







hen Dr. Adithya Hari talks about nuclear oncology, it’s clear he sees the field not just as a medical specialty, but as a new frontier in the fight against cancer. Combining cutting-edge imaging with targeted treatment, nuclear oncology is changing how physicians detect, monitor and attack cancer at its source.
“Nuclear medicine uses radioactive molecules to study organ function and metabolism,” Dr. Hari explains. “In nuclear oncology, we take it a step further to see exactly where the cancer is, how it’s behaving and how it’s responding to treatment.” This approach has two components: advanced imaging and a breakthrough therapy called theranostics. Theranostics pairs a diagnostic imaging molecule with a therapeutic one. The result is a precise, targeted strike against cancer cells with fewer side effects than traditional chemotherapy. “We can deliver radiation directly to the tumor, sparing healthy tissue,” says Dr. Hari. “Patients often tolerate it better than some of the more potent chemotherapy agents.”
Recently joining LSU’s Pennington Biomedical Research Center, Dr. Hari brings a unique focus on the relationship between cancer and metabolism. Cancer often causes widespread metabolic dysfunction,
altering body composition, diet response and energy use. Dr. Hari’s research aims to understand these changes and integrate metabolic optimization into cancer care –improving both survival and quality of life.
Pennington Biomedical’s long-standing expertise in metabolism and lifestyle interventions makes it an ideal home for this work. With its expansion into cancer research, Pennington Biomedical has become an active member of the Louisiana Cancer Research Center (LCRC) – a statewide collaboration uniting LSU Health New Orleans, Tulane University, Ochsner Health, and Xavier University of Louisiana.
Dr. Hari will also dedicate a portion of his time to direct patient care through a clinical partnership with Mary Bird Perkins Cancer Center. This dual role allows him to bring the latest scientific discoveries from the lab to the clinic, ensuring Louisiana patients benefit from cutting-edge diagnostics and treatments as quickly as possible.
“Louisiana unfortunately leads the nation in rates of cancer, obesity and diabetes,” Dr. Hari notes. “But that also means we have a unique opportunity to lead in research that addresses these overlapping health challenges.”
A key driver of progress is the shift
toward precision medicine. Instead of a one-size-fits-all approach, treatments are increasingly tailored to a patient’s unique metabolic profile. In nuclear oncology, that means using specific tracers to determine the best treatment path and adjusting or even halting therapy based on how the patient responds.
One exciting area is dosimetry, which measures how much therapeutic radiation a patient absorbs over time. “We can evaluate after each cycle of treatment whether to continue, stop or save doses for future use,” Dr. Hari says. “It’s about making therapy as effective and safe as possible.”
Looking ahead, Dr. Hari predicts that nuclear oncology will become central to cancer management – both in diagnosis and treatment planning – within the next decade. “With new tracers and targets emerging for cancers like ovarian, gastric and prostate, we’re entering an era where imaging and therapy are more closely linked than ever before,” he says.
For Louisiana patients, that means earlier detection, more personalized care and a better quality of life during and after treatment. “Our ultimate goal,” Dr. Hari emphasizes, “is not just to treat cancer, but to help patients live well while we do it.”

CANCER IS MORE THAN A MEDICAL CONDITION. It’s a lifelong journey fueled by information, inspiration and medical innovation. Meet some Baton Rouge area caregivers leading the way.


At Our Lady of the Lake Cancer Institute, we’re bringing the future of blood cancer care to Baton Rouge. Our expert team uses innovative treatment options, including CAR T-cell therapy and bone marrow transplants, to deliver precise, personalized care for patients battling leukemia, lymphoma and myeloma.
That’s why we’re the region’s leading cancer treatment destination. That’s why it all counts here. Learn more at ololrmc.com/cancer.

Harry Sequeira, MD; Hana Safah, MD; and Nakhle Saba, MD
Heme-Malignancy and Cell Therapy




It’s a lifelong path that challenges patients and families physically, emotionally and spiritually—a road best traveled with expert guidance and compassionate support.
In Baton Rouge, patients don’t have to walk that road alone. Our community is home to nationally recognized cancer specialists who combine advanced training with a deep commitment to the people they serve. These doctors are more than providers of care — they are partners in healing, educators who make complex science understandable, and advocates who ensure patients feel heard at every step. On the following 20 pages, you’ll meet some of the region’s leading oncologists and surgeons specializing in everything from lung cancer and lymphoma to colorectal, head and neck, and melanoma care.
They’ll share insights on how new treatments are reshaping outcomes, what patients can expect as they move through surgery or medical therapy, and how supportive care — from nutrition to emotional well-being — is just as important as medicine itself.
Their answers don’t just reflect medical expertise. They reveal a philosophy of care rooted in compassion, innovation, and hope. For patients and families navigating the uncertainty of cancer, these conversations offer reassurance that progress is real, possibilities are growing, and healing is always more than treatment.
You’ll also read about some of the ways that cancer care is evolving — and about Baton Rouge health care institutions like Woman’s Hospital and Our Lady of the Lake Cancer Institute that are on the forefront of that change.
From surgical suites to research labs to community clinics, innovation is reshaping what treatment and recovery look like for patients.
Robotics are transforming once-daunting surgeries into minimally invasive procedures that shorten hospital stays and speed healing.
Treatment and diagnosis-related depression and anxiety are being taken ever more seriously, with treatments ranging from medicinal marijuana to transcranial magnetic stimulation.
Precision oncology and clinical trials are matching therapies to each patient’s unique genetic profile.
And once-competitive health care institutions are teaming up to ensure local patients can access the same protocols and expertise found at the nation’s top cancer centers.
Together, these advances — and the brilliant caregivers who employ them — underscore a hopeful reality: Cancer care in the Capital City can provide you with the help you want, the hope you need, and the health you deserve.


When most people think of cancer treatment, radiation and chemotherapy are the first options that come to mind. While those remain critical weapons in the oncologist’s multi-front battle against the disease, less invasive surgical technology and techniques have made surgery part of a patient’s cancer diagnosis and treatment more often than not.
“Our approach to surgery for cancer patients really is personal to the individual,” Baton Rouge General (BRG) Surgical Oncologist Dr. John J. Tabor said. “Sometimes biopsies are done very early to give us a better idea of what’s going on. Surgery can be part of a treatment plan at different times in the journey. It could come first to remove the primary tumor; after chemotherapy to clean up what’s left; or in between treatments.
“In some cases, if the cancer is isolated, and we are confident it can be completely removed, surgery may be the only treatment.”
Advancements in robotics have expanded surgical options and improved recovery times. A common misconception is that a robot is singularly performing surgeries.
In reality, robotic technologies take better advantage of the human surgeon’s skill and experience by providing them “smaller hands” to perform more precise incisions.
Using high-definition cameras, robotic tools also give human surgeons incredibly detailed views on larger video monitors without having to make a large cut. The benefits for patients: less pain, less blood loss, quicker healing and shorter hospital stays.
“We treat a lot of patients with pancreatic and esophageal cancer, and the surgeries to treat them used to be pretty gruesome,” Dr. Tabor says. “These cancers often require a major resection, which means removing tissue or part or all of an organ. Before, surgeons had to make an incision from the bottom of the sternum all the way down to the pubic bone for a pancreatic resection. For an esophageal resection, they had to
put their hand in the patient’s chest to separate the esophagus from the surrounding tissue. Now with robotic surgery, we can do these very complex cases through just four 8-millimeter incisions.
“That has a huge impact on a patient and being able to get back to a normal quality of life.”
With six robots dedicated to oncology, surgeons at the BRG Cancer Center have performed procedures to treat cancer patients from more than 300 ZIP codes inside and outside of Louisiana. Oncologists at Mary Bird Perkins Cancer Center, the Surgeons Group of Baton Rouge, Ochsner MD Anderson Cancer Center and Our Lady of the Lake Robotic Surgery Institute are among the other Capital Region health care providers who also use robotic surgical tools to treat cancer in addition to radiation, chemotherapy, and other treatment plan components.



GYNECOLOGIC ONCOLOGY Woman’s Hospital
WHAT SYMPTOMS SHOULD WOMEN NEVER IGNORE WHEN IT COMES TO THEIR REPRODUCTIVE HEALTH?
Every year, I stand on a different soapbox when it comes to this. The list below is in no particular order because I feel equally passionate about each one.
· Bleeding after menopause is not normal…ever. If you have gone 12 months without a period, then you have gone through menopause. Any bleeding that happens after that should be evaluated. Abnormal vaginal bleeding of any sort is not okay and deserves to be evaluated by a gynecologist.
· Look at your vulva! Each woman should know her own body and what it looks like and what is normal for her. Any deviation from that normal should be evaluated.
· Get your pap smear! It is the only tool we have that can help us prevent a cancer. By collecting cells from the cervix, our pathologists can look at them under a microscope and determine if they are becoming abnormal before they actually become a cancer and then we can remove them before they become cancerous.
· Find a gynecologist you trust. See her or him every year until you physically can’t anymore. This 15-minute interaction can change the course of your life.
· Talk to your family members. Why did every woman have a hysterectomy? What did grandma die from? Knowing your family history can alter your story.
· Get a second opinion! Do not be afraid of judgment or being viewed as crazy. If you feel like something is wrong, but you do not understand what is happening, ask someone else.
• Please respond by e-mail or phone with your approval or minor revisions.
• AD WILL RUN AS IS unless approval or final revisions are received within 24 hrs from receipt of this proof. A shorter timeframe will apply for tight deadlines.
• Additional revisions
Carefully

BREAST SURGEON
Woman’s Hospital
WHAT’S THE FIRST THING YOU WANT A NEW PATIENT TO KNOW?
I want patients to understand the specific type of breast cancer that has been diagnosed because not all breast cancers are the same, and they may require different types of treatments. Each woman’s journey is unique. I try to educate patients about their individual treatment plan and the expectations for each step of their journey.
TO
Our high-risk team does a great job of evaluating and discussing each person’s individual risk and forming plans that are right for them. There are other options for patients who are at high risk of developing breast cancer, including increasing their screening with clinical exams every six months. We can also add MRIs to their surveillance which are very sensitive to any changes in the breast tissue.
Woman’s Hospital has a great survivorship clinic that includes cancer navigators who help patients with any long-term side effects from their treatment. Woman’s Center for Wellness also has many programs for post-treatment surveillance of lymphedema, a cancer fit program and massage therapists who understand the challenges and needs of breast cancer patients.
We are constantly educating our patients about the benefits of lifestyle changes. We recommend 3-4 hours of exercise a week including weight-bearing exercise at least twice a week. We also recommend eating a healthy diet limiting processed foods, sugars, and alcohol.
•
•

GYNECOLOGIC ONCOLOGY
Woman’s Hospital
WHAT ADVANCEMENTS ARE IMPROVING GYNECOLOGIC CANCER DIAGNOSIS?
The most significant advancement has been genetic testing to confirm individuals at risk for developing gynecologic cancers. Another advancement that is a bit more mature is testing for papilloma virus DNA, which can help to distinguish which precancerous conditions of the cervix, vagina, and vulva may develop into malignancy.
HOW DOES GENETIC TESTING INFLUENCE DIAGNOSIS AND RISK ASSESSMENT?
Knowledge of genetic predisposition to cancer can help women determine whether risk-reducing surgery is right for them and can help them plan when they would like to have such a procedure performed. It is also helpful in allowing other family members to understand their risks as well.
HOW IS IMAGING TECHNOLOGY IMPROVING DIAGNOSIS AND TREATMENT?
Advanced imaging tests such as CT scans, MRIs, and PET scans can help us to determine cancers that are limited in size and location and may be better suited for surgery. These tests also help us plan the appropriate sequence of chemotherapy and surgery for cancers of the ovaries, tubes, and uterus.
ARE THERE MYTHS ABOUT GYNECOLOGIC CANCERS YOU OFTEN FIND YOURSELF CORRECTING?
Probably the most common misconception is that they should have a low risk of cancer if no one else in their close family has ever had cancer. On the contrary, most cases of cancer are not associated with any family history.

BREAST SURGICAL ONCOLOGIST
Woman’s Hospital
WHAT’S THE FIRST THING YOU WANT A NEW PATIENT TO KNOW?
I want my patients to know that I am an open book. Surgery, by its very nature, can make patients feel vulnerable, and I am deeply aware of that. That is why I believe it is essential for patients to feel complete trust in the person caring for them.
WHAT STRATEGIES REDUCE THE RISK OF RECURRENCE?
I promote a healthy lifestyle to reduce the risk of cancer recurrence. This includes no tobacco, limiting alcohol consumption, regular self-breast awareness, routine exercise, and a balanced diet. To keep it simple, what is good for your heart is good for your breast.
HOW DO YOU BALANCE SAFETY WITH A PATIENT’S COSMETIC GOALS?
It requires a multidisciplinary approach involving breast surgeons, medical oncologists, radiation oncologists, and plastic surgeons. The primary goal is to ensure the complete removal of the tumor and minimize the risk of recurrence. Long-term data shows that combining advanced surgical techniques like hidden scar surgery or oncoplastic breast surgery are safe and effective.
WHAT SUPPORT SERVICES DO YOU FIND MOST HELPFUL AFTER TREATMENT?
A cancer diagnosis can deeply impact all aspects of a person’s life, from their physical to mental, emotional, financial wellbeing and beyond. This is something we take very seriously at Woman’s Hospital. We have resources to help with each patient’s individual needs. We are especially proud of the services offered at the Woman’s Center for Wellness that address functional issues such as lymphedema, balance, strength training, and medical tattooing.


Advances in cancer treatment are a good news, bad news, good news situation.
Good news: Cancer treatments are becoming more sophisticated and effective.
Bad news: Cancer rates continue to rise. According to the most recent CDC data, Louisiana has more cancer deaths per 100,000 residents than over 40 other states.
Good news: Health care providers are fighting back by teaming up. Partnerships designed to enhance cancer care are taking root at hospitals all across the U.S., and Louisiana is on the leading edge of this life-saving trend.
The Mayo Clinic Care Network gives a group of affiliate hospitals from Pennsylvania to California access to Mayo’s clinical protocols, education, and consultation.
The Cleveland Clinic’s Taussig Cancer Institute collaborates with hospitals in Ohio and Florida on specialty cancer services and research capabilities.
Closer to home, Ochsner Health and MD Anderson Cancer Center formally estab-
lished a partnership in May, making Ochsner the first and only provider in Louisiana with a fully integrated cancer program based on MD Anderson’s standards and treatment plans.
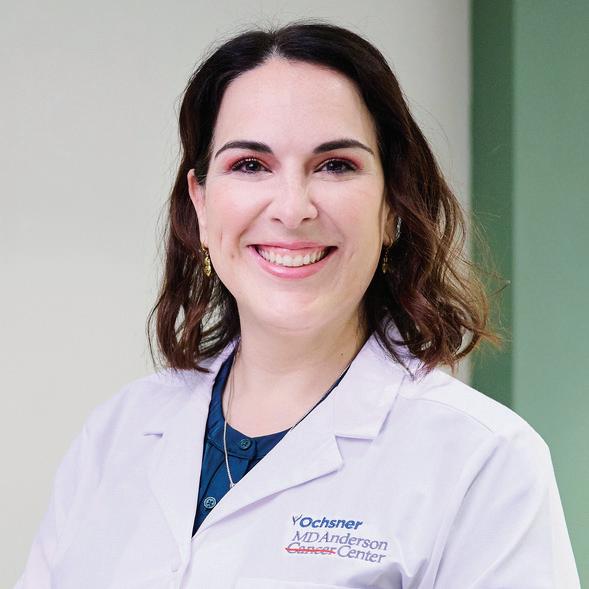
Dr. Jennifer Perone, surgical oncologist at Ochsner MD Anderson Cancer Center, is excited about what the partnership offers patients.
“Our goal is to bring Baton Rouge-area patients the same level of cancer care that they would get if they were able to travel to MD Anderson for treatment,” says Perone.
“It’s wonderful to have access to those kinds of experts.”
Ochsner and MD Anderson are the most recent but certainly not the only cancer care partnerships benefitting Louisiana residents.
Baton Rouge-based Mary Bird Perkins Cancer Center has long worked to reach patients both statewide and regionally through collaborations with a variety of partners, including OneOncology in Nashville and Woman’s Hospital and Baton Rouge General in the Capital Region.
Louisiana Cancer Research Center, a
partnership in New Orleans among LSU Health, Tulane University, Xavier University, Ochsner Health and others, focuses on collaborative cancer research, clinical trials, and population health.
Tulane Cancer Center partners with local hospitals including University Medical Center in New Orleans. And St. Tammany Health System and Ochsner Cancer have a joint cancer center under the Ochsner umbrella.
These and other partnerships of their kind allow patients to receive advanced care closer to home and help major institutions recruit more participants and scale enrollment for clinical trials, expanding research opportunities.
In addition to the benefit of associating with national leaders in oncology, patients at smaller community hospitals also have opportunities for the consistent treatment protocols, data sharing, and training found at widely known facilities. The cost efficiency of sharing technology, research, and infrastructure reduces redundancies and lowers costs – a lifeline for facilities whose budgets are already limited.

Scott Sonnier, MD Hematologist and Oncologist
Ochsner Health and MD Anderson Cancer Center are clinically integrated to provide advanced cancer care right here in Baton Rouge. This means access to life-saving clinical trials for innovative therapies, more specialists and more resources for our patients. Through this collaboration, Ochsner is the first and only provider in Louisiana with a fully integrated cancer program based on MD Anderson’s standards and treatment plans. Learn more at ochsner.org/EndCancer.

COLON AND RECTAL SURGERY
Our Lady of the Lake Cancer Institute
WHAT DO NEW COLORECTAL CANCER PATIENTS NEED TO KNOW?
I want them to understand the disease and what drives our treatment decisions. We talk about further imaging or X-rays that must be done as well as blood work and possibly genetic testing. We like to review all the details, so each patient has a clear perspective.
HOW IMPORTANT IS SCREENING — ESPECIALLY COLONOSCOPY?
Colorectal cancer is the second most common cancer in the United States. Most start from a small polyp or growth on the colon wall. If this is found during a colonoscopy, it can be removed and will not grow into cancer. Please do not wait until you have symptoms … it could save your life.
WHAT CAN PATIENTS EXPECT IN TERMS OF RECOVERY?
Overall recovery can be dictated by your health status and activity level going into surgery. There is great data to support a prehabilitation program to improve strength, nutrition and medical status before surgery. We also have an extensive survivorship program to aid in recovery after cancer treatment.
The highest risk of cancer occurrence is the first two years after diagnosis and drastically decreases thereafter. All patients with colorectal cancer should undergo a clinical exam by a physician every three months for two years and then every six months for the next three years for a total of five years.


HEAD AND NECK SURGERY
Our Lady of the Lake Cancer Institute
WHAT TYPES OF CANCERS FALL UNDER ‘HEAD AND NECK SURGERY’?
There are numerous cancers that occur above the clavicles. Multiple skin cancers can occur within the head and neck. The head and neck are home to unique glands such as salivary glands or endocrine organs such as the thyroid or parathyroid glands, all of which can develop cancerous tumors. Lymphoma and other immune cancers occur here as well. One of the most common head and neck cancers that we see includes cancers of the oral cavity or mouth, the throat, and the larynx.
The best tools for early detection are the patients themselves! Patients should watch out for new moles on the skin or old moles that change, bleed or won’t heal. Any type of new growth or lump in the neck should be reported to your doctor. Any prolonged symptoms that don’t resolve after several weeks should be reported including voice changes, sore throat, ear pain, coughing up blood, difficulty swallowing, difficulty breathing, ulcers in the mouth, facial pain or numbness.
Survivorship is a lifelong commitment, and we view our patients and their caregivers as part of our extended family. Long-term care for head and neck cancer survivors extends far beyond the final surgery, radiation session, or celebratory bell ringing. Our teambased approach remains focused on addressing ongoing concerns, supporting caregivers, and ensuring the highest possible quality of life for survivors through continuous, compassionate care.


PULMONOLOGY
Our Lady of the Lake Cancer Institute
WHAT ROLE DOES A PULMONOLOGIST PLAY IN CANCER CARE?
Lung cancer is usually identified first by an abnormal chest CT scan. That typically leads to an evaluation by a pulmonologist, who often guides the patient through the process of a biopsy to diagnose malignancy, establishes a stage for the lung cancer and directs the patient onto the treating team of providers which can include oncologists, thoracic surgeons, radiation oncologists and occasionally palliative medicine team.
WHAT RECENT ADVANCES IN PULMONARY CARE ARE IMPROVING OUTCOMES FOR LUNG CANCER PATIENTS?
This is a particular exciting time to be involved in lung cancer care. New drugs and treatment approaches are being identified through research that are improving outcomes. Robotic bronchoscopy has changed the way most lung cancer is diagnosed by offering a highly safe and accurate avenue to sample even small lung lesions and identify cancer early. Another recent addition to our diagnostic abilities is a mobile cone beam CT that we recently obtained at the Lake – the first in Baton Rouge.
WHAT STEPS CAN PATIENTS TAKE TO PROTECT THEIR LUNG HEALTH?
Patients can protect lung health first and foremost by quitting smoking. This reduces their risk of future cancers and also improves their treatment course. They should remain physically active, engage in pulmonary rehab if appropriate and remain vigilant for any new signs or symptoms.


HEMATOLOGY ONCOLOGY
Our Lady of the Lake Cancer Institute
WHAT ADVANCES ARE GIVING CANCER PATIENTS MORE OPTIONS?
It is remarkable the number of advances that we have seen over the past few decades. Immunotherapy and targeted therapy are just the tip of the iceberg. Other exciting advances include bispecific antibodies, CAR-T therapy, antibody drug conjugate, and other new treatments that are not only more effective but also are tolerated better.
I feel like this is the most important aspect of my profession. There is a lot of anxiety surrounding the side effects associated with cancer treatments and how it will affect someone’s life. We mitigate the risk of side effects with different strategies including use of medications, lifestyle strategies and supportive care.
HOW DO YOU PERSONALIZE THE TREATMENT PLAN?
Cancer care is truly a team effort. We meet with physicians from other specialties on a weekly basis as part of a multidisciplinary group. We review each patient’s case in great detail and put together a plan in keeping up with the latest treatment guidelines.
There are a lot of new and upcoming treatments such as K-ras inhibitors, antibody drug conjugate such as Datroway, cancer vaccines, and utilization of CAR-T therapy in solid tumors which are otherwise hard to treat. Integrating AI into cancer care is accelerating drug discovery, enhancing biomarker prediction, and transforming clinical trial design.




FDA-approved for treatment-resistant depression for adults and adolescents 15 years and older
86% of patients have their symptoms reduced by 50% while 68% have achieved full remission from their depression
Covered by most insurances
Non-invasive - No surgery, no anesthesia
No medications or side effects
Long-term remission

Acancer diagnosis is life-changing in every sense, and given the physical demands of treatment— surgery, chemotherapy, radiation or newer targeted therapies—it should be no surprise that the emotional toll can be just as profound.
Studies show cancer patients are two to three times more likely to experience depression and anxiety than the general population. Whether driven by fear of outcomes, the strain of side effects or the disruption of everyday life, these emotional challenges often follow patients through treatment and beyond.
Traditional treatment options for depression and anxiety include prescription medications, cognitive behavioral therapy and counseling. Antidepressants and anti-anxiety drugs can be effective, but they may also produce new side effects or interfere with existing medications. Meanwhile, talk therapy and counseling can help, but the rigor of cancer treatment often undermines motivation to seek care.
For patients who have tried traditional therapies without finding lasting relief, the search for options can feel discouraging. But Louisiana is home to a treatment that is both effective and widely available. Transcranial Magnetic Stimulation (TMS) offers a different path forward for those living with mental health conditions that haven’t responded to standard care. Fortunately, clinics across the state provide TMS access to patients who might otherwise feel they’ve exhausted their options.
“TMS uses gentle magnetic pulses to stimulate the part of the brain that regulates mood,” explains Jourdan Generes, CEO of Neurojust, which operates TMS therapy at its clinics in Baton Rouge and Metairie. “It balances brain activity, so patients are no longer living in constant fightor-flight mode. There are no systemic side effects, no drug-to-drug interactions, and it won’t interfere with cancer treatments.”
That last point is key for oncology patients. Cancer regimens are often a delicate balance of medications, procedures and
supportive care. Adding another drug to the mix can be complicated, if not risky. TMS offers a non-invasive, non-pharmaceutical alternative that can be used alongside chemotherapy, radiation or immunotherapy without fear of negative interactions.
Though it remains unfamiliar to many, TMS is far from experimental. The science dates back to the mid-1980s, and the FDA approved its use for depression in 2008. Since then, more than 20 million Americans have received TMS therapy.
The outcomes are encouraging. According to Generes, 64% of patients achieve full remission from severe depression and anxiety, while 86% see significant improvement.
“That often means moving from debilitating depression to only mild symptoms,” he says. “That kind of relief can be life changing. Cancer treatment isn’t just about attacking the disease—it’s about supporting the whole person. When you lift the weight of depression and anxiety, you give patients the mental strength they need to keep fighting.”

As Baton Rouge grows, so does the demand for accessible, high-quality health care. At Ochsner Medical Complex – The Grove, we’re meeting that demand by expanding our facility and the services families rely on. We’re doubling our operating rooms, adding a cardiac catheterization lab, offering advanced imaging, and expanding primary care alongside OB-GYN, pediatric, and musculoskeletal services. Our new fifth floor will add 30 exam and treatment rooms dedicated to women’s and children’s care.
This investment reflects our deep commitment not only to Baton Rouge, but also to the surrounding communities we serve. We’re proud to grow alongside this region and remain dedicated to bringing the best care close to home.
Learn more at ochsner.org/br.

COLON, RECTAL SURGEON
Ochsner MD Anderson Cancer Center
HOW DO COLON AND RECTAL CANCER TREATMENT DIFFER?
Typically, colon cancer starts with surgical resection then chemotherapy could be possible after surgery. Rectal cancer varies in treatment from local resection to a combined treatment with chemotherapy and radiation before surgical intervention. Each plan is tailored to the patient.
DO MINIMALLY INVASIVE AND ROBOTIC PROCEDURES HELP?
Minimally invasive, and especially robotically assisted surgery, have proven to have better patient outcomes, including decreased pain after surgery, shorter hospital stays and faster recovery overall. The patient can begin additional treatments like chemotherapy as soon as they recover and return to their regular activities sooner.
CAN
Although surgery may look small on the outside with small incisions, it is still a big surgery on the inside. This requires a lot of energy to heal, so most patients feel easily fatigued. Early walking and oral intake of nutritious food, even starting the day after surgery, is crucial for a quick recovery.
HOW CAN YOU REDUCE COLON AND RECTAL CANCER RISK?
A healthy lifestyle is critical to prevent colon and rectal cancer. We recommend smoking cessation, limiting alcohol intake and a diet that’s high in fiber and plant-based protein, while low in red meat, processed foods and saturated fats. We also encourage regular exercise and weight loss where applicable. And, as always, get your colonoscopies. •

SURGICAL ONCOLOGIST
Ochsner MD Anderson Cancer Center
WHAT IS THE VALUE OF A MULTIDISCIPLINARY APPROACH?
Patients each have a unique journey, and they often need any number of services for support. Ochsner MD Anderson brings together experts across oncology, radiology, surgery, nutrition, pain management and other specialties. We also provide a “nurse navigator” to help keep patients informed and on schedule.
HOW DOES THIS TEAM APPROACH IMPROVE CANCER TREATMENT?
It combines expertise. Dieticians help ensure patients get the right nutrition for maintaining their strength. Treatment and recovery might call for physical rehab and pain management. Patients often need mental health care professionals to address their emotional and social needs. We treat the whole patient, not just the disease.
Clinical trials open the door to cutting-edge therapies that may not yet be widely available but hold great promise. Patients in Louisiana can access some Phase 1 trials, which are the earliest stages of testing new treatments. At the same time, technology like telemedicine and remote monitoring makes it easier for patients to stay connected.
I started as a theology major and spent time shadowing a hospital chaplain. I realized I wanted to be someone who could both care for patients physically and walk with families through some of their darkest days.


In the war on cancer, experimental and cutting-edge clinical trials are no longer just a last resort—they’re often the frontline strategy. And right now, Louisiana is fast becoming a hub for this transformational work.
Across the state, cancer centers and hospitals are transforming cancer treatment—offering patients access to clinical trials that provide early use of promising new therapies, often years before they’re available to the broader public. These trials are central to growing “precision oncology,” a personal approach using genetic sequencing to uncover specific mutations in a patient’s cancer. Once identified, researchers can match patients with therapies designed to target those genetic markers directly, leading to better outcomes and fewer side effects.
“The classic way to treat cancer has been through non-targeted chemotherapy that’s rather indiscriminate,” explained Dr. Victor Lin, medical director of clinical research at Mary Bird Perkins Cancer Center.
“But now we’re able to look at the genetic sequence of these cancer cells and find out what specifically drives them. Since every cancer is different, we’re able to offer better targeted therapies tailored to each type. It’s a significant evolution.”
That evolution is happening right here in Louisiana, where a first-of-its-kind lung cancer trial is underway at Mary Bird Perkins, marking a major milestone for the state’s research community. Sponsored by Lilly, this phase 3 trial builds on an earlier-phase trial. It’s one of several early-phase trials now accessible in Louisiana, expanding options for patients and allowing more of them to receive advanced care close to home. In a notable reversal, patients from outside the state are even traveling here to participate in trials they can’t access elsewhere.
“We’re bringing access to treatments that patients used to leave the state for,” said Lin. “Now, the unthinkable has happened: patients are coming from out of state to enroll in trials here.”
The benefits of this shift reach well beyond individual care. Growing clinical trials strengthens medical infrastructure, attracts research talent and spurs economic development. Importantly, these trials are also helping address health disparities by expanding outreach to underserved communities.
A recent $400,000 grant is funding efforts to improve participation among rural and minority populations, groups that have long been underrepresented in clinical research. By increasing access to trials, institutions like Mary Bird Perkins are working to ensure that innovation benefits all patients—not just a privileged few. As it rises as a leader in precision oncology, Louisiana’s scientific progress shows that it is most meaningful when it’s accessible. “The goal isn’t just to move the science forward,” said Lin. “It’s to bring that science home—to make sure patients in our communities have access to the very best care, right where they live.”
Mary Bird Perkins is 100% devoted to you and to fighting cancer.

SPECIAL ADVERTISING SECTION
GYNECOLOGIC ONCOLOGY
Woman’s Hospital
WHAT SYMPTOMS SHOULD WOMEN NEVER IGNORE WHEN IT COMES TO THEIR REPRODUCTIVE HEALTH?
I would encourage women to seek evaluation with any bleeding after menopause, heavy or irregular bleeding prior to menopause, persistent abdominal bloating or swelling, persistent pelvic pain or sudden weight loss or weight gain.
WHAT SCREENING OPTIONS SHOULD WOMEN DISCUSS WITH THEIR PROVIDERS BASED ON AGE OR FAMILY HISTORY?
From a gynecologic cancer standpoint, women should make sure that they are having annual pelvic examinations and pap smear testing. Additionally, the U.S. Preventive Services Task Force (USPSTF) publishes screening guidelines for cancers that have screenings available.
HOW DO YOU INVOLVE THE PATIENT IN DECISION-MAKING WHEN MULTIPLE TREATMENT OPTIONS ARE AVAILABLE?
At the first consultation, I try to assess where patients are in processing their diagnosis, who they trust to help them make complex decisions, and what their overall goals are for cancer treatment. Then I usually write out each algorithm of choices, and we identify a plan that most aligns with their goals.
HOW CAN MOLECULAR OR GENETIC PROFILING INFLUENCE CARE PLANS?
Molecular profiling of tumors can inform therapy options for most gynecologic cancers. The information from tumor testing allows us to add in targeted therapies with known treatment efficacy, as well as trial novel therapies.
BREAST SURGICAL ONCOLOGIST
Woman’s Hospital
WHAT ROLE DOES A BREAST SURGEON PLAY ON THE CARE TEAM?
We serve as the quarterback of our breast cancer care team. Alongside the patient’s OB/GYN, we provide education, reassurance, and serve as a focal point for trust in the larger team. We help you organize and manage everything you will need in the complex world of healthcare.
WHAT’S THE FIRST THING YOU WANT A NEWLY DIAGNOSED PATIENT TO UNDERSTAND ABOUT THEIR TREATMENT JOURNEY?
It is going to be a tough year, but we will get you through it. We have an entire team to take care of you every step of the way. We know this may be new to you, but this is what we do every day.
WHO ARE IDEAL CANDIDATES FOR BREASTCONSERVING SURGERY?
With oncoplastic surgery, almost all patients, even those with multiple or some larger tumors, can be candidates if they are motivated to save their breast. Oncoloplastic surgery combines traditional breast cancer surgery with reconstructive plastic surgery. The goal is to remove cancer while preserving or improving the natural breast appearance by rearranging the patient’s own breast tissue in one surgery. This often helps avoid a distorted breast and allows patients to heal physically and emotionally.
HOW CAN PATIENTS FEEL CONFIDENT THEY’RE PICKING THE RIGHT OPTION?
The right surgical option is extremely personal. There’s no onesize-fits-all for everyone, and each person’s cancer is unique, just like they are. The best plan is the one that makes you feel most comfortable, not just now but for the next 10 years and beyond.

DR. WILLIAM MILLS Owner, Alinea Performance Physical Therapy
HOW CAN MEN’S PELVIC FLOOR PHYSICAL THERAPY AID MY PROSTATE CANCER PROGNOSIS?
Prostate cancer treatments often carry side effects such as urinary incontinence and erectile dysfunction, both of which impact quality of life. Whether you are preparing for treatment or recovering, pelvic floor physical therapy is an important option to consider. Research shows it can significantly reduce both the frequency and volume of urinary leakage and improve erectile function. Our best outcomes are seen in patients who begin strengthening prior to treatment.
WHAT ACTUALLY HAPPENS DURING PELVIC FLOOR PHYSICAL THERAPY?
While Kegels are part of the process, our therapy approach is much more comprehensive. Our approach empowers patients with practical strategies for bladder control and overall health, including hydration management, bladder scheduling, fiber intake, partner communication, proper core bracing, breathing techniques, and more.
WHAT MAKES ALINEA PERFORMANCE’S SERVICES SO VALUABLE TO YOUR RECOVERY PLAN?
Let’s hear from a past patient:
“I had my prostate removed June 3, 2024. My surgeon referred me to Alinea because they specialize in post-surgery rehab primarily to slow and stop bladder leakage. I followed a program with Dr. Mills that included in-person visits and an app that schedules exercises and tracks daily urine volume leakage. I started around 1,600 grams/week and now am below 64 grams/week. Dr. Jake Lape also treats me with “dry needling” which is virtually painless. Special thanks to Dr. Mills.”





The use of medical marijuana is becoming an increasingly mainstream prescription remedy for a wide range of conditions. While the general public typically associates the growing popularity of cannabis with younger users, many if not most medical marijuana users are patients of all ages seeking relief from a wide range of severe or chronic ailments.
Capitol Wellness Solutions is the only dispensary licensed to sell medical marijuana in the Baton Rouge area. CEO and founder Randy Mire says there’s a common misconception about the customers he serves.
“You’re more likely to find a middle-aged female suffering from anxiety or sleeplessness, or a customer suffering from chronic pain, cancer, epilepsy or PTSD in my dispensaries,” he explains.
This shift in patient demographics highlights the evolution of cannabis as a therapeutic option.
A key driver of this trend is the mounting
body of research validating cannabis’s effectiveness, particularly in alleviating the difficult side effects of chemotherapy. The American Cancer Society website, for example, reports that “the strongest benefits have been shown when cannabis is used to help relieve pain, nausea and vomiting and loss of appetite.”
Data shows a sharp increase in usage over the last two decades. A study from Carnegie Mellon University, which analyzed data from more than 1.6 million respondents, found the per capita rate of people reporting past-year use increased by 120 percent between 2008 and 2022, while the number of days of use per capita surged by 218 percent during the same period.
That same research revealed that in 2022, for the first time, there were more daily or near-daily cannabis users (17.7 million) than daily or near-daily alcohol drinkers (14.7 million) – a historic sociological shift.
The increase is largely attributed to changes in public perception and policy. The Pew
Research Center reported in a January/February 2025 survey that around 9 of every 10 U.S. adults believe marijuana should be legal for either medical and recreational use (54 percent) or medical use only (33 percent).
This broad public support has translated into widespread state-level legalization, with nearly 15,000 dispensaries now operating nationwide. As of early 2025, more than 3.6 million people were registered in medical cannabis programs across the country.
As Mire puts it, his patients are “really just looking to sleep better at night or live a better life.”
While the medical community continues to advocate for more rigorous, large-scale clinical trials, the evidence is compelling. Medical marijuana is not a “cure” for these conditions, but rather a tool for symptom management that can significantly improve a patient’s quality of life.



For more than 55 years, Woman’s has stood beside women at every stage of life. When a gynecologic cancer diagnosis changes everything, our expert team is here to help you move forward—with the con dence, strength, and compassionate care you trust.
Our team of board-certi ed gynecologic oncologists, specialized nurses and cancer navigators o er advanced treatments and personalized support designed for women. From diagnosis to survivorship, the team who knows women best stands with you. You are never alone.
If something doesn’t feel right, don’t wait. Trust your instincts. Trust Woman’s with your care. womans.org/GYNcancer







t Woman’s Hospital, breast cancer care is about more than treatment – it’s also about restoring confidence and quality of life. Our team of specialized breast surgeons – Dr. Cecilia Cuntz, Dr. Lindsey Fauveau and Dr. Jamie Patterson – work closely with each patient to help them find the path that best supports their healing and recovery.
Breast reconstruction is most commonly performed using two primary methods: implant-based and autologous procedures. Autologous procedures use the patient’s own tissue, while implant-based reconstruction uses medical-grade implants. Both approaches are available at Woman’s Hospital, allowing each patient to choose the option that best aligns with their individual needs, preferences and treatment plan.
One advanced option for those who qualify is the DIEP (Deep Inferior Epigastric Peforator) flap procedure, which uses a patient’s own tissue to restore the breast after surgery. During this procedure, the team of specialized breast surgeons works alongside reconstructive plastic surgeons to remove and reconstruct the breast.
“The DIEP flap is a highly advanced, autologous reconstruction technique,” explains
Dr. Fauveau. “We use the patient’s own tissue, including fat and blood vessels from the abdomen, to reconstruct the breast. This approach offers a more natural look and feel, and often results in a flatter abdomen.”
Woman’s Hospital is uniquely positioned to offer this procedure. The DIEP flap was pioneered in Louisiana in 1992, giving Woman’s team of breast and plastic surgeons extensive experience through strong regional training.
“Our team of breast surgical oncologists and reconstructive plastic surgeons brings more than 30 years of combined experience performing this procedure,” says Dr. Fauveau. “Patients in Baton Rouge and beyond benefit from a legacy of expertise that is rare elsewhere in the country.”
To determine if a woman is a candidate for the DIEP flap procedure, the team at Woman’s Hospital uses advanced imaging and thorough evaluations to carefully assess each patient’s abdominal blood vessels and overall health, ensuring the best possible outcome.
“Prior surgeries, especially those involving the abdomen, can affect eligibility,” she notes. “But with modern, minimally invasive techniques, many women – even those with previous surgeries – may still qualify.”
Recovery typically ranges from six to eight weeks.
“Our patients appreciate the natural appearance and the peace of mind that comes with using their own tissue,” Dr. Fauveau shares. “Many also value not having to return for implant replacements years down the line.”
At Woman’s Hospital, a dedicated team of breast specialists — including experienced nurses and surgical staff — provides a wide range of comprehensive surgical solutions.
“We have tremendous staff and a dedicated breast team, which is special because they are committed to the cause, and this is what they do every day. We pride ourselves on a smooth, collaborative approach that ensures patients feel supported at every stage,” says Dr. Fauveau. “From the initial consultation to recovery, our focus is on high-quality, evidence-based care in a supportive environment.”
For women facing breast cancer, the extensive team at Woman’s Hospital offers hope, healing and a renewed sense of self. Scan the QR code or visit womans.org to learn more.