Summer 2025
SunSmart
Staying safe all year long
Show Your Pride
Celebrating the LGBTQIA+ community
Matters Win


Contents Editor’s Letter

1 Raising autism awareness in the Traveller community
2 How to be SunSmart and sharing that knowledge with patients
4 Spotlight on oral hygiene
5 Exercise PANDORA
6 Spotlight on mental health
8 In focus: Maternity
9 Photobiomodulation for mucositis
10 In focus: BowelScreen
11 Neuro-Mapping Project Phase 2
16 Updates from HSE Dublin and South East
22 Digital for Care
26 Updates from HSE South West
32 New report shows important role of community champions in improving equity in screening
33 Tick awareness
Optimising health service productivity 46 Updates from HSE Dublin and North East 52 Climate action 56 Updates from HSE West and North West
62 Taking Pride 64 National Ambulance Service student shines in All-Ireland competition
65 Competition: Share a snap of Health Matters and be in with a chance of winning a €100 One4all voucher
66 Updates from HSE Dublin and Midlands 72 National Service Plan (NSP) 2025
In other news… Updates, events, awards, celebrations and milestones
Thank you to everyone who has submitted stories for this edition. If you would like to see your initiative or work featured, you can submit your ideas through our online form at bit.ly/HealthMattersForm
Meet the team
Welcome to the summer issue of Health Matters. As we look ahead to long days that stretch well into the evening, we’re reminded of the importance of staying safe under the sun’s rays, whether the skies are bright blue or cloudy and grey.






Turn to page 2, where Evelyn Power, Candidate Advanced Nurse Practitioner in Skin Cancer, Dermatology at University Hospital Limerick shares her advice on how to ensure you and your patients follow the SunSmart code.
Another important issue to carry front of mind during the warmer months is the danger of tick bites. Read up on how to watch out for the signs and what to do if you notice a bullseye rash on page 33. And as we celebrate Pride Month in June, on page 62, we hear from two HSE staff members on why showing support and solidarity with the LGBTQIA+ community is as crucial as ever.
On page 10, Tuam funeral director Joe Grogan shares his first-hand experience of the BowelScreen programme, which is now available to everyone aged 59 to 70. And on page 1, we learn how autism awareness is being raised among the Traveller community.
Elsewhere in this issue, we shine a spotlight on mental health services (page 6), patient safety (page 42), maternity news (page 8), kidney disease (page 13) and oral hygiene (page 4). Plus so much more, from HR supports and Digital for Care news to advancements in treatments and climate action.
We hope you find inspiration throughout this issue and that you’ll share your feedback with us (check out our reader competition on page 65 and learn how you can be in with a chance to win a €100 One4all voucher).
Whether you’re flipping through these pages on your breaktime or taking a copy of Health Matters with you on holidays, we wish you a summer filled with joyful workdays, good health and happiness in all your endeavours.
Meg Walker Editor
Raising autism awareness in the Traveller community
Assistant Primary Health Care Coordinator Mary Collins and Traveller parent Alice McDonnell share their experience
Mary
Collins, Assistant
Primary Health Care Coordinator, TravAct
I have been a Traveller Primary Health Care worker for 25 years and now work as an Assistant Primary Health Care Coordinator in the Coolock area. I work with all the Traveller families in the area.
Many of these families have newborn babies and the team often accompany the public health nurse on their visits if needed. A lot of mothers are afraid to get childhood vaccinations due to misinformation around vaccines causing autism. Social media has played a terrible role in this. We explain that the vaccines are very important and the protection the babies get outweighs everything else. There are great health materials, such as leaflets and videos, developed for Travellers and we use these in our work and signpost families to the Pavee Mothers website.
Having access to information through the Primary Health Care for Travellers Project (PHCTP) means parents often recognise signs of autism in their children, such as not speaking or making eye contact. I often tell parents that every child progresses at a different rate but encourage them to talk to the public health nurse or their GP. The public health nurse can write a letter of concern on behalf of the family if needed. The early intervention team does great work with families and children but unfortunately, like many public health services, the waiting lists are long. There are also other supports we signpost to if the child has already been diagnosed, or if they are older.
I would advise other Traveller community health workers, and other health workers working with Travellers, to encourage families to get childhood vaccines for their children. It is our job to communicate the seriousness of the diseases and debunk the misinformation about the link between autism and vaccines.
Alice McDonnell, Traveller parent
I have two boys, aged 18 and 14. Paddy, my 14-year-old, is autistic. He was fully diagnosed when he was five. Initially, I was upset because I didn’t know what the future held. As Paddy got older, he could do everything; I have no worries about him anymore.
When Paddy was diagnosed, we got a lot of support. His first year in school was difficult because he hadn’t got his diagnosis paperwork. The following year, he came on leaps and bounds because he received support from the school and was in the autism spectrum disorder (ASD) class. Even
in his first three months he made so much progress compared to when he was in Junior Infants and didn’t have support.
I would tell other Traveller parents with an autistic child, it’s hard but the best thing to do is accept it and reach out for support. Support networks can work with you to figure out what’s best for your child and help them progress. The ASD class has really helped Paddy compared to the mainstream one, which can be hard for some children with ASD. In the ASD class, the children can learn more and have one-to-one support. They have more breaks, which is vital.
I would say to other Traveller parents, if you think your child is autistic, don’t be afraid to seek a diagnosis. The earlier you get a diagnosis, the faster your child can progress. Family members can also be a great support.
Sometimes you hear misinformation around vaccinations and autism. My children are fully vaccinated. Childhood vaccinations are important to protect your children’s health throughout their life. I don’t think there is one thing you can pinpoint that causes autism and I will say that to people. Link in with your Traveller Primary Health Care Project if you have questions.
Paddy is now in an ASD class in secondary school. He’s going into second year in September and is flying it. He’s an average 14-year-old now and loves art and Lego. He’s one in a million, a real character, though it isn’t always easy for him; he doesn’t always love being associated with autism.
Pavee Point Traveller and Roma Centre, AsIAm, the HSE National Social Inclusion Office, Department of Public Health Dublin and South East, and the National Immunisation Office worked together on co-designing a culturally appropriate information video on autism for Travellers highlighting the facts and signs of autism, breaking down the myths and how to get support if needed. The video is a resource for Traveller primary healthcare workers, public health nurses, GPs and other healthcare professionals to share with the Traveller community, to increase awareness of autism.
HOW TO BE... SunSmart and sharing that knowledge with patients
Evelyn Power, Candidate Advanced Nurse Practitioner in Skin Cancer, Dermatology at University Hospital Limerick
shares her insights

My journey as a nurse began 31 years ago when I started my training as a student nurse in what was then known as the Regional Hospital in Limerick. What has followed has been a fulfilling career that has led to many enjoyable experiences, including a year nursing early on in Australia. It was during that year that I first became aware of many of the things I do in my job today. Australians at the time, even in the outback regions I worked in, spoke to us about how we were too fair to be out in the sun and needed to wear at least factor 30 and ‘Slip, Slop, Slap, Seek, Slide’, a campaign that began in 1981 as a response to their rapidly increasing skin cancer cases.









“When working outdoors, you are exposed to two to three times more UV rays. Damage from sun rays adds up over time, increasing your risk of skin cancer.”
My nursing career has evolved over the years and I eventually found myself back at my original starting point, now University Hospital Limerick (UHL) as a clinical nurse specialist in dermatology. My interest in skin cancer continued and in 2014, it was becoming evident that skin cancer cases were on the rise nationally. I became the first skin cancer nurse involved at the formation of the UL Hospitals Group melanoma multidisciplinary team (MDT) meeting. Subsequently, I have acted as a patient advocate at these discussions and informed patients of the outcome for their care plan.
Intra-professional collaboration is integral to patient care and I have developed working relationships with oncology, radiation oncology (radiotherapy), the maxillofacial department and plastic surgery department in Galway. This can be incredibly important when a patient with melanoma
is involved with multiple specialities, as we can help patients to navigate these services while undergoing treatment.
Unfortunately, skin cancer cases are continuing to rise and it is now the most common form of cancer in Ireland, with over 11,000 cases diagnosed annually (NCRI, 2024). In 2018, I was appointed as a National Cancer Control Programme (NCCP) clinical nurse specialist in skin cancer together with seven other nurses nationally, initially to meet the needs of these patients.
Every day in the dermatology clinics, we meet patients presenting with cancerous or precancerous lesions and on a weekly basis, I work with patients with metastatic melanoma. New treatments for advanced melanoma have meant that more patients are now living with and beyond cancer. These patients attend for surveillance and many require significant support during their cancer journey.
My professional development is still ongoing. I am currently completing a post-graduate diploma in advanced practice in NUIG as the NCCP Candidate Advanced Nurse Practitioner in Skin Cancer in UHL. In this role, I have drawn on my 18 years’ experience as a clinical nurse specialist in skin cancer and dermatology. Advanced training in the recognition of skin lesions, dermoscopy and evidence-based practice has provided me with the knowledge to perform a full health assessment for each patient. I believe that building and maintaining relationships is an important part of the advanced nurse practitioner role, both as part of the nurse/ patient relationship and the multidisciplinary team.
I am also a member of the National Skin Cancer Implementation Group, which is made up of a wide range of health professionals and patient advocates whose purpose is to oversee the implementation of the National Skin Cancer Prevention Plan 2023-2026.
Health Promotion is hugely important in the prevention of skin cancer and each consultation in the clinic includes a conversation about how to identify any suspicious lesions. We advise on sun protective behaviours, to follow the 5 S’s and be SunSmart.
Many patients express that they were not aware that they must use sun protective measures even on cloudy days in Ireland and some admit that while they look after their children, they rarely apply sunscreen in Ireland themselves but will apply it when abroad on holidays.
I believe this information should be expanded to other specialities so health professionals can use the opportunity to ‘make every contact count’ if they see a patient who has a suspicious lesion or needs sun protective advice.
To support education of the public and especially staff in the UL Hospitals Group, in conjunction with the Irish Skin Foundation and the NCCP, the dermatology department in










UHL created a digital-animated, hospitalbased campaign targeting all aspects of sun protective behaviours. Based around visual awareness of the Healthy Ireland SunSmart message, we created five animated videos to increase awareness and adoption of skin cancer protective measures, which were shown on the visual display units across the six hospitals of ULHG, through social media and on the staff app from April to September.
Over 1,100 staff took part and the campaign had a positive impact on their attitudes towards skin protection and skin cancer awareness. Healthcare workers represent a unique cohort for health promotion, given the opportunities that arise through patient interaction.
The findings of the study were published in the Skin Health and Disease journal in 2023. Among the population that took part, there was a high uptake of sunscreen use, although a less favourable adoption of seeking shade, protective clothing and hats. The initiative was favourably received by staff and those who completed the postcampaign questionnaire reported a positive impact on self-reported sun protective habits, skin cancer awareness and confidence discussing sun protection with others. Sharing knowledge is important to the development of the skin cancer nurse role, both to patients and their families and the health professionals who care for them. To this end, I have been involved in educational programmes for nurses in the dermatology department and other hospital areas, other health professionals, patient support groups and the public.
Be SunSmart. Skin cancer is largely preventable by protecting skin from UV rays and not using sunbeds. Protecting your skin from the sun, whether at home or abroad, can reduce your risk of skin cancer.

Spotlight on Oral Hygiene
Keeping a healthy smile
Prevention is always the best course of action
Oral health is a key part of overall wellbeing, but it’s often overlooked until problems arise. In a recent episode of the HSE Talking Health and Wellbeing podcast, Dr Anne O’Neill, Oral Health Lead shares clear and practical advice on how we can all protect our teeth and gums throughout life.
Dr O’Neill explains why regular dental visits are so important – not just for spotting problems early, but also for getting advice tailored to your individual needs. The episode covers brushing techniques, the correct use of fluoride toothpaste and why you should spit rather than rinse after brushing. The podcast also looks at the importance of flossing and highlights how oral health is linked to general health, from heart conditions to diabetes.
Dr O’Neill also provides practical tips for parents when it comes to their children’s dental routines and talks about building in regular daily times to build those small oral health habits at a young age.
The discussion also focuses on changes to dental practices, specifically about how dental amalgam is no longer being used in fillings due to a new EU directive, which is ending the routine use of these silver fillings on account of environmental concerns around mercury. These fillings won’t be removed unless there’s a clinical need, but this change supports the importance of prevention.
To reduce your risk of dental problems, eat a balanced diet, limit sugary snacks and drinks, and brush twice daily with fluoride toothpaste.
Scan the QR code to hear more from Dr O’Neill.

Tips for good oral hygiene
• Eat a healthy diet, limiting sugary and acidic foods and drinks to meal times.
• Brush your teeth twice daily with fluoride toothpaste.
• Spit out the toothpaste and don’t rinse your mouth.
• Floss or use an interdental brush.
• Visit your dentist regularly to identify potential problems as early as possible.
Exercise PANDORA
Working to ensure our health system remains resilient in the face of infectious disease threats
On 6 March, the HSE National Health Protection Office, in collaboration with the National Office for Emergency Management, conducted Exercise PANDORA, a national command post exercise. Exercise PANDORA aimed to test the HSE’s capabilities to deliver actions and responsibilities as described in the Operational Pandemic Plan (OPP), in response to an escalating avian influenza emergency. Published in July 2024, and informed by the learnings from COVID-19, the OPP provides a framework that encompasses early detection, resource management, stakeholder coordination, preventative measures, medical interventions, and recovery planning to ensure a proactive, agile and effective response to a pandemic emergency.
Exercise PANDORA brought together senior leadership teams from across the health service, with key stakeholders both regionally and nationally. At the national level, representatives from the HSE, Department of Health, the Department of Agriculture, Food and the Marine, and the National Virus Reference Laboratory participated. Regional teams included stakeholders from the regional health areas including acute and community services, public health, hospital groups, emergency management, environmental health, and regional executive officers.
“Key focus areas included early detection, resource management, interagency collaboration, and the rollout of a highly effective vaccine.”
Planning for Exercise PANDORA began in July 2024, requiring extensive coordination across the HSE. The exercise featured a series of scenario injects simulating the progression of a pandemic, challenging participants to identify and address gaps and vulnerabilities in the OPP. Key focus areas included early detection, resource management, interagency collaboration, and the rollout of a highly effective vaccine.
One national and six regional playing teams engaged in Exercise PANDORA. The escalating pandemic scenario tested critical elements of preparedness, including coordination,




communication, and disease control measures. Observers from within the HSE and external agencies, including the Food Safety Authority of Ireland (FSAI) also participated, providing valuable insights into cross-sectoral collaboration.
The event was attended by senior stakeholders, including the chief medical officer (CMO), deputy CMOs and the chief clinical officer, as well as cross-sectoral observers from Northern Ireland, reflecting the cross-jurisdictional importance of pandemic preparedness. The exercise identified key successes, including effective communication, the utilisation of existing structures, and strong interagency collaboration. All regional and national playing teams agreed, or strongly agreed, that Exercise PANDORA improved their understanding of the HSE OPP’s operational aspects.
Evaluation of Exercise PANDORA is ongoing, using a structured framework that includes both hot and cold debriefs to capture immediate and reflective feedback. These insights will inform future refinements to the OPP, ensuring that Ireland’s health system remains resilient in the face of emerging infectious disease threats.
Thanks to all playing teams who contributed to the success of the exercise, as well as the chief clinical officer and regional executive officers for their ongoing support. We also appreciate the efforts of the facilitators and scribes across the country, whose dedication ensured productive discussions and thorough data capture.
Spotlight on Mental health
New HSE Balancing Stress programme to enhance mental wellbeing
To support people across Ireland in managing everyday stress, HSE Mental Health and Wellbeing in partnership with HSE Psychology have developed a free, easyto-access online programme: Balancing Stress. The programme offers six self-directed online video sessions (each around 35 minutes) and was officially launched on 2 May by Jennifer Murnane O’Connor TD, Minister of State for Public Health, Wellbeing, and the National Drugs Strategy.
Delivered by Dr Niamh Clarke, HSE Principal Psychologist, this programme features expert interviews with Professor Alan Carr, School of Psychology, UCD and guided stress management exercises across all sessions. Participants can watch the programme at their own pace, in their own time, using a phone, tablet or laptop.
The new programme complements existing HSE mental health and wellbeing supports and reflects the HSE’s commitment to accessible, preventative mental health services at a population level.

Key features of the programme:
• Understanding stress
• Managing worry
• Managing anxiety
• Managing low mood and depression
• Understanding relationships and stress
• Balancing stress into the future
Each session includes:
• Practical strategies based on CBT and Positive Psychology
• Guided relaxation and breathing exercises
• Expert interviews with Dr Niamh Clarke and Professor Alan Carr
HSE South West Mental Health Services host Back to Basics masterclass in Ballincollig
Mental health service users are experiencing a marginalised gap in life expectancy of up to 20 years, dying prematurely due to preventable conditions. With support from NMPDU South West, HSE South West Mental Health Services hosted a masterclass to support mental health nurses within their education/training needs. The theme was ‘Back to Basics’ with keynote speakers Bridie O’Sullivan, HSE South West Regional Director of Nursing and Midwifery, and Dr Michael Nash of TCD, who has conducted extensive research within this area. There were a variety of experts within the areas of respiratory, oncology, sepsis, metabolic monitoring and diabetes. There was an overwhelming response to the day with over 90 mental health nurses in attendance and positive feedback. This was just a starting point and will inform future training/education of mental health nurses across CAMHS and AMHS within HSE South West.
The programme can be accessed online at hse.ie/balancingstress
It is promoted to the general public across HSE services. Promotional material can be ordered from healthpromotion.ie

The Shine Green Ribbon Campaign
The annual Green Ribbon Campaign takes place in September and is Shine’s largest campaign, supported by – among others – the HSE National Office for Suicide Prevention. It is a key opportunity for the organisation to lead the way on stigma reduction around mental illness in Ireland.
Planning is underway for 2025’s campaign and Shine welcomes discussions on collaborative events or initiatives with any partners, for example in health, corporate or business settings. In 2025, Shine will showcase the campaign again at high-profile events like Electric Picnic and the National Ploughing Championships.
The theme this year is ‘Step Up to Stamp Out Stigma’. Shine is asking people to ‘step up’ – to do their bit. For change to come about, everyone needs to play their part.
If you have any ideas for this year’s campaign activities and events, you can contact Kieran Murphy: kmurphy@shine.ie
To learn more and order supplies of free green ribbons, visit shine.ie
Launch
of PeskygNATs-ID


computer-based interventions for adults with intellectual disabilities
Cheeverstown and University College
Dublin, with funding from the HSE, have developed two computer-based programmes that support suitably qualified mental health professionals to deliver psychological interventions to adults with intellectual disabilities:
The Pesky gNATs-ID ‘Feel Good Island’ game is an evidence-based computer-assisted cognitive behavioural intervention for adults with intellectual disabilities who are
experiencing anxiety, low mood, and/or depression.
The Pesky gNATs-ID ‘Mindful Island’ game guides the delivery of an adapted mindfulness intervention specifically tailored for adults with intellectual disabilities.
In both games, people visit a 3D world and meet a team of avatars, voiced by actors with intellectual disabilities, who explain key therapeutic concepts.
Both games are designed for use in sessions where a person with an intellectual disability plays the game alongside a mental health professional; and are supported by printable workbooks and videos of the exercises. They combine gaming with the highest quality psychological content to support evidence-based interventions for adults with mild and moderate intellectual disabilities.
Licenses to use the games, which are free for professionals in Ireland and the UK, are available at peskygnatsid.com
Maternity
National Maternity Experience Survey 2025
Women who’ve recently given birth can have their say until the survey closes in July
The second ever National Maternity Experience Survey opened on 1 May 2025. The survey offers women who have recently given birth the chance to share their experiences of maternity services. The goal is to improve the quality and safety of care provided to women and their babies. This initiative is part of the National Care Experience Programme, a collaboration between the HSE, the Health Information and Quality Authority (HIQA) and the Department of Health.
Every conversation counts
Support maternal pertussis vaccination and inclusive public health
The HSE is urging healthcare professionals to encourage pregnant women to receive the whooping cough (pertussis) vaccine between 16 and 36 weeks of pregnancy. The vaccine, available free of charge from participating GPs, provides critical immunity to newborn babies during their most vulnerable early months. Whooping cough tends to surge every five to six years, and 2024 saw a record high with over 539 confirmed cases. The trend has continued into early 2025, with cases expected to rise further into the spring and summer months.
Women aged 16 and over who gave birth in February or March 2025 are invited to participate. Participants will receive an invitation by text message to take the survey approximately three months after giving birth, between May and June 2025. Participants can choose to take the survey in English, Irish, Polish or Romanian.
The survey includes 64 questions covering every stage of the maternity journey, including antenatal care, labour and birth and postnatal care in the community.
Survey responses will be anonymised, analysed and compiled into a national report detailing the quality of maternity care. This feedback leads to real, meaningful change in maternity care.
Dr Chantal Migone of the HSE’s National Immunisation Office (NIO) emphasised, “Young babies are most vulnerable to whooping cough as they do not start their vaccinations until two months old. This leaves them susceptible to serious complications, including respiratory distress, hospitalisation and, sadly, death. Vaccination during pregnancy passes on critical immunity to babies so that they are protected from birth.”
Inclusive communication is crucial
The HSE NIO recognises the importance of ensuring public health messages resonate with all communities. Inclusive imagery, multilingual materials and culturally sensitive resources are

For more information, visit yourexperience.ie or follow the National Care Experience Programme on social media @careexperience
central to the campaign. Research shows people are more likely to follow health advice when they feel represented.
To support greater vaccine uptake across Ireland’s diverse population, the HSE NIO has collaborated with community organisations to deliver accessible information to migrant and underserved groups.
Take action today:
• Encourage maternal pertussis vaccination during consultations
• Order free inclusive campaign materials from Healthpromotion.ie
• Reinforce that vaccination is safe, free and essential
For more information, visit immunisation.ie
Photobiomodulation for mucositis
The dental team at Children’s Health Ireland (CHI) at Crumlin have a new light-based therapy to help children receiving chemotherapy who develop oral mucositis. Kirsten FitzGerald, Consultant Paediatric Dental Surgeon at CHI tells us about it.
“We are thrilled to have such an effective, simple and child-friendly treatment to offer for oral mucositis,” says Kirsten FitzGerald. “For well over a decade, we have used a laser to help children with mucositis to heal faster. But now we have a new LED-based device that is much more child-friendly, and it’s great to see it in action.”
What is oral mucositis?
One of the most debilitating side effects of cancer treatment is oral mucositis (OM). It affects up to 80% of children receiving chemotherapy. OM causes painful ulcers that limit the ability to swallow, eat, speak, sleep and take medications. It can result in delays to treatment schedules, increased length of stay and unplanned admissions. OM takes a physical toll, but psychological effects are also apparent when children struggle to eat and communicate, or have to spend long periods of time in hospital.
How is OM managed?
care and in using and maintaining the equipment, they develop a really good connection with the children and families as they often provide this treatment for several days in a row and over many cycles of chemotherapy.”
What is the new device?

Thanks to a generous grant from the Children’s Health Foundation, the dental team have been able to purchase a THOR Oral LED device. This device delivers light in a way that is so simple that even small children can now treat themselves in minutes. A 13-yearold girl who has experienced both laser and LED PBM says, “When I used the laser, it was quite sore because I had to keep my mouth open. The LED device is a lot better because I get to use it myself.”
demonstrating how to use the light-based therapy.
For decades, the mainstays of treatment for mucositis have been pain relief (usually with opiates) and the (largely ineffectual) use of topical mouthrinses. In more recent years, research has demonstrated significant reduction in OM-associated problems with the use of light therapy, known as photobiomodulation or PBM.
What is PBM?
PBM involves applying light to the tissues to stimulate the body’s healing process. The light can be from a laser or an LED source. In recent years, LED-based systems have come on the market, allowing for safer, more child-friendly therapy.
Kirsten says, “Our dental nurses have become the experts in PBM for children here in Crumlin. Aside from being highly knowledgeable regarding oral
How can this make a bigger impact?
The dental team at CHI at Crumlin would be happy to share their learning with other centres where patients might benefit. In addition to the obvious improvements for individual patients, there are environmental benefits associated with PBM. Carbon savings are made when medication use (morphine, antibiotics, etc) and length of stay are reduced. Financial costs to the health service are similarly reduced.
What are the challenges?
Given the value of PBM in both prevention and treatment of mucositis, there has always been a high level of demand for the service in Crumlin. Many paediatric hospitals internationally have not implemented this therapy for this very reason – it requires extra staffing. The dental service is very keen to expand this service to all those who would benefit, but this will require increasing numbers, especially of dental nurses.
If you’d like to get in touch with Kirsten for more information, you can email kirsten.fitzgerald@childrenshealthireland.ie
BowelScreen
extended to include people aged 70
man Joe Grogan details diagnosis after screening

Since 1 April this year, BowelScreen is available to more people, with the eligible age range extending to include 70-year-olds. This makes free bowel screening available to everyone aged 59 to 70.
In October 2023, BowelScreen began offering screening to people aged 59. Among the people invited for screening was 59-year-old Tuam funeral director Joe Grogan.
Joe’s first screening test was followed by a colonoscopy, and he was subsequently diagnosed with bowel cancer in December 2023. He received chemotherapy, radiation therapy and surgery and says, “I’m alive and kicking and that’s really all thanks to a letter I got from BowelScreen.”
Joe encourages all eligible people to take the BowelScreen test and he played an important role in this year’s Bowel Cancer Awareness Month in April. His story featured in several newspaper articles, radio interviews and a podcast.
BowelScreen invites eligible people to take part every two years, with a
Bowel Screen


test kit sent to their home. To take the test, you place a sample of poo in a tube and send it back in a freepost envelope for testing in the lab. The test looks for the presence of blood. If the amount of blood found is above a certain level, you will be referred for a colonoscopy.
Joe was initially hesitant and says, “When I got the letter, I thought, ‘I don’t need this’. I felt good. Then I picked it up again and said to myself, ‘What have I got to lose?’ I rang the freephone number and got the kit sent out to my home.”
The kit comes with instructions and is easy to do. Joe explains, “I read what I had to do and thought, I’ll leave



























that for a day… then I changed my mind and just got on with it. It’s five minutes of your life. Once the little sample is in the tube, that’s it. For what those five minutes have meant to me, I’d do it every day if I had to.”
Every year, around 2,500 people get bowel cancer in Ireland. It is the second most common of all invasive cancers in men in Ireland, and the third most common in women.
BowelScreen refers around 3,500 people each year to have precancerous growths (known as polyps) removed. Around 5% of those referred for colonoscopy through BowelScreen will have cancer detected.
Watch Joe’s video on YouTube by searching ‘Joe Grogan – BowelScreen Testimonial’. For more information, visit hse.ie/bowelscreen
Neuro-Mapping Project Phase 2
Working together towards integrated care in the community for people with neuro-rehabilitative needs

From left: David Walsh, National Director within Access and Integration, HSE; Marie Lynch, DFI Project Lead, Neuro-Mapping; Bernard O’Regan, Assistant National Director, National Disability Team, Access and Integration, HSE; Elaine Teague, CEO, Disability Federation of Ireland; Pascal Derrien, Chairperson, NAI; Minister Anne Rabbitte, Minister of State, DCEDIY; Nicola O’Malley, Research Officer, NAI; Joe Condon, Early Onset Parkinson Disease; Sinead Bradley, NAI Coordinator; and Ciara Lynch, Programme Manager, National Neuro-Rehabilitation Strategy, HSE. Photo by Leah Farrell / Photocall Ireland.
The Neuro-Mapping Project is a joint project between the HSE, Neurological Alliance of Ireland (NAI) and Disability Federation of Ireland (DFI) 2024. It aimed to further understand the current service and support pathways that occur between existing and developing community services for those with neuro-rehabilitative needs. We are very grateful to the 56 people with neurological conditions and 137 service providers across CHO 2, 3 and 6 who shaped the report findings and recommendations.
The main objective was to establish the views of people living with neurological conditions and community service providers, of navigating, accessing and providing services and identify challenges and enablers from their perspectives.
The feedback from the people with neuro-rehabilitative needs was very similar to those of service providers and the key findings are summarised below:
• The lack of community specialist services available
• The complexity of navigating community services
• The sense of isolation and abandonment on discharge
• The gaps in the provision of long-term care for people with neurorehabilitative needs
• The obstacles in accessing services – including transport and diagnosis
• The current underinvestment in the development of specialist services
The findings and recommendations will inform the work programme of the national neuro-rehabilitation programme and its community workstream programme, who had overall governance for the project. They will also inform the model of service of the community neuro-rehabilitation teams, which are currently being established across the country.
The other significant aspect of this report is the method of engagement with those with lived experience, and how their views have shaped the findings and recommendations. The approach used has been recognised as a leading example of public and patient involvement in health and social care research.
For more information, see bit.ly/NeuroMappingProject
The following five areas for improvement have been identified, and a series of actions are listed under each of these recommendations in the report to guide the changes required:
1. Increasing knowledge and information of services that are available in the community for people with neurological conditions.
2. Improving how services work together with enhancements to how information is gathered and shared between services, to enable a more seamless service-user journey.
3. Providing equitable access to services based on rehabilitative need and preference of the individual.
4. Adequately staffing and resourcing specialist services in the community so that they can provide timely and high-quality interventions to people with neuro-rehabilitative needs.
5. Redesigning and restructuring community neuro-rehabilitation services, in addition to adequate resourcing of supports such as personal assistance hours and transport services, to facilitate the continuum of care for people with neurological conditions, particularly those who live with a long-term or progressive disability.
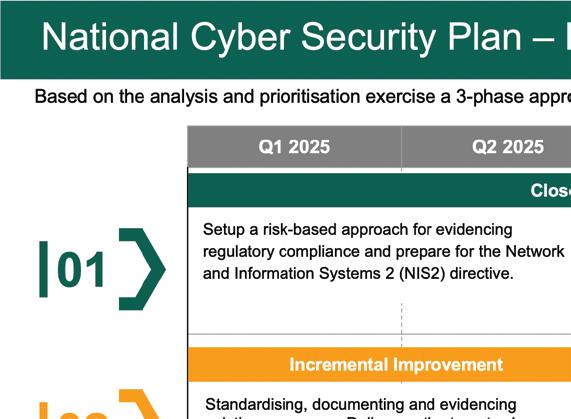
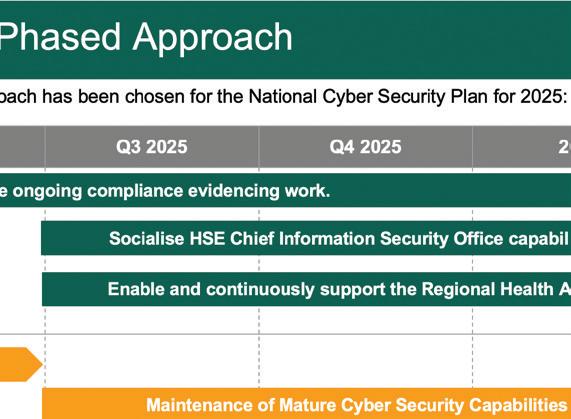
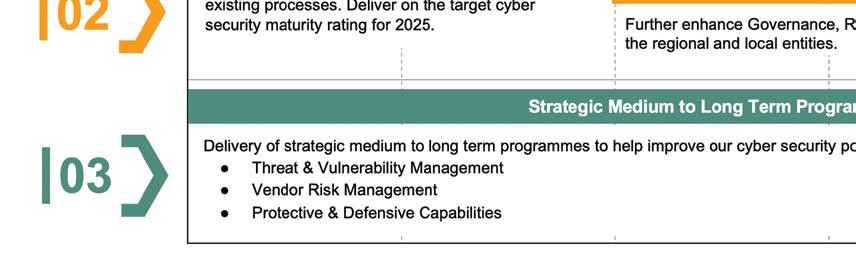
Safeguarding Ireland’s digital health future
Neal Mullen, Chief Information Security Officer (CISO) on the important role we all play Cybersecurity is no longer just a technical concern; it’s a vital part of delivering quality healthcare. Following the HSE’s Cyber Security Statement of Strategic Intent 2024-2027, which aligns with the broader Digital for Care 2030 strategy, the new CISO Office National Cybersecurity Plan is now in motion. This plan is about more than just securing systems; it aims to build a resilient digital health ecosystem that can adapt to evolving cyber threats.
As HSE employees, your role in this digital transformation is critical. By staying informed and engaged with these initiatives, together we can protect Ireland’s public healthcare services and build a more secure future for all.

Advice for HSE staff on dealing with data breaches
Data Protection safeguards your privacy by ensuring personal information is handled responsibly and lawfully. In the event of a data breach, you must act quickly to report and contain the incident, reducing potential harm and ensuring compliance.
What is a personal data breach?
A personal data breach is any accidental or unlawful destruction, loss, alteration, unauthorised disclosure, or access to personal data. Personal data is information related to an identified or identifiable living individual.
The initiatives called out in the National Cybersecurity Plan deliver on our NIS2 regulatory requirements, making the plan easily:
• Auditable
• Compliant
• Standardised
• Measurable
• Future-proofed
The plan takes to heart the lessons learned from the 2021 cyberattack on the HSE. By using recommendations from the Post Incident Review, it aims to develop and enhance cybersecurity across Ireland’s public healthcare system. It focuses not only on today’s challenges but also on strengthening the system for the future.
The plan embraces the use of modern technologies for more efficient operations and secure data management. Trust is another cornerstone; both patients and healthcare workers can have greater confidence in the system’s resilience. Finally, the plan emphasises a coordinated approach to risk management and effective response strategies, ensuring we’re ready to face any cyber incident.
If you suspect or confirm a potential data breach, what should you do? Report it immediately. Notify your line manager and local deputy data protection officer (DDPO) as soon as you suspect or confirm a data breach. The HSE must report notifiable breaches to the Data Protection Commission within 72 hours. This is done through your local DDPO following consultation with the local service where the breach occurred.
Reporting process
Your line manager will help you identify if the incident is a potential data protection breach and support you to complete a data breach incident report form. Completed forms should be submitted to your local DDPO, who will:
• Verify if the incident qualifies as a data breach and report to the Data Protection Commission as appropriate.
• Provide guidance on necessary actions.
• Advise if the breach poses a high risk to individual rights and freedoms, in which case the affected individuals must be informed.

KidneyDisease
Early detection of chronic kidney disease is key to
long-term health

Professor Austin Stack, Consultant Nephrologist, UHL; Foundation Chair of Medicine at the School of Medicine, University of Limerick; and lead investigator at the National Kidney Disease Surveillance System.
Approximately 40,000 people in the Mid West are living with chronic kidney disease (CKD), and University Hospital Limerick (UHL) runs one of Ireland’s busiest kidney programmes. However, UHL consultant nephrologist, Prof Austin Stack insists that we must do more.
At the end of 2023, UHL was caring for 277 dialysis patients and 147 transplant recipients, and on World Kidney Day in March, Prof Stack led UHL’s participation in global efforts to raise awareness about kidney health, focusing on early detection to prevent progression of the disease.
Prof Stack says, “With early diagnosis giving people the best chance at maintaining long-term kidney health, we continue to press that central World Kidney Day message, to ask yourself, are my kidneys okay?”
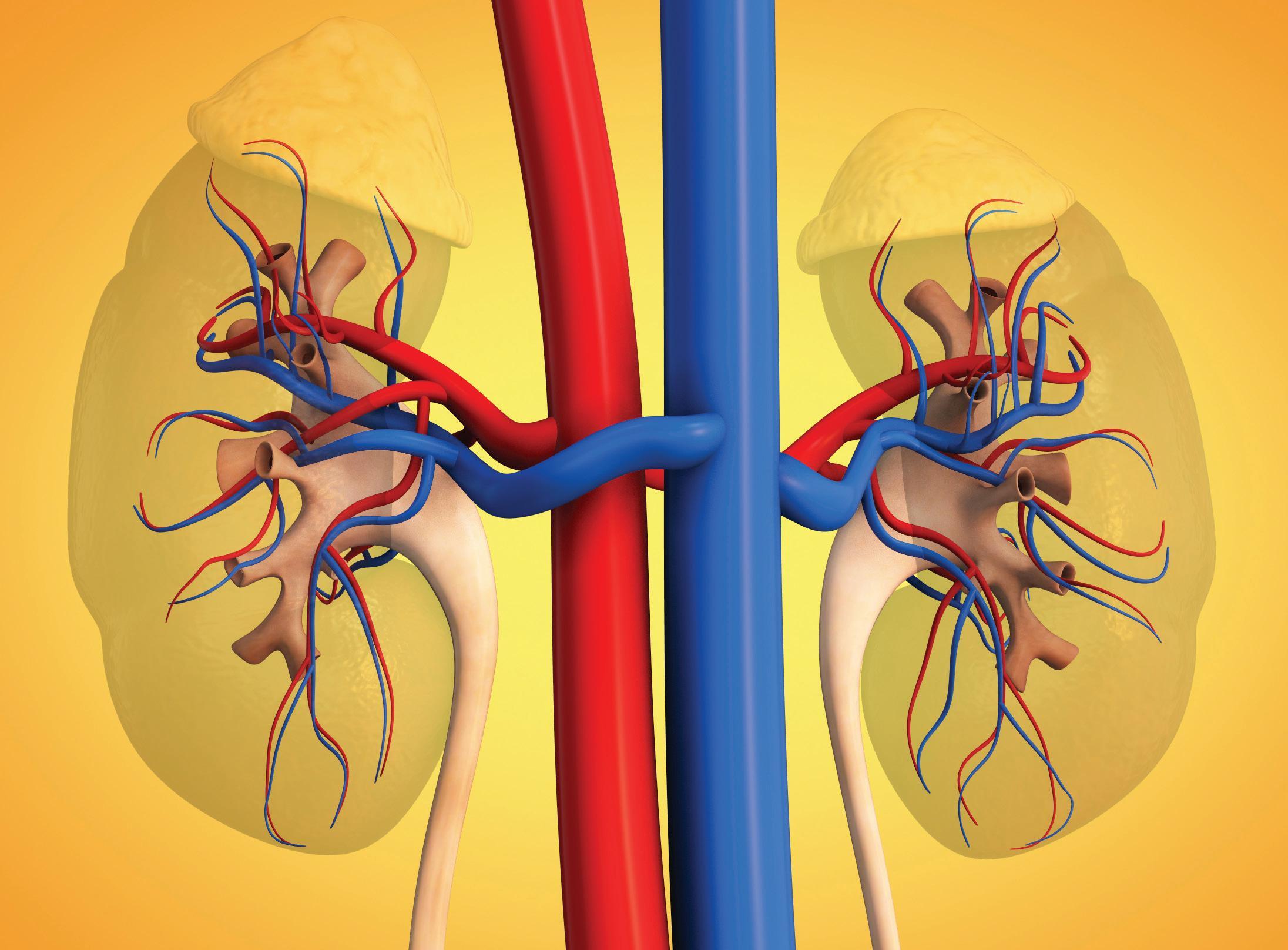
CKD is linked to conditions like diabetes, hypertension, heart disease, cancer and obesity, especially in older adults and those from disadvantaged backgrounds. Many people remain undiagnosed, despite the fact that kidney disease can be detected early through simple blood and urine tests.
Encouragingly, new treatments can slow or prevent progression to kidney failure. UHL, in partnership with the University of Limerick, is leading research that identifies high-risk groups for early intervention.
A critical next step is embedding a national kidney surveillance programme into the Irish health system to screen these groups. Later this year, CKD will be added to the HSE’s Chronic Disease Management Programme.
Kevin the Kidney travels over 1,400 km in World Kidney Day challenge
To mark World Kidney Day 2025, on 13 March, the Renal Unit at Tallaght University Hospital (TUH) set up a countrywide challenge. The aim was to help Kevin the Kidney ‘join the dots for kidney health’ by cumulatively travelling the distance between the 25 dialysis units around the country. Staff, patients and families were invited to take part and choose to either walk, run or cycle. The circuit distance was 1,365 km and participants covered 1,405 km. Most impressively, 100.26 km was covered by haemodialysis patients at TUH, who were having their treatment on the day in the Vartry Renal Unit.
Deepen your leadership practices for change with the blog series, Inside the Change Guide
The Organisational Change Unit has published a series of articles taking a deeper dive into the HSE Change Guide – People’s Needs Defining Change. The insights shared in this blog series can be applied to a wide range of services within health and social care. Local context is key when it comes to planning for change, especially in complex adaptive systems where many dependencies and boundaries exist. As you delve into the full blog series, you will build your understanding of areas to focus on to deliver the right change, in the right way. This also means recognising that change is not linear, can be messy at times (and that’s ok) and requires space for iteration to respond to emerging needs. We hope you enjoy the leadership insights shared. You can access the articles via the links provided.
• Leading Change –An Intricate Tapestry, bit.ly/InsideTheChangeGuide1
• Defining Change Through People’s Needs – A Leadership Perspective, bit.ly/InsideTheChangeGuide2
• Defining a Roadmap for Change –Leadership Exploration, bit.ly/InsideTheChangeGuide3
• Designing Change – Leader’s Guide to Human Centred Co-Design, bit.ly/InsideTheChangeGuide4
• A Leadership Roadmap for Implementation and Sustainability, bit.ly/InsideTheChangeGuide5

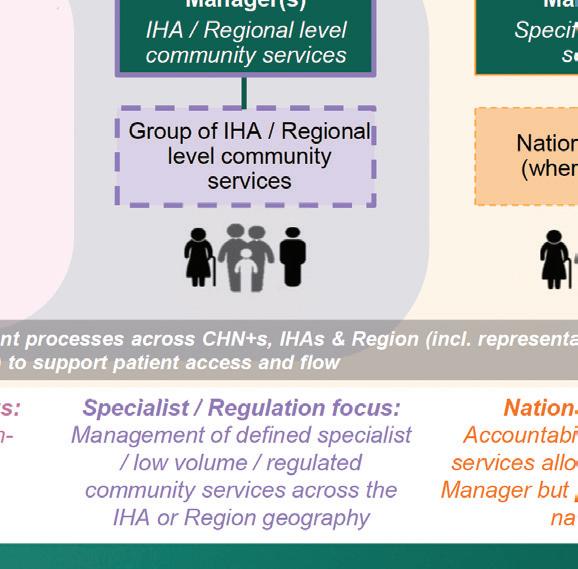
Integrated Service Delivery Model
In March 2025, Nuala Scannell and Angela Ryan (Organisational Change Unit, HSE) presented the engagement process undertaken in the co-design of the Integrated Service Delivery (ISD) Model (pictured below) at the All-Ireland Conference on Integrated Care. The ISD co-design process was underpinned by the HSE Change Guide and the Department of Public Expenditure and Reform design principles. Extensive engagement was undertaken in 2023 and 2024, with nearly 900 stakeholders engaged directly. This involved a multimodal approach: in-person sessions and online sessions; briefings and updates, co-design workshops; sense-checking meetings; and individual meetings, focused small group sessions, and large groups events. A wide range of stakeholders were involved, including:
• patient and service-user partners
• managers and staff from:
• clinical and operational roles
• hospital and community services
• HSE and partner agencies
• Department of Health and Department of Children, Equality, Disability, Integration and Youth
• academic experts

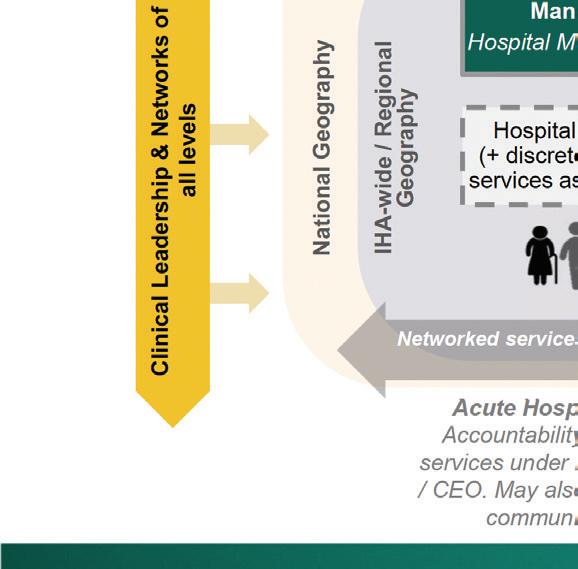

Following this extensive engagement, the Health Regions Steering Group, chaired by the CEO, approved the ISD Model (December 2024) and the Integrated Healthcare Area (IHA) structure (February 2025).
Five of the six health regions are currently in the implementation phase, focusing on the implementation of the ISD Model.
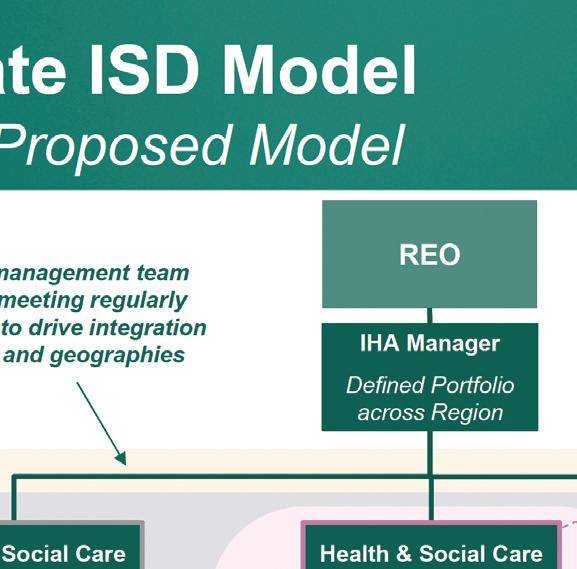
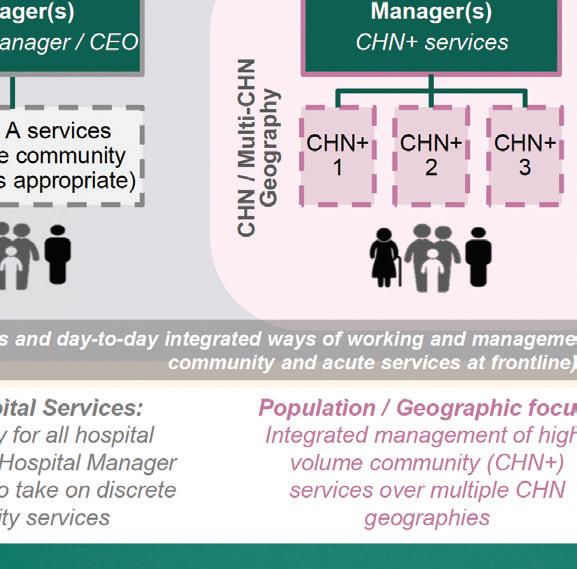
HSE Mid West is preparing for implementation, which will begin at a later date.
The Health Regions Programme Team were delighted to receive a nomination from IPPOSI for the international Made with Patients Awards for the patient and serviceuser partnership work undertaken as part of the ISD co-design.
Updates from HSE Dublin and South East
Martina Queally
HSE Dublin and South East Regional Executive Officer
It has been a busy and productive period across services in HSE Dublin and South East. Firstly, I would like to acknowledge our staff for their continued dedication in delivering quality care, despite rising service demands and challenging severe weather events that impacted service delivery.
Despite a 14% rise in Emergency Department attendances among those over 75 in our region, admissions for this group increased by only 4% – a remarkable achievement in the context of a progressively older and increasing population. Our staff are meeting that challenge and I wish to acknowledge that effort.
Trolley counts have dropped by 8%, indicating better patient flow, while delayed transfers of care have decreased by over 11%, reflecting improved community integration. These accomplishments highlight the resilience and innovation of our teams.
In terms of our transition to our new health region structure, our executive management team is now in place, and work on the geography and service alignment of our region is complete. Our focus now turns to the next phase of implementation
“Trolley counts have dropped by 8%, indicating better patient flow, while delayed transfers of care have decreased by over 11%, reflecting improved community integration.”

– how our healthcare areas will operate under the new, nationallyagreed Integrated Service Design (ISD) model.
Community Healthcare Networks (CHNs) continue to be the foundation of this transformation, creating opportunities to enhance service alignment and integration.
Engaging with staff remains a priority, and we have recently hosted our third staff webinar to outline how this next phase of implementation will impact our services. We will continue to engage with staff and share further updates as they become available.
Once again, I would like to sincerely thank all staff across our health region for your support and collaboration during this transition process.
Poetry collection launched by HSE supported writers’ group

A Flake of My Soul is a new collection of poetry produced through a creative writing project supported by HSE mental health services in Waterford. The project was developed in partnership with the Waterford Healing Arts programme and supported by Rethink Ireland and Creative Waterford.
Participants, who were new to writing, availed of the opportunity through their local HSE mental health services.
Throughout the group’s meetings, participants learned to explore the world around them and use their observations to write poetry. This project highlights the benefits of participation in the arts for everybody and how creativity is hugely beneficial in exploring self-identity, in nurturing connectedness and promoting a sense of wellbeing.
Updates from HSE Dublin and South East
Ageing Well Together: Enhancing community support for older persons
HSE Dublin South and Wicklow recently hosted an Ageing Well Together stakeholder engagement event, aiming to further enhance the lives of older people living at home. This event was the culmination of a series of consultations with service users, HSE services and community organisations.
Attendees heard the outcomes of these consultations, which highlighted some of the great work already happening, and also explored areas where meaningful integration could further support this work. There was a particular focus on the community organisations that enable healthy ageing through befriending services and practical supports to older people who are vulnerable, isolated or alone.
An integrated care for older people approach helps health and social care systems effectively respond to the diverse and complex needs of older people. Preservation of

Stakeholders at the Ageing Well Together event.
independence is among the most important health priorities cited by older adults. Building integration across services for, and with, older persons supports the Sláintecare
Minister launches Period Dignity for All –Diverse Voices and Photography Exhibition
As part of Women’s Health Week in March, colleagues from HSE Social Inclusion, alongside Minister of State at the Department of Health with special responsibility for Public Health, Wellbeing and the National Drugs Strategy Jennifer Murnane O’Connor TD, launched the Period Dignity for All – Diverse Voices and Photography Exhibition.
The exhibition illustrates the experiences and challenges of diverse groups of women in dealing with sexual and reproductive health, including the menstrual cycle. Developed by HSE Dublin and South East Social Inclusion, the exhibition also shines a spotlight on the demand for, and impact of, period dignity programmes nationwide. Research shows that up to 1 in 4 women may experience period poverty on occasion, while 1 in 10 school-aged girls have reported being unable to afford period products. Period dignity schemes run by the National Social Inclusion Office focus on reaching those experiencing consistent poverty, including homeless people, those living with addiction and minority groups.
living well at home ethos. Integrated care will ensure better planning based on population needs and provide better understanding of services available.

Linda Latham, HSE Social Inclusion and Minister of State Jennifer Murnane O’Connor TD.
St Vincent’s University Hospital exoskeleton operation success
An 18-year-old patient from Mayo, who was paralysed from the waist down following a road traffic accident in 2022, has regained movement and sensation in his legs after undergoing a pioneering spinal cord stimulator procedure. This first-of-its-kind procedure was performed by Prof Kirk Levins, Consultant Pain Specialist at St Vincent’s University Hospital.
Yousaf Ghaffar, the patient, was initially given a prognosis that he would never walk again. Following the accident, he experienced severe spasticity and paralysis in his lower limbs, which significantly impacted his quality of life.
In September 2024, Prof Levins, in collaboration with a research team from the United States, performed the ground-breaking procedure. This technique, which is yet to be named, involved inserting rigid wire leads through an epidural needle to stimulate the spinal cord at a specific frequency and location. This approach, different from existing methods, not only restored movement but also revived sensation in the patient’s legs.
“While we were confident that the procedure would help with spasm management and improve the patient’s quality of life, we were never certain that motor and sensory function would be fully restored,” said Prof Levins. “This result far exceeded our expectations and has the potential to transform the lives of other people with similar spinal injuries.”
Yousaf immediately began showing movement in his legs – something that hadn’t happened in over two years. Weeks later, sensation returned, marking a breakthrough in his recovery. While he is not yet walking independently, he is making remarkable progress using an exoskeleton and continues to relearn how to walk.

“This
result far exceeded our expectations
and has the potential to transform the lives of other people...”
A critical part of this journey has been postsurgical rehabilitation, which played a vital role in helping his brain relearn how to control movement after prolonged paralysis. Under the expert care of Dr Cara McDonagh and her team at the National Rehabilitation Hospital, along with physiotherapist Eleanor Phillips, Yousaf has been steadily reclaiming strength, mobility and independence – taking one step closer to a future he never thought possible.
This opens up new possibilities for patients with spinal injuries who were previously told they would never walk again. “We see great potential in this technique for restoring movement and sensation, and it could offer new hope to patients with spinal injuries,” Prof Levins added. “However, the procedure is expensive, and wider adoption will require careful consideration.” The team is researching the procedure’s potential and looks forward to its application to other cases in the future, including exploring its use in conditions beyond spinal injuries, such as endometriosis.
Yousaf was back in college after a few weeks and is eager to share his inspiring story. “I’m still amazed by how much I’ve recovered,” he said. “This procedure has given me a second chance at life, and I’m excited about the future.”
Updates from HSE Dublin and South East
A new chapter for neonatal care as children’s book trolley arrives at University Hospital Waterford
A new children’s book trolley initiative, in partnership with Waterford Libraries, Garter Lane Arts Centre and Waterford Healing Arts (part of Réalta) was recently implemented to bring comfort, joy and emotional support to families with newborns in the Neonatal Unit at University Hospital Waterford (UHW).
The children’s book trolley will contribute towards a nurturing and supportive environment for both infants and their families.
REO
Designed to bring a sense of normalcy and comfort during a challenging time, the trolley will provide families with the opportunity to read aloud to their babies, share stories and create meaningful memories. This collaboration highlights the community’s commitment to supporting the wellbeing of babies and families facing the challenges of neonatal care.

visit to St Luke’s General Hospital, Carlow/Kilkenny
On 13 March, Regional Executive Officer (REO) of HSE Dublin and South East Martina Queally visited St Luke’s General Hospital, Carlow/Kilkenny. The REO was brought on a tour of the hospital and the new Ormond Wing. There was an opportunity to meet with staff and speak to them about the care being delivered in the hospital’s emergency department, Acute Medical Assessment Unit, paediatrics department and inpatient wards. The REO also attended a presentation on the hospital’s services and its development plans, given by St Luke’s Clinical Director, Professor Garry Courtney.

Le Chéile project team featured on 100th episode of Talking Health and Wellbeing podcast – Supporting your Teen with Anxiety
Le Chéile is a primary care project for children and adolescents with complex presentations, running in Community Healthcare Network 4 in South Dublin. The project tests a more enhanced model of integrated multidisciplinary team working within primary care and received funding from the Government of Ireland’s Sláintecare Integration Innovation Fund. The team were featured on the 100th episode of the HSE Talking Health and Wellbeing podcast. Muireann Treacy (Clinical Psychologist), Niamh Garavin (Occupational Therapist), and Rosemary Kavanagh (Speech and Language Therapist) spoke about the complexities of adolescent development, with a focus on anxiety. This episode emphasises the value of a supportive atmosphere, active listening and nonverbal cues, while also exploring co-regulation, the role of social media, and the importance of self-care for parents.
Listen wherever you get your podcasts or watch on the HSE Health and Wellbeing YouTube channel.
REO and Integrated Healthcare Area Manager visit Wexford
hospital and community services
REO Martina Queally and Integrated Healthcare Area (IHA) Manager of Waterford Wexford Dr Sinéad Reynolds visited hospital and community services in Wexford on 8 April. Their visit included viewing current building works at Wexford General Hospital; the Endoscopy, Minor Operations and Outpatients departments at Ely Hospital; Selskar Psychiatry of Later Life Residential Centre; Abbeygale Residential Care Centre; and Wexford Primary Care Centre. The REO and IHA Manager welcomed the opportunity to meet with management teams and staff across the various sites and extended their gratitude to staff for facilitating the visits and their onsite engagement.

UcanACT – Promoting open-air physical activity in Kilkenny to combat cancer

The HSE’s physiotherapy services have been supporting an Urban Action Against Cancer (UcanACT) programme in Kilkenny, where the emphasis is on physical activity in public, urban, green spaces to aid cancer prevention. Held throughout 2024 and funded by the Erasmus+ instrument of
the European Commission, UcanACT has operated as a pilot project and an inter-sectoral initiative, bringing together physiotherapists, local authorities, non-profit organisations and higher education and research institutions from Belgium, Germany, Spain, Italy and Ireland.
The project’s overall objective is to engage adults and senior citizens in open-air exercise for the benefit of their health. The field of cancer prevention was chosen by UcanACT’s project partners due to the importance of this topic for European public health. Results of the pilot programme showed improvements across a number of outcome measures, and qualitative evaluation was also very positive. HSE physiotherapy community services in Carlow and Kilkenny welcome future opportunities to support this pathway, which exemplifies a collaborative and communitybased physical activity programme for people at risk of cancer, those living with cancer and also survivors of cancer.
Updates from HSE Dublin and South East

State-of-the-art new mental health facility opens in Dungarvan
A major step forward for mental health services in the HSE Dublin and South East region took place on 28 February with the opening of Seabreeze – a new state-of-the-art, high-support, community residence in Dungarvan, Co Waterford.
Developed on a standalone 1.9 acre site on the town’s Youghal Road, Seabreeze comprises of two blocks hosting 10 en-suite single bedrooms and two apartments, with an adjoining third block featuring communal facilities and administrative offices. This new purpose-built facility replaces accommodation previously provided at Springmount House, which is located on the grounds of Dungarvan Community Hospital.
Seabreeze was officially opened by Government Chief Whip and Minister of State at the Department of Health with special responsibility for Mental Health Mary Butler TD. Welcoming the Minister and also speaking at the official opening of Seabreeze, Dr Sinéad Reynolds, Integrated Healthcare Area Manager for Waterford Wexford said, “The HSE are here to support those with mental health needs and we encourage individuals and their families, in the event
of any issue they have, to make contact with a GP or to consult the various services. The HSE’s dedicated mental health staff, based in its facilities and in the community, are committed to the provision of a highquality and safe mental health service to the population we serve. In that regard, we are delighted to have the Minister with responsibility for Mental Health here with us in Dungarvan today to mark our investment in upgrading our facilities. The role and function of Seabreeze, as a high-support community residence, is to enhance the personal autonomy of adults with enduring mental illness and to enable those individuals to lead as fulfilling a life as possible.”
In a project led by HSE Estates in collaboration with HSE Dublin and South East’s mental health services, the Seabreeze complex was designed by Paul O’Toole Architects. Its construction by Mulcahy Construction Ltd began in November 2022. By November of last year, occupants of Springmount House moved into the upgraded new surroundings of the fully completed Seabreeze. The facility has been nominated in the healthcare projects category of the Irish Building and Design Awards 2025.


Digital for Care

Driving safer, connected and patient-centred care, improving healthcare delivery for both staff and patients in Ireland


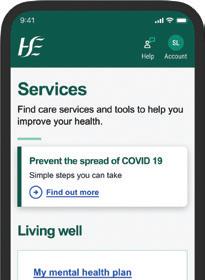
Encourage patients to download and use the HSE Health App today
Over 75,000 people have downloaded the HSE Health App since its launch in February, a major milestone in the HSE’s Digital for Care plan for 2025. Features available in the first release include:
• Digital versions of your European Health Insurance Card, Drug Payment Scheme, long-term illness and medical cards
• Hospital appointments for maternity services
• List of self-declared and reimbursed medication
• COVID-19 and flu vaccination records
• Information about urgent and emergency care services
• Health A-Z
Did you know you can see digital versions of your European Health Insurance Card, Drug Payment Scheme, longterm illness and medical cards on the HSE Health App?
We’re urging you to download the HSE Health App and give feedback and suggestions so it can be continuously improved. You should encourage people who use our services to download and use the app too, especially those in maternity settings. For maternity patients, the app lets them check their upcoming, past and cancelled hospital appointments from their smartphone.
Support and accessibility
HSE Live is there to provide support to people if they need it when using the app. If people don’t want to or can’t use the app, they can still access services and healthcare in the usual way.
Evolving over time
The HSE Health App team are now working with nominees from each health region to make appointments available in the app across our acute hospitals and specialities by the end of this year.
Other enhancements planned for this year include support to quit smoking and week-by-week healthy pregnancy information. More ambitious plans are in development as the HSE invests in additional digital systems to support services and staff.
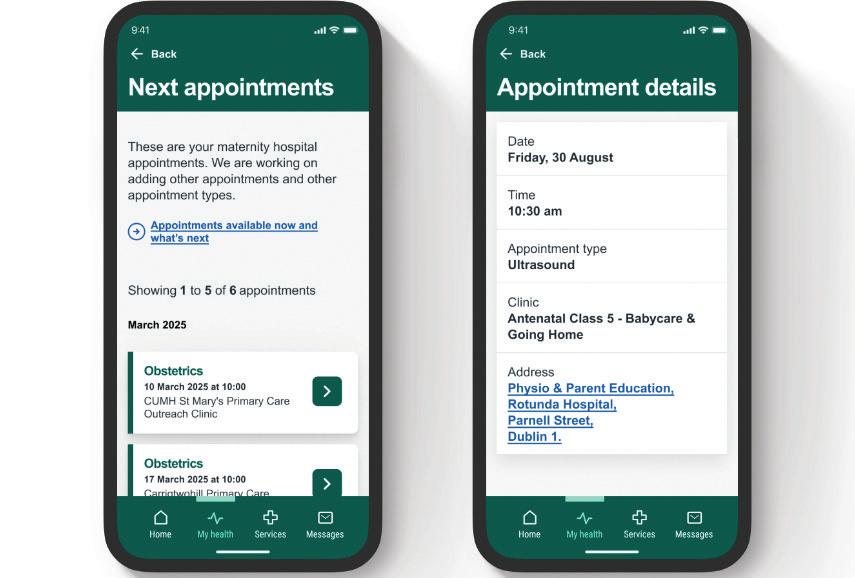
These are some of the planned future app features:
• Appointment notifications and reminders
• Acute hospital appointments
• Quit smoking support
• Prostate cancer self-care pathway
• Chronic disease management support
• Web chat support
You can find more information and download the HSE Health App from hse.ie/health-app You can download the app from Google Play or the App Store.
Digital for Care
Using data to increase patient access to surgical care
The HSE’s National Perioperative Patient Pathway Enhancement Programme (NPPPEP) is taking a closer look at how we use one of our health system’s most valuable assets – our operating theatres.
Driving sustainable change
Supported by the HSE Chief Clinical Office, the Royal College of Surgeons in Ireland (RCSI) and the National Clinical Programmes for Surgery and Anaesthesia, NPPPEP is part of a broader national strategy to improve scheduled care.
The goal is to use data to drive practical improvements that help more patients receive the right care, at the right time, in the right place. By creating a system that identifies and reduces constraints, NPPPEP enables theatre time to be used more effectively, allowing more patients to be treated.
A whole-system approach to surgical care
There are many factors, beyond the operating theatre itself, that impact the efficiency and effectiveness of operating theatres. NPPPEP takes a system-wide view of the perioperative pathway, incorporating the full surgical journey, from pre-assessment to discharge. This broader perspective captures how delays, cancellations and bottlenecks across the hospital impact theatre flow and, ultimately, patients’ access to care.
From data to action
NPPPEP is designed to be practical and actionoriented. At the heart of the programme is the use of standardised national metrics to track how operating theatres are used. By using consistent, real-time data, hospital and regional teams can identify additional capacity that allows more patients access to surgical care.
Hospital teams regularly review data on theatre access, capacity and flow to inform improvements. A multidisciplinary team approach, including surgeons, anaesthetists, theatre nurses and hospital management, ensures that changes are driven by those closest to the work. Teams are supported with structured training, coaching and ongoing guidance.
Early results and expansion
Since the pilot programme was introduced in South/Southwest Hospital Group, 108 theatres and procedure rooms have successfully adopted this model. These include:
• Reeves Day Surgery Centre, Tallaght University Hospital
• Roscommon University Hospital
• Midlands Regional Hospital Tullamore
• St Michael’s Hospital, Dún Laoghaire
• St Vincent’s University Hospital
• University Hospital Galway
• Sligo University Hospital
Building on this momentum, the programme is now expanding to additional sites, including:
• Beaumont Hospital
• Connolly Hospital
• Midland Regional Hospital Portlaoise
• Midland Regional Hospital Mullingar
TECH workshop with Google volunteers in Carew House
“What’s a podcast?” This question, posed by a man attending an anxiety management group, prompted colleagues in Older Adult Mental Health services to run a project to bridge the digital divide for older adults. Staff teamed up with volunteers from Google Inc to host a workshop at Carew House, on the grounds of St Vincent’s House, aimed at demystifying using phones and tablets to access the internet. Input from a service user ensured relevance and Google staff covered internet safety and access. Participants reported increased confidence with terminology, and many learned new ways of managing their devices. This project highlights the need for further workshops to support service users who might be apprehensive about seeking this support elsewhere.
NPPPEP is proving that real-time, standardised data, when combined with local expertise and multidisciplinary collaboration, can lead to meaningful, lasting improvements in surgical care. As more hospitals come on board, the programme is helping to create a more responsive, efficient system that works better for patients and staff alike. We are laying the groundwork for a more sustainable and equitable model of surgical care, one where more patients can access the procedures they need, when they need them. |
Digital for Care
Care closer to home: how video consultations are improving accessibility in Wexford
Liz Murphy, Cardiovascular Specialist Nurse with the ECC Chronic Disease Hub in Enniscorthy, shares how an Attend Anywhere telehealth pilot in Wexford is enhancing healthcare accessibility and efficiency for patients.
When Storm Éowyn forced the cancellation of a 93-year-old patient’s cardiology assessment for the third time, Cardiovascular Specialist Nurse Liz Murphy saw an opportunity. Thanks to a new video consultation pilot using Attend Anywhere, Brigid O’Brien could still attend her cardiology appointment – without leaving the comfort of her home.

Brigid, from New Ross, who is living with the effects of a stroke in 2023 and has significant mobility issues, had previously found it difficult to attend in-person appointments. Her daughter, Catherine, explains: “My mother was due to have an in-person appointment with Liz, which unfortunately needed to be rearranged twice due to Mam being ill. When a video consultation was suggested, we jumped at the chance. There was no need to book a wheelchair taxi, no stress about going out or worries about infections. Once Mam heard she could do the appointment from her chair, she was delighted.”
Liz sent Catherine a video link, which worked seamlessly from her phone. “Liz introduced herself to Mam, and since Mam’s hearing is practically gone, I was able to communicate to her any information she missed. This was great as Mam is used to my voice – it made it easier for her to understand,” says Catherine.
Together, they completed a full consultation at home. Catherine took blood pressure readings and checked for fluid in Brigid’s legs under Liz’s guidance.
“The appointment lasted about 30 minutes, and afterwards Liz sent all the information to Mam’s doctor, along with medication recommendations. I honestly couldn’t recommend the video
consultation enough. It was stress-free and made a huge difference for our family.”
Liz explains: “Brigid had been struggling to attend her in-person cardiology appointments. With Storm Éowyn causing further disruptions, it became clear that she needed an alternative way to access care.
With the support of her daughter, Catherine, Brigid was able to complete her assessment via video consultation using Attend Anywhere. It even allowed her son to take part, making it a truly inclusive, patient-centred experience. Despite the severe weather, she got the care she needed, right from her home, showing just how valuable video consultations can be.”
The introduction of the Attend Anywhere pilot at the Wexford Chronic Disease Hub has had a significant impact on both patients and healthcare delivery.
• A post-trial evaluation with 12 out of 19 patients showed a 100% reduction in missed appointments, as virtual consultations removed barriers that often led to non-attendance.
• Video consultations were also 68% more time-efficient than face-to-face visits, while saving a total of 1,029 km in travel distance and nearly 19 hours of travel time for patients.
• Feedback was overwhelmingly positive, with patients describing the experience as “the best appointment I’ve had” and “a game-changer”.
Attend Anywhere video consultations
Attend Anywhere enables healthcare staff to offer video consultations to patients. It’s now being rolled out nationwide to Enhanced Community Care (ECC) teams.
Benefits of video consultations:
1. Better access to healthcare
2. Increases patient choice
3. Saves on time and travel
4. Improves flexibility
5. Patients are less likely to cancel or not attend their appointments
6. Enhances patient experience and engagement
7. Supports integrated care – multiple clinicians or family members can participate on a call
To learn more, visit the Enhanced Community Care hub on HSeLanD and the ECC Community on Viva Engage. To get involved, email eccmetrics@hse.ie.
Virtual Fracture Assessment Clinics – a new approach to orthopaedic care
Virtual Fracture Assessment Clinics (vFACs) are consultant-led services designed to manage stable fractures through a virtual, multidisciplinary approach. Introduced early in the COVID-19 pandemic, vFACs have since become an integral part of routine orthopaedic care. These clinics align with international best practices by prioritising patient safety, efficiency and experience. vFACs reduce the need for unnecessary hospital visits by ensuring that only patients requiring in-person assessment are referred to traditional fracture clinics. This approach streamlines care, enhances patient satisfaction and conserves valuable healthcare resources. Led by consultant orthopaedic surgeons and supported by a multidisciplinary team, vFACs enable timely clinical decision-making and promote continuity of care. Their proven effectiveness supports a more responsive and patient-centred healthcare model, optimising outcomes for individuals with stable fractures while relieving pressure on busy outpatient departments. vFACs exemplify innovation in care delivery, demonstrating how virtual models can enhance service quality in a modern health system.
The SMILE programme is transforming the way patients with chronic illnesses manage their health
“I know before I know”: a patient’s journey with SMILE
Five years ago, Paul Wallace’s life changed after emergency surgery revealed not just spinal issues, but that his heart was functioning at only 10%. With intensive treatment, his heart function improved to 40% but managing multiple chronic conditions became his new reality.
That changed when Paul joined SMILE (Supporting Multi-morbidity self-care through Integration, Learning, and eHealth), a remote monitoring programme supporting patients with chronic diseases through daily self-checks and virtual care.
Using connected devices and the ProACT digital platform, patients monitor their health at home.
Real-time data is sent to the SMILE nursing team, who can escalate concerns to specialists if needed.
“Patients’ readings come to our screens daily,” explains Niamh Ann
Flanagan, SMILE Clinical Lead Nurse. “If anything is off, we call them straight away to prevent deterioration.”
“The SMILE programme has changed the way I manage my health condition, it has given me a regime,” says Paul. “I check my vitals – blood oxygen, heart rate, blood pressure – every day. It’s helped me feel in control of my health.”
SMILE 2 is part of the Enhanced Community Care (ECC) programme, delivered in partnership with Caredoc and chronic disease community specialist teams.
Covering Carlow, South Tipperary, Kilkenny, Waterford and Wexford, it serves over 500,000 people and was developed in direct response to a need from patients. This proactive, integrated approach improves care while reducing pressure on hospitals and GPs. For patients enrolled in SMILE 2 for a period of six months, the project saw:
• 55% reduction in emergency department visits
• 75% fewer hospital bed nights
• 81% drop in GP visits
For more information visit bit.ly/HSESMILE2Report
Watch a video featuring patient Paul Wallace; Dr Anna Marie O’Brien, GP; Liz Murphy, Cardiovascular Nurse Specialist; and Niamh Ann Flanagan, SMILE Nurse, as they share their experiences with the programme: bit.ly/HSESMILE
Some 94% of patients reported improved wellbeing, and 72% saw stabilisation in symptoms – more than double the original target. Patients feel informed and supported, a sentiment echoed by healthcare professionals.
“SMILE empowers patients to manage their own care because they have access to their own information,” says Dr Anna Marie O’Brien, GP at Abbey Medical based in Wexford Primary Care Centre.
For cardiovascular nurse specialists like Liz Murphy, who is based at the Wexford Integrated Chronic Disease Team, the ability to access live patient data is a gamechanger: “I can look at the data, make a clinical decision, confirm with [the patient] over the phone that it is accurate, send a prescription to their pharmacy, and I would estimate that it’s probably reduced their amount of clinic visits they require by 80%.”
SMILE 2 covers eight chronic diseases, including heart failure, diabetes, COPD and asthma. It offers a scalable blueprint for integrated chronic disease management nationwide.
“The future of my health feels less uncertain,” says Paul. “SMILE helps catch problems before I even know they’re there.”
Updates from HSE South West
Dr Andy Phillips
HSE South West Regional Executive Officer
Making our Cork and Kerry communities proud of their health service
We formally stood up Cork and Kerry’s new integrated health region, HSE South West on 3 March 2025 and I am very proud of the progress we have made since.
All our staff have risen to the challenge as we moved our governance from the old hospital group and community healthcare organisation structures to HSE South West, which is now responsible for delivering all health and social care services across Cork and Kerry.
Our whole team is focused on delivering health services that the people of Cork and Kerry can be proud of. The current priority is moving to delivering integrated care seven days a week with a commitment to rostering over 10% of our staff to work across weekends by the end of June 2025.
Our staff can be very proud of their commitment to patient care and the improvements made to the quality of
many services. We have much work still to do in reducing waiting times – particularly for children with disabilities – for improving mental health services, delivering health equality, and for supporting people to look after their health and wellbeing.
In standing up HSE South West, our commitments to the people of Cork and Kerry are:
• We value your time.
• We put ourselves in your shoes.
• We involve you as equal partners.
• We avoid harm to patients and staff and continually work hard to improve our services seven days a week.
Our commitments to staff are:
• We live our values every day.
• We support each other to be the best we can be.
• We are one system, one team and one budget.
• We govern our services with transparency, accountability, participation, integrity and capability.
These 8 commitments are based on the HSE values of care, compassion, trust and learning.

Building the culture of HSE South West, the way we do things around here is my key priority, which is why we’ve been working on a programme based on these 8 commitments, which we call Integr8.
A series of workshops is supporting staff to make real these 8 commitments as part of our Integr8 programme. That programme has extended from an initial cohort of 30 to a wider group of 300, who all have my authority as REO to transform the health system in Cork and Kerry by living the Integr8 commitments every day to make our communities proud of their health service.
In the second week of May, we held Gatherings of Kindness at three of our sites across Cork and Kerry. These joyful events, led by staff on the ground at Cork University Hospital, University Hospital Kerry and St Mary’s Healthcare Campus in Cork city, provided us with the opportunity to join together and appreciate our joint work in creating a safe, supportive environment for patients and colleagues alike.
The HSE South West’s Gathering of Kindness events were uplifting occasions where we hosted a diverse array of events and activities dedicated to nurturing kindness in healthcare settings across Cork and Kerry. We had tree-planting ceremonies, theatre performances by local theatre group Graffiti Theatre Company, live music performances, and thoughtprovoking discussion forums –including a very special address by Professor Catherine Crock from the Hush Foundation and inspirational talks from Professor Brian Dolan.
I am really heartened by the efforts of our staff across Cork and Kerry. It is clear to me that working together, we can really impact our organisation’s culture of kindness – making positive changes to enhancing our wellbeing, creating stronger teams, and improving patient care.
Updates from HSE South West
New endometriosis centre provides specialist care for women
Minister for Health Jennifer Carroll MacNeill TD officially opened the HSE’s Supra-Regional Endometriosis Centre in Cork to improve access to care for women with advanced endometriosis. The state-of-the-art centre, which is already seeing patients from across Ireland, is located at the Lee Clinic and operated by Cork University Maternity Hospital (CUMH).
Endometriosis is a condition in which tissue, similar to the lining of the womb, grows outside of the womb, affecting approximately one in 10 women globally. The Endometriosis Centre at CUMH will provide comprehensive, tailored and specialist care for women.

Developed by the HSE and the HSE National Women and Infants Health Programme (NWIHP), this centre aligns with the National Endometriosis Framework. The framework outlines, for the first time, a defined clinical care pathway for women with endometriosis in Ireland.
Professor John R. Higgins, Professor of Obstetrics and Gynaecology, UCC; Clinical Director, Ireland South Women
Problem drug use study launched
The first-ever report into problem drug use in Cork city, which was co-funded by HSE South West, found that there are over 850 opioid users in Cork, with one-third of these not currently availing of the treatment services.
The study, “Problem Drug Use in Cork City, a study on Prevalence and Harms”, commissioned by HSE South West and Cork City Council, examined the scale of problem drug use in Cork city using multiple data sources, and estimated that there were 859 problematic opioid users in Cork city in 2022. The research was undertaken by the School of Public Health at UCC, aided by colleagues in the Health Research Board and National Suicide Research Foundation.
and Infants Directorate says, “Endometriosis has long been a Cinderella condition – often underdiagnosed and undertreated. It is wonderful to see the government investing in a truly national endometriosis service, of which we can all be proud. We are determined to ensure that world-class services are available for every woman in the wider Munster region.”
David Lane, HSE General Manager for Social Inclusion says, “The HSE team work every day to support problematic drug users but to solve addiction issues, we also need to have reliable research to guide us in planning supports and services. This report is a milestone which marks the HSE’s commitment to strengthen the region’s response to support very vulnerable people and provide compassionate, community-based support for individuals on their path to recovery from addiction. HSE South West believes that recovery is possible when individuals are given the right support and tools, and we witness the transformative power of recovery every day.”
The study can be found at drugsandalcohol.ie/42736
Telemedicine initiative expanded across Kerry
Kerry community mental health patients benefitting from a transformative telemedicine initiative have reported that their experience of the video consultations have been largely positive.
North Kerry Community Mental Health Services began offering adult video consultations through a pilot telemedicine initiative in late 2022, under the guidance of Executive Clinical Director Dr Maura Young. The telemedicine model had already been introduced to younger people under the care of South Kerry CAMHS.
The initiative provides outpatient mental health services and offers service users video appointments with a consultant based in another country. The initiative is the first of its kind in an adult community mental health outpatient clinic in Ireland and came about as a practical response to recruitment difficulties.
Recent research into the pilot has found that both clinicians and service users found their experiences of telemedicine largely positive. Two qualitative research studies were conducted involving clinicians and service users to explore their experiences. The service user experience study was completed by Orla Healy and Bridget Langford; while the staff perceptions piece was completed by Dr Sinead Hanafin and Bridget Langford.
Feedback from patients included:
• “Whether they are in the chair beside you, or on the screen, it’s the same thing. I felt really listened to.”
• “I can see it makes a lot of sense in relation to reducing people’s time on the road, reducing waiting times in waiting rooms.”
• “I found it reassuring; it is good to have someone there just in case I get upset or if something happens to the video call. She was able to explain things to me if I couldn’t quite get what the doctor was asking.”
• “It is something that I can see helping a lot of people.”
Patients also recognised the continuity of care they receive and the flexible treatment options available. Many welcomed the innovation and highlighted the benefit of having staff present to support the process.

row, from left: Bernadette Fitzgerald, ADON; Sinéad Connaire, Director, NMPDU, HSE South West; Dr Ana Goles, Consultant Psychiatrist (on TV screen); Bridget Langford, CNS; and Dympna Griffin, Telemedicine Admin. Front row, from left: Orla Healy, Psychology Assistant; Eimear McWalters, Psychology Assistant; and Michael O’Shea, A/CMHN. Photo by Sinead Hennessy, Practice Development Co-ordinator.
The entire team at North Kerry worked together to ensure that the service works for staff and patients. They have developed a protocol that defines the responsibilities of all staff, so that service users receive the best possible care. Service users attend their outpatient clinics in person and are supported by a psychology assistant during their video consultation with the remote consultant psychiatrist.
The team have observed that people are more likely to attend a telemedicine appointment and have attributed this to the fact that team administrators are in contact with patients beforehand to confirm consent for the telemedicine appointment.
Both clinicians and service users expressed a preference for a hybrid model, balancing virtual and face-to-face care, with clinicians recognising that in-person sessions remain the gold standard.
Supported by strong governance, multidisciplinary collaboration, and ongoing service user feedback, telemedicine has proven to be a viable and effective alternative in delivering mental health services, with promising implications for future service development.
Updates from HSE South West
Developing HSE South West culture through Integr8 workshops
More than 300 HSE South West staff have attended Intgr8 workshops in recent months, supporting them to make real HSE South West’s 8 commitments, which are based on the HSE values of care, compassion, trust and learning. The staff taking part in the series of workshops are developing awareness and skills in order to embed these values into the fabric of HSE South West, and day-to-day behaviours and decisions.
HSE South West REO Dr Andy Phillips says, “My main role is to set the culture of the organisation, centred around the people of Cork and Kerry being proud of their health service. We’ve worked together to make these Integr8 commitments centred around the core HSE values. We are holding ourselves to account by delivering on those commitments, such as valuing patients’ time.”

Regional Director of People for HSE South West Deborah Harrington says, “The energy and enthusiasm at these workshops was palpable. They really demonstrated that colleagues in HSE South West are committed to the values of care, compassion, trust and learning – but also what caring, creative and dedicated people work across our organisation. Core values only work
HSE South West marks National Health and Social Care Professionals Day
HSE South West marked the nationwide celebration of Health and Social Care Professionals (HSCP) Day, honouring the essential contribution of over 2,500 HSCPs working across Cork and Kerry.
The HSCP workforce represents one of the most diverse and dynamic groups within the health service, encompassing 26 distinct professions across diagnostic, therapeutic and social domains. In recognition of HSCP Day 2025, events took place across HSE South West sites, celebrating the ongoing commitment of HSCPs to improving the health and wellbeing of their communities. Highlights of the celebrations included an all-day research poster display, a showcase of innovative work, and Cork City Hall was illuminated in orange.
if they are embraced and championed by all of us and when they guide our everyday actions; such as how we behave around each other and our communities, and how we make decisions. These workshops are a great support in helping us to bring these values to life. I want to thank everyone who attended. It was great to see colleagues making new connections and getting to know each other.”
This year’s theme, Innovating Health and Social Care: Embracing Technology, Research, and Evidence, highlights the transformative impact of these staff in advancing patient care and service delivery through innovation and evidence-based practice. Sarah Shanahan, HSE South West Health and Social Care Professions Regional Integration Development Lead says, “HSCP Day is an opportunity to recognise the incredible innovation happening across Ireland’s health and social care professions. These professionals are the drivers of change – adapting services to better meet the needs of people and communities; and embedding research and technology into everyday care. We are incredibly proud of their contribution.”

Endoscopy unit opens at Bantry General Hospital
A new endoscopy unit has become operational at Bantry General Hospital. The team at Bantry General Hospital are proud of this new, modern, patient-centred facility, which is a significant development for the hospital. It has two procedure rooms, six recovery bays, a discharge lounge and a welcoming reception area. The project cost was in excess of €8m.
Opening this purpose-built unit will lead to an increase in the level of endoscopy activity undertaken at Bantry General Hospital and will assist in addressing endoscopy waiting lists across the HSE South West region.
Integrated Healthcare Area Manager for Cork South and West Priscilla Lynch says, “This exciting development of a new endoscopy unit at Bantry General Hospital represents a vital investment in the health and wellbeing of the people in West Cork. This modern facility will enhance our diagnostic capabilities, reduce waiting times, and ensure patients have access to high-quality care closer to home. This investment benefits not just the people of West Cork, but the wider population as the unit is receiving referrals from across the South West region. We are proud to take this important step forward in expanding services and supporting better outcomes for our community.”
General Manager of Bantry General Hospital Carole Croke says, “The opening of the new endoscopy unit is a significant milestone for our hospital and the wider community. It not only enhances the range of services we can provide locally, but it’s also a testament to the dedication and collaboration of our exceptional team.

The supportive, professional environment here in Bantry has been key to bringing this project to life, and we look forward to continuing to deliver safe, high-quality care in this state-of-the-art facility. We expect that this new unit will allow us to double the endoscopy activity at the hospital over the next 18 months. Feedback from patients already has been very positive, and it’s also been great to see that staff feel this is a very positive environment to work in.”
The new unit can carry out a range of endoscopy services including colonoscopy, gastroscopy, proctoscopy and sigmoidoscopy. It can carry out not just diagnostics, but also therapeutic services as well. Referrals typically come electronically from community services, particularly GPs and are triaged by the clinical team based on symptoms.
Updates from HSE South
Community Healthcare collaboration sees Listowel celebrated as a dementia inclusive town
The Community Healthcare team in HSE South West have been supporting local services, businesses and organisations to work collaboratively over the last three years, and help to increase awareness and improve support for those living with dementia in Listowel, Co Kerry.
Dementia Inclusive Listowel, an initiative launched in late 2022, recently celebrated Listowel becoming one of Ireland’s first dementia inclusive towns. This milestone will feature in a national advertising promotion with the HSE’s Dementia: Understand Together campaign. The group have hosted dementia-training workshops for more than 100 people and organisations, and held two information evenings with more than 250 people attending. This is a long-term project, with a commitment from the community to keep the conversation, education and understanding going.
Dolores McElligott, Team Leader, Community Worker, who features in the new videos, says, “Dementia is not just a health issue, it’s a social issue and requires a community response. Most people with a diagnosis of dementia are living in their communities; it’s vital that they can continue to access businesses, services and amenities that understand their needs, and be able to remain active and engaged.”

If you’d like to learn more about the work of Dementia Inclusive Listowel, email understandtogether@hse.ie | Watch the video here: bit.ly/DementiaInclusiveListowel
Cork libraries and HSE South West join forces to support Your Good Self
Your Good Self, a joint initiative between the HSE and Cork County Library and Cork City Libraries, is providing trusted, quality information on emotional wellbeing to people in Cork.
HSE South West experts, including psychologists, have compiled an extensive list of books, websites and other recommended resources. Details of these materials are promoted in libraries across Cork city and county, and on the websites of the Cork city and county libraries.
All materials, which have been approved by experts in Primary Care Psychology Services in Cork, provide information, knowledge and ideas on how best to deal with life’s challenges.
The resources are practical and helpful and cover an extensive variety of topics including parenting, stress management and self-esteem, and the overall aim of the programme is to provide quality information on how to look after one’s emotional wellbeing as part of overall health.
Lists of these materials are available on the links below, in local participating libraries and on the Cork county and city library websites.
Psychologists in Primary Care in Cork city and county also regularly do free public talks in libraries on emotional wellbeing topics.
Resources For Adults: bit.ly/YourGoodSelfAdults For Children and Families: bit.ly/YourGoodSelfChildren Booklet: bit.ly/YourGoodSelfInfo

New report shows important role of community champions in improving equity in screening
A new report shows the impact of community champions who are reaching people who might not otherwise choose screening. The report was published by the HSE’s National Screening Service, which encompasses the three national cancer screening programmes: BowelScreen, BreastCheck and CervicalCheck; as well as Diabetic RetinaScreen, which screens for retinopathy in people who have diabetes.
Community champions are health workers who are trusted, respected and influential within their communities. They are typically advocates, or individuals who have strong ties to a specific group or population. Their role is to bridge the gap between healthcare providers and people in their communities, fostering trust and encouraging participation in health initiatives, including screening programmes.
The National Screening Service (NSS) developed a training programme and new resources to support this work, including:
• An interventions toolkit
• Animated videos that explain what happens at screening
• Presentations about our four screening programmes
• A communications partner pack
The NSS provided access to an online training platform that has additional tools and resources to support the community champions, as well as advice from access officers, screening programme staff and the health promotion team.
For the pilot project, the NSS trained 40 people across five sites in Cork HSE, Kerry HSE, Dublin city co-op, Galway, and Dublin South, Kildare, West Wicklow Community Healthcare area. The project included peer support workers, community
health workers, migrant support workers, Roma support workers, and health promotion staff.
The evaluation report shows that the training helped to build the confidence of community champions, and that they reached people in many communities including migrants, Roma, Travellers, disabled people, homeless people, the LGBTQIA+ community, refugees, people who live in deprivation, and people with addiction.
Some of the barriers to screening identified by community champions included fear of diagnosis, relocation issues, language barriers, logistical challenges and cultural factors. Some of the challenges included addressing symptomatic health issues and explaining abnormal results. This highlighted the need for more training materials and support in these areas.
Senior Health Promotion Officer with the NSS, Lynn Swinburne says, “We will continue to provide training and support to our community champions, while also building our network and training additional people. We will regularly assess the impact of the work being carried out by our community champions, identify and respond to areas for improvement, and ensure that the project is continually meeting its objectives.”
This year, the community champions project is working with the Roma health network, training a total of 30 champions.
Find out more about the work being done to improve equity in screening at hse.ie/equityinscreening
Tick awareness
Practical advice on how to protect against tick bites

People spend more time outdoors in the summer months and anyone who spends time outdoors should protect themselves against tick bites. This includes ramblers, campers, mountain bikers, people who work or walk in woodland, parkland and heathland, especially in grassy areas. Preventing tick bites prevents Lyme disease.
Ticks are present everywhere in Ireland, including urban and rural areas, and are active from spring to autumn. They are tiny spider-like creatures that feed on the blood of humans, animals and birds, and are more numerous and active in the summer.
From April onwards is when we see cases of Lyme disease most frequently in Ireland, because it’s when more ticks are around.
Tick bites can be prevented by:
• Wearing long trousers, a long-sleeved shirt and shoes.
• Wearing a hat and tucking in hair.
• Using an insect repellent (preferably containing DEET).
• Checking skin, hair and warm skin folds (especially the neck and scalp of children) for ticks after a day out.
• Checking for ticks and removing any from your pets/clothing/outdoor gear.
• Removing any ticks and consulting with a GP if symptoms develop.
Ticks will bite adults most commonly on the legs and arms. But they can bite any part of the body, especially warm and sweaty parts not covered by clothing. In children, ticks are most likely to bite around the head and neck. These are the areas to cover up and protect, and to check after playing outdoors.
Rash
Most cases of Lyme disease are very mild, and many infected people may not have symptoms. The most common sign of infection is a skin rash (commonly known as a “bullseye” rash). In a small number of cases, the infection can be more severe, leading to serious nervous system, heart and joint disease.
Anyone who develops a rash or other symptoms should visit their GP and explain they have been bitten by a tick. If you think you may have been bitten and develop a skin rash, speak to your GP, who may prescribe antibiotics if it is likely to be Lyme disease, which will clear the infection.
How to remove a tick
Some ticks can carry Lyme disease. If a tick is removed within the first few hours, the risk of infection is very low. The entire tick, including its mouthparts should be removed with tweezers by gripping it close to the skin. Wash the skin where the tick was found with soap and water and check over the next few weeks for swelling or redness.
Step by step instructions on how to remove a tick are available at bit.ly/TickBiteLyme


Spotlight on HR






A round-up of some of the services and supports available











HR and Payroll Self Service update
In April 2025, the HSE reached a major milestone with all statutory HSE areas now live on SAP HR and Payroll system.
“We are now paying 186,115 employees and pensioners, made up of 158,450 in the statutory HSE and 27,665 in non-HSE areas, through the SAP HR and Payroll System,” says Bernard Gloster, CEO of the HSE. “The successful implementation of the SAP HR and Payroll solution throughout our entire organisation is an impressive accomplishment for the HSE. The effective use of consultation, engagement, teamwork and diverse support in this delivery process has driven real change. The introduction
of the solution has established a robust ‘hire to retire’ management system for HSE employees.”
What is HR and Payroll Self Service?
This is an online tool that allows employees to view payslips, view or change personal information, submit leave and travel requests. Managers use it to approve travel and leave as well as access a variety of reports.
HR and Payroll Self Service –how to get started
If you have yet to register, it only takes a few minutes. Scan the QR code and complete the instructions.







New e-learning programme: Inclusive Recruitment – Building a Better Workforce
HR Shared Services Recruitment Quality Standards unit has launched a new e-learning programme, Inclusive Recruitment – Building a Better Workforce, designed to enhance the diversity, equality and inclusion (DEI) skills of all those involved in the recruitment process within the HSE. The programme helps to bring a DEI focus to recruitment and interview practices, ensuring that hiring managers, HR staff, and interview board members are equipped to attract and retain a diverse workforce. Learners will gain practical insights into how DEI can improve recruitment and interview activities through creating inclusive job descriptions, attracting the widest pool of candidates, and managing reasonable accommodation requests for interview candidates.
How can I find out more about HR and Payroll Self Service?
There are video tutorials and step by step guides on the NiSRP support site.
There are HR and Payroll Self Service modules (Employees and Manager and Approvers and Travel) on HSeLanD.
The NiSRP helpdesk is available by email: support.nisrp@hse.ie and phone, Monday to Friday from 9am to 4.30pm: 0818 300 296.
For more information, including the video tutorials and guides, visit hse.ie/nisrp

With a completion time of approximately 30 minutes, the module offers interactive knowledge checks, scenario challenges, and a summative assessment to reinforce learning. Participants who successfully complete the course will receive a certificate of completion.
The course complements the existing HSE Recruitment Interviewer Skills and Chairing Interviews Effectively modules on HSeLanD and should be completed by all those involved in HSE selection boards in order to gain confidence and skills in this important area.
To access and complete the e-learning course, search for ‘Inclusive Recruitment – Building a Better Workforce’ on HSeLanD.
Retirement Form HR107(a)
The HSE pensions team has launched a video to guide staff through completing the Retirement Form HR107(a) – this is a key step in the retirement process.
Now available on YouTube, the short video clearly explains each section of the form, using step-by-step instructions and a sample completed version to make the process as straightforward as possible. For those who prefer a printed copy, a completion guide is also available on the pensions website for viewing or download.


This is part of a broader update to the pensions website, which now offers clearer, more accessible information on the HSE pension schemes, the retirement journey, and what to expect after retiring.
Whether you’re preparing to retire or supporting a colleague who is, this video is an essential tool to help get the paperwork right.
Updates from HSE Mid West
Hospital-standard care for patients in the comfort of their own homes
A new Virtual Ward in University Hospital Limerick (UHL), which uses technology to provide patient care at home has saved more than 2,000 inpatient bed days since its introduction last summer; 325 patients were cared for in the Virtual Ward between July 2024 and the end of February 2025. Patients used technology to link with UHL for monitoring two to three times daily, in the process freeing up 2,053 bed days for hospital treatment of more acutely ill inpatients.
“The Virtual Ward is about ensuring high-quality care in patients’ homes, enabled by technology. This new model of care empowers our patients through increased knowledge about their health and self-management of their conditions,” says Patricia O’Gorman, Nurse and Midwifery Informatics Officer, who led the implementation of the Virtual Ward at UHL.
Patients referred from the hospital’s emergency department, acute medical assessment unit and medical wards receive a full technology kit, including a tablet and medical diagnostic equipment. At home, this equipment links the patient with a central hub in UHL, allowing for 24/7 monitoring. Average length of stay on the UHL Virtual Ward is 6.6 days.
The Virtual Ward was implemented in collaboration with HSE National Strategic Programmes and eHealth offices, and in partnership with European virtual ward specialists Doccla.


Nurse and Midwifery Informatics Officer Patricia O’Gorman, who led the implementation of the Virtual Ward at UHL.
Minister for Health tours 96-bed block nearing completion at UHL

Updates from HSE Mid West
Arts and health awareness day at Nenagh Hospital

left: Ann-Marie
Eimear
Nenagh Hospital hosted an arts and health awareness day in February, offering staff, patients and visitors an opportunity to enjoy creative activities and to share ideas on how arts may benefit the health and wellbeing of the hospital community.
Part of the RENEW Group’s programme of work, the event was developed by the HSE National Healthy Ireland Team in partnership with Réalta, the national resource organisation
for arts and health, and delivered in partnership with Nenagh Hospital staff, Creative Ireland, Tipperary County Council and local artist Vi Bell.
Cathrina Ryan, Director of Nursing at Nenagh Hospital says, “We hope that our staff, patients and visitors enjoyed the day. We would like to thank everyone for taking time to engage and share their thoughts and we are excited to see where this may lead.”
Service users are a key element of Whose Shoes event in UMHL
Staff at the Specialist Perinatal Mental Health Services (SPMHS) in University Hospital Limerick (UHL) held a special Whose Shoes board-game-style event at University Maternity Hospital Limerick (UMHL) in April, looking at the experience of the service not just from the perspective of hospital staff and the SPMHS team, but crucially from that of service users. Representing all of these perspectives was essential to the success of the workshop, which is based on a boardgame guiding open discussion in a supportive workshop environment, on four major themes, covering the transition to parenthood; engaging with dads/becoming a dad; the role of professionals; and communication and language. The workshop was rated as excellent by the majority of
A new series of leaflets aimed at raising awareness of mental health within the Traveller community has been created by the HSE Mid West Mental Health Service and Traveller Primary Health Care Projects.
Winnie Harty, a Traveller Community Health Worker from West Limerick, emphasises the importance of the new leaflets within the Traveller community, where topics like mental health can still be taboo. During her outreach work, Winnie met someone who wanted this information for her aunt who frequently travels, so that she has vital support numbers to reach out for help.
participants, who also said it was extremely likely or likely that it would influence their thoughts on doing things differently in future.
Since the inception of the service at UMHL in April 2018, the SPMHS team has worked closely with its service users, taking every opportunity to involve them in planning events, in the education of staff and in research and audit.
Maria Gibbons, Registered Advanced Midwife Practitioner SPMHS/Birth Trauma said afterwards, “We have always enjoyed such huge support from our service users, and this event was no exception. They want to be involved, to share their stories and, most importantly, to help continually improve the service into the future.”

Health workers Bridgie O’Donoghue and Margaret O’Reilly shared a powerful moment when a woman recognised her anxiety symptoms after reading the leaflet, saying, “That’s what I have. I didn’t know what it was.”
Another leaflet aimed at addressing concerns about someone else’s mental health was
Traveller Mental Health Matters leaflets launched in Mid West
well received by Traveller community health workers in Clare. They expressed pride in the collaborative process of creating easily understandable material tailored for their community.
In North Tipperary, a new leaflet on grief and loss is in development, addressing another crucial topic for the community. Pearl O’Reilly noted that the goal is to provide accurate information and resources, ensuring Travellers understand mental health and know where to find help.
HSE launches new hub for medical research in the Mid West

HSE CEO Bernard Gloster has opened the first of the HSE’s new regional Research Directorates, at St Camillus’ Hospital Limerick, hailing the initiative as a key HSE commitment to advancing the delivery of modern healthcare.
“The best medical care in the world,” he said, “is built upon the latest scientific knowledge, and this knowledge is constantly being added to through research. Healthcare research makes new discoveries, it drives improvement, it makes treatments more effective and processes more efficient. Whether its focus is on technology, surgery, medicine or the patient experience, research helps improve health and social care for our patients and clients, and the HSE, through its Regional Directorates, is committed to supporting research and embedding it across our services.”
The Research Directorate Mid West, led by Prof Declan Lyons, will oversee all aspects of clinical research within the HSE locally, with the aim of promoting the advance of scientific knowledge and medical treatments.
From left: Mr Bernard Gloster, HSE CEO, officially opens the new HSE Research Directorate Mid West at St Camillus’ Hospital Limerick, with Ms Sandra Broderick, Regional Executive Officer, HSE Mid West, and Prof Declan Lyons, Mid West Regional Director of Research.
As a single point of entry for healthcare researchers in the region, the directorate will streamline researchers’ access to professional advice, expert regulatory support, and the infrastructure needed to conduct effective and innovative research.
At the official opening on Friday, 21 March, Prof Lyons said the opening of the directorate was “an important step for the HSE in driving the research agenda forward. In collaboration with our academic partners, our mission in the Mid West is to facilitate reliable, high-quality and innovative research across a range of fields relevant to the people of the locality.”
He cited as an exemplar of such research the recent trial of a comprehensive multidisciplinary assessment of older patients living with frailty who present to the emergency department (ED) at University Hospital Limerick (UHL). Led by Consultant Geriatrician Dr Aoife Leahy, the research identified key benefits for patients, including reduced wait times in ED, fewer hospital admissions, lower rates of ED reattendance and fewer nursing home admissions. Patients also reported better quality of life and function at 180 days.
Prof Lyons said such studies continue to drive improvement in healthcare, and his vision for the Research Directorate Mid West is to help foster a thriving research culture that enables innovative studies that will impact patient lives locally, nationally and internationally.
Prestigious RCSI honour for UHL surgeon, Associate Professor Christina Fleming

ShineVR Wellbeing initiative: a new era of employee support
The Mid West Health and Wellbeing team have unveiled a transformative innovation tailored for the region’s acute healthcare services. The ShineVR Wellbeing programme, which leverages immersive interactive virtual reality headsets, has been rolled out successfully at Croom, UHL, and Nenagh, with fantastic feedback from participants.
One staff member in cancer services at UHL said, “The environments were so soothing; I felt completely rejuvenated afterward.”
The key benefits of ShineVR Wellbeing include stress reduction, improved wellness, and enhanced memory and cognition. The team is in the process of scheduling sessions at the region’s other hospital sites later this year, with a plan to offer one dedicated day of ShineVR experiences at each location.
HSE Mid West Consultant Colorectal Surgeon, Associate Professor Christina Fleming (PhD FRCSI) recently had the honour of delivering the 47th Millin Lecture on the future of training in surgery to a standing-room-only audience at the Royal College of Surgeons in Ireland (RCSI).
Prof Fleming is an early adopter of surgical innovation, in particular robotic surgery, in which she first trained in at University Hospital Limerick (UHL). In 2016, UHL became the first public hospital in Ireland to install the Da Vinci Xi surgical robot. Almost a decade on, many hundreds of patients across multiple surgical specialities in the Mid West have benefitted from these surgeries, which are less invasive and significantly reduce the length of stay in hospital.
The Millin Lecture is one of the most prestigious accolades for surgeons in this country, and is the centrepiece of the annual RCSI Millin Meeting, which honours former two-term RCSI President Terence Millin, who pioneered prostate cancer surgery and trained surgeons worldwide to perform it.
Prof Fleming’s 2024 Millin Lecture argued for the need to think outside the box when training future surgeons with continuous advances in new surgical technologies, using current robotic surgery training as a template.
Prof Deborah McNamara, President, RCSI commended Prof Fleming for a fantastic talk “laying out an ambitious vision for the future of surgical training and practice”.

The key benefits of ShineVR Wellbeing include stress reduction, improved wellness, and enhanced memory and cognition.
A DAY IN THE LIFE OF...
Bernadette Mullins
Senior Health Promotion and Improvement Officer for Cancer Prevention, HSE Mid West
Working with the Cancer Prevention team at the HSE’s National Cancer Control Programme (NCCP), I find great satisfaction in helping people understand how to reduce their cancer risk and giving them the information and support they need to live healthier lives. I also really enjoy the diversity of my role. In the past month alone, I have worked with HSE staff in primary care, County Council outdoor workers, farmers, primary and secondary school students, Traveller Health Projects, and my colleagues in acute hospital services. This all keeps the job very interesting.

My mother is a nurse, which initially sparked my interest in a career in healthcare.
I am passionate about helping people, empowering them to take control over their own health, and supporting them in making informed health choices.
April was Bowel Cancer Awareness Month, and so was really busy with campaigns, education sessions, and events to promote bowel cancer prevention, symptom awareness, and screening. Another big focus has been the HSE and Healthy Ireland SunSmart campaign, which
runs from April to September. I work across two fantastic teams: the HSE’s NCCP team, and here in the Mid West I am based in the Health and Wellbeing division, working with the Health Promotion and Improvement team. Outside of work, I love kayaking, swimming, snorkelling and anything to do with the sea. I train with Kilrush Currach Rowing Club and live close to the sea in West Clare so I try to get a walk on the beach most days. I always make time for movement in my day, no matter how busy I am. Every move counts!
More children getting surgery closer to home, Limerick conference hears

More than 130 children to date have had surgery at University Hospital Limerick (UHL) under a new national model of care for general paediatric surgery, improving access for children and families and bringing surgical care as close to home as possible.
Prof Tara Connelly, Consultant General Surgeon with a special interest in paediatric surgery, updated attendees at the annual Sylvester O’Halloran Perioperative Symposium in March on the development of UHL as a regional paediatric surgical centre under the new HSE model of care launched in the Royal College of Surgeons in September 2024. In addition to Prof Connelly’s appointment, UHL also became the first centre in Ireland to welcome a visiting consultant paediatric surgeon from Children’s Health Ireland (CHI), Ms Nicola Brindley, who commenced running theatre lists and CHI’s UHL Outreach Surgery Clinic in Limerick in 2024.
While UHL has for many years provided acute surgical care for children, as well as subspecialities including ear, nose and throat (ENT), orthopaedics, dental and maxillofacial surgery; the majority of patients requiring general paediatric surgery have until recently had to travel outside of the region for their procedures.
Prof Connelly, Ms Brindley and their team have led the expansion of paediatric surgery in Limerick by setting up the first regional paediatric surgical facility in the country under the new model of care. For the first time, the majority of children who need common elective surgeries including hernia repair, endoscopy, skin lesions and undescended testis fixation, can now have their procedures in the Mid West. Prof Connelly is also running paediatric endoscopy lists as well as outpatient clinics in UHL and in Ennis Hospital, with over 500 outpatient department attendances across the region to date.
Spotlight on Patient Safety


Quality and Patient Safety Competency Navigator launched
In January, HSE National Quality and Patient Safety launched the first ever Quality and Patient Safety (QPS) competency framework for the Irish health service.
The QPS Competency Navigator is the result of a two-year extensive co-design project led by the National Quality and Patient Safety Education team and the IRIS Centre at the UCD School of Nursing, Midwifery and Health Systems.
What is it?
The QPS Competency Navigator is a resource designed to support healthcare students, staff, leaders and patients to identify their quality and patient safety learning needs and help them plan their training and development to support the delivery of quality and safe care. It can also be used by educators to inform quality and patient safety curricula
in undergraduate and postgraduate teaching and learning.
How does it work?
There are four simple steps to using the QPS Competency Navigator.
1. Select the role category that best describes you. A good place to start is with the ‘Everyone Working in Healthcare’ category, which provides
The QPS Competency Navigator is hosted on the National Quality and Patient Safety Website, hse.ie/nqps and can be viewed online or downloaded. It can also be accessed by scanning the QR code.
key foundational competencies.
2. Select which of the six core topics you would like to explore.
3. Review the competency statements for that topic and select the ones that you feel you need to learn more about.
4. Review the suggested learning resources available and transfer into your professional development plan.



Operation Preparation podcast empowers patients on their perioperative journey
The staff of the Pre-Anaesthetic Assessment Clinic (PAAC) in St James’s Hospital recognised a need for accessible patient information surrounding the perioperative journey. To meet this need, they have launched the podcast, Operation Preparation, which features discussion-style episodes with the staff of PAAC on a range of topics relating to the perioperative journey. This audio podcast is the first of its kind in the northern hemisphere. The aims and objectives of the podcast is to help patients become more empowered and educated regarding their perioperative journey, minimising delays, cancellations, reducing perioperative risk, decreasing length of stay, and increasing patient safety.
QPS TalkTime webinar series explores quality improvement in practice
Do you want to expand your quality and patient safety knowledge? If so, join the fortnightly QPS TalkTime webinar series to hear from national and international experts as we explore the latest thinking, learning and examples of quality improvement in practice. Hear about topics like learning health systems, civility saves lives, psychological safety and how we can work together to improve and build a culture of quality and patient safety. It is free and open to anyone to join.
Watch past episodes of the series or register for upcoming sessions at hse.ie/qps-talktime
New Walk and Talk Improvement podcast episodes
The Walk and Talk Improvement podcast is now available on even more platforms, including Podbean, Spotify and Apple Podcasts. The series brings together esteemed guests who share their wisdom on a diverse range of topics underpinned by the Patient Safety Strategy.
The latest episode, “Healing Healthcare: Quality is Goodness” with special guest Don Berwick, a leading authority on health care quality and improvement, explores the role of intrinsic motivation and personal experience in sustaining our passion for improving healthcare; leadership lessons to foster a culture of quality, patient safety and continuous learning; the value of community engagement in driving meaningful change; and future-proofing our health care system.
If you’re interested in topics like quality and patient safety culture, clinical audit, patient partnership, common causes of harm, governance, motivation and self-regulation, you can access the podcast at hsenqps.podbean.com
Building trust from within: the role of the designated person in open disclosure
Open disclosure is the open, honest, compassionate and timely approach to communicating with patients and/or their relevant person following patient safety or notifiable incidents. It is an integral part of the incident management process.
The Patient Safety (Notifiable Incidents and Open Disclosure) Act 2023 introduced a new subset of incidents referred to as notifiable incidents, setting a new legal standard for transparency in healthcare. With the implementation of the act and the revision of the HSE Open Disclosure Policy in 2025, the role of the designated person (DP) has become central to how we respond to patient safety and notifiable incidents. But more than that, it’s about doing the right thing for patients and staff.
The DP acts as a trusted point of contact between a service provider and a patient and/or their relevant person following an incident. The DP’s responsibilities extend beyond delivering information; they offer or signpost to support, answer questions and help navigate the complex emotional and procedural aftermath of an incident. But the true value of the role lies in how it fosters trust, both with patients and among colleagues. By facilitating honest conversations, DPs help transform what could be purely procedural into moments of

genuine connection that honour patient dignity.
In February, the National Open Disclosure Office, which is part of the Quality and Patient Safety (QPS) Incident Management Team of National QPS, held a workshop for people on the role of the DP. Bernie O’Reilly from Patients for Patient Safety Ireland said, “A room full of designated persons, where 20 years ago there were none – how far we have come! The collective potential, the collective harm that will be averted for people... these DPs are the pioneers.”
Services may have several people taking on the role of DP, as the appointment of a DP is often on a case-by-case basis. As such, the support offered to DPs, and
by extension their services and the patient population, needs to be ongoing, and responsive. The National Open Disclosure Office has developed a range of practical training and tools to support people who assume the role of the DP, including guidance and eLearning, on HSeLanD. By embedding openness into the fabric of healthcare, the DP role strengthens public trust and ensures that safety is not just a goal but a shared commitment. The Patient Safety Act and HSE Open Disclosure Policy set the legal and policy frameworks, but it’s the commitment and empathy of our teams that bring them to life – for our patients, our teams and the entire health service.
For more information on the DP role, contact the National Open Disclosure Office on opendisclosure.office@hse.ie

National Inpatient Experience Survey visit to Tipperary University Hospital
A joint HSE, HIQA and National Patient and Service User Forum visit took place at Tipperary University Hospital (TUH) on 25 March. The event began with an overview presentation of the findings of the 2024 National Inpatient Experience Survey, followed by an address from partner representatives. The visit was an opportunity for the hospitals in HSE Dublin and South East to showcase the quality improvement initiatives underway across their sites in response to the findings of the 2024 survey.
Optimising Health Service Productivity
Ensuring we use everyone’s time more efficiently and effectively in Outpatient Departments (OPDs) to support increased access to new outpatient appointments and improved compliance with Sláintecare targets in line with the HSE National Service Plan 2025 and the Waiting List Action Plan 2025
Following on from our feature in the Health Matters winter edition 2024, the National Productivity Unit is excited to provide an update on progress of collaborative work being undertaken with our hospitals as part of the HSE’s ongoing work to improve access to OPD appointments, in line with Sláintecare targets. The National Productivity Unit (NPU) engaged with a range of hospital models in late 2024 and early 2025 to undertake a point-in-time review of OPDs. The purpose of this work was to highlight and recognise good practice based on what has worked well and lessons learned to date. Through on-site observation of OPD clinic operations and feedback from staff in these hospitals, an in-depth review of OPD processes and data was achieved. All participants in the process generously contributed their time and provided insights into what was working well and what processes might be amenable to review and improvement across the areas of demand management, capacity utilisation and data optimisation to support the delivery of Sláintecare targets. The NPU recommended an operational focus be given to two opportunities arising in the areas of OPD capacity utilisation including clinic planning.
As a next step in this process, further collaborative work is currently underway with the regions, which is focused on operational excellence to:
• Evaluate and baseline OPD clinic ‘core’ capacity
• Enhance OPD clinic planning through the deployment of an appropriately standardised clinic capacity planning tool, the implementation of which is underway
Commencing in April, small regional teams are visiting OPDs in hospitals to gather site and service level capacity data and actionable insights to enable a data-driven, standardised approach to OPD clinic planning to support the best use of our existing resources.
These OPD on-site visits will generate a view of capacity management over the course of a typical week. These visits are not an audit or inspection against standards. Each hospital will receive a supportive analysis of their capacity utilisation and training in a practical planning tool to be deployed, embedded and sustained as part of the day-to-day operational management of their OPD clinics going forward.
Updates from HSE Dublin and North East
Celebrating inclusion projects in Meath
People communicate and experience the world in a variety of different ways. As understanding of communication differences has increased in recent years, so has the number of individuals, schools and local groups working to create accessible and inclusive spaces. This enthusiasm for community action sparked the Gradam Ceannródaithe Cumarsáide (‘Pioneers in Communication’). This is a monthly award presented by HSE speech and language therapists in Meath to projects that are helping to make Meath more accessible.
Annette Murray, Chairperson of Duleek Fair Day was inspired to create a sensory-friendly Santa experience. “My grandson, who is three, was diagnosed with autism so I really wanted to make sure Santa was accessible to neurodivergent children.” The Duleek Fair Day team were able to create a positive experience for children who communicate differently. “We had a non-verbal child, we used a core board and it was so emotional to see the excitement in the child’s eyes when Santa handed it to her.”
This desire for accessibility in the community is shared by the Trim Autism Friendly Town (TAFT) Committee. Melissa Barwell, TAFT Chairperson, wants to see a “fully integrated community” in which her autistic son can thrive. “We want every autistic person to feel included. Our mission is to have equal access and equal opportunity.” TAFT have big plans for the town of Trim. These include awareness training for businesses to help reduce unemployment
amongst autistic adults; priority checkouts in large shops; and working with the Knightsbrook Hotel, Spa and Golf Resort to create a sensory playroom for resident and community use.
Schools in Meath are also adapting to facilitate communication differences in response to everevolving student needs. “Last year, we had two pupils with Down syndrome, both of whom used Lámh. We decided to become a Lámh-friendly school,” Tom Brennan, the Principal in Scoil Cholmcille Skryne, told the awards committee. “Key members of staff completed a Lámh training course. Following on from this, our special education team ran a campaign whereby the whole school learned three signs per week. Our pupils with Down syndrome, along with others, modelled the signs for everyone. Across the school, we watched Dizzy Deliveries, the Lámh-friendly TV programme made by RTÉjr, every day. It was lovely to see the wider school using Lámh and making connections with the children who rely on it.”
It is inspiring to see inclusion projects expanding into local sports groups. Bohermeen Celtic – Football for All, Walterstown Peil for All-Stars, and the Rathkenny Rockets have been making strides to create safe, fun and accepting spaces for neurodivergent individuals who play sport differently. Coaching is adapted to the communication style of the individual, and training activities are child-led and flexible. “The idea of the Rathkenny Rockets came about when my daughter, Chloe, who has Down syndrome, came out to train
with the U5 training,” Joy, one of the founders, explained. “Chloe could do some of the drills she liked, but when not motivated, she would like to roam and explore the pitch. A few coaches spotted that there were a few other children in the community who loved football and the drills but wanted to train their own way or who needed more support or different instruction other than verbal.” Sports are a vital part of a community, and it is wonderful to see the growth of inclusive sports teams.
Another essential part of a community is hairdressing. Ben Garry Hairdressing in Navan have taken action to create sensoryfriendly haircuts for individuals with additional support needs. Similarly, Kerry O’Neill from KLO Haircare is passionate about supporting individuals and their families to create a stress-free haircut experience. Kerry works with children with additional needs in their home and adapts her approach based on individual needs and preferences.
The range of award-winners in 2024 highlights a positive move towards inclusion and accessibility in various facets of community life.
If you know of a person or group in Meath working to promote communication inclusion, acceptance and accessibility, you can nominate them for this award in 2025 by contacting Meath Speech and Language Therapy on Facebook or Instagram (@meathslt), speaking to your local speech and language therapist in Meath, or emailing swmeath.chn@hse.ie.
Updates from HSE Dublin and North East
Rainbow Badges presented in Louth Meath
The Louth Meath Health Promotion and Improvement team completed their Rainbow Badge Initiative (RBI) in March, culminating with badge presentations in both Navan and Ardee. The Rainbow Badge initiative gives healthcare staff a way to show that their place of work offers open, non-judgemental and inclusive care for all who identify as LGBTQIA+.
The initiative originated at Evelina London Children’s Hospital in the UK and was adapted for the HSE by Linn Dara Child and Adolescent Mental Health Services in Dublin.
The Health Promotion and Improvement team in Louth Meath fully embraced the spirit of the initiative, including an information session from Outcomers, an organisation who works with those who identify as LGBTQIA+. All participating staff completed the LGBTQIA+ modules on HSeLanD. A signposting resource was also developed locally, which provides information on the support services

available nationally and locally. A local stop smoking advisor said about the initiative, “It has made me much more aware of the importance of language and how to be more LGBTQIA+ aware in my practice with clients.”
On the day of badge presentations, events were held in both Navan and Ardee. Participating colleagues
Confidential Sta Health Check service celebrates first birthday
signed the Rainbow Badge pledge and received the information resource to help in signposting and support.
Health Promotion and Improvement in Louth Meath will continue to support other colleagues and departments who may wish to complete the Rainbow Badge initiative.
For more information on the initiative and to access the toolkit, see bit.ly/RainbowBadgeToolkit
HSE Dublin and North East is pleased to announce the one-year anniversary of the Confidential Staff Health Check service, now being rolled out across all areas within the region. This service is designed to support the identification of early signs of health issues among healthcare workers.
The Confidential Staff Health Check service covers a range of important areas including:
• Medical history
• Family history of disease
• Lifestyle factors such as diet, weight, physical activity, cholesterol, blood sugar levels, alcohol use, and smoking habits
This comprehensive health check will provide staff members with valuable information about their overall health and wellbeing and will help to identify any potential risk factors for future health issues.
In addition to providing staff with important health information, the service will also signpost them to services they may require in the community. If a GP visit is warranted, it will be the responsibility of the individual staff member to arrange, as indicated on the consent form for the service.
The Confidential Staff Health Check service will operate from a dedicated space within the hospital, demonstrating management’s commitment to valuing and protecting the health and wellbeing of all healthcare workers. By offering this service, HSE Dublin and North East aims to support the mental and physical wellbeing of its staff.
Working in healthcare is a rewarding but challenging career and it is essential that healthcare workers prioritise their own health and wellbeing. HSE Dublin and North East is proud to offer this important resource to its staff and looks forward to supporting the health and wellbeing of all healthcare workers within the region.
New Lung Health Check pilot research programme
Lung Health Check is an innovative pilot research programme that will be operational in Dublin and North East in 2025. Lung Health Check aims to engage people at higher risk of lung health problems and offer them comprehensive screening to support early detection of lung problems, including lung cancer. The checks will take place in mobile units in four community settings across the Dublin and North East region.
This pilot programme is a partnership between Alliance Medical, Beaumont Hospital, the Irish Cancer Society and the Royal College of Surgeons in Ireland (RCSI) University of Medicine and Health Sciences. Recently, the Louth Meath Health Promotion and Improvement team provided training and support to staff involved in the rollout of the programme. The training encompassed the full suite of MECC (e-learning and an in-person workshop) and information on stop smoking services and referrals processes.
Through MECC signposting, Health Promotion and Improvement are supporting staff working on this pilot programme to enable greater knowledge of local community and voluntary supports.
Participants who smoke will be offered access to support from a trained stop smoking advisor in their local area and free stop smoking medication to support their quit attempt.

“Feedback on the support to staff for both MECC and the stop smoking service was positive, especially around the local MECC signposting resources.”
Staff working on this pilot initiative have now completed the MECC e-learning and enhancing your skills workshop. They have also been set up as referrers on QuitManager, the national electronic system for the HSE stop smoking service, so they can refer directly to the service.
Feedback on the support to staff for both MECC and the stop smoking service was positive, especially around the local MECC signposting resources.
The collaboration has been an important step to link local HSE practice with research in the
wider learning community.
Brian Meehan, Lung Health Check Programme Manager said, “The training and ongoing collaborative support provided by the Health Promotion and Improvement team has been excellent. The MECC online core modules were easy to navigate, extremely informative and gave a great understanding ahead of the in-person training session. The MECC trainers provided tailored support, guiding team members on smoking cessation methods, benefits, signposting and referral pathways.”
More information: Stop smoking services: bit.ly/Quit28days MECC programme: bit.ly/MECCprogramme
Updates from HSE Dublin and North East
Our Lady of Lourdes homebirth reunion: celebrating safe and empowering birth experiences
Choosing to give birth at home can be a safe and empowering option for women with low-risk pregnancies. The Registered Homebirths Annual Report 2022 (NPEC 2024) supports that, for certain women, a planned homebirth is a safe and viable alternative to hospital births. The homebirth service, provided at no cost to eligible women, is facilitated by community midwives who focus on continuous care throughout pregnancy, labour and the postnatal period. Outcomes for homebirths have mostly proven to be exceptional, with many women reporting high satisfaction levels.
Louth Meath homebirth service falls under the auspices of Our Lady of Lourdes Hospital, Drogheda. To celebrate the women and families who gave birth at home and foster connections among those with similar journeys, a special reunion event was organised by the Our Lady of Lourdes Maternity Unit. This gathering took place on 14 April at the Cottage Hospital in Drogheda. Designed as a celebration of the homebirth service, the
North East update

reunion welcomed women, their babies and partners, alongside expectant mothers planning their first homebirth. The event also brought together the dedicated community midwives, along with Patricia Kingsnorth, the Designated Midwifery Officer overseeing the homebirth service, and Gráinne Milne, Director of Midwifery, who delivered a warm welcome to the attendees.
The reunion was a great success, marking the first of its kind in Ireland. It provided a platform for women to share their experiences and offer
HR and Payroll Self Service
how to get started
If you are yet to register, it only takes a few minutes. Scan the QR code and complete the instructions on the screen. Further details and support at hse.ie/nisrp

valuable feedback, which will help shape and enhance the homebirth service in the future, and was overwhelmingly positive. Comments included, “I felt very supported during my pregnancy”, “It is an excellent service”, and “My homebirth experience was incredibly positive – truly the gold standard”.
With hopes of making this reunion an annual event, there are plans to expand this initiative across Ireland. International Homebirth Day is 6 June 2025 as we continue to celebrate and support safe birthing choices.

Rotunda Hospital promotes compassionate care
As health practitioners, we are involved in writing ‘stories’ every day. The clinical record is our interpretation of our patients’ stories (history) and a summary of our response to this (examination and management plan). This record does not allow for much creativity on the part of the writer, and is very limited in its ability to assist the clinician in making sense of what has gone on for them at a personal level.
Dr Hilton Koppe, author, GP and experienced workshop facilitator presented a reflective writing workshop to staff in the Rotunda Hospital in March. This interactive session gave participants the opportunity to experience the use of reflective and expressive writing as a means of helping them to better manage some of the more challenging aspects of their working lives, and to gain a deeper understanding of what it means to be a health practitioner. This workshop, sponsored by Attuned in Practice, is designed to reduce professional isolation, burnout, and compassion fatigue.
“We believe that all frontline practitioners deserve learning spaces to reflect and connect with their core beliefs, values and purpose.”
Dr Maeve Hurley, one of the Attuned in Practice members who attended the workshop in the Rotunda said, “We were delighted to see a great turnout of multidisciplinary healthcare professionals for our collaborative initiative. At Attuned in Practice, we believe that all frontline practitioners deserve learning spaces to reflect and connect with their core beliefs, values and purpose.”
This event has hopefully gone some way towards supporting practitioners to sustain themselves and bring their best to their work, and to encourage organisations to build reflective spaces into systems of care. The aim of Dr Koppe’s workshop was to address the growing issue of burnout among healthcare professionals.
PEACEPLUS funding success for cross-border health and social care
The new year brought good news to all engaged in cross-border health and social care. As a partner in the cooperation and working together (CAWT) cross-border partnership, the HSE, along with Northern Ireland Health Authorities, have secured in excess of €42m from the PEACEPLUS programme to implement specific cross-border health services.
The funding has been secured from PEACEPLUS Investment Area 4.1 (Collaborative Health and Social Care) to support the development of innovative community-based health care interventions, which complement statutory provision, contribute to improving population health and wellbeing and help to reduce health inequalities.
This significant funding will support 5 large-scale cross-border health and social care projects to be delivered over the next 3 to 4 years in the areas of mental health, frailty, alcohol addiction and obesity. All 5 projects have some common aims:
• Prevention of ill health and intervening early
• Reducing health inequalities
• Building strong partnerships with the community and voluntary sector
• Maximising use of existing health and social care infrastructure
The geographic areas that will benefit primarily from this funding include the HSE border counties along with the Northern Ireland border region.
For more information, email Paula.Keon@hse.ie
Project Description
Community Connection and Wellbeing
Project
Early Intervention Support Youth Hubs
Early Frailty Intervention Project
Healthier Futures
Project
Community Alcohol Detox+ Project
Updates from HSE Dublin and North East
Support to adults with mild and/or emerging mental health difficulties by enabling access to programmes and support in the areas of:
• Low-intensity psychological support;
• Psychosocial mental health and wellbeing programmes; and
• Psychosocial activities and community support programmes.
Support services for families with children and young people with social, emotional or behavioural issues, to include:
• One-to-one consultation with parents, offering initial assessment and meaningful/ therapeutic conversation, leading to support and guidance, signposting/navigation and introductory workshop;
• Suite of workshops and parenting programmes tailored to individual need; and
• Personalised support.
Assessment and consultation for older people with or at risk of frailty, after which a programme of care will be identified from the following areas:
• Frailty screening including a one-to-one session with a specialist health professional;
• Frailty education programmes delivered in community settings by specialist staff; and
• Introduction of older people to community locally based support and networks.
Programmes that intervene early to prevent obesity to include the development and implementation of:
• New childhood weight management programmes in HSE border areas; and
• Adult weight management programmes in Northern Ireland.
Support to people with alcohol dependence syndrome, and their families/carers.
Following assessment, the project will offer:
• An alcohol detox programme for those considered ready to detox;
• A harm reduction programme for those not ready for detox, via alternative community-based programmes;
• Wrap-around/aftercare support and education to help maintain abstinence and recovery after detox/harm reduction programme; and
• Personalised support to address issues such as loneliness, chronic stress, unemployment, poverty and trauma.



CAWT PEACEPLUS PROJECTS









Climate Action
HSE Climate Programme publishes guidance frameworks
Progressing implementation towards a net-zero health service





















Climate change presents a fundamental threat to human health. It affects the physical environment as well as all aspects of natural and human systems, including social and economic conditions and the functioning of health systems.
Following publication of the HSE Climate Action Strategy 2023-2050 and committed deliverables under the Government Climate Action Plan, the HSE has developed a number of climate action framework documents.
Drafted in collaboration with expert working groups, the strategic frameworks will focus on priority areas, including transport, mobility, greener environments











and spaces, waste, water, sustainable procurement, and greener models of healthcare.
The purpose of the frameworks is to translate the HSE’s vision for a net-zero health service that is environmentally and socially sustainable into a practical programme of actions to be delivered.
Each framework document includes key building blocks for each area, implementation guidance from a national and local perspective and best practice examples. They will help regional and local green teams in implementing this work.
For more information on the guidance frameworks, email climateandsustainability@hse.ie
HSE awarded ISO 50001 certification for energy e iciency e orts
The HSE has achieved certification to the ISO 50001 global energy management standard for its approach to continuously improving energy efficiency and performance. Greener and more sustainable HSE facilities and services benefit the health of the population as well as having a positive impact on the environment.
This certification builds on the work done to date by HSE Capital and Estates in partnership with the Department of Health and the Sustainable Energy Authority of Ireland (SEAI) to establish the systems and processes necessary to improve energy performance. These include monitoring consumption, conducting energy audits, setting energy performance targets and identifying opportunities for energy improvement.
For more information, visit bit.ly/HSEISO50001
Royal Victoria Eye and Ear Hospital Sustainable Awareness Week
There was something of interest for everyone at the Sustainable Awareness Week in the Royal Victoria Eye and Ear Hospital, Dublin, 11-13 March. Organised by John McCarthy, Sustainability Project Lead, the event was supported by Paul Cullen, HSE Energy Officer, Karl Dalton and Samuel Awe, HSE Sustainability Officers, and Eileen O’Leary of the Clean Technology Centre.

The hospital can look forward to a more sustainable future with the commitment and support from its CEO, Tommy Bracken, who spoke of the significant effort healthcare needs to make in reducing its impact on the environment. With the establishment of a green team, the hospital ensures that the sustainability journey is embedded in its culture.
It was a wonderful opportunity for the hospital to highlight how progress is being made in the many aspects of its green healthcare delivery, including waste management, water usage, surgery, transport, green spaces and energy.
Conference highlights climate action roadmap
The HSE partnered with the Institute of Healthcare Engineering and Estate Management (IHEEM) Ireland, who held a joint conference on 1 April in the Aviva Stadium, Dublin.
Micheál Conneely, Interim National Director of Capital and Estates, opened the morning session with an overview of the Capital Plan. Then HSE Chief Architectural Advisor Eleanor Masterson spoke about delivering new-build programmes in healthcare.
The mid-morning session, “The Road to Net Carbon Zero Estates”, was chaired by Peter Smyth, National Lead for Capital and Estates Sustainable Infrastructure Office, and provided an overview of the HSE Infrastructure Decarbonisation Roadmap.
In the afternoon, Brian O’Connell, National Director for Strategic Health Infrastructure and Capital Delivery opened the session with an overview of Ireland’s strategic priorities in healthcare infrastructure. This was followed by presentations led by Aidan O’Connor and Capital and Estates focusing on electricity and water capacity, grid and infrastructure resilience, and strategies to meet growing demands and climate challenges.







Climate and sustainability event in Maynooth
On 6 February, Maynooth University hosted a climate and sustainability event, organised by HSE Dublin and Midlands, aimed at showcasing valuable projects and fostering dialogue and action on sustainability across healthcare systems.
Kate Killeen White, Regional Executive Officer (REO) of HSE Dublin and Midlands opened the event emphasising the importance of integrating sustainability into the healthcare sector and ensuring that environmental concerns are woven into future healthcare strategies.
Quoting Dr Philip Crowley, the REO stated, “Caring for the health of the environment goes hand-in-hand with caring for the health of patients. It will support and protect the health and wellbeing of future generations.”
for of future generations.”
attended and included O’Kelly,
The event was well attended and included Mary O’Kelly, the Integrated Health Area (IHA) Manager for Kildare West Wicklow. A variety of formats were used to encourage learning, sharing, and collaborative discussions. Oral presentations provided key insights into ongoing sustainability initiatives, while poster presentations showcased
•
•
innovative ideas from healthcare professionals across the region. These served as a catalyst for table discussions where participants engaged in conversations on the opportunities and challenges related to climate action within the healthcare sector.
served as a catalyst for challenges related to the healthcare sector.
A few central themes of the day were discussed, including:
• The role of green teams
• The importance policies in sourcing
• The importance of procurement policies in sourcing environmentally friendly products and services
• Achieving buy-in from all levels of staff, and the need for education



“The greatest threat to our planet is the belief that someone else will save it.”
Overall, the day was an sustainability in the
and training to ensure that sustainable practices are embedded in the culture of our workplaces
address the question of and instil a collective the environment within motivate through the
The workshop sought to address the question of how to shift mindsets and instil a collective sense of responsibility for the environment within healthcare institutions and to inspire and motivate through the sharing of good practice. Overall, the day was an insightful exchange of ideas, laying the groundwork for future initiatives to support sustainability in healthcare and beyond.
If you are interested in setting up a green team, contact evan.weatherup@hse.ie or samuel.awe@hse.ie
More information on climate and sustainability can be found at hse.ie/sustainability
Regional climate action workshop highlights opportunities for change
HSE Dublin and South East recently hosted a climate action workshop that was attended by senior management and over 50 staff representing different functions. The HSE Climate Action Strategy and Implementation Plan was shared in advance of new climate action frameworks and the upcoming formation of a regional climate group. An overview of the HSE Climate Action Strategy was

provided by Roisin Breen, HSE Climate and Sustainability Programme Manager, along with presentations from HSE Capital and Estates and Procurement. The workshop explored what sustainability means to people personally and focused on opportunities for change in health services
across the HSE climate focus areas – greener models of healthcare; green spaces and biodiversity; adaptation and resilience; mobility and transport; and waste and water management. Ask your line manager how you can get involved with your local green team today.
Winners
announced of the first national GreenTech award in healthcare

“We are delighted to be involved in the GreenTech in healthcare initiative with Health Innovation Hub Ireland (HIHI) and the Irish College of GPs,” says Dr Philip Crowley, National Director, HSE Climate and Global Health. The project identified six innovative products and services promoting environmental sustainability in healthcare. The winning products and services will be trialled before wider implementation.
The call is a positive step towards tackling the research and innovation gap in sustainable product pathways in Irish health and sets a strong precedent for future collaborations in green healthcare innovation.
Updates from HSE West and North West
University Hospital Galway first public hospital to employ innovative cardiac procedure
University Hospital Galway (UHG) became the first public hospital in the country to employ the convergent procedure, a groundbreaking approach for treating atrial fibrillation (Afib), putting it at the pinnacle of heart surgery.
Afib affects around 1-2% of the population, with increasing incidence in over-65s, and if left untreated, can lead to blood clots, stroke, heart failure and other heart-related complications.
Consultant Cardiothoracic Surgeon Professor Alan Soo says, “Afib is a condition where your heart beats irregularly (arrhythmia), usually much faster than normal, and this is caused by disruptions in the electrical signals that regulate your heart, making it harder for the upper and lower chambers of the heart to work together. While medication or catheter ablation can successfully treat Afib, some patients’ symptoms recur or worsen. Now with the convergent procedure, such patients have another treatment option, allowing for minimal discomfort, lower risk of complications, faster recovery time and a shorter hospital stay.”
This minimally invasive procedure is performed by a cardiothoracic surgeon and a cardiac electrophysiologist. Radiofrequency

Professor Alan Soo, Consultant Cardiothoracic Surgeon with Sean Rankin from Newcastle in Galway City, the
at UHG.
energy is used to make ablations, or small lesions/burns on the heart, that will effectively block the irregular electrical signals or heartbeat. It is one of the most effective surgical techniques in treating individuals with persistent Afib.
Galway resident Sean Rankin was the first patient to undergo the convergent procedure, which was carried out at UHG by Professor Alan Soo and Consultant Cardiac Electrophysiologist Dr Stephen Tuohy. Sean, who had been suffering from
Afib affects around 1-2% of the population, with increasing incidence in over-65s, and if left untreated, can lead to blood clots, stroke, heart failure and other heart-related complications.
Afib for many years said, “I sought treatment for my condition following the success of my lung cancer surgery with Professor Soo. I’m doing very well and I am very pleased with the way everything went. I’d like to express my sincere appreciation to Professor Alan Soo, Dr Stephen Tuohy and my GP Dr Richie Baggott for everything they’ve done for me. This is a new beginning for me and I look forward to the future.”
Hospital Manager Chris Kane says, “This is a first for University Hospital Galway, and we welcome this new treatment option for patients. It will significantly improve the patient experience, and we are delighted to have debuted this innovation here in Galway.”
Updates from HSE West and North West
Roscommon University Hospital appoints advanced nurse practitioner in diabetes
Roscommon University Hospital is delighted to announce the appointment of Brid Ní Chlochartaigh to the role of Advanced Nurse Practitioner (ANP) in Diabetes.
In her new position, Brid plays a vital role in managing the care of people living with diabetes in the hospital setting. She is responsible for assessing, diagnosing, treating, prescribing and discharging patients, ensuring effective diabetes management from early diagnosis through advanced care.

“We have an excellent diabetes service here at Roscommon University Hospital, and to have two visiting consultant endocrinologists from Sligo and Galway University Hospitals aligned to the service and supporting us, is fantastic,” says
Brid. “My role within the service is to care for patients on the ward and in outpatient clinics, ensuring they are assessed and treated in a timely manner, resulting in improved patient outcomes. I also work with public health nurses, general practitioners, and patients seeking information or guidance in relation to diabetes care, and I maintain a direct link with clinical nurse specialists who work in integrated care within the community and particularly those living with type 2 diabetes who are on oral hypoglycaemic agents.”
Brid, originally from the Gaeltacht of Connemara, began her nursing career as an intensive care unit (ICU) nurse at Portiuncula University Hospital, where she enhanced her clinical skills and
Older persons day and disability respite services in Inishowen
There was good news for Donegal recently with the reopening of day services for older persons and also respite services for children and adults with disabilities in Carndonagh.
Respite services at Riverwalk Respite House in Carndonagh, which had been unavailable for a prolonged period due to emergency residential placements, reopened on 3 April. The house provides both day and overnight residential respite care for children and adults with disabilities.
During alternate weeks, the house will serve 3 adults and 3 children. The facility includes comfortable, private rooms for each resident, along with shared amenities such as a kitchen-diner, two sitting rooms, a laundry room, and bathroom facilities with residents receiving care from a dedicated team of nursing and care staff.
gained invaluable experience working in a high-pressure, critical care environment. To broaden her knowledge and expertise, Brid pursued and qualified with a higher diploma in intensive care nursing, which expanded her understanding of critical care procedures and the complexities of managing severely ill patients.
Brid enrolled at University College Dublin, where she completed a higher diploma in diabetes nursing. This specialised training allowed her to develop a comprehensive understanding of diabetes management, from acute care to long-term management.
After a two-year candidature process, and a postgraduate certificate in advanced nursing practice from University of Limerick, Brid was appointed Registered Advanced Nurse Practitioner in Diabetes at Roscommon University Hospital.
Meanwhile, on 14 April, Carndonagh day services for older persons became operational again at the Spraoi agus Spórt facility. This follows the relocation of services from Carndonagh Community Hospital in 2023, when it was determined the hospital was no longer suitable for providing day services.
The day service will operate Mondays and Tuesdays 10am to 3.30pm. It is anticipated that between 10 to 15 people will attend each day, benefitting from a variety of activities tailored to their individual preferences. These activities will be based on the What Matters to Me document, allowing attendees to share their interests and needs with care staff to ensure activities are scheduled around the attendees’ preferences.
Letterkenny University Hospital announces Quality Improvement Plans for enhanced patient care
At a recent meeting at Letterkenny University Hospital (LUH), staff, managers and senior leaders from hospitals in the West and North West along with members of the National Care Experience Programme, HIQA, the Department of Health, and members of the LUH and National Patient Forums gathered to collaborate and share the ways they are improving services to their patients as a result of the National Inpatient Experience Programme.
The 2024 survey saw over 30,000 patients from 40 acute public hospitals, including LUH, invited to take part and share their experiences. With a response rate of 41%, 12,367 patients shared their valuable insights. Overall, from those who responded to the survey, 85% rated their overall hospital experience as good or very good. However, the survey also highlighted areas for improvement, such as the need for better communication regarding post-discharge care, more time with doctors, and increased support for patients’ concerns, including worries and fears.
Martina Porter, Quality and Patient Safety Manager at LUH said, “In response to these findings, LUH is pleased to announce a series of Quality Improvement Plans (QIPs) aimed at enhancing patient care and experience. These initiatives are part of the ongoing commitment to providing high-quality healthcare services and ensuring patient satisfaction.”
Among the areas patients identified as needing improvement were: patients who wanted to give feedback or make a complaint and did not know how or where to do so; and the provision of support for patients with disabilities or long-term conditions.
LUH is using the results of this survey to help prioritise quality improvements for the coming year and as part of that is introducing patient feedback initiatives. These initiatives include improved feedback accessibility, with the increased availability of feedback forms placed in Perspex boxes in high-visibility areas near ward entrances and exits. New posters with QR codes will be placed at each bedside, providing information on how to make a complaint or give feedback. Staff awareness information sessions will be conducted for clinical and non-clinical staff to support the patient

Back row, from left: Iolo Eilian, Assistant National Director, Patient and Service User Experience Lead Public Involvement, Culture and Risk Management; Seán Murphy, LUH Hospital Manager; Tracy O’Carroll, Deputy Director, National Care Experience Programme, HIQA; Maura Heffernan, Director of Nursing SUH; Margaret Healy, QPS Manager, Mayo University Hospital; Angie Gallagher, Patient Partner; Claire Conlon, QPS Manager, Roscommon University Hospital; John McElhinney, Group Quality and Patient Safety Manager. Front row, from left: Aileen Killeen, National Patient Forum; Christine Fenton, National Patient Forum; Martina Porter, Quality and Patient Safety Manager, LUH.
feedback process. LUH will also be increasing patient partner feedback so complaints will be reviewed quarterly with the Patient and Family Experience Group to identify areas for improvement.
One of the initiatives LUH will also introduce is supports for patients with disabilities or long-term conditions. These supports will include the Hello My Name Is campaign to help patients with disabilities identify staff members, improving communication, HSE Health Passport promotion to encourage the use of the health passport for patients with intellectual disabilities to better communicate their needs, including information about John’s Campaign in the patient information booklet to support patients with disabilities and their carers, and recruiting patient partners with disabilities to the Patient and Family Experience Group to ensure their representation.
In addition, LUH will be promoting education sessions and online modules to enhance staff communications skills, designing and displaying posters to inform patients about available pastoral supports, enhancing the use of patient information booklets, and ensuring effective discharge planning with clear communication and support information.
Updates from HSE West and North West
MaDE for better patient flow
HSE West and North West held a number of very successful multidisciplinary agency discharge events (MaDE) over recent weeks to drive improvements in patient flow across our hospitals. MaDE is a collaborative initiative that brings together local health and social care providers to streamline patient discharge processes and enhance flow.
Helene Horsnell, Unscheduled Care Lead for HSE West and North West led the events in University Hospital Galway, Mayo University Hospital and Sligo University Hospital throughout February and March, along with Laura Connolly, data analyst. The primary goal of these events was to unblock delays and simplify processes across the whole system; to free up beds, increase flow as part of an escalation process, to reduce length of stay, and to increase morning discharges.
One of the most important aspects is collaboration between acute and community services during the
University Hospital Galway World Obesity Day
Specialists in the obesity service, Galway University Hospital (GUH) acknowledged World Obesity Day in March.
Dr Sarah Summerville, Specialist Clinical Psychologist at GUH says, “Until recently, the complex nature of obesity was not fully understood. It is now recognised as a biological, clinical disorder rather than a reflection of an individual’s intelligence or personality and is affecting about one in four adults in Ireland. We all have a responsibility to compassionately understand and manage our own beliefs about weight, which are often shaped over generations and driven by media and industry. Within the Bariatric Psychology Service in GUH, our aim is to provide an accessible, effective and person-centred psychological service aimed at maximising the health, wellbeing and quality of life of all adults living with obesity. Psychological care is focused on evidence-based principles of chronic disease management based on lived experiences and moves beyond simplistic approaches of ‘eat less, exercise more’.”
Obesity is a complex, progressive and relapsing chronic disease that impairs both physical and mental health. The specialist obesity service at
MaDE. Representatives from older persons services, disability services, home care supports, primary care, acute hospital staff and the IHA manager were involved in the two-day events and worked together to share learning and experience.
A bespoke tool was created to allow the team to capture key information using Red and Green Day analysis so that the participants could focus on:
• The progress of each patient’s care (reviewing notes and speaking to key team members).
• What was the next critical step to support discharge?
• Is that next critical step happening today?
• If not, what can be done to enable this to happen today?
The events have resulted in closer integration between services and a renewed focus on addressing the challenges that lead to delayed discharges for patients across the region.

From left: Eoin Connolly, Clinical Specialist Physiotherapist; Alby Baby, Candidate Clinical Nurse Specialist; Grace O’Shea, Senior Clinical Psychologist; Paul Cromwell, Bariatric Surgeon; Robert Moloney, Administrator; Dr Enda Murphy, Research Associate; Sinead Molloy, Administrator; Professor Francis Finucane, Consultant Endocrinologist; Síle Ní Mháille, Clinical Specialist Occupational Therapist; Caitriona Lynch, Clinical Nurse Specialist; and Dr Wei Keong Kon.
GUH was established in 2011 but has recently expanded significantly under the direction of the HSE’s National Clinical Programme for Obesity. The service now has a full multidisciplinary team, with psychological, medical, surgical, anaesthetic, nursing, occupational therapy, physiotherapy, social work and dietetic expertise.
This has been a major development for patients with severe and complicated obesity not just regionally, but nationally, with patients coming from all over Ireland.

World Kidney Day at Portiuncula University Hospital
“World Kidney Day gives us an opportunity to stop and think about kidney disease, raise awareness of it and encourage everyone to actively know what their own kidney health measures are,” says Dr Paul O’Hara, Consultant General Physician and Nephrologist at Portiuncula University Hospital. Since it opened four years ago, the hospital’s kidney clinic under the remit of Dr O’Hara has been providing care to patients with kidney conditions across the hospital’s catchment area of East Galway and Roscommon. The clinic treats a wide range of kidney conditions, with referrals from both the hospital and GPs. Between 2023 and 2024, the clinic saw a 15% increase in new referrals, reviewed almost 600 patients and saw a 62% increase in patients with kidney disease receiving infusion-based therapies. Patients receiving haemodialysis and those undergoing kidney transplants are cared for at Merlin Park University Hospital.
The existing kidney day ward was recently relocated to the new 50-bed ward block to provide additional capacity in a new clinical space, significantly enhancing patient care to the highest standards.
Between 2023 and 2024, the kidney day ward saw an 81% increase in attendances with over 1,300 patient interactions. It allows for medical and nursing assessments, investigations and education on an ambulatory and outpatient basis. It also provides an ambulatory care pathway from the emergency department, allowing for rapid assessment of conditions for those who do not require hospitalisation.
Day Ward, Portiuncula University Hospital.
Hereditary haemochromatosis education programme for GPs
Ireland has the highest reported prevalence of hereditary haemochromatosis (HH) in the world, and the prevalence is highest in the West of Ireland. HH is a disease resulting in excessive absorption of dietary iron from the intestine. Over time, excess iron accumulates in the cells of organs including the liver, pancreas, heart and pituitary gland, causing damage.
In the North West, the majority of people living with HH are managed by either haematologists or gastroenterologists in Sligo University Hospital (SUH) and attend the day service for venesection. This procedure is low risk, with more than 80% of patients requiring minimal specialist input to manage their care. Therefore, this procedure can be provided safely in primary care. A small project team was established to explore transitioning care for these low-risk patients to primary care, providing care close to home in a GP practice, eliminating the need for patients to travel. This will also increase the capacity in SUH for other day case procedures and reduce waiting lists. It was determined that a bespoke venesection education programme for GP practices was required as no such project existed in Ireland.
The Centre for Nursing and Midwifery Education (CNME) Sligo, Leitrim, supported the development by Charlotte Hannon of a competency-based education and training programme, which has been approved by the Nursing and Midwifery Board of Ireland. The project team and the CNME worked in partnership with the Irish Haemochromatosis Association, which provided
Cancer programme and Organisation of European Cancer Institutes (OECI) update
Following a comprehensive review of our regional cancer programme from 2022 to 2024 – encompassing all aspects of cancer service delivery and involving staff at every level, from departments to senior leadership across all West and North West (WNW) hospital sites – we are proud to have achieved OECI Cancer Centre certification. This prestigious accreditation recognises excellence in patient-centred care, research, and organisational management, and affirms our ongoing commitment to continuous improvement through our Quality Improvement Plan.
EU collaborations
As part of the EU Mission for Cancer, the HSE WNW Cancer Programme are participating in WP9 of the European Network of Comprehensive Cancer Centres (EUNetCCC) initiative focusing on lung cancer initially. The establishment of the EUCCC network represents a harmonised and integrated approach to cancer care across the continent. The EU pilot sites convened in Berlin in February with Irish representation from the Department of Health, the National Cancer Control Programme (NCCP) and HSE WNW; Dr David Breen, Lung Cancer Respiratory Lead; Geraldine Cooley, GM Cancer MCAN; and Helen O’Reilly, OECI Coordinator.
Updates from HSE West and North West

From left: Emma Ball, General Manager Primary Care Sligo, Leitrim; Teresa Donnelly, Director Sligo CNME; Lynn Stoddart, General Manager Enhanced Community Care, Cavan, Donegal, Leitrim, Monaghan, Sligo (CDLMS); Akhtar Arif, Senior Nurse SUH DSU; Katy Taaffe, General Practice Nursing Coordinator CDLMS; Miriam Forde, Executive Director, Irish Haemochromatosis Association; Margaret Lee, Specialist Nurse; and Charlotte Hannon, Senior Tutor, CNME Sligo.
expert haematology nurses to support the programme and conduct the nurse competency assessments. Community Infection Prevention and Control and the primary care dietetics team were also involved in the delivery of the programme. The programme was delivered in the Sligo CNME on 5 March.
Presenter on the programme Dr Conor Mitchell, GP and HSE GP Lead for the Sligo/South Donegal Community Healthcare Network stated, “This is a vital training programme for GPs and GP practice nurses. The collaborative approach of specialist SUH consultants, GPs, the HSE North West and Sligo, Leitrim CNME has made delivery of this programme possible. We are delighted that more GP practices will now be able to provide this care to their patients. This will potentially remove the need for patients to attend hospital for a venesection procedure.”
‘Deep dive’ visit to Ireland
The CC14EU Deep Dive is an initiative focused on exploring how Comprehensive Cancer Centres across Europe can implement and sustain highquality, patient-centred cancer care aligned with Europe’s Beating Cancer Plan. Ireland’s cancer programme is being evaluated as Comprehensive Cancer Care Infrastructure. This involves in-depth analysis, knowledge sharing, and strategic discussions to strengthen collaboration and improve cancer outcomes across the EU. GUH was selected to host day one of the second ‘deep dive’ two-day visit as part of our National Cancer Programme review by European experts.
Behind Invisible Bars conference examines the health consequences of children living
in congregated settings
The reality of children living in congregated settings was examined at a conference in Sligo on 1 April 2025. Entitled Behind Invisible Bars, it brought professionals’ perspectives of the barriers and facilitators in accessing healthcare and optimising health outcomes and their experiences in delivering same. They addressed how to improve access to healthcare for vulnerable and excluded children, informed by a human rights-based approach. Children and young people living in temporary congregated accommodation are particularly vulnerable to poor health outcomes and face challenges in accessing healthcare in comparison to the general population. Attendees listened to an audio account from ‘John’, a child who has lived in congregated settings. He described how at one stage there were nine of his family living in two rooms. There was no privacy, no space to do homework. As they were sharing a kitchen with up to five other families, the spread of viruses was commonplace. He explained that getting a council house was “like a fresh start” and he now has privacy. Social exclusion can arise for many reasons and is common among people who experience state care in childhood, drug addiction, incarceration, homelessness, forced migration and/or those who belong to a minority ethnic group such as Traveller or Roma communities. It is crucial that health and social care providers understand and respond to the barriers people experience in accessing healthcare and the HSE Social Inclusion Unit based in Sligo plays a key role in reducing health inequality regionally.

From left: Jackie Austin, Director of Public Health Nursing, Dublin North; Máire McGetrick, Director of Public Health Nursing, Sligo, Leitrim; Emma Ball, HSE GM Primary Care, Sligo, Leitrim; Dr Aoibhinn Walsh, Consultant Specialising in Paediatric Social Inclusion, Temple Street; Patricia Garland, Social Inclusion Manager HSE West and North West; Teresa Donnelly, Director CNME Sligo, Leitrim; John Fitzmaurice, IHA Manager Sligo, Leitrim, South Donegal, West Cavan; and Dr Ray Nethercott, Royal College of Paediatrics and Child Health Officer for Ireland.


Taking Pride
June marks Pride Month but being an LGBTQIA+ ally and showing support is something we can all do, all year long. Here, two members of our HSE community share how they’ll be celebrating Pride…
MY STORY
Welverson Carvalho, Accountant and Financial Analyst with the HSE
Ten years ago, I moved from Brazil to Dublin in search of new opportunities and found a new home and my true self. I built my career as an accountant and financial analyst at the HSE National Drug Treatment Centre. Proudly queer, I have been part of the HSE Reach Out Network for over a year, building space for all of us and bringing the Pride celebration to the National Drug Treatment Centre. I am happily married for six wonderful years to a lovely Galway man.
Over the past few years, my friends and I have always made sure to be at the Dublin Pride Parade to support our community. I’m always looking to get involved in community events, like taking part in public projects at the Outhouse LGBTQ+ Centre. I participate in peer support groups and do my best to offer help and encouragement wherever I can.
I’ve tried all my life to show up for the LGBTQIA+ community and try to be part of Pride events every year. One of my fondest memories is my very first Dublin Pride Parade in 2015, just after the Marriage Equality Referendum – seeing families with their kids waving flags, smiling and showing up in full support of our community. As a gay immigrant from Brazil, where there’s still a lot of discrimination, witnessing that love and acceptance in Dublin was unforgettable. I felt safe and so welcomed. This year, I’ll be attending the parade again (alongside all my friends and Irish family) as part of the HSE Reach Out Network, and promoting Pride at the National Drug Treatment Centre for my work colleagues to be part of the celebrations, as well as getting involved in our community.
Pride Month to me is so much more than a celebration, it’s about visibility, resilience and community. It’s a time when I feel most connected to my identity and to others















who’ve walked similar paths. Showing up for each other, especially now with growing anti-LGBTQIA+ movements in other parts of the world fuelled by political power and fake information spreading on social media, Pride is more important than ever.
We’ve always had challenges, but one of the biggest facing our community today is the rise in hate and discrimination, especially against trans and non-binary people. In some parts of the world, laws are being made that take away our rights or make it unsafe to be ourselves. Mental health is another big issue. Many people, especially young people, deal with stress, anxiety or depression because of bullying, rejection or feeling alone.
My advice to anyone who wants to show their support and become an ally to the LGBTQIA+ community is to start by creating a safe, respectful space where people feel seen, heard and accepted. Educate yourself with the history and awareness about the community, using correct pronouns, challenging discrimination when you see it, taking time to connect with the community… Spaces like the HSE Reach Out Network are powerful for learning and building real support.





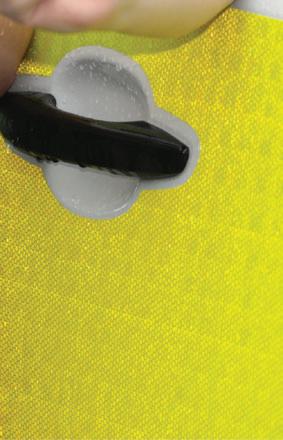





“Being inclusive, listening to people, displaying support, and respecting cultures, genders and who people are, is so important. And it’s not just during Pride Month, but all year long.”



MY STORY






Woods at Pride.
Julie Woods, CNM2, HSE Dublin and South East
I am currently working as a Clinical Nurse Manager 2 (CNM2), mostly in the area of health protection, a job I love. I’m from Carlow and live there still. I’m 52, have a husband, Paul, and three adopted children, who make me very happy.
I go to the Pride parade every year. My family and I also attended an event recently at Collins Barracks to celebrate 10 years of marriage equality. This year, I’ll be putting myself forward as a member working in the HSE at the Carlow Pride parade. I also celebrate in the office, too, with a Pride flag on my wall, some other decorations, and a T-shirt to wear. I’m also a member of the Proud to Work for Ireland Network and the HSE Cultural Diversity Network.
I just believe everybody has a right to live their lives and be as happy as they can be, without judgement, criticism
For information on Pride parades near you, and how you can join in on this year’s celebrations, visit bit.ly/HSEPride
or people telling them what to do. A while back, I took part in a programme called Landmark, and I met a lot of gay men at that time who expressed their desire to have a family. I recently ran into one of those men who told me I had inspired him and his partner to foster a child; they’ve been looking after a little boy now for five years, and I was so happy to hear their news. I think it’s so important for people to be able to be who they are, have a family if they choose, and to be shown respect.
It’s up to all of us to use our platforms to express where we stand with regards to allowing people to live freely and openly. Being inclusive, listening to people, displaying support, and respecting cultures, genders and who people are, is so important. And it’s not just during Pride Month, but all year long.
National Ambulance Service student shines in All-Ireland competition
The National Ambulance Service (NAS) is proud to celebrate the outstanding achievement of Ríona Bowen, Paramedic Intern, who recently led her interdisciplinary team to victory at the All-Ireland Interprofessional Education Conference (AIPEC) competition.
Ríona joined the UCC AIPEC team following an interprofessional learning seminar on dementia held at University College Cork (UCC). The seminar served as the launchpad for the competition, bringing together students from a variety of healthcare disciplines to collaborate and learn from one another. Following this, Ríona and her team competed in the UCC regional round on 12 March, successfully overcoming two other UCC teams to win a place in the national final.
The final, held in University College Dublin (UCD), brought together eight teams from colleges across Ireland. Representing UCC, Ríona’s team delivered a compelling presentation that secured them the top spot at the national level.
The competition centred on a case study involving an 82-year-old man living with heart failure and experiencing acute pulmonary oedema. Each team was tasked with developing a patient-centred care plan. Ríona’s team took a distinctive approach, focusing heavily on the social and quality-oflife aspects of care. Their plan addressed not only the clinical needs of the patient but also offered


support to his daughter, aiming to empower them both in navigating future healthcare decisions.
As team leader, Ríona credits her group’s success to the collaborative spirit and dedication of her teammates: Niamh Robertson (Postgraduate Medical Student), Catherine Hegarty (Social Work), Margaret Quigley (Physiotherapy), and Rachael O’Sullivan (Pharmacy). The team met weekly online in preparation for the final, pooling
their expertise to formulate a comprehensive, multidisciplinary care strategy.
Reflecting on the experience, Ríona described it as a turning point in her professional development: “It really broadened my understanding – not just of managing heart failure, but of how different disciplines approach care. It was eye-opening to see how our perspectives came together to build a stronger, more holistic plan.”
She encourages other students to embrace similar interprofessional opportunities, noting how the experience enhanced both her clinical knowledge and teamwork skills.
Congratulations to Ríona on her remarkable achievement! NAS is delighted to see the values of collaboration, patient-centred care and professional growth reflected so strongly in her work. Her success highlights the exceptional calibre of our student paramedics and the bright future of integrated healthcare in Ireland.
Win a €100 One4all voucher

To enter:
1. Email us a photo of yourself reading Health Matters
2. Tell us where you picked up your copy
3. Let us know your favourite article from this issue
You must have all three parts to be entered into the draw.
Congratulations
We’re delighted to congratulate Maria Heuston, Clerical Officer at Tipperary University Hospital, Clonmel as the winner of our Health Matters photo competition.
Maria loves reading Health Matters and finds the articles both informative and relevant. She mentioned that the day ward team often discuss some of the articles during their breaks. Maria’s favourite read in the spring edition was about Gardaí and HSE disability services working together in Tipperary.
Enjoy your One4all voucher, Maria – and thank you for being a loyal reader.
We love seeing our readers enjoy Health Matters. Now we are giving you the chance to win a €100 voucher just for sharing a snap.

Send your entry to internalcomms@hse.ie with the subject line ‘Health Matters photo competition’.
The competition closes on Friday, 27 June 2025. One lucky winner will be selected at random. Happy reading and good luck!
Updates from HSE Dublin and Midlands
Let’s Connect campaign launched to mark World Maternal Mental Health Day
World Maternal Mental Health Day is an international campaign dedicated to talking about mental health problems during and up to one year after pregnancy. It’s all about raising public and professional awareness of maternal mental health difficulties, advocating for women affected, changing attitudes, and empowering women and families by helping them access the information, care and support they need to keep well and recover.
Recent research by the RCSI Centre for Positive Health Sciences, in collaboration with Minding Me, the Perinatal Infant and Early Childhood Mental Health Working Group in Dublin South, Kildare and West Wicklow, revealed that 77% of respondents experienced feelings of loneliness sometimes, often or always.
A range of activities took place in Dublin South, Kildare and West Wicklow on World Maternal Mental Health Day, 7 May, for the Let’s Connect campaign, including distribution of information materials to key audience groups in the form of ribbon cards, postcards and poster displays.
The Let’s Connect ribbon cards are available in maternity hospitals and have been distributed to local groups that work with mothers and young families and family resource centres. The card represents connection and we are encouraging those in the community, including new mothers, to reach out to one another. The cards outline the difficulties new mothers
New Quality and Patient Safety (QPS) manager for Women and Infants’ Services

From left: Emma Berney, Co-ordinator, Co Kildare Children and Young Persons Services Committee; Eileen Whelan, Regional Director of Nursing & Midwifery, HSE Dublin and Midlands; Emma Reilly, Child Health Programme Development Officer; Niamh Crudden, Resource Officer for Suicide Prevention, HSE; Paul Ridgeway, Interim Regional Clinical Director, HSE Dublin and Midlands; Adele Kane, Social Worker, National Maternity Hospital Perinatal Mental Health Team; Pauline Keogh, Director of Public Health Nursing, Kildare; Carole Broadbank, Integrated Healthcare Area Manager, Midlands; and Fionnuala Curry, Co-ordinator, Co Wicklow Children and Young Persons Services Committee.
can experience and where they can get information to support them in the first year after giving birth.
Kate Killeen White, Regional Executive Officer for HSE Dublin and Midlands said, “I am delighted to give my support to the Let’s Connect campaign, which aims to empower and support women to look after their mental health and wellbeing. This campaign is about raising awareness of mental health challenges during pregnancy and the year after birth –something that affects one in five women. It’s about talking openly, reducing stigma, and supporting women and families to get the care they need.
“This year’s campaign reminds us that while motherhood brings joy, it can also be tough – and that support, connection, and community make all the difference. Over the coming weeks, the campaign will encourage conversations, connections, and action through simple gestures like sharing a ribbon card or directing someone to themotherhoodprogramme.ie for support. Thank you for being part of this important conversation.”
You can follow the campaign on our social media channels and reshare the content to your page using #maternalmentalhealthmatters #mindingmeDSKWW #letsconnect
Ms Joy Geraghty started her new role as QPS manager for Women and Infants’ Services in HSE Dublin and Midlands in May. Joy has extensive midwifery, nursing and QPS experience. Congratulations Joy. Wishing you every success in your new role.
Updates from HSE Dublin and Midlands

Basia Award presented to Tullamore nurse
Nicola McCormack, Orthopaedic Scrub
Nurse is the first ever recipient of the Basia Award in the Midland Regional Hospital Tullamore (MRHT). This award was created by the Operating Theatre Department in memory of deceased colleague Barbara Michalec (Basia), a perioperative nurse in MRHT who went above and beyond to ensure her patients received the highest quality of care. Organisers of the award said, “Nicola, a new graduate when she entered
the Operating Theatre Department, quickly developed into an exemplary nurse, showcasing remarkable skills and knowledge in her area. As a strong patient advocate, she verbalises their needs to all team members honestly and respectfully. Nicola’s commitment to continuous professional development is evident through her pursuit of a postgraduate diploma in perioperative nursing.”
This award celebrates nurses who demonstrate excellence in their roles. Nicola is the winner of the €1,000 education bursary donated by the Orthopaedic Trauma Service from the Irish Hip Fracture Database Fund.
Celebrating a life-changing initiative: the launch of Cian’s Kennels mobile pet therapy service at Regional Hospital Mullingar
In a heart-warming celebration that intertwines hope, healing and the unconditional love of furry companions, Cian’s Kennels launched its ground-breaking mobile pet therapy service at the Regional Hospital Mullingar on 11 April. This initiative comes as a compassionate response to the profound impact pet therapy has had on patients, particularly exemplified by the special bond formed between two-year-old LJ Kiernan from Collinstown and Walter, a dedicated therapy dog. LJ’s journey through cancer treatment at Crumlin Hospital was filled with uncertainties and challenges. Yet, in those moments of struggle, Walter, the lovable therapy dog, offered much-needed comfort and companionship. The bond formed during their time together became a beacon of hope and resilience, proving that sometimes, healing comes in the form of a wagging tail and a warm, furry friend.
LJ officially launched the new service by cutting the ribbon at the launch in Regional Hospital Mullingar.
The mobile therapy service will allow Cian’s Kennels to bring trained

therapy dogs like Walter directly to paediatric patients in Mullingar, offering emotional support during their recovery journeys. Research has shown that animal-assisted therapy can significantly reduce anxiety, improve mood, and foster a sense of security, making this initiative an invaluable addition to the hospital’s care services.
Speaking at the launch, Margaret Kelleher, Hospital Manager, Regional Hospital Mullingar said, “We are delighted this morning to welcome Cian’s Kennels into service in Mullingar Hospital. It will deliver such an important service to the children that are inpatients in our hospital.
Pet therapy has a profound effect on the delivery of care and this is such a great day, a great initiative for Mullingar Hospital. And thanks to Cian’s Kennels for all their efforts.”
Dr Jennifer Finnegan, Consultant Paediatrician, Regional Hospital Mullingar added, “Cian’s Kennels is a fantastic initiative where patients from the paediatric ward can come out to the mobile unit and spend time with therapy dogs, relieving stress and anxiety and ultimately helping in their treatment.”
For more information, visit cianskennels.ie
Over 90% of locals feel Tallaght University Hospital (TUH) is of benefit to the local community
The Health Assets and Needs Assessment (HANA) report, carried out by leading academics at Trinity College Dublin, found that over 76% of those living in Tallaght are satisfied with the quality of care they have received at the hospital, while almost 78% would recommend TUH to a friend.
The HANA report, which was supported and funded by the Adelaide Health Foundation and the HSE, was launched on 13 March in Tallaght Community Library. This study is an important one for hospital management as it informs how they will develop and plan their services in the future.
Some of the report results:
• Healthier lifestyles: Smoking rates have dropped from 69% in 2001 to 32% in 2024.
• More active residents: Since 2014, strenuous exercise has more than doubled, rising from 2.7% to 5.8%, with increasing participation across all activity levels.
• Greater use of community spaces: 98% of residents value public recreational areas, and 84% use public transport, reflecting the impact of investments in parks, cycle lanes, and local infrastructure.
• Educational gains: The proportion of residents with a third-level qualification has grown from 6% in 2001 to 35% in 2024, helping them get better jobs and improve their lives.
• Expanded healthcare facilities: 47% of residents attended TUH for tests or treatment in the past year – more than double the 2014 rate.

The results of the last HANA report (2014) informed which areas we prioritised for development:
• Waiting lists was a key issue identified in the last HANA study. The Reeves Day Surgery Centre, opened in 2020, has significantly reduced wait times for day surgery cases.
• Additional mental health services was a HANA (2014) recommendation; TUH developed a new liaison service to manage issues related to self-harm.
Other improvements include: 48 new beds were added for age-related services with the opening of the Medical Age-Related Unit at Tymon North in 2020.
For more information and access to the full report, Health Assets and Needs Assessment (HANA) in Tallaght 2024, visit bit.ly/TCD-research
Updates from HSE Dublin and Midlands
The Butterfly Project: children grieve too
The Intensive Care Unit (ICU) at St James’s Hospital was proud to launch a new range of resources that support children coping with the death of a loved one in critical care. The launch took place in November 2024 during National Children’s Bereavement Awareness Week and marked ten years of The Butterfly Project.
The project provides a range of material available to children affected by bereavement and an information booklet for their caregivers. The packs also contain a symbolic butterfly bookmark designed by ICU nurses Caoilfhionn Hasket and Natalia Fernandez.
Prepared by ICU staff, the resources are handed over with care, offering comfort and connection to families during difficult times. Over the past decade, The Butterfly Project has
SAP to go live in Dublin and Midlands

Members of the nursing team at the launch of the new resources.
supported children, fostering hope and healing. This milestone celebrates its impact while renewing our commitment to supporting grieving children and families with compassion and understanding. Assistant Director of Nursing,
Rynagh Gilligan, End-of-Life Care Coordinator Bettina Korn, and Jean O’Reilly, who initiated the project 10 years ago, were present to mark the launch of the new resources, along with current project lead, Shona Keogh, and sponsors IIS Space.
We’re preparing to switch from our old systems to IFMS SAP S/4HANA in the Dublin and Midlands region. This process is known as a ‘cutover’ and means that the final data migration will take place and the new system will go live. System changes commenced on 2 May and will be complete by 14 July with no system outages expected. The system will go live on Tuesday, 1 July and users will have phased access. Training is mandatory for all impacted teams. Your line manager will help you to access the training you need. A list of frequently asked questions (FAQs) to help you understand what IFMS means for you is available on SharePoint at bit.ly/IFMSFAQ
Tallaght
University
Hospital appoints new CEO

The Board of Tallaght University Hospital (TUH) have announced the appointment of Barbara Keogh Dunne (Registered General Nurse) as CEO.
Professor Anne-Marie Brady, Chair of the Hospital Board says, “I am delighted to welcome Barbara as our new CEO. She brings a wealth of experience, energy and insight to our hospital as well as a proven track
record in healthcare leadership. I want to acknowledge the work of John Kelly, who has acted as Interim CEO for the last few months.”
Barbara Keogh Dunne says, “I am honoured to accept the role of chief executive officer at Tallaght University Hospital. I look forward to working with the team to further lead and drive innovation and to positively impact on patient and staff experience at the hospital.”
Ms Keogh Dunne’s most recent role was General Manager of Connolly Hospital, Blanchardstown.
St James’s Frailty Intervention Team
In January 2024, St James’s initiated a service improvement strategy to redesign the care of adults aged 70+ in the emergency department (ED), which led to the introduction of the Acute Frailty Pathway by a multidisciplinary team known as the J-FIT Team. J-FIT is dedicated to the early identification and comprehensive assessment of at-risk patients in the ED. Once assessed, holistic and personalised treatment plans are swiftly implemented in collaboration with ED medical and nursing teams.
After a fall at home, 81-year-old Gerry came by ambulance to St James’s Hospital. Following medical assessment, J-FIT completed a comprehensive assessment and put a plan in place so Gerry could go home four hours later with a supportive discharge plan.
“When I met her [a member of the J-FIT team], she actually stayed with me for some considerable time and she eased my pain. She explained what had happened and what would happen next. I couldn’t believe I might get home that day,” says Gerry.
Gerry was discharged on a recovery pathway with a visit at home the next day from the St James’s Active Recovery Team (ART).
Three weeks after his ED visit, “I’m after amazing myself,” Gerry says. “Today, I walked down the road and back, and I am good, I’m very pleased and very thankful.”
In the first 12 months:
• 31% of patients were discharged directly from the ED
• Admission rate reduced from 59% to 55.3%
• Length of stay reduced from 14.5 days (February 2024) to 11.29 (December 2024)
These findings support international evidence that early access to the right care leads to better patient outcomes and significant cost savings.
From bump to baby: healthy snacks address wellbeing needs of MRHP maternity patients
In January 2024, the maternity ward at the Midland Regional Hospital Portlaoise, in conjunction with the Nutrition and Hydration Steering Committee, introduced snack bags to support maternity patients’ nutritional needs. This initiative was developed by Dietitian Caoimhe Kenny-Bowe in collaboration with the hospital’s catering department. The snack bags are especially helpful for breastfeeding mothers who require extra energy and may feel hungrier throughout the day. This initiative is provided to all patients on the maternity ward. The bags include a variety of nourishing items such as homemade flapjacks, crackers with cheese or peanut butter, fresh fruit and cartons of orange juice.
The feedback has been overwhelmingly positive. Patients have described the snack bags as “great”, “very good and lovely” and appreciated that “they keep us well fed throughout the day”. One mum shared, “I don’t eat them then and there – I save them for later.”
The initiative reflects our ongoing commitment to supporting the comfort and wellbeing of new mothers and their babies.
Minding Your Wellbeing programme gets underway in the Midlands
The National Learning Network (NLN) Athlone attended the Minding Your Wellbeing programme, delivered by Health Promotion and Improvement (Midlands). This programme incorporates a universal approach to the promotion of positive mental health and wellbeing for everyday living.
The main aim of this training is to increase participants’ understanding of what influences mental health and wellbeing and develop strategies that can be used to promote positive mental health in their personal lives and professional role.
Participants are provided with a unique opportunity to learn and practise key elements of mental wellbeing such as mindfulness, gratitude, self-care and resilience. The programme, designed by the Health Promotion and Improvement Service, is available to all HSE staff, section 38 and 39 employees. Attendance can be face to face for a full day, or alternatively, viewed online in a series of five 20-minute videos.
You can book a place on the one-day workshop by contacting your local health promotion officer.
For Minding Your Wellbeing in the Midlands, please contact healthpromotion.midlands@hse.ie or visit bit.ly/HSEWellbeing

Martin Murphy, and Emma O’Connell, Programme Instructors, NLN; Sara Ganly, Secretary; and Michele Baker, Health Promotion and Improvement Officer, Health and Wellbeing, Athlone.
Updates from HSE Dublin and Midlands

Clubhouse Manager; Barry McKeever, participant; Lucy Bell and Mary Ruth Fallon, facilitators.
Empowering health through literacy – closing the digital gap
In today’s digital world, understanding health information online is essential, especially for those with mental health challenges and chronic health conditions. Members of Platinum Clubhouse, Newbridge, Co Kildare decided to tackle the digital divide head-on as they found tasks like emailing for prescriptions, understanding medication labels, deciphering medical terms and navigating online health resources overwhelming. To bridge this gap, Platinum partnered with Adult Literacy for Life, Newbridge Family Resource Centre and Bergin’s Pharmacy in Newbridge and co-created a practical hands-on course to demystify the digital world.
“I was happy for the learner to visit the pharmacy and practise the skills they learned in the classroom… a pharmacist wants to always ensure what is dispensed is understood. No one should ever feel a question is not important,” says John Tallon, Pharmacist at Bergin’s Pharmacy in Newbridge.
Members discovered simple solutions like printing bottle labels in a bigger font was a practical ‘hack’ they could ask for to empower them to manage their medication safely and effectively. Soon, members reported feeling less lost with medical jargon, more confident asking healthcare providers for clear explanations, and more secure managing their health online.
“I found the information of how to engage and talk to your doctor and ask questions very relevant to me as I didn’t even know that I could ask questions. I normally just agreed and nodded with my doctor. It was a real eye-opener to realise I wasn’t the only one who felt that way,” says one learner on the course.
This programme will be offered across EVE’s network of services and is being adapted for those with chronic health conditions.
Dementia Awareness for An Garda Síochána
Dementia awareness is crucial for public service providers, especially An Garda Síochána (AGS), who support individuals living with dementia in the community. AGS plays a key role in assisting during crises, such as when someone living with dementia experiences a delirium or difficulty orientating their way home following an episode of purposeful walking.
During the COVID-19 pandemic, AGS recognised the increasing need for support for vulnerable individuals, particularly older people. The Dublin South West Integrated Care Programme for Older Persons Community Specialist Team (DSW ICPOP CST) supported many of these individuals to remain living at home. Both the DSW ICPOP CST and AGS recognised the need for better collaboration to support this group effectively. Thanks to existing strong relationships between AGS and DSW ICPOP, a new integrated pathway was created to identify and assist older people living with dementia. A Memorandum of Understanding and Steering Committee was established to allow direct referrals to the DSW ICPOP CST.
AGS expressed interest in dementia training for their members, leading to the development of a tailored HSE education programme for local community policing teams in Dublin South West. The programme, designed by DSW ICPOP professionals, covers dementia, delirium, communication, safer walking strategies, assistive technologies, and the Assisted Decision Making (Capacity) Act 2015.
The training has been well-received, with AGS participants reporting increased knowledge and confidence. The programme was extended to wider AGS members in the Dublin Metropolitan South and West Regions and to new probationary Gardaí. In recognition of its impact, the initiative won the Best Community Project HSE Spark Innovation Award in 2023 and was presented at the Irish Gerontological Society Conference and the All-Ireland Conference on Integrated Care. HSE staff interested in learning more about dementia can access a new course on HSeLanD entitled “Support pathways for people with non-cognitive symptoms of dementia”.
Platinum Clubhouse is a peer-led community that provides mental health recovery programmes. For more information, contact caroline.darby@hse.ie | Watch a video about the course on YouTube at bit.ly/DigitalHealthKildare
NATIONAL SERVICE PLAN 2025
The HSE’s National Service Plan (NSP) 2025 was published on 14 January. The plan sets out the range of health and social care services that will be provided to the people of Ireland, by the HSE, within the allocated budget of €26.9bn, a €1.6bn increase on 2024. This includes a €297.8m investment in new service developments including enhancing mental health, older persons and disability services.
The publication of the plan coincides with the 20th anniversary of the establishment of the HSE. During this time, health and social care services have been significantly reshaped to improve health outcomes for the people of Ireland. While we have seen significant progress over the last three years, a priority for the HSE in 2025 will be to further reduce waiting times.




We will place a specific focus on maximising an integrated approach to care delivery across community and acute settings, enabled through our new health regions.
IN 2025…
99%
95% of children aged 24 months who have received the MMR vaccine
3.8M of all attendees aged 75 years and over at emergency departments who are discharged or admitted within nine hours of registration
110K community intervention teams referrals
219K women in the eligible population to have a complete mammogram
1.2M contacts with GP out of hours service 24M home support hours to be provided to 60,000 older persons persons to be covered by medical cards
home support hours delivered to persons with a disability
1.5M
Over
2M inpatient and day cases to be discharged
31,166 general adult community mental health referrals seen by mental health services
KEY PRIORITIES FOR 2025
Collectively, these commitments are the framework within which the HSE will deliver services and measure its performance throughout 2025.
Healthy communities
We will work to improve people’s health and wellbeing and reduce inequities by:
• Delivering screening programmes to detect health issues early
• Improving opportunities for people with disabilities
• Supporting population-based planning for health and social care
• Making sure women’s voices, needs and experiences shape women’s healthcare, improving health outcomes
• Protecting and improving children’s health so they can live their healthiest lives
Receiving the right care
We will build meaningful engagement between patients, families, health professionals and organisations by:
• Revising our approach to services for adults and children with disabilities
• Improving support for adults who may be at risk of harm or abuse
• Delivering safe, high-quality, person-centred health and social care through better models of care, clinical strategies and service user-driven initiatives
• Using the best available research and evidence to guide health service care, management, strategy development and reform
Receiving
care in the right place
We will ensure our planning efforts support our population to remain active and independent in their communities and homes for as long as possible:
• Supporting community-based care, focusing on general practice and primary care options
• Expanding alternative care pathways
• Continuing to implement the National Cancer Strategy 2017-2026
• Continuing to set up an inclusive trauma system for Ireland
• Providing palliative care that improves the quality of life of both patients and their families
• Making sure disability services support people in their own communities
Receiving care at the right time
We will continue to promote positive mental health and mental wellbeing across the population:
• Improving access to health services for vulnerable and excluded groups
• Reviewing how disability support needs are assessed and improving access times
• Improving urgent and emergency care across hospital admission, ED operations, patient flow and discharge
• Working towards wait time goals of 12 weeks for inpatient/day cases and gastrointestinal (GI) scopes

and 10 weeks for new outpatient appointments
• Managing payments to healthcare professionals for community-based free or reduced-cost services
Strong foundations
We will support, develop, retain and expand our workforce to ensure the provision of quality healthcare to the public, designing further tailored approaches to attract and retain professionals within our services:
• Providing for a new maximum year-end Whole Time Equivalent (WTE) limit of 133,306 in 2025; a net additional 3,553 WTE in new service developments
• Shaping a service-wide culture that reflects the values of the HSE – care, compassion, trust and learning
• Delivering information and communications technology services and support throughout the HSE to facilitate integrated care
• Seeking to secure government approval for the national Electronic Health Record (EHR) business case and starting procurement
• Beginning the Community Connect System project that will support the administration and delivery of services and care within and across community healthcare settings
• Implementing key solutions such as the single national immunisation system and national medical laboratory solution and completing delivery of the national imaging solution (radiology)
If you would like further information on the National Service Plan, please contact the National Planning and Performance Team at planning@hse.ie The National Service Plan 2025 is available at: bit.ly/HSENSP2025

Celebrating 30 years of the Bone Service at St James’s Hospital
In February, the dedication and commitment of Professor J. Bernard Walsh, Director of the Bone Health and Osteoporosis Unit at St James’s Hospital, who founded the service 30 years ago, was celebrated.
The event featured guest speakers, including Professor Eugene McCloskey from the University of Sheffield and Dr Emer Ahern, President of the Irish Gerontological Society and Consultant Orthogeriatrician at Cork University Hospital. Professor Walsh spoke about the history of MISA and the establishment and continued growth of the Bone Health Unit.
In other news...
Celebrating cultural diversity
The HSE’s Cultural Diversity Network for staff from diverse cultural backgrounds held a celebratory event in May at Dr Steevens’ Hospital. Network members shared food from their cultural backgrounds, wore traditional clothing, and learned about the rich cultural diversity of their HSE colleagues.
“Our workforce has long been one of the most diverse in the state, and non-Irish staff now make up almost a fifth of our total workforce,” says Anne Marie Hoey, HSE Chief People Officer. “I look forward to seeing the network continue to grow. By hearing the voices and lived experiences of staff, we will further strengthen the culture of inclusion in the HSE.”
The network now has members from all over the country and offers support, visibility and a voice for staff; provides an opportunity for staff to contribute personal stories and experience into HR policy and practice; and assists with raising awareness on DEI issues to the wider workforce.

Second National HSE Men’s Health Plan launched –Play Your Part
The second National HSE Men’s Health, Healthy Ireland – Men (HI-M) 2024-2028 was launched late last year by Dr Philip Crowley to a large webinar audience of staff and stakeholders. The new plan outlines a range of tasks for the coming years to be delivered in conjunction with a number of HSE departments with the support of the Department of Health.
The plan is available to download at bit.ly/MensHealthPlan | Men’s Health Week takes place 9-15 June. For information and campaign assets, visit mhfi.org
Advancing procurement through partnership and collaboration
Procurex Ireland 2025
Procurex Ireland is the leading national event for public procurement, uniting buyers, suppliers, and policy influencers from across Ireland’s procurement community. Designed to drive strategic improvement, it offers direct engagement with decisionmakers, innovative suppliers, and practical solutions to enhance procurement outcomes, particularly in sectors like healthcare.
21st National Health Summit
The event welcomed over 850 attendees at the RDS in Dublin. Guest speakers included Emer Higgins TD, Minister of State for Public Procurement, Digitalisation and eGovernment, and Anne Stewart, Assistant Secretary General, Office of Government Procurement. As an official event partner, HSE Procurement delivered a keynote address on “Navigating Procurement in the Health Service”, highlighting the crucial role of
procurement opportunities in enhancing patient care outcomes.
Speaking at Procurex Ireland, Siobhan Dunphy, Assistant National Director of Procurement, highlighted the importance of the event as a forum for meaningful exchange: “It provides opportunity for a two-way dialogue – we were able to explore new and innovative solutions, while suppliers gained insights into upcoming opportunities for doing business with the HSE during 2025.”
HSE Procurement participated in the 21st National Health Summit at Croke Park, Dublin – an influential event where healthcare leaders, professionals and experts gathered to discuss new strategies for planning, service delivery, and improving patient experiences across Ireland. The summit provided a key opportunity to highlight procurement’s critical role in fostering innovation and enhancing outcomes within the healthcare sector. Within the “Productivity and Organisational Change” theme, Siobhan Dunphy, Assistant National Director of Procurement joined a panel discussion to discuss productivity challenges in our health service. The panel demonstrated strong alignment, with Siobhan offering insightful perspectives on how strategic procurement plays a vital role in advancing patient care.
Staff inspire secondary students at nursing and midwifery careers day
An annual event in University Hospital Limerick (UHL) promoting nursing and midwifery careers in the Mid West was attended by an enthusiastic audience of secondary students from Limerick, Clare, Tipperary and North Cork. Led by the Nurse Practice Development Unit team, the HSE Mid West Promoting Nursing and Midwifery Showcase brought together nurses and midwives from emergency medicine, theatres, oncology, high dependency unit, public health, mental health, children’s nursing and pain to speak to the young students about the many career options available within the professions of nursing and midwifery. The event drew appreciative comments from the students for the inspiring presentations from staff and the many interactive stands that were prepared for the event, which took place in the Clinical Education and Research Centre at UHL. The occasion was also one of the last major engagements attended by Maura FitzGerald, Head of Nursing Integration and Development, who retired at the end of the month after a long career in nursing at UHL.
Aids and Appliances – supporting care across the Mid West
The Aids and Appliances (A&A) department provides a comprehensive in-house service across the Mid West region, supporting community healthcare by supplying essential equipment. We support people in managing medical conditions, and those in recovery and maintaining their independence, through supply of mobility aids, bathroom and bedroom supports, orthotics and prosthetics, daily living aids, and respiratory care.
In 2024, A&A delivered over 52,000 pieces of equipment and recycled 14,500 items, representing €4.5m being reused to support care needs. Our stores team expertly manages equipment through its lifecycle, from tagging and stock control to decommissioning and recycling. Using the AssetTrak system, all assets are tracked, ensuring efficiency and full traceability. Serving over 600 product types, we support the Sláintecare vision of enabling individuals to live independently at home. We encourage the return of unused items (arranged via email to aastores.mw@hse.ie). The items are decontaminated, tested and reactivated for reuse, contributing to both sustainability and cost-effectiveness in community healthcare.
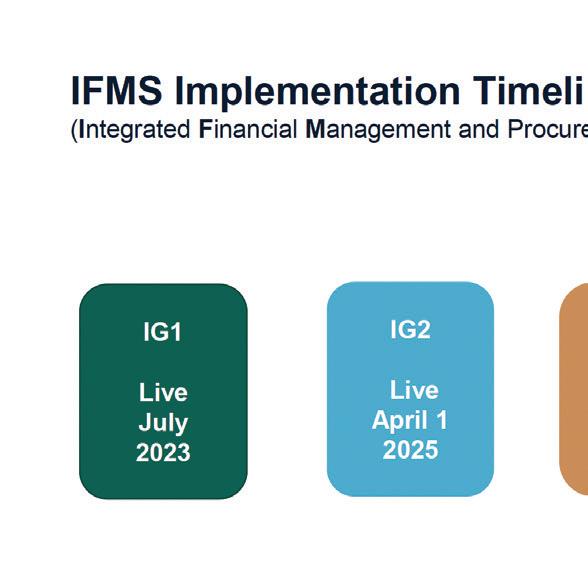
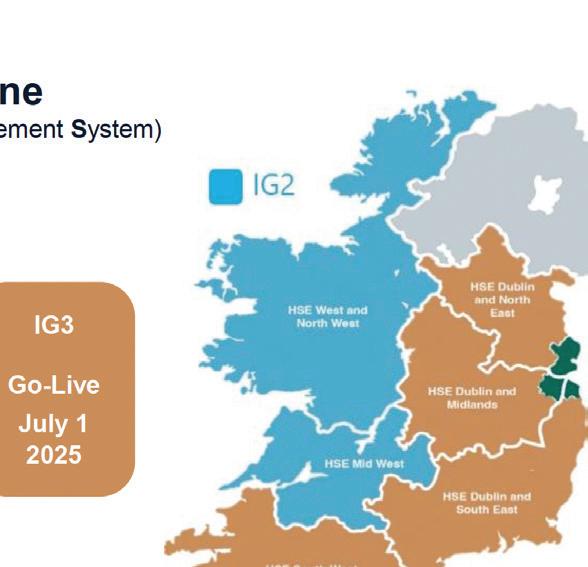

Update on IFMS project
IFMS, the finance and procurement system used by staff to order and pay for goods or services for the HSE, went live in HSE Mid West and HSE West and North West on 1 April 2025. HSE Dublin and Midlands, HSE Dublin and North East, HSE Dublin and South East and HSE South West are on track to go live on 1 July. Staff training has commenced and will continue across May and June. In the weeks post go-live, staff will be supported via dedicated helpdesks and onthe-ground support. IFMS brings many benefits to users of our health services.
Health Passport (HSE) App gets an update
The National Disabilities Quality Improvement team have updated the Health Passport (HSE) App, which now includes additional content and functions, with sections on critical information, personal information, communication, decision-making, medical history, food and drink, and personal care. Updates include:
• New layout with tabs

• Updated email function
• Medication list input
• Reminder function
• Read/edit tab
The app can be used by any adult/ child for whom communication is difficult (e.g. people with disabilities, dementia, mental health issues, or those from other countries who do not have English as their first language).
There is a guidance document, and YouTube video to support you to fill in the passport. Scan the QR code for further information, or if you have any questions, contact Health.Passport@hse.ie
Partnership project aims to highlight link between smoking and persistent HPV
The National Screening Service has led on a project with Tobacco Free Ireland, the Nurses in Colposcopy Clinics in Ireland Association, and UCC’s School of Public Health to create new resources about smoking and HPV (human papillomavirus).
HPV is the cause of most cervical cancers and smoking increases the risk of having an active HPV infection. This can lead to harmful health outcomes such as cell abnormalities in the cervix and cervical cancer.
The resources help healthcare staff to support women attending colposcopy to understand the link between smoking, HPV and cervical cancer; and access smokingcessation services if they choose to.
Information leaflets for patients can be ordered at healthpromotion.ie
HSE Talking Health and Wellbeing podcast reaches 100th episode
The HSE Talking Health and Wellbeing podcast celebrated its 100th episode on 7 May with a focus on advice for parents of anxious children. This episode featured colleagues in the HSE South East region who work as part of the Le Chéile family support pilot programme, which is funded by Sláintecare. Episodes such as this, with parenting advice, are some of the most popular of the series.
To date, the podcast has showcased a vast array of health professionals, service users and partner agencies, and the themes and topics covered have varied widely from healthy eating and obesity to sexual health, stress and psychological support and advice. To listen, visit hsepodcasts.podbean.com
All-Island Medication Safety Conference
Reducing medication-related harm was the theme of the first ever All-Island Medication Safety Conference – an interactive workshop held at Dublin Castle in November. Research, safety initiatives and resources were shared by patient advocates, policymakers from the Departments of Health (North and South), the World Health Organization and healthcare professionals. Learning was shared through 100 posters, six oral presentations and lively discussions. The co-hosts IMSN and Transforming Medication Safety in Northern Ireland, and partners the HSE National Medication Safety Programme and RCSI School of Population Health, aim to make this a biennial all-island conference, ensuring ongoing collaboration and learning.
HSE and HealthTech Ireland launch National Health Collaboration Council
The HSE and HealthTech Ireland have evolved the partnership from the Memorandum of Understanding (MoU) signed late 2024 to now establish the National Health Collaboration Council. The council, with shared governance between the two organisations, has the vision of the MoU at its core “to identify initiatives that will enhance patient care, address healthcare challenges and realise opportunities for improvement”. Several key initiatives are now underway, each with a defined vision, objectives and timelines. These initiatives are in the areas of Medical Devices and Diagnostics, Technology and Transformation, Clinical Informatics, Procurement, and Innovation and Strategy. The role of the National Health Collaboration Council (HSE and HealthTech Ireland) is comprehensive and includes but is not limited to:
• Strategic collaboration to support the successful creation and delivery of HSE national strategies, frameworks and programmes of work.
• Incorporating international insights, learnings and member perspectives in a structured, facilitated way to accelerate the success of programmes of work.
• A forum to collectively address pressing challenges in areas like procurement, sustainability, regulation, and reform.
HealthTech Ireland is an independent trade association representing health technology companies in Ireland, supporting innovation to improve patient care and healthcare delivery.
HSCP Day 2025
National HSCP Day was celebrated on 9 April with the theme “Innovating Health and Social Care: Embracing Technology, Research and Evidence”. Health and social care professionals enhance patient outcomes, improve service delivery, and foster a forward-thinking approach to care by focusing on the transformative power of integrating technology, research and evidence-based practices in health and social care. Teams of HSCP in each of the health regions participated in the day sharing innovative projects, research findings and success stories. The day ended with the lighting of Cork City Hall to acknowledge the contribution of HSCP.

From left: Claire Keating, Radiation Therapy Services Manager, CUH; Louise Reid, Psychology Manager, CUH; Olivia Wall, Health and Social Care Professions Regional Practice Education Coordinator; and Megan Goodale, Occupational Therapy Manager, CUH.
NICCIA Conference Celebrates 25th anniversary in Waterford
The Nurses In Colposcopy Clinics Ireland Association (NICCIA) Conference marked its 25th anniversary in March at the Granville Hotel in Waterford. The event brought together healthcare professionals, researchers and industry experts for two days of presentations and networking. Among the guest speakers were Karen Farrer, a retired advanced nurse practitioner who presented the history of the NICCIA; Dr Zeta Dooly, a lecturer and researcher in digital education who gave a talk on learning through artificial intelligence; Shirley Trimble, a clinical specialist physiotherapist in pelvic health and continence; Dr John Stratton, who spoke about cervical cancer treatment; Aoife Hartwell, who talked about supporting women following a cervical cancer diagnosis; and Professor Walter Prendeville, who shared insights on the evolution of technical developments in cervical cancer prevention. The event blended education, innovation and celebration, honouring the achievements of the past while looking ahead to the future of cervical care.
New programme supporting quality care for children with complex needs in the community
The Centre of Children’s Nurse Education (CCNE) launched a new programme in September 2024: An Introduction to Caring for Children with Complex Needs in the Community. Developed by a multidisciplinary team, the programme addresses integrated care pathways, child- and family-centred care and explores the psychosocial challenges that children and their families may experience. To date, 102 participants have completed the programme, reporting enhanced knowledge and confidence to deliver the unique and specialised care these children require. To increase accessibility, the programme will be delivered nationally by the CCNE and regional Centres of Nursing and Midwifery Education.
Upcoming programme: 4 September CCNE, Children’s Health Ireland at Crumlin; bookings via HSeLanD for registered nurses and health and social care professionals.
Driving change: Patient Flow Academy
The HSE Patient Flow Academy continues to progress its work in 2025. The academy aims to improve patient flow by supporting staff to identify, define and improve processes, pathways and systems for the safe and timely delivery of care. This is driven by a culture of continuous improvement, collaboration and sharing of what works well for sites.
‘‘Our programme plan for 2025 includes initiatives to continue to support and drive patient flow best practice, innovation, networking and collaboration,” says HSE National Clinical Advisor and Group Lead Dr Mike O’Connor. “Our monthly Patient Flow Academy webinar series attracts hundreds of mainly frontline clinical staff logging on every month to listen, learn, share and collaborate on good practices around patient flow and safety. We are very focused on sharing learning around innovative practices. It’s a supportive environment with the emphasis on sharing information to improve how we all work. Our March webinar focused on ‘Urgent and Emergency Care 2025 and Beyond: Breaking the Cycle’. Our April webinar discussed ‘Innovation in Urgent and Emergency Care: Virtual Care’ and included presentations by Cork University Hospital staff on Urgent Virtual Care and by St Vincent’s University Hospital staff on Virtual Care Wards.”
You will find all of the webinars and other Patient Flow resources at hse.ie/patientflow
Child and Family Nursing conference looks at evolving services Cork University Hospital (CUH) hosted its 15th Child and Family Nursing conference in April. Ms Helen Cahalane, Director of Nursing, gave an inspiring opening address, welcoming a full auditorium from counties throughout Ireland and the USA. The conference theme was ‘Evolving Landscapes in Children’s Nursing’, demonstrating great advancements in delivering quality care to children and their families. The large attendance reflected shared personal and professional interest in keeping up to date and a desire to continue evolving services. The presentations and poster display revealed great innovation and developments in child and neonatal healthcare.
Making Every Contact Count (MECC)
In February, the MECC programme hosted a successful webinar titled “Making Every Contact Count and Integrated Care in Chronic Disease Prevention”. The webinar aimed to inform health and wellbeing stakeholders about the Chronic Disease Programme, the Integrated Care Programme, and how the MECC initiative aligns with these frameworks. A total of 571 people registered. One participant commented, “I am so inspired and reassured by hearing this group of professionals reminding us of the importance of making closer connections, building relationships and using a people-centred approach in our work.”
Watch the webinar recording on YouTube at bit.ly/MECCwebinar
For further queries, please contact makingevery.contactcount@hse.ie
New €2m cath labs at University Hospital Limerick enhancing local patient access to innovative cardiac procedures

At the official opening of the new cath labs at UHL were Ian Carter, Integrated Healthcare Area Manager, Acute and Older Persons Services, HSE Mid West; Edel Wyse, Munster Heart Foundation; Dr Cormac O’Connor, Consultant Cardiologist; Liam Keehan and Barry Long, both Munster Heart Foundation.
The new catheterisation laboratories (cath labs) at University Hospital Limerick (UHL) are driving significant improvements to cardiology services in the region, creating increased capacity and access to procedures never before available in the Mid West.
The €2m capital costs were partly met by the HSE, with a €1.65m contribution raised by the Munster Heart Foundation through supporter donations and a successful grant application to the JP McManus Pro-Am.
The new cath labs have capacity for up to 20 additional cardiology sessions per week, with technology that allows for higher imaging quality, management of more complex cases, and greater safety for cardiologists who are exposed to higher radiation doses than any other healthcare worker.
Menopause and Me webinar HSE Mid West
Launch of HSE National Clinical Guidelines
The National Cancer Control Programme (NCCP) launched three recently published HSE National Clinical Guidelines:
• Diagnosis and staging of patients with breast cancer
• Active surveillance for patients with prostate cancer
• Neoadjuvant treatment of patients with locally advanced rectal cancer
These guidelines integrate the best current evidence with clinical expertise and patient values. They aim to reduce variation in practice regarding access, quality and cost with the overarching goal of improving patient outcomes. The guidelines were developed for all healthcare professionals involved in cancer care, ensuring a multidisciplinary approach. They are patient-centred, incorporating patient values and experiences into clinical decisionmaking. Full guidelines are available on the HSE National Central Repository.

Health and Wellbeing and the Complex Menopause Clinic in Nenagh Hospital ran a hugely successful online menopause webinar in February, with 1,258 people logging in and more than 2,800 registrations for the online event. “The many ways to manage your menopause” webinar included an expert panel of speakers as well as women from across the Mid West who courageously shared their personal experiences of menopause. There has been an overwhelmingly positive reception for the insights aired during the webinar. One person hailed the “comprehensive and compassionate” approach, and another said the session would empower her to “approach my GP more confidently”.
Super Nursing and Midwifery Grand Rounds
In December 2024, the Nursing and Midwifery Planning and Development Unit (NMPDU) Midlands hosted a well-attended Super Nursing and Midwifery Grand Round event in the Mullingar Park Hotel. This one-day event celebrated the success of the introduction of Grand Rounds in the Midlands and supported the integration of nurses and midwives from all services and provided them with a regional platform to share their grand round story. Since March 2023, the
NMPDU have supported the introduction and development of the Nursing and Midwifery Grand Rounds (NMGR) in the Midlands. NMGR have embedded a culture of learning, sharing of knowledge, whilst raising the profile of the many and varied experts within the nursing and midwifery profession, while providing an opportunity for staff networking and collaboration. This event showcased innovation, collaboration and the commitment to improving patient care.
Launch of the NMPDU Midlands Nursing and Midwifery Innovation Projects at a Glance booklet
A key function of the Office of the Nursing and Midwifery Services Director (ONMSD) / NMPDU is to strategically lead and support nurses and midwives to deliver safe, high-quality, person-centred care. On behalf of the ONMSD, the NMPDUs manage and process a designated budget for nursing and midwifery service improvement initiatives. The NMPDUs provide support, advice and expertise to enable services to engage in innovative activities that bring about service improvement in nursing and midwifery practice.
This booklet highlights some of the service improvement initiatives that nurses and midwives have led in the past few years in the Midlands. A number of the initiatives have been award-winners in innovation at a national level.
Link to booklet: bit.ly/NMPDUMidlands
For more information, email nmpdu.midlands@hse.ie or follow @NMPDMidlands on X.

Nursing and Midwifery Planning and Development Unit Midlands team, from left: Dr Mary Nolan, Interim Director; Gráinne Keena, NMPD Officer; Sheila Browne, Senior Executive Officer; Jeremiah Nally, NMPD Officer; Jennifer O’Shaughnessy, Assistant Staff Officer; Finola Gill, NMPD Officer; and Emer McTiernan, NMPD Officer.

Ann Marie Burke, Practice Development Co-ordinator; Karen Moran, Clinical Facilitator; Mary McKeon, Community Dietitian; and Carola Diettrich, Community Dietitian, Older Persons Residential Services Longford/ Westmeath with the award-winning Think Drink Hydration Project funded by NMPDU Midlands.
Celebrating International Day of the Midwife and International Nurses Day
An event on 24 April was jointly organised by the HSE Office of Nursing and Midwifery Services Director (ONMSD), the office of the Chief Nursing Officer (CNO) at the Department of Health and the Nursing and Midwifery Board of Ireland (NMBI) to celebrate and prepare for International Day of the Midwife on 5 May and International Nurses Day on 12 May 2025. This event was hosted in the NMBI Offices by NMBI Vice President Áine Lynch. The audience of frontline nursing and midwifery staff from across all disciplines listened to stories from Mattie Lambden, Clinical ID Nurse Manager 2; Emer Shine, Clinical Midwife Manager 2; Elena Prendergast, NMBI Student Nurse Ambassador; Colette O’Neill, Clinical Skills Facilitator;
Sean Dowling, Clinical Midwife Manager 1; Vandana Iqbal, Care of the Older Persons, Director of Nursing; and Jess Sears, Candidate Advanced Nurse Practitioner. The patient perspective was shared by Dr Geralyn Hynes and Ashley Murphy.
Storytelling from guest speakers and audience participation encapsulated the key values of nursing and midwifery, which was captured on film for sharing with colleagues and service users on both days.
Closing remarks were delivered by Rachel Kenna, Chief Nursing Officer, Department of Health; Carolyn Donohoe, Interim CEO, NMBI; and Dr Geraldine Shaw, Nursing and Midwifery Services Director, ONMSD and Interim Adviser to HSE CEO.
Data protection is everyone’s responsibility
D ouble-check contact details before you post
A lways use clear windowed envelopes


Take a moment to check the address
A lways protect patient privacy



















How to avoid postal errors:
• Regularly update the patient’s postal address to ensure letters go to the correct address
• Take the time to ensure the correct patient documents are attached to the right cover letter
• Use windowed envelopes (ensure no sensitive information can be seen through the window)
• Always check details carefully before posting to avoid common mistakes
HSE National DPO Office



Maternity hospital appointments
Urgent and emergency care services finder



Digital EHIC and medical cards
Medicine and vaccination records





