






I am very pleased to welcome you to this special Trainee Issue of Anaesthesia News. Trainees contribute hugely to anaesthesia practice in Great Britain and the Republic of Ireland while on the journey from novice to senior. We are especially valued out-of-hours by trainees in other specialties, aiding with practical tasks and advice when they request help ‘sideways’, rather than trying to go up the ladder of their own seniors.
This year marks 55 years for the Association Trainee Committee, and we are proud to bring you this annual themed issue of Anaesthesia News dedicated to topical trainee matters. The particular theme for this year’s issue is What’s on your mind?, tales from behind the mask Most hospitals are still asking staff and visitors to wear a face mask which has continued since the start of the COVID-19 pandemic; while we have made a lot of progress, anaesthesia trainees have had to deal with a lot over these 22+ months. Some of these problems have been ‘masked’ by the fact that we are highly skilled and efficient professionals who mostly love to come across as having a situation under control. We therefore thought that this trainee issue should be dedicated to all that has gone on –noticed and unnoticed.
We recognise the ongoing low morale within the whole healthcare environment; however, within this issue of Anaesthesia News we want our readers to remember that there is always a way around any challenge. We are grateful to all the authors who have contributed articles to this issue, including: accounts about examination innovation during the pandemic; recognising diversity in the specialty; switching specialties; sustainability; the graft of examinations; and the work of balancing career and family. I hope that you enjoy reading this issue as much as I have, and appreciate the power in these voices. I also hope that more trainees will contribute their skills and talents to the Association by serving on the Trainee Committee.
ST7 Anaesthetics, North-West England
Elected Member, Association of Anaesthetists Trainee Committee
Twitter: @UChukwumaife

Introduction
Innovation in exam preparation - delivering the first high-fidelity online examination practice event
What’s on your mind? Tales from behind the mask
Thoughts on swapping speciality training from emergency medicine to anaesthetics
Training in anaesthesia and intensive care; our enthusiasm for workforce and environmental sustainability needs to reach beyond the hospital walls
Visit to Red Lion Square: my nine-year exam journey
Nine steps to FRCA success
Trainee Conference: the workshop perspective
Scavenging, when do we really need it?
The POPPY Study; RAFT’s fourth national research project blossoms
Particles
Digested
letters
Association of Anaesthetists
21 Portland Place, London W1B 1PY
Telephone: 020 7631 1650 Website: www.anaesthetists.org
Anaesthesia News Editorial Committee Editor: Mike Kinsella
Robert Self (Chair), Seema Agarwal, Mark Stacey, Ugonna Chukwumaife (Trainee Committee), John Shubhaker (SAS Committee) and Officers of the Association (ex-officio).
Address for all correspondence, advertising or submissions: Editorial Assistant: Kate Mooney Email: anaenews@anaesthetists.org
Design: Chris Steer
Digital Designer
Telephone: 020 7631 8803
Email: chris@anaesthetists.org
Printing: CKN Print
Copyright 2022
Association of Anaesthetists
The Association cannot be responsible for the statements or views of the contributors. No part of this magazine may be reproduced without prior permission. Advertisements are accepted in good faith. Readers are reminded that Anaesthesia News cannot be held responsible in any way for the quality or correctness of products or services offered in advertisements.

The COVID-19 pandemic presented unanticipated challenges; the long hours and increasing physical and psychological demands were very obvious, but less apparent was the additional stress and uncertainty for anaesthetic trainees who were preparing for upcoming FRCA examinations. In September 2020 examinations moved to an online format, which made traditional exam preparation courses seem obsolete and to have lost fidelity; furthermore, many were unable to keep up with face-to-face sessions because of social distancing restrictions. Innovation was required rapidly to allow continuing provision of examination support to trainees.
The ‘Final Written Exam preparation day’ was well established within the Northern School of Anesthesia, organised and delivered by consultants and trainees with an interest in education, many of whom having experienced their own exam challenges. The team were intrinsically motivated to provide support for their colleagues and to adapt the course to accommodate the new exam structure, so replicating the online format as closely as possible. This was a daunting task, the success of which relied on many factors: IT expertise and web design; a suitable bank of questions, answers and mark schemes; faculty to invigilate, mark papers and provide personalised feedback; and consultant-level quality control to address any issues.
The online exam system was custom-designed and built by a faculty member who is also a local trainee. It is an interactive system that runs on a web browser and has the facility to store answers to allow for later review and marking. There is an inbuilt exam dashboard operated by the faculty, used to start and stop the exam in addition to monitoring candidate progress throughout the mock exam period. Questions were adapted from the local question bank, written by senior trainees and consultants, and uploaded into the online system. Candidate log-in and invigilation by faculty were done remotely.

On 24 August 2020 the first event in this new format was launched online with three local candidates. Unanticipated IT snags were resolved in real time as the exam practice proceeded. We were delighted to able to deliver a high-fidelity practice exam with timely marking and feedback. Before the following event, further tests and system checks were performed to ensure smooth running of the online exam platform and minimise disruption to candidates. Having established the system functionality, we advertised the day to external candidates. Demand for places exceeded expectation, and we even had a candidate login from Australia! This highlighted the need for more faculty to ensure that we maintained the ability to provide timely feedback.
Further adaptations have seen candidate numbers capped and spread throughout a week, with smaller numbers on each day and a more efficient marking process. Candidate feedback has been mostly positive, with many emailing to say how helpful the day had been (which made the hard work worthwhile)! One or two candidates however felt unhappy that we did not offer the full exam questions along with their personalised feedback.
We continue to develop our question bank, modifying and adding new questions between events, and plan to continue offering an online format in the future. There have been many learning points along the way, most importantly the value of determination and teamwork.
Lianne Martin
ST7 Anaesthesia, Royal Victoria Infirmary, Newcastle
Tom Johnson
ST7 Anaesthesia, Royal Victoria Infirmary, Newcastle
Sara Scott
ST7 Anaesthesia/ ICM, Royal Victoria Infirmary, Newcastle
Consultant Paediatric Anaesthetist, Great North Children’s Hospital, Newcastle
Twitter: @DrLmartin1; @jetbackwards89; @Cat_people; @Lwaring







In August, I will begin anaesthetics training, and to be completely honest, these are words I never thought I would write. I recall being a very impressionable F1 who was awestruck by anyone who knew more than me. I remember attending an arrest call and seeing the anaesthetic trainee arrive with an air of calm and confidence. “I want to be like that” I recall thinking. “I want to be as skilled as she is.” I never imagined that I could be, because I had never met or seen anyone in anaesthesia who looks like me. By the way, what does an anaesthetist actually look like? I had a skewed sense that the specialty was reserved for the espresso-drinking, upper-middle-class bike aficionado. At that point, I abandoned even the thought of pursuing a career in anaesthesia..
I began to think about anaesthetics again towards the end of F2. I persuaded myself to organise a taster week. I was greeted with open arms by two very kind registrars, and I fell absolutely in love with the specialty. I debated whether or not I should apply, and for a long time I grappled with the idea. I wondered if anaesthetics, a specialty in which black doctors are severely underrepresented, would feel like a safe training environment for me, a black trainee. Feeling safe and comfortable in training has always been important to me because it has a direct impact on the quality of training received, which is particularly relevant in an apprenticeship model like anaesthetics.
I decided to do some research on black anaesthetists in the NHS. This was difficult, as there are very few; however, in October 2021, Dr Sethina Watson led a campaign on Twitter for representation of black doctors in anaesthesia and critical care. It was refreshing to see black anaesthetic trainees and consultants in the UK. Although I am still yet to meet one in person, seeing them on social media was nonetheless encouraging. The campaign also highlighted for me that I was not the only one who had noticed and felt discouraged by the absence of black doctors in the speciality. This was deeply validating.
The application process for anaesthetics training opened a month after this. I was absolutely certain that this is what I wanted to do and decided to apply, after overcoming my biggest reservation. I am excited that I will start training in August, and I am hopeful that more people who look like me will apply for anaesthetics in order to develop a more diverse workforce. I can only hope to be, for someone else, what I saw in so many of these black anaesthetists and intensivists on Twitter.
‘You can’t be what you can’t see’ I always thought to be a cliché. I now see so much truth in it, particularly in medicine. There are specialties that are traditionally represented by specific groups, and it can be quite daunting and difficult to infiltrate and feel like one belongs – because, ultimately, this is what we all want: to feel like we belong, to feel like we deserve to be in a space, just as much as anyone else.
“So, when are you swapping to anaesthetics?” It’s a common question to EM trainees rotating through anaesthetics and ICM during their second year of ACCS training – usually tongue in cheek, accompanied by a wry smile and based on prior experience of trainees having made the jump.
As an ACCS EM trainee, I’d been given advance warning about having my choice of specialty gently challenged. I began my second year of ACCS training resolute; it is however tricky to be away from one’s parent specialty for 12 months and remember clearly why one chose it in the first place: I’d enjoyed the teamwork, learning through exposure to new problems and being challenged to formulate a diagnosis and management plan with limited history and investigations. And didn’t the days off during the week make the difficult rota more palatable?
However, as I was welcomed into the anaesthetic department and became familiar with working in theatres, my resolve waned. I started to focus on the positives of working in a career in anaesthetics. I returned to the ED for my third year of ACCS with more than a grain of doubt about whether to continue training in EM. A decision to give up a run-through training number in a specialty is not easy. I considered taking an out-of-programme pause to spend time back in anaesthetics, chatted through the possible routes to changing specialities with the anaesthetics training programme director, and weighed up the pros and cons with a mentor from the Health Education England mentoring scheme. Once I had made the mental commitment to swap specialities, I decided to reapply for anaesthetic training for the security of a training programme, rather than completing the corelevel equivalence certificate in anaesthetics outside a programme.
The factors that encouraged me to change speciality were a combination of a push from one side and a pull from the other. The ED is an extremely challenging environment to work in day in, day out. Looking into a future working in an overcrowded department struggling with the effects of limited bed capacity, the resultant exit block, and increasing attendance numbers was unappealing [1]. It is exhausting and hard to feel that one is providing the best possible care in a perpetually busy department. It’s interesting to note that few EM registrars work a full-time rota, most reducing their hours in a bid to avoid burnout. Clearly there are difficulties faced during any specialty training programme: for anaesthetics there are the notoriously tricky FRCA Primary, highly competitive registrar training application [2] and the enormous backlog of patients awaiting surgery [3].
Some people are more suited to jobs than others. Whilst I have huge respect for anyone able to work in ED, for me anaesthetics provides exposure to many of the good bits of EM such as interesting patients, problem solving and teamwork, without the pressure that results from being on the very front line. I enjoy the strong focus on patient safety and the widespread recognition of the effect of human factors on our patients and colleagues [4]. It is a luxury to manage one patient at a time in theatres, and to work with a team whose sole responsibility is also that patient.
COVID-19 has encouraged many medical staff to rethink their priorities. What’s important to us now has shifted as a result of lockdowns, the exhaustion of working during the COVID-19 peaks, and exposure to both personal and large-scale suffering. I would encourage others who are considering a career change to seek support and be encouraged that, although the decision may be hard, the grass really may be greener on the other side.
Amy FosterACCS Anaesthetics
Bradford Royal Infirmary1. Royal College of Emergency Medicine. RCEM Acute Insight Series: crowding and its consequences, 2021. https://rcem.ac.uk/wp-content/uploads/2021/11/RCEM_ Why_Emergency_Department_Crowding_Matters.pdf (accessed 18/8/2022).
2. Royal College of Anaesthetists. Anaesthesia National Recruitment 2021 applicants CT1 and ST3, 2021. https:// www.rcoa.ac.uk/news/anaesthesia-national-recruitment2021-applicants-ct1-st3 (accessed 18/8/2022).
3. Royal College of Anaesthetists. RCoA response to HEE training places, 2022. https://rcoa.ac.uk/news/rcoaresponse-hee-training-places (accessed 18/8/2022).
4. Katz D, Blasius K, Isaak R, et al. Exposure to incivility hinders clinical performance in a simulated operative crisis. BMJ Quality & Safety 2019; 28: 750-7.

A recent tweet of mine about commuting distances garnered much attention and discussion beyond the specialty [1]. My colleagues and I travelled a total of 678 miles over a weekend on-call. As a specialty, we are rightly focused on wellbeing and our impacts on the environment, but I think we need to look at the journeys that trainees make as part of this.
On the weekend described in the tweet, a conservative estimate of our collective CO2 emissions was 165 kg. Using the Association of Anaesthetists eCO2 calculator [2], for the same CO2 amount I could give my usual anaesthetic of sevoflurane/oxygen/air at a FGF of 1 l for 125 h, and still have CO2 to spare. Travel is where we need to focus our efforts, surely? Small decreases in anaesthetic CO2 contribution are inconsequential if we have already emitted ten-fold this amount by the time we arrive at work.
I am not alone in dreading a rotation to a faraway hospital that takes an hour to get to, and even longer to return home in rush hour. When I arrive at work, I am already tired. I don’t feel that I can be my best, but thankfully the rotation is a short three months. It is only when I rotate closer to home that I realise what a strain it has been. The connection between commuting, low job satisfaction and burnout is recognised [3, 4], but hasn’t been explored in our own attempts to reduce burnout. Yes, there is hospital accommodation available, but this is of highly variable quality, away from our homes and our families, and for many is not an acceptable solution.
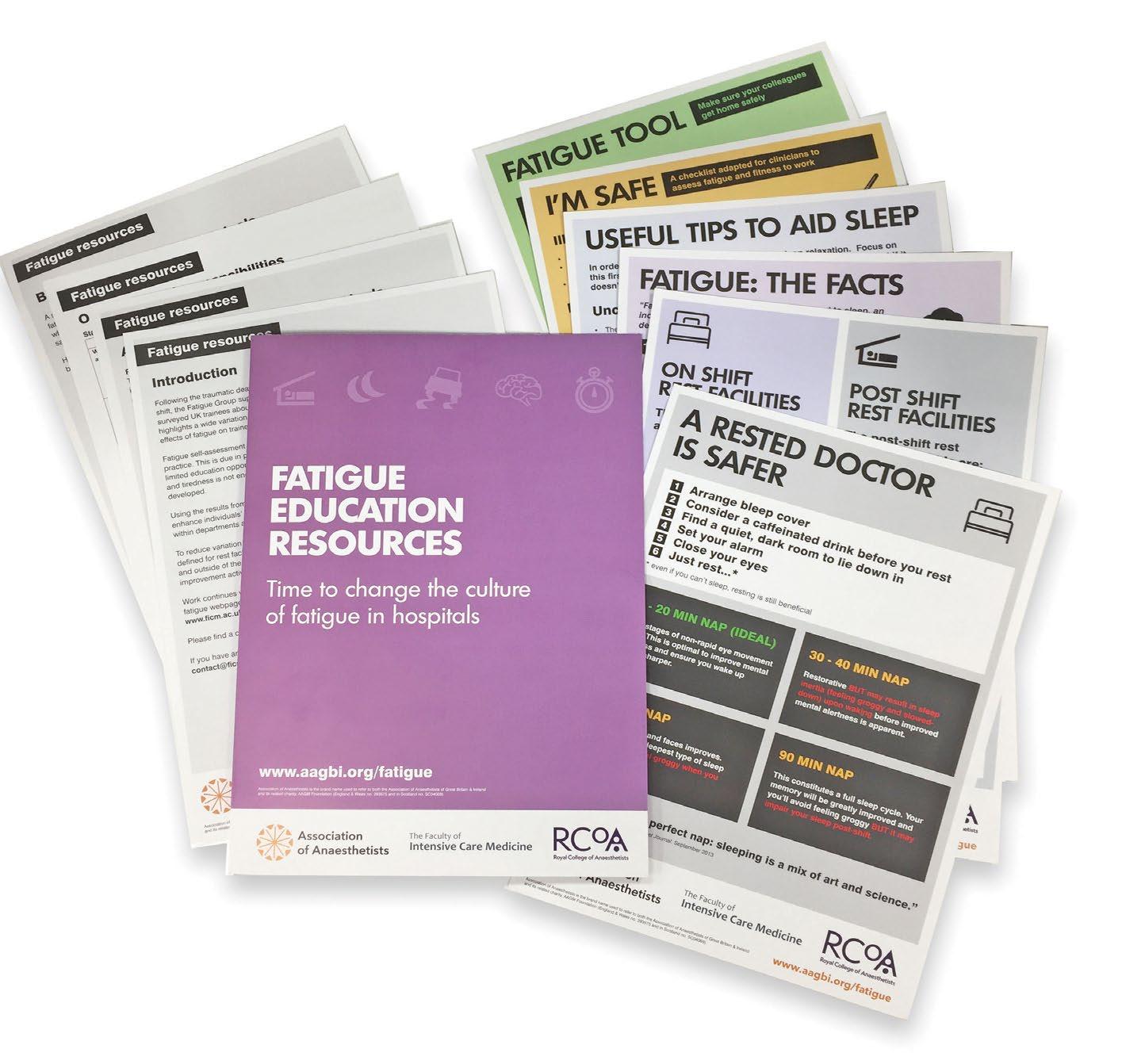
The death of Dr Ronak Patel in August 2015 on the way home from a night shift in anaesthesia caused changes to our attitudes towards fatigue. A majority 57% of responders to the Association of Anaesthetists national fatigue survey said that they had experienced an accident or a near-miss when travelling home from a night shift [5]. Positive changes in availability of night rest facilities did occur, but I think we need to consider the necessity for doctors to rotate to hospitals long distances from home for specific competency acquisition.
Once again, the rotating doctor is at a disadvantage when looking to reduce their carbon footprint. Cycle-to-work schemes and salary sacrifice opportunities to purchase electric cars are not open to those of us on short term contracts. A lead employer could change all that and enable environmental and financial advantages.
So to those deciding that we need to rotate, I ask “Can we reduce the carbon footprint of anaesthetic trainees by making different decisions?”
Acknowledgements: Thanks to Dr D. Marriott and Dr Z. Whitman for encouragement and input
ST7 Intensive Care Medicine and Anaesthesia, East Midlands Deanery
Twitter: @frantait85
References
1. Twitter. Commuting for training, a thread inspired by @gabyadkins, 2022. https://twitter.com/frantait85/status/1518129499686289408 (accessed 12/8/2022).
2. Association of Anaesthetists. Anaesthetic gases calculator, 2019. https://anaesthetists.org/Home/Resources-publications/Environment/Guide-togreen-anaesthesia/Anaesthetic-gases-calculator (accessed 12/8/2022).
3. Amponsah-Tawiah K, Annor F, Arthur BG. Linking commuting stress to job satisfaction and turnover intention: The mediating role of burnout. Journal of Workplace Behavioral Health 2016; 31: 104-23.
4. HaGani N, Englard Hershler M, Ben Shlush E. The relationship between burnout, commuting crashes and drowsy driving among hospital health care workers. International Archives of Occupational and Environmental Health 2022; 95: 1357-67.
5. McClelland L, Holland J, Lomas JP, Redfern N, Plunkett E. A national survey of the effects of fatigue on trainees in anaesthesia in the UK. Anaesthesia 2017; 72: 1069-77.

I had my first encounter with the FRCA examinations as a second-year medical student when I started working with the Mersey School of Anaesthesia (MSA) helping with the administration of exam preparation courses for trainee anaesthetists. After having a glimpse into the world of anaesthetic exams, I vowed to myself then that I wouldn’t ever be an anaesthetist. Fast forward nine years, and I am now a CT2 anaesthetic trainee who recently sat the first Primary OSCE/ SOE exam held face-to-face at the RCoA since the COVID pandemic.
I continued my involvement with the MSA and the aspect I enjoyed most was meeting anaesthetic trainees from across the country (and world!). These doctors, despite being in the midst of intense revision for exams, seemed to love their job and even strongly suggested a career in anaesthetics to my medical student self. Plus, I got the overwhelming impression that anaesthetists were a lovely group of people! I have all of those who took the time to chat to me, offering advice and support during a stressful and busy time of their lives, to thank for my decision to apply for core anaesthetics when the time came.
After hearing many trainees’ stories of the trip to Red Lion Square over the years, I was quietly disappointed that I might not have the same experience (and importantly miss out on a visit to the infamous Square Pig!) due to COVID restrictions and the movement of the exam to an online format. However, with the return to face-to-face exams this year, I was within the first cohort to sit the OSCE/ SOE at the RCoA since 2020.
In the final few weeks of revision, I had doubts about my preparedness for the exam and constantly felt as though I didn’t have enough knowledge. Encouragement and support from friends and colleagues assured me that this was an all-toocommon feeling, and that all Trainees tend to focus on what they don’t know, rather than thinking of all they do know.
I travelled to London the day before my exam. A close friend very kindly came with me as a pillar of support, which was invaluable. On the train we found ourselves sitting across from a fellow trainee anaesthetist. Upon reaching Euston, a lady who had been sitting behind us and had overheard our conversations wished us the best of luck, explaining that her husband was an examiner for the surgical exams and assured us that “All of the examiners want you to pass”, reassuring words to hear from a kind stranger.
We had booked a hotel within walking distance of the RCoA, and went out for dinner and enjoyed a glass of wine whilst chatting about anything other than the upcoming ordeal. En route back, we visited Red Lion Square and the RCoA, which at this time was in darkness. It seemed a far less intimidating building than that which I had envisaged, changing my mindset somewhat when walking through the doors the following morning. That morning, after a few laps of Red Lion Square to clear the mind, I watched a motivational YouTube video ‘I am a champion’ and power-posed in front of the mirror – initially feeling very silly but resulting in me walking into the RCoA with a positive mindset thinking that, just maybe, I could somehow pull this off.
It was an exceptionally hot day in London, with the air conditioning in the RCoA not working. My first component was the pharmacology and physiology SOE, the pharmacology being the topic about which I was most apprehensive. I came away unconfident in many of my answers, but pleasantly surprised at the friendliness and approachability of the examiners; they really did give off the impression that they wanted you to pass. After a short interlude, and another lap of Red Lion Square, I headed back inside for the OSCE. My first station happened to be a rest, not an ideal start but immediately an examiner coordinating the movement of candidates offered me a drink of water – another demonstration of their kindness. The OSCE was a long and exhausting couple of hours, with the important advice of treating each station as a fresh start very apparent; I forced myself to take a few deep breaths and forget about the last when reading the instructions for the next.
A longer interlude until my last SOE of the day; the examiners again were approachable and were clearly experienced in guiding candidates through the SOE, ensuring that I didn’t spend unnecessary amounts of valuable time talking about certain points, and steering me through the SOE in a way in which I was allowed to demonstrate my knowledge.
Overall, the day was well-organised, particularly with it being the first face-to-face delivery in over two years, with an abundance of examiners and staff ensuring that candidates were looked after, in the right place at the right time, and putting us at our ease.
In the period between the exam and results I felt in a strange limbo, finding myself thinking that I should be revising at every opportunity as I had the previous months. I convinced myself I that I would be repeating my journey down to London for a re-sit in a few months time, and all I could think about was what felt like the countless times I had said “I don’t know” in various forms throughout the day. Much to my surprise, I opened the results email with the news that I had passed both components; I have re-checked that email many times since, thinking I must have read it wrong in my post-night shift haze.
I have the MSA to thank for introducing me to the world of anaesthesia and their pearls of wisdom in the mindset and approach to the exam – charm, composure and concern for the examiners. My advice to future trainees would emphasise this and to enjoy the trip to London as much as possible; you have worked hard and owe it to yourself to go into the exam with a fresh mind and give your best performance.
Acknowledgements: Kirstie Gray and Mersey School of Anaesthesia
Kristianne Jones
CT2 Anaesthetics, Mersey Deanery
Trainee & Communications Liaison Officer, Mersey School of Anaesthesia
Twitter: @kristiannejones
The Association of Anaesthetists will award the Wylie Medal to the most meritorious essay on this year’s topic: How can we address the gender gap in anaesthesia, as well as medicine in general? written by a medical student at a university in Great Britain or Ireland.
Prizes of £500, £250 and £150 will be awarded to the best three submissions. The overall winner will receive the Wylie Medal in memory of the late Dr W Derek Wylie, President of the Association 1980-82.
For further information and to apply please visit our website: https://anaesthetists.org/Home/Get-involved/Grantsawards-and-prizes/Wylie-Undergraduate-Essay-Prize or email secretariat@anaesthetists.org
Applications for funding towards a medical student elective period taking place between April and September 2023 are invited from medical students studying in Great Britain and Ireland (subject to confirmation of eligibility).
Preference will be given to those applicants who can show the relevance of their intended elective to anaesthesia, intensive care or pain relief. A key focus of the Association is support for projects in the developing world, hence elective placements supporting work in developing countries are given priority.
For further information and to apply please visit our website: https://anaesthetists.org/Home/Get-involved/Grantsawards-and-prizes/Undergraduate-Elective-Funding or email secretariat@anaesthetists.org.
Closing date for applications: 18 January 2023
Only those who have gone through these exams will truly appreciate what that statement means! The hugs and handshakes you receive from colleagues when they congratulate you are littered with unspoken communication: “I feel the pain you’ve been through and I feel your relief!”
If the RCoA want the exam to be a rite of passage, we should congratulate them on achieving this aim. So how did I manage revision, life, children and work? Here are my tips; I hope you find them useful…

My CT1 year started with three months of anaesthetics, then nine months of maternity leave. My first child was eight months old when I started revising for the Primary. I tried to revise, return to work and manage home life with a baby, coming up to winter. This was never going to end well! As the onslaught of winter bugs arrived, revision time dwindled and so did my morale. The best advice I received was to stop – so I did! Whether it’s babies or something else, plan for quiet.
I started revising again in spring. This was better – less bugs meant more sleep. My clinical confidence was improving, allowing me to turn to books. My first child was two years old when I passed the Primary. When it came to the Final, I had learnt from past experiences: I started revising eight months before the exam at the start of spring!

I have a lovely non-medic husband. This helped when coordinating childcare but posed a challenge when finding study time, so we negotiated and agreed terms. Every week I would stay late twice to study. Another day I would drag myself out of bed at 5.30 A.M. and go in early to study (madness I know!) He would occupy the kids for one weekend day until around 2.00 P.M., then normal family life would resume.
My mum helped a lot during Primary; she had just the one grandchild, so depending on her was easy. By the time the Final came around she had five grandchildren, and so we bit the financial bullet. Full-time nursery it was – this enabled me to be mum at the weekend without having a nervous breakdown about not finding enough study time.
My family understood that I needed to give it my all. And that’s how we went forward, as a team. United in our desire to pass.
The syllabus is too wide and too deeply examined to wing it by cutting corners. I strongly advocate starting early.
What I will say is that 30 minute chunks got me through both exams. When you are shattered just say “Okay 30 minutes, learn one thing”. You’ll find a few 30 minute chunks a day – for me it was lunchtime, waiting for meetings, sitting outside the kids rooms at bedtime. I stopped folding the washing, that became my husband’s job.
This is REALLY important. For the Primary I found three great people while revising for the OSCE/ viva. If you’re a lone worker that’s fine, but this is a talking exam so find people to revise with if you can.
For the Final (I’m about to get super mushy so bear with me), I found three different friends. We revised together for the written. Once every few weeks we’d meet after work and teach each other core topics. It started in May and finished in December. I can safely say I love these three and they know it. The support and knowledge we have shared is unparalleled from anything I have experienced before – it was like we were trapped in a bunker fighting for survival, and on that fateful day in December when we all passed… we were freed! We will forever be pals based on the experience. Ok I’m done –dramatics over with! Find good people.
Talk to podcasts, yourself, animals. People will offer viva practice – those that don’t just hand them a book and they’ll test you, if they don’t they’ll send you off to find someone who will. I even taught my five-year old about mechanisms of extravasation injury on the train to Legoland (remember 30 minute slots)!
I’m in the Northern Deanery and I am going to shout about it from the rooftops. What an ace place to work. We have great consultants, supportive, accommodating, understanding and helpful people. My fellow trainees are wonderful – giving up their time to teach, viva practice, share resources or just offer words of wisdom.
There will be dark times, times you feel you don’t deserve it, times you’ll believe you are never going to know enough, times you feel like a failure. Take solace in the fact that if you feel this rubbish you’re probably working hard enough.
Keep it in perspective on the last lap, as the bell rings. This drove me mad when people said it… but it’s true.
One of my study pals said she was envious of my home situation!!! “Eh?!” I exclaimed. She replied “You have a part of your life more important than these exams, when you go home you don’t have time to stew cause you’re in ‘mummy mode’ ” She didn’t have that luxury. (study pals = good people!) When you’re stressed and it’s too much, look at your little monsters, be grateful for your mandatory off-switch!
I really thought I would never get through the final and considered pulling out a month before the viva. My revision wife and my real life husband emotionally blackmailed me into sitting it –I’m glad they did. Even if I hadn’t passed it was worth a shot.

This exam is really quite like giving an anaesthetic, it’s all in the preparation, timing and team around you. Good luck to those sitting it – I’ve got my fingers, toes, legs and arms crossed for you. I understand what it means, and although you cannot pass this exam on luck alone I’m not daft enough to ignore that you need a bit of luck too.
Selena Sehgal
ST4 Anaesthetic Trainee
Royal Victoria Infirmary, Newcastle
Twitter:
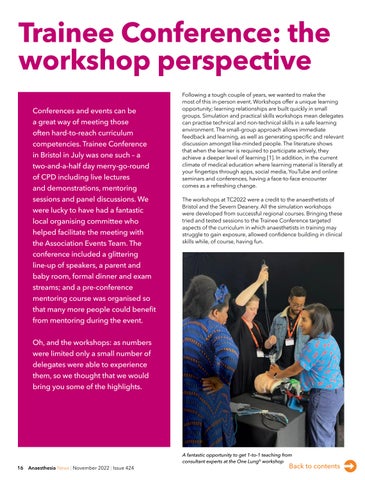
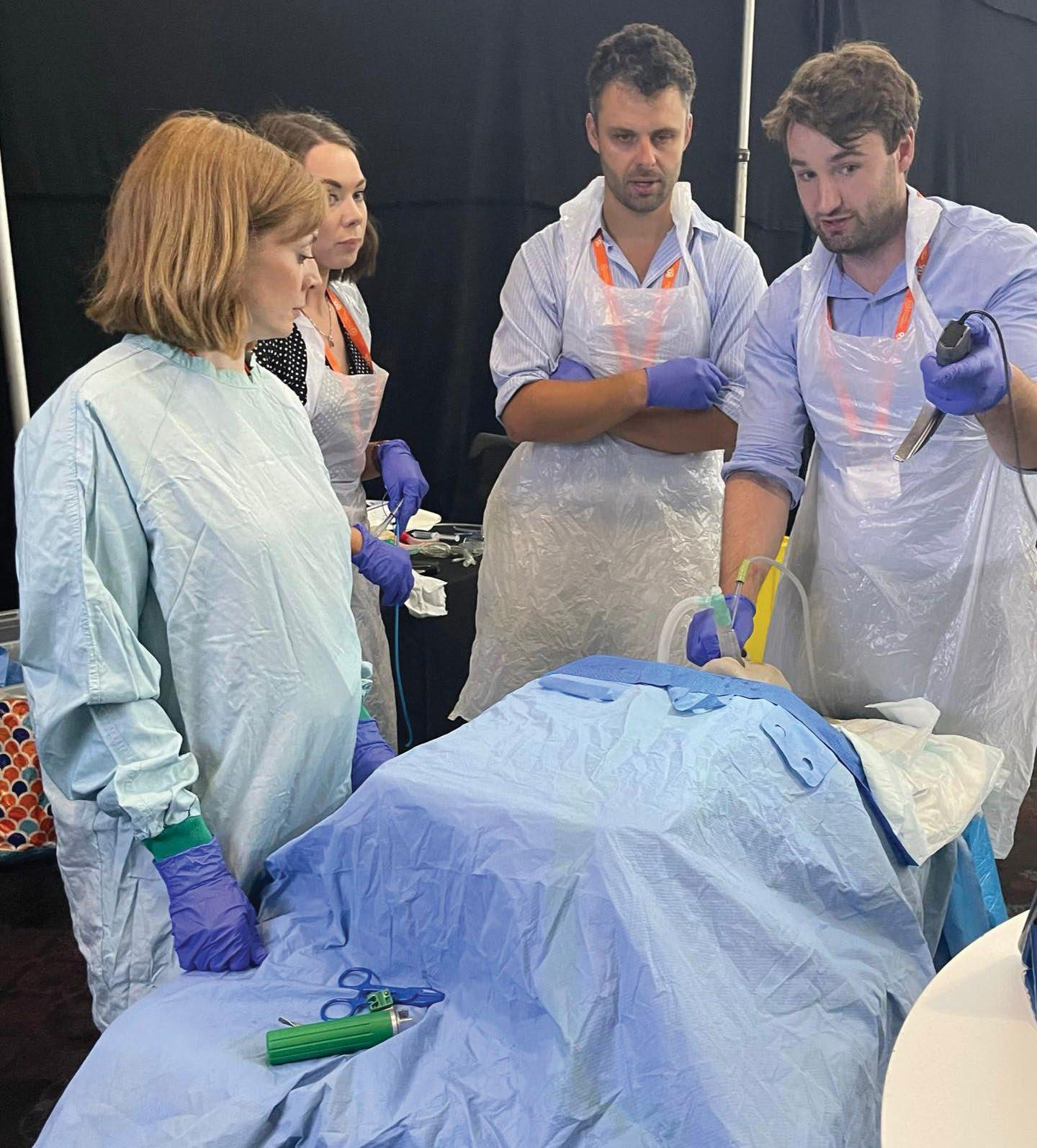
Conferences and events can be a great way of meeting those often hard-to-reach curriculum competencies. Trainee Conference in Bristol in July was one such – a two-and-a-half day merry-go-round of CPD including live lectures and demonstrations, mentoring sessions and panel discussions. We were lucky to have had a fantastic local organising committee who helped facilitate the meeting with the Association Events Team. The conference included a glittering line-up of speakers, a parent and baby room, formal dinner and exam streams; and a pre-conference mentoring course was organised so that many more people could benefit from mentoring during the event.
Oh, and the workshops: as numbers were limited only a small number of delegates were able to experience them, so we thought that we would bring you some of the highlights.

Following a tough couple of years, we wanted to make the most of this in-person event. Workshops offer a unique learning opportunity; learning relationships are built quickly in small groups. Simulation and practical skills workshops mean delegates can practise technical and non-technical skills in a safe learning environment. The small-group approach allows immediate feedback and learning, as well as generating specific and relevant discussion amongst like-minded people. The literature shows that when the learner is required to participate actively, they achieve a deeper level of learning [1]. In addition, in the current climate of medical education where learning material is literally at your fingertips through apps, social media, YouTube and online seminars and conferences, having a face-to-face encounter comes as a refreshing change.
The workshops at TC2022 were a credit to the anaesthetists of Bristol and the Severn Deanery. All the simulation workshops were developed from successful regional courses. Bringing these tried and tested sessions to the Trainee Conference targeted aspects of the curriculum in which anaesthetists in training may struggle to gain exposure, allowed confidence building in clinical skills while, of course, having fun.
A fantastic opportunity to get 1-to-1 teaching from consultant experts at the One Lung© workshop

The One Heart Course©: introduction to cardiopulmonary bypass and One Lung©: an introduction to lung isolation techniques offered excellent ‘hands-on’ experience in these complex specialities. The Transport of the critically ill patient workshop, run by experienced pre-hospital anaesthetists, obviously ticked the fun box as delegates rushed up and down the corridors of the conference centre pushing their ‘patient’, but also managed to cover areas of the curriculum where supervised experience is difficult to gain. Major obstetric haemorrhage, Managing emergencies in paediatric anaesthesia and Airway emergency simulation targeted building confidence in managing difficult situations that all anaesthetists will encounter at some point in their career. More specifically aimed at developing essential non-technical skills was Hot Huddles: introduction to a peer support model following difficult events at work. This workshop, described as ‘inspiring and thought provoking’, highlighted the appetite for evidence-based ways of managing challenging events at work, managing our mental health and developing resilience.

Overall the workshop element of the conference was a resounding success, with a median feedback score of 8.5 out of 10. Delegates seemed to really enjoy the hands on, simulation and team building aspects of the workshops. There were some comments that pitching to a varied audience was sometimes difficult, and that some of the workshops were a little pressed for time. This feedback is something we will certainly address going forward; however, as in previous years the workshop format continues to be a success, and will be a feature of future Trainee Conferences – perhaps even expanded to give more delegates the chance to benefit from these fantastic learning opportunities.
Acknowledgements: the Trainee Committee would like to thank the Local Organising Committee (Francesca Millenchamp, Amy Dodd, Anne Kendall, Melanie Cockroft, Toby Shipway and Victoria Male) for all their hard work and dedication to TC2022 –we could not have done it without you!
We would like to thank the following Bristol anaesthetists for their time and expertise in running the workshops: Dr Elizabeth Hood and the One Lung© team; Dr Matthew Bell and the One Heart Course© team; Dr Claire Abeysekera and the Managing Emergencies in Paediatric Anaesthesia team; Dr David Luther and the Novice Obstetric Course team; Dr Heather Rodgers and the Transport of the Critically Ill Patient Course team; Dr Joe Greenhill and Dr James Peters and the Novice Anaesthetist Course team; Oonagh Koppel and Maria Clare, the Hot Huddles team.
A huge thank you to the University Hospitals Bristol and Weston Bristol Medical Simulation Centre (BMSC) who supported the conference with a huge amount of simulation kit and staff; also thank you to Dräger and Hamilton Medical who lent medical equipment to allow us run high fidelity simulations.



Lead, Local Organising Committee, Trainee Conference 2022
Naomi Freeman Chair, Trainee Committee, Association of Anaesthetists
References
1. Belay HT, O’Ruairc B, Guerandel A. Workshops: An important element in medical education. British Journal of Psychiatric Advances 2019; 25: 7-13.
In our trust each scavenging unit uses an average of 1.5 kW energy per hour, the equivalent of running a dishwasher. There are 15 of these units running throughout our various theatre suites, so that’s 15 dishwashers running 24/7 - a whopping £8952 per year, and 60.8 tCO2e (metric tons CO2 equivalent; Table 1) [1] – the equivalent of jumping in a car and driving around the equator over six times (a few times more if one has already gone electric) [2]!
We only really need the emergency theatre and the obstetric theatre to run 24/7. If those scavenging units were kept on all the time, and we kept the one for the trauma theatre on 8:0020:00 seven days a week and the rest of the theatres from 8:0018:00 Monday to Friday, we could save £4622.11 or 42 tCO2e! Fuel prices are rising so we anticipate even greater savings to be made in the future (Table 1).
We have been trying to encourage all our theatre staff to think about turning off the scavenging at the end of the list. We have recently analysed our practice; currently we’re managing it 40% of the time, which means a saving of £1849 compared with the possible saving of £4622, so there is plenty of room for improvement. We think that with further education, and posters to remind staff, we can improve on this. There is a risk of the scavenging not being turned on the next day, but a thorough anaesthetic machine check in the morning should avoid this.
With significantly rising energy costs and the impact of climate change, cutting down power consumption is hugely important. With such large costs associated with the energy costs of scavenging, it may now be worth the investment in switching to volatile capture technology. This would not only have the potential to save money but reduce the harmful effects of anaesthetic gases on the environment. Once we have addressed the major problem of unnecessary scavenging, the next area for attention might be to turn off unused appliances and lights.
Electricity (KwH) 208,926 88,620 120,306

Cost March 2022, (5.14p/kWH day; 3.43p/kWH night) £8952 £4330 £4622
Potential future cost, (25p/kWH day 20p/ kWH night) £47,008 £21,498 £25,510
1. GOV.UK. Greenhouse gas reporting: conversion factors 2021, 2022. www.gov.uk/government/publications/greenhouse-gasreporting-conversion-factors-2021 (accessed 14/9/2022).
2. United States Environmental Protection Agency. Greenhouse gases equivalencies calculator– calculations and references, 2022. www.epa.gov/energy/greenhouse-gases-equivalencies-calculatorcalculations-and-references#miles (accessed 14/9/2022).
Scavenging is something that we just take for granted. It’s on the anaesthetic machine, we check it’s on in the mornings and it helps to stop the theatre team falling asleep. But why is it always on?
Following the success of previous national RAFT (Research and Audit Federation of Trainees, www.raftrainees.org) projects, including iHype (Intraoperative Hypotension in the Elderly) and DALES (Drug Allergy Labels in Elective Surgical population), RAFT will soon be undertaking its fourth national research project, the POPPY study: Patient reported Outcomes, postoperative Pain and Pain relief in day case surgery. This snapshot observational study aims to measure patient-reported outcomes in UK day case surgery patients. This includes capturing the short-term outcomes of quality of recovery, pain severity, and analgesic use. It will also look at the long-term outcomes, including the incidence of persistent post-surgical pain and persistent postoperative opioid use, which have not been investigated previously in the UK day case population.
In 2021, anaesthetic trainees from SWARM (South West Anaesthetic Research Matrix, www.ukswarm.com) were successful in having their idea for the next project accepted by the RAFT panel in a national competitive process. Since winning the pitch proposal, SWARM have developed the project alongside the RAFT committee, University Hospitals Plymouth research team, pain specialists, statisticians and lay members. This allowed evolution of the topic selection, development of the protocol and widening the scope to include patientreported outcomes. Long-term follow up will use an innovative automated text message system to collect outcome data after hospital discharge. This is a novel method for postoperative follow up at this scale, and a first use in national trainee-led research, expanding the scope of this and future projects. We will run a qualitative study alongside the quantitative study, looking in detail at the peri-operative experiences of a subgroup of patients from the main study who report persistent problems after their surgery. We have been granted research funding from the NIAA and University Hospitals Plymouth charitable research fund.
Currently, approximately 70% of operations in the NHS are carried out as day cases [1], with patients considered to be suitable having increasingly complex comorbidities. It is
therefore important to understand the different short- and long-term trajectories of recovery. Patients undergoing day surgery will often have variable or no planned follow up, resulting in significant negative outcomes going unrecognised. There is increasing evidence that day case patients commonly develop long-term health problems following surgery, including persistent post-surgical pain [2]; pain continuing beyond three months postoperatively is common with up to 18% of surgical patients suffering long-term moderate to severe pain [3]. Inappropriate long-term opioid use after surgery from mismanaged persisting pain or opioid misuse disorder is a major public health concern, with 6% of opioid-naïve patients in the USA using opioids persistently [4]. Discharge opioid prescriptions are frequently not patient or procedure-specific, and over-prescription is a serious concern [5-6]. Persistent post-surgical pain and persistent postoperative opioid use are significant problems in day case patients, but information about the UK population is lacking.
Planning is underway to run an embedded pilot of the project in early 2023 and then to open nationally in mid- to late 2023. The POPPY study spans peri-operative medicine, pain medicine and day case surgery, thus appealing to many trainees across all sites. As with previous RAFT studies, trainees at each site will be
invited to undertake recruitment and engage in data collection on the day of surgery. This will offer an opportunity for trainees to develop research skills, while also helping address the new RCoA curriculum research requirements. Our study aims to help inform surgical, anaesthetic and prescribing practices that have an impact on short-term recovery, which could reduce the risk of developing both persistent post-surgical pain and persistent postoperative opioid use.
For more information email plh-tr.poppystudy.raft@nhs.net or website www.RAFTrainees.org
Matthew EversonCo-Investigator for POPPY Study, SWARM Fellow Registrar in Anaesthesia and Intensive Care Medicine, Royal Devon University Healthcare NHS Foundation Trust, Exeter
William Hare
Co-Investigator for POPPY Study Registrar in Anaesthesia, University Hospitals Plymouth NHS Trust, Plymouth Anna Ratcliffe
Co-Investigator for POPPY Study, SWARM Chairperson Registrar in Anaesthesia, University Hospitals Plymouth NHS Trust, Plymouth
Mark Rockett
Chief Investigator for POPPY Study Consultant in Anaesthesia, University Hospitals Plymouth NHS Trust, Plymouth
Twitter: @RAFTrainees
References
1. GIRFT Getting It Right First Time. National Day Surgery Delivery Pack, 2020. https://www.gettingitrightfirsttime.co.uk/bpl/day-surgery/ (accessed 20/9/2022).
2. Hoofwijk D, Fiddelers AAA, Emans PJ, et al. Prevalence and predictive factors of chronic postsurgical pain and global surgical recovery 1 year after outpatient knee arthroscopy: a prospective cohort study. Medicine 2015; 94: e2017.
3. Johansen A, Romundstad L, Nielsen CS, Schirmer H, Stubhaug A. Persistent postsurgical pain in a general population: prevalence and predictors in the Tromsø study. Pain 2012; 153: 1390-6.
4. Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surgery 2017; 152: e170504.
5. Delaney LD, Gunaseelan V, Rieck H, Dupree JM, Hallstrom BR, Waljee JF. High-risk prescribing increases rates of new persistent opioid use in total hip arthroplasty patients. The Journal of Arthroplasty 2020; 35: 2472-9.
6. Daliya P, Adiamah A, Roslan F, et al. Opioid prescription at postoperative discharge: a retrospective observational cohort study. Anaesthesia 2021; 76: 1367-76.
Month prize
be
of the
events. The


of the
cash alternative
be
for 12 months.

New England Journal of Medicine 2018; 379: 711-721.
There is limited evidence for the safety and efficacy of adrenaline (epinephrine) as a treatment in out of hospital cardiac arrest (OOHCA). Adrenaline has potential benefit by increasing aortic diastolic pressure, thereby augmenting coronary blood flow [1]. However, potentially harmful effects include increased myocardial oxygen demand and platelet activation leading to thrombosis and impaired microvascular flow, thus increasing cerebral ischaemia [2-4]. A previous large observational study reported higher rates of return of spontaneous circulation but worse neurological outcomes with adrenaline [5]. The current placebo-controlled trial sought to determine if the administration of adrenaline in OOHCA is beneficial or harmful.
A double-blind trial involving 8014 patients with OOHCA across five ambulance trusts in the UK randomly allocated 4015 patients to receive parenteral adrenaline and 3999 patients to saline placebo, alongside standard care. The primary outcome was survival at 30 days. The study also measured rate of survival until hospital discharge with a favourable neurological outcome. Favourable neurological outcome was defined as a score of < 3 on the Modified Rankin Scale.
Survival at 30 days was 3.2% in the adrenaline group compared with 2.4% in the placebo group (unadjusted odds ratio for survival 1.39; 95%CI 1.06-1.82; p = 0.02). There was no evidence of a significant difference in the proportion of patients who survived until hospital discharge with a favourable neurological outcome (2.2% versus 1.9%; unadjusted odds ratio, 1.18; 95%CI 0.86-1.61). However, at the time of hospital discharge severe neurological impairment had occurred in more of the survivors in the adrenaline group than in the placebo group (31.0% versus 17.8%).
The use of adrenaline in patients with OOHCA resulted in a significantly higher survival rate at 30 days when compared with placebo. There was no significant difference between groups in the rate of favourable neurological outcome as more survivors had severe neurological impairment in the adrenaline group.
This is a pragmatic, well-delivered trial with the largest set of randomised data on this subject to date. It suggests that adrenaline improves 30-day mortality in OOHCA, however this may be at the cost of worse neurological outcome. While there was good internal validity due to rigorous methodology with clinical patient-centred outcomes, the primary outcome of the study was mortality, not neurological outcome; therefore, the power to detect meaningful differences in this important secondary outcome was low.
The study highlights the poor overall survival rates for OOHCA and contextualises the potential benefit of adrenaline for survival against other treatments in the chain of survival, suggesting that improving access to defibrillators and early CPR offer the greatest benefit for survival.
Rory Cullen SHO, Craigavon Area HospitalReferences
1. Perkins GD, Cottrell P, Gates S. Is adrenaline safe and effective as a treatment for out of hospital cardiac arrest? British Medical Journal 2014; 348: 2435.
2. Callaway CW. Epinephrine for cardiac arrest. Current Opinion in Cardiology 2013; 28: 36-42.
3. Larsson PT, Wallén NH, Egberg N, Hjemdahl P. Alpha-adrenoceptor blockade by phentolamine inhibits adrenaline-induced platelet activation in vivo without affecting resting measurements. Clinical Science (London) 1992; 82: 369-76.
4. Ristagno G, Tang W, Huang L, et al. Epinephrine reduces cerebral perfusion during cardiopulmonary resuscitation. Critical Care Medicine 2009; 37: 1408-15.
5. Loomba RS, Nijhawan K, Aggarwal S, Arora RR. Increased return of spontaneous circulation at the expense of neurologic outcomes: is prehospital epinephrine for out-of-hospital cardiac arrest really worth it? Journal of Critical Care 2015; 30: 1376-81.







Implementing nitrous oxide cracking technology in the labour ward to reduce occupational exposure and environmental emissions: a quality improvement study
Pinder A, Fang L, Fieldhouse A, et alThe environmental impact of anaesthesia is rightly an increasing concern for our speciality, but the imperative to reduce our carbon footprint must be balanced against the need to maintain high quality patient care and excellent patient experience. At the forefront of this balancing act are concerns around the use of nitrous oxide in the delivery suite. This potent greenhouse gas accounts for more than 10 times the combined environmental damage of volatile agents. Rather than restricting the use of nitrous oxide in
labour, the authors have demonstrated in this study that its environmental effects can be minimised through innovation. Using a ‘cracking’ device, which takes exhaled nitrous oxide and converts it to nitrogen and oxygen, ambient nitrous oxide levels were reduced by up to 80%. Midwives reported finding the device easy to use and parturients were highly engaged during the study. This device represents an elegant solution to a significant problem. Expect it to appear on a delivery suite near you in the near future.
Judd L, Hof L, Beladdale L, et al.
The majority of blood transfusion guidelines now recommend a restrictive approach to transfusion; in particular, the routine transfusion of single units of blood is encouraged, as encapsulated in the Canadian transfusion campaign maxim “Why give two when one will do?”. This principle appears to have been adopted in Germany where the authors conducted a retrospective observational study of anaemia in more than 23,000 patients across a 12-year period from 2007-2019. Their primary
outcome was overall prevalence of anaemia, which has reduced only marginally from 37% to 35%. However, transfusion rates per 1000 patients have more than halved. The authors attribute this, in part, to a decrease in the number of two-unit transfusions while single unit transfusion rates have remained constant. Furthermore they conclude that, with no increase in mortality over the same period, a more restrictive approach to transfusion is likely to be safe for most patients.
The authors developed a scoring system for anaesthetic complexity that encompasses several variables having an impact on overall difficulty of a case, such as blood loss, airway issues and communication difficulties. In 688 patients undergoing surgery, the anaesthetist was asked to decide what grade of anaesthetist was most appropriate for the case. This information was used to validate the OxAnCo score calculated for the patient. The scoring system was excellent at predicting the need for
consultant input, as well as which cases could be performed by more junior anaesthetists. The authors suggest that OxAnCo scoring would allow caseloads to be matched more effectively to the anaesthetic workforce, including physician assistants. With ever-growing waiting lists and an impending workforce crisis, all suggestions for increasing efficiency are surely welcome. More work is needed to understand the impact of this tool and its role in workforce management.
Louise Savic, Editor, Anaesthesia

Send your letters to: The Editor, Anaesthesia News at anaenews.editor@anaesthetists.org
Please see instructions for authors on the Association's website www.anaesthetists.org
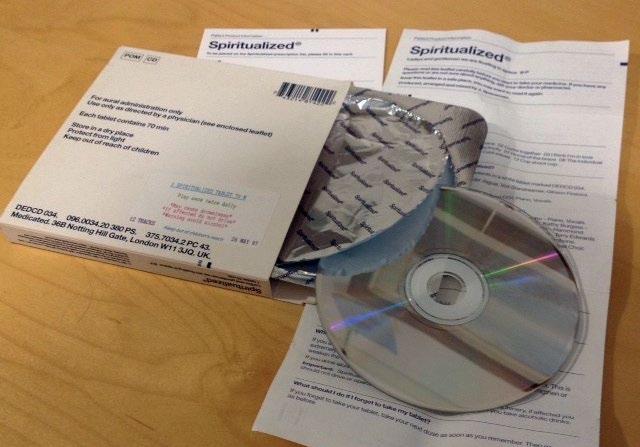
Dr Aitken's letter in the August issue [1] described her discovery of a T-shirt emblazoned with a strange device (recognisable to the initiated as an intravenous cannula) promoting the band Spiritualized. Dr Aitken may not be aware (as I wasn't) that this is not the only indication of the band's fascination with things medical.
Having shown Dr Aitken's letter to my husband, imagine my surprise when he promptly disappeared to his shelves of CDs. On his return he presented me with a cardboard box a little larger than a standard CD case. It appeared to contain a prescription medicine from "Spiritualized®" called ‘Ladies and Gentlemen we are floating in Space’ containing one 70 minute tablet. Turning it over I found the warning ‘For aural administration only'. Use only as directed by a physician (see enclosed leaflet). Each tablet contains 70 min Store in a dry place. Protect from light. Keep out of the reach of children.’ A stick-on label instructed that it be played once twice daily and warned that it might cause drowsiness (‘If affected do not drive’) and to avoid alcohol.
A 16-year-old male patient underwent a left zygomatic arch reduction on the emergency theatre list under general anaesthesia, with airway maintenance using a size 4 single use-reinforced integral silicone laryngeal mask (Fannin, Dublin, Ireland).
On waking in the recovery ward, the patient bit through the shaft of the laryngeal mask (Figure 1). The staff attempted to remove the device by pulling the shaft, but this resulted in exposure and unravelling of the metal reinforcing wire which became caught around the patient’s lower teeth and braces. The attempt to remove the laryngeal mask was then stopped until the patient was awake enough to open his mouth voluntarily, when disentangling of the wire and complete removal of the device was successful.

It is accepted clinical practice for patients to be transferred unconscious to the recovery ward with a supraglottic airway still in situ, to be removed by appropriately trained recovery staff [1]. A bite block is sometimes inserted when a laryngeal mask is to be retained until the patient is awake, but was not used in our case. It is important for anaesthetists to be aware that laryngeal masks are not bite-proof, and that complications including airway obstruction may occur during biting.
Esme Brittain
FY1 in Anaesthetics/ Intensive Care Medicine
Thomas Liddell-Lowe
FY1 in Anaesthetics/ Intensive Care Medicine
Jonathan Dauncey
ST3 in Anaesthetics
Consultant Anaesthetist
Murthy Varanasi
Inside, I discovered a blister pack containing a CD and a folded patient product information leaflet. The headings included ‘What are the active ingredients of Spiritualized tablets?’ (crediting the contributors) and ‘What is Spiritualized used for?’ (‘To treat the heart and soul’). More detailed research on Wikipedia has revealed that the band have produced at least one other album making use of pharmaceutical style packaging, as well as one entitled ‘Songs in A&E’. My husband tells me that he took the medicine regularly from its release in 1997 but has only occasionally resorted to it in the last 20 years. I fear that I may have provoked a relapse.
Diana JolliffeRetired Consultant Anaesthetist, Northampton
References
1.
Congratulations to Diana Jolliffe for winning November's Letter of the Month prize.
Speciality Doctor in Anaesthetics
Prince Charles Hospital, Merthyr Tydfil
References
1. Gataure PS, Latto IP, Rust S. Complications associated with removal of the laryngeal mask airway: a comparison of removal in deeply anaesthetised versus awake patients. Canadian Journal of Anaesthesia 1995; 42: 1113-6.