QUIT SMOKING FOR GOOD








MATTERS





Celine shares her quit journey









SPRING 2023
Welcome to the latest edition of Health Matters.

No doubt, given the time of year, many of you are starting on a journey to finally give up the cigarettes. We share the inspiring story of Celine O'Shea, who is now six months smoke-free thanks to her own willpower and the support of smoking cessation officer Nuala Cody.

The theme of the new Quit campaign is to take back control and Celine has certainly done that.
In this edition, we revisit the Transforming Lives programme where people across the country are moving from congregated living to homes of their own. We find out what life is now like for three men - Seamus, Robert and Pat - who have lived most of their lives in a campus-based setting, but who have now moved to a new community home together in Co Kerry.
The trio are a firm part of their new community and go shopping, visit the church and even do their own recycling. Their family have reported a massive change in them as they revel in their independence.
Ukrainian doctor Regina Morais describes to us the welcome and support she has received since she arrived in Ireland in March last year.
She expressed her gratitude for all the work that is being done here to accommodate her and her fellow Ukrainian refugees.
Health protection nurse Leah Evans, speaks about her fascinating trip to a leprosy hotspot in Nepal and her experiences helping out there.
They are just a small number of the many stories we have for you this edition.
Once again, a big thank you to all the teams around the country who have submitted their initiatives and programmes. It is great to be able to showcase the amazing work being done to make life better for people who use our services.
Joanne Weston Editor
CONTENTS
Asthma action tools
Transforming Lives 4 AI can revolutionise healthcare industry
HSE projects scoop awards 6 Take back control and quit smoking for good 9 Mobile vaccinations 10 Care closer to home
Managing chronic conditions 11 Integrated care programme 12 Delivering Change Together 13 Time for a dip 14 Healthy Communities 16 Huge support for Pathfinder project 17 HR and Payroll Self Service 17 Community collaboration for wellbeing support 16 EAP healthcare workers and grief 17 Winning midwife 18 Milestone anniversary for addiction service 18 Infant Mental Health Masterclass in Mayo 18 150 extra meals on wheels in Clare 19 Inaugural midwifery conference 19 Team turns red for World AIDS Day 20 New neonatal unit at Crumlin 20 Education initiative 20 New forum for neurology nurses 22 A return to nursing 23 Excellence Award 23 'Life-changing' support for Ukrainian doctor 24 Visit to Nepal 26 Mental health initiatives 31 Gastroenterology triage slashes wait times for children 32 Eliminating cervical cancer 34 Flu campaign collaboration 36 Traveller health 38 Record highs for National Ambulance Service 40 Waterford placement service 42 Diversity hub 43 End of Life survey 44 Sexual wellbeing back on campus 45 Your opinion counts 46 New supervised injecting facility 47 New screening laboratory 48 Alcohol during pregnancy 49 HSLA graduates 50 Dementia 52 Patient and public partnership network 54 Consent policies 56 Organ donation 58 Integrating our European neighbours 59 Make every contact count 60 Clinical programme conference 61 Patient Safety Together 62 Human Factors e-learning module 63 Open Disclosure 64 Genetics and genomics in Ireland 66 Be well without antibiotics 67 Cancer e-learning programme 68 First endoscopic surgery 69 EHealth migration 70 Estates capital projects 73 Procurement plan 74 Single Financial Management System 75 National Financial Regulations 76 Garden project A MESSAGE
OUR EDITOR
1
2
5
11
FROM
Emma Finn Internal Communications Team
Yvonne Costello
Ann McLoone
Amy O'Neill
Frances Plunkett
Shane Larkin
Paddy Crosse
Keeva Carpenter
Asthma To s
Action
New tool to help caregivers of children with allergy and asthma


Midland Regional Hospital (MRH) Portlaoise Paediatrics Allergy and Respiratory Services have launched a series of videos to educate caregivers of children with asthma and allergies. Parents of children with asthma or allergies can share these videos with anyone who provides care to their child including childminders, schools and crèches/ childcare facilities.
The video series consists of short, step-by-step videos that will show all caregivers exactly what to do if a child in their care experiences an allergic reaction or asthma exacerbation. The series includes instructory videos on: Inhaler technique; Asthma Action Plans; Adrenaline Auto-injector administration; and Allergy Action Plans.
Early recognition and intervention are vital when it comes to the successful management of asthma and allergy in children. While primary caregivers, usually the parents, are trained to manage an allergic reaction or asthma exacerbation, there is a lack of information provided to the child’s secondary caregivers. They should all be equipped with clear, concise information so that they feel competent and confident to employ early interventions when needed.
“These videos will be an invaluable resource for caregivers of children with asthma and allergy. They will provide information and educate caregivers on allergy and asthma action plans, medication, and early interventions, so they can act as e ective first responders at the onset of symptoms,” said Lisa Egan, Registered Advanced Nurse Practitioner in Paediatric Respiratory.
“Our ultimate goal is to ensure consistency of care in the treatment of allergy and asthma in children. Prompt action is essential in the safe management of these conditions so it is imperative that schools, crèches, grandparents, etc. know when and how to intervene during the early onset stages of an exacerbation.”
| 1 HEALTH MATTERS SPRING 2023
MEET THE TEAM HSE Head
Lisa Egan, Registered Advanced Nurse Practitioner in Paediatric Respiratory, Midland Regional Hospital Portlaoise, with child Faye Hinc and Andy Asthma, a child-friendly training doll to help educate children and their parents about the fundamentals in asthma and allergy care.
of Internal Communications
ASHVILLE MEDIA GROUP Editor
Art
Áine
y Creative
Published by Ashville Media, Unit 55 Park West Road, Park West Industrial Estate, Dublin 12, D12 X9F9. Tel: (01) 432 2200 ISSN: 0332-4400 All rights reserved. Every care has been taken to ensure that the information contained in this magazine is accurate. The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher is prohibited. © Ashville Media Group 2022.
Joanne Weston
Director
Du
Director Jane Matthews
Lives Transforming
Joyful ceremony celebrates new lives with residents of St Raphael’s in Youghal

The event celebrated the new lives of 36 former residents of the St Raphael’s building who have moved into new homes, integrated into their community.
There are now 12 houses in the East Cork area where residents who previously lived in a campus setting are living new lives.

Residents, their families and invited guests gathered at the St Raphael’s campus in Youghal, Co. Cork to celebrate the successful move of 36 former residents to community living. There are now 12 houses in the East Cork area where residents, who previously lived in a campus setting, are enjoying new lives.
Michael
Fitzgerald, Chief Officer of Cork Kerry Community Healthcare, said that the move to a new way of living and of delivering services required huge faith
HEALTH MATTERS SPRING 2023 2 |
Care assistants and residents of St Raphael’s Ben Mastradonato, Brian Fitzgerald, Care assistant, Mary Butler, Care Assistant, John Whelan, Thomasina Cripps, Mary Ansbro, Care Assistant, Billy Bullman, Care Assistant and Keith Bullman at the celebration of St Raphael’s campus in Youghal to the successful move to community living.
Photo Darragh Kane
and commitment from sta , residents and families. He paid tribute to families and residents in particular for their commitment.
“A huge amount of work and e ort has been invested over the last six years to make this a reality and we are glad to have a chance to mark this achievement,” he said.
Susan Wall, Director of Services at St Raphael’s, explained that sta , residents and families went through a time of rapid change and paid tribute to their resilience.
“We have seen not just a physical move away from institutions and into community living in ordinary houses, but also a change in mind set and approach, in terms of how we can best support people with disabilities. Our sta can now enable and support residents to live lives in their communities, making their own choices.”
Residents began moving to new homes in 2016. The last residents moved from the old St Raphael’s building in 2019, and the last two of the 12 community houses welcomed residents in December 2021.
Across the country, through the Transforming Lives programme, people living in congregated type-setting have, or will be o ered, alternative housing in the community. Congregated settings are defined as living arrangements where ten or more people share a single living unit, or where the living arrangements are campus-based.
Majella Daly, Head of Disability Services with Cork Kerry Community Healthcare said, “The motto of the Transforming Lives programme is about living ordinary lives in ordinary places, but what we have seen here is nothing short of extraordinary. Through the extraordinary e orts of residents, their loved ones and sta , we have seen an immense level of positive change for many of our residents.”
She added, “The success of this is in no doubt due to a number of factors and people involved in the project over the last number of years, but special mention must be made for the residents, families and sta who were part of the project and supported it over the years.”
Making Tullig House a home
Baking, doing laundry and grocery shopping are welcome daily chores for three residents of St Mary’s of The Angels, who have transitioned to their first community home in Tullig, Killorglin, Co Kerry.

These three men - Seamus, Robert and Pat – had lived most of their lives on the campus-based setting of St Mary’s of the Angels and this move has transformed their way of living in the most positive way. The residents have made this house a home; making their own choices, integrating with the local community and living their life on their terms.
Resident Pat Tagney’s mother Nina said he is more relaxed and much calmer in himself.
“Pat has an intellectual disability, he is autistic and he is non-verbal. Pat lived in St Mary of the Angels for almost 28 years before moving to Tullig House. We were very worried about this community living because we weren't sure how this transition was going to work out for Pat – would he have the same services?
“Pat moved out into the community in May of 2019 and we feel that it has worked very well. He still has full access to GP,
physiotherapy, dietitian and all the multi-disciplinary team.
“He partakes in the community activities. He helps with the grocery shopping, he goes for the walks and he gets out into the car for them. Pat loves food, he likes to watch the food being prepared and the sta here prepare all his meals with him. The house is lovely and spacious. It's well furnished, well decorated, they all have their own bedroom, and it's nice and warm,” she added.
Funding for the move came from the HSE’s Transforming Lives Programme and the transition was greatly supported by a dedicated sta team, families and the local community. Sinead Kelly, Social Care Worker at Tullig House has seen a massive improvement in the residents since the move.
“They're just so much more sociable in the community. They go shopping, they go into the church to light their candles and they're doing their own recycling. They're way more involved in the community and it's just amazing to see it. I see Seamus when he goes into the community, people are calling him by his name. They're going up to greet him and he responds, so even him initiating conversation with other people outside the
| 3 HEALTH MATTERS SPRING 2023
organisation and outside of his family is a huge achievement,” she said.
Healthcare Assistant Freda Purcell says the successful move is down to teamwork.
“The sta here work as a team. All the support that they had on campus like pool, physio, OT, psychiatrists, psychologists, GPs - that still continues either on campus or in the community. They attend their GP at his own surgery here in the community and they go to the chiropodist. So just because they've moved to the community doesn't mean that all these things stop. We are absolutely thrilled for them and their families that it has worked out, because it was a big step for them all round,” said Freda.
Transforming Lives Project Co-Ordinator Killian O’Dowd said, “It has had a positive impact on the residents because it is giving them freedom, independence and a new lease of life. We are hoping this story will lead to more houses that we can turn into homes here in Kerry service. We would like as many people as possible to have the same experiences and be able to have the freedom and opportunity of community living.”

AI can revolutionise healthcare industry, forum hears
Attendees from all healthcare sectors were treated to a stimulating day of education and inspiration at HSE Spark Innovation Programme’s recent Artificial Intelligence (AI) and Machine Learning (ML) in Healthcare Forum in Dogpatch Labs, Dublin.


The event focused on the potential that both have to revolutionise the healthcare industry, with the belief that cross discipline innovation in this space can improve patient care and health outcomes.
In the morning, an eclectic mix of expert speakers from the HSE, industry and academia discussed topics ranging from the current reality of healthcare data, ethical considerations and the potential impact of AI and ML in healthcare. This was followed by a showcase from some of the most exciting Irish companies operating in the AI and ML in healthcare space.
After lunch, Spark’s collaborators on
the event, EIT-Health and Deloitte facilitated two workshop sessions aimed at highlighting the supports that the attendees felt they needed within the ecosystem, as well as clinical opportunities for AI and ML. Professor Seán Kennelly, Consultant Physician in Geriatric Medicine and Director of Cognitive Clinical Trials Unit and Memory Service, Tallaght University Hospital, led the closing session of the day sharing how Gaitkeeper, a new AI digital solution is enhancing his patient’s care.
“This technology is a game-changer for clinicians as to how we can monitor and gauge how well and fast our patients can walk. This is a key indicator of a person’s wellness and the technology will be easy to use in any care setting. This technology e ectively o ers us a digital biomarker of a patient’s wellness,” he said.
The HSE Spark Innovation Programme is a frontline, sta -led initiative that seeks to
support, promote and recognise innovation amongst healthcare sta . This event was organised in collaboration with Deloitte, EIT Health Ireland-UK and the Department of Public Expenditure and Reform.
You can find out more about the HSE’s Spark Innovation Programme by visiting the website hse.ie/spark or following their social media channels.

HEALTH MATTERS SPRING 2023 4 |
l-r: Patrice O’Neill, Interim Disability Manager Cork Kerry Community Healthcare; Killian O’Dowd, Transforming Lives Project Co-ordinator; Robert McCarron (front), resident; Sheila Marie Fitzgerald, Director of Nursing St John of God Kerry Services; Seamus O’Connor, resident; Siobhan O’Donoghue, Tulligmore sta member; Freda Purcell, Tulligmore sta member; Pat Tagney, resident and Majella Daly, Head of Disability Services Cork Kerry Community Healthcare.
My Health, My Language scoops award
The National Social Inclusion Office was delighted to win the Equality Initiative of the Year at the Irish Healthcare Awards for My Health, My Language, a suite of multilingual videos aiming to make health advice more accessible to Ireland’s migrant community.

Dr Margaret Fitzgerald, Public Health, former lead for social inclusion, said, “We would like to thank Translate Ireland who we worked with in the development of this comprehensive series of multi-lingual videos.
“The videos, which have been produced in 17 different languages, offer clear information on important health information such as how the Irish health system works, accessing different types of health care, services that are free and information on pregnancy and new-born and maternal health. This initiative would not have been possible without the healthcare staff who took time out of their busy schedules during the COVID-19 pandemic and the recent Ukrainian crisis to participate in the videos. A special thanks to all who took part.”
Many people come from countries with very different healthcare systems to Ireland, and navigating an unfamiliar health service on arrival in a new country has been shown to be stressful experience and can result in a lack of access to essential services.
The videos are presented by doctors, nurses and other healthcare workers, who live and work in Ireland but moved here from abroad, speaking in languages such as Arabic, French, Ukrainian, Polish, Slovak and Mandarin Chinese (Simplified). People are often assured when they see a member of their own community delivering factual, trustworthy health information in the videos.
Visit hse.ie/MyHealthMyLanguage
DIGITAL MEDIA AWARD GOES TO QUIT CAMPAIGN
The HSE’s QUIT campaign was awarded a Bronze Award for in the Best Government and Not-for-profit category in the Digital Media Awards 2022 in December. The award is for the work undertaken to increase sign-ups for online QUIT plans in 2022, which saw paid search programme sign-ups increase by 28% and helped more people who smoke to quit than ever.
People who click on the search ads can use a range of online supports to quit smoking and find information on local face-to-face services in their area as well as evidencebased advice on how to quit successfully.
Martina Blake, National Lead Tobacco Free Ireland Programme, said, “It is great to see the hard work of the team who work on the QUIT campaign recognised with this award. As people who smoke become harder to reach, we constantly need to use innovative approaches to reach them and this an excellent example of this at work.”
The HSE’s COVID-19 campaign was also shortlisted for an award in the Best Technology Innovation category for its digital display campaign.
| 5 HEALTH MATTERS SPRING2023
Resident Seamus O’Connor with staff member Siobhan O’Donoghue in the kitchen.
Kick the habit
HSE helps people who smoke to take back control
In January of this year, the Tobacco-Free Ireland programme together with HSE communications launched a new advertising campaign for the Quit service.

The campaign shows how people who smoke can start to take back control over their addiction in just 28 days with help from the Quit service.
In 2022, almost one in five people in Ireland still smoke. The prevalence of smoking in Ireland remains at 18% and has not declined since 2019.
Dr Paul Kavanagh, HSE Public Health Medicine Lead with the Tobacco Free Ireland Programme, explained, “While we have made good progress in tackling smoking over the last two decades, smoking continues to cause harm on a huge scale in Ireland. Each week, almost 100 people die and 1,000 people are hospitalised because of smoking related disease. This is preventable, and stopping smoking remains the single most important thing you can do for your health.”
The campaign seeks to highlight the reality that nicotine is highly addictive and can take control of people’s lives.

Martina Blake, National Lead, HSE Tobacco Free Ireland Programme, said, “In developing our new advertising campaign, we listened carefully to people who smoke so we could better understand how we can connect with and support them to quit. They told us about the control smoking has over them and across many aspects of their lives and how their daily routines and habits are set for them by their smoking. People often leave social situations to go outside to smoke. They told us how the costs, about €100 per week, means smoking also has control over their finances.
“It’s all too easy to see smoking as an individual choice. However, the reality we are calling out in our new adverting campaign is that smoking is highly addictive and takes control of people’s lives. People who smoke told us they want to take back control.”
The HSE Quit services are here to help with support that tackles the addictive nature of smoking. Many people will try to quit cold turkey without any help or support, but nicotine is highly addictive. You are five times more likely to quit for good if you use evidence based stop smoking medication, get ongoing support from a HSE
HEALTH MATTERS SPRING 2023 6 |
Edward Murphy, Tobacco Free Ireland Programme; Pauline Kent, Tobacco Free Ireland Programme; Nuala Cody, Stop Smoking Advisor; Celine O’Shea Secretary to the Director of Nursing, St Francis Hospice; Martina Blake, Tobacco Free Ireland Programme; Aishling Sheridan Tobacco Free Ireland Programme; Darina Carr, QUIT Campaign Manager.
stop smoking advisor, stop smoking and stay quit for 28 days. Our trained stop smoking advisors are available for free to everyone in the Health Service. They can work with you to create a personalised stop smoking plan tailored to fit your lifestyle. Nicotine Replacement Therapies (NRT) double your chance of quitting by helping address the physical cravings. Free NRT is now available for everyone if they access the stop smoking support programme through our trained stop smoking advisors.
promised them I would quit and try and get more healthy not only for them but for myself too,” she said.
“I wanted to feel better, in myself. I always felt tired and sluggish. As I work in an office, the only time I seemed to go outside and see other people during the day was on a break when I used to smoke. Smoking had control over my routine. I knew I needed to change my whole daily pattern for the better.”
Nuala has a wealth of knowledge and spoke to Celine about her reasons for smoking, NRT available and how to beat cravings.
“From the very first time I met Nuala, at the talk during Wellness Week, I knew this was my chance to really quit my smoking habit. The one-to-one weekly meetings with Nuala was for me, the most essential part of my Quit journey – Nuala and I would talk about my upcoming plans i.e. a wedding or a stressful event that would normally trigger me to smoke.
Celine now six months smoke-free
Celine O’Shea, Secretary to the Director of Nursing in St Francis Hospice Blanchardstown is smoke-free since October 2022.
As part of a Wellness Week last year, Stop Smoking Advisor, Nuala Cody visited the hospice to give a talk to staff about the Quit programme.
Celine explained why she wanted to quit once and for all.
‘’I have three sons who absolutely despise smoking and I had
“By discussing these plans with Nuala and putting an alternative ‘action’ in place, I was prepared in a planned & unplanned situation and did not go in search of ‘a smoke’, instead I would have a piece of gum, a lollipop, make a phone call, anything to distract me. I began to change my thinking, instead of going for a smoke to relieve my stress, I told myself that it was the worst thing I could do, that I was making myself unwell by going for a smoke. That it was NOT helping me but magnifying my stress.”
Nuala urged anyone who wants to quit to take that first step.

“You can go on to the HSE quit page, text or use the live chat to contact your local QUIT Smoking support service.By doing so, you will be taking that first step on the road to becoming an ex-smoker. You might be nervous about quitting but our trained advisors are here to support your journey.”
To find out more on the support available visit https://www2.hse.ie/living-well/quit-smoking/support-services/
| 7 HEALTH MATTERS SPRING2023
“It’s all too easy to see smoking as an individual choice. However, the reality we are calling out in our new adverting campaign is that smoking is highly addictive and takes control of people’s lives. People who smoke told us they want to take back control.”
Celine O’Shea, who quit smoking six months ago, pictured with Stop Smoking Advisor Nuala Cody
Integrated Care and Regional Health Areas
In 2023 , the HSE will begin setting up 6 Regional Health Areas (RHAs) within the HSE. These will replace our Hospital Groups and Community Healthcare Organisations from 2024 onward.
Limerick, Tipperary and Clare
Donegal, Sligo, Leitrim, Roscommon, Mayo, and Galway
North Dublin, Meath, Louth, Cavan, and Monaghan
RHA B
Longford, Westmeath, Offaly, Laois, Kildare, and parts of Dublin and Wicklow
RHA C
Tipperary South, Waterford, Kilkenny, Carlow, Wexford, Wicklow, part of South Dublin
HEALTH MATTERS SPRING 2023 8 | Making Progress on Integrated Care
RHA A
RHA D Kerry and Cork
RHA E
RHA F
Mobile vaccinations
Mobile units bring vaccines to the community
There are plans to have 12 mobile vaccination units working out in communities this year, making vital vaccines as accessible as possible for key target groups.
The Cork Kerry Community Healthcare vaccination team deployed the first two in 2022, providing the COVID-19 vaccine. West Cork took delivery of the first mobile unit in the country in the run-up to winter, with North Cork receiving a mobile unit shortly thereafter.

Cora Hayes, the vaccination lead at the West Cork vaccination centre, said the team in Bantry are delighted to be increasing access to the vaccines.
“Our vaccination team has done close to 75,000 vaccinations since the start of the COVID-19 vaccination programme. Most of these were done through the vaccination centres in Clonakilty and Bantry, but 1,250 were done during visits to homes, to residential care facilities, to an island clinic, to international protection accommodation services and to workplaces,” explained Cora.
“We are delighted to utilise the mobile vaccination unit in West Cork, which allows us to offer a more flexible service and improve accessibility for the people of the region.”
The mobile units are being used to:
• Add capacity to the vaccination programme in residential care facilities (eg nursing homes).
Provide flu vaccinations for healthcare workers in the region. Easy access to the flu vaccine for healthcare workers was key to keeping the people they work with safe and well this winter.
• Operate pop-up vaccination clinics at Clonakilty and Bandon GAA clubs.
The HSE want to acknowledge and thank sincerely the Scottish Ambulance Service for its assistance in establishing this model within the Republic of Ireland.
| 9 HEALTH MATTERS SPRING 2023
The National Social Inclusion Office team collect their award at the Irish Healthcare Awards
Care closer to home



After a few years of breathlessness, wheezing and a persistent cough, Celine Naughton was diagnosed with asthma. But after receiving specialist respiratory services in her community, she is back in the gym and feels the support she received has changed her life altogether.
The 62-year-old explained that after she was diagnosed with asthma, her GP referred her to the specialist respiratory service on her doorstep in Bray, Co Wicklow. Celine said she was seen within a matter of weeks by specialist respiratory nurse Joyce O’Hara (part of the hub's Community Specialist Team), where she learned how to manage her condition and is now confident about her future.
“Joyce gave me all the time I needed and listened to what my lifestyle was like. She said I had a combination of chronic sinusitis and asthma. She told me what we were going to do which would involve me changing some things in my lifestyle. Joyce told me that whatever exercise I could do, even if it was only a gentle stroll, to do that for now,” Celine said.
“The result is that now, about six months later, I am going to the gym three or four times a week and really enjoying it. And I think, altogether, this has changed my life for the better. I wish every community had it as this is a shining light and I just hope everybody can be able to avail of a facility like this on their doorstep.”
Celine was one of the first patients to receive treatment in the new Integrated Care Hub in Bray that opened in mid-2022. It is part of the Enhanced Community Care programme, a core part of the Sláintecare reforms, which seeks to ease pressure on services.

The Community Specialist Teams provide the community with access to specialist services, close to home, for people living with lung, heart and diabetes chronic disease and/or multi-morbidity. The team at the hub includes consultants, clinical nurse specialists, advanced nurse practitioners, physiotherapists, podiatrists and dieticians. Through the hubs, patients are able to access community-based diagnostics such as echocardiogram, spirometry and ProBNP Testing.
“I run the Respiratory Service here in the Integrated Care Hub. It’s a fantastic service for the patients because they can have this specialist testing in their community, in their area, and they don’t have to come into hospital,” said Rachel Anglin, Chief Respiratory Physiologist at St Vincent’s University Hospital describing the benefits of the Integrated Care Hub in Bray.
Community Specialist Teams will service a population of 150,000 equivalent on average to three Community Healthcare Networks. Ideally, the teams will be co-located together in ‘hubs’ located in or adjacent to Primary Care Centres reflecting a shift in focus away from the acute hospital towards a general practice, primary care and community-based service model. The services are fully aligned with the acute system. Clinical governance is provided though the relevant model 3 or 4 hospitals or GPs, but with the services being delivered in the community setting.
The Integrated Care Programme for Chronic Disease aims improve access to care, reduce specialist waiting lists, emergency department presentations and hospital stays, as well as enabling prevention, earlier diagnosis and intervention. The overriding objective is to support GPs to care for patients at home as much as clinically appropriate.



HEALTH MATTERS SPRING 2023 10 | Making Progress on Integrated Care
“This has changed my life for the better, I wish everyone could have facilities like these on their doorstep”.
Celine Naughton, a patient of the Integrated Care Hub in Bray
Integrated care is where services, funding, and governance are co-ordinated around the needs of the patient, encompassing acute, primary, and community care.
Celine O’Hara with specialist respiratory nurse Joyce O’Hara.
Empowering patients to prevent and manage chronic conditions


Regaining independence


Integrated Care Programme lets older people keep their independence

The HSE’s Integrated Care Programme for Chronic Disease is actively improving the standard of care for patients living with chronic disease in Ireland through the national roll-out of the Structured Chronic Disease Management Programme (CDM) in General Practice.
The CDM programme provides a structured management programme in General Practice for people who are at risk of, or have a diagnosis of, cardiovascular disease, COPD, asthma and type-2 diabetes. It focuses on disease prevention, patient empowerment, early diagnosis and intervention and the provision of care as close to home as possible
The programme provides two visits to the practice nurse and two visits to the GP every year. Part of the HSE’s Enhanced Community Care programme, the CDM programme is helping over 230,000 people with chronic disease to avoid hospital and stay well at home. The programme is available to patients aged 18 years and over who have a medical card or GP visit card.
“The CDM programme emphasises lifestyle and medical risk factor control, disease management and the creation of a patient care plan,” explained Dr Orlaith O’Reilly, National Clinical Advisor & Group Lead for Chronic Disease and the Integrated Care Programme for Chronic Disease.
“The GP works in partnership with the patient to identify what matters most to them in the management of their chronic conditions to develop a care plan to achieve their goals. Supporting patients to live well and to manage their own chronic conditions is at the heart of the CDM programme and a wealth of resources are being rolled out across Ireland to support patients in this regard. For example, 30 new cardiac rehabilitation teams and 30 new pulmonary rehabilitation teams are being established in communities across Ireland to support patients to live well following a heart attack or COPD admission.”
Tina Maria Morrison of Wexford said she was delighted to be part of the programme. “Anyone thinking of going on the programme, I would talk to your GP or your nurse, and get on the programme because it’s very beneficial. Personally, I find it’s great because I know my levels of blood that I need every six months. I can keep an eye on that then. Generally I know I’m on the right path. I can set goals then for the next six months, so yeah, it’s very good,” she said.
“I wouldn’t have been able to be at home and get up on my own feet if it wasn’t for the care those girls gave me.”
Rita Condren was describing the impact of the Integrated Programme for Older Persons has on the health and wellbeing of many older persons right across the country.
From Bray, Co Wicklow, Rita had a fall at home and broke her hip. She was treated in St Vincent’s University Hospital Dublin but was faced with reduced mobility because of her fall and the subsequent surgery.
The Occupational Therapy team in St Vincent’s referred Rita to her Integrated Care Programme for Older People, based in Bray where she got intensive physiotherapy and occupational therapy period over eight weeks helping her regain her physical strength and her confidence.
Marianne Goll, Senior Occupational Therapist who works for the Integrated Care Programme for Older Persons based in Bray, explained that Rita would be “a very typical client of ours, referred post hip surgery and returned home to the community. The community team felt she would benefit from occupational therapy and physiotherapy in her home. And that’s how we got involved.”
With the support of the Department of Health and Sláintecare, these models are now being implemented at scale, by the HSE. The establishment and full rollout of 30 Community Specialist Teams for Older People and 30 Community Specialist Teams for Chronic Disease to support CHNs and GPs to respond to the specialist needs of these cohorts of the population will link the care pathways between acute and community services with a view to improving access to and egress from acute hospital services, as well as improved patient outcomes.
| 11 HEALTH MATTERS SPRING 2023
Tina Maria Morrison with Denise Behan, Practice Nurse; and Dr Joe Gallagher, HSE / ICGP Primary Care Lead for Integrated Care Programmes (Cardiovascular Disease) at The Palms GP Surgery, Co Wexford.
Rita Condren
Delivering Change Together
Finding a common solution to our common problems

Renowned healthcare change and service improvement leader Helen Bevan delivered a masterclass as part of the launch of the HSE’s Delivering Change Together programme.

Sligo was the location for the first collaborative experiential programme on building change capacity in what will become one of the Irish health system’s Regional Health Areas as part of Sláintecare reforms.

Participating on the day were over 150 multidisciplinary healthcare colleagues from across the West and North West regions.
Helen, Strategic Advisor, NHS England, said she was ‘very privileged’ to be in Ireland for the launch.
“One of the things that I really love about the programme is how it brings together organisation development, programme management, a focus on action learning and quality improvement in such a powerful, integrated way. I will remember this for a long time,” she said.
This initiative is co-sponsored by the CEO of Saolta University Health Care Group and the Chief O cers of Community Healthcare West and Community Health Care Cavan, Donegal, Leitrim, Monaghan, Sligo. The development of this programme is a collaboration between the respective Programme Management O ces in the partner organisations with the support of National Organisation Development, Change & Innovation within the HSE.
As organisational and service needs were identified and validated, other support services got involved. It is an example of how pooling
expertise and resources can support change and service improvement practices at regional and local level.
The day enabled participants to hear about change including the learned experiences and evidence from within their own services and also from Helen’s experience over many years. Attending the launch, John O' Hora, Community Healthcare Network Manager from South Donegal and Sligo Network said, “It's great to work with colleagues in Saolta and Community Healthcare West to help find common solutions to our common problems.”
HEALTH MATTERS SPRING 2023 12 | Making Progress on Integrated Care
Steering Group & Convenors of Communities of Practice. Back row: Susan Healy, Elaine Birkett, Brendan Power, Irene McGuire, Róisín Egenton, Helen Bevan, Marie O’Haire, Siobhán Rogers, AnneMarie Keane, Juanita Guidera, Ellie Cooley, Denise O’Shea, Lisa McDaid. Front row: Bernie Austin, Deirdre Driver, Martina Vaughan, Helen O’Neill, Caitríona Heslin.
For further information on the Health Services Change Guide and associated resources and supports please visit us at hse.ie/ changeguide or contact changeguide@hse.ie

Discussion and group activities on the day allowed those present to tap into the collective wisdom within the organisation. Catherine Flynn, Community Healthcare Manager, Galway City North and West Network, said, “My real hope is that we can really drive forward true integrated care across the community so that for all of us we can experience a health care system that really delivers coordinated, cohesive integrated care for all of us.”
Catherine Sheridan, Quality Improvement Paediatrics, Saolta University Health Care Group, said, “I see myself as someone who will be helping to lead change within the children’s services and I hope to take with me some useful tools in order to help me assist my colleagues throughout that change process whilst keeping the patient at the centre of everything we do.”

Nine Communities of Practice were established with crossorganisational and service representation. 80 multidisciplinary service leaders are now connected, who might not otherwise have had the opportunity to interact across hospital and community services. Each Community of Practice is supported by a Convenor and by their local Programme Management O ces along with national services.
Ohbuoy
–it’s time for a dip!
Sea swimming has been the saviour for many people’s mental and physical wellbeing over the COVID-19 pandemic and a Healthy Ireland initiative is now making life easier for the intrepid sea swimmers – and even encouraging a few newcomers to the water.
Healthy Ireland Swim distance marker buoys have been placed at 100-metre intervals to create a 600-metre sea swimming circuit at Ventry Beach in Co Kerry.

Gabrielle O’Kee e, Head of Service Health, Wellbeing & Strategy, Cork Kerry Community Healthcare, launched the project and highlighted the importance of initiatives which facilitate physical activity and wellbeing.
“As a coastal county, we have an enormous asset available for everyone to enjoy. I am



Caitríona Heslin, Assistant National Director, Organisation Development, Change and Innovation, Healthcare Strategy said, “This Experiential Change Programme is a really good example of collaborative and integrated planning between national and local services – we share the same ambition of wanting to provide development opportunities for people who are leading and delivering change and service improvements across our health system. We will learn from this initiative and it will allow us to combine and maximise our expertise in connecting services and supporting the establishment of Regional Health Areas based on local knowledge, insights and context.”
Check out the launch video at https://youtu.be/kkRmNZw1uc4

confident that the swim markers will encourage existing and new users to get into the water and swim, an activity that is good for mind and body,” she said.
Gabrielle O’Kee e thanked Maebh Uí Ainiféin, Chairperson of Kerry Water Safety, who led the project locally and the many stakeholders involvedincluding Nigel Collins, Dingle Harbour Master; Billy Horgan, Cork Water Safety; the Ventry Wild Atlantic Women swimming group, Niall O’Sullivan and Liam Brosnan, Kerry County Council.
The implementation of the swim distance markers in Ventry provides increased
opportunities for safe and enjoyable physical activities, adding healthy habits to our daily and weekly routines.
The Healthy Ireland swim distance marker buoys will encourage safer swimming among novice and experienced open water swimmers making the healthy choice the easy choice.
| 13 HEALTH MATTERS SPRING 2023
Healthy Communities
19 areas to get wellbeing boost as part of Sláintecare Healthy Communities Programme
The goal of the Sláintecare Healthy Communities Programme (SHCP) is to improve the long-term health and wellbeing of 19 deprived communities across Ireland, tackling health inequalities with a focus on the social determinants of health.
It will provide major supports for smoking cessation, parenting, nutrition and social prescribing to help boost the health of these communities.
19 areas of greatest need were identified by the HSE, the Department of Health and local authorities, using the HP deprivation index, based on the 2016 census. Some of these areas are located in our major cities, whilst others are in rural towns and areas.
The communities identified have on average 24,000 people and a broad mix of population types.
Sláintecare Healthy Communities Coordinators, working in HSE Health and Wellbeing at local level, play a key role in the implementation
of the SHCP. Local Development Officers employed in each of the 19 areas and have been given funding to identify and fund projects that the local area and people's health and wellbeing.
To support the work of the Local Development Officer, each local authority has been given a seed funding budget of €75,000 as well as €250,000 Enhancement Scheme funding per community to support projects identified within the community that will support health and wellbeing. Some 112 projects were funded in 2022.
SHCP supports not only the physical and mental health of people living in the Sláintecare Healthy Communities; but also supports improvement in the wider determinants of health, including education, social support and the built environment.
Each of the respective local authorities have signed a Service Level Agreement (SLA) to coordinate and support the Sláintecare Healthy Communities Programme with the Local Community Development Committees and their existing Healthy City and Healthy County plans.
Keeping it real
Showcasing the essence of Sláintecare Healthy Communities
During 2022, most of the areas took the opportunity to mark this investment and organised their respective local launch events. The launches took place in each area, in venues such as Ballymun Axis Centre, Dublin; Hollyhill Library, Cork; Aras Inis Gluaire Civic Centre, Belmullet, Co Mayo; Fettercairn Community Centre, Tallaght; Athy Library, Kildare; and Donegal, to name a few. Each of the launches showcased the range of services and community partners who are working to deliver health and wellbeing services in each of the 19 areas.
Service users who engaged in some of
Focus on RHAs
Regional Health Areas will reform our health service. They will align and integrate hospital and community healthcare services across each regional area, meaning that health services will be based on the region’s populations and their needs.
the programmes, were central to the launch events. The launches provided the opportunity for each area to remind everyone what the services are really about. Videos, interviews and illustrations were all used to ensure that members of the local communities who avail of the local services and their stories were shared and highlighted.
These included examples of service users who managed to stop smoking, used the parenting programmes or learnt how to cook healthier meals.
Attendees at the launches heard powerful
stories about how the programmes impacted local service users' lives and the lives of their families. Tom James, Head of Health & Wellbeing, Department of Health, said, “Our shared future is committed to tackling health inequalities based on race, gender and socio-economic background. I believe passionately that we must invest in all our communities, especially those in greatest need, so that none are left behind.” Each of the launches were attended by representatives from the HSE, local authority and a range of community partners. The remaining launches will take placein early 2023.
HEALTH MATTERS SPRING 2023 14 | Making Progress on Integrated Care
DSKWW at the Clondalkin launch. 4. The launch of the Sláintecare Healthy Communities in Donegal. 5. Aisling Logan, Southill Hub; Tanya Carey, SHC LDO; Frank Feighan TD, Maria Bridgeman, CO HSE Mid-West CH; Cllr Francis Foley; Niamh Wallace, HSE Mid-West H&WB, Seamus O’Connor; Ger Fahy, HSE Mid-West CH SHC Coordinator 6. Lisa Marren, Social Prescribing Link Worker; Louise O'Malley, Foróige; Brenda McNicholas, Stop Smoking Advisor in Castlebar 7. Back: Alan McDonnell, HSE HP&I; Colm Ward; Daniel McLoughlin; Margaret McQuillan, H&WB. Front: Jennifer Moroney Ward; Mary O’Kelly, HSE DSKWW; Mayor Emma Murphy; Frank Feighan TD; Aine Buggy, Senior HP&I O icer, HSE; Grainne Meehan.







Key HSE Health and Wellbeing components
Social Prescribing: A Social Prescribing link worker will provide interventions and referrals to community-based services in the statutory and non-statutory sector. Social prescribing o ers GPs and other health professionals a means of referring people to a range of non-clinical community supports which can have significant benefits for their overall health and wellbeing and has been used to target social isolation, loneliness and emerging mental health di iculties.
Stop Smoking Advisor: A Stop Smoking Advisor will provide one-to-one support to quit smoking including the provision of NRT or other Stop Smoking medication. They will also promote and support the extension of smoke free environments.
We Can Quit: We Can Quit is a friendly and supportive 12-week programme, providing group behavioural support, nicotine replacement therapy and other stop smoking medication, to help attendees quit smoking and stay quit for good. This group programme has been proven to support people around their smoking by utilising peer and social support as well as professional input.
Parenting Programmes: Universal Parenting Programmes will provide families with greater access to evidence-based parenting programmes. Parenting programmes have been shown to be one of the most e ective ways to improve child and parental mental health and wellbeing.
Healthy Food Made Easy: The Healthy Food Made Easy (HFME) programme will provide a user-friendly nutrition and cookery course that helps people increase their skills to implement a healthy diet, plan meals on a budget and make easy to cook meals.
MECC: The Making Every Contact Count (MECC) programme will work with local health professionals to ensure they have the up-to-date skills to deliver brief interventions and advice for all patients regarding healthy behaviours (smoking, alcohol use, physical activity, diet and nutrition). This will see an increase in service users and patients being advised to make healthy lifestyle choices and directed to supporting resources and programmes to do so.
| 15 HEALTH MATTERS SPRING 2023
1 6 4 2 7 5 3
1. Lorraine McGowan, HSE Senior HP&I O icer/ Slaintecare Healthy Communities (SHC) Co-ordinator and Mark Garvey, HSE HP&I O icer at the Ballymun launch 2 The Cavan launch of the Slaintecare Healthy Communities initiative 3. Karen Heavey, HSE HP&I manager, DSKWW; Jennifer Moroney Ward; Margaret McQuillan, HSE Head of H&WB, DSKWW; Colm Ward; Deputy Mayor Joanna Tu y; Tom James, Head of H&WB, and Healthy Ireland; David Morrissey, Clondalkin LDO; Keith Ryan, HSE SHC HP&I O icer, Clondalkin; Aine Buggy, HSE SHC Coordinator,
The National Ambulance Service
Older people strongly back National Ambulance Serviceled Pathfinder service
Older people who benefitted from the National Ambulance Service (NAS) led service

Pathfinder have strongly backed the programme, showing that the initiative to safely keep older people in their own homes and out of Emergency Departments (ED) when they phone 112/999 is working.
Pathfinder improves outcomes for older people by providing safe alternative care at home rather than in hospital. The service is being provided by NAS sta working with colleagues from HSE acute hospitals.
A service evaluation of patient and carer feedback after Pathfinder responded to their emergency calls resulted in very positive observations.
Older people and their next-of-kin voiced a clear preference for hospital avoidance, and strongly valued the opportunity to be treated in their homes at the time of an Emergency Medical Service call rather than default conveyance to the hospital ED. They appreciated the importance of a skilled multidisciplinary team with a follow-up service that e ectively positions itself between the acute hospital and community services.
Older people experience high rates of adverse outcomes following ED presentation. There is growing evidence to support alternative care pathways for certain types of emergency medical services (EMS) calls. Pathfinder is one such service and targets patients aged 65 years and over, whose presenting issues can be safely managed at home by immediate paramedic, occupational therapy, and/or physiotherapy interventions. The aim of this service evaluation
was to understand how older people feel about being treated at home as a result of EMS calls and to understand their experiences of the Pathfinder service.
The evaluation appears in a paper prepared by Royal College of Surgeons in Ireland (RCSI) qualitative researchers and co-authored by the Beaumont Hospital Pathfinder team. An extract of the paper was published earlier this year in the prestigious US journal Prehospital Emergency Care.
The feedback found that out of 573 service users, telephone interviews were conducted with 429 (75%).
Five primary themes were identified:

• Professionalism of the multidisciplinary clinical team
• ‘The right service, in the right place, at the right time’
• Role of Pathfinder in ‘getting the ball rolling’
• Lasting e ects of the experience on the patient and his or her next-of-kin
• Value of skilled communication with the older person.
Siobhán Masterson, National Ambulance Service
Lead for Clinical Strategy and Evaluation, said the evaluation was a great example of the patient voice in a patient-centred service.
Pathfinder is now live in the catchment areas of Beaumont Hospital, Dublin, UL Hospital Group, Limerick, Tallaght University Hospital and University Hospital, Waterford.
The Pathfinder ‘Rapid Response Team’ respond to 999/112 calls for people aged over 65 years in
Sláintecare
in action:
€240 million is being spent on Enhanced Community Care (ECC).
To date, the ECC programme has established
• 94 out of 96 Community Healthcare Networks (CHNs),

• 21 out of 30 Community Specialist Teams for Older People,
• 21 out of 30 Community Specialist Teams for Chronic Disease,
• 21 Community Intervention Teams with national coverage
• Recruited over 2,500 additional sta with 1,000 more to come
• Provided over 250,000 scans in 2022 through GP Access Diagnostics


their homes. The older person is assessed by both an Advanced Paramedic and Occupational Therapist/Physiotherapist.
Where safe, the team supports the older person at home rather than transporting them to an ED by linking with a wide range of alternative hospital and community services. Pathfinder also operates a ‘Follow-Up Team’ (Physiotherapy and Occupational Therapy) which provides immediate home-based rehabilitation, equipment provision and casemanagement in the subsequent days.
HEALTH MATTERS SPRING 2023 16 | Making Progress on Integrated Care
Pictured in Limerick as the service went live were, left to right, Blaithin Lally, senior physiotherapist; Linda O’Rourke, advanced paramedic; Nicola Donohue, clinical specialist physiotherapist; Pat McCarthy, advanced paramedic and Niamh Ganley, senior occupational therapist.
Photo: Brian Arthur
HR & Payroll Self Service
goes live in HSE South
HR & Payroll Self Service (formerly called My HSE Self Service) is an online facility, using SAP software, which allows employees to view or change a range of personal information, request leave and submit travel/expenses claims. Managers use the tool to review applications for leave and travel.
It gives you easier access and more control over your own information, is available 24/7 online and reduces paperwork and streamlines tasks, saving time for both employees and managers.
The HSE South implementation continues, with a ‘go live’ date of March 2023. In the past few months, there have been a series of live webinars providing general awareness of HR & Payroll Self Service for employees and managers.
If you need further support you can log your query with the NiSRP Helpdesk via the new Health Shared Services Self-Service Portal https://hse. microsoftcrmportals. com/ Email the NiSRP Helpdesk at support. nisrp@hse.ie or call 0818 300 296.
If you work in HSE South and wish to hear more about HR & Payroll Self Service, please speak to your line manager. NiSRP have sent
Community collaboration
the key to promoting mental health and wellbeing supports


Mental health support services in north Cork are reporting a large increase in calls following a hugely successful community awareness day at Mallow Castle.

More than 3,500 people attended the ‘Together at the Castle’ event, organised by Cork Kerry Community Healthcare (CKCH) in partnership with Mallow Chamber of Commerce, Cork County Council, See Change and Shine.
It is now hoped to use this model of collaboration in other parts of Cork city and county, as well as seeing replicated across all counties, across all communities.
“The impact of this event has been very real, as local businesses, education providers, youth and sports groups are all wanting to take part in the next mental health awareness event in the Mallow region,” explained CKCH Resource O cer for Suicide Prevention Martin Ryan.
Part of the Connecting for Life strategy in Cork, the focus was to promote wellness and mental health supports, while engaging with all aspects of the community. The aim of ‘Together at the Castle’ was to normalise help-seeking behaviour across all ages, as suicide prevention is everyone’s business. This event was created to highlight key support services, while having fun at the same time.
The event was an innovative way to promote mental health and wellbeing supports available in the area. It included a diverse range of entertainment, recreational activities, workshops and informational spaces. Dozens of local groups took part in the family-friendly event which, as well as spreading information, also featured kids’ entertainment and music.
Martin said the event successfully made people aware of the supports available to them locally.
“It proves that when agencies work together, both public and private,

information packs to managers for distribution to all employees. There are live webinars specific to HR & Payroll Self Service being held each week and you will see information stands on site starting in early February. This will be a great opportunity to view the online tool and chat about the benefits of HR & Payroll Self Service. We would encourage you to come along and meet the NiSRP team to avail of more information.
How do I get support?
The NiSRP Support Site www.hse.ie/nisrpselfservice contains video tutorials, step-by-step guides and FAQs. There are also three eLearning certified modules available on HSeLanD and each module takes approximately 15 minutes to complete. Search for NiSRP at www. hseland.ie to find the course.
great things can happen. In my role, I’m very much aware that when I meet with groups or individuals, often they want to know what supports are available in their local area. Therefore, it is really important that we can signpost people to relevant services, matching the right service with their needs,” he said.
“This event was in collaboration with Cork County Council, Mallow Chamber of Commerce, Green Ribbon campaign and HSE Connecting for Life Cork. On the day, we showcased the stigma reduction campaign (green ribbon) where we distributed well over 30,000 ribbons and 20,000 tea packs. This was also supported by over 40 local businesses carrying the green ribbon - showing their solidarity to reduce mental health stigma across all aspects of community.
“We produced a great event that all of the community was proud of. We supported all agencies to come together within their own community so they can network more e ectively. On the day, we had well over 3,500 people walk through this event therefore we have 3,500 people bringing home the clear message of hope and recovery.”
For information, please see connectingforlifecork.ie or yourmentalhealth. ie or directly contact Martin Ryan martin.ryan8@hse.ie
| 17 HEALTH MATTERS SPRING 2023
MILESTONE ANNIVERSARY FOR ADDICTION SERVICE
Adolescent Addiction Service celebrated its 25th anniversary recently, marking this significant milestone with a conference in Bridge House, Cherry Orchard Hospital.


The service was established in 1997 as the Irish health service was faced with the challenge of responding to an increase in the numbers of young people presenting with significant drug problems, especially in relation to heroin.
Given the incidence of heroin use and associated health complications the service focused on the needs of this cohort of young people initially by establishing a programme with a multidisciplinary team including GP, pharmacist, family/systemic psychotherapist, nurse, general assistants and sessional art and aromatherapist to meet the needs of a vulnerable adolescent population in south west Dublin, serving the communities of Inchicore, Ballyfermot, Chapelizod, Palmerstown, Clondalkin and Lucan.
The conference was attended by representatives from multiple services. Delegates reported appreciating opportunity to meet with people face to face which allowed for exchange information and ideas focusing on diversity of services for young people and community of practice that exists a national level.
They discussed issues currently in relation to youth substance misuse, the challenges faced by services in responding to the needs of young people and their families and approaches to intervention that are considered to be most effective. In relation to current issues, concern was expressed in regard to normalisation of substance use within society, especially when it comes to alcohol and cannabis/weed which is now available in many formats including cookies, muffins, jellies and vapes containing Tetrahydrocannabinol (THC) a psychoactive substance that is not registered for use in Ireland. Additional, concern expressed about community breakdown, increased violence/intimidation, poverty, mental exploitation and indebtedness.
FIRST EVER INFANT MENTAL HEALTH MASTERCLASS FOR MAYO
Various professionals across the HSE, Tusla, disability and the voluntary sector representing key services that support families and children from conception to infancy attended the first Infant Mental Health Masterclass in Mayo.

Everyone was there eager to learn more about the concept of infant mental health to further support the social and emotional development of children and parental wellbeing.
This event, which took place in the Atlantic Technological University, Castlebar, was hosted by the Mayo Infant Mental Health Forum, with the support of the HSE and Mayo CYPSC. The event was facilitated by two leading IMH specialists from the Irish Association for Infant Mental Health, Catherine McGuire and Mairead Carolan.
The masterclass covered the scientific evidence and theory that supports and underpins infant mental health as well as the clinical application in which parents and babies are supported via an infant mental health lens. Sensitively responding to baby’s needs by trying to read their nonverbal cues, making eye contact, comforting through gentle touch, holding, snuggling and sharing in mutual pleasure are ways to support the attachment parent-infant relationship.
The masterclass was very instructive in emphasising the importance of supporting parents own developmental needs as they transition into parenthood and all of its challenges. Parents are empowered, not by being told what to do necessarily but by their own unique parental experiences and needs in relation to their individual babies validated by a trusted other. This process of ‘being with’ and engaging parents to adopt a reflective curious stance regarding their baby’s needs and communications is the essence of an IMH approach.
MIDWEST COMMUNITY HEALTHCARE HELPS DELIVER AN EXTRA 160 MEALS PER DAY ACROSS CLARE

HEALTH MATTERS SPRING 2023 18 |
Some of the delegates who attended Adolescent Addiction Service’s 25th Anniversary Conference.
Dr Jeananne Garavan, Senior Clinical Psychologist and Chairperson of Mayo Infant Mental Health forum; Facilitators Mairead Carolan and Catherine Maguire, IAIMH; Seamus Beirne, Manager of Mayo Primary Care Services; Mary Skillington, Early Childcare Education ATU and Chairperson of the Early Years CYPSC Committee, Mayo.
Left: Páraic McMahon, volunteer; Kate Tierney, volunteer; Eimear Murphy, Meals on Wheels Co-Ordinator; Alice Delaney, volunteer; Vincent Delaney, volunteer; Eileen McGrath, volunteer; Siobhan O'Driscoll, Operations Manager, Obair CLG; and Conor Mulqueen, Kitchen Assistant.
Right: Alannah Slevin, Chef, and Erica Long, Head Chef, Obair Meals on Wheels Service.
INAUGURAL MIDWIFERY CONFERENCE A WONDERFUL LEARNING AND NETWORKING OPPORTUNITY
The HSE Midlands Nursing and Midwifery Planning and Development Unit and the Regional Centre for Nursing and Midwifery Education collaborated with the Maternity Units at Regional Hospital Mullingar and the Midland Regional Hospital Portlaoise in presenting the Inaugural Midlands Midwifery Conference.
The conference, titled Woman-centred Care through Collaborative Midwifery and Obstetric Practice, was attended by approximately 100 delegates, representing maternity units from all over Ireland, while frontline midwives could follow proceedings and engage virtually through live streaming.

It provided an educational platform for midwives to showcase their advancements in maternity care, while learning from keynote speakers from the UK - Sascha Wells Munro, Deputy Chief Midwifery Officer for England; and Professor Donald Peebles, Professor of Maternal Foetal Medicine; who have made significant strides in promoting collaborative care and maintaining and promoting a strong emphasis on quality and safety in practice.
The voice of a mother, Malvina Walsh, touched the hearts of all present as she shared her personal experiences of maternity care. Much credence was afforded to her valued input, heightening awareness
TEAM TURNS RED FOR WORLD AIDS DAY
The Contact Management Programme (CMP) turned red in support of HIV Ireland’s campaign against HIV stigma and in memory of those who have died from HIV. The team set out to raise awareness for World AIDS Day with the help of the HSE’s Sexual Health Programme.
World AIDS Day has been occurring every December 1st since 1988 and was the first ever global health day to exist. It was set up to unite in the fight against HIV and remember those who have died from HIV related illness. The theme for 2022 was Equalize, a slogan that is a call to action and a prompt to work for the proven practical actions needed to address inequalities and help end AIDS.
HSE MidWest Community Healthcare and Obair Community Development Organisation were delighted to announce the expansion of Obair’s Meals on Wheels service to parts of North, East and West Clare.
Obair has been in existence in Newmarket on Fergus for over 30 years and has been providing Meals on Wheels since 2012. It is a community-based organisation that works with people of all ages to combat social exclusion, as well as supporting older people in the community through the provision of Meals on Wheels. Meals are available
and stimulating attendees as they embrace an evolving journey towards woman-centred care.
Midwives were inspired and enthused by the interrelated presentations and resultant discussions provoked by our keynote speakers, other featured speakers, exhibitors and poster presenters, each passionately representing their individual areas. The inaugural conference was very positively evaluated by all and was seen as both a wonderful learning and networking opportunity for those leading and providing maternity services in the Midland Region and beyond.
For World AIDS Day 2022, Noah Galli in the CMP created displays on the noticeboards with information on HIV, including information on health; services available; history of the day; and book and documentary recommendations. Staff were also encouraged to wear red as part of HIV Ireland’s campaign: #GLORED4WAD which was very successful and incredible to see so much support in the office. A coffee morning was organised where more information on HIV and PrEP & PEP was provided alongside some delicious baked goods provided by CMP staff members. Throughout the coffee morning red ribbons were made available to purchase to raise much needed funds for HIV Ireland. The CMP raised a total of €251.63, which has been sent to HIV Ireland.
primarily to older and retired people who might not be able to cook for themselves due to increasing age, ill-health or isolation.
Obair currently provide approximately 200 service users with Meals on Wheels over seven days a week. Hot meals are delivered five days per week with two cold meals provided on a Friday for Saturday and Sunday.
Over the next six months, this service will expand to include the additional areas, providing an additional 160 meals a day to older people in our community.
Maria Bridgeman, Chief Officer, HSE MidWest Community Healthcare, said, “The HSE is delighted to support this expansion of Obair’s Meals on Wheels service. The commitment of Obair’s staff and volunteers will ensure that this service continues to provide hot meals to more people in more parts of Clare, but also an important social support. Throughout COVID in particular, this was a vital resource for many and I am pleased that this will now be the case in many more communities in East, West and North Clare.”
| 19 HEALTH MATTERS SPRING2023
Midwifery staff from the Regional Hospital Mullingar Maternity Unit: Jennifer Buckley Eighan; Marie Corbett, Director of Midwifery; Maureen Revilles, Assistant Director Midwifery; and Caroline Earley.
Children’s Health Ireland launched the opening of a new Neonatal Unit in Children’s Health Ireland at Crumlin, marking a major step on the way to delivering the neonatal intensive care unit (NICU) in the new children’s hospital and providing world-class neonatal care.

The 18-bedded unit in CHI at Crumlin includes six neonatal high dependency beds for babies with additional care needs. Together with six well-established neonatal high dependency beds in CHI at Temple Street, this will provide long-planned specialised cots for a particularly vulnerable group of patients.
The new unit, which will transfer directly into the new children’s hospital, will also contain specialist equipment, suitable for taking care of small and delicate babies. Particular thanks to Children’s Health Foundation who are making this possible.
Professor Adrienne Foran, Clinical Director in Children’s Health Ireland, said, “The fantastic work behind the scenes now essentially means we will be ready to transfer the service directly into the new hospital as a fully operational service. This is a huge undertaking, with recruitment and training of specialised staff a particular focus. The new hospital will deliver an outstanding neonatal service tailored to patients and families, while investing in staff development and wellbeing.”
EDUCATION INITIATIVE AIMS TO BOOST YOUNG PEOPLE'S MENTAL HEALTH
The University Hospital Limerick-based Junior Health Sciences Academy, a partnership between UL Hospitals Group, HSE MidWest Community Healthcare and University of Limerick (UL), has joined an exciting new psychology education initiative aimed at promoting mental health and wellbeing in young people.

My-Psychology (MY-Psy) is an innovative programme with a focus on positive mental health and well-being promotion, led by Dr Jennifer McMahon, a senior lecturer in Psychology at UL and Director of SCYLab, the School, Child & Youth Mental Health & Well-Being Lab. The initiative is funded by Science Foundation Ireland.
MY-Psy has been rolled out in five schools in the Midwest, with a view to scaling up and delivering the programme to a broader number of schools this year.
MY-Psy has been created with youth stakeholders, who have informed the design of the 12-session programme for Transition Year students. The programme focuses on the science of managing social media, understanding emotions, and building relationships. It also includes sessions on changing health behaviours, and how to engage in research. Speaking for the young people involved in the initial phase of the programme, David Sheahan, a Transition Year student at Castletroy College and member of the MY-Psy Youth Advisory Panel, said: “This type of programme can capture young people’s interest in learning more about science, by getting involved in research that takes the time to listen to and take on our ideas.”
NEW FORUM TO ADVOCATE FOR NEUROLOGY NURSES
A new group has been established to provide support and advocacy for all neurology nurses in Ireland.
The Irish Neurology Nursing Forum (INNF) was formalised in December in The Hodson Bay Hotel, Athlone and a committee was elected. The aims of this group is to:
• Represent and promote the critical role of nurses working in neurology throughout Ireland.
• Provide collegial support and advocacy through continuing educational activities and the promotion of evidence based practice and research and sharing of best practice.
• Collaborate with other professional and voluntary organisations
across the scope of neurology on issues related to patient advocacy, services, policies and guidelines to support excellence in practice.
• Provide opportunities to network locally, nationally and internationally.
• Ensure the delivery of patient-centred quality care.
“Together we are stronger, and we should support our development, encourage education and succession “plan,” explained Sinead Jordan, RANP, Multiple Sclerosis at St Vincent’s Healthcare Group, Dublin.
“Our priority for the year ahead is a focus on education for neurology nurses, to support acquisition of new neurology nurses, CPD, post graduate training, career progression and retention of existing staff and succession planning.”
HEALTH MATTERS SPRING 2023 20 |
NEW NEONATAL UNIT A MAJOR STEP TOWARDS WORLD-CLASS CARE
Dr Jennifer McMahon, Project Lead of MY-Psy; youth advisors David and Cliodhna from Castletroy College, Limerick; and Miriam McCarthy, Manager, Junior Health Sciences Academy.
FIRST ROBOTIC GUIDED CORONARY INTERVENTION IN GALWAY UNIVERSITY HOSPITALS
Galway University Hospitals has carried out the first Robotic Guided Coronary Intervention in Ireland and the UK.
The innovative procedure combines the benefits of coronary intervention with the precision of robotics, offering a range of benefits to patients. The new technology is used in stent procedures to relieve blockages in the arteries of the heart. It allows for greater precision in positioning stents, allowing the Interventional Cardiologists to move the stent a millimetre at a time.
It also allows the medical team to have an enhanced, close up view of the angiographic images and information during the entire procedure.
Prof Faisal Sharif, Consultant Cardiologist, who carried out the first procedure in UHG, welcomed the addition of the CorPath Robotic Angioplasy as a game changer.

“Robotic innovation has come a long way in the last decade. And we in Galway are delighted to have performed the first Robotic Guided Coronary Intervention in Ireland and the UK. The main advantage of robotics is that it is safe and very precise in stent placement,” he said.
The use of robotics in the procedure will also benefit staff, reducing their exposure to radiation. Traditionally, the coronary stent placement procedure is performed in the Cardiac Cath Lab resulting in radiation exposure.
Please see video link for more information: https://www.youtube. com/watch?v=n_uoMV1qsr0
PROPER SUPPORTS CAN HELP PREVENT ADULT ABUSE VIDEOFLUOROSCOPY
Portiuncula University Hospital introduced a new Videofluoroscopy Service for patients in the hospital who need an x-ray assessment of their swallow. The videofluoroscopy service is led out by the Speech and Language Therapy Department in partnership with the Radiology Department.
Supporting decision-making prevents adult abuse and supporting people to respond and report adult abuse if you have a concern were the themes of this year’s Adult Safeguarding Day.
Prior to Adult Safeguarding Day, Safeguarding Ireland, in collaboration with the HSE National Safeguarding Office, an online half-day seminar was held. The seminar focused on hidden abuse among marginalised groups, homeless people, coercive control, etc. Speakers included Dr Michael Browne, Billy Murphy, Amanda Casey, and Sarah Mahon with a video message provided by James Browne, Minister of State for Law Reform at Department of Justice. There were in excess of 400 participants at this seminar.
A number of events were held around the country:
Cork Kerry Community Healthcare held four service engagement sessions with services for older persons and disability services. In the South-East an information stand
was positioned in each of the county areas, manned by a member of the Safeguarding team distributing information and raising awareness. The South-East Safeguarding and Protection Team also launched their new Freephone number (0818 101 101).

CHO6 East held a learning event in Wicklow Library open to anyone interested in learning more about how together, as individuals, families, services and professionals can work to prevent adult abuse and neglect.
Members of the East Safeguarding Team also manned safeguarding information stands in Nutgrove, Ballinteer and Bray Shopping Centre.
CHO7 hosted a network morning with representation from An Garda Siochana Community Sergeant John Dunn, HSE Older Person Services, Consumer Affairs, and Disability Services including staff from KARE.
Videofluoroscopy is an x-ray examination of the swallow and is considered the ‘gold standard’ for the assessment of swallowing difficulties and can be used for assessment, diagnosis and management of dysphagia.
Dysphagia is the medical term used to describe swallowing difficulties which may be a symptom of a range of medical conditions such as; stroke, progressive neurological conditions for example Dementia and Parkinson’s disease, respiratory conditions, head and neck cancer, physical and intellectual disabilities, palliative care needs or the normal ageing process.
Speaking about the new videofluoroscopy service at the hospital, Fiona Brennan, Senior Speech and Language Therapist, said, “On behalf of myself and the team we are delighted to be able to offer this service to our in-patients at PUH as previously patients had to travel elsewhere for the procedure, which took time and was an inconvenience for patients. Having videofluoroscopy will not only improve the range of services we can deliver but also provide a more positive experience for the patient.”
| 21 HEALTH MATTERS SPRING2023
From left: Dr Simone Fezzi, Prof Faisal Sharif and Dr Max Wagener.
Geraldine Power, SPT Business Manager, SECH Safeguarding & Protection Team; Philip O’Reilly, Medical Social Worker Carlow/ Kilkenny ICPOP; Kate Kileen White, SECH Chief Officer; Rob O’Connor A/ Principal Social Worker, SECH Safeguarding & Protection Team; Stephanie Lynch, Head of Service, SECH Quality Safety & Service Improvement; and Susan Bolger, Clerical Officer SECH Safeguarding & Protection Team.
Return A Nursing to
Marian Thérèse Keyes had just retired as the librarian at dlr Lexlcon, the largest public library in Ireland, but a break was not on her mind. Instead of thoughts of retirement, she was taking on the challenge of a return to nursing after 30 years.
“When I found out that I had been accepted for the Return to Nursing Practice Course (RTNP) 2022, I was over the moon. I was also a little anxious - it was just over 30 years since I had been nursing in a hospital environment. Yet I was thrilled to have this opportunity to upskill and return to Connolly Hospital where I had trained in the early 1980s. What changes would I see, would I be able for the pace and above all, could I make a useful contribution?” explained Marian
Thérèse.
This year, the RTNP Programme was delivered nationally, using a Hub and Spoke model with the Regional Centre for Nursing and Midwifery Education Dublin North acting as the Hub. There were 35 participants on the programme from around the country and five general nurses carried out their placement in Connolly Hospital, including Marian Thérèse.
The course started with intense online sessions at end of May, interspersed with attendance in Portrane and Blanchardstown for practical skills and reflection.

“HSeLanD was an excellent resource on just about any topic imaginable – the videos, Q&A, tests, and feedback sessions were light years away from the overhead projectors and transparencies of study blocks in the 80s,” she said.
She was assigned to Laurel Ward, an acute surgical ward specialising in Gastro-Intestinal surgery. “I faced day one with trepidation and nervous excitement. It was terrifying for the first few hours as I worked closely with my preceptor amidst constant groups of doctors doing rounds, phones ringing non-stop, physios, dieticians, occupational therapists, and palliative care teams, not forgetting my nursing colleagues, the backbone of life on Laurel Ward,” she said.
“Meanwhile my biggest personal challenge on day one was getting the beds raised and lowered as there seemed to be an endless variety of gizmos, none particularly intuitive to the novice. Managing patients’ observations for the INEWS sheets and taking diabetic blood sugars were major achievements for the first day.
“As advised by Áine, Liz and Rosita, our hugely supportive and encouraging clinical supervisors, we kept our own Learning Logs. It was gratifying to see how quickly we learned new procedures and put old skills quickly back into practice. I thoroughly enjoyed being back with the patients again. I realised just how much I had missed those interactions – the ability to assist patients on their road to recovery in a very practical way.”
For a fortnight, we worked short days from 7.45am to 3.45pm, followed by a further week of remote learning before the final four weeks of clinical placement with long days ie 7.45am to 8.30pm. It was a challenging period as the days were very busy. The weeks went by quickly and before we knew it, we were working away on our essays and presentations, due by end of July. It was a discipline to work on the wards but also to find time to pull the PowerPoint together and to write up the 2,000 word assignment - but we did it! My chosen topic was Bowel Cancer and Colostomy Care, and this dovetailed very well with my experience on Laurel Ward.”
“Next step for all of us is to fine-tune our CVs and explore future working options. I hope to work part-time, ideally in a surgical or day ward environment. I’m so excited by the prospect of continuing to learn and upskill. I am extremely grateful to have had the opportunity to don the uniform and fob watch once again and to have learned so much from the professional, committed, and caring staff on Laurel Ward,” she added.
HEALTH MATTERS SPRING 2023 22 |
Marian Thérèse Keyes (second from the left) with some of her nursing colleagues.
It was gratifying to see how quickly we learned new procedures and put old skills quickly back into practice
Ukrainian doctor praises ‘life-changing’ support in Ireland
Life-changing is how Ukrainian national Dr Regina Morais describes the welcome and support she has received since her arrival in Ireland in March last year. Now working as a medical translator with Edoc (Out of Hours Urgent GP Service in the east around Dublin and surrounding areas), Dr Morais explained how her work contributes to a better experience for both patient and doctor.
“I am a General Practitioner specialising in General Surgery in Ukraine. I have been working here in Ireland since March of last year – mainly with the Ukrainian population, a lot of whom of course, don’t speak English. It can be very hard for the medical practitioners to be able to obtain the right kind of information from them,” she said.
“And that’s where I come in - because I have a medical background, I am able to not just translate what the patients are saying but can also interpret and explain the nuances and the differences between the medical systems in both countries. This makes it easier for the doctor to be able to understand where the patient is coming from. It’s a lot about empathy and trying to cater for what the patient is looking for.
“A lot of the medications and a lot of how we do things really is different and so for the doctor to be able to not just make a proper diagnosis, but also to make the patient happy, it's best to understand those differences.”
Explaining how her initial arrival in Dublin Airport was a positive experience, Dr Morais outlined how the Immigration Officer she met asked her if she knew where she was going and if she knew anyone in Ireland. She didn’t.
“I told her no, I didn’t know anyone and I didn’t know where I was going. I came because I wanted to finish medical training. She looked at me and she said don’t worry, we're going to take care of you.
“And so for me to hear that, and see her smile, honestly the load that was I was carrying just fell off me. I completely relaxed and I was just knew I was going to be ok.”
Expressing her gratitude, Dr Morais stressed that “we are just really grateful, we truly are for the work that everyone is doing to accommodate us. It really means a lot – it's life-changing.”

Excellence Award
The UCC/HSE Clinical Therapies (Occupational Therapy, Physiotherapy, Audiology, Speech and Language Therapy) Practice Education Team received an Excellence in Teaching Award in University College Cork.
This team comprises UCC and HSE staff members from across the South and South East who work collaboratively to support students and their practice educators before, during, and after placements.

The Teaching Excellence Awards scheme at UCC is the longest-established scheme of its kind in Ireland. These awards recognise staff who have made an outstanding contribution in the pursuit of teaching excellence through innovative and creative forms of teaching, learning and assessment.
The photo shows representatives from the four teams receiving the award.
| 23 HEALTH MATTERS SPRING2023
“She looked at me and she said don’t worry, we're going to take care of you.”
‘Visit a once-in-a-lifetime experience that will stay with us forever’
Leah Evans, Health Protection Nurse at Public Health Mid-West, speaks about her trip to leprosy hotspot in Nepal
Leprosy is a serious bacterial disease that can cause disability, blindness, skin lesions, and paralysis. Many of us hearing the word ‘leprosy’ may assume that is a chronic illness of the past, or a distant problem of Biblical times. However, in some parts of the world, particularly Nepal, this disease continues to have devastating impacts on communities. What makes the picture even starker is the fact that it is a curable disease and one whose worst outcomes can be prevented by multi-drug therapies.
The extreme poverty, deprivation, and poor sanitation in the southern hot flat Terai of Nepal, and nearby northern-eastern India, renders this region a global leprosy hotspot. It was within this context that my colleague, Siobhain Treacy, and I visited Lalgadh Leprosy Hospital Services Centre (LLHSC) in Nepal, a Nepal Leprosy Trust (NLT) project. We visited with a team from NLT Ireland.
Since 2015, the Department of Public Health Mid-West has had strong a partnership LLHSC in Nepal, facilitated through ESTHER Ireland. The European ESTHER Alliance is an initiative that supports the development of partnerships between hospitals in developing countries and health institutions in Europe. In Ireland this initiative is supported by the HSE.

At LLHSC they strive to eliminate leprosy as well as treat the root causes of this cruel disease, namely poverty and socioeconomic deprivation.
The partnership with Public Health Mid-West focuses on improving surveillance and research capacities, and strengthening the provision of preventative and equitable measures of healthcare. In 2022, our department undertook fundraising for a laboratory development project, raising a total of €50,000 through department led events and donations. This fundraising has assisted with the purchasing of laboratory equipment such as analysers and instruments, and the development of staff training and recruitment.
This investment has expanded the precision and testing capabilities in the lab allowing for better targeted treatment of leprosy. It is also envisioned that the lab will be able to develop an income stream from private testing that can then be funnelled into LLHSC to further their work.
Our visit in December was an amazing opportunity for us to gain an understanding of the situation in Nepal. We were given the chance to observe the work being done by LLHSC under their three major programme arms; Hospital Services; Training and Capacity Building;
HEALTH MATTERS SPRING 2023 24 |
A view of the local town
and their Community Programme. LLHSC proudly demonstrated the wonderful care provided through their hospital services, skilled care o ered with compassion, kindness and ambition, and with limited resources.
Treating the leprosy is, broadly speaking, the clinically straight forward part. When you treat a disease, this is generally the end of the clinical pathway when it comes to acute or hospital treatment. However, therapy, rehabilitation, and social and community integration are a major part of the post-treatment process for LLHSC. The stigma associated with leprosy can result in leprosy a ected individuals being ostracised, abused, and forced out of their communities and families. The permanent deformities impact their ability to work, and to provide for themselves and their families.
At LLHSC, we met women who were in-patients along with their small children by their side, a solution that means they are o ered an equal opportunity for treatment.
Even for those who experience heart-breaking lows caused by leprosy’s stigma and disability, the atmosphere within the complex is one of sanctuary, hope and initiative.

The training and capacity building in LLHSC is a space where leprosy a ected individuals are educated on how they can live a healthy life. As a result of nerve damage, they often experience a loss of sensation in their extremities (e.g. hands, feet, and eyes especially). Blindness can result from repeated corneal injury on eyes that cannot feel and cannot blink.
Peer-led self-help groups focus on educating individuals on caring for their eyes and extremities through injury prevention and treatment. There is an in-house prosthetics and device department that provides bespoke solutions including sandals designed to avoid abrasion to the desensitised foot.


We met people who were undertaking skills development, such as beadwork, to provide an income source for their families and we were fortunate enough to be able to purchase some beautiful jewellery. We met people who have received micro-loans for initiatives like purchasing
a goat. By purchasing the goat the person can earn a small income from selling the milk. They are empowered to pursue further borrowing opportunities, based on their ability to pay o the initial loan.
It was humbling and inspiring to see, first-hand, how a person who had been shut out and excluded from society is now being supported to become self-reliant and active again in society.
The highlight of the trip was seeing the work done by LLHSC through their community programme.
The centre oversees the Village Alive Project (VAP), an initiative which has been funded by Irish Aid for the past ten years, through their Civil Society Fund, and overseen by NLT Ireland. Through health education, infrastructure improvements, women’s empowerment, adult literacy, and economic and educational supports, the project supports whole communities in their fight against leprosy and poor living standards. The peer leaders from the self-help groups apply for their village to become a VAP village and, if successful, it is they who will provide the link between the centre and the village.
We were very lucky to visit a VAP village on the 4th International Dignified Menstruation Day, an initiative also supported by the NLT Ireland. During our visit the women were given a talk on healthy menstruation and provided with sanitary protection. We were shown around the village and were able to witness the successes from the project, such as a pump with clean water, meaning the women no longer have to travel distances to access water. There was a shelter for women to wash safely in private and a community hall was in progress where future meetings could be convened, with men from the community engaged in its construction. We met the men and women a ected by leprosy who were now an integral part in the success of their communities. We met recipients of micro-financing who proudly displayed their small businesses that allowed them to support themselves independently. We met young children who were being sponsored to attend school rather than work to support the family income.
Our visit was truly a once-in-a-lifetime experience and is one that will stay with us forever. The strength, hope, ambition and love we experienced was humbling and inspiring. Lalgadh Leprosy Hospital Services Centre showed us what can be done when strong joined up thinking is matched with drive and compassion. Our department is honoured that our fundraising e orts to date and into the future, will in some small way, play a part in the elimination of leprosy as an endemic disease in Nepal.
| 25 HEALTH MATTERS SPRING 2023
Mr. Jiban Thapa (Laboratory Technician) with some of the equipment purchased from the fundraising
Leah Evans, Public Health Nurse in Health Protection at Public Health Mid-West (PHMW) and Siobhain Treacy, CNM2, reviewing skin smear samples with Mr Jiban Thapa, Laboratory Manager
A nurse dresses the ulcerated foot of a leprosy a ected person at Lalgadh Leprosy Hospital and Services Centre (LLHSC)
Mental Health
Young people using Child and Adolescent Mental Health Services (CAMHS) in Kerry have access to a new independent advocacy service. The service is provided by Youth Advocate Programmes (YAP) Ireland and funded by the HSE.
This is the first time that an independent advocacy service of this nature has been provided for young people using CAMHS in the South West. Independent advocacy services have been available in Galway and parts of Dublin and have successfully helped young people to engage with mental health services in a meaningful way.
An independent mental health advocate has already started work in Kerry and is now available to young people using CAMHS in all parts of Kerry.
The goals of the independent advocacy service are to:
• Ensure that the voice of young people using CAMHS is heard
• Empower young people and their families
• Ensure there is good communication between young people and their CAMHS team
• Empower young people to raise issues as early as possible
• Assist young people and families to resolve any issues that may arise as early as possible
Minister for State Mary Butler said the initiative encourages young people and families to speak up for themselves, to ensure good communication with keyworkers and teams, and to support those requiring advocacy to raise important issues when necessary.

Michael Fitzgerald, Chief O cer of Cork Kerry Community Healthcare, said the service feels very fortunate to be able to o er this service.
“At the core of all our mental health services must be a commitment to working towards recovery. We hope that this investment will help young people and their families feel that we are listening to them and consulting with them in a meaningful way. We also hope that our commitment to working with young people will help us to rebuild trust and confidence in CAMHS in the region.”
For more information, see yapireland.ie
HEALTH MATTERS SPRING 2023 26 | |
Independent advocacy service for Kerry CAMHS users
Minister of State for Mental Health and Older People Mary Butler, with Danielle O'Sullivan, independent mental health Advocate from Kerry and Alix Condon, a service user from Cork.
Mental health assessment room ‘part of a vital process to improve the experience and journey’
Cork Kerry Community Healthcare (CKCH)Mental Health Services have opened a new mental health assessment room within the emergency department of University Hospital Kerry (UHK).

The assessment room will be a confidential and therapeutic setting for anyone presenting to UHK in a mental health crisis.
The room is a joint initiative between CKCH Mental Health Services and healthcare professionals from UHK. It creates a separate, calm space which will be used by Clinical Nurse Specialists in Self Harm who already provide a seven-day service (from 8am to 8am), o ering a rapid response to people presenting to Emergency Departments with self-harm and suicidal ideation. The room will also be used by the psychiatric doctor on call to assess patients presenting to ED with a mental health emergency.
24- hour mental health assessment is provided by consultant psychiatrists and non-consultant hospital doctors within the department.
Dr Maura Young, Executive Clinical Director Kerry Mental Health Service, said she was delighted that people presenting to UHK in a mental health crisis can now meet with mental health professionals in a ‘confidential and therapeutic setting’.

“It is my hope that the new mental health assessment room will improve the experience and will benefit all those who access the service in the Emergency Department in University Hospital Kerry,” she said.
Dr Herlo Coetzer, Consultant in Emergency Medicine, said: “Our new dedicated assessment room is not a destination, but forms part of a vital process to improve the experience and journey of a vulnerable patient cohort. The new assessment room helps improve patient and sta safety, promoting an environment for mental health professionals to assess patients, while aiding in reducing patient stress levels so they have better care outcomes.”
Cathy O’Sullivan, Assistant Director of Nursing, Kerry Mental Health Service, said, “The importance of creating and maintaining a safe environment is a top priority for those in need of mental healthcare.”
DEVELOPING A MENTAL HEALTH PROMOTION PLAN FOR THE IRISH HEALTH SERVICE



An article outlining the process of developing a mental health promotion plan for the Irish Health Service was recently accepted for publication to the Journal Advances in Mental Health. Stronger Together: The HSE Mental Health Promotion Plan, 2022-2027, is a five-year plan, and includes action areas focused on promoting positive mental health across the population and among HSE sta .
The plan takes a life course approach and includes actions of relevance to the general population. It considers the needs of specific population groups such as children and young people, the working aged population, older people and other priority groups and also specifically takes into account how the reach of this Plan can be extended beyond the Health Service. The Mental Health and Wellbeing Programme led on the development of the Plan with the support of a wide range of internal and external partners.


The article outlines the process of developing Stronger Together, the first Mental Health Promotion Plan for the HSE, together with key reflections and learnings from the experience. The framework for the development of Stronger Together and the processes involved are outlined. This constituted three distinct phases: (i) planning; (ii) identifying core actions; (iii) stakeholder engagement over a two and a half year period. The development of this plan marks a watershed in placing mental health promotion on the policy agenda at a national level within the HSE and in Ireland, building on the existing health promotion policy and practice infrastructure in Ireland. A national implementation oversight group is now in place within the HSE to oversee the implementation of the plan.

| 27 HEALTH MATTERS SPRING 2023
Dr Herlo Coetzer, ED Consultant; Dr Maura Young, Executive Clinical Director, Kerry Mental Health Services; Mairead O’Sullivan, A/Assistant Director of Nursing; Cathy O’Sullivan, Assistant Director of Nursing; Gerard Sheehan, ED Crisis Nurse; Declan Cronin, Assistant Director of Nursing (MHS); and Tess O’Donovan A/COO, South/ South West Hospital Group at the opening of the new mental health assessment room at the Emergency Department of UHK. Photo: Dominik Walsh
PALS co-ordinator will bring voice of patient to forefront
The newly appointed Patient Advocacy and Liaison Service (PALS) Co-ordinator at Sligo University Hospital ‘will bring the voice of the patient to the forefront of everything we do’. Welcoming the appointment of Catherine Kelly (pictured right) as its first PALS Coordinator, Grainne McCann, Hospital Manager, said, “This service will be the focal point to enable us to learn from patients’ experience of the service, provide feedback on their concerns and be a catalyst for further improvement and change.”
The PALS Co-ordinator acts as the main contact between patients, their families, carers and the hospital. They ensure that the patient voice is heard either through the patient directly or through a nominated representative.
Catherine, a native of Sligo, gained valuable experience working with patients and their families having previously worked as a Clinical Nurse Manager and Clinical Facilitator in the Emergency Department at SUH.
Speaking of her new role Catherine explained, “Communication is a key part of the role and I work closely with health care staff across all disciplines on patient care issues and speak on behalf of those patients and their families who wish me to do so.
“I place the value of kindness, care, compassion and trust at the core of my daily work. It is important that we respect our patients and ensure that the ethos and values of Sligo University Hospital are evident through the work carried out by all of our staff.”
Maura Heffernan, Director of Nursing at the hospital said, “We are so delighted to introduce the Patient Advocacy and Liaison Service to Sligo University Hospital. Catherine has worked in the hospital for many years and will bring the voice of the patient to the forefront of everything we do.”
VOLUNTEER ROLE IS ‘HUGELY REWARDING’
THE Patient Advocacy Liaison Service
(PALS) of UL Hospitals Group is looking for volunteers to join their teams to welcome patients and visitors, assist with way-finding and general queries, and help patients and their loved ones to give feedback on their experience of hospital service.
PALS volunteers are ambassadors for hospitals, a crucial element of UL Hospitals Group efforts to improve care standards and the patient experience. Volunteers dressed in distinctive red tabards with embroidered gold logo, serve in multiple roles, whether giving directions or accompanying patients to appointments, giving out information, or gathering patient feedback.
The service has been recruiting people willing to volunteer in the hospitals for a minimum of three hours per week during the mornings between 8.30am and 12.30am.
Virginia O’Dowd, a retired teacher and former public representative from Nenagh, said getting involved as a PALS volunteer in Nenagh Hospital has been hugely rewarding and called on people who may have free time on their hands and are interested in


volunteering, to put their names forward.
“As a PALS volunteer, you make a huge difference for patients, and their relatives and visitors, by doing simple things well. Before I got involved, I knew that even visiting hospitals can be quite daunting and disorientating, so I often thought that having somebody there to meet and greet, just to give a friendly smile, to help if needed, would be a very nice intervention,” Virginia recalled.
“I get a lot more out of PALS than can be actually measured. It’s only one morning a week, and most people if they have the free time could easily give one morning a week. I like interacting with people and I like giving them a hand where possible. I always come home feeling richer and more appreciative of my own health, and it also gives me a great sense of pride in Nenagh Hospital and its services to the community,” she added.
In Ennis Hospital, Assistant Director of Nursing Mary McInerney said local people volunteer for PALS for a wide range of reasons.
“One of our longest serving volunteers told me simply that they enjoyed giving something back to their
local community, and PALS gave them a very social way of doing it. One volunteer who comes from overseas got involved with the service as a way of making connections and friends when they were settling into the area. Yet another volunteer joined the service after the death of their husband: they found it very important to commit to something positive; helping others helped them to adapt to their new life,” she said.
For some, volunteering for PALS can be the very first step on a new career path. One of the very first volunteers for the service in Ennis Hospital subsequently became a porter in the hospital. Anyone interested in volunteering for PALS is asked to send an email outlining hospital preference and available hours to UHLPals@hse.ie
HEALTH MATTERS SPRING 2023 28 |
Virginia O’Dowd pictured at Nenagh Hospital in the distinctive red tabard that is worn by volunteers with the Patient Advocacy Liaison Service.
Let Play Cork
Creating playful towns and cities across Ireland
Cities face challenges of ageing, climate change and social exclusion and play can be used as a lever for fun, inclusive, healthy and sustainable urban development. Streets aren’t just for cars and libraries aren’t just for books – they can also be a playground! Any well planned public space can be transformed into a playground for everyone.
Cork, through the interagency ‘Let’s Play Cork’ Partnership, became a transfer partner in the European Playful Paradigm network, led by the city of Udine in Italy. Both cities had an existing relationship through the WHO Healthy Cities Network, a programme co-ordinated in Cork by Senior Health Promotion O cers in the Health and Wellbeing Department. However, this was Cork’s first URBACT experience.
The city of Cork was then chosen as an exemplar city to develop a culture of play for the benefit of all ages and abilities. Ireland’s National Playful Paradigm Transfer Network (NPTI) lasted 18 months, with Cork as the lead city transferring the good practices to five partner towns - Portlaoise, Sligo, Donegal, Rush and Rathdrum.
From the very beginning, Cork embraced the idea of ‘play’ as a mechanism to stimulate dialogue in the city.

The most impactful action during the project was to open streets for play, which ultimately led to the permanent pedestrianisation of the Marina area of Cork city. This set the wheels in motion to develop pedestrian-friendly city centre streets, helped by the pandemic lockdown. These streets made a lasting impression on the Cork public and politicians, with a growing recognition that streets are more than
just functional transport infrastructure. Let’s Play Cork is now at an advanced stage to secure a permanent play street in the city centre.
Cork City is continuously finding ways to develop a stock of play equipment for communities to embrace play in their events. Partnering with the Cork Sports Partnership and with the assistance of Healthy Ireland funding, the 10 libraries in Cork city have embedded a play bag loan system, story bags for playful storytelling for children and a stock of board games and Lego.
With the shift to remote working, Let’s Play Cork also seized the opportunity to develop and distribute 8,000 play packs to families with young children and older adults living alone and in nursing homes all over Cork City and county during the lockdown periods.
The development of the Cork City Playful Culture Trail involved the development of a map of cultural institutions across the city and was complemented by the provision of playful elements to make visits to these venues more fun. Participating cultural institutions such as art galleries, historical museums and churches found it worked well for their visitors and especially attracted more local families than usual.
The Cork playful journey is a great example of an integrated and creative approach to healthy and sustainable urban development. At local level, Cork has e ectively engaged partners across policy areas, whilst at the same time connecting with European, national and local players and resources. Let’s Play Cork has helped to forge a momentum and energy between the stakeholders that would probably not have happened without this European funding opportunity.
| 29 HEALTH MATTERS SPRING 2023
Pancreatitis app
Tallaght team develop app for chronic sufferers

Tallaght University Hospital (TUH) and its interdisciplinary Chronic Pancreatitis team have showcased an innovative mobile phone app, termed the SmartCP app. This app empowers patients to take control of their condition and will improve communication with the hospital team. The app will streamline and coordinate patient management and will enable TUH to care for patients in their homes and communities.
The SmartCP project is supported by an innovation grant from the Department of Public Expenditure and Reform. The project was coordinated by Professor Kevin Conlon Consultant Surgery at TUH and Professor of Surgery at Trinity College Dublin; Sinead Duggan, a Senior Research Fellow in Trinity College Dublin and former TUH Nutrition and Dietetics Department member; and Marie Egan, Clinical Nurse Specialist in TUH.
It was developed in collaboration with TUH’s Innovate Health Team, ICT and Finance Departments, as well as, the Department of Computing in Technological University Dublin. Patients with chronic pancreatitis have also been central to its design and development. In tandem with this project, the group at TUH set up the first Patient Support and Advocacy Group for chronic pancreatitis in this country, Chronic Pancreatitis Ireland.
Chronic pancreatitis is a condition where the pancreas is inflamed and becomes progressively more damaged over time. It is incurable and management centres around dealing with symptoms and complications as they arise. Patients with chronic pancreatitis suffer from debilitating gastrointestinal symptoms (steatorrhoea, bloating, nausea, vomiting), they often lose weight and become malnourished. As the disease progresses, they develop brittle diabetes, osteoporosis and nutrient deficiency. Patients typically suffer from severe, untreatable, abdominal pain. Patients also have a higher-than-normal lifetime risk of developing pancreatic cancer. They are complex patients requiring specialist, multi-disciplinary care.
TUH runs the biggest centre for chronic pancreatitis care on the island of Ireland and currently has more than 300 patients on their clinical database. Many of them live outside of Dublin. There are several types of out-patient clinics for chronic pancreatitis per week, including a Clinical Nurse Specialist led clinic and a specialist type 3c diabetes clinic. TUH research has shown that Ireland has among the highest numbers in Europe of those suffering from chronic pancreatitis.
Professor Conlon, project PI, said “Our hospital is very well placed to take a lead on the development of this technology, we run the only dedicated chronic pancreatitis service nationally, providing care for over 300 patients. This new digital tool will improve patient access to specialist care, no matter where they live in the country. The team and I are grateful to DPER who funded us, to the Meath Foundation who have funded much of our research over the years, and to the Innovate Health Team in TUH for their ongoing support and encouragement. Our Clinical Nurse Specialist, Marie Egan, is central to both the running of our service and to the practical roll-out of this innovative technology.”
Core functions of SmartCP
Clinical symptoms: Patients are able to react more quickly to deteriorating health and provide better and more accurate care to physicians using the app’s graphical information.
Information: The app contains information through text on video on: the pancreas, chronic pancreatitis, diabetes, nutrition/ exercise/lifestyle, and pancreatic cancer, as well as informational videos from the multidisciplinary team.
A better patient experience: Patients are empowered to take control of their chronic disease and will have the confidence that they are being heard.
Better care for patients based outside of Dublin: As the only chronic pancreatitis multidisciplinary service in Ireland, many of the hospital patients reside outside of the city. SmartCP enables clinicians to provide a better service for those patients, ensure that care is not dependent on geography, whilst reducing expense and time-burden for patients.
Resource savings: With improved disease management there will be less attendances to ED, fewer crisis phone-calls, a reduction in emergency admissions and hospitalisation. There will be more rationale allocation of clinic time to those who need it (preventing unnecessary follow-up in some cases) –therefore reducing the burden on the hospital and enabling valuable clinical resources to be used to see more patients.
Next steps: The team’s next step is to formally launch the app early next year and complete a study to determine the feasibility of SmartCP in the management of patients with chronic pancreatitis. They will also explore the effect of the intervention on crisis events, patient symptoms, hospitalisation and cost of care.
HEALTH MATTERS SPRING 2023 30 |
At the first showcase of the new innovative mobile phone app, termed the SmartCP app, at TUH were Dr Natalie Cole, Head of Innovate Health at TUH; Aidan McGrenra, Patient Representative; Professor Kevin Conlon, Consultant Surgeon at TUH and Professor of Surgery at TCD; and Chris Kiernan, Public Service Innovation Fund Manager.
Innovative new clinic
Time and persistence pays off as new gastroenterology triage clinic slashes children’s wait times

An innovative new clinic is providing timely and e ective family-centred care while reducing waiting lists and times for children to be seen by the Gastroenterology team at Children’s Health Ireland (CHI) at Tallaght.

The Gastroenterology Active Triage (GAT) clinic is a collaborative multidisciplinary team approach to triage of referrals into condition-specific groupings. The initial triage is consultant-led, followed by CNM2 and dietetic virtual review. Results and history are re-triaged by the consultant and outcomes are decided.
Due to cancelled and reduced clinics during the pandemic, children with Inflammatory Bowel Disease (IBD), Eosinophilic Oesophagitis (EOE), Coeliac Disease (CD) and other gastroenterology conditions were waiting up to 18 for urgent, and up to 35 months for routine gastroenterology review.




Waiting as long as 35 months for review adversely a ects a child’s socialisation, family life, growth and development. Early triage through GAT helps children either achieve a diagnosis sooner or move on from the sick role, missing school or sports; etc, explained Emer O’Toole, Paediatric Gastroenterology CNS.
“While it took a great deal of time and persistence to set up GAT, especially during such a time of upheaval and crisis, however, the pandemic also provided many opportunities for change. We had to focus on how we could do things more e ectively with the resources we had and so the idea of Gastroenterology Active Triage (GAT) evolved. Through GAT, children avoid unnecessary anaesthetics. It identifies
those that need it most, also making the best use of consultant and theatre time. Intensive education and resources are o ered to children and their families through GAT,” said Emer.
GAT has resulted in a 70% reduction in the new patient waiting list across all priorities.
GAT clinic was set up in Children’s Health Ireland at Tallaght in March 2021 it initially provided virtual management of new urgent referrals and since March 2022 includes routine referrals. GAT is operated by a CNM2 and a dietician who take a detailed medical history over the telephone and then investigations – bloods, faecal calprotectin; etcare ordered as appropriate. The history and test results are reported to the Consultant Gastroenterologist at the weekly meeting who then decides the clinical outcomes.
“By October 2022, we had achieved all our aims: triage of all new referrals within three weeks, reduction in waiting times for all referrals, and the avoidance of double wait periods, and we have eliminated the New Urgent Patient waiting list by 2023,” said Emer.
“It has been incredibly exciting to see this scheme through from design to fruition and, of course, wonderful that it benefits our patients.”
GATs success has been recognised at the Irish Healthcare Awards 2022 where it was highly commended in the category of Outpatient Initiative of the Year. The team said they would be delighted to share their GAT system.
“It would be amazing if it could be rolled out to other specialists and across other hospitals and services,” added Emer.

| 31 HEALTH MATTERS SPRING 2023
Molly Fitzgerald, dietitian; Ciara Barry, CNM2; Dr Shoana Quinn, Consultant Paediatric Gastroenterologist; Emer O’Toole, CNS Paediatric Gastroenterology; and Amy Mizell, GAT clerical o icer.
The team at the Irish Healthcare Awards: Niamh Brosnan, dietitian; Dr Shoana Quinn, Consultant Paediatric Gastroenterologist, Emer O’Toole, CNS Paeditric Gastroenterology; and Ciara Barry, CNM2 Paediatric Gastroenterology.
Eliminate Cervical Cancer
Join us on the journey to make Ireland one of the first countries to eliminate cervical cancer
Ireland is one of the first countries in the world to publicly declare its commitment to the global initiative to eliminate cervical cancer.
In January, the National Screening Service, National Immunisation O ce and National Cancer Control Programme published Ireland’s roadmap to cervical cancer elimination to mark Cervical Cancer Prevention Week 2023. The roadmap sets Ireland on a path to reach global targets set by the World Health Organisation (WHO).
Welcoming its publication, Minister for Health Stephen Donnelly said it’s “a truly significant initiative in women’s health” and that Ireland is “in a strong position” to reach the targets.
The launch of the roadmap was covered by national and local media, including Newstalk Breakfast and the Karl Henry podcast Real Health. The Irish Independent’s Health and Living supplement also featured our patient spokesperson for the campaign, Kim Hanly, who was diagnosed with cervical cancer in her early 20s. Dr Sarah Fitzgibbon also recorded a video explaining what cervical cancer elimination is and how Ireland will achieve it, here
What does elimination of cervical cancer mean?


The current rate of cervical cancer in Ireland is around 11 women per 100,000 per year. The WHO defines elimination as fewer than 4 women developing cervical cancer per 100,000 per year. Reaching this milestone would make cervical cancer a very rare disease and bring us to a point where there are so few women diagnosed with cervical cancer that it is no longer a public health problem. When a disease is eliminated, prevention measures, in this case screening, HPV vaccination and early detection and treatment, need to continue to maintain the low rates of disease.
What are the targets?
Known as the 90-70-90 targets, the WHO says every country should reach these by 2030 to put the world on course to elimination:
• 90% of girls vaccinated against HPV by 15
• 70% of women screened by age 35 and again by age 45





























• 90% of people identified with cervical disease treated




Are the targets achievable?
In Ireland, we have all the tools we need to prevent and/or reduce the burden of the disease and to achieve the global targets of timely HPV vaccination, regular HPV cervical screening, and early detection and treatment for those who need it. The HPV vaccine, screening test and cervical cancer treatments o ered in Ireland are among the highest quality available internationally, and importantly, all of these services are free of charge through the HSE. This places Ireland in a position to be able to reach the targets set out for elimination.
How do we get there?
We’re currently working with an international team of experts in Australia to estimate Ireland’s target date for elimination. This will be announced before the end of the year. Once Ireland’s elimination date is established, an action plan will be developed to ensure high uptake of the HPV vaccination and screening programmes, and timely treatment for those identified with cervical disease. Especially among those people who are less likely to take up their vaccination or screening invitation, or access pre-cancer or cancer treatment at an early stage.
Achieving the targets equitably requires vaccination, screening and treatment services to work together taking a whole of society approach. This includes collaboration with patient advocates, and relevant NGOs. This is already happening with the establishment of a Cervical Cancer Elimination Partnership in 2021. This will expand further in 2023 to include wider representation from education and health sectors, advocacy groups and patient representatives.
The aim is to provide an environment in which all people have inclusive and equitable access to vaccination, screening, pre-cancer treatment and cancer management services that meet their needs. Work is required to understand why some people do not access services regularly. it is important to understand the barriers some groups of people face and work them to overcome these.
Around 300 cases of cervical cancer are diagnosed in Ireland annually. National Cancer Registry Ireland data from its report ‘Breast, cervical and colorectal cancer 1994-2019: National trends for cancers with population-based screening programmes in Ireland’ shows that screen-detected cancer cases were, on average, detected at a substantially earlier stage than other cases diagnosed at the same ages. In general, the earlier a stage the cancer is diagnosed at the more treatable it is and the better the outcome.
The NCRI report also showed that cervical cancer incidence rates have reduced each year by 2.8% since 2009 with the introduction of screening. As we see the impact of vaccination in the coming years we expect the rates to continue to drop. There are some types of cervical cancer that cannot be detected in screening, including types that are not caused by HPV.
Cancer can also develop between screening tests. That’s why being aware of the symptoms of cervical cancer is so important. If you do experience symptoms, even if you’ve recently had a normal screening test, it’s really important that you contact your GP.

HEALTH MATTERS SPRING 2023 32 | |
TELL EVERYONE…
Cervical cancer could be the first cancer ever to be eliminated globally. Screening, vaccinations and treatment are key to getting us there. In Ireland, we have all the tools we need. Now more than ever, as we drive towards elimination, let’s each play a part with ensuring that everyone who is eligible benefits from these vital services.
As WHO Regional Director for Europe, Dr Hans Henri P Kluge remarked in support of the publication of Ireland’s roadmap to elimination, “A cervical cancer-free future is within our grasp. We look to Ireland as a trailblazer in achieving this ambitious goal.”
By Susan Donlon, NSS Communications










HOW YOU CAN SUPPORT ELIMINATION














There are several ways to support Ireland’s e orts to eliminate cervical cancer. Everyone can play a part and thousands of people are already doing so.


• #GetInformed so you can talk to patients about elimination and how important it is to come for screening, get vaccinated and recognise the symptoms of cervical cancer. You can find out more at https://www.screeningservice.ie/cervical-cancer-elimination.html
• Health and social care workers can support people to make informed decisions about accessing screening and vaccinations:
» Complete the short eLearning Course ‘Reducing cancer risk: PopulationBased Cancer Screening Programmes’ to learn more about the National Screening Service programmes. This 20-minute overview will provide you with the knowledge to encourage and support people to consider the benefits of participating in screening.
» Refer people to trusted sources of information CervicalCheck.ie and HPV.ie.
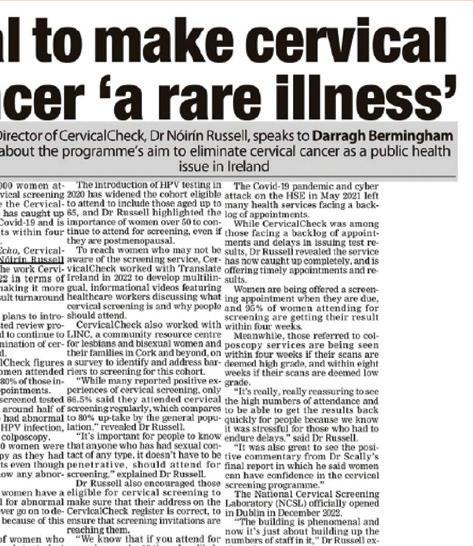




































































» Order free resources (posters and leaflets) for your practice, clinic or service at HealthPromotion.ie








• Parents, their children and young people are playing a significant role in reaching global targets by participating in the HPV vaccination programme. Anyone aged 16 to 25 years who missed out on the vaccine in secondary school can now get it through the Laura Brennan catch-up programme.



































• Every eligible person (women and people with a cervix aged 25 to 65) can check the register online at cervicalcheck.ie to find out when their next screening test is due and to ensure that current address and contact details are correct to receive invitations to screening, reminders and results. When screening is due, make an appointment with a GP, clinic or any registered provider, you can find a list at HSE.ie.





• Listen to this Real Health podcast with Karl Henry and Dr Sarah Fitzgibbon chatting about everything you need to know about preventing cervical cancer, from screenings to symptoms and HPV vaccinations. Share it with family, friends and colleagues.



















| 33 HEALTH MATTERS SPRING 2023
Flu vaccination campaign

boosted by new collaborations
Collaboration brings us together, makes us focus on the task at hand and allows us to share expertise and learning with colleagues across a range of disciplines. Each year our committees and working groups roll into action, muscle memory at the ready, drawing on the latest research and evidence to engage with our population on lots of health protection and disease prevention campaigns.
Every year representatives from across Community Healthcare, Hospital Groups, Section 38 agencies, vaccination teams, long-term care facilities and Public Health come together to work on the Winter Influenza Vaccination Campaign. We use evidence-based research from abroad and at home to advise healthcare workers and the public on what to expect in the winter months.
Navigating Reform in Public Health has led to increased opportunities for collaboration and also the increased challenge of working across new geographical areas. As a newly geographically realigned area in Area C (CHO5/SECH & CHO6), we are now sitting around the table with new colleagues, familiarising ourselves with new place names, addresses and settings and developing relationships and networks to best protect our population and staff.
So as this year’s winter plan rolled round and while we knew the challenge ahead, it was very uplifting to work alongside new people and share our experiences in best
practise. This was the first collaboration piece between Public Health Area C, SECH and CHO6 Influenza Leads and SECH and CHO6 Community Infection Prevention and Control Teams. Improving our service is always at the forefront of our work and this year once again we reviewed previous campaigns, analysed what worked and challenged ourselves to see what else we could deliver for our healthcare workers to assist in supporting the influenza vaccination programme.
Providing up to date information in an easy format clearly written and divided into quickly accessible, marked subsections were our key deliverables and this was done through a user-friendly
printed Influenza Management Folder which was also available electronically. Seven sections including National Guidance, Outbreak Management Guidance, FAQs, useful contacts and posters all at staff fingertips.
To amplify it into a living working folder, we included a small number of Influenza and COVID-19 swabs within the folder. Through the guidance of our Communications Officers in Public Health and SECH, we produced a short video promoting influenza vaccination featuring staff from across Area C to share on social media channels.
Developing the folders is only part of the task and credit is due to our teams on the ground who delivered them to the Long-term Care Facilities and our Peer Vaccinators who work so hard to deliver the Influenza vaccination campaign and highlight the resources available.
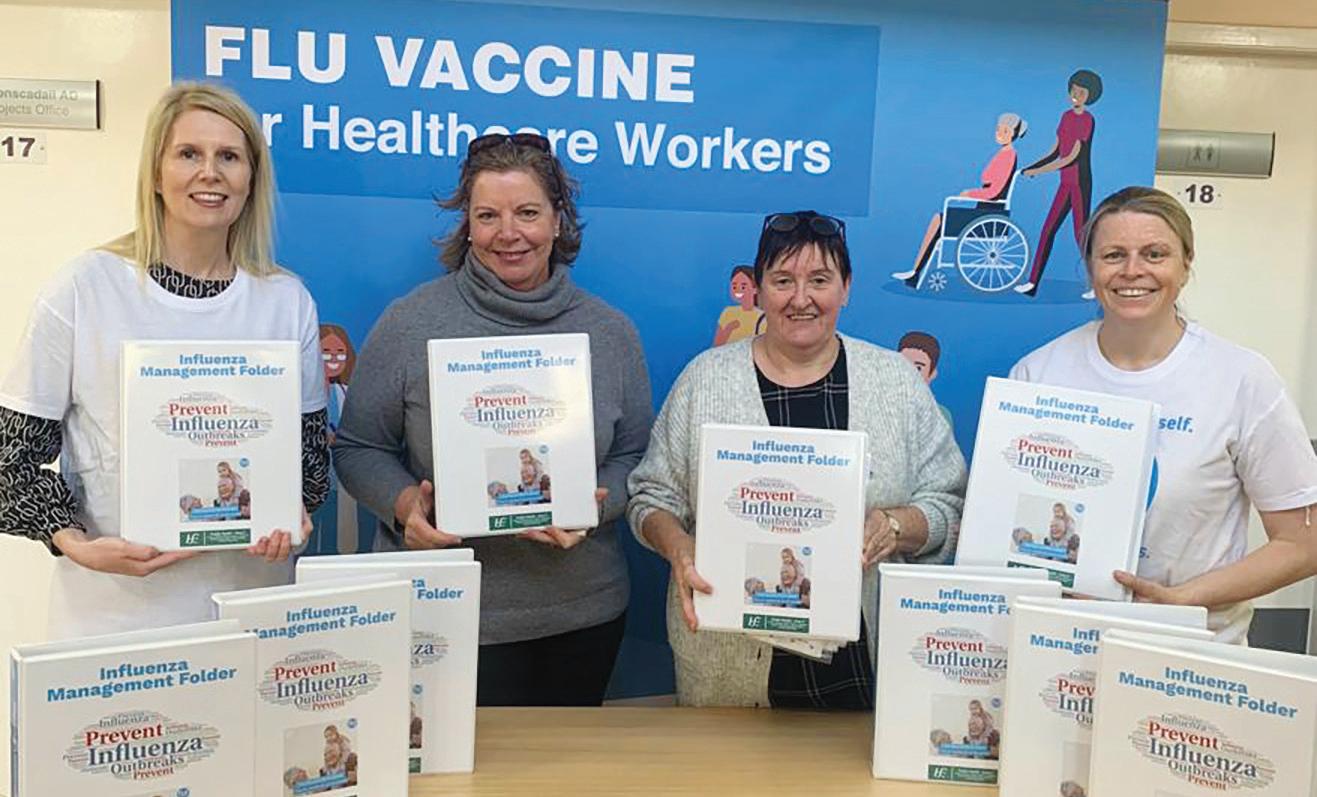
Feedback from our frontline healthcare workers has been very positive and we are looking forward to our next campaign and our collegiate collaboration.

HEALTH MATTERS SPRING 2023 34 |
Pictured alongside the Mobile Vaccination Unit were Ciara Monahan, campaign administration support; Dr Catherine Lynch, specialist Public Health; Gillian Buggy, Flu Lead SECH; Sarah Cripps, Public Health; and Fatemah Mirasehmi.
Video still featuring (front row) Tara Donnelly, nursing team; Dr Catherine Lynch; Laura Fennell, nursing team; and Dr James Gilroy; (back row) Shogi George and Anne Healy, nursing team; Dr Therese McGlacken; and Michelle Connolly, ADON.
Nicole Nugent, ADON QSSI; Annette O’Higgins, DON Dalkey Community Nursing Unit; May Kavanagh, DON St Coleman’s Hospital Wicklow; Deirdre Duffy, Co Flu Lead in HSE Community Healthcare East.
Virtual Wellbeing Hub
designed by ‘listening to new mums’
The Maternity Department at University Hospital Galway has introduced a ‘New Mums Virtual Wellbeing Hub’ which provides online support, advice and signposting on postnatal services available to mothers and their families both in the hospital and the community. The hub is a collaborative initiative between the Maternity Department, UHG and Community Healthcare West. The team includes a Midwife, Social Worker, Paediatrician, GP, Pharmacist, Public Health Nurse, Dietician, Physiotherapist, Lactation Consultant, Urogynaecology Specialist Midwife and a member of the Perinatal Mental Health Team.

Carmel Connolly, Clinical Nurse Manger 2 and Project Lead, said, “The lack of support and connection, change in identity and unrealistic expectations of parenthood due to the influence of social media has affected maternal wellbeing. Feeling overwhelmed, exhausted and lonely is not uncommon.
“Listening to our mothers concerns led to the design of this new service. Mothers need to connect with other mothers. There is a real fatigue and loneliness after giving birth for many women. They need
consistent, evidenced-based information and signposting to services available to them in Galway.
“We launched the hub in November and had 19 couples in attendance. It is so reassuring to see the difference the hub has already created in the lives of mothers and their families. There has already been increased referrals to Physiotherapy, Lactation Consultant and Urogynaecology Specialists. Mothers have connected with these services as a direct result of attending the wellbeing hub”
The virtual hub is live on the third Tuesday of every month at 11am and booking is available via www. uhgmaternity.com.
One mother who attended the hub said, “It was lovely to be able to connect with other mothers. I was having breastfeeding issues and I knew who to contact after the hub. It is reassuring to see the healthcare team from the hospital and the community working together. It is a fantastic service.”
Another mother said, “I wish this service was available after my first baby. I did not know what was normal. I was so down in myself and was embarrassed to look for help. I picked up lots of skills from the Clinical Psychologist. I am very grateful for the support of this hub.”
| 35 HEALTH MATTERS SPRING2023
“Listening to our mothers concerns led to the design of this new service. Mothers need to connect with other mothers.”
From left, Ailish Killilea, Assistant Director of Public Health Nursing, Community Healthcare West; Helen Murphy, Director of Midwifery, University Hospital Galway; Carmel Connolly Project Lead and Clinical Midwife Manager 2, University Hospital Galway; June Barrett Dietitian, University Hospital Galway; Peter Kidd, Pharmacist, University Hospital Galway; Anne Marie Grealish Assistant Director of Midwifery, University Hospital Galway; Eithne Gilligan, Clinical Nurse Manager 2, Community Midwives, University Hospital Galway; Marie Conway, Masters Student, Social Work Department, University Hospital Galway and Mary Moran, Midwife, Parent Education Services, University Hospital Galway.
Traveller
Health
First National Traveller Health Action Plan to improve health outcomes
Improving the health experiences and health outcomes for Travellers is the aim of the recently launched first National Traveller Health Action Plan.

The Action Plan acknowledges the severe health inequalities that Travellers experience, arising from the social determinants of health, and the obstacles they can face in accessing healthcare services. It will provide a solid foundation upon which to build and maintain a legacy of success in addressing the additional health needs of the Traveller population.
Speaking at the launch, Minister for Health Stephen Donnelly said he “strongly endorsed” the Plan as it “aligns with my department’s strategic priority to improve access to healthcare for socially excluded groups. It is a comprehensive public health response to the health needs of Travellers that that sets out tailored and affirmative measures to prevent disease, promote health and prolong life, and are delivered in partnership with Travellers.
“In particular, I welcome the focus on the mental health needs of Travellers, which is in
line with the prioritisation of Travellers in my department’s mental health policies. To address the needs of Traveller women who experience homelessness additional funding is being provided from the Women’s Health Action Plan.”
The plan includes health and social care interventions that will have the most impact on Traveller health including mental healthcare and chronic disease diagnosis, early interventions and management.
Mary Brigid Collins, Primary Health Care for Travellers representative on the National Traveller Health Action Plan Steering Group, said she was “delighted at the publication of this much-needed National Traveller Health Action Plan. I believe it has the potential to bring about real positive change for Travellers around the country. It has Traveller inclusion at the centre of the plan and recognises the impact of racism, discrimination, poor living conditions, poor outcomes in education and unemployment have on health outcomes.
“It recognises also the importance of active Traveller participation and the role of Traveller Health Units and Traveller Primary
Health Care Projects. Travellers look forward to continuing to work with the Health Service Executive and the Department of Health and will continue to highlight the need for recurring and realistic budgets if we're serious about implementing the Plan.”
Martina Queally, Chief Officer of HSE Community Healthcare East and Chair of the National Traveller Health Steering Group, said, “The National Traveller Health Action Plan is an important step forward in our work to achieve better health outcomes for Travellers. By working together and implementing targeted actions that address Travellers’ specific health needs, we can make a positive impact on Traveller health in Ireland and help reduce health inequalities. I look forward to continuing to work with our partners to support this important work.”
The HSE is establishing a steering group to check and report on the implementation of the plan at national and regional levels. Traveller Health Units will also develop a five-year implementation plan and publish an annual report.
HEALTH MATTERS SPRING 2023 36 |
At the launch of the first National Traveller Health Action Plan were Martina Queally, Chair of the National Traveller Health steering group; Minister for Health Stephen Donnelly, Minister for Public Health, Wellbeing and the National Drugs Strategy Frank Feighan; Traveller comedian Martin Beanz Warde; Mary Brigid Collins, Pavee Point Traveller Primary Health Care Project; and Minister for Children, Equality, Disability, Integration, and Youth, Roderic O'Gorman.
New mental health online information source for Travellers unveiled
The Pavee Point Traveller and Roma Centre have created a new mental health online information resource for young Travellers called Young Pavees – Mind Your Nuck in collaboration with the HSE. The aim of youngpavees.ie is to provide young Travellers and their carers (parents, grandparents etc.) with culturally appropriate information on the mental health services and supports available to them.
The website was developed by Pavee Point with support from young Travellers and the HSE Eastern Region Traveller Health Unit. Mental health advice and support covers common challenges faced by all young people, but particular issued experienced by Travellers such as; racism, discrimination, drug issues and unemployment. Youngpavees.ie also o ers information and contacts for Traveller parents to help them support their children.
Martina Queally, Chairperson of the HSE Eastern Region Traveller Health Unit (THU), and Chief O icer of HSE Community Healthcare East, said, “The website presents a clearly innovative solution to addressing Traveller mental health inequalities. It also will support implementation of key actions in the forthcoming National Traveller Health Action Plan.”

Pavee Point mentioned that users can explore content with their smartphone and the information is available in listening mode which addresses literacy issues and privacy issues.

Pavee Point's Mental Health Co-ordinator Patrick Reilly said the tragic deaths of young Travellers around the country in recent months have sent shockwaves through the community and Traveller parents are worried for their children’s mental health.
He welcomed the launch of this resource “that has been developed by Travellers for Travellers but will be hopefully used by HSE colleagues and services in supporting Travellers in accessing and using their services.”
Health education session for Traveller held in Balbriggan
A session was held recently to educate members of Traveller Primary Health Work Team in Balbriggan, Co Dublin, on the new Traveller specific Safety Wall Chart launched by the HSE. Education sessions were held for members of the Balbriggan Travellers Project and in Priorswood for members of Travact. Both sessions were very successful and plenty of new connections were made and plans made for further education on a variety of child and adult health topics.
Julie an inspiration to her community
Julie Duke McDonagh is Ireland’s first Traveller peer support worker appointed to the HSE mental health team in Cavan/ Monaghan. She is also the first Traveller person to uptake the peer mental health study at Dublin City University, sharing her own lived experiences of mental health challenges.
Julie said she left school at a very young age and never dreamed of returning to education. She said she really enjoyed being back in the classroom, making new friends and learning about mental health. Currently Julie works as part of the Cavan/ Monaghan mental health team supporting members of her own community as they access the mental health services with follow up one to one supports.
Ita Madden, regional coordinator, mental health services for Travellers, North East, explained “Traveller mental health is in crisis with Traveller women six times more likely to take their own life and Traveller men is even higher so having this post is a real benefit to tackling this problem.”

Ita said she was delighted to be part of this young lady's journey over the years and more recently mentoring her through DCU. She said there is a lot of stigma around mental health and we all need to be encouraged to talk openly as we all have good days and bad. Julie is the first of her family and extended family to attend university and such an inspiration for her community and other Travellers planning to return to education and be part of positive change in Traveller mental health into the future.

The meetings were arranged by Siobhan Ni Mhurchu, Child Health Programme Development O icer for Dublin North City and County, in conjunction with Eiméar Close, public health nurse, and Sinead Burke, Primary Health Care Project Co-Ordinator.
“There was plenty of discussion, debate and of course tea and biscuits! Many thanks to all the Primary Health Workers form both groups who participated and contributed during the sessions,” said Eiméar.

| 37 HEALTH MATTERS SPRING 2023
At the launch were Martina Queally: Chief O icer, HSE Community Healthcare East and Eastern Region Traveller Health Unit Chairperson; Winnie McDonagh: Traveller Primary Health Care Worker; Mary Butler, Minister of State for Mental Health & Older People; Patrick Reilly, Eastern Region Traveller Health Unit; and Linda Moore: Head of Service, Mental Health, HSE Community Healthcare East.
Julie Duke McDonagh with Ita Madden, Mental Health Service Coordinator for Travellers in CHO1 who supported Julie throughout her studies in Dublin City University.
Eiméar Close, public health nurse; Sinead Burke, Primary Health Care Project Co-Ordinator; Siobhan Ní Mhurchu and members of the Balbriggan Traveller Project
Record High
New record for ambulance calls in early 2023

Incoming calls to the National Emergency Operations Centre in the National Ambulance Service (NAS) reached a record high during a nine-day period in the first half of January. Over a two-week period from early January, there were nine days where NAS received more than 2,000 calls a day, which represents a new record.
For NAS staff and the entire healthcare system it was one of the busiest winter periods to date, both in our acute hospitals and across our primary and social care services.
Levels of infectious respiratory diseases in the population were at exceptional levels, a situation that was experienced by almost all health systems in Western Europe.
Between January and November last year, NAS demand increased by 15%.
In early January, Robert Morton, Director of NAS, and Dr Cathal O’Donnell, Clinical Director of NAS, jointly thanked staff, supervisors, managers and volunteers for their exceptional efforts.
In a letter they acknowledged that the service was experiencing “extreme and unprecedented pressures” which were being borne by patients who required their assistance and NAS staff, supervisors and managers who they said had stepped up to meet the challenges and worked hard to ensure the service was doing the best it could for patients.
A key part of the service’s contingency planning was the commitment and support of many volunteers across Ireland, such as those with Community First Responder teams supported by CFR Ireland, Critical Care Doctors supported by Irish Community Rapid Response and
other associated charities, voluntary organisations such as the Order of Malta Ambulance Corp, the Irish Red Cross or St John’s Ambulance Brigade or from organisations such as the Civil Defence, Local Authority Fire Services or the Irish Coast Guard.
“Each of these activities contributes enormously to our overall response to meet the needs of our patients. In this context we wanted to say a sincere thank you to all of our staff, supervisors and managers and in particular all of the many volunteers for everything you have done and are continuing to do for our patients,” the letter stated.
During the period of escalation NAS engaged private capacity and voluntary ambulance services to support hospital discharges. Community First Responder Schemes responded to elderly patients and did welfare checks on patients waiting for emergency ambulances. NAS also put in place Hospital Liaison Personnel to expedite turnarounds and coordinate care handovers.
At the beginning of December last year, NAS activated a new Tactical Management Unit operating 24/7 to support staff and proactively manage pressures and escalations within the service for this winter and beyond. The Tactical Management Team works under the direction of a Senior Tactical Manager 24/7 who works closely with acute hospital colleagues to reduce the impact of arrival to handover delays while supporting hospital turnarounds. The team continues to work in this capacity following the winter period. Tactical Managers work in collaboration with local area managers and hospital group management. The Defence Forces also supported NAS for a time during the peak winter pressures providing ambulances, paramedics and EMTs in Dublin, Cork and Kildare.
HEALTH MATTERS SPRING 2023 38 |
NAS recruitment campaign produces excellent results



The National Ambulance Service (NAS) ran a new advertising campaign to promote jobs in NAS and recruit student and qualified paramedics across the country. The campaign included two bursts of radio and social media advertising in August 2022 and January 2023.




During each burst, the ads were live on national and local radio for two weeks and on multiple social media platforms for three weeks. Potential candidates were directed to www.hse.ie/jobs where they could search for NAS jobs using the keyword ‘ambulance’. The ads were aimed at a young diverse audience and encouraged applications for the student

NEW LOOK FOR THE NATIONAL AMBULANCE SERVICE
Sta from the National Ambulance Service (NAS) began 2023 by showing o their smart new uniforms.

Designed specifically for the needs of NAS personnel, they are tailored to provide comfort and maximum e iciency for all who wear them.


The uniforms arrived after a 12-month project between a sta implementation group and the NAS suppliers.
NAS worked very closely with its suppliers at each stage of the process to ensure they arrived at a solution its members can be proud to wear.
The new uniforms were designed through
paramedic panel. Qualified paramedic roles are available on an ongoing basis but the campaign aimed to drive tra ic to these roles too.
There were two radio ads created for the campaign which highlighted that no matter your background, there is a place for you in the National Ambulance Service. One of these ads was also produced in Irish. A photoshoot was held in Dublin South Central Ambulance Station and NAS sta from di erent areas of the country took part to help the campaign. The photos taken were used to create engaging images and GIFs for Facebook,
a process of focus groups, design workshops and trials. The process recognised the vital role NAS staff play in our national front-line services.
The professional operational uniform will become easily recognisable and synonymous with the NAS, allowing our sta to create a cohesive professional image. Watch out for the new look as you spot NAS sta in your community.
The high-quality uniform range represents a new era for the NAS as it grows, changes and develops in the coming years.
Instagram, Snapchat and TikTok. The August 2022 phase produced excellent results with 420 eligible applications received for the student paramedic panel and 14 for the qualified paramedic roles. The January 2023 phase, at the time of writing, is performing well with high engagement on social media. The campaign would not have been possible without the involvement of NAS sta who gave their time to participate in the photoshoot; thank you to Alex Pocci, Anna Boisko, Nora Bodnar, Tomasz Fedorowicz and Vasile Lung for taking part. And thank you to all who supported the campaign.
| 39 HEALTH MATTERS SPRING 2023
IPS Waterford
Support service helps to get people with mental health difficulties back into employment
Employment is an important goal for many of the individuals supported by Waterford Mental Health Service. Employment has been shown to provide social connection, increased sense of identity, improved selfesteem and independence, as well as reduction in hospital admissions and negative symptoms.
The Waterford Individualised Placement and Support (IPS) Employment Specialist Service was launched in Waterford City in April 2019 to help people with mental health challenges to get into the workforce. It is a partnership between Waterford Mental Health Service and the National Learning Network (NLN).
Many identify work as a crucial component in their recovery however unemployment rates for individuals with mental health difficulties remain significantly higher than the general population.
There are many barriers, both individual and structural, that many with mental health difficulties face when obtaining and maintaining employment, including:
Low motivation
Low confidence
Side-effects of medication
• Fear of losing welfare benefits
• Employers’ attitudes
• Perceived stigma and discrimination
• Healthcare professionals’ low expectations
Individual Placement and Support (IPS) is an evidence-based model of supported employment which has been shown to be effective in supporting individuals with mental health difficulties into work.
This service is fully integrated into both Waterford City metal health teams and co-located within the Waterford Primary Care Centre. The Waterford IPS ES service has made strong links with a range of employers around Waterford City and has developed a close working relationship with the local DEASP.
Since its establishment in April 2019, the IPS ES has received approximately 150 referrals from across the two mental health teams which highlights the huge need for this service. The programme has gone from strength to strength, as reflected in the testimonials from clients, employers and colleagues.
Due to the success of the IPS service, funding has been secured to maintain and expand the service.
MICHELE'S STORY
Michele delighted to return to the workforce with support from IPS Service
Michele Power is just one of the many people who have found success with the IPS Service. After three years out of the workforce, she is now happily employed with the High Horse coffee shop in Waterford and said she would recommend the service to anyone.

“I am so pleased at how the entire process worked for me and amazed that with this support service I re-entered the workforce with such ease,” she said.
“I genuinely cannot recommend the service enough to anyone who like me has suffered with mental health issues and has worked through the recovery process but perhaps their confidence has taken a battering with being out of work or whatever other issues they have been through. If you feel you are ready to get back to working but know you need a helping hand like me and if you are motivated to find a job, embrace this service. I am still getting support from my Employment Specialist Jamie Power who touches base with me to make sure all is going well and reassures me that any issues at all to simply contact him and he will help in any way he can.”
She said she found out about the IPS Service when she was attending the Waterford Mental Health Services for Post Traumatic Stress Disorder.
HEALTH MATTERS SPRING 2023 40 |
“I was very aware that having been out of employment for three years due to my mental health, re-employment could be di icult, due to lack of confidence, and knew I needed help too with my CV,” said Michele.
“Being out of work while dealing with your issues can be very isolating. So when you feel ready to return to the work force it can be daunting. I didn’t hesitate when I was informed by my psychologist of the IPS service and that I could get support in finding a job.
“I was very excited about the possibility of re-entering the workforce and was very open to any suggestions or guidance by Jamie. After my first meeting, I was first of all put at ease that I would be supported throughout the whole process of getting a job.
“When a potential job came up to suit me, within a very short period of time having first met Jamie, I was guided in submitting my CV and arranging my first interview. Thankfully again with immense support from him, I got a month’s trial in my new employment, but the job suited me so well I was hired after two weeks.”

Michele is safe in the knowledge that the support of the IPS service will always be there for her.
“I hope to continue working in my current employment for the foreseeable. I can say that I am happy in my work, this was unexpected for me. I am very aware that should there be any change in my employment circumstances or if I needed to seek other employment, I will have the support now of the IPS service and I will have the confidence in myself to keep moving forward,” she said.
EMPLOYER'S STORY
It can be hard for employers to find sta that are a right fit for your business. Sean Byrne of High Horse co ee shop said it was one of the reasons why he was happy to support the IPS Employment Service.
“Overall it has been a very positive experience for me. I’m sure most businesses would agree that sta ing is a major issue. It is very hard to find trustworthy and hardworking sta . This is exactly what we gained in Michele and so much more to go with that,” said Sean.
“Jamie clearly did his homework to get the right fit for us and for his client. He was incredibly supportive to Michele, accompanied her to the first interview, the three of us had a chat and got to know each other which definitely made the process easier on myself and Michele.
“Michele has been a roaring success. Super motivated, great work ethic and has just been a breath of fresh air. You can see Michele’s personality coming out more and more by the day, so I think that the experience has definitely helped her and it has been amazing for us.”
He said he didn’t really have any previous knowledge of IPS before Jamie Power, an Employment Specialist with the service, approached him about taking on Michele.
“I would definitely recommend any business to collaborate with IPS. My experience has been nothing but positive, for me it benefits everybody. We have gained a trustworthy, hardworking and motivated employee which is so hard to find. For the client they are getting a fresh start and as an employer it feels good to know that you’re helping someone. I would definitely have no hesitation in working with the IPS programme again if I was looking for extra sta , it has just been an incredibly rewarding experience.”
Feedback from members of the multidisciplinary team at Waterford Mental Health Service
Neil, Clinical Nurse Manager
“For the client base I work with the impact of the Employment Specialist Service has been excellent. Unfortunately in my experience persons with long-standing mental health di iculties often face a level of discrimination in society when it comes to employment. Similarly they often lack the confidence and direction to seek employment and the service has definitely made a di erence here.”
Jennifer, Occupational Therapist
“The addition of Jamie to the team has had huge benefits for the clients I work with. Previously, if someone wanted or needed a job, it would fall under the realm of OT but I would never have had the time, resources or skills to do what Jamie does - making new contacts, linking in with employers, o ering ongoing support. Now I might do a small piece of work if someone is still unsure about returning to employment but then when the decision is made, I refer on to Jamie if they are interested in working.”
Frances, Psychologist
“I find that having an employment specialist within our team means that clients can meet with Jamie in surroundings that they are familiar with. They have someone that will help them bridge that gap towards employment, particularly if they haven’t worked for some time or if they’re lacking in confidence to approach employers on their own. There may be aspects of their mental health that they would like the employer to be aware of or they would like support to prepare a CV or to prepare for interview.”
Emily, Nursing
“The preparation and support given to clients by Jamie ensures an increase in their self-esteem and confidence in returning to work. It’s an additional resource that clients greatly benefit from and give them hope. It also helps to focus and support clients in the area of returning to work and a structured, relaxed manner.”
| 41 HEALTH MATTERS SPRING 2023
‘We have gained a trustworthy, hardworking and motivated employee which is so hard to find’
Poss s ible l Think
Celebrating partnership and involvement
DiversityHub


Hub
HSE launches First National Diversity, Equality and Inclusion Hub and Strategy
The HSE has launched a new Learning Hub to provide managers and sta with resources and information on Diversity, Equality and Inclusion (DEI) topics.
Available now on HSeLanD, the Hub will assist managers and sta with day-to-day topics that come up in the workplace relating to diversity, equality and inclusion, including the nine grounds outlined in the Employment Equality Acts 1998 – 2015 (age, civil status, disability, race, family status, gender, membership of the Traveller community, religion and sexual orientation) and how these protections impact on the workplace.

Providing advice and guidance on diversity, equality and inclusion enquiries is a key function of the HSE’s national DEI team. In 2022, many enquiries were received by the team in relation to a broad range of topics, in particular enquiries relating to support at work for sta with disabilities, such as assistive technology, software, workplace ergonomics, communication and literacy support. Other enquiries related to engaging with HSE sta networks, information on organisational policies and guidelines, guidance on inclusive terminology and language and recruitment and selection related enquiries.
“The number and range of enquiries continue to grow each year, highlighting the need for a Learning Hub. Having these resources to hand, all in the same place, will have a really positive impact in supporting sta e orts to create an inclusive and positive workplace culture in the HSE”, said Michele Guerin, HSE Equality O cer.
“The DEI team is available to o er support and information to sta and managers on DEI topics and contact with our team is always welcome.”
Commenting on the new Hub, Ray Leonard, Counsellor/Therapist HSE National Counselling Service and Co-Chair of Reach Out Network, the
HSE’s sta network for LGBTQIA+ sta and their alliessaid,“IfeelexcitedbywhatIseeintheDEIHub. It holds so much potential for supporting a vital elementof ourworkinglives,namelyapositiveHealth Service where we are encouraged to contribute to the delivery of the service from within the richness of humanity as it uniquely manifests through each one of us. It’s inspiring”
“IthinktheHubwillproveagamechangerinterms of shining a light into unexplored areas of bias and marginalisation and promoting cultural change throughout the HSE. The Hub will give a voice to highlyablesta who feel they have no voice. Iwould highly recommend it to sta and managers in the HSE”saidDrPatriciaWalsh,ConsultantPsychiatrist and Multi-Disciplinary Team Lead.
TheHubsupportstheHSE’sfirstnationalDiversity, EqualityandInclusion-Sta site (hse.ie), which was launched in January this year. Developed to help implementtheHSE’sPeopleStrategy2019-2024,this strategy sets out the main priorities and actions to enhancediversity,equalityandinclusionintheHSE.


Before the Hub was launched, an internal accessibilityauditwascarriedoutonthefunctionality of theplatformbymembersof theHSE’sDigitalTeam.
“TheHubcontainsinformationandresourceswhich arerelevantforallsta in the HSE, regardless of grade, position or geography,” said Maria Barry, Diversity Equality and Inclusion Manager. “Topics relating to diversity, equality and inclusion are constantly evolvingsoweencourageallsta to regularly dip in and out of the Hub. The Hub will be updated on an ongoingbasisasnewinformationbecomesavailable”
TheDEIHubcanbefoundhere:https://www.hseland. ie . Go to Hubs & Resources > Diversity, Equality and InclusionHub
If you have any feedback on the Hub or would like share any resources for inclusion on the Hub, please contactdiversity.hr@hse.ie
The Equality and Inclusion Committee in the Health Sciences Academy, which includes representation from University of Limerick Hospitals Group, Mid West Community Healthcare, and University of Limerick, ran an inaugural conference for all healthcare and academic sta . This was a multidisciplinary event which promoted inter-professional collaboration and learning across all disciplines.
Key speakers addressed the importance of partnership and involvement and encouraged delegates to embrace the opportunities and benefits that sta diversity can bring to the workplace. Health and education colleagues presented local initiatives demonstrating how diversity and inclusion are incorporated into the health and school environments.
The hosting of this inaugural conference provided valuable insights into diversity, equality and inclusion in the workplace. The conference was evaluated very positively, and created an interest and awareness amongst delegates about the importance of embracing and celebrating diversity.
• 12% of people living in Ireland are from a migrant background 49% of nursing and midwifery registrants (2022) are internationally trained
• The importance for all of us to be aware of our unconscious biases
• The need to engage with di erence.
• Intercultural competencies should be promoted within the workplace
HEALTH MATTERS SPRING 2023 42 |
End of Life Survey
End of Life survey will help us learn from people’s experiences


The National End of Life Survey, the first national survey asking bereaved relatives about the care provided to a family member or friend in the last months and days of their life, is taking place this year.
The purpose of the survey is to learn from people’s experiences of end of life care in order to improve the services provided both to people who are dying, and to their families and those close to them.
Individuals who registered the death of a family member or friend that occurred between September 1st and December 31st 2022 will be invited to participate. They will receive an invitation letter asking them to take part and a survey questionnaire in the post between March and May 2023. People who died suddenly or through an accident will not be included in this survey. Participation in the survey is voluntary and it takes approximately 30 minutes to complete.
A project team from the HSE’s Operational Performance and Integration division, led by Aileen Killeen, are working on the survey with the Health Information and Quality Authority (HIQA), the Department of Health and a range of HSE service areas including sta from acute hospitals, community operations and palliative care.
HSE National Director of Operational

Performance and Integration Joe Ryan said, “This is an important survey which will allow us to learn from people’s experiences of end of life care in order to improve the services provided both to people in the last days of their lives, and to their families and those close to them.
“Their feedback will provide us with valuable information on the standard of healthcare services in Ireland and help to identify areas for improvement.The results will be used to guide and drive service improvement actions aimed at continuously improving the services provided both to people at the end of their life, and those important to them and will be published on www.yourexperience.ie.”
The care settings include acute hospitals, nursing homes, hospices,
Bereavement support
The death of someone close can be the greatest loss we will experience in our lives. Many people find their own way through bereavement with support from friends and family, however support is also available from the following organisations.
Irish Hospice Foundation

The HSE, in partnership with the Irish Hospice Foundation, provides a helpline to support people who have experienced the death of a family member or friend. You can call this Freephone service on 1800 80 70 77 to talk to a bereavement support volunteer. The Freephone service is available from 10am to 1pm, Monday to Friday. You can also access support through the website www.bereaved.ie
Samaritans
Samaritans provide emotional support for anyone who is struggling to cope or needs someone to listen to them without judgement or pressure. You can contact Samaritans 24 hours a day, 7 days a week on Freephone 116 123 or by emailing jo@samaritans.ie For more information, please visit www.samaritans.ie
Information and support
Patient Advocacy Service
If you have been impacted by any issues with regard to end-of-life care and would like information or support, or if you would like to provide feedback on the care provided to your loved ones, you can do so by contacting the Patient Advocacy Service on 0818 293 003 or at info@patientadvocacyservice.ie For more information, please visit patientadvocacyservice.ie
@CareExperience
community hospitals, private hospitals and family homes.
Healthcare sta will be asked to have a look at feedback from bereaved people replying to this survey which will inform us what we are doing well and what can be improved to enhance care at end of life.
Sta are being asked to ensure that no other surveys of bereaved people are undertaken relating to care of people who died between September 1st and December 31st 2022. Survey findings for all of the surveys run by the National Care Experience Programme are published on yourexperience.ie and shared with service providers, policy makers and the public.
The HSE and healthcare services then respond to the survey results by developing quality improvement initiatives.
The survey is being run by the National Care Experience Programme, a joint initiative from HIQA, the HSE and the Department of Health. People are asked about their experiences of care in a range of surveys in order to improve the quality of health and social care services in Ireland.
Youwillfindmoreinformationonyourexperience.ie

| 43 HEALTH MATTERS SPRING 2023
Joe Ryan
HSE Sexual Wellbeing is back on Campus
The Sexual Wellbeing live event roadshow has made a return to third level campuses around the country this 22/23 academic year.
The Sexual Wellbeing campaign is run by the HSE Sexual Health and Crisis Pregnancy Programme (SHCPP). It is primarily aimed at 18 to 30 year olds in Ireland with the aim to provide information to improve sexual health and wellbeing and to prevent unplanned pregnancies and sexually transmitted infections. The campaign includes the website sexualwellbeing.ie which hosts important information and materials; as well as a number of out of home initiatives on the ground, including live events on campuses.
The first of these live events took place in third level campuses in September 2022, visiting University of Galway, UCC, UCD and UL during Freshers’ weeks.
More recently, in February 2023, this roadshow continued across seven third level campuses as part of their Sexual Health and Guidance (SHAG) weeks. Campuses visited included SETU (Carlow), TU Athlone, TUS Moylish (Limerick), MTU Cork, ATU Sligo, TU Dublin and IADT.
These events form part of the wider Sexual Wellbeing media plan, to help promote sexual health information and prevention messages directly to third level students.
To date, these events have resulted in:
• Distribution of condoms and lube to a key audience
• Generated awareness and discussions
relating to sexual health and wellbeing, in particular focussing on new services such as free home STI testing and free contraception for 17 to 26 year olds.
• Promoted the availability of information and advice on sexualwellbeing.ie
The roadshow consists of a high-visibility, interactive event site that is set up at each third level campus. A spin the wheel quiz helped effectively engage with students, taking an educational and youth-focused approach. There has been a warm welcome of Sexual Wellbeing’s return to campus, with thousands of students engaged in learning more about their sexual health.
To help bring the conversations from these events to an even broader audience, SHCPP in partnership with two universities, developed a youth focussed video series for social media. These were promoted primarily on TikTok and Instagram Reels.
Presented by Welfare Officers at University of Galway (Imogen O’Flaherty Falconer) and MTU Cork (Kelda McManus), these two series cover information about free home STI testing, free prescription and emergency contraception, how to access free condoms and the My Options service.

The first of these series, which focuses on STI free home tests, has already proven popular with the audience, with series one achieving over 1.8 million views on TikTok alone.

You can view these series on Sexual Wellbeing’s social media platforms:
Instagram: @hserespectprotect TikTok: @Sexualwellbeing.ie Facebook: @hserespectprotect The live events and social media series were delivered in partnership with Headcase Marketing.
For more information about the live events or wider campaign please contact Muireann Kirby, Campaign Manager for sexual health campaigns at muireann. kirby@hse.ie.
For information about the work of the Sexual Health and Crisis Pregnancy Programme contact Anita Ghafoor-Butt SHCPP Communications Manager at anita.butt@hse.ie
HEALTH MATTERS SPRING 2023 44 |
Above: A student attending the Sexual Wellbeing roadshow. Right: The Sexual Health team at the roadshow.
Your Opinion Counts
Actions in response to the 2021 Sta Survey
APPOINTMENT OF HSE DATA PROTECTION OFFICER (DPO)
M ary Deasy has been appointed HSE Data Protection O cer (DPO). Coming from a clinical background, Mary has extensive qualification and experience in the areas of Risk Management, Quality and Patient Safety and Data Protection.
Thank you to everyone who took the time to complete the Your Opinion Counts - 2021 Sta Survey. Since the first Sta Survey in 2014, there has been immense change in our health service, particularly over the last three years, due to the pandemic and the cyberattack. Survey results identify opportunities for improvement which help us build a better health service for all. From encouraging feedback, valuing sta and listening to them, significant action has been undertaken across the HSE. Some of these actions are highlighted in the infographic below. The next Sta Survey is taking place in May 2023. Don't miss your opportunity to answer the survey this time around. Watch out for information in the coming weeks on how to take part.
YOUR OPINION COUNTS
Actions in response to the 2021 Staff Survey
JOB & ROLE
Staff recognition awards, staff appreciation days, retirement and long serving staff recognized Roll out of the Values in Action programme and other staff engagement processes
RELATIONSHIP WITH LINE MANAGERS
Regular team meetings being promoted and scheduled to discuss team and individual objectives
Continued focus on the Performance Achievement process
RELATIONSHIP WITH SENIOR MANAGERS
Face-to-face town hall style/roadshow meetings continue with Senior Managers providing strategic organisational updates Information sessions about the new Regional Health Areas Exit interviews
Quarterly Staff Newsletters
HEALTH AND WELLBEING
Scheduled health and wellbeing events such as exercise classes, yoga and meditation
Remote, flexible, and blended approaches to work Employee Assistance Programme and Occupational Health information actively shared through internal communications, staff apps and WhatsApp
TRAINING AND DEVELOPMENT
New guide on Developing Organsiational Culture
Provision of new training resources
New programmes on HSeLanD
Mentoring and shadowing opportunities
Sponsoring formal academic programmes, interview skills training and job rotation opportunities
DIGNITY AT WORK
New policy launched
New mandatory training programme on HSeLanD
New Support Contact Persons and Nominated Persons training provided New empathy initiatives HR clinics continue to be rolled out across many services
DISCRIMINATION IN THE WORKPLACE
New Diversity, Equality and Inclusion strategy launched
Unconscious Bias and People Management- the Legal Framework training available across services, new suite of diversity e-learning courses available
Diversity, Equality and Inclusion enhanced with new staff networks, communications and awareness-raising across the HSE HR policies enhanced by new equality-proofing process
Mary has spent the last four years working in the role of Deputy Data Protection O cer as part of her role as Regional Manager for Consumer A airs in HSE South and has completed an Advanced Diploma in Data Protection Law at Kings Inns. The HSE’s National Data Protection O ce can be contacted at dpo@hse.ie
Contact details for Deputy Data Protection O icers
Deputy Data Protection O cer West, (excluding voluntary agencies)
• CHO 1 – Cavan, Donegal, Leitrim, Monaghan, Sligo
• Community Healthcare West –Galway, Mayo, Roscommon
• Mid-West Community Healthcare –Clare, Limerick, NorthTipperary
• Saolta Hospital Group
Phone: 091 775 373 | ddpo.west@hse.ie
Deputy Data Protection O cer Dublin North-East (excluding voluntary hospitals and agencies)
• Midlands, Louth, Meath Community Health Organisation
• Community Health Organisation Dublin North City & County
• CHO 6 –Dublin South East, Dublin South & Wicklow
• RCSI Hospital Group
• National Children’s Hospital Kells O ce: 046 9251265 Cavan O ce: 049 4377343 | ddpo.dne@hse.ie
Deputy Data Protection O cer Dublin mid-Leinster (excluding voluntary hospitals and agencies)
• Dublin Midlands Hospital Group
• Ireland East Hospital Group
• Community Healthcare Dublin South, Kildare & West
• Wicklow
Tullamore O ce: 057 935 7876
Naas O ce: 045 920 105 | ddpo.dml@hse.ie
Deputy Data Protection O cer South (excluding voluntary hospitals and agencies)
• Cork & Kerry Community Healthcare
• CHO 5 –Carlow, Kilkenny, South Tipperary, Waterford & Wexford
• UL Hospital Group
• South South-West Hospital Group
Cork O ce: 021 492 8538
Kilkenny O ce: 056 778 5598
ddpo.south@hse.ie
HEALTH MATTERS SPRING 2023 | 45
Injecting facility
Medically supervised injecting facility granted for Dublin
The go-ahead has been given for the development of a Medically Supervised Injecting Facility (MSIF) for a pilot period of 18 months commencing from first opening of the service. An Bord Pleanala granted permission in December 2022.
A MSIF is a safe healthcare environment where people can inject drugs, obtained elsewhere, under the supervision of trained health professionals. They o er a compassionate, personcentred service, respecting an individual’s dignity and basic human rights, which reduces the harms associated with injecting drug use and can help people access appropriate services. These services can help health service sta to reach and support vulnerable and marginalised people who often do not, cannot or no longer engage with existing health services.
Typically, supervised injecting facilities provide people who use drugs with sterile injecting equipment; counselling services before and after drug consumption; emergency response in the event of overdose; and primary medical care. The supervised injecting facility aims to:
• reduce drug-related overdose deaths
• reduce the risks of disease transmission through shared needles
• reduce public health risks such as needle-stick injuries due to drug related litter and connect the most vulnerable and marginalised people who use drugs with treatment services and other health and social services.
This facility will be based at Merchants Quay Ireland’s Riverbank Facility in Dublin 8 selected following a tender review process. The facility will provide a sterile, safe, medically supervised service for people who inject drugs together with a space where people can receive support from relevant health services and support groups to help improve their health and social circumstances. The facility will have an assessment/ waiting area, seven injecting booths, along with an aftercare area and a one-to-one space will be integrated with the other services currently provided by Merchants Quay Ireland. The facility can potentially operate three sessions per day, Monday to Friday, and two sessions on Saturdays and Sundays. It's envisaged by Merchants Quay Ireland that about 60 to 100 people would use the injection facility per day, with the busiest times expected in mornings and evenings. There are now approximately 90 of these facilities worldwide, in Europe, Canada, and Australia. There is significant evidence gathered from these facilities of their benefits to people who use drugs and the wider society.
Once this service commences, there will be an 18-month pilot period for it to operate and this phase will be subject to evaluation. A monitoring committee will be established and chaired by the HSE and will include members from the Department of Health, An Garda Síochána , Dublin City Council, The Union for Improved Services, Communication and Education (UISCE) and other relevant stakeholders.
Further news will be added to Drugs.ie to report on the development of this service.

NEW NALOXONE EDUCATION RESOURCES LAUNCHED

Naloxone Training Available Today
The HSE National Social Inclusion O ice has developed new naloxone resources explaining how to use this life-saving medication. In Ireland, opioids are the main drug group involved in drug overdose deaths. Naloxone temporarily reverses the e ects of an overdose caused by heroin and other opiates or opioid, such as methadone or morphine, giving emergency services time to help. The World Health Organization recommends that people likely to witness an opioid overdose e.g. close friends, a partner or family member, and sta or volunteers working with people who use drugs, should have access to naloxone and be trained to administer it.
The HSE established a Naloxone Training Programme for service providers following a successful pilot project in 2015. This training programme has been developed in order to maintain the focus on reducing drug-related deaths and non-fatal overdoses. During 2020 and 2021 there was a significant increase in naloxone provided by Addiction Services as they were advised to prescribe naloxone to all those who commenced on OST during the COVID-19 pandemic as a harm reduction measure. Training in overdose awareness and the administration of both intranasal and intramuscular naloxone is organised by the National Social Inclusion O ice and was a priority in 2022, with 369 sta , service participants/peers and family members people trained last year.
The first report analysing the expanded naloxone programme was published in 2022 and found that between 2018-2020, the supply of naloxone units by the National Social Inclusion O ice increased by 149%. The report showed that 569 people were administered naloxone in the period 2018-2020, with 62% of those who received it having overdosed by injecting drugs, and just over half having taken more than one drug. The report estimated that at least 22 people's lives were saved over the three-year period due to the administration of naxolone.
The National Social Inclusion O ice has developed new training resources, including new demonstration videos with step-by-step information on how to respond to an opioid overdose and administer naloxone for sta , people who use our services and their families, are available at https www.drugs.ie/resources/naloxone/. To book your naloxone training email jennifer.smyth2@hse.ie
HEALTH MATTERS SPRING 2023 46 |
Cervical screening lab
New laboratory at The Coombe now on journey to global excellence

The National Cervical Screening Laboratory at The Coombe Hospital processed its first samples for the CervicalCheck programme in December 2022. This significant step marked the end of the journey to build and equip the laboratory, and the beginning of the journey to establish it as not only the primary processor of the programme’s samples but also as a global centre of excellence.
The Coombe Hospital was identified as having the expertise and governance in place to run the service for CervicalCheck. The decision was therefore taken - in conjunction with the Board of The Coombe Hospital, the National Screening Service, which operates CervicalCheck, and the HSE - to redevelop the existing Coombe laboratory into a new purpose-built facility on the grounds of the Coombe hospital site. The redevelopment was funded by the Department of Health.
Dr Cillian De Gascun, Interim Director of the NCSL, believes the laboratory is unique as it is dedicated to cervical screening, housing all the elements of the screening test process under one roof.
“It’s a very exciting time and a very exciting opportunity. This laboratory is certainly the first of its kind in Ireland and probably in Europe, to be dedicated to cervical screening,” he said.
Samples coming into the lab are tested initially for the presence of high-risk HPV, if no HPV is found the result is returned to CervicalCheck which sends the result letter to the woman. If HPV is found the same sample is used to make a slide which is then looked at for abnormal cell changes by two medical scientists, specialising in cytology, under a microscope. If there are any potential differences in the opinions of the medical scientists, the sample is passed to a consultant cytopathologist who will examine the sample. The outcome of this determines whether CervicalCheck recalls the woman for further investigation in colposcopy or for another
screening test in 12 months’ time.
Each stage of the testing process – from the sample arriving at the specimen reception to being examined by cytology and the result reported - will happen in NCSL. While the plan is that the laboratory will become the main processor of CervicalCheck samples, reaching that point will take time. The ongoing recruitment of dedicated NCSL staff including medical scientists, consultant pathologist and key support staff such as IT and admin, is a high priority.
Dr Aoife Doyle, Lead Pathologist, said, “This is an exciting work opportunity for any specialist who wants to come to Ireland, this is a unique opportunity in a purpose-built lab encompassing the screening arm with HPV testing and cytology, as well as the smaller diagnostic arm with histopathology. It’s a lab that’s very much wanted by the Irish public and by scientists in Ireland, but it’s not about doing it quickly, it’s about doing it correctly.”
Dr De Gascun added, “It’s key that we don’t get caught up in the misnomer that this laboratory will be better than the US-based laboratories that currently process the bulk of our cervical screening tests. We all work to the same set of CervicalCheck quality assurance standards, so from a quality perspective, women in Ireland can be assured that the quality of service they are receiving from laboratory in the US is equivalent to the service they receive here.
“That being said, I am very strongly of the opinion that we should be self-sufficient at NCSL, that eventually we should have capacity to deliver the service. We will always need a contingency, because obviously we saw what happened with the two cyberattacks that affected The Coombe Hospital last year.
“Seeing the first samples being processed in December since the cyberattacks was a real milestone - it’s great to see the staff here getting back to doing what they enjoy doing.”
| 47 HEALTH MATTERS SPRING2023
Dr Cillian De Gascun, Interim Director of the National Cervical Screening Laboratory (NCSL) at The Coombe Hospital and Dr Aoife Doyle, Lead Pathologist, NCSL.
Alcohol during pregnancy
HSE develops new videos to highlight risks of drinking alcohol during pregnancy
The HSE is encouraging pregnant women, and women planning a pregnancy, to have an alcohol-free pregnancy. Even a small amount of alcohol at any stage of pregnancy can harm a baby’s development and may have lifelong effects such as Fetal Alcohol Spectrum Disorder (FASD).
FASD is a group of disorders caused by prenatal alcohol exposure and are associated with a range of lifelong physical, mental, educational, social, and behavioural difficulties. FASD is often an invisible disability, yet prenatal alcohol exposure is the leading preventable cause of neurodevelopmental disorder.
Often when people think of FASD they have an mental image of visual facial disfigurement but only a small proportion of children with FASD have visible facial features (facial dysmorphia); the majority of children with FASD have no visible signs of disability at birth, and difficulties may not manifest until preschool or school age.
The HSE has undertaken a number of communication campaigns to promote the advice that ‘No amount of alcohol at any stage of pregnancy is safe for your baby’.
Prof Maeve Eogan, Consultant Obstetrician and Gynaecologist, HSE, said, “It is important that we support people to have alcohol free pregnancies. Alcohol passes from the mother's blood into the baby's blood through the placenta and even a small amount of alcohol can harm a baby’s development and may have lifelong effects.”
VIDEO'S CAN BE FOUND HERE: https://www. youtube.com/ watch?v=ENAiB8LW58&list=PLltga nnkj2UElt7aqHxWuir mnElJ8wU9t
Dr Mary O’Mahony, Consultant in Public Health Medicine and the HSE’s Clinical Lead for FASD Prevention, said, “FASD can cause learning difficulties and behavioural issues for your child. Your child may struggle getting along with other people and have emotional and mental health problems. They may also be smaller than expected and have problems with eating and sleeping.”
Research conducted by the HSE to inform its ‘Ask About Alcohol’ communications campaign found that women do not always receive clear and consistent information on the importance of avoiding alcohol during pregnancy.
With clear information, many pregnant women will abstain from alcohol for the duration or the remainder of pregnancy.
She added that consistency is key. Women may have many caregivers during pregnancy and they should get the same information and advice about alcohol from every caregiver they meet during pregnancy.
As part of this ongoing campaign and to encourage consistency in messaging, HSE Health and Wellbeing have developed some new videos to inform and support staff in delivering this key message.
These videos are for healthcare workers, GPs, social care workers, midwives and obstetricians. The videos provide examples of brief interventions for healthcare professionals dealing with different scenarios that may arise throughout their patient’s antenatal appointments.
These videos can be used as a guide to open a conversation and discuss alcohol and pregnancy. They include interventions from a GP, social worker, midwife, and obstetrician.
Some women will need additional support to abstain from alcohol during pregnancy. Effective interventions include screening and brief intervention (SBI) for alcohol use by healthcare professionals, through implementation of the HSE’s MECC (Making Every Contact Count) and SAOR (Support, Ask and Assess, Offer Assistance, Refer) initiatives.
HEALTH MATTERS SPRING 2023 48 |
Health Service Leadership Academy graduates


are honoured

























The Health Service Leadership Academy was delighted to be able to hold graduation ceremonies for its Leading Care I, Leading Care II and Leading Care III programmes in November and December 2022 and January 2023.






The graduation ceremonies were a long time coming for the participants as they had been postponed due to the COVID-19 pandemic. Indeed, graduates from many of the cohorts had to overcome particular challenges to graduate, as they had the highly unusual experience of having their programmes interrupted and temporarily suspended due to COVID-19.
Four graduation ceremonies took place with over 315 graduates graduating with either an MSc in Leadership in Management, Postgraduate Diploma in Leadership in Healthcare, a Postgraduate



Certificate in Management, a Professional Diploma in Management, a Professional Diploma in Management in Healthcare or an IMI Graduate Award in Executive Healthcare Leadership. Sadly two awards were made posthumously, to the late Rosaleen (Roz) Cashman and Patricia O’Connell.


The ceremonies were held in the IMI in Sandyford and were very enjoyable occasions where graduates were joined by family members and guests to mark the special occasion for them. Stephen Mulvany, Interim CEO, and Anne Marie Hoey, National Director of HR, both addressed graduates and those attending the ceremonies. They conveyed how proud the HSE is of those graduating and of what graduates have achieved in completing these very challenging programmes.

| 49 HEALTH MATTERS SPRING 2023
W
Dementia
Aproject focused on the needs of people with dementia is improving the patient experience at Nenagh Hospital. Patients are invited to take a simulated train journey through the interactive RemPods platform, which has been in use in care homes and hospitals in the UK for a number of years.
An LCD screen displays footage of rolling countryside, pulls through tunnels and into stations along the journey, facilitating reminiscence to reduce anxiety and stimulate positive memories in older patients with cognitive impairment.

Vimal John Mathai, Clinical Nurse Specialist in the Integrated Care Programme for Older Persons in Thurles, said this quality improvement project for Nenagh met a need where acute hospital environments were not as well set up for persons with dementia as care homes.
Vimal has a specialist interest in dementia and has led out on the RemPods/ Reminscence Therapy project in Nenagh.
“A quarter of all patients admitted to Nenagh Hospital have dementia. I have worked in Nenagh myself and all the team there are focused on what we can do to improve things for this older group of patients. It’s fair to say that the clinical environment in an acute hospital is not as dementia-friendly as in a nursing home, for example,” he said.
“Admission to an acute hospital can be confusing and frightening for a person with dementia. Even though they need to be in hospital, the stay might also have a negative impact on their physical, mental and cognitive abilities. How acute hospitals are designed very often doesn’t meet the needs of people with dementia. Signage can be confusing; lighting can be poor; the environment can be cluttered with inadequate space for visiting.”
The train project in Nenagh, which has now opened on Medical Ward 1, focuses in particular on the different care needs of people with dementia. The initiative has been supported by management and ward staff, including ward manager Elaine O’Sullivan.
Patients will board the train while having a meal, while welcoming a visitor for hospital or while waiting to be transferred or discharged. Feedback has been very positive from patients, families and staff to date, Vimal explained.
Through the RemPods platform, patients are encouraged to share their life experiences, memories and stories from the past. This is known as reminiscence therapy.
“Typically, a person with dementia is more able to recall things from many years ago than recent memories, so reminiscence draws on this strength. In many cases, recent memories deteriorate first for people with Alzheimer's and other forms of dementia. By sharing memories from the past through reminiscence therapy, people with dementia can develop more positive feelings while reducing stress and agitation,” he said.
“Reminiscence therapy encourages discussion of memories that have been stored away. It helps stimulate those memories through sensory organs. This causes the brain to react differently than usual. Those reactions can impact emotions or behaviour. Studies have shown that reminiscence therapy can help older adults become more engaged.”
Commenting on the new project, Prof Michael Watts, Consultant Physician, UL Hospitals Group, said, “This is yet another example of Nenagh Hospital adapting to the challenges of providing care for the patients of UL Hospitals Group. Congratulations to Elaine, the staff on Medical 1 and to Vimal for all of their work.”
HEALTH MATTERS SPRING 2023 50 |
Nenagh hospital train project aims to make care environment more dementia-friendly
Pictured on a simulated train journey on Medical Ward 1 in Nenagh Hospital were Siobhan Toomey, CNS Patient Flow, Nenagh Hospital; Vimal Mathai, CNS ICPOP Thurles; Celia Dwan, ADON Nenagh Hospital; and Elaine O’Sullivan, CNM2 Medical Ward 1, Nenagh Hospital. This quality improvement project for people uses reminiscence therapy to improve the experience of patients with dementia in Nenagh.
Roscommon Sacred Heart Hospital (SHHR) is a service provider for older people located in Roscommon town. The aim of the service is to provide high standards of care and to enhance the quality of life of residents in line with HSE policies and HIQA.
SHHR recently introduced the Tovertafel Table, also known as Magic Table, to enhance the awareness of Dementia and Alzheimer’s for staff, residents and family members.

The Magic Table is an interactive user-friendly technology which consists of a portable unit mounted to the ceiling and projects infrared sensors, speakers onto the surface below such as a table or desk top surface. There are different levels of interactive games for the users to enhance social, physical, sensory and cognitive functioning.
The games that have been developed respond to hand and arm movements with light animations projected by Tovertafel. Any cognitive dysfunction can reduce or limit the individual’s interactions with other people and family members. The loss of common human communication can be stressful to individuals. Being present with other people i.e. taking part in activities, having a bit of fun and laughter is essential for all of our lives.
Residents at SHRR enjoyed the training sessions with staff and everyone has been able to actively participate. The different levels of activities are suitable for residents with variable cognitive abilities. The Activity staff were delighted with this new interactive equipment and the feedback so far has been brilliant. Everyone seems to be fighting for a chance to be engaged with the competitive games with the hope being that the enthusiasm will bring about a great sense of wellbeing for the residents’ lives.
Isaac Bontha, Senior Physiotherapist, SHHR, said, “During the activities, staff also noticed enhanced social interactions and it is great for group and individual focused activities. It was a moment of togetherness to have fun, communicate and laugh - happiness was the feeling around the magic table. It is also enjoyable to be part of a group rather than being isolated and unable to communicate. The user can often make choices to decide which games or activities they would like to play and there is a shuffle option to mix the games to make it more interesting.”
DEMENTIA: UNDERSTAND TOGETHER LAUNCHES NEW DEMENTIA INCLUSIVE COMMUNITY SYMBOL
In consultation with people with dementia, carers, community champions and national partners, the Dementia: Understand Together campaign will be launching a community symbol nationally this March. The campaign is encouraging organisations and services in communities to display the symbol to help raise awareness of dementia and show their solidarity with the 64,000 people living with the condition in Ireland. Some 40 partners, ranging from voluntary and community groups, health services and academia to retail, transport and financial services, are backing the campaign and taking action to help support people with dementia and their families and friends.
As well as displaying and using the symbol on shop fronts, windows, websites, newsletters and on social media, partners and champions are encouraged to take part in free dementia awareness training. Staff and volunteers will explore how simple actions can make a real difference to making their services and businesses more accessible, not just to people living with dementia, but to everybody living in our diverse communities. By understanding together, we can all make a difference and help people in our communities to stay connected and included. If you’d like to join the campaign, you can find out more and check training opportunities at understandtogether.ie
| 51 HEALTH MATTERS SPRING2023
Sacred Heart Hospital launches the ‘Magic Table’ to promote awareness of dementia and Alzheimer’s
Residents and staff from Roscommon Sacred Heart Hospital enjoying the Magic Table.
‘Not just there to tick a box’
National Screening Service seeks new members for its Patient and Public Partnership network
For Keith Cairns and Will Kennedy, joining the National Screening Service’s Patient and Public Partnership (PPP) was an opportunity to give back and shape a service they had personal experience of.
In the months since joining, they have found the experience rewarding and feel their input has been heard and has made a real impact. As the PPP becomes more embedded into the NSS, the team is seeking more recruits to the panel. Here, we look at what the PPP is, its work, who can become a PPP representative, and how to find out more.
At the National Screening Service we want to ensure that our services meet the needs of the people using them and are truly person-centred. We have four population-based screening programmes: BreastCheck, BowelScreen, CervicalCheck and Diabetic RetinaScreen. We work in partnership with participants of each programme in a variety of ways through our Patient and Public Partnership.
What is our Patient and Public Partnership network?
We established our PPP network in 2019 and it has 33 PPP representatives from across Ireland. They provide the patient voice on NSS projects, working groups and committees through different levels of involvement including consultation and partnership in decision-making.
To achieve the best result from this work, we know the importance of a diverse and inclusive PPP network that represents the people who live in Ireland.
Who is invited to join the Patient and Public Partnership network?
» We are building a PPP network made up of people from different backgrounds, with different perspectives, experiences and interests.
» To do this, we’re seeking people who have an interest or knowledge of at least one of the four population screening programmes and who do not already formally represent any organisation or group.
» A clinical background is not needed, as participants are ‘experts by experience’. Any additional training and supports will be given, as required.
» PPP representatives should be 18 years or older
What does joining the Patient and Public Partnership network involve? Representatives participate in many different ways. You can:
• Assist in the design, delivery, and evaluation of NSS services
• Share your views and expertise and participate in NSS discussions and project work virtually or face-to-face
• Support the NSS as we seek to put patients and the public at the heart of our decision making
In recent years, our PPP representatives have worked on a variety of projects including: NSS Corporate Strategy development, Cervical Cancer Elimination Project, Strategic Equity Framework development, the Expert Reference Group and Interval Cancer Groups. Their expertise, developed through experience, has been invaluable and we are grateful to all who have given their time and voice to these projects.
In 2023, there will be many more opportunities for our PPP representatives as we continue to make sure their voice is central to our projects, groups and activities.
What specific skills or experience do I need to join?
• Some experience of screening services either as a patient, carer, relative or member of the public is desirable
• Ability to provide critical and constructive feedback
• Good communication skills
• The confidence to voice your own opinions clearly and take part in group discussion
The ability to listen and respect differing opinions
An awareness of equality and diversity – maybe these issues have affected you?
A positive attitude
How to get involved?
If you would like more information on our Patient and Public Partnership (PPP) network or on how to get involved, please email: ppplead@screeningservice.ie
To learn more about the work completed by PPP please see here (https://www.screeningservice.ie/publications/PPP-StrategyProgress-Report-2019-23-Final-V-1.6.22.pdf
HEALTH MATTERS SPRING 2023 52 |
KEITH’S STORY
For Keith Cairns, from Terenure in Dublin, it was a good experience with BowelScreen that motivated him to become a PPP rep.
Keith, a 73-year-old former bank manager, had taken up his invite for BowelScreen when invited, on his last screen with the programme the result showed a level of blood in his stool and he was asked to come back for further investigations.

“They investigated and I thought it was a really satisfactory process, I came away reassured about my health and the whole process. I saw the HSE getting a lot of stick about everything in the media and emailed the programme to say I had a good experience with the HSE and it wasn’t all bad.
“They thanked me and asked if I’d be interested in being in a campaign promoting BowelScreen. I have no medical skills, no medical background, just my own experience of the process. I got something for nothing and I wanted to give something back so agreed. That led to me joining the PPP.
“I’ve been able to help people like me by bringing a plain man’s thoughts to something that’s very technical. So, when I read the language in a poster, flier or brochure and it comes across a bit jargony or over technical I’d say when I think they should say it another way so people understand it better.
“You have to be prepared to give up a bit of time and if I ever felt I’d wasted my time I’d be the first off the bus, but there is great enthusiasm and the NSS are genuine about making the service better. The other PPP people are great and represent a great cross section of society.
“It’s a completely different experience to anything I’ve done before. I’d sum it up as dealing with committed staff helping to bring the common person’s thoughts to the programme. It gives you a hand in making it what it is. It’s a great service, that’s free, and if you can make it better then why not?”
‘All of us are listened to…’
WILL’S STORY
Will Kennedy, aged 65, from Glen in Cork City has been a PPP Rep for about a year. Will was working on the National LGBT Helpline when he was asked if he would be interested in representing the LGBT community on the PPP.
Will’s initial reason for joining was to promote equity and diversity in NSS communications. However, Will found he had another connection to the work of the NSS. He had been diagnosed with Burkitt’s lymphoma via a health check he receives as an HIV patient every six months. His cancer was detected at an early stage when it was treatable through intensive chemotherapy. While the treatment was arduous, it saved his life and Will puts this down to the preventative health screening checks he is offered as an HIV patient. For him the parallels with the preventative role of the three free cancer screening programmes offered by NSS were obvious.
“My experience shows, if you have the opportunity to get screening, why not? I talk to friends and encourage them to take part in screening themselves. Screening was really beneficial for me, early detection is what saved me. I didn’t need radiotherapy or bone marrow treatment, and now I’m a cancer survivor – a thriver!
“I suppose I might have been sceptical about taking part in another panel, on a lot of them I felt I was there to fill a position as a ‘token’ representative, or to tick a box. Not once on the PPP have I felt like that. At every meeting all of us are listened to. More importantly when we’re reviewing documents or leaflets, if we make a recommendation, at the next meeting you can see where the changes have been implemented. That is what I really like about being on the National Screening Service PPP. Your voice is listened to. I’m thrilled with the programme.
“In any medical service if you want to make change you have to make your voice be heard, and this is the perfect opportunity. From my own experience of being a member I can guarantee that changes will occur by people like me speaking up. The only way to make change is to get involved.”

| 53 HEALTH MATTERS SPRING2023
‘I help patients by bringing a plain man’s thoughts to something technical’
KEITH CAIRNS WILL KENNEDY
The HSE National Consent Policy 2022


Launch of the Easy-to-read version of the HSE National Consent Policy 2022
Elaine McCaughley, Senior Project Manager, National O ce for Human Rights and Equality Policy, explains the publication of the policy
In March 2022 the National O ce for Human Rights and Equality Policy published the revised HSE National Consent Policy 2022. The 2022 policy reflects legislative changes in recent years, and emphasises the will and preferences of the person in anticipation of the Assisted Decision-Making (Capacity) Act (2015). There are two eLearning modules for sta on the HSE National Consent Policy 2022 and these are available of HSEland.
On December 5th 2022 we launched an Easy-to-read version of the HSE National Consent policy 2022. Easy-to-read information is important for people with intellectual disabilities and people with other conditions a ecting how they process information, and a useful tool for the sta who support them. Experts, by experience, were involved in reviewing the Easy-to-read document during development, providing feedback on the language and images used.
Aisling Mason is a service owner in Enable Ireland, Dun Laoghaire, who communicates in words, gesture and with an AAC device. Aisling made a video presentation for the launch. She told us that ‘consent’ means deciding if she wants something or not. Aisling said, “As an adult I can, and will, give my own consent.”
Aisling explained that ‘Plain language, time to think and answer, time for questions, easy read using pictures’ all help her to understand the relevant information and make a decision.
Paul Crilly is an advocate and expert by experience with Ace Communication. He has an intellectual disability and a keen interest in accessible communication and information. Paul was involved in deceloping the Easy-to-read version of the HSE National Consent Policy 2022. Paul said “Easy-to-read information is very
important for people with intellectual disabilities, and for people that cannot read or understand complicated information. I feel very strongly that we have a right to information in a way that we can understand,” said Paul.
“The HSE National Consent Policy is an important policy. When I have information in the right way, I can understand and exercise my rights. I know what to expect of the sta that support me when it comes to consent. I know when, how and why I should be asked for consent.”
We hope that the Easy-to-read version of the HSE National Consent policy will help each person to know their rights and to make their own choices. Every adult should be presumed to have capacity to consent on their own behalf and should be provided with relevant information in a way they can understand.
The full HSE National Consent Policy 2022, the Easy-to-read version and a recording of the launch, and a range of other resources on consent are available at hse.ie/nationalconsentpolicy. /

HEALTH MATTERS SPRING 2023 54 |
Consent in Health and Social Care Research
HSE National Policy for Consent in Health and Social Care Research
The HSE National Policy for Consent in Health and Social Care Research was launched on February 9th.
Philip Crowley, HSE National Director for Strategy and Research, who launched the policy, said, “Health and social care research is a dynamic and interactive process. It has to be based on trust and on respect for the mutual aims of improving health, wellbeing and patient outcomes. The policy, a milestone for the HSE, aims to ensure that impactful research can be conducted safely, ethically, and in compliance with legal requirements, while maintaining the confidence of the participants and keeping them at the centre of the research process.”
The policy builds on the work completed in February 2022 by the National O ce for Human Rights and Equality Policy when they published the HSE National Consent Policy.
For the purpose of this policy, the term ‘consent’ refers to the informed and explicit agreement of a prospective research participant to take part in a research study and, when relevant, to the use of their personal data for such research. The agreement for both must be ethically obtained, recorded, and retained; the proposed consent protocol must be approved by an appropriate Research Ethics Committee (REC) and, when applicable, comply with Irish data protection legislation.
Ann Cullen, a patient representative who participated on the panel discussion during the launch, said, “The new HSE National Policy for Consent in Health and Social Care Research is a progressive and welcome document, which, through its development, placed Patient and Public Involvement (PPI) at the centre of a dynamic policy development process. In doing so, it reinforces the position of the participant at the very centre of the research consent process. It provides guidance for researchers in health and social care, to consent research participants in quality research, which is carried out within a legal and ethical framework and conducted in a consistent way.”
Dr Ana Terrés, Research and Evidence Lead, HSE Strategy and Research, said “International evidence has shown that health services where research is formally integrated as part of the organisational
structure deliver better care. Research supports best practice and optimal healthcare outcomes.The new HSE National Policy for Consent in Health and Social Care Research will guide high-quality health research in the context of the HSE National Framework for Governance, Management, and Support of Health Research.”
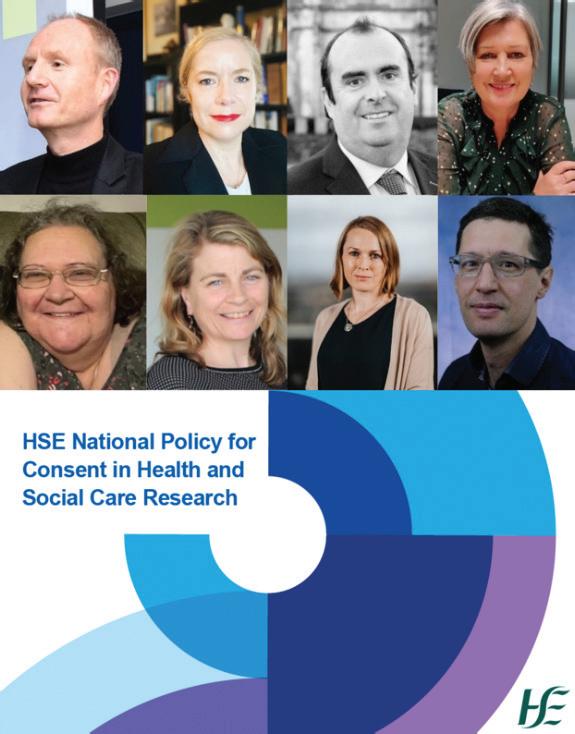
The policy provides one overarching HSE policy to guide healthcare services hosting research, particularly to those conducting research and to Research Ethics Committees approving research in the HSE and its funded organisations.
The policy clearly outlines that consent is a choice. Participants must understand what they are being asked to take part in and be given su cient information about the study including any potential risks and benefits. They should be given time to consider their participation and be given the opportunity to ask questions. They should be aware that they can choose to take part (give consent), choose not to take part (refuse consent), choose to consent to specific elements of the study (and not others) and choose to withdraw their consent. It should be explained to them that their usual care will not be a ected. The policy also describes the following:
• What is consent for health and social care research
• What is informed and valid consent
• How to process personal data for health research
• Obtaining, recording and retaining consent
• Participant Information Leaflet
• Re-consent
• Withdrawal of consent
• Capacity to consent in adults
• Research involving children
• And other considerations should as broad consent, retrospective chart reviews for research purposes and research involving biological materials.
This policy does not extend to clinical audits, standard service evaluations, or public health or advanced health analytics work carried out by the HSE for the purpose of fulfilling its legal obligations for the planning and delivery of health and social care services.
For more information, please see - https://hseresearch.ie/consent/
| 55 HEALTH MATTERS SPRING 2023
Our latest Initiative
GIVE your patient the opportunity to be an organ donor
Without the altruism of patients through their wish to donate their organs and the honouring of those wishes by their families, organ donation and transplantation would not be possible. Having that conversation with family and friends regarding your wishes around organ donation can make the decision easier for your family if ever faced with an end-of-life organ donation conversation in ICU. Specialist clinical roles to support organ donation were established in 2015 as recommended with the implementation of the European Directive 2012, ensuring organ donation is offered to patients and their families where appropriate. Organ Donation Nurse Managers (0DNM) and Consultant Clinical Leads in Organ Donation (CLOD) work in hospitals nationally, providing guidance and support to families and multidisciplinary healthcare teams when
exploring the wishes of patients and their families and hands-on clinical care during this process.
Organ donation occurs in every Intensive Care Unit throughout Ireland. The Organ Donation Nurse Manager, along with the Clinical Lead in Organ Donation, have pivotal roles in identifying potential organ donors, optimising opportunities for patients and families whom wish to donate, offering clinical expert advice where warranted while continuing to support and protect the interests of potential donor patients and their families. In addition, the Organ Donation Nurse Manager and the Clinical Lead in Organ Donation have a central role in education regarding all aspects of organ donation and provide clinical leadership in raising awareness of organ donation. This specialist team collaborate in delivering multi-disciplinary education sessions throughout the country. Prior to the COVID-19 pandemic, face-to-face sessions
enabled healthcare professionals throughout Ireland to meet, discuss and learn from each other’s experiences. During the pandemic, teaching sessions were adapted and continued online. The team are delighted to confirm a return to in-person and continuing of blended education sessions in 2023.
Organ Donation Nurse Managers and Clinical Leads in Organ Donation work with the National Organ Procurement Service in Organ Donation Transplant Ireland (ODTI) to foster a positive culture towards organ donation. We are fortunate to work collaboratively with highly skilled Critical Care and wider healthcare teams in promoting and facilitating organ donation, particularly in the Intensive Care Unit, Emergency Medicine and Theatre Departments. Their commitment, dedication and compassion contributes to a positive attitude to organ donation.
The Organ Donation Nurse Manager's

HEALTH MATTERS SPRING 2023 56 |
Bernadette Nohilly, UL Hospital Group; Breda Doyle, South/South West Hospital Group; Karen Healy, RCSI Hospital Group; Nicola Phillips, Dublin Midlands Hospital Group; Gillian Shanahan, Saolta Hospital Group; Orla Craddock, Ireland East Hospital Group.
responsibilities include dissemination and implementation of national guidelines and procedures for organ donation within the Hospital Groups, the delivery of education and completion of a Potential Donor Audit. Service planning and development is also a fundamental part of the Organ Donation Nurse Manager’s role while managing activity within the clinical area. Our philosophy of care encompasses the principles that we are committed to providing support to grieving families when considering the option of organ donation for their loved one and guiding them through the donation pathway. We are dedicated to providing individualised patient-family-centred care while incorporating our core values of care, compassion, and commitment while upholding the patient’s dignity and respect. Families we encounter are often grieving tragic and sudden circumstances surrounding a loved one. It is vital to acknowledge the difficulties being experienced by the family. As a team, we are skilled and competent to approach the conversation regarding organ donation. It is crucial that families have a clear understanding that their loved one will not survive before the topic of organ donation is explored. For families, the option of organ donation can be a positive decision in an otherwise tragic situation. Working within the ICU team to support the family through each stage of the process and delivering of a high standard of care is always our priority.
OUR LATEST INITIATIVE
Our overarching aim is to ensure that organ donation is considered, where appropriate, as a usual part of end-oflife care.
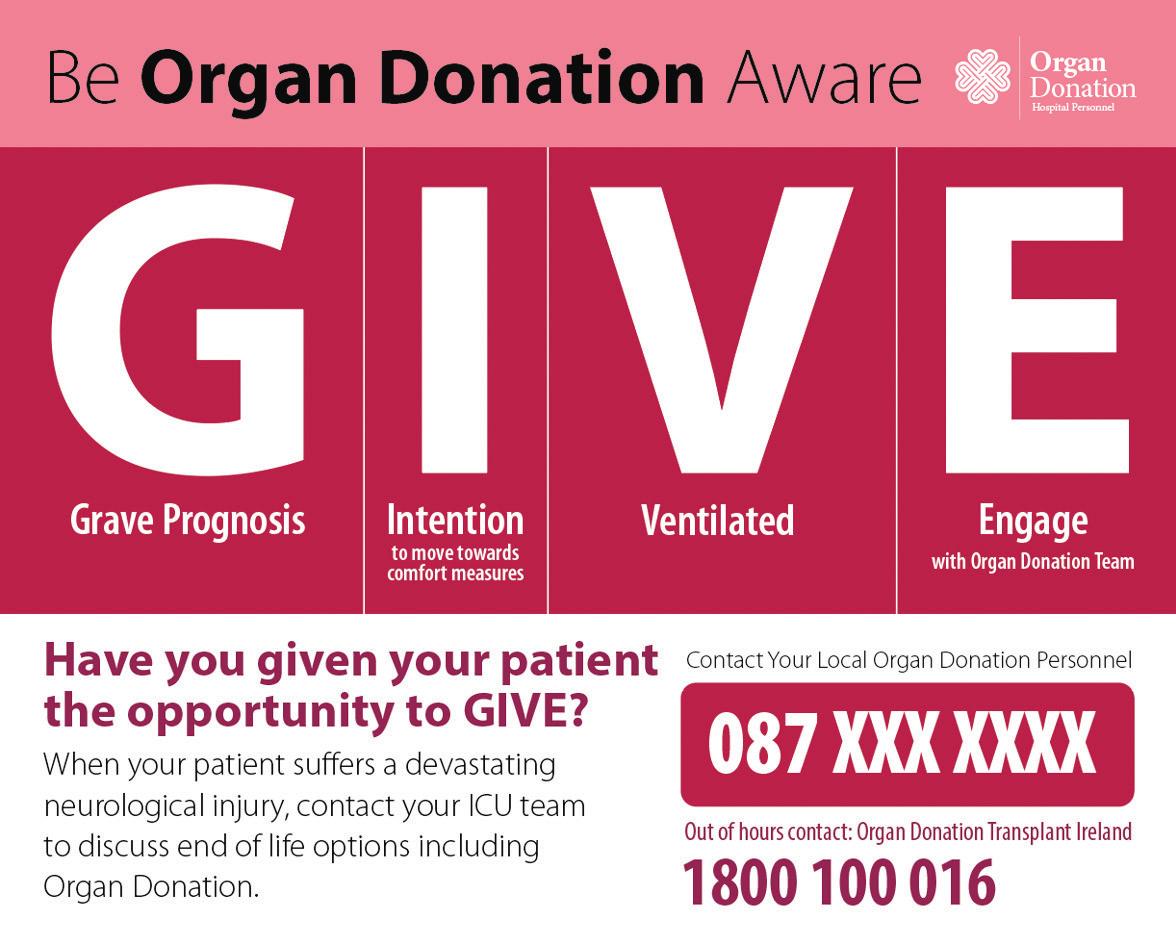
In Ireland all patients that donate after death, die in ICU. The vast majority of these patients have been admitted from the Emergency Department. While many people support organ donation, circumstances enabling patients to be offered the opportunity to become an organ donor is a rare event. Therefore, a systematic approach within our hospitals is integral to identifying patients who may be possible donors.
The core principle of our latest initiative is to ensure that organ donation can be explored to maximise the opportunity to facilitate organ donation as per the wishes of the patient and family. The G.I.V.E acronym is a quality improvement project introduced by the Organ Donation Nurse Managers and Clinical Leads in Organ Donation team. As a group we have adapted an Australian project aimed at considering organ donation in end-of-life situations and providing information on how this can be facilitated. This is a hospital-wide initiative focusing on Intensive Care Units and Emergency Departments around the country. G.I.V.E acts as a clinical support tool. It is designed to assist clinical healthcare staff in prompt potential donor patient detection.
The G.I.V.E clinical trigger provides guidance on categories of patients who may
fulfil the criteria for Organ Donation after brain death and circulatory death. In addition, the contact numbers for organ donation personnel, specifically the Organ Donation Nurse Manager for the relevant hospital group, is provided to support clinical staff with end-of-life options and organ donation. It is endorsed by the Intensive Care Society, the Irish Association of Emergency Medicine and the Irish Association of Critical Care Nurses.
Identification of the potential donor is an imperative step in the organ donation process. Patients must be clinically managed throughout, so that organ donation remains an option. This can be particularly challenging given the physiological effects of brain death and requires expert Medical and Nursing care. Families will be asked to consider their loved ones’ wishes after brain death is declared or, as is the case in donation after circulatory death, as part of end-of-life discussions.
These discussions are not a one-off event, but rather a series of discussions with the Organ Donation Nurse Manager or Clinical Lead in Organ Donation. Families are assured that their wishes will be respected regardless of their intent to donate or not. The collaborative efforts of the Organ Donation Nurse Manager and local Critical Care multidisciplinary teams can guide and support families through all aspects of the organ donation process.
Notably organ donation requires significant teamwork of healthcare experts from various disciplines including Emergency Departments, Critical Care Units and Theatre Departments who work tirelessly despite everyday pressures to ensure that organ donation is facilitated to the highest standard. Respect, empathy, and kindness are widely demonstrated by teams to donor patients and their families. Most importantly we acknowledge all organ donors and all families for considering organ donation.
| 57 HEALTH MATTERS SPRING2023
Families we encounter are often grieving tragic and sudden circumstances surrounding a loved one. It is vital to acknowledge the difficulties being experienced by the family.
Integrating our European neighbours into our healthcare system
The Health Identity Management Services (HIDS) team’s data transformation project
Tens of thousands of Ukrainian refugees have arrived in Ireland, fleeing the war in their homeland. Securing their medical history and personal data to be accessed by healthcare teams all around the country was a vital part of their arrival.
Gathering the information was the key aim of the data and informatics group, one of nine main workstreams established by the HSE National Ukrainian Health Response Planning and Coordination Group.
The data and informatics group collaborated across clinical, operations and technical teams by leading the governance, digital health questionnaire development and data insights to enable and support decision-making for the IT leadership in a time of crisis.
Director of the Health Identity Management Services (HIDS) Maria McCann led the workstream to deliver a data and informatics response to support the HSE's planning and coordination group, supported by EY and Microsoft Global Disaster Recovery Team.
They worked with representatives from National Social Inclusion Office, Integrated Information Services (IIS), HSE Language translation team, Primary care, Community Operations, Operations team at National Transit Centre (NTC) at Citywest, and Health Intelligence Unit.
The group were able to deliver a reliable, secure and scalable digital solution to capture the demographic and health service questionnaire medical information of the incoming displaced person. This was then shared with the displaced person in the language of their choice (Ukrainian or Russian) via email and had the English translation for healthcare professionals to view when the displaced person presented to them.
The technology can provide up-to-date reports and illustrate daily and weekly trends on key data elements from the digital solution for the health status questionnaire and triage information. This data is then shared with the Health Intelligence Unit for predictive modelling.
The modelling highlighted accommodation stressors given the uneven geographical distribution of accommodation for Ukrainian citizens in Ireland; different health needs and associated age brackets. This gives the HSE departments and policy makers a snapshot in time of an evolving situation. So essentially, they can make informed decisions based on the insights provided by the data.
The data challenge and opportunity
Ukrainian nationals were entering Ireland at multiple locations via ports and airports.
This necessitated a system of data collection at the point of entry in order to ensure health information was acquired and urgency of care identified.
The IT system built out ensured that demographic data (name, age, sex, passport identity; etc), along with a health questionnaire, was collected immediately on entry at the Citywest Convention Centre designed as the official National Transit Centre for beneficiaries of temporary protection.
The technology
Behind the scenes, the back-end systems to support a large-scale, everchanging movement of people – into and then around Ireland – was being built in an expedited manner.
The HIDS team, in collaboration with EY and Microsoft, used the MS Dynamics 365 and power platforms to develop a health questionnaire form that captured the demographic and high-level medical details of the displaced person.
Once the details are filled in, the displaced person receives an acknowledgement email with a PDF that contains the information they provided in their language of choice and in English for health care professionals to read. The data captured is then transformed to dashboards using Power BI for HSE personnel to use to support demand and capacity planning across the nation.
“We worked with the team onsite to build a reliable, secure, userfriendly, easy to navigate, scalable digital health status questionnaire solution, ensuring a key focus on delivering a product that was suitable for rapid deployment and addressed the various operational and governance challenges,” explained Brian Kearney, Operational Lead, NTC, Citywest.
Maria McCarthy, who is Assistant Director of Public Health Nursing at the NTC, said the digital health questionnaire solution was a ‘gamechanger’ for their processes.
“Not only has it improved the patient experience by supporting them to easily complete their health questionnaire online in different languages, but it has also improved our clinical operations by providing real-time access to patient data. This has made it easier for our clinical staff to make informed decisions and provide personalised care.”
HEALTH MATTERS SPRING 2023 58 |
Contact
Make Every Count
Occupational Health Department making sure every contact counts
WHAT IS MAKING EVERY CONTACT COUNT?
Making Every Contact Count (MECC) enables the opportunistic delivery of consistent and concise healthy lifestyle information and enables individuals to engage in conversations about their health at scale across the health service.
The Making Every Contact Count (MECC) programme, developed by the HSE, aims to train all healthcare professionals to support patients to adopt healthy behaviours during routine healthcare contacts. Even small changes to behaviour can make a real difference to people’s health and quality of life. Through the millions of contacts with patients each year across the health service, healthcare professionals are being asked to take the opportunity during their daily contacts with patients and service users to:
Congratulations to the Occupational Health Department Mid-West who are walking the talk when it comes to Making Every Contact Count.
The department is now a Making Every Contact Count implementation site – the first such announcement within the HSE Occupational Health Departments nationally to date.
“Occ Health Mid-West currently use every opportunity to embed brief interventions within its service provision – one conversation at a time. It is fantastic to receive recognition for the ongoing work the team are doing, on a daily basis,” said Occupational Health Mid-West Clinical Nurse Manager 3 Claire Curtin.
“It will also be a great opportunity to join with other teams to promote services that are available to healthcare workers within the HSE. Teaming with other frontline HSE staff to implement Making Every Contact Count will have a positive impact on the health and wellbeing of our service users - this is what it’s all about. Evidence suggests that the broad adoption of MECC across the health service can have a significant positive impact on the health of our population. We want to play our part.”

“Each clinical team member within the department has completed the MECC training online and in the classroom setting. Feedback for this was extremely positive.”
Earlier this year, Occupational Health Mid-West formed a small working group to develop a MECC implementation plan for the service, liaising closely with the Mid West Health& Wellbeing Unit. The plan covers communications, resources, recording and quality improvement processes. It was informed by national guidance and current research, Implementation of Making Every Contact Count (MECC): Developing a collaborative strategy to optimise and scale-up MECC. By Making Every Contact Count, Team Mid-West staff are improving the quality of the care they provide to healthcare workers who avail of the service, providing support to those who support the public.
The service is the first of its kind in the Occupational Health setting nationally to date. We look forward to working with healthcare workers, hearing all their success stories and learning from our interventions also! For now, it is congratulations and thanks to Mid-West team for reaching their ‘go-live’ date.
1. support patients to make lifestyle choices that help prevent chronic diseases
2. promote self-management of existing chronic diseases
Implementing Making Every Contact Count means:
1. staff complete the full Making Every Contact Count training (8 eLearning modules and workshop)
2. staff undertake regular brief interventions in day-to-day practice
3. staff record and monitor brief interventions using agreed processes decided by the service itself
4. there is a system in place to use the data collected for service improvement decided by the service itself
For more information: https://bit.ly/38SCNNh
| 59 HEALTH MATTERS SPRING2023
The Occupational Health Department Mid-West.
Recovery, resilience and reform
















Clinical programmes conference draws large crowd













Almost 300 delegates gathered on a wet Friday morning in Croke Park for the first National Clinical Programmes Conference Day since the advent of the COVID-19 pandemic. The wet weather didn’t dampen the mood as colleagues were eager to meet in person, some for the first time.
The conference theme focused on recovery, resilience and reform. The opening address came from our HSE Chief Clinical O cer, Dr Colm Henry, who spoke about the impact and HSE response to COVID-19, lessons learned from the pandemic and the need to build on the momentum gathered in areas such as healthcare digitalisation.





This was followed by the Minister for Health Stephen Donnelly, who focused on the impact of the National Clinical Programmes (NCPs) and Sláintecare on our healthcare system. Stephen Mulvany, HSE Acting CEO, subsequently outlined to the audience his vision of translating strategy and corporate objectives into building resilience and lasting. The morning session concluded with a lively panel discussion from Dr Henry, Dr Philip Crowley, HSE National Director, Strategy & Research, Mr Damien McCallion, HSE Chief Operations
O cer, Mr Mulvany and Dr Siobhán Ní Bhriain, HSE National Clinical Director, Integrated Care, on the topic of ‘What we need to do to absorb, adapt and transform reflecting upon the last three years in the system to build lasting reform’.





Co ee break gave the opportunity for delegates to peruse the 40 posters on display which showcased innovative quality improvement work led by the national clinical programmes, while also highlighting the extensive stakeholder collaboration between the programmes and clinical community and patients/services users.
The winning poster of the NCP Conference Day Poster Competition was ‘NCP for Paediatrics and Neonatology Response to the COVID-19 Pandemic’. The award was accepted by Jacqueline de Lacy, Programme Manager, on behalf of NCP Paediatrics and Neonatology. Dr Tara


Gill and Dr Mustafa Mehmood received a special commendation for their work on ‘Domestic violence in Emergency Department in St James’s hospital’, during the COVID-19 pandemic.

The mid-morning session kicked o with Professor Samuel Cromie, Director, Centre for Innovative Human System, TCD, presenting on ‘What do we mean by a resilient healthcare system?' Jean Kelly, Clinical Lead and Operational Site Manager for the Vaccine Programme in CHO2, and Irene Maguire, Senior Physiotherapist, HSE West, finished this session by introducing ‘Better Together’, the Health Services Patient Engagement Roadmap.
The afternoon session breakout rooms gave delegates the opportunity to hear about further developments by the clinical programmes as well as HSE strategic projects, innovation and Sláintecare-funded initiatives. The national clinical programmes shared learnings on how they have designed, developed and supported the implementation of clinical models of care and pathways over the past three years, aimed at improving/ reforming population healthcare, focusing on health and wellbeing, enhancing the quality of healthcare and a re-orientating healthcare to the community. Speakers from the innovation breakout room covered topics from genetics and genomics to new roles and services across a mix of healthcare professions. While some of the Sláintecare Funding initiatives covered included: SMILE: Supporting Multi-morbidity self-care through Integration, Learning and eHealth; Social Prescribing; Integrated Care Pathway for the Management of Headache/ Migraine; Heart Failure Virtual Consultation Service and ‘Living Well’ to name a few.
On behalf of both the CCO and Dr Siobhan Ni Bhriain, Clinical Design and Innovation would like to thank all the speakers as well as attendees who made this year’s conference so enjoyable. For those of you who would like more information on the Conference including some of the presentations from the day please visit https://www.hse.ie/eng/about/ who/cspd/resources/conference-resources/
HEALTH MATTERS SPRING 2023 60 |
Dr Siobhán Ni Bhriain, National Clinical Director, Integrated Care presenting at the National Clinical Programmes Conference Day 2022.
Morning session speakers and chairs from left to right: Dr Siobhán Kennelly, Consultant Geriatrician, Connolly Hospital/ CHO9; Dr Colm Henry, Chief Clinical O icer; Dr Siobhán Ni Bhriain, National Clinical Director, Integrated Care; Dr Philip Crowley, National Director for Strategy and Research; Prof Áine Carroll, School of Medicine, UCD.
Dr Colm Henry, Chief Clinical O icer, presenting at the National Clinical Programmes Conference Day 2022.
Mid-morning session speakers and chairs from left to right: Professor Samuel Cromie, Director of the Centre for Innovative Human System, TCD, Pat Healy, National Director, Clinical Programme Implementation & Professional Development, Irene Maguire, Senior Physiotherapist, HSE West, Jean Kelly, Clinical Lead and Operational Site Manager, Vaccine Programme CHO2, Fran Thompson, Chief Information O icer, Professor Richard Greene, Chief Clinical Information O icer, Prof Ristéard Ó Laoide, National Director, National Cancer Control Programme, Dr Eimear Brannigan, National Clinical Lead, Antimicrobial Resistance & Infection Control, Dr Paul Kavanagh, National Health Intelligence Unit, HSE Strategy and Research.
Patient Safety Together
The National Quality and Patient Safety Directorate launches Patient Safety Together: learning, sharing and improving
Patient Safety Together is the new sharing learning component of the patient safety programme to support the HSE’s Patient Safety Strategy 2019-2024. This freely available online resource will provide a reliable and easily accessible approach to sharing patient safety learning within Irish healthcare.

How
will Patient Safety Together share learning?
Using up-to-date quality and patient safety (QPS) information including incident management data and national and international evidence, Patient Safety Together will enable all users to:
1. Learn directly from Patients/Service Users and Sta
• Patient Safety Stories led by Loretta Jenkins, NQPSD, will give a voice to both patients/service users and sta who have been involved in, or impacted by, patient safety issues and want to share learning. They will be available in video and narrative format and will share learning from areas of excellence, positive scenarios that occurred in our system and when things go wrong.
• The Patient Safety Community will create a national peer-supported online community for QPS sta .
2. Learn from Incidents, Research and Data
• HSE National Patient Safety Alerts (NPSAs) are high priority communications in relation to patient safety issues, which require HSE services and HSE-funded agencies to take specific action(s) within an identified timeframe, in order to reduce the risk of occurrence or recurrence of patient safety incidents that have the potential to cause serious harm or death. They are issued by the HSE in conjunction with
relevant stakeholders (subject matter experts, patient representatives, clinical and academic experts).
• Patient Safety Supplements will inform HSE and HSE-funded agencies of timely and relevant quality and patient safety information for learning purposes. Content will be identified from several patient safety intelligence sources including the analysis of incident reporting, reports from frontline services, or new national or international research and evidence.
3. Access Further QPS Learning
• Signposting to QPS academic papers, resources, conferences etc.
• Bi-monthly HSE Patient Safety Digest developed by the HSE Health Library Ireland Services - in collaboration with the NQPSD cataloguing journal articles and reports relating to patient safety
There were over 16 areas across our health services involved in co-developing Patient Safety Together.
Speaking at the launch, Dr Orla Healy, National Clinical Director, NQPSD, and Lorraine Schwanberg, Assistant National Director, NQPSD, acknowledged everyone’s important contribution and highlighted the collaborative way the team with Catherine Hogan as project lead, supported by Noemi Palacios, worked together determinedly over the last three years to build this important new platform.
By actively identifying and sharing learning, Patient Safety Together will be a valuable learning resource to help reassure everyone using and working in our health services that we aim to continually improve our patient care, support our sta and help prevent patient safety incidents occurring or recurring.
Patient Safety Together: learning, sharing and improving together www.hse.ie/pst
If you are a sta member interested in joining the Patient Safety Community please email patientsafetytogether@hse.ie
SERVICES INVOLVED IN THE PROJECT GROUP
• Forum for Irish Post Graduate Medical Training Bodies
• Health Information and Quality Authority
• Mental Health Commission
• National Patient Safety O ice, DoH
• Patient RepresentativesPatients for Patient Safety
IRELAND & HSE NATIONAL PATIENT/SERVICE USER FORUM


• State Claims Agency
• HSE
• CCO Clinical Forum
• HSE Digital Team
• National Ambulance Service
• National Health & Social Care Professions O ice
• National Quality and Patient Safety Directorate
• National Screening Service
• O ice of Nursing and Midwifery Services Director
• QPS Acute Operations
• QPS Community Operations
| 61 HEALTH MATTERS SPRING 2023
Lorraine Schwanberg , Assistant National Director, National Quality and Patient Safety Directorate
Catherine Hogan, Patient Safety Together Lead, National Quality and Patient Safety Directorate.
Maureen Flynn, QPS Connect Team Lead, National Quality and Patient Safety Directorate; Flavien Plouzennec, User researcher, Communications Division; Ulla Devitt, Digital development and user experience manager, Communications Division; Noemi Palacios, Patient Safety Learning Coordinator, National Quality and Patient Safety Directorate.
Human Factors
National Quality and Patient Safety Directorate publishes their annual prospectus
The National Quality and Patient Safety Directorate (NQPSD), led by Dr Orla Healy, works in partnership with HSE operations, patient representatives and other partners to improve patient safety and quality of care.
Everything we do is anchored in the Patient Safety Strategy 2019-2024. A key commitment of this Strategy is to empower and engage sta and patients to improve patient safety. We aim to honour this commitment by supporting a culture of continual learning through education programmes, resources and learning opportunities. To that extent, we are delighted to launch our annual Prospectus of Quality and Patient Safety education and learning programmes.
What is the QPS Prospectus?
This prospectus provides information about the education and learning programmes available to sta , students and patient partners through e-learning, virtual learning and face-to-face workshops. Our programmes cover key areas relating to quality and patient safety such as:

• Quality Improvement
• Incident Management
• Open Disclosure
• Clinical Audit
• Human Factors
This year we are pleased to include contributions from our colleagues in National Governance & Risk, National Complaints, Governance and
Learning, the National Safeguarding O ice, AMRIC (Antimicrobial Resistance and Infection Control) Organisation Development, Change and Innovation as well as information about programmes o ered by the Library Services to support education, learning and research.
How will this resource help you? This resource will help you identify learning programmes that will support you in your day-to-day work to improve quality and patient safety and it will also support you in planning your personal or professional development. Many of our programmes are eligible for CPD credits from RCPI, NMBI and CORU. We hope you find it a useful resource to support you in your own development and we look forward to welcoming you onto our programmes in 2023.
The QPS Prospectus can be found on our website.
(scan QR code )


Introduction to Human Factors: new e-learning programme
According to national and international evidence, one in eight patients su ers harm while using healthcare services. In addition, it is estimated that 30-70% of adverse events that occur in hospitals are preventable.
Human Factors is the science that looks at the role of human involvement in any situation, giving consideration to both our capabilities and limitations. It provides an understanding of the impact that organisational culture, system design, equipment and the work environment have upon human behaviour and task performance.
The implementation of Human Factors knowledge and research is a key component in our collective approach to ensuring safe, e cient and high-quality care throughout the healthcare system and in maximising sta performance and wellbeing.
Human Factors is not new. As a science it has grown steadily in high-risk industries since it was first introduced in aviation during the Second World War. It was first adapted for healthcare in the mid-1990s. Since 2015 the need for targeted Human Factors training and education has been highlighted in the National Clinical Guidelines in Ireland, but until now, no specific programme was available in the HSE.
The Introduction to Human Factors e-learning programme is a 20-minute, self-directed programme developed by the NQPSD and Human Factors Facilitators Group to meet this learning need by:
• Introducing Human Factors as a new way of thinking about safety in everyday work.
• Supporting learning about factors that impact on our capabilities and limitations as humans and using this knowledge to improve our wellbeing and performance and make our healthcare systems safer.
This Introduction to Human Factors programme is o ered as the first step in a learning pathway that aims to build the learner’s knowledge and skills relating to Human Factors. It aims to entice participants to want to know more about why and how human factors can improve the performance and wellbeing of individuals and teams and influence safety in the healthcare system. The interactive content covers topics such as definition; the history of human factors; key factors; Human Factors in practice.
Throughout each stage of development, we collaborated and tested the content with the Facilitator Group and others. Their input assisted us in refining the flow, imagery, graphics and script of the programme and in collating the additional resources for extended learning.
The Introduction to Human Factors is available on HSELand and is suitable for all sta (clinical and non-clinical) and patient partners across all areas of the health service.
For further information, please contact QPS.EDUCATION@hse.ie
For more information about this and other Human Factors Programme work, contact Margaret.Codd@hse.ie, National Quality & Patient Safety Directorate.
HEALTH MATTERS SPRING 2023 62 | |
Open Disclosure Themed Week raises awareness
The HSE National Open Disclosure Office - with Open Disclosure leads across HSE and HSE funded services - planned and facilitated an Open Disclosure themed week.


The purpose of this week was to
• promote and raise awareness of the importance of open disclosure to patients and their families and to patient safety and quality improvement generally

• ensure that sta are aware of their obligations in relation to Open Disclosure
• ensure that sta are aware of and compliant with mandatory training requirements
• raise awareness of the resources available for services, sta and the public to support them when engaging in open disclosure discussions.
The week focused on a number of themes pertaining to Open Disclosure including the patient perspective, documentation, approaches to implementation of the HSE Policy, training and sta support.
Date for your Diary: Open Disclosure
Themed week 2nd – 8th October 2023.
Email opendisclosure.o ice@hse.ie for further information and resource pack. https://www.hse.ie/eng/about/who/ nqpsd/qps-incident-management/ open-disclosure/open-disclosure.html
The Patient Perspective: Preparation for the week involved communication and input from patient representatives and advocacy services to ensure that the patient voice was strongly represented throughout the week. Patient representative groups, independent patient representatives and advocacy services were actively involved in messaging and promotions. The public page of the Open Disclosure website was updated and launched and a resource document providing a list of Support Services and Resources for Patients and Service Users following an Incident was published.
Documentation: The importance of good documentation of open disclosure was reinforced and links provided to supporting resources available on our website.
Training: Training and promotional events were held across many services and there was an increased uptake of the online training modules during this week.
Approaches to implementation: Sta from the National Open Disclosure O ice and from across HSE service areas discussed various approaches to implementation in an Open Disclosure webinar attended by 328 sta . An implementation checklist is available on our website.
Sta support: The importance of providing support to all those involved in patient safety incidents was emphasised with links provided to the ASSIST ME Model of sta support and a new resource providing a list of the support services, resources and training programmes developed and launched, available on our website.
Acknowledgements: The sta in the National Incident Management Team and National Open Disclosure O ice would like to sincerely thank all of the Open Disclosure area leads, site leads, managers and sta and all who engaged in promoting Open Disclosure during this week and we look forward to future similar events.
| 63 HEALTH MATTERS SPRING 2023
Patients for Patient Safety Ireland
Dr Aine Mitchell, ED Consultant and Open Disclosure Clinical Lead, Sligo University Hospital
Mater Hospital
New National Strategy Provides Path Forward for Genetics and Genomics in Ireland
Improved
Our genes hold powerful information that can be used to help diagnose conditions, guide more e ective treatments, and predict our risk for disease.
Genomic medicine harnesses this power to improve patient outcomes and overall population health and wellbeing through an approach to healthcare that is more personalised, predictive, preventative, data-driven, and cost-e ective.

Ireland has made progress in developing its genetic and genomic services, with pockets of excellence evident throughout the country. However, to fully realise the benefits of genetics and genomics, there is an urgent need to mainstream them so that they can become an integral part of our routine care delivery.
In early 2022, the Strategic Programmes O ce (SPO) within the O ce of the Chief Clinical O cer, in collaboration with the Department of Health, began the process of developing Ireland’s first national strategy to advance the field of genetics and genomics.
After eight months of work and the invaluable input of more than 100 healthcare professionals, academics, international experts, and patient representatives, the HSE launched the National Strategy for Accelerating Genetic and Genomic Medicine in Ireland in December 2022.
The National Strategy was designed to centre the voices of patients and families, to build upon existing good practice, and to speak to key areas of concern including data and privacy, testing infrastructure, and workforce development. Moreover, it provides a singular vision for the development of a nationally led genetic and genomic medicine service.
HSE Chief Clinical O cer Dr Colm Henry said, “Advancing Ireland’s genetics and genomics service means improving healthcare for everyone in Ireland. Through this new expert-informed strategy, we can work toward a future where genetic and genomic medicine will be part of routine care delivery that can be accessed equitably across the country, from visits to the GP to extended care for rare disease or cancer.”
With initial funding from the Department of Health of €2.7 million for 2023, work on rolling out the strategy has already begun.
A detailed plan that outlines a number of key objectives for this first year of implementation has been developed, with the first order of business being the creation of a new HSE national o ce for genetic and genomic medicine and the recruitment of key roles within it.
The o ce, once established, will provide oversight and a standardised approach to the delivery of the genetics and genomics service as outlined in the National Strategy.
To enhance patient and public knowledge and understanding of genomic medicine, and to keep HSE sta informed and engaged throughout this time of change within the genetics and genomics service, a targeted communications programme is being developed. Patient and public involvement (PPI) e orts, continued from the National Strategy’s development process, are already underway.
Work has also progressed to commence the development of a dedicated workforce plan to support the recruitment, retention, education, and career development of the current and future genetics and genomics workforce. This plan will be aligned with broader HSE and Department of Health workforce plans and will build upon previous work, such as the HSE’s 2019 Review of the Clinical Genetics Medical Workforce in Ireland.
Additionally, the new national o ce will begin in 2023 to develop a national test directory for genetics and genomics to enable appropriate and equitable testing, and it will start the process of reviewing existing genetic and genomic data capacity and sharing capabilities with a view to modernising and harmonising laboratory services across the country. Deirdre McNamara, Director of the SPO, said, “Through this new strategy, we will build upon the good work in genetics and genomics already taking place throughout the country to create a more equitable, e cient and e ective service that will improve patient outcomes and experience while advancing research, innovation, and discovery.
The National Strategy for Accelerating Genetic and Genomic Medicine in Ireland is available on the HSE website at https://www.hse.ie/eng/ about/who/strategicprogrammes-o iceoverview/nationalstrategy-foraccelerating-geneticand-genomic-medicinein-ireland/
HEALTH MATTERS SPRING 2023 64 |
outcomes for patients and families and new career opportunities within the health service on the horizon
I can pinpoint the start of my interest in genetics to a lecture at the National University of Ireland, Galway, over 20 years ago whereby a professor outlined various genetic diseases and the link between certain traits and changes in a person’s genetic make-up.
Following my studies, I worked at the University of Melbourne, Australia with world-renowned specialists in the fields of epilepsy genetics.
One particular memory from that time that has stayed with me is of a mother learning after some years the genetic diagnosis of her young daughter who had severe epilepsy and developmental delay. Although the diagnosis was not easy to hear, she had worried she’d caused her daughter’s illness whilst pregnant and was relieved to learn
I discovered genetics in school, a subject that combined two of my loves: maths and biology. I also learned early on that I have an affinity for caring for those experiencing intellectual or physical difficulties.
I went on to study genetics in Trinity College Dublin. In my final year, we had a course of lectures on genetic counselling. I knew then the career I wanted to pursue, and went on to complete a new Master’s course that had just begun in Manchester.
Following my Masters, I joined the team at the National Centre for Clinical Genetics in 1999. The service had just started, and we all wanted to make a difference. However, the service was to struggle as there was no overall direction, no strategy,
that it was instead due to ‘bad luck’.
Since returning to Ireland, I helped develop the epilepsy gene panel and am currently the Chief Clinical Scientist leading the diagnostic team at a new purpose-built laboratory for germline genetic testing. Although my role is not patient-facing, the patient is always at the forefront of my work. Through multidisciplinary meetings, the impact of our work and genetic diagnoses is further realised.
This impact continues to drive my interest and love of the profession and is always at the centre of any discussions I have with people not familiar with the field of genetics.
As my career progresses, I would like to see genetic testing becoming an integral part of the clinical work-up for patients in Ireland.
and no national plan. I moved in 2016 to work in the National Rare Disease Office.
As a genetic counsellor, I had found it frustrating that there was no national listing of clinical expertise for referral purposes. The NRDO is responsible for cataloguing all clinical expertise and runs an information line to signpost families and healthcare professionals.
Through the years I have met some amazing families and inspiring clinicians. I have been part of numerous working groups and have just stepped down as Chair of the Irish Society of Human Genetics. I am delighted to see the Government funding the implementation of this strategy and I look forward to fully supporting its implementation.




Q&A WITH CCO DR COLM HENRY

QUESTION: WHY INVEST SO MUCH IN GENETICS AND GENOMICS?
Answer: Genomic medicine has the power to transform our healthcare future by allowing for better diagnostics, treatments and disease prevention. Enhancing our ability to seize the opportunities presented by this exciting and evolving area of medicine will allow us to improve patient outcomes, drive down the cost of care, and fuel the translation of scientific innovation and discovery into clinical practice.
Q: WHAT SORTS OF CHANGES CAN STAFF EXPECT IN THE COMING YEARS?
A: The service will benefit from national coordination and oversight with the establishment of a national office, and we will begin working immediately to address shortages in the frontline workforce such as genetic counsellors and clinical geneticists. There will also be a great deal of opportunity in the coming years for professional development in this area, both for specialists and non-specialists.
Q: WHAT WILL BE THE CHALLENGES OF IMPLEMENTING THIS STRATEGY?
A: All countries face similar challenges in this area, particularly workforce development and enhancing laboratory and data infrastructure to drive advancements in genetics and genomics. With this National Strategy, as well as our recent entry into Europe’s 1+Million Genome initiative, (1+MG) and the European Genomic Data Infrastructure Project, we are now in a much stronger positon to meet these challenges
| 65 HEALTH MATTERS SPRING2023
DR SINÉAD HOWARD CHIEF CLINICAL SCIENTIST
JACQUELINE TURNER GENETIC COUNSELLOR
Margaret Cuddigan; Dr Mark Bale; and Karen Morgan.
Deirdre McNamara; Robert Watt; Dr Mark Bale; Dr Colm Henry; Prof Eileen Treacy.
Prof Eileen Treacy; Prof Owen Smith; Anne Lawlor; Orlaith Brennan; Dr Derick Mitchell; Jennifer Moran.
Prof Mary Horgan, President, RCPI; Prof Brendan Loftus; Deirdre McNamara.
Under the Weather
Staying well and managing symptoms when antibiotics are not needed

For the vast majority of us most of the time we can manage the common symptoms of a viral infection by ourselves, easing the worst of the symptoms while our own immune system kicks in and the virus runs its course. Learning how to manage common illnesses with confidence and common sense is a great life skill and improves our understanding of when we need antibiotics and when we don’t. Looking after our health is something that we learn from our parents, friends, doctors, from our own experience and, more and more, from the internet. undertheweather.ie is a HSE website that gives practical, common-sense advice and information on dealing with many common illnesses like colds, flu, earaches, sore throats, tummy bugs and rashes. Last year more than 800,000 visitors went online to get advice on the many di erent illnesses listed on undertheweather.ie
Dr Eimear Brannigan, HSE AMRIC Clinical Lead, explained that most infections are caused by viruses. For example, 98% of sinus infections are caused by viruses.
“Having lived through a pandemic we have all learnt a lot more about viral illness and how we can protect and treat ourselves. What we really need to do now is to continue to reinforce the message that we can usually manage the symptoms of viral infections ourselves without looking for an antibiotic. Most people are aware that antibiotics don’t work for viral illnesses and we saw a reduction in antibiotic use during COVID-19. However antibiotic use is going up recently and they just do not work for viral illnesses,” she said.
“There is plenty you can do, such as taking paracetamol or ibuprofen for pain relief and to bring down temperature, to running a steamy shower to clear out nasal passages. If you are coming down with a virus, accept that it will take time to run its course. We expect to feel better straight away but in fact, if you


have a sore throat it’s typically going to take seven days, an earache will take three to five days and a cough can last three weeks.

“The website also highlights the need to change our culture around antibiotics; we need to ensure that we reserve antibiotics for those cases where they are really needed – that is for bacterial infections. Part of the change in culture is using undertheweather.ie. If we all understand that we can usually get better ourselves without an antibiotic, that’s better for everybody.”







Some people still believe antibiotics can help them to get better from common illnesses like tummy bugs, rashes, coughs etc. In fact, antibiotics are useless against most of these infections because they are caused by viruses and antibiotics just don’t work on viruses. Antibiotics are powerful drugs that that can help us to survive a dangerous bacterial infection by killing the bacteria that make us sick.
But using antibiotics comes with a cost. The cost is side e ects as they also kill o a lot of our good bacteria. This means that other less friendly bacteria and fungi can get a foothold and grow. This is why antibiotics can cause diarrhoea and thrush. Antibiotics can also interact with other drugs and can cause skin rashes and some of them upset the rhythm of the heart and brain. When we really need an antibiotic we have to accept the side e ects risk but taking antibiotics we don't need is likely to do us more harm than good. Never share leftover antibiotics or take them without medical supervision.
Antibiotics are a precious resource. There are only a fairly small number of antibiotics so if we don't want to run out of antibiotics that we can use then they must be managed sustainably. It’s in all our best interests to protect antibiotics. Over-use prescribing and incorrect use of antibiotics is taking a toll on their e ectiveness. Already, every year some people’s lives are shortened from bacteria that are resistant to antibiotics and people are dying before they need to because the antibiotics we have don’t work.
HEALTH MATTERS SPRING 2023 66 |
Cancer
e-learning
New reducing cancer risk e-learning programme launched
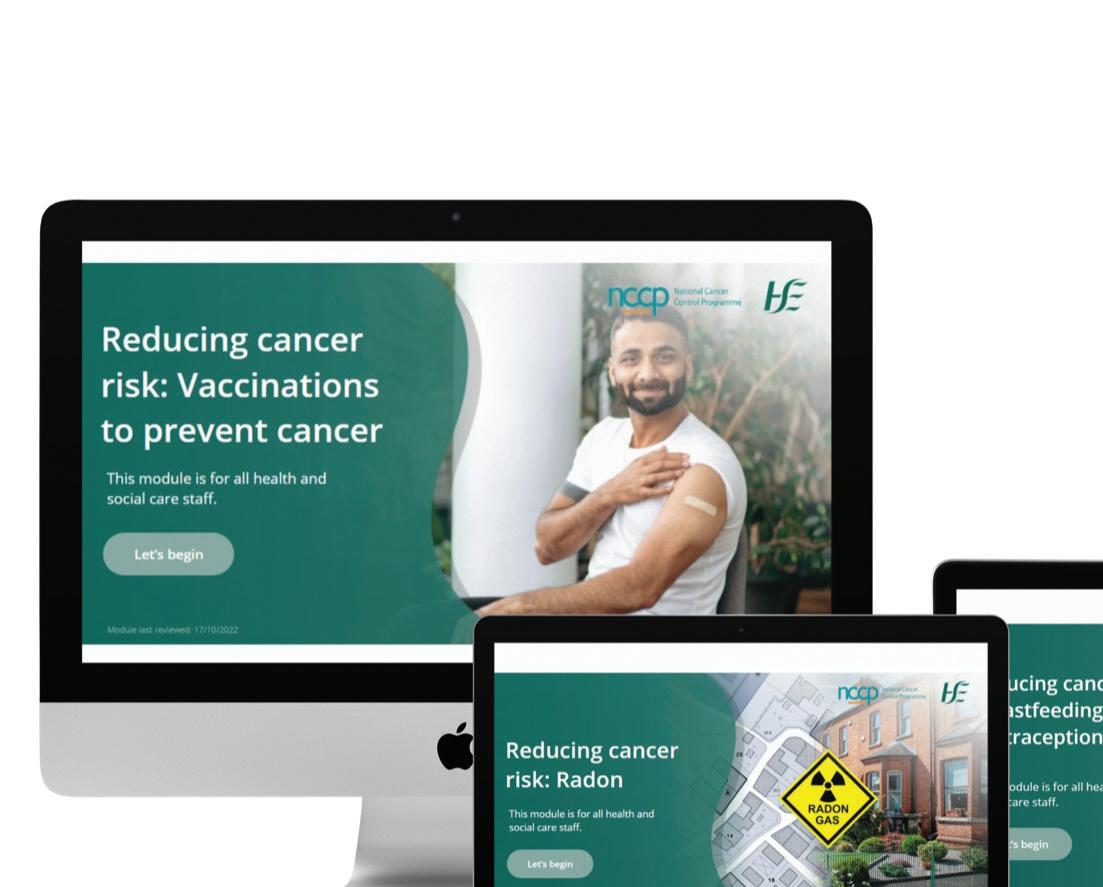
The National Cancer Control Programme (NCCP) has launched a new eLearning programme on reducing cancer risk. This programme for health and social care professionals aims to develop knowledge and understanding of modifiable cancer risk factors.

The programme consists of 11 short modules on the things we can change to reduce our cancer risk - otherwise known as 'modifiable cancer risk factors.' Modifiable cancer risk factors include tobacco smoking, alcohol consumption, physical activity, healthy eating and protecting our skin from the sun.
The 11 modules are available on HSeLanD and cover: smoking tobacco, alcohol, skin protection, body weight, eating for health, physical activity, radon, screening, breastfeeding, oral contraceptive pill and HRT, vaccines and workplace carcinogens.
Each module will take 10 – 15 minutes to complete and include assessments and additional resources to ‘extend your learning’.
Each module covers:
• How the modifiable risk factor a ects cancer risk
• Which cancers are related to the risk factor
• Cancer risk reduction advice
• Signposts to resources and further trusted sources of information, for both you and the people you support
Learners can dip in and out of the programme at any time. You can find it by searching for ‘reducing cancer risk’ in the search box on HSeLanD or by accessing it through the NCCP course catalogue. The new eLearning programme has been led by the NCCP team with support from subject matter experts from HSE clinical teams and has been designed and developed in collaboration with the HSeLanD team.
Dr Triona McCarthy, Consultant in Public Health Medicine, HSE NCCP said, "The reducing cancer risk e-learning programme arms health and social care professionals with invaluable knowledge and resources, on how we can reduce cancer incidence. This is the first online programme of its kind in Ireland. The programme aims to increase knowledge and understanding of these risk reduction behaviours in an Irish context, empowering learners to signpost service users to the supports available and to engage in cancer risk reduction behaviours."
NEW GUIDE ON DATA PROTECTION IMPACT ASSESSMENTS FOR INDIVIDUAL HEALTH IDENTIFIERS
The HSE has published a new guide on Data Protection Impact Assessments (DPIAs) for the Individual Health Identifier (IHI).
The continued national roll-out for the IHI brings benefits for service users, health care providers and social care providers, including
• Ensuring accuracy of data
• Scalability of ICT systems
• E iciency of administration and service provision



• Enabling eHealth applications

• Privacy of patient personal data
• Preparedness for future emergencies e.g. another pandemic, supporting refugees
The document which is now available on the HSE website is a summary of several DPIAs that the HSE has
commenced and concluded in relation to the IHI.
The IHI is a key enabler for many of the objectives of the eHealth Strategy, the Sláintecare Implementation Strategy and Action Plan 2021-2023 and HSE Corporate Plan.
Read more at: www.hse.ie/eng/about/ who/national-services/individualhealth-identifier/
| 67 HEALTH MATTERS SPRING 2023
Visit www.hseland.ie and search for ‘Reducing Cancer Risk’ to access the modules.
First in Ireland
Endoscopic Radial Harvest at UHG
University Hospital Galway is the first hospital in the country to introduce a new minimally invasive surgery for coronary artery bypass grafting.

The endoscopic radial harvest programme reduces significantly the risk of complications and infection for the patient.
The procedure was carried out for the first time in Ireland by Dr Sadiq Siddiqui as part of the minimal access surgery programme in the Department of Cardiothoracic Surgery, University Hospital Galway.
Dr Siddiqui is an integral member of the surgical team led by Consultant Cardiothoracic Surgeons; Mr Fabio Bartolozzi, Mr Ronan Kelly and, Mr Alan Soo.
Traditionally in coronary artery bypass grafting (CABG) operations, a number of arteries and veins are removed from their natural position and used as conduits to bring blood to the narrow or blocked coronary arteries on the surface of a patient’s heart.
The standard surgery leaves large scars on the patient’s legs and forearms that are often slow to heal and can be disfiguring. This new endoscopic approach leaves two tiny scars on the forearm in place of a foot long scar along the whole arm. These heal quicker and with less pain.
“The radial artery from the forearm has been shown to be a longer lasting and superior vessel to use in Coronary Artery Surgery operations particularly in younger patients,” said Dr Siddiqui.
After performing over 400 endoscopic saphenous vein harvests (EVH) in Galway as part of coronary artery bypass operations, Dr Siddiqui travelled to the Royal Brompton National Heart Hospital in London to further his training in endoscopic surgery. There he trained in this new technique to also harvest the radial artery from the left forearm.
“We are very grateful to the Royal Brompton Hospital for the assistance and expertise,” he added.
Prof Pat Nash, Chief Clinical Director with the Saolta University Hospital Group added: “The Endoscopic Radial Artery (ERAH) programme will further advance the burgeoning minimally invasive cardiac surgery programme in Galway and improve the care of patient’s undergoing coronary artery surgery in Galway by reducing their risk of complications and infections.”
Chris Kane, hospital manager at GUH congratulated the team describing the innovating procedure as an important step in enhancing patient care.
“This healthcare innovation will greatly improve our patient’s care. Introducing new techniques and procedures is an important part of our role as a teaching hospital and I am delighted to see such progressive surgeries take place here,” she added.
HAVE YOUR SAY
Would you like to have a say in HSE campaigns? The HSE Communications division would like to invite frontline healthcare workers to share their views on future campaigns through an online research platform. To date, healthcare workers’ views have been vital in informing public messaging for the Covid-19 #ForUsAll campaign, Flu and Winter vaccine adverts and many more. Participation is online, often through a short (approx. 10-15 minute long) survey or discussion forum. You can take part at a time that suits you, usually within a week long window.
If you think you’d be interested in forming part of the community of healthcare workers that help shape and strengthen HSE campaigns, please contact campaign.research@hse.ie
Please contact campaign.research@hse.ie for a link to the survey.
HEALTH MATTERS SPRING 2023 68 | |
Endoscopic Radial harvest 1: The surgical team for the first endoscopic radial harvest surgery for coronary artery bypass grafting in Ireland at University Hospital Galway. From left: Mr Alan Soo, Consultant Cardiothoracic Surgeon; Dr Sadiq Siddiqui, Cardiothoracic Surgery Registrar and Mr Ronan Kelly, Consultant Cardiothoracic Surgeon. Missing from the photo Mr Fabio Bartolozzi, Consultant Cardiothoracic Surgeon.
eHealth Migration
Digital migration programme a key building block for future HSE programmes
The HealthIRL Migration programme, initially established in 2017 as the ONE programme, is of strategic importance for the HSE in terms of digital transformation and enhanced cyber security. HealthIRL is a foundational building block for many other planned programmes of work across the HSE.
The purpose of the HealthIRL Migration Programme is to migrate all users, devices and mailboxes from the regional based domains to a central shared domain (database), called HealthIRL. This gives the HSE a single central view of the eight legacy regional domains, which were aligned with the old Health Board regions. HealthIRL is a critical enabler in terms of ability to use cloud systems.
From an organisational point of view, the HealthIRL programme offers key benefits in terms of best practice identity management, resiliency and security, and is a key recommendation of the PWC report, following the HSE cyber-attack.
The HealthIRL domain is the largest database of users in the organisation and represents HSE staff (partners/ vendors) from every division of the HSE. As the programme is re-establishing, we would like to target users for migration in an efficient, effective method, while ensuring business communications are not interrupted and the migrations are delivered in a business-logical manner.
In order to do this, we have established a number of workstreams, such as Acute Hospitals Self-Managed, and Building by Building approach with the CHOs. A pilot site was chosen for each workstream, University Hospital Galway and CHO3 respectively.
This is not easy - we need to be in this together. This is unpicking 30 years of legacy across regional areas, it is not easy for anyone. It is technically challenging and may reveal issues which are unique to your area as we move across the country. We will commit to addressing these issues promptly and supporting you and your teams through the migration. What we need from you and your teams is to give the migration priority as the key enabler it is.
HEALTHIRL MIGRATION USER BENEFITS
Once on HealthIRL, users will be able to:
• Avail of the enhanced communications and collaboration platform, which includes Microsoft Teams, Microsoft Planner, Sharepoint and Office 365.
• Avail of a single mail platform, with the ability to apply for Exchange Online.
• Locate any HSE staff member in one single email directory.
• Share calendars with national colleagues across all locations.
• Login from any location, on any HSE device.
• Relocate between HSE regions, whilst keeping the same identity.
• Access national applications and shared folders from any location.
• Reset expired/forgotten passwords at any time with Self-Service.
• A more connected and standardised user experience.
ACUTE PILOT SITE
As the pilot site, UHG have been delivering HealthIRL migrations to their users for a number of months, through the Acute Hospitals Self-Managed workstream. UHG ICT, HealthIRL Migration team and Technology Office have worked closely to support the migrations in UHG. As the pilot site, there were several issues identified at the beginning of the process, which, as per our commitment above, have been worked through to resolution.
Over 100 acute users in UHG have been migrated to date and the team in UHG plan to ramp up migrations shortly. There
are a number of other hospitals planning to adopt this self-service model in 2022, including Wexford General Hospital, University Hospital Kerry, University Hospital Group Limerick and Tipperary University Hospital. Other hospitals are in the early engagement phase and preparing to line up to begin HealthIRL Migrations in 2023.
CHO BUILDING BY BUILDING PILOT SITE
As the pilot site, CHO3 Digital and ICT team have been working closely with the HealthIRL Migration team to help plan, schedule and manage migrations in their area. These teams have been instrumental in this area, providing the HealthIRL team with user listings, communicating with the users and being the key liaison point between the HealthIRL programme and the CHO3 users for migration.
We are also engaged in migrations with the other CHO Digital and ICT teams, and hope to expand in all CHO areas in the near future.
FUTURE MIGRATION PROJECTS
The HealthIRL programme is a programme of collaboration, requiring close partnership working across many areas of the organisation. We have established close working relationships with many of the Digital and ICT CHO Leads, Hospital ICT and Senior Management teams, eHealth Directors and other eHealth Departments, such as National Service Desk, Regional Operations, Device Refresh Programme, Office365 and Tech Office.
But most importantly it needs YOU – all of us in the HSE have a responsibility to commit to and support HealthIRL – it is the future of our digital strategy.
The HealthIRL Migration programme can be contacted on - healthirl. migration@hse.ie
We welcome all communications from sites in relation to joining any of our active workstreams for HealthIRL Migration.
| 69 HEALTH MATTERS SPRING2023
HSE Capital and Estates

Supporting better delivery of healthcare services
The HSE is the largest property owner in the State, so staying on top of all our facilities is key to the smooth functioning of our entire health system. HSE Capital and Estates manage the healthcare estate and is committed to creating a high quality physical environment that will enhance wellness for patients, service users and staff wellbeing.

With a property portfolio which includes acute hospitals, primary care centres, community nursing homes, civil registry offices, office accommodation, laboratories and warehouses, Capital and Estates are central to ensuring that appropriate infrastructure is in place when and where required.
The programme of work for HSE Capital and Estates is both dynamic and multifaceted. It ranges from Capital Projects, Maintenance and Technical Support, Equipping, Health and Safety, Fire Safety and Sustainability. A new National Estates Information System (NEIS) is currently being introduced enabling better data, better decisions and better outcomes which is aligned with the Sláintecare vision.
During 2022, the HSE Capital and Estates team oversaw approximately 400 projects, each with a total individual project cost in excess of €500k. A similar profile of work is anticipated for 2023.

National Director of HSE Capital and Estates Paul de Freine said, “I want to take this opportunity to sincerely thank and acknowledge the work of all Capital and Estates staff. Our teams around the country are committed to progressing a programme of work to support better delivery of healthcare services to the entire population. I am delighted to say that capital expenditure in 2022 exceeded €1bn., which is both an acknowledgement of the need that exists and a vote of confidence in the Capital and Estates team to deliver. It is a milestone moment for healthcare investment, one that I hope we can build on into the future.” In this edition we showcase some of the major milestones and remarkable developments by HSE Capital and Estates in 2022.
HEATHER HOUSE COMMUNITY NURSING UNIT
Heather House Community Nursing Unit (CNU) is a HIQAregistered, purpose-built Older Persons Residential healthcare facility located on the grounds of St Mary’s Health Campus in Cork city. Heather House provides 24-hour nursing care to both male and female residents whose dependency ranges from low to maximum, as well as offering palliative care.
In November 2020 the HSE engaged in a plan to deliver an extension to the current unit and increase capacity by an extra 60 beds, thus increasing the facility’s accommodation to a total of 110 beds. The delivery of these additional beds will allow the HSE to respond to the considerable demand for older persons’

HEALTH MATTERS SPRING 2023 70 |
An aerial view of Heather House CNU in Cork city.
One of the new rooms in Heather House CNU in Cork.
An Taoiseach Micheál Martin at the opening of Heather House.
NEW INTENSIVE CARE UNIT FOR TALLAGHT UNIVERSITY HOSPITAL
The new 12-bed ICU facility at Tallaght University Hospital (TUH) was completed in August 2022. The opening of the new unit enabled a decant of existing ICU services which facilitated a renovation of the existing nine-bed unit and brings Critical Care capacity up to 21 beds.
All 12 new single occupancy rooms were designed to the latest health building notes (HBN) and health technical memoranda (HTM) standards, all with full visibility from the centrally located nurse’s station through a double set of automatic interlinked hermetic glass sliding doors. Bedrooms were also visually connected to each other through a series of large internal screens with interstitial blind controls in each room.
Staff offices, family rooms, changing areas, large bulk storage, training facilities and conference rooms were included to both aid and support the staff so that they could deliver more effective care for the patient.
The project design incorporated HSE’s energy efficient design process with a focus on fabric-first design and incorporation of a natural ventilation strategy where possible. Photovoltaic panels were also utilised in conjunction with high efficiency condensing gas boilers. The overall energy improvement for the building was determined to achieve a reduction of 53% below national benchmark, which equates to an A3 BER rating.
NATIONAL CERVICAL SCREENING LABORATORY AT THE COOMBE HOSPITAL
The new National Cervical Screening Lab at the Coombe Hospital was completed in 2022 and is now operational. The facility was designed as a National Centre of Excellence for Cervical Screening Services with design capacity to process the full national workload of up to 300,000 specimen tests per annum.
long-term accommodation in Cork. Despite the many challenges associated with the pandemic, this substantial extension was completed in just over 18 months.
The unit was designed with social distancing and Infection prevention and control needs in mind. It also boasts single occupancy rooms with en suite facilities, spacious shared areas for recreational and dining purposes, designated space for therapies, as well as safe and inviting outdoor spaces.
Communal space includes day rooms, dining rooms, activities rooms, quiet rooms, a prayer room, visitor’s rooms and access to internal courtyards.


The design incorporates Lean Sigma principles to streamline the flow of samples through the lab and optimise the space utilisation on a tight site footprint. Site challenges included the limitations and congestion at the Coombe Hospital and construction in a very tight corner of the site. This was overcome through the support of Dublin City Council for the project and the establishment of a Licence agreement to permit access to their lands adjacent to the campus during the construction phase.
The project design incorporated HSE’s energy efficient design process with a focus on fabric-first design, incorporation of a natural ventilation strategy achieving a BER A3 rating.

| 71 HEALTH MATTERS SPRING2023
The new 12-bed ICU facility at Tallaght University Hospital (TUH).
The new National Cervical Cancer Screening Lab at the Coombe Hospital.
THE NATIONAL FORENSIC MENTAL HEALTH SERVICE (NFMHS) PROJECT, ST ITA’S, PORTRANE
The new National Forensic Mental Health Service Hospital replaces the Central Mental Hospital Dundrumwhich dates back to 1850 - with a new national centre for the provision of modern forensic mental health services. The hospital will provide psychiatric treatment in conditions of high and medium security, including acute, medium and longer term psychiatric care. It has been designed in accordance with model of care and recommendations outlined in the Department of Health and Children’s 2006 report ‘A Vision for Change’ and it meets all modern healthcare standards for the provision of acute mental health services. The new hospital has also achieved a BREEAM “Excellent” environmental and sustainability rating.
The overall campus accommodates 170 patients in single en-suite in-patient bedrooms comprised of 130 secure beds in the National Forensic Mental Health Service Hospital, co-located with an adjacent but separate 10-bedroom Forensic Child and Adolescent Mental Health Unit (CAMHS), and a 30-bedroom Forensic Intensive Care Rehabilitation Unit (ICRU).



The new hospital is patientfocused, designed to provide a safe, secure, and healing environment that contributes to a patient’s recovery. Interior features include subtle measures to reduce noise and resulting stress, by discrete integration of out-of-reach acoustic panels, and the elimination of opportunities for self-harm by careful selection of materials, fittings and fixtures. Variety in spatial character, brightness, colour, and scale make the spaces visually stimulating while set in a secure internal environment.
NEW PRIMARY CARE CENTRES
Primary care is an integral component of Sláintecare, and this is reflected in the 2023 HSE National Service Plan. HSE Capital and Estates delivered an incredible 18 Primary Care Centres in 2022 - three were funded through the HSE Capital Plan and 15 were delivered via the HSE Primary Care Centre Operational Lease model. These new centres are an important development for health service delivery within local communities and provide general practitioner services, public health nursing, speech and language therapy, physiotherapy, occupational therapy, audiology, dental, ophthalmology, dietetics, social work and psychology counselling services.
In addition to these services, primary care centres also provide accommodation for community diagnostic services, community mental health services, disability services, ambulance rapid deployment points and Tusla services.
HSE Capital and Estates are currently managing the construction of 14 Primary Care Centres which are due to become operational in 2023 and 2024 with a further 80 centres being planned for development, the majority of which are being delivered via the HSE’s Primary Care Centre Operational Lease mechanism.

HEALTH MATTERS SPRING 2023 72 |
|
Arklow Primary Care Centre.
Carrickmacross Primary Care Centre.
Primary Care Centre, Ferrybank, Co. Wexford.
INTEGRATED PROCUREMENT APPROACH FOR HEALTH WITH SECTION 38 AND 39 AGENCIES
The HSE Corporate Procurement Plan 2022-2024 signals the importance of an integrated procurement approach for the health sector. This was a central theme at a recent HSE Procurement Information Session for Section 38 and Section 39 Agencies. The event, which took place at Cherry Orchard Hospital, welcomed representation from a selection of healthcare agencies.
National Director of HSE Procurement John Swords welcomed the audience by saying, “It is important to emphasise that this collaboration is significant for our way of working together. We are all aware that procurement activities take place within a highly regulated environment and it is critical that procurement spend on goods and services is carried out in a transparent and efficient manner. By working together we take an integrated approach to procurement which supports the patients and service users across the health sector.”
The event was organised and facilitated by Siobhan Dunphy, Assistant National Director of Sourcing and Contracting within HSE Procurement.
“We are the largest purchaser in the State with a Procurement spend of €4 billion approximately and therefore we are accountable for effective and compliant procurement that delivers value for money with security of supply,” she said.
She outlined that a key part of improving efficiency is transforming our ways of working around procurement activities, which incorporates:
• Coordination and collaboration with all HSE organisations to agree a Multi-Annual Procurement Plan (MAPP) aligned to the implementation of the HSE Corporate Procurement Plan. The MAPP refers to the planning of the organisations future procurement requirements.

Spend Under Management (SUM) is spend that is actively managed by procurement and finance professionals across the health sector to optimise compliance.
• Improve SME participation through the HSE MAPP pipeline of upcoming tenders that will be published each Quarter to inform SME’s and Micro Enterprises of upcoming opportunities in advance of tender publication.
• Sustainability: The health service has a significant role to play in achieving Ireland’s climate action obligations. HSE are required to
apply appropriate procurement processes, award criteria and weighting to support innovation, social inclusion, economic and environmental sustainability priorities into all procurement processes.
A further insight into the procurement operating model included an overview of Logistics and Inventory Management and Corporate Procurement Planning and Compliance Improvement.
HSE Procurement were delighted to welcome Kevin Cleary, Assistant National Director of the HSE Compliance Unit, who spoke about the compliance environment and on the importance of increasing the level of procurement compliance to help the HSE meet its obligations in terms of accountability. Continuing with the theme of collaboration, guest speakers from the Office of Government Procurement (OGP) presented on the common categories of products and services which they procure across the public sector.
The afternoon session gave an informative demonstration on the HSE Procurement Portal introducing the Procurement Agreements and Contracts eRepository (PACE) which provides information on HSE / health sector agreements and contracts for goods and services. This was followed by an overview of the HSE Procurement Sourcing and Contracting categories across the Procurement portfolios. The Procurement Assistant Heads outlined their programmes of work across five portfolios of:
1. Medical Professional Services
2. Rapid Response
3. Medical, Surgical & Pharmacy
4. Medical Diagnostics & Equipment
5. Digital Health & Innovation
A lively questions and answers session included positive feedback on the opportunity for the agencies to engage and collaborate on the procurement agenda.
Closing remarks from the National Director of Procurement referred to the strong engagement over the course of the day.
“Service delivery with the patient at the centre of our activities is key to everything. However, we can’t bring real value without ensuring compliance and accountability within our regulatory obligation,” he concluded.
| 73 HEALTH MATTERS SPRING2023
Sean Hoolan, HSE Procurement, Corporate Procurement Planning & Compliance Improvement John Swords, National Director of HSE Procurement
Siobhan Dunphy, Assistant National Director of Sourcing & Contracting HSE Procurement Francis Mollen, Assistant National Director of Logistics & Inventory Management HSE Procurement Miriam Rourke, Business Relationship Manager, HSE Procurement, Corporate Procurement Planning & Compliance Improvement
Single Financial Management System
Bringing complete business transformation to the HSE
IFMS, the Single National Integrated Finance Management and Procurement System for the entire health sector, will replace multiple legacy finance and procurement systems across the HSE, Tusla, Section 38 organisations, and larger Section 39 organisations.
Many of these legacy systems are outdated, or no longer supported, and are not fit for purpose. The number, variety and age of legacy systems makes it very di cult to gather, analyse and compare financial and procurement information in an e cient, timely and reliable way. The industry-leading platform on which IFMS
BENEFITS OF IFMS FOR OUR HEALTH SECTOR
IFMS will bring many benefits including:
• Better and more timely financial reporting and forecasting
• Improved financial management, governance, compliance and transparency
• Better overall financial control environment
IFMS will, for the first time, provide quality standardised financial and procurement information across both statutory and a voluntary services, facilitating:
1. Valid comparison of costs across the entire sector
2. A more equitable and evidence-based resource allocation model
3. Demonstration of value for money to support investment in service development
4. Having quality data at a catalogue item
will run is SAP S/4 HANA.
The IFMS project is not just a SAP implementation or technology project - it is a complete business transformation, delivered through standardised national finance and procurement processes and a strengthened financial control framework. It will be underpinned by new operating structures, ways of working, and a shared services delivery model in line with the Government mandate to expand and accelerate the use of shared services in the Irish Public Service, as one of the key crosscutting reform initiatives under the Public Service Reform Programme.

level, leveraging the full procurement capacity of the health sector
5. position-level reporting of pay costs for more than 125k WTE (c. 81k WTE statutory and c. 45k WTE voluntary)
PROJECT UPDATE
The IFMS Project reached a key milestone in October 2022, with the completion of system design validation and review. The Project has now commenced the Build and Test Stage which will run to March 2023.

Implementation activity has now commenced in preparation for Implementation Group 1 (IG1). Go-Live date is July 3rd 2023.



Our Management of Change team will support stakeholders along their journey. A number of activities will be taking place to prepare for implementation. These will be communicated to impacted stakeholders.
Implementation Group 1 (East)
• CHO 6
• CHO 7
• CHO 9
• Connolly Hospital
• Naas General Hospital
• St. Columcille’s Hospital
• St Luke’s Radiation Oncology Network
• HSE Corporate and National Services
• National Capital Income and Payments
• National Distribution Centre
• PCRS
• Tusla
Implementation Group 2 (West)
• CHO 2
• Galway University Hospital
• Mayo University Hospital
• Merlin Park University Hospital
• Portiuncula University Hospital
• Roscommon University Hospital
• St. Michael’s House (S.38)
• Western Care Association (S.39)
Implementation Group 3 (South)
• CHO 4
• CHO 5
• Bantry General Hospital
• Cork University Hospital
• Kilcreene Orthopaedic Hospital
• Mallow General Hospital
• South Tipperary General Hospital
• St. Luke’s General Hospital Kilkenny
• University Hospital Kerry
• University Hospital Waterford
• Wexford General Hospital
Implementation Group 4 (Midwest and North West)
• CHO 1
• CHO 3
• Croom Orthopaedic Hospital
• Ennis General Hospital
• Letterkenny University Hospital
• Nenagh General Hospital
• Sligo University Hospital
• University Hospital Limerick
• University Maternity Hospital Limerick
• S.38 Acute
Implementation Group 5 (Midlands and North East)

• CHO 8
• Cavan General Hospital
• Louth County Hospital
• Midland Regional Hospital, Mullingar
• Midland Regional Hospital, Portlaoise
• Midland Regional Hospital, Tullamore
• Monaghan General Hospital
• Our Lady of Lourdes Hospital
• Our Lady’s Hospital Navan
HEALTH
SPRING 2023 74 |
MATTERS
2022 2025
Throughout February and March, a suite of webinars and launch training will be available with details announced each Thursday, so keep an eye out for the Health Service News email update
The Financial Regulations
National
User-friendly for all
The refreshed National Financial Regulations (NFRs) have now launched with an effective date of January 31st 2023, and are accessible within a new area of the Finance page on the HSE website (www. hse.ie/eng/about/who/finance/nfr/ about-nfrs.html).
In July 2020, the Executive Management Team (EMT) approved a two to three year, single, co-ordinated and structured programme called the Internal Controls Improvement Programme (ICIP). This was designed to drive lasting and continuous improvement in the effectiveness of the system of internal controls across the HSE. Included in this programme was the refresh of the NFRs to ensure they are user-friendly and accessible to all.
Following subject matter expert consultation (which included SME workshops with participants invited from all sectors of the HSE), a revised framework was designed which resulted
in reducing the previous 31 NFRs into 11 The 11 NFRs are structured into four overarching areas:
• A - sets out the HSEs overarching Internal Controls Framework and general control Principles.
• B - a set of seven operational regulations which are aimed at practical audiences to cover such areas as Procurement, Payroll, Travel and Subs, Cash handling and so forth.
• C - a set of two HSE custodian regulations which include Patient Private Property and Community Residence Finances.
• D - a document with an AFS financial reporting focus.
User-friendly features include:
• Helpful icons to assist the reader
• Plain English principles applied where applicable
• Visual aids to present complex processes
• External links - Links to other HSE policies and external content
• Internal links - Easily move within and between the NFRs
In addition to the development work on the NFRs, some new related resources have been created which include:
• Introduction video - To provide helpful tips when accessing the NFRs
• Frequently Asked Questions (FAQs) - To answer commonly raised questions
• Key controls checklist - To highlight key controls
• Change Management Form - To allow you to suggest updates
• YouTube Channel - To provide training materials
We would like to thank everyone who assisted in the completion of this piece of work. The refreshed NFRs would not have been possible without collaboration from across the HSE and with our external partners, KPMG. We hope the updated content is helpful and informative. Any queries can be made to govn.compliance@hse.ie
| 75 HEALTH MATTERS SPRING2023
Garden project
Service users help to landscape Le Brun and Whitehorn House gardens
Positive outcomes for Horticulture Therapy pilot project


A four-week Horticulture Therapy Project was recently piloted in HSE Community Healthcare East across five di erent sites - Dalkey Community Unit, St Colman’s Residential Care Centre, Clonskeagh Community Nursing Unit, SSID-Hawthorne House and Old Age Psychiatry, Carew House, St Vincent’s University Hospital.

The programme began in September 2022 and was run by Fiona Brauneisen, Health Promotion and Improvement O icer, and Horticulture Therapist Marie Hirsch.

Residents of two in-patient mental health units in Co Dublin now have the use of renovated garden spaces, giving them a therapeutic open space with paths and green areas.

Le Brun House and Whitehorn House are located within the grounds of Clonskeagh Hospital, South Dublin and provide in-patient Mental Health services in HSE Community Healthcare East. Both units were built in the late 1980s and have enclosed courtyard garden spaces that were in need of upgrade.
In 2020, a Garden Committee was formed in both units which included a full multidisciplinary team and resident representation. The group agreed to fund a designer to help create a Dementia and wheelchair friendly garden that would be a therapeutic space to suit all residents’ needs.
Designs were agreed and work commenced on both gardens in August 2022. While at times the work was disruptive, the residents commented that they enjoyed watching and monitoring the progress of the gardens. Both gardens were completed to the agreed design in November 2022.
The garden paths are wide enough for two people and provide
resting and sitting areas for people with limited mobility. The pergola and other shaded areas o er shelter from the sun, rain and wind. The residents can enjoy familiar activities such as digging and planting as the garden provides them with a raised planting area.
For people with dementia who walk a lot, time spent in the garden o ers sensory stimulation and can help them feel calm and relaxed. As the garden o ers a safe and wheelchair friendly environment, it is a calming area accessible to all residents all through the year.
The feedback from residents of Le Bren and Whitehorn House has been fantastic:


“The view of the garden is di erent from di erent windows, I enjoy looking out at night when the lights are on in the planted area.”
“I feel like we are in a hotel as it looks so good.”
“It looks very romantic.”
“I enjoy sitting in the pergola area.”
“I’m looking forward to the summer when we will be able to use the garden more.”
“It’s great that wheelchairs can move freely.”
Thank you to everyone who helped secure funding and supported this project at all stages.
Horticulture Therapy is a therapeutic practice used to improve health and wellbeing through actively caring for plants.
The aim of the programme was to increase the wellbeing of participants across all sites through caring and working with plants. More specifically, the programme sought to increase social inclusion, physical activity and self-care and decrease stress and loneliness amongst service users and residents.
Themes included: Mindful activities to appreciate nature, edible gardening, learning how to propagate plants and creating a planter. After each session there was a ‘take home’ product for each participant which added a sense of ownership and purpose.
An evaluation piece took place in order to review the sustainability of the project. The main impact reported was an increase in social inclusion and wellbeing. One participant noted, “It was nice to do it all together in a group. I love gardening and sowing seeds and this took me back to long summer days in my own garden with my children. The smells, the feel of the leaves, it was just lovely to get to be a part of that again. It provided a lovely sense of calm and peace, I would love to do it again.”
The evaluation, learnings and outcome of the pilot program will help shape and scale for a bigger Horticulture Therapy programme in 2023.
HEALTH MATTERS SPRING 2023 76 | |
Wellness Walkway
A walk towards wellness at Mayo hospital


Anew Wellness Walkway at Mayo University Hospital was launched by Prof Brian Dolan.
The walkway, which is located on the first floor of the hospital, aims to promote the health and wellbeing of patients during their recovery from illness and injury. The walkway is 130m long with exercise stations and seated areas to allow patients to get away from the busy ward environment.
Caitriona Davey, Clinical Nurse Manager 3 and Wellness Walkway Project Team member, said, “We have designed the walkway to support patients to remain active during their hospital stay and we have exercise stations designed by physiotherapists at intervals along the walk with wall panels illustrating different lower and upper body exercises.
“We know from research how important it is for patients to stay mobile while in hospital. We have implemented the national ‘Get Up, Get Dressed, Get Moving’ campaign in the hospital and to complement this, the new Wellness Walkway provides a protected space for patients to keep moving to prevent loss of muscle, strength and fitness.
“The walkway also has a continuous handrail to improve the experience for those who might need support when walking. Around the seated areas we have added 15 large scale photographs of iconic locations in Mayo, including Achill Island, Blacksod Lighthouse, Lough
Lannagh and Tourmakeady Waterfall, where patients can sit alone or in the company of others to help reduce anxiety associated with a hospital stay.
“Along the route the signage, clocks and furniture were selected in line with ‘Dementia Friendly Hospitals Universal Design Approach’ principles to provide patients with symptoms of dementia and their families/carers with a designated and stimulating space outside of the ward.”
Catherine Donohoe, Hospital Manager said, “We were delighted to welcome Prof Brian Dolan OBE to the hospital to launch our Wellness Walkway. Prof Dolan, who is originally from County Mayo, created the NHS campaign ‘End PJ Paralysis’ which has been adapted by hospitals around the world, including here in Ireland as ‘Get Up, Get Dressed, Get Moving’. It is extremely fitting that Prof Dolan joined us to launch an initiative which provides a designated space for patients to keep active, reduce muscle deconditioning and support cognitive function and social interaction.
“A huge amount of planning went into creating the walkway to help enhance our patients’ hospital experience and to maintain their physical and mental wellbeing. We are extremely grateful for the valuable input from one of our patient experience advisors who was able to provide a lived experience of a hospital stay and insight into patients’ needs, as part of the design process.”
| 77 HEALTH MATTERS SPRING2023
From left: Prof Brian Dolan; Catherine Donoghue, Hospital Manager; Padraig O’Luanaigh, Director of Nursing; John McCormack, Patient Experience Advisor; and Caitriona Davey, Clinical Nurse Manager 3 Medical Division.
Right: The Wellness Walkway Project Team, from left: Grace Mullaney, Physiotherapist; Sarah Ronayne, Occupational Therapist; Mary Conlon, Clinical Nurse Manager 2 B Ward; John McCormack, Patient Experience Advisor; Caitriona Davey, Clinical Nurse Manager 3 Medical Division; Aisling Bell, Physiotherapist; and Laura Walsh, Occupational Therapist.
Enjoy the sun safely Be SunSmart
For more information visit www.hse.ie/ sunsmart, contact prevention@ cancercontrol.ie or #SunSmart on social media.
The first national Skin Cancer Prevention Plan 2019-2022 was a landmark commitment which arose from the National Cancer Strategy 2017-2026. The plan set out to develop and implement evidence-based strategies to increase awareness and adoption of skin cancer prevention behaviours and required extensive cross-sectoral collaboration. Skin cancer prevention is a long-term goal, however, and preventative measures need to be taken from childhood through to advanced age in order to prevent skin cancer occurrence. As a result, there is a continued commitment to reducing the burden of skin cancer in Ireland with the new Skin Cancer Prevention Plan 2023-2026. To download the plan visit www.hse.ie/sunsmart.
While skin cancer is the most commonly diagnosed cancer in Ireland, accounting for almost 13,000 cases annually, most cases are preventable. The number of people being diagnosed with skin cancer in Ireland is also rising and the National Cancer Registry of Ireland (NCRI) expects this number to double between 2015 to 2045. Risk of skin cancer can be reduced by avoiding overexposure to ultraviolet radiation (UV) from sunlight or artificial sources such as sunbeds.
The new plan addresses awareness of skin cancer risk reduction measures, with particular consideration to the priority groups of children, adolescents and young adults, outdoor workers, sport, recreation and tourism, and sunbed users.

The SunSmart campaign is a key initiative that is continuing. This runs annually with the HSE’s National Cancer Control Programme (NCCP), in collaboration with Healthy Ireland and cross-sectoral partners. The SunSmart campaign aims to get us into the habit of protecting our skin everyday using a range of SunSmart behaviours, whether that’s wearing longsleeved clothes, seeking shade, wearing a hat and sunglasses, or using sunscreen. The campaign runs from April to September and outlines the steps you, your family, friends and colleagues can take to protect your skin from the sun and reduce your risk of skin cancer.
Follow the 5 Ss to keep safe in the sun:
• Slip on clothing that covers your skin, such as long sleeves or collared t-shirts
As well as the 5 Ss it is important to remember:
In Ireland, the UV radiation levels from the sun are highest from April to September, even when it is cloudy. Stay safe by limiting time in the sun when UV is strongest, typically between the hours of 11am and 3pm
• Do not deliberately try to get a suntan
• Avoid getting a sunburn
• Never use a sunbed
• Slop on broad spectrum (UVA/UVB) sunscreen on exposed areas, using factor 30+ for adults and 50+ for children. Reapply regularly. No sunscreen can provide 100% protection, it should be used alongside other protective measures such as clothing and shade
• Slap on a wide-brimmed hat
• Seek shade - especially if outdoors between 11am and 3pm - and always use a sunshade on a child’s buggy
• Slide on sunglasses to protect your eyes.
HEALTH MATTERS SPRING 2023 78 |
The HSE National Cancer Control Programme and Healthy Ireland have launched the new Skin Cancer Prevention Plan 2023-2026.
While skin cancer is the most commonly diagnosed cancer in Ireland, accounting for almost 13,000 cases annually, most cases are preventable
Happy Hearts
Newcomers at Lourdes Hospital take gold on first attempt
Healthy changes to the menu at Our Lady of Lourdes Hospital in Drogheda has earned the catering team lots of positive feedback- as well as a Gold Award at the Happy Heart Healthy Eating Awards.
The annual awards, organised by the HSE and Irish Heart Foundation, saw 30 healthcare sites that provide meals for over 27,000 HSE employees honoured for their commitment to providing healthy food choices on their sta and visitor menus.


18 facilities achieved gold status for their commitment to creating a healthier food environment for sta and visitors. This is a record number since the HSE and Irish Heart Foundation partnered for the awards in 2020. Eight sites received silver and four were bronze winners. A special recognition was give to seven sites new to the Awards in 2022.
The Lourdes Hospital, one of these new sites, certified at the highest standard - a Gold Award, a fantastic achievement for new entrants.
Sharon Gallagher Catering Manager, was thrilled. “We discussed the awards with the team here and the standards required for each. We were all of the same belief that we should aim high because healthy eating within a healthcare setting is important for the wellbeing of patients and sta alike, so we aimed for the Gold Award.
“We also felt that any positive changes made to our menu would automatically carry through to patient services. The team brought some good ideas to the menu and tried out new recipes and this was a great boost to sta morale. We received a lot of positive feedback from our cafeteria users, which made it all worthwhile. In the end, the biggest obstacle we faced was reducing the number of days that chips were available, which when looking back wasn’t that bad of an obstacle.”
Professor Donal O’Shea, HSE National Clinical Lead for Obesity, spoke on the awards night.

“Our sta in the HSE are our most valuable resource – supporting


their health and wellbeing in the workplace is a key priority for Healthy Ireland in the health services. Creating a healthier food environment and providing healthier options at mealtimes supports our sta to make the healthy choice the easy choice. The awards recognise the hard work and dedication to quality improvement and health promotion of catering sta across healthcare,” he said.
The Happy Heart Healthy Eating Awards is a partnership between the HSE and the Irish Heart Foundation. The programme coordinated by HSE Healthy Eating Active Living programme aims to support healthcare services to implement the HSE Nutrition Standards for provision of food and beverages to sta and visitors through an Awards programme. Catering facilities in healthcare services are assisted and supported to adopt healthier cooking practices and provide healthier food choices without incurring substantial costs.
Catering services and sta have an important role to play in positively influencing the quality and nutritional content of food and beverages available in health services, making the healthier choice the easier choice for all. The Nutrition Standards support sta involved in the preparation and provision of food to ensure that a range of healthier choices are available every day.
Currently there are 43 certified catering facilities across the health services Facilities involved range from hospitals, to sta canteens in administrative buildings, to older peoples and disability services. Together these 43 sites support the health and wellbeing of over 43,000 sta . The focus in 2023 is to expand the programme across the health services and increase the number of new sites involved and to encourage current cert holders to ensure continuous improvement and quality.
For more information or to sign your catering facility up for the Awards visit: www.hse.ie/healthyeatingatwork or contact HealthyEating.ActiveLiving@hse.ie
| 79 HEALTH MATTERS SPRING 2023
From left: Sharon Gallagher, Catering Manager, and Liz King, Catering O icer, Our Lady of Lourdes Hospital Drogheda, with Tim Collins CEOIHF and Professor Donal O’Shea. The hospital earned the Gold Award.
BELOW: New Silver Award winner Aska Pasek, Catering Supervisor, and Shane Loughlin, Head Chef, representing the National Rehabilitation Hospital.
Christmas The 2022 Concert

Fifth festive concert spreads joy across the health services

The 2022Christmas Concert, hosted by HSE Health and Wellbeing and Healthy Ireland, was the fifth since its initiation in 2018 and the third to be delivered virtually. With COVID having dominated so much of the lives of healthcare workers in recent years, this year’s event illustrated once again how music lifts and transcends, providing joy to all involved.
HSE sta choirs from across the organisation showcased their magnificent talents as they sang a range of traditional Christmas and other well-known songs. It was so encouraging and uplifting to see a number of choirs including service users and members of the community as part of their choral groups in 2022.
Taking part in a sta choir has been shown to have a great impact on health and wellbeing and also o ers sta an opportunity to meet sta from di erent areas of the service. Dr Philip Crowley, National Director for Strategy and Research, noted among other things the impact on hearing and seeing the choirs perform in ‘celebrating the spirit of our workforce’. Dr Crowley reminded us all of the many benefits to singing and more importantly singing within a sta choir.
“Singing is neurologically good for you, it is good for your immune system, your brain health and your mental health and wellbeing. Participation in a choir is great for social interaction, but also hugely beneficial for team building in the workplace,” he said.

Singing brings an overwhelmingly positive response in terms of
physical, social and emotional benefits, which is often then shared when sta choirs perform locally for their colleagues, for charities and for their patients.
A special thanks to the following choirs who performed in the concert and who made it possible: Letterkenny University Hospital Choir; Carlow Melodies Choir; Tullamore Sta Choir; St John’s Choir Limerick; Roscommon Key Notes Choir; Tallaght University Hospital Our Voices Community Choir; St James’ Yes We Can Choir.
Some very special guests also performed during the concert, including Jerry Fish, Niamh Kavanagh and Gerald Peregrine, who have done such amazing work bringing music and joy through the Care Concerts initiative, where over 100,000 people have heard the Care Concerts in the grounds of residential care homes, hospitals, psychiatric/disability services, day care centres and direct provision centres. Jerry and Niamh, accompanied by Gerald and Vincent Lynch, performed a number of Christmas classics in addition to the Eurovision song sung by Niamh, ‘In Your Eyes’.
For those who missed the live virtual event, or for those who just want to watch it again, you can view it on the HSE Health and Wellbeing YouTube channel.
The 2022 HSE Christmas Concert was a virtual event supporting a greener environment. The Carbon Footprint per person watching virtually was estimated at 0.04kg CO2e (Kilograms of Carbon Dioxide equivalent emissions) versus 293kgCO2e/day for an inperson conference event (Source: Integrated Media Solutions 2022).

HEALTH MATTERS SPRING 2023 80 |
Steps to Health
5 week staff challenge 2023
Starts: Monday 8th May
Finishes: Sunday 11th June
Closing date for registration: Wednesday 19th April
• Steps to Health is a walking challenge for our staff and others working in the healthcare field.


• Walking in teams of 2–10 people during the five weeks, you can count your daily steps while trying to increase your physical activity.
• While many will reach 10,000+ steps daily, it is those who start from a low base and make improvements will gain the most from this challenge. So don’t shy from taking part if you aren’t a star walker.
• Steps to Health is a fun way to connect and socialise with colleagues and improves our mental health as well as our physical wellbeing.

• So join in the fun, set up a team and give yourself a name. There will be prizes for the best team names and other competitions.
For more information and to register a team, visit hse.ie/stepschallenge
Make sure you’re protected
The HPV vaccine protects against HPV related cancers including cervical cancer
“When I got my diagnosis I decided that I would do anything to stop this from happening to anyone else.”
If you missed out on the HPV vaccine at school, see if you are eligible to get one now as part of the Laura Brennan catch-up programme on HPV.ie
 Laura Brennan,1994 - 2019
Laura Brennan,1994 - 2019
































































































































































































































































































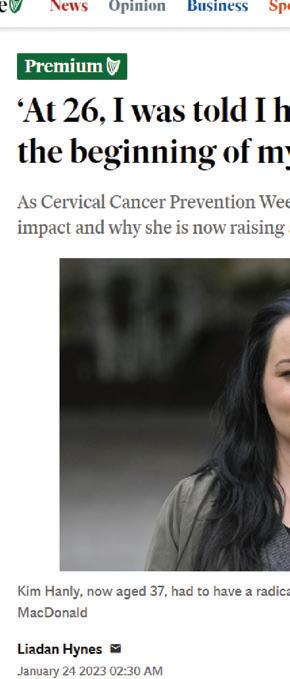




















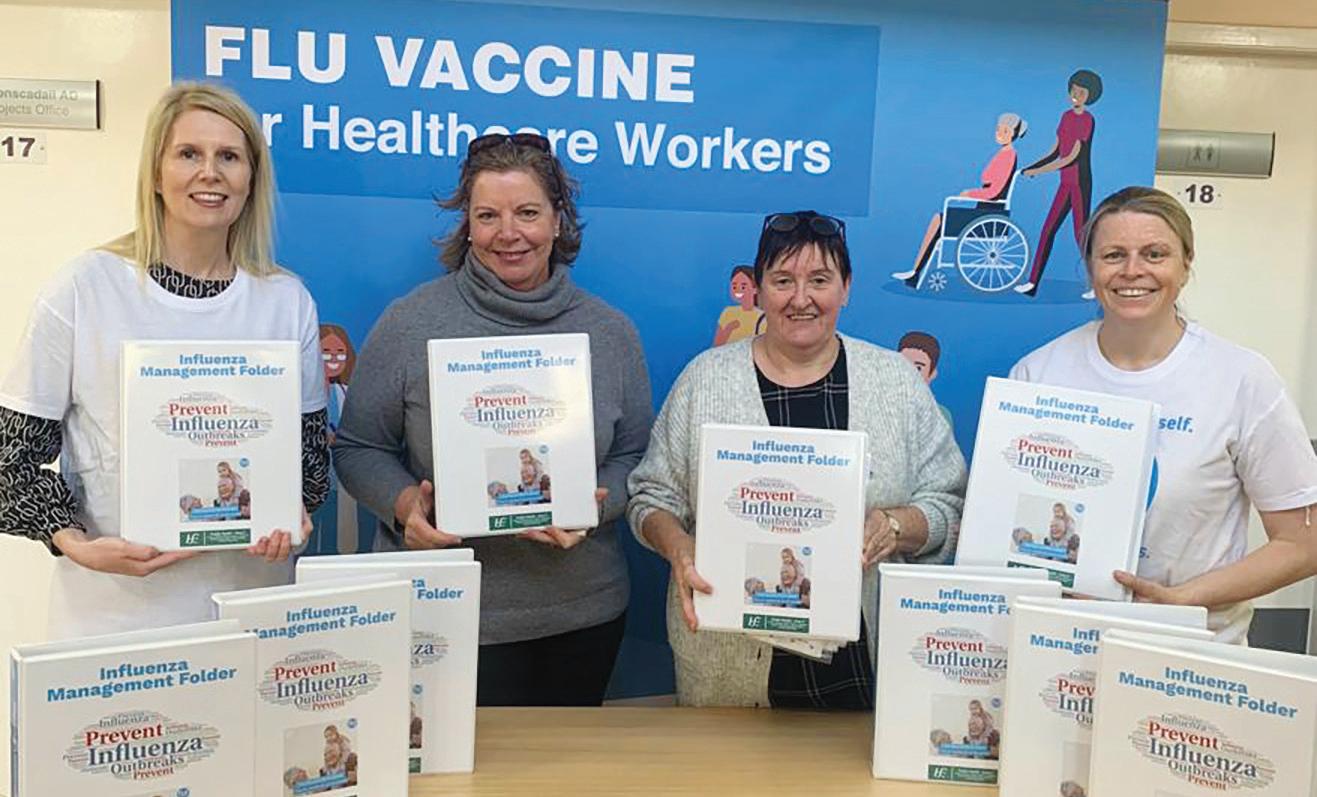














































































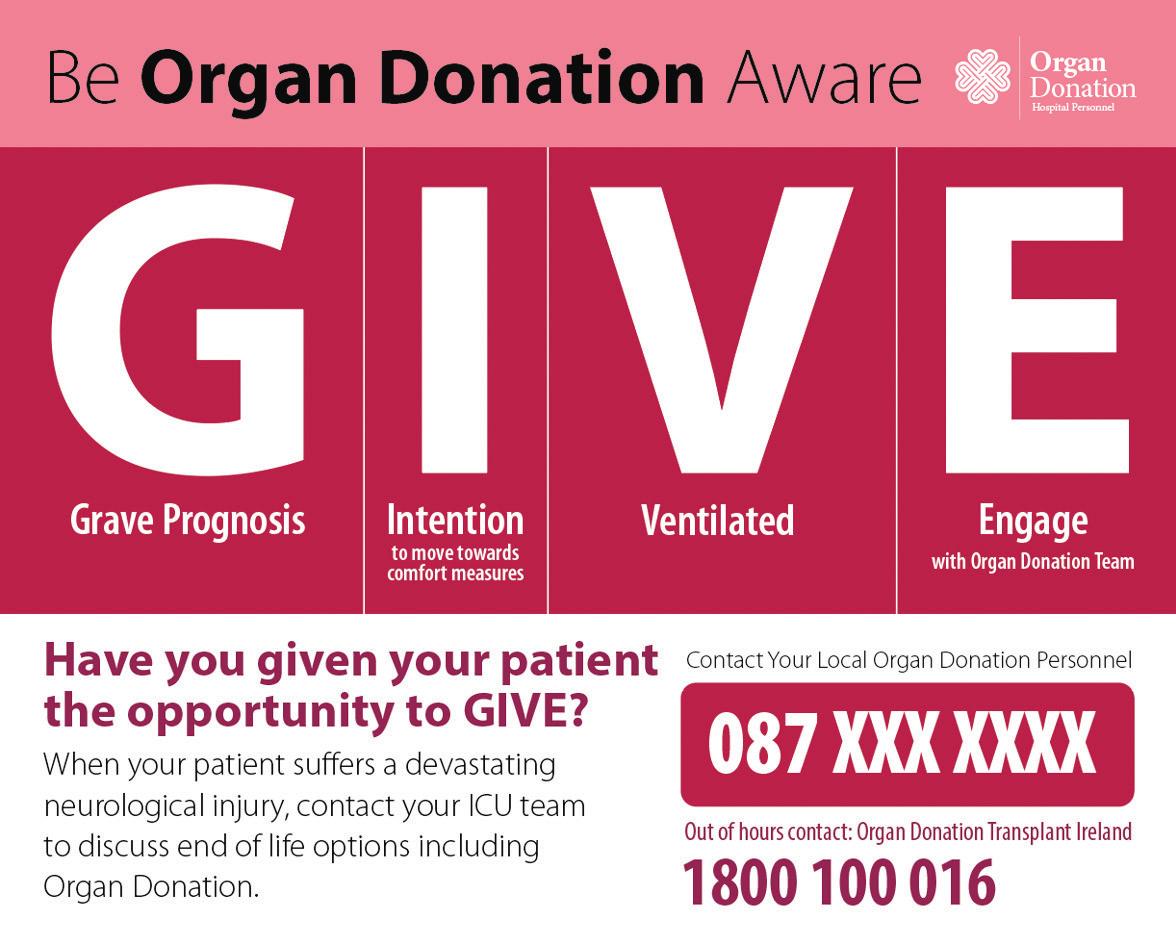





























































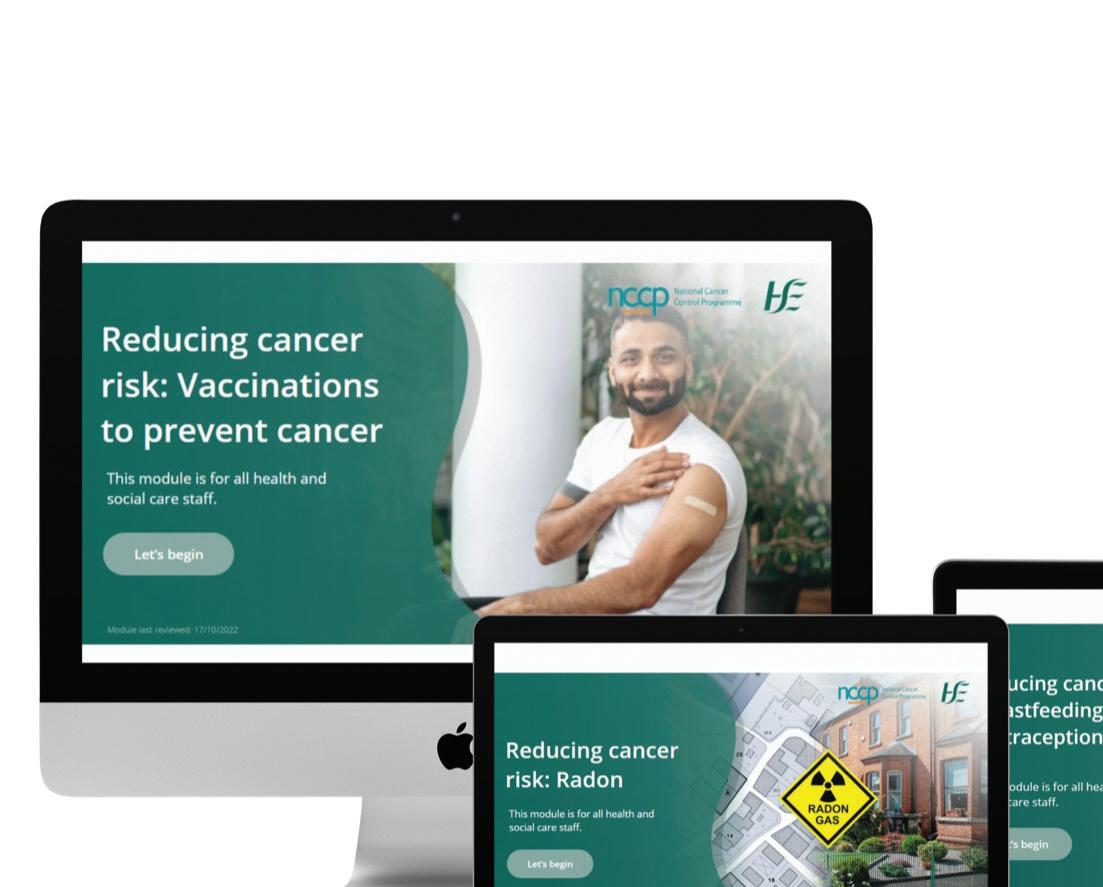














































 Laura Brennan,1994 - 2019
Laura Brennan,1994 - 2019