


















































MATTERS SPRING 2024 HSE Dublin and Midlands HSE Dublin and North East HSE Mid West HSE South West HSE Dublin and South East HSE West and North West ONE HEALTH SERVICE HSE Health Regions in place from 1 March 2024
Welcome to the latest edition of Health Matters.
We are already a quarter way through 2024 and a lot has already happened as we move towards the implementation of the health regions. Hopefully staff will be able to see how the new structure is coming together and the positive impact it will have on how we do our work.
In this edition, we give you a chance to look at the geographical structure of each one of the six health regions and introduce you to the new Regional Executive Officers who will oversee the individual regions.
At the heart of all the change is the opportunity to deliver integrated care between acute services and the community to our service users.
Also in this edition we speak to experts in the field of child psychology who help explain the best ways parents can speak to their teenagers about drugs and alcohol, and guiding them to make healthy decisions.
In our Meet the Team section, we get a chance to look at the work of the innovative Crisis Resolution Team based in Sligo which has been put together to help people suffering with a mental health crisis avoid hospital admissions and treating them in their own home. It is an initiative that has the potential to transform care for many people and has already seen fantastic results.
Again, we keep an eye on climate action across the HSE and see what green programmes are being put in place as part of the HSE Climate Action Plan.
A sincere thanks to all those who have sent in contributions to this edition.
Joanne Weston Editor
1 Lifesaving brother to the rescue at wedding 2 Centre for young people with eating disorders 4 Talking Point: Fertility Services in the HSE 6 Spotlight on Cervical cancer 7 Domestic violence support 8 How to talk to your teenager about drugs 10 A Day in the Life: Dr Jane Cunningham 11 Tell our story - amplify the ordinary as well as the extraordinary 12 HSE radio stars promote dementia friendly communities 14 What is: Newborn Hearing Screening 16 Meet the Team: Crisis Resolution Team 18 Hot Topic: The Irish language and our obligations 20 Return to Nursing - a personal testimonial 21 Care and support for children with NAS service 22 Learning to Talk video series produced 23 John's Campaign to empower family carers while patient is in hospital 24 Hot Topic: Overdose awareness 25 Spotlight on Postnatal Care 26 Spotlight on AI in healthcare 28 Hot Topic: National Consent Policy 29 Spotlight on Diversity 30 Peer support for HPV vaccine in prison 31 Autism Reality Bus heads to the north east 32 Talking Point: Climate Action 36 News part 1 38 Spotlight on Patient Safety 40 HSE Health Regions 44 Integrated care in action across the health service 48 Health Service Excellence Awards - a closer look at the award-winning projects 52 Making Every Contact Countthe important role of the local champion 53 Lactation specialist appointed in Mayo 54 Defining, designing and delivering frontline improvements with Change Framework 56 Antenatal educators programme up and running 57 Updated Emergency Multilingual Aid now available 57 New RANP in Emergency Nursing for Injury Unit 58 A first for Saolta nursing graduates 59 Innovative programme to help patients prepare for surgery 60 Directory of Services for older people 61 Infection Prevention and Control Link Practitioner Programme delivered in South East 62 News part 2 64 Data protection - avoiding postal data breaches 64 At-home testing for Hepatitis C 65 Early Intervention in Psychosis 65 Role of health care assistants to be highlighted 66 Review to Inform the Strategic Direction of Laboratory Medicine 69 New contact details for Your Service Your Say 68 Telehealth Roadmap will provide the building blocks for future 71 Antiobiotic prescribing website becomes new go-to for GPs 72 Awards and accolades 74 Events 78 Health and wellbeing HSE Head of Internal Communications: Emma Finn Internal Communications Team: Yvonne Costello, Ann McLoone, Amy O'Neill, Frances Plunkett, Shane Larkin, Paddy Crosse, Emily Torsney Ashville Media Group Editor: Joanne Weston Art Director: Áine Duffy Creative Director:Jane Matthews Published by Ashville Media, Unit 55 Park West Road, Park West Industrial Estate, Dublin 12, D12 X9F9. Tel: (01) 432 2200 ISSN: 0332-4400 All rights reserved. Every care has been taken to ensure that the information contained in this magazine is accurate. The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher is prohibited. © Ashville Media Group 2023. Meet the team
Contents Ed's Letter
My brother, the hero
Big brother paramedic Kieran saves his sister Eithne’s life

With 70% of cardiac arrests happening in the home, chances are it will be a loved one or someone you know who you will need to perform CPR on.
Little did paramedic Kieran Minihan from Cork know that at a family wedding in Youghal he would find himself, along with colleagues from the National Ambulance Service (NAS) and the local fire brigade, resuscitating his own sister Eithne in her hotel room.
The drama began in a hotel in Youghal in August when Eithne developed severe pain in her teeth at a family event. She became very unwell and went up to her room. Kieran, who works as a paramedic with the NAS in Cork, was also at the wedding.
Kieran tended to her and, owing to his 16 years of experience, recognised that she was very unwell and called for an ambulance. The ambulance

"The ambulance crew were on scene for 7 minutes and during that time Eithne went into cardiac arrest so Kieran and two other paramedics immediately began resuscitation."
arrived and they did an ECG on Eithne and discovered that she was having a heart attack. The ambulance crew were on scene for 7 minutes and during that time Eithne went into cardiac arrest so Kieran and two other paramedics immediately began resuscitation. They provided CPR and delivered three shocks from the ambulance defibrillator which converted Eithne’s heart back into a perfusing rhythm, her heart began beating again and she was breathing on her own.
The local fire service in Youghal was also called. The fire station is 600 meters from the hotel. A NAS advanced life support unit was dispatched as well. Youghal is a 35-minute drive from Cork City.
Eithne came out of hospital a week later and is recovering well from her ordeal. She has already been back to Youghal to meet the fire crew who helped her and NAS are inviting her to meet the ambulance crew who looked after her.
She said she will be forever grateful to her big brother Kieran, his paramedic colleagues, and the Youghal Fire Brigade. HM
If you are interested in joining a Community First Responder Group contact www.becomeacfr.ie for more information.
| 1 HEALTH MATTERS SPRING2024 Feature

HEALTH MATTERS SPRING 2024 2| Feature
New centre
recovery
eating disorders Further information on the NCPED can be accessed at https://www.hse.ie/eng/about/who/cspd/ncps/mental-health/eating-disorders/
'It's like a community'
for
for young people with
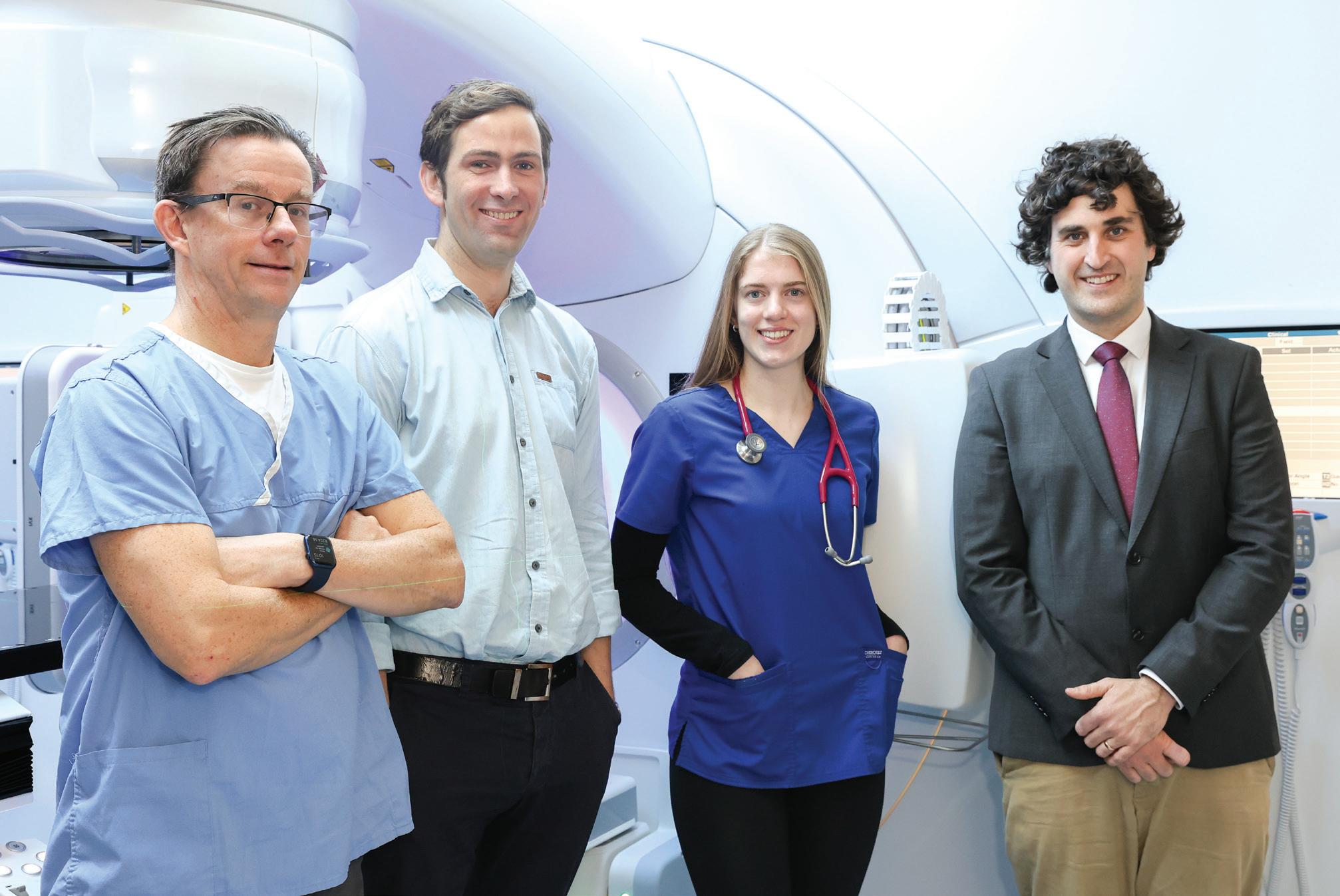
Dr Sandra Chong, NCHD; Dr Sara McDevitt, Consultant Child Psychiatrist; Sinead Buckley, Senior Occupational Therapist; Orla Fogarty, Senior Social Worker

Fastnet House in Cork is the new home of the Child and Adolescent Regional Eating Disorder Service for Cork and Kerry (CAREDS), providing specialist outpatient eating disorder care for people under 18 years.
CAREDS is part of the HSE National Clinical programme for Eating Disorders (NCPED) and works closely with mental health, hospital services and general practitioners across the region.
The new facility aims to improve the care experience for young people who attend. As one service user said, “It feels like a very open atmosphere in there and like a community.”
Spaces for consultations and group therapy contribute to a welcoming environment, where individuals have space to engage in the recovery process. The facility is accessible, close to public transport with onsite parking.
However, the benefits of this new centre extend beyond infrastructure, enabling improvements in CAREDS clinical programmes.
Dr Sandra Chong, NCHD, Dr Jay Venketramen, Consultant Paediatrician, Steve Maricle, Senior Social Worker and Family Therapist


The patient journey begins in a dedicated waiting area with reading materials, team information and therapeutic and research opportunities. A young person’s creative project provided art material for the centre.
The Family Room is where young people can relax while engaging in therapies. Sensory boxes have been developed for clinical spaces to support those with sensory regulation needs. Steve Maricle, Senior Social Worker, said, “It’s great to be able to work with young people to develop the
Marie Corbett, CNS, Steve Maricle Senior Social Worker and Family Therapist, Claire Bywater, Senior Speech and Language Therapist, Dr Jay Venketramen, Consultant Paediatrician, Jacqueline Hughes, CAREDS Administrator


"Families really appreciate the chance to have family meals in a bright, homely space designed to help them recover"
environment that supports them, through their artwork and sensory boxes.”
The clinical kitchen enables CAREDS to develop the family meal and meal support programme. Elaine Costello, Senior Clinical Psychologist, said, “Families really appreciate the chance to have family meals in a bright, homely space designed to help them recover.”
The observation and integrated multidisciplinary spaces facilitate the team to collaborate and deliver care plans effectively together. The facility also has controlled access to clinical spaces, serving a dual purpose of patient privacy, while maintaining the optimal safety.
As an integrated team, CAREDS Cork Kerry includes a consultant child psychiatrist and consultant paediatrician. A key innovation in the new centre is the inclusion of a dedicated medical assessment room, with the essential equipment needed to conduct comprehensive physical assessments.
“We hope that this will support our acute hospital colleagues in reducing hospital attendance when medically safe to do so,” said Dr McDevitt, Consultant Child Psychiatrist at CAREDS. HM
| 3 HEALTH MATTERS SPRING 2024 Feature









































Talking point
HSE Fertility Treatment Services
Busy first six months for publicly funded fertility treatment services
In September 2023, the HSE implemented a structured referral pathway for advanced fertility treatment, inclusive of IVF.
This pathway of care is available to public patients who attend one of six HSE Regional Fertility Hubs and are clinically identified as requiring such advanced treatment, and meet the national access criteria for such treatment.
This treatment is accessed by means of a referral
from one of the hubs, to a private clinic who has been authorised by the HSE to treat public patients.
Since the introduction of this structured referral pathway for advanced treatment, over 1,500 couples have been referred by their GPs to one of the HSE’s Regional Fertility Hubs in place, with over 400 couples referred onward for Advanced Human Reproduction treatment at approved private providers.
There are six Regional Fertility Hubs based in public

HEALTH MATTERS SPRING 2024 4 |




maternity hospital networks across the country. These hubs are located in the the Rotunda Hospital, the National Maternity Hospital, the Coombe Hospital, Galway University Hospital, Nenagh General Hospital and Cork University Maternity Hospital.
The fertility teams at the hubs offer a range of fertility tests, investigations, treatments and advice.


These include relevant blood tests, specialised ultrasound scans and x-rays, semen analysis, fertility-related surgery and medical management and treatment including ovulation induction.
WHAT TO EXPECT AT A REGIONAL FERTILITY HUB
You may be referred to a regional fertility hub by a GP or a consultant if you are having problems getting pregnant.
Before your first appointment
We'll send you an information pack after you get a referral. The pack will include a questionnaire. There will be a separate one for your partner, if you're in a couple. You need to complete and return these questionnaires to us.
After we get these, we will:


Many people who attend a Regional Fertility Hub will get the fertility treatment they need in the Hub, without needing to advance to IVF or IUI treatment.
For some couples, AHR (Advanced Human Reproduction) treatment may be recommended based on the results of investigations and management undertaken by the specialist fertility team in the hub.
• arrange specialist tests for you and your partner, if you are part of a couple
• make an appointment for you to meet a consultant together
At your appointment
A consultant will meet you and your partner. They will talk to you and go through your:
• medical history
• fertility problems

AHR treatment includes IUI, IVF and ICSI.
IUI (Intrauterine Insemination) is also called artificial insemination. It is when a sample of a man’s sperm is injected into the woman’s uterus (womb) around the time of ovulation.


IUI is far less invasive and complicated than IVF and works well for couples with unexplained infertility. It is usually the first treatment recommended in that situation.

• any test results they have
They will talk to you about next steps and any treatment you may need.
After you meet your consultant
The next steps may be:
• more tests
• treatment
• going to another specialist
You may meet your consultant again to go through test results and your treatment options.
IVF (In Vitro Fertilisation) is where a woman’s eggs and a man’s sperm are placed together in the laboratory where they will hopefully fertilise and form embryos.

One embryo is then placed into the woman’s womb where, hopefully, it will implant and lead to a healthy pregnancy.
ICSI (Intracytoplasmic Sperm Injection) is a more specialised form of IVF used for certain sperm and embryo problems, and involves the injection of sperm directly into an egg.
Having a fertility problem can be an extremely lonely and stressful time for those wishing to conceive. It is the aim of all the staff working in the HSE Fertility Services to provide patients with support, guidance and information on your fertility journey.
To this end, healthcare staff from the Regional Fertility Hubs attended the inaugural Future Fertility Show in the RDS in early March to speak with and provide information to couples starting their fertility journey, and how to access publicly funded fertility treatment.
For anyone concerned about their fertility, their port of call is a GP who can refer to the local Regional Fertility Hub. HM
Visit HSE.ie/fertility for more information
Tests you may have
You may have specialist tests at a Regional Fertiilty Hub. These include:
• AMH blood tests - to check how many eggs you may have in your ovaries
• pelvic ultrasound - to check for cysts, fibroids or severe endometriosis
• sperm tests - to check the quality and number of sperm
• blood tests - to check for other hormones
• HyCoSy scans or HSG x-rays - to check your womb and fallopian tubes
• hysteroscopy - to check the inside of your womb
Treatment you may need
The treatment you need depends on what's affecting your fertility.
The treatment you may be offered at a regional fertility hub includes:
• advice about things you or your partner can do to help your chance of getting pregnant
• tablets or injections for women who are not ovulating (producing an egg every month)
• medicine to improve sperm production
• surgery for ovarian cysts, endometriosis, tubal disease or pelvic scarring
• surgery to unblock or repair the tubes that transport sperm
• specialist fertility treatment like IVF
| 5 HEALTH MATTERS SPRING 2024
Talking point
Spotlight Spotlight on Cervical Cancer
Ireland on track to eliminate cervical cancer by 2040

Ireland can eliminate cervical cancer within our lifetime: this was the message from Minister for Health Stephen Donnelly (pictured inset) who announced 2040 as the year Ireland can eliminate cervical cancer, on Cervical Cancer Elimination Day of Action.
The projected target date of 2040 is the result of a detailed modelling project with Australia’s Daffodil Centre using Ireland’s HPV vaccination rates, screening coverage and population data.
consultation in 2024.
“Today is an extraordinary day. No baby girl born today in Ireland will have to worry about cervical cancer. Thank you to all involved in the delivery of screening, vaccination and treatment services, to our passionate patient advocates and to all the partnership stakeholders,” said Minister Donnelly

The Cervical Cancer Elimination Partnership is developing an action plan to ensure Ireland remains on track to eliminate cervical cancer by 2040. This starts with a national public
The HSE’s Cervical Cancer Elimination Strategic Advisory Group comprises the Department of Health, the HSE’s National Screening Service, the National Immunisation Office, the National Cancer Control Programme, the National Women and Infants Health Programme, the National Cancer Registry of Ireland, patient advocates, the
Marie Keating Foundation and the Irish Cancer Society. The event was attended by members from across the Cervical Cancer Elimination Partnership.
Head of the Strategic Advisory Group Dr Caroline Mason Mohan added, “In doing all of this work, we also need to make sure that no-one gets left behind. We know that often, those with the greatest need are the people who are under-served by our services. A key part of our drive to elimination will be to address any inequities through partnership working.” Bernie Brennan, mother of the late Laura Brennan, who campaigned to raise awareness and uptake of the HPV vaccination, highlighted the importance of everyone having access to the HPV vaccine. “The HPV vaccine saves lives,” she said. HM
HEALTH MATTERS SPRING 2024 6 |
Members of the Cervical Cancer Elimination Partnership at the Department of Health on Cervical Cancer Elimination Day of Action, when Ireland's target date to eliminate cervical cancer was announced.
Domestic violence support












The HSE’s new Domestic Violence Policy encourages discussion around domestic violence and provides information about workplace supports, including domestic violence leave.
The policy applies to employees in the HSE and Section 38 organisations. This includes full-time, part-time, permanent and temporary employees.
National HR Employee Helpdesk
Phone: 1800 444 925
Email: ask.hr@hse.ie
The helpdesk is open 8am to 5pm, Monday to Friday








Domestic violence leave
• All employees have the right to take paid leave for domestic violence
• There is no minimum service required to qualify for domestic violence leave
• If you are experiencing domestic violence or supporting a 'relevant person' you may take this leave




Domestic violence leave enables you to get:
• medical attention
• services provided by a victim service organisation
• psychological or other professional counselling
• temporarily or permanently relocated
• an order under the Domestic Violence Act 2018
• advice or assistance from a legal practitioner
• assistance from an Garda Síochána
Role of HR
If you would prefer to disclose domestic violence to someone outside of your work area you can contact HR.
HR will direct you to specialised support services. They will not attempt to resolve the problem or act as a counsellor.
Notice to request leave
While notice to take leave is preferable, you do not have to notify your manager in advance of your intention to take domestic violence leave. This is because domestic violence situations may arise urgently. When you take domestic violence leave, you should notify your manager as soon as you can.
Number of days leave
• You are entitled to take up to 5 days' paid leave in any 12-month period.
• Taking domestic violence leave for part of a work day counts as one day of leave.
• You may request other types of leave (paid or unpaid) if you have used up your domestic violence leave entitlement. This may include annual leave, unpaid leave, and parental leave (if applicable).
| 7 HEALTH MATTERS SPRING 2024 In Focus
How to talk to your teenager
Professor Bobby Smyth, Consultant Child and Adolescent Psychiatrist; Emer Loughrey, Psychotherapist; and Monica Whyte, Systemic Family Psychotherapist, who are part of the HSE Youth Drug and Alcohol Service in Tallaght (YoDA), give their expert advice
The Youth Drug and Alcohol Service team explains that while there are many influences on adolescents regarding alcohol and drugs, parents are the most important single influence to guiding and supporting their children towards healthy choices.
Sometimes as parents, we look at our teenagers and ask why they make such impulsive decisions.
“It’s really important for parents to know that remarkable changes are happening to the teenage brain during adolescence. The most significant period of change and development happens from about the age of 11 until the brain reaches 'maturity' in the mid-twenties,” explained Prof Smyth.
“The last part of the brain to develop is the frontal cortex, and this part of the brain is a bit like the brain’s braking system. So, this means that teenagers are at a disadvantage at appraising risk. Part of our job as parents is to be that braking system on their behalf. The best way to support that ‘braking system’ is to have a presence in their lives and work on the relationship.”
According to the team, the developing brain is particularly sensitive to the effects of alcohol and drugs. There is concern that substances like alcohol and cannabis

HEALTH MATTERS SPRING 2024 8 | Interview
For more information and resources go to www.drugs.ie/parents
can interfere with the developmental process of the teenage brain. Long-term follow-up studies show that extensive use of these substances by young people aged 14 to 16 years can result in adverse impacts, including some alterations to brain structure and a small decline in IQ. “The worry is that the developing brain is particularly sensitive to the effects of alcohol and drugs," noted Prof Smyth.
Parents often wonder if it’s a good idea to let their teenager drink at home in the hope that they learn to drink in a low-risk manner. According to Prof Smyth the evidence shows that this approach is actually counterproductive.
“The research is pretty clear that allowing our children to drink alcohol at home in their mid-teens is actually ineffective. Young people who are allowed to drink at home tend to drink the most, and take even greater risks when they are out and about with their friends.”
Another risk of substance use in young people is that it can take over the reward circuit in the brain. The team recommends that teenagers learn how to relax and have fun with their friends without relying on substances like alcohol.
Monica Whyte, Systemic Family Psychotherapist, explained, “If your son or daughter links fun with alcohol, we run the risk that without it, things may seem boring to them. This is where we see many examples of teenagers dropping out of their activities or sports in favour of hanging out with friends who are substance-using.”
A challenge for parents can be figuring out if their child is experimenting with drugs and alcohol or if they have a more



serious problem. Counsellor Emer Loughrey said it’s a real dilemma and one that many families do face.
“It’s about figuring out if your child is trying out drugs in an experimental way through curiosity or if their relationship with substances has become more patterned and problematic. To help us figure this out, we need to be reflecting on things like how is school going? What’s happening with the friends? How have they been at home? What changes do you notice?” Emer said talking to your young person is always a good first step.
“The first piece of advice is to have the conversation with your child. But timing is everything; if your young person arrives home heavily under the influence—eyes glazed over and stumbling—this is not the time to have a chat. The time to have the chat might be the following day. We have a little saying, ‘striking when the iron is cold’. As a parent, you have to regulate your own emotions because if you overreact, then the conversation will shut down. They need to know you are there to help them through this stage, to support them to figure out how to do things safely the next
time and learn to navigate the risk differently.”
Signs of a problem may also include a decline in motivation, a poor mood, increased aggression in the house, unusual withdrawal from the family and dropping out of activities that they once enjoyed.
Emer’s advice to parents is “trust your instincts; more often than not, when parents approach us, they are correct that something is amiss.”
The team advised that according to feedback from young people, the most helpful approach is when their parents listen, show empathy and provide clear boundaries around acceptable and unacceptable behaviour.
“It is okay to make it very clear what behaviours you consider acceptable and unacceptable. Keeping track of where they are, who they are with and how they are all form part of our role too.
We incrementally give our children more freedom as they gradually move towards adulthood. Where they make wise choices with that freedom, we then give them more. If a pattern of poor choices is emerging, then freedoms may need to be reined in,” said Prof Smyth. HM
| 9 HEALTH MATTERS SPRING 2024 Interview
Emer Loughrey and Monica Whyte
A day in the life


A inDay the Life...




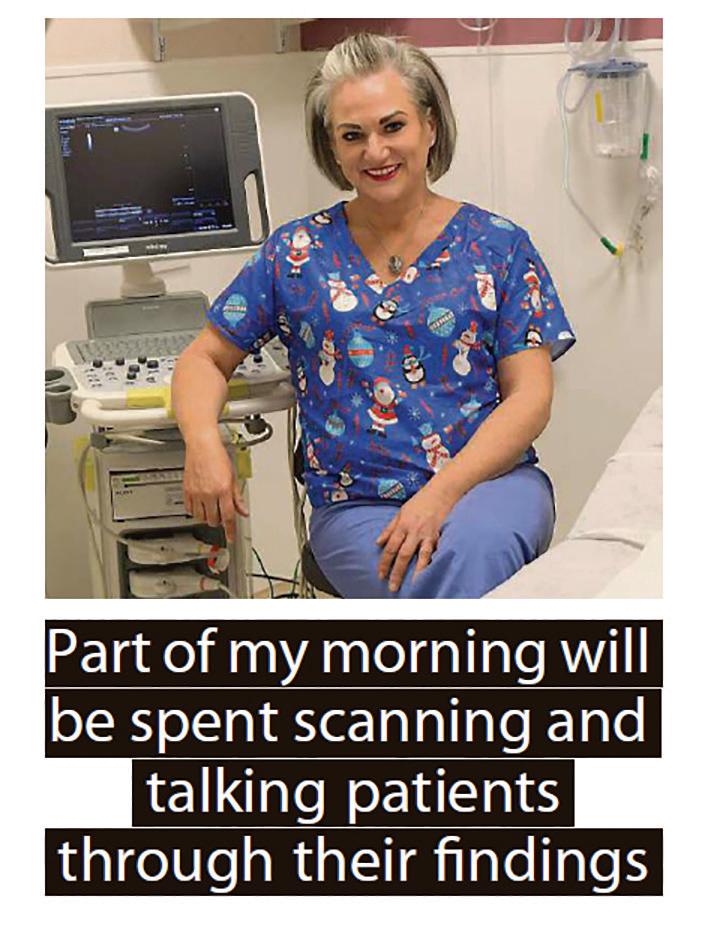
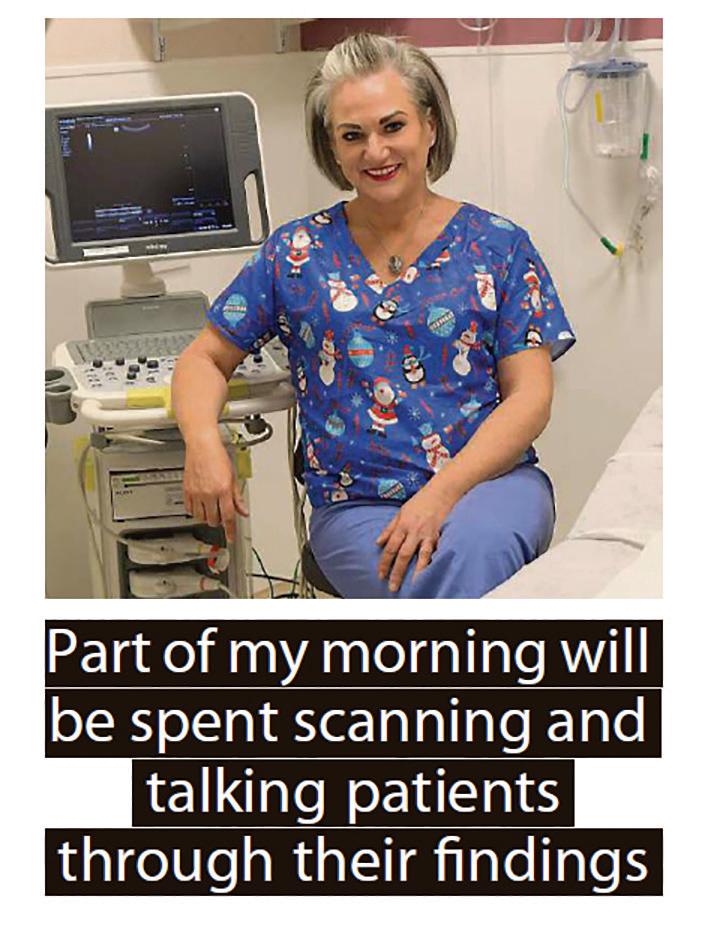
Dr Jane Cunningham
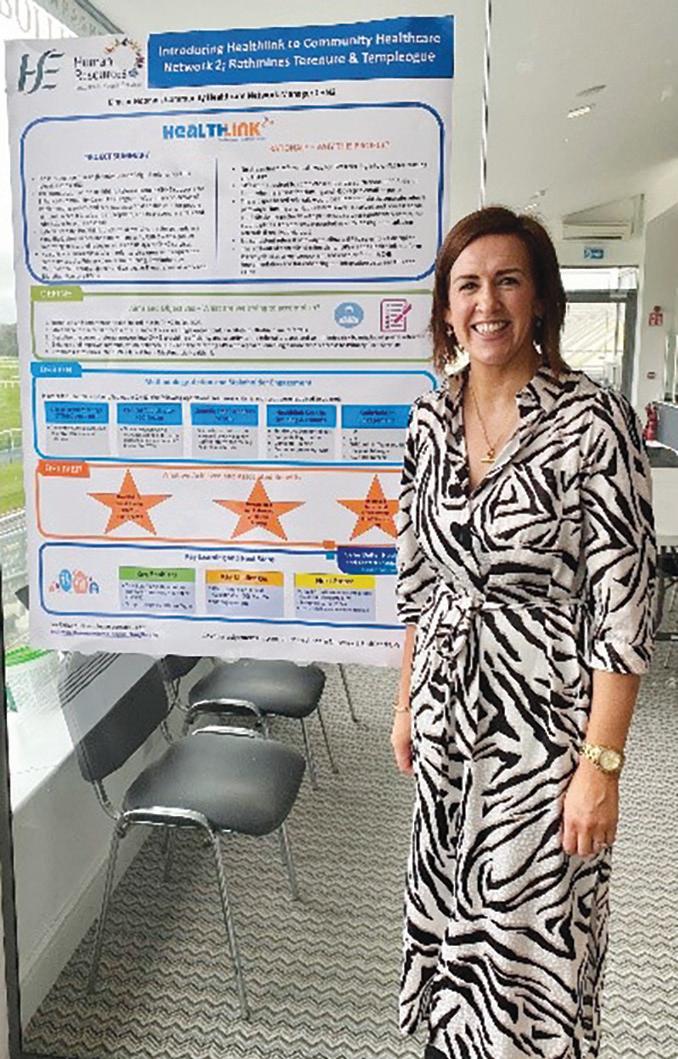
Consultant radiologist, BreastCheck Southern Unit, Cork
7am: Alarm goes off. I enjoy the brief time at home and my bowl of porridge before hitting the road.
8am: I arrive at BreastCheck Southern Unit to a warm welcome from colleagues at reception who are in early to greet women coming for either routine mammograms or for further assessment if something has been spotted on their mammogram.
I work in the assessment clinic and before it begins, we review each woman’s imaging as a team and plan how best to investigate what has shown up on their mammogram.
9am: The assessment clinic kicks off. We do our best to put every woman at ease as we understand how anxious they may be. The most rewarding part of my

job is talking and listening to patients as I perform ultrasound examinations or biopsies using imaging guidance.
11am: Clinic continues throughout the morning. I’m part of a multidisciplinary team and we work together to look after every woman thoroughly, compassionately, and efficiently.
1pm: As one of the consultant radiologists, I peer-review every patient’s case after clinic. This helps us prepare for our weekly meeting where we collaborate with pathology and surgical colleagues to discuss biopsy results and decide on personalised treatment plans.
2pm: After a quick lunch, I usually report routine screening mammograms. Two radiologists read each mammogram to
improve cancer detection. Five mobile breast screening units move around Munster, so women can go for breast screening in a location convenient for them.
3pm: Sometimes, I’ll report MRI studies which can help with pre-operative planning. I enjoy performing image-guided localisations to help with breastconserving surgery.
It’s great to see advances continually being made in breast cancer treatment and outcomes.
6pm: I try to squeeze in a jog after work. I wish there were more hours in the day for all the things I’d love to do, but I’ve learned in this job to be grateful for what I have – health and life are precious so what better way to spend my evenings than enjoying time with those I love. HM
HEALTH MATTERS SPRING 2024 10 |



Tell our health service story, amplify our ordinary





Important things are happening every day across our health service. Significant life-saving and lifeprotecting things, but also the less visible (but no less important!) things. The stories of the small gestures, actions, words, going the extra mile. The things that come together to form the overall health experience of each person who comes to us for our care and expertise should be told.
We must acknowledge that our work is not without challenges, but where there may be bad news, there is also so much good, made possible by the dedication and actions of you and your colleagues.
Whether it’s a home support worker facing the stormy elements on Christmas day to visit an older







client living alone, or a welcoming smile from a hospital porter to a young patient nervous before their first appointment, or a worker delivering naloxone training to a family to protect their loved one from a dangerous overdose, or a local smoking cessation officer checking in on their new client after the first tough week of quitting smoking or a mental health support worker providing non-judgemental support to someone during a time of crisis, one thing is clear: Our people are our health service. Our actions, big and small, every day, are our stories. Sharing these stories demonstrate how we make a difference, helping to build trust, credibility and confidence in what we do. HM
If you have a story to share, let’s work together. Amplify our ordinary as well as the extraordinary, contact press@hse.ie today to see how we can share your work with the media.
| 11 HEALTH MATTERS SPRING 2024 Your story HEALTH










































HSE radio stars














Staff highlight the importance of social connection for people with dementia


During January and February, Community Healthcare teams were helping to raise awareness for dementia and the various services and supports available locally and nationally.

As part of the national Dementia: Understand Together campaign, 14 radio stations across the country featured interviews with a range of experts, including people living dementia, people caring to support them, healthcare professionals and community champions. These are just a just a few highlights from the staff interviews that took place. HM














































to get everyone from every walk of life involved in helping people to live well with dementia. The key way this works is by building awareness and understanding of dementia nationally but by also encouraging people, encouraging businesses and services to take action to support and include people with dementia in their communities and there’s lots of different steps that can be taken along the way.”
Mary Hickey, Dementia Advanced Nurse Practitioner, Kilkenny and Carlow








“The language is really important. The term suffering, it’s a poor word, a negative word. When a person is living with dementia, it doesn’t affect every factor of their life, but it affects some pieces of their life and their day to day activities. So, they have to live with it and find ways to work around it and for families and communities to help people work around it and live with it a little bit better.”
“The campaign is all about creating an awareness of dementia within Ireland and including people living with dementia and the idea is that we want















If you break it down, even going out to a GAA match, or going to church, or going to the shops, whatever interest the person has – if you’re a local champion or not – just support that person to get out of the house, to engage.


"You’re getting some exercise by walking to wherever you’re going to go, you’re going to meet people so you’re going to have a conversation, it’ll force you to form an opinion, so again you’re being challenged cognitively as well.
" You’re getting out and meeting people, so it’s also good for your mood and again, it hits all of those risk factors around dementia.
"By getting people out and about you’re actually doing a huge service to that person.”
Paul Maloney, Programme Manager, National Dementia Office, HSE
HEALTH MATTERS SPRING 2024 12 |




































































































“Our goal (with Dementia Friendly Tralee) was to ensure that the person with dementia continued to engage with the community. It sparked a great response at the time from a number of different agencies. The Chamber Alliance were very proactive about how they could support their colleagues and friends who had a diagnosis to continue to come into Tralee, to continue to engage in business, to continue to go for their coffee, and from that we developed an interagency working group. Our aim was to create an awareness and that it wasn’t the end of road if you got a diagnosis.”












GP, whether it’s your public health nurse or it could be a friend or a familiar member. Just to speak to somebody about it. The key for people to be able to engage in all services is getting a diagnosis earlier. Learning the compensatory strategies to be able to cope with the diagnosis and engage in the community.”
Catherine Murphy, Occupational Therapist, Memory Technology Resource Room, Tralee
Dolores McElligott, Team Leader, Community Support Worker, Cork Kerry Community Healthcare











“Research has shown to keep people as active as possible. If people enjoyed going for walks, defi nitely get out there, keep walking on the beach, there are some great local schemes. Let the person be as engaged and as independent as possible.”
“It’s not just the health service that’s going to solve participation in community, it’s the community that are at the basis and that’s where the key message of awareness comes in. That’s really the goal of dementia inclusive communities, while it is a medical condition, it does require a community to support that person. We want to ensure that people continue to engage and that’s really the critical component. It’s a collective responsibility.”









Emer
Finn,
Occupational Therapist, Memory Technology Resource Room Wexford
“The importance of not being afraid to get a diagnosis of dementia is key. For people to go early, if you notice any diff erence in your memory, we all forget where we put our keys, but if it’s aff ecting your everyday life to go and speak to somebody. Whether it’s your
Eibhlis Cahalane, Community Support Worker, Cork Kerry Community Healthcare
“Our community and specialist teams are delivering quality care to people with dementia across the country every day of the year. So it’s great to see some of their experiences and expertise highlighted through our local radio stations and we’re grateful to Mary, Emer, Dolores, Catherine, Eibhlis and Paul for giving their time to support the campaign and share these important messages.”
Sean O’Dowd, Clinical Lead, National Dementia Office
The campaign is always looking for staff and partner organisations to share their local dementia inclusive initiatives and we’re also encouraging services and staff, especially those working directly with people affected by dementia, to display the national inclusive community symbol. If you’d like find out more about how to get involved and to request a link to listen to the interviews in full, please email understandtogether@hse.ie. For resources, including free awareness training, and to sign up to become a community champion, visit www.understandtogether.ie
| 13 HEALTH MATTERS SPRING 2024 Feature
Marguerite Keating from the Irish Dementia Working Group was interviewed about her experience of living with dementia by Tipp FM.
What is...
What is...
Newborn screeninghearing

It is just over 10 years since the Newborn Hearing Screening Programme was rolled out nationwide. Newborn hearing screening helps check if a baby has permanent hearing loss in one or both ears.
Approximately 80 to 90 babies are diagnosed each year with a permanent childhood hearing loss through the programme, according to a recently published three-year report summarising activity between 2020 and 2022.
Newborn hearing screening, along with newborn bloodspot
screening, is delivered as part of the National Healthy Childhood Programme, the universal child health programme which also includes health and development checks, key health messages and support to parents and vaccinations. The key focus of both screening programmes is early identification and appropriate interventions to support babies and their parents.
Dr Abigail Collins, HSE National Clinical Lead Child Health Public Health, explained, “Spotting hearing problems early means we
“Parents are often surprised that a baby does not need to react to the noise – we can detect a physical response inside the baby’s ear on our device.”
HOW THE HEARING SCREENING IS DONE
The screening process is very simple, and doesn’t cause pain or discomfort to the baby.
The newborn hearing screening checks the baby's inner ear (the ‘cochlea’). When a healthy ear receives sound, the inner part produces an oto acoustic emission (“echo”). Recording this tells us that the hearing is satisfactory.
Screening can be repeated if there is not a clear response in one or both ears.
1. The screener will put a small soft-tipped earpiece in the baby’s outer ear.
2. They will play clicking sounds into the baby’s ear.
3. The screening equipment checks the baby’s inner ear to see if it is echoing the clicking sounds.
4. The screener can repeat this if necessary.
Parents get the results at the time the screening is undertaken. If the results are not clear, the screener will do a second screen at another time.
HEALTH MATTERS SPRING 2024 14 |
IN NUMBERS
• Approximately 1 to 2 babies in every 1,000 are born with a hearing loss in one or both ears.
• About 5,000 babies are screened every month.
• Most babies have their hearing screening completed before they leave hospital. The aim is to have all babies screened before they are four weeks old.


can treat babies more effectively. Those who require a referral to audiology services will be seen to quickly for diagnostic testing. If a baby is identified as having a hearing loss, they are set on the correct pathway for hearing aids, cochlear implants or referral to speech and language services. The success of newborn hearing screening is testament to the work of the hearing screeners in the maternity hospitals, audiologists in the community services and particularly to Dr Gary Norman, our very committed National Clinical Lead.”
Newborn hearing screening is available to all eligible babies in Ireland and is undertaken soon after birth. Screening is primarily carried out while the mother and baby are still in the maternity hospital/unit as inpatients.
"It is a privilege to interact with mothers and babies in those first days of life"

NEC Software Solutions is contracted by the HSE to deliver the screening element of the programme. They aim to provide complete newborn hearing screening to all eligible babies by the time they are four weeks old.
Newborn hearing screening is undertaken by trained screening staff at each of the 19 maternity hospital/units using equipment specifically designed for use with newborn babies.
Myra Jordan is a Newborn Hearing Screener based in the Coombe Hospital, Dublin.
“Coming from a background in customer services, but always having had a desire to work in a hospital, this role has been a very satisfying one for me. It is a privilege to interact with mothers and babies in those first days of life,” she said.
She said parents sometimes ask if the process will be uncomfortable for their baby.
“The screening process is very simple and doesn’t cause pain or discomfort to the baby. We place a soft-tipped earpiece into the
baby’s ear and then produce a series of clicking sounds. Parents are often surprised that baby does not need to react to the noise –we can detect a physical response, called an oto-acoustic emission (“echo”), inside the baby’s ear canal on our sensitive device.”
Hearing screening identifies babies who require additional hearing testing. This enables a permanent or temporary hearing loss to be picked up at an early stage, helping to improve the long-term outcomes for children and their development and provide parents with support and information.
Dr Gary Norman, HSE National Clinical Lead for Audiology, said, “This really is a health success story. The programme has transformed the lives of many children born with deafness. The programme so far has identified 1,478 babies who have gone on to access early support and intervention services, including from HSE audiology, Chime, National Council for Special Education, medical investigations and cochlear implantation where appropriate.
“The combination of the HSE’s community audiology service with NEC screening means we have a highly effective and efficient national screening programme to ensure timely diagnosis and optimal management of early hearing loss in infants. The screening programme is vital for early diagnosis and intervention to ensure children with hearing loss can commence their school days with age-appropriate language and communication skills.” HM
For further information, see www2. hse.ie/conditions/newborn-hearingscreening/ or search ‘HSE newborn hearing screening’ in your browser.
Hearing loss can arise later on. Parents concerned about their baby or child’s hearing can use the childhood hearing checklist available on hse.ie. Use the link below or search for ‘HSE if you are worried about your child's hearing’ in your browser to find the page.
https://www2.hse.ie/services/audiology/children-babies/worried-about-your-childs-hearing/
| 15 HEALTH MATTERS SPRING 2024
What is...
Dr Gary Norman Myra Jordan Dr Abigail Collins
Meet the team Crisis Resolution Team
Community-based mental health crisis team offering an alternative to hospital visits
A new initiative in the north west has been helping people dealing with a mental health crisis to avoid admission to the Emergency Department (ED) by treating them in their community.
The Crisis Resolution Team (CRT) in Sligo is a communitybased multi-disciplinary team who provide rapid and intensive support over a six-week period to those experiencing an acute mental health crisis as an alternative to in-patient hospital admissions.
The service philosophy is to provide integrated crisis resolution services to people referred with the right response at the right time for the right amount of time to enable and empower people on their recovery journey. Its person-centred and recovery-focused approach recently earned it the Sláintecare
award at the Health Service Excellence Awards.
The team treat people over the age of 18 years experiencing an acute mental health crisis.
They accept referrals from GPs, any member of the Community Mental Health Team, a member of the Liaison Psychiatry team in the CRT learning site location hospitals, authorised offi cers, as well as mental health inpatient units.
Dr Elizabeth Gethins, Consultant Psychiatrist, CRT, explained that the team came about from a desire to provide an alternative service to people presenting with a mental health crisis in the ED.
“It was born out of a frustration that there were people who could and should be seen and managed within the community setting. There was an escalation in local demand for services and a 250% increase in mental health
attendances at ED so there was a great need there,” she said.
“We launched a limited service on 5 December 2022, just to Sligo Town and opened on 9 January to take referrals from other teams,” she said, noting the significant support from management and the local steering group.
The team cover a large geographical area from their Sligo base – going as far as Enniscrone, Laghey, Carrigallen and Carrick-on-Shannon.
“We never turn anyone away because of where they lived. We will make sure we get out to them,” said Elizabeth.
“We have worked hand in hand with the Mental Health Change and Innovation Office, and we are very proud of the team and of the service that we have developed,” she said.
Liz Sheridan, CNM2, CRT, said, “We have been very clear from
HEALTH MATTERS SPRING 2024 16 |
the beginning of this project that this service is available to everybody who needs it in our catchment area, which is Sligo, Leitrim, South Donegal and West Cavan. This is a very rural community but we feel very strongly that no one should be denied a service because of where they live.”
Ray Slevin, Clinical Nurse Specialist, CRT, said it was great to work with people in their own homes and he felt very privileged to be able to do that.
“We are providing for a rural catchment area where it is traditionally difficult to access services. That in itself is very rewarding,” he said.
Enda Moylan, CNM3 and Crisis Resolution Team Lead, explained what the CRT was all about.
“When someone has experienced a mental health crisis, we can now offer an alternative to hospital admission or presentation to ED. We will see the person on the day of the referral, we will see them in their own home and we will work intensively with them and their loved ones. This can mean actually seeing them two to three times daily but these visits can be reduced as they progress with the Crisis Team,” he said.
Joan Epping, Clinical Nurse Specialist, said the team’s working hours are aimed at providing the most appropriate care for service users.
“We work 12-hour shifts and take on referrals Monday to Friday. There are two staff covering at weekends. At the start of the day, we all meet, have a look at our client board and try to manage the caseload. New referrals have first priority, then we assess current risk, the stage their crisis is in, how long they are in team, and that keeps us in track,” said Joan.
Roisin Kearns, Senior Occupational Therapist, CRT, explained that the team works across extended hours from





8am to 8pm seven days a week so that service users and their families are fully supported. The team has one phone contact number and one email address for ease of contact.
“There is lots of learning along the way. One is managing documentation and gathering data. We have develop a fileshare which can only be accessed by our team. It is paperless, contains a patient’s clinical notes and supports us to keep our files up to date despite the travel and out of office. We will eventually move to specialist software,” explained Roisin.
“We have also been developing relationships and pathways. We have met with GPs, mental health teams such as psychiatry of old age, addiction services, and local gardaí.”
Therese Tierney is Senior Social Worker in the team.
“We have a very experienced multidisciplinary team with a broad range of skills and expertise. This helps us to meet the treatment and care needs of service users,” she said
As of December 2023, the team had 224 referrals, 160 of which were accepted.
The reasons why some referrals would not proceed would be if the assessment process was
enough for the service users through sign-posting more appropriate services, nonengagement from the service user, and if the person needed admission to acute services. The impact of the team has been clearly evident in the time it has been in place, with a 20% reduction in admission to the Acute Mental Health Unit (AMHU) from ED by offering an alternative pathway. There have also been 26 service users who have been supported in an early discharge from the AMHU.
The Crisis Resolution Team has also helped reduce some of the acute demand on Community Mental Health Teams, with a reduction in numbers referred from ED to CMHT of 25%.
There has also been a reduction by 25% in GP referrals to the ED in just eight months.
Catherine McHugh, Team Administrator, said, “We can already see that our service is having a positive impact. It has taken some of the pressure off admission beds, our community mental health team and the Emergency Department.”
Dr Mohanad Eltieb, Psychiatry Registrar, CRT, added, “The most gratifying part of our work comes from the feedback of the service users and their families.” HM
| 17 HEALTH MATTERS SPRING 2024
Meet the team
The Crisis Resolution Team receive their Health Service Excellence Award: Tomás Murphy, Liz Sheridan, Joan Epping, Dr Elizabeth Gethins, Jackie Nix, Ray Slevin, and Enda Moylan.
An Ghaeilge
Tá sé mar aidhm ag Acht na dTeangacha Oifigiúla (Leasú) 2021 cur le húsáid na Gaeilge i seirbhísí poiblí agus leagann sé dualgais nua ar FnaSS agus ar eagraíochtaí eile san earnáil phoiblí.
Tá eagraíochtaí na hearnála poiblí – lena n-áirítear FnaSS – ag cur creat nua dualgas agus seirbhísí teanga i bhfeidhm, dírithe ar a chinntiú gur féidir le cainteoirí Gaeilge teacht ar sheirbhísí sa dá theanga oifigiúil.. Ón 10 Deireadh Fómhair 2022, ba cheart go mbeadh ar a laghad 20% d’fhógraíocht na hearnála poiblí i nGaeilge, agus ar a laghad 5% den chaiteachas sa bhuiséad fógraíochta á chur sna meáin Ghaeilge.
DUL CHUN CINN FnaSS GO DTÍ SEO :
• Tá feachtais faisnéise poiblí FnaSS ar bhealaí teilifíse, raidió agus eile ar fáil anois i nGaeilge agus i mBéarla
• Tá post amháin as gach cúig phost meán sóisialta ó chuntais FnaSS i nGaeilge, agus tá leathanach Facebook Gaeilge tiomnaithe ag FnaSS
• Cruthaíodh Mol Foghlama Gaeilge laistigh den Chrios Fionnachtana ar HSELanD agus tá rochtain oscailte ag gach ball foirne air.
• Forbraíodh aistriúchán deimhnithe ar gach teideal poist agus cód gráid de chuid FnaSS, agus tá sé ar fáil ar HSELandD agus ar shuíomh Gréasáin FnaSS.
• Tá foirne earcaíochta FnaSS ag fógraíocht poist i nGaeilge agus i mBéarla
AN RAIBH A FHIOS AGAT?
• Ba chóir go mbeadh gach comhartha i seirbhísí FnaSS sa dá theanga, Gaeilge ar dtús
• Ba chóir go bhfreagrófaí i nGaeilge cumarsáidí ó úsáideoirí seirbhísí i nGaeilge
• Caithfidh aon chóras iarratais nó áirithinte ar líne de chuid FnaSS a bheith ar fáil sa dá theanga


Dualgais atá le teacht:
• Faoi dheireadh mhí na Nollag 2030, caithfidh ar a laghad 20% d’earcaigh nua san earnáil phoiblí a bheith inniúil sa Ghaeilge.



• go mbeidh córais ríomhaireachta uile FnaSS in ann ainmneacha, seoltaí agus an síneadh fada a úsáid i nGaeilge
• Caithfidh gach foirm iarratais FnaSS a bheith sa dá theanga
• Beidh amlínte do na dualgais seo ar fáil le linn 2024.

Tá ról le himirt ag gach ball foirne agus ag gach bainisteoir seirbhíse in FnaSS chun a chinntiú go dtacaímid lenár n-othair agus lenár n-úsáideoirí seirbhíse a labhraíonn Gaeilge, agus go gcomhlíonaimid ár ndualgais nua agus reatha. Tá tacaíocht ar fáil ar HSELandD. Le haghaidh tuilleadh eolais ar conas é seo a dhéanamh, tabhair cuairt le do thoil ar www.hse.ie/teanga
HEALTH MATTERS SPRING 2024 18 | Ábhar mór cainte
The Irish language




Ireland’s Official Languages (Amendment) Act 2021 aims to enhance the use of the Irish language in public services and gives new duties to the HSE and other public sector organisations.

Public sector organisations - including the HSE – are rolling out a new framework of language duties and services, aimed at ensuring Irish speakers can access services in both official languages.
Since October 10th 2022, at least 20% of public sector advertising should be in the Irish language, and at least 5% of the advertising budget spend should be placed within Irish language media.
HSE PROGRESS TO DATE:
• HSE public information campaigns on TV, radio and other channels are now available in both Irish and English
• One in five social media posts from HSE accounts are in Irish, and the HSE has a dedicated Irish language Facebook page

• An Irish Language Learning Hub has been created within the Discovery Zone on HSELanD and has open access to all staff.

• A certified translation of all HSE job titles and grade codes has been developed, and is available on HSELandD and the HSE website.
• HSE Recruitment teams are advertising posts in Irish and English
DID YOU KNOW?
• All signs in HSE services should be in both languages, Irish first
• Communications from service users in Irish should be answered in Irish
• Any HSE online application or booking system must be available in both languages
Upcoming duties:
• By the end of December 2030, at least 20% of new recruits to the public sector must be proficient in the Irish language
• All HSE application forms are to be in both languages
• All HSE computer systems are to be able to use Irish names, addresses and the síneadh fada
• Timelines for these duties will be available during 2024.
Every member of staff and every service manager in the HSE has a role to play in ensuring that we support our Irish speaking patients and service users, and meet our obligations both new and existing. Support is available on HSELandD. For more information on how to do this, please visit www.hse.ie/teanga.
| 19 HEALTH MATTERS SPRING 2024
Hot Topic
‘At the end of the eight weeks you have achieved so much’
Cathy McKenna reflects on her return to nursing after 10 years

I applied to the Return to Nursing Practice course a couple of years in a row before I found myself in a position to accept my place on the course. As a mother of three young boys and with a husband that travels often for work, I found the timing of the course to be quite tricky - it runs from the end of May through to the third week of July and it only runs annually. This required a huge amount of planning before and during the course. The fact that the course straddles term time and school holidays meant I had ever-changing childcare requirements. Therefore, I booked camps, paid for childminders (plural) and called in favours from friends and family. This was one of the many positive unexpected discoveries I made on this journey. Friends and family were so invested in helping me through this course, not only to see me succeed, but in recognition of the need to support nursing in general.
My advice for anyone applying for this course is to obtain as much information as you can about the course layout, expectations and timings as well as researching nursing roles and careers you might like to pursue after the course – so you can tailor your experience. Understand your pay grade for re-entry into a HSE role so there are no surprises when it comes to accepting job offers on completion of the course.
One of the biggest stressors my colleagues and I experienced was the realisation that during the course the time commitment was even greater than we had originally anticipated. In addition to the course work itself, it takes a lot of mental fortitude and bravery to reenter the workforce after an extended absence - in my case 10 years. You will be tired and emotional at times.
However, it is a relatively short course all things considered and although the pace can feel overwhelming at times, at the end of the eight weeks you have achieved so much.
Anyone who is familiar with the workings of a busy public ward in a teaching hospital can appreciate that an immediate immersion back into the pace isn’t easy. It will most certainly get you the exposure you need to leave the course feeling confident and competent and ultimately that is your sole purpose.
The feeling of achievement at the end of the course will be great and I was personally reminded how much I missed the diversity and challenge of nursing.
I have found employment locally with hours that fit my busy and responsible home life. There are many different and flexible opportunities out there and I wish anyone looking to take the brave step to re-enter the nursing profession the best of luck. HM
HEALTH MATTERS SPRING 2024 20 | Feature
Cathy McKenna, centre with lanyard around her neck, with the 2023 Return to Nursing Practice Regional Centre of Nursing and Midwifery Education (RCNME) Dublin North participants
Care and support for children
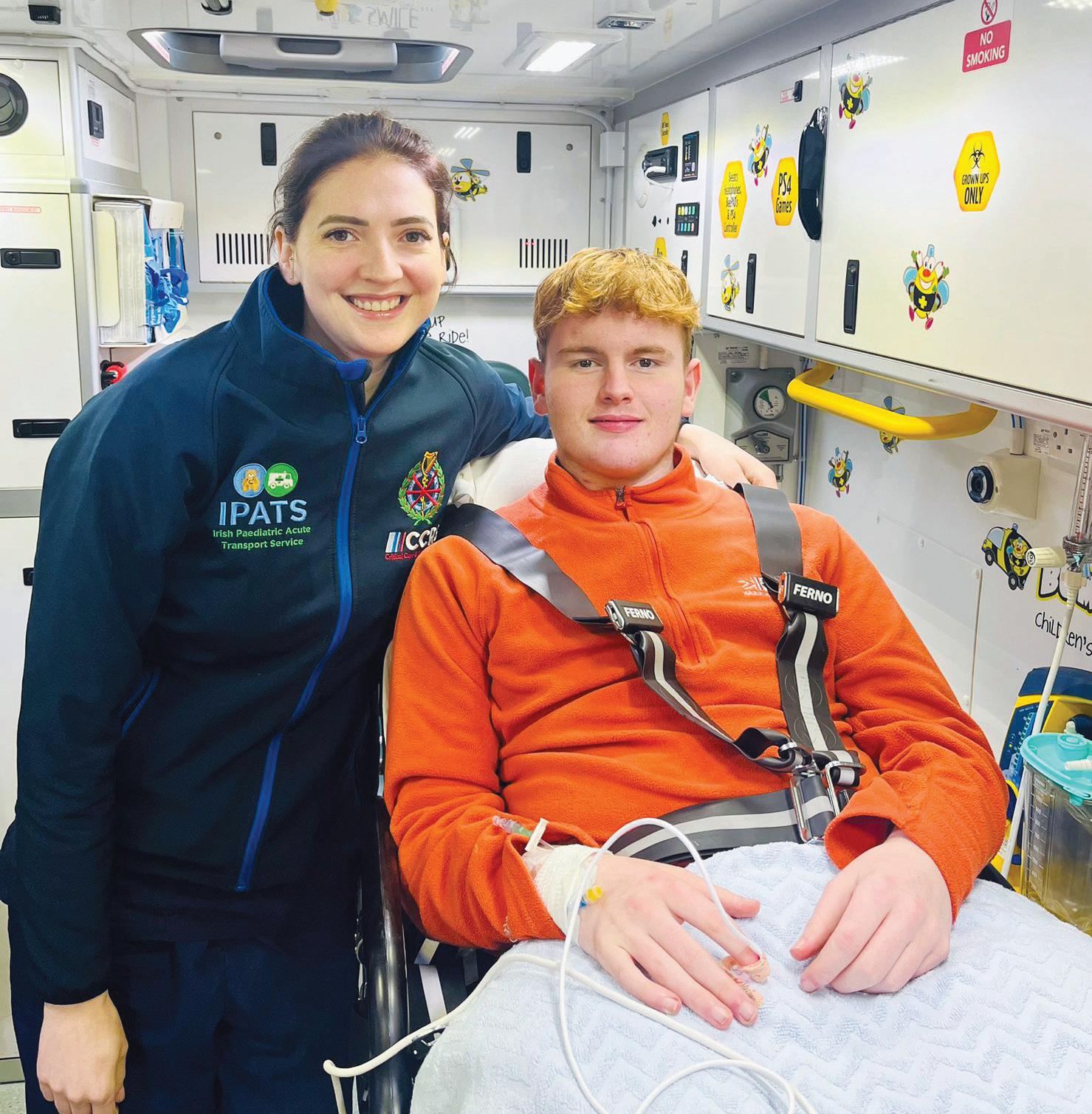
NAS launches nurse-led repatriation service for Children’s Health Ireland hospitals
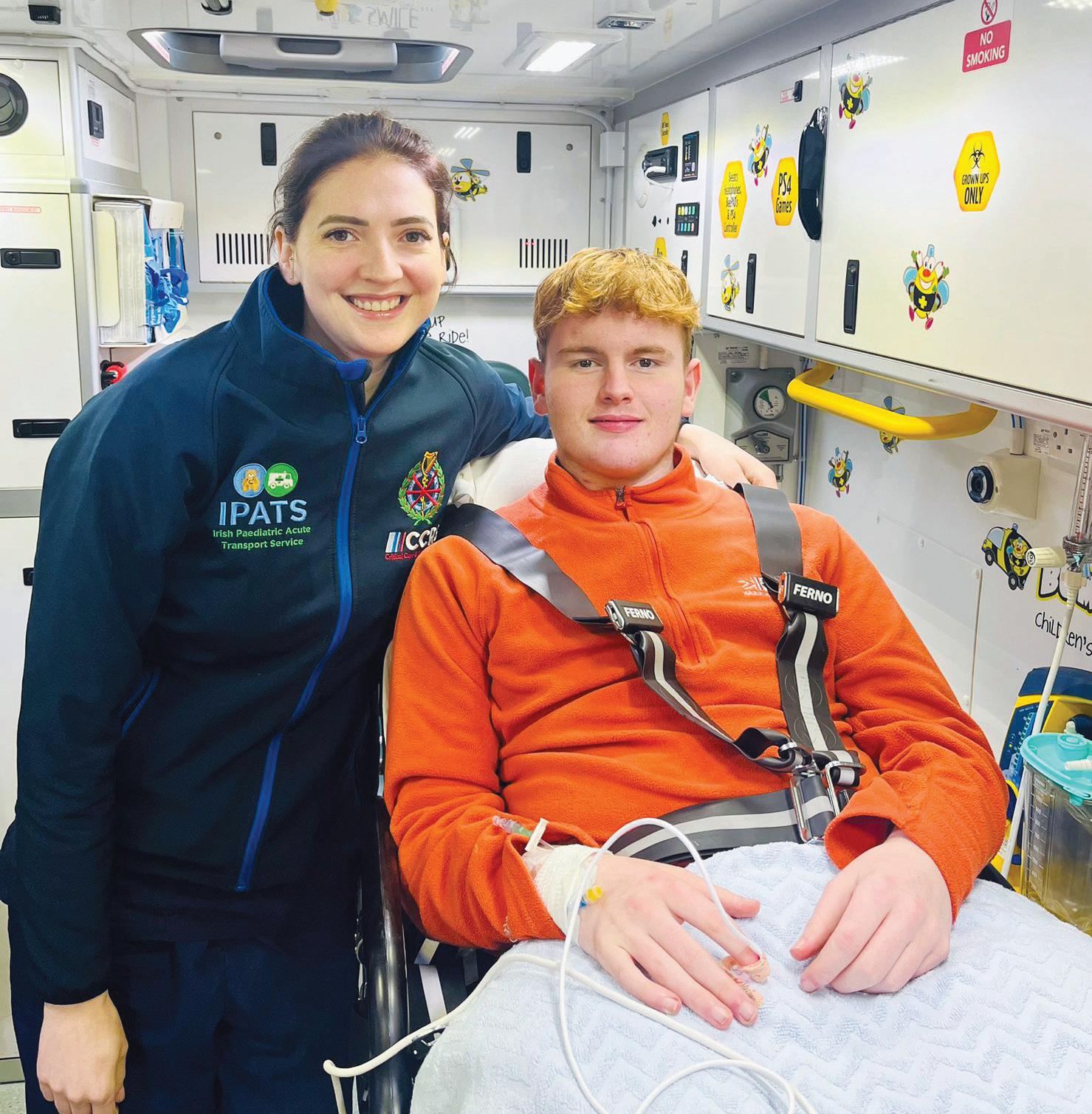
The National Ambulance Service (NAS) has recently established a nurse-led repatriation service to safely bring children and teenagers back to their local hospital once they no longer need specialist Dublin-based care. The service is being delivered by the Irish Paediatric Acute Transport Service (IPATS) which is part of the NASCCRS (Critical Care and Retrieval Service).
“The new IPATS Repatriation Service aims to provide care and support for children and families during a very stressful time and to keep a flow of children into and out of the specialist hospitals so that every child can get the most appropriate care when they
“When a child no longer needs specialist services in a CHI hospital, they can be safely moved back to their local hospital and medical team, close to their home and family."

need it most,” said Anne McCabe, Director of Nursing, NASCCRS and NEOC.
“When a child is transferred to Dublin it is often part of a ‘sharing of care’ model between CHI and a regional hospital that aims to deliver the right care to the child, in the right place, at the right time. When a child no longer needs specialist services in a CHI hospital, they can be safely moved back to their local hospital and medical team, close to their home and family.
“A child will only be referred to the IPATS Repatriation Service team if they are fully stabilised, have seen all the specialist teams they need, and have had any special tests and procedures completed or booked.” Before transfer, a care plan for any child being moved is made between the child’s consultant in Dublin and their consultant in their local hospital. Once both teams are happy with this plan, they will contact the IPATS Repatriation Service and request the transfer to take place, which will usually then take place within 24 hours.
The IPATS Nurse Led Repatriation team completed 25 transfers in its first 30 days of service, including 14-year-old Sean Gibbons. Sean was transferred to CHI in Temple Street by the NAS IPATS critical care team and was then brought closer to home by the team to complete his treatment at University Hospital Kerry. IPATS nurse Pamela Allen, NAS Technician Tommy O'Reilly and Sean’s mum Samantha were on board and taking care of him throughout his journey. HM
| 21 HEALTH MATTERS SPRING2024 Feature











Learning to talk




Learning to Talk video series provides support for parents and healthcare professions



“How do I help my child use more words?” “How can I help them understand more?” “How do I know their speech is okay?” These questions, or variations of them, will be familiar to almost every health professional working with families and young children across the country.

Giving advice is not easy: communication development is complex, and finding reliable, accessible, parentfriendly information can be tricky.



In response to this, HSE Speech and Language Therapy in the Mid-West and ABC Startright in Limerick have collaborated to create the Learning to Talk series; a YouTube video playlist for families and caregivers to support children in their early communication development. Information previously provided by SLTs only in oral and written form has been digitised, allowing access to evidence-based ‘tips and tricks’ on their phone or laptop, from the comfort of their own home. Videos contain real-life examples of strategies and they can be viewed again and again.











together with parents during a session, or parents can be pointed to videos which will be helpful for them.
The idea for the Learning to Talk series was born in 2021 when it was clear that an alternative to in-person speech and language therapy supports would be helpful. Initial videos, although rough around the edges, proved to be popular and were used widely by SLTs and colleagues in the Mid-West. The videos were updated and improved in 2023.

The Learning to Talk playlist is now ready to be used by health professionals across the country. The playlist on the HSE YouTube channel has 20 videos; 16 with tips and advice relevant for anyone who interacts with young children and four videos with more targeted support for children who have a stammer or are reluctant to speak.

The series doubles as a tool for health professionals to highlight or reinforce specific strategies and ideas for families they work with. Videos can be watched


YouTube features allow captions for 80 languages which greatly increases the videos accessibility. Full translation of the videos into different languages is being considered and one video is currently available ‘as Gaeilge’. The Learning to Talk series was shortlisted for a 2023 HSE excellence award in the ‘engaging a digital solution’ category. HM














HEALTH MATTERS SPRING 2024 22 |
John's Campaign
Family carers welcomed as active partners in patient care
A new initiative which ensures that family carers are welcomed in the hospital as active partners in patient care was launched in Letterkenny University Hospital (LUH) recently.
LUH became the first hospital in the country to implement a new policy for patients and their carers, based on John’s Campaign. This development gives carers access to their loved one outside of general visiting times and recognises the role of the carer in the planning of patient care.
A family member or friend of a patient can apply for a carer’s passport with any member of staff. Once they have completed a short form and are registered they will have access to the person they care for at any time, day or night, outside of conventional hospital visiting hours, whenever they feel it is needed.
Martina Porter, Quality and Patient Safety Manager in LUH said, “In LUH we are continually striving to enhance patient-centred care. This initiative is an excellent example of empowering patients, their families and the wider healthcare team to create a care environment where a patient’s individual needs

are met. This partnership has the potential to reduce the common causes of harm, lead to better communication and ultimately, improve patient outcomes.”
Nikki Gerard, who founded the John’s Campaign in the NHS named after her late father Dr John Gerrard, said, “We are so
"John’s Campaign is about compassion, about patient-centred care, about keeping people connected to those they love the most at the time they need them most."
delighted that Letterkenny University Hospital is going to implement John’s Campaign and become the first hospital in the Republic of Ireland to do so.
“John’s Campaign is about compassion, about patientcentred care, about keeping people connected to those they love the most at the time they need them most. We will always be grateful to the staff of the hospital for being pioneers and taking this important step and we look forward to working with you all over the years.” HM
Aoibheann Moreton, Quality and Patient Safety Team; Niamh O’Donnell, End of Life Care Coordinator; and Martina Porter, Quality and Patient Safety Manager in LUH at the launch of John’s Campaign.
| 23 HEALTH MATTERS SPRING2024 Feature
Overdose awareness































The emergence of new synthetic drugs being sold on the Irish heroin market led to clusters of overdoses in Dublin and Cork regions in late 2023. The National Social Inclusion Office continues to monitor the emergence of synthetic opioids including nitazenes drugs on the Irish drug market. These drugs are relatively new to the European market. The risks associated with nitazene drugs are far higher than with heroin or fentanyl.
The NSIO issued a ‘red alert’ for people who use heroin advising of the extra risk and strongly recommended people not to try new types or new batches of drugs. An Irish National Red Alert Group has been formed to monitor cases of concern and to rapidly respond to future outbreaks should they occur.
This cross-sector group is coordinated by the HSE National Clinical Lead for Addiction Services.













Opioid Overdose Awareness and Naloxone Administration
Training course –Module 1 - is now live on HSeLanD. The training course was developed by the NSIO. It aims to provide learners with the skills to recognise, intervene and respond to an opioid overdose, including the administration of naloxone.
The HSE is urging all services that may encounter opioid overdoses to support the provision of naloxone and administration training. Overdose involving synthetic opioids may require both higher doses and multiple administrations of naloxone to temporarily reverse the overdose while waiting for medical care to arrive. In 2023, close to 2,000 people received overdose awareness and Naloxone administration training and 6,500 units of Naloxone were supplied by the HSE to services.
The HSE will provide updates on the emerging situation on the Drugs.ie website and through the Drugs.ie social media channels.
A new overdose prevention programme has been launched by the NSIO. The programme is training people who use drugs to prevent and treat overdoses and includes training in how to administer naloxone. The new Circle Peer to Peer programme began a six-month pilot phase in 16 locations at the start of the year. Some 30 staff members have undergone training to roll out the Circle programme in each of the 16 areas.
HEALTH MATTERS SPRING 2024 24 |
Hot Topic
Spotlight on POSTNATAL CARE
A new pilot service, which will further enhance midwifery care, has been launched by the Maternity Department at Sligo University Hospital. The establishment of a community midwifery service, as an outreach service from the hospital, will provide women and babies with integrated care as close to home as possible.
Postnatal clinic appointments will be offered to all women on day 8 and day 20 after their baby is born. This is in addition to the service currently being provided by GPs and Public Health Nursing.
Women will be invited to attend a clinic in Primary Care Centres in Ballyshannon, Carrick-onShannon, Sligo town and also Ballymote depending on where they live. At the time of discharge from the Maternity ward all women will be provided with an appointment to attend a postnatal hub nearest their home. Each appointment will consist of a consultation with a midwife who will carry out a full mother and baby check. Referrals and follow-up care will be provided as clinically required.

In addition, a midwife is available, Monday to Friday, at designated times, to provide telephone postnatal support to the women.
Karlene Kearns, Clinical Midwife Manager 2, Sligo University Hospital, said, “The aim of the service is to provide enhanced postnatal care, early signposting for additional services, breastfeeding support and reduce postnatal admission. “The service was created in response to feedback from a patient engagement
survey, which revealed that postnatal midwifery care needed to be improved. We are very pleased to be selected as a pilot site by the HSE’s National Women and Infants Health Programme and secured funding for additional resources to support to roll out this pilot.”
Juliana Henry, Director of Midwifery at the hospital, said, “It will help us to provide women with integrated care as close to home as feasible by collaborating with our Public Health Nursing colleagues and GPs. We will be actively monitoring the success of the pilot and adapting it as required to meet the needs of the women using our service.” HM
| 25 HEALTH MATTERS SPRING 2024 Spotlight
Pilot community midwifery service will provide enhanced care
Jenny Greene, Midwife; Karlene Kearns, Clinical Midwife Manager 2; and Michelle McLoughlin, Midwife.
Spotlight Spotlight on AI
Teams using AI to transform how we treat patients with kidney disease
Clinicians and researchers from Galway are using Artificial Intelligence to transform how we treat patients with kidney disease. The collaboration involves the Saolta University Health Care Group, HSE National Health Intelligence Unit, College of Medicine, Nursing, and Health Science, University of Galway, The National Renal Office, HSE Integrated Information Services, Insight Data Analytics, Health Innovation Hub Ireland, and eHealth Ireland. It has been funded by the Public Service Innovation Fund operated by the Department of Public Expenditure, NDP
Delivery and Reform (DPENDR).
Chronic Kidney Disease (CKD) is a progressive condition that affects approximately 10% of people worldwide. Some patients with CKD progress to kidney failure requiring lifesaving treatments like dialysis or kidney transplant. The Kidney Disease Clinical Patient Management System (KDCPMS) is an electronic health record to manage the care of patients receiving dialysis or kidney transplant. One challenge faced by healthcare providers is extracting actionable information from large quantities of
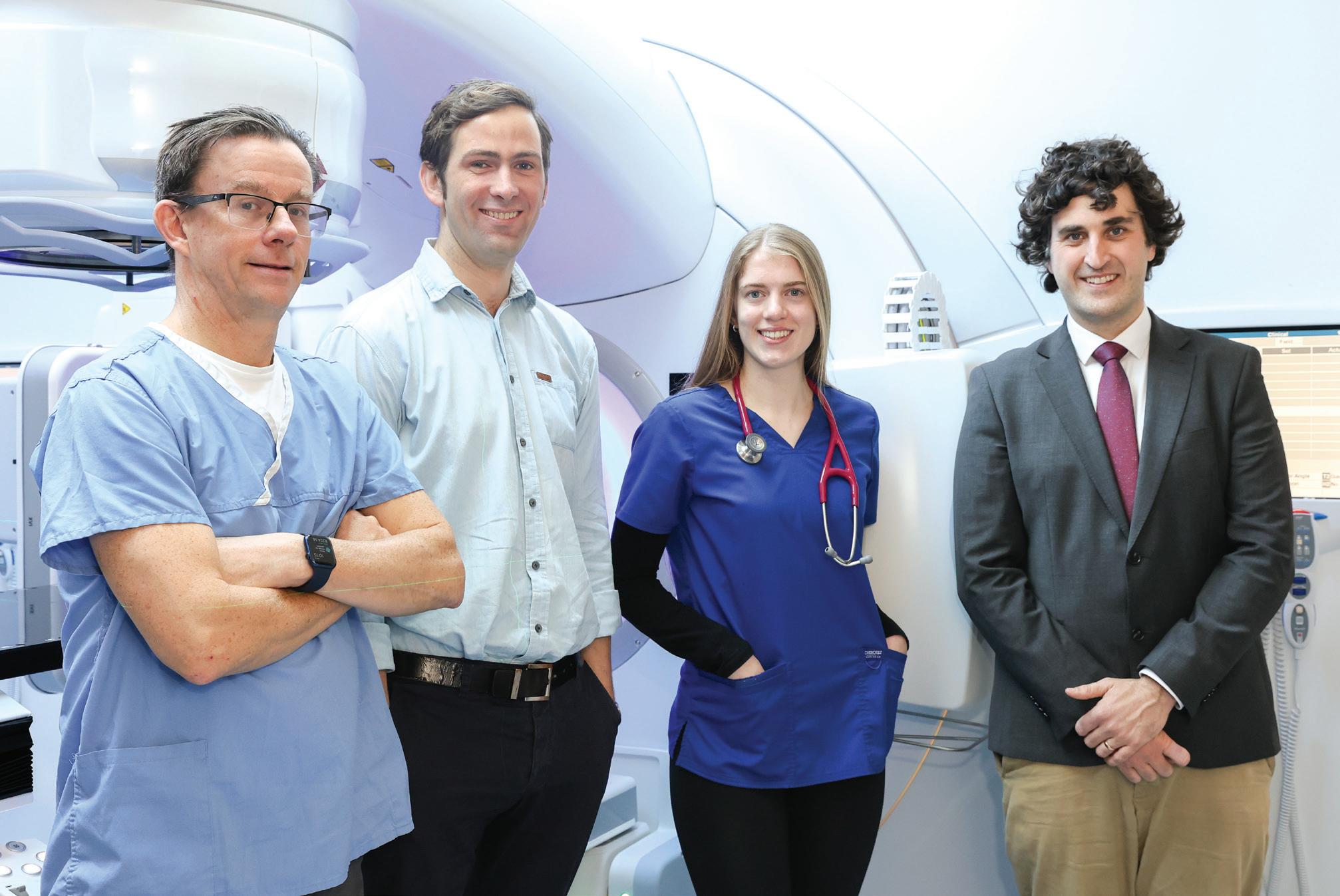
Prof Donal Redden, Consultant Nephrologist at Galway University Hospital; Dr David Keane, Postdoctoral Researcher at the University of Galway; Dr Sarah Monahan, Senior House Officer in Nephrology at Galway University Hospital; and Dr Conor Judge, Consultant Nephrologist at Galway University Hospital.
HEALTH MATTERS SPRING 2024 26 |
“Using Artificial Intelligence in this way will allow us to harness this rich data source to improve patient care in a way that has not been possible to date. We are grateful to the team in the Public Service Innovation Fund who support these types of initiatives..."
unstructured free text, such as clinical notes and outpatient letters, stored in the KDCPMS. This data in its current form is difficult to organise and used for making national decisions about kidney care in Ireland.
Now, the renal AI project is using Artificial Intelligence Language Models to extract key structured information from the free-text clinical notes to inform the national kidney disease strategy.
The AI-powered solution will ensure uniformity and clarity in health records. This information is now being used to compare the quality of Irish patient care to other European and international nephrology centres, a previously impossible task.
Dr Conor Judge, a consultant nephrologist at Galway University Hospitals and senior lecturer in Applied Clinical Data Analytics at the University of Galway, and Clinical Lead in Health Innovation Hub Ireland, is leading this transformative project. He expressed his excitement for the project. “Using Artificial Intelligence in this way will allow us to harness this rich data source to improve patient care in a way that has not been possible to date. We are grateful to the team in the Public Service Innovation Fund who support these types of initiatives that will improve our healthcare system in a meaningful way for patients, staff and the public.”
Dr Howard Johnson, Clinical Director of the HSE National Health Intelligence Unit, added, “This project could pave the way for similar initiatives across other parts of our health services to use the vast amounts of available and unused data to support the delivery of high-quality, efficient, and effective health care.” HM
RESEARCH PROJECT TAKES PLACE INTO USE OF AI FOR BOWEL CANCER SCREENING
The national bowel cancer screening programme BowelScreen is taking part in a five-year research project exploring the use of artificial intelligence (AI) to improve the effectiveness of bowel cancer screening.
The Microb-AI-ome research project aims to analyse gut or stool microbiome data to determine how effective it could be as a screening tool. The research will involve the recruitment of 4,000 people who have had a FIT (faecal immunochemical test)-positive bowel screening result and are undergoing colonoscopy. There will be 1,500 people from the BowelScreen programme at the Mater and St Vincent’s hospitals in Dublin, and the Mercy hospital in Cork; and 2,500 participants in France.
Changes in the gut microbiome happen in people with bowel cancer, or early signs of bowel cancer. Using AI to perform a more detailed analysis of this microbiome data could improve the sensitivity of the screening test used to detect bowel cancer early.
Bowel screening programmes use a FIT to predict the need for colonoscopy to find early signs of bowel cancer. This screening method is effective at reducing bowel cancer incidence and deaths, but the limitations of this test can result in unnecessary colonoscopy treatments for some people.
Recruitment will start in the first quarter of 2024 and all patient data will be anonymised. This research has received ethical approval in Ireland and France. Samples will be analysed at the Alimentary Pharmabiotic Centre (APC Microbiome Ireland) at University College Cork.
The project will receive approximately €6 million from the EU’s Horizon Europe research and innovation programme. Eight partner organisations from Ireland, France, Germany, Romania and Austria are involved in the project, combining international expertise in bowel cancer screening and treatment, microbiomics, AI, software development and privacy protection.
BowelScreen Clinical Director Professor Pádraic Mac Mathúna said, “I see this as the next step in our onward battle against bowel cancer. Our screening methods can be effective in reducing bowel cancer mortality, but the use of AI-generated microbiome analysis has the potential to make our screening programme even more effective.”

Caption: BowelScreen Clinical Director Professor Pádraic Mac Mathúna
| 27 HEALTH MATTERS SPRING 2024
Spotlight
Hot Topic
National Consent Policy
















































The HSE National Consent Policy 2022 has been updated to incorporate the provisions of the Assisted Decision-Making (Capacity) Act. This will help you to bring the Act to life in your work by applying the general principles. This includes the presumption that every adult has capacity to make decisions about whether or not to consent to a health or social care intervention. You must make information accessible, and support each person to make their own decision. It also provides helpful stepby-step guidance on how to proceed if a person’s capacity to consent is in question or lacking.
The Assisted Decision-Making (Capacity) Act 2015:
• introduces new guiding principles about interacting with a person who has difficulties with their decision-making capacity
• establishes a tiered system of decision support arrangements for people who need help with making decisions
• abolishes the current wardship system and requires all wards of court to be discharged from wardship within three years of commencement of the Act.
• establishes the Decision Support Service
• The updated policy and recordings of the webinar events are available at hse. ie/nationalconsentpolicy
These webinars provide staff with the opportunity to develop their skills, knowledge and confidence by exploring real case scenarios.
Over 5,000 staff registered to attend webinars about this updated policy. You can watch recordings of these events on hse.ie/ nationalconsentpolicy. These webinars provide staff with the opportunity to develop their skills, knowledge and confidence by exploring real case scenarios. Topics for discussion included the legal basis to providing an intervention if the person lacks capacity to decide, the role of families, supporting decisionmaking, and how to proceed if a person refuses an intervention.
This updated National Consent Policy, and the scenarios discussed in the webinars, should help staff to ensure that every person can access the care they need. If a person's will and preferences are in agreement with an intervention, the healthcare worker is acting in good faith and for the benefit of the person and those who must be consulted agree, then an intervention may proceed without a court order. Assessments of decision-making capacity should not be seen as a means to override a person's will and preferences.
HEALTH MATTERS SPRING 2024 28 |
Spotlight on DIVERSITY
The new eLearning programme, Diversity, Equality and Inclusion in the Workplace, is available now on HSeLanD
The HSE Diversity, Equality and Inclusion team has devised a new programme which aims to support all staff members across the health service to apply the principles of diversity, equality and inclusion to our working environments and teams.
“We wanted to develop a useful and practical learning resource for all staff members,” said Maria Molony, Diversity, Equality and Inclusion Manager in National HR Capability and Culture. “We designed this programme to provide information and guidance on some of the most common types of enquiries that our team receives from staff on topics relating to diversity, equality and inclusion in the workplace.”
The eLearning programme has been developed with support from the three HSE Staff Networks:
• The Cultural Diversity Network for employees from diverse ethnic and cultural backgrounds and their allies
• The Le Chéile Network for employees with disabilities and their allies
• The Reach Out Network for Lesbian, Gay, Bisexual, Transgender, Queer, Intersex and Asexual (LGBTQIA+) staff and their allies.
“The new eLearning programme holds great significance as it

brings attention to the challenges and issues faced by staff from marginalised groups on a daily basis, which often go unrecognised by the broader community,” said Cathy Blake, Assistant Staff Officer in the Finance Department in Community Healthcare Organisation West, who is also Vice Chair of the HSE’s Reach Out Network for LGBTQIA+ employees.
“The modules motivate us to take into account the lived
experiences of our fellow colleagues in the workplace and be mindful of the difficulties they may encounter.”
The eLearning programme is available on HSeLanD and consists of three modules. You can find the programme in the Human Resources course catalogue, or by searching for each module name in the HSeLanD search engine. The three modules are Introduction; Inclusive Communication at Work; and Working in a Diverse Team. HM
If you have any feedback on the eLearning programme or if you would like further information or guidance, please contact diversity.hr@hse.ie.
| 29 HEALTH MATTERS SPRING 2024 Spotlight






Free vaccine for prisoners


Peer support plays major role in HPV vaccine uptake in

prison



Caption:
Dr Breda Cosgrove, Consultant in Public Health Medicine; Dr Claire Sharkey, Specialist Registrar in Public Health Medicine; and Elaine Dunne, National Infection Control Team, Irish Prison Service.
THE HSE in the Mid-West region joined forces with the Irish Prison Service to deliver one of its most successful vaccination initiatives in the region in 2023, as part of the Laura Brennan HPV Vaccine Catch-Up Programme.


Launched in 2022, the Laura Brennan HPV Vaccine Catch-Up Programme was a nationwide, HSE-led plan of action to provide free and accessible HPV vaccines to young people who had missed, or did not have the opportunity to avail of this life-saving vaccine during their school years.
The HPV vaccine protects against the types of HPV that cause approximately 90% of cervical cancers; 90-95% of HPV-related anal cancer; and 90% of genital warts.




HPV-related cancers can leave a devastating impact on individuals, families and their communities, as it can affect young men and women, particularly among those in vulnerable groups or areas of deprivation.
This is why Public Health HSE Mid-West, Primary Care Services, and Limerick Prison collaborated to deliver on-site engagement and information, followed by free vaccine clinics to prisoners in December 2023.




The prisoners proved to be the key asset, as five individuals - two men and three women - acted as effective on-site promoters of the HPV vaccine.




staff face-to-face to share key information on HPV and the vaccine, but also to learn about their own health information needs on the ground. Of a cohort of 30 eligible individuals, 12 received their life-saving HPV vaccine at a clinic, organised by ADPHN Jacqueline Gibson and Primary Care Services Manager, Marion Kennedy. The clinic was delivered by nurses Anne Delahunty, Miriam Lupton and Mary Breen, and Dr Phil Fitzgerald.
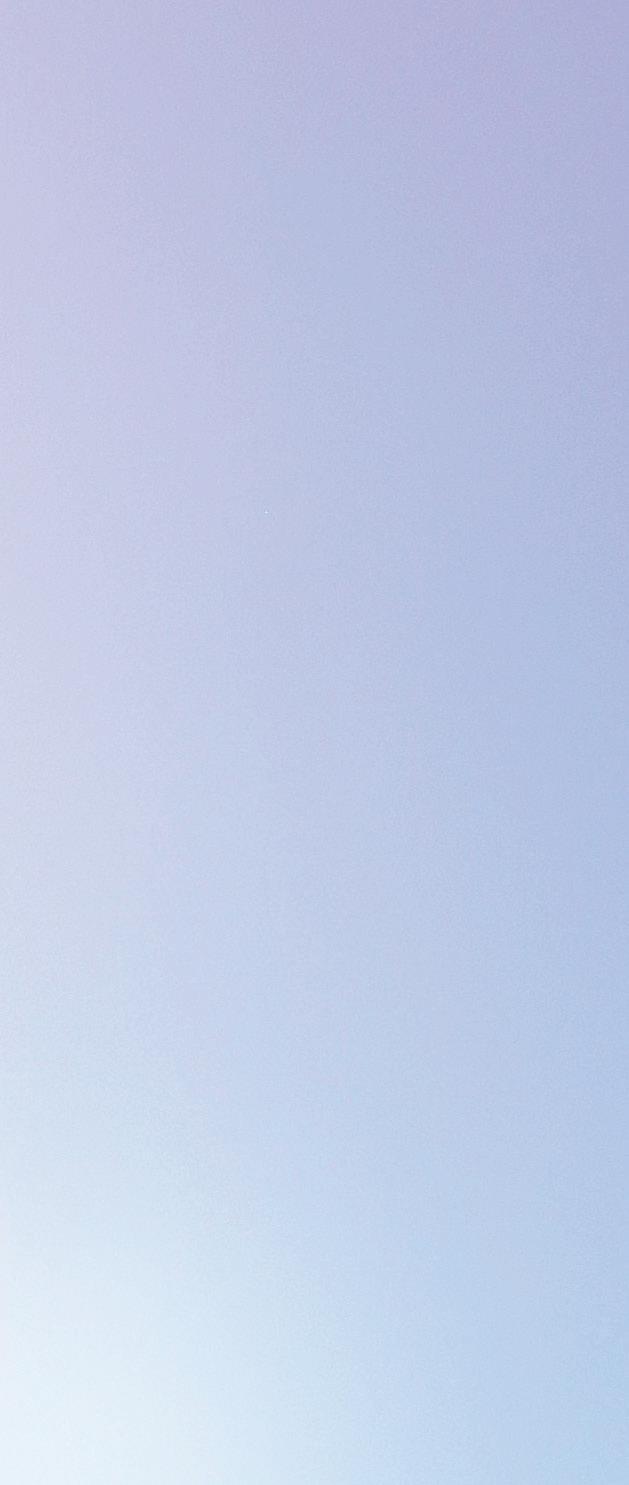

Dr Breda Cosgrove, Consultant in Public Health Medicine, hailed the initiative as a visible success in multi-stakeholder vaccine promotion.

This was made possible through the innovative Irish Red Cross Prison Programme, which enables the prisoners to be wellinformed peer-to-peer educators on the ground as familiar, trusted individuals.
In additional to substantial preclinic planning and logistics, a multidisciplinary Public Health team met with prisoners and


“This initiative would not have been possible without the support and enthusiasm of all those involved - the Irish Prison Service, our colleagues in HSE Community Healthcare, our own team in Public Health HSE Mid West and especially the five Red Cross peer-to-peer educators. It was a very positive experience and a great example of collaboration between organisations in the region,” she said.
Approximately 1,100 people were vaccinated as part of the Laura Brennan HPV Vaccine Catch-Up Programme in the Mid-West, which ended on 31 December. HM

HEALTH MATTERS SPRING 2024
30 |
Autism Reality Bus
Autism Reality Experience gives unique insight for healthcare staff

Staff in the north east have been given the opportunity to experience how the world might be viewed by an autistic person. Autism is a neurological condition that can affect people in very different ways. How they experience and interact with the world around them will also vary greatly. Sensory processing can impact on the person’s ability to interact and communicate socially as well as affecting their mental health by increasing their anxiety.
The Autism Reality Experience has been developed by UK Company Training to Care to simulate the sensory experiences of the autistic person.
Drawing on the knowledge and advice of Sensory Integrated Occupational Therapists and an advisory group composed of people with autism they built a simulator that exposes and stimulates the person’s senses to ‘overload’.
Participants attending this event were provided with 10 minutes in the simulator followed by a debriefing session to reflect and acknowledge what they have just been experienced.
The Centre for Nursing and Midwifery Education covering Cavan, Louth, Meath and Monaghan were delighted to provide this experience to their services. Over seven days, this very immersive and hands-on Autism Reality Experience travelled across four counties bringing an innovative approach to autism training. At Our Lady of Lourdes Hospital in Drogheda, the Autism Reality Experience delivered the simulator and
debriefing session to 24 staff across multiple disciplines.
Supported by the Nurse Liaison Carmel Daly, this training will be an essential component and addition to staff facilitating reasonable adjustments which can assist people who may require extra supports within an acute setting.
It also visited other healthcare services around the region including primary care and disability services.
One staff member said, “As an A&E paediatric nurse, the experience provided me with greater awareness and understanding of the sensory needs of the autistic person.”
Another said, “This was an invaluable insight into what an autistic person experiences. It exceeded all my expectations and will fundamentally change how I perceive autism going forward.” HM

| 31 HEALTH MATTERS SPRING2024 Feature

Talking point
Climate Action
Building a sustainable healthcare service
Across the HSE we aim to deal with the growing health impacts of climate change by reducing emissions and becoming a more sustainable healthcare service.
The focus in 2024 is to build on our existing work and on the extensive work progarammes set out in the HSE Climate Action Strategy launched last June. In addition the HSE must meet requirements in the latest Government’s Climate Action Plan 2024 that sets out new responsibilities for all public sector bodies. HM




































32 | p ====� l�\ � (� -•� O;i�'8 n ··Q;. & -� -� ____.___I I I I l IA-8� 8 ---
The National Climate Action Plan provides the overarching national policy framework for implementation of the HSE strategy. To meet public sector targets, the Climate Action Plan commits the public sector to:
• Achieve the emission reduction and energy efficiency targets
• Strengthen climate action reporting
• Provide climate related training and up-skilling
• Transition to Zero emissions vehicles and have a charging infrastructure plan for fleets
• Implement Green Public Procurement
• Scale up decarbonisation, retrofit and energy efficiency of public sector buildings
KEY ACHIEVEMENTS ACROSS HSE CLIMATE ACTION
A HSE Climate Action Steering group is established and work programmes, delivering on 10 strategic objectives, have been set up with programme leads in place across all.
The HSE Climate Action Strategy focuses on the following priority areas:
• sustainable buildings and the green environment
• transport and mobility
• sustainable procurement
• greener models of healthcare
• water and waste management
• adaptation and resilience
An approach has also been agreed to underpin the HSE Strategy which is focused on practical implementation through six regional green committees and local green teams.
CLIMATE ACTION PROGRAMME HIGHLIGHTS INCLUDE:
• infrastructure Decarbonisation Roadmap updated for 2024
• 583 minor capital projects delivered by HSE Capital and Estates with ROO of €28M and 8,837 CO2e savings
• upscaled deep retrofit plan commenced
• capital approval for five sites and seven sites at stage 2 design
• Energy Efficient Design and Net Carbon Zero in all Capital Projects
• site visits complete to all 15 Green Environment pilot sites
• 16 Certified Energy Manager training sessions delivered to 469 participants
• green theatres and sustainable inhalers early mobilisation initiatives launched to drive greener models of care programme
• four pilot water stewardship projects completed
• climate and Health Alliance charter signed
• regional Green teams established nationally
• over 145 Energy and Green teams established across the HSE.
Staff information campaign
The recent HSE ‘Your Opinion Counts Staff Survey’ indicated over 60% of staff want to be involved in activities to support positive climate action. A HSE staff campaign on Climate Action went live in November 2023, promoting simple positive actions that can be taken individually and collectively to tackle climate challenges in local environments and to make sustainability and adaptation part of our daily routine and culture. The ‘We’re Taking Climate Action’ information campaign has been important in promoting the HSE’s commitments to the climate agenda and our six areas of focus to work. It will be continued in 2024 and help empower staff to be more involved in local initiatives and in Energy and Green teams.
| 33 HEALTH MATTERS SPRING 2024
point
Talking
I I
____.___I I I
Visit hse.ie/climateandhealth for more information #ClimateAction
Things YOU can do
At work
• save energy
• turn off non-essential equipment like computers, photocopiers and appliances over lunch breaks, nights and weekends if not needed
• make best use of daylight and turn off lights in unused rooms and corridors when not needed and safe to do so
• dress for building temperature, avoiding the need for personal heating or cooling appliances
Ordering materials or services
• reduce, reuse, recycle
• switch from using disposable to reusable products
• share ideas for more sustainable products with your local management
• consider the possibility of reducing or reusing your equipment
• take into account the necessity, packaging, and environmental impact when requesting supplies
• healthcare waste awareness - potential health hazards should be disposed of properly
Healthcare models
• be an active promoter for healthy living
• reuse clinical and medical products when safe to do so
• consider environmental impact of medications
• use online meetings and consultations

• print only when necessary using recycled FSC paper, printing double sided and in grey scale
• think about having plants or developing a green space
On the move
Water and waste
• go plastic free and use reusable cups, glasses and dishes




• avoid unnecessary travel
• switch your mode of transport from cars to walking, cycling, or public transport
• car pool with colleagues to reduce your car travel footprint

• use the cycle to work scheme

• use Teams for meetings where appropriate

• if you must use disposable items ensure they are biodegradable or compostable
• use a 'keep cup' or water bottle and ask for water dispensers to allow staff to fill their bottles

• bin it right - check the bin label and separate waste appropriately




• go binless in your office

• every drop counts - be conscious of your water usage and only use what’s necessary





Adaptation and resilience
• learn about the health impact of climate change on your service quality and safety
• has your service been affected by severe weather events, for example, flooding, power loss, indoor overheating?






• has your service adapted effectively to protect the health of your patients and staff
• speak to colleagues about concerns and how to take positive action












34 | p ====� l�\ � (� -•� O;i�'8 n ··Q;. & -� -� ____.___I I I I l IA-8� 8 ---

2GoCup targets daily reduction of 1,200 single-use cups
A waste reduction initiative at University Hospital Limerick has the potential to take up to 1,200 single use cups a day out of the waste stream.
UL Hospitals Group has teamed up with its catering partners Compass Group to minimise its impact on the environment through the introduction of reusable cups at two cafes across UHL.
Customers pay a €2 deposit for their coffee or tea and return the cup for a refund or keep it for future use. The cups are dishwasher safe and have a lifespan of 1,000 uses, or approximately 3 years.
In this initiative, we have partnered with an Irish company 2GoCup, which is also involved in the successful scheme in Killarney as the tourist town aims to go single cup free.
“At UL Hospitals Group, we are dedicated to reducing our impact on the environment in line with the HSE Climate Action Strategy 2023 to 2050, which was published in June. We are going to be hearing more and more about the circular economy over the duration of that strategy and this is exactly the kind of project we hope to see a lot more of,” said Maria Quirke, Directorate General Manager, Operational Services, UL Hospitals Group.
“There has been a very positive reaction from our customer base on the first day of this initiative on Monday and our staff distributed approximately 200 2GoCups in the first two hours of trading alone. It shows that there is a real desire among the public to think about our growing consumption and its impact on the environment and we are delighted to be part of this initiative at our hospital cafes,” said Conor Nestor, General Manager, Compass Group, University Hospital Limerick. HM
EVENTS RAISE AWARENESS OF CLIMATE ACTION IN HOSPITALS
Acute hospitals across the country are pulling their weight in the climate action fight, hosting a series of Energy and Climate Action Awareness Days. All were a great success and well attended by hospital staff, with information stands giving advice on taking climate action, energy reduction, water conservation and waste prevention measures.
Midland Regional Hospital (MRH)
Tullamore held a Sustainability Awareness event, organised by the MRHT Green Team. The Green Team consists of a group of interested staff members, supported by dedicated HSE Capital and Estates Energy Officer Evan Weatherup and Sustainability Officer Kenneth Hyland.
Their colleagues in MRH Mullingar held a staff energy awareness day on 1 December with support from the OPW. Hospital Manager Kay Slevin, Facilities Manager William Harding and Capital and Estates Energy Officer Evan Weatherup were also there to support the event.
Sligo University Hospital Green Campus Committee held a Sustainability Awareness Day for staff on 6 December, with support from Capital and Estates Sustainability Officer Ruairi Keane and Energy Officer Declan Barrett.
Meanwhile, Letterkenny University Hospital held a ‘LUH Big Switch-Off Weekend’ event in December, supported by Capital and Estates Energy Officer Noel Gallagher.
The aim of the LUH Switch-Off event was to change the approach to energy usage and conserve as much electrical and thermal energy as possible in the hospital during the weekend and demonstrate the cumulative impact of small individual actions across the workplace.
All events support the achievement of Government Energy and Carbon Reduction Targets, the HSE Capital and Estates Infrastructure Decarbonisation Roadmap Actions and the wider HSE Climate Action Strategy.
| 35 HEALTH MATTERS SPRING 2024 Talking point HEALTH
Plaque commemorates Cork City Hall being used as a vaccination centre
A plaque was unveiled at City Hall Cork to commemorate that the building was used as a vaccination centre during the COVID-19 pandemic. The steel plaque incorporates a newspaper image of the exterior of the vaccination centre, with people queuing for vaccinations.
Damien McCallion, Chief Operations Officer, HSE, joined officials from Cork Kerry Community Healthcare (CKCH), Public Health Area D, Cork City Council and the South West Hospital Group to watch Lord Mayor Cllr Kieran McCarthy reveal the plaque, which reads, ‘City Hall Cork, in use as a community vaccination centre from April 2021 until March 2022. In memory of all those who passed through and those we lost during the COVID-19 pandemic.”
Tess O'Donovan, Chief Officer CKCH, said, “While COVID-19 vaccination is now integrated into our wider vaccination programme, we will never forget how the difference which centres like this one made to all our lives.”

Ita-Marie Dunne, Patient Experience Manager; Niamh Barrett, Deputy General Manager; Dr Nader AL-Mane, ICU Clinical Lead; Sonja Soerensen; Steffen Soerensen; Dr Bilal Jamil; and Ruth O’Connor, Theatre Nurse.

National Inpatient Experience Survey 2024 takes place shortly
The National Inpatient Experience Survey returns in May and will off er patients the opportunity to describe their experiences of care in public acute hospitals in Ireland. Thank you to the staff of participating hospitals for their continued support with this survey.
The National Inpatient Experience Survey 2024 will
Danish tourist returns to hospital to thank staff who saved his life
A Danish tourist has returned to Naas General Hospital to thank the doctors and nurses who saved his life while holidaying in Ireland.
After collapsing in Tinahely, Co Wicklow, Steffen Michael Soerensen, a was admitted to Naas General Hospital in November 2021 where he underwent surgery following a life threatening condition and was revived after suffering two cardiac arrests, on one occasion receiving CPR for 29 minutes.
Speaking to the staff of Naas General Hospital, Steffen said, “Thank you to all of the doctors, nurses and hospital staff at Naas General Hospital that were involved in my care and recovery. I can only express my deepest gratitude for the incredible actions and management that the team displayed when they saved my life. Words cannot express how thankful I am and I will never forget what you all did for me.”
want to hear from patients who were discharged from hospital in May 2024. Patients aged 16 and over who spend 24 hours or more in a public acute hospital, have an address in the Republic of Ireland and are discharged in May, are invited to participate in the survey. It is the largest survey of its kind in Ireland and offers patients the opportunity
HEALTH MATTERS SPRING 2024 36 | News
100% compliance for third year in a row at Waterford care facility
For the third year running, the Mental Health Commission has recorded a 100% compliance rate in its inspections of the HSE/South East Community Healthcare’s Grangemore residential support facility in Waterford. Located on the grounds of St Otteran’s Hospital, Grangemore provides continuing mental health care and rehabilitation to 14 residents.

The Mental Health Commission (MHC) plays a key role in inspecting and measuring compliance to its regulations at inpatient and residential care centres. The MHC holds providers to account for achieving and maintaining a range of standards, identifying areas for improvement in mental health services and helping to ensure that the best possible service is provided to all service users.
Head of Service/Mental Health for HSE/South East Community Healthcare (SECH) Anne Donaghey said, “Including through the challenging times of pandemic, there is an enormous contribution being made every day by my dedicated colleagues in our mental health services. In congratulating Consultant Psychiatrist in Rehabilitation and Recovery Dr Darina Sloan, Clinical Nurse Managers 2 Grace King and William Browne, CNM 1 Helen Murphy and all of the team on this achievement, I know they’re also keen to include patients and their families for their support in this ongoing success story.”
to share their experiences of hospital care and tell us what improvements they believe are necessary.
Eligible patients will receive an invitation and two reminders in the post between June and July to take part in the survey. Patients can take part online or complete the hard copy survey they will receive in the
HSE County
Clinic
staff Carrie Brogan, Sharon Dowling, Susan Finnegan, Denise Walsh, Colet Murphy, Helena Mongey and Joe Lawlor, OLHN, present the cheque to Frances (on the right) from Meath Women’s Refuge.
Some of its team members pictured at Grangemore Continuing Mental Health Care and Rehabilitation residential support facility in Waterford.
Back: Dr Vausra Abuzaid, Senior House Officer); Robin O’Donoghue, Staff Nurse; Natasha Blanchfield, Student Nurse; Emily Murphy, Nurse Intern; and Ella Stack, Nurse Intern.
Front: Grace King, Clinical Nurse Manager 2; Ife Solaoldokun, Senior Staff Nurse; and Dr Darina Sloan, Consultant Psychiatrist in Rehabilitation and Recovery.
post. As a change in this edition of the survey, the hardcopy questionnaire will no longer be sent with the invitation letter but with the first reminder. A full advertising campaign will take place before the survey goes live.
The National Inpatient Experience Survey is part of the National Care Experience

HSE staff raise over €2,800 for Meath Women’s Refuge and Support Service Charity
The HSE staff in the Meath County Clinic decided to do a Christmas Jumper Raffle in December 2023, with over 15 beautiful handmade hamper prizes to be won, raising a brilliant €1,760 in aid of Meath Women’s Refuge in Navan. The aim of the raffle was to raise awareness and donations for the people who have worked tirelessly throughout Meath to provide care and support for women and children in crisis.
In addition to this, a generous donation of €1,040 was added by Joe Lawlor from Our Lady's Hospital, Navan, in collaboration with the GAA, through helping out with their car parking overflow for matches held in Páirc Tailteann, which brought the total fundraising figure to a fantastic €2,800. Frances from Meath Women’s Refuge collected the cheque, saying, “We are absolutely grateful to the HSE staff who have raised so much money to help improve the wellbeing of the women and their families. I want to say a huge thank you to all of those who donated to us and a big thank you goes to everyone who took part in organising the event, as this would not be possible without your support.”

Programme (NCEP) – a partnership between the Health Information and Quality Authority (HIQA), the Health Service Executive (HSE) and the Department of Health. Find out more about the National Inpatient Experience Survey including FAQs on yourexperience.ie and on Twitter, Instagram, or Facebook.
| 37 HEALTH MATTERS SPRING 2024 News
Spotlight Spotlight on Patient Safety
What does the Patient Safety Act (Notifiable Incidents and Open Disclosure) 2023 mean for me
The Patient Safety (Notifiable Incidents and Open Disclosure) Act 2023 is due to be commenced this summer. The exact date is to be confirmed by the Department of Health. In this article colleagues and partners share their views on the legislation.
Bernie
O’Reilly – Chair Person Patients for Patient Safety Ireland
As a patient I want to be involved in all aspects of my healthcare and I want and am entitled to be informed when something goes wrong during my care. This Act, while it mandates for open disclosure in a number of serious harm events, will I feel strengthen the HSE Policy on Open Disclosure for all patient safety incidents. As a patient I want to be reassured that when an incident happens that it is reported and reviewed and that there is learning across the system and this Act places an obligation on services to ensure that this happens.
Carole Broadbank – Chief Officer CHO8
As Chief Officer I fully support a culture of openness and transparency. The Act will bring some changes but fundamentally supports what we are trying to do already. For ease of implementation I understand that the HSE Open Disclosure Policy will align to the Act and additional resources and training will be made available for our staff which will be welcome. We will be overseeing its implementation and resources are available for staff if they need additional support during its commencement this summer.
Dr Jack McCarthy – SHO NCHD
Adverse patient outcomes are our worst nightmare as NCHDs. The HSE Open

Disclosure Policy has helped guide us in our conversations with patients and family members when these unfortunate incidents happen. Following on from this the Patient Safety Act will further help us with clear direction on our next steps in these situations in relation to our responsibilities both to our patients and their relatives in particular in relation to the list of Notifiable Incidents. All of this will be exceedingly helpful late at night at the end of a long shift when clear guidance can be hard to find.
Ruth Finlay - CNM3 Dublin South East Mental Health Services CHO6
All the notifiable incidents are very serious. One of the 13 notifiable incidents’ (NI) that may be reported in a mental health service is a death by suicide. This is already an SRE. Being dually governed by the HSE and Mental Health Commission, the reporting of an SRE is currently conducted via a double reporting system through NIRF documentation and the MHC comprehensive information system (CIS). We also have analytical processes utilised by the Serious Incident Management Team to further review such tragic events and follow the HSE OD Policy. The Act sets out specific
requirements for the coordination of the open disclosure meeting following a notifiable incident and provides direction in terms of the required written follow-up with the relevant persons. Importantly, in my role I would aim to ensure a designated person is identified early to support the family and that my staff are supported throughout the aftermath of the incident as it would be traumatic for all involved.
Moya Wilson – Quality and Patient Safety Manager, Sligo University Hospital

This Act requires that I ensure staff recognise when a notifiable incident has occurred so that the process of alerting the regulator can be triggered. While our hospital operates an Open Disclosure Policy, we must ensure that the additional requirements of the Act are adhered to such as ensuring that the record of the OD meeting is sent out within five days of the meeting being held. Whilst the Senior Accountable Officer is always informed of serious incidents there are one or two notifiable incidents that might not have been automatically reported before such as those relating to therapeutic hypothermia. It will be important to work closely with services such as maternity. Training for staff will be important.
HEALTH MATTERS SPRING 2024 38 |
THE DESIGNATED PERSON – A CRITICAL ROLE IN INCIDENT MANAGEMENT AND OPEN DISCLOSURE
Angela Tysall, National Open Disclosure Office, explains the role of the Designated Person
Patients who have suffered harm as a result of a patient safety incident need practical, emotional and psychological support and this should arrive seamlessly. The early assignment of a named designated person by the health services provider is essential to ensure that the person affected/their relevant person(s) do not feel isolated and do not feel the effects of compounded harm due to a poor experience during the incident review process.
Staff should have the necessary skills and experience required to fulfil this important role. The designated person will act as the liaison person between the service provider and the patient/their relevant person ensuring that their support and communication needs in respect of the plans for the management of the incident, including review and open disclosure, are identified, communicated and addressed.
The name of the designated person must be recorded in the incident management/open disclosure record and their contact details provided to the patient/relevant
Gerry Clerkin
- Head of Service, Quality Safety & Service Improvement
CHO1

This Act supports our work on implementation of the HSE Open Disclosure Policy and a culture of openness and transparency across all services. For community settings I need to ensure we have robust processes in place across all services to capture all notifiable incidents and ensure compliance with the legislation in the management of these incidents. Monitoring notification to the regulator will be important. Ensuring that support is provided to all those impacted by serious incidents must be considered in the implementation of this legislation. There must be mechanisms in place to measure performance and provide assurance to the Chief Officer or Regional Executive Officer going forward.
Dr John Fitzsimons – Consultant
Paediatrician, CHI Temple Street and Clinical Director for Quality Improvement (NQPSD)
I see the Act as a way to improve patient
person and staff members involved.
The appointment of a designated person is a requirement of the HSE Open Disclosure Policy 2019, the DOH National Open Disclosure Framework October 2023 and HSE Incident Management Framework 2020 and is a provision of Part 4 of the Civil Liability Amendment Act 2017. It is not only seen as a nice to have role but essential and will be a requirement in law under the Patient Safety (Notifiable Incidents and Open Disclosure) Act 2023 once it commences this summer.
In preparation for the commencement of the Patient Safety Act this year, service managers must identify the staff in their service who fulfil the role of the Designated Person and ensure that they have access to the resources and training available to them. The HSE will be offering resources and training for these staff.
Further information on this role is available here Designated Person Checklist is available here

care and enhance learning, in a protected way, for all healthcare professionals. I believe the Act aligns with the principles and values outlined in the Irish Medical Council’s recently updated Guide to Professional Conduct and Ethics.
Several components of the Act will affect medical practice so it’s important to become familiar with it. Doctors will need to be aware of the list of mandated notifiable incidents although these are relatively few and additional guidance is being developed. The Act also creates protections for individuals to prevent information from clinical audit being used in legal or disciplinary proceedings. As with any change this will require engagement, time and trust to embed but I believe the end result will be good for both medical practitioners and patients.
Lucy Nugent – CEO Tallaght University Hospital
As the CEO of a hospital I am the accountable officer for the

implementation of the Patient Safety Act in my hospital. Thankfully I won’t be doing this on my own as we have a great team who will be supporting this work.
I want to make sure that open disclosure is part and parcel of the care we deliver and that the Act is not seen as something overly new and complex but part of our every day.
It’s important that we meet our reporting requirements and maintain a good relationship with the regulator.
Dr Orla Healy – National Clinical Director National Quality and Patient Safety Directorate
The National Quality and Patient Safety Directorate are here to support staff and organisations with the implementation of the Act. We will be sign-posting regular updates and provide training for staff. We are working with colleagues on key pieces required for its implementation such as the technical changes to the NIMS system through which the regulators will be notified of a Notifiable Incident.
| 39 HEALTH MATTERS SPRING 2024
Spotlight
HSE Health Regions
New Regional Executive Officers to lead health regions
HSE CEO Bernard Gloster has announced details of the appointment of Regional Executive Officers (REOs) for the six new health regions. As part of implementing Sláintecare, the HSE has organised service delivery into the six health regions, effective from 1 March 2024.
Each REO will be the accountable officer at health region level, responsible for the delivery of high-quality, safe and accessible services for the population of their region.
REOs will report directly to the HSE CEO on the operation and management of the health regions. They will form part of the core HSE
FOLLOWING A PUBLIC APPOINTMENTS SERVICE-LED PROCESS, THE HSE CEO HAS APPOINTED:
Sara Long - REO, HSE Dublin and North East (North Dublin, Meath, Louth, Cavan and Monaghan)
Martina Queally - REO, HSE Dublin and South East (Tipperary South, Waterford, Kilkenny, Carlow, Wexford, East Wicklow, parts of South Dublin)
Kate Killeen White - REO, HSE Dublin and Midlands (Longford, Westmeath, Offaly, Laois, Kildare, West Wicklow and parts of South Dublin)
Tony Canavan – REO, HSE West and North West (Donegal, Sligo, Leitrim, West Cavan, Roscommon, Mayo and Galway)
Dr Andy Phillips - REO, HSE South West (Kerry and Cork)
Sandra Broderick - REO, HSE Mid West (Limerick, Tipperary and Clare)
Senior Leadership Team, providing regional input into the development of national policies and standards.
“The move to the new regions, and a reformed and repurposed HSE Centre, represents a considerable change to our organisational structures,” said Bernard Gloster.
“I am confident we have assembled a strong team of the six most senior officials in the HSE, reporting directly to me. Individually and collectively, they bring a broad range of skills and experience, placing them as the healthcare experts who will lead the next phase of health service delivery in Ireland. I look forward to working with them.
“I want to emphasise that structural change is not the main goal of this reform. The idea behind reorganising our structures is to ensure that people experience just one health service, providing whatever care they need at the right time and in the right place.
"When we talk about ‘integrated care’, this is what we mean.
“I’d like to thank HSE staff around the country for their support and hard work as we transition this year.
"I look forward to working with each of the new REOs, and the teams they will form over the coming months, to provide a better health service for everyone living in Ireland.” HM
"The idea behind reorganising our structures is to ensure that people experience just one health service, providing whatever care they need at the right time and
in the right place."
For more information on HSE health regions visit www.hse.ie/healthregions.
HEALTH MATTERS SPRING 2024 40 | Making progress on Sláintecare and integrated care
Timeline
From 1 March 2024
2025 onwards
Health regions will continue to be embedded and enhanced
Health regions in place from 1 March as REOs are appointed. The health regions will continue to develop in line with the implementation plan. Current CHO and Hospital Group boundaries adjusted in line with health region boundaries. The CHO and Hospital Group management teams will support and report to the REOs until the EMTs are appointed.
September 2024
CHOs and Hospital Groups stood down by end of the month
Health region
EMT appointed
Glossary
REO: Regional Executive Officer
IHA: Integrated Health Area
ISD: Integrated Service Delivery
EMT: Executive Management Team
CHOs: Community Healthcare Organisations
BENEFITS OF HEALTH REGIONS
Health regions will function as part of a strengthened regional health and social care service, with their own budget, leadership team and increased local decision-making.
The structure of health regions will enable staff to provide services that are:
• integrated
• locally planned and delivered
• easier to access and navigate
• available closer to home
Patient benefits include:
• care closer to home
• services based on the region’s population
• consistent quality of care
• patient involvement in their own care and treatment
• strengthened governance and accountability
Health regions' objectives include:
• aligning and integrating hospital-based and community-based services to deliver joined-up, integrated care closer to home
• clarifying and strengthening corporate and clinical governance and accountability at all levels
• supporting a populationbased approach to service planning and delivery which aims to address health inequalities
• improving equitable regional investment and balancing national consistency with appropriate local autonomy to maintain consistent quality of care across the country
• running an efficient, highly productive, and transparent health and social care service with aligned incentives to provide people with timely access to safe, high-quality, integrated care.
| 41 HEALTH MATTERS SPRING 2024
progress on Sláintecare
care
Making
and integrated
HSE Dublin and Midlands
HSE Dublin and North East HSE Mid West HSE South West HSE Dublin and South East HSE West and North West


Sara Long







Regional Executive Officer
HSE Dublin and North East
Sara Long was appointed Chief Executive of the Education Authority in Northern Ireland in 2019, having joined in 2016 as Director of Operations and Estates. Sara has extensive experience of building strategic partnerships, driving service performance and achieving results. Highlights from her career in the Education Authority include: establishing a Centre of Procurement Expertise; taking forward digital solutions for admissions and transport; leading the organisation through COVID-19 and driving forward a significant transformation programme in relation to Special Educational Needs services.
Sara has previously enjoyed an extensive career within Health and Social Care including management posts in acute and community care across the Western Health and Social Care Trust, most notably as its Director of Performance and Service Improvement. She worked regionally as an Assistant Director at the Health and Social Care Board in Northern Ireland leading on the commissioning of cancer services and performance management. Sara will take up her role as Regional Executive Officer, HSE Dublin and North East on 15 April 2024.
Martina Queally

Regional Executive Officer
HSE Dublin and South East
Martina Queally has over 30 years health service leadership experience with particular expertise in strategic change management in public services and integrated service delivery. Since 2015, as Chief Officer in HSE Community Healthcare East, she has led the planning and delivery of all community health services in South Dublin and Wicklow, a range of national programmes, and a combined HSE and voluntary workforce of nearly 4,000 staff.
Martina has led a range of change, crisis and service transformation programmes; in 2011 as Integrated Services Area Manager for Dublin South East Wicklow she amalgamated three community health services and an acute hospital network, and in 2005 she led the establishment of the Local Health Office structure in Kildare and West Wicklow. Martina trained as a Registered General Nurse before qualifying as a Midwife and Public Health Nurse and she graduated with a MSc. in Heath Services Management from Trinity College Dublin in 2002. Martina has completed further study in areas of quality and service improvement and is a qualified executive coach and mentor.


Kate Killeen White






Regional Executive Officer
HSE Dublin and Midlands
Kate Killeen White will join HSE Dublin and Midlands from her role as Chief Officer for South East Community Healthcare where, since 2019, she had operational responsibility for delivery of all HSE community services in Carlow, Kilkenny, South Tipperary, Waterford and Wexford, leading a workforce of nearly 5,000 staff. She was previously Head of Service for Social Care in South East Community Healthcare, Chief Executive Officer of St Catherine’s Association disability service and practised as a Barrister from 2008 to 2013.
Kate has more than 16 years’ senior operational experience across health, regulatory and legal environments. With a strong academic background including Barrister-at-Law degree, Masters in Law, Executive Diploma in Governance and an Executive Diploma in Coaching, she brings a specialist knowledge of Health Law and Policy, Public Administration, Corporate Governance, Corporate and Commercial Law including corporate re-structuring and reform and change management strategies and principles to this important role.
HSE Dublin and North East will serve the people of Cavan, North Dublin, Louth, Meath and Monaghan.
HSE Dublin and South East will serve the people of Carlow, Kilkenny, South Tipperary, Waterford, Wexford, East Wicklow and parts of South Dublin.
HSE Dublin and Midlands will serve the people of Longford, Westmeath, Offaly, Laois, Kildare, West Wicklow and parts of South Dublin.
HEALTH MATTERS SPRING 2024 42 | Making progress on Sláintecare and integrated care
Tony Canavan







Sandra Broderick
Regional Executive Officer
HSE West and North West
Tony Canavan is the CEO of the Saolta University Health Care Group. He has worked in the health services in the West for over 30 years. Over that time he has held a number of appointments with the Western Health Board in Mental Health Services, the Department of Public Health, Primary Care Services and Acute Hospital Services. In 2012, he was appointed Chief Operating Officer of the first Hospital Group in the country, known then as the Galway Roscommon University Hospitals Group, which subsequently became the Saolta Group and was extended to include Letterkenny and Sligo. In 2015, he became Chief Officer of Community Healthcare West, before returning to the Saolta Group four years later as CEO.

Regional Executive Officer
HSE Mid West
A qualified nurse, Sandra has extensive experience in leading and delivering health and social care services in the UK and in Ireland. Sandra worked in General Nursing with the NHS in both community and acute services, and then moved into various healthcare management roles across the NHS including senior advisory roles within health and social care. Sandra has worked as a Bed Manager, Head of Site Operations, Senior Clinical Commissioner and Director of Nursing and she also held regional service improvement advisory roles.
Sandra returned to Ireland in 2018 to join the HSE as Assistant National Director for Older People Services. Sandra together with the people of the region, the Mid West workforce, local elected representatives and partner organisations will lead the region, build capacity in our services and improve access to integrated health and social care services.

Dr Andy Phillips







Regional Executive Officer
HSE South West
Welshman Dr Andy Phillips comes to the HSE from his role as Acting CEO of Safer Care Victoria, Australia. He has worked in clinical, operational and strategic executive leadership roles in healthcare for the past 37 years. Andy maintains his clinical qualification as a consultant clinical scientist.
Since 2009, Andy has been leading large scale health system transformation in Wales, New Zealand and Australia, with a passion for integrating health and social care. Andy has practised co-creating health and relationship centred healthcare for over 20 years, with recent work leading kindness and compassion in healthcare.
HSE West and North West will serve the people of Donegal, Galway, Leitrim, West Cavan, Mayo, Roscommon and Sligo.
“I want to emphasise that structural change is not the main goal of this reform. The idea behind reorganising our structures is to ensure that people experience just one health service, providing whatever care they need at the right time and in the right place. When we talk about ‘integrated care’, this is what we mean." - HSE CEO Bernard Gloster
| 43 HEALTH MATTERS SPRING 2024
on Sláintecare
Making progress
and integrated care
HSE Mid West serves the people of Clare, North Tipperary and Limerick.
HSE South West will serve the people of Cork and Kerry.

Wait time for children’s eye appointments significantly reduced by initiative
An eye care clinic recently completed a very successful waiting-list reduction initiative, which resulted in almost 1,600 people accessing an appointment.
The initiative was conducted by the Integrated Eye Care Centre for Ophthalmology in Ballincollig Primary Care Centre, Cork. Patients receive a high quality service using modernised equipment and
have access to a range of clinicians and specialities. A full multidisciplinary eye care team - including doctors, optometrists, orthoptists, nurses and administration staff - worked together to help reduce children’s waiting list times for ophthalmology appointments.
This work and other work under way in ophthalmology has significantly reduced

children’s waiting list times. The regional eye care centre is an integrated service and Cork Kerry Community Healthcare remains committed to working with their colleagues in South South West Hospital Group and South Infirmary Victoria University Hospital in the development of integrated eye care services; in line with Modernised Care Pathways.
Over 260 people attend new primary care centre daily
Ballincollig Primary Care Centre, one of the biggest in the country at 66,000 sq ft, opened with a flourish recently. It is part of the HSE Community Healthcare Network which covers Ballincollig, Bishopstown and Macroom - serving a population of 71,943. There are approximately 260 people attending Cork Kerry Community Healthcare service appointments each day at the facility, which is the local base for physiotherapy, occupational therapy, speech and language therapy, public health nursing, social work and home support
HEALTH MATTERS SPRING 2024 44 | Making progress on Sláintecare and integrated care
managers. There are also three GP surgeries based there.
Other HSE services working from the centre include:
• Cork Adult ADHD Tertiary Care Hub (CATCH)
• Ballincollig Sector Community Mental Health Team
• Specialist Neurodevelopmental ADHD Pathway (SNAP) Team
• CUMH outreach maternity clinic
• The Regional Eye Care service (Ophthalmology)
• Smoking Cessation
• Community breastfeeding support group led by the PHN service lactation consultant
Head of Primary Care at Cork Kerry Community Healthcare Priscilla Lynch said, “In 2024, we plan to improve links from services in the building with other services including Chronic Disease Management, the ICPOP team, Community Welfare Groups and our partners in Acute and Community Hospitals. Our overall aim is to make the transition from hospital to the community smoother for people who use our services."
New HSE Area Finder will help healthcare professionals secure the best services for patients
A new innovative online tool, HSE Area Finder, designed to support healthcare professionals to streamline patient care and enhance the quality of healthcare services is now live.
Aimed at healthcare professionals, HSE Area Finder provides a point of contact in primary care and community services, and assists with timely communication between community and hospital systems.
According to Dr David Hanlon, HSE National Clinical Advisor Primary Care, “By having this information at your fingertips, healthcare professionals can swiftly connect with the appropriate point of contact, ensuring that patients receive the care they need promptly.”
HSE Area Finder enables users to identify contact information for Community Healthcare Networks and for healthcare services such as Public Health Nursing, Community Specialist Teams for Older People and Community Specialist Teams for those dealing with Chronic Diseases.
Most recently, Area Finder has been extended to include generic contact details for the Children’s Disability Network Teams (CDNTs) across the country. Additional contact information will be added to the tool on a phased basis, for example Adult Disability Services and Mental Health Services.
HSE Area Finder is available for free and is accessible on any internet-enabled device: www.HSEAreaFinder.ie
Ambulances can bring some patients to injury unit instead of ED
The National Ambulance Service (NAS) and Roscommon University Hospital (RUH) have agreed a programme that will allow for some patients to be transferred directly to RUH Injury Unit if they meet strict criteria.
The programme which involves strict clinical and geographical criteria will see a small cohort of patients with minor injuries transferred by NAS to the injury unit for treatment.
Roscommon Injury Unit is an alternative to a busy ED, treating breaks, sprains, dislocations, burns and wounds. Staff take x-rays, apply plaster casts and treat wounds by stitches or
other means. They provide swift access to tests, can refer patients to specialist care and arrange follow-up appointments where necessary.
Under this new agreement, the NAS paramedics will also transfer patients with minor injuries to the unit. Patients that meet the agreed clinical criteria and live within the catchment area will be referred to RUH instead of an ED when it is safe to do so.
The pathway will result in patients receiving medical treatment in a hospital closer to their home and will release ambulances more quickly to respond to other emergency calls.
112/999 patients that do not meet these clinical criteria will continue to be transported to Emergency Departments for assessment and treatment.
Ann Cosgrove, Chief Operations
Officer with the Saolta University Health Care Group, which oversees RUH, welcomed the move. “This pathway involves a clear definition of patient groups who would benefit from such a referral. This is essential so that all healthcare professionals concerned, including paramedics and doctors, can be assured that we are bringing the right patients to the right location.”
Making progress on Sláintecare and integrated care | 45 HEALTH MATTERS SPRING 2024
Service keeping older people safely at home expands into Clare and Tipperary
A service that aims to safely keep older people who phone 999 in their home rather than bringing them to a hospital emergency department is now responding to calls in Clare and north Tipperary.
A partnership between the National Ambulance Service (NAS) and the UL Hospitals Group, Pathfinder launched in Limerick in October 2022 and has in recent weeks expanded its geographical area of operations across the Mid-West.
In its first six months in the Mid-West,188 patients were assessed by the regional Pathfinder team, of whom 47% were supported at home without the need to go to the ED.
One patient with direct experience of the Pathfinder service is Pa Buckley, 70, from Ballinacurra Weston in Limerick city, and who lives with a number of health conditions including asthma and chronic inflammation.
“I have been lucky enough to have the Pathfinder team out to me more than once and

With patient Pa Buckley at his home in Ballinacurra Weston, Limerick, were members of the Pathfinder team, from left, Niamh Ganley, senior occupational therapist; David O’Connor, advanced paramedic; Nicola Donohue, clinical specialist physiotherapist; and Claire O’Brien, clinical specialist occupational therapist
I think they provide a great service. I have a few health conditions so I am used to going in and out of hospital. I always get great care in UHL but, like everyone else, I would prefer to stay at home if I could avoid it,” he said.

Swift access to psychological support: Sláintecare in action
A psychological service has just celebrated 10 years in operation in Roscommon, where it has proven that continuous and sustainable access to community services can be provided with the right workforce in spite of limited resources – and without waiting lists.
When the HSE Roscommon APSI (Access to Psychological Services Ireland) began in 2013, no one had access to adult
HEALTH MATTERS SPRING 2024 46 | Making progress on Sláintecare and integrated care
Healthy Communities Project having a massive impact in north inner city
The success of any Sláintecare Healthy Communities Project is dependent on the level of trust and engagement between the community and the agencies that seek to provide services, according to Mellany McLoone, Chief Officer, Community Healthcare Organisation, Dublin North City and County.
The North East Inner City (NEIC) Sláintecare Healthy Communities Project: Impact Evaluation Report demonstrates the huge success that the project is having in Dublin’s inner city thanks to a high level of this necessary engagement.
It features many case studies illustrating its impact, including one participant, diagnosed with cancer, who explained that they were “close to shutting the door cause I was so hurt. They did more for me than anything. The staff member gave me inspiration to come back to life. Small steps maybe. It’s done me a world of good. To even know that they care for me. They rang me, texted me, listened to me. There are things out there to help. They put me on to little things - opened doors for me. Cause I didn’t have the mind to.”

Celebrations in North Inner City as Children from first class Central Model Infants’ School in Deverill Place, Dublin 1 celebrate the launch of North East Inner City Sláintecare ‘Healthy Communities Project: Impact Evaluation Report’: Phoebe Harcourt, Minister Paschal Donohue, Anas Jama, Minister Hildegarde Naughton and Safa Mohammed.
Noel Wardick, Chief Executive Officer, Dublin City Community Co-Op, said, “The Healthy Communities Project in the NEIC is proof that targeted and sustained investment, combined with passionate staff and a genuine multiagency partnership approach, bears fruit and transforms lives. The challenges in the NEIC may run deep but so too do the resilience, determination and humanity of its residents.”
psychological services in primary care. As a predominately rural county this meant many individuals were struggling in isolation.
“Since 2013, there has been a decade where the people of Roscommon have had swift access, within days, to evidence-based psychological support, local to where they live - at five different bases across the county - free at the point of contact,” explained Dr Pádraig Collins, Senior Clinical Psychologist.
“With over 4,400 separate individuals seen, close to one out of every 10 adults in the county, the depth of reach into the community has been significant. Consequently, it is a source of great satisfaction and hope that the clinical results demonstrate clearly that the majority who complete an intervention with us recover.”
Dr Michael Byrne, then Principal Psychologist, argued in 2013 that there was a compelling case for creating a ‘stepped-care’ service. This would mean individuals with milder presentations would immediately get low intensity input and those with more severe difficulties would be swiftly ‘stepped –
up’ to more intensive input.
Importantly such a model of a high volume of ‘low intensity’ input and a smaller volume of longer ‘high intensity’ input would both match the profile of need in the community but also ensure no waiting lists would be created.
By 2013 funding for a pilot stepped-care, primary care service was achieved and drawn down with a strong evaluation element built-in. In essence, at this point in time the HSE Roscommon APSI was born and service users throughout the county gained access to psychological intervention within days of referral.
As a primary care model it adheres strongly to the ideals of ‘the right care, in the right place, at the right time’.
The majority who entered the service with clinical levels of depression and anxiety and who completed a course of intervention left the service having clinical recovered. The ‘no waiting list’ model had worked, where in every area that a practitioner was employed service users were seen within days of a referral.
| 47 HEALTH MATTERS SPRING 2024 Making progress on Sláintecare and integrated care
Excellence Awards

Carol Desmond, Emma O'Kane, Maria Gibbons, Anne Marie Hoey, Sheree O'Brien and Fiona Callanan at the awards.
Lavender Clinic supports women who have undergone traumatic birth experience
The Lavender Clinic is a multidisciplinary team (MDT) clinic to support women following a traumatic birth experience at University Maternity Hospital Limerick (UMHL). It’s a weekly afternoon clinic held off-site, and since opening in April 2023 more than 50 women have been seen.
Leading the initiative is Maria Gibbons, Advanced Midwife Practitioner (AMP) and Dr Mas Mohamad, Consultant Psychiatrist of the Specialist Perinatal Mental Health Service (SPMHMS) at UMHL; Dr Naro Imcha, Consultant Obstetrician and Clinic Director of Maternal and Child Health, UL Hospitals Group; and Emma O’Kane, Clinical Specialist Physiotherapist. Those who meet the criteria for the referralonly clinic have access to obstetric debrief; physiotherapy assessment; birth reflection; and Birth Trauma Resolution (BTR) therapy; and liaison with a consultant psychiatrist.
“The Lavender Clinic initiative came about
"The Lavender Clinic is fully dedicated to moms and dads who have experienced trauma in their obstetric journey.”
from listening to our service users. The opportunity to be able to talk about their birth experience in a safe, protected space ensures that women and their partners will attend postnatal appointments and receive timely support, care and compassion from our integrated team of healthcare professionals,” said Maria.
The Lavender Clinic project won the national ‘Improving Patient Experience’ title at the recent HSE Health Excellence Awards, which honour examples of the great work across the health service, and encourage and inspire healthcare staff to develop and improve care and services for patients.
“We’re very proud of our HSE Excellence Award which will guide us in future planning of women-centred care and hopefully inspire our colleagues to showcase the wonderful work they are also doing every day,” she added.
Dr Naro Imcha said, “We owe our service users our gratitude for their feedback, which made it possible for us to initiate this project. The Lavender Clinic is fully dedicated to moms and dads who have experienced trauma in their obstetric journey.” HM
HEALTH MATTERS SPRING 2024 48 |
Awards
Awards

Rare disease holistic model of care reduces burden on parents
A team at Children’s Health Ireland team had undertaken complex care co-ordination for paediatric patients with the rare condition 22q11 Deletion Syndrome. The project involved integrating and co-ordinating medical, developmental and psychosocial services to ensure holistic care for the individual. They work closely with 22q Ireland.
Dr Suzanne Kelleher, Consultant Paediatrician, CHI Crumlin, explained, “In 2017, I set up a clinic for children affected with 22q1 Deletion Syndrome. It’s a very rare complex medical condition in that children are born with up to 180 different problems which can affect, for example, their heart, their palate, it can affect their learning, their mental wellbeing.
“In setting up the clinic, I linked up with Ann Lawlor, who is the chairperson of 22q Ireland and we discussed the multiple needs that this population have, particularly the need for co-ordinated care.
“Our Complex Care Co-ordinator has been in
Lorna Kerin, Veselina Gadancheva, Dr Yvonne MacAuley, HSE Board member Brendan Whelan, Dr Suzanne Kelleher, Anne Lawlor of 22q Ireland, and Wesley Mulcahy.
post for two years and this has made a huge difference to the running of the clinic. It means that instead of coming to Crumlin for multiple different appointments, that care can be co-ordinated on the same day. We can co-ordinate care in the community and it reduces the stress and burden on parents and extended families.”
Wesley Mulcahy, Complex Care Coordinator 22q, CHI Crumlin, added, “We pride ourselves in providing holistic functional wellbeing and health assessment for young people living with a myriad of complex needs. It involves complex case management, family liaison, engaging with multiple services and advocacy. It involves creating research, engaging with the users at the end of the healthcare to ensure that it’s appropriate. And we have a single point of contact for queries and questions.”
The initiative won the Excellence in Quality and Patient Safety Award at the HSE Health Excellence Awards. HM
| 49 HEALTH MATTERS SPRING 2024
HEALTH
Awards

Award-winning Transforming Theatre Programme reduces surgical waiting lists
“The true reward of everyone’s collective efforts is reflected in the increased number of patients who have already benefited and will continue to benefit from the improvements driven by our staff every day,” according to Grace Reidy, Transforming Theatre Programme Lead, South/South West Hospital Group (SSWHG).
The Transforming Theatre Programme was an 18-month pilot programme developed in response to long waiting lists for surgical care. It was a collaboration between the HSE, the Royal College of Surgeons Ireland (RCSI), the SSWHG, and the National Clinical Programmes for Surgery and Anaesthesia.
The project recently won the Innovation in Service Delivery award at the HSE Service Excellence Awards. In September, the project won the European Innovation Award 2023, presented by the European Association of Hospital Managers at an event in Luxembourg.
Prof Mark Corrigan, Clinical Lead, Transforming Theatre Programme, SSWHG, said, “Working on this programme has been an immense privilege. “It has personally allowed me to witness the remarkable transformation achieved by
Charlie Dineen, Karen McCarthy, Julie McCarthy, Sarah Dwan, Aisling Lehane, Grace Reidy and Plaxcedes Jeche, HSE Board member Matt Walsh, Martina Sheehy, Deborah McNamara, Mark Corrigan, Tess Traynor, and Celia Lane.
empowering our staff across 10 hospitals and 56 operating rooms. Their skill in identifying and driving improvements is exceptional.”
The programme uses an integrative approach to improve patient flow through the operating theatre. Theatre teams from each hospital in SSWHG were trained in Lean methodology to implement change across their perioperative service. It supported the hospitals to maximise their theatre resources as efficiently as possible.
The impact of the programme is evident, with improved operating theatre effectiveness across SSWHG. In the first six months of 2023, used theatre time increased by 1,363 hours, and 1,775 additional patients were seen compared to the same period in 2022.
Due to the success of this project, the programme has now been extended and will be rolled out nationally as the National Perioperative Patient Pathway Enhancement Programme. The programme is a collaborative initiative, nationally coordinated by the HSE Strategic Programmes Office, and is currently being rolled out in two hospital groups: Dublin Midlands Hospital Group and Saolta University Healthcare Group. HM
HEALTH MATTERS SPRING 2024 50 |
Awards
HSE Excellence Award for app that improves patient flow
An app-based project in the north west that improves patient flow with real-time data on bed use is delivering efficiencies for the health service, while improving patient flow.
The team involved explained that “with those working in HSE Community Healthcare Organisations right across the country needing to have a detailed picture of the current use and occupancy rates of hospital beds, to optimise and better manage their availability for medical care and hospitalisation, this project delivered an app that rapidly provides that capability in an integrated and innovative way.”
Frank Morrison, Head of Service, Older Persons Service, Community Healthcare Cavan Donegal Leitrim Mayo Sligo (CH CDLMS), explained that the project commenced in 2022.
“Prior to this, we mainly depended on a manual paper process which in itself brought many challenges. For example, the lack of appropriate and adequate data, the timeliness of people giving back replies, sometimes it could take up to a calendar month for data to arrive. That
made planning very, very difficult,” he said.
Aisling Gannon, General Manager, Digital Health Team, CH CDLMS, said initially the older person service approached her team looking for an ICT system.
“But after several discussions, we identified this was a digital transformation project looking at improving data management for capturing their bed utilisation. We worked with them to transition their bed register from Excel spreadsheets to intelligent digital solutions,” she said.
Melissa Kelly, Acting General Manager, Older Persons Service, CH CDLMS, added, “The bed app enables us to track bed occupancy over time, identify bed usage patterns and optimise bed usage in each of the units. The bed app has been readily adapted by our staff, saving them time to focus on patient care and other essential tasks.”
The initiative recently won the Engaging a Digital Solution to Provide a Better Service Award at the Health Service Excellence Awards. HM

| 51 HEALTH MATTERS SPRING 2024
Maria Burns, Sam Wallace, Frank Morrison, Stephen Mulvany, Aislinn Gannon, and Melissa Kelly pictured with the award.
M aking E very C ontact C ount
The important role of local champions in Making Every Contact Count

One of the key recommendations from the recent research on Making Every Contact Count (MECC) as effective as possible points to the crucial role of local champions ‘to model best practice and share experiences’ of MECC.
The work of MECC champions is really progressing in Dublin North City and County (DNCC), with another 43 champions recruited for 2024. This is building on work in this area last year, where an intial 35 champions were recruited for the first time. A champion’s role is to promote, support and mobilise the implementation of MECC. All
champions are supported by their Network Health Promotion and Improvement Officer.
The work of the champions in DNCC supported furthering the implementation of MECC through different initiatives. This included training an additional 301 staff and supporting the establishment of a ‘Peer Champion Network’.
A Lifestyle Series pilot was developed with healthcare professionals in Grove Court and Hartstown Health Centre. The aim of this pilot was to promote and encourage health care professionals to complete all MECC eLearning modules. Each
"The event provides an opportunity to build on, to share experience, develop professional practice and provide a
creative space in tackling new challenges."
month a different MECC lifestyle topic was linked to an event or activity. For example, to promote the completion of the Tobacco Free module, a Mindful Breath Workshop was organised, funded by the Tobacco Free Campus bursary. Some 26 healthcare professionals attended this session and completed this module.
The second champion event for DNCC will take place in St Marys Hospital, Phoenix Park in March. The aim of the event is to continue to promote, support and mobilise the implementation of Making Every Contact Count. The event provides an opportunity to build on, to share experience, develop professional practice and provide a creative space in tackling new challenges. HM
Visit HseLanD for Making Every Contact Count training information or email makingevery.contactcount@hse.ie for further information.
HEALTH MATTERS SPRING 2024 52 | Feature
Making a diff erence
New lactation specialist making a difference to breastfeeding mothers
This specialist post is to provide expert antenatal and postnatal breastfeeding support and education in MUH.
“In my role as Clinical Midwife Specialist in Lactation in MUH I see lots of mums who experience various challenges with breastfeeding, especially in the early hours and days. There can be issues with position and attachment, some mums can find it difficult to breastfeed after a caesarean section, others can have concerns about milk supply and need reassurance.
Breastfeeding is a learned skill and takes patience and practice and this is where my role becomes important as I can give that skilled help, support and follow up in those early days in hospital,” she said.

Ashling Neary from Castlebar is Mum to baby Lilly, aged seven months. Speaking about the support she received in her breastfeeding journey Ashling said, "Breastfeeding my first child was always something that was very important to me, I didn't expect that we would have such difficulty.
“I met with Mary before I was discharged and I came back a few days later to meet with her for advice and guidance. She really helped put me at ease and made exclusive breastfeeding possible for us.
“Lily was born on the 17th of February and due to a difficult labour I was unable to breastfeed or even get her to latch for days. I had given up on this happening for us. I had to stay in hospital one extra

night due to a blood transfusion and thank goodness I did because the next day I met Mary Sammon, who was invaluable.
“I met with Mary before I was discharged and I came back a few days later to meet with her for advice and guidance. She really helped put me at ease and made exclusive breastfeeding possible for us. Lily was five days old when we got her to latch and feed. Without Mary and the support she provides it would not have been possible for us. We have also engaged with the local lactation consultant Claire Larkin who holds several groups during the week supporting new mums across Mayo.
“I would encourage any new mum who is struggling, to reach out to the supports that are in place.” HM
| 53 HEALTH MATTERS SPRING 2024 Feature
Mary Sammon has been looking after mothers and babies in the Mayo University Hospital (MUH) Maternity Unit as a midwife for 27 years but has just become its first Clinical Midwife Specialist in Lactation.
Making our services better
A look at some of the many initiatives
taking place across the HSE
Change Framework: Defining, designing and delivering frontline improvements
Across the services staff are influencing much-needed change and addressing challenges by adopting a person-centred approach. This is evident in the wide array of poster presentations we see our colleagues present each year. This important work brings experience-led creative thinking to designing new systems. Embracing a collective approach offers a special opportunity to address very real health and wellbeing challenges while piloting new practices, processes and systems.
Here we share three case studies from the Change and Innovation Hub on www.hseland.ie that offer value to the services we deliver and reflect great strides in improving patient/service user outcomes and experiences.
"The project aim was to connect GP services and the primary care team and to develop a more efficient process to manage referrals."
In each case the change was framed using define, design and deliver guidance from the Health Service Change Framework.
The project aim was to connect GP services and the primary care team and to develop a more efficient process to manage referrals. The Healthlink platform enables GPs refer patients in need of the five essential health and social care professional services (HSCPs) of nursing, physiotherapy, occupational therapy, speech and language therapy, and dietetics to a Primary Care Team. It is recognised as a key enabler for the integration between GPs and CHNs.
Eimear’s team used the Change Framework poster template to clearly define the project. This helped to communicate the operational readiness, set out the steps to reach that readiness and co-design the most appropriate process.
Optimising Prescribing Together Senior Pharmacist, Leon O’Hagan, investigated the ‘Prevalence of
‘Introducing the Healthlink Referral Form in Community Healthcare Network 2Rathmines, Terenure and Templeogue’ was presented by Eimear Noonan, Community Healthcare Network Manager (CHNM).
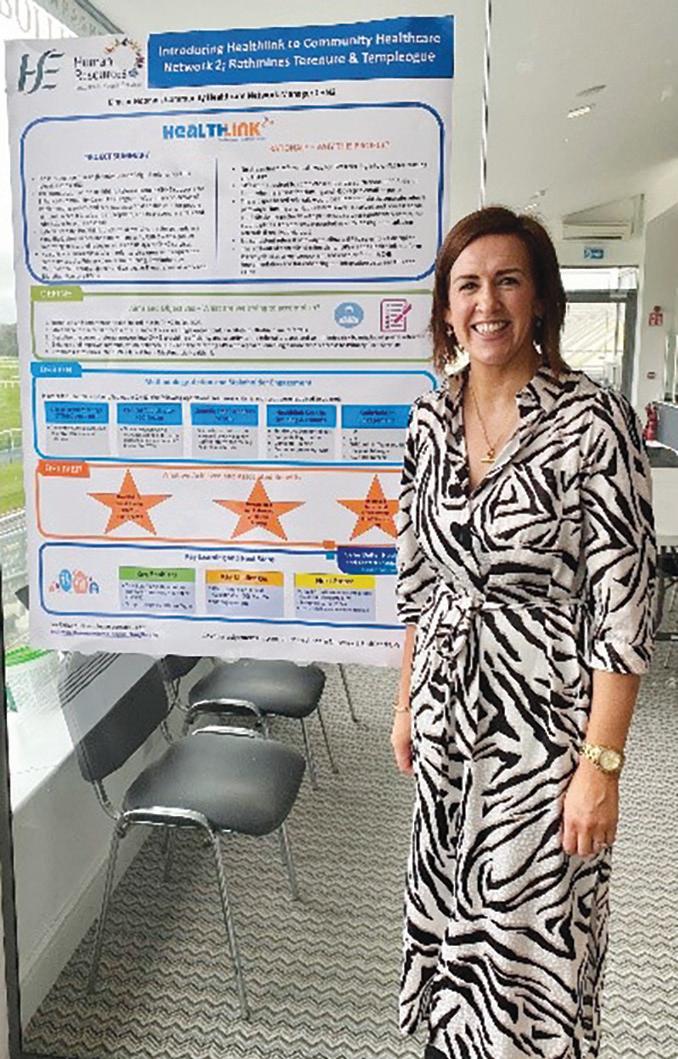
Prescribing High Anticholinergic Scoring Medications Amongst over 65-year-Old Patients in Primary Care’.
It is generally advisable to use anticholinergic drugs with caution in the elderly population as an anticholinergic score of three or more is associated with an increased risk of confusion, falls and death.
In defining his project, Leon recorded the 48 most commonly prescribed medicines in the service and checked them on www.acbalc.com. This website provides a comprehensive list of medicines with an anticholinergic burden score of 3.
As a result of this research project, the service determined that patients who have a high anticholinergic score should have their medicines optimised through a shared decision-making framework, to ensure current therapy is beneficial. Using the Health Services Change Framework poster presentation template enabled Leon to clearly communicate his approach to defining, designing and delivering this change for the service.
HEALTH MATTERS SPRING 2024 54 |
working
Better ways of
Better ways of working

St Finbar’s Ward, Galway University Hospital’s Clinical Nurse Manager 1 (CNM1), Catherine Keane, presented her work to address a change improvement ‘To Evaluate Nursing Compliance with Malnutrition Screening Tool (MST) on the Orthopaedic Trauma Ward’
Catherine and her team conducted an audit on the orthopaedic trauma ward in January 2023. The result revealed that patients were not routinely being screened for risk of malnutrition. The team then included a nutritional MST screening assessment into the process to establish a patient’s baseline. This assisted with the identification of patients who are at risk or those who are malnourished.
Effective communication with staff nurses regularly was essential to this quality improvement initiative. Staff empowerment was endorsed by encouraging education. Teamwork and regular communication provided an opportunity for essential feedback. Using the Change Guide resources prompted a focus on team communications and this proved key to this change initiative. HM
"Using the Health Services Change Framework poster presentation template enabled Leon to clearly communicate his approach to defining, designing and delivering this change for the service."
Webinar can kickstart your patient safety journey
Do you want to expand your quality and patient safety knowledge in 2024?
Register for QPS TalkTime webinars to hear from national and international industry experts and colleagues improving quality and patient safety in our health service. QPS TalkTime can help you kick start your work to improve patient safety by hearing about similar projects and incentives taking place across Ireland and abroad and the latest information on the major causes of harm. Our fortnightly webinar series is free to join. Listen by yourself or join or start a group locally. It aims to connect likeminded people interested in QPS and provide a platform to share learnings and experience to better our healthcare service.
For more information visit
https://www.hse.ie/qps-talktime Follow us on X / Twitter: https://twitter.com/ QPSTALKTIME
Watch back on previous episodes: https://bit.ly/QPSTalkTimeYouTube-playlist

To read more Case Studies of change and improvement such as these visit the Change and Innovation Hub at www.hseland.ie
To access Change Guide resources visit www.hse.ie/changeguide
| 55 HEALTH MATTERS SPRING 2024
Leon O’Hagan
Better ways of working
Antenatal Educators Programme
A new HSE National Education Programme for Antenatal Educators has been piloted with midwives from around the country, who will in turn provide training to antenatal education peers on future programmes.
Professor Mary Nolan from the University of Worcester initiated the pilot in October.
The programme content draws from a draft transition to parenthood programme curriculum, commenced by Professor Nolan and the HSE’s Cathy O’Sullivan following the launch of the HSE National Standards for Antenatal Education in Ireland (2020).
Following the COVID-19 pandemic, in 2022 the Office of the Nursing and Midwifery Services Director and the National Women and Infant Health Programme collaborated to complete the work. The passion and expertise of both Mary and Cathy, together with their firm belief that antenatal education is the cornerstone in the preparation for childbirth and parenting for most parents, is consistently evident and interwoven throughout the new Programme.
Ten staff from Dublin, Kerry, Sligo, Waterford, Portlaoise and Galway gathered for a one-and-a-half day workshop with Mary. She supported participants to try out new antenatal education activities with a view to understanding both why the content of the activity was important, and how to facilitate it in such a way that parents acquire new knowledge, skills and attitudes. The baby’s relationship with his or her parents was

central to the workshops as this should be the core of all antenatal education sessions.
She emphasised the need to actively engage fathers in antenatal education from the start of their transition to parenthood as antenatal education is the only kind of parent education in which men are likely to be involved in large numbers in.
After a very hard-working, hugely enjoyable and excellently evaluated two days, participants are now preparing to provide the NMBI Category One approved three-day programme to their peers in antenatal education around the country. The first programme will take place in March 2024 in the Centre for Midwifery Education, located at the Coombe Women and Infants University Hospital. Regional Centres for Nursing and Midwifery Education will co-facilitate the programme with their local antenatal educator colleagues at various dates throughout 2024 and beyond. HM
For more information please contact Margaret Quigley, National Lead for Midwifery, ONMSD Margaret.quigley@hse.ie
Become a ‘citizen epidemiologist’
The HSE’s Health Protection Surveillance Centre (HPSC) has created a new system to provide easy access to the latest statistics reported on notifiable infectious diseases in Ireland.
Principal Epidemiologist at the HPSC, Dr Patricia Garvey explained that one of the main roles of HPSC is to provide information on infectious diseases so that outbreaks can be picked up quickly to help prevent
further spread of disease.
“This new system will allow HSE staff, and members of the public, to become ‘citizen epidemiologists’ and to keep informed and up to date on trends and updates in relation to infectious diseases in Ireland. Previously, HPSC produced data in PDF reports. However, now it will be possible for the first time to view interactive data for 80 infectious diseases, making it easy to explore the information over a five year period.
“Since the COVID-19 pandemic
people have become much more aware of infectious diseases and our new data hub will be a valuable resource for HSE colleagues and for the public.
The Data Hub is an advancement in the way HPSC displays the data we collect. It is an extra tool to use alongside HPSC’s existing outputs. It will inform and guide health service prevention, preparedness and response to protect the Irish public from infectious diseases,” she said. Explore the data at: https:// notifiabledisease.hpsc.ie/
HEALTH MATTERS SPRING 2024 56 |
Professor Mary Nolan (top centre) actively engaging participants at the workshop
Better ways of working
Updated Emergency Multilingual Aid now available
The multilingual phrasebook with visual aids in 18 languages is now available to order for free from healthpromotion.ie.


























































Roscommon Injury Unit appoints new RANP in Emergency Nursing



































Roscommon University Hospital is delighted to announce that Eoin McGinn has recently been appointed as Registered Advanced Nurse Practitioner (RANP) in Emergency Nursing at Roscommon Injury Unit.























The updated Emergency Multilingual Aid supports healthcare staff to communicate with people who don’t speak English as a first language.
It is quick, accurate and easy to use. It covers common medical questions and terms, and helps staff make an initial assessment in an emergency situation while waiting for interpreter services.
Developed by HSE clinicians in conjunction with NGOs and services users, this resource draws on best international examples adapted to an Irish context. It is intended for use prior to requesting the services of an interpreter or while awaiting the interpreter's arrival in emergency situations. The guide is not intended to replace the services of an interpreter.
Dr Ciaran Browne, HSE National Lead for Inclusion Health Acute Operations explained, “Patients presenting in acute or emergency situations can sometimes have difficulty communicating their symptoms in English. The roll out of this Emergency Multilingual Aid is one measure taken by the HSE to improve access to health and care services.”
The resource supports frontline staff to engage with patients who may face language barriers when arriving at an emergency department or maternity hospital. The aid includes visual cues and language identification card to assist in assessments.
Ruth Armstrong, Project Manager, National Social Inclusion Office, added, “The Emergency Multi Lingual Aid is quick, accurate and easy to use. It covers common medical questions and terms to support frontline staff make an initial assessment while awaiting interpreter services.” HM
The Emergency MultiLingual Aid is available at healthpromotion.ie.
RANPs are the highest level of clinical experts in the nursing profession in Ireland today and are transforming services for patients through an expanded scope of practice, greater clinical autonomy and decision-making.
The creation of ANP posts across the Saolta Group is transforming services for patients not only in hospitals, but in the community and in the home through an expanded scope of practice for highly skilled nursing professionals, greater clinical independence and decisionmaking. Ongoing education and research as well as mentoring of nursing colleagues are also key parts of the role. Claire Conlon, Interim Hospital Manager said, “I am delighted to welcome Eóin to his role in the Injury Unit. Advanced Nurse Practitioners are transforming services for patients. With seriously ill patients prioritised for treatment in our Emergency Departments, injury units are a vital resource for maximising efficient patient flow and minimising wait times for patients.”
Newly appointed Registered Advanced Nurse Practitioner at Roscommon Injury Unit, Eóín McGinn.
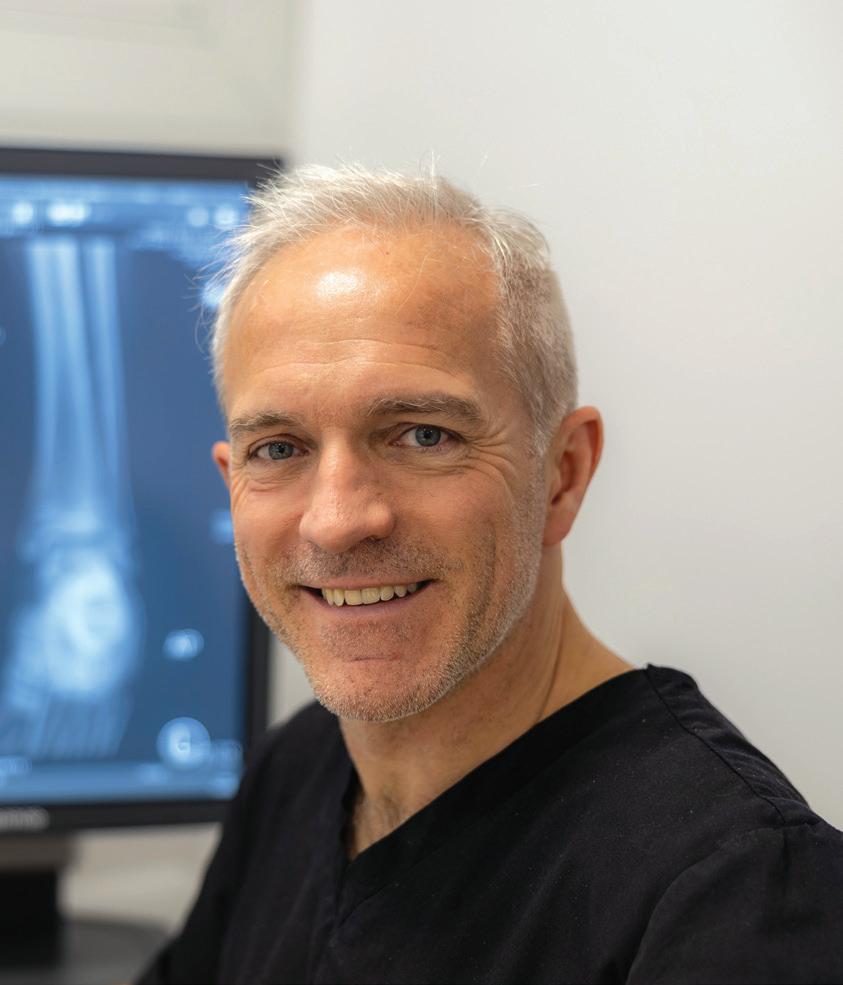
| 57 HEALTH MATTERS SPRING 2024
01 Emergency Multilingual Aid ENGLISH / ARABIC A multilingual, illustrated communication phrasebook, for use by patients and staff
Better ways of working

A first for Saolta’s Children’s Nursing graduates
Seven new Children’s Nursing Specialists graduated from an innovative postgraduate programme developed by Saolta in conjunction with Trinity College Dublin and Children’s Health Ireland last year.
The newly qualified specialist nurses are based in Letterkenny University Hospital, Sligo University Hospital, Mayo University Hospital, Galway University Hospitals and Portiuncula University Hospital.

This programme is unique in that it delivers a blended learning model with remote and in-person lectures, and is the only pathway which allows postregistration nurses to pursue a Higher Diploma in Children’s Nursing without undertaking a course based in Dublin.
Lorna Middleton, Specialist Children’s Nurse in Sligo University Hospital is presented with a graduation medal by Saolta Chief Director of Nursing and Midwifery, Paul Hooton
Children’s healthcare services are facing everincreasing demands due to the evolving profile of children’s healthcare needs. The number of Children’s Nurses qualifying is low in comparison with other disciplines and this programme was born from a need to ensure Saolta’s nursing teams continue to have the highest level of skill, qualification and training to care for our younger population. Saolta are now training specialist Children’s Nurses in the west and north west of Ireland and have the opportunity to expand the number of registered Children’s Nurses available to care for children across our acute and community services. HM
The programme will be open to new applications shortly, for more information email Karen Grennan (Karen.Grennan2@hse.ie)
Patient Service User Experience: partnering with service users
The objective of the HSE Patient and Service User Experience (PSUE) team is to facilitate partnering with patients, service users, family members and carers in the planning, design, development and improvement of services at strategic and policy level.
Led by HSE Assistant National Director, Iolo Eilian, the PSUE team works very closely with the HSE National Patient and Service User Forum which is Chaired and CoChaired Independently to the HSE. Its membership has representatives of advocacy organisations, disability organisations, patient groups, individual patients, family members and carers.
A key current PSUE focus is also the implementation of the ‘Better Together Health Services Patient Engagement’ roadmap. The team has had a number of learning and information sessions around patient engagement with HSE teams and other countries including Scotland and Northern Ireland. Other sessions are planned with the UK, New Zealand and Australia. The sessions with key health service teams include HSE national screening service and the National Office of Clinical Audit. You can contact Iolo Eilian and the PSUE team at Patient. Parnership@hse.ie

Members of the Patient Service User Engagement team with patient partners and HSE national director Operational Performance Integration, Joe Ryan: Mila Whelan, Kara Madden, Laura Kavanagh, Joe Ryan, Anne Lawlor, Julia Barry and Nicola Williams.
HEALTH MATTERS SPRING 2024 58 |
Seven nurse specialists graduate from Saolta’s first hybrid postgraduate Children’s Nursing Diploma in conjunction with CHI and Trinity College Dublin. From left, Amy Gannon, Helen Rooney, Faith Zinyemba, Agnieszka Maria Kuczewska, Lorna Middleton and Soumya Assariparambil Renjan. (Absent from the photo is Cáit Costello)
Better ways of working
NCCA launches Clinical Audit Toolkit
The HSE National Centre for Clinical Audit (NCCA) has produced a Clinical Audit Toolkit, a powerful tool that empowers healthcare professionals to conduct meaningful clinical audits and drive continuous quality improvement.
The NCCA has had a comprehensive work programme aimed at assisting staff to carry out clinical audit in their own health or social care setting. Building on the existing work and listening to staff feedback, the NCCA are pleased to share the Clinical Audit Toolkit.
The toolkit is a valuable resource developed by the NCCA to support healthcare professionals in conducting effective clinical audits, with the ultimate goal of improving healthcare quality and patient outcomes.
Key features of this toolkit are its user-friendly interface and customisable templates which include a clinical audit proposal form, report template, quality improvement/action plan template and template for local clinical audit committees. The template can be accessed: https:// www2.healthservice.hse.ie/ organisation/ncca/clinical-audittoolkit/
Further work is planned to support local clinical audits, such as supporting the Irish Clinical Audit Network, development of ICT supports for clinical audit and sharing audit tools. From a national perspective, the NCCA wish to ensure there is a National Programme of Prioritised Clinical Audits with appropriate resources.
Majella Daly has been appointed new Assistant National Director for the NCCA. In her most recent position as Head of Service for Disabilities in CHO4, she has experienced first-hand the challenge of ensuring standards are being met while there are ongoing challenges with staffing levels, and other enablers such as ICT infrastructure, knowledge and time for clinical audit. HM

Members of the Stronger for Surgery team Joanne Coffey, TUH Communications Manager; Dr. Valerie Twomey, Head of Psychology at TUH; Siobhán Power, Clinical Specialist Dietitian for Perioperative Services; Maria Whelan, Consultant General and Colorectal Surgeon; Laura Hammond, Senior Physiotherapist; Dr Natalie Cole, Head of Innovate Health at TUH.
Absent from picture Úna Delahunt, Health Promotion and Improvement Officer.
TUH launches innovative programme to help patients prepare for surgery
A series of short videos with key advice for patients scheduled to have surgery has been produced by Tallaght University Hospital (TUH). Malnutrition, frailty and cigarette smoking are all risk factors for poor outcomes after surgery. The materials have been developed as a way to educate and empower patients to reduce these very changeable risk factors.
Waiting for surgery can be a stressful time for patients, having access to these materials clearly outlines things they can do, turning waiting time into preparation time, giving patients better results during and after surgery.
The weeks and months leading up to surgery are a great time for patients to get their minds and body prepared so that they can recover quickly afterwards. The series focuses on some of the most important ways patients can help themselves.
Consultant General and Colorectal Surgeon Maria Whelan explained, “Surgical prehabilitation is a way to prepare physically and mentally to meet the challenge of surgery. It has been shown that following a surgical prehabilitation programme reduces the risk of developing complications such as chest infections and wound infections.”
The materials will be accessible from the Department of Surgery page on the hospital website, www.tuh.ie, the Hospital YouTube channel with QR codes included in letters to patients about their scheduled surgery.
Funding for the initiative was made available via the HSE Spark Ignite Programme which is supported by the National Quality Improvement Team, the Nursing and Midwifery Services Director and the National Health & Social Care Professions Office.
| 59 HEALTH MATTERS SPRING 2024
Better ways of working
Directory of Services to assist older people to live well at home
HSE Midlands has launched a directory of services with information to assist Older People in Laois/Offaly live well at home.
A working group comprising HSE, other statutory agencies, community and voluntary partners developed the directory with the aim of linking existing cross-sectoral communitybased assets.
Local consultation with older people across Laois and Offaly informed the contents and design of the directory. Engagement with older people found loneliness to be a real problem in rural areas and there was an identified need to signpost opportunities for supports, resources and ways to form better social connections.
The directory provides information and contact details for services available to keep older people well at home, as well as information of who to contact when they need health or social care services.
Information on issues that matter to people are included such as transport and entitlements, information on how to access supports such as day care or lunch clubs and it lists groups and activities available across both Laois and Offaly to connect people socially with a full chapter on ‘Social Leisure and Educational Activities’. It also provides information on the HSE social prescribing service and cites the contact details for social prescribers in both Laois and Offaly. The directory is available from health care front line staff, and in public offices and can be downloaded on www.hse.ie
Emma Ganoud, Acting Head of Service Older Persons Services; Dr Mary Doolan, Operational Lead Integrated Care Older People; Anna May McHugh, Managing Director, NPA; and Molly Buckley, Age Friendly Council Representative.

Falls prevention booklet launched in Community Healthcare East
HSE Community Healthcare East recently launched a new booklet to help those at increased risk of a fall to learn more about preventing falls.
A recent Major Trauma Audit (MTA) in Ireland highlighted that low falls (falls of less than two metres) are the leading cause of trauma in our hospitals. As we get older we are more at risk of falling and the majority of falls occur at home. Feeling unsteady when standing or walking can also increase the risk. Many falls are preventable, and simple steps such as making our home environment safer and keeping steady and strong can help.

The booklet entitled ‘Take Control: Reduce your Risk of Falls’, is available to download by scanning the QR code. HM
For more information contact Alison Wellwood, Falls Co-ordinator for Older Persons Services, CH East at alison.wellwood1@hse.ie
Pulmonary Rehabilitation Programme participants in Bray take on a ‘Step Challenge’ for World COPD Day
Pulmonary Rehabilitation Programme participants in Bray marked World COPD Day by taking on the Step Challenge last November. Participants took part in a penalty shootout, bowling, balance and multi-task games, a seated obstacle course challenge and a baton pass. Along with their respiratory physiotherapy team and nurses, those taking part surpassed the target Step Count of 380,000 and reached a massive 472,325 steps! Well done to all involved!







HEALTH MATTERS SPRING 2024 60 |
Pulmonary Rehabilitation Programme participants and staff enjoy taking on the Step Challenge to mark World COPD Day
Children’s Disability Network Teams facilitate 26 Family Forums in first year
An initiative of the reconfiguration of the Children’s Disability Network Teams (CDNT) was to establish Family Forums which offer families an opportunity to discuss general issues and ideas about the service they avail of with senior managers. Family Representatives are elected to sit on the Governance Group responsible for the delivery of services from the Family Forums.
Since 2022, a total of 26 Family Forums and seven Family Representative Group meetings have been held in Community Healthcare East which also saw parent representation elected to the Governance Group which comprises of the lead and partner agencies.
Families working with the CDNTs across the country have said they want to see improvements in delivery of services, have a voice and be heard by management and decision makers. Family Forums have provided a means to build positive relationships, improve communications and transparency, build partnerships, value lived perspectives and provide opportunities for co-design and feedback between families and management.
Key themes expressed by families were: challenges with interagency collaboration, need for improved communication, challenges in recruitment and retention, and extensive waiting lists. These themes have been incorporated into the CDNT Strategic Plan for the delivery of services in 2024. HM

Better ways of working
Infection Prevention and Control Link Practitioner Programme delivered in South East
Throughout the month of February, the HSE delivered an intensive five-day Infection Prevention and Control Link Practitioner Programme for staff of private nursing homes and disability services organisations in the South East.
The building of capacity within community health and social care services to identify and manage Infection Prevention and Control risk is a key priority for the HSE and its Quality, Safety and Improvement Team in its South East Community Healthcare organisation.
A total of 24 private nursing homes in counties Carlow, Kilkenny, South Tipperary, Waterford and Wexford and four disability care organisations completed the programme, in its first delivery in a community setting in the South East.
Following this training, recognised Infection Prevention and Control Link Practitioners (IPCLPs) will act as a local resource and role model for their service, whilst also being supported by a wider network of HSE Community Infection Prevention and Control Clinical Nurse Specialists.
The Infection Prevention and Control Link Practitioners (IPCLPs) role is designed to support service providers to implement effective Infection Prevention and Control practices in their facility or service.
Speaking following a programme session in the Hoban Hotel, Kilkenny, Mary Clare Hayes, Assistant Director of Nursing/Infection Prevention and Control, HSE/South East Community Healthcare, said, “Where actively engaged and with the support of their management, IPCLPs have over the past three years proven to have a valuable role in supporting their entire health and social care team to provide safe, quality care to service users in a wide variety of community health and social care settings. IPCLPs act as a local resource and role model for their service whilst also motivating their colleagues to improve infection prevention and control practices.”
| 61 HEALTH MATTERS SPRING 2024
Caption: Some of the Family Representative Group elected members at a recent meeting: Kasha Huse, David Rolland, Renaith Keane, Cathy Magee, Dorota Zurek and Chris Keogh.
BreastCheck opens new screening location in north Cork city
A new BreastCheck breast screening unit opened in Cork city in January to serve women from the north side of the city and county. The additional unit means that eligible women are now being offered breast screening at one of three locations in the city. The new location is on the grounds of St Mary’s Orthopaedic Hospital, Baker’s Road, Gurranabraher, Cork. The new unit is fully accessible and there is free parking.
BreastCheck Programme Manager Suzanne Lynch said, “It is our aim to have as many women as possible choose to come for breast screening. This means addressing as many barriers to screening as we can. We know that access can be a barrier and we hope that our new unit on the grounds of St Mary’s Orthopaedic Hospital will make screening more accessible to women living on the north side of Cork city and county. We are grateful to St Mary’s Orthopaedic Hospital for hosting us.”
The two existing screening locations in Cork are:
• BreastCheck Southern Unit, Infirmary Road, Cork
• The grounds of St Finbarr’s Hospital, near Block 23, Douglas Road, Cork
BreastCheck, the national breast screening programme, invites women aged 50 to 69 to choose to come for breast screening every two years. The programme reminds all women in that age group to check that they are on the BreastCheck register at www.hse.ie/breastcheck.

Professor Aidan Flynn, Consultant Cardiologist; Andrea Cooke, Cardiac Physiologist; Carol Glynn, Healthcare Assistant; Caroline Hanniffy, Cardiac Physiologist; Claire Mc Dermott, Chief II Cardiac Physiologist; Ann Donohue, Cardiac Physiologist; Dr Núria Farre, Consultant Cardiologist; Niamh Corrigan, Cardiac Physiologist; and James Keane, Hospital Manager.
NCCP launches updated prostate guide for patients
An updated guide called ‘Having your Prostate Checked: A Guide’ is now available at healthpromotion.ie.
The guide is for anyone who is thinking about having their prostate checked.
Prostate cancer is the most common cancer diagnosed in males in Ireland. Over 3,300 men are diagnosed with prostate cancer each year and it is the second most common cause of cancer death in men in Ireland. Almost 1 in 3 of all invasive cancers in men in Ireland are due to prostate cancer.
The National Cancer Control
Programme (NCCP) guide provides information on prostate issues. It also highlights the importance of shared decisionmaking when having a prostate check.
A prostate check can include:
• questions about your health
• a Prostate Specific Antigen (PSA) blood test
• having your prostate examined
Printed copies of ‘Having your Prostate Checked: A Guide’ can be ordered free of charge or downloaded from healthpromotion.ie.
Portiuncula’s Echocardiography Department receives European Accreditation
Portiuncula University Hospital has recently received European accreditation for the Echocardiography Department by the European Society of Cardiology (ESC) following a process of quality standards and improvements. The European Association of Cardiovascular Imaging (EACVI) established a European Echocardiogram standard in laboratory practices and patient care. The aim of laboratory accreditation is to raise quality standards of practice and equipment across Europe in a uniform manner. It is also designed to be used as an educational tool to improve the overall quality of Cardiac Investigation departments.
Portiuncula University Hospital is the third Hospital in the country to be accredited by the European Association of Cardiovascular Imaging.
Claire McDermott, Chief II Cardiac Physiologist said, “I am delighted and extremely proud of our team here in the Cardiac Investigations Department for having achieved such a highly regarded world recognised accreditation. We now have certification for five years, which would not have been possible without the commitment and dedication of such a fantastic team.
"It is an exciting time for our department as we continue to focus on quality improvement, embrace new methods of working, new technology, and more integration to ensure we continue to provide our patients with the utmost care.”
HEALTH MATTERS SPRING 2024 62 | News
Support for stroke patients
Mayo University Hospital launched a book containing resources and supports for stroke patients and their families. The book, called My Stroke Journey, is a 67-page guide to all aspects of this life-threatening condition, developed by the multi-disciplinary stroke team in MUH in collaboration with patients.
The book is designed to help stroke survivors and families to understand and manage their diagnosis during their admission to hospital and also directs patients to the supports available in the community on discharge from hospital.
My Stroke Journey includes general information on stroke, types of stroke, treatments and hospital stay, how stroke may affect a person, how to manage your stroke lifestyle and medical risk factors and discharge planning. It also includes a directory on local and national supports available to stroke survivors, their families and carers. In the book, patients will find important checklists and questions to ask healthcare professionals about their stroke.
Speaking about the development, Niamh Kelly, Senior Occupational Therapist in MUH said, “A diagnosis of stroke can be an overwhelming experience for a person due to the shock of their diagnosis, and people may also have to cope with the effects of stroke which can impact on their daily activities.”
Minister for Health Stephen Donnelly turns the sod alongside local councillors and HSE representatives. My Stroke Journey is available to all patients in MUH and can be downloaded at www.saolta.ie

Sod turned on new community hospital in Donegal
Minister Simon Harris during visit to ATU with representatives from Saolta, ATU and the HSE.
New partnership with university aims to build healthier future
Atlantic Technological University (ATU) and the HSE, including Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo (CHCDLMS), Community Healthcare West (CHW), Public Health West and North West, Saolta and the National Ambulance Service (NAS) have formed a new partnership aimed at advancing education, skills development, research and innovation to build a healthier future.

health inequalities, excellence in education and training, collaboration in research and innovation, and stakeholder engagement.
The Memorandum of Understanding (MoU) was officially launched recently, solidifying the commitment of both organisations to collaborate and address regional and national policy objectives. Strategic priorities of the partnership include regional service development, addressing
The MoU outlines a five-year agreement between ATU and the HSE. The partnership aims to strengthen the existing relationship between the two organisations and provide a platform for development of stronger health and academic links into the future.
The sod has been turned on the new Letterkenny Community Hospital. The completed development will comprise of 110 beds including a mix of long/short stay rehabilitation and dementia care with associated resident accommodation.
The net construction cost of the facility is €52 million, and it is anticipated that the new Community Hospital will be operational in early 2026.
The first floor of the new Letterkenny Community Hospital will provide two 25 bed households for stepdown or medical rehab use alongside a Rehabilitation Unit. The unit will comprise physiotherapy treatment rooms, occupational therapy rooms, speech and language therapy room, consultation room and outdoor therapy space.
The ground floor of the development will provide two 25 bed household units which will accommodate 50 long stay residential beds with outdoor space.
The lower ground floor will provide a 10 bed Dementia Specific unit which has been designed as a household model with an additional multi-sensory room, quiet room and courtyard spaces/garden. The design of the Dementia unit will support the continued engagement of the residents living with dementia in meaningful personcentered activities.
News | 63 HEALTH MATTERS SPRING 2024
Changes and updates
Focus on Data protection: Tips to prevent postal data breaches

The HSE sends out hundreds of letters and appointments by post every day. Administrative errors in issuing letters and appointments by post are the most common type of data breach in the HSE. Postal data breaches occur in a very small number of letters issued by the HSE, but they can be upsetting for individuals when they occur.
HSE Data Protection Officer Mary Deasy explained, ‘Postal breaches most commonly occur when staff use incorrect addresses, use old addresses, mistakenly include more than one letter or appointment in the same envelope or mistakenly attach a document relating to another person to a letter.
"They can also occur when envelopes are not sealed securely. A breach like this can be stressful and upsetting, especially if neighbours or family members receive a person's confidential data.
"We’re asking staff to use the tips outlined below to reduce the risk of a postal data breach. There’s also useful videos with tips on reducing your risk of a data breach on the HSE staff webpages.’’
Cork residents urged to order free HSE at-home test for Hepatitis C
The HSE’s National Hepatitis C treatment programme encourages people living in Cork to check if they need a free at-home Hepatitis C test at www.hse.ie/hepc.
Up to 3,000 people in Ireland may currently have the blood borne virus, which infects the liver and, if left untreated, can cause serious and potentially life-threatening damage.
Recognising the importance of reaching diverse communities, the HSE is promoting the free at-home hepatitis C test at four bus shelters in Cork city ensuring accessibility
To reduce the risk of errors, you should:
• use a 3-point check for patients' addresses:
• check the patient's address is correct when drafting the letter
• check again after printing
• do a final check before it goes into the envelope
• use windowed envelopes (ensure no sensitive information can be seen through the window)
• make sure the envelope contains only the individual's information (double-check the front and back of each letter)
• check that 'private and confidential' is on the envelope
• be alert
If you know there has been a data breach or if you think there may have been one, ask for help from your line manager and your local Deputy Data Protection Officer. HM
and awareness among the local population.
Prof Aiden McCormick, HSE Clinical Lead for the Hepatitis C Treatment Programme, said, “It can be difficult to reach individuals infected with the hepatitis C virus as many have no symptoms. The HSE is piloting on-street advertising in Cork city to see if this encourages increased engagement with screening services.
“So if you are 18 or older and living in Cork, visit www.hse.ie/hepc to order a free at-home hepatitis C test today. If you’re unsure if you need a
test, you can answer some optional questions on the website to check your risk.”
The National Hepatitis C Treatment Programme has treated over 7,000 people, 95% of whom are now cured. The HSE is promoting the athome hepatitis C test as part of its commitment to making hepatitis C a rare disease in Ireland by 2026, and eliminating it in Ireland by 2030 aligning with the World Health Organization target.
Order your Hepatitis C Home test on www.hse.ie/hepc
HEALTH MATTERS SPRING 2024 64 | Updates
Updates
Support pathways for people with non-cognitive symptoms of dementia
The HSE National Dementia Office has developed a HSeLanD Module entitled ‘Support pathways for people with noncognitive symptoms of dementia’. This 30-minute module will help you to determine the best person-centred supports for a person with non-cognitive symptoms of dementia and to recognise the risks of unnecessarily prescribing a psychotropic medication.
The module is suitable for all healthcare professionals who provide care to people with dementia across all settings and contains three key topics:
1.Non-cognitive symptoms of dementia
2.Tailored person-centered support
3.Risks of psychotropic medication
The module includes an assessment and extend my learning pieces for those who wish to undertake further learning or who want practical activities to help transfer the learning into their local area of work.
As of January 2024, almost 3,000 people have completed the module. The feedback to date on the module has been very positive.
Please search “non-cognitive symptoms of dementia” on the HSeLanD website to find this module. The module can also be found in the “clinical skills” section of the course catalogue on HSeLanD.
Early Intervention in Psychosis
Psychosis is a condition that affects the way the brain processes information. It affects 3% of the population. Psychosis is associated with an array of mental illnesses including schizophrenia, bipolar affective disorder and severe depression. There are often long delays between people starting to experience symptoms and accessing mental health care, with an average of two years’ delay.
Early intervention in psychosis (EIP) services provide rapid access to expert assessment, a range of evidencebased interventions including medication, psychosocial, physical health, and vocational support. In the absence of an EIP service treatment is typically accessed late, in crisis and may be medication-focused.
Over 20 years of evidence in UK, Australia, Scandinavia, Canada and more recently in USA indicate that EIP services reduce relapses, improve outcomes and save the economy money. The Early Intervention in Psychosis National Clinical Programme, Model of Care was published in May 2019. There are five EIP teams in operation in Ireland.
The National Clinical Audit of Psychosis has been run each year across all Early Intervention in Psychosis teams in Ireland for the past three years Ireland (2019/2020: 2 teams, 2021- 2023: 4 teams). The Audit is conducted as a collaboration between Royal College of Psychiatrists and Health Quality Improvement Partnership (HQIP) in the UK. The audit standards are based on NICE guidelines for Early Intervention in Psychosis.
Ireland’s participation this year was part funded by the HSE Quality and Patient Safety Directorate and HSE Mental Health Operations. The findings demonstrate timely access to care and high rates of uptake of evidence-based interventions including psychological interventions, employment support and family interventions.
Below is a summary of the Key Findings for the NCAP Audit in 2022/2023. HM
Project aims to boost role of health care assistants
The Health Care Assistant Project has been set up under the auspices of National HR to roll out the recommendations of the Review of the Role and Function of Health Care Assistants report published in December 2018.
An oversight group and four workstreams, namely ‘Role and Function’, Training and Development’, Data and ‘Communication and Stakeholder Engagement’, was established to deliver on these recommendations.
The updated job specifications for health care assistants working in
Acute, Older Persons and Mental Health sector were issued recently and these documents can be accessed from HSE website using the link www.hse.ie/eng/about/ who/healthbusinessservices/ hbshumanresource/patientclient-care-health-and-social-careassistants.html.
Further work is in progress to update the job specifications for health care assistants working in other sectors and in specialties.
A pilot is underway to test the template designed to gather the educational qualifications of health
care assistants.
As part of Life Long Learning opportunities that are available for healthcare assistants, a review of HSELanD courses is currently underway.
In liaison with HSE Communications, plans are in progress to carry out a few activities to raise the profile of health care assistants.
Health Care Assistants constitute 14% of health service workforce and work as members of the multidisciplinary setting across various sectors in providing highquality patient care.
| 65 HEALTH MATTERS SPRING 2024
Launch of the Review to Inform the Strategic Direction of Laboratory Medicine
The Review to Inform the Strategic Direction of Laboratory Medicine was launched on 22 January. The purpose of the review was to inform the development of a strategic, integrated approach to develop a sustainable and scalable future for laboratory services in Ireland.
The review was commissioned by the Chief Clinical Officer and led by Patricia Byron as the Independent Chair and Dr Siobhán Ní Bhriain, National Clinical Director for Integrated Care. The report details the comprehensive findings and considerations of a highly motivated, dedicated, multi-disciplinary Working Group comprising of various stakeholders and laboratory professionals with scientific, clinical, management and leadership expertise.
Dr Ní Bhriain said, “Laboratory medicine is an integral part of our healthcare system and is an essential component of patient care. It is reliant on
a highly trained workforce, effective infrastructure, leveraging the benefits of modern equipment and automation, as well as information technology and data integration.
“The collaborative approach of the working group ensured the voices and concerns of the various professionals operating within the system were central to the process. The review has provided vital insight and recommendations to support the future development of laboratory services, which will include the adoption of innovative technology and advances in scientific practice.”
The next stage in the journey is the development of a Strategy for Laboratory Services 2025-2029, which will be led by Prof Martin Cormican, Clinical Lead for Laboratory Services Reform. The review will inform that strategy and the process will consult with all stakeholders. HM
The Review to Inform the Strategic Direction of Laboratory Medicine is available at https://www.hse.ie/eng/about/who/cspd/ncps/pathology/resources/programmedocuments-resources.html
See full review at hse.ie/eng/about/who/cspd/lsr

Patricia Byron, Steering Group Independent Chairperson; Dr Fraser Thomson, Manager, Deloitte Healthcare; Marie Culliton, President, International Federation of Biomedical Laboratory Science; Jennifer Brady, Consultant Clinical Biochemist, CHI; Dr Siobhán Ní Bhriain, National Clinical Director, Integrated Care; Dr Sean Costelloe, Consultant Clinical Biochemist, CUH; Breda Rafter, Principal Officer, Strategic Workforce Planning, DoH; John Gibbons, Laboratory Manager, St James’s Hospital (retired); Stephen Power, Medical Laboratory Scientist, CUH; Danielle Farrelly, Consultant, Deloitte Healthcare; Sharon Hayden, GM, Office of the CCO; and Jackie Reid, National Lead, NHSCP Office, all members of the Working Group.
HEALTH MATTERS SPRING 2024 66 | Updates
Updates
Use HR and Payroll Self Service to apply for leave
It’s that time of year when we are making plans for holidays. We all want to make the best of Spring with our remaining leave days or perhaps plan for Summer.
What leave can you apply for on HR & Payroll Self Service?

Using HR and Payroll Self Service, you can apply for any leave type which requires only one level of approval such as annual leave as seen below.
Can you edit or change leave requests?
You can delete any leave request by clicking on the bin icon or edit the request by clicking on the pencil icon.
Apply and take Carry Forward Leave
If you have leave remaining at the end of March 2024, discuss this with your manager to confirm the amount of leave hours to carry forward. This can then be applied for on the Leave Carry Forward tile on Self Service from 1 April 2024.
When you request annual leave, the system will automatically take from your Carry Forward leave balance first. You can check this on the My Leave Request tile.
Where do I find my leave entitlement for the year?
“Leave Balances” tile under “Calc A/L for Year”. This report also shows you the number of annual leave hours remaining for the year.
You will find more detailed information on the Leave Requests support page on www.hse.ie/nisrp. Scan support QR code to go direct the leave requests page.
New contact numbers for Your Service Your Say
The contact numbers for Your Service Your Say, the HSE's public feedback service, changed in December 2023. The new contact numbers are:
• Freephone 1800 424 555 when calling from inside Ireland
• +353 1 642 4555 when calling from outside Ireland
New posters and leaflets are available for HSE services to inform people of the new contact numbers for Your Service Your Say. If you work on a site and need copies of the new YSYS posters or leaflets please order them through www.healthpromotion.ie
Should you have any queries, please contact nationalcglt@hse.ie

| 67 HEALTH MATTERS SPRING 2024
HSE Telehealth Roadmap
will provide building blocks for expansion of telehealth
Conor Kennedy, Senior Project Manager, eHealth Telehealth Programme Team, and Dr Orna Fennelly, Digital Health Consultant Researcher, explain the benefits of embracing telehealth
The new national ‘HSE Telehealth Roadmap 2024-27: Building Blocks for the Embedding and Expansion of Telehealth’ was formally launched at the Digital Healthcare Conference in December. The roadmap was developed by the National Telehealth Steering Committee following consultation with patients and staff to provide a coherent and strategic plan to ensure safe, effective, efficient, scalable, sustainable, and interoperable development and embedding of telehealth across the health service.
Embracing telehealth can expand opportunities to deliver high-quality and safe care, and provide real benefits to patients including reduced exposure to infection risk, travel time and associated costs, carbon emissions, and time away from work, school, families and communities. Telehealth can also support early intervention and reduced hospital admissions, and empower patients to manage their health and wellbeing closer to home.
68 | HEALTH MATTERS SPRING 2024

What is Telehealth?
HSE telehealth encompasses three elements:
1. Consultations and care appointments conducted remotely by healthcare providers
2. Remote health monitoring which allows clinicians to track vital signs, physical symptoms, chronic conditions, patient feedback etc., from the patients’ own day-to-day environment, and
3. Online supports and therapies that use internet and messaging-based solutions and resources
The roadmap envisages a future state where telehealth ‘seamlessly integrate(s)… into businessas-usual within the healthcare service, providing high quality and safe healthcare, accessible to all, no matter who they are or where they live’.
This vision will be guided by six core principles:
1. High-quality care is the priority, regardless of the medium.
2. Patients as empowered partners - putting individuals and service users at the centre, with respect to personal choice.
3. Ensuring digital access is inclusive and equitable for all.
4. Empowering our healthcare workforce to effectively deliver care using telehealth.
5. Continue our uncompromising commitment to
patient safety, quality of care and continual improvement and evaluation.
6. Maintain and build upon our stringent data, security, and interoperability standards for seamless operations.
The roadmap proposes seven key building blocks to provide a firm foundation for telehealth within the HSE and across the wider health service. Within each of the building blocks there are key aims and actions to be completed across community and acute services. HM

The HSE Telehealth Roadmap 2024-27 and the report of the HSE Telehealth Consultation Day 2023 The Now, The Next, The Future’ are available to download at https://healthservice.hse.ie/staff/procedures-guidelines/digital-health/
| 69 HEALTH MATTERS SPRING 2024
Talking point
Annette Connolly, NMPD Officer HSE West Mid West; Paula McGreal, NMPD Officer, HSE West Mid West; and Grainne Glacken, NMPD Officer, HSE North West at the ONMSD Professional Development Planning for Nurses and Midwives stand at the conference.
From the eHealth Telehealth Programme were Dr Conor Kennedy, Emer Sheridan, Elaine Aughey, Ciara Clarke, Tracey McCluskey and Julie Bellew.
Video enabled care creating a better experience for pregnant women with diabetes
University Hospital Waterford (UHW) implemented video enabled care (VEC) for their gestational diabetic mellitus service using a VEC Toolkit and the service has become invaluable to modern-day management of the pregnant diabetic lady in UHW.
The purpose of the VEC toolkit is to guide healthcare professionals and administrative support staff working in this service, on the implementation of online health appointments and video communication to support the delivery of healthcare.
Before the introduction of VEC in June 2023, UHW had a traditional model of care in place with face-to-face encounters that brought challenges for women attending the service.
Janet Murphy, Assistant Director of Nursing and Midwifery, UHW, explained, “The overarching aim of video is to mimic as close as possible the way face-to-face meetings and visits happen, without the need for either the patient/service user or the healthcare professional or both, to physically attend in-person. It gives both healthcare professionals and service users choices and facilitates a blended care approach to healthcare.
“At UHW a working group was convened which included obstetric consultant, IT Support, clinical midwife specialist in diabetes, senior midwifery management and administration support. The VEC toolkit was the guiding document helping to keep the team on track.”
From the commencement of the service at UHW, valuable improvements can be noted in the service. These include a reduction in face-to-face meetings, prompt intervention care when required, prescriptions updated in real time, very low DNA rate, patient feedback weekly is at 100% satisfaction, prompt intervention by the CMS has reduced unscheduled care episodes, and women have a better understanding of their diagnosis and management. Weekly intervention and management of women with diabetes has reduced the amount of GDM insulin therapy in labour, and has reduced the neo-natal intensive care admissions for poor control of blood sugars. Currently UHW are rolling out VEC within the booking interview system.
For further insights, the VEC Toolkit can be accessed at https://www.ehealthireland. ie/ehealth-functions/community-health/ telehealth-programme/video-enabled-carevec-/video-enabled-care-vec-toolkit/
National Digital Health Conference told of roadmap for expansion of telehealth

Following the resounding success of the initial National Digital Health Conference, the hybrid conference was held again recently to further advance the collective vision to optimise digital healthcare in Ireland.
Welcoming delegates, Loretto Grogan, HSE National Chief Nursing and Midwifery Information Officer, reflected on digital progress made so far.
“The COVID-19 pandemic enabled momentum in digital health developments that may have otherwise taken years. It is crucial that we build on this, putting strong foundations in place to digitise, connect and transform services safely and securely to improve the outcomes, experience and safety for people accessing our health service.
“The potential benefits of telehealth are clear. For example, remote video and telephone consultations can reduce travel time, costs, emissions and time away from work, school, families and communities.”
Another core theme of the conference was the digital empowerment of the health service workforce.
Professor Richard Greene, Chief Clinical Information Officer, HSE, said, “While digital health incorporates software, hardware, services and everything from mobile health apps to electronic health records, we must acknowledge that these will not deliver healthcare improvements alone. We need integrated and standardised workflows, improved resource management and a renewed focus on patients and carers needs. Our focus is optimising these tools for the benefit of our patients and healthcare workers.” Fran Thompson, Chief Information Officer, HSE, acknowledging the fundamental role of staff, said, “Significant steps are being made to improve the digital capability in our health services in line with Slaintecare requirements. This conference brings to the fore the combined vision of healthcare staff to provide connected digital care to the people of Ireland.”

HEALTH MATTERS SPRING 2024 70 |
John Ward, HSE CTTO; Michael Redmond, HSE COO, and Fran Thompson, HSE CIO.
Paul Gallagher, Loretto Grogan, Ger Shaw, Dr Colm Henry, Siobhan Ní Bhriain, Minister Ossain Smyth, John Ward, Fran Thompson and Professor Richard Greene at the Better Together for Digital Healthcare Conference.
antibioticprescribing.ie

HSE infection website the go-to for Irish GPs
The most widely used resource for clinical practice guidance amongst Irish GPs is now antibioticprescribing.ie





Antimicrobials are essential in treatment of many serious infections. However, they can also cause harm: not only to the individual, but also have wider implications by promoting the development of antimicrobial resistance. Antibiotic stewardship is all about using antibiotics wisely, to optimise patient outcomes, and minimise harm. Evidence-based antimicrobial guidelines are a key tool in promoting antimicrobial stewardship. The HSE website antibioticprescribing.ie hosts national guidelines for antimicrobial use in community settings, and is the key reference source for healthcare professionals such as GPs, dentists, nurses and pharmacists who are treating common infections in the community.



This resource is a collaboration between the HSE Antimicrobial Resistance and Infection Control (AMRIC) team and HSE Community Antimicrobial Pharmacists. The HSE AMRIC National Clinical Lead provides oversight with delegated authority for guidance approval from the HSE Chief Clinical








Officer. There are over 80 guidelines available. Expertise is provided to each guideline review by an extensive panel of advisors. The website also highlights when antibiotics may not be appropriate for management of infections and what other steps may be taken to support patient care. It also provides other resources to support healthcare professionals in practicing antimicrobial stewardship, including antibiotic audit tools, links to patient information, information on common antimicrobial drug interactions, dosing in children and renal impairment.



A recent study found it is the most widely used resource for clinical practice guidance amongst GPs in Ireland, with 76% of 499 GPs surveyed reporting they use the website. The antibioticprescribing.ie website reach continue to grow annually, and in 2023 it had almost 2 million pages views. HM


If you prescribe, dispense or administer antibiotics in community settings, please refer to these guidelinesthey are readily accessible on antibioticprescribing.ie











| 71 Feature HEALTH MATTERS SPRING 2024
Awards
Awards and accolades
Cahersiveen intergenerational IT project wins Age Friendly award

Cllr Jim Finucane, Cathaoirleach/ Mayor of Kerry; Lucy Higgins, student; Mary Daly, Cahersiveen Active Retired; Siobhán Griffin, KCC; Patrick Moran, student; Aisling Murphy, teacher, Coláiste na Sceilge; Clíonadh O’Shea, student; Patricia Maher, Cork Kerry Community Healthcare; Séamus Daly, Cahersiveen Men’s Shed; and Kathleen O’Sullivan, Cahersiveen Social Services.
An IT project supported by Kerry Community Work Department has won a Judges’ Special Recognition Award at the National Age Friendly Awards Ceremony.
The intergenerational IT project was a collective effort involving older participants from local community groups, Transition Year students in Coláiste na Sceilge, Kerry Diocesan Youth Service (KDYS), University of Limerick (UL) and Age Friendly Kerry and the Community Work Department.
A total of 14 TY students took part, along with 12 people from the Active Retired, Men’s Shed Group and Cahersiveen Social Services.
The IT programme used was an adapted version of the Hi Digital Programme, which is a course designed for anyone who needs a bit of help developing their digital skills, particularly those who have rarely or never been online (often 65+ years old). It consists of bite-sized lessons organised around key digital themes including smartphones, online banking and travel.
The students met with the older people one morning a week for six weeks and taught them how to use their smartphones and
incorporate technology into their everyday lives. In return, the older participants taught the students about their locality, encouraging a sense of pride and connection to their community. Great relationships formed during the programme between the community participants and the students.
One TY student said, “I really enjoyed this class every Tuesday. Each week, we were getting to know each other better and had very interesting conversations.”
One of the participants said, “We loved coming here every week – the students we were working with made us feel young.” HM

HEALTH MATTERS SPRING 2024 72 |
Cork and Kerry staff honoured at lively awards ceremony
Awards

Cork Kerry Community Healthcare recognised the outstanding contribution of staff at a gala awards ceremony at Cork City Hall. The awards were an opportunity for Cork Kerry Community Healthcare to demonstrate the depth, complexity and quality of services delivered in the community. Twelve shortlisted projects were finalists in four categories, with HSE Chief Operations Officer Damien McCallion presenting certificates to all finalists.
The winners in each category were:
• Kerry Pictures for Palliative – winner in the category Improving Service User Experience
• Establishing the National Incident Management System Inputting Service for CKCH – winner in the category Innovation and Integration in Service Delivery
• Multidisciplinary Care Pathway for Autistic Teenagers – winner in the category Excellence in Quality and Patient Safety
• Staff Wellness at Work Event on Midsummer’s Day at St Stephen’s Health Campus – winner in the category Staff Health and Wellbeing Initiative.
The finalists and overall winners in each category were chosen by a panel of four independent judges. The chair of the judging panel was former HSE staff member Barry O’Brien and the other judges were Elaine Prendergast, Head of Health and Wellbeing from Community Healthcare West (CHO2); LeeAnn Scott, CKCH Patient and Service User Engagement officer and David Tully, Head of HR from CHO7 . HM
See www.hse.ie/corkkerrystaffawards for more details.
Cavan and Monaghan singled out for breastfeeding achievements
Cavan and Monaghan have won two national breastfeeding awards for the regionbreastfeeding support group of the year for Virginia and Lactation Consultant of the Year for Mairead McCahill.
It also captured three national breastfeeding nominations in roles that recognise allied health professional support, breastfeeding mum of the year and breastfeeding advocate of the year.
Mairead, the award-winning HSE Lactation Consultant for Cavan Monaghan, said, “This year was an especially special year for the Virginia Breastfeeding Group when it won the Friends of Breastfeeding national award for Breastfeeding Group of the Year 2023.
“These groups help to normalise breastfeeding whilst supporting mothers through peer support and providing the ‘village network’ that is missing for some mothers as they are embarking on their mothering and breastfeeding journey.

Edel McAweeney, HSE; Annmarie Rice, HSE; Aileen Doyle, HSE; Mairead McCahill, HSE, Collette Deeney, Tusla; Monica McRory, HSE; Ciara Ni Chionnaith, Teach Na nDaoine, Monaghan; and Ellen McMeel, HSE.
| 73 HEALTH MATTERS SPRING 2024
HEALTH
Events
Events and functions

11th Annual Multidisciplinary Research Symposium held
The 11th Annual Multidisciplinary Research Symposium was held at Letterkenny University Hospital (LUH) recently.
The event, organised by the LUH
Conference
showcases
Postgraduate Medical Education Department, showcased some of the excellent research taking place within LUH and the broader community, with oral and poster
role
of social workers in mental health services
The Midlands Louth Meath Community Healthcare (MLMCHO) Social Work Mental Health Services recently held a conference to showcase the work undertaken by Mental Health Social Workers across the region.
The purpose of the conference was to assist multi-disciplinary team members becoming more understanding of the range and depth of services and skills that social workers can bring to enrich and enhance service provision.
This will contribute to better practice and better mental health outcomes for all our service users.
Social Workers are an integral part of multi-disciplinary teams located across the geographical area and their work is embedded
Front: Dr O Dunne, Renal Consultant; Dr C Richardson, Associate Director of Postgraduate Medical Education and Training, LUH; Dr L Moran, Anaesthetic Consultant.
Back: Prof R Costello, Respiratory Consultant and Guest Speaker; Dr K Gallagher, Rheumatology Consultant, Crumlin Hospital; Prof K Mulpeter, Geriatric Consultant and Dr AM Moran, Renal Consultant.
presentations from staff representing a wide range of disciplines within our healthcare services as well as University of Galway medical students. HM
within the delivery of Mental Health Services in both adult and child and adolescent services. The role is central to the successful outcomes for people who use the service in the application of the systemic and bio psychosocial model of service delivery. This one-day conference was an opportunity to highlight some of the roles of social work within this delivery context and explored areas such as recovery-focused practices, working with maternal mental health, developmental trauma/trauma-informed care, family-focused interventions such as family talk, values of nonjudgemental and unconditional positive regard and how they inform social work practice, BFT, the use of theraplay in social work practice, and mapping journeys to recovery in the context of co-produced multi-disciplinary working.
HEALTH MATTERS SPRING 2024 74 |
Lisa Farrelly, General Manager, HIDS Business and Siobhain Duggan, GSI

Data Collaborathon spearheaded by HIDS attracts 250 health tech professionals
The second annual Data Collaborathon event organised by the HSE’s Health Identifier Service (HIDS) took place with 241 health professionals attending from across the country.
The hybrid event was open to both public and private sector to share best practice around data management and governance with a series of HSE case studies presented. First held in 2021, Data Collaborathon is a concept born within the HIDS team to bring co-thinking, conversation and solutions to the challenges of data management and data governance.
As a team who works with data every day to drive forward the HSE’s ambitions around health identity services, HIDS felt there was value in sharing best practice and experience among peers.
Maria McCann, Assistant Director of National Identity Services said, “Events such as this provide a platform for stakeholders to share their learnings and challenges and to work together to find existing and new solutions. These events are open to a cross-section of the health ecosystem, which can lead to fresh perspectives and creative solutions to complex digital and data challenges.” HM
A copy of the Data Collaborathon Report 2023 can be obtained by emailing hidsoffice@hse.ie.
Galway well represented at speech and language therapy conference
Three senior speech and language therapists (SLTs) had posters selected for presentation at the national biennial Irish Association of Speech and Language Therapists (IASLT) conference, describing SLT services, multidisciplinary working and case study across the range of caseloads covered by SLT services.
Hannah Loughnane, Valerie Monaghan and Méabh Sheridan are all SLTs working at Galway University Hospital. Their posters were selected to be presented at the national biennial IASLT conference.
They were required to submit abstracts through a competitive process, vying with other SLTs providing services to adults and paediatrics across the country for oral or poster presentation at the national SLT conference.
Portiuncula Hospital SLT was also represented by Aisling Ní Cheannabháin who presented on behalf of the SLT department.
Hannah won the Best in Show - Day One poster for her service evaluation of the Fibreoptic Endoscopic Evaluation of Swallow (FEES) over a year throughout GUH, a Level 4 hospital. Her colleagues Méabh and Valerie described a case using neuromuscular electrical stimulation as an advanced dysphagia treatment method.
Hannah presented a final case study poster with Palliative Care and General Surgery, describing the improvement in swallow and voice with standard rehabilitative exercises, once significant secretion burden had been appropriately managed.
Despite ongoing clinical challenges including staffing, high caseload numbers and increasing patient complexity, the SLTs remain committed to providing evidence-based therapy, appropriate to each patient.
Events | 75 HEALTH MATTERS SPRING 2024
Events







‘Our Voice Our Choice’ promotes self-advocacy
HSE Disability Services in Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo (CH CDLMS) hosted ‘Our Voice Our Choice’, a self-advocacy event, in collaboration with Inclusion Ireland, recently. Attendees at the event included selfadvocates, people accessing disability services, key workers, staff from Disability Services, staff from other support services and senior managers.
‘Our Voice Our Choice’ showcased presentations from various self-advocates and their support staff. The presentations demonstrated the importance of selfadvocacy in fostering autonomy, respect and mutual support to ensure disabled people are empowered in decision-making. The exemplary and thought-provoking presentations also demonstrated new ways of working and thinking outside the box, finding a way forward when the path is not clear.
This event also launched the Self-Advocacy Strategy for CH CDLMS by Edel Quinn, Head of Service for Disability Services in CH CDLMS. The strategy details a model of self-advocacy and describes a framework for building and fostering a positive culture that enables the participation in planning and decisionmaking of disabled adults using Disability Services in the CH CDLMS area. HM
Top:
Barry Lynch, Inclusion Ireland, Edel Quinn, HSE, Head of Service for Disability, Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo (CH CDLMS), Colm Lehane, Clara Learning and Aidan Quinn, HSE, Disability Services, Donegal at the 'Our Voice Our Choice' event in Donegal
Bottom: Arindam Gosh, HSE, Project Manager
Disability Services, Bernie Donaghy, HSE, General Manager
Disability Services, Edel Quinn, HSE, Head of Service for Disability, CH CDLMS, Barry Lynch, Inclusion Ireland, Mary McGroarty, HSE General Manager, Disability Services Donegal and Caroline Bradshaw HSE, Patient & Service User Engagement Officer, at the 'Our Voice Our Choice' event in Donegal.
Cervical Cancer Prevention Week 2024 highlights the people of CervicalCheck
During Cervical Cancer Prevention Week, which ran from 22–28 January, the National Screening Service highlighted the importance of cervical screening in preventing or reducing the risk of cervical cancer. The campaign encouraged women to choose screening, and focused on the people who deliver, support and advocate for the CervicalCheck programme.

There are over 4,500 people involved in delivering CervicalCheck, including Orla Loftus, an Advanced Nurse Practitioner who is a registered sample taker with CervicalCheck.
Orla began her nursing career in 1997 when she joined her father’s GP practice in Crossmolina, Co Mayo. She said her father, Dr Michael (Mickey) Loftus, inspired her to take up a role in caring for women in her community. This was before Ireland had a cervical screening programme. She said it was a time when there was very little awareness of cervical cancer, and when screening was “haphazard, and the results took ages”. She described the introduction of CervicalCheck in 2008 as an uplifting moment because “cervical screening prevents cancer”. When the cervical screening programme was introduced, Orla says her practice at Knock Medical Centre “took it and ran with it. I’ve been working in practice for 26 years. I understand my patients and take a holistic approach in providing care. Some of the patients I vaccinated when they were babies are now coming to me for cervical screening. It’s a privilege and opportunity, as part of an ongoing therapeutic relationship, to be able to offer our patients cervical screening.”
HEALTH MATTERS SPRING 2024 76 |
Events
Conference celebrates 21 years of nursing and midwifery education
The recent National Education Conference facilitated a unique opportunity to celebrate the past, reflect on the present and focus on the future of nursing and midwifery education.
The conference was held by the HSE Office of the Nursing and Midwifery Services Director (ONMSD) to celebrate 21 years of nursing and midwifery education. It provided a valuable learning experience for attendees. A broad range of speakers from regulatory and policy perspectives provided insight to current best practice and future trends in education. Attendance at this inaugural event provided an opportunity to network and broaden professional connections.
Since the inception of the education centres 21 years ago, this conference marked the first opportunity to highlight the ongoing contribution of the centres in leading on the provision of evidence-

based Continuous Professional Development (CPD) education for registered nurses, registered midwives and those that support these roles.
It was attended by approximately 200 delegates representing key areas involved in the development, delivery and future direction of nursing and midwifery education.
The conference focused on recent advances and future trends in nursing and midwifery education and the key influencing factors such as Nursing and MIdwifery Board of Ireland (MMBI) regulatory policy, Department of Health
Sharing conference showcases best practice initiatives
A Sharing Best Practice Conference for nursing and midwifery staff highlighted the importance of creating opportunities for collaboration, sharing of ideas, and supporting nurses and midwives to showcase exemplars of best practice initiatives.
Over 70 nurses and midwives, representing all disciplines of nursing and midwifery services from across the region, had the opportunity to showcase examples of best practice through oral and poster presentations. The conference was hosted by Nursing and Midwifery Planning and Development Unit (NMPDU) HSE West Mid-West.
Three keynote speakers addressed the conference: Professor Helen Bevan, Professor of Practice in Health and Care Improvement/ Strategic Advisor –NHS Horizons; Dr Ray Healy, Director of Registration with NMBI; and Dr PJ Harnett, National Programme Manager for the National Integrated Care Programme for Older Persons.
They addressed the challenge of supporting, developing, and sharing best practice, and
education policy and the ONMSD strategic policy.
This inaugural conference provided the platform to communicate the education and research initiatives that are being undertaken locally, regionally and nationally. Evidencebased research has had a direct impact on the provision of high standards of care, delivered to patients and service users. It also raised awareness of advances in the fields of simulation, virtual reality and artificial intelligence in digital learning and transformation for education in the future.

encouraged delegates to embrace the opportunities and benefits that integrated care will bring to the workplace. Nursing and midwifery colleagues showcased a wide variety of initiatives demonstrating a wealth of exemplars of best practice.
Back: Brendan Power, NMPD Officer, NMPDU HSE West Mid-West; Margaret Crowley Murphy, Director, CNME HSE Mid-West. Middle: Dr Patrick Glackin, HSE West Area Director, ONMSD; Dr PJ Harnett; Dr Ray Healy, Director of Registration with NMBI; Professor Helen Bevan; Paula McGreal, NMPD Officer, NMPDU HSE West Mid-West; Valerie Ryan, Staff Officer NMPDU HSE West Mid-West. Front: Carmel Hoey, Director NMPDU HSE West Mid-West; Grainne Ryan, Director Public Health Nursing, Clare, CHO3; Anne McCarthy, Researcher NMPDU HSE West Mid-West; Annette Connolly, NMPD Officer, NMPDU HSE West Mid-West.
| 77 HEALTH MATTERS SPRING 2024
The conference organising committee.
Health and wellbeing

Funding of over €100,000 awarded for arts, creativity and health projects
As part of the collaborative work on arts, creativity and health between HSE Healthy Ireland, Creative Ireland and the Arts Council, the HSE submitted two applications to Creative Ireland and were awarded a total of €114,470.
‘Celebrating Culture Diversity through the Arts for Staff Health and Wellbeing’ received €54,320 for nine Community Health Organisations (CHOs) and Hospital Groups (HG).
The funded projects included an intercultural musical collaboration performed and recorded by staff to play in waiting rooms; a series of multicultural singing workshops where staff were invited to sing and share a song from their culture; and a photography competition on the theme of cultural diversity.
The RCSI Hospital Group, in collaboration with Midlands Louth Meath Community Healthcare Organisation, hosted a wonderful Christmas market event with stalls showcasing the rich culture diversity of staff through food, crafts, music and art.
The aim of these projects was to develop a better understanding and appreciation among staff of the different cultures in the HSE but also to increase staff awareness of the role of the creative arts in positively impacting on their health and wellbeing.
The ‘Celebrating Culture Diversity through the Arts for Staff Health and Wellbeing’ also funded a participative festive workshop which took place in Dr Steevens' Hospital on Wednesday, 20 December 2023.
As part of the day, a series of fun and interactive music workshops were also held. Both the workshops and the festive performance brought lightheartedness, fun and joy to those who attended. The day also supported staff health and wellbeing by providing an opportunity for social connection with colleagues and enjoyment of the creative arts.
A further €60,150 from Creative Ireland will support and strengthen existing arts and health initiatives in hospitals, and allowed for the expansion of this concept into new hospitals.
The aim of these funded projects is to create awareness and advocate for use and integration of arts to positively contribute to the health and wellbeing of service users, staff and visitors. HM
Sarah McCormack, National Healthy Ireland Lead; Sally-Ann McLaughlin, Senior Dietitian and Staff Health Lead, Midlands Louth Meath; Dolores Donegan, RCSI Hospital Group Programme Manager; and Paddy Clerkin, Chief Operating Officer RCSI Hospital Group, pictured with staff from RCSI Hospital Group at their Christmas market event.
HEALTH MATTERS SPRING 2024 78 | Health

Taoiseach shares his favourite recipe for the new Tallaght hospital cookbook
Taoiseach Leo Varadkar kindly shared his favourite recipe in the new Tallaght University Hospital (TUH) Cookbook, which has just been launched to celebrate the 25th anniversary of the hospital.
'Global Family FavouritesRecipes and Stories from Our Families to Yours' is a collection of recipes and stories from hospital staff and includes starters, main courses, and desserts.
It contains 62 recipes with accompanying stories from 25
Head of Library and Information Services at TUH Jean McMahon with TUH CEO Lucy Nugent, pictured at the launch of the Global Family Favourites book.
different countries, including Ireland, China, The Philippines, Grenada, Nigeria, Poland, Spain, France, Albania, and the Czech Republic - to name but a few! There are eight recipes from India and five from staff in the Catering Department, including the famous TUH shortbread. Many international staff leave behind their homes and families to come and look after our patients, and each other.
Jun Cao, a Clinical Nurse Manager who works in our Cancer Services. Jun grew up in the city of Shijiazhuang near Beijing, in the Hebei province of northern China.
Non-Consultant Hospital Doctor’s Health and Wellbeing Hub
A centralised Workplace Health and Wellbeing service for Non-Consultant Hospital Doctors (NCHDs) was recently launched. This service will offer support with occupational health assessments to NCHDs. The service is available to those who have an NCHD contract with the HSE or a Section 38 service.
This service will offer
• Advice on workplace adjustment for psychological and medical issues
• Disability and work advice
• Work-related stress support
• Fitness for work assessments
• Psychological support relating to your role as an NCHD
The NCHD Hub can be accessed by self-referral or via a referral from local Occupational Health Service, Medical Manpower, National Specialty
Jun shares her grandmother’s recipe for Chinese Dumplings. There’s also some Irish recipes, like the one for boxty from Head of Catering Valentine Farrell, which she learned to cook during her childhood in Killeshandra, Co Cavan.
The cookbook was edited by Head of Library and Information Services, Jean McMahon.
“The one thread running through all of the pages is love - love of home, love of family, and how love is shown through preparing and sharing food, with family, friends, colleagues, patients, and community,” she said.
Senior Biomedical Scientist
Lissy Durhuus Ryan, who is from the Faroe Islands, gave her family recipe for Faroese Apple Cake, explained, “When you get married in the Faroe Islands, you take out an ad in the local paper and ask people to RSVP to let you know if they would like to attend. It’s not unusual for a wedding to have several hundred guests.” HM
Director (NSD) or relevant training body.
Bernard Gloster CEO, HSE, said, “NCHDs represent approximately 5% of the HSE workforce and their wellbeing is vitally important. This is a very significant service development, with benefits for our doctors and our patients as a result. The Hub is one of the recommendations of the Department of Health National Taskforce on NCHD Workforce 2023, with the final report due to be published this year.”
Anne Marie Hoey, National Director of HR, explained, “This development follows identification of the requirement to provide this support for the health of the NCHD workforce, who are a transient group within our health service and will benefit from access to one Hub when they require to access it.
The NCHD Health and Wellbeing Hub will provide enhanced case management for NCHDs, who rotate annually from one site to another, many up to four times per year. Additionally the service will be networked to all training sites around the country. For further details see https://healthservice.hse. ie/staff/benefits-and-services/nchd-hub/ Email: nchd.hub@hse.ie
Health | 79 HEALTH MATTERS SPRING 2024




Listowel staff ‘take 30’ to relax and recharge
As part of promoting positivity at work, staff in CHN1 North Kerry are availing of their 30 minutes Health and Wellbeing time once a week to walk, meditate, run, or have a coffee. In Listowel Primary Care Centre, staff went one step further and set up a dedicated Wellness Room.
While discussing what the team like to do during this valuable time, it became apparent that it was difficult to find a space that was quiet enough for them to enjoy such activities as reading, meditating, or just listening to music in a quiet room. This sparked the idea that a positive addition to the centre would be an allocated space for quietness and relaxation.
The Wellness Room is a quiet space where staff can go to if they are feeling unwell, stressed, or just need some time out. Escaping for a few minutes can allow the brain time to relax and recharge; improving overall motivation and increasing productivity.
Staff are delighted with their allocated space which features swinging egg chairs, blankets and cushions, a water fountain, a diffuser, books, plants and a sensory box.
More ideas come to light daily on how to improve the Wellness Room to suit everyone’s needs and there has been very positive feedback from all the staff availing of the area. HM
CUH culture of wellbeing supporting nursing students
The Nurse Practice Development Unit, in conjunction with Cork University Hospital (CUH) Staff Wellbeing Unit, has developed a mental health and wellbeing resource leaflet for nursing students.
Mental health in young people has been described as a societal crisis in recent years, with reports of rising numbers and increasing complexity in student presentations.
The information leaflet provides a number of resources offered through the HSE and University College Cork that may help students to better understand mental health and plan a self-care journey when the need may arise.
CUH nursing students receive this leaflet at the commencement of each academic year and it is available to them at any time from their Clinical Placement Coordinators and Allocations Liaison Officers.
This resource signposts nursing students towards the promotion of good mental health, as well as information on mental ill-health prevention and early intervention, as promoted in Sharing a Vision: A Mental Health Policy for Everyone.
Charlie Mackesy, author of the The Boy, the Mole, the Fox and the Horse, gave permission for the front cover illustration to be used as the theme of the leaflet fit well with the themes in his famous book.
HEALTH MATTERS SPRING 2024 80 |
We’re taking climate action
We’re taking action across the health service on:
1 Sustainable Buildings and the Green Environment
4 Greener Models of Healthcare
3 Sustainable Procurement
2 Transport and Mobility
5 Water and Waste Management
6 Adaptation and Resilience
Scan the QR code
Or go to hse.ie/climateandhealth #ClimateAction