













Digital
Cyber
Data
Screening




















































Digital
Cyber
Data
Screening





































1 How autism awareness training can help us all better understand people’s needs
2 We chat to members of Le Chéile to learn how the HSE network supports employees with disabilities, neurodiverse conditions and long-term health conditions
4 Scéal Le Chéile as Gaeilge
6 A look at disability day services and palliative care
7 NiSRP updates
8 Spotlight on climate action
11 Improving our culture in the HSE
12 Every second counts: Siobhán McGrath shares her experience of stroke at 34
14 Protect yourself and those you care for this winter: the latest on vaccines and antimicrobial resistance
16 Updates from HSE Dublin and South East
22 Digital for Care
26 Updates from HSE South West
32 In focus: policies and guidelines
35 Help protect against threats with the new cyber security awareness training
36 Updates from HSE Mid West
42 Spotlight on screening
44 How to avoid common postal data breaches
45 Competition: Share a snap of Health Matters and be in with a chance of winning a €100 One4all voucher
46 Updates from HSE Dublin and North East
52 Highlights from the Integrated Healthcare Conference 2025
56 Updates from HSE West and North West
62 Meet the winners of the Health Service Excellence Awards 2025
65 In focus: Vaping and teens
66 Updates from HSE Dublin and Midlands
72 In other news… Updates, events, collaborations, celebrations and milestones













Welcome to the winter issue of Health Matters. As we look back on a busy 2025 and anticipate the start of 2026, now is the perfect time to pause, take some time out from the frantic pace this season can bring and reflect on our achievements over the last 12 months, before setting new ambitions for the year ahead. Learn about the winners of this year’s Health Service Excellence Awards on page 62, while on page 52 you can check out the poster winners from the Integrated Healthcare Conference 2025.
As we look back on International Day of Persons with Disabilities on 3 December, it’s important to remember that celebrating our differences, making room for everyone and finding out how we can all better support each other’s needs is something we should strive for all year round. On page 2, we catch up with three members of Le Chéile to find out how the network has brought them a sense of support and community (and if you’d like to read this story in Irish, you’ll find this piece as Gaeilge on page 4). You can also find out how autism awareness training can further your understanding of neurodiversity on page 1.
In this edition, we also look to raise awareness of some of the issues facing service users nationwide. On page 12, Siobhán McGrath tells how seeking immediate care was crucial to her recovery from stroke at the age of 34. While on page 65, we look at the rise of vaping amongst teenagers, the signs to watch for and practical advice for parents.
Winter is a time when we’re likely to see a rise in cases of flu and COVID-19. Find out how you can protect yourself and others on page 14. Of course, protection extends beyond vaccines and on page 44, we outline the steps to take




On the cover: From


Dr Emer Rutledge, Consultant Psychiatrist, Open Dialogue


Clinical Lead and Siún O’Connor, service user representative, Louth Meath Mental Health Service, HSE Dublin and North East


to avoid postal data breaches, while on page 35 we highlight how cyber security awareness training can ensure you’re up to date on how to shield yourself –and everyone else – from a cyberattack. The last year has seen great work being done across the health regions. Turn to pages 16, 26, 36, 46, 56 and 66 to catch up on all the news from the six health regions. Elsewhere, we focus on disability day services and palliative care (page 6), NiSRP (page 7), climate action (page 8), organisational culture (page 11), Digital for Care (page 22), policy and guidelines (page 32) and screening (page 42).
We hope you find inspiration throughout this issue and that you’ll share your feedback with us (check out our reader competition on page 45 and learn how you could be in with a chance to win a €100 One4all voucher).
Wishing you all a wonderful festive season and a very happy new year.
Meg Walker Editor


Thank you to everyone who has submitted stories for this edition. If you would like to see your initiative or work featured, you can submit your ideas through our online form at bit.ly/HealthMattersForm is prohibited. © Ashville Media Group 2025.






All rights reserved. Every care has been taken to ensure the information contained in this magazine is accurate. The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher



Autism awareness training helps us all better understand people’s needs




“Autism is not an illness, it’s not a disease, it’s a difference,” says Grainne Morrison, Public Health Nurse in Kildare and West Wicklow Integrated Healthcare Areas and mother of three boys. Grainne is well placed to know this as two of her boys are autistic, one has another type of neurodiversity and Grainne herself is autistic.
Grainne is one of the presenters of the HSE autism awareness training. There are three training videos, developed with individuals with lived experience, subject matter expertise and clinical insight. The training is designed to support all HSE staff and service providers in their understanding of and communication with autistic and neurodiverse people.
The training explains what autism and neurodiversity are, along with the varied nature of autistic sensory perception and communication. It outlines how we can make work and healthcare environments more autisticfriendly, and use a rights-based, neuro-affirmative and person-centred approach.
Sensory perception and regulation are central to the experience of autistic people, as many have heightened or different sensitivities. Sarah Jane Lavin is autistic and has an intellectual disability. She explained how a quiet room and some quiet time before an appointment is helpful for her to get the most out of it.
Eoin O’Cathasaigh is autistic and non-speaking. Eoin is currently studying history and literature. He outlined his experience of communicating by using an alphabet board. He explained when healthcare providers talk to his mother Catherine instead of him, it’s because they
think he can’t communicate or understand what they’re saying. It makes him feel non-human. His message for healthcare providers is, “We understand everything and more.”
All the contributors with lived experience outlined one thing that has made a difference to them when accessing healthcare. Jane O’Sullivan, Anaesthetist, has autistic family members and has done autism research. She explained how using the SPACE framework can help heathcare professionals to adapt their work environment and be sensitive to the needs of autistic people.
The autism awareness training emphasises that good services for autistic people benefit everyone. Every person – including those with autism – is unique and autism is not necessarily a distinct experience, but it can often overlap with other conditions and experiences.
The Service Improvement Programme for the Autistic Community – a cross-sectoral programme working across disability, primary care and mental health services –developed these modules through a process of co-design. From ideation to identifying content, planning, presenting and reviewing the training, autistic people were central in its co-production. Several of the autistic presenters in the videos are health service staff, highlighting that this training is not about “them”, it’s about all of us.
Over 4,000 staff have already completed the training, with 88% saying they would recommend it to others, and 83% agreeing that it had given them new practical skills.
To access the training, log in to HSeLanD and search the course catalogue for “autism awareness training”.

As we look back on another important celebration of International Day of Persons with Disabilities on 3 December, we catch up with three members of Le Chéile. An Irish word meaning “together”, this is the HSE network for employees with disabilities, neurodiverse conditions and long-term health conditions, and their allies.
I’ve known I was autistic since I was 10, and I’ve always been very open about it. Throughout my life, I’ve taken any opportunity to get to know other people in the disability community and learn more from them, and to raise awareness about people with disabilities. I recently joined Le Chéile to meet other people like me and also, not like me. I’ve enjoyed listening to other members at the meetings. Knowing there are other people like me elsewhere in the HSE has been very reassuring. And learning more about the experiences of people with other disabilities or longterm health conditions has been really insightful. I also find being a member offers the chance to start a conversation in the workplace – about disability awareness in general and more specifically, my own circumstances.
For anyone thinking of joining Le Chéile, I’d say it’s definitely worth a try and if you’re unsure, just sit in on a meeting or sign up to the newsletter to learn what the network is up
to. If you have a story to share, even an indirect experience – say if you have a family member or partner with a disability, neurodiversity or long-term health condition, that’s an interesting perspective others can benefit from hearing.
Speaking as someone with an invisible disability – because disability is so broad, and I can never speak on behalf of someone with a physical disability or chronic health condition because that’s not my lived experience – the biggest barrier I’m coming up against at work and in my personal life is the assumption that everything’s fine. Just because someone looks physically able doesn’t mean they’re not struggling. I would love for people to lead with kindness and understanding. If someone is having trouble with a colleague at work, take a moment to think, could they be going through something? Are they having a hard time for a reason? Is there something I’m not seeing? We all need to be more inclusive and open to others’ perspectives.
As someone who’s lived with a stammer my whole life, I can tell you, stammering has nothing to do with a person’s intellectual quotient nor is it a learning disability or a psychiatric issue. It’s the one disability that is sometimes treated like a personal failure, and this needs to change with more education around it. Stammering needs to be normalised more within the workplace, too. It should never be considered abnormal for a person with a stammer to answer a phone or chair a meeting. Being a member of Le Chéile has helped me to better understand a broad range of disabilities and the experiences of other colleagues in the HSE. It’s wonderful to have that support network, too, to discuss any issues you may be having.
“It’s the one disability that is sometimes treated like a personal failure, and this needs to change with more education around it.”

Gráinne Leach is Diversity, Equality and Inclusion Officer for the HSE
I have worked in the HSE for many years and was Chief Officer for the National Haemophilia Council for 11 years before recently joining the Diversity, Equality and Inclusion (DEI) team. Forty years ago, I was hit by a bus while riding my bike, an accident which led to my right arm being amputated along with multiple injuries. I was 22, lucky to be alive, but my life was forever altered. My confidence was shattered. Back then, there was no counselling offered to support my mental health after the accident. I felt very isolated and alone for a long time. It was tough and very challenging. I’ve had to advocate for myself and work really hard both in my work and personal life. I have four children who are all now grown but let me tell you, changing nappies with one arm isn’t easy. I try to wear my resilience hat as much as I can, every day.

I’ve been a member of Le Chéile since the network began two years ago. I listen to other members’ stories, and I understand their frustrations. It’s a great network of like-minded people. The DEI team do phenomenal work for the various networks, supporting people with different challenges and needs on a daily basis. I’d encourage anyone thinking of joining Le Chéile or any other network to do so. I’d also like to see more managers get involved in their local networks, so they can better support their teams. There are so many of us who struggle in various ways, whether it’s a physical disability or an invisible disability or health condition you cannot see. Be kind, show people dignity and respect, and do what you can to help others get through the day. I’ve seen things change a lot in the last four decades since my accident – there’s greater acceptance and inclusion, and discussion around mental health, but we can still improve further and we all need to do our part. Connect, engage, don’t be afraid to speak up, and reach out to others. International Day of Persons with Disabilities is a day of celebration – of how far we’ve come, our differences, and what makes us all unique.

Damien McCallion, Príomhoifigeach Teicneolaíochta agus Claochlaithe agus Leas-POF; Anne Marie Hoey, Príomhoifigeach Daoine; comhaltaí den fhoireann Éagsúlachta, Comhionannais agus Cuimsithe agus ceannairí sinsearacha ag teacht le chéile le baill Le Chéile chun Lá Idirnáisiúnta na nDaoine faoi Mhíchumas na bliana seo a cheiliúradh.
Agus muid ag féachaint siar ar cheiliúradh tábhachtach eile ar Lá Idirnáisiúnta na nDaoine faoi Mhíchumas ar an 3 Nollaig, buailfimid isteach ar triúr ball den líonra ‘Le Chéile’. Is é ‘Le Chéile’ an líonra atá ag FSS do na fostaithe siúd atá faoi mhíchumas, ar a bhfuil riochtaí néara-éagsúla agus riochtaí fadtéarmacha sláinte, agus a gcuid comhghuaillithe.
í Meagan McGlynn in FSS an Iardheiscirt
Bhí a fhíos agam go raibh uathachas orm ó bhí mé 10 mbliana d'aois, agus bhí mé an-oscailte faoi i gcónaí. I gcaitheamh mo shaoil, thapaigh mé aon deis chun aithne a chur ar dhaoine eile sa phobal atá faoi mhíchumas agus chun tuilleadh a fhoghlaim uathu, agus chun feasacht a mhúscailt faoi dhaoine atá faoi mhíchumas. Ghlac mé páirt in Le Chéile le déanaí chun bualadh le daoine eile atá cosúil liomsa, agus atá éagsúil freisin. Bhain mé taitneamh as éisteacht le baill eile ag na cruinnithe. Chuir sé go mór ar mo shuaimhneas mé aithne a chur ar dhaoine eile atá cosúil liomsa atá ag obair i rannóga eile in FSS. Agus bhain mé léargas mór as tuilleadh a fháil amach faoin gcaoi a n-éiríonn le daoine ar a bhfuil míchumais eile nó fadhbanna fadtéarmacha sláinte eile. Tugaim faoi deara freisin gurb ionann mo bhallraíocht agus deis dom tús a chur le comhrá san áit oibre – faoin bhfeasacht maidir le míchumas i gcoitinne agus faoi mo chúinsí sonracha féin. Molaimse do dhuine atá smaoineamh ar pháirt a ghlacadh in Le Chéile, gur cinnte gur fiú triail a bhaint as, agus mura bhfuil tú cinnte faoi, suigh isteach ag cruinniú nó liostáil leis an nuachtlitir chun foghlaim faoina bhfuil ar bun ag an líonra.
Má tá scéal le roinnt agat, fiú más eispéireas indíreach é – abair má tá ball teaghlaigh nó páirtí agat atá faoi mhíchumas, nó atá néara-éagsúil nó ag a bhfuil fadhb fhadtéarmach sláinte, is dearcadh suimiúil é sin a bhféadfadh daoine eile leas a bhaint as.
Agus mé ag labhairt mar dhuine atá faoi mhíchumas dofheicthe – de bharr leithead na míchumas éagsúil agus toisc nach mbeadh sé ceart ná cóir dom a bheith ag labhairt thar ceann duine le míchumas coirp nó riocht ainsealach sláinte, mar ní hé sin mo thaithí ar an saol – is é an bac is mó a bhíonn romham ag an obair agus i mo shaol pearsanta ná daoine ag glacadh leis go bhfuil gach rud go breá. Fiú má tá an chuma ar an duine go bhfuil sé breá ábalta, ní hé sin le rá nach bhfuil sé ag streachailt. Ba bhreá liom dá dtabharfadh daoine tosaíocht don chineáltas agus don tuiscint. Má tá achrann ag duine lena chomhghleacaí ag an obair, smaoinigh nóiméad ar na cúinsí a d'fhéadfadh a bheith ag luí go trom ar a shaol. An bhfuil rud éigin á chrá ar chúis shonrach? An bhfuil rud ann nach bhfeicimse a scáil? Caithfimid go léir a bheith ionchuimsitheach agus oscailte i leith dearcthaí daoine eile.
Cléireachais í
Bhainisteoir Limistéar
Comhtháite Cúraim
Sláinte, Cill Dara agus
Cill Mhantáin Thiar
Toisc go bhfuil stad i mo chuid cainte ó bhí mé sa chliabhán, is féidir liom a rá leat go cinnte nach bhfuil baint ar bith ag an stadaireacht le héirim ná le heagna duine, ná ní míchumas foghlama ná fadhb shíciatrach í ach an oiread. Is é an t-aon mhíchumas atá ann a gcaitear leis mar theip phearsanta in amanna, agus caithfear an dearcadh sin a athrú trí oideachas. Ní mór normalú a dhéanamh ar an stadaireacht san áit oibre freisin. Níor cheart a mheas in aon chás nach bhfuil duine a bhfuil stad ina chuid cainte in ann glaonna fóin a fhreagairt ná cathaoirleacht a dhéanamh ar chruinniú. Bhí mo bhallraíocht in Le Chéile ina cuidiú agam tuiscint níos fearr a fháil ar réimse leathan míchumas agus fáil amach faoi na heispéiris ag comhghleacaithe eile in FSS. Is iontach an rud é gurb ann dá leithéid de líonra tacaíochta freisin toisc gur áit iontach é le plé a dhéanamh ar aon fhadhb a d'fhéadfadh a bheith ag duine.

Tá mé ag obair in FSS leis na blianta, agus bhí mé i mo Phríomhoifigeach don Chomhairle Náisiúnta um Haemaifilia ar feadh 11 bhliain roimhe sin, sular ghlac mé le post le déanaí ar an bhFoireann Comhionannais, Éagsúlachta agus Ionchuimsithe. Daichead bliain ó shin, bhuail bus mé agus mé ag rothaíocht, tionóisc ar dá barr ar teascadh mo lámh dheas, gan trácht ar chuid mhaith gortuithe eile. Bhí mé 22 bhliain d'aois, bhí an t-ádh liom nár maraíodh mé, ach ní bheadh mo shaol mar an gcéanna riamh. Bhí mo mhuinín ionam féin scriosta. Ní raibh aon chomhairleoireacht á tairiscint sa ré úd chun tacú le mo mheabhairshláinte tar éis na tionóisce. D'airigh mé scoite amach ón saol agus fágtha i m'aonar ar feadh i bhfad. Cás crua agus fíordhúshlánanach domsa é. B'éigean dom labhairt amach ar mo shon féin agus obair go fíorchrua i mo shaol oibre agus pearsanta araon. Tá ceathrar clainne agam atá lánfhásta go léir anois, ach táimse á rá leat, nárbh aon dóithín é clúidíní a fhriotháil le leathlámh. Déanaimse iarracht a bheith chomh hathléimneach agus is féidir liom, gach lá beo.

Táim i mo bhall den líonra Le Chéile ó cuireadh tús leis dhá bhliain ó shin. Éistimse le scéalta ó na baill eile, agus tuigim na dúshláin atá acu ina saol. Is líonra iontach é atá lán le daoine comhchosúla. Déanann an fhoireann comhionannais, éagsúlachta agus ionchuimsithe obair na gcapall ar son na líonraí éagsúla, agus iad ag tacú le daoine a bhfuil dúshláin agus riachtanais dhifriúla acu ó lá go lá. Thabharfainn spreagadh do dhuine ar bith páirt a ghlacadh in Le Chéile nó in aon líonra eile de chuid FSS. Ba mhaith liom freisin go nglacfadh tuilleadh bainisteoirí páirt ina líonraí áitiúla, le gur féidir leo tacaíocht níos fearr a thabhairt dá bhfoirne. Tá an oiread sin daoine ann a bhíonn ag streachailt leo ar bhealaí éagsúla, bíodh sé faoi mhíchumas coirp nó míchumas dofheicthe nó riocht sláinte dofheicthe. Is é an chomhairle atá agam duit a bheith cineálta, dínit agus urraim a léiriú do dhaoine, agus do chuid féin a dhéanamh chun cabhrú le daoine eile a gcuid gnóthaí laethúla a chur i gcrích. Chonacthas an oiread sin athruithe ar chúrsaí le dhá scór bliain anuas ó bhain an tionóisc domsa – tá glacadh níos mó le daoine faoi mhíchumas anois, agus pléitear an mheabhairshláinte, ach is féidir linn go léir feabhsú tuilleadh agus ár gcion féin a dhéanamh. Cruthaigh naisc, bí páirteach, ná bíodh leisce ort labhairt amach ná lámh a shíneadh le daoine eile. Lá ceiliúrtha is ea Lá Idirnáisiúnta na nDaoine faoi Mhíchumais – ar a bhfuil bainte amach, ar ár ndifríochtaí, agus ar na rudaí a fhágann nach ionann an cás ag aon dá bheirt.
Across Ireland, over 21,600 people with disabilities avail of HSE-funded adult day services. Day services aim to support people to live meaningful lives and be active members of their communities.
The HSE National Office for Adult Day Services are partnering with people who receive day service supports, the service providers, the National Disability Authority, and ACE Communications to co-design a way of evaluating and supporting the quality improvement of day service supports and outcomes. This work set out to ensure that people who receive day service supports shape the monitoring system. People supported are central in developing the monitoring system and are working as assessors with lived experience within the monitoring team during a trial to co-design the monitoring system. The development of this

assessor role provides a strong model for embedding lived experience across a range of HSE services.
This approach has shown that when people are meaningfully involved from the beginning, evaluating the quality of services becomes less about compliance and
New plan aims to deliver timely, high-quality palliative
The publication of the HSE National Adult Palliative Care Policy Implementation Plan 2025–2026 will ensure that more people who need palliative care will receive a timely and high-quality service at home or as close to home as possible. In 2024, specialist palliative care teams treated 17,239 patients in hospital, 4,395 patients at a hospice and 15,253 patients in their own place of residence.
The Implementation Plan, which was developed with stakeholders from the statutory, voluntary and community sectors, includes measures to strengthen public understanding of palliative care, develop new hospice facilities, increase the palliative care workforce and deliver more palliative care education to healthcare professionals.
“The inclusion of patient voices in the development of policies impacting them is vital to the delivery of high-quality, person-centred care,” says Will Higgins,
more about making sure that what matters most to people is at the centre of improving services. Together, these efforts move beyond consultation toward meaningful partnership and co-creation, offering a template for broader use across health and social care systems.
member of Voices4Care, the All Ireland Institute of Hospice and Palliative Care’s volunteer group. “We are grateful for the opportunity to contribute the lived experiences of people receiving palliative care to the development of the Implementation Plan that will enhance accessibility and quality of these essential care services.”
Dr Feargal Twomey, HSE Clinical Lead for Palliative Care adds, “I invite the public, the patients we meet and their families, and all healthcare professionals to actively join and share in the work of recognising our patients’ palliative care needs at the earliest opportunity to ensure they can receive the right palliative care, in the right place, and at the right time for them.”
For more information, visit bit.ly/PalliativeCarePIP
Since April 2025, all statutory HSE areas are now live on the SAP HR and Payroll System. This one system for all brings many benefits to all staff, from managers and employees to retirees. The National integrated Staff Records and Pay Programme (NiSRP) asked some users about their experiences:
What do you like about SAP HR and Payroll in addition to HR and Payroll Self Service?
I find the leave planning, the simplicity of applying for travel claims and having all the documentation very useful. In relation to SAP HR and Payroll, the level of data provided to us has been phenomenal compared to what was available previously. To be able to have accurate, reliable data for planning and forecasting is really important from a financial perspective. Having a data-driven system that provides real-time data on what your payroll consists of is very powerful.

What do you like about HR and Payroll Self Service?

I really like how easy and convenient it is. I can view my payslip, update my personal details like bank details without any paper forms. It’s processed much faster. We’re moving with the times. There’s less duplication and fewer mistakes, everything flows more smoothly, and it’s saving time, so it’s a much better experience for everyone.
Overall, how would you rate the support and success of the implementation?
We had great communication from the NiSRP team, who were available to us for any issues or concerns we had along the way. They were very helpful with queries. Their communication was excellent. I think the implementation went really well. It was a great success for the West and North West.
Overall, how would you rate the support and success of the implementation?
The team were very responsive whenever I raised an issue. There was a lot of reinforcement of messages and engagement locally. I’d hold up the sort of change model that the NiSRP team had as a really good example in terms of how to engage. They were determined to get things right. The experience, the determination, it really was impressive.
Where we’re at as of 2025…
155k employees and pensioners transitioned from legacy systems to a single, supported payroll system
Registration for the new technology exceeded 90% within weeks of the most recent region’s go-live
Over 1.5m transactions are made each year on employee self-service
700k online travel expenses are processed each year



Over 130k staff hours are saved across the health system per annum
Find HR and Payroll Self Service modules at hseland.ie
For more information about NiSRP visit hse.ie/nisrp
The awards recognised initiatives, collaborations and scalable solutions driving progress on climate action and environmental stewardship.
Winner: Cork University Hospital (CUH) for its remanufactured electrosurgical devices, which reduce the environmental impact of surgery at CUH and Cork University Maternity Hospital (CUMH).
Runner-up: Our Lady Of Lourdes Hospital, Drogheda for food waste reduction using AI technology.


Above: Aidan Turley, Chair of HSE Waste Programme with Dr Sean Owens, accepting on behalf of Dr Cathy Burke and the team at Cork University Hospital (winner: Sustainable Waste Management). Left: Aidan Turley with Sharon Gallagher, Elizabeth King and Kate Barlow at Positive Carbon, who partnered with Our Lady of Lourdes Hospital (runner-up).
Winner: Tallaght University Hospital for its green inhaler project
Runner-up: Tallaght University Hospital for its Spark-funded My Green Lab.
Dr Philip Crowley, Iarlaith Doherty, Dr Ana Rakovac and Siobhan Power, Spark Innovation Programme (winner: Greener Models of Care). Below: Kevin Sheridan, HSE Estates Manager with Maura Beegan, Eileen Burke, Samuel Awe and Siobhan Power, Spark Innovation Programme (winner: Buildings and Green Environments). Buildings and Green Environments
Winner: Maynooth Community Care Unit for social care –sustainability and climate action in older person services.
Runner-up: North Dublin Mental Health Service and St Joseph’s Intellectual Disability Service for Detect, Repair, Save: A Strategic Water Conservation Project at St Ita’s Campus.



We’re taking climate action – the time is now Conference highlights urgent need to build a more sustainable healthcare system

Planetary health means protecting both people and the environment we depend on. The healthcare sector has a key role to play in this. In addition, because Ireland is vulnerable to unstable energy markets, it’s urgent that we move towards a lowercarbon, renewable energy system.
In 2024, the HSE and the Climate and Health Alliance asked partner organisations for a joint declaration of action on planetary health; 33 organisations (hospitals, colleges, NGOs, charities and other community groups) have signed this charter. There has been a lot of activity from individuals and organisations: frameworks and toolkits, research output and audits, initiatives and interest groups.
The HSE Climate and Sustainability Programme recently partnered with the Climate and Health Alliance and HSE Spark Innovation Programme to host a second conference with a number of speakers sharing learnings and insights.
Planetary health means protecting both people and the environment we depend on. The healthcare sector has a key role to play in this.

Climate change presents a fundamental threat to human health. It affects the physical environment as well as all aspects of natural and human systems; including social and economic conditions and the functioning of health systems.
In line with the Climate Action Strategy 2023–2050 and the Government Climate Action Plan, the HSE has developed a number of framework documents. Drafted in collaboration with expert working groups, the frameworks focus on priority areas including transport, mobility, greener environments and spaces, waste, water, sustainable procurement and greener models of healthcare.
Each framework document includes key building blocks for each area, implementation guidance from a national and local perspective and best practice examples. They will help regional and local green teams in implementing this work.











From 9–10 September, HSE Capital and Estates hosted over 20 project partners from the Interreg Europe DAPHNE (Decarbonising Healthcare in EU Regions) Project. At this interregional learning event, HSE Capital and Estates Sustainable Infrastructure Office shared learnings with project partners in relation to the HSE’s approach to energy and carbon reduction, data gathering, information systems, achievement of ISO 50001 certification and the HSE’s meter improvement project in order to enhance the capacity of national, regional and local authorities in designing and implementing better policies to decarbonise the healthcare sector.
On 10 September, partners participated in a study visit to St Brigid’s Hospital in Ardee who, with support from HSE Capital and Estates Energy Bureau, have implemented a range of energy improvement projects and are on track to meet 2030 energy-related carbon reduction targets five years early.
The HSE are one of ten organisations from seven EU countries participating in the DAPHNE Project.














































































As part of the HSE’s commitment to creating a healthier future by reducing the environmental impact of healthcare, the HSE Climate and Sustainability Programme has launched the Climate and Sustainability Learning Hub. The aim is to connect environmental responsibility and promote sustainability with the delivery of safe, effective and equitable patient care. The Climate and Sustainability Learning Hub can be found on HSeLanD under Hubs and Resources.
Find out more at interregeurope.eu/daphne Find out more at hseland.ie
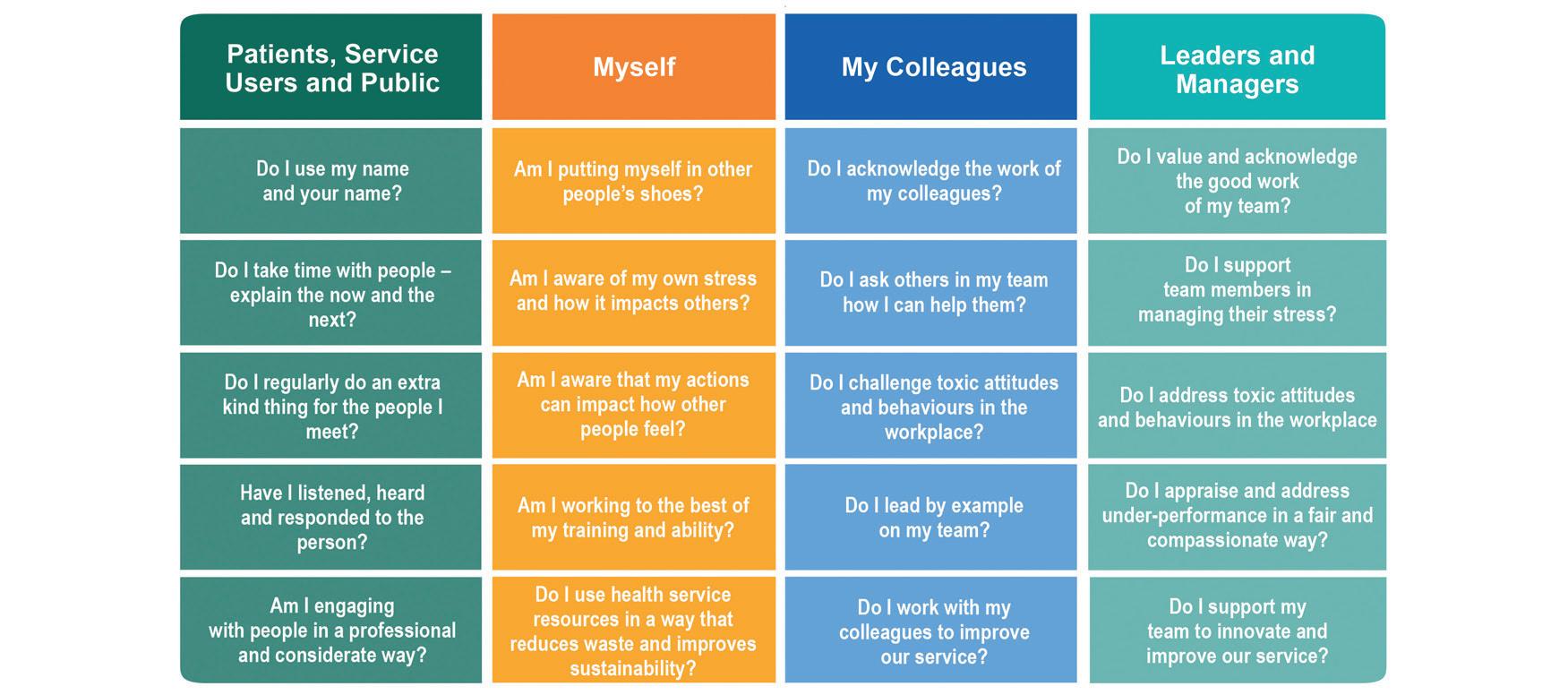
You’d be hard-pressed to attend a health event or read a recent health service report or policy without encountering frequent references to the importance of culture. Yet despite its widespread mention, culture is often left undefined, with its meaning varying depending on the context in which it is discussed.
The recently published Enabling Framework for Organisational Culture aims to provide guidance and outline a clear pathway for individuals, teams, services and regions to follow as they work to cultivate the kind of culture we want to see across health services.
public’s confidence in our services.”
Joe Ryan, National Director HSE Public Involvement, Culture and Risk Management is committed to supporting every area in the organisation to find its own way to the desired culture. “Organisational culture is not a static concept,” he says. “It is dynamic and lived –reflected in how we interact with each other, how we care for patients, how we respond to challenges, and how we lead. It influences the quality of care, the wellbeing of our workforce, and the
Professor Michael West is a valued contributor to the framework and has inputted his expertise into the culture work in the HSE. In developing the framework, he was keen to point out the importance of values, behaviour and teamwork in achieving a high-performing culture in healthcare: “The health service is made up of teams, and its overall
culture reflects the culture of those teams. By committing to our values and showing the right behaviours, health services can create safe, high-performing teams and make the desired culture the norm.”
Each region of the health service is actively working on its own culture development plan and it is expected that we will see these plans completed throughout 2026.
The Enabling Framework for Organisational Culture is available at bit.ly/EnablingFramework
Over recent months, HSE Organisation Development and Design (OD&D) has collaborated with system integrators to develop the Model for Integration, a practical, evidence-informed framework designed to support teams in delivering more integrated, person-centred care. Adapted from the SCIE Logic Model for Integrated Care (UK), it has been tailored specifically for the Irish health and social care context.
Following a call-out, eight diverse teams from across the country volunteered to test the model and its supporting resources. These include templates, prompt sheets and signposting to tools from the Health Services Change Guide, along with an introductory webinar and instructional videos.
The “test and refine” programme offers a unique opportunity for participants to co-design a national resource. Over eight weeks, participating teams engage in shared learning sessions facilitated by OD&D, creating space to exchange insights and learn from each other’s experiences. This initiative marks the first in a suite of team-based resources to support integrated care. Once refined, the Model for Integration will be rolled out nationally in 2026, with additional resources currently in development.
To find out more, see linktr.ee/hsechangeguide

As Siobhán McGrath discovered three years ago, just one symptom of stroke is enough of a sign that you need to act fast
Every year, around 7,500 people in Ireland experience a stroke. It’s the third leading cause of death and the single greatest cause of adult neurological disability. About 30,000 people in Ireland live with disabilities as a result of a stroke. The Irish National Audit of Stroke (INAS) found that in 2014, 73% of stroke patients reached hospital within the vital 4.5-hour window. By 2021, this figure had fallen to 58%, reducing opportunities for timely, effective treatment. The HSE’s latest campaign aims to increase awareness of the importance of acting quickly and the key symptoms to look for.
Professor Rónán Collins, HSE National Clinical Lead for Stroke says, “Every second counts when it comes to stroke. We know that public awareness of the symptoms has improved thanks to previous FAST campaigns, but many people still hesitate before calling an ambulance. This new
campaign is designed to close that gap – to make sure the second you suspect a stroke is the second you dial 999 or 112.Doing so saves lives and reduces disability.”
Siobhán McGrath (37) was a fit and healthy Dublin senior football team player when she had a stroke three years ago. “I awoke that morning feeling lethargic. Trying to get dressed, my fingers were going in different directions, I had numb feelings down my arms and I was getting confused. I tried to open a window to get some air, and couldn’t grip the handles. Pulling at the window set off my house alarm so I went downstairs to turn it off, but couldn’t enter the code in the right sequence.
“I knew something was wrong and this could be a stroke. I went to the mirror but my face looked fine. I tried talking to myself and the words came out all gibberish. I knew I needed to call someone, but had trouble unlocking my

phone and getting a sentence out. I finally called my mam. She could tell I needed her to come straight over. At this stage, it had been 20 minutes since my symptoms started and by the time my mam arrived, they subsided a bit.
I had to think about what I was trying to say, but was able to formulate a sentence. So I thought I overreacted, that it was a blip.
“My advice to anyone is, when there is just one of the symptoms, you need to act fast. Don’t wait. One sign means you need to ring for an ambulance.”
“I went to the doctor two hours later. He ran the main tests, and I wasn’t showing signs anymore, but he did think it was very weird so wrote a letter and sent me to A&E. I had more tests there, and then an MRI showed I had a change in the brain. I was like, is this really happening? Once I was in the stroke ward, the realisation sunk in, and I considered myself extremely lucky.”
Siobhán is now fully recovered and recently had a baby girl. “It turned out I had a hole in my heart. Although there’s no guarantee that’s what contributed to it, no other reason came to mind for why I would have had a stroke, considering my circumstances and lifestyle, and everything else showed up clear. I had the hole closed up so the risk of me having another stroke is greatly reduced. I returned to normal life as quickly as I could for my own mental state and went back to playing football. My advice to anyone is, when there is just one of the symptoms, you need to act fast. Don’t wait. One sign means you need to ring for an ambulance. Also, educate everyone around you about the signs to look for, and that stroke can happen at any time – to anybody.”
• Face – has the face drooped or become weak on one side?
• Arm – has an arm become suddenly weak or clumsy on one side?
• Speech – has speech suddenly become slurred or confused in nature?
• Time – time to act FAST: phone 999 or 112 for an ambulance immediately.
If you work in a healthcare setting, you’re at high risk of being exposed to respiratory viruses including flu and COVID-19. The flu vaccine is strongly recommended for all healthcare workers. Getting the flu vaccine will provide you with the best available protection against the serious complications of flu. Getting vaccinated will also reduce the chance of spreading the flu infection to family members, colleagues and patients, many of whom may be more vulnerable to serious complications.
As a healthcare worker, the COVID-19 vaccine is recommended if you are aged 60 years and older or if you have an underlying medical condition that puts you at risk of severe illness. Any healthcare worker who wants a COVID-19 vaccine can get one. Flu and COVID-19 vaccines may be available where you work. They’re also available for free from GPs and pharmacies.
Find your local staff vaccination clinic at hse.ie/staffclinics
Antibiotics are life-saving drugs. We’ve become reliant on antibiotics to treat or prevent infection during routine or critical surgery (e.g. transplants), cancer treatments and many illnesses. Unfortunately, antibiotics that once worked well to treat an infection no longer work as well or do not work at all. Bacteria (superbugs) have become resistant to different types of antibiotics; this is known as antimicrobial resistance (AMR) and is caused by overuse of antibiotics in people, animals and crops over many years.
As we mark 20 years of the National Immunisation Office (NIO), we have taken the opportunity to look back on the journey of vaccination in Ireland, what we have achieved together, and what still lies ahead.
Launched during World and European Immunisation Weeks 2025, the “Then and now: The power of vaccines” campaign was a tribute to both the science of immunisation and the people who deliver it. The campaign theme, aligned with the World Health Organization #HumanlyPossible message, highlighted the remarkable public health progress made possible through vaccines, and the continued work needed to protect future generations.
At its core, this campaign aimed to reconnect the public with the real-world impact of vaccines by showing how far we’ve come. Through digital storytelling, we showcased personal reflections, historical vaccine cards and voices from across the health service. These stories helped bridge the gap between the past and present, reminding people that the diseases vaccines protect us from were once common and devastating.
One of the most powerful moments in the campaign came from Dr Louise Marron, Public Health Consultant at the NIO. She shared her personal experience of being hospitalised with pertussis as a baby in the 1980s: “Vaccines prevent illness and save lives. It is a privilege to practise medicine in an era where vaccines mean there are many illnesses we no longer have to see, but we must not take that for granted.”
What can be done? Everyone can make a difference to address this growing threat.
• Use antibiotics only when prescribed, as prescribed. Finish the course and never reuse or share leftover antibiotics.
• Use good infection prevention control practices to prevent infections spreading and keep up to date with your vaccinations. If we prevent infection, we need antibiotics less. Hand hygiene is the most effective way to help prevent the spread of infection. It’s mandatory for all HSE staff and those working in HSE-funded
Her story captured the heart of the campaign, reminding us that the diseases we protect against are still real, and that trusted, evidence-based information is more important than ever. In an age where misinformation spreads easily online, stories like Dr Marron’s underscore the life-saving importance of vaccines and the vital role healthcare professionals play in guiding the public toward reliable sources like immunisation.ie
At the heart of this campaign were the public healthcare professionals and community partners who make Ireland’s immunisation programme possible. From those on the frontline, GPs, pharmacists, school vaccinators and general practice nurses, to the public health teams who ensure vaccines reach those who need them most, your expertise, leadership and dedication form the backbone of our national programme. The campaign also recognised those who drive vaccine awareness and education, helping to build public trust and understanding.
As the winter vaccine rollout continues, the message remains clear: vaccines work, and the people behind them matter. This season, our campaigns include flu, COVID-19, school vaccines and the introduction of the chickenpox vaccine to the primary childhood programme, ensuring comprehensive protection for all age groups.
Let us keep celebrating what is possible and continue to protect public health.
services. It’s important that all staff, not just those working in a clinical setting, understand infection prevention and complete the hand hygiene training on the AMRIC hub of HSeLanD.
AMR action plan:
The HSE’s action plan 2026–2030 was published on European Antibiotic Awareness Day in November in response to Ireland’s one health action plan, iNAP3. It sets out the HSE’s actions to address AMR. Details of the action plan are available at bit.ly/AMRactionplan
For information, visit bit.ly/HSEantibioticresistance

Riverside House Community Eating Disorder Services, a new hub for specialist community mental health services for children, adolescents and adults with eating disorders in the Dublin South and Wicklow healthcare area was officially opened by Mary Butler TD, Government Chief Whip and Minister for Mental Health in October.
A joint HSE and St John of God Community Mental Health purpose-built clinical facility, Riverside House Community Eating Disorder Services consolidates and expands on existing multi-disciplinary services and provides a co-location for two specialist outpatient teams for children, adolescents and adults experiencing eating disorders.
The adult eating disorder team was previously based at St Vincent’s University Hospital and the more recently developed child and adolescent eating disorder team was based at Lucena Clinic, Rathgar. At Riverside, the two teams will deliver evidence-based, specialist interventions within a stepped model of care, ensuring patients receive the right level of care and treatment at the right time.
The teams are part of the network of eating disorder teams recommended by the HSE Model of Care for Eating Disorder Services. They aim to provide safe, accessible and quality eating disorder services, leading to better clinical outcomes and recovery for service users.
Minister Butler praised the €5 million investment, calling Riverside House a “flagship for our developing national network of eating disorder services”. She highlighted the importance of early intervention and community-based care, noting that the national programme has grown from one team to 14, with over 100 clinicians now delivering specialist support across Ireland.
Aisling Heffernan with staff at the official opening of Riverside House Community Eating Disorder Services.
Key developments include:
• Specialist interventions: A range of evidencebased treatments, including specialist individual, family and group interventions, are available at this co-located service, which fosters a collaborative and multidisciplinary approach.
• Eating disorder day programme for adults: This new service provides intensive, structured treatment for individuals with severe eating disorders. It functions as a vital ‘step-up’ from routine outpatient care and, crucially, as a ‘stepdown’ for those leaving inpatient treatment.
• A lifespan approach: By having child, adolescent and adult services together, Riverside House will manage the critical transition from CAMHS to adult services. This integrated approach helps prevent patients from disengaging from treatment during a traditionally vulnerable period, ensuring continuity of care and improving long-term outcomes.
“Riverside House is more than a new building. It’s a vital new resource that will transform treatment for people with eating disorders in our healthcare area,” says Aisling Heffernan, Integrated Healthcare Area Manager, Dublin South and Wicklow. “It demonstrates our commitment to providing highquality, person-centred healthcare that is aligned with national clinical strategy. I am confident that this new service will lead to significant improved outcomes for our service users and their families.”
Minister for Health Jennifer Carroll MacNeill TD recently visited Carlow, where she was updated on development plans for several community facilities. She visited St Dympna’s Woodlands Garden Project, Kevlin Court, and the Sacred Heart Hospital. She was joined by Minister of State Jennifer Murnane O’Connor TD and Catherine Callaghan TD. The Ministers met with staff and joined patients for arts and crafts.

▲ Minister for Health, Jennifer Carroll MacNeill TD at the opening of the Medical 3 Ward at St Luke’s General Hospital, Carlow/Kilkenny, pictured with Regional Executive Officer Martina Queally; Roseanne Killeen, Integrated Healthcare Area Manager for Carlow Kilkenny and Tipperary South; Hospital Manager Niamh Lacey; Minister of State Jennifer Murnane O’Connor TD; local elected representatives and members of the Regional Health Forum.
The Health Minister also paid a visit to St Luke’s General Hospital, Carlow/Kilkenny to officially open the newly-refurbished Medical 3 Ward, adding 14 additional beds to facilitate winter surge capacity. She was welcomed by Regional Executive Officer Martina Queally, Roseanne Killeen, Integrated Healthcare Area Manager for Carlow Kilkenny and Tipperary South, and Hospital Manager Niamh Lacey.
St Vincent’s University Hospital (SVUH) was one of the lead global sites in a landmark clinical trial published in The New England Journal of Medicine that could transform how a rare and debilitating lung disease is treated in Ireland.
The IMPALA-2 trial, the largest and most comprehensive study ever conducted in autoimmune pulmonary alveolar proteinosis (autoimmune PAP), found that an inhaled therapy – molgramostim – significantly improves lung function, breathlessness and quality of life. Until now, the only treatment option has been whole lung lavage, an invasive procedure requiring general anaesthetic and hospitalisation. The new therapy offers a lifechanging alternative for patients in Ireland.
Led in Ireland by Professor Cormac McCarthy, Consultant Respiratory Physician at SVUH and Associate Professor at UCD, the trial signals a major breakthrough in how this life-limiting disease can be diagnosed and treated.


Professor Cormac McCarthy (second from right) with members of his team.

“St Vincent’s University Hospital was selected as a lead European site and played a key role in this landmark study,” says Professor McCarthy. “It shows that Ireland can lead on complex, rare disease research and most importantly, that patients in Ireland can benefit directly from global breakthroughs right here at home.”
This study would not have been possible without the expertise and support of the UCD Clinical Research Centre, which played a key role in enabling patient participation and trial delivery.
Catherine Daly, Senior Primary Care Occupational Therapist at the Memory Harbour, Clonskeagh, has received the prestigious Ann Beckett Award for her programme, Yellow Days at the recent Association of Occupational Therapists of Ireland (AOTI) annual conference. Yellow Days is a poetry group for people affected by memory impairments and dementia, developed in collaboration with the Dún LaoghaireRathdown County Council Arts Office. Over the course of the programme, group members were supported to write poems, which they then performed at a launch earlier this year. The programme supported their executive functioning, helped build their cognitive reserve, sparked their creativity and fostered meaningful social connections through occupation.
Staff of the new high-flow cataract operating theatre at its official opening at University Hospital Waterford.

University Hospital Waterford (UHW) recently celebrated the official opening of Theatre 9, a purpose-built cataract operating theatre complex. Although operational since 2023, the event marked the formal recognition of the theatre’s impact on eye care services in the South East.
Designed for high-volume, highefficiency cataract procedures, Theatre 9 has already facilitated approximately 2,400 surgeries, significantly improving access to timely treatment for patients across
the region. The theatre complex includes a pre-operative ward area where patients are prepped for local anaesthetic cataract procedures, an adjoining eye operating theatre where cataract surgeries are carried out under local anaesthetic, ancillary facilities and a recovery area.
Patrick Condon, retired Consultant Ophthalmic Surgeon said, “This theatre complex reflects our healthcare goals of shorter waiting lists, clinical excellence and provides greater access to patients
in the South East to care nearer their homes. I am proud to support UHW in delivering these important services that enhance patients’ quality of life.”
John Stokes, Consultant Ophthalmic Surgeon, UHW added, “The opening of this theatre has made a real difference to patients needing treatment and care in the South East. And it has been a welcome and much-needed addition to the great work being done by our eye team at the hospital.”
The HSE Dublin and South East’s staff vaccination campaign launched in October, with free staff clinics now taking place across the region. These clinics offer healthcare workers convenient access to flu and COVID-19 vaccines, helping protect themselves, their colleagues and the patients they care for. The response from staff so far has been positive, with many welcoming the convenience of on-site clinics and the opportunity to take proactive steps for their health. Whether you’re on the frontline or behind the scenes, your wellbeing matters – and vaccination is one of the simplest, most effective ways to stay protected.
Clinic locations and schedules are available at hse.ie/staff clinics
A new Activity Garden was opened on the grounds of St John’s Community Hospital in Enniscorthy.
The garden will be a multi-functional space for gatherings and health and wellbeing activities in the heart of the healthcare campus for residents, staff and visitors.
The Minister for Housing, Local Government and Heritage, James Browne TD, carried out the official opening, while Minister of State at the Department of Health with special responsibility for Public Health, Wellbeing and the National Drugs Strategy Jennifer Murnane
O’Connor TD was also a guest at the ceremony.
Speaking at the opening event, Dr Sinéad Reynolds, Integrated Healthcare Area Manager for Waterford Wexford said, “We are all looking forward to the Activity Garden enabling patients, their companions or visitors and HSE staff on site at the St John’s Community Hospital campus to enjoy some fresh air and, during fine weather, offering an opportunity for outdoor events and activities.”
The Activity Garden project was supported by Wexford County
Regional Executive Officer Martina Queally, together with the regional executive management team, senior managers, staff and our patient and service user partners from across the region, recently hosted our first Regional Patient and Service User Workshop.
The workshop aimed to ensure a consistent approach across the HSE in establishing regional patient and service user participation councils and their implementation plans. Independently facilitated, the workshop provided a valuable opportunity to explore what is working well in patient and service user partnership across HSE Dublin and South East. Participants discussed emerging themes and objectives for a future patient partnership strategy, with a focus on embedding meaningful partnership structures throughout the region.
Building on this momentum, senior leaders also attended the HSE National Public and Patient Partnership Conference.

Minister of State Jennifer Murnane O’Connor TD and Minister James Browne at the opening of the Activity Garden.
Council’s Culture and Creativity team and Age Friendly programme, in partnership with the HSE, Creative Ireland, the Irish Architectural Foundation and the Enniscorthy Men’s Shed.

This offered further opportunities to explore areas where patient and service user partnership is working well and how we can further embed partnership structures across our services. Both events highlighted the importance of listening to and working with patients and service users to shape services that reflect their needs and experiences. These initiatives mark a significant step forward in enhancing patient-centred care and ensuring that partnership is embedded in how we design and deliver health services.

St Luke’s General Hospital, Carlow/Kilkenny has launched Hearts and Mind: Knitting Care and Compassion, a creative initiative supporting palliative and bereavement care. It is a partnership with the Integrated Care of Older Persons team and the Loughboy Library Knitting Group, funded by Creative Ireland and Kilkenny County Council. The project builds on the hospital’s 2023 Knitted Hearts and Blankets initiative. Staff and volunteers provide handmade blankets and hearts to patients on palliative journeys and to bereaved families. Margaret Ryan, End of Life Care Coordinator, said these heartfelt items offer comfort and connection, showing how creativity can support emotional healing at end of life.

Stakeholders at the Ageing Well Together event.
Health Promotion and Improvement in HSE Dublin South and Wicklow is proud to lead the Ageing Well Together initiative. This collaborative project is designed to support older people in living independently and well in their communities through enhanced integration of services.
Rooted in the Sláintecare ethos of Living Well at Home, the project
brings together over 140 stakeholders across Dublin South and Wicklow – from local authorities, sports and community partnerships and charities to GPs, Traveller organisations and HSE services including Public Health, Public Health Nursing, Integrated Care of Older Persons (ICPOP), Social Inclusion, hospital services and many more.
Through extensive engagement and co-design with service users, the project has identified key needs, challenges and gaps in local services. The aim is a more integrated, person-centred approach to care. The proposed longer-term outcome of this project is to reduce reliance on hospital and community services, ease waiting lists, and improve quality of life for older adults.
If you want to know more about this project, or get involved, contact jim.gorman@hse.ie
visits local health services in Waterford
The Minister of State at the Department of Health with special responsibility for Public Health, Wellbeing and the National Drugs Strategy, Jennifer Murnane O’Connor TD was in Waterford to visit the HSE’s Health and Wellbeing Hub. The Minister met health and wellbeing teams and community partners who provide integrated service delivery, supporting the vision of the Sláintecare strategy. She also paid a visit to Primary Care and Social Inclusion services at St Otteran’s Hospital. The Minister heard from team members about local supports, including addiction services and homeless services, Traveller health, migrant health, family support and work with the Roma community. The visit highlighted the collaborative efforts across services to improve public health and wellbeing in the region.

The Community Neuro-Rehabilitation team for Dublin South Wicklow officially launched on 29 September, marking a significant step forward in delivering specialist neuro-rehabilitation in the region. This team forms part of the national Managed Clinical Rehabilitation Network (MCRN) being established under the National NeuroRehabilitation Strategy, which provides a tiered approach to neuro-rehabilitation:
•Level 1: National Rehabilitation Hospital –complex, tertiary care
•Level 2: Royal Hospital Donnybrook –local specialist inpatient service
•Level 3: Community Neuro-Rehabilitation team –community-based specialist neuro-rehabilitation
Operating from Bray Civic Centre, the team offers goalfocused, person-centred, time-limited interventions for individuals aged 18+ with a confirmed neurological diagnosis and neuro-rehabilitation needs that can be met by the team. Specialist neuro-rehabilitation is delivered in clinic-based settings, at home or via telehealth, depending on the person’s needs and location.

The service aims to support recovery and improve quality of life through a holistic approach tailored to each individual. The Rehabilitation Prescription is the referral form for the service and once completed, it can be submitted to the Network Rehabilitation Coordinator at neurorehabilitation.referrals@hse.ie
For more information, visit hse.ie/neurorehabguide
Dublin South and Wicklow Integrated Healthcare Area has taken a significant step in supporting colleagues through menopause. Feedback from recent staff focus groups highlighted the impact menopause can have on working lives and the need for more visible workplace supports. One participant noted, “Many women are struggling to cope with symptoms but feel they must do so in silence.” Another added, “Women don’t attribute their symptoms to menopause. Awareness is key.”
In response, the Menopause Working Group launched a Menopause Champion Training Initiative, delivered by the Menopause Hub. Thirteen staff were trained in October, coinciding with World Menopause Day (18 October). Menopause champions are staff volunteers who
raise awareness, signpost colleagues to supports, and provide a confidential and empathetic listening ear. The initiative also promotes the HSE Menopause Policy and HSeLanD training modules, helping to create a workplace that is open, understanding and free from stigma. Staff have welcomed this initiative, expressing gratitude for the open and supportive approach to menopause. It is hoped that this initiative will help build a culture where staff feel informed, valued and confident throughout their menopause journey.
To find more information on the project, or to get involved, contact Frances.Joyce@hse.ie





2025 was an eventful year for Digital for Care, with key programmes laying the groundwork for more progress in 2026 toward a better, more connected health service. Progress includes:
• The National Electronic Health Record is heading towards the procurement stage, with a decision expected by the end of 2026.
• Release 1 of the National Shared Care Record (NSCR) will be in use in selected healthcare areas in November, and rolled out to healthcare professionals nationwide over the coming years.
• The HSE Health App was launched nationwide in February 2025. In-person hospital appointments were added, alongside other key functionalities.
Digital for Care 2030, a strategy developed jointly by the Department of Health and the HSE, outlines the digital future of Ireland’s health system. It provides a clear framework to guide progress across six key areas:
• Empowering patients
• Advancing care management systems
• Supporting innovation
• Strengthening infrastructure
• Improving data and analytics
• Enabling the workforce through better tools and insights
• Community Connect completed nationwide discovery and blueprint, with national Single Point of Access and regional implementation set to begin in 2026.
• The Maternal and Newborn EHR went live in the Coombe Hospital, making it the sixth site nationally to implement this new electronic health record system, and bringing coverage close to 70% of births and 65% of neonatal intensive care activity nationally.
Underpinning this work is the development of Ireland’s first National Digital Patient Panel. As co-design workshops get underway, patients, carers and the public will have a voice in shaping digital health. This will ensure that the Digital for Care framework is guided by lived experience.
Ultimately, these various initiatives will be brought together, helping Ireland advance to become one of the leading EU countries in interconnected digital healthcare.
“Through innovation and design thinking, we will strive to make best use of existing resources,” says Damien McCallion, HSE Chief Technology and Transformation Officer and Deputy CEO. “However, to get to where we need to be, we must bring everyone along on the journey, ensuring consultation with patients – the people we serve – and staff nationwide.”
Anyone interested in joining the National Digital Patient Panel can sign up at bit.ly/DPP-SignUp
In busy clinics, every minute counts. For Helen Murphy, Director of Midwifery at Portiuncula University Hospital, the introduction of the HSE Health App will transform how expectant mothers are supported through pregnancy: “I’m encouraging staff and the public to use the app more,” she says. “It’s much easier to have the information in one place and know the content is evidence-based and up to date.”
“Time is of the essence,” Helen continues. “I want women to leave their consultations feeling fully informed about the options available to them, and the app enables them to review and reflect on these choices at their own pace.”
The HSE Health App consolidates guidance into one user-friendly location. Whether an expectant mother asks about a common condition during pregnancy or needs reassurance about medication safety, midwives can refer to the app with confidence.
The app also brings practical benefits beyond clinical use. For clinics, there is less of a need to store printing paper and information leaflets and there is the cost saving that comes with that.
The HSE Health App is available for download on Google Play for android or the App Store for iOS.

According to Helen, patients are noticing the difference. “Everything you need is on your phone,” she explains. “And we are reducing the amount of information expectant mothers have to physically carry.”
As a keen user and advocate of the app, Helen emphasises the importance of medical staff using the app to become well-versed with the content, enabling them to promote it effectively to patients: “We need to be familiar with what’s on the app. That way, when someone asks a question, we can answer it quickly or even better, show them how to find the answer themselves in the app.”
Hospital appointments for maternity services have been available in the app since its launch in February. Since then, thousands more hospital and community appointments have been added, and app downloads have grown to over 190,000.
With an increased number of appointments and users of the app, HSE staff are encouraged to use the HSE Health App as a means to guide patients, knowing the information is aligned with current best practices and guidelines.
Over 190,000 people have downloaded the HSE Health App to date and over one-third of users can see their upcoming appointments in the app. Downloading and using the app makes it easier for people to access their own health information and navigate the health service.
Included in the latest November 2025 HSE Health App release are waiting lists for day and inpatient cases in public and voluntary hospitals where patient administration systems have been integrated. GP referral information and health data for patients in the Structured Chronic Disease Treatment Programme have also been added.
Staff are encouraged to recommend patients and the people who use our services to download the HSE Health App from the App Store or Google Play.
The app’s capabilities are ever-increasing with the latest release adding more functionality to improve transparency, reduce administrative workload, and empower patients through greater access to their care information.
This release is another milestone and example of how the HSE is delivering Digital for Care. Over time, the app will become the main channel for people to securely access their health information and a range of services.
The integration of AI and intelligent automation into healthcare promises to enhance the quality of care, streamline operations, and provide more personalised and efficient patient experiences. The healthcare system is evolving, and innovative technology is playing a key role in supporting this. Empowering healthcare workers with advanced technological solutions can help to enhance clinical decision-making, streamline administrative processes, and improve patient care.
Several AI initiatives are underway across the HSE including:
• AI-assisted radiography interpretation
• Predictive modelling
• Ambient scribing
• AI-based translation
• Process automation
Integrating AI in healthcare has a range of benefits including:
• Improved diagnostic accuracy
• Personalised treatment plans
• More efficient resource allocation
• Analysis of vast amounts of data quickly and accurately
• Providing healthcare professionals with valuable insights that can lead to better patient outcomes
• Algorithms that can identify patterns in patient data which may indicate the early onset of diseases, allowing for timely intervention and treatment
In the coming months, the HSE will launch its first Artificial Intelligence (AI) Strategy for Healthcare in Ireland, AI for Care. Jointly commissioned by the Department of Health and the HSE, the strategy will set out the healthcare system’s aspiration for AI in healthcare and opportunity areas for
AI deployment in Ireland’s Health Service to 2030. An accompanying AI implementation framework will outline how AI for Care will be implemented. It will provide a toolkit for implementing AI projects across the HSE to guide the safe, ethical and effective deployment of AI technologies and to ensure regulatory adherence.
Ireland is one of the first six EU Member States to reach the critical milestone of designating competent authorities (of which the HSE is one) which will be responsible for the enforcement of the EU Artificial Intelligence (AI) Act. Looking ahead, a National AI Office will be established to act as the central coordinating authority for the EU AI Act in Ireland. These initiatives aim to ensure that AI adoption is aligned with clinical priorities, supported by robust governance, and embedded within a culture of safety and transparency.
For further information, contact AIandAutomationCoE@hse.ie
2025 has been a landmark year for Community Connect, a digital system for managing patient information (referrals, appointments, documentation) in all community services.
This work marks a major step toward modern, connected community care –reducing paperwork, improving access to information, and freeing staff to focus on what matters most: patient care.
A collaborative approach
The programme has placed staff voices at its centre. Over 1,000 community service
staff across all health regions took part in regional engagement sessions designing the solution proposal. More than 800 members joined the Community Connect Change Network – a growing community of staff continuing to shape and guide this transformation.
What’s next?
The National Single Point of Access for Paediatric Community Referrals is due to launch in June 2026. Community Connect’s first region, HSE Mid West, will officially go live in Q3 2026.
For more details, email communityconnect@hse.ie
If you’d like to join the Change Network and help shape the future of Community Connect, scan the QR code.

The Maternal and Newborn Clinical Management System (MN-CMS) is the Electronic Health Record (EHR) of the National Women and Infants Health Programme (NWIHP). It replaces paper-based records enabling doctors, midwives, nurses, pharmacists and health and social care professionals to easily access up-to-date patient information.
The MN-CMS EHR national programme team in collaboration with Oracle Cerner, the Coombe Hospital and HSE Mid West implementation teams have announced the successful completion of phase 2 of the national programme. This reflects the dedication of both local and national teams working together, including significant support from the phase 1 sites, to deliver digital change.
On 11 October, the Coombe Hospital became the final standalone maternity hospital to successfully adopt the MN-CMS EHR followed by its community-based antenatal clinics from 13 October. This follows the successful implementation in HSE Mid West. This region was the first in Ireland to complete the implementation of the MN-CMS EHR with all specialities; maternity, neonatology as well as gynaecology in July 2025. They join Cork University Maternity Hospital, University Hospital Kerry, the Rotunda Hospital, and the National Maternity Hospital in this national programme.
This is a significant advancement in the delivery of maternity, neonatology and gynaecology care as the MN-CMS EHR now supports approximately 62% of all births in Ireland and marks a key milestone in the HSE’s commitment to delivering safe, integrated and

Members of the Coombe Hospital multidisciplinary implementation team, including Grainne Gillett, Project Manager; Helen Curley, Change and Transformation Lead; Ann McIntyre, Director of Midwifery; Professor Martin White, CCOO; and Patrick Donohue, Secretary and GM.

Pictured are members of the multidisciplinary teams from the Coombe Hospital, Oracle Health and MN-CMS EHR National Project teams.
person-centred care. It strengthens communication across hospital and community services, supporting safer, more coordinated care for women and newborns.
“This milestone strengthens safety and quality of care for women and babies across the Dublin and Midlands Region,” says Kilian McGrane, National Programme Director, NWIHP. “With MN-CMS now live in all major tertiary units –covering over 60% of births nationally – we look forward to continued collaboration towards full national implementation, a key goal of the National Maternity Strategy.”
“Women and babies can now expect improved patient care as a result of improved communications,
supported decision-making and effective planning of care,” adds Fran Thompson, Chief Information Officer.
As part of the HSE Digital for Care 2030 strategy, all 13 remaining maternity units, and their related clinics are expected to implement the system in the next five years as part of this transformative national programme.
To keep up with the latest achievements in Digital for Care, see bit.ly/digitalforcare

HSE South West staff are availing of their winter vaccinations at clinics and workplaces across Cork and Kerry. The campaign began in early October, with staff encouraged to get their vaccines as soon as possible. There’s still time to get vaccinated, with Dr Anne Sheahan, HSE South West Regional Director for Population and Public Health encouraging staff who aren’t yet vaccinated to do so as soon as possible: “People can get very ill from both flu and COVID-19, so protect yourself and others around you by getting your vaccinations. Protect yourself early to avoid the need for isolating and missing out on social and seasonal get-togethers. Don’t let yourself or your family be sidelined by flu or COVID-19 this winter.”
“We strongly encourage all healthcare workers to get vaccinated for flu and COVID-19,” says Gabrielle O’Keeffe, Head of Service for Health Wellbeing and Strategy. “Staff members are at a much higher risk of being exposed to flu and COVID-19. Vaccines are an effective way to prevent serious illness, and it is safe to have both vaccines together. By getting vaccinated, staff are helping to keep themselves well, as well as the patients they care for.”
Vaccinations are available on site at many hospitals and residential settings, as well as a series of clinics; for details, visit hse.ie/staff clinics




Ireland’s first theatre for cancer-prevention surgery has opened at South Infirmary-Victoria University Hospital (SIVUH), in partnership with Cork University Hospital (CUH). Pictured are Dr Ruth Lernihan, Director of Nursing, SIVUH, and Louise Burke, Clinical Nurse Specialist, Oncological Prevention Service, SIVUH.
Ireland’s first protected theatre resource dedicated to cancer-prevention surgery for people at high genetic or clinical risk has opened in Cork. This new theatre pathway at Cork University Hospital (CUH) is one of only a handful of dedicated cancer-prevention theatre resources in Europe and marks a major step forward for prevention-led care in the region and nationally. The protected theatre resource secures regular time and beds for risk-reducing surgery while allowing the theatre to be used by other specialities between booked sessions. It forms the final, essential element of a comprehensive regional prevention programme that links rapid genetic testing, specialist risk clinics, radiological surveillance, surgical and reconstructive expertise, and one-to-one psychological and specialist nursing support.
This achievement has been driven by regional collaboration across clinical, academic and community partners.
“This initiative matters because up to 40% of cancers are preventable; earlier identification and timely risk-reducing interventions will reduce cancer incidence, improve outcomes and spare families the concern of a cancer diagnosis for their loved ones,” says Professor Mark Corrigan, Surgical Oncologist at CUH.
“This is a proud milestone for HSE South West,” adds IHA manager Priscilla Lynch. “It gives people clear, timely options to reduce cancer risk and creates a model that can be adopted across Ireland and Europe. The rapid rollout of local genetic testing and the establishment of a coordinated clinical pathway means families can access answers and interventions much sooner than before.”

Thousands of people have attended a series of events highlighting mental health and wellbeing supports across HSE South West in recent months. Together at the Castle in Mallow, Co Cork; Together at the Lodge in Midleton; and the West Cork Feel Good Festival have seen HSE South West work with local partners, including Chambers of Commerce, Cork County Council, Cork Mental Health Foundation, local development partnerships, See Change, SHINE, and An Garda Síochána.
More than 50 local and regional community groups and organisations took part in the events, which fostered a sense of community and raised awareness about the support services available for mental health and wellbeing. The wide variety of entertainment, recreational activities, workshops and informational spaces was enjoyed by thousands.
“This series of events is a powerful example of what can be achieved when communities come together,” says Resource Officer for Suicide Prevention Martin Ryan. “By blending joy, creativity and open conversation, we’re breaking down stigma and building stronger local supports for mental health. These events are a living network of hope, recovery and support. People leave events feeling connected, informed and less alone. That’s how we reduce stigma and prevent suicide.”

The new Bellevue day service in Mallow, Co Cork is supporting adults with intellectual disabilities to live the life of their choice to their fullest potential. The vibrant HSE South West-funded service provides individualised supports for each service user, and is a great example of the implementation of New Directions, the HSE approach to supporting adults with disabilities who use day services in Ireland.
New Directions proposes that day services should take the form of individualised outcome-focused supports to allow adults using those services to live a life of their choosing in accordance with their own wishes, needs and aspirations, and Bellevue certainly delivers on that.
St Joseph’s Foundation, funded by HSE South West, proudly opened the service in the middle of Mallow town earlier this year. It’s a vibrant and welcoming space for adults with intellectual disabilities where every individual’s voice is promoted and heard.
Since opening, Bellevue has quickly become a busy, dynamic service providing individualised supports for the service users attending.
Ten service users attend Bellevue, supported by a dedicated team of three staff. The service in Bellevue is
“Since opening, Bellevue has quickly become a busy, dynamic service providing individualised supports for the service users attending.”
centred around promoting independence, community access and skills building for a good and full life.
Helen Nunan, the local coordinator of day services for St Joseph’s Foundation said the team at Bellevue strongly believe in creating opportunities for everyone to reach their potential: “We’re proud that three service users are in paid employment two days a week, two are gaining valuable work experiences, one volunteers in a local charity shop and another volunteers in a local nursing home.”
“Four service users are in their second year attending University College Cork’s ID Plus project in Cork city, a two-year course that will lead to a certificate in social citizenship – a fantastic opportunity for learning and personal growth,” she continues. “One of our service users is also completing courses in the local Q centre, furthering their skills and confidence.”
The HSE programme Active Healthy Me is also underway in Bellevue weekly, exploring healthy lifestyle choices to help individuals reach their own health goals. There is also a strong emphasis on having fun and enjoying what life has to offer in the local community, building connections and hobbies for life – activities include attending chair yoga at Mallow Community Health Project, boxing in a local centre, zumba, swimming, basketball, knitting, and meeting up with friends.
“Every day at Bellevue is about progress, participation, and positivity,” Helen explains. “We’re proud of what our service users have already achieved and were excited for everything still to come.”

HSE South West supported Cork city’s first Recovery Walk, celebrating recovery from addiction. Part of International Recovery Month, the inaugural event was a collaborative effort led by the Cork Recovery Academy, alongside agencies including HSE South West. The aim of the family-friendly event was to make recovery visible, challenge stigma and celebrate the successes of individuals and families on their recovery journey. It also highlighted the vital work of Recovery Communities.
“In line with the HSE’s aim to reduce health inequalities and improve access to services for vulnerable and excluded groups, this walk was a testament to the power of recovery and the strength of community,” says David Lane, General Manager, HSE South West Social Inclusion. “It was an opportunity to walk side by side with those on their remarkable journey and remind them they are not alone.”
HSE South West recently hosted events in both Cork city and Listowel, Co Kerry to mark the launch of Communities in Action, a strategy to reduce alcohol harm.
The strategy is a joint initiative between HSE South West, the Cork and Kerry Alcohol Strategy Group, the Southern Drug and Alcohol Taskforce and the Local Drug and Alcohol Taskforce. It aims to reduce harm caused by alcohol across the region, and prioritises public health, improved health and social outcomes for individuals, families and communities, and considerably reduced morbidity and mortality from alcohol consumption.
Launch events took place in Cork and Listowel as they are the region’s two SAFER community locations, among 12 across the country. The SAFER project uses the World Health Organization’s SAFER package of five measures to provide practical interventions at community level.

There’s a fresh sense of freedom rolling through the streets of Youghal, thanks to the arrival of five new vehicles at St Raphael’s Centre. For the residents, these new wheels represent far more than just transport – they’re a gateway to independence, inclusion and joy. Since 2016, St Raphael’s has been transitioning residents from congregated living to communitybased homes. The final move from the original building was completed in 2019, with all 12 community houses fully occupied by December 2021. This shift has empowered residents to live more independently and engage more fully with their local community.
The new additions to the centre’s fleet – comprising both buses and cars – will significantly enhance the lives of residents living in those community homes. With improved access to educational programmes, day services, and recreational outings, the vehicles are already making a meaningful impact.
From beach walks and cinema trips to shopping excursions and social visits, the expanded transport options are helping residents live fuller, more connected lives.
Susan Wall, Director of Nursing at St Raphael’s, expressed her gratitude saying, “This isn’t just about vehicles, it’s about giving our residents the chance to live their lives to the fullest, to be included in their community – living ordinary lives like everyone else. We’re so grateful to the HSE South West for helping us make that happen.”


The Integrated Care Programme for Older Persons in Kerry celebrated its fifth anniversary with its oldest patient, Lilly Kelliher, who recently turned 100.
University Hospital Kerry held a series of events, involving staff and speakers, to mark its commitment to Clinical Pastoral Care.
University Hospital Kerry (UHK) has marked its commitment to Clinical Pastoral Education (CPE), a training programme which helps individuals learn how to provide emotional and spiritual supports.
A full day of events took place at UHK to mark and reaffirm the hospital’s commitment to CPE. Since its inception in Boston 100 years ago, CPE has become a global movement, training spiritual care providers to offer empathetic support to individuals during times of illness, crisis and transition.
Dr Margaret Naughton of UHK said the hospital is proud to be part of this legacy: “With guidance and supervision, participants learn to listen deeply, reflect on their own beliefs and emotions, and develop the skills needed to care for others with compassion, understanding and respect, regardless of faith or background.”
Nurses and midwives from across Cork and Kerry gathered at SuperValu Páirc Uí Chaoimh for this year’s HSE South West Nursing and Midwifery Regional Conference. Centred on the theme “One Region, One Vision: Nurses and Midwives Driving Excellence Through Integration”, the day was inspiring from start to finish.
The Integrated Care Programme for Older Persons (ICPOP) in Kerry marked its fifth anniversary this year. Since starting in 2020, the programme has helped older people with complex health needs get the care they need closer to home. Instead of relying on hospitals, ICPOP supports people through local hubs with expert teams who work together to help maintain independence. The Kerry hub offers services like ambulatory care, outreach, and geriatric emergency medicine, making it easier for older people to access the right care in the right place.

Participants at the annual HSE South West Nursing and Midwifery Conference.
Attendees enjoyed dynamic presentations from keynote speakers that included HSE South West Regional Executive Officer Dr Andy Phillips, Professor Áine Carroll, Dr Seán Healy, and Professor Helen Bevan. Their insights on the importance of change, integration and the power of the right relationships set the tone for an exciting day of learning and collaboration. There were also a number of service presentations from teams across the region showcasing incredible projects and developments and proving how nurses and midwives are driving excellence locally. The open-space discussion, which took place in the afternoon, gave everyone a chance to share feedback on key themes shaping the nursing and midwifery practice of the future. The event was truly a celebration of teamwork, innovation and shared vision for the region.
HSE South West recently supported two major specialised training events for doctors involved in the treatment of patients with the most serious complex and life-threatening injuries. Cork University Hospital (CUH) is identified as a Level 1 Major Trauma Centre, one of just two in the country.
A specialist training course for consultant anaesthesiologists, offering advanced, hands-on experience in damage control resuscitation and major trauma care ran in conjunction with an Emergency and Resuscitative Surgery Skill Course (ERSSC) in the autumn. Together, the two courses aimed to better prepare both surgeons and anaesthesiologists to deliver effective damage control resuscitation and surgery for patients suffering major trauma.
“The course focuses on improving patient safety and survival in high-stakes trauma situations,” says
Dr Alan Horan, Consultant Anaesthesiologist at CUH. “Participants practised essential procedures such as advanced airway management, bleeding control and vascular access. The course ensured maximum one-to-one teaching and feedback from a distinguished faculty of anaesthesiology and trauma experts from Ireland and the UK.”
“The Emergency and Resuscitative Surgery Skill Course was a unique training event aimed at teaching lifesaving skills to surgeons who will find themselves providing care for the seriously injured,” adds Professor Brain Manning, Vascular Surgeon at CUH. “We aimed to create highly realistic simulations of the initial emergency room management of seriously injured patients. These simulations took place in purpose-built simulation suites at the ASSERT centre at UCC’s Brookfield Health Sciences Complex.”
Community work staff and community partners came together in Ballyphehane to mark 50 years of community work in Cork city. The event, held especially for Section 39-funded organisations and local community and voluntary groups, was a vibrant celebration of dedication, collaboration and impact.
The gathering featured inspiring talks, engaging films and live music. It also honoured the work of groups who have supported community work across Cork. Certificates were presented to community organisations, recognising their long-standing commitment to improving lives and fostering inclusion.
“Attendees had the opportunity to share stories, reflect on achievements, and connect with others who share a passion for community development,” says Kevin Mooney, HSE South West Community Worker. “The event was a testament to the strength of Cork’s community spirit and the vital role these groups play in supporting the broader healthcare landscape. As we look ahead, the legacy of these 50 years continues to inspire us all to build stronger, more connected communities – where health and wellbeing are at the heart of everything we do.”

Celebrating five decades of community efforts in Cork city, local groups and volunteers received certificates of appreciation for their commitment to fostering inclusive communities and promoting health and wellbeing throughout the city.


Verbal, physical or online aggression towards staff is never acceptable. It is everybody’s responsibility to ensure a safe workplace. The new National Policy on the Prevention and Management of Work-Related Aggression and Violence 2025 outlines steps to protect healthcare workers and create safer working environments.
The updated policy outlines how we:
• prevent incidents of violence, harassment and aggression;
• assess risks to staff safety in the workplace;
• manage situations where staff may be abused, threatened or assaulted in connection with their work.
Healthcare workers face challenging situations daily. Ensuring they feel safe at work is essential not only for their wellbeing, but for delivering safe and high-quality patient care.
Conflicts may arise in healthcare settings, but aggression or violence should never be seen as normal, unavoidable or acceptable.
Challenging behaviour happens for many reasons. It may be unintentional and linked to a medical condition, or it may be deliberate and even criminal. Responses should reflect the situation – from compassionate care to firm boundaries and appropriate action.
To support the policy, the HSE has launched a campaign called “Keeping our services safe for everyone”. Posters are available for display in public areas.
The full policy is available at bit.ly/HSE_VHA
The Primary Care Reimbursement Service (PCRS) supports the delivery of a wide range of services to the public through approximately 6,600 primary care contractors (general practitioners, dentists, pharmacists and optometrists/ ophthalmologists) across a range of community health schemes. Through the National Medical Card Unit, it processes medical cards, GP visit cards, drugs payment scheme, long-term illness, and European Health Insurance cards. PCRS also makes payments to suppliers and manufacturers of high-tech drugs and facilitates direct payments to hospitals involved in the provision of national treatment programmes. Altogether, in 2024, PCRS made total payments and reimbursements of €4.4 billion. Details of claims and payments for 2024 are contained in its annual report, which is now available to download from the PCRS publications website at hsepcrs.ie Here, you will also be able to access monthly reports with detailed breakdowns of spending and volumes of drugs reimbursed.
In 2025, PCRS expanded its services to include the reimbursement of hormone replacement therapy medicines and products and, from 1 October, it began reimbursing contractors nationally for all primary childhood immunisations.
For more details, contact the PCRS Analysis and Reporting Unit at PCRS.
ReportQueries@hse.ie
The HSE has launched a new Social Media and Data Protection Staff
Use Policy to support staff in using digital platforms responsibly while protecting patient confidentiality and organisational integrity. The policy applies to all employees, covering both professional and personal use of social media, data protection as well as the use of recording devices in healthcare settings. It sets clear guidelines on when it is appropriate to post content online, how to avoid breaches of confidentiality, and the importance of obtaining consent before sharing any identifiable information.
Real-world case studies highlight the risks of inappropriate posts, including breaches on platforms like WhatsApp, Instagram and
LinkedIn, which resulted in disciplinary or legal action. The policy also provides practical guidance for staff on managing recordings by patients and visitors
The Decision Support Service (DSS) Register for Approved Organisations is now available to HSE health and social care services and other eligible providers. Access is essential for services such as hospitals, primary care, mental health, and nursing homes.
Established under the Assisted Decision-Making (Capacity) Act 2015, the DSS Register supports individuals who may need help making decisions about personal welfare, healthcare or finances. It promotes respect for each person’s rights, will and preferences while providing a secure platform to record and verify formal decision support arrangements.
Health and social care services may need to search the DSS Register to confirm that a valid arrangement is in place or to identify the legal authority of a decision supporter. This ensures clarity, safeguards confidentiality, and supports lawful sharing of information when a co-decision-maker or representative is acting on behalf of a person.
and how to respond or deal with social media posts from the public. Staff are encouraged to read the policy carefully and incorporate its principles.
“The
policy applies to all employees, covering both professional and personal use of social media, data protection as well as the use of recording devices in healthcare settings.”
Read guidelines here: bit.ly/AccessDSSRegister
• Bipolar disorder: mania, hypomania, depression and prophylaxis
• Recurrent depressive disorder: used to augment antidepressants
• Reduction of intentional self-harm and suicidality
Appropriate information and monitoring is imperative to ensure best outcomes for patients on lithium therapy and reduce likelihood of harm. This initiative is intended to provide and promote safer lithium therapy and support patients to engage with their healthcare professional to discuss all aspects of lithium therapy, monitoring and side-effects.
The patient information booklet was produced and updated by Audrey Purcell, Chief 2 Pharmacist and the Saint John of God University Hospital Drug and Therapeutics Committee. The booklet has been edited and reviewed by the National Adult Literacy Agency and awarded the plain English mark by NALA. St John of God University Hospital, the HSE National Medication Safety Programme, the Irish Pharmacy Union, the College of Psychiatrists of Ireland and the Irish Medication Safety Network have all collaborated to launch the booklet.
The booklet is available online at bit.ly/LithiumPatientBooklet Hardcopy booklets can be ordered from surveys.hse.ie/s/EAFX45 or via St John of God University Hospital at hospital.pharmacy@sjog.ie
At the HSE, every staff member has the legal right to make a protected disclosure under the Protected Disclosures Act 2014 (as amended) without fear of retaliation. Making a protected disclosure is also known as “whistleblowing”.
If you witness or suspect wrongdoing, remember:
• You have the legal right to make a protected disclosure.
• Your identity and role as a reporting person are protected by law.
• You are safeguarded against retaliation, disadvantage or unfair treatment.
You can report concerns where:
• The health or welfare of patients, clients or the public may be at risk.
• Your employer is not meeting their legal obligations.
• There is misuse or waste of public funds.
We need to continue to foster a culture where we all feel confident to speak up and know that our concerns will be taken seriously. By speaking up, you help strengthen accountability and integrity across the HSE. Protected disclosures can be made confidentially to the HSE National Office of Protected Disclosures (NOPD).
The NOPD has published a revised version of the HSE’s National Procedures for the Handling of Protected Disclosures on their website. For further information and guidance on how to make a protected disclosure, visit hse.ie/protecteddisclosures

In today’s ever-increasing digital world, cyber security threats are constantly evolving and becoming more sophisticated and frequent. The HSE relies heavily on IT technology to operate, and this makes the HSE a prime target for cyberattacks. Within the HSE, we provide a secure environment and deploy a number of technical cyber defences, such as firewalls, antivirus software, multi-factor authentication, network monitoring and regular software updates. However, when cybercriminals attack organisations like ours, they usually start by targeting people and not technology, because people are often the easiest entry point into an organisation’s IT network. In fact, recent reports state that 90–95% of cyberattacks involve exploiting human behaviour. Human mistakes, like using weak passwords, mishandling sensitive data or clicking on a link within an email, could potentially allow cybercriminals to launch a cyberattack. These attacks could damage, compromise or disrupt the HSE’s IT infrastructure and/or steal
or alter data. This is why regular cyber security awareness training is crucial for all staff.
Cyber security is a shared responsibility, and it is important that everyone plays a small part in helping to defend against cyberattacks. Awareness training is a key part of the HSE cyber security programme. The purpose of this training is to educate staff on how to recognise and respond to cyber threats. By being informed and remaining vigilant, staff can become a critical first line of defence.
Cyber security awareness training was first launched in May 2022 and updated in June 2023. On 6 October, the HSE launched its new cyber security awareness training, which is available to all staff on HSeLanD (hseland.ie). This training is mandatory and must be completed on an annual basis.
90–95% of cyberattacks involve exploiting human behaviour
Each module is 2 to 6 minutes long and is broken down into the following parts:
• Training video
• Relevant cyber security case study
• Interactive exercise or test
• Summary of key points
The new HSE cyber security awareness training is a fully customised HSE branded course, designed by the HSE. The course is made up of seven modules and each module focuses on a particular cyber security topic, such as:
• What is cyber security
• Cyberattack techniques
• Phishing
• Passwords
• Email and internet use
• Securing your working environment
• Course completion recap
Where feasible, non-technical plain English is used throughout the training course, and closed captions are included. It takes 35–45 minutes to complete the course, and it can be paused and resumed at any time. Remember, by remaining vigilant to the dangers, and taking positive security actions, we can all contribute to building a strong human firewall against cyber threats.
Flynn, Project
Roy Browne, Contracts Manager, and Leanne
Kevin Jackson, Director, Kevin Jackson Architects; Roz Murphy and Victor Lowe, Directors, O’Connell Mahon Architects; Joe Hoare, Assistant National Director, and Mary Prendergast, Estates Manager, HSE Capital and Estates; Brian O’Sullivan, Director, Lawlor Burns and Associates; Margaret Stackpoole, Project Equipping Manager, HSE Capital and Estates; Declan Doyle, Director, Varming Consulting Engineers; and Brendan O’Brien, Regional Director, John Sisk and Son.

Minister for Health, Jennifer Carroll MacNeill TD officially opened a new 96-bed inpatient block at University Hospital Limerick (UHL) in October, marking the largest capital project delivered by the HSE in 2025. The €105 million development spans 6,700 square metres and significantly boosts UHL’s capacity, addressing critical bed shortages in the Mid West region highlighted by HIQA.
The new facility, known as Block A, is connected to UHL’s critical care services and comprises of four floors of 24 en suite single rooms, increasing the hospital’s total inpatient beds to 650. It includes two wards for older persons, one renal ward and one trauma ward. Each ward features specialist rooms such as bariatric, isolation and disabled-access rooms, enhancing infection control and patient safety.
Rooms are grouped in clusters of eight, each supported by dedicated
nursing stations. Designed with patient wellbeing in mind, all rooms offer natural light and views of Limerick city or landscaped courtyards. Spacious layouts support family interaction, with each ward offering waiting areas and family meeting rooms.
The expansion has enabled the redesignation of two additional medical wards within the hospital, improving patient flow and care delivery. Nearly 400 new staff are being recruited to support the new block, with most already in place.
Minister Carroll MacNeill emphasised the importance of the development for the region, noting that by 2031, UHL will see an 82% increase in bed capacity, with over 572 new beds planned. She reaffirmed the Government’s
commitment to investing in healthcare infrastructure to ensure high-quality patient care.
The project was led by HSE Capital and Estates and delivered by John Sisk and Sons. The design team included O’Connell Mahon Architects, Kevin Jackson Architects and several engineering and planning consultants.
A €3 million investment ensured the wards were fitted with modern technology, including mechanical ventilation, in-built hoists and integrated digital systems.
Sandra Broderick, HSE Mid West Regional Executive Officer, described the opening as a symbol of hope for patients and staff, while Ian Carter, CEO of Acute and Older People Services, highlighted the impact on patient flow and care quality.
“Nearly 400 new staff are being recruited to support the new block, with most already in place.”
A free service is transforming patient care by allowing individuals on intravenous (IV) antibiotics to be discharged early from hospital and treated safely at home or in the community. The Mid West region’s outpatient parenteral antimicrobial therapy (OPAT) service not only enhances patient experience but also frees up vital hospital beds, saving more than 3,200 bed days annually through admission avoidance and reduced hospital stays.
Established in 2017, the Mid West OPAT service operates 365 days a year and ensures that no patient remains in hospital solely for IV antimicrobial treatment if they are otherwise fit for discharge. Between 2017 and the end of 2024, 1,049 patients have been supported through the service, saving an estimated 24,000 bed days.
Maria Molyneaux, candidate Advanced Nurse Practitioner (cANP), OPAT explains, “We aim to review all patients within 24 hours of referral and discharge those who meet national OPAT criteria within 48 to 72 hours.”
Nationally, patient satisfaction is high, with 98% of patients saying they would use the service again,

The OPAT service is available daily from 8am to 8pm through the community intervention team (CIT). Patients remain under the care of their primary and infectious diseases consultants, with weekly reviews at the OPAT clinic.
Two models of care are offered:
• H-OPAT: A CIT nurse administers IV antibiotics at home or in a CIT clinic.
• S-OPAT: Patients are trained to self-administer their IV antibiotics.
92% rating it as excellent, and 96% preferring it to hospital care.
Patients like Joseph O’Carroll Jnr from Cappamore and Oliwia Szafran from Limerick have praised the service for its compassionate staff and the independence it offers. Oliwia, who learned to self-administer her medication said, “Being able to manage my treatment from home brought normalcy back to my life.
The nurses were patient and supportive, and knowing help was just a call away gave me great confidence.”
The HR team at St Joseph’s Health Campus, Mulgrave Street has launched a sustainability initiative to reduce environmental impact. Key changes include replacing single-use plastic bottles with reusable glass and cardboard alternatives, switching to glass yoghurt jars to reduce food waste and using compostable packaging for meals. These efforts collectively reduce carbon emissions by approximately 832.52 kg CO2e monthly – nearly 10 tonnes annually. CO2e (carbon dioxide equivalent) measures the impact of greenhouse gases. These small but meaningful changes show how everyday actions can contribute to a healthier planet.
The service delivers hospitalequivalent outcomes while reducing the stress of hospitalisation. It also supports antimicrobial stewardship and reduces the risk of hospitalacquired infections.
The OPAT model aligns with Sláintecare goals by promoting patient-centred, community-based care. Its expansion across Europe and globally reflects a broader shift toward more efficient, cost-effective healthcare delivery. By adhering to national criteria and focusing on appropriate patient selection, the Mid West OPAT service continues to deliver high-quality care without compromising clinical outcomes.


Michael Cronin has been appointed Regional Patient and Service User Engagement Lead for HSE Mid West. With extensive experience across acute and community services, Michael brings deep insight into the challenges faced by patients and the importance of designing services that reflect community needs.

A new and permanent mural exhibition entitled “Handled with Care”, focusing on building community through art, was unveiled in March at University Maternity Hospital Limerick. The concept was created and managed by Italian artist Giulia Coli, who invited over 100 artists from across the Mid West to come together and collaborate on the themes of family, support and shared experiences. After the birth of Giulia’s daughter, Maeve, the artist realised she had a deep need for connection with other parents, which inspired the project.
The “Handled with Care” mural, exhibited in the second floor cafeteria of University Maternity Hospital Limerick.
In his new role, Michael will work closely with Regional Executive Officer Sandra Broderick and the executive management team to ensure patient and service user voices are central to decision-making. He will also sit on the newly formed Regional Interim Patient and Service User Council, helping to advise and advocate for responsive, equitable and person-centred care across the region.
Michael’s approach focuses on meaningful engagement, stating: “A typical day involves being out in the community – listening, facilitating conversations and working in partnership with people from all walks of life. It’s about co-designing services so that the people of the Mid West are at the heart of every decision.”
His previous work includes leading the North Side Engagement Project, a patient-led initiative that identified barriers to accessing services and co-created solutions with local communities. This work empowered individuals who had previously felt unheard to contribute ideas that were implemented in practice.
Michael’s appointment strengthens the connection between community engagement and executive leadership, supporting the HSE Mid West’s vision of partnership and participation in healthcare planning and delivery.
HSE Mid West Regional Executive Officer, Sandra Broderick and regional Patient Partner, John Wall were among hundreds of participants who attended the HSE Patient and Public Partnership Conference to share their experiences and improve healthcare services nationwide. The theme, “Navigating Our Patient Partnership Journey Together” highlighted the growing collaboration between the HSE and service users. Patient partnerships ensure lived experiences shape the design, delivery and evaluation of care. The discussions, in numerous workshops, plenaries and Q&A sessions, spanned disability, homelessness, mental health, chronic illness, children’s rights and technology, reviewing existing initiatives and sparking new ideas, reinforcing the importance of co-designed, person-centred healthcare across Ireland.

Sheena Friel, Clinical Midwifery Manager 2, University Maternity Hospital Limerick
I’ve lived in Ennis, Co Clare for 25 years and worked at University Maternity Hospital Limerick (UMHL) for 22 years. My husband and I have two teenage daughters, and we love

supporting their busy lives. I began nursing in St James’s Hospital in 1992 and later worked as a theatre nurse in the UK, New Zealand and Ireland.
After moving to Ennis, I completed a higher diploma in midwifery and worked in theatre and the neonatal unit. Since 2022, I’ve been a Clinical
Midwifery Manager 2 on the infant feeding and lactation/parent education team.
My time in the neonatal unit inspired me to become an international board certified lactation consultant (IBCLC). I saw first-hand how breastmilk supports premature and ill infants – boosting immunity, reducing inflammation and helping develop a healthy gut microbiome. Breastfeeding is natural but not yet the societal norm in Ireland, so early support is vital.
At UMHL, I work with a dedicated team offering antenatal and postnatal breastfeeding support, education and clinics. We also support mothers across HSE Mid West hospitals. In 2024, we launched the Lactation Station – a welcoming space for mums to receive personalised care. Seeing new mothers grow in confidence is the most rewarding part of my role.
For further information on breastfeeding support, visit bit.ly/BreastfeedingHSE To learn more about the Lactation Station, visit bit.ly/LimerickLactation
The HSE Mid West Health and Wellbeing Conference took place on 16 September in the Clinical Education & Research Centre (CERC) in University Hospital Limerick, bringing together healthcare professionals, wellness advocates, and staff from hospital and community settings. Organised by the acute services health and wellbeing team, the event focused on exploring innovative approaches to health and wellbeing.
Throughout the day, attendees engaged in insightful discussions and presentations led by experts in areas such as sustainability, cancer prevention, menopause, mental health, sleep and building healthier habits. These sessions aimed to inspire practical strategies for improving personal and workplace wellbeing.
A highlight of the conference was guest speaker John Kiely, Limerick Senior Hurling Manager and All-Ireland winner, who shared his experiences on leadership,

and
General
Operational Services, HSE Mid West; John Kiely, Manager of the Limerick Senior Hurling team; Eimear Laffan, Healthy Ireland Project Manager, HSE Mid West Acute Services; and Mairead Hughes, Admin Support, HSE Mid West Health and Wellbeing.
teamwork and performing under pressure. His talk resonated strongly with attendees, offering valuable lessons from the world of elite sport that can be applied in healthcare settings.
The event fostered collaboration, learning and reflection, reinforcing the importance of wellbeing in healthcare environments.

The Mid West region is pioneering one of Ireland’s first co-located inclusion health services for adults and children, aiming to reduce health inequalities among socially excluded groups. Led by consultant paediatrician Dr Siobhán Neville, the paediatric service launched in July 2024 and has since supported around 180 children through over 400 outpatient appointments and 140 inpatient bed days.

Clinics are held monthly in Ennis, Nenagh and University Hospital Limerick (UHL), with weekly ambulatory care and inpatient consultations. The service supports children experiencing homelessness, living in overcrowded housing or from refugee, Traveller, Roma and other marginalised backgrounds.
Paediatric inclusion health is a growing speciality focused on addressing the unique challenges
The Clare children’s disability network team (CDNT) physiotherapy and occupational therapy teams proudly supported a Co Clare build for the forthcoming new season of the RTÉ show, DIY SOS, hosted by Baz Ashmawy. CDNT expertise informed the design of a fully accessible bedroom and bathroom for a young person from Clarecastle with a complex physical disability. This included environmental assessments, layout advice and recommendations for specialist equipment funded by the HSE. CDNT staff worked closely with the DIY SOS team throughout the build and provided hands-on training to the family. DIY SOS highlights the vital role of CDNT in supporting children with disabilities and their families.
From left: Paediatric Inclusion Health Lead for the region, Consultant Paediatrician Dr Siobhán Neville, with Dr Róisín Coyne, SHO in Paediatric Inclusion Health, HSE Mid West.
faced by children affected by poverty, trauma and social exclusion. These children often experience higher rates of asthma, skin conditions, developmental delays and behavioural issues due to poor living conditions and limited access to healthcare.
Dr Neville highlights the urgent need for tailored care: “We aim to provide equity, not just equality –ensuring every child has the support needed to achieve the same health outcomes.”
The adult inclusion health service currently operates from UHL’s emergency department, supporting patients with complex social needs. Both services are part of a nationally funded pilot, following successful models in Dublin.
Looking ahead, the Mid West aims to expand staffing and make these services permanent. Early results show improved outcomes and reduced hospital bed usage.
Dr Neville hopes these efforts will lead to systemic change, making such services unnecessary in the future – but vital for now.

From left: Fiona Cuddihy, Senior Physiotherapist; presenter Baz Ashmawy; and Deirdre Talty, Senior Occupational Therapist.

There was late summer delight for patients, residents and staff at Nenagh Hospital and Community Hospital of the Assumption, Thurles, when the conquering All-Ireland hurling champions Tipperary turned both facilities into a sea of royal blue, gold and broad smiles during their visits with the Liam MacCarthy Cup and James Nowlan Cup.
The Premier County players were greeted with cheers, applause and congratulatory handshakes as they made their way through the main corridors to visit patients and

residents and chat with staff in both facilities.
Team Manager Liam Cahill and Captain Ronan Maher and other members of the hurling squad were roundly congratulated, not just for the famous sporting victory
Making every contact count in the Mid West – Diabetes
Clinical Nurse Specialists
that made the summer for all Tipperary people, but for being so generous in the time they spent meeting with staff and residents throughout both facilities, and allowing them to get their hands on their newly acquired silverware.

Brid Collins (left) and Karen Guico.
A recent audit of nurse-led diabetes clinics across four Integrated Care networks in Limerick has shown encouraging outcomes for people living with type 2 diabetes. The review of 175 patients discharged in 2024 revealed significant improvements in health and wellbeing.
Diabetes Clinical Nurse Specialists (CNSs) Brid Collins and Karen Guico lead outpatient clinics in Newcastle West, Croom, Kilmallock, Ballynanty, Kings Island, Barrack View and Dooradoyle. Their work highlights the impact of accessible, community-based care. “Bringing services closer to people makes attendance easier and increases engagement,” says Brid. “We have over 2,000 patient contacts annually, both virtual and in-person.”
Karen explains the clinic’s comprehensive approach: “We review blood sugar, blood pressure, cholesterol, medications, diet, exercise and lifestyle. We also educate patients on using monitors and sensors, which we track remotely, and follow up regularly by phone.”
Patients are either discharged back to their GP or referred to other specialists within the Integrated Care team. The audit results demonstrate the effectiveness of nurse-led care in improving outcomes and reducing emergency interventions.
Brid adds, “These results show the real value of our work. It’s about making every contact count – empowering patients and delivering better care.”
BreastCheck, the national breast screening programme, has just completed a community champions project in Cork to make breast screening more accessible for women who’ve recently arrived in Ireland.
Working with community champions, translators and local health workers, the BreastCheck team identified barriers for women attending screening. Together, they put practical supports in place for women to access breast screening, including translated information, group bookings, transport, and translators at clinics. As a result, 50 women from three accommodation centres attended screening in a supportive, welcoming environment.


The project not only gives these women access to screening, but also offers valuable lessons in how to break down barriers and improve equity in healthcare.
“In our experience as community workers, we find people prefer having a person to talk to about what a medical process involves and what they will experience, rather than reading the information materials in their own language,” explains Tania Baliukonis, Support Officer at Nasc, the Migrant and Refugee Rights Centre. “It is always better to have someone to speak to directly and ask questions. The community champions project, where we are upskilled to give information to women and answer their questions in their own language, allows us to be those people.”

“When I started as a community champion for screening, I wanted to help other women understand how important early detection is.”
“When I started as a community champion for screening, I wanted to help other women understand how important early detection is,” says Rola Abu ZeidO’Neill of Cork North and East Community Work Department. “So many times, we hear about someone being diagnosed with stage 3 or 4 cancer – and by then, it’s often very serious. I wanted our community to know that screening can make all the difference.”
BreastCheck participants can now use the HSE Health App to see their appointment date and time; their BreastCheck clinic name and location; and a phone number and email address to get in touch with their local clinic. More than 10,000 app users are in the eligible BreastCheck population (aged 50–69). BreastCheck will continue to send appointment letters by post in addition to the details being available on the app.
The app also signposts information on how to get ready for a mammogram, how to change or cancel an appointment, and what women need to tell us before their appointment.

In October, BowelScreen launched a new online register that makes it easier for people to take part in the national bowel screening programme. People can now request their home test kit on the online register. They can also check they are on the register, check when their next test is due, and provide their contact details online. In November, BowelScreen announced it has added around 60,000 more people to its register by extending the eligible age range from 59–70 to 58–70. Eventually, bowel screening will be offered to people aged 55–74.
The new BowelScreen online register can be accessed at hse.ie/bowelscreen or by scanning the QR code.



























































The HSE sends out hundreds of letters and appointments by post every day. Administrative errors in issuing letters and appointments by post are the most common type of data breach in the HSE. Postal data breaches occur in a very small number of letters issued by the HSE, but they can be upsetting for individuals when they occur.
• Postal breaches most commonly occur when:
• Using incorrect addresses
• Using old addresses
• Mistakenly including more than one letter or appointment in the same envelope
• A document relating to another person is mistakenly attached to a letter
• An envelope is not sealed securely
A breach like this can be stressful and upsetting,
especially if neighbours or family members receive a person’s confidential data.
Avoiding postal data breaches
To avoid errors, you should:
• Use a 3-point check for patients’ addresses:
1. Check the patient’s address is correct when drafting the letter
2. Check again after printing
3. Do a final check before it goes into the envelope
• Use windowed envelopes (ensure no sensitive information can be seen through the window)
• Make sure the envelope contains only the individual’s information (double-check the front and back of each letter)
• Check that “private and confidential” is on the envelope
• Be alert
What to do if you suspect a data breach has taken place
The GDPR section of the HSE website provides the necessary guidance for staff to report and manage data breaches. If you are ever in doubt or suspect a data breach, stop, think and ask for help from your line manager and from your local Deputy Data Protection Officer (DDPO).
Watch this short video for tips on how to avoid data breaches when sending letters or appointments: bit.ly/DataLetters
You will find a list of HSE DDPOs at hse.ie/GDPR and the team is happy to advise and help so get in touch. Remember that data protection in the HSE is everyone’s responsibility.

To enter:
1. Email us a photo of yourself reading Health Matters
2. Tell us where you picked up your copy
3. Let us know your favourite article from this issue
You must have all three parts to be entered into the draw.
Congratulations
We love seeing our readers enjoy Health Matters. Now we are giving you the chance to win a €100 voucher just for sharing a snap.

We’re delighted to congratulate Denise Scully, a receptionist and phlebotomist in Inchicore Family Doctors, Dublin. Denise enjoyed reading a copy of Health Matters at the clinic where she has worked for over 20 years. Denise most enjoyed our spotlight on tobacco, nicotine and other inhaling products. She said the use of vapes concerns her for many reasons including that her young adult daughter vapes at home. Enjoy your One4all voucher, Denise – and thank you for being a loyal reader.
Send your entry to internalcomms@hse.ie with the subject line ‘Health Matters photo competition’.
The competition closes on Friday, 16 January 2026. One lucky winner will be selected at random. Happy reading and good luck.

Representatives from the HSE, the GP and nurse triage services including staff of the NEDOC (North East Doctor On Call) service, both past and present, attended a celebration to acknowledge the success of the service over the past 25 years. NEDOC continues to serve the population of the North East with a collaborative and patientfocused approach to provide a high-quality service.
Dialogue
Attendees at the celebration recalled the history of the service and outlined the successes and challenges faced by the service since 2000. The commitment and diligent contribution of all stakeholders was acknowledged as key to the success of the service.
NEDOC is a partnership between the HSE and general practitioners in the North East. The service was a huge innovation in general practice.
HSE Louth Meath Mental Health Service recently hosted a public Open Dialogue conference, co-produced with service users and families. The Open Dialogue conference was led by project leads Dr Emer Rutledge and Michelle Darcy. It highlighted lived experiences and explored collaborative approaches to care. Speakers shared powerful insights, including an art exhibition and play by NOVA and Navan Theatre Group. Open Dialogue, now practised across Meath and Louth, fosters empathy, transparency and teamwork. Marie Mahon, Nurse Practitioner, described it as “a person-centred approach where networks work together toward recovery”.
Over 93,000 contacted the service in 2024 compared to 54,000 in the first year. NEDOC has four treatment centres, one in Drogheda, Cavan town, Castleblayney and Navan, with a call centre based in Ardee. NEDOC offers urgent out-of-hours care to patients, either by phone or in person at one of the treatment centres or at home for those who are non-ambulant or too ill to attend the centre.


The HSE Dublin and North East Region continues the journey towards integration outlined in Sláintecare. This journey was celebrated in September at the HSE Dublin and North East Regional Quality and Patient Safety Conference in Croke Park. The theme was “Improving Quality and Patient Safety Together –Ní Neart Go Cur Le Chéile”. The conference was attended by 300 people, including patient advocates, health and social care professionals, clinicians and managers and focused on integration of services across several themes.
Following an opening address by Dr Eamon Dolan, Regional Clinical Director, the first speakers
underlined the role of digital health as a key enabler of safe care. The first presentation was “Transforming health and social care through digital excellence” by Dr Dermot Hughes from the Encompass Programme in Northern Ireland. This lived experience of implementing an Electronic Health Record (EHR) was followed by Damien McCallion, COO and Deputy CEO of the HSE, who illustrated how patient care will be improved and transformed through an EHR. Reflecting on the key theme of integration, Professor Aine Carroll, from UCD, spoke about Ireland’s journey towards Integrated Care and illustrated what it could mean for patients and families. Continuing this theme, Adam
“Feedback following the conference has been very positive, highlighting that in an integrated system we are very much Ní Neart Go Cur Le Chéile.”
Harris challenged the audience to consider “Autism accessible practice as a quality and safety tool”, noting that autism accessible practice improves services for all.
Acknowledging staff are fundamental to service integration, Gavin Oattes led an interactive session on leadership, resilience and motivation. Showcasing the role of staff, four oral presentations were delivered, with a prize for best presentation. There was an inspiring array of topics, such as “Cardiorespiratory rehabilitation in an Integrated Care centre” in Dublin North West, “Harnessing digital technology to enhance cancer care” in Beaumont Hospital, “The use of My Health Matters folder” in the Older Person’s Integrated Care Programme and “Home blood pressure monitoring” in Our Lady of Lourdes Hospital, Drogheda. Professor Mary Dixon-Woods, University of Cambridge and Director of The Healthcare Improvement Studies (THIS) Institute and The Health Foundation, provided an evidence-based but practical session outlining “How we can improve how we are doing improvement in healthcare”.
A total of 96 posters were displayed throughout the day, providing a great opportunity for attendees to ask questions and collaborate with their colleagues. The topics that won a poster prize were “Sexual safety/An Garda Síochána (AGS) collaboration” from the safeguarding and protection team in Dublin North City and County and “Testing the implementation of the national OA hip and knee pathway in Meath” from the physiotherapy department in Our Lady’s Hospital, Navan. Feedback following the conference has been very positive, highlighting that in an integrated system we are very much Ní Neart Go Cur Le Chéile.

Louth Hospitals, including Our Lady of Lourdes, Louth County Hospital and the Cottage Community Hospital, achieved the prestigious American Nurses Credentialing Center (ANCC) designation of Pathway to Excellence.
The nursing team, who participated in the EU programme Magnet 4 Europe Programme prior to their application, have been on the pre-application journey for 12 months.
The Pathway to Excellence programme is a globally recognised quality standard, a designation by the ANCC that recognises healthcare organisations for creating positive practice environments for nurses.
It focuses on building healthy, inclusive workplaces that support nurses’ wellbeing, professional development
and engagement, ultimately leading to improved patient care and nursing and healthcare excellence.
The programme emphasises shared decision-making, interprofessional collaboration and staff wellbeing, and provides a framework for organisations to both achieve and sustain excellence.
Petrina Donnelly, Regional Director of Nursing and Midwifery, congratulated the team and said, “The Pathway to Excellence designation will put us on the global map as a positive and inclusive place to practise nursing, which in turn has better outcomes for our patients through nursing excellence, ensuring we continue to attract and retain the very best nurses.”
St Joseph’s Community Nursing Unit (CNU), Trim, marked National Palliative Care Week with three days of meaningful activities led by the Solace Group. The events focused on raising awareness around end-of-life care planning and empowering residents to voice their wishes. A candlelight memorial service welcomed Nina Carberry, MEP, and Cllr Joe Fox, who spoke with residents and staff. Director of Nursing Silin Joseph highlighted the centre’s commitment to dignity and person-centred care. Recently, St Joseph’s CNU won Nursing Home of the Year at the Irish Healthcare Centre Awards, reflecting its excellence and ongoing redevelopment.

Hospitals in Dublin and North East (DNE) were announced as winners of the Menopause in the Workplace Award for Public Sector and Government at the Menopause Hub Academy Awards 2025. These awards mark a major step forward in Ireland’s menopause movement. Some of the largest organisations in the country are now leading by example – creating real policies, offering meaningful supports and showing that menopause belongs at the heart of workplace wellbeing.
The DNE hospitals, for their part, are creating a network of 20 menopause champions per hospital to implement the HSE Menopause Policy. The HSE DNE Menopause Champions Programme is an accredited initiative funded by Healthy Ireland and delivered in partnership with the Royal College of Surgeons in Ireland (RCSI). This programme is training staff from diverse disciplines to become champions who offer guidance, raise awareness and foster inclusive, menopause-friendly workplaces.
The impact has been far-reaching: improved staff wellbeing, reduced absenteeism and increased retention. The success of the first cohort has inspired expansion to more hospitals in 2025 and 2026, with tailored content including bone health, nutrition and core strengthening exercise.
With over 75% of the workforce being highly skilled women, this initiative ensures that employees experiencing menopause are supported through education, flexible work arrangements and access to wellness resources.
Dolores Donegan says, “Taking menopause in the workforce seriously will be good for the Dublin and North East hospital employment brand and part of future-proofing our organisation to make it an attractive place to work. This award is a testament to our commitment to inclusion, compassion and future-proofing our healthcare workforce. Congratulations to all involved.”

▲ Infant feeding lactation specialists Fiona Carty, Victoria Maguire and Eva Cunningham attend the DCU Seminar.
celebrated at Dublin
To celebrate National Breastfeeding Week 2025, the Infant Feeding Lactation Specialist Service in IHA Dublin North City and West and Dublin North County hosted a seminar in partnership with Dublin City University (DCU). The event took place at the Alice Reeves Building in DCU and this year’s theme, “Hold Me Close: The Power of Skin-to-Skin Contact” guided the discussions. Key highlights included updates on safe skin-to-skin practices, laid-back breastfeeding techniques and responsive feeding approaches. Professor Gillian Paul shared valuable insights from her research on long-term breastfeeding in the Republic of Ireland. The seminar was a wonderful celebration of ongoing efforts to support and promote breastfeeding.
It was well attended by HSE staff, maternity services and community organisations, fostering important networking opportunities and encouraging collaboration among attendees committed to supporting infant feeding practices. The seminar complemented other local Breastfeeding Week activities, such as local breastfeeding support groups focusing on skin-to-skin contact and breastfeeding promotion stands in shopping centres.

World Physiotherapy Day 2025 was celebrated across a number of sites in both IHA Dublin North City West and IHA Dublin North County.
A promotional and educational video was launched about healthy ageing by the physiotherapy department at St Mary’s Hospital in the Phoenix Park. The video highlights the importance of physical activity in preventing frailty and falls. Links to HSE guidelines on physical activity, resources to encourage more movement and less sitting, and resources for building physical reserve for later life are included in the video.
Staff participated in a group step challenge, racking up a total of 2,871,939 steps in five days. Patients surpassed the ambitious 285km Dublin to Killarney mobility goal, clocking in an extra 103.7km in five days.
In Kilbarrack, the team based at Tonlegee Primary Care Centre promoted positive ageing to staff and service users by conducting some functional fitness tests and promoting positive ageing leaflets and literature.
And in Balbriggan Primary Care Centre, a lunchtime challenge was organised for staff to celebrate the importance of health and strength in the workplace. Staff participated in the plank and the sit to stand challenge, showing off their determination, fitness and team spirit.
The Hospital Medicines Management System (HMMS) at the Phoenix Pharmacy Department, based in St Mary’s Hospital in Dublin, has gone live. It’s the first community hospital to roll out this national system.
HMMS will become the platform to support electronic prescribing and electronic medicines administration when Irish hospitals are ready to adopt these solutions. The ultimate technology and transformation vision is to implement a closed loop medication management system: from pharmacy orders and supply to patient areas to e-prescribing and e-discharge. Phoenix Pharmacy was nominated in 2019 to be in the phase one rollout. HMMS provides acute and non-acute hospital pharmacy services with a modern, robust and scalable solution with enhanced functionality in key areas such as systems integration, ward-based work, drug procurement, inventory management and finance. Medicines remain the most common therapeutic intervention available to clinicians. Progression to a modern pharmacy solution is a logical step to further build and improve on existing services while facilitating the wider business objectives and medicines management agenda.
For further information, visit bit.ly/EhealthHMMS
Our Lady of Lourdes Hospital and Drogheda United Football Club are proud to announce a new collaboration that brings together two pillars of the Drogheda community in a shared commitment to health, wellbeing and local pride. The collaboration will see both organisations working closely on initiatives that support physical and mental health, including wellness campaigns for men’s health, women’s health and Mental Health Week.

The Irish Association of Directors of Nursing and Midwifery (IADNAM) held its annual conference in Dundalk in October. Regional Executive Officer, Sara Long and Regional Director of Nursing and Midwifery, Petrina Donnelly participated in the panel discussions.
Congratulations to Fiona Hanrahan, Director of Midwifery,
Rotunda, who is the newly appointed President of IADNAM.
The work of the maternity services staff in Our Lady of Lourdes was showcased at the IADNAM Conference. They have worked together to take a values and behaviour approach to their culture.
The Assistant Director of Midwifery described to the conference how an intentional focus on behaviours has
Service users have achieved another vital milestone on their recovery journey from substance use through the Soilse Addiction Service in IHA Dublin North City and West and Dublin North County.
A graduation ceremony honouring the participants was attended by General Manager Brian Kirwan, who congratulated all the graduates on their remarkable achievement. Former RTÉ broadcaster Joe Duffy also attended the ceremony.
Soilse provides a comprehensive, holistic addiction rehabilitation service that empowers those in recovery to move towards a drug-free lifestyle in Dublin’s inner city.
This journey led the participants through a continuum of care process from active drug use, residential stabilisation and detoxification, residential rehabilitation
impacted the day-to-day life in the maternity services. “We asked for help from the National Organisational Culture team and they supported us to design and begin our own change. There had been a significant improvement in the staff culture of the maternity services in Drogheda.”
Karen Harmon, Clinical Midwife Manager, who leads the culture work in partnership with her peers, highlighted how staff were reporting “a better atmosphere, less complaints, better communication, staff retention and overall improvement in the day-to-day working lives of the Clinical Midwife Managers.”
Grainne Milne, Director of Nursing, was keen to emphasise that she noticed that “living agreed and values-based behaviours did not impact on the workload and was not an additional task. The behavioural change became a part of how staff showed up for work every day.”

and finally to the drug-free day programme in Soilse for the next six months of their treatment.
They have all successfully graduated and the positive impact for them, their loved ones and communities is huge.
The health impact for all service users who reduce substance use is better health. Dedication, perseverance and hard work have truly paid off and the graduation was a wonderful celebration of their success.
The HSE Integrated Healthcare Conference brought together health service staff, patients and service users, their representatives, voluntary service providers and those from the broader health community to hear about the ongoing transformation and innovation within Ireland’s healthcare system.
Centred on the theme “Empowering People through Transforming Care”, the second annual event was opened by HSE Chairman Ciarán Devane and featured a fireside interview with Minister for Health Jennifer Carroll MacNeill TD.
A highlight of the day was the keynote address from Dr Richard Lewanczuk, Senior Medical Director for Health System Integration in Canada, who challenged the audience to rethink how care is delivered. “In healthcare, we spend up to 96% on repairs and very little on keeping people well,” he said, emphasising the need to shift from treatment to prevention. He noted that “around 80% of what determines our health happens outside the healthcare system, in homes, schools, communities, relationships,” and described integration as “local, messy, but it works when we share a vision”.
Over 300 posters were displayed, showcasing research and service improvements across the HSE that are making a real difference in people’s lives. Seven were selected for recognition, with An Taoiseach Micheál Martin TD, and HSE CEO Bernard Gloster presenting the awards to the winning entrants.

Congratulations to interRAI Ireland programme manager Natalie Vereker and her team, who picked up an award for their poster at the recent Integrated Healthcare Conference 2025. The interRAI Ireland System Management platform employs the internationally validated suite of interRAI assessments to support comprehensive health and social care needs assessment. As a national system, interRAI provides real-time insight into the health and social care needs of people across Ireland.

For posters, presentations, photos and video recordings, visit hsenationalconference.com
In 2024, data from 4,169 assessments show that:
• The user profile had an average age of 82 years (range 40–104)
• 69% of assessments took place in the home setting
• 46% lived alone and almost all (95%) had a primary family carer
• Common clinical characteristics included coronary heart disease (31%), diabetes (24%), COPD (15%), depression (18%) and pain (56%), while 86% had bladder or bowel incontinence and over half reported being in pain
This snapshot of the interRAI assessment data provides staff with real-time information supporting decision-making and care planning, reducing duplication and improving quality of care at regional and national levels.
Congratulations to Liz Murphy, Dublin and South East regional winner of the poster presentation award. The Wexford Chronic Disease Hub’s Integrated Cardiology Service implemented a waitlist improvement project to address a surge of referrals in April 2025, which risked delaying access and overwhelming staff. Guided by Sláintecare principles, the team developed a triage model using multidisciplinary collaboration, community records and seven tailored care pathways, including novel virtual and digital options for low-complexity cases. This approach prioritised complex patients for in-person care, reduced unnecessary face-to-face appointments and streamlined operations.
Key impacts:
• 63% reduction in waitlists (from 12 to under 8 months)
• 103% increase in clinical nurse specialist capacity
• 68% less clinical time per video consult
• Significant reduction in do not attend rates
• High patient satisfaction

Poster winner for Dublin and South East, Liz Murphy, Integrated Cardio-Vascular Specialist Nurse, Wexford Chronic Disease Hub, with HSE CEO Bernard Gloster and An Taoiseach Micheál Martin TD.
By using technology, the service enhanced productivity, improved access and demonstrated a scalable, data-driven model for integrated, patient-centred care that can be rolled out nationally.

Gemma Brennan, Operational Lead at Cuan Aoibheann, St Mary’s Hospital Campus, Phoenix Park, Dublin, with her award-winning poster, alongside Professor of General Practice Ray Walley and HSE Dublin and North East Regional Executive Officer, Sarah Long.
Findings include:
• GP referral rates increased each year
• Referral mechanisms became more seamless; one of the first to adopt Healthlink
• Inappropriate referral rates remain low – 92.3% of referrals accepted
• Representation on specialist workstreams from GP leads has supported ongoing quality improvement and co-design of solutions to challenges faced
Congratulations to Gemma Brennan, Dublin and North East winner of a poster presentation award. This project explored the creation of a strategic partnership between GP leads and integrated care
consultants to promote GP engagement across the community health networks in Dublin North West for the delivery of the Integrated Care Programme for Chronic Disease.
The findings highlight the importance of integration to drive engagement strategies, resulting in improved coordination, trust and sustainable practices that are responsive to clinical needs and system priorities.
Congratulations to HSE Dublin and Midlands region winners, Laura Tier, Patrick Ormond, Anthony Edwards and the Dermatology Department at St James’s Hospital, the first hospital in Ireland to integrate clinical photography with teledermatology, transforming outpatient care.
Key results:
• 620 of 993 patients who had teledermatology did not require a consultant outpatient appointment
• Dermatology received an average of 847 referrals per month in 2025
• Waiting times were significantly reduced to 6–9 months for patients using teledermatology, compared with 24–36 months in the control group
• Surpassed Waiting List Action Plan 2025 targets, improving access, reducing waiting times and supporting person-centred care
Patient feedback:
• 94% reported comfort during photography sessions
• 94% felt the process was clearly explained
• 93% rated their overall experience positively
• 87% would recommend the clinic to others


Congratulations to Ciara Kirke, HSE Clinical Lead Medication Safety, HSE West and North West regional poster winner. Ciara’s poster, Safety and Savings: Economic analysis of pharmacist-led person-centred medicines reviews in general practice, presented findings from the iSIMPATHY project. This project aimed to conduct a cost-benefit analysis of pharmacists in general practice providing person-centred medicines reviews to patients prescribed 10 or more regular medicines or with high-risk prescribing criteria.
Pharmacists conducted reviews using the 7 Steps to Appropriate Polypharmacy approach, incorporating shared decision-making.
Results:
• 1,471 patients were eligible for inclusion with a mean age of 76 years
• 12 approx interventions per review
• Analysis shows annual net savings of €124,968 to €347,844 per pharmacist, with a net saving of €288 to €741 per review
Pharmacist-led person-centred medicines reviews in general practice significantly reduced medicines-related harm and achieved meaningful cost savings.
Congratulations to Mags McAuliffe and the Kerry Integrated Care Programme for Older People (ICPOP) team, who were the HSE South West poster winners. The Early Supported Discharge/ Outreach Service in Kerry ICPOP is part of the National Care Programme for Older People. It aims to improve and standardise the quality of care for older people in Ireland.
“What Matters Most” puts the patient’s needs at the centre of all care planning. Each patient’s situation and needs must be considered as part of the “what matters most” care plan. This collaborative approach, guided by the principle of what matters most, transforms traditional models of care through person-
Congratulations to HSE Mid West poster award winners Grace Kelly, Maura Cleary and Hilary Stoddart for their poster, Smart Moves: Empowering Children in Disadvantaged Areas through Targeted Motor Skills Intervention. The Smart Moves project emerged in response to a high volume of referrals for children presenting with motor coordination difficulties in Roscrea, a community facing significant socio-economic challenges. With a deprivation rate of 45.1%, this project promoted early identification and support for children within a school-based, sustainable approach that can easily be transitioned into the community.
Results:
• Increased participation in physical activity and fundamental movement skills
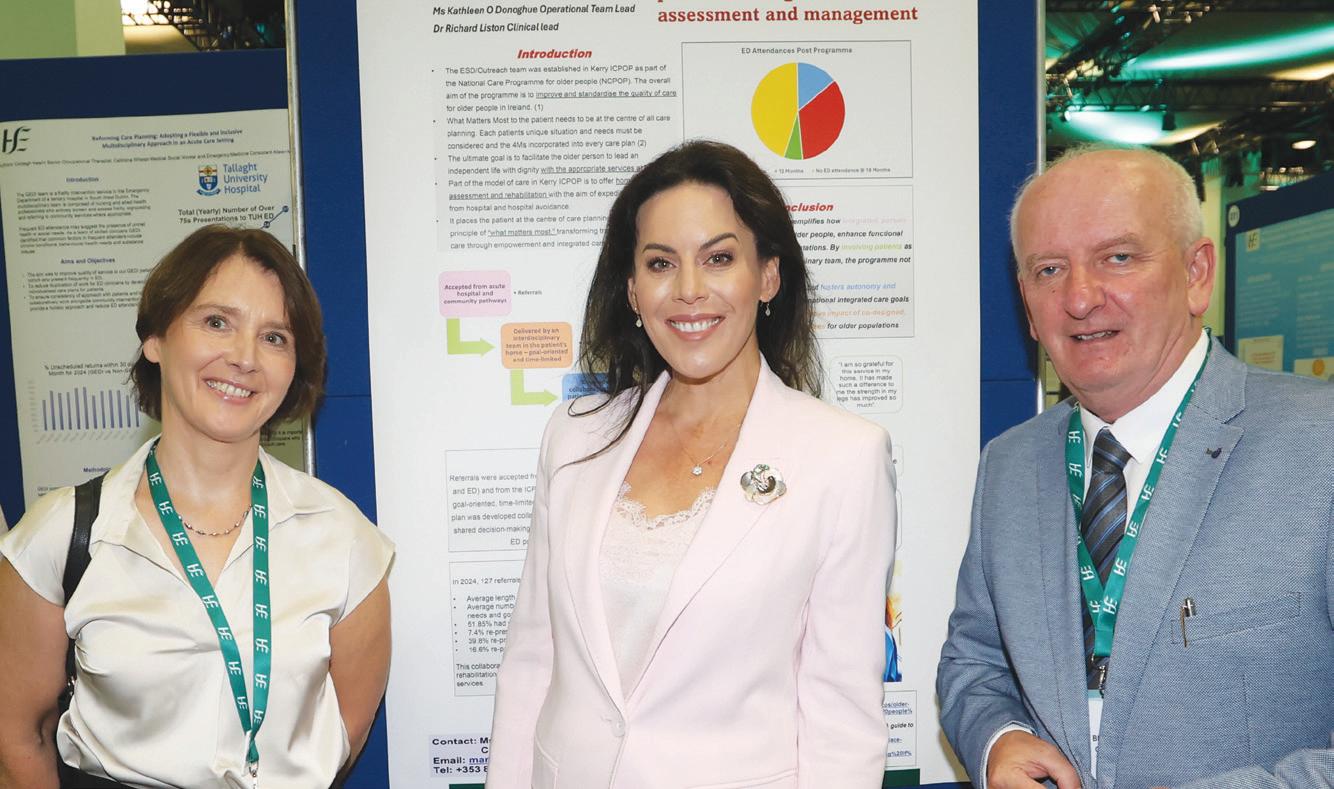
centred and integrated care pathways. The programme has shown improved patient outcomes, including enhanced physical recovery, reduced ED presentations, and stronger
patient confidence. This model supports national integrated care goals by promoting rehabilitation for older populations and enabling people to live independently for longer.

for children who may have motor coordination difficulties or have limited access to physical activity opportunities
• Empowered teachers to identify and support motor needs early within school settings
• Reduced referrals for motor coordination issues received by primary care teams, allowing
services to focus on children with significant resource constraints
The Smart Moves project demonstrates that embedding early, school-based intervention effectively supports health equity, empowers teachers and improves participation for children within disadvantaged communities.

HSE services have expanded care for people living in remote and island communities with a number of outreach clinics taking place in rural Galway and the offshore islands over the summer.
A team of specialist geriatric practitioners have brought care closer to home by visiting older people in their community, including outreach clinics on the Aran Islands. An important part of this service, in a Gaeltacht area, is the delivery of healthcare through the Irish language.
Advanced Nurse Practitioner, Máire Ní Neachtain is a native Irish speaker and part of the team who are carrying out comprehensive geriatric assessments on Inis Mór.
Speaking about her role Máire said, “One of the aims of our Integrated Care for Older People’s service (ICPOP) is to enhance specialist geriatric care and enable older people to live well and independently.”
“Within an Irish speaking community, and older person’s services in particular, it is very important to be able to facilitate clinical appointments in a patient’s native language.
“Patients are referred to our service by GPs, primary care and the local hospitals and we care for people who may have had falls, are experiencing frailty or changes in cognition.
“Our role is to carry out comprehensive geriatric assessments, which is seen as gold standard in older person assessments.
Anne Beatty is a 91-year-old resident of Inis Mór and describes the benefit of having specialist services closer to home: “I am delighted that the service is coming to Aran, you would get nervous going to Galway on a bad day, the plane or the boat might not be able to come and it’s great that the service is available in Irish too, because that’s our native language.”
Dr Robert Murphy, Consultant Geriatrician said, “Within the Galway City and Galway West ICPOP service we have a number of outreach clinics in Clifden, Carraroe and the Aran Islands, we work closely with primary care colleagues, island GPs and public health nurses to provide timely and responsive care to older adults closer to their home.”
A video highlighting Anne’s experience of the ICPOP service is available on YouTube at youtu.be/RaMjIPzIBUE
Tá Feidhmeannacht na Seirbhíse Sláinte (FSS) ag leathnú cúram do dhaoine atá ina gcónaí i bpobail iargúlta agus ar na hoileáin le sraith clinicí for-rochtana atá ar siúl i gceantair thuaithe i nGaillimh agus ar na hoileáin amach ón gcósta i rith an tsamhraidh.
Tá foireann cleachtóirí speisialtóireachta geiriatracha ag cur cúraim ar fáil atá níos gaire don bhaile trí chuairt a thabhairt ar dhaoine scothaosta ina bpobal féin, lena n-áirítear clinicí for-rocthana ar Oileáin Árann. Is gné thábhachtach den tseirbhís seo, i gceantar Gaeltachta, an soláthar cúraim sláinte trí mheán na Gaeilge.
Is cainteoir dúchais Gaeilge í an tAltra Ardchleachtóra, Máire Ní Neachtain, agus tá sí mar chuid den fhoireann atá ag déanamh measúnuithe cuimsitheacha geiriatracha ar Inis Mór.
Ag labhairt faoina ról, dúirt Máire: “Ceann de chuspóirí ár seirbhíse um Chúram Comhtháite do Dhaoine Scothaosta (ICPOP) ná cúram geiriatrach speisialtóireachta a fheabhsú agus daoine scothaosta a chumasú le maireachtáil go maith agus go neamhspleách.”
“I bpobal labhartha na Gaeilge, agus go háirithe laistigh de sheirbhísí do dhaoine scothaosta, tá sé an-tábhachtach coinne chliniciúil a chur ar fáil i dteanga dhúchais an othair.”
“Tagann othair atreoruithe chuig ár seirbhís ó dhochtúirí teaghlaigh, cúram príomhúil agus na hospidéil áitiúla. Cuirimid cúram ar fáil do dhaoine ar baineadh titim dóibh, do dhaoine atá leochaileach nó a bhfuil athruithe tar éis teacht ar a gcuid cognaíochta.
“Is é ár ról measúnuithe cuimsitheacha geiriatracha a dhéanamh – an caighdeán is airde i measúnuithe do dhaoine scothaosta. Gné lárnach den tseirbhís ná aitheantas agus freastal ar riachtanais shonracha an othair, lena n-áirítear cinneadh a dhéanamh i dtaobh cad is tábhachtaí dóibh féin.”
Duine a bhfuil cónaí uirthi ar Inis Mór agus atá 91 bliain d’aois í Anne Beatty agus mhínigh sí buntáistí na seirbhíse: “Tá an-áthas orm go bhfuil an tseirbhís ag teacht go hÁrainn. Bíonn imní ort dul go Gaillimh ar dhrochlá, seans nach dtiocfadh an t-eitleán ná an bád. Tá sé iontach go bhfuil an tseirbhís ar fáil i nGaeilge freisin, mar is í sin ár dteanga dhúchais.
Dúirt an Dr Robert Murphy, Geiriatraí Comhairleach: “Laistigh de sheirbhís ICPOP Chathair na Gaillimhe agus Iarthar na Gaillimhe, tá clinicí for-rochtana againn ar an gClochán, ar an gCeathrú Rua agus ar Oileáin Árann.
Tá an físeán seo ar fáil as Gaeilge freisin: youtu.be/dnTzPdIN2TA

Sligo University Hospital (SUH) is delighted to announce the appointment of Lorraine Cooney to the role of Patient Advice and Liaison Service (PALS) Coordinator. Lorraine, a native of Co Roscommon, has over 15 years’ clinical experience as a radiation therapist, and for the past two years worked as the PALS Coordinator at Mayo University Hospital prior to her recent appointment.
“Building on the foundations laid by the previous PALS coordinator, I am committed to fostering a culture of open communication and partnership with our patients and their families or carers,” Lorraine says. “I appreciate that being in hospital can be a difficult and vulnerable time, and I hope that the PALS role serves as a helpful point of contact for support and guidance. Patient feedback is invaluable, and I will channel all feedback via PALS to ensure the patient voice is embedded in the day-to-day operations, and future planning.”
Desmond Egan, the first patient to undergo the Convergent Biaxial 3-Dimensional (CB3) fixation procedure, pictured with Professor Alan Soo, Consultant Cardiothoracic Surgeon at University Hospital Galway, after a successful procedure that represents a milestone in rib fracture.
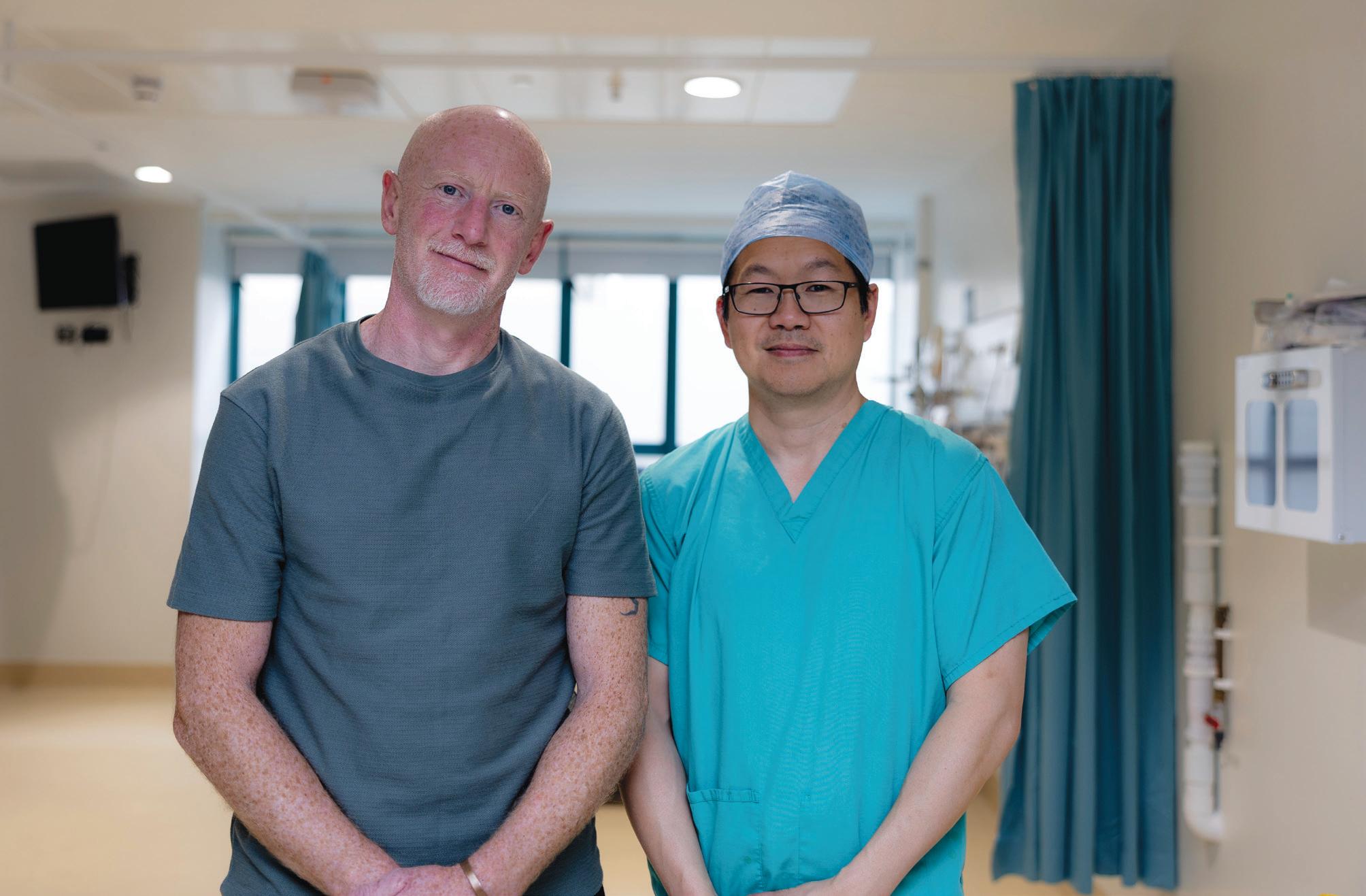
University Hospital Galway has reinforced its commitment to innovation and excellence in patient care with the introduction of a pioneering surgical procedure for the treatment of rib fractures.
The hospital has become the first in Ireland to introduce the Convergent Biaxial 3-Dimensional (CB3) fixation. Specifically designed for rib fractures to make rib fracture surgery safer and more efficient, this innovative approach delivers a stronger, more reliable repair than traditional methods, particularly in areas where the bone is under pressure or weakened.
It reduces operative risks while providing stronger support for healing and simplifies the implantation process, allowing plates to be placed at all locations of the chest wall without the need for large incisions. It enables quicker implantation, which reduces anaesthesia time and enhances overall surgical efficiency.
The first patient to benefit from this procedure was Desmond Egan from Ballintubber, Co Roscommon, who sustained multiple rib fractures following a fall. Thanks to the CB3 procedure, Mr Egan received a stronger and more secure repair, supporting a smoother and safer recovery.
“Rib fractures are very common, particularly in the West of Ireland, where we frequently treat injuries resulting from farming and construction accidents,” says Professor Alan Soo, Consultant Cardiothoracic Surgeon and lead of the procedure. “We are proud to be the first hospital in the country to adopt the CB3 procedure. Its advanced design enhances patient safety and surgical precision, helping to reduce risk, minimise painkiller use, lower the rate of post-injury lung complications such as pneumonia, and shorten hospital stays.”
There was fun indoors and outdoors at St John’s Community Hospital Sligo for the second Wise Roots Age-Friendly Festival. Residents, their families and friends were treated to a day of entertainment, music and treats at the community hospital. Music was also provided by Buncrana group Revival as well as many local talents such as Bridget and Tabby Callaghan and the Sligo Filipino community. The good weather saw residents going outside to visit some of the smaller animals of the Kiltimagh pet farm.
The Garden Room hosted an array of stalls, with an art gallery, face painting, hair braiding, cultural cuisines, taster facials and crafts and plants created by the residents in St John’s Community Hospital on sale.
On 5 September, the Minister for Mental Health, Mary Butler TD, officially opened the Solace Café in Sligo. Solace Café offers a free, confidential out-of-hours, nonclinical mental health service for adults aged 18 and over in the Sligo Leitrim area.
The service is facilitated by and based at Cornerstone (formerly Sligo Social Services) Retreat House, The Lungy, Sligo and funded by HSE West and North West.
Solace Café is one of five pilot services nationwide and is part of the crisis resolution services, which along with the crisis resolution team provide rapid assessment and intensive support to adults experiencing mental health crisis. Services offered at the café include crisis intervention and crisis prevention, through an informal safe space that is part of the community and social landscape, where people will feel comfortable seeking help when times are tough.
The café opens Thursday to Sunday from 5pm to 10.30pm. People who come to the Solace Café will be able to learn about coping strategies and access a range of supports, including one-to-one, peer, psychosocial and recovery supports.

▲ Minister for Mental Health Mary Butler TD (centre) with staff at the official opening of Solace Café in Sligo, from left: Sarah McGeever, Co-ordinator; Christina McTaggart, CEO; Sinead Casey, Operations Manager; Brian Fahy, Peer Connector; Aolish Gormley, Co-ordinator; Leanne Dineen, Administration; John Fitzmaurice, HSE IHA Manager, Sligo, Leitrim, South Donegal and West Cavan; and Melina Thieme, Peer Connector.
Staff who were nominated for the DAISY Award from Letterkenny University Hospital.

Three staff members received a DAISY Award at a recent ceremony in Letterkenny University Hospital (LUH). The DAISY Award is an international recognition programme that celebrates the clinical skill and compassion nurses and midwives provide to patients and their families every day.
At LUH, four DAISY Award ceremonies are held annually, with three honourees selected per quarter to receive the award. Honourees receive a handcarved Healer’s Touch sculpture, an honouree pin, a certificate, and cinnamon buns to share with colleagues – a tradition that began with the Barnes family, who established the award following the passing of their family member, J. Patrick Barnes.
The three winners of the recent awards were:
• Lorna Sweeney, Clinical Midwife Specialist, Loss and Bereavement – nominated for her calming, kind approach and clear, compassionate communication of difficult information, which helped a bereaved family to navigate the practical and emotional elements of their tragic loss.
• Pauline Ferry, Advanced Midwife Practitioner, Diabetes in Pregnancy – nominated for her empowering approach to the delivery of information, guidance and support and genuine care and dedication to all her patients.
• Claire McBride, Staff Nurse, Haematology/ Oncology Ward – nominated by the family of a patient, not only for her exemplary nursing skills, knowledge and compassion but her genuine interest in their father on his final journey.
For more information about the DAISY Awards and to read about past LUH honourees, search for “Letterkenny” at daisyfoundation.org

Fr John Carroll cuts the ribbon at Aurora with Anouska Vion and Conor Hickey along with HSE staff and management and Conor and Anouska’s mothers.
HSE Disability Services in Sligo, in partnership with the HSE Estates Department, officially opened the Aurora and Aurora Hub, two HSE-run day services for adults with intellectual disabilities.
Aurora Hub, based on Kempton Parade, opened its doors in November 2023, while Aurora, located at Duncan’s Island, Finisklin, welcomed individuals for the first time in September 2024. Combined, the two centres currently support more than 15 adults.
“Aurora and the Aurora Hub services represent what person-centred support looks like. The supports provided are inclusive, empowering and rooted in community.”
These day services are guided by the HSE’s New Directions, Personal Support Services for Adults with Disabilities, which is a national framework that supports a personcentred approach. Aurora and Aurora Hub are dedicated to promoting inclusion, independence and active participation in community life, offering opportunities that reflect the interests, goals and needs of each individual availing of the services.
“We are pleased to celebrate this milestone and the incredible progress of the people supported by Aurora
and the Aurora Hub,” says Edel Quinn, Head of Service, Disability Services in the North West. “Aurora and the Aurora Hub services represent what person-centred support looks like. The supports provided are inclusive, empowering and rooted in community. We are very proud of the achievements being celebrated today by the individuals who attend the service, well done to each and every one of them. My thanks to my colleagues, the dedicated staff of Aurora and Aurora Hub, who work tirelessly to support the individuals in living meaningful, connected lives guided by each individual’s person-centred plan.”
Aurora and the Aurora Hub is rooted in enabling each person to make choices about how they live their lives, how they spend their days and how they connect with others. The services provide tailored supports so that young adults with intellectual disabilities can access a wide range of opportunities to enhance their educational, social and occupational potential.
The Endoscopy Unit at Roscommon University Hospital (RUH) has once again been awarded JAG accreditation through the UK-based accreditation programme for gastrointestinal endoscopy.

▲ From left: Michelle Kelly, Staff Officer/JAG administrator; Marie Doorly, Interim Hospital Manager; Mairead Rogers, Clinical Nurse Manager 2 Endoscopy; Caroline Connaughton, Clinical Nurse Manager 1 Endoscopy; Mr Mohamed Eldin, Consultant Surgeon and Clinical Lead Endoscopy Services; Sean O’Brien, Assistant Director of Nursing Perioperative; and Mr Tapas Chatterjee, Associate Specialist Endoscopy.
The Joint Advisory Group on GI Endoscopy (JAG) accreditation is widely recognised as one of the most innovative quality assurance programmes in the healthcare sector. It emphasises a model of care that is both patient-centred and workforcefocused, ensuring excellence in clinical practice, safety and patient experience. Accreditation through JAG is a prestigious achievement that demonstrates the unit’s ongoing commitment to the highest standards of care. Services that achieve accreditation are granted the JAG quality mark, which must be maintained through annual reviews for four consecutive years, with a full reaccreditation assessment taking place in the fifth year. RUH has consistently upheld these standards, proudly maintaining JAG accreditation since 2012.

▲ Kelly Coughlin, the first patient in the world to receive treatment with the Recana Thrombectomy Catheter System, pictured with Professor Gerry O’Sullivan, Consultant Interventional Radiologist at University Hospital Galway, following the successful procedure that represents a global breakthrough in the treatment of complex venous obstructions.
University Hospital Galway (UHG) has achieved a global medical breakthrough by becoming the first hospital in the world to successfully trial a revolutionary new catheter device, designed to treat complex venous obstructions, particularly
blocked or damaged leg veins that have previously been stented and fail to return blood efficiently to the heart.
The Recana Thrombectomy Catheter System, developed by InterVene, Inc. is the first fully
integrated mechanical thrombectomy device specifically engineered to treat in-stent restenosis, a condition in which veins narrow again after stenting. The minimally invasive device is inserted through a small incision in the leg, allowing clinicians to access and clear previously obstructed veins. This restores healthy blood flow and offers new hope to patients who have exhausted all conventional treatment options.
“This marks a significant advancement in the treatment of chronic venous disease,” says Professor Gerry O’Sullivan, Consultant Interventional Radiologist at UHG, who led the procedure.
“The long-term impact of venous obstructions, especially in previously stented vessels, can be life-altering. It offers a powerful, minimally invasive solution for patients who have exhausted conventional treatment options.”
The Health Service Excellence Awards celebrate the outstanding work happening every day across Ireland’s health service. Now in its ninth year, the awards promote shared learning and inspire improvement through the success stories of teams nationwide.
The 2025 ceremony took place on Thursday, 4 December at Farmleigh House, Phoenix Park, Dublin.
Bernard Gloster, HSE CEO, praised the winners: “These awards create the opportunity to show innovation and creativity, which ultimately improves the services that we provide. Well done and thank you to all those short-listed as well as the winners. It is your work that helps pave the way to a brighter
future for Ireland’s health service. I am enormously struck by the generosity of healthcare staff to innovate, explore and share, all for the public good. You are remarkable.”
Anne Marie Hoey, Chief People Officer, highlighted the broader impact: “As well as recognising the great work of staff and teams across our wide range of services, the Excellence Awards are an important channel to share learnings across the health service. Through this pooling of knowledge and expertise, the projects inspire pride, teamwork and collaboration –positively impacting staff environments and improving outcomes for those who rely on our care.”








Winner: Older Persons Longterm Residential Care Facilities, Corporate/National Services
Project: IRESTORE Residential Older Persons Early Warning System (EWS)
Mary Bedding, Project Lead, National Deteriorating Patient Improvement Programme (DPIP), explained: “After COVID-19, staff in residential care facilities identified the need for an Early Warning System to aid early recognition and management of acute deterioration. A test of concept was launched in 2022.”
Pilot data 2024 versus 2023 baseline data demonstrated reductions in:
• Unplanned transfers (down 25%)
• Usual GP transfers (with/ without review) (down 48%)
• Non-falls medical emergency transfers (down 25%)
• 69% deterioration episodes –soft-signs (early flags of deterioration) present
• Positive staff evaluations
Runner up: University Hospital Waterford, HSE Dublin and South East
Project: Occupational Therapy Led Reablement
Winner: St James’s Hospital Theatre Department, HSE Dublin and Midlands Project: Operation Green –Sustainability Suggestion of the Month (SSM)
This initiative encouraged sustainable practices in the theatre department, promoting staff engagement and environmental awareness.
Dr Sinéad O’Brien, Anaesthesia Specialist Registrar, said: “We saw the impact of theatre-wide cooperation with visible adoption of our suggestions and measurable success, especially in waste management.”
Findings include:
• Increase in staff engaged with daily sustainability practices – 88% reporting they incorporated them regularly
• Measurable increase in general and glass recycling, resulting in an approximate reduction of 70 tonnes of CO2e production and €99,000 savings per annum
Runner up: Our Lady of Lourdes Hospital Drogheda, HSE Dublin and North East Project: Food Waste Reduction in Acute Hospitals
Winner: National Chronic Disease Prevention and Treatment General Practice Programme (CDM), Corporate/National Services Project: National Chronic Disease Prevention and Treatment Programme
The CDM programme supports structured management in general practice for patients with cardiovascular disease, COPD, asthma and type 2 diabetes. It emphasises prevention, early diagnosis and care close to home.
Impact (as of May 2025):
• Over 400,000 patients enrolled
• 91% receiving routine care in community settings
• 30% fewer emergency department visits
• 26% fewer hospital admissions
• 33% fewer out-of-hours GP visits
Runner up: University Hospital Limerick and St Vincent’s University Hospital, Corporate/National Services
Project: National Virtual Ward Programme




Joint winner: HSE Health Regions, Corporate/National Services Project: Patient and Service User Partnership Co-designing Integrated Service Delivery Model
The Integrated Service Delivery Model ensures patients and service users are central to service design. From 2023 to 2025, five workshops were co-designed with service users, focusing on their perspectives.
This resulted in:
• Stronger relationships and trust
• Improved engagement and outcomes
• Evaluation rated workshops 4.3 out of 5
• 100% of participants willing to collaborate again
Joint winner: IHA Midlands (Formerly CH08), HSE Dublin and Midlands
Project: CHO8 Children’s Services Design-Led Project
Human-centred design was employed to redesign children’s services with over 370 stakeholders (service users, frontline staff, managers) from disabilities, mental health and primary care. The initiative aimed to create a unified, timely and family-focused service.
Key outcomes included:
• Co-designed single point of access
• Integrated autism assessment pathway
• Parent communication resources
Runner up: Louth Meath Mental Health Service, HSE Dublin and North East Project: Open Dialogue: An Integrated Approach to Mental Health Crisis

Joint winner: ADMiRE, ADHD Specialist Service, Linn Dara CAMHS, HSE Dublin and Midlands Project: Developing ADMiRE: A Specialist Paediatric ADHD Service
Led by Professor Jane McGrath, Consultant Child and Adolescent Psychiatrist, HSE and Associate Professor, Trinity College Dublin, the team addressed a critical gap in ADHD care. “In Ireland, one-in-three children in CAMHS are diagnosed with ADHD. ADMiRE was developed to provide consistent, evidence-based intervention.”
Outcomes includes:
• Service user satisfaction exceptionally high (2022–2024)
• ADMiRE protocol, psychoeducation site and training resources now used nationally
• Safer, standardised, evidence-based ADHD-care nationally
Joint winner: Féileacán Bán, Cherry Orchard Hospital and Community Healthcare, HSE Dublin and Midlands Project: Co-Designed Nursing-Led Community Services, Transforming Dementia Care Delivery
Edel Carey, Registered Advanced Nurse Practitioner described the project: “The idea for Féileacán Bán emerged in 2018 from my frontline experience witnessing gaps in dementia care. Inspired by patients’ and caregivers’ stories, I began co-designing a compassionate, community-based service. The first pathway launched in 2019, expanding into five integrated pathways by 2021.”
Findings include:
• Improved confidence (91%), mood (53%), quality of life (51%) and reduced anxiety (44%)
• Carer burden decreased by 54%, with 57% reporting improved quality of life
• 94% satisfaction
• €863,704 in cost savings
Runner up: Primary Care Ophthalmology Service, HSE Dublin and Midlands Project: Bringing Clarity Closer: Evaluating a Community Cataract Assessment Service
Learn more about the winning projects at hse.ie/excellenceawards
Almost 3,000 people registered for the recent HSE Parents Matter webinar, “Vaping products and psychoactive substances: What you should know as a parent”. Across Ireland, vaping among young people has risen sharply. High-nicotine products, colourful packaging and fruity flavours have made vapes especially appealing to teenagers, which often masks the real risks to their physical and mental health.
“E-cigarette use among young people has doubled, with clear links to nicotine addiction and future smoking risk,” says Martina Blake, Lead for the HSE Tobacco Free Ireland Programme. “While some view vaping as a quit aid, evidence shows it’s no more effective than approved stop-smoking medications and carries its own harms. With new laws banning vape sales to under-18s and tighter restrictions on the way, parents and schools play a vital role in open conversations and education to protect young people’s health.”
The webinar speakers encouraged early, honest conversations about substance use. Teens who can talk openly with parents or teachers are less likely to experiment or hide risk behaviours.
“We’re seeing a worrying rise in teenage vaping – about one in eight 15-to-16-yearolds now vape daily,” explains Professor Bobby Smyth, HSE Adolescent Addiction Psychiatrist. “Nicotine addiction has become stronger and faster with these products, and for some, it’s a gateway to more harmful substances like HHC and THC. These newer psychoactive vapes are linked to psychosis, anxiety and mood problems, yet are often marketed as harmless. While parents are just one of many influences upon substance use by adolescents, we know that parents are the most important single influence. Families have the potential to act as a major protective force in the lives of children and adolescents. Mutually supportive family relationships alongside some boundaries and rules generally influence the prevention of substance use among young people.”
“Parents don’t need to have all the answers,” adds Emer Loughrey, Senior Counsellor, HSE Youth Drug and Alcohol Service (YoDA). “Just being present, listening and keeping communication open can make the biggest difference in helping young people stay safe.”
For more information, visit drugs.ie/parents or freephone the confidential HSE Drugs and Alcohol Helpline on 1800 459 459. Watch the Parents Matter webinar at bit.ly/HSEvapinginfo
1. Stay connected – talk during everyday moments.
2. Listen before you lecture – if your teen opens up, thank them and explore why they started.
3. Do your homework – learn about vaping and drug trends so you can discuss facts.
4. Celebrate healthy decisions – if your teen avoids vaping, be curious about the reasons they had for opting not to use.
5. Set clear boundaries –explain family rules and why they matter. Consistency keeps teens safe.
6. Model healthy coping skills –show positive ways to deal with stress, like walking, talking or reading.
As we continue to embed the new health region structures, HSE Dublin and Midlands is proud to reflect on a period of progress, innovation and collaboration. Our teams across the region continue to work tirelessly to improve services and outcomes for the communities we serve.
Over recent months, we’ve seen:
• Innovation in action: Congratulations to Laura Tier, Patrick Ormond, Anthony Edwards and the dermatology department at St James’s Hospital (SJH), winners of a Poster Presentation Award at the HSE Integrated Healthcare Conference 2025. This NTPF-funded innovation is the first of its kind in Ireland and has streamlined the accuracy of triage, empowering clinicians to make faster and safer decisions for a large number of patients.
• Productivity in action: Naas General Hospital is proud to be the first in Ireland to pilot the
Clinic Planning Tool, developed by the National Productivity Unit (NPU). This innovative tool helps hospitals plan outpatient clinics more effectively, improving access and aligning with the HSE National Service Plan and Waiting List Action Plan 2025.
• Academic partnerships: In partnership with Maynooth University, the region is delighted to support the first ever School of Nursing for Maynooth University as they welcomed their first students in September following official approval by the Nursing and Midwifery Board of Ireland (NMBI). This is Ireland’s first new university nursing school in two decades, advancing communitybased care under Sláintecare. In October, Regional Executive Officer Kate Killeen White represented our region at the Annual Chief Academic Officer Conference. Kate was joined on stage by Lily Collison, global advocate for cerebral palsy and author. She spoke to the region’s goal to continue to build on the work of Sláintecare to integrate our health services and get the best health
Tori, St Luke’s community dog has quickly become a favourite amongst staff, patients and visitors. Community dogs are specifically matched to work in designated facilities alongside a trained handler and play a valuable role in a variety of settings such as schools, care facilities and therapeutic environments. Tori brings surprise and joy when meeting people. Human traffic flow in the corridors of St Luke’s usually takes some time to resume when Tori is making her rounds! Please feel free to meet and greet Tori if you see her around.
outcomes for our populations and doing this with our key partners. Kate also attended the launch of Tallaght University Hospital’s latest year strategy launch (2025–2029) and the launch of the Peamount Strategy for Rehabilitation Care. Both strategies reflect commitment to excellence in care and a clear understanding of the evolving needs of our communities. We are encouraged by the strategic ambitions of these service providers.
• Staff engagement and regional development: With great attendance at our regional webinars, we are committed to transparent communication and inclusive leadership. The phased implementation of the new Integrated Healthcare Area (IHA) structure is progressing and work is underway for the next phase of implementation over the coming months.
As we move forward, our focus remains on delivering a unified, responsive health service that meets the needs of every individual in our care. We are grateful to our dedicated staff, partners and communities for their continued support and collaboration.

Ian Healy, a Porter, and Gillian Kelly, a Health Care Assistant, both working at Tallaght University Hospital (TUH), are making an inspiring leap in their careers by returning to college to undertake a four-year nursing degree programme. Their journey has been made possible by the HSE Nurse Sponsorship Programme, an initiative that offers 30 places nationally to healthcare support staff who wish to retrain as nurses or midwives.
Ian Healy, 45, has been a dedicated TUH Porter for over 26 years. He spent the past 20 years working in the TUH endoscopy unit. “I was ready for a new challenge and wanted a change in my career,” he says. “Thanks to the sponsorship programme, this is now possible.”
Gillian Kelly, 38, has been working as a Health Care Assistant (HCA) at TUH for the past three years. She currently works on Franks Ward, which specialises in orthopaedic care. “I love the job – it’s busy, but that suits me,” says Gillian.
The HSE Nurse Sponsorship Programme is designed to support existing healthcare staff in their journey to become registered nurses or midwives. Participants receive continued salary support during their academic studies and return to their existing roles during academic breaks.


• Regional Director of Technology and Transformation, Katie O’Rourke
• Regional Director of People, Olwyn Hughes
• Regional Lead for Governance, Compliance, Culture and Risk, Paul Hannon
• First Patient Service User Lead for HSE Dublin and Midlands, Mairead Holland

As we approach the Christmas period, remember that it is not too late to get your recommended winter vaccinations. By getting the seasonal flu vaccine, you protect yourself from infection with flu and the complications of flu infection, e.g. pneumonia or sepsis. You also prevent the spread of flu to people around you, including family members and patients you care for.
The flu vaccine is recommended for all healthcare workers in any healthcare setting. The COVID-19 vaccine is recommended for some healthcare workers at risk of serious illness.
Any healthcare worker who wants a COVID-19 vaccine can get one. The best way to protect yourselves, your families and the people you care for every day is to get your recommended winter vaccinations. They’re available for free from GPs and pharmacies.
For flu and COVID-19 vaccination clinics for staff, visit hse.ie/staffclinics

Tallaght University Hospital (TUH), one of Ireland’s busiest and most innovative teaching hospitals, has recently launched its new Strategic Plan for 2025–2029. The strategy sets a bold course for the future, built around a single, powerful mission: to deliver innovative, patient-centred care that continuously anticipates and adapts to meet the evolving needs of our community.
Highlights of the plan include:
• Expansion of bed and workforce capacity to meet rising demand.
• Investment in integrated community care through partnership with Integrated Healthcare Areas (IHAs).
• Initiatives to enhance digital health, innovation and sustainability.
• Commitment to fair, timely and compassionate care for every patient.

Regional Executive Officer, Kate Killeen White said, “I am honoured to be invited to launch this visionary hospital strategy. It reflects a deep commitment to excellence in care and a clear understanding of the evolving needs of our communities. I warmly congratulate the team behind this initiative and look forward to supporting its realisation, knowing it will serve the people of Dublin and the Midlands with compassion, innovation and impact.”
“With this new strategy, we reaffirm our commitment to every patient who walks through our doors,” added Barbara Keogh Dunne, CEO of TUH. “Together, we will build a future-ready health service that is caring, connected and resilient.”
Read the full plan at tuh.ie/About-us/ Strategic-Plan-2025-2029.pdf
Dr Christina Zacharatou, Senior Physicist at Beaumont Centre; Ema Staunton, Arts and Health Programme Manager; and Brian Carrie, Facilities Co-Ordinator, have organised a “fun corner” for the main waiting area in Beaumont Centre, providing a welcome distraction from what can often be a stressful period for patients. The table is equipped with colouring pages, colour pencils and markers, as well as puzzle pages. The tables have been warmly received by patients, who have expressed their gratitude to the staff. One commented, “Really enjoyed the colouring. The time flew while I coloured away. Thank you for making the time go by faster. Keep up the good work.”
The Green Ribbon campaign is an important initiative aimed at reducing the stigma surrounding mental health and encouraging open, supportive conversations. By wearing a green ribbon, individuals show their commitment to promoting understanding, compassion and awareness of the mental health challenges that affect people in all walks of life. The campaign highlights that mental health is just as important as physical health and everyone should feel comfortable seeking help and discussing their wellbeing without fear or judgement. In September, the health and wellbeing team in HSE Dublin and Midlands focused on raising awareness for this campaign and engaging with staff by signposting to supports locally which are accessible.
At the recent Patient Partnership Conference, a collaborative presentation was delivered by Mary Rose Cunningham, Self-Management Support Coordinator, Health and Wellbeing HSE; Mairead Holland, Patient and Service User Lead; and Paddy Flavin, Patient Partner. The presentation showcased a successful patient partnership in practice, highlighting a project aimed at improving health literacy for individuals living with chronic conditions.
The project was built on a collaborative approach involving both internal stakeholders and external community organisations. The pilot targeted communities with a high prevalence of chronic disease, prioritising partnerships with local organisations capable of effectively delivering the programme. Ensuring local facilities could integrate the
The many benefits of mental health promotion in the workplace include improved overall wellbeing, increased resilience, enhanced productivity and strengthened relationships.
As part of the initiative, Health Promotion in Laois held coffee mornings and gatherings for staff to provide a relaxed, welcoming environment where staff could come together to talk about mental health. These informal gatherings offered an opportunity to share experiences, learn from one another and strengthen connections among colleagues. Resources and supports were provided for staff to support their mental health and wellbeing. These events encourage social connection which plays a vital role in maintaining good mental health and overall wellbeing.

programme into their existing services was also essential.
Designed for flexibility and responsiveness, the programme actively involved patients in shaping the content to meet their specific needs. A multidisciplinary team –including health promotion officers, an adult literacy coordinator, clinicians and community partners – worked together to develop the six-week programme.
From left: Mairead Holland, Kate Killeen White, Paddy Flavin, and Mary Rose Cunningham.
Regional Executive Officer, Kate Killeen White attended the conference and met Paddy Flavin, gaining insight into his experience with the programme. His expertise was highly valued, underscoring the critical role of patient involvement in co-designing health initiatives.

Patients across the Midlands now have faster, easier access to liver disease care thanks to a new Single Visit Clinic recently launched by Midland Regional Hospital Tullamore (MRHT) – a first-of-its-kind service for assessing and managing metabolic associated fatty liver disease (MAFLD), marking a major step forward in patient-centred care.
MAFLD is a condition estimated to affect up to 60% of the adult Irish population. It accounts for 30% of referrals to the hospital’s gastroenterology service. Until now, patients faced wait times of over a year and required up to four separate outpatient visits for assessment and management. The new clinic model streamlines this process into a single, comprehensive
hospital visit, significantly improving patient experience, reducing costs and increasing service capacity.
Dr Mairéad McNally, Consultant Gastroenterologist and Project Lead, who recently received the National Doctors Training Best Doctor-Led Project at the HSE Bright Spark Awards says, “This project is about equity, efficiency and compassion. Patients now have access to a diagnostic test previously only available in tertiary centres. We’re proud to offer high-quality care locally, reducing travel, anxiety and delays.”
The clinic is now fully operational, with consultant-led and newly launched nurse-led fibroscan clinics under Dr McNally’s governance. Patients are triaged, invited for
blood tests in advance, and assessed with a fibroscan during their visit. They receive tailored literature and a GP summary, with many discharged after one visit. Those needing further care are reviewed promptly.
Brendan Malone, Interim Director of Nursing at MRHT adds, “This initiative has empowered our nursing team to take on new clinical responsibilities and develop specialist skills with a nurse-led clinic.”
“This is a fantastic example of innovation and collaboration in action,” says Michelle Maher, Operations Manager of Midland Regional Hospital Tullamore.
“The Single Visit Clinic enhances service delivery and supports our commitment to continuous improvement. The project also benefits our staff. Our administration colleagues are actively engaged and receiving feedback, nurses have gained new skills and career development opportunities, and consultants are benefitting from faster access to diagnostic tools. We’re proud to support this forwardthinking approach to healthcare.”
“Patients should not be disadvantaged by geography,” concludes Dr McNally. “This clinic ensures equitable access to fibroscan diagnostics for all patients in the Midlands.”
This initiative reflects MRHT’s commitment to innovation, collaboration and delivering compassionate, efficient care closer to home.
Key outcomes:
• Faster patient flow and reduced wait times
• Local access to fibroscan diagnostics
• Fewer outpatient visits and lower patient costs
• High patient satisfaction
• Over 40% discharge rate for appropriately triaged patients
• Timely consultant review for concerning results
On 31 July, the cardiology team in St James’s Hospital became the first in Ireland to implant the Aurora EV Implanted Cardioverter Defibrillator (ICD) in an adult patient, in a public hospital. This device is especially helpful for patients at risk of sudden cardiac arrest due to abnormal heart rhythms, and it represents a major step forward in cardiac care for patients in St James’s Hospital.
The Medtronic EV ICD is a pioneering extravascular defibrillator that helps control heart rhythm without any hardware being placed inside the patient’s veins. It offers the advantage of avoiding complications associated with traditional transvenous leads, which are placed inside the veins, and reduces the potential for any injury to the veins or arteries. It is the only extravascular ICD to offer anti-tachycardia pacing; gentle electrical pulses to control rapid heart rhythms, and has a projected longevity similar to standard ICDs, at 11–13 years.
The procedure was carried out by Dr Derek Crinion, Consultant Cardiologist and Electrophysiologist, with Ms Sarah Early, Consultant Cardiothoracic Surgeon, in attendance. External and inhouse training provided by Medtronic, with preparation by the cardiac physiologists, and the arrhythmia specialist nursing team; Marissa Corcoran, Advanced Nurse Practitioner, and Niamh Kelly, Clinical Nurse Specialist.


A ground-breaking innovation in emergency care is transforming how clinicians respond to suspected sepsis cases at St James’s Hospital.
The idea originated during the planning of the hospital’s first Sepsis Symposium, where an internal audit revealed a critical delay in sepsis response: clinicians were losing valuable time searching for supplies across wards during the “golden hour”. In response, the team initially developed a compact sepsis response box but thought that a more comprehensive solution was needed.
Clinical Nurse Manager, Adelina Baciu explains, “We couldn’t fit all the necessary supplies for the Sepsis 6 bundle into a small box. So, we designed a dedicated trolley that could carry everything required for rapid intervention.”
Designed for speed and efficiency, the trolley features six organised drawers, each tailored to a specific aspect of sepsis care:
• Cultures
• Bloods and Lactate
• IV Access
• IV Fluids
• Oxygen
• Catheterisation
Since its implementation, the trolley has led to a notable reduction in time between symptom onset and treatment initiation. Clinicians report fewer cases of severe deterioration and a decrease in ICU admissions, marking a significant improvement in patient outcomes.
The concept of a population health approach has gained increasing emphasis in health policy and services in Ireland, yet no universally accepted definition exists. This may hinder coordinated efforts to improve population health.
A collaborative project between HSE Public Health and the School of Population Health at Royal College of Surgeons Ireland aims to develop a shared definition and core principles for a population health approach. Key steps include stakeholder analysis and engagement, a scoping literature review and co-design workshops with cross-sectoral stakeholders.
To date, the project has been characterised by strong stakeholder engagement, highlighting that the process and surrounding dialogue are as important as the results. A shared understanding of a population health approach is envisioned to support greater alignment and impact of policies, programmes and strategies focused on improving population health. We look forward to sharing a summary of our project journey and results in 2026.
For more details, visit bit.ly/HSEpopulationhealth

A milestone in dementia care was reached in May, when Minister Kieran O’Donnell TD officially launched the Irish Dementia Registry at the Memory Assessment Services Symposium in Trinity College Dublin. The registry will be developed by the National Office of Clinical Audit in partnership with HSE National Dementia Services, the Enhanced Community Care Programme and the National Centre for Clinical Audit. The Registry is now six months into a three-year development phase. For the first time, the registry will provide a national, systematic picture of how dementia is diagnosed, treated and supported in Ireland. By capturing accurate, timely and complete data, it will guide service planning, research and policy, improving access, equity and outcomes. By combining data with lived experience, this landmark initiative will transform how Ireland plans and delivers dementia care for decades to come.
The Office of the Nursing and Midwifery Services Director (ONMSD), together with public health and community nursing staff, have developed a new career booklet. It highlights the vital roles nurses play in community settings across Ireland.
Designed to inspire and guide nurses considering a transition into public health or community nursing, it offers a comprehensive






Pictured are Bernie O’Loughlin, Louise Mullen and Dawn Whelan, NCCP; Linda Houlihan and Patricia McKeever, ARC Cancer Support Centre; and Maureen Lynch, Empower Trainer, Counsellor and Psychotherapist.

Support for those impacted by menopause as a result of cancer treatment
Empower – Menopause and Cancer Survivorship is an eight-week in-person and online group programme for those impacted by menopause as a result of cancer treatment. Participants watch pre-recorded modules by expert contributors who address the physical, emotional and psychological symptoms of menopause induced by cancer treatment.
This is followed by an interactive peer support element where participants come together to share their experiences, feelings and knowledge with the confidence that everything they say is confidential. Every session is 2.5 hours and provided free of charge by the Community Cancer Support Centres. National coordination and training for the programme is provided by the National Cancer Control Programme.
For further information, contact info@cancercontrol.ie or visit hse.ie/survivorship
overview of career options, featuring real-life profiles from current staff. It includes information on education pathways, qualifications, daily responsibilities, areas of specialisation and guidance on professional development and career progression.
Reflecting Sláintecare’s goal of shifting care from hospitals to the community, it showcases the dynamic nature of community nursing across homes, health centres, schools and clinics. It emphasises autonomy, variety and opportunities for continuous learning and advancement.
For more information or to access the booklet, visit bit.ly/HSENursingCareer
For career opportunities, visit careerhub.hse.ie
Find out more about the public health nurse sponsorship scheme at bit.ly/PHNsponsorship

Pictured at the launch of the first National Lived Experience Awareness Day on 15 October were Catherine Brogan, CEO, Suicide or Survive; Michael Ryan, Head of Mental Health Engagement and Recovery, HSE; and Jessica Curtis, National Programme Manager, Genio. The day was led by the HSE, with the support of the Department of Health and in collaboration with the Strengthening Lived Experience Programme (a partnership between the HSE, Genio and the Housing Agency). National Lived Experience Awareness Day will be marked annually on 15 October from now on. Lived experience expertise is the unique wisdom gained through directly experiencing and rebuilding one’s life when faced with significant challenges, such as mental health difficulties, social exclusion, disability or homelessness. While everyone experiences adversity, lived experience expertise comes from navigating life-changing challenges and using that insight to shape better services. The National Lived Experience Awareness Day recognises, celebrates and promotes this expertise across health, social and housing services.

The Community Healthcare Network (CHN) GP lead supports the development and maintenance of relationships between GPs, GP practices and primary care professionals, ensuring the delivery of high-quality, personcentred care to the local population. Within the 96 CHNs, this key strategic role provides leadership to transform care delivery in accordance with the principles of Sláintecare by bringing services closer to home, reducing acute hospital attendance and admission, focusing on the population needs
of the CHN and improving the patient experience through collaboration and learning.
The first in-person event hosted in the new Irish College of GPs offices in Dublin coincided with the recent HSE Integrated Care Conference. This forum was facilitated by Dr David Hanlon, National Clinical Advisor and Group Lead, and Alice McGinley, Head of Service. It provided a vibrant platform for collaboration and
shared learning with sessions covering CHN developments, embedding new ways of integrated working, digital advances and future plans. Dr Shane McKeogh, GP provided valuable insight from the Chronic Disease Hubs.
The attendance of the Chief Clinical Officer, Dr Colm Henry reinforced the importance of GP leads in shaping primary care delivery while also ensuring coordinated high-quality services.
Further details are available on the Enhanced Community Care (ECC) Hub, cnh.hseland.ie
Ireland’s Early Intervention in Psychosis (EIP) programme made a powerful impression at the 15th International Early Intervention in Psychosis Conference (IEPA15) in Berlin, themed “Breaking Boundaries”. HSE clinicians, researchers and lived experience partners joined forces with colleagues from Trinity College Dublin, University of Galway, University College
Dublin and the Royal College of Surgeons in Ireland to showcase how Ireland is leading the way in youth mental health and psychosis care. Highlights included the national evaluation of the EIP Model of Care, development of a rapid cognitive screening tool and Near Patient Testing for metabolic monitoring – shortlisted for a 2024 HSE Excellence Award. Ireland’s
evidence-based stance on cannabis regulation and its innovative psychosis prediction tool also received international recognition. With continued ministerial support and meaningful patient and public involvement, Ireland’s EIP team is demonstrating how collaboration, compassion and innovation can transform mental health care.
The HSE Safer Nightlife Programme continued its harm reduction work at Electric Picnic and District X this summer, providing on-site drug checking to identify risky batches of drugs. Drug harm reduction teams provided hundreds of drug interventions with 28 hours of outreach in terms of support and harm reduction advice. Over 176 drug samples were submitted from festival attendees across both events, helping to identify emerging drug trends and issue real-time public health alerts.
Over the four-year pilot period, the programme has seen an evolving MDMA market; ketamine commonly reported as a drug of choice at festivals; and a number of novel drugs identified, including increasing use of 2-CB. It has issued real-time alerts in relation to high-strength MDMA linked to medical emergencies, 3-CMC being sold as cocaine without people knowing, and cases of 100% pure cocaine, which is rare but can lead to extreme medical situations or fatalities. Synthetic opioids sold as heroin and benzodiazepines has also been highlighted.
It is always safer not to use drugs, but for those who choose to, practical steps to help reduce harm are available at drugs.ie


Learning that a residential facility is closing or that major change is underway can be an emotional time for residents, family and staff. A HSE working group has developed resources to help service providers communicate with residents, families and staff during the initial phase of a residential facility closure or major change. They apply to:
• Residential services for older people (public and private services)
• HSE Older Persons
• HSE Disability Services
• HSE Mental Health Services
• Voluntary service providers HSE Public Involvement, Culture and Risk Management led the project, which involved a wide range of stakeholders. These included patient partners, HSE staff, service providers, representative groups and patients. Their feedback fully informed the development of these guiding principles and resources.
Details are available at bit. ly/HSEresidentialclosures
For more information, email cultureandrisk@hse.ie

“Hold me close: The power of skin-to-skin contact” was the theme of this year’s HSE National Breastfeeding Week, 1 to 7 October. It highlighted the benefits of safe skin-to-skin contact in supporting feeding, bonding and recovery after birth.
The National Women and Infants Health Programme in partnership with the National Perinatal Epidemiology Centre (NPEC) also announced a new infant feeding survey for mothers to share feedback on their experiences of feeding support from maternity and community healthcare professionals during pregnancy and after birth.
Along with events held in hospitals and community settings across the country, the week also saw the launch in the Coombe Hospital of a new video on antenatal colostrum harvesting.
The video is available on YouTube at bit.ly/ColostrumHarvesting For more information, visit mychild.ie/breastfeeding
The HSE Spark Innovation team are delighted to announce Spark Impact 2026 – an initiative that empowers frontline healthcare professionals to turn innovative ideas into real healthcare solutions. Funding from €5,000 to €90,000 is available to support projects that can make a meaningful impact and scale across the health service. We invite doctors, nurses, midwives, health and social care professionals and pharmacists to apply – whether you’re developing a concept, piloting an initiative or ready to implement change.
Key dates:
months), Eimear Hughes and Gabriel (8 months), Daria Sexton and Xena (8 months), Katherine Nolan and Isla (2 years), Noelle Smith, HSE Public Health Nurse, Grangegorman Primary Care Centre and Katie Holohan, Assistant Director Public Health Nursing, HSE Dublin and North East at the launch of HSE National Breastfeeding Week at Grangegorman Primary Care Centre, Dublin 7.
• Design Thinking Workshop: Wednesday 10 December (note: completing this step is required before applying)
• Closing date for applications: Sunday 4 January 2026
• Pitching week for shortlisted applicants: Monday 9 February 2026
The application portal is now live. Full details, including the applicant guide, FAQs and application form are available at hse.ie/spark
In October, the National Screening Service launched a new survey that will gather feedback from people who take part in Diabetic RetinaScreen. Participants in retina screening who receive a normal screening result are invited by text message to take part in an online survey about their recent screening experiences.
The survey asks questions about:
• The person’s diabetes, such as number of years since their diabetes diagnosis
• Their views on the invitation process
• What they thought about their screening appointment, the physical surroundings and timeliness
• Their general satisfaction with the programme
There are additional questions for women who took part in screening during pregnancy. The survey is part of the National Screening Service Patient Reported Experience Measures (PREMs) initiative to gather feedback from our screening participants. By listening to the voices of people using our services, we can find out what is working well and identify areas for improvement.
A consistent, trusted identity helps people recognise and connect with the HSE.
The HSE National Guideline for Visual Identity and Naming sets out how every part of the health service should present itself – clearly, simply and consistently. Here’s what you can do:
• Use the HSE master logo on all communications, signage and digital channels
• Retire local or legacy logos as materials are updated
• Follow the approved naming format: HSE [Service/Location] (for example, HSE Community Healthcare West)
• Apply the visual standards for colours, fonts and templates available
• Ask before you design: contact your local communications team or the National Communications and Public Affairs team for guidance
By following the guideline, we’ll present one clear, unified voice for Ireland’s health service – trusted by the public and recognised everywhere.
The guideline is available at bit.ly/HSEVisualIdentity Guidelines
In October this year, people across the HSE and HSE-funded services came together to recognise the importance of open disclosure for staff, patients and service-users, along with their support persons and caregivers.
This year’s Open Disclosure Themed Week focused on promoting an open, honest and fair culture – one that focuses on learning and quality improvement following notifiable incidents. Online training sessions touched on the importance of leadership and the crucial role everyone has to play in open disclosure and improving patient safety.
A webinar, “Courage to Speak, Freedom to Care: Promoting Psychological Safety and Cultural Awareness in Healthcare”, was delivered by Dr Teresa Donnolly and Selene Daly Tarpey from the Centre of Nursing and Midwifery Education (CNME) Sligo, Leitrim, West Cavan. It offered practical approaches to creating positive learning spaces and developing inclusive spaces and practices.
The webinar is available at bit.ly/OpenDisclosureWebinars







The HSE Children First National Office has launched an eLearning programme, Recognising and Responding to Adult Retrospective Disclosures of Childhood Abuse on HSeLanD. The module is designed to provide staff with the knowledge and confidence to recognise and respond to adult retrospective disclosures of childhood abuse.
This module is aimed at frontline staff working in HSE roles, including those in HSE-funded and contracted services or with general practice services. Whilst this module is not mandatory, all staff and those who have line manager responsibilities can benefit from this programme, as adult disclosures of childhood abuse can arise in any service context.
To access the module, log in to your hseland.ie account and type in “Retrospective Abuse” in the search bar.
On completion of this programme, you will be able to:
• Explain what is meant by retrospective abuse and give examples of this
• Summarise the legal and policy requirements around reporting child protection concerns
• Describe how you should respond to an adult disclosing retrospective abuse
• Apply your organisation’s reporting procedure when you have a child protection concern
This eLearning module was developed in collaboration with the HSE Children First National Office and the National Counselling Service Child Protection Working Group. Other stakeholders also reviewed and contributed to the module.
Naas General Hospital is proud to be the first in Ireland to pilot the new Clinic Planning Tool, developed by the National Productivity Unit (NPU). This innovative tool helps hospitals plan outpatient clinics more effectively, improving access and aligning with the HSE National Service Plan and Waiting List Action Plan 2025.
The NPU collaborated with hospitals nationwide to assess outpatient department operations, focusing on capacity assessment and utilisation to inform data-driven planning. Naas was selected to lead the rollout, with teams visiting since April to gather insights and provide training together with robust, real-world-informed analysis.
The tool helps hospitals to understand their core clinic capacity and optimise scheduling. General Manager Kieran McDonald says, “This marks a major step in enhancing patient access and operational efficiency. We’re proud to contribute to a more responsive health service.”
Dr Mary Coghlan, Director of the NPU adds, “We have been delighted to work with the team in Naas to show that innovative leadership backed by a datadriven transformation approach can have a significant impact in a relatively short period of time.”
Naas General Hospital’s leadership reflects its commitment to high-quality, timely care and national healthcare priorities.

Five cross-border CAWT (Co-operation and Working Together) PEACEPLUS funded projects launched in the autumn. In total, €42.6m has been made available by the Special EU Programmes Body (SEUPB) for cross-border projects.
The projects support mental health, children’s services, obesity, older people and alcohol addiction services, in the Northern Ireland/Ireland border region up to 2029. The HSE, in co-operation with the Northern Ireland Health Authorities will oversee the implementation of these projects.
The Early Frailty Intervention Project launched in Omagh focuses on supports to those aged 55+ who are at risk of frailty. Community-based teams will provide access to screening, assessment, education and supports aimed at empowering individuals to maintain independence and manage their health and wellbeing.
The Early Intervention Support Youth Hubs project, launched at the NorthSouth Ministerial Council offices in Armagh, provides early intervention and supports to children and young people who present with neurodevelopmental type conditions. These will be provided in partnership with voluntary and community organisations.
“The CAWT partner organisations are committed to developing innovative cross-border services which serve the needs of our populations,” says HSE National Director and CAWT Director General Pat Healy. “We are thankful to the SEUPB and both Departments of Health for this PEACEPLUS funding and for their support and trust in the CAWT partnership to deliver for citizens living in border counties.”
The other three projects – Healthy Futures, Community Connections and Wellbeing, and Community Alcohol Detox – were successfully launched in Donegal and Monaghan in mid-November.
For further information contact Paula Keon at Paula.Keon@hse.ie
For more details, visit bit.ly/CAWTPEACEPLUS

Early Frailty Intervention Project launch, Omagh, 1 October, from left: Front rows, from left: Breege Donoghue, General Manager, Community Supports Teams, Older Persons Services, HSE Dublin and North East; Paula Keon, EU and North/South Unit, HSE; Pat Healy, National Director, HSE and Director General of the CAWT Partnership; Melissa Currid, ICPOP Operational Lead, Sligo Leitrim, HSE West and North West; Clare McAleer, ICPOP Operational Lead, Donegal, HSE West and North West; Cathy McCloskey, Chief Officer, CAWT; Eamon Dolan, Regional Clinical Director, HSE Dublin and North East; and Danielle McLaughlin, Deputy Chief Officer, CAWT. Back row, from left: Frank Morrison, Co-Chair of the PEACEPLUS Early Frailty Intervention Project Board and Head of Service, Older People, HSE West and North West and Professor Paula Hickey, Consultant Geriatrician, Sligo University Hospital, HSE West and North West.
The HSE Annual Report and Financial Statements 2024 highlights the delivery of health and social care services to a growing and ageing population at a time of significant structural reform. Published in July, the report also offers a detailed breakdown of the organisation’s management of finances and public resources. 2024 marked a major milestone for the HSE with the establishment of six new health regions. The report outlines performance across acute and community services, progress on the implementation of the six new health regions and the financial challenges of meeting rising demand. It also details the organisation’s work to improve access, reduce waiting times and deliver care closer to home. 2024 also marked the final year of the HSE Corporate Plan 2021–2024 and the beginning of work on the Corporate Plan 2025–2027.
The HSE Annual Report and Financial Statements 2024 is available at bit.ly/ HSEAnnualReport24 The Corporate Plan 2025–2027 is available at hse.ie/corporateplan

The Dementia: Understand Together campaign has been working with parkrun for a number of years. We all know the importance of physical activity on our health and wellbeing, but staying socially connected is also vital and plays a key role in improving our brain health too. parkruns are a great example of an activity that is inclusive for all.
The recently launched “Your parkrun and Dementia Manual” aims to support organisers and attendees to better understand dementia and the ways they can support people to be involved. Over 150 parkruns take place every Saturday across the country, so there is always a welcoming and safe place for people to get outdoors and enjoy time with others nearby.
We’d encourage healthcare staff, especially those working in occupational or physical therapy, with older adults and in community-based services to use the manual. You may want to consider if you could build this, or similar activities, into support options for people with dementia who you feel could benefit from more social interaction or activity.
To download or order a copy, select dementia as the topic from the drop-down menu at healthpromotion.ie
The HSE National HR Conference 2025, Transformation through People, Claochlú Trí Dhaoine was held in October. Chief People Officer Anne Marie Hoey opened the conference, while CEO Bernard Gloster addressed delegates, emphasising the importance of the HR function and its impacts on service delivery.
The day was structured to include presentations from international and national speakers under three subthemes:
1. Agility, adaptability and flexibility
2. Employment legislation
3. Inclusiveness in its broad context
Speakers included Peter Cheese, CEO, Chartered Institute of Personnel and Development; Damien McCallion, Chief Transformation and Technology Officer and Deputy CEO; Gillian Ledwidge Dunne, Regional Director of People (RDOP), Dublin and North East; Declan Hynes, RDOP, Dublin and South East; Patrick Walshe, Head of Employment Group, Philip Lee LLP; Michelle Ní Longáin, Head of Employment Law, Byrne Wallace Shields LLP; Laura Serrant, Laura Serrant Ltd; and Niamh Fawl, Senior Standards and Monitoring Officer, National Disability Authority.
Sessions were moderated by Paul Hume, Interim HoS, HR, HSE Community Services; Maria Daly, HoHR, HSE NHR/ER Services; and Eamonn Ross, ER Manager, Dublin North East RHA. The conference provided opportunities to learn, network and be inspired to play an effective part in the HSE transformation. All speeches are available to view on the Discovery Hub of HSeLanD within the Conference section.





If you work in healthcare, you are at increased risk of being exposed to flu and COVID-19

� Vaccines are safe and effective and provide the best protection from flu and COVID-19.
� All healthcare workers are recommended a flu vaccine.


� Some healthcare workers are recommended a COVID-19 vaccine. Any healthcare worker who wants a COVID-19 vaccine can get one.
� Vaccines may be available at work and are also available free of charge from GPs and Pharmacies.



