A home away from Seniors get a chance to bloom































































































A home away from Seniors get a chance to bloom






























































































Welcome to the latest edition of Health Matters.
We speak to new HSE CEO Bernard Gloster as he takes the reins. He outlines his vision and hopes for the next five years and talks to us about 'Mrs O'Neill' the fictional patient that he keeps in mind during the course of his work. He reminds staff not to lose sight of those individuals such as Mrs O'Neill in case we get desensitised to their needs and wants.
Again we get an update on the new health regions that are quickly beginning to take shape. The transition has already begun and it will be completed in 2024.
At the heart of the new health regions is integrated care and allowing patients and service users to access health services more easily, no matter where they live. It also makes it easier for our staff to deliver more joined-up care. We take a look at a number of projects from around the country that are already delivering this integrated care, to the benefit of patients and staff.
In this edition, we also hear from Gráinne Cunningham O'Brien, new HSE Confidential Recipient. She explains how her role is to be 'a voice, an advocate and speak up and out for vulnerable adults with a disability and older people'.
More areas around the country became 'Healthy Communities', the Sláintecare programme that has targeted 19 deprived areas to give them the support they need to boost their health and wellbeing. It is an incredible programme that is tackling the many health inequalities in our communities.


They are just a small number of the many stories we have for you this edition.
Once again, a big thank you to all the teams around the country who have submitted their initiatives and programmes. It is great to be able to showcase the amazing work being done to make life better for people who use our services.
Joanne Weston EditorYvonne Costello Ann McLoone
Amy O'Neill
Frances Plunkett
Shane Larkin
Paddy Crosse
Keeva Carpenter
Teenager Noah Winders has been honoured for his heroic e orts that saved the life of his friend by administering CPR to him during a basketball match.

The Castleknock teen, who is fully trained in CPR, carried out chest compressions on his teammate Charlie Rutter until the arrival of the emergency services during the incident at St Vincent’s Basketball Club in Glasnevin in 2022.
Almost a year on, Charlie has had an internal defibrillator fitted and has come through his mock Junior Certificate exams and is doing well.
Charlie’s mother Fionnuala explained, “I dropped Charlie o for training at St Vincent’s Basketball Club at 9am. Charlie had started the warm up, running up and down the hall. He fell over and it was thought that he had tripped. He was helped up and he continued, but he fell over again.
“Charlie’s coach Dave Winders (Noah’s dad) started CPR and then Noah, who is fully trained in CPR, took over and continued until a Dublin Fire Brigade crew arrived and treated Charlie with an Automated External Defibrillator.”
In March of this year, the National Ambulance Service (NAS) presented Noah with a special Bravery Award in recognition of the courage he showed while rescuing his friend. The 16-year-old student of St Vincent’s in Castleknock received his CPR experience while training to be a lifeguard, and those who attended the incident were impressed with his calm and brave response and wanted to acknowledge this with a certificate of bravery.
Amanda Ross, Community Engagement O icer, NAS, who made the presentation, said, “It is important to recognise that young people in their teens can very e ectively administer CPR, especially when they have received the appropriate training. We would encourage any young person interested to avail of CPR training opportunities.”
The NAS Community Engagement Team delivers CPR training in schools, as well as supporting the Irish Heart Foundation’s CPR for Schools initiative around the country. Training is also available from voluntary Community First Responder groups.
Kidney transplant patients hail new programme run by TUH as a boost to both their health and their happiness

11%
The percentage of patients in the Irish health system a ected by chronic kidney disease
Kidney transplant recipients have praised a transformational new lifestyle programme at Tallaght University Hospital (TUH).

Those who attended the new diet and exercise classes at TUH say it not only improved their overall physical health, but also boosted their confidence.


Sarah Williams, who is 14 years post kidney transplant, said the new programme came ‘at a time when I needed it most for my physical and mental health’.


“It has been great, the combination of exercise and nutrition is so important. I have even started sea swimming. I am more confident and the regular checks with the team in TUH, help keep me on my toes,” said Sarah.









Brendan O’Brien had a kidney transplant over 12 years ago.
“The new diet and fitness programme for kidney transplant patients run by Tallaght University Hospital is smashing and I am sticking to it. This is the first time I have ever tried something like this. It is a challenge but the benefits are so worth it. My vitals are improving,” he said.
Francis Davis, five years after his own kidney transplant, said, “I am feeling much better both physically and mentally and have more confidence since taking up the new diet and fitness programme. The support from the team is so important and the programme gets you right back into proper habits. I am now walking and swimming and feel so much better now.”
These are the second group that have completed the new programme. The eight-week virtual classes took place online twice per week and included both an exercise element led by a physiotherapist and an education session led by a dietitian.
Oonagh Smith, Clinical Specialist Renal Dietitian at TUH, explained, “The healthy eating element of the programme took the form of a 15 to 20 minute discussion at the start of each online session. As part of this, participants were encouraged to ask any nutrition-related questions, with a di erent topic discussed each time, for example what constitutes a healthy diet for kidney disease, as well as menu planning and behaviour change techniques.”
Cliona Barrett, Senior Renal Physiotherapist, TUH, outlined the part that physical activity plays in the programme.

“The fitness classes comprised of both aerobic and strengthening exercises and took place virtually for 45 minutes, twice per week. The exercise section was adapted to patients’ home environment, where no equipment was required except for resistance bands for strengthening exercises. They worked to a moderate intensity level during the class,” she said.
Simon Appleby, who is nine years post kidney transplant, said that he can see a marked improvement in himself following participating in the programme.
“This was the first time I had done something like this, the programme was great. The focus on diet and fitness means I am a lot healthier than I was and can do a lot more. It also gave me the confidence to try up new things and I have taken up yoga and am doing a lot more walking. I can see a marked improvement,” said Simon.
Keith Armstrong is barely a year after his kidney transplant but the lifestyle programme has been a major boost for his fitness levels.

“I learnt all about keeping fit and healthy and can push myself a lot further now. I don’t get so out of breath and am getting out more. I have taken up wheelchair rugby and have gone back to college,” he said.



Consultant nephrologist Professor Peter Lavin, who is also the lead clinical director at TUH, says, “Chronic kidney disease a ects over 11% of patients in the Irish health system. There are currently 5,000 adults and children requiring treatment by dialysis or kidney transplantation in Ireland. This is an increase of nearly 50% in 13 years. I want to compliment the renal team at TUH for introducing this important initiative. It is showing real benefits not just for the physical but also the mental health of our patients.”
250 organ transplants took place in Ireland in 2022. The figure includes kidney transplants from 33 living donors. 163 kidney transplants in total were completed last year.
“The new diet and fitness programme for kidney transplant patients run by Tallaght University Hospital is smashing and I am sticking to it."Top: Oonagh Smith, Clinical Specialist Renal
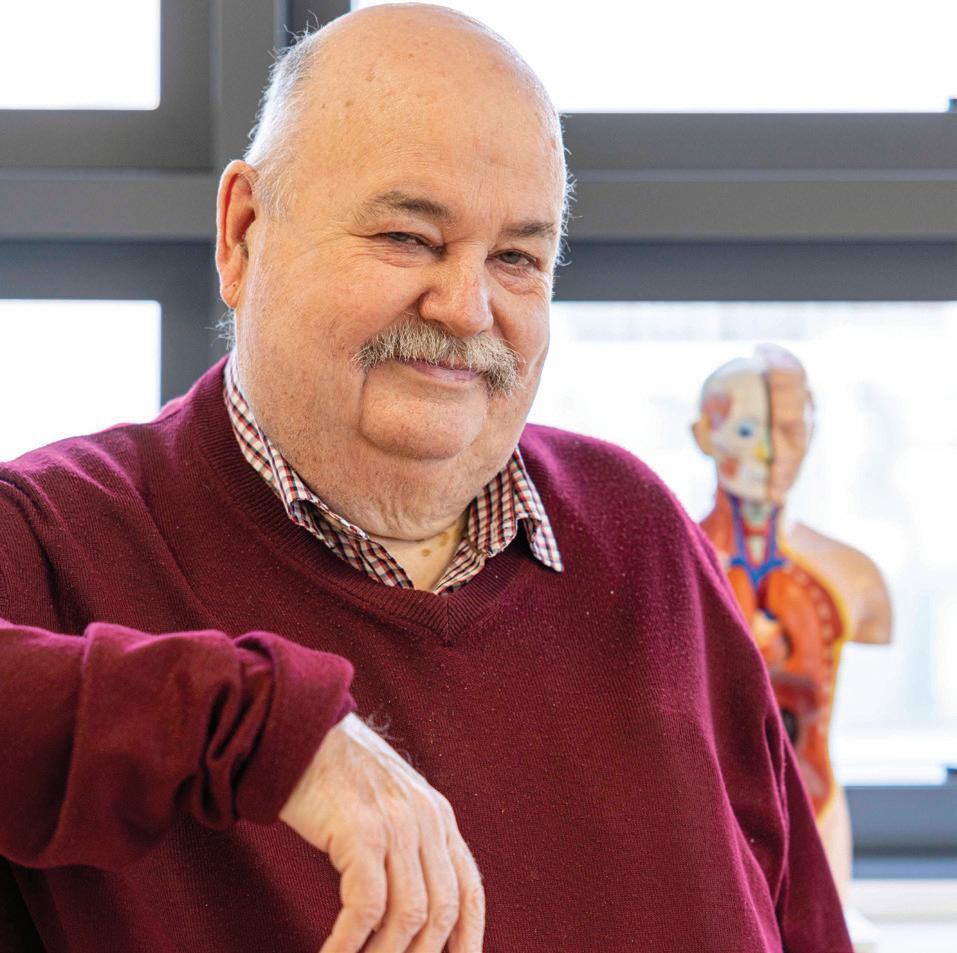
Bernard Gloster says the importance of simple kindness cannot be underestimated

Since starting his new role as HSE CEO, Bernard Gloster has asked all our staff to keep their thoughts on the people we care for; Mrs O’Neill is a persona he uses to bring that to life.

Mrs O’Neill is a 79-year-old old widow with two chronic health conditions, and your typical HSE service user.
“I always think about Mrs O'Neill. She wants simple and accessible health services, and particularly from health service providers who talk to each other. Not a big ask for Mrs O'Neill. But if we forget the importance of Mrs O'Neill and lose sight of that individual person, we can become a bit desensitised. We can become detached, and that's where we lose the empathy, and the kindness that is so important in all we do.”
Bernard has identified culture change as a priority and believes the importance of simple kindness cannot be underestimated.
“I see the need to change the culture as much as the structure. I'm not someone just focused on the structure that says, well, if I change the structure now, everything will be grand, it won't,” he said.
“Kindness is a huge part of our culture for me - and respect, which is probably a little bit different to kindness. Respect is more in the space of understanding everyone has a place or has a role and relevance.”
When he started in the CEO role on 6 March, Bernard outlined his three main priorities for the HSE: improving access, timely implementation and public confidence. He believes a change of culture can help achieve these goals.
“When we talk about access, it’s to the obvious ones, which is waiting lists and trolleys - and they require a lot of attention. But apart from the resources, the processes and the systems, we know there's a lot of people out there who just find that delay too hard and rightly so. So one of the things I'm trying to focus on is the attitude of the organisation towards access,” he said.
“For a person managing a theatre, it’s about the booking and the slots and so on. For a bed manager, it's nearly like magic trying to make it work. But I think we have to go wider than that. I think we have to go right across the whole system. You could be somebody working in an office that never sees the public. But you're obviously doing a job that's
an important part of the organisation. So if you get a freedom of information request from a member of the public or a subject access request for someone's personal information and I had a lot of experience with this in Tusla, with adoption and so on to that person, that access is as important as a clinical appointment or something else.
“I think if we change our view of the importance of access for the public, it'll be easier to change the process and it will be easier to maximise the resources we have. We won't make access perfect without more capacity, but my job first and foremost, is am I using the capacity as well as I can.”
Speaking about timely implementation, he admitted, “We don’t do implementation so well.”
“There are two things with implementation, we’re either too slow, which is the timely bit, or we’re inconsistent. So we do really well in Sligo but five years later, we're still talking about doing it in Limerick or Cork. So timely implementation and a consistent approach is the priority,” he said.
The new CEO said that building public confidence in the new system will be crucial.
“Public confidence for me is where really the judgement of public service is at. The public can't be 100% delighted with us all the time by the nature of what we do. But public confidence to me is not about not having problems. It’s about how mature we are as an organisation, in identifying a problem, being transparent about it, ensuring that the public know we are on top of it and we're resolving it and are making improvements.
“I don't think the public expect us to be perfect. Instead, they want us to be on our game, to be on top of our issues and to be constantly improving. We often get quite defensive about that and the story becomes about do we have a problem or not rather than making it better, so to me, that's what public confidence absolutely is about.”
Bernard is 35 years in the public service and he describes it as a career of two halves, the first as a social care worker, before moving on to management roles. He held several senior management positions including Chief Officer of HSE Mid-West Community Healthcare, and worked in or managed in both community and acute hospital operations. He joined Tusla as CEO in September 2019.
He is well aware he is taking on a job many would deem too overwhelming but he insists it is a privilege to get the opportunity to serve.
“Yes, this is a very difficult job. It's just enormous. But look at the privilege that's in that. I get to lead and manage and direct the entire response of the Irish Health Service for five million people,” said Bernard.
“I guess I saw a very similar challenge in the HSE with the culture to the one I saw when I went to Tusla. But I think what motivated me or maybe didn't make the job as daunting is I had seen what could be done with it, and what could be done by following the Practice, Culture, Structure line and following the three in step.”
“While people may say I'm very conservative in some ways, I believe I am actually quite disruptive in the way I approach change. I try not to allow myself to be taken off down rabbit holes of complexity.”
Of course, with the move to health regions, Bernard will also be overseeing one of the biggest structural changes the HSE has seen.
“If it's just about the structure it’ll have no real benefit,” said the HSE CEO.
“But there are two real potential benefits we can gain with the move
“Yes, this is a very difficult job. It's just enormous. But look at the privilege that's in that. I get to lead and manage and direct the entire response of the Irish health service for five million people."
to health regions. The first is integration and the ability to integrate at the right level locally. The second potential benefit, is appropriately decentralising. Right now, the centre is too top heavy and too controlling. It's impossible for people to make effective and timely decisions at local management level. At the same time, we have to have some common standards, particularly in clinical services, and we also need some controls. Without these there is a risk that every part of the country operates differently. So the opportunity is to redefine the centre that is appropriately supporting the six regions.”
He said he will be taking full advantage of the opportunity to have a better operational grip of the health service while he is changing it.

“I can't just say I'm here to change the structure. I have to run the service today because there has to be an immediate benefit to the public. I can't expect the public to wait for me to have six health regions in place. That's not going to make any difference to patients like Mrs O’Neill who are waiting today to have surgery.”
He urged staff not to be distracted by the incoming changes.
“What I've started to say to people is, don't wait for a regional CEO to be appointed. Don't wait for a health region that you think is going to change the world. It will certainly help but, actually, today you can have all the benefits of the region if you start to work in and behave in regional pods. So not just the chief officer in the community or the hospital group CEO. They already pretty much work together. But the Director of Estates, the Director of ICT, the different people who are
already in the region. They might be reporting nationally, they might be reporting five different ways,” he said.
“The challenge I’ve given to senior managers to come around the table today and start making collective decisions for the population they manage. If they do that, they'll start to get the benefit of a health region.”
Bernard himself is an active walker and particularly loves walking on the beach. He lives 40 minutes from Ballybunion beach at his Co Limerick home.

“Walking is great for my own head space,” he said, explaining how he manages his own work stresses.
He is determined to give the job his all and make sure he leaves with no regrets.
“I think ultimately the test of what success I have will be ‘have we made life better for Mrs O'Neill and people like her?’” he said.
“I've got under five years left in the job now, so I have to use that time well because I won't get that time again. I’ll have loads of time for myself – time to walk the beach, loads of time for hobbies when I am done. So I just want to use this time now for what it is and it is an amazing opportunity.”
“I've got under five years left in the job now, so I have to use that time well because I won't get that time again."
“The ‘Little Journey’ app was developed to help change the way children experience hospitals by empowering them and giving them the information they need to reduce their anxiety in a fun, interactive format.
A new virtual reality app helps children between the ages of three and 12 to prepare for surgery and allay their anxiety in advance of their hospital stay.
The ‘Little Journey’ app, launched by Portiuncula University Hospital (PUH), provides 360 degree views of all the areas the children will visit at the hospital as well as useful information about anaesthesiology tailored to the age of the child.

Dr Vinod Sudhir, Consultant Anaesthesiologist, PUH, said “Preoperative anxiety in children and parents is a very real phenomenon before undergoing general anaesthesia. As healthcare professionals we recognise the increasing impact of anxiety and the physiological negative impact it can have on the child’s and parent’s ability to cope with events surrounding the experience of anaesthesiology and surgery.
“Children may have anxiety around the multidisciplinary environment of theatre, their expectation of events, meeting unfamiliar people and even fear of pain.
Parents/guardians can accompany their young children to theatre and be present with them during induction of anaesthesia. Some of the parent’s anxiety comes from their fear of the unknown and the steps surrounding their role with their child at the time their child undergoes anaesthesia. By providing information through the app, which uses child-friendly animation, we can begin to prepare parents/guardians and children for surgery and ease their distress.
“The ‘Little Journey’ app was developed to help change the way children experience hospitals by empowering them and giving them the information they need to reduce their anxiety in a fun, interactive format. The app helps children to familiarise themselves with the hospital and the handy checklists included will help families to prepare in advance of the hospital stay.
“Last year the demand for general anaesthetic increased in children due to the increase of paediatric day case surgery at the hospital. We want to help alleviate any distress due to anxiety whether the child is
presenting for surgery or investigative procedures," he said.
Martina Fallon, mum to Diarmuid, said the app was so helpful for him.
“He could visualise his hospital experience through the app and it really helped not only him but me to prepare. He loved the different characters and games and played the games all the way in the car to the hospital. It is also a great information tool for parents; we loved it, it’s a great resource,” she said.
The ‘Little Journey’ app is free to download from Google Play Store or App Store. It can be used on a smartphone in 2D or using a 3D virtual reality headset. The app gives children the chance to meet the animated healthcare characters who will explain what they do and what happens on the day of surgery, see some of the equipment which will be used to care for them, find out more about what to expect on the day of their procedure and includes a virtual tour of the children’s day ward, the theatre room and the recovery room at PUH.
New buses driving community living for St Mary of the Angels residents

St Mary of the Angels was initially funded for one wheelchair-accessible bus but it soon became apparent that with more transport, more residents could access activities outside of the campus. There are now three buses, which allows the social and recreational service team to carry out leisure sampling activities for each of the residents.
Shopping, movies, gym sessions and overnight stays - new buses are allowing residents of St Mary of the Angels in Beaufort access the local community more regularly.
From horse riding and hairdressing appointments, to library visits and sports, more transport means more regular activities beyond their home. Skills teaching plays a big role in each of the community outings. The importance of road safety, the use of tra c lights, how to choose from a menu, or pay for an item in a shopthese are all independent skills people can practise and achieve in the community.

St Mary of the Angels was initially funded for one wheelchair-accessible bus but it soon became apparent that with more transport, more residents could access activities outside of the campus. There are now three buses, which allows the social and recreational service team to carry out leisure sampling activities for each of the residents.
The additional transport a ords the freedom to go on faraway day trips without clock-watching to get the bus back. The team have also been able to facilitate and commit to weekly community activities such as gym sessions, swimming at the community pool, beautician appointments, personal shopping, meals out and many more. Each outing is tailored to the wants and goals of the person.
The extra transport also supports the residents to go further afield for overnight trips. One resident, Tomas, went to Cork City for the night, visited Fota Wildlife Park, did some shopping, and took in a movie and dinner. The pure joy that this trip alone brought to Tomas was easy to see. Previously, with only one bus, the other people that live with Tomas would have been housebound for two days to allow this trip to happen.
Another resident, Reece, is supported by the social and recreational service to attend the gym in Killarney each week for his personal training session with coaches, Connor and Stephen. Not only have these gym sessions contributed to his health, Reece has built a great rapport with his coaches and the other sta . He is known by name by the regulars that train at the same time as him.
These are just two examples of the many experiences that each individual now has, made possible by the new buses and the Social and Recreational Service. Goals for 2023 include numerous overnights for many residents, as well as community art classes and day trips!
HSE Cork Kerry Disability Services welcomed the allocation of once-o national funding that allowed for these new buses.
“This funding has allowed us to update aged vehicles across a number of agencies in Cork and Kerry. St John of God Services received funding to purchase two extra vehicles for their day and residential services and what a di erence it has made,” said Majella Daly, Head of Disability Services, Cork Kerry Community Healthcare.
“You can see how much it has enhanced the lives of the residents. It gives them so much freedom and independence, as well as opening up a whole world of activities that adds meaning to their day. They get to meet new people, plan days out and integrate more into their local community. It’s fantastic to see how the new buses have helped to change and improve lives.”
Maurice Jo is a regular attendee of the Kerry Aphasia Café. Like many others with aphasia, he finds it di cult to interact with people in settings outside of the home, despite the encouragement of family and friends.
The Aphasia Cafe was set up in March 2020 to provide a supportive group setting for people living with aphasia. Aphasia occurs due to injury to the brain, most commonly from a stroke. Brain injuries resulting in aphasia may also arise from head trauma, brain tumours, or infections.










Maurice Joe’s reduction in opportunities to communicate since his stroke has become a barrier to progress in speech and language therapy, as he has fewer occasions to use language, fewer conversation partners and fewer opportunities to put the therapeutic approaches targeted in his therapy appointments into practice.
Since he started attending the café, anything and everything is up for discussion. From local GAA rivalries to Six Nations rugby, the Rose of Tralee to the Eurovision, greenways to motorways, Maurice Jo has given his opinion on it all - although he draws the line at discussing wedding planning!
Over a cup of tea, he gets to experience a wide variety of communication partners, more natural communication tasks than those targeted in a clinical session and greater opportunities to interact and take turns in conversations. Having aphasia can impact your ability to speak, read, write and understand language. Service users with aphasia often report feeling socially isolated and lack the confidence to communicate with others. They avoid going out in public and no longer go for meals with friends, or enjoy everyday activities such as going for a co ee.
The Aphasia Cafe was set up by Cork Kerry Community Speech and Language Therapy Department, Kerry Stroke Support Group and Kerry Community Work Department in order to provide opportunities to connect and converse with others with similar communication needs, in a supportive setting outside of the therapy room.
It runs on the third Monday of the month in Ballygarry Estate Hotel and Spa, Tralee. There is usually have a group of about six attending each month and their carers or family come along too. The sessions are facilitated by speech and language therapists across the three community healthcare networks in Kerry. Even the hotel sta have received training on how to facilitate conversation with people with aphasia, in order to make the experience supportive for service users.
As well as o ering the attendees increased opportunities for social participation, the café also provides a means of signposting to other organisations, groups and support networks. Individuals can attend independently or come supported by family, carer or community therapy colleagues.
For more details, contact the Kerry SLT Dept on 066-7104949 or 086-1181812.

Cork Kerry Community Healthcare (CKCH) welcomed Minister of State for Mental Health and Older People Mary Butler to Kinsale recently to officially open the Kinsale Community Health and Wellbeing Resource Centre (The Well).

The Well is the first project of its kind in Ireland and provides accommodation for three community groups which are involved in promoting mental health and wellbeing in the community.
CKCH provided the location, a former health centre, and The Well volunteers secured funding for work on the building. CKCH has also provided extra funding to complete the works needed to transform the centre into a community resource. The name 'The Well' was chosen as traditionally a well was a community resource where people gathered and was the provider of a life-giving force. The Well is also an acronym for Wellness, Education, Life-giving and Life-skills.
The centre will foster inclusive community participation by providing an environmentally friendly facility where health and wellbeing, education, recreation, celebration, and arts are all enjoyed.
“It gives me great pleasure to see this collaborative, multi-agency project which will benefit the health and wellbeing of people of all ages in Kinsale and the wider community. It is wonderful to see so many people and groups come together with a shared vision to improve
health and wellbeing facilities for the community,” said the minister. “This vision has been turned into a reality here today thanks to the hard work and commitment of all involved.”
Interim Chief Officer, CKCH Gabrielle O'Keeffe said it was a fantastic achievement to see the community hub up and running in the heart of the town - a headquarters for so much support and positive work.
“I know just how vibrant and important these three groups are within this community and it is wonderful that they now have a permanent hub, fully kitted-out, where they can work together to improve the mental health of both young and old. The fact that a Youth Café sits alongside a Men's Shed here is truly inclusive and mutually beneficial,” she said.
“The repurposing of the vacant health centre premises is an absolute credit to Carmel Murphy and her ‘Well’ volunteer team, who have worked so hard and fundraised so much to help make this happen. We are delighted to be able to support ‘The Well’ by providing the premises and wish to congratulate everyone involved on such a remarkable achievement.”
In autumn 2017, a project team tasked by the chief officer, CKCH assessed the potential of the former and then-vacant health centre to provide a base for a number of community and voluntary organisations, providing health and/or social care services in the community, which urgently required more appropriate or alternative accommodation.
The project team undertook a number of consultations and meetings in Kinsale, facilitated by the CKCH Community Work Department, to establish and assess options. This process resulted in a viable proposal from a group of community organisations - KYSS, Kinsale Youth Centre/Café and Kinsale Men’s Shed.


They proposed to form a health and social services umbrella group to provide a hub and focus for community-based health and social care initiatives in Kinsale. This proposal was accepted by the CKCH Management team and progressed on the basis of a lease that would reflect that:

• the HSE contribution to the project was the premises.
• the organisation would take responsibility for the running costs of the building
• the organisation would manage the building and provide access opportunities to other groups
• the Management team of the organisation reflected representation of the three community and voluntary organisations and community reps and would be supported by CKCH Community Work department
After an agreed legal process, a lease was signed off and the building was handed over in its present condition with a nominal rent from the HSE to the Kinsale Community Health and Well Being Resource Centre, a registered charity.
The Well volunteers have worked over the last four years to renovate the building. They connected with Clann Credo to secure a loan and successfully accessed funding from SECAD (Development Company) and Pobal to reimagine the building. They also ran several fundraising events, including a car draw and selling tickets to guess the number of lobster pots in the Lobster Pot Christmas Tree.
"It is wonderful to see so many people and groups come together with a shared vision to improve health and wellbeing facilities for the community."Cllr Alan Coleman; Kevin Murphy, deputising for Cork county mayor; Minister of State for Mental Health & Older People Mary Butler; The Well chairman Carmel Murphy; Christopher O'Sullivan TD; Cormac Dineen, chairperson of Men's Shed; Cllr Marie O'Sullivan, chairperson of Municipal District Authority; Cllr Gillian Coughlan; and members of The Men's Shed. Above left: Cllr Alan Coleman; Christopher O'Sullivan TD; Carmel Murphy, chairperson The Well; Kevin Murphy, deputising for Cork county mayor; and Minister of State for Mental Health & Older People Mary Butler with volunteers from Kinsale Community Health and Wellbeing Resource Centre (The Well). Above right: Volunteers from Kinsale Youth Centre, part of Kinsale Community Health and Wellbeing Resource Centre (The Well) at its official opening.
Our health service is being restructured into six health regions
HSE West and North West: Donegal, Sligo, Leitrim**, Roscommon, Mayo, and Galway
HSE Dublin and North East: North Dublin, Meath, Louth, Cavan**, and Monaghan
HSE Dublin and Midlands: Longford, Westmeath, Offaly, Laois, Kildare, and parts of Dublin South and Wicklow*
HSE Midwest: Limerick, Tipperary and Clare
HSE Dublin and South East: Tipperary South, Waterford, Kilkenny, Carlow, Wexford, Wicklow, part of South Dublin
HSE South West: Kerry and Cork
*West county Wicklow: West county Wicklow continues to be aligned with Kildare for health services
**West county Cavan: A small portion of west county Cavan continues to be aligned with Sligo/Leitrim for health services
• allow us to deliver more integrated care closer to patients’ homes
• allow us to plan and deliver services around the needs of local populations
• improve governance and accountability at all levels
• strengthen local decisionmaking
• provide consistent quality of care across the country
We have started to transition to health regions this year. To begin this transition, the CEO decided to expand the HSE Centre Executive Management Team and create a Senior Leadership Team (SLT). This team is made up of Hospital Group CEOs and Community Healthcare Organisation Chief O cers. This paves the way for the further transition to health regions.
Key programme activities for 2023 will include:
• ongoing engagement with stakeholders, including patients, sta , voluntary organisations, GPs and others,
• recruitment of health region CEOs,

• creating six integrated pods that reflect the new health region geographical structures,
• developing the Integrated Service Delivery Model in more detail,
• agreeing how clinical and corporate governance will operate in the new structures,
• agreeing how populationbased funding will operate,
• agreeing the digital, ICT, and capital needs of each health region,
• gradually aligning Hospital Group (HG) and Community Health Organisation (CHO) responsibilities and boundaries with the new health region boundaries,
• agreeing on a transition approach to support future structures,
• agreeing on a framework and conducting a population needs analysis within each health region.
From February 2024, we expect to begin the transition to the new health region structure.
This will include:

• appointing new health region CEOs
• Health Region CEOs becoming accountable for the delivery of all services within their health region boundary
• appointing members of each health region Senior Leadership Team (SLT)
• implementing a transition approach and options for sta consideration to support future structures
• CHO COs and HG CEOs remaining in place and reporting to health region CEOs until a SLT is appointed
After the new health region structure has been set up, we will:
• recruit health region senior teams
• transition to the Integrated Service Delivery Model
• move towards a more advanced state of integration in 2024
• continue to engage with patients, sta and other key stakeholders throughout all phases of the programme
• address requirements under key areas: workforce, data and information, infrastructure (including Capital / Estates), governance, integrated processes, and service delivery / clinical pathways
• stand down HG and CHO structures by the end of 2024
Integrated care allows patients and service users to access health services more easily, no matter where they live. It also makes it easier for our sta to deliver more joined-up care. It is a system of care where patients’ needs come first.
Health regions are a crucial step in an ongoing process to reduce barriers to integrated care. By improving our structures and working more closely together, healthcare providers, public health professionals and community organisations can address the challenges our system faces and improve overall health outcomes for everyone.





An oncology research project led by advanced nurse practitioner (ANP) Dr Janice Richmond at Letterkenny University Hospital is providing practical benefits to patients receiving oral anti-cancer medication in Donegal.

ANPs are the highest level of clinical experts in the nursing profession in Ireland today. Dr Richmond qualified as the first accredited ANP in oncology in Ireland in 2006 and was recently awarded Senior Researcher of the Year by the Irish Cancer Society for her work on this project.
The primary goal of the research project was to develop and investigate the potential transition of care from the hospital to community settings for patients receiving oral anticancer medications. The possibility of this had long been discussed by the oncology day ward sta , who believed that there was a better way to care for these patients.
In line with the Sláintecare model of ‘right care, right time, right place’, the ANP integrated care model, successfully trialled by Dr Richmond and the wider team, was about improving the patients’ experience of receiving treatment with the oral anti-cancer medications to make the process as e cient and convenient as possible. Another benefit of this is that it frees up hospital capacity in the oncology day ward for patients who need to attend to receive acute therapies. Overall, the model has huge potential for national implementation. The pilot of reviewing patients receiving oral anti-cancer medications in a community setting commenced in January 2022. 37 patients were enrolled on the trial and they had their assessments for oral anti-cancer therapy in a community setting either in person or virtually.
Throughout the four-month pilot, 152 patient assessments were carried out by Dr Richmond in a separate location aimed to mirror a primary care setting. The benefit to patients is shorter waiting times, ease of access, and continuity of care while the hospital benefits from additional capacity added back to the oncology day unit.
Speaking about the potential of the trial, Dr Richmond said, “With an integrated approach and with support and access to the wider hospital-based multi-disciplinary team there is huge scope for this model to be implemented in other regions providing a similar positive experience for patients.”
Olive Gallagher, Director of Nursing for the Saolta Group Cancer Managed Clinical and Academic Network (MCAN), praised the trial. “Janice’s work is a key enabler of the NCCP Systemic Anti-Cancer Therapy (SACT) Model of Care and plays a critical role in creating additional capacity in the oncology/ haematology day ward, it demonstrates the real value of nurse led research in shaping future healthcare delivery for our patients.”
The project was supported by the Irish Cancer Society, the Health Research Board, National Cancer Control Programme, HSE O ce of Nursing and Midwifery Services Director.
HSE Community Healthcare East hosted a free, drop-in awareness event in Bray Primary Care Centre recently to highlight the range of community support services that are available for those who have been diagnosed with Parkinson’s Disease. Guests at the event were also treated to a special performance by the Wicklow Parkinson’s Choir.
Parkinson’s Disease is widely considered the second most common neurodegenerative condition after Alzheimer’s Disease in Ireland.
Martina Queally, Chief O cer, HSE Community Healthcare East, said, “A diagnosis of Parkinson’s Disease can be a very overwhelming and worrying time for patients and those that care for them. We wanted this event to reassure these people that there is a full range of community support out there that can help.”
The idea originated from Fiona Craven, adult speech and language therapist in North Wicklow, who runs a Parkinson’s Speech Therapy Support Group in Bray Primary Care Centre. Having seen how beneficial this group was to Parkinson’s service users and their carers, Fiona initially approached Dawn Tyner, Community Healthcare Network Manager for North Wicklow, with the idea.
“I thought it was a great idea and something new that we haven’t done before. Given that April is International Parkinson’s Disease Awareness Month, we thought this would be the perfect time to hold our own first-of-its-kind local awareness event. We wanted to give patients and carers the opportunity to speak directly to local support
services to help them find out what support is out there and how to access it,” said Dawn.
“The event was an excellent example of Sláintecare and our Enhanced Community Care Programme in action. It demonstrated how our multidisciplinary teams in the Community Healthcare Networks work together, alongside our community organisations, to benefit the individual needs of our service users. GPs and consultants have excellent knowledge of the range of support that is available and are often the first point of contact for referrals to community-based services like these, but I also encourage people to reach out to us directly for advice and support if required,” added Martina Queally.
Organisation Development, HSE Change and Innovation has recently launched Creating Conditions for Change and Integration. This resource has been designed to provide practical help and guidance to individuals and teams to increase readiness for change and support integrated working enabling the implementation of Health Regions across the country. It is aligned to the Health Services Change Guide programme of work which is focused on building change capacity and capability across the system.
Creating Conditions for Change and Integration recognises the importance of:
• Focusing on people and culture as a key platform for change
• Understanding the complex nature of health and social care services
• Assessing readiness so that changemakers know when and how to intervene appropriately The evidence on change is clear – we need to engage with the people who will be impacted by the change early and often. Their experience and insight will be key to informing what needs to be attended to and how best to progress change at local level. There are helpful prompts included in this resource that will assist teams to consider all of the different elements:
• Why is this change so important?
• How will it impact on me and the team I work with?
• What do we need to do to improve readiness and support the transition?
It is also important to recognise that change within health and social care systems is complex, unpredictable and often quite messy. It rarely follows a step by step process. To bring about meaningful change it is important that we take the time to understand our own local context and all of the factors that make it unique – the people, relationships and the ways we do things. This resource outlines three simple rules:
1. Agree a shared purpose – this will help to unite people on what is really important
2. Focus on relationships – connecting with people and working together to find solutions
3. Use appropriate interventions – thinking about what will work best in your team or service based on your needs.
For more information about Parkinson’s Disease support in Wicklow email CHN7.Cheast@ hse.ie. To find out more about the Wicklow Parkinson’s Choir email wicklowparkinsonschoir@gmail. com. Other community support organisations include www.move4parkinsons.com and www.parkinsons.ie

Speaking at the launch, Caitríona Heslin, HSE Organisation Development, acknowledged the importance of having change, project management and quality improvement supports in place for teams and services across the country to enable the implementation of Health Regions and to build on the work that is already taking place on delivering integrated pathways of care. “We have a responsibility to support change leaders at all levels to find solutions to the many challenges they face on a daily basis in delivering services to local communities. We cannot be change leaders on our own and we need to develop networks of support locally. This resource is intended to help in a practical way and builds on the work we have been doing in recent years to join up our efforts to support service improvements.”
Hard copy available on request by emailing changeguide@hse.ie or download from www.hse.ie/changeguide

Connect with us on LinkedIn at Health Services Change Matters for updates or follow us on Twitter @HSEchange_guide

"Given that April is International Parkinson’s Disease Awareness Month, we thought this would be the perfect time to hold our own first-of-its-kind local awareness event."ABOVE: Susan Healy and Elaine Birkett, Organisation Development, HSE Change & Innovation with Liam Woods, National Director, Health Region Implementation. BELOW: Pauline Burke; Tony Canavan, CEO; Helen O’Neill; and Siobhan Rogers, Saolta University Healthcare Group.
Cork is piloting a new health promotion programme called ‘Be Active Be Well’, which encourages those living with chronic disease and older people who have become increasingly inactive to get moving!

The Healthy Ireland survey showed that over 60% wanted to be more active but needed more support. Be Active Be Well is a community-based programme, based on peer support, so adults of all ages and abilities can take part. Each session covers a di erent topic to help participants become more active for health and wellbeing.
It’s the first programme in the country to focus on physical activity and include behaviour change techniques to support people in becoming more active. The pilot programme was delivered in Mallow and feedback from the programme was very positive.
One participant told Health Matters, “The exercises that we learnt on the programme have been great to encourage me to do something every day. My doctor was delighted I was being active, as I must return for chemotherapy and radiotherapy in January. I always feel better when I do them. I really enjoyed the programme.”
Another user reported that the Be Active Be Well programme ‘gave me my motivation back’.



“Doing the exercises helps me get more motivated and it’s very helpful in an appropriate and supportive way. It’s very good, well worth it,” they said. There are five sessions in total and each session is two hours long. The first four sessions take place once a week, over four weeks and then eight weeks later is the fifth and final session. These group sessions take place in local community venues. The sessions consist of input from programme facilitators, group participation, individual reflection and practical exercises such as stretching, walking, strength and balance.

“I’m delighted as I am in a much better place physically now,” said Joan Lynch, who has arthritis, and who recently benefitted from exercise classes as part of an outreach programme designed to fast-track patients who otherwise may experience significant waiting times.
Eavan Lennox, Senior Physiotherapist, Primary Care, North Wicklow, explained that the MSK Knee Outreach Programme is a “collaboration between St Vincent’s University Hospital, clinical physiotherapists, and the community services here in Bray.”
“I’ve had arthritis since I was 36 and I started with hip replacements at 40. I arrived here and as soon as I came in there was just respect and love and everything else that the girls gave us."
The programme is facilitated by HSE, Physical Activity Health Promotion Officers from the Health Promotion and Improvement Department, Cork Kerry Community Healthcare. Further information can be found on www.thewellbeingnetwork.ie
“Many people with osteoarthritis of the knee were not getting the treatments we knew they should be getting. A lot of people were sitting on our waiting lists, waiting for a surgeon to tell them they needed physiotherapy here in their primary care area. They may then wait up to two years for that appointment and then may wait an additional year to receive the services here. So we decided to try and fast-track the whole process and get them seen here in the
The programme is currently available to those living in the North Wicklow catchment area via GP referral. You can also watch how John and Joan illustrate the success of the programme on the HSE Internal Communications YouTube Channel.
community first, getting their first-line core treatments here in group format.”
She added, “And then we have the second strand to the programme too which is absolutely terrific because we can now get these people into St Vincent’s University Hospital if they need to be fast-tracked to see a surgeon within a matter of weeks.”
For Joan, the experience has been very rewarding. “I’ve had arthritis since I was 36 and I started with hip replacements at 40. I arrived here and as soon as I came in there was just respect and love and everything else that the girls gave us. By the second time I came they knew our names – I really felt part of something. And then when the exercises began it was great – I loved them.”
Sinead O’Sullivan, Clinical Specialist Physiotherapist, St Vincent’s University Hospital, further explained that the programme has been “hugely beneficial for patients – they really do seem to enjoy it. And we’re collecting lots of outcome measures which show many benefits.”

She added, “We are also building a lot of collaborative links between the acute services and primary care services. And we have lots of other ideas on how we can increase collaboration and improve pathways of patient care.”




For client John Gibbons, the engagement he experienced was particularly positive.
“I found the classes very good. One of the main things I found was that everyone got involved and everything was well explained and demonstrated. I found them really good every week.”

A number of new primary care centres have been opened in communities across the country recently.

The primary care centres have been developed as part of the HSE’s €240 million national Enhanced Community Care (ECC) programme, which is making substantial progress nationally in reducing pressure on services and dependence on the acute hospital-centred model of care through enhanced and increased community services.



In the last few months, Minister for Health Stephen Donnelly visited the new state-of-the-art facilities in Newpark and Thomastown, Co Kilkenny; Enniscorthy, Co Wexford; Drumcli e and Grange in Co Sligo; and Donegal Town.


Speaking at the o cial opening of the Newpark Primary Care Centre, Minister Donnelly said, “Enhanced Community Care is a huge investment in community healthcare services in the HSE, aiming to provide more services closer to people’s homes, and provide extra services for older people, or people who live with longterm health conditions.
“94 Community Healthcare Networks, 21 Community Specialist Teams for Older Persons, 21 Chronic Disease Community Specialist Teams and 21 Community Intervention Teams are now in place, with national coverage. Community diagnostic services provided over 253,000 scans to patients in 2022.
“The national Enhanced Community Care programme is, at its core, a reform programme representing an investment of €240 million to develop and enhance care in the community. It has been developed under the Sláintecare Programme to ensure all HSE primary and community care services work together e ectively.
“Primary Care Centres, such as this new, state-of-the-art one in Kilkenny, together with the Integrated Care for Older People hubs, allow us to provide integrated and high-quality services closer to people’s homes. I want to thank the HSE sta , working in partnership with GPs and Primary Care Teams, who are already making a di erence to the lives of people throughout Ireland.”
The primary care centres provide of a range of health services from a single integrated, modern facility to help serve the healthcare needs of the people of the surrounding areas.
Denise Cahill, Cork Healthy Cities, on community food growing in public parks in Cork City
The Green Spaces for Health interagency group works with communities to maintain existing public green spaces and seek out new greening opportunities for planting food across Cork City. The work extends the understanding of greening, to encompass deep ecology, protecting biodiversity, and the creation of new habitats.
In 2018, the Healthy Ireland Fund for Cork City was utilised by Cork Healthy Cities - an initiative co-funded by the Health Promotion Department, HSE Cork and Kerry Healthcare in Cork City and Cork City Council - to develop an innovative partnership focusing on the benefits of health promotion and environmental sustainability, entitled Green Spaces for Health. Cork Food Policy Council collaborated with this innovative project to develop community food-growing initiatives across the city.
Promoting the regeneration of nature with minimal interference or cultivation by humans, the co-ordinator encourages city dwellers to become citizen scientists, learning about biodivserity, recording and mapping aspects of our natural world to help inform future decisions.
Green Spaces for Health collaborates with as many individuals and organisations as possible to realise a greener city.
Food growing communities have been established and supported across the city with the onset of over 30 community food-growing spaces now in existence in Cork city. The community gardens have become a hub for learning about nature, discussing sustainability and of course, opportunities to enhance social, physical and mental health of those who engage.

Green Spaces for Health has developed a number of exciting and ground-breaking initiatives including:
a Seed Library in partnership with Hollyhill Library
a Beehive on St John’s College in the heart of Cork City
a tree audit of a parish in the city centre
a natural dye garden
• erection of two polytunnels in a public park

• the establishment of a tree nursery with staff in St Finbarr’s Hospital
• planting of over 1,000 trees across the city
• the building (in partnership with Men’s Sheds) and installation of a Sand Martin Wall to attract the birds to nest in Cork city centre installation of a hexagonal large bed housing over 100 plants in June with people living at the flats complex on Fort Street bat detection workshops community digging of a pond in a public park
• a Bioblitz day-long event
• planting of a hedgerow of 360 native trees
• publication of a community cookbook for produce from community gardens in the city designed for children
Green Spaces for Health has also worked with local schools to set up tree nurseries to support the growing of native trees by collecting and harvesting fruit. The long-term plan is to yield 1000s of trees if adopted widely by community gardens, schools and public sector work sites.
The new facility is operational since January 2023 at the Errigal Chronic Disease Management (CDM) Hub located opposite the entrance to the Emergency Department at Letterkenny University Hospital (LUH).


This is the fifth community x-ray location operating across Donegal Community Healthcare Network areas from which patients can receive a plain film x-ray which is accessed via an electronic referral from their GP. The other facilities are located in Community Hospitals at Dungloe, Carndonagh, Donegal Town and Killybegs. These facilities currently undertake 1090 x-rays on average per month.
Gerry McMonagle, Chairperson of the
Regional Health Forum West, said, “This facility complements the Sláintecare reform programme as it improves safe, timely access to care and promoting health and wellbeing, is focused on integration, safety, prevention, shift of care to the right location, productivity, extra capacity and achieving Sláintecare waiting time targets. It is testament to the HSE’s commitment to investing in the health and wellbeing of the people of Donegal.”
There are two full-time senior radiographers in place to support the facility.
Dermot Monaghan, Chief Officer Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo (CH CDLMS),



said, “This facility ensures the rollout of the Enhanced Community Care Programme within Donegal. It will greatly enhance our ability to provide our patients with the highest quality of care.
"Through this investment we are reaffirming our commitment to the health and wellbeing of the communities we serve, and we look forward to continuing to enhance our services in the years ahead.”
Noeleen Gallagher, Senior Radiographer, said, “We are thrilled to have this new facility. It will benefit patients as it will improve timely access to diagnostics in the community, and reduce pressure on the acute hospital services and Emergency Department.”
A new state-of-the-art community x-ray facility has been unveiled in LetterkennyGerry McMonagle, Chairperson of the Regional Health Forum West with HSE staff, and public represenatives, Front from left are Dermot Monaghan, Chief Officer, Community Healthcare, CH CDLMS; Maura Gillen, General Manager, Primary Care; Cllr Gerry McMonagle; Mandy Doyle, Head of Service, Primary Care, CDLMS;and Jennifer Mulcahy, General Manager, Primary Care. L-R: Dermot Monaghan, Chief Officer, Community Healthcare, CH CDLM; Gerry McMonagle, Chairperson of the Regional Health Forum West; Daniel McDermott, radiographer; Maura Gillen, General Manager, Primary Care
people can thrive’
Two more areas have joined the growing Sláintecare Healthy Communities Programme, an initiative set up to deliver increased health and wellbeing services in 19 areas of greatest need across Ireland.

Lord Mayor of Dublin Caroline Conroy visited the Finglas Youth Resource Centre to officially launch Finglas and Cabra as a Sláintecare Healthy Community site. It followed the launch of the programme in Cherry Orchard and Ballyfermot at a community event in the Ballyfermot Civic Office.
Speaking at the Ballyfermot launch, Cllr Vincent Jackson said, “The challenge of addressing health inequalities in our communities requires not only interventions to target particular health risks, but also a broad focus on addressing the wider determinants of health. To make real and lasting change we need to work together to create communities where people can thrive, putting in place the right building blocks for health, stable jobs, good pay, quality housing, good education and accessible amenities that enhance and improve our built environment.”
Sláintecare Healthy Communities Seed Funding was allocated to enhance community amenities to address health inequalities by improving the socioeconomic determinants of health and wellbeing. Some of the services that have benefitted from this funding in the Ballyfermot area to date include:
FamiliBase is a centre for children, young people and families based in Ballyfermot, Dublin who provide a systemic Trauma Therapy service which has been delivered in FamiliBase since 2019
• The Ballyfermot Family Resource Centre provides a Listening & Supporting initiative that was established in 2020 which provides counselling to young people as an early intervention measure, and to prevent more acute and serious mental health difficulties.
In addition, €250,000 as a once-off Sláintecare Healthy Communities Enhancement Fund was made available to support the redevelopment and completion of the Ballyfermot People’s Park. Meanwhile, the funding of €250,000 for the Finglas and Cabra area will be used to support improvements to Ventry, Mt Bernard and Johnstown Parks. This includes redesign and upgrading of Ventry Park to provide a new playground, community garden and a multi-sports area to support community healthy place making and wellbeing. The council is also looking to provide outdoor gym equipment which will be installed in Mt Bernard and Johnstown parks this year.
Local development officer Talent Nyamakope has been working with community partners and local groups to identify the health and wellbeing needs of the Finglas and Cabra communities. Talent will continue to engage with all stakeholders and build a realistic and accurate understanding of the communities’ priority needs and ways to address these through the seed funding.
As part of the HSE’s commitment to the development of the health regions, the importance of working in partnership with patients/service users is recognised. A series of engagement sessions have been planned to ensure that the patient’s voice is represented as part of health regions design.
The health regions team attended a meeting facilitated by the Patient and Service User Experience Office with patient representatives and some Patient and Service User Experience Leads in January 2023. Following this, the health regions team received feedback from a number of patient representative groups as to what members view as important in the design of the programme.
On 10 May, Patient Partners and Service Users, the health regions team and staff from the Department of Health attended a Patient Engagement Workshop, at the Ashling Hotel, Dublin. This provided an opportunity to ensure patient and service user engagement is core to the Health Regions programme. A further patient engagement workshop is scheduled for 7 June 2023.




HSE National Ambulance Service (NAS)-led service called Pathfinder, designed to safely keep older people who phone 112/999 in their own home rather than taking them to a hospital emergency department, has gone live in Letterkenny.



Pathfinder improves outcomes for older people by providing safe alternative care at home rather than in hospital and will be provided by NAS sta working with colleagues from Letterkenny University Hospital.
Welcoming the introduction of the service to Letterkenny, Sean Murphy, Hospital Manager, Letterkenny University Hospital, said, “We are pleased to be able to o er this service to suitable older people in our local communities. Through the Pathfinder Model, many older patients can be safely and appropriately managed in their own home rather than being transported to the ED for assessment when they dial 112/999.
“Pathfinder aims to reduce congestion in busy EDs and makes for a better environment for patients and sta on the floor whilst improving
overall flow through the ED. The service enables increased ED capacity to care for other patients, by supporting this cohort of complex, frail patients at home,” he added.
The Pathfinder ‘Rapid Response Team’ respond to 999/112 calls for older people (65 years and older) in their homes. The older person is assessed by both an advanced paramedic and occupational therapist/ physiotherapist. Where safe, the team supports the older person at home rather than transporting them to emergency department, by linking with a wide range of alternative hospital and community services. Pathfinder also operates a follow-up team of physiotherapy and occupational therapy which provides immediate home-based rehabilitation, equipment provision and case-management in the subsequent days following a 999/112 call. On average two thirds of patients seen by Pathfinder following a 999 call have remained at home rather than being brought to the Emergency Department.
The World Health Organization defines integrated service delivery (ISD) as the ‘the management and delivery of health services so that clients receive a continuum of preventive and curative services, according to their needs over time and across di erent levels of the health system’.
An ISD Workstream Group has recently been established by the HSE Health Regions programme team to progress the design of an ISD model for the regions. The Workstream Group consists of patient / service user representatives, members of Department of Health, the HSE, Voluntary Organizations and Academics.
The group met on 17 May to begin working collaboratively on the key considerations to support integrated service delivery within health regions, and to consider potential organizational arrangements.

new national Tuberculosis (TB) study revealed that a smart health option would cost the HSE €300 per patient, just 8% of the current system cost of €3,362 per patient, over a six-month treatment period.
The Health Innovation Hub Ireland (HIHI) and National TB Centre study of 34 patients investigated the use of technology against in-person care in TB medication adherence over 18 months. Some 16 study participants were on the current Irish standard of care, Direct Observed Therapy (DOT) where a public health nurse must physically witness patients taking medication. 18 participants were randomised to the World Health Organization (WHO) recommended UK and US standard of care - Video Observed Therapy (VOT).
Patients take TB medications remotely, recording through their smartphone and sending securely to the clinical team. A total of 3,634 videos were viewed during the study period.
Using the current method of Direct Observed Therapy (DOT) HSE cost is €3,362 per patient over six months, compared to €300 Video Observed Therapy (VOT) for same period.
Time for each public health nurse to carry out DOT in person using hard copy records for one patient was up to 60 minutes. For VOT each patient video was on average one minute at the Seven participants were transferred from DOT to VOT due to inability to comply with DOT citing work hours, or reported undue stress due to DOT.
Patient sentiment with VOT was extremely positive. VOT empowered continuation of normal work/life routines and taking medications at a time convenient to them. Contrastingly, those on DOT had to be available at set times suitable to the public health nurses, which
was disempowering and restrictive.
VOT can facilitate twice daily dosing at no additional cost. For patients on twice daily dosing on DOT, typically the second afternoon dose in the PM could not be facilitated due to time constraints of the public health nurse. As a result, not all doses were observed, which is a significant health risk.
Co-principal investigators, Lorraine Dolan, TB Clinical Nurse Specialist, and Prof Ann Marie McLaughlin, said, “We urge the Irish health system to review TB care in Ireland based on the overwhelming results of this new study. VOT is hugely cost saving; time saving across staff teams,
supports patient self-management and increased TB patient medication observation per day.”
Health Innovation Hub Ireland Manger, Dublin Eimear Galvin said, “Health Innovation Hub Ireland focus is introducing innovative solutions to our health system that meet priority needs of Irish patients. HIHI was thrilled to work with the TB team to deliver this important study, which shows remarkable health system savings, increases treatment access and supports self-management in the community. The need for this kind of remote care and patient self-management is even more obvious now since COVID-19.”

"The need for this kind of remote care and patient self-management is even more obvious now since COVID-19.”
Angela McCloskey has been appointed to the role of patient advice and liaison service (PALS) coordinator at Letterkenny University Hospital (LUH). Angela is from Letterkenny and spent 19 years working as a radiographer in LUH prior to her appointment as PALS co-ordinator. The patient advice and liaison service co-ordinator acts as a visible focal point for patients, families and carers and is often the main contact within the hospital. They help to resolve issues for patients and their families and work towards improving the patient experience at any available opportunity.
Speaking about her appointment, Angela said, “Within the hospital, every contact we have with a patient can have a lasting impact and I try and make that contact as positive as possible.
"My role involves ensuring that the
patient voice is heard either through the patient directly or through a nominated representative.
“If a patient wants to provide feedback or make a comment about the hospital and the care they received, I can assist them in doing so, or refer them to the appropriate person who will be able to assist them further.”
Sean Murphy, General Manager, LUH, added, “This is the first appointment of a PALS co-ordinator to Letterkenny University Hospital and I am delighted to welcome Angela to the role.

"PALS co-ordinators have a very important function as they help to embed the voice of the patient in the workings of the hospital.
"Patients are at the centre of everything we do and through the PALS service we can learn more about the patient experience and put plans in place to make necessary improvements.”
Sligo University Hospital has opened a new 290-square metre extension to the intensive care unit (ICU). The extension consists of a single-storey building adjacent to the existing ICU comprising four en-suite isolation rooms with associated facilities.

In addition, the existing ICU is being renovated as part of the project and works to date have included upgrade works to the existing isolation rooms in line with current regulations and additional ancillary facilities to include a staff base and utility rooms.
The new extension is accessible from the existing ICU on level 8, with its own central nursing station. It will be supported by additional staff comprising nurses, medical, health and social care professionals, as well as other staff grades.
This development sees the hospital increasing its critical care capacity from six to eight beds, as well as having more single room facilities within the ICU. This will also allow the hospital to provide different levels of critical care such as ICU level 3 care and HDU level 2 care within the setting.
“If a patient wants to provide feedback or make a comment about the hospital and the care they received, I can assist them in doing so, or refer them to the appropriate person who will be able to assist them further.”Bernie Lindsay, Healthcare Assistant; Denise McCameron, Staff Nurse; Kate Dolan; Clinical Nurse Manager 2; Mary McDonald, Clinical Nurse Manager 2; Ciara Lee, Staff Nurse; and Anna Giraldez, Consultant Anaesthetist.



The Steps to Health challenge 2023 kicked o on 8 May and over 800 teams across CHOs, hospital groups and community voluntary services are busy walking, stepping and being motivated by their co-ordinators to get their daily steps and improve their health and wellbeing.
This year, Health Promotion and Improvement colleagues across the CHOs are busy co-ordinating the challenge locally, motivating and supporting teams in their CHOs to get and keep involved.
Bernadette Mullins, Health Promotion and Improvement O cer, Mid-West Community Healthcare, is one such co-ordinator who is busy motivating and organising over teams in her CHO. Weekly messaging and local competitions have been taking place over the challenge with teams in the area vying hard to top the weekly leader board in CHO3.
“I’ve been involved in the Steps to Health challenge since 2017, for three years as a team co-ordinator in both acute and community services and as a coordinator for the Mid West since 2020 when I joined

the Health & Wellbeing division as a health promotion and improvement o cer,” explained Bernadette.
“I am excited for this year’s challenge and getting teams across the Mid West engaged enjoying the challenge. On a personal level every year I look forward to the challenge and it gives me a great push to increase my physical activity levels.
Simple swaps like a 10-minute walk instead of a co ee break make all the di erence to your step count and to how you feel. The added bonus of being in a workplace team means one of your colleagues is always there to give you an extra nudge to get steps in. It’s a brilliant way to connect with your colleagues.”

St Mary’s Health Centre Thurles were competition winners in 2022 and are busy this year stepping and trying to strive for success again this year. “In 2022 we formed friendships, encouraged teamwork, celebrated success, changed lifestyles. It was a very positive experience and we are delighted to be part of the Steps challenge 2023,” said a team spokesperson.

Five jockeys who rode out in the prestigious Punchestown Horseracing Festival visited renal patients undergoing dialysis treatment at the state-of-the-art Vartry Renal Unit, at Tallaght University Hospital (TUH).


The jockeys are taking part in a special fundraising race for the Punchestown Kidney Research Fund which in turn pays for the arts and health programme at TUH, for patients undergoing kidney dialysis.
Professor Catherine Wall, Consultant Nephrologist at TUH, who took the jockeys on a tour of the Vartry Renal Unit, explained, “For many patients, our arts and health programme o ers a very valuable distraction during their dialysis sessions which can feel tedious and repetitive, taking place three times a week for many years. We are grateful for the valuable support provided by the Punchestown Kidney Research Fund (PKRF), so we can continue this worthwhile initiative.”
One of the jockeys taking part in this year’s race who visited TUH to meet dialysis patients is Katie McManmon from Ballyteague, in Co Kildare. Katie also works as a horse-racing coach in the Racing Academy in the Curragh and says she wanted to ride in the charity race, after watching a close colleague su ering from kidney failure. “In my first proper job, the head man at the stables had a problem with his kidneys. It gave me an important insight into the very real hardship caused by the disease.”
Alison Baker Kerrigan, Arts O cer, TUH, paid tribute to the ongoing support provided by the charity noting the jockeys had ‘improved the hospital experience for kidney dialysis patients by making the arts accessible to all’.


















“Our artist in residence Lucia Barnes, who facilitates the patient art sessions, does an amazing job of listening to the patient’s likes and needs before working with them to create a piece of art that is both enjoyable to do and important to them. Lucia’s combined skillset as both a qualified nurse and professional artist is hugely beneficial to all involved,” she said.



This charity horserace set up by the Punchestown Kidney Research Fund is now in its 32nd year and to date has raised over €1.7m for patients su ering kidney failure.







new one-page document for residents and tourists, detailing what do in an emergency while on a West Cork island, was launched on Sherkin Island recently.


The 10 volunteers, who initially trained as first responders, are the first in the country to go on to complete the PHECC Emergency First Responder Course – which provides significant aid for island residents and visitors in times of medical emergency need.
The West Cork islands – Sherkin, Cape Clear, Long, Heir, Whiddy, Bere and Dursey – are part of a national All-Ireland Islands HSE Primary Health Programme. The West Cork Islands have worked in partnership with Cork Kerry Community Healthcare (CKCH), HSE Cork South Community Work department and the emergency services to produce the information document on what do in an emergency.
Last year, CKCH, HSE, National Ambulance Service (NAS), Coast Guard and RNLI supported a demonstration on what happens in an emergency on an island. Community volunteers trained as first responders and AED were purchased for the islands.
Head of Primary Care for CKCH Priscilla Lynch said, “I want to thank all on the West

Cork Islands Health Forum – emergency sub group – for all their work in building local resilience and emergency skills to deal with di erent types of medical situations. The combination of enhanced first responders, AEDs on all the islands and a one-pager information card for all islanders/ visitors is vital in times of a medical emergency, particularly cardiac arrest, chest pain, strokes and choking episodes.
“The newly-qualified enhanced community first responders play a critical role if there is an emergency to ensure a safer, faster response - using the combined e orts of Coast Guard, RNLI and ambulance. This will save lives and improve island health. Based on the success of this programme, it is now envisaged that this initiative will be rolled out across the country, building resilience in all communities,” she said.
Emer Shanley, Enhanced Community Care Network Manager, West Cork, said it was a ‘great example of what can happen when you bring the right people together’.
“As part of this exciting collaboration between CKCH, HSE, our community partners and island residents, the Coast Guard, the RNLI, NAS, and community first responders, we worked to identify the unmet needs across all island
• Resident islanders
• Holiday home residents
• Tourists and visitors
• Ferry services
communities and developed a collective informed response,” she said.


The training took place during January of 2022 at Whiddy Island and was twofold, to train the volunteers as first responders but also to allow them to go back to their respective island to conduct public training as instructors.
Following this, a community first responder service went live in February 2022 and have been activated a number of times by NAS to calls across the Islands during 2022.
Following the success of this programme, a more enhanced first responder training session took place in January 2023, namely the PHECEmergency First Responder course. As part of this programme, 10 responders from across the islands' community attended training on Bere Island with instructors from NAS and the first responder community, to learn how to deal with di erent types of medical situations that may happen across an island landscape - beyond what they were previously trained for. This enhanced emergency first responder service went live across the islands in March 2023.
The HSE’s Ukraine Data and Informatics team was delighted to win the Crisis Leadership award at the CIO and IT Leaders Awards 2023 recently.

Since tens of thousands of Ukrainian refugees have arrived in Ireland, securing their medical history to be accessed by healthcare teams has been of vital importance. Gathering this information and providing data and insights was the key focus of the HSE’s Data and Informatics group, one of nine main workstreams established by the HSE National Ukrainian Health Response Planning and Coordination Group.
Director of the Health Identity Management Services (HIDS) in the HSE’s Operational Performance Integration Division, Maria McCann, led the workstream to deliver a data and informatics response to support the HSE’s planning and co-ordination group.
Maria said, “The technology can provide up-to-date reports and illustrate daily and weekly trends on key data elements from the digital solution for the health status questionnaire and triage information. This data is then shared with the Health Intelligence Unit for predictive modelling.
“The HIDS team, in collaboration with EY and Microsoft, used the MS Dynamics 365


and power platforms to develop the health questionnaire. This provides real-time access to patient data which makes it easier for clinical sta to make informed decisions and provide personalised care. The team worked incredibly hard on this. It is an honour to be recognised. There was collaboration across multiple departments and organisations and I am grateful for the opportunity to work with such talented and committed individuals.”
"The team worked incredibly hard on this. It is an honour to be recognised. There was collaboration across multiple departments and organisations and I am grateful for the opportunity to work with such talented and committed individuals.”
Shauna Delaney, a critical care clinical nurse educator who has worked in the Intensive Care Unit (ICU) at Tallaght University Hospital (TUH) for the past seven years, has just won a major award from Trinity College Dublin (TCD).

The Carlow town native has just been awarded the Dean of Health Sciences Award for Outstanding Contribution to Teaching in Professional Practice under the School of Nursing and Midwifery. Shauna was nominated for this award by her critical care colleagues and students.
She was awarded a scholarship from TCD in 2022, to complete a PhD in Critical Care where she is now exploring the unmet support needs of critical illness survivors in Ireland. Paying tribute, one close colleague at TUH said, “Shauna really wants to improve patient care and has a phenomenal work ethic. She is an innovative, educational leader who has helped transform the landscape of critical care nursing in Ireland by developing and implementing the first ever NMBI accredited New-Graduate Nurse in Critical Care Programme.” This programme has enabled the
transition of new graduate nurses into the critical care environment, without having the historical prerequisite of several years’ ward experience first.
HSE Procurement partnered with Procurex Ireland 2023 for invaluable opportunities to network and learn across public procurement and the healthcare marketplace.

The RDS opened its doors to the Procurex Ireland event during April to innovate, educate and collaborate with public sector procurement. The one-day event provided a unique and interactive opportunity for both the buyers and suppliers within the public procurement community to engage across a range of innovative event features.
As the largest purchaser in the State, HSE Procurement were delighted to be one of the official event partners. This collaboration is part of the commitment, signalled in the HSE Corporate Procurement Plan 2022-2024, for continued strong engagement with current and prospective suppliers.
John Swords, National Director for HSE Procurement, said, “It is wonderful to be back at this event, meeting people in person and shaking hands really adds a different dimension to the networking we had to adapt over the past few years.”
He reflected on the many challenges encountered since he last addressed the Procurex Ireland audience. Thanking the suppliers for their support and collaboration, particularly over the course of the pandemic, he highlighted the importance of working together to
protect frontline patient services.
On the day attendees were invited to join a number of skill development zones which were centred on four separate themes of social consideration, digital and innovation, bid support, and green procurement. Suppliers interested in learning more about how to do business with the HSE visited the HSE Procurement stand and took part in a meet the buyer session where there was an opportunity to have one-to-one meetings with HSE Procurement Purchasers.
THE NATIONAL DIRECTOR OF HSE PROCUREMENT TOOK THE OPPORTUNITY TO ADDRESS A NUMBER OF THEMES WITH THE AUDIENCE ON THE DAY, WHICH INCLUDED:
• HSE Corporate Procurement Plan – Security of supply, supporting patient care, compliance, value for money
• IFMS - A Single National Integrated Finance and Procurement Management System for the Irish health sector
• The impact of price increases – ‘Responsibilities both ways’
• The power of innovation and collaboration
• The importance of climate action and sustainability
• Working in partnership
– The importance of strong engagement with our current and prospective suppliers will be needed to help us in transforming how we deliver our services and achieve agreed Sláintecare objectives.
“In the HSE we have shared responsibilities, with our supply base we have shared responsibilities, all of which are centred on delivering a better patient experience.”
The sun came out to cheer on the 49 young people who took part in the inaugural Junior Parkrun at St Mary’s Health Campus Gurranabraher, Cork in April


Parkrun is a global phenomenon which helps communities all over the world to be physically active. The aim is to enable communities to participate in timed walk/run events, which are free and sustainable. Participants register on www.parkrun.ie/register/ and are provided with a unique personal barcode identifier. This barcode can be scanned at any Parkrun that you attend anywhere in the world and your timed results are uploaded to the website and emailed to you, to recognise your achievement.
Each Parkrun is run by volunteers who take on a variety of roles, including course set-up, marshalling, timing, barcode scanning, warmup and most important of all - encouraging the runners on the day.
The adult Parkrun is 5km long and takes place on Saturdays at 9.30am, no matter where the venue is. The Junior Parkrun is 2km long and designed for children between ages four and 14; these take place on Sunday mornings at 9.30am.









The health benefits of being physically active outdoors are well recognised and Parkrun has identified a health and wellbeing benefit for volunteers also.




Michelle McNamara, Healthy Ireland Primary Care Lead, Cork Kerry Community Healthcare, explained, “The idea of bringing a Junior Parkrun to this HSE community health setting stemmed back to 2019/2020, when an original plan to create a Junior Parkrun was created. However, these plans ground to halt with the COVID-19 pandemic. Recent enquiries from the paediatric occupational therapy team for accessible physical activity resources in the community for their service users, inspired the reactivation of the Junior Parkrun plans at St Mary’s health campus.
“The response from the HSE sta and the community to volunteer was enthusiastic and heart-warming. Over half of the volunteer team are HSE primary care employees,” she said.

“The HSE estate manager was very proactive and made planning the run, from a risk and insurance perspective, seamless. Local Parkrun ambassador John Kissane mapped out the 2km route and was integral to supporting the whole project. We were fortuitous that Parkrun Ireland manager Matt Shields came to visit the site and met with myself and other local HSE stakeholders Martina Corkery, Sinead O’Brien, Andrea Cronin, Shirley O’Shea and Liz O’Sullivan. The support was very encouraging and helped bring the project to fruition e ciently,” said Michelle.
The application form for the Nursing Home Support Scheme, also known as FairDeal, has been updated. Over recent years there have been a number of updates to the scheme in line with legislation. To ensure that the application form was responsive to applicants and their families, the National Nursing Home Support Office in conjunction with the National Communications Division commissioned in-depth qualitative research with previous applicants and prospective applicants to understand the needs of applicants, understand how the current information material works for their audience(s) and to bring insights back to the team provide a clear direction for future communications development.
Retinopathy screening for women with Type 1 or Type 2 diabetes who become pregnant is being rolled out nationally by the Diabetic RetinaScreen programme.
The new screening pathway was first piloted by the programme through the Dublin maternity hospitals in October 2022. Diabetic RetinaScreen is working with maternity units to provide the service nationally by August this year.
Women who have Type 1 or Type 2 diabetes at the time they become pregnant have an increased risk of developing diabetic retinopathy and should be screened for retinopathy regularly during pregnancy.
Around 40 women in the Dublin region were referred for retina screening during pregnancy in the first quarter of 2023. Diabetic RetinaScreen Programme Manager Helen Kavanagh said the service expects to screen over 250 women with diabetes who become pregnant annually, once the programme has been rolled out nationally.

Based on this research, the application form has been redesigned to include:
• Plain English
• A pull-out section with clear instructions on which parts are to be completed by all applicants, the support documents to be submitted with the form, a check list and an outline of what happens when the form is submitted
• Colour-coded sections
• Notes and explanations of key terms beside all fill-in boxes
• Increased font size and the overall spacing makes the form easy to navigate The National Nursing Home Support Office are committed to improving the experience for applicants when applying for nursing home care. Application forms and information on the Nursing Home Support Scheme is at www.hse.ie/fairdeal

A new community nursing unit (CNU) is currently in development in Thomastown, Co Kilkenny.
The HSE entered a public private partnership (PPP) with EquiSisk Community Care Partnership Ltd in December 2022 for the design, build, finance, operation and maintenance of seven Community Nursing Units - including the unit in Kilkenny to replace the adjoining St Columba’s Hospital.
The construction period now under way will take two years and, following a 25-year period, the ownership and responsibility for operation and maintenance will revert to the HSE.
Helen McDaid, Head of Service/ Older Persons and Acting Chief Officer, HSE/South East Community Healthcare, said, “There is a long history of dedicated care for the older person at St Columba’s Hospital but we are delighted that this will be now set to continue in a state-of-the-art new facility being constructed on an adjacent site.
“The 95-bed CNU will comprise three households of 25 en-suite rooms. This model a person-centred approach which focuses on the quality of life, which supports autonomy and the opportunity to continue to direct residents’ own lives in accordance with their cognitive and physical abilities. There will also be two 10 en-suite bedroomed dementia-specific residential households. The environment will reflect the comforts of home, with assistance provided as necessary in the performance of everyday tasks. There is provision within the entire compliment for 10 short-stay places.”

A new peer support group for those living with Chronic Obstructive Pulmonary Disease (COPD) in Carrick-on-Suir and the surrounding areas is now meeting weekly on Mondays at 11am in the Carrick Swan Juvenile GAA Centre. There is no charge. COPD is one of the most common respiratory diseases in Ireland. The establishment of the free charge group in the Carrick area results from collaboration between the COPD Support Ireland organisation, Tipperary Sports Partnership, the HSE Community Specialist Respiratory team in South Tipperary and people living with breathlessness in the Carrick-on-Suir locality.
Weekly group meetings provide an opportunity to exercise safely amongst peers, improve self-management and quality of life. It is suited to all fitness levels. The friendly group will has the services of a fully qualified trainer.
The goal of these free peer-to-peer support groups is to motivate, engage and support people living with COPD overcome any negative feelings and physical symptoms in their day-to-day life through the integration of peer support and care. The importance of interacting with those in your community who live with the same condition is part of the COPD Support Ireland self-
management plan.
Sinéad Delahunty, Senior Respiratory Physiotherapist with the HSE’s Community Specialist Respiratory Team, South Tipperary Chronic Disease Management Hub, St Brigids Hospital, Carrick-on-Suir, said, "It will be a great community support that will assist patients and their families to exercise, be smoke free, and look after their physical and mental health while having fun and making friends.”
For further information on venues and times for activities, contact 083-086 4118 or e-mail support@copd.ie
Pictured at the launch of the new Carrick-on-Suir COPD Support Ireland Group were Daphne Masterson, Candidate Advanced Nurse Practitioner Respiratory Chronic Disease, South Tipperary; Rosaleen MacUistin, Self-Management Support Co-ordinator for Chronic Health Conditions, HSE/ South East Community Healthcare; Joan Johnston, COPD Ireland General Manager; Pearl Sheehan, COPD Support Ireland Clonmel group representative; Patricia McQuillan, Operational lead, Lntegrated Care Programme for Chronic Disease South Tipperary, HSE/South East Community Healthcare; Bridie Mullins, COPD Support Ireland Clonmel group representative; Michael Drohan, COPD Support Ireland Waterford group representative; Sinéad Delahunty, Senior Physiotherapist, Respiratory Chronic Disease Management, South Tipperary; and Niamh Julian, Clinical Specialist Physiotherapist, Respiratory Chronic Disease Management, South Tipperary.
Galway University Hospitals has become the first hospital in Ireland to introduce an ‘incisionless’ minimally invasive surgery to help correct blockages of the oesophagus. Achalasia is a rare condition which causes a blockage in the muscles of the lower oesophagus causing dysphagia or difficulty in swallowing, including in pronounced cases, liquids.
The procedure was carried out by Mr Paul Carroll, Consultant Oesophagogastric and General Surgeon, specialising in minimally invasive surgery and endoscopic surgery for oesophago-gastric cancer and benign disease.
The introduction of this procedure has added to the expanding Minimally Invasive Upper GI programme in Galway and the Saolta University Health Care Group, which also provides endoscopic surgical interventions for early oesophageal and gastric cancers. GUH is one of only two centres in Ireland with this capability.

Mr Carroll thanked his team for their support in bringing the procedure to Irish patients.
“I am personally delighted that I have been able to introduce this procedure into Ireland for treatment of this disease process. It would not have been
possible without the support and training I received whilst on fellowship in the University of Toronto and finally without the unwavering support of the late Marie Farragher, Clinical Nurse Manager in theatre and her team of nurses for pushing boundaries with me,” he added.
Máire Cooper, Theatre Staff Nurse; Noreen Keelan, Senior Anaesthetic Staff Nurse; Paul Carroll, Consultant Oesophagogastric and General Surgeon; Ashitosh Waidande, CNM 2, GI Theatre; and Deirdre Hoade, Senior Staff Nurse, Theatre.
‘incisionless’
New HSE confidential recipient Gráinne Cunningham O’Brien will be ‘a voice, an advocate and speak up and out for vulnerable adults with a disability and older people’.

“It’s a very important role because by the time the vulnerable adult, family member or sta are coming to me, they’ve generally already tried to resolve the raised concern and or complaint at local level- for example, maybe through the individual service provider, other avenues available through the HSE and/or self-advocacy.
They’ve tried many avenues and they feel they are not being heard,” she said.
“When the vulnerable adult and their family finally feel they are being heard, they are relieved to receive understanding and empathy. It is important to value the opinions and experiences of vulnerable adults, family members and the significant people in their life who are trying to have their voice heard and the issues they raise understood and taken seriously. There is reassurance in this in itself.”
She is a social worker by background, which, she said, is really important to this role because the vulnerable adult can speak with someone who understands the terminology, understands the processes, and the di culties they’ve faced.
“Very often, they’re telling you the end of the story before they get to the beginning. They’re sharing their frustrations and heartache and letting it all out,” she said.
The confidential recipient role is representing vulnerable people when they wish to raise a concern and or complaint in relation to a service they are receiving from the HSE or from one of their funded agencies.
The types of raised concerns and or complaints must pertain to HSE or HSE-funded services including residential, day services, community services, mental health, and primary care.
“Whether its service users, family members, sta or anonymous users, my goal is to reach a resolution of the raised concern and or complaint,” said Gráinne.
Gráinne Cunningham O’Brien, HSE Confidential Recipient, speaks about her new role to Sheema Lughmani, HSE National Quality and Patient Safety Directorate
“Very often, they’re telling you the end of the story before they get to the beginning. They’re sharing their frustrations and heartache and letting it all out."
EXAMPLES OF COMPLAINTS CAN CENTRE ON (BUT NOT LIMITED TO) INCLUDE:
• dissatisfaction with home support services



• funding around residential services
• service user dignity
• right to selfdetermination and hearing the service users voice
• mistreatment or abuse
• negligence
• poor practice
“We know things can go wrong; we accept that. It’s important to acknowledge that and say ‘I’m sorry’."
“What is most disheartening for me to hear from vulnerable adults and their families is the sense of hopelessness they have, the lack of trust they have in HSE services. They query what di erence l can make and will they just get the same generic response. I invest time in empowering the vulnerable adult and their family that it is their right to a service, their right to speak up and speak out and that l will stay the course with them to get the reassurance.”
She stressed that family members, friends, neighbours, sta , legal representatives and anonymous callers can make a complaint on a vulnerable person’s behalf but noted that informed consent is central to "what I do because the vulnerable adult has ultimate control".
“I could receive a raised concern and or complaint from a parent, sibling, care giver, sta member, but if the vulnerable adult doesn’t want it, then they have the autonomy to choose not to pursue it. It’s about what the vulnerable adult wants. The will and preference of the vulnerable adult is at the heart of the confidential recipient role,” explained Gráinne.
“To establish that, I have clear informed consent processes, and I work with the vulnerable adult and their family to make sure they understand their right to self-determination and support that gives them control, to make the choices that are right for them and to essentially be respected as an adult in their own right.”
She explained that there is no typical case for the confidential recipient.
“Every case is unique and deeply personal to the vulnerable adult. I practice to that standard. It is my role to advocate, speak up and out and be the voice of the vulnerable adult. What may seem as miniscule to the HSE is paramount to the vulnerable adult when it impacts their needs and right to a health service. This is the core of the service because the vulnerable adult must remain at the centre of the process throughout,” said Gráinne.
She wanted to stress that HSE sta don’t have to fear raised concerns or complaints.
“We know things can go wrong; we accept that. It’s important to acknowledge that and say ‘I’m sorry’. This is about dignity and respect- not about going on the attack when a complaint arises. So much can be resolved by good engagement and communication,” said the confidential recipient.
“Also, language and narrative are so important and it needs to be friendly and inclusive. Listening is a powerful tool that should be used to hear the vulnerable adult and support them to speak up and speak out in whatever way works for them.
“The culture in the HSE needs to change and a good enough attitude is not acceptable to service provision. The vulnerable adult has a right to assert an opinion and raise a concern and or complaint.”



Online antenatal education classes, which commenced nationally due to the COVID-19 pandemic have been a huge success, with 98% of participants saying they were highly satisfied and 87% reported they would be happy to continue with online classes.
An evaluation of the classes was undertaken by Sinead Thompson, National Women’s and Infant Health Programme, and Gráinne Keena, Nursing and Midwifery Planning and Development Unit, Tullamore, on behalf of the Online Antenatal Education Forum.

The report findings on the feedback of online classes will assist two work stream groups in their body of work in the implementation of the National Standards for Antenatal Education, which is overseen by the National Women’s and Infant Health Programme, (NWIHP). A total of 174 questionnaires from service users were completed.
“The findings from this report are twofold. Firstly, valuable feedback has been provided by participants, which antenatal educators can use to further enhance the quality of their classes. Secondly, it provides evidence that shows the online classes have been
successful and educators can build on this evidence post the COVID-19 pandemic,” explained Sinead.
“One of the most encouraging aspects to emerge from the report was that midwives and educators responded to the needs of the women and their chosen birth partners by setting up and providing very e ective online antenatal education during the pandemic. The information and feedback will now feed into the body of work being undertaken at national level by two work streams that are responsible for the implementation of the Standards.
“The Standards, highlighted the importance of the evaluation process under Person Centred Care - Theme 1. It is hoped going forward that this evaluation tool and process can be adopted by the 19 maternity units in order to provide updates in the area of parent education. The organisations can then factor this feedback into service planning to ensure continuous improvement in the service provided for women and their chosen birth partners.”
Participants overall had a positive experience of online antenatal classes however, not all of the findings were positive. The three most frequently reported disadvantages of online classes were, no opportunity to meet other

• design a combined online and face-to-face evaluation tool that can be adapted and used by the 19 maternity units across Ireland
• get service user’s experience of attending online antenatal education classes during the COVID-19 pandemic
• test the e ectiveness of the evaluation tool by carrying out a small-scale pilot study over a six-week period within five maternity units.
women, get a tour of the labour ward or develop a relationship with the midwife. Antenatal education classes whether they return to face-to-face or remain online, have to be aligned with the Standards. There was a general consensus among the participants that the classes were interactive, helped participants to learn and participants would be happy to continue with online classes.
"The classes were interactive, helped participants to learn, and they would be happy with them to continue online"
An innovative campaign has now successfully launched the new dementia inclusive community symbol. Minister Mary Butler joined people living with dementia, their families, national partners and community champions at a celebration event led by people with dementia. Guests heard the positive impact this visible symbol will have for those a ected by the condition, and about the many dementia inclusive actions that are changing our communities for the better.
Things like staying in touch with family or














message that I am a valued and respected member of my community. Living with dementia is a new life but you have got to embrace it,” she said.
friends, supporting someone to keep doing the things they enjoy, or making a small change in a business that means a person can use a service independently can make a big di erence to the life of someone living with dementia. By using and displaying the symbol, we show our solidarity with over 64,000 people living with the condition in Ireland, be it a business, community group or service.
Kathleen Farrell, who features in the launch poster campaign, has lewy body dementia.
“I am delighted to be involved in developing this symbol and I am looking forward to seeing it when I am out and about. It is very supportive to think that businesses and communities are making changes that mean I can continue to do the things I enjoy and stay connected in my community. Being able to travel and attend appointments or use my bank is very important to me and it sends a strong
Fiona Munro is a clinical nurse specialist in dementia at Our Lady of Lourdes Hospital, Drogheda. She and her colleagues attended the launch event. “We were so happy to meet the minister and all of the other campaign partners and champions. This symbol will help raise awareness of dementia and we hope people will feel more at ease using our services and asking for support where they see it,” said Fiona.
Sean O’Dowd, Consultant Neurologist and Clinical Lead for the HSE’s National Dementia O ce, explained, “It is wonderful to see so many people and organisations embracing this new community symbol. Social isolation is more likely with a person with dementia. Staying socially active and engaged in their communities can help in many ways.
“As well as slowing the progression of dementia, it can positively a ect a person’s mood and overall health and well-being. Seeing this symbol displayed and people’s commitment to learn more about the condition, will help people with dementia to retain some independence and feel more open to new opportunities.”







Psychiatry for the Elderly (Psych-El) provides a consultation-liaison service for older adult inpatients in St James’s Hospital. For many of their inpatients, hearing impairment is an issue that they face, and it can cause great difficulty when staff communicate and engage with patients. This can often result in distress on both sides.
A pilot mental health screening programme conducted by advanced nurse practitioner (ANP) Martina
Power found that almost 50% of all patients screened recorded hearing difficulties. However only 2% had access to hearing aids. In order to address this unmet need, the Psych-El team applied for funding from the HSE Dublin South-Central Mental Health Service for hearing amplifier devices, and they were successful in their application.
Hearing amplifiers can be used to enhance communication with patients who have hearing impairment and no hearing aids. They are wearable devices that use a microphone to pick up nearby sounds, and they can be disinfected between each use and have multiple users. Since their introduction they have proved to be a great asset for patients and multidisciplinary teams.
To date, the team has distributed a hearing amplifier to the clinical nurse managers on 15 different wards. Additional funding has also been secured for nine more devices, with the goal of ensuring that every ward in the hospital has a hearing amplifier.
All staff members who care for patients with a hearing impairment are advised to avail of the amplifiers,
ensuring that they are used to their full potential. Since their introduction, feedback has been incredibly positive from both patients and staff.

“Every day, different staff from the MDT are using the device to engage with patients on the ward. Before, we may have had to raise our voices if someone was hearing impaired, now we can engage in a more personcentred way, using a natural tone of voice when communicating. It’s really great for the patients.” – Alda Rodrigues Silva, CNMII
“It’s such a great idea for those of us who have a hearing impairment. If someone is really deaf they can communicate really well with others, you can have a conversation without shouting.” – A patient
"If someone is really deaf they can communicate really well with others, you can have a conversation
shouting.”
Gemma Willis’ life changed utterly when she was involved in a serious road crash in 2015. The young Carlow woman had 14 operations in 16 months. She was treated by seven doctors and cared for in three hospitals.
Gemma, now a patient representative on the Trauma Steering Group Committee, explains that the new Trauma System for Ireland would mean that, had her accident happened today, she would be transferred immediately to the Mater Hospital where all her needs would be overseen by one doctor.

“I can see how important trauma care services are and how different my accident could have been after the new trauma system was set up. I’d be brought straight to the Mater and there would be one doctor overseeing all my medical needs instead of the seven doctors that I did have, all trying to deal with individual injuries. Your rehab needs would be assessed at an earlier stage which should mean that you will get to somewhere like the NRH sooner than the
support a network of hospitals across the Central Trauma Network, accepting the transfer of severely injured patients from other networked hospitals. It is forecast that an additional 1,500 patients will be managed by the MTC at the Mater once the trauma system is fully operational. Similarly, the MTC at CUH will support trauma across the South Trauma Network and is forecast that an additional 380 trauma patients will be managed at CUH once the Trauma System is fully established.
When Gemma had her accident, she was brought to nearby Naas hospital where she was stabilised and assessed but they were not equipped to deal with her severe injuries.
“It took 16 hours before I was brought to the Mater Hospital. Those 16 hours were so crucial. In those 16 hours I might not have lost my leg, I might not have lost my toes. It shows how important it is to be brought to a hospital that is able to look after trauma and deal with trauma,” she said.
nine months I had to wait,” she said.
The recent launch of major trauma services at the Mater Hospital and Cork University Hospital (CUH) represents the first phase in the development of the National Trauma System. As Major Trauma Centres (MTC), they will provide the highest level of specialist trauma care to the most severely injured patients for the two trauma networks, the Central Trauma Network and the South Trauma Network. In addition to the two MTCs, a network of Trauma Units will be developed in each trauma network to deliver more general trauma care to the majority of patients who do not need the specialist expertise of a MTC.
The Mater Hospital will now begin to
“My father was told when I left Naas that I might not make the journey to the Mater. When I arrived at the Mater they put me in an induced coma and started operating straightaway. I had multiple operations on multiple injuries.
“I had 11 operations in total in the Mater in nine months. While I was in the Mater, spinal fluid had leaked into my brain and was putting severe pressure on my brain so there was an emergency call to the Beaumont to get me there as soon as possible. I was transferred there and Beaumont said I wouldn’t have lasted the weekend if I hadn’t arrived when I did.
“After nine months in the Mater, I got transferred to the brain injury section of the NRH. I did three months on the brain injury ward before I eventually got transferred down to the spinal ward where they worked hard on me for four months before I finally came home to my new life,” she added.
“I can see how important trauma care services are and how different my accident could have been after the new trauma system was set up."












Cork City’s LGBTI+ Inter-agency group recently hosted the International Rainbow Cities Network in City Hall for three days of intensive work, drafting LGBTI+ policy guidelines for local governments as part of the EU for Citizens policy initiative.
It was seen as the perfect opportunity to invite other cities on the island to attend, if they had an interest and openness to developing, supporting and learning from one another in progressing LGBTI+ inclusion.

Representatives from Limerick, Galway, Derry, Belfast, Dublin and Waterford all attended or linked in to this side-event and stronger links are being made across the island for progressing LGBTI+ inclusion, participation and acceptance.
Cork is the first city in Ireland to be a member of the RCN and while it o cially became a rainbow city in 2020, it only received its certificate in person in 2023. However, the story began with the creation of a smallinnteragency steering group in 2002. This group was established to advance objective 86 of the City








Development Board plan - a service needs analysis of Cork City and public agencies response to LGBT communities.

















One of the founding members of this group was HSE community worker Eleanor Moore and since 2002, a HSE community worker has been part of the LGBTI+ Inter-agency Group in the city. The group is jointly funded by HSE Cork Kerry Community Healthcare and Cork City Council.



The inter-agency group evolved over time and today has representation from all of the public agencies, LGBTI+ NGOs and community representatives. Over the years, the Inter-agency has been to the fore in organising, representing and promoting LGBTI+ human rights and inclusion. This includes an annual awareness week that coincides with IDAHOBIT (International day against homophobia, biphobia, lesbophobia and transphobia) in May each year.
In 2014, City Hall in Cork was the first civic or public building in Ireland to o cially fly the rainbow flag. 2016 saw LGBTI+ inclusion actions included in the city’s Local Economic and Community Plan. San Francisco, with
IN 2014, CITY HALL IN CORK WAS THE FIRST CIVIC OR PUBLIC BUILDING IN IRELAND TO OFFICIALLY FLY THE RAINBOW FLAG.
whom Cork City is twinned, co-signed a rainbow memorandum pledging to work together on LGBTI+ issues in 2018. A number of other initiatives and conferences have been held over the years for community, public and private sector employers and organisations to raise awareness, share best practice and promote inclusivity for LGBTI+ people.

The HSE Community Work Department provides management support and is the primary funder of Section 39 groups including: The Cork Gay project; Lesbians in Cork community resource centre and the Sexual Health Centre, which provides a nonbiased, non-judgemental and inclusive



















health service. The Community Work Department also work closely with the Youth Health Service, a free HSE sexual health service for young people aged 23 and under and they provide funding, via Lottery, to Gay Pride Cork.
Work promote,

The Community Work promote, advocate for and support various training and awareness initiatives. This has included training in the CUMH for LGBTI+ parents, ensuring Section 39 organisations can access LGBTI+ training on HSELand, flag raising, prominent displays of LGBTI+ inclusion support, for example stickers and lanyards, as well as supporting wellness committees on campuses.
In 2023, we mark the 30th anniversary of decriminalisation of homosexuality in Ireland, a Victorian-era law which forced Gay men to conduct their personal and private lives in secret, for fear of legal sanction and which had a chilling e ect on the entire LGBTI+ community. Decriminalisation was a major milestone in the history of LGBTI+ communities in Ireland and a significant step towards advancing human rights and inclusion for LGBT people.




While Ireland is becoming ever more culturally diverse, we must embrace diversity, promote equality and provide inclusive health practice across all our services.

"In 2023, we mark the 30th anniversary of decriminalisation of homosexuality in Ireland, a Victorianera law which forced Gay men to conduct their personal and private lives in secret, for fear of legal sanction and which had a chilling e ect on the entire LGBTI+ community. "
Further information and training is available via HSELand.ie, LGBT.ie, LINC.ie, Gayproject.ie or your local LGBTI+ group. Also, see rainbowcities.com

The new HSE National Ambulance Service (NAS) ambulance station at Devlin Road, Mullingar was o cially opened at the end of March.

The new station replaces the previous base, which was on the Regional Hospital Mullingar campus on the Longford Road. It accommodates emergency services, administrative and sta accommodation facilities, and enclosed ambulance parking areas.
The State’s investment in this modern facility reflects a wider commitment by the HSE and the NAS to providing optimal pre-hospital care to communities across the country and to providing appropriate facilities to ambulance crews.
Speaking at the opening, Minister for Health Stephen Donnelly, said, “It’s fantastic


to be here today in Mullingar to o cially open this vital local health service resource. This new facility is the latest example of the Government’s continued investment in the National Ambulance Service, not just here in the Midlands, but across the country.
"The local community in Mullingar and surrounding areas will now benefit from a new ambulance station that supports the delivery of optimal emergency and community health services. This new facility will also enhance the wellbeing of our dedicated NAS sta .


“The NAS sta here in Mullingar and across the country, whom we all depend upon to deliver an essential frontline emergency service, have played a pivotal role over the last three years in delivering the HSE’s COVID-19 pandemic response. I also want to acknowledge their role in driving wider healthcare reforms.
“Despite significant increases in demand for emergency services in recent years, NAS have continued to rise to meet this demand and I want to reiterate my thanks once again to the members of the NAS for the vital work they carry out every day of the year, 24/7, and for their unwavering commitment to the highest standards of patient care around the country.”
Robert Morton, director of NAS, said, “I very much welcome the development of this new ambulance station, which will be great asset to the town of Mullingar and surrounding areas. This facility is an important one and

will assist the NAS to fulfil its mission to provide high-quality, safe and patient-centred services.




“This care begins immediately at the time an emergency call is received and continues through to the safe treatment of the patient and transportation and handover of the patient to the clinical team at the receiving hospital emergency department if required.












“I have no doubt that this new ambulance station will be important in helping us to achieve our ultimate aim of improving patient outcomes whilst ensuring appropriate care delivery. I would like to wish every success to the NAS crews based here in Mullingar and to thank everyone who helped to bring this new station to fruition. It will be a tremendous asset to the National Ambulance Service for many years into the future.”

Construction of the new single-pitch ambulance building commenced in May 2021 and was completed in June 2022. The station is designed to accommodate 28 sta and allows for swift access and exit from the site, which includes 16 car parking spaces and a boundary fence with swing gates. The accommodation also includes training facilities, a reflection and study room for sta and indoor bays for duty crews. The station was constructed by Kealy Construction, Dunshaughlin, Co Meath and designed by Dublin-based architects MCA.

“DESPITE SIGNIFICANT INCREASES IN DEMAND FOR EMERGENCY SERVICES IN RECENT YEARS, NAS HAVE CONTINUED TO RISE TO MEET THIS DEMAND."
The National Service Plan 2023 (NSP 2023) was launched on 29 March 2023 and sets out a partnership approach to the type and volume of health and social care services to be delivered by the health service in 2023 with a revenue budget of over €21.6 billion. The NSP 2023 outlines the third year’s implementation of our Corporate Plan 2021-2024 and serves as a shared vision for the HSE, providing transparency in what our patients and service users can expect and laying out the key objectives, actions and targets developed by service teams for the organisation.
In addition, the NSP has regard to and is guided by the primary considerations of: the Programme for Government; the priorities set by the Minister for Health; and Sláintecare and the component plans resulting from that policy.
Health expenditure has continued to rise in the last decade, as it has in many countries, driven by a rise in population, an ageing profile and medical inflation. Total public expenditure on healthcare in Ireland increased from €13.6bn in 2012 to €21.5bn in 2021, a 58% increase. The total population in Ireland is set to grow by an additional one million people in the period to 2041 (a 21% increase). More significantly, the population aged 65 years and older is expected to double over the same period and the population aged over 80 years will increase almost three-fold. Our population needs are likely to outpace the resources available. Hence, the future requires us to continuously strive for excellence by proactively thinking di erently and optimising our current resources to their fullest potential. It is through this lens that the NSP 2023 has been developed.
Our planning recognises and seeks to respond e ectively to significant, long-standing challenges that exist within our health service. There are long waiting lists for scheduled care in hospitals and long waits in emergency departments, particularly for older people and for those with more complex needs. Waiting lists for community-based services such as therapies, mental health and disability services also pose significant challenges.
Extensive co-ordinated service planning occurred across the HSE to ensure the a ordability and deliverability of our NSP 2023 in light of the significant challenges which present a complex context that requires careful monitoring and management.
Hospitals: We will continue to deliver safe, timely access to hospital care by implementing a range of measures to ensure better access to unscheduled care, improved cancer care and prevention, and to build on proven waiting list initiatives and ambitious waiting time targets set for outpatients.
Community: The Enhanced Community Care Programme (ECC) will continue to roll out nationally to ensure more people can access healthcare in their local community rather than within the acute hospital setting.
Mental Health: There will be an increase in the number of referrals seen across all mental health services, including referrals to Child and Adolescent Mental Health Services.
Disability: We will improve the delivery of a range of specialist community-based disability services and increase service capacity in the areas of day, respite, multidisciplinary, residential and personal assistant services as well as progressing the delivery of the Assessment of Need process in line with legislative obligations.
Recruitment: The HSE is addressing complex challenges in workforce planning and recruitment while maintaining focus on strengthening the retention of the existing workforce.
We continue to work to transform the delivery of our services informed by local population health needs, and to create a culture which embraces innovation and new models of care to improve health outcomes.
Sláintecare sets out a vision to systematically reform the

delivery of care and address a broad range of complex issues across the health sector, improving safe timely access to care, promoting health and wellbeing, and addressing health inequalities. The establishment of six health regions will align and integrate hospital and community services based on defined populations and local needs.
The HSE is also committed to creating a culture primed for
innovation, underpinned by mechanisms to e ectively spread and scale good practices and digital solutions at pace. We will seek to e ect these changes in partnership with a vibrant voluntary sector and working closely with key private sector organisations. The scale of reform and innovation required is significant and will impact every part of our health system, including our sta and the people we serve.
Of the total 2023 revenue budget, €240m is for investment in new measures, including:


€101.2m in respect of eligibility measures
€50.1m in national services, workforce and reform
€25.0m in disabilities

€14.0m in mental health measures
€8.7m in acute funding
€10.6m in women’s health
€17.9m in primary care
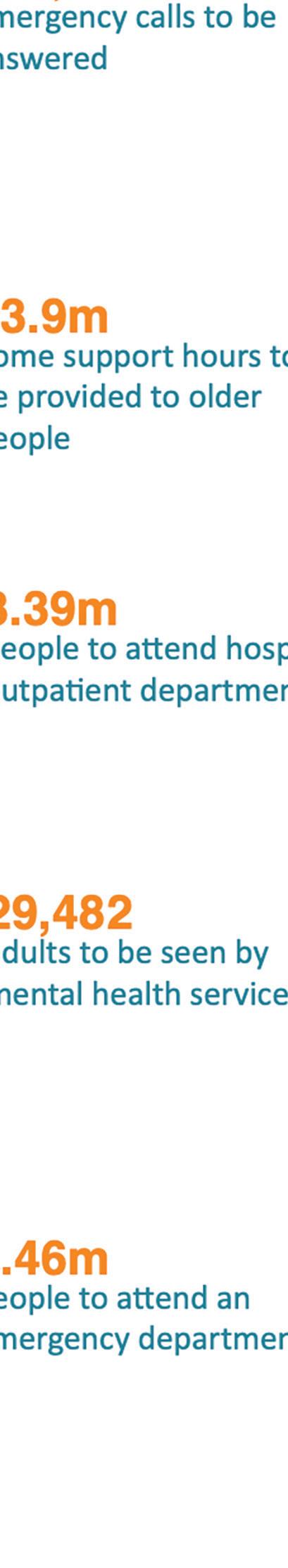
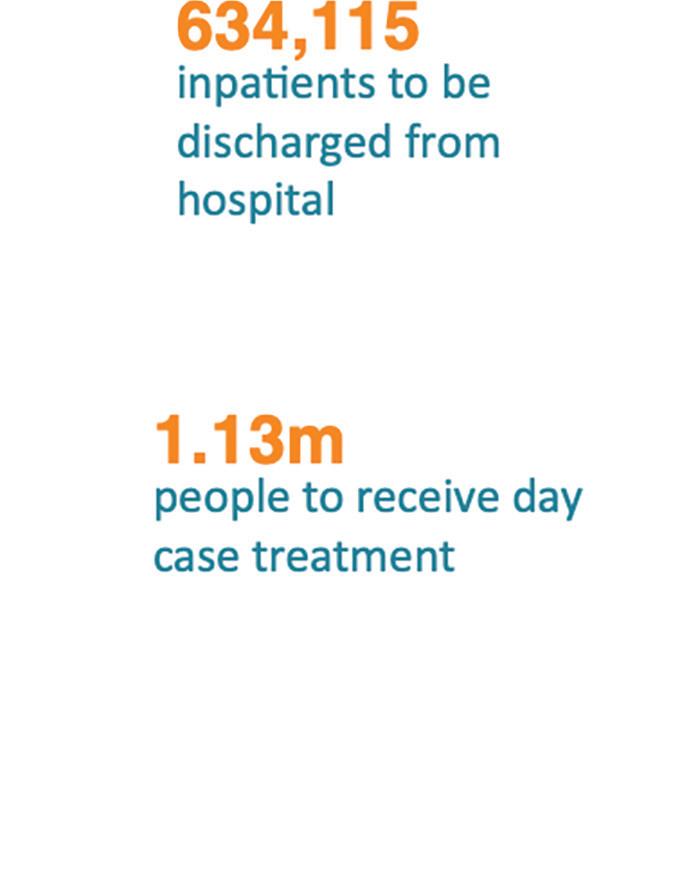
€11.8m in older persons’ services

€0.8m in health and wellbeing
If you would like further information on the National Service Plan, please contact the Planning team in the Office of the National Director, Strategy and Research at planning. ddg@hse.ie or telephone 021-4923531. The National Service Plan 2023 is available at: https://www.hse.ie/ eng/services/publications/ serviceplans/nationalservice-plan-2023.pdf
The Design and Dignity programme was born out of an understanding that surroundings affect those going through the trauma of death. This programme was an initiative of Irish Hospice Foundation (IHF) and is managed in partnership with Health Services Executive (HSE Estates), it strives to bring about a transformation of both the physical setting within acute hospitals and the culture of care.
Paula O'Reilly, CEO of Irish Hospice Foundation, explained, “The vision of Design and Dignity is that every adult, paediatric and maternity hospital in Ireland has warm and welcoming spaces to enable dignity and respect for patients and families facing dying, death and bereavement.”
The HSE has adopted the Design and Dignity Guidelines, which support staff and hospitals to provide compassionate and dignified spaces during dying, death and bereavement for patients, relatives, and staff. Mortuaries should offer a sanctuary where life and death can be
revered in a serene, respectful, and reassuring atmosphere. However, for some in their current state of disrepair, hospital mortuaries are struggling to provide this and don't reflect the compassionate care provided by staff.
Micheál Conneely, Corporate Estates Manager - Capital, HSE Estates, said the projects are making a ‘real difference’ to patients, families, and staff.
“The success of these projects is due to the support and passion of staff and management of the hospitals who have championed these projects and can see the benefits they bring to their hospital setting,” he said.
In August 2019, IHF and the Design and Dignity programme proposed the need for ring-fenced funding specifically for mortuaries. This was supported by the HSE, having identified a need for mortuary refurbishments to create dignified sanctuaries for the deceased and their loved ones.
May 2023 marked the completion of works on St Columcille’s Hospital
Mortuary, Loughlinstown, Dublin (pictured above), with refurbishment having begun in January 2023. This is the product of years of advocacy, made possible by the devoted team at St Columcille’s, who are working to continually improve end-of-life care within the hospital.
One key member of this team has been Marianne Quinn, who was hospital chaplain for 17 years. Mary Henry, Senior Anatomical Pathology Technician, has worked within the mortuary for the past 25 years and provided her insight to the value of this project, stating that the project ‘shows the family that their time with their loved one is valued’.
The project at St Columcille’s focuses on the relatives area, modernising the viewing room and facilities for families and access to the mortuary, including four designated parking spaces for the bereaved. It will provide an environment which respects the dignity of the patient and their closest family.


Kells primary care team participated in a sta fitness challenge in both January and April 2023.
Sta working in the primary care building in the Co Meath town participated in a fitness assessment along with body composition analysis and a physical activity profile. This was assessed by the physiotherapy team and the dietician based in the centre. The assessment used was based on Operation Transformation Minimum Fitness Tests, which is recommended on the Sta Healthy Weight Management Programme run by CHO8.
Participants’ body composition was first analysed by the dietician and advice was given on diet and lifestyle interventions that were appropriate to the individual. The sta were then asked to participate in a number of fitness challenges which included: grip strength test; press up test; sit to stand test; and balance test.
Participants were made aware of the endurance test that was recommended by Operation Transformation, and advised to take this test themselves. Sta were then advised on ways to practice these things and how to improve their
overall fitness. This was then retested again in April 2023.

There was great interest on both occasions in the assessment days. The team was very kindly provided with goodie bags from the health and wellbeing o ce in Louth County Hospital and from health promotion and improvement team in Navan for all participants. These days were a huge success and very enjoyable for all involved.
“It was a great motivation for all who participated, as there was some healthy competition from all departments. We also gave participants information on locally run sta wellbeing programs such as HSE Stress Control, HSE Steps to Health Challenge, Sta Healthy Weight Management Programme and Kick Start to Sta Health. These programmes are run both nationally and by CHO8 health promotion teams and are a great addition to sta looking to improve their health and fitness,” said one of the organisers.
“We would like to thank all who participated and were involved in this sta fitness challenge and who made it such an enjoyable experience.”
A new eLearning programme for current and potential sta to guide and support them in securing a role in the HSE, from the initial application through to the interview itself, is now available.
The ‘Getting a Job in the HSE’ eLearning programme is made up of three modules running 10-20 minutes each, with an approximate total duration of 45 minutes, depending on how quickly you work through them.


The programme is available to existing HSE sta on HSeLanD. Prospective external candidates can access the modules on www.hse.ie.
The job application and interview process can seem daunting for many, and often prevents people from taking opportunities to progress in their career with the HSE. We aim to remove as many perceived
barriers to job applicants and hope that the eLearning programme will guide people through the process and provide them with the skills they need for a successful application.
Module 1 will help you recognise the main elements of HSE recruitment processes, feel confident in completing the application form in a way that puts you in the best position for getting a job, and avoid some of the common mistakes that people sometimes make in filling out an application form.
Module 2 is about the interview process, providing practical ways to prepare for an interview and information on managing interview anxiety.
Finally, Module 3 gives you a chance to conduct an actual practice interview and evaluate it afterwards.
“It was a great motivation for all who participated, as there was some healthy competition from all departments."
Cork and Kerry primary care paediatric occupational therapists work on developing children’s functional independence in the activities that they need to engage in at home and in school. This can include self-care skills such as dressing and toileting, but can also include school skills such as writing skills and being able to organise themselves and their belongings.

The video series was developed following an identified need and request from schools and families to make intervention strategies accessible to those wishing to refer to the service. “Creating easy-to-access online intervention strategies on the HSE website and YouTube channels, we feel supports and empowers families to receive the advice and support they seek at an early stage, even before the need to attend primary care paediatric occupational therapy arises,” said Brenda O’Connor, Paediatric Primary Care Occupational Therapist.
“It is important that we continue to explore new modern ways that we can provide occupational therapy intervention to parents and children, not just in a clinic setting. The video series can be watched easily at any time from home when working on skills such as toileting, dressing, organisational skills, early writing skills, fine and gross motor skills. These skills are best practised in the child’s natural setting.”
CORK AND KERRY PRIMARY CARE PAEDIATRIC OCCUPATIONAL THERAPY ONLINE VIDEO SERIES
COMPRISES:
• Sensory Regulation: The Alert Programme ‘How does your engine run’
• Teaching Organisational Skills in the Home
• Large Movement Skills: Balance, Aiming & Catching, Co-ordination
• Developing Independence in Dressing Skills
• Developing Functional Independence in Toileting



• Oral Motor Skills & Feeding
• Sensory Sensitivities in Feeding
• Developing Fine Motor Control
• Developing Your Child’s Early Writing Skills
Watch the paediatric OT videos on the Cork Kerry Community Healthcare YouTube channel.
A new video series aimed at families and those seeking tips and strategies on how to develop their child’s functional skills has been launched
Nurses and midwives across the disciplines and from a variety of roles and services came together to discuss and agree on future research priorities for their practice The HSE O ce of the Nursing and Midwifery Services Director (ONMSD) commissioned the scoping exercise with and for nurses and midwives working in the HSE and HSE-funded services.
Nurses and midwives of all grades and disciplines have the experience and expertise to know what future research would enhance their practice and enhance the quality of the service and experience of people using health services.

The scoping exercise was conducted in 2022, inviting nurses and midwives of all disciplines, grades and settings to take part. The overall aim of the scoping exercise was to identify research priorities for nursing and midwifery for the period 2023-28, to support enhancement of service delivery, and improve care and practice experiences for persons using services.
The categories identified for focus in the future included workforce planning, service delivery, service user involvement and access to services, the role of nurses
and midwives, education and development, digital health, clinical and practice expertise, governance and leadership and change and improvement.
As would be expected, it was evident that nurses and midwives want to continue to enhance and improve the quality of the care and practice they provide to persons using their services.
Phase one of the scoping exercise involved two online surveys, conducted during the months of July and August 2022. The survey questions were based on 10 themes identified from an extensive literature review of current strategic policy documents relevant to nursing and midwifery. After a second round survey was conducted, data analysed identified the 10 most frequently occurring categories and 47 subcategories from a total of 2,928 topics put forward by participants.
Phase 2 of the exercise engaged with a nominal group of experts to develop a final set of research priorities that reflected the findings from phase 1. Ten research categories and 20 associated research statements emerged from the data analysis and nominal group meeting.
This exercise demonstrates that it is possible to be inclusive when planning an
















engagement exercise with a large number of people. In the case of this scoping exercise, all nurses and midwives working in the HSE and HSE funded agencies (Section 38) were invited to take part. Of that cohort, 640 took part in the first survey and 176 in the second survey. The nominal group consisted of 28 people on the day contributing their expertise to the overall process.

e research priorities for nurses and midwives for the next ve years have been outlined
The HSE and Munster Technological University (MTU) and its Students Union recently collaborated to promote the common mental health di culties of ongoing stress, anxiety, low mood and sleep to students.
Posters, social media and the student union magazine were used to share messages aimed at MTU’s 18,000 students. Thomas Broderick, lecturer at MTU’s Sport, Leisure and Childhood Studies Department recorded a student podcast with Mark Smyth, HSE Senior Clinical Psychologist.
Mark Smyth advised, “If young people can spot small things in themselves that are starting to persistently bother them, seeking advice and support as soon as they become aware of them can really help. This isn’t always easy as the busyness of life can distract young people from the impact that low mood, stress, anxiety and lack of sleep can have on them.
“What also helps students is knowing that they are not the only one who worries a lot or are feeling down because of a relationship or an exam result. Knowing many other students experience the same stress and anxieties and have the same low or sad feelings makes getting support seem less daunting. I’d encourage students to share their feelings with family and friends. If you are not ready to talk, the online supports such as mindfulness, CBT or a stress control programme may suit.




“Keeping an eye on one’s sleep pattern is also essential. Students are juggling di erent aspects of academic life and need energy. Sleep gives their bodies, brains and minds time to take a rest, recharge and get strength. Students who habitually stay up late and want to change could start by pulling back bedtime by 15 minutes a night.”
MTU president, Professor Maggie Cusack, said the university was delighted to join with the HSE and the Students Union to raise awareness of the Your Mental Health campaign.

“At MTU, our students are the heart of our university, and we are committed to
doing everything we can to support their mental health and wellbeing. The practical messages promoted through this campaign will ensure our students are informed and empowered to make better decisions around their mental health as they journey through MTU,” she said. Head of student counselling, MTU Cork, Dr Honor Carroll, highlighted how “fostering a culture of mental health awareness is key to student wellbeing. Along with the HSE’s yourmentalhealth.ie we have support services in Cork and Kerry including our online peer support platform, digital mental health programmes, and the text ‘MTU’ to 50808 service, all of which are free and accessible to students and sta 24/7.”
“Keeping an eye on one’s sleep pattern is also essential. Students are juggling di erent aspects of academic life and need energy. Sleep gives their bodies, brains and minds time to take a rest, recharge and get strength. Students who habitually stay up late and want to change could start by pulling back bedtime by 15 minutes a night.”Pictured at the o icial launch of the mental health student awareness campaign were: Kelda McManus, VP welfare, Student’s Union; Norma Deasy, HSE Campaigns Manager; Michael Hennessy, HSE Service Improvement Lead, Mental Health; Prof Maggie Cusack, MTU President; Thomas Broderick, lecturer, Sport, Leisure & Childhood Studies Department; Dr Honor Carroll, MTU Head of Student Counselling; Keith Brown, MTU digital o icer; and Michael Loftus, MTU Vice President for External A airs.
IF YOU WOULD LIKE TO CONTACT ANY OF THE TEAM FOR RESOURCES, ADVICE OR JUST A SIMPLE QUERY, PLEASE DO SO.
• Martin Ryan (Cork) Martin.Ryan8@hse.ie
• Helena Cogan (Cork) Helena.Cogan@hse.ie

• Donagh Hennebry (Kerry) Donagh.Hennebry@hse.ie
Connecting for Life is Ireland’s national strategy to reduce the number of people who die by suicide.
In 2017, Cork Kerry Community Healthcare (CKCH) launched two local plans - one for Cork and one for Kerry. Although these plans are similar and plenty of suicide prevention work is carried out across the whole region, having separate plans gives us the opportunity to have specific actions unique to each area.
There are fantastic initiatives across the two counties, which take a holistic view on a person’s mental health and involve bringing together statutory and non-statutory agencies and organisations to work together. This collaboration aims to improve the mental health and wellbeing of those that may be vulnerable.
CKCH has three Resource O ces for Suicide Prevention working across the region. Martin Ryan co-ordinates the implementation of Connecting for Life in Cork, Donagh Hennebry is the co-ordinator in Kerry and Helena Cogan co-ordinates suicide prevention training across the two counties. Key achievements from the local Connecting for Life Plans include:
Cork and Kerry are the only locations in Ireland to have a real-time data surveillance system in place to monitor suspected suicides. This project is a collaboration between the HSE, the coroners in Cork and Kerry, and An Garda Síochána. All of this is overseen and co-ordinated by the National Suicide Research Foundation (NSRF).
Fest
This week-long festival across the county of Kerry runs annually to coincide with World Mental Health Day. It is organised by a fantastic group of people who work within the community. Over the past five years, it has seen over 600 free events held in Kerry and online to support mental health.

Cork Community Events
Connecting for Life has funded and helped to organise successful public events in Cork to encourage the whole community to improve their mental
health. These include Joy in the Park (in Fitzgerald’s Park in Cork City), Together at the Castle (at Mallow Castle) and the launch of the Green Ribbon mental health stigma reduction campaign.

CKCH has developed a wide range of resources, ranging from Adult Mental Health booklets and Youth Mental Health booklets, to Safety Plans for vulnerable persons and resources with contact numbers for anyone in crisis (including posters, car stickers and key rings).
CKCH o ers a wide range of free suicide prevention training for members of the public and professionals. These include START, safeTALK, ASIST, Understanding Self Harm and STORM. These range from online 90-minute Introduction to Suicide Prevention Workshops, to longer and more in-depth professional training.

Mary Butler, Minister of State for Mental Health, and Bernard Gloster, HSE CEO, recently addressed an event which marked one year since the launch of the first implementation plan for ‘Sharing the Vision –A Mental Health Policy for Everyone’.


The event was attended by 125 people involved in progressing the implementation of the national mental health policy. The audience included sta and colleagues from across the health services and related areas, Government departments, as well as representatives from the voluntary and community sector, many of whom work in partnership with the HSE.

Significant progress has been made on some of the 100 recommendations in Sharing the Vision over the last 12 months.
These include:




• developments in areas such as digital mental health, including HSE online guided cognitive behavioural therapy (CBT) (Recommendation 16)
• the establishment of the Women’s Mental Health Specialist
Group and subsequent publication of the group’s report (Recommendation 3)
• investment in a number of mental health clinical care programmes, including Early Intervention in Psychosis (Recommendation 52)
• the development of forensic mental health services, including the opening of the National Forensic Mental Health Hospital (Recommendations 47, 54, 56)
“This time last year the first of three implementation plans for Sharing the Vision was launched. Our goal then was, and still is, to provide a modern and enhanced mental health service that meets the needs of the entire population. In the last 12 months alone we have seen a huge investment in mental health and while we have a long road ahead in delivering Sharing the Vision I am heartened by the progress that has been made to date, in not only improving our mental health services but in making them more accessible to people who need them," said Minister Butler.
“Mental health is everyone’s business and collaboration across the entire health service is key. In my previous role within the HSE I was acutely aware of the need for joined up services. Sharing the Vision is a wonderful example of how the services within the HSE are working together to provide person centred care at all levels. In my role as CEO I am committed to supporting the work being undertaken to ensure that policy becomes practice.”
Other contributions at the event came from Dr Colm Henry, Chief Clinical O cer, HSE; Gregor Henderson, international mental health advisor; Professor Philip Dodd, mental health policy and clinical specialist, Department of Health; Siobhan McArdle, Assistant Secretary, Department of Health; and John Saunders, Chair, National Monitoring and Implementation Committee (NIMC).
Members of the Sharing the Vision reference group also contributed on the day, to share a personal perspective on the policy.
And the following presentations highlighted Sharing the Vision in action:
• Making the Connections, HSE national mental health literacy campaign (Roisin Guiry, HSE Communications)
• Digital developments in mental health (Derek Chambers, HSE)
• Women’s Mental Health Specialist Group (Professor Siobhan MacHale, College of Psychiatrists of Ireland)
• Regional Psychosocial Supports (Dr Caoilfhionn O’Riordan, HSE Social Inclusion Psychology)
• Foróige’s Big Brother, Big Sister programme (Mary Lynch, Foróige)
• Early Intervention in Psychosis programme (Dr Karen O’Connor, HSE)
• Youth Mental Health Transitions Specialist Group (Mark Smyth, HSE CAMHS)
Jim Ryan, Head of Operations, HSE Mental Health, and chair of the HSE Implementation Group (HIG) said, “I have seen first-hand the dedication of our sta working in mental health services who go above and beyond to provide a safe and e ective service, and who are working with us as we modernise our mental health services.
“In the last 12 months our policy implementation team has established 10 workstreams which will enable us to e ectively deliver on all 100 recommendations within Sharing the Vision. We know improvements still need to be made and Sharing the Vision provides a framework in which we can implement real change. Through the HSE implementation group (HIG), we will continue to drive the implementation through e ective interagency and interdepartmental collaboration.”
You can read more about Sharing the Vision and view the quarterly implementation reports, at hse.ie/sharingthevision.
If you would like to keep up to date with news and events related to Sharing the Vision, please email us on sharingthevision@hse.ie and we will add you to our mailing list.
The opening of the new Central Mental Hospital (CMH) in the National Forensic Mental Health Service (NFMHS) Portrane, Co Dublin heralds a new era in mental health services and forensic mental health in Ireland.
The relocation of the CMH in Dundrum to this new state-of-the-art, purpose-built facility, is a major achievement in the development of mental health services. It is Ireland’s largest capital project and cost in the region of €200m. The new facility will provide care for 130 patients, and has capacity to care for 170 patients on campus when fully-operational in the future, as well as community and prison in-reach services. The hospital also has a Forensic Child and Adolescent Mental Health Service (FCAMHS) and an Intensive Care Rehabilitation Unit (ICRU) on site.
For 175 years, the CMH operated as a therapeutic facility run under a hospital ethos and o ered a range of forensic mental health services to its patients. It is the only centre in the Republic to provide specialist forensic psychiatric treatment for acute, medium and longer-term psychiatric care. Now it moves to a new purpose-built facility by the sea in north county Dublin.
Patrick Bergin, Head of Service at NFMHS, said, “The opening of the Central Mental Hospital in Portrane as part of the National Forensic Mental Health Service is a key milestone in the delivery of a modern forensic service to our patients. We now have the opportunity to be a centre of excellence and evolve our delivery of treatment and care for patients further. This is a welcome day for patients, family/ carers and our sta and this new facility provides us with opportunities to be a world leader in this specialist field.”
The design concept for the new facility is to support the underlying roles of therapeutic care and security with dignity, delivering a unique world class hospital embodying the best principles of high secure mental healthcare design. 130 single patient bedrooms are laid out in small wards around shared indoor and outdoor spaces, in which collective activities and therapies take place. A ‘village centre’ provides shared recreational facilities, including a horticultural area, a gym, a woodwork workshop and a music room, while a series of courtyards and secure perimeter gardens allow patients direct access to nature from each ward. The village centre also houses mental health therapeutic services, a GP and a dentist.
The NFMHS plans on being fully operational by 2024. The recruitment of nursing and health care professionals across a range of disciplines is ongoing with additional sta expected to be in place over the course of 2023.
“THIS TIME LAST YEAR THE FIRST OF THREE IMPLEMENTATION PLANS FOR SHARING THE VISION WAS LAUNCHED. OUR GOAL THEN WAS, AND STILL IS, TO PROVIDE A MODERN AND ENHANCED MENTAL HEALTH SERVICE THAT MEETS THE NEEDS OF THE ENTIRE POPULATION."
Why
Training and education are key components in improving national Quality and Patient Safety (QPS) and at present there is a wonderful opportunity to build a shared consensus around QPS-related knowledge, skills, abilities, and behaviours required to deliver safe, quality care within the Irish healthcare system.
A national QPS competency framework will support and inform national educational and training programmes and will inform how we can best prepare sta for engagement in QPS work in practice. Its aim is to standardise the approach to building QPS competencies across the healthcare system and to provide a guide for evidence-based resources to support people to continually assess and develop their competence in QPS.
The HSE, in collaboration with colleagues at University College Dublin (UCD), is working on this two-year project to define what components should constitute the relevant competencies to support staff, students and patient partners in education, training and engagement in QPS activities. This is a collaborative research project led by Dr Mary Browne from the National Quality and Patient Safety Directorate of the HSE (NQPSD HSE) in Ireland and Dr Aoife De Brún at the UCD Centre for Interdisciplinary Research, Education, and Innovation in Health Systems (UCD IRIS Centre), School of Nursing, Midwifery and Health Systems, UCD.
How are we developing this QPS framework?
Work has commenced to collaboratively develop an evidence based QPS competency framework for sta , students, and patient partners to identify the competencies required to support them in delivering quality safe care. This research aims to co-design an evidence based QPS competency framework by harnessing available knowledge internationally, learning from stakeholders in the Irish system and determining through co-design the structure and content to best prepare the health workforce to engage in QPS at all levels in the Irish healthcare system.
What are the benefits?
We believe there are many benefits of a QPS competency framework in building a collection of competencies that together define successful performance and development for an organisation. There is an opportunity to promote consistency and clarity around language, key skills and competencies for QPS. This will inform sta how to integrate QPS into their work, and will support job descriptions, employee induction, and professional development in relation to QPS. It will support academic bodies to guide and inform the development of under- and post-graduate curricula. It provides an opportunity to build shared ownership for this framework, at policy level, at service delivery level, at regulatory level, and across professional groups and academic bodies.
delivery level, at regulatory level, and
"Its aim is to standardise the approach to building QPS competencies across the healthcare system."
FINDINGS FROM THIS SYSTEMATIC REVIEW OF THE TWO DECADES OF INTERNATIONAL RESEARCH
INDICATE THAT:
• exclusive breastfeeding for infants aged four to six months and older significantly lowered hospitalisation, length of stay, supplemental oxygen demand and admission to intensive care units
• non-breastfeeding practices pose a significant risk for severe RSV-associated ALRI and hospitalisation
UL Hospitals Group consultant neonatologist Prof Roy K Philip was to the fore of a major review of two decades worth of international research that suggests breastfeeding o ers protection to infants from the most severe respiratory syncytial virus (RSV)-associated illnesses of the kind that drove a huge wave in paediatric hospitalisations across Ireland and around the world prior to Christmas 2022.
The RSV-associated study was one of two pieces of research emerging from University Maternity Hospital Limerick (UMHL) that have gained international attention in the year to date, not just in academic journals but also in the pages of The New York Times.
Prof Philip and colleagues Gabriela M Mineva, Helen Purtill and Prof Colum P Dunne, have just published the report of their findings in the journal, BMJ Global Health.
The researchers contend their findings point to the need for global promotion of breastfeeding as an adjunct primary preventative measure against RSV illnesses.
There is no vaccine available for RSV-associated acute lower respiratory infections (ALRIs), for infants and children and there is no e ective or standardised treatment currently available. Costly immunoprophylaxis-based prevention, delivered via monthly injections, is available only for high-risk infants.


RSV is a contagious virus that in most infants infects the upper respiratory tract, with symptoms such as mild cough, cold or runny nose. But in approximately 25% of infants, the virus penetrates deep into the lungs and causes bronchiolitis or pneumonia, acute lower respiratory infections (ALRI) that lead in some cases to hospitalisation.
Prof Philip and colleagues’ systematic review analysed English language
research from 2000 to 2021 into exclusively or partially breastfed infants of under 12 months who developed RSV-associated ALRI. More than 1,368 studies were screened, and the final analysis drew from research undertaken in 12 countries, including a total of 16,787 infants from 31 countries.
The findings underline the results of a 2022 study by Prof Philip and colleagues from University Maternity Hospital Limerick (UMHL), the School of Medicine at University of Limerick (UL) and Dublin City University. That study, published in the peer-reviewed Maternal & Child Nutrition journal, analysed 20 years of birth data from UMHL. The paper included 10 recommendations for elevating the regional and national breastfeeding rates, currently among the lowest in the world, to more favourable international levels.
For Prof Philip, breastfeeding is the most natural feeding strategy for a baby, and the latest research provides yet another compelling reason for prioritising a national promotional campaign on breastfeeding and addressing deficits in prenatal and antenatal educational support.
“We know that breastfeeding rates, not just in the Mid West, but in Ireland, are too low. This is for a variety of reasons, and it’s important that we should not forget that for some women and infants, breastfeeding may not be possible. However, what we do know from our studies is that almost two thirds of women in UMHL are initiating breastfeeding while in hospital. However, this falls o after discharge, because the system has not done enough to support it. With investment in promotion and support showing the benefits of breastfeeding, society begins to feel that breastfeeding is a norm, and it should be our national vision to get breastfeeding initiation rates above 90%,” Prof Philip said.

Making Every Contact Count (MECC) aims to develop a culture within the health service where we use every opportunity possible to talk to patients about healthy lifestyle choices.
The areas covered include quitting smoking, reducing alcohol intake, improving their diet, increasing physical activity, managing their weight and minding their mental health and wellbeing. Such conversations can help our service users to feel supported to make healthier lifestyle choices, which helps to prevent and manage chronic diseases.

The implementation of MECC is progressing nationally, with over 8,000 HSE health professionals completing the MECC eLearning training to date. To assist the MECC national team to further enhance their implementation planning, a research project 'Making MECC Work’ was commenced in September 2020.

WHERE CAN I FIND OUT MORE ABOUT THE MECC PROGRAMME AND RESEARCH?
makingeverycontactcount.ie or contact the MECC programme at makingevery. contactcount@hse.ie
The research findings provides evidence-based recommendations to scale up implementation in the health service. The research recommendations developed with our stakeholders are presented in the Making MECC Work policy brief available at www.makingmeccwork.com/ study-outputs/
The ‘Making MECC Work’ research project was funded by HSE Health and Wellbeing and a Health Research Board Applied Partnership Award, and run by the Health Behaviour Change Research group at the University of Galway. The project sought to understand the key enablers and barriers in implementing MECC across the health service, working with the HSE MECC team to develop an evidence-based implementation strategy to optimise and scale up MECC. The implementation strategy was informed by three studies:
Study 1: Survey study of 357 healthcare professionals who had completed MECC eLearning training to determine barriers and enablers to MECC intervention delivery.
Study 2: Qualitative interview study with 36 healthcare professionals and those involved in MECC implementation to understand the individual-level and organisational-level enablers of and barriers to the implementation of MECC.
Study 3: Consensus study.
Phase 1: Online consultation with 23 key stakeholders to generate strategies to enhance MECC implementation.
Phase 2: A two-day in-person workshop with 17 key stakeholders to achieve stakeholder consensus on the strategies.
Recommendations to enhance the implementation of MECC
1. Provide dedicated time to practitioners to attend training and use MECC
2. Empower and engage management and senior sta to take responsibility for MECC delivery
3. Implement a user-friendly and integrated system of recording MECC delivery



4. Develop service directories for healthcare professionals to refer patients
5. Have local MECC champions to model best practice and share experiences
6. Have a dedicated resource centre on the MECC website with information regarding MECC training courses and contacts







7. Have a HSE national communications campaign to promote MECC to sta and patients
8. Generate and highlight evidence for the impact of MECC on patients
9. Enhance integration of MECC with undergraduate healthcare professional education
An Implementation Plan to address these recommendations is currently being developed.
The Health Service Executive (HSE) logo represents our health service. The HSE logo assures patients and the public that the information and services that carry it are trustworthy.
There is a risk to the public’s trust and confidence in the services that are o ered if they are not easily identifiable as being from the HSE.
For that reason, it is important that we adhere to our visual identity guide consistently.
Our visual identity includes a logo, font, colours and imagery styles that work together, delivering our communications in a clear and reliable way for everyone.
HSE branding is instantly recognisable and associated with trust and confidence. Using the logo means patients and the public can easily identify communications from the HSE.
Use the guidelines in any new communications. This might include stationery, reports, emails and information materials. Existing communications, signage, uniforms or printed materials do not have to be changed to meet these guidelines.


These guidelines are for use by the HSE and can be followed by all HSE-funded organisations.
HSE BRANDING WE:

• standardise how our communications look and feel
• ensure consistency across our di erent services






• build trust and confidence with our patients, the public and stakeholders
HELP AND SUPPORT
Communications teams across the country provide support and advice for HSE services and the wider health system.

HSE Communications Division
T: 01 635 2180
E: business.unit@hse.ie www.hse.ie/communications
There is a risk to the public’s trust and confidence in the services that are offered if they are not easily identifiable as the being from the HSE.
Contact your Hospital Group or Community Health Organisation Head O ce, or find contact details on: www.hse.ie/communication
Download templates at www.hse.ie/branding
The HSE Communications team have developed an easy visual identity checklist to help you. You can download it at: www.hse.ie/eng/about/who/communications/branding/visualidentity-checklist.pdf
Sepsis claims more lives than lung cancer, and more than breast cancer, bowel cancer and HIV/ AIDS combined. Sepsis causes significant morbidity and mortality. It can a ect anyone at any age. However, the very young, older adults, and those with a weakened immune system are often at higher risk.
Sepsis is a time-dependent medical emergency. Early recognition and prompt treatment is fundamental to increasing survival rates and improving outcome for survivors. It is a major burden on healthcare providers and the economy. Due to its sometimes vague clinical symptoms, sepsis is often considered a di cult condition to diagnose. The early symptoms of sepsis may include a high or low body temperature, chills, elevated heartbeat and/or breathing problems. There were 12,455 cases of sepsis documented in acute hospitals in Ireland in 2021.
The National Clinical Programme for Sepsis was established in 2014 and the first National Clinical Guideline was published. The focus of the programme is to improve early recognition, prompt management and awareness of sepsis. Much work has been progressed on education to help recognise the signs and symptoms of sepsis in adults, maternal patients and most recently paediatrics. The sepsis Assistant Directors of Nursing deliver key education to many groups inside and outside of the hospital setting. Contact details on the website www.hse.ie/ sepsis. You can also find education aids, posters, presentations and material on the website. Sepsis education modules are available on HSeLanD.
The future of the Sepsis Programme
The National Clinical Guideline for Sepsis recognises an important role for primary care in early identification and timely management of people with possible sepsis. In order for patients to have the best opportunity to survive sepsis, they need to present as early as possible to their GP or hospital and receive timely treatment. The HSE are now actively working on improving sepsis awareness in the community, where 70 to 80% of sepsis cases develop.
The HSE has appointed a GP Sepsis lead. This new postholder is engaging with GPs and developing an education programme and a protocol for the management of sepsis in general practice. The sepsis team has established a steering group to provide strategic and operational leadership, oversight and support for this objective. This steering group includes the key stakeholders in HSE primary and secondary care, academia and patient representation. The aim is to provide sepsis education to all GPs in Ireland.

13 September is World Sepsis Day. The National Sepsis team are urging all healthcare professionals to run campaigns over the month of September to raise awareness, not only to peers but to members of the public. The Sepsis team will attend the Ploughing Championships again, which has an attendance of over 250,000.

Scan the QR codes below to download the maternity, adult and paediatric information leaflets.



The National Emergency Management O ce (NEMO) and the UK Health Security Agency (UKHSA) held the first Emergo Training System (ETS) senior instructor training programme. 23 attendees successfully completed the course, including emergency management, National Ambulance Services (NAS) and emergency medicine personnel.


The ETS is a simulation system, utilised worldwide for education and training purposes including the testing of organisational preparedness and management of emergencies.
NEMO have developed an Irish version of the ETS pre-hospital and hospital sets. The ETS sets consist of magnetic symbols
representing patients, sta and resources that are placed on whiteboards to illustrate an emergency type. There is a ‘victim bank’ that represents injured patients which can be divided into categories depending on the injury type. The ETS Instructor constructs the simulation scenario based on the aims and objectives of the training or exercise. Plans to implement simulated exercises are underway and the customised sets will be utilised to deliver training/exercise sessions. NEMO has commenced engagement with acute hospitals, community services, NAS and others to prepare real-life scenarios that will allow HSE sta to gain experience in testing preparedness and managing di erent scenario types to identify gaps and further develop emergency plans.



National Clinical Guideline Number 21, 'Appropriate prescribing of psychotropic medication for non-cognitive symptoms in people with dementia’ guides the appropriate use of psychotropic medication for non-cognitive symptoms being experienced by people living with dementia in any setting.
The guideline is relevant to all doctors, nurses, pharmacists and health and social care professionals working across all settings in Ireland who provide care to people with dementia. It provides guidance and standards for improving the quality, safety and coste ectiveness of dementia care provision in Ireland.
Through engagement in Emergo simulation training, sta can evaluate their response capabilities and identify areas for improvement. The process facilitates collaboration and coordination amongst di erent teams and stakeholders involved in an emergency response. By deploying Emergo, it helps establish communication channels, clarify roles and responsibilities, and identify potential issues that may arise during an emergency. The learning assists in refining emergency plans/procedures, ultimately improving responses to actual emergencies.
Emergo simulations are an important tool to enhance emergency preparedness, improve response capabilities, and minimise the impact of emergencies on the HSE.
Evidence from the UK and the USA shows that there is a decrease in the use of psychotropic medications for dementia after the implementation of similar guidelines. The National Dementia O ce is now rolling out National Clinical Guideline Number 21 through a comprehensive implementation plan.
A HSeLanD module, ‘Support pathways for people with non-cognitive symptoms of dementia’, developed as part of the implementation programme, is available now on HSeLanD.
A facilitator programme of education will be rolled out across a variety of settings later this year.
For the second year running, the HSE sent significant healthcare donations to countries in need as part of its Global Health Programme. The programme provides leadership in global health in Ireland, builds capacity to contribute to improving global health, and implements activities to improve healthcare and health outcomes in low and middle-income countries (LMICs) and in Ireland.
In 2021, the HSE provided much needed PPE, vaccines, and life-saving equipment to countries struggling with the COVID-19 pandemic, such as Nepal, Zambia, Brazil and Lebanon, with a total value of over €10m.
This substantial contribution was repeated in 2022 due to the continued struggle with COVID-19 in African countries and the sudden and immediate health emergency arising from the conflict in Ukraine. In 2022, medical equipment and supplies, ambulances, PPE and medicine donations totalled €8.61m.
In recognition of the importance of taking a global approach and supporting countries in crisis, the HSE Service Plan includes a key objective to continue to donate medical supplies and equipment to Ukraine and
HSE’s Global Health Programme plays key humanitarian role
THE TOTAL DONATIONS MADE UP OVER ONE MILLION ITEMS VALUED AT ¤8.62M.
countries in Africa for essential health services. Donations are made from surplus stock, and decommissioned equipment and vehicles no longer in use.
The main goal of the programme is to make an e ective contribution towards improving health in less developed countries, based on the aspiration that everyone globally has access to quality health care, and advances and practices in health are shared equitably. Its lead is Dr David Weakliam.
• Partner and collaborate with healthcare in low and middleincome countries (LMICs) to improve quality and access.



• Share and enhance learning and knowledge with LMICs to strengthen health systems.
• Promote knowledge and build capacity in global health to improve healthcare in LMICs and Ireland.
As well as evacuating seriously ill Ukrainian patients through medevac operations and establishing a health service targeted at supporting the health of Ukrainian refugees arriving in Ireland, the HSE had a central role in coordinating and donating a large number of emergency healthcare donations.
The HSE Ukraine donations coordination group was set up to provide a rapid response and to make sure donations that were needed were sourced expediently, and were tracked from the time they left the health facility or warehouse right through to the health facility in Ukraine.
By the end of March 2022, four containers of urgently needed medical supplies, equipment and pharmaceuticals and nine fully kitted ambulances had arrived in Ukraine. By the end of 2022, the HSE had delivered 16 containers and 19 HSE ambulances to Ukraine. Containers consisted of hospital instruments, medical supplies and consumables, medical equipment, pharmaceuticals, aids and appliances and PPE. The total donations made up over one million items valued at €5.46m.

Five countries in sub-Saharan Africa received 41 containers of over 31 million items of PPE in 2022, valued at €3.16m. The PPE was delivered to urban and rural health facilities across Tanzania, Kenya, Zambia, Zimbabwe and Uganda in collaboration with the respective governments and in partnership with Crown Agents, an international development organisation.

As part of the HSE partnership with the Royal College of Physicians Ireland on the EQUALS Initiative, the HSE donates surplus equipment and items to LMICs in Africa. The EQUALS initiative aims to support the development of healthcare in low to middle income countries by donating high quality, reusable medical equipment and training sta to use that equipment safely and e ectively, in hospitals and clinical settings. In 2022, two containers of equipment and PPE were sent to Zambia in support of this initiative.
European Immunisation Week (EIW) takes places every year during the last week of April, to raise awareness of the importance of vaccines for everyone’s health and wellbeing. This theme for EIW this year is The Big Catch-Up, and it aims to remind us to catch up on any missed or delayed vaccines.
Many children in Ireland and Europe right now have missed out on important vaccines like the HPV vaccine because of the COVID-19 pandemic, explained Dr Tom Barrett, senior medical o cer at the HSE National Immunisation O ce.
If you missed out on a HPV vaccine, you now have a chance to get protected through the Laura Brennan HPV vaccine catch-up programme," he said. “Both boys and girls are recommended to get vaccinated against the human papillomavirus (HPV). HPV is a major cause of cancers in young boys and men so it is very important that they get vaccinated too,” he said.
Up to a quarter of cancers caused by HPV are seen in men every year
HPV is a common virus. In most people, it does not cause any problems. However, HPV infection can be very serious. “HPV is a leading cause of cervical cancer. But it can also cause other cancers. For example, in boys, HPV infection can lead to cancer of the anus, penis and head and neck. HPV can also cause genital warts in both boys and girls”.
Each year in Ireland, HPV causes 406 cancers in both men and women. Up to a quarter of these cancers caused by HPV are seen in men.
Visit hpv.ie
more information about the HPV vaccine and the Laura Brennan HPV vaccine catch-up programme
VACCINATION IS THE BEST WAY
The HPV vaccine gives young people the best protection from HPV and HPV-related cancers. For boys and men in particular, the vaccine protects against nine out of 10 anal cancers, says Dr Barrett. The vaccine is safe and effective. Over 550,000 people in Ireland have been vaccinated against HPV.
“For boys and men aged 16 or older that missed out on a HPV vaccine, there is an opportunity now for them to get protected through the Laura Brennan catchup programme. The vaccine is their best protection against the cancers HPV cause, so it is so important they catch up too.”
The Laura Brennan HPV vaccine catch-up programme gives young people a chance to get a free HPV vaccine if they missed out.

“You can check if you are eligible for the catch-up programme and book a HPV vaccine catch-up appointment online at hpv. ie,” he said.
“The HPV vaccine saves lives. We know that health and care workers are a trusted source of vaccine information. We are asking you to encourage those eligible, including men and parents of young boys, to get vaccinated. The more people that get vaccinated against HPV, the closer we become to eliminating HPV infection and HPV-related cancers.”
“We know that for women and people with a cervix, almost all cases of cervical cancer are caused by HPV. But it is important to know that HPV is a major cause of cancers in men too and the HPV vaccine is their best protection against these cancers,” said Dr Barrett.
The global healthcare sector has a significant role to play in tackling the climate crisis, the loss of biodiversity and pollution. If the international health industry were a country, it would be the fifth-largest carbon emitter in the world.
The HSE recognises it has a significant role to play to become a more sustainable healthcare provider. As Ireland's largest public body, it can help tackle the climate crisis by dealing with the growing health impacts of climate change and by curbing emissions.
At the recent launch of the HSE Climate Action Strategy (2023-2050), Dr Philip Crowley, HSE National Director for Strategy and Research, said, “We are delighted to have recently published the HSE Climate Action Strategy. The reality is that the climate crisis is a health crisis and the healthcare sector is a considerable contributor to net global emissions estimated to be between 5 and 15%.”
The strategy is intended to provide readers with a clear climate action roadmap which outlines how the HSE intends to put Ireland on a more sustainable path, cut emissions, create a healthier, cleaner, and greener society, and help protect and prepare the population from the health consequences of climate change. To do this, the HSE will reduce Scope 1 and 2 emissions, while also reviewing and addressing Scope 3 emissions - including services, procurement, and others. Climate adaptation measures will also remain a focus, prioritising disease prevention, health promotion and public health services.
This srategy represents a step-change in intent on climate change and sustainability. It critically seeks to build on the existing progress within the HSE, including the already established Capital and Estates Climate Action and Sustainability O ce, and the Energy Teams in place across the country, together with the work of the HSE Health and Wellbeing Team and the many other examples of local action and leadership shown to date.


In recent years, the HSE has made strong progress on measuring and improving the environmental footprint and energy usage of the HSE Estate. Further details can be found in Capital and Estates’ Infrastructure Decarbonisation Roadmap on www.hse.ie which outlines the detailed actions to decarbonise our built environment.

The HSE is committed to achieving net-zero emissions no later than 2050, delivering healthcare which is environmentally and socially sustainable
To achieve our vision, we have outlined six priority areas of focus [as outlined above] with 10 corresponded and interconnected strategic objectives. The implementation of thestrategy will be enabled by the development of a suite of frameworks and supporting implementation plans targeting priority areas that will encourage and support climate action and sustainability activities at a local level.
As we deliver our strategy, we will measure and report on key metrics, internal benchmarks and set targets to continually improve our performance. We will also review our strategy annually and update, where necessary, as additional guidance and policy information becomes available, carbon hotspots are identified and when specific targets are made more granular and timebound.

The HSE Climate Action Strategy (2023-2050) seeks to build on the existing progress within the HSE and support and promote a positive cultural change making sustainability part of day-to-day work.
The HSE appreciates and looks forward to the significant role it will play in tackling the climate crisis, helping to reverse biodiversity loss, limit pollution and support and protect the health and wellbeing of future generations. Our workforce is central to the successful development and delivery of this strategy. We hope to enable and support sta and service users to act as sustainability and climate action activists and lead the transformation to make the Health Service a more sustainable provider.









• Established the Capital and Estates, Climate Action and Sustainability O ce in 2021.










• Published the HSE’s Infrastructure Decarbonisation Roadmap,which outlines our approach to achieving the energy and building-related emissions targets set out in the Governments Climate Action Plan. It also addresses strategic objectives of the HSE Capital and Estates Strategy and the HSE Climate Action Strategy.

• Developed a joint three-year rolling Capital Funded Partnership Agreement with Sustainable Energy Authority of Ireland (SEAI).
• Progressed the collation and consolidation of energy usage data.







• Commenced a Meter Improvement Programme comprising of the collation of improved metered data and utility supplier data, and including integration with the new National Estates Information System (NEIS).
• Established three Regional Energy Bureaus and employed 11 energy o cers to support local energy management teams at our significant energy users, with 112 energy teams in place.
• Implemented a Shallow Retrofit Energy Minor Capital Upgrade Programme to support the work of energy management teams.
• Engaged with stakeholders in relation to exploring district heating opportunities in the greater Dublin area
• Adapted and Implemented an Energy E cient Design and Towards Carbon Zero Design methodology on all new and replacement buildings on the HSE’s Capital Plan.









• Commenced a Pilot Pathfinder Programme, in partnership with SEAI, progressing detailed design at 10 representative sites by a broad base of design experts to develop a report on viable deep energy retrofit solutions to meet climate targets.
• Commenced development of an online sustainability assessment tool for smaller healthcare sites, providing support and guidance on energy, carbon, water and waste reduction.
• Commenced rollout of water conservation and waste prevention training through the HSEs Green Healthcare Programme.
“We are delighted to have recently published the HSE Climate Action Strategy. The reality is that the climate crisis is a health crisis and the healthcare sector is a considerable contributor to net global emissions estimated to be between 5 and 15%.”
The inaugural National HR Conference ‘Enhancing Healthcare Delivery through our People’ was hosted recently. It celebrated the strong foundations that HR teams in the health services are working from and provided the opportunity to acknowledge and embrace the challenges that lie ahead.
The conference also aimed to share ideas and learn from innovations and shared experiences in developing the role of HR in the health services. This will allow HR practitioners to continue to empower all sta to provide better, safer healthcare.
Anne Marie Hoey, National Director of













dedicated to HSE’s Resourcing Strategy, and actions to recruit and retain sta which were delivered by Philippa Withero, Liz Roche and Eithne Fox. A series of parallel workshops focusing on ‘Building a Psychosocial Safety Climate’, were provided by Nodlaig Carroll and Morgan Lucey from the HSE Workplace Health and Wellbeing Unit. The workshops included ‘Probation, Policies and Formal Processes’ delivered by Graham Finlay from the HSE Corporate Employee Relations team and ‘Shaping your Organisational Culture,’ delivered by Vera Kelly, Capability and Culture. The parallel workshops were chaired by Enda Maloney, Janice Benson and Margaret Sorohan.
HR, provided the opening address and welcomed 230 delegates to hear key notes from Bernard Gloster, Caroline Beardall, Prof Ciaran O’ Boyle and Simon Haigh.

The conference programme served to re-a rm to the HR delegates in attendance that their commitment to working with health services sta was a fundamental part of supporting the HSE values and of working collectively to make the HSE an employer of choice.
The health service is faced with the worldwide challenges of increased competition for the healthcare workforce and during the conference attention was placed on supporting and enabling our HR teams to implement the new model of recruitment. The conference was an opportunity to share with those attending the progress being made across our health services and the plans for the future.
The morning sessions, moderated by Sonia Shortt and Anne Curley, commenced with a presentation by Jo Shortt on the introduction of Health Regions followed by presentations
In the afternoon session, moderated by John Delamere, ICT Developments and Robotics, ICT enablers to support HR performance were discussed by Tom La an and Kevin Kelly.
The programme gave participants the opportunity to reflect on the role of HR in the health service and their shared purposes. It o ered information on practical supports, overviews of new directions in culture development, attraction and retention, and also provided information on the new Health Region structure.
Thanks to the organising committee led by Theresa Heller – Liz Roche, Mary Hanley, Gillian Ledwidge Dunne, Janice Benson, Graham Finlay, Marie O’Sullivan, Heather Whelan, Agnieszka Kobus and Andrew Lynch and all who supported on the day.

The Performance Achievement (PA) process was introduced in January 2020 for all staff in the HSE and Funded Agencies of the HSE, with the endorsement of all Staff Representative Groups and Trade Unions, across all grades and disciplines. The engagement of all healthcare staff in the Performance Achievement process continues to be a top priority for the CEO, the Senior Management Team and the HSE Board.
PA is focused on the conversation between the staff member and their line manager in the context of the work they do. The objective is to provide greater opportunity for staff engagement and to improve organisation performance through the development of staff skills and capabilities.
Therefore, PA is a forward-looking process that empowers staff. It is about your current role and what you and your manager can do together to improve the service we each provide to our service users in line with the goals of the organisation. It is an opportunity for staff members to engage with their line manager, to agree learning and development needs and identify training opportunities to achieve job, career and service related goals.
The Performance Achievement Hub on www.HSeLanD.ie has many resources, videos, tools and templates to guide line managers and teams through the process.
As a part of their ongoing role to support staff members and line managers in the adoption of the PA process nationally, the Office of the Corporate Business Partner (National HR) have been delivering learning sessions across acute services, community service and national services to highlight the benefits of the Performance Achievement process. These have been delivered both in person and virtually and are focused on providing an overview of PA: benefits to the individual, organisation and service user; and practical solutions to overcome any local implementation challenges. The National HR team have also greatly benefitted by receiving feedback from staff members and line manager to enable continuous improvement of the Performance Achievement process. Effective performance achievement improves health service delivery for the benefit of patients and the population. Some
of the other benefits of PA reinforced during the learning sessions include:
• increased engagement between staff members and their line managers, and increased support and development of the skills, knowledge and capabilities of our staff;
• enhanced staff confidence in the performance of their role which increases job satisfaction;
• setting goals and targets for the individual and the wider team, empowering staff and encouraging innovation.
As well as the benefits to staff members and line managers, there are also a number of broader benefits, including healthcare system benefits and organisational financial benefits (reduced turnover, improved value for money).
While it is acknowledged that many of the professions and services within the HSE undertake performance or engagement meetings regularly using templates appropriate for the objectives of the process, PA is the only mandatory engagement process in the HSE.
The Professional Development Planning (PDP) Framework for Nurses and Midwives (2017) has been revised in the context of the HSE PA process. A cross-service and cross-sectoral National Oversight Group concurred that nurses and midwives will now use the PDP for the HSE PA. The digital PDP has also been revised to support PA reporting. A suite of resources have been developed and are available on HSeLanD to support implementation, including line manager support on https:// pdp.hseland.ie/Resources.
The implementation of the PDP as PA coincided with International Day of the Midwife and International Nurse Day in May. The ONMSD and HSE HR are available to support services with implementation of PDP as PA. The ONMSD Clinical Programme Implementation and Professional Development and the HSE HR Performance Achievement teams are available to support services. For further information, please contact andrew. lynch2@hse.ie (Performance Achievement)
Line managers across all disciplines and grades are requested to have at least one performance achievement meeting per year with each of their team members as soon as possible. The National HR team are available to discuss the delivery of additional Performance Achievement Learning Sessions nationwide.
In our autumn edition, we shared an update on a new Recruitment Reform and Resourcing Programme of work, which commenced in summer 2022. This programme aims to support our services to enhance their recruitment capability and retain, attract and build the workforce that we need to support our patients, service users and their families, and enable us to implement new service developments such as Sláintecare and models of integrated care. It brings together our ongoing work to develop, improve and digitise our recruitment processes, with a new resourcing programme.
In the past three years, our services have demonstrated incredible commitment and resilience in the most difficult of circumstances, truly living our values of care, compassion, trust and learning.

During this time, our recruitment colleagues have worked hard to grow our workforce, adding 17,400 WTE since 2019 to enable us to respond to service demand and service developments.
Recruitment is a critical part of how we will continue to grow and develop our workforce.
To date, the Digital Recruitment Improvements Programme has focused on supporting the transition to the new Recruitment Operating Model, along with enhancing the quality and success of recruitment across the health service.
In addition to this important work, we must also develop our approach to how we resource our services safely and sustainably and consider how we encourage and support our colleagues to remain within our services and to build their careers with us.
To chart a path forward, the Resourcing Programme has worked closely with over 80 representatives from across our services, professions and care groups. Our colleagues generously brought their lived experience to share the resourcing challenges they are facing within our services, which can be grouped as follows:
The Resourcing Actions are focused on engaging, retaining, developing and supporting our colleagues as part of a holistic approach.
Representatives from our services and professions then worked to identify the resourcing actions that we need to take collectively to address these significant resourcing challenges. The Resourcing actions are focused on engaging, retaining, developing and supporting our colleagues as part of a holistic approach.
To date, a total of 112 resourcing actions have been identified and now form the first HSE Resourcing Strategy. These actions, created by our colleagues, aim to grow our workforce and have a positive impact on the experiences of our colleagues, service users and their families.
Implementation of these resourcing actions has commenced, with 27 prioritised for implementation in the first phase. At every step of the way, this will be led by colleagues in our services and professions, to ensure that the rich experience of those working in each staff category is at the forefront of our approach. This is envisaged to be a multi-year programme. We are at the beginning of our journey and are setting the foundations to ensure that our services and professions are set up for success in the future.
Since our last update in winter 2022, the Digital Recruitment Improvements Programme has continued to develop, improve and
digitise our recruitment processes to support our services in recruiting the significant numbers of staff that we need to deliver our services.
In November 2022, the Recruitment Gateway was launched. The Gateway offers a digital job order form to request recruitment support and speed up the recruitment process for services and recruitment teams.
A dedicated support team has worked with users and HR teams post go live to resolve issues and implement system enhancements based on user feedback.
Additionally, on 17 April 2023, National HR successfully launched the HSE Career Hub. This is a new portal where interested candidates can register to get weekly job alerts for suitable job vacancies advertised on the HSE Jobs page.
Key benefits of the Career Hub include:

• growing the talent pool of candidates for our services
• building the talent pool of candidates who are interested in working for the HSE
In further phases, the Career Hub will be expanded to offer additional benefits to services including providing additional candidate data to recruitment teams, and by developing information and interactive career pathways for existing staff.
Should you wish to find further information on the Resourcing Programme, please visit HSELanD https://www.hseland.ie [Go to Hubs
> Discovery Zone > Human Resources > Resourcing Programme]
For further information on the Recruitment Gateway, please contact askNRS@hse.ie for any support. Access to the Recruitment Gateway can be requested here. Work will continue to progress across both Programmes of work and further updates will be shared in due course.














Akey objective of the National Service Plan 2023 is to accelerate infrastructure development to support service delivery. The dynamic programme of work by HSE Capital and Estates is being progressed at pace and is central to the commitment of creating a high-quality physical environment across the healthcare estate. In this edition, we highlight some new developments that showcase the provision of high-quality healthcare infrastructure which will support current and future service needs.
In December last year, the HSE entered a public private partnership (PPP) to design, build, finance, operate and maintain seven community nursing units (CNUs) across Ireland. These residential care facilities include both short and long stay beds for older persons. They will be delivered in Midleton, Co Cork; Killarney, Co Kerry; St Finbarr’s Hospital, Co Cork; Clonmel, Co Tipperary; Thomastown, Co Kilkenny; Athlone, Co Westmeath and Ardee, Co Louth. Construction is expected to be completed over a two-year period with all seven CNUs delivered by the end of 2024.

The CNUs will range in size from 50 bed to 130 bed units. In total the facilities will deliver 530 beds with en-suite accommodation for all residents. The brand new energye cient CNUs will include both single and twin bedrooms, dining, recreational and care rooms, overnight accommodation for family visits, and clinical treatment, physiotherapy and occupational health facilities.
The new CNUs will replace existing facilities and have been designed to create a person-centred ethos. The aim is to provide the opportunity and supports required for residents to continue to direct their own lives in accordance with their cognitive and physical abilities in an environment which reflects the comforts of home.
Elaine Maye, Project Director, HSE Capital and Estates, said, "We are delighted the project has reached this stage of delivery, we now have contractors mobilised on all seven of the CNU sites. Projects of this size and scale take a great deal of planning, successful delivery requires the involvement, commitment and dedication of many stakeholders. Like many others, this project faced challenges along the way including dealing with the impact of COVID-19 and other challenges such as the war in Ukraine. The key to resolving those challenges has been our ability to work closely with all our stakeholders.”
Elaine went on to say that this project was a “great example of successful collaboration across the public sector. HSE Capital and Estates worked closely with our colleagues in HSE Services for Older Persons to design and develop the project requirements. PPPs are complex contractual structures requiring a range of expertise to enable their successful delivery. In that context, the HSE has worked in close collaboration with the National Treasury Management Agency and the Departments of Health, Finance and Public Expenditure and Reform. It is through the e orts of all these parties that the HSE was able to successfully conclude the planning stage and sign the PPP contract for delivery of the seven CNUs by the PPP provider.”
The new €67m radiation oncology facility at University Hospital Galway is a state-of-the-art unit for the treatment of cancer. The 8,060m2 facility includes bunkers for six linear accelerators and support accommodation, a HDR brachytherapy suite, superficial therapy unit, MRI Suite, 2 CT scanners, on-treatment support, technical and administration support accommodation. Works were carried out on an active hospital campus site and involved the design, construction and equipping of a highly serviced building with links to the existing hospital building via a link corridor. The building will be the main facility for the provision of radiotherapy treatments to patients from the west of Ireland.

 The new €67m Radiation Oncology facility at University Hospital Galway.
The new €67m Radiation Oncology facility at University Hospital Galway.
"Like many others, this project faced challenges along the way including dealing with the impact of COVID-19 and other challenges such as the war in Ukraine."

Behind every piece of personal data lies a person. Their personal information can be sensitive and deserves to be treated respectfully and in accordance with the law. Information governance, in a healthcare setting, is all about ensuring that healthcare organisations collect and use personal information in accordance with high standards. This involves designing and implementing systems, structures, policies and procedures that ensure personal health information is handled legally, securely, e ciently and e ectively in a manner that delivers the best possible care to the service-user.
Information governance practitioners aim to maintain the confidentiality, availability, and integrity of personal information. That means we work to ensure that personal information is only disclosed to those who need it; that it is of su cient quality to be used appropriately for the healthcare provider’s objectives; and that it is readily available and accessible to be used by the healthcare provider in delivering its service.
Good information governance is a core feature of patient safety and quality. In the context of the National Screening Service (NSS) and its four programmes - BreastCheck, BowelScreen, CervicalCheck and Diabetic RetinaScreen - a safe and high-quality population screening programme processes significant volumes of personal information.
The systems in place must ensure that the right person gets invited to the right screening at the right time, and that their journey is managed from invitation, to screening, to access to diagnostic services and onwards to treatment if required. The success of the screening programme is significantly dependent on the quality of the data in that system.
To support the system, we need robust structures of management and oversight that assure data quality, comply with regulatory standards for information management, as well as an organisational culture that is aligned to continually improving its practices.
Within the NSS we have 1.8m people actively engaged with our programmes – 51% of the adult population. We have a responsibility towards those participants to safeguard their data and use it to improve the quality of our services.
In its guidance on information governance, the Health Information and Quality Authority (HIQA) notes that ‘accurate, relevant and timely data is essential in order to improve health and social care, to inform decision-making, monitor diseases, organise services, inform policymaking, conduct high-quality research and plan for future health and social care needs’. In short: good information governance contributes to improving patient care and keeping people safe.
Over the last two years, the NSS has been building an information governance framework that aims to:
• build an organisational structure to achieve compliance with regulatory requirements and best practice in data management
• increase awareness and confidence among sta about how to manage patient data appropriately
• enhance trust in the e ectiveness of our management of data
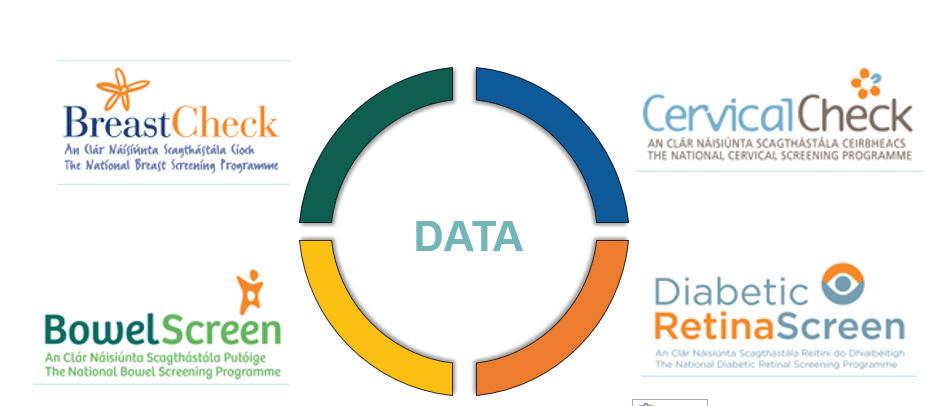
• ensure the confidentiality, availability and integrity of the data we hold, process, and share to achieve our healthcare objectives.
To achieve this, we developed a crossfunctional project steering team and mapped our current compliance against HIQA’s information management standards. This helped to define a project plan with 68 actions across nine work packages. Through completing these actions, we have developed our information governance framework for the NSS.


One of the key commitments of the HSE Patient Safety Strategy states, “We will work to embed a culture of learning and improvement that is compassionate, just, fair and open … Sta must be actively encouraged to speak up for safety, feel psychologically safe, be involved in decisions which a ect the safe delivery of care…”


Just Culture is defined in the HSE Incident Management Framework as a values-based supportive model of shared accountability which recognises that individual sta should not be held accountable for system failings. Instead, organisations carry a level of accountability for its safety culture and need to encourage sta to report incidents and near-misses and apply system-learning to improve safety.
To set us on our collective journey towards the implementation of a sustainable Just Culture, a conference entitled Building a Just Culture in Healthcare: a HSE Dialogue was held in Croke Park on Wednesday 23 May.


Addressing the audience, Bernard Gloster, CEO, HSE, said, “We are committed to creating a compassionate, just, fair and open culture where our sta are actively encouraged to report incidents or raise issues that pose a risk to the safety of patients. This provides opportunities to learn from such events and supports us in delivering high-quality and safe patient care. A Just Culture also ensures open and honest communication, which helps us build trust among our patients and stakeholders.”
Opening the conference, Dr Colm Henry, Chief Clinical O cer, HSE, spoke about the importance of support for Just Culture at leadership level and across the organisation, through clinical, strategic and operational representation.
Dr Orla Healy, National Clinical Director for National Quality and Patient Safety Directorate (NQPSD), defined Just Culture and introduced stakeholder representatives, Joan Johnston, Patient Partner; Deirdre Naughton, Director of Midwifery, Portiuncula University Hospital; Dr Suzanne Crowe, President, Irish Medical Council; and Gerry Clerkin, Head of QSSI, who described why the implementation of a Just Culture is important to them and their stakeholder groups.
This was followed by Dr Barry Lyons, Paediatric Anaesthesiologist, CHI, who spoke about his research in relation to shame and vulnerability in relation to healthcare sta and the impact of being involved in incidents has on them.

Roisin Guiry, Senior Communications Manager, HSE, described current work in building trust and confidence in the HSE. This work was highlighted as central to the culture change required for the implementation of a just, open and transparent culture.

Key note speakers, Amanda Oates, Executive Director of Workforce, and Joe Rafferty, Chief Executive of Mersey Care NHS Foundation Trust, provided an overview of the Mersey Care Trust experience of implementing Just Culture including the challenges, barriers and opportunities. The outcomes, successes and lessons learned were discussed and key actions for the implementation of Just Culture were described. Their experience has been extremely positive and we look forward to applying their learning in our HSE.

Prof Marie Ward, Health Systems Learning and Research Facilitator, St James's Hospital, and Prof Sam Cromie, Director of the Centre for Innovative Human Systems at Trinity College, spoke about current research and thinking in relation to the implementation of Just Culture and its relationship with how people make judgments around culpability. The research is helping us understand current barriers and perceptions of staff, media and the public.
Lorraine Schwanberg, Assistant National Director, and Dr Samantha Hughes, QPS Incident Management Team, outlined that in the HSE we do not want to compound harm from incident reviews on those involved and that there are already building blocks in place in the HSE to support the implementation of a Just Culture. We need to join up collectively and enhance the good work already being implemented to support a Just Culture and improve psychological safety to support our staff and colleagues. It was acknowledged that the most recent HSE Staff Survey highlighted that 44% of respondents felt they were not treated fairly following an incident and, as an organisation, we need to understand why this is so.
The day concluded with a panel session, facilitated by Dr John Fitzsimons, involving the key note speakers and other speakers from the day. Included was Damien Mc Callion, HSE Chief Operations Officer, who, along with the panel, discussed essential actions that needed to be implemented by their teams and services to commence/ continue their Just Culture journey.
A poster submitted by UL Hospital Group, entitled ‘This is not about shame and blame; this is about changing the game- Experience of organisational support and feedback succeeding an adverse event’ was a worthy winner of the poster competition.
Dr Healy, closed the conference, thanked all for their active participation and honest discussions in relation to the requirement and the challenges to implementing a true Just Culture in the HSE.
“WE ARE COMMITTED TO CREATING A COMPASSIONATE, JUST, FAIR AND OPEN CULTURE WHERE OUR STAFF ARE ACTIVELY ENCOURAGED TO REPORT INCIDENTS OR RAISE ISSUES THAT POSE A RISK TO THE SAFETY OF PATIENTS."Keynote speakers Amanda Oates, Executive Director of Workforce, and Joe Rafferty, Chief Executive of Mersey Care NHS Foundation Trust.
The HSE launched the first two Managed Clinical Rehabilitation Networks (MCRNS) for those living within Community Healthcare East and Community Healthcare Dublin South, Kildare and West Wicklow catchment areas.
These are the first networks in the country that bring together specialist neuro-rehabilitation services. Neuro-rehabilitation is a term used for a range of various services and supports that assist people after serious neurological illness or injury. It improves health outcomes, reduces disability and improves quality of life.
There is one referral form for all services within the network. This referral form is received by a network rehabilitation coordinator who directs the referral to the most appropriate service within the network. This will increase equitable access for people to specialist neuro-rehabilitation services to meet their needs.
These networks consist of the National Rehabilitation Hospital (Level 1) providing complex specialist neuro-rehabilitation and local specialist
inpatient neuro-rehabilitation services (Level 2) at Peamount Healthcare and the Royal Hospital in Donnybrook. In the coming months, Community Neuro-Rehabilitation Teams (CNRTs) will be added to these networks of services. These teams will o er an intensive period of specialist neuro-rehabilitation to people within their community.
Speaking on the launch of these new services Dr Paul Carroll, Consultant in Rehabilitation Medicine and Cinical Lead for the National Clinical Programme in Rehabilitation Medicine, said, “I firstly would like to acknowledge the hard work that has gone into getting these networks up and running and to thank all those involved. We are in a resource-short environment. Through these networks we are working towards person-centred care, reducing waiting times, and making the most of services. This is a first step in building up nationwide networks. We are learning from this and we will use this learning to expand these networks nationally.”
Healthcare is constantly evolving and it's important to keep up with the latest trends and innovations in the field. However, finding the time to learn more about quality improvement can be a challenge for busy healthcare workers.
The All-Ireland podcast: Walk and Talk Improvement: Ideas for Safe Quality Care is a handy way to stay up-to-date and learn the latest in quality improvement and patient safety while on-the-go. The series shares stories from healthcare professionals across Ireland, Northern Ireland, and the UK who are leading the charge in quality improvement and patient safety e orts.
In episode 5, Human Factors: designing for people, the podcast dives into the field of human factors and how it is being used to make healthcare safer for everyone. Colleagues in Cork, Galway, and Scotland share real-life stories and experiences of using human factors in their work. You will hear stories of a former paramedic using human factors in his work and learn from the lived
experiences of colleagues in NHS Scotland. It provides valuable insights into this growing field and its potential to improve patient safety.
In episode 6, leaders in healthcare across the All-Ireland share their experiences and insights on the importance of e ective leadership and governance to improve patient safety. They share their own stories and inspirations on their quality and safety journeys, o ering listeners the chance to find their own inspiration.
Whether you're commuting to work or going for a walk, tune in and gain valuable insights from colleagues across All-Ireland who are working to make healthcare safer for everyone. Download Walk and Talk Improvement: Ideas for Safe Quality Care today and join the conversation.
Coinciding with the occurrence of National Traveller Ethnicity Day, HSE/ South East Community Healthcare o icially launched the tin-smithed copper art project involving Travellers from across counties Carlow and Kilkenny.

The project, titled ‘Gloak our Laces’ (meaning ‘look at us’), draws on themes of positive mental health and wellbeing.
It was arranged by the HSE/South East Community Healthcare’s mental health services, with support from HSE Social Inclusion O ice, working in collaboration with Traveller Projects in counties Carlow and Kilkenny.
The arts project was led out by artist Mary Cassidy and the launch took place recently in the Newpark Hotel, Kilkenny.
The ‘Gloak Our Laces’ project has been documented on a short video and the finished pieces are to feature as an exhibition at the Department of Psychiatry acute mental health inpatient facility located on the grounds of St Luke’s General Hospital Carlow/Kilkenny.
Speaking at the launch, Traveller Mental Health Co-ordinator with HSE/ South East Community Healthcare Mary Byrne said, “The project provided a space for participants to talk about minding mental health and wellbeing in a relaxed space while engaging in a shoulder to shoulder activity together,” she said.
Tallaght University Hospital (TUH) marked World Innovation Day with the launch of a new virtual resource for patients living with Long COVID. The new self-help video contains guidance from leading psychologists on how patients can cultivate psychological flexibility to support them in living meaningfully, even in the presence of ongoing symptoms.
The concept of Psychological Flexibility is drawn from a therapeutic approach - Acceptance and Commitment Therapy (ACT) - that has proven benefits for those living with a range of di erent physical and mental health conditions. Funding for this resource was provided by the Adelaide Health Foundation’s innovation fund.
Some of the most commonly reported symptoms of Long COVID include significant and disabling fatigue, cognitive dysfunction or ‘brain fog’, shortness of breath and pain; many people living with this condition also experience anxiety and low mood. Those living with Long COVID can encounter significant di iculties resuming their normal day-to-day responsibilities or returning to work. As such, the impact of Long COVID can be, and very often is, extremely distressing for those living with it and for those supporting them.
Ashley Bazin, a team leader on the oncology and haematology clinic at Tallaght University Hospital (TUH) has just won the Irish Cancer Society Support Sta of the Year Award for 2023, in recognition of her contribution to driving forward clinical trials in TUH.

Ashley (pictured right) is an experienced research nurse and has been the team leader in the clinic for over 16 years.
She says her main focus is ‘on ensuring patients have access to the best treatment options as well as engaging with Cancer Trials Ireland and pharmaceutical companies to bring promising new treatments to patients’.

Her colleagues say Ashley is integral to the operation of the unit and plays multiple roles: research nurse, team leader, manager and teacher, while always being a strong advocate for the
patients taking part in the trials. In addition to coordinating a large portfolio of oncology and haematology trials, Ashley manages the funding for the entire unit.
She supports the investigators by helping them to find patients. To do this, Ashley first meets with the patient to explain the trial.
She then stays in contact with the person during the research, ensuring their trial medicines are available and that all the necessary trial assessments are done and the valuable data recorded and saved.
One colleague noted, “Ashley is a wealth of information and a skilled trainer. She is always happy to share her knowledge and learnings with others. She really is a pleasure to work with. Very often she works outside of the scope of a team leader as she strives to bring the best options to her patients.”
The Urology Department at University Hospital Galway (UHG) has picked up a prestigious award at an international Urology Conference.

The European Association of Urology Nursing Conference took place in Milan, Italy in March. It saw the UHG Urology Department awarded second prize for setting up a clinical-academic partnered hybrid journal and research club.
The aim of the journal and research club is to provide the nursing team with a safe learning space in which to develop their research skills.
Rachael Dalton, ANP in prostate cancer, who is a journal and research club member, presented the practice development initiative at EAU23.
“Within nursing practice it is profoundly important to develop research skills. This set of skills a ords nursing teams the ability to critically review and utilise evidence-based practice within
nursing care,” she said.
The creation of the space was led by Robert McConkey, ANP in bladder cancer at Galway University Hospitals, who added, “Unfortunately there are multiple barriers to development in this area including lack of time and indeed low levels of research confidence. Creating a supportive space for the urology nursing team to develop their research skills is an important development.”
The club meets bi-weekly, alternating between research and club meetings. It has held over 30 meetings to date, critiquing 17 peer-reviewed journals. The group has published one paper within the International Journal of Urology Nursing and currently one collaborative nurse-led research study is at data analysis phase. Participant feedback has been very positive with members citing the club as a safe, non-judgemental learning space.
This project was awarded second prize at this international conference. Therese Kelly ANP in Benign LUTS accepted this award on behalf of the journal and research club members.




We all make decisions, every day of our lives.
On 26 April 2023, the Assisted DecisionMaking (Capacity) Act 2015 (the Act) was commenced. The Act gives each person the right to be assisted to make decisions with legally recognised supports regardless of disability or any condition which may a ect a person’s decision-making capacity. The Act ensures each person’s right to make autonomous and independent decisions for as long as possible.
Why is the Act important?

A core principle of the Act is that all persons should be presumed to have decision-making capacity and should be supported to make their own decisions as far as is possible. The Act emphasises minimal restriction of a person’s rights and freedoms and the importance of respect for the person’s past and present will and preferences.
Key reforms include the abolition of the wards of court system for adults under the Lunacy Regulation (Ireland) Act of 1871 and the discharge of adults from wardship within three years of the commencement of the Act.


INSET LEFT: Caoimhe Gleeson, General Manager, HSE National O ice for Human Rights and Equality Policy; Anne Rabbitte, Minister of State for Disability; Paul Alford, Inclusion Ireland, one of the champions for the Decision Support Service Campaign; Aine Flynn, Director of the Decision Support Service; and Jacqueline Grogan, Project Manager, HSE National O icer for Human Rights and Equality Policy
ABOVE: Caoimhe Gleeson and Jacqueline Grogan from the HSE National O ice for Human Rights and Equality Policy with Roderic O’Gorman, Minister for Children, Equality, Disability, Integration and Youth and Helen Rochford Brennan, global dementia ambassador and one of the champions for the Decision Support Service campaign TOP RIGHT: Event in Merrion Square on Commencement Day of the Assisted Decision-Making (Capacity) Act.


Act.





INSET RIGHT: John Farrelly, Chief Executive O icer, Mental Health Commission; Aine Flynn, Director of the Decision Support Service; and Dr Philip Crowley, National Director, Strategy and Research, HSE, at the launch of the Decision Support Service public awareness campaign.
A public body called the Decision Support Service has been established to register the new decision support arrangements and supervise the individuals who are providing a range of supports to people who may have di culties in exercising their decisionmaking capacity.
The role of the Decision Support Service is to promote public awareness of the Act and to provide information about their services. This includes providing information and guidance to people who may use this service and to their families.










The Act will provide a new tiered framework of formal supports for those who need them, with supervision by the Decision Support Service. The three levels

of supports for people who may require support with making decisions are decision-making assistants, co-decisionmakers and decision-making representatives. These decision supporters will likely be someone that the person knows and trusts, such as a family member or a close friend.
As anyone could face challenges with decision-making in their future lives, the Act provides new tools for any adult who wishes to plan ahead by way of an advance healthcare directive or an enduring power of attorney.
The Decision Support Service have published 13 Codes of Practice on the Act, including a Code for Healthcare Professionals. This Code has been developed to guide healthcare professionals in carrying out their functions and duties when interacting with a person who uses their services and who may need support to exercise their decision-making rights.


The Decision Support Service has also developed a range of accompanying materials, including a plain English guide to the codes; plain English leaflets; informational videos on each code; accessible guidance documents for people who want to make a decision support arrangement; an easy-read guide to the Act and the functions of the Decision Support Service; and materials setting out 60 di erent scenarios to help to explain how each code could apply in real-life.
What does the Act mean for healthcare professionals?
The guiding principles of the Act require healthcare workers to:
• presume every person has the capacity to make decisions about their life
• support each person as much as possible to make their own decisions
• not assume a person lacks capacity just because they are making, have made or are likely to make an ‘unwise’ decision


• take action only where it is really necessary
• take the least restrictive action on a person’s rights and freedoms
• consider how urgent the action is
• give e ect to the person’s will and preferences
• consider the views of other people
• use information appropriately
It is important to remember that this Act supports and builds on existing clinical practice and guidelines on personcentred care.
The HSE National O ce for Human Rights and Equality Policy have developed a range of resources to support your day-to-day work. These include e-Learning programmes, frequently asked questions, and webinar recordings. The development of resources and guidance will be ongoing as new issues arise over the coming months and years.

Bernard Gloster, CEO, in a video supporting the commencement of the Act, explained, “ADM is a very important step in human rights terms. It is not new… when we look across safeguarding and other aspects of the care we provide, many of these same principles… are now embodied in legislation… It is important that we move to a modern way of supporting people - assuming they have capacity, inquiring as to what their wishes are and respecting their right to selfdetermination.”
The Decision Support Service launched a public awareness campaign on the Act on 25 April in the Lighthouse Cinema, Dublin. Dr Philip Crowley, National Director, Strategy and Research, said “This is a vitally important piece of human rights legislation that many people have been waiting a long time for. The launch of the public awareness campaign is key to ensuring that as many individuals as possible are aware of this Act and the benefits that it could bring to their lives.”

Waterford Walls bring splash of colour to St Otteran’s
Two colourful murals depicting scenery around the Metal Man maritime beacons in Tramore have been produced by users of Waterford’s mental health services.


The HSE/South East Community Healthcare and the Waterford Walls project unveiled the results of a collaborative murals initiative where service users, under guidance of the service’s rehabilitation and recovery team members, have been working with Dublin-based illustrator and mural artist Juliette Viodé. Together, they have produced two colourful pieces on walls at the Grangemore residential facility, which is located on the grounds of St Otteran’s
HSE mental health management and sta , service user participants, family members of participants, representatives of Waterford Walls and the artist gathered at a reception in Grangemore to launch the completed works.
Music on the occasion was provided by the Waterford Healing Arts Trust.
Speaking at the launch, Dr Darran Flynn, Clinical Director, Waterford/Wexford Mental Health Services, said, “For us in the HSE, this is a very exciting co-production project between the clients in Grangemore, Waterford Walls and artist Juliette Viodé.
“Those of us working in the mental health services in the south east have been very impressed by what emanates from the annual Waterford Walls Festival each August. In addition to an obvious and beautifully vibrant stamp on various locations around Waterford, we were also aware of the project’s artistic exchanges and collaborations focused on connecting diverse people and communities.
powerful tool to convey emotions in visual art.”
diverse people and communities.
“HSE/South East Community Healthcare were delighted when an opportunity arose to put together a programme that enabled our mental health service users to forge their creative expression.
"As shown in this programme, colour is a

















































































































































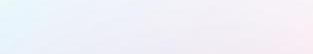



































































The Kellogg’s GAA Cúl Camps have teamed up with the HSE’s National Cancer Control Programme and Healthy Ireland to support the SunSmart campaign. The campaign aims to increase awareness of the steps you and your family can take to protect your skin from the sun and reduce your risk of skin cancer in Ireland.

As part of the campaign, coaches are undertaking training to increase their knowledge about skin cancer prevention and introducing to children to the SunSmart 5 Ss in a fun way. The coaches are able to act as positive role models for children attending the camps to encourage them to protect their skin by following the SunSmart 5 Ss when outside.
We all love the sun and taking part in sport and leisure activities are good for our physical and mental health. However while we are spending time outside we need to be careful about how much of its powerful ultraviolet (UV) rays we are exposed to. Children and young people are particularly vulnerable to the damaging e ects of the sun’s UV rays. When children are taking part in sports or playing and spending time outdoors it is important to protect their skin. If a child is badly sunburned more than three times before the age of 20, they more than double their risk of skin cancer as an adult.
In 2022, over 30 national and international artists created large-scale mural artworks around Waterford City and the surrounding areas as part of the Waterford Walls Festival, which consisted of 10 days of live art, music, workshops, guided tours and much more. The ninth annual staging of Waterford Walls, Ireland’s largest international street art festival, will take place from Friday 11 August to Sunday 20 August 2023.
Healthy Ireland’s simple SunSmart 5 Ss tell you how you can enjoy spending time outdoors in the sun, protect your skin and avoid getting sunburnt.



• Slip on clothing: We need to cover our skin as much as we can, using tops that have long sleeves to cover arms and collars to cover our neck.
• Slop on broad spectrum (UVA/UVB) sunscreen on exposed areas. Children need a stronger sunscreen than adults, with a SPF of at least 50, while adults should wear a sunscreen with a SPF of at least 30. The sunscreen used should be water resistant and be reapplied every couple of hours.
• Slap on a wide-brimmed hat: This will shade the face, ears and neck from the sun.


• Seek shade - especially if outdoors between 11am and 3pm and always use a sunshade on a child’s buggy.
• Slide on sunglasses to protect eyes. Remember even when it is cloudy you should protect your skin as the sun’s UV rays can travel through cloud.
For more information and to learn how to protect yourself and your family visit the SunSmart hub at www.hse.ie/sunsmart and check out #SunSmart on social media.
A virtual nationwide audience of thousands of secondary school students logged on to one of Ireland’s largest healthcare careers events in early March, as the Junior Health Sciences Academy at UHL opened its annual virtual Early Careers Fair for Transition Year and Fifth Year school-goers.
Hosted by the Health Sciences Academy (HSA), with Limerick and Clare Education and Training Board and Limerick Education and Support Centre (LESC), the half-day event was open to pupils in all secondary schools all over the country.

The HSA is a partnership of University of Limerick (UL), UL Hospitals Group (ULHG), and HSE Mid West Community Healthcare (MWCH), and the Junior Health Sciences Academy is a key element of this partnership. It supports students in early careers, health promotion and leadership, fulfilling the shared aim of nurturing and improving the health and wellbeing of the people of this region.

There was something for all interests, with sta , leaders, and students from the three HSA partner organisations, including doctors, nurses and midwives, paramedics and allied health professionals, delivering presentations and answering students’ questions about the huge sweep of healthcare specialties in the mid west.
Dr Philip Crowley, National Director for Strategy and Research, HSE, contributed to the inaugural Creative Brain Week which was hosted by the Global Brain Health Institute (GHBI) in Trinity College Dublin recently.
This pioneering event explored how brain science and creativity collide to seed new ideas in social development, technology, wellbeing and physical, mental and brain health throughout our lives.
Dr Crowley particularly focused on the role of arts and creativity to promote health and improve healthcare with ‘evidence that the arts contributes to the promotion of good health, and prevention of a range of mental and physical health conditions, as well as treatment and management of acute and chronic conditions’.
“For example, singing has been found to improve a sense of general wellbeing, improve quality of life, improve cognitive function, reduce depression and improve social
connectedness. Another example is the Lived Lives project in UCD that goes behind statistics and uses the art of storytelling to capture stories of some of the young lives lost to suicide in Ireland which is both very powerful and very important,” he said.
There is an increased focus and investment in arts and health within the HSE through an agreed partnership between Department of Health, Creative Ireland, The Arts Council and HSE. Dr Crowley acknowledged the challenges of developing and integrating arts in health, but also identified opportunities.
“This includes the increased need to focus on creativity and innovation to continue to improve services for the public. Also, the potential of arts and creativity to help deliver on a key area of Sláintecare in promoting health and wellbeing. Arts and health is an area we will continue to invest in the HSE and develop across all areas,” he said.
Miriam McCarthy, Health Sciences Academy Manager, said the secret of the event’s success was in how well it demonstrated the variety of career options in healthcare, as well as its ability to resonate emotionally with all young people approaching the most significant crossroads of their formative years. This year, the organisers added a new section on ‘business in health’ with the hospitals group’s director of HR and operational services manager, as well as business students from UL, talking about their roles. This enhanced the richness of the event, demonstrating the diversity of career options in healthcare outside of frontline care.
From left: Local secondary schools students join the organisers of the Junior Health Sciences Academy Early Careers Fair to show the range of healthcare career options available in the region. From left: Peter Admanski, Thomond Community College; Sophie Hartigan, Castletroy College; Rebecca Hickey, Gaelcholáiste Luimnigh;
There is an increasing urgency to make better use of data to deliver more efficient and effective services to support healthcare professionals in the delivery of care to citizens, those attending a recent Data Collaborathon were told.

The purpose of the event was to view presentations from our data colleagues in HSE on the importance of data in health and how we can collaborate to create positive impacts in our area of work. Data Collaborathon was organised for all HSE and Section 38/39 to collaborate in an environment conducive to learning from colleagues in different areas of work.
It was held in the Health Identifiers Service (HIDS) office in Southgate, Drogheda, attended by 163 health professionals.
The Data Collaborathon was organised by the Human Digital Transformation Programme, which aims to use data and digital training to equip HSE employees to understand health data, transform their data-related skillsets and capabilities in providing solutions for better health/patient outcomes.
There were a number of presentations, which focused on importance of data literacy, common challenges and opportunities in the presenter’s area of work.
Joe Ryan, National Director of Operational Performance and Integration, spoke about how data enables the nine pillars of integrated care and is universally recognised as essential to sustainable integrated care delivery.
Michael Redmond, COO EHealth, talked to those present about implementing individual solutions across healthcare and integrating them together.
Maria McCann, Director of Identity Management Services, gave an overview of the Health Identity Management Services and the Human Digital Transformation Programme.
Loretto Grogan, National Chief Nursing & Midwifery Information Office, spoke to the attendees about the person’s journey in the health system and how data can improve each aspect of that journey.
In the feedback sessions after the presentations, 70% of the participants agree that accessing good quality data can empower them to:
• improve the quality and safety of treatment
• identify risk factors and accelerate diagnosis
• make well-informed decisions
• enhance public health strategies
HSE Community Healthcare East hosted a staff Lunch and Learn event on the theme of the Enhanced Community Care (ECC) Programme. The event included a variety of speakers from different organisations and services. The aims of the event were to educate staff on what ECC is and what it means for the future of healthcare services in Ireland, to increase positive engagement in the ECC programme and help aid its implementation, and to offer staff from different services and locations a face-to-face networking opportunity.
During the first half of the event, senior managers from Community Healthcare East and IEHG introduced the concept of ECC and its strategic significance in the context of Sláintecare. The second half of the event was dedicated to frontline staff and clinicians who outlined case studies and videos of ‘ECC in Action’ to show how the Programme has benefitted our staff and service users. Both sessions allowed for an open Q&A between the audience and the speaker panel.
Clinical innovation at the Symptomatic Breast Unit at University Hospital Limerick is improving patient outcomes and quality of life, consultant surgeon Mr Chwanrow Baban has told one of Ireland’s largest medical conferences. Mr Baban, Consultant General and Oncoloplastic Breast Surgeon, UL Hospitals Group and senior lecturer in surgery at the UL School of Medicine, was a keynote speaker at the annual Sylvester O’Halloran Perioperative Symposium.
After several COVID-interrupted years during which it moved online, Ireland’s largest perioperative meeting was again held face-to-face over three days at the University of Limerick and University Hospital Limerick (UHL).
Delivering the keynote Sir Thomas Myles Lecture on ‘My Journey in Surgery and Innovation’, Mr Baban spoke of his longstanding research interests, including the standard of care for older breast cancer patients and exploring the relationship between bacteria and tumours.
More immediately, patients in the breast service Limerick were already benefiting through the introduction of new technology by Mr Baban and his colleagues.
Mr Chwanrow Baban, Consultant General and Oncoplastic Breast Surgeon and Prof Shona Tormey, Consultant Breast sSrgeon, UL Hospitals Group at the School of Medicine, University of Limerick, for the Sylvester O’Halloran Perioperative Symposium 2023. Mr Baban delivered the keynote Sir Thomas Myles Lecture on ‘My Journey in Surgery and Innovation”

The Saolta University Health Care Group held its eigth Neonatal Study Day Conference at the Clayton Hotel in Galway. Over 100 delegates from the Saolta Group and other hospitals attended.

The conference, which was organised by the neonatal team at University Hospital Galway, with special thanks to neonatal advanced nurse practitioners Jean James and Aine Binchy, provided an opportunity for the neonatal multidisciplinary team to meet face-to-face following the COVID-19 pandemic, and to share best practices, stay up to date on evidence-based practice, and learn new skills.
The conference featured speakers from the local, national, and international communities, covering a wide range of neonatal topics, which sparked a lot of questions and discussion. A number of skill stations organised and facilitated by the neonatal team, provided an excellent opportunity for delegates to update existing skill sets or consider bringing a new skill back to their respective neonatal units in order to improve and strengthen neonatal care provision.
The theme for The National Patient Safety Office (NPSO) conference was ‘Working Together for Patient Safety’ and the speakers explored collaboration for patient safety and how people are drivers of change.
The conference was chaired by Chief Nursing Officer Rachel Kenna and the day was brought to a close by the Minister for Health Stephen Donnelly. Chief Medical Officer Prof Breda Smyth and HSE Chief Clinical Officer Dr Colm Henry chaired sessions throughout the day.

The morning keynote speaker, Professor Suzette Woodward, a former paediatric intensive care nurse, spoke about perspectives on Safety II. The afternoon keynote speaker, Professor Eilish McAuliffe spoke about how to assess and cultivate psychological safety in healthcare teams.
For the first time, the QPS Talktime webinar was hosted live from Dublin Castle. In addition to a broad variety of speakers, a ‘Pearls of Change’ session, the programme included two workshops covering evidence synthesis and patient safety. There were two poster competitions, including the inaugural Students and Graduates of the Last Decade (GOLD) competition for research on Antimicrobial Resistance and Infection Prevention and Control. Organisations, including the HSE, HIQA and Patients for Patient Safety showcased their work at the conference stands.


The Saolta University Health Care Group, in collaboration with the National Women’s and Infants Health Programme, hosted a national conference titled ‘Quality, Patient Safety and Risk in Maternity and Gynaecology Services’ in Galway recently.

The conference included a nuamber of focused lectures and interactive sessions from a multidisciplinary team of experts in obstetrics, midwifery, and healthcare management, from within Saolta and at national level.
The conference featured speakers from Saolta Women’s and Children’s MCAN (Managed Clinical and Academic Network) and from other hospital groups across the country..
Prof John Morrison, Clinical Director of the Saolta Women’s and Children’s Managed Clinical and Academic Network (MCAN) thanked all those who took part in the conference.
“The conference served to share learning, promote quality of care, reduce predisposing factors for risk, and address practices aimed at a culture of attaining a high standard of care and transparency for the women and infants who are users of our services,” he added.
Dr Cliona Murphy, Clinical Director of the National Women and Infants Health Programme, said, “The quality of speakers, and the breadth of attendees from across the maternity services, demonstrated a spirit of genuine collaboration and multidisciplinary engagement.”
HSE Health and Wellbeing – Healthy Eating Active Living Programme hosted a workshop on WholeSystems Approaches to Obesity Prevention.
Sarah O’Brien, National Lead Healthy Eating Active Living Programme, facilitated the seminar. The aim of the workshop was to share insights and start a dialogue on whether taking a whole systems approach could assist with e orts to tackle the obesity pandemic in Ireland.
As well as inputs from leading experts the seminar was attended by a range of people working in health, local authority and community sector at local level and some key national stakeholders like Department of Health.

On the day Prof Donal O’Shea, HSE Clinical Lead Obesity, spoke to how most of the factors that influence obesity lie outside the control of individuals. The places where we are born, grow, live, work and age have a significant impact. Science tells us that obesity is a complex disease where weight a ects health it is a contributing factor in more than 200 other diseases.
Professor Gavin Breslin, University of Ulster, outlined the emerging evidence from systematic reviews and case studies on a Whole Systems Approach to preventing obesity. A number of areas in Northern Ireland, Scotland, Wales and England are starting to apply the approach.
Dr Jenny Mack, Public Health Specialist with Institute of Public Health, shared a rapid review of evidence to inform the new obesity policy in Northern Ireland. The review identified a range of areas where there is potential to have impact, from strengthening regulation of advertising of high fat, salt and sugar foods; improving active travel infrastructure and use of it to using taxation and subsidies to reduce consumption of unhealthy foods and promote consumption of vegetables and fruits.
A group of Patient Partners and HSE sta recently became the first group to undertake the Facilitator Education Programme o ered by the National Quality & Patient Safety Directorate, with one participant saying it gave them ‘the security and a springboard for further innovation and creativity’.

This programme is based on that developed by the National Clinical Leadership Centre and the Centres for Nursing and Midwifery Education. It consists of two ‘in-person’ days with a practice session between Day 1 and Day 2.
One participant reported that their motivation for doing the programme was ‘becoming better at getting people to talk and have conversations with others’.
“Part of our approach in Patients for Patient Safety Ireland (PFPSI) is to run workshops and we needed to have this structure and approach to do that, so for us the timing was excellent,” they said.
Another said that it was “an opportunity to really collaborate as patient partners and sta together.”
Topics included new ways of working with the group coming together to implement the Patient Engagement Roadmap. There was also a fourhour workshop on ‘Fundamentals – what you need to know’ for members and non-members of the PFPSI group.
Anyone can become a great facilitator – if they have the right tools, techniques and skills. This programme is about building and/or refreshing those skills. Information about the National Facilitator Education Programme is available here or through the QR code shown.


A self-advocacy learning event was hosted by the HSE in collaboration with Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo (CH CDLMS) Disability Services, the Disability Federation of Ireland and Inclusion Ireland in Jacksons Hotel, Ballybofey, Co Donegal.


Self-advocacy is essentially the action of communicating and representing your needs, views or interests. It is about understanding your rights, speaking up, taking action and taking control of your life. Where people cannot speak up for themselves they are supported to do so by others. E ective self-advocacy will mean that a person has good information, training, the right support when needed, opportunities to learn by doing, confidence in themselves and will understand that self-advocacy can be at an individual or group level.
Attendees at the event included self-advocates, persons accessing disability services, key workers, service and senior managers from the disability services, facilitators and sta from other HSE support services. The learning event consisted of keynote speeches and facilitated workshops.


The inaugural National Public Health Conference took place on Thursday, 27 April in Dublin. The aim of the conference was to provide an opportunity for staff to connect in a learning environment, as we continue to build upon our evidence-based ethos in the reform era of public health in Ireland. The themes of the day focused on health improvement and health service improvement, brought to life by our international keynote speakers Professor Sir Michael Marmot, Professor of Epidemiology and Public Health at UCL; and Dr Josep Figueras, Director of the European Observatory on Health Systems and Policies.
The objectives of the conference were:
• to create an opportunity for networking and shared learning amongst public health staff to learn from and engage in discussion with international experts to learn from and engage in discussion with national colleagues

Recently appointed National Director of Public Health Dr John Cuddihy reflected on the progress to date which included the establishing of six new Public Health Areas aligned to future Sláintecare health regions, led by Area Directors of Public Health, managed through Senior Leadership Teams, and delivering a consultant-led Health Protection Service in line with the Hub and Spoke model.
He outlined the out-of-hours service aligned to the six new Public Health Areas and a National Health Protection Strategy 2022-2027 launched in October 2022, enabling progress towards delivery of an integrated national health protection function with an all-hazards approach.





Get involved at understandtogether.ie

Wherever you see this symbol, there is support for people living with dementia.