questionnaire recommended by Neurolens to screen for patients with potential Trigeminal Dysphoria before they come in for their routine examination. We continue to screen all primary eye care patients for Dry Eye disease using a DEQ5 survey as well as lower lid screening meibography.
We have had patients describe their lenses as “magic glasses” and others become emotional because no other Optometrist could figure out their eye issues. These are lenses that cannot be purchased just anywhere or online. Neurolens allows our clinicians to provide amazing care while increasing the likelihood of future purchases through our offices and a “patient for life” mentality.

The cherry on top for me is that Neurolens is so confident that patients will appreciate the
product that they guarantee patient satisfaction. This aligns with our clinic philosophy that we guarantee satisfaction. While most companies believe they have good products not all companies will stand behind the office and the patient until they are happy. If you are interested in learning more about Neurolens and how it can fit into your clinic, reach out to your BC representative, Kristina Smith, at kristina.smith@neurolens.com



On June 14th in the House of Commons, Hon. Judy Sgro, MP for Humber River-Black Creek, introduced Bill C-284 to establish a National Eye Care Strategy.
Fighting Blindness Canada (FBC) applauds this step. For years, FBC in partnership with other vision organizations including Canadian Council of the Blind, CNIB, Vision Loss Rehabilitation Canada, Diabetes Canada, Canadian Association of Optometrists and Canadian Ophthalmological Society have advocated for a National Eye Care Strategy. This strategy is necessary to focus energy and resources on eye health and the impact that vision loss has for health and well-being.
When introducing the Bill, Mrs. Sgro said “Mr. Speaker, I am very happy today to have the opportunity to introduce this bill calling for a national strategy on eye care, something that, for many years, Canadians have been calling for, and something that the government has promised many times before that.
I want to acknowledge that I am introducing this Bill in memory of my grandmother, Annie Steeves, and I continue to see my aunt Ruby Gentile and my long-time friend and mentor Paul Valenti, who suffer from blindness.”
Mrs. Sgro cited the over eight million Canadians living with a blinding eye disease as why the House needs to pass this Bill. “I ask all of my colleagues to just imagine how their lives would change if they lost their eyesight. We take it for granted, and we do not stop to think enough. Over eight million people currently live with a blinding eye disease that puts them at risk, and these numbers are expected to grow to almost 14 million people.”
“Many of us currently in the House may also develop macular degeneration, and I would like to see February designated as macular degeneration awareness month.” Mrs. Srgo continued.
“The Canadian Council of the Blind, Fighting Blindness Canada, CNIB and countless other organizations have been calling for an eye strategy for Canada, to move forward with the commitment made previously to develop a national eye strategy that will protect the eye health of all Canadians.”
The Bill’s first reading motion was adopted and the Bill will now move to a second reading. FBC urges you to send a letter to your Member of Parliament to encourage them to support the Bill.
Learn more and send a prewritten letter at eyecarestrategy.ca.



Article republished from Review of Optometry https://www.reviewofoptometry.com/article/a-different-approach
There are many similarities between eye care and dentistry. Why am I bringing up dentistry in an optometry magazine? Preventing ocular surface disease (OSD) is imperative to keeping our patients’ eyes healthy, just as preventing gum disease is imperative to keeping mouths healthy. Does this mean a preventative model for OSD is possible?
Beginning with diagnostics, dentists use mirrors and magnifiers to closely observe the mouth, but especially the gingiva or gums. Likewise, we need to spend more time not just observing the cornea

and internal eye, but truly scrutinizing the eyelids.
Dentists use X-rays, and we can use imaging ranging from meibography (LipiScan, Oculus) to slit lamp cameras (Haag-Streit BQ900) to advanced diagnostics such as tear film imaging (AdOM) and dry eye analysis (Oculus). Dentists have teeth whitening options and ODs can consider eye whiteners that don’t constrict arteries, like Lumify (Bausch + Lomb). Finally, dental patients with morning symptoms typically have bruxism (teeth grinding) and eyecare patients with morning symptoms have inadequate lid closure.
To effectively manage OSD, shift your focus from the ocular surface to the eyelid. The reason is that 86% of dry eye disease (DED) involves meibomian gland dysfunction (MGD).1 Some clinical signs to observe include a frothy tear film, a sheen on the lids indicative of biofilm, collarettes or a volcano sign where debris is present at the base of the lashes indicating Demodex or staphylococcal blepharitis. Capped glands, posteriorly placed meibomian glands and thickened or scalloped eyelid margins are all key signs.
Next, have the patient look down, increase magnification and scan the upper eyelid margin. Finally, express the meibomian glands. Not doing this is akin to saying you want to manage glaucoma but don’t want to observe the optic nerve or manage macular degeneration without looking at the macula.
In the world of dentistry, the term for biofilm is plaque. Dentists or hygienists spend the majority of their time removing biofilm because it leads to diseases like gingivitis and eventually loss of teeth. We should do the same by focusing on microblepharoexfoliation (BlephEx) and debridement (Bruder), which may prevent meibomian gland loss or atrophy. Dentists recommend patients continue to work on preventing plaque through brushing and flossing, and we can recommend lid scrubs from (Ocusoft) and Bruder mask hydrating compresses.
Dental patients who have morning symptoms are often diagnosed with bruxism, and the solution is an overnight bite guard. In eye care, patients with morning symptoms almost always have inadequate lid seal issues, and the treatment involves overnight lid seals (SleepTite).
An area where optometrists and dentists diverge
is in disease prevention. Dentists treat plaque every six months to prevent loss of tissue and teeth. Perhaps we should consider this to prevent meibomian gland atrophy and chronic DED. While it might be a stretch for us to treat patients without signs or symptoms, start treatment when signs are first evident, including MGD-based on expression or froth in the tear film, blepharitis or biofilm, with signs including a sheen, collarettes or debris on the lashes, or inadequate lid closure.
The second thing we can learn from dentistry is to preappoint patients. Dentist offices know how essential it is to reschedule a patient every six months. In our case, we need to make the decision based on the level of disease, such as DED vs. MGD, but it’s important to schedule that patient for a follow-up exam so we can avoid the progression of OSD.
It’s important to take all of the steps necessary to prevent ocular surface disease or at least manage it properly, even if it means taking a different approach and shifting your focus. So, maybe it is possible to follow this model and have not just happy patients, but happy optometrists!
1. Lemp MA, Crews LA, Bron AJ et al. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: A retrospective study. Cornea. 2012;31(5):472-8. 1.
 By Staff
By Staff
Article republished from Review of Optometry https://www.reviewofoptometry.com/news/article/online-va-tool-can-screen-postop-cataract-patients
The efficiency of postoperative cataract care could be enhanced with remote services using teleconsultation and online/remote measurements. However, these encounters are only partly applicable in eye care since they lack objective outcome parameters for visual acuity (VA) and refractive state. The increased use of digital tools in general supports the implementation of electronic health solutions.
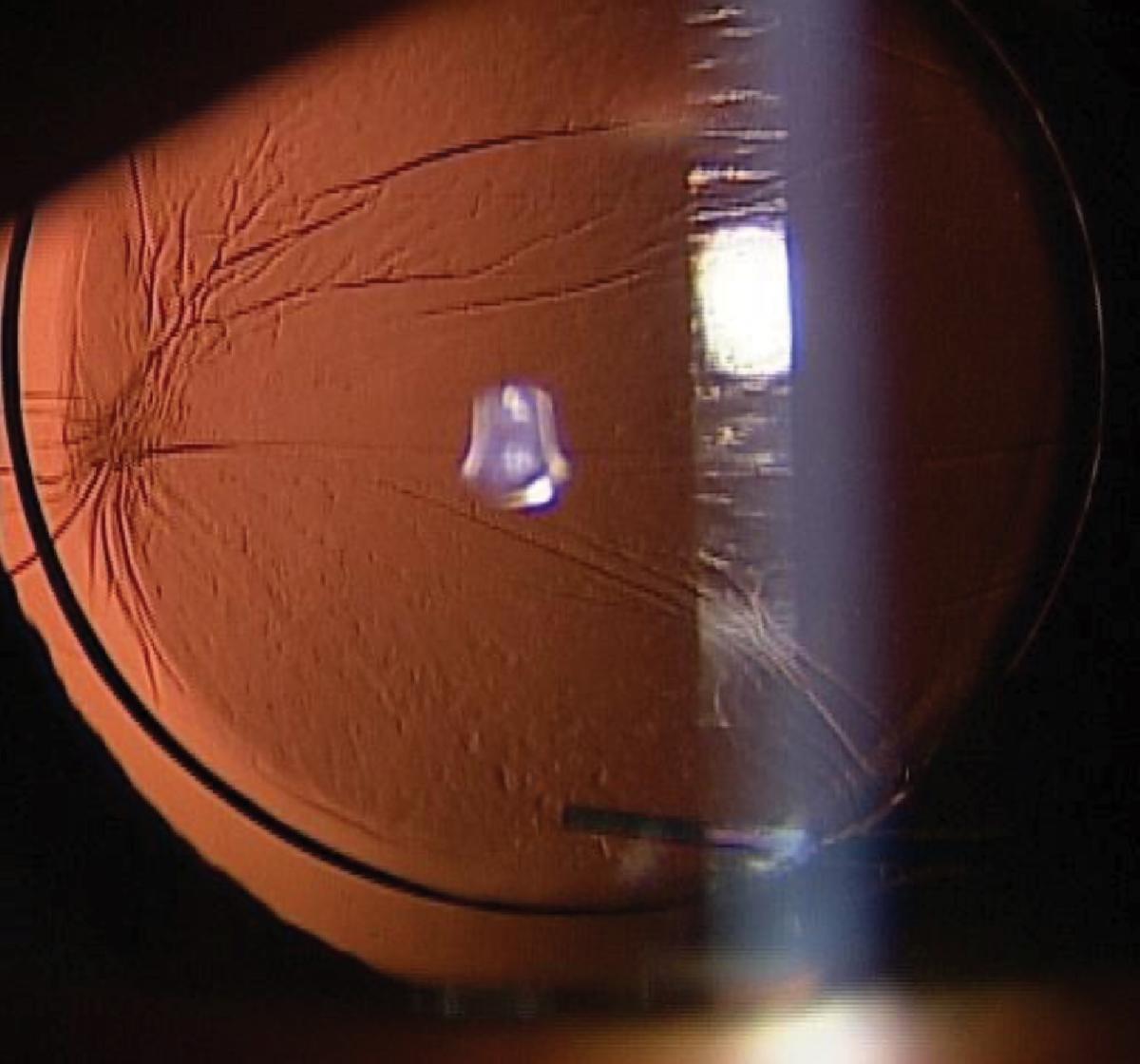
that could not characterize the nature of the implant’s status in a way comparable to slit-lamp exam. Photo: Alia Cappellani, OD.
An upcoming online health application is the Easee web-based tool, which allows patients to individually assess their VA and corresponding refraction using a smartphone and computer screen. A recent study validated the tool for VA assessment of patients who underwent cataract surgery and assessed the agreement between the measurements carried out by the tool as compared with conventional assessment. The researchers noted that the tool showed different outcomes compared with conventional ETDRS and Snellen charts for both uncorrected (UDVA) and corrected distance VA (CDVA), but the vast majority of these differences were within the established clinically acceptable limit of ±0.15logMAR.
A web-based tool showed promise in acuity testing after cataract surgery, but would only provide crude assessment of visual status
The study included 75 operated eyes of 46 participants between the ages of 18 and 69. The difference in UDVA between the web-based tool and ETDRS or Snellen charts was -0.05logMAR and -0.04logMAR, respectively. For the CDVA, these differences were -0.04logMAR and -0.07logMAR, respectively. The correlations between the web-based tool and ETDRS or Snellen acuity were statistically strong. However, the research-
Day 1 acuity testing was done digitally, with encouraging results. Researchers stress that the method is not sensitive enough to replace in-clinic ophthalmic care.
emphasized that this correlation cannot be defined as agreement, as it only measures association.
In total, 73% to 88% of the VA measurement differences were within 0.15logMAR. Also, questionnaire outcomes showed that the majority of participants had a positive attitude toward the tool. Still, the team highlighted that patients need to have basic digital skills to perform web-based VA assessment.
“These results are sufficient to introduce the web-based tool as a reliable screening method for detecting significant deterioration or lack of improvement of VA in post-cataract patients,” the researchers wrote in their paper. “It should be
noted that remote VA testing will not completely replace ophthalmologic examination at the outpatient clinic but can enhance the efficiency of cataract care.”
Using these applications could lower the burden on patients after cataract surgery by saving follow-up visits at the outpatient clinic, which may improve efficiency and lower costs.

Wanten JC, Bauer NJC, Claessens JLJ, et al. Evaluation of a visual acuity eHealth tool in cataract patients. J Cataract Refract Surg. December 6, 2022. [Epub ahead of print].



As you become a seasoned Optometrist, you may want to open your own practice. Considering this can be an expensive venture, you may bring on a partner, or another Optometrist or an investor. Picture this: you both agree on a vision for the business and it’s “ off to the races”. Life is great, business grows, no negative outcomes over the years, and you reach retirement and decide to sell the business shares, you're at a great price with no dispute and live happily off the profits forever. While reading this dream scenario you may have chuckled to yourself. Why? Because you know that this outcome is highly unrealistic. No business venture or partnership comes without some troubleshooting, concerns or even turmoil at times. So how do you manage the inevitable ups and downs during the life of your business between partners?
The answer is simple… a shareholder agreement.
This is a document between all shareholders of a business and will protect against situations that could have potentially damaging financial impacts. A shareholder agreement would clearly stipulate how the business should handle a variety of potential scenarios. These include: a shareholder’s death, extended disability, retirement, bankruptcy, divorce, a partnership conflict, amongst other things. shareholder agreements provide a smooth transfer of business during unforeseen situations, and create liquidity from an illiquid asset such as shares of a private company.
TIP: Don’t wait, get a shareholder agreement put into place as early as possible before these circumstances occur, when all parties are getting along and positivity is high, otherwise it may be difficult to find common ground.

It’s important to look into drafting this agreement with your lawyer. Similar to drafting up a will, there is a fact-finding process that follows. Once an agreement has been drafted to include all of the situations that would be actioned under the agreement, it’s time for all shareholders to review it. It’s extremely important that all parties sign this agreement or else it is not binding. the importance of taking this to the finish line by signing it cannot be emphasized enough, do not let that slip through the cracks of time.
The last step is to include a way to fund the contract, otherwise, it is worthless. Your lawyer will usually have this worded into the agreement
discussing how the shareholders will be paid for their shares. This is where a financial planner, such as Portfolio Planning, would step in and figure out the most effective way to fund this policy.
The most common methods of funding a policy are:
• Using cash from a business account or personal
• Borrowing funds such as a line of credit
• Using insurance that is generally purchased by the business.
At Portfolio Planning, we help our clients answer key questions about funding an agreement by looking at:
• What the price of shares would be
• What is the timing before the agreement will be executed
• What the tax treatment on such a payout would be
Portfolio Planning has helped business owners put this complex process in place by maximizing their corporate CDA account and keeping opportunity cost in mind for a growing business. Let’s run through some scenarios…
You graduated with a friend who is a respected Optometrist. Together you decide to purchase a turnkey practice from a retiring colleague. You had intentions of following the above steps but got sidetracked and never got around to it. Seven years later, you both are married, have families and have a successful practice with multiple locations. Unfortunately, your business partner passes away in a car accident while driving to work and leaves behind a husband and two kids. Without an agreement in place the deceased partner's spouse has now received his wife’s shares. Now your business continues to pay a salary to the spouse while you carry the load of a large practice all by yourself. Some of the holders of your business's debts are concerned by the death of the shareholder and the impacts this could have on your practice so they recall some of the outstanding loans, leaving you with little cash flow and needing to continue the business. You decide you need to sell some of the shares to a new partner to help, however the ex-partners spouse doesn’t accept the suggested share price. Now you are stuck in a struggling business.
On the flip side, if you had a signed and funded shareholder agreement in place, you could have had a clause that states that in the event of a death, the corporation would purchase the shares of the deceased shareholder at a previously agreed-upon price using a life insurance policy. Your partner's spouse would receive a lump sum equal to the price of their shares, the business would acquire the shares, and you can purchase the shares from the corporation using a payment schedule over multiple years. Now you hold 100% shares of the
business and your partner's family is taken care of. You maintain all control over your business, no relationships are strained, and all debt holders, suppliers, employees, and key customers remain reassured of the future success of the business.
Shareholder agreements are key.
If you have questions regarding your current business strategy, please reach out to a financial planner and your lawyer to review.
Portfolio Planning is a team of net worth advisors, seasoned financial planners and consultants, who work closely with medical professionals and incorporated business owners. Our firm is boutique size and independent, which allows us to serve our clients better and quicker. Our team has helped many of your colleagues navigate questions around shareholder agreements and more. If you’re feeling that you want more for yourself financially, book a complimentary discovery call with one of our financial planners.
We’ll help you, and your partners, see eye to eye.
Visit us on social media @portfolioplanning or our website portfolioplanning.ca





Hi! I am Mindy Blumberg, an optometrist who always looks for adventure. I graduated with honours from the University of Waterloo and moved to British Columbia to live in the mountains. I worked as a forest fire fighter and had the opportunity to connect with locals in rural communities in Canada. During my admittance interview, I shared my goal of committing to helping rural communities get access to eye care services. In 2019, I started my first mobile eye clinic in Bella Coola with the Nuxalk Nation. It was an amazing experience for me to get to know the community and help my patients improve their quality of life with better vision. In 2020 I started Sea to Sky Optometry and has two locations in Pemberton and Lillooet. I have connected with many different First Nations communities to provide mobile eye clinic services and continued eye care. For me, these mobile eye clinics are always an adventure. You just never know who you are going to meet, what stories your patients will share, and what challenges will be along the way. I provide community eye care days where I partner with community services to get patients in need eye exams and glasses at no cost.
With two clinic locations and one optometrist (we
are currently hiring), I had to pivot and provide synchronous telemedicine optometric exams. The inspiration for telemedicine optometric services came from the BCDO Rural Access initiative in offering this equipment and service to the Nuxalk Nation. This technology has been a positive addition to the clinic to increase accessibility to excellent eye care. My mission is to continue to connect with those in need of vision services by taking the time to listen to her patients and collaborate to find the best solution for them.
Success for me is to be able to enjoy practicing in independent optometry clinics and having the freedom to provide the best possible care you can to your patients. Having time away from work to refresh and go on adventures is important to me. Spending time outside every day is how I can stay focused at work. Luckily, I live in Pemberton where there are many opportunities to have little mini adventures.
As a practicing optometrist in BC, how does BCDO help you?
There are so many things that the BCDO does to

help but my favourite is the Rural Access Initiative. This lines up with my values, and I am so happy that this group exists to increase access to eye care and helping Canadians who really benefit from our services. I have been fortunate to travel to some very interesting places in British Columbia that are not frequently visited and meet locals to help them in a very meaningful way. Mobile eye clinics are always an adventure. These rural clinics push your clinical skills and allows you to practice skills that you do not have to do often with routine pre-testing. They also challenge the way you run a business. I have been known to trade glasses for artwork, salmon, and even an ocean tour. It is all part of what I like to call adventure optometry.
Why is being a member of BCDO important to you?
Being a member of BCDO helps provide a sense of community. Being an optometrist in a rural practice as a solo practice owner, having a community of peers for advice and support is important. Attending CE events is critical to stay up to date with current research to continue to give patients the best possible care.

Being an optometrist gives me a sense of purpose in my community. Being available to help my community with any vision problems. From diagnosing ocular health issues that will help save sight, to finding the right contact lenses to meet lifestyle demands, being an optometrist allows me to enhance the quality of life to many members of my community.
What are the most rewarding aspects of your job?
I am so grateful to be able to give glasses to someone for the first time, it is really a gift to see patients experience clear vision and get to see the world clearly.
Do you have a specialty? If so, what made you choose
I try to be able to offer all services to my patients. We focus on primary care but because it can be a two-hour drive (or more) to another optometry clinic or ophthalmologist we offer some specialty services as well. I love vision therapy and postconcussion vision rehabilitation because it makes such a difference in patients’ quality of life. Specialty
contact lenses have been an interesting addition to the clinic, and I get excited when I get to fit a scleral lens on a keratoconic patient, or a patient is interested in Ortho K lenses. Dry eye disease has always been an interest of mine and now that there are more treatment modalities available, I’m enjoying treating more dry eyes. We recently invested in the IRPL which has been a nice addition to the conversation we all have too often about hot compress, omega 3, eye drops, lid hygiene… Optometry is such an interesting profession because there are so many technological advances that make our careers more exciting and help our patients.

My advice for new grads is to have a growth mindset
and strive to continue learning. Graduating is just the first step to building your dream career. Take every opportunity that aligns with your values and learn from as many people as you can. Listen to your patients, and your patients will teach you how to be a better optometrist. Smile, laugh and breathe, this is the best stress reliever during a long day, plus it helps you reset your energy for your next patient.






British Columbians continue to be challenged by long wait times to see family doctors and access much-needed health care services. Against this backdrop, Edelman continued Phase 2 of BCDO’s public awareness campaign, “You’ve only got one pair of eyes”. The campaign focused on increasing awareness of Doctors of Optometry as primary health care providers for British Columbians’ eye health and positioned BC Doctors of Optometry as the “go-to” healthcare professionals for routine and emergency eye health care.
As we approached Phase 2, we refined our strategic communications approach based on discussions with the BCDO board and members. Our Influencer strategy was amended to leverage social media platforms and BCDO members to create short-format videos showing how BCDO doctors serve their communities and provide valuable eye-health related insights. This pivot allowed us to continue with our successful digital public awareness and education strategy, while responding in real time to the feedback of the board and members to implement a new program.
“You’ve only got one pair of eyes”.
British Columbians are dealing with pressures from inflation, possible recession, the ongoing impact of seasonal illness, the Ukraine War, and their news and information feeds are full of these messages. In this social media and digital landscape, BCDO continued with a personable, sensible, and sensitive approach with our concept, “You’ve only got one pair of eyes”. The imagery features the faces of people from diverse backgrounds, ethnicities, ages and genders in a personal and poignant manner.
The Edelman team actioned the most impactful findings from Phase 1 to guide digital campaign development for Phase 2 spanning paid, owned and earned channels. With the findings from Phase
1 captured, Phase 2 of the campaign focused on targeting an older audience who is more likely to click through to the website with potentially less influence from competitors/fast fashion while also sharing urgent care messaging.
Our province-wide campaign targeted two specific sub-categories: Adults 25-54 who had an interest in health and personal care, and parents with children aged 4-18, with the following objectives:
• Establishing BC eye doctors as primary care providers of choice in British Columbia for eye health.
• Continuing to drive awareness of eye health and the importance of routine, comprehensive eye exams.
Phase 2, incorporated learnings from Phase 1 and ran from September 12 until October 24, using Facebook, Instagram, Google paid search, and earned media as the primary campaign channels. The primary messaging for this stage of the campaign remained focused on urgent care, and reaching adults aged 25-54.
Annual survey: The annual BCDO survey provides insights to help guide the overall business strategy for BCDO and provide insights into areas of focus for the 2023 strategy. The survey also provides mediagenic results to guide BCDO media outreach and position BCDO as thought leaders in eye health care in BC. This year, the survey focused on identifying barriers to receiving care for eye health related issues, the unhealthy eye care habits of British Columbians and assessed the level of awareness about visiting an optometrist for urgent eye issues.
Paid media & Google search: We continued with paid social and programmatic display ads simultaneously to expand reach and campaign
efficiencies to push our messages to audiences who may not follow BCDO or eye-care related topics. This approach allowed us to drive awareness of routine eye health and the importance of comprehensive eye exams and introduce urgent care messaging to adults across British Columbia. We continued with always-on paid search tactics throughout Phase 2 and will continue targeting high intent keywords to keep up with the impression share.
Earned: We have launched an earned campaign based on our 2023 survey showing how health inequity extends to eye health access for British Columbians, and the BCDO solution through rural/ remote access and MSP coverage awareness. We will leverage the information from the 2022 research survey to launch this media relations campaign to highlight the survey results.
Organic social: The Digital team continues to create engaging and informative content on BCDO’s Facebook and Instagram channels using BCDO’s content pillars. Three to four posts are scheduled per month. The team is making the most of the Doctor-Generated Content to ensure BCDO social channels accurately reflect BCDO members by spotlighting eye doctors in Reels and providing educational and informative content to our current and prospective followers. We are also sharing through story posts each time BCDO is participates in the media.
Phase 2 ran from September 15 – October 24, 2022, using Google Search, Facebook & Instagram and programmatic ads, to drive awareness of urgent eye care among the target audience and to drive them to the Find a Doctor (FAD) page.
The Google search campaign was activated earlier this year in May 2022 alongside Phase 1 of the campaign, running through Phase 2, and will continue until the end of 2022 with an ‘always on’ approach. This helps us ensure BCDO’s website
and content appears consistently when people search for eye health-related terms. Organic social channels stay active throughout the year and will feature newly created DGC content.
For Search, BCDO continues to build on the success for Phase 1 with highest search impression share of 28.02% among the top competitors, including Specsavers which was at 25.57%. Specsavers appeared to be bidding on BCDO brand keywords but BCDO's impression share stands at 95% for brand paid search campaigns that are currently running. The keyword "emergency eye care center" drove high Search intent traffic to the FAD page at a clickthrough rate CTR of 27.92% and it was found that urgent care and symptom messaging performed stronger on social and resonated best with an older demographic (A35+). Paid search campaign delivered 408k impressions between May 2022 – Oct 24 2022 at an average CTR of 5.38% driving almost 22k clicks to the website. The campaign resulted in almost 3,000 users using the search functionality on the FAD page.
The paid amplification across social and programmatic channels for Phase 2 delivered over 12 million impressions, generating 11,191 link clicks to the BC Doctors of Optometry website. Implementing campaign learnings, we saw an increase in performance across phases.
The Phase 3 campaign is currently in progress running during October and November and includes continuing emphasis on eye doctors as primary care providers with content including children’s vision. Facebook and Instagram programming continues with an emphasis on DGC, with continuing ads around the creative concept “You’ve only got one pair of eyes”.
Doctor Generated Content (DGC) is allowing the Edelman team to build connections with the
BCDO board and members to feature BCDO eye doctors who are serving their communities. Our eye doctors are our truth, and it is important that they shine through on our social channels. Providing useful, informative content while deploying Instagram’s engagement tools, we will continue to establish eye doctors as a primary care providers and gain a larger, dedicated following.
Social media is becoming a hub of informative content, and healthcare influencers are gaining popularity while building trust and relationships beyond the walls of their clinics. Featuring our doctors in this capacity displays them in an approachable, authentic way, while establishing their credibility on eye health and the overall health of British Columbians. Participating members will receive guidance on content themes that will embed seamlessly into our existing strategy, including common eye issues, eye health as selfcare, urgent care and children’s eye health.
We will continue to develop content with BCDO eye doctors who feature the geographic and cultural diversity of BCDO members and highlight
the DGC program through different member vehicles to give doctors the opportunity to be featured on BCDO channels. A direct invitation from board members so far, instead of a callout, has generated strong results. Using BCDO channels to tag eye doctors or clinics will help us improve the performance of the video but this is not required. We are developing and posting one to two DGC videos per month to assess performance and make ongoing optimizations.
As Phase 3 evolves, we will continue to direct traffic from our paid advertisements, organic content and DGC to the Find a Doctor tool, encouraging our audience to book an appointment with a Doctor of Optometry in their community. The Edelman analytics team will continue to track the FAD tool and website visits through link clicks.
Stay tuned for fulsome updates on the performance of DGC and new strategies that will build upon BCDO’s success in 2022 to allow for continuing leadership and innovation in 2023!





