












































































































































































































































































































































































































Innovation and shared learning on show at Excellence Awards






1 New procedure room at Children's Health Ireland
2 Excellence Awards winners
4 HSE celebrates International Day of Disabilities
5 Day in the Life – oncology nurse Susan Nagle
6 Fight back against antibiotic resistance
9 HSE Productivity Unit
10 Digital for Care - a look at continual digital innovation in our health services
12 HSE website updates
13 Effies award win for QUIT team
14 Updates from the Health Regions Programme Team
16 Message from HSE Dublin and South East REO Martina Queally
17 HSE Dublin and South East updates
22 Benefits of HSCP placements for clinicians and students
24 HSE Career Hub
25 Patient Safety Act
26 Message from HSE South West REO Dr Andy Phillips
27 HSE South West updates
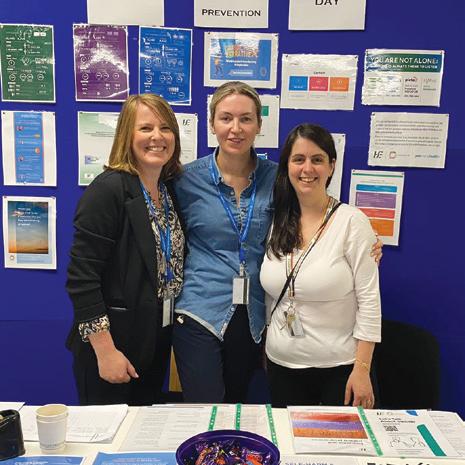
32 Let’s Talk about Suicide launch
33 Bereavement training
34 Surgical Hubs
36
HSE Annual Report and Financial Statements 54 Easy to Read consent policy
Assisted Decision Making mentorship
55 Meet our new Chief Social Worker 56 Message from HSE West and North West REO
Canavan 57 HSE West and North West updates
Updates
Spotlight on Climate Action measures
Spotlight on Screening
Message from HSE Dublin and Midlands REO
Thanks to everyone who has submitted stories for this edition. If you would like to see your initiative or work featured, you can submit through our online form at https://www2.hse.ie/services/forms/health-mattersstory-submission.html
Welcome to our winter edition of Health Matters, marking another year of change, innovation and challenges across our health service.
To see just how teams up and down the country are dealing with this transition, you only have to look at the finalists in this year’s Health Service Excellence Awards. The breadth of amazing work being done to make things better for our patients, service users and their families, as well as our colleagues, is outstanding.
In this edition, we reveal the winners in this year’s awards, which again generated huge interest. The awards continue to be a unique opportunity to showcase the work that is happening in teams and settings all across our health service every day. It also gives staff a chance to see what other teams around the country are doing and has led to much shared learning.
2025 will be the year that our health regions will be fully established, with all the structures in place by the beginning of March. Although change can bring some worries and anxiety for everyone involved, the new structure will ensure we can take a more patient-centred approach to healthcare.
We continue to shine a spotlight around the health regions to see what work is being done in each. We were delighted to learn about the 100th water birth in Our Lady of Lourdes Hospital after the resumption of the service last year. It is a fantastic option for all women to have and hopefully their experience can help other maternity units in the future.
It was also great to meet some of the community and public health nurses that play such a vital role in our communities. And their work will become even more invaluable as the aims of Sláintecare are implemented fully in the coming years.
This is just a small taste of the many stories we have featured inside. Thanks to everyone for their submissions for this edition.
Joanne Weston Editor
All rights reserved. Every care has been taken to ensure that the information contained in this
is
The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher is prohibited. © Ashville Media Group 2024.
Young patient Ruairi with the staff of St John’s Ward in the













New space at CHI ‘a testament to dedication and compassion’ of staff
A new intrathecal procedure suite in CHI at Crumlin has been designed specifically for children and young people to make the experience as comfortable and stress-free as possible.
Dr Jane Pears, Consultant in Oncology with CHI, said the opening of the new suite on St John’s Ward represents a ‘monumental step forward’ in the care they provide for their young patients.
“It underscores Children's Health Ireland’s ongoing commitment to
“Ruairi



recognising the strength and resilience of children who have cancer and enhancing their care and safety,” she said.
Children and young people aged 0 to 16 years who have blood disorders and/or cancers may be admitted as inpatients to St John’s Ward. Some of these patients need intrathecal chemotherapy – a treatment in which chemotherapy drugs are injected directly into the fluid-filled space between the thin layers of tissue that cover the brain and spinal cord.
and all of his friends on St John’s Ward have been so well looked after. Since he was first diagnosed, the team here make difficult experiences as easy on him as possible with kindness, humour and play.”
Until recently, patients on the ward who needed an intrathecal procedure were brought to theatre, but now they make a much shorter journey to the new state-of-the-art procedure room. This purpose-designed space will significantly improve the delivery of care for these patients. It will streamline treatments and ease the journey for children and their families during what is often a difficult and emotional period.
Ruairi was one of the first inpatients on St John’s Ward to use the new intrathecal procedure room. Ruairi’s Mum, Orla, said, “Ruairi and all of his friends on St John’s Ward have been so well looked after. Since he was first diagnosed, the team here make difficult experiences as easy on him as possible with kindness, humour and play.”







The Health Service Excellence Awards is an opportunity to showcase and celebrate examples of the great work that happens every day across our health service. This is the eighth year of the awards which aim to promote shared learning for other teams through our awards success stories.
The 2024 award ceremony took place on Thursday, 28th November in Farmleigh House in Dublin’s Phoenix Park.
Bernard Gloster, HSE CEO, commended the winners, “These awards create the opportunity to show innovation and creativity, which ultimately improves the services that we provide. Well done and thank you to all those short-listed as well as the winners. It is your work that helps pave the way to a brighter future for Ireland’s health service.”
Anne Marie Hoey, Chief People Officer, highlighted the positive outcomes achieved. "As well as providing an opportunity to recognise the great work of staff and teams across our wide range of services, the Excellence Awards is an important channel to share learnings with our colleagues across the health service.
"Through this pooling of knowledge and expertise, the projects inspire a sense of staff pride, teamwork and collaboration. This will positively impact the overall environment for our staff whilst improving outcomes for the people who rely on our care and support.”
Right Care Right Place Right Time – Sláintecare Mid West Community Healthcare are joint winners in the in the Right Place, Right Time Sláintecare category for the 'My Perinatal Self Care – Taking Care of Me' project.
A cross-service collaboration between Mid West ARIES and the Specialist Perinatal Mental Health Team (SPMHT), University Maternity Hospital Limerick began in April 2023 with a wellbeing workshop for women attending SPMHT. Participants requested practical support on how to implement a daily self-care routine.
A follow-up survey identified needs and resources including a co-produced self-care workbook.
The Meath Specialist Lymphoedema Clinic, HSE Dublin and North East were also joint winners in the Right Care Right Place Right Time – Sláintecare category. Their project titled 'Proof of concept initiativeEstablish community-based Specialist Lymphoedema Clinic' was deemed a deserving joint winner.
Speaking about this project, Thelma Dunne, Senior Physiotherapist, Specialist Lymphoedema Clinic said, “The aim of this service as per the model of care was to assess, treat, and manage clients with lymphoedema living in Co Meath. To improve the quality of life for clients living with lymphoedema. Also, to reduce the GP visits, public health nurse visits, risk of cellulitis and reducing hospital admissions”.
Public Health Nursing Primary Care, Corporate/ National Services won the award in the Excellence in Quality and Patient Safety category for their project, ‘Standardised maternal postnatal care in the Public Health Nursing Service’.
Public health nurses are mandated to visit families within 72 hours of discharge from the maternity services. This encompasses a comprehensive assessment of the postnatal mother. Preceding the development of this initiative, practices varied in relation to this assessment. There was no national guideline on maternal postnatal care and there were 13 different maternal postnatal records in use in the country.
CARE Community Virtual Ward, HSE West and North West was this year’s winner in the Improving Patient Experience category for the 'CARE— Community and Acute Respiratory Excellence Healthcare initiative'.
COPD hospital care in Ireland costs €90 million annually with multiple readmissions and little alternative to hospital care available. A proof of concept for a Community Virtual Ward ICT system, incorporating



respiratory rate trends, was designed with a small cohort of patients and was highly successful, achieving 100% hospital avoidance.
Sláintecare funded the model's expansion to all COPD patients in Donegal in May 2023.

The team from the Department of Cardiothoracic Surgery in University Hospital Galway, HSE West and North West won the Innovation in Service Delivery category with their project ‘Minimally Invasive Vessel Harvesting for Coronary Artery Bypass Grafts Surgery'.
Describing their project the team said, “Our unit's leg wound infection rate was up to 7% with open vein harvesting. We have reduced the wound infection rate from 7% to 0% with the introduction of minimally invasive vessel harvesting while maintaining our excellent clinical outcomes and improving patient satisfaction from the cosmesis of their wound and the avoidance of post-operative complications."
Engaging a Digital Solution
St James's Hospital, HSE Dublin and Midlands won the Engaging a Digital Solution category.
Previously, St James’s Hospital patient flow processes were fragmented and manual, requiring high volumes of staff time to identify and
Area and location
St James's Hospital, HSE Dublin and Midlands
Public Health Nursing Primary Care, Corporate/National Services
Mid West Community Healthcare, HSE Mid West
Meath Specialist Lymphoedema Clinic, HSE Dublin and North East
CARE Community Virtual Ward, HSE West and North West
Department of Cardiothoracic Surgery, University Hospital Galway, HSE West and North West
Prosper Group, HSE Dublin and North East
Category



communicate bed management matters. Additionally, no forum existed for multi-disciplinary teams to proactively coordinate discharges. A digital solution to visualise patient flow, reduce cumbersome processes and improve communication was proposed. The results were their project titled 'Visual Hospital Management System improves patient flow and bed management'.
Working together for a Greener Health Service Working together for a Greener Health Service is a new category this year. Prosper Group, HSE Dublin and North East were the winners in this category with their 'Energy Management and Sustainability (EMS) initiative'.
Prosper Group provides supports to 530 adults with intellectual disabilities across Fingal and Meath. The issue of climate action came to the fore with growing concerns of the organisation's carbon footprint, energy costs and the disproportionate impact that climate change has on the individuals that they support.
Pat Lacey, Procurement Officer, Prosper Group said, "The Energy Management Sustainability initiative within the Prosper Group has been monumental. It has helped in so many ways, staff and service users in entering into a world where service users not just believe that they can be involved in a movement to change but that they can actually drive it."
Watch videos and learn more about each of the winning projects on www.hse.ie/excellenceawards
Engaging a Digital Solution
Excellence in Quality and Patient Safety
Right Care Right Place Right Time - Sláintecare
Right Care Right Place Right Time - Sláintecare
Improving Patient Experience
Title of project
Visual Hospital Management System improves patient flow and bed management
Standardised maternal postnatal care in the public health nursing service
My Perinatal Self Care – Taking Care of Me
Proof of concept initiative - Establish community based Specialist Lymphoedema Clinic
CARE—Community and Acute Respiratory Excellence Healthcare Initiative
Innovation in Service Delivery Minimally Invasive Vessel Harvesting for Coronary Artery Bypass Grafts Surgery
Working together for a Greener Health Service
Prosper Group's Energy Management and Sustainability (EMS) Initiative
Le Chéile Network, the HSE's national staff network for staff with disabilities, long-term health and neurodiverse conditions and allies, recently kicked off its 2024 International Day of People with Disabilities (IDPWD) campaign with energy and excitement. IDPWD takes place on Tuesday, 3rd December 2024, with the aim of promoting empowerment and helping to create real opportunities for people with disabilities. This year, the focus of the campaign is on the importance and positive impact of reasonable accommodations in the workplace.
The term ‘disability’ is used to reference many different conditions that can be either visible or invisible. This may include visual, hearing, mobility, learning, speech, neurological and other types of disabilities. Different definitions of disability are used in different contexts, for example to set eligibility for services, or to outlaw discrimination on grounds of disability. There can also be a wide range of difference between how individuals with a particular condition are affected, ranging from mild to severe difficulties.
12% of the HSE workforce reported a disability. Approximately 15 to 20% of the population has a neurodevelopment condition such as ADHD, Autism, Dyspraxia or Dyslexia amongst others.
Le Chéile Network
Le Chéile Network has grown from strength to strength since its formation in 2022, and now has

members from all parts of the HSE. Supported by the HSE’s Diversity Equality and Inclusion team, it aims to promote a positive working environment where all employees feel supported and valued. It acts as a representative voice for staff with disabilities employees, a forum where staff can discuss experiences and share insights in a safe space, and a resource on disability topics. The Le Chéile Network has a virtual meet-up every two months.
Le Chéile Network also assists with raising awareness on issues to the wider workforce such as the importance of inclusive communications and the provision of workplace adjustments for staff with disabilities. Reasonable accommodations can include adapting a workplace premises, providing equipment or assistive
technologies, or providing training or other supports that might help a staff member carry out their work.
“I have integrated the use of assistive technology into my daily work practices. As someone with dyslexia, I really struggled with the documentation demands of my job role. However, having access to a reasonable accommodation has positively enhanced my experience and productivity in the work place,” said Kellie O’Farrell.
Managers play a key role in supporting staff with disabilities in the workplace and ensuring that staff have the correct supports to perform the duties of their roles.
Contact diversity.HR@hse.ie if you are interested in joining the Le Chéile Network
I took up my post as an Acute Oncology Clinical Nurse Specialist in June 2021. The Acute Oncology Service (AOS) provides telephone triage to cancer patients at home who have issues or concerns while they are under the care of the haematology or oncology teams.
The service aims to keep cancer patients well at home and out of hospital. It also provides the patients with a regular point of contact, and a name they will know. This encourages early intervention, which is very important, given the kinds of side effects some cancer patients can experience from their medications.
My day starts before 8am with a check of the hospital computer system to see how many patients

are on the wards and in the ED. Not all of our patients can be treated at home and some need to come in. I see these patients, take bloods when needed, and provide support and education to nursing staff there. As well as liaising with the haematology and oncology teams and other members of staff on the wards, I will also go to see specific patients.
Telephone calls from patients start coming in from 8am. I answer these calls and return any that I miss as a matter of priority. The lines are open Monday to Friday, 8am to 5pm.
A big part of my role is liaising with support services in the community, including palliative care teams, GPs, public health nurses and the community intervention team. I also see patients who come to us
for their first appointments with the oncology consultants, giving them support and education around chemotherapy.
What I enjoy about my job is that every day is different. My favourite part is having the chats with the patients, whether on the phone or in person, and helping to bring a smile to their faces.
Observing the positive impact of healthcare expertise on someone’s life is deeply fulfilling and constantly reaffirms my passion for nursing.
Above all, my goal is to provide compassionate care that helps patients not only survive but also thrive. Seeing patients regain their health and vitality is incredibly satisfying, and gratifying.
Taking an antibiotic when it isn’t necessary does more harm than good
As we enter cold and flu season, we must remember to ask ourselves that key question: do I need to see a doctor or can I treat this illness myself at home?
European Antibiotic Awareness Day (EAAD) is an annual event to remind everyone how valuable antibiotics are, how important it is that we only use them when we need them, and highlight that these amazing drugs are under threat from the growing problem of antibiotic resistance.
Dr Eimear Brannigan, HSE National Clinical Lead for Antimicrobial Resistance and Infection Control (AMRIC), explained, “Antibiotics are amazing drugs that eliminate bacteria and are usually very safe for us. We have become dependent on antibiotics for many of our routine operations, treatments and for critical surgery such as organ transplants, cancer treatment and many, many illnesses.”
Your GP will be able to judge if you are likely to have an infection that needs treatment with an antibiotic. If your GP says you do not need an antibiotic, this is good news because antibiotics should only be taken when you need them to treat a bacterial infection.
Antibiotics can cause more harm than good if taken unnecessarily. Most common illnesses, including influenza and colds, are viral infections – antibiotics do not work
Dr Eimear Brannigan, National Clinical Lead, HSE AMRIC.



for infections caused by a virus.
Antibiotic resistance is caused by the overuse of antibiotics. It happens when bacteria or bugs becomes resistant to different types of antibiotics. These are sometimes called superbugs. So, antibiotics that once worked well to treat an infection may no longer work as well as before or, do not work at all.
“We want to get the message out that it can be very harmful to take an antibiotic if you don’t need it. If you are suffering from a cold or flu and think that an antibiotic is useful to take ‘just in case’, the next time you have an infection that needs an antibiotic, the bacteria in your body may have become resistant to it because it was previously used unnecessarily. It is not just about a societal worry about the rise of superbugs. We are putting our own health directly in danger,” said Dr Brannigan.
The AMRIC lead said that doctors are starting to turn the tide against overuse of antibiotics by using their consultation skills to educate their
The COVID-19 and flu viruses circulate at high levels this time of year. As a healthcare worker, you’re at high risk of being exposed to these viruses.
Protection from previous vaccines or a previous infection weakens over time, and the COVID-19 and flu viruses are changing. Getting your COVID-19 and flu vaccines this winter is the best way to protect yourself and the people you care for.
The vaccines are free for healthcare workers and safe to get at the same time. They may be available where you work, or you can go to a participating GP or pharmacy.
Find staff vaccination clinic details at HSE.ie/ staffclinics.


Your GP will be able to judge if you are likely to have an infection that needs treatment with an antibiotic. If your GP says you do not need an antibiotic, this is good news because antibiotics should only be taken for when you need them to treat a bacterial infection.
patients and reassure them if they have an illness that can’t be treated with an antibiotic.
“Our GP colleagues are using their expertise and knowledge in the consultancy room. They are the frontline of the messaging that antibiotics are useless against viral infections and can often do more harm than good,” she said.
“Of course, we know there are pressures on doctors to prescribe antibiotics if a patient presents feeling particularly unwell and is expecting to get an antibiotic. And we understand that a doctor at the start of the day can be better equipped to deal with these demands than a very busy GP at the end of the day. So it’s also vital that we educate the public and manage their expectations about getting prescribed an antibiotic.”
She acknowledged that it can be difficult for people to recognise when they might need an antibiotic, particularly parents of young

AMS
staff in University Hospital Waterford (UHW) kicking off European Antibiotic Awareness Day and World AMR Week with an information stand in UHW.

children who don’t want to take any risks with illnesses.
Dr Scott Walkin, GP and ICGP Lead for Antimicrobial Resistance, said, "A key message of EAAD is to use antibiotics only when they are likely to help someone who is sick get better. Antibiotics do not help you to get better any quicker if the infection is caused by a virus. As a GP, I still get some requests for antibiotics from people who have colds and flus or for their children. Antibiotics will not help them and, in fact, can cause side effects like upset tummies,
“We have been holding events for staff across the new health regions to teach awareness about antibiotics. We have found that hearing patient stories first-hand has the most impact."
or skin
It is safer for you not to take an antibiotic you do not need, because antibiotics, like all medicines, can have side effects. Vaccination reduces many viral infections, so it is important for us all to be fully vaccinated.”
Dr Brannigan highlighted the fact that educating healthcare workers on the dangers of overuse of antibiotics is crucial to getting the message out to the public too. “We have been holding events for staff across the health regions to teach awareness about antibiotics. We've found hearing patient stories first-hand has the most impact. So we have been travelling around with patients telling their stories, sharing the impact having an antibiotic-resistant infection has had on them,” she said.
Coughing is part of your body’s way of protecting your lungs. It is better to cough up phlegm than to have it stay lower in your lungs. Coughing spreads the germs that caused your cough in the first place so it is important not to spread the illness to others. You can do this by coughing into your elbow or coughing into a tissue, binning the tissue immediately and washing your hands afterwards.
Most coughs are viral not bacterial; that means they get better just as fast without antibiotics. If your cough is caused by a cold (virus) and you need advice, talk to your pharmacist first. Over-the-counter cough remedies may ease your cough and help you to bring up phlegm so that coughing is easier. Paracetamol or ibuprofen will relieve pain. Many people also find that hot honey and lemon drinks are helpful.
Antibiotics do not actually ease a cough – they kill bacteria. You can get unpleasant side effects from taking antibiotics, including tummy upsets, rashes, vomiting, nausea and abdominal pain. You should only take antibiotics if you need them or they might not work when you do need them. Resting, drinking plenty of liquids and taking time

to allow your immune system to fight the infection are very important. If your child has a cough but is in reasonably good form and is drinking well, there is often no need to do anything. Your child’s immune system will fight the bug that is causing the cough. If you need advice, talk to your pharmacist. Paracetamol or ibuprofen will relieve pain or fever. If your child is over six years of age, they can also take overthe-counter cough remedies. Saline nose sprays can help to clear the nasal passages. Coughing spreads germs so get your child to cough into their elbow or cough into a tissue, bin the tissue immediately and wash their hands. If you are worried, especially about young children or older people, then it’s best to have a face-to-face consultation with your GP. If your GP tells you your own immune system can fight this infection, and you do not need antibiotics, then this is good news. It means you don’t have to take any chance of getting antibiotic side effects.
It can be difficult to tell when you need to see a doctor and when you just need to treat the symptoms at home. The HSE, in partnership with general practitioners and pharmacists, has a website which gives practical, commonsense advice and information on dealing with many common illnesses like colds, flu, earaches, sore throats, tummy bugs and rashes www.hse.ie/conditions/commonillnesses/ provides sound advice to give us the confidence and skill we need to take care of ourselves and our families without resorting to antibiotics.
The most effective weapon against common viral infections is your body’s immune system. The best way to treat symptoms of most common viral infections is rest, drink fluids and take paracetamol or ibuprofen. It is still important to get checked by your GP if you are worried, especially for very young children, older people and those with long-term medical conditions or whose immune system is suppressed.
How long will it last?
Earache – Most get better by 3-7 days
Sore throat – Most get better by 7-8 days
Cold – Most get better by 14 days
Cough – Most get better by 21 days
'Ensuring we use everyone's time more efficiently and effectively - small changes, big results'
Investment in our health service is now at its highest level in the history of the State. The ever evolving nature of health service demand and care delivery pathways (including personalised medicine) means providing the maximum amount of appropriate patient care to the population is an ever increasing challenge. This challenge needs to be addressed in a sustainable way. Ensuring we are optimising the productive use of our available and finite resources to deliver the maximum amount of patient care is vital to achieving this.
In this context, one of our most valuable resources is time. To quote the author William Penn, "Time is what we want most, but what we use the worst." Ensuring we use everyone's time - our service users', their families', and our staff's - in the most efficient and effective way is key to optimising the productivity of the health and social care services we deliver to the public every day.
By eliminating unnecessary variation, duplication and waste from our processes, we can release time to staff to deliver more care to the public we serve. We can achieve this through process optimisation and innovation, operational and clinical efficiencies, and faster decision-making.
Stephen Donnelly, Minister for Health, established a joint Department of Health/HSE Productivity and Savings Taskforce in January 2024 to focus on optimising the productivity of the health service.
Our CEO Bernard Gloster established a dedicated HSE National Productivity Unit (NPU) in June 2024 to support the work of the joint taskforce.
The NPU is the focal point through which a standardised framework for productivity throughout the HSE will be delivered.
This productivity framework will enable staff across our health regions and HSE Centre to collaboratively
innovate, embed, sustain and scale data-led and evidence-based initiatives to improve efficiency and optimise productivity across operational and support services.
Our aim is to support health regions in their continued focus to improve the quality of care, to reduce wait times and deliver better health outcomes for patients.
We will highlight and recognise good practice based on what is known, what has worked well and the lessons learned. We wil support staff to create and share new ideas for a better patient and staff experience, helping them to build a culture of continuous improvement, collaboration and innovation.
Our current area of focus is Acute Out Patient Departments (OPDs). We will be applying learnings from other initiatives to our OPD processes, to optimise productivity and ultimately progress towards achieving the Sláintecare maximum wait time targets.

Digital for Care 2030 webpage - Stay informed. Get involved
The Digital for Care 2030 programme team recently launched the Digital for Care 2030 webpage. Digital for Care 2030 is the framework approved by Government for investment in digitisation of our health services.
The webpage will give you up-to-date information on many of our programmes, from the big strategic initiatives like the implementation of Electronic Health Records (EHR) to some of our smaller initiatives.
It will focus on keeping staff up-to-date on evolving plans to help enhance their digital health literacy and capabilities.
The webpage will also host details around a Digital Health Clinical Safety framework to support healthcare providers in the efficient, effective and safe delivery of healthcare.
In addition, it will give you information about who to talk to, how to get involved and how to share our Digital for Care 2030 news.
Since the publication of the Department’s Digital Health Framework and our Digital Health Roadmap 2030, there have been a number of key milestones. The launch of virtual wards in two hospitals, the launch of MedLIS in Beaumont, and the progression of the innovative Single Sign On Project are among the great ongoing developments to support our digital transformation journey. Through robust stakeholder engagement and purposeful communication, we’re looking forward to taking the next steps together with transformational programmes such as our HSE app and EHR developments.
Digital Health Learning Passport on the way
It's important to build upon our foundations and to take full advantage of the opportunities digital health technology has to offer. The HSE Digital Health Learning Passport is currently being developed to equip all HSE staff with tools and skills to enhance their digital health capabilities.
The Digital Health Learning Passport will provide valuable insights and practical skills for all staff to apply to their daily work. At first, this will consist of three foundational learning modules:
• Digital Health Literacy
• Data Literacy
• Digital Health Clinical Safety
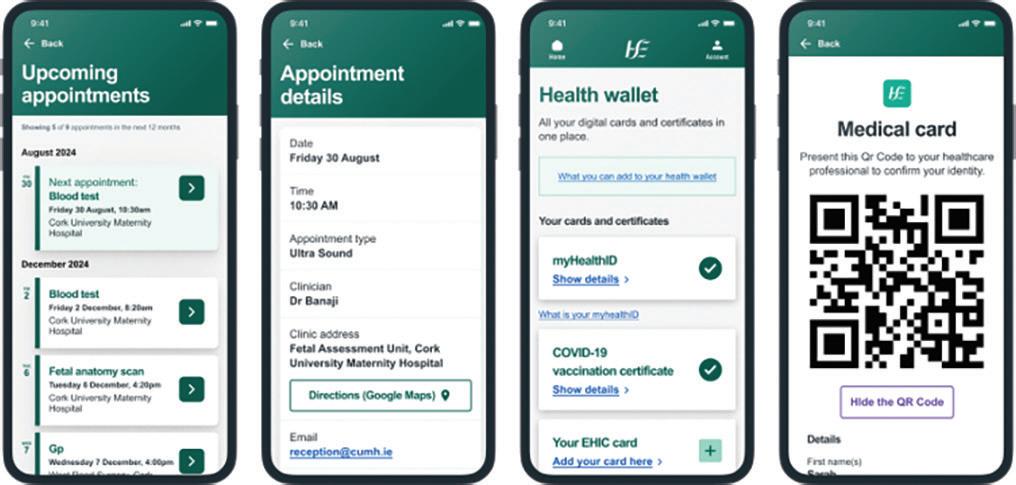
The Department of Health and HSE have developed a new digital health service, the HSE App. It gives people secure access to information about their healthcare. It is one of the first initiatives delivered as part the HSE's implementation of Digital for Care, the government digital health framework.
Over time, the app will become the main channel for people to securely access their health information and a range of services online, with an initial focus on enabling access to their hospital appointments, carrying a list of their self-declared and reimbursed medication, COVID-19 and flu vaccination records and digital versions of their European Health Insurance Card and Medical Card.
The first release is focusing on maternity services. Expectant mothers are able to view their hospital appointments. During 2025, people using the app will be able to see all their hospital appointments, along with their referrals and waiting list information.
The team is working with patients and clinicians to design the app and a pilot ran with a group of expectant mothers in Cork University Maternity Hospital in June of this year. Feedback from the pilot helped us to refine and improve the app’s functionality before its wider release.
The app was very well received during the pilot, with one expectant mother telling us, “The app has been amazing, very handy, and completely invaluable to me during my third trimester with all the extra appointments.”
To support the rollout, the project team are engaging with maternity services around the country. The launch of the app is a significant step towards putting your health in your hands and a great example of how the HSE is delivering Digital for Care. For the first release, the HSE App is available in English and Irish. Other languages are being explored for future versions. Any member of the public aged 16 and over can use the HSE App. The app will be available from the App Store or Google Play Store when it launches.
For more information see www.hse.ie/HSEapp
Further information will become available as the Digital Health Learning Passport development progresses. For all queries, please contact: digitalforcare@hse.ie
Update on two significant projects currently being worked on by the HSE Digital team.
The HSE Digital team has been working to transform HSE.ie over the last five years. Based on extensive user research, we are in the process of separating the website into three distinct web presences.
HSE.ie is focused on patients and service users and is where they can go to take care of their health and access health services.
HSE Staff (https://healthservice.hse.ie/staff/) is where staff members can find news, events, training and policy information relating to their employment.
About the HSE (https://about.hse.ie) is where stakeholders in health can go to find useful, trusted and engaging information about the HSE as an organisation. A web presence for each of the six new health regions is also available on about.hse.ie.
We would like to provide an update on two significant projects that are currently being worked on by the Digital team.
This new web presence provides information about how the health service works. Users can also find information about HSE teams (the high level structure of the organisation), along with publications, news and a new jobs search that will be available in quarter 4 2024.
There are two topic-based sections, ‘Our work’ and ‘Leadership and operations’, where users can find out:
• what the HSE does
• who is in charge
• how the HSE is structured
• what the HSE’s values are
• how the HSE is improving
{myregion}.hse.ie is where users go to understand how each health region works and learn more about: :
• what services are in each region
• regional news
• regional publications
• the region itself
• regional jobs (quarter 4 2024)


You can access the health regions web presences using the following links:
• dublinnortheast.hse.ie
• dublinmidlands.hse.ie
• dublinsoutheast.hse.ie
• midwest.hse.ie
• southwest.hse.ie
• westnorthwest.hse.ie
Content transformation
We are in the process of transforming the content for the About the HSE and Health Regions web pages. Content transformation is the process of rethinking existing content and making it more purposeful and accessible.
We are basing new content on user needs. These are the specific requirements a person has when they view or engage with your content. User needs are important because they help us to:
• understand what our users want from us
• create new content where needed, or repurpose existing content
• create a simpler website structure to increase engagement
For more information: digital@hse.ie
Benefits for stakeholders in health
• Users will not need to have an understanding of the organisational structure of the HSE to get the help they need or engage with the HSE as an organisation
• There will be less content which means it will be easier to navigate, maintain and ensure that it is accurate and up to date
• Users will be able to understand the highest priorities of the organisation and how it aligns with their own needs
In a survey conducted by the Digital team in January 2023, 61% of the respondents said they had come to the site looking for information on a HSE service
Information about health services is one of the main reasons why people visit HSE.ie. In a survey conducted by the Digital team in January 2023, 61% of the respondents said they had come to the site looking for information on a HSE service.
Services on HSE.ie is where people who use our services can find the information to access the care they need. It’s also where the people who provide healthcare can find the information they need about the services that their patients can access.
The Digital team has been working to improve the user experience for discovering health services online.
The most up-to-date service listings can be found by searching for ‘HSE urgent and emergency care’, ‘Find a hospital’ or ‘Find a primary care centre’.
Benefits for service users
• The service listings can be grouped and searched by:
» region
» type of service
» age group or patient cohort
» services near me
• Service listings are optimised for search engines
• The information within the service listings can be made available through different channels, such as HSE.ie, the HSE App and other websites
• Service information can be combined with the appointment reminders in the HSE App, providing timely information to patients when they need it
The teams are working to iteratively map services by health region and by health area to represent the changing structures in service delivery across the HSE.
The QUIT campaign has won a Gold Effie. Effie Worldwide stands for effectiveness in marketing and spotlighting ideas that work. The Effie Awards are known by advertisers and agencies globally as the most distinguished award in the industry.
The awards were entered by over 70 advertisers and only 30 got shortlisted. At the awards ceremony a total of 19 Effies, including four Gold, six Silver and nine Bronzes, were handed out.
The HSE Communications and Public Affairs Division Campaigns team leads on behaviour change and social marketing campaigns for the HSE. We use evidence and research insights to create campaigns that help people to navigate health services and improve their health and wellbeing.
We entered the QUIT campaign in the Public Service and Government Category with our creative ‘Take back control’ which launched in January 2023. ‘Take back control’ contributed to the most successful year ever for the HSE in terms of people accessing QUIT services for support.
Winning a gold Effie is a fantastic achievement and it shows the hard work carried out by all those in the Communications and Public Affairs Division in close collaboration with the Tobacco Free Ireland programme. There is a large team of people who work across QUIT including colleagues in Campaigns, Press and Media, Digital, Internal communications and Social Media. The QUIT campaign works in partnership with Publicis Dublin on the advertising creative and Spark Foundry on the media planning and buying.

Bringing community health services and hospitals together means we can take a more personcentred approach to healthcare. This means that patients / service users can be cared for closer to home, whatever their health needs.
Transition to the interim health regions structures
Health regions will be fully established by Monday, 3rd March 2025. Until then, an interim structure is in place in 5 of the 6 health regions. In HSE South West, all existing arrangements will stay the same until 3rd March 2025.
During this time, our main priorities will be:
• maintaining existing levels of service
• maintaining quality and patient safety
• making sure only necessary changes are made
• communicating these changes in a timely way
• concluding the future state design
Recruitment
Integrated healthcare area managers started in their posts on Tuesday, 1st October. Executive Management Teams are in now in place in each health region. Recruitment is also underway for six Regional Patient and Service User Lead roles.
Watch back the health regions webinar from Thursday, 26th September on YouTube. For more information email healthregions.team@hse.ie.
The HSE Patient and Public Partnership Conference took place in September. The conference included a presentation on the design of patient and service user structures within health regions. Ray Bonar, General Manager, Health Regions Programme, and Joan Johnston, Patient and Service User Partner, gave the presentation.
Health regions webinar series
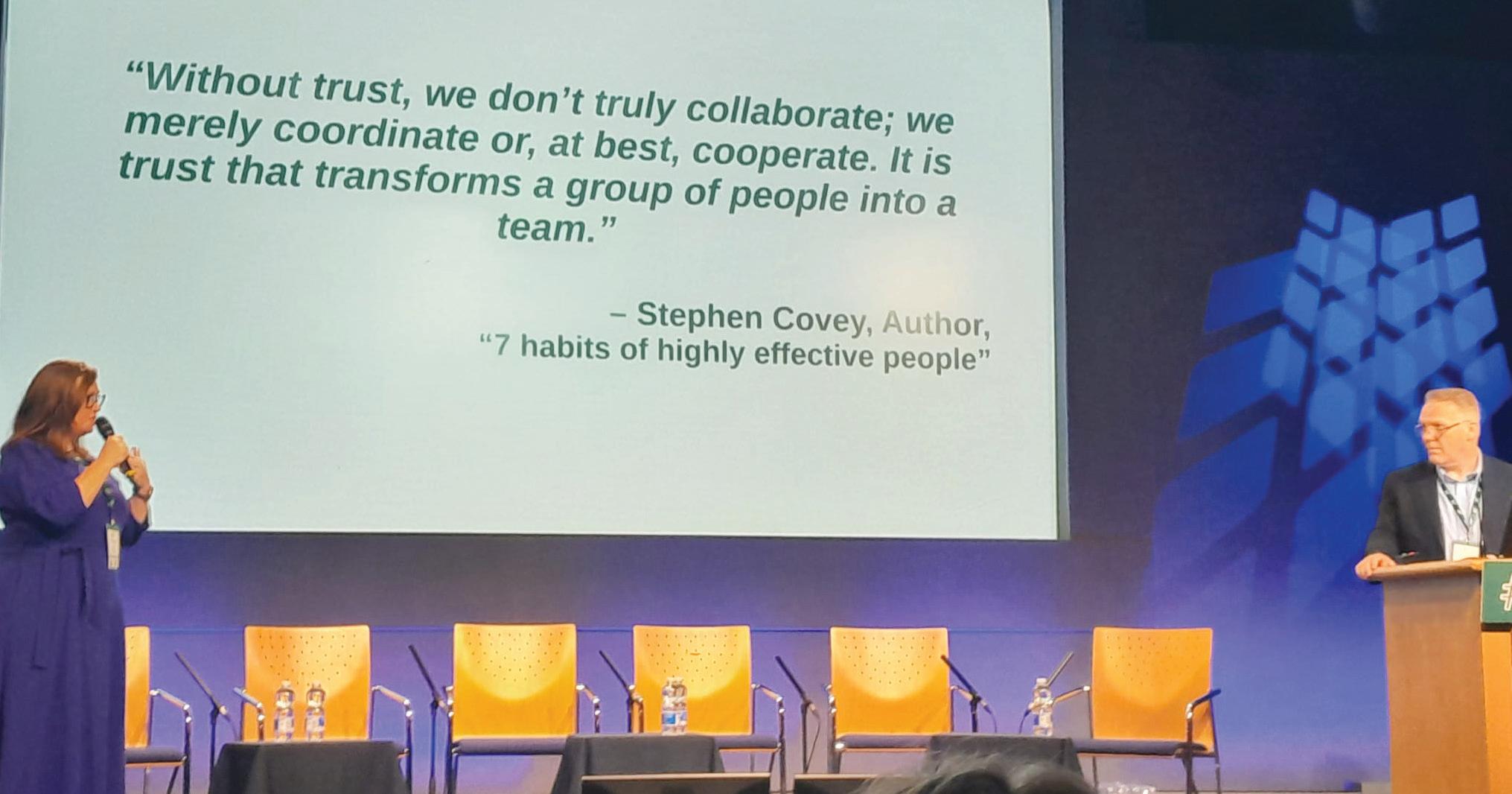
The second webinar in the health regions webinar series took place on Thursday, 26th September. The webinar titled ‘Balancing Stability with Change’ creating conditions for integration:
• provided an update on health regions implementation
• focused on managing change in the HSE as we move towards more integrated care
• shared relevant resources and first-hand experiences of implementing change from the Integrated Care Programme for Chronic Disease
• The next webinar in on Thursday, 12th December from 1pm to 2pm. Registration is now open at bit.ly/IntegratedWorkingWebinar
Key considerations during change
At times of change, creating a sense of stability for teams is really important. This can be challenging given the level of uncertainty and ambiguity that we often face.
Maintaining a clear focus on shared purpose and prioritising communication and engagement are the most important considerations as we progress Health Region reforms.






Image from the health regions webinar in September, ‘Balancing Stability with Change: creating conditions for integration’.
We know that people do their best at work when:
• their environment is predictable
• the point of their efforts is readily apparent to them
• they have some sense of control over their immediate surroundings
• they are part of a stable set of relationships
• they feel connected to place and ritual
Attending to these core elements in our work environment can create the conditions for change and enable individuals and teams to contribute meaningfully and add value. It is important that people know what is expected of them in addition to being clear on individual responsibilities to act collectively. Getting the ‘whole system in the room’ is key
– creating space for conversations to take place locally, bringing a wealth of experience to finding solutions that work. Teams will constantly be challenged with emerging issues, so being flexible and learning how to adapt to the unpredictable is important.
Access team-based resources on Creating the Conditions for Change and Integration here: bit.ly/ChangeIntegration
It has been a busy and productive number of months since taking up my role as Regional Executive Officer (REO) of HSE Dublin and South East. Several key achievements have been met to prepare for, and enable, the transition to our new health region structures.
Getting the right management structure in place was an immediate priority. I wanted to build an expert team to support change and drive service improvement. I am delighted that our new Executive Management Team (EMT) for the region is now almost fully in place, with just a few positions remaining to be filled.

reform we wish to deliver. With this in mind, we have communicated and engaged regularly with staff to ensure they are kept appraised as we navigate this time of change.
Another important step towards a more integrated healthcare model was the establishment of three new Integrated Healthcare Areas (IHAs) within our region. These new structures came into effect on 1st October, marking a significant milestone.
These healthcare areas will be pivotal in bringing together acute and community services in each area to support and enable integrated care. The boundaries of these new health region structures are defined as follows; Carlow, Kilkenny and South Tipperary; Waterford and Wexford; and Dublin South and Wicklow. An IHA Manager has been appointed to each IHA where they will plan and deliver services tailored to the specific needs of the populations in these areas.
It is very important to our EMT that we continue to engage with our staff in this change as they will be integral to the
“I am absolutely focused on building on the opportunities the new health structures in our region present. We want to transform health and social care services – ensuring that the right care is delivered in the right place and at the right time.”
I have also enjoyed meeting and speaking directly with service users across our region. Service user engagement is vital to achieving a person-centred model of service delivery and I will continue to engage with this important group of stakeholders.
Our vision is to realign our structures into a new, fullyintegrated model of healthcare delivery by March 2025.
I am absolutely focused on building on the opportunities the new health structures in our region present. We want to transform health and social care services – ensuring that the right care is delivered in the right place and at the right time.
I want to thank staff for their support to date during this period of change and to acknowledge their incredible commitment to providing a quality service for the people we serve. I have witnessed first-hand the breadth of integrated work already taking place throughout our region, and it is upon these foundations that we will look to build on. You are all working during a time that is very exciting. Real changes are being made that will have a lasting impact on the health and wellbeing of our local communities.
I would also like to take this opportunity to appeal directly to staff to avail of their free winter vaccines to protect yourself, your loved ones and our service users this winter. Vaccination is the safest and most effective way to protect against flu and COVID-19.
And lastly, I wish all our staff across HSE Dublin and South East a safe and peaceful Christmas.


To mark World Parkinson's Day, Primary Care services in Bray, Co Wicklow hosted a free, drop-in event, showcasing the range of support services that are available for those with Parkinson's Disease.
The event, a collaboration between local HSE clinical services and community partners, gave patients and carers the opportunity to speak directly to local services to find out what support is out there and how to access it. The purpose of the event was driven by Sláintecare, which aims to support people to stay healthy in their own homes and communities for longer.
Gary Boyle, Patient Advocate, praised the event. “It shows what can happen when you bring people together who are living with Parkinson’s. It lifts everybody. But for people living with Parkinson’s, it does something more. It gives them that confidence that the more I do this, the better it will become. And that might sound strange with a deteriorating condition such as Parkinson’s, but it really can get better. You can slow that down. And with a little support, you can slow it down even more.”
One of the highlights of the event was a performance by the Wicklow Parkinson's Choir.
Valerie McCoy, a member of the choir, said, “I love going, I wouldn’t miss it, it’s every Monday morning and I value that time. I live on my own and I’ve Parkinson’s. I live out in the country, so I’m really cut off from civilisation and from social life. So for me, it’s absolutely vital. And of course, coming here together as a group is great because the carers, husbands and wives can share helpful hints, you know. There are things about taking your medication at certain times of the day that are vital that I never knew about, but I learned about from there. So you know, we share ideas and we help each other.”
Wicklow Parkinson's Choir perform at the event.
Awareness morning was held in the SETU Arena in Waterford to mark Heart Health month. It was a joint initiative between University Hospital Waterford Cardiology Service and the HSE South East Community Healthcare’s Integrated Community Cardiovascular Team.
Laura Fennessy, Cardiac Rehab RGN, and Mairead Hanrick, Chest Pain CNS at the HSE’s cardiovascular health awareness morning.
The occasion provided the public with an opportunity for cardiovascular health screening, to gain risk management education/awareness and access to cardiovascular specialists. Michelle Brennan, Integrated Care Cardiovascular Clinical Nurse Specialist/Waterford Primary Care Centre and UHW said, “This event was an opportunity for people to connect with support services in their local community and to hear some talks from healthcare professionals to help understanding of how to take care of one’s health and heart. We hope to have another such occasion early in the new year, in conjunction with our chronic disease services, including podiatry, diabetes and respiratory supports.”
Clinical rooms at St Luke's introduce mobile devices
St Luke's General Hospital, Carlow/Kilkenny (SLGH) promoted medicine information and medication safety across the hospital with the recent introduction of mobile devices to clinical rooms.
Mobile tablet devices were
introduced in clinical rooms across SLGH to reduce the reliance on paper-based documents and to provide access to quality, accurate information at the point of medicines administration. The mobile tablet devices are
pre-loaded with relevant medicines information resources, standardised policies and guidelines. These are written and managed by the Pharmacy Department and approved by the Drugs and Therapeutics Committee.

Four years of study in the South East Technological University (SETU), featuring 80 weeks of clinical placements in HSE South East Community Healthcare Mental Health services, was marked in a ceremony in Waterford for the graduates of SETU’s BSc (Honours) in Psychiatric Nursing.
Concluding their fourth year of the course and a 36-week continuous internship with HSE South East Community Healthcare
(SECH), the students were presented with their qualifications at an occasion hosted in the Tower Hotel.
Speaking at the ceremony after making presentations to the students, Emer O’Donnell, Clinical Placement Coordinator/Assistant Director of Nursing, HSE South East Community Healthcare, said, “This group of graduates commenced their training in 2020 at an unprecedented time in the Irish health services. They have
both our sincere appreciation and admiration for their commitment.
“Psychiatric/Mental Health nursing is a specialist field within the healthcare profession. It involves an interpersonal, caring process which acknowledges the uniqueness of each person.
"The psychiatric nurse is concerned with the promotion of mental health, the prevention of mental illness and the provision of care to those with mental health problems.”
Shankill Primary Care Centre, Co Dublin recently hosted a Community Day to highlight a range of health and community supports available in the area and how to access them. The first-of-its-kind event for the area welcomed service users and residents to tour the Centre and meet with staff from a range of on-site services, including nursing, psychology, dietetics, speech and language therapy, physiotherapy, social work and occupational therapy.
Representatives from the HSE’s Social Prescribing, Chronic Disease Management and Integrated Care
Programmes Older Persons (ICPOP) services were also available to outline the range of specialised support that is available in the region for those that need it. HSE services were joined by a range of partner organisations that are active in the community, including Purple House Cancer Support, Alone, Healthy Foods Made Easy and Living Well with Dementia.
In addition, visitors were welcome to attend a great line-up of talks from experts, including Falls and Frailty, Service User Engagement, Aging Well and Tots and Tums for New Mums.

The Dublin South and Wicklow Social Inclusion team are committed to supporting the national movement to address period poverty for women and girls.
The Period Dignity team supply period products to diverse groups of women, including LBTQI, Ukrainian, International Protection applicants, Irish Traveller women, homeless and other marginalised groups. The range of period products supplied are fully sustainable including reusable pants, pads, cups, eco-friendly tampons and pads.
In addition to supplying products, the team also created information booklets on Period Dignity and Women’s Sexual and Reproductive Health which explain the movement, the issues and importantly the physical and hormonal processes that occur for women and girls in the period of menstruation. These resources aim to address the information gap that can occur around topics of women’s reproductive health due to stigma, embarrassment, lack of opportunity or access to health education and poverty.
The aim is to normalise and celebrate periods and the natural processes that occur as young girls develop into women. Hard and digital copies are available, with links to further health and information and support groups on many topics.
Education masterclasses have also been rolled out following collaboration with patient engagement services and focus groups. These sessions gave up-to-date health information on women’s health and issues. The team has also partnered with Dun Laoghaire-Rathdown County Council and Wicklow County Council to facilitate additional education masterclasses in the coming months.
In addition, the Period Dignity teams across HSE Dublin and South East are planning an upcoming awareness exhibition. The exhibition will be in libraries, health centres and councils countrywide.
The Social Inclusion team with the awareness material.
Sinead Lawlor, National Practice Development Officer for Public Health Nursing, who won first prize for her poster at the recent National Sepsis Summit.
The Mental Health Liaison Psychiatry team at their World Suicide Prevention Day event at St Vincent's University Hospital.

Sinead Lawlor, National Practice Development Officer for Public Health Nursing (PHN), won first prize for her poster presentation on ‘Maternal Postnatal Sepsis Recognition and Early Referral in the PHN Service’ at the recent National Sepsis Summit in Dublin Castle.
This national quality improvement initiative was developed in response to a maternal death from sepsis. The project aims to improve PHNs’ postnatal care to mothers to include sepsis awareness. The award is great recognition for local PHN services, who have rolled out a new postnatal assessment education and maternal health record over the past few months with great success.
Well done to Sinead for her work and for sharing the great work of PHNs to recognise and refer maternal sepsis.
To mark World Suicide Prevention Day, the Mental Health Liaison Psychiatry team in the Dublin South and Wicklow Healthcare Area hosted an event in St Vincent’s University Hospital. Their goal was not only to generate awareness of suicide and the supports that are available to those effected by it, but also to change the narrative around suicide. Changing the narrative on suicide aims to encourage individuals, communities, governments and organisations to engage in open and honest conversations about suicide and suicidal behaviour. Starting these important conversations at local, national and international levels assists in raising awareness and promoting a culture of support and understanding around suicide.

A new Alternative Respite Centre for children, offering a unique and innovative support service for young people and their families living in the Dublin South and Wicklow healthcare area, was opened by Taoiseach Simon Harris recently.
Designed for those with an Individual Family Service Plan, developed by the Children’s Disability Network Team (CDNT), Sánas provides additional social and developmental supports to help children achieve their identified goals. The centre operates a daily after-school respite service from Monday to Friday during term time. In addition, the centre provides two sessions a day on Saturdays, Sundays and Bank Holidays throughout the year.
The new centre is based in Wicklow town within walking distance of local amenities, shops and parks. The fully accessible 4,000 sq ft space is modern, bright and spacious. Each room has been designed with services users and activities in mind. There is also a multisensory room along with kitchen and dining facilities.
Sandra Keogh, Director of Alternative Respite, Sánas, explained that the service is centred around five core values: Supportive, Alternative, Nurturing, Active and Social.
“The ethos of our service is to support individuals to achieve their goals and dreams through creative thinking, fostering growth, offering person-centred activities and facilitating social interactions and community engagements. Children can engage in group activities, one-to-one sessions or play with their siblings and friends. We are close to local amenities in the local community such as the bowling alley, soft play centres and playgrounds,” she said.
Children can be referred to this service through their CDNT. Please contact your child’s CDNT to find out more.


Staff from Dublin South and Wicklow Healthcare Area promoting the 2024 Staff Engagement Initiative.
Sánas CEO James Magrane with Sánas staff, Taoiseach Simon Harris; Martina Queally, REO HSE Dublin and South East; and Patricia McEvoy, Head of Service Disabilities at the official opening of the Sánas Alternative Respite Centre in Wicklow.
Grace Chan (pictured left receiving the award) and the Antimicrobial Stewardship team at University Hospital Waterford (UHW) have won the Antimicrobial Resistance Competition at the NPSO Conference for their SE AMS initiative. Well done to Meadhbh Collison, Susan Lapthorme, Joseph Healy, Anna May Whelan, Maeve Doyle and Grace on their hard work and for bringing such well-deserved recognition to the hospital.
The Staff Engagement Initiative (SEI) returned this year to support the health and wellbeing needs of staff from the Dublin South and Wicklow health area. A total of 61 applications were approved across the health area.
21 of the applications approved were for walking groups, with each group receiving up to five Fitbits plus three months of fruit delivery. Eight applications were approved for Minding Your Wellbeing Programme training with fruit delivery and care packs on the day. 32 applications were approved for Staff Health and Wellbeing groups with fruit delivery and seed funding for events.
In all, close to 1,000 staff members from across the area will benefit from the SEI initiative this year.

ED have great fun at Knock-Me-Down
The dedicated staff from the Emergency Department and Medical Assessment Unit of Tipperary University Hospital (Tipp UH) came together to tackle the Knock-Me-Down Challenge, showcasing their remarkable fitness and teamwork through cycling, running and kayaking.
The team, consisting of Helen, Catherine, Paul, Niamh, Theresa, and Sarah, represented a diverse array of roles, including nurses, occupational therapists, physiotherapists and healthcare attendants.
The day was filled with camaraderie and fun, with everyone earning well-deserved medals. Special thanks to Healthy Ireland and Time for Design for sponsoring and printing the t-shirts and caps, proudly displaying the Tipp UH logo and highlighting the unity of the ED team.
Congratulations and well done to all involved.
The Eastern Region Traveller Health Unit (ER THU) held the launch of their Traveller Health Action Plan (THAP) recently. Regional Traveller health action plans have been developed across the country to support the implementation of the wider National Traveller Health Action Plan (NTHAP), which was launched in 2022.
The Eastern Region Traveller Health Action Plan aims to create a health service in which all Travellers can achieve wellbeing and where the wellbeing of all Travellers is supported at every level.
The Tipp UH team who took part in the challenge.
Members of the newly formed Leopardstown Walk and Talk group enjoying the sunshine and fresh air.
The Traveller Health Action Plan is launched.

A new Leopardstown Walk and Talk programme launched in September, a collaboration between HSE Health Promotion, Leopardstown Primary Care and Making Connections, a local befriending and wellbeing charity.
This follows the success of the programme in Churchtown which has demonstrated improvements for participants in physical activity levels, muscle strength and wellbeing through socialisation.
Senior Health Promotion and Improvement Officer Shane Lee, from the project team, presented findings from the programme at HEPA Europe, the European Network for the Promotion of Health-Enhancing Physical Activity’s (HEPA) annual conference which was held in Dublin this summer.

The ER THU is the largest and longest-established unit in Ireland covering more than one quarter of the Traveller population in Ireland. It is committed to strengthening partnerships between the HSE, the Traveller Health Unit, local Traveller organisations and Traveller primary health care projects.
A lot of work has been going on to increase the number of Health and Social Care Professionals (HSCP) entering the Irish health service now and into the future.
The National Health and Social Care Professions Office (NHSCPO) established four working groups in 2023. These groups were set up to bring HSCP working in healthcare services and those working in education together, in an effort to provide more essential practice placements for HSCP students.
Eoghan Fitzsimons, Physiotherapy Manager, Mater Hospital, Dublin, explained the benefits of practice education. His department takes over 100 students each year from UCD across all stages of their programme, supported by two tutors.
“It’s a very competitive environment for recruitment, so it’s important for students to experience what it's like to work in the hospital and have a very positive student experience. Then they will consider applying to join the department on graduation,” he said.

Eoghan Fitzsimons
to other areas, helping the department and patients in assisting caseload management, all the time ensuring that the students are getting something positive out of it and that it is a positive learning experience for them,” he said.
“They are a real help when you're running a busy service and even just having just a second pair of skilled hands to help you with rehabilitation. It's really, really important.”
For staff, it’s clear that there are professional development benefits from teaching students. It gives them experience with managing people, for example, and develops their organisation skills.
Eoghan was keen to stress the importance of engaging with the students. He meets them at the end of all the placements to discuss their experience and seek feedback, including if they would consider coming back to work.
“We need to look beyond next year and the year after. We need to look into the future. If you can offer a really good student placement, a supportive environment, a nice team, they will come back.”
“We ran two big panels over the last two years, and a high percentage of the staff grades that have started here have all had placements here and said that's one of the reasons that they wanted to work here. We like to see that they feel they are welcome and part of the team. And that there's lots of learning opportunities for them.”
Eoghan has observed that, within a few weeks of placement, the majority of students are up and running carrying caseloads. In his department, there is a focus on encouraging students in each of the areas to support or run some of the classes, such as classes in the pool, balance class, outpatient classes, and get involved in the pulmonary rehab class. This enables students to develop their organisational skills.
“It releases physiotherapy and physiotherapy assistant time
“You can make space work if you integrate your students into your team, like having lunch with the students, allowing students to come to meetings, allowing students to be there in the morning.
When you're organising, you can integrate students into your department. Obviously it has to be what suits the team, but equally it is important that students feel part of the department. The students don't want to feel like they're extra,” he said.
“The support of the university is very important and the Mater has an excellent relationship with UCD. The benefit of being in a large teaching hospital is that there are lots of different learning opportunities.” These include department meetings, hospital learning opportunities such as grand rounds, study days and in-service training, and spending time with other professionals, he noted.
Eoghan said he feels HSCP have a responsibility as professionals to offer something back and teaching is part of the role. Changing the culture around practice placements for HSCP who are not currently taking students can bring many benefits to HSCP, HSCP managers and to students.
“When you go in with an open mind, and you show an interest, the scientists are fantastic. They know so much and if you show them that you're interested, they have a plethora of knowledge they are very eager to teach."
Sarah Keating, final year Medical Science student, Technological University Dublin, talks about her experience on practice placement.
I found my placement really important as, from an academic point of view, it consolidated a lot of those kind of intangible concepts. I found going into the lab and actually seeing the machinery there and understanding how it functions was brilliant. We also had the opportunity to learn about open disclosure and auditing, things that again are hard to digest in college, which was really useful. I found placement really just put everything into context.

When you go in with an open mind, and you show an interest, the scientists are fantastic. They know so much and if you show them that you're interested, they have a plethora of knowledge they are very eager to teach. I think something that I struggled with at the start is learning where to place myself in a new environment when you don't know anyone. You can feel like an imposter. But once you settle down, after you get through your first
rotations, you understand how it works and where you're needed. The key learning I took from my placement was a deeper understanding of the purpose of a medical scientist. It gave me a lot of purpose, especially coming back for fourth year. It's a really nice reminder that what I'm going into as a job is something that's quite important to people, it's going to hopefully positively impact patients and their care.
your next career move

Make sure you don’t miss out! Register now at careerhub.hse.ie

The Career Hub has made it so much easier to avoid missing out on the next promotion opportunity or chance to expand your career in the HSE. Simply register your details on the website and get an email alert whenever a job vacancy relevant to you is posted.
It is just over a year since the dedicated HSE careers website went live. In that time, over 36,000 people have signed up for job notifications.
When you register, you will be given the option to choose from a variety of job disciplines and locations to be alerted about, doing all the job-hunting work for you. You may be actively looking for a change of role or simply waiting for that perfect opportunity to arise. Either way, the Career Hub alerts will keep you up to date with the HSE jobs market.
It also features candidate support materials which help you complete your job application form and prepare for an interview.
The Career Hub has information to help overseas healthcare
“Its aim is to attract people to careers in the health service by providing information on entry requirements, training and development opportunities, as well as the pathways available for career progression.”
workers to move to Ireland. This includes eligibility for visa and work permits, professional registration, an overview of the Irish health system and the financial assistance available to help with relocation costs.
The website is constantly expanding its content base and career pathways are currently being developed on the site. Its aim is to attract people to careers in the health service by providing information on entry requirements, training and development opportunities, as well as the pathways available for career progression.
Another recent addition is the health regions section giving an

overview of services and opportunities in each of the six health regions in the country.
The Spotlight Service on the Career Hub, meanwhile, promotes a difference discipline or service every few weeks, coordinating with national recruitment drives in those areas. They provide an invaluable insight for potential staff on the type of work the service provides as well as testimonials from current staff.
There are plans to have a Spotlight Service within each of the health regions pages, addressing some services that might have a particular staffing need in that region.
Staff came together to celebrate and promote the work that is done to support open, honest and compassionate conversations between staff and people who use our services during Open Disclosure Themed Week.
Open disclosure leads and trainers in services across the country delivered a fantastic variety of engagement activities to promote the week.
Performing this role in addition to their full-time job, these colleagues were nonetheless ambitious and creative in their approach to developing activities. These included information and promotional stands in public areas and visiting services to ensure that all staff can learn more about Open Disclosure, take away resources and discuss any questions they might have.
In addition to this, there was an opportunity to promote and support staff with the implementation of the requirements of the Patient Safety (Notifiable Incident and Open Disclosure) Act 2023. The act commenced on 26th September, just days before Open Disclosure
Themed Week began, so the timing was perfect for supporting staff in gaining a better understanding of how this new legislation would impact their work and care.
The Patient Safety Act seeks to strengthen openness and transparency throughout the public and private Irish health care system. It aims to do this through the introduction of a legal duty to disclose key information about a specified list of incidents called 'notifiable incidents' when they are identified as having occurred in a health service.
This new act requires health services providers to be open and transparent with patients, their families, or both, depending on the patient's choice, when a notifiable incident happens while the patient is receiving care.
The act outlines a clear process for open disclosure, ensuring that patients, their families, or both, receive truthful and timely information in any health or social care setting when a notifiable incident happens.

Helen Thompson, QPS Manager, and Siobhan Carrigan, QPS Advisor, at O'Casey Rooms, Fairview Community Unit.
It is essential for the delivery of safe, highquality healthcare that we nurture a culture of openness and trust when an incident occurs. The introduction of this act builds on the HSE Open Disclosure Policy and the successes of the Open Disclosure Programme and its aim is to deliver a person-centred approach to incident management and communication.
To support services to implement the act, online resources are available. These are:
1. Patient Safety (Notifiable Incidents and Open Disclosure) Act 2023 (bit.ly/ PatientSafetyAct2023) and
2. Resources for staff and organisations (bit.ly/ OpenDisclosureResources). There is also a module on HSeLand that offers an overview and guidance of the act. This can be found by searching the catalogue for ‘Patient Safety Act’ on HSeLanD.
For more information, contact opendisclosure.office@hse.ie or scan qr code:
HSE SOUTH
REGIONAL EXECUTIVE OFFICER
The
first few months have been very enjoyable and exciting in getting out and about to listen to the communities and staff in Kerry and Cork. I’ve had a very warm welcome and have been struck by the commitment to improving the health outcomes for the people we’re privileged to serve. I’ve visited around half of the 300-plus locations where we provide care across Cork and Kerry. In a busy and complex role, meeting frontline staff helps me to remain focused on delivering what’s important.

My main role is to set the culture of the organisation, centred around the people of Cork and Kerry being proud of their health service. We’ve worked together to make eight commitments based on the core HSE values. We are holding ourselves to account by delivering on those commitments, such as valuing patient’s time.
"I want HSE South West as the best employer in the state and the people of Cork and Kerry to be the healthiest in the world."
One of our Integr8 projects is providing Urgent Virtual Care for people through virtual consultation instead of visiting the Emergency Department. We have started to take a Healthcare Systems Engineering approach to the design and delivery of care, an approach which will deliver improved outcomes for staff and patients using the same resources.
The overall aim is for our services to be safe and calm. Despite an increase in ED presentations of 12% and an increase in admissions of 19%, the hard work done across community and hospital services has seen the number of people waiting on trolleys drop very considerably. Similarly, we’ve seen a 19% increase in outpatient referrals but will see a significant reduction in numbers of people waiting as well as a reduction of average waiting times to around seven months.
My priorities will always be balancing service quality (and in particular, improving access), getting the best value from every euro spent, ensuring staff have the best experience of work, ensuring our communities are the healthiest they can be, ensuring equitable health outcomes and reducing our impact on climate.
I am looking forward to March when we will fully stand up HSE South West into a single integrated health region with three health areas. I want HSE South West as the best employer in the state and the people of Cork and Kerry to be the healthiest in the world.
Through transforming our hospital and community services, we will continue to deliver improved outcomes, with shorter waiting times for appointments, diagnostic tests and treatments, particularly cancer, and better access to acute and emergency care. We will have the Regional Executive Management Team in place with key deliverables and behaviours defined by our Integr8 commitments that our staff and patients will hold us accountable for.
A message to staff
Thank you, thank you, thank you all. This year has been very challenging, not least in the uncertainty caused by the changes to the organisational structure. We can look forward to 2025 where we’ll have an effective organisational structure in place. We will be working together to make sure that the whole system feels safe and calm. Happy holidays. Please take some time with families and friends to celebrate the year, refresh and look forward to continuing to make a tremendous difference to the lives of our communities next year.

A Kerry man climbed the highest mountain in each of the four provinces in just three days to raise funds for Ballyphehane Day Care Centre in his grandfather’s memory.
Mark Tynan did the Four Peak Challenge in July –climbing Lugnaquilla in Co Wicklow, Slieve Donard in Co Armagh, Mweelrea in Co Mayo and Carrauntohill in Co Kerry. He took on the challenge to raise money to help fund services in the Day Care Centre that his grandfather, William ‘Billy’ Tynan attended. He ended up raising over €7,000 for his efforts.
He said that he did it for dementia care as Billy had dementia and the care he received in Ballyphehane Day Care Centre was ‘outstanding’. His grandmother still attends services at the centre but Billy has since passed.
The day care centre provides a home-from-home environment with a multidisciplinary team promoting independence, and to trying keep clients out of the hospital setting.
“These services are really important and kindness always wins,” said Mark. “I wanted to do it to raise funds to provide music and entertainment for clients in the day care centre because music is medicine.”

Two family fun days, two wellbeing festivals and one conference –it’s been a busy time for the Connecting for Life team in Cork and Kerry.

Roisín O'Neill from Mitchelstown at the event.
Almost 10,000 people turned out for two family fun days hosted by the Connecting for Life (CFL) team and other community partners, in Mallow and Midleton.
Together at the Castle and Together at the Lodge aim to foster a sense of community and raise awareness about the available support services for mental health and wellbeing.
These free community events, now in their third year in Mallow and second year in Midleton, stand as a testament to the ongoing commitment of Cork Kerry Community Healthcare – in partnership with local businesses, Cork County Council, See Change, Shine, Cork ETB and local Gardaí - in promoting these aims.
The events featured an extensive array of entertainment, recreational activities, workshops and information spaces; provided by up to 50 local and regional community groups and organisations. Cork's C103FM was also on board with a media partnership and Red Patrollers on the day.
The CFL team also joined forces with community partners for Together at the Hall, a mental health and wellbeing community event in Dunmanway, West Cork.
As part of the month-long West Cork Feel Good Festival, Together at the Hall featured entertainment, recreational activities and information stands provided by local community groups and organisations.
The team then moved to The Kingdom, where they were heavily involved in the 2024 Kerry Mental Health and Wellbeing Fest, which raises awareness of the available supports and services in the county.
An aim of the Fest is that there is something for everyone – runs, walks, arts and crafts, indoor bowls, coffee mornings, movie nights, workplace wellbeing, parenting information, mindfulness, volunteering, information sessions, wellbeing workshops and much more. The Fest has continued to grow, with over 130 free events county-wide this year.

A memorial to those who lost their lives during the pandemic has been unveiled in HSE Bandon Day Care Centre by Bandon native, TV presenter and author Graham Norton.
Graham joined older people from the day care centre and local Transition Year students at the Allin Institute in the town to unveil the large waterside plaque they created.
Entitled ‘Light to Dark – Womb to Light, Every Spring Rebirths’, the intergenerational monument was created as part of the Creative Bandon 'Making Meaning of COVID' project.
Made from Kilkenny stone, the tablet holds clay tiles created by the participants depicting daily rituals, habits and friends that helped them through the pandemic.
Among those in attendance was Bridie O’Mahony, aged 96, from Bandon, who attends the day care group on Tuesdays.
“COVID-19 was difficult. I live on my own, and it was a lonely time,” she said. “But this project was lovely. The teenagers came along, and we joined in, and it was great.”
Noreen Walsh, the clinical nurse manager of the HSE Bandon Day Care Centre, said the project really helped people return to normal life.
“Everything closed down. And it was difficult to support our clients because we just closed down and we were gone for a year and a half,” she said.
“I was redeployed five times. But we had great volunteers and every month we divided up the areas, and we would do a drop, like flowers, a card, or teabags, just to let them know that ‘we were still here’ and we would wave at them through their windows.
“And when they came back, they said ‘thank you’ for keeping the connection.”

The Centre for Mental Health Care and Recovery (CMHCR) is an acute admissions unit located at Bantry General Hospital. Re-opened after recent upgrades were completed to the facility, the CMHCR offers assessment and acute admission facilities for people in the West Cork area.
The building upgrades include enhanced measures to improve the quality and safety of patient experience, as well as aiding staff in delivering the highest possible standard of care.
The aim of Mental Health Services is to provide excellent care that promotes the well-being and recovery of those facing mental health challenges; while maintaining strong connections with community and voluntary agencies, in promoting a recovery-focused approach.
Continuous improvements in facilities and services reflect the ongoing commitment from the service and staff to provide high-quality, safe care for all who access the service.

Ophthalmology services in Cork and Kerry have been centralised with the official opening of a new unit at the South Infirmary Victoria University Hospital (SIVUH) by Tánaiste Michéal Martin.
While the surgical element of Ophthalmology has been operating at SIVUH for some time, the outpatient element has now transferred from Cork University Hospital and all patients are cared for in a purpose-built facility in Cork city centre. The unit expects to treat up to 45,000 patients per year.
The new rooms in the Centre for Mental Health Care and Recovery following its renovation.
The new Ophthalmology building represents a 90% increase in clinical rooms. It will host outpatient and emergency care services, in addition to two new operating theatres and a day unit. It includes two laser rooms, eight consulting rooms, a corneal topography room, a pre-admission assessment suite and a medical retina room; along with a new electrophysiology room – a service which patients previously had to travel to Dublin for.
At the opening of the new Ophthalmology unit at the South Infirmary Victoria University Hospital were Aldine Denny, CNM 1 Ophthalmology; Mary O'Mahony, ANP, Ophthalmology; Eamonn O’Connell, Consultant Ophthalmic Surgeon; Helen Donovan, CEO, SIVUH; Minister Colm Burke; Sean Kearns, Director, Reddy Architecture; Tánaiste Micheál Martin; Cormac Smith, Associate Director, Clancy Construction; Dr Nora Mohd, Consultant Medical Ophthalmologist; Pádraig O’Sullivan TD and Gillian Keating, Board Chair, SIVUH.
Ophthalmology patients in the Cork and Kerry region have experienced long waiting times, due to increasing patient numbers as a result of diseases of the ageing eye, such as cataracts and glaucoma. The development of innovative new treatments has also led to an increase in demand for services.
The increased theatre capacity will initially focus on long-waiting cataract patients, thus reducing the considerable waiting list.
As part of the transfer of services, the Ophthalmology (Eye) Service Ballincollig Primary Care Centre opened in August 2023. This state-of-the-art facility has six consulting rooms, five imaging rooms, a laser room and two injection rooms. Following the transfer of Ophthalmology services, the Ophthalmology Service in Ballincollig Primary Care Centre will also come under the governance of the South Infirmary Victoria University Hospital.


The HSE Youth Health Service (YHS) celebrated 20 years of providing sexual health support, services, education and information to young people across Cork; with all services provided free of charge.
The YHS started as a pilot service back in 2004 and has supported over 11,000 young people since, providing approximately 88,000 appointments and sessions to young people over the past 20 years. It is the only service of its kind in Ireland.
There are a wide range of free dedicated services under one roof at Penrose House in Cork city, to meet the needs of young people in the area of sexual health, including:
• general advice and support in relation to sexual health
• STI screening/clinic
• contraceptive clinic
• unplanned pregnancy counselling
• pregnancy testing, information and support
• post-termination medical checks and counselling
• one-to-one youth work support for sexual health education and information
• drug and alcohol support and counselling
• sexual health-related counselling
Youth Health Service Manager Geraldine Gannon said, “We are a non-judgemental, informal, friendly and supportive service for young people with a team of professionals who are extremely dedicated and committed. We are very proud to be celebrating 20 years supporting young people with their sexual health needs.”

Liam Doocey, Youth Development
Officer YHS, Dr. Andy Phillips, Regional Executive
Officer of HSE South West and Sharon O'Sullivan, Health Promotion Manager HSE
Service user presentations with self-harming behaviours are increasing. Life can be stressful and many factors can contribute to this stress. The Self Harm Department Clinical Nurse Specialists (CNS) in the Emergency Department (ED) of University Hospital Kerry (UHK) have developed SOS toolkits to help individuals to self-soothe and distract themselves from engaging in such behaviours.
Sharon O'Sullivan, Health Promotion Manager HSE and original YHS committee member; Cliona Hatano and Noreen Hosford, both YHS staff; Dr Andy Phillips, Regional Executive
Officer of HSE South West; Eleanor Moore, Principal Community Worker Cork Kerry Community Healthcare HSE; and Frank Horgan, YHS staff.
Photo: Jim Coughlan.
This toolkit is a free educational resource and a coping mechanism for people. A pilot project began March 2024 with funding from the Kerry Mental Health Association. Service users using the SOS tool kit are giving positive feedback.
“Distraction can help self soothe from distressing thoughts and behaviours. It is helpful to have a resource easily accessible for individuals to use. We work closely with individuals with self-harming behaviours in ED and decided to develop and offer individuals such a resource,” explained Eleanor Fitzgerald, Mental Health CNS. She developed the toolkit with her colleague and fellow mental health CNS Gerard Sheehan.
“We thought providing service users with an easily accessible resource to help them cope with distressing thoughts, which may lead to self-harming behaviours, may be beneficial. We developed the SOS toolkit to assist them in reducing self-harming thoughts and behaviours. In turn, these kits would help reduce the frequency of attendance to the Self Harm Department in the ED
So far, the frequency of service users revisiting the Self Harm Department with self-harming behaviours has reduced.
The Youth Health Service can be contacted on 021-493 7250, email yhs@hse.ie or see mysexualhealth.ie/youth-health-services for information.

Staff from 16 different countries celebrated their diverse cultures across a number of Older Persons residential settings in Cork and Kerry.
Events took place at Fermoy Community Hospital, Cois Abhainn, Youghal Community Hospital, Clonakilty Community Hospital and Killarney Community Hospital, as well as at Cork city-based Farranlea and Heather House Community Nursing Units.
These events celebrated the cultural diversity of staff members through their national cuisine, costume, dance and even a flower carpet.
Great efforts were made in representing the 16 different nationalities, with flags unfurled on building facades to the delight of staff, residents and the local community.
Killarney Community Hospital invited staff to create a series of posters to represent their countries. These were great fun to make and will have a lasting impact as they hang on walls around the building.

Fermoy Community Hospital
staff: Midhun Baby, Sajeev Thareparambil, Anuja Rose Joseph, ADON Lisa Harrington, Meenukutty Joseph, Joma Jacob, DON Marie Hayes, Pooja Zacharias and Minu Rose Ken, CNMI.
Cois Abhainn
staff: Binish Benny, Evleen Rani, Souyma James, Rosemy Joe, Jasmine Augustine and Rebecca Amosu.
Staff members from 11 countries working at Fermoy Community Hospital hosted a Cultural Diversity Day, with demonstrations of dancing, costumes and make-up, samples of Indian food, an Indian cookery demonstration, and a display of floral artwork prepared by staff at the hospital entrance.
Flags and decorative art prepared by hospital residents in their activity groups were also displayed on the walls.
Marie Hayes, Director of Nursing at Fermoy Community Hospital, said, “This is a wonderful opportunity to celebrate the rich cultures of our colleagues and to enjoy their customs in their home from home. Sharing these traditions amongst our staff and residents builds mutual understanding and respect.”
Gabrielle O’Keeffe, Head of Health and Wellbeing with Cork Kerry Community Healthcare, said, “This initiative is a wonderful example of how staff can support each other in engaging and creative ways,” she said.
This initiative was funded through the 2024 RENEW Arts Project: Celebrating Culture Diversity through the Arts for Staff Health and Wellbeing.
This creative project is one of many being delivered through the Cork Kerry Community Healthcare Health Promotion and Improvement Department Healthy Ireland Arts and Culture Portfolio.


This year the HSE National Office for Suicide Prevention (NOSP) introduced Let’s Talk About Suicide, a new and innovative online suicide prevention training programme, available to everyone. The free programme, which takes 90 minutes to complete, aims to provide people with the tools and confidence needed to have open conversations about suicide and provide support to those in need.
The programme focuses on helping participants recognise signs that someone may be thinking about suicide, engaging with the person in a compassionate, non-judgmental way, and connecting them with appropriate resources and services for further help. Additionally, the















training emphasises the importance of self-care after having these difficult conversations.
Let’s Talk About Suicide is designed for a wide audience, including members of the public, healthcare workers, community leaders and educators. The goal is to make suicide prevention accessible and to foster a culture where talking about mental health is normalised.
Participants will learn to engage confidently in these critical conversations, supporting the message that asking about suicide can be life-saving.
The programme encourages individuals to take the first step in addressing suicide risk and promoting mental health awareness. By starting open dialogues, participants can break down the stigma surrounding suicide and create a supportive community.
To further promote Let’s Talk About Suicide, a national paid campaign is under way. It features advertisements across Irish radio stations and on social media,

with community voices including HSE resource officers for suicide prevention and local training advocates.
Since September, the programme has also been available on HSeLanD making it easily accessible for HSE staff and healthcare workers.
The HSE NOSP is calling on all its employees to enrol and complete the training. This programme is an important step in reducing the incidence of suicide and improving mental health support across all our communities.

To enrol and complete Let’s Talk About Suicide, search for the programme on HSeLanD or visit hse.ie/letstalk
For more information on HSE suicide and self-harm prevention training programmes, visit nosp.ie/training or email training@nosp.ie
















One third of all referrals to the HSE’s primary care counselling service is related to bereavement, new figures have revealed.
The National Counselling Service’s (NCS) Counselling in Primary Care (CiPC) and the Irish Hospice Foundation (IHF) recently collaborated on a successful training initiative in delivering bereavement support.
The HSE’s NCS is a professional, confidential counselling and psychotherapy service available free of charge in all regions of the country. It was established in 2000 to provide counselling to those who experienced childhood abuse.
In 2013, the NCS expanded to provide the CiPC, which counsels adult patients experiencing mild to moderate psychological difficulties who present in the primary care
setting. Currently, all adults in receipt of a medical card are eligible for the service.
CiPC is available in each of the six health regions and provides up to eight counselling sessions with a professionally qualified counsellor or therapist.
It is generally accepted that 90% of mental health needs can successfully be addressed in primary care settings. CiPC provides a person-centred, high-quality service in the community.
For GPs, CiPC offers an alternative to medication for people presenting with mild to moderate mental health difficulties. While depression and anxiety constitute the main reasons for referral to CIPC, bereavement issues constitute almost a third of referrals (31%). Competency in working with bereavement is a key
“It is generally accepted that 90% of mental health needs can successfully be addressed in primary care settings. CiPC provides a person-centred, high-quality service in the community.”








requirement for CiPC counsellors. IHF are the national leader in the development of bereavement care and developed a bespoke training programme for CiPC counsellors. 201 NCS counsellor/therapists have completed both days of the programme, representing almost 70% (68%) of all NCS counsellors. The training initiative was developed by Orla Keegan, Director of Bereavement and Education, and Catherine Tierney, Bereavement Clinical Manager, IHF and psychotherapist, with the support of Philip Dodd, Clinical Advisor National Office Suicide Prevention, and Oliver Skehan from the National Office for Suicide Prevention. Training was delivered by Catherine Tierney and Dr Anne Dodd, psychotherapist. This training ensures staff have a level of competency in grief and bereavement practice. This means that when NCS counsellors work with bereaved clients, they will be using the most up-to-date evidencebased practice and approaches, helping clients receive an effective and supportive service.



Hubs are being developed to reduce number of people waiting for non-complex, high-volume day case care and reduce length of time people are waiting
Background
The first surgical hub in Ireland was established in the Reeves Centre at Tallaght University Hospital and since opening in December 2020 there has been a reduction in both the total number of patients waiting for a day case procedure and the length of time patients are waiting.
Building upon this success, the Government approved six additional HSE Surgical Hubs which will be located in South Dublin, North Dublin, Galway, Cork, Waterford and Limerick.
The surgical hubs are being developed under the governance of Model 4 hospitals to expand capacity for planned day case surgery and minor procedures.
What is a surgical hub?
The HSE Surgical Hubs will be developed on a standard building design with two operating theatres and two minor procedure rooms, as
“The hubs will open from 8am to 8pm, 6 days per week. Patients will come in, have their procedure, recover and go home on the same day.”
well as areas where patients will recover after their procedures.
The hubs will open from 8am to 8pm, 6 days per week. Patients will come in, have their procedure, recover and go home on the same day.
The hubs will provide a wide range of day case specialties including general surgery, dermatology, gynaecology, ophthalmology, ENT and orthopaedics and will care for patients who require non-complex procedures which are in high demand for example varicose veins, hernia repair and other keyhole surgery.
The hubs will be in separate buildings with dedicated resources protected for patients requiring these procedures.
Once fully operational each hub will be able to deliver an additional 10,000 operations or minor surgical procedures and roughly 18,500 additional outpatient appointments per year.
Separating emergency and non-emergency care
Reducing waiting lists and waiting times for patients is a key priority for the HSE.
One reason that waiting lists are growing is the ever-increasing pressure on hospital emergency departments which can result in non-urgent procedures being postponed.
There is significant international evidence to




support the separation of emergency and non-emergency care for improving services for all patients. It can lead to fewer cancellations and fewer delays for people who are waiting for procedures.
By moving many day case procedures to the surgical hubs, hospitals around the country will have greater capacity for patients who require emergency and more complex care.
In addition, by reducing the length of time that people are waiting for their procedures this can help prevent their condition from getting worse and this will lead to better health outcomes and improved quality of life for those individuals and for their families.
As part of the Sláintecare vision for the future of healthcare in Ireland, in December 2021 the Government committed to establishing new standalone national elective hospitals in Cork, Dublin and Galway.
“The new elective hospitals will result in significant additional capacity and will enable the delivery of highquality and timely planned care to meet the known demographic changes up to 2035, which anticipates up to a 40% increase in day case surgeries.”
The new elective hospitals will result in significant additional capacity and will enable the delivery of high-quality and timely planned care to meet the known demographic changes up to 2035, which anticipates up to a 40% increase in day case surgeries.
The additional capacity which will be provided by the overall Elective Hospitals Programme, in terms of procedures, treatments, and diagnostics, is estimated to be 977,700 annually.
The elective hospitals planning phase is underway and an integrated design team and a project control team will progress the detailed design and pre-tender business cases for the proposed sites in Cork (St Stephen's Hospital, Sarsfield Court) and Galway (Merlin Park University Hospital). The preferred sites for the development of new elective hospitals in Dublin are Connolly Hospital, Blanchardstown and the current Children’s Hospital site, Crumlin.
In the shorter term, the six HSE Surgical Hubs are being developed to reduce the number of people waiting for non-complex, high-volume day case care and to reduce the length of time that people are waiting, in line with the Sláintecare waiting list targets.
EXECUTIVE OFFICER
It’s fast approaching the end of my first year as REO in the Mid West. Over the last 12 months I have witnessed firsthand the impact staff have on the lives of people who live and work in our region and I’m incredibly proud to be part of this team.
The year has been an extremely busy one as I’ve spent time getting to know the region, the people and the service. I’ve received a warm welcome from everyone I’ve met and I have learned so much from speaking with people who deliver our services as well as hearing what our patients and service users have to say. I’m aware that staff are very ambitious for the region and I am committed to doing everything I can to help realise that ambition. We have an awful lot to be proud of but I’m aware that some of the great work that we do can at times be overshadowed by our capacity and service demand challenges. However, we have seen unprecedented levels of funding in the Mid West which has enabled us to make some very quick decisions around addressing bed capacity challenges in the short and medium term. Since September we opened 70 sub-acute beds in Ennis and Nenagh enabling us to transfer patients from UHL to a more appropriate care environment. We will open 16 new acute beds in UHL in December and that will very quickly be followed by 96 new beds in mid 2025. In addition construction has already started on the second 96 bed block which will be completed in 2027.

"I'm aware that staff are very ambitious for the region and I'm committed to doing everything I can to help realise that ambition. ”
Establishing the new Regional Leadership Team was a significant milestone and enables us to establish the framework to begin to implement reforms and drive change throughout the region. I’m committed to collaborating with staff to do this and will continue to engage throughout this change process.
Addressing health inequalities is one of the main issues
we face as I begin my second year as REO. Our region has two of the highest areas of deprivation in the country and as a result there is a significant need for health services. Nearly a quarter of our population is socially deprived. We must understand the implications of this for our region, for service delivery, for demand and above all for outcomes. I will be working closely with our public health and community services colleagues to create a multi-agency, public health-led strategy to address health disparities for these populations.
No doubt there are challenges ahead but I’m confident that working together, using our local expertise and knowledge we can deliver a health service of which we can all be proud.
Staff at University Maternity Hospital Limerick (UMHL) helped to forge a distinctively intimate bond between 30 newborns and their mums and families during what has become an annual ‘read-a-thon’ event in the hospital’s neonatal department.
The third annual UMHL Neonatal Read-a-thon ran in September, building on the success of previous events thanks to the support within the hospital community, as well as among leading figureheads and outlets in books and reading in Limerick city and county.
Led by Vivienne Fitzgibbon, Neonatal Discharge Coordinator/ Clinical Midwifery Manager 2, and Mairead Fitzgerald, Clinical Specialist Speech and Language Therapist, Neonatal ICU, UMHL, the event is modelled on the international ‘Baby With Books’ Read-a-thon project.
The practice, which aligns with the UMHL ethos of family-centred care in the neonatal department and across the hospital community, has many emotional and practical benefits for parents.
Mairead discussed the feedback of one parent who participated.
“This mum was telling me that when you come in to a neonatal unit

as a parent, the first thing you notice is all the wires and equipment and the busy activity, and it can make you feel very emotional and overwhelmed.
"When you’re with your baby in that environment, and you want to communicate with them, you might not be able to think of the words, and this very simple activity, of holding your baby close and reading a book to them is very relaxing and comforting for both parents and babies.”
Vivienne added, “A big part of our work is about supporting parents
Clare All-Ireland Hurling champions recently visited some of their proudest and most passionate fans at St Joseph’s Hospital, Ennis. The Banner boys were met with tears of joy in each of the five units of the hospital, as residents congratulated them on their victory against the Rebel County in this year’s All-Ireland clash. One resident, Nora Griffin from Kilmihil, aged 104, held the Liam MacCarthy Cup while player Eamonn Foudy remarked that the cup itself was only 101 years old! Sisters Philomena McCarthy and Mai Keating, and husband and wife Michael and Monica O'Loughlin were also photographed with the cup, congratulating players Cian Broderick and Eamonn Foudy and kitman and staff member Liam Devitt.
and promoting bonding with the child – reading to a baby in the neonatal context is a positive, normal activity in what you might call the ‘abnormal’ world of the ICU.”
Externally, the initiative is supported by Limerick City Library (Brenda Frawley) and the county libraries in Dooradoyle (Ciara Barry) and Kilmallock (Carmel Elliott); by Limerick book stores O’Mahony’s and Quay Books, and by Genius Juniors, an online children’s book shop that provides an option to purchase a book of your choice for a child in Children’s Hospital Ireland.

Regina Jordan, Director of Nursing, said, “We were thrilled to welcome our All-Ireland champion hurlers into St Joseph’s Hospital. It meant the world to many of our residents to meet and congratulate the lads and we thank them for all the excitement they’ve provided us this season. It was a day we won’t stop talking about or celebrating for a long time. Thank you so much on behalf of myself, the staff and our residents to the lads and the County Board for making the visit possible.”

Students from across the Mid West gathered alongside Minister Patrick O’Donovan at Gaelcholáiste Luimnigh in Limerick to launch the 2024 Junior Health Sciences Academy Early Careers event, which took place online in early October.
The minister raised the curtain on a diverse line-up of speakers and activity, aiming to inspire second level students through a varied programme with an insightful edge, informed by the experience of clinical staff, academics and students from the frontline of healthcare in hospital, community and third level education in the region.
Targeting Transition Year, Fifth Year and Leaving Certificate students interested in careers in healthcare, the annual online event
is organised by the Health Sciences Academy based at University Hospital Limerick, along with Limerick and Clare Education and Training Board (LCETB) and Limerick Education Support Centre.
Clinical staff representing more than 20 healthcare professions participated, as well as academic staff and students from health programmes at University of Limerick (UL). For the first time, students from the Technological University of the Shannon (TUS) shared their experiences and provided insights into the health programmes on offer at TUS.
Miriam McCarthy, Health Sciences Academy Manager, said, “Our aim is to support students interested in healthcare careers by providing the opportunity to hear
from clinical staff working in hospital and community healthcare settings across the Mid West, and from students at UL and, for the first time, TUS. From previous years, we know that students find this really helpful in making informed choices.”
Donncha Ó Treasaigh, Acting Chief Executive, LCETB, said, “We are delighted to support the launch of www.healthcareers.ie.
This innovative platform will play a key role in attracting and nurturing the next generation of healthcare professionals across Limerick and Clare.
"With our region's growing healthcare sector, it is crucial that we inspire the next generation to consider the vast array of rewarding careers available.”
A team of specialist physiotherapists from University Hospital Limerick (UHL) has been recognised for significantly reducing the incidence of clinical lymphoedema in cancer patients in the Mid West.
Sinead Cobbe and Kathy Nugent are at the heart of the lymphoedema early detection service, which has been honoured at the Hospital Professional Awards 2024 by winning the MSD Excellence in Oncology Award.

Lymphoedema is a swelling that can occur in the arm, hand or torso after cancer treatments including surgery, radiotherapy and chemotherapy. These treatments can compromise the lymphatic system and lead to a build-up of lymph fluid which causes pain, skin changes and reduced function. This can be very distressing and adversely affect quality of life.
Since the establishment of the UHL service in 2021, initially with the support of the Irish Cancer Society, the evidence has shown that patients can significantly reduce their risk of developing lymphoedema through prompt assessment, patient education and ongoing monitoring.
Senior physiotherapists
Sinead Cobbe and Kathy Nugent from the lymphoedema early detection service with Shirley Real, Allied Health Lead, Acute Hospitals, HSE Mid West.
Fertility investigations and treatments are available to public patients for the first time through the development of regional hubs, such as the new Mid West service based at Nenagh Hospital.
Dr Lucia Hartigan, Consultant Obstetrician and Gynaecologist and Clinical Lead for the UL Hospitals Group Regional Fertility Hub, explained how one in six heterosexual couples in Ireland have fertility problems.
“Infertility can be a devastating diagnosis for men and women alike. It can be socially isolating, lead to low self-esteem and have a negative impact on the couple’s relationship. Up until recently, Ireland was one of the few countries in Europe that did not offer any publiclyfunded assisted human reproduction (AHR) treatments like in vitro fertilisation (IVF),” said Dr Hartigan.
“Thankfully, in recent times, the landscape has changed for couples who are challenged with their fertility with the rollout of six fertility hubs nationwide and the provision of public-funding for AHR treatments for eligible couples.”
The regional Fertility Hub services of the UL Hospitals Group launched in September 2023. They provide comprehensive fertility investigations for couples across the Mid West. Assessment and treatment requires
Of almost 450 patients – the majority with a diagnosis of breast cancer – referred to the service between September 2021 and January 2024, the incidence of clinical lymphoedema has reduced from an expected 25% to under 2% through the intervention and support of the UHL team.
“What our work and research has shown is that lymphoedema is not only preventable, but also reversible when it is caught early. Our message to patients who have had lymph node surgery done, or who are otherwise at risk, is to know their risk level. Those at high risk can lead a normal life but do need to add in some maintenance strategies like massage, losing excess body weight and exercise,” said Sinead. Kathy said, “When patients initially come in to see us, they are very worried about what they may have been told or read online about lymphoedema.
"We help them to learn about their risk and hopefully they walk out of our service knowing what they can do about it. We are always available for any patient who goes on to develop symptoms.”
specialised, skilled care by a team of doctors, an andrologist, specialist nurses and clinical specialist radiographer sonographers.
Ultrasound scans, phlebotomy, consultations, outpatient hysteroscopy and HyCosy (test of fallopian tube patency) all take place in the recently-renovated ambulatory gynaecology unit at Nenagh Hospital. Semen analysis is currently performed at Waterstone’s clinic in Limerick, although soon this investigation will also be available in Nenagh hospital. The hub currently receives approximately 60 new referrals per month.
In order to be investigated for infertility, patients must be referred by the female partner’s GP. They must be 42 years or under (women) or 59 or under (men) and have a BMI between 18.5 and 35.
To be eligible for referral for AHR treatments such as IUI (intrauterine insemination), IVF and ICSI (intracytoplasmic sperm injection), the female partner must be aged 41 or under and have a BMI of between 18.5 and 30. Both partners must be non-smokers.
Further information is available at www.hse.ie/fertility

October was Health Literacy Month. Good health literacy means that we, as a healthcare professionals, communicate clearly with our patients and service users. When patients understand what we are telling them, it increases their levels of knowledge, understanding and confidence when navigating our services. In turn, it helps them to play more of an active role in their own health and wellbeing journeys.
HSE Mid West marked Health Literacy Month by sharing a series of plain language tips with staff. They also shared social media graphics highlighting the work under way to make healthcare information more accessible to service users.
Staff also attended a ‘Health Literacy Lunch and Learn’ event,
where Health Literacy Officer Catríona Kiely and guest speaker, NALA Literacy Ambassador Michael Power, spoke about using Plain English in a clinical setting and what we can do to support services users with unmet literacy needs.
The event took place in the Clinical Education and Research Centre at University Hospital Limerick, and was also livestreamed to allow staff from across the region to join and engage with the speakers.
HSE Mid West hopes to create an environment across all our sites where our patients and service users feel comfortable to ask questions about their care, and have all the information they need at their disposal. Plain language is such a powerful tool in keeping our patients and service users healthy and safe.
38% of people have taken the wrong dose of medication at least once 33% of people only sometimes ask their GP or a healthcare professional to explain something they do not understand 42% of people cite embarrassment as the main reason for not asking for further explanation


A new free online resource is highlighting the numerous benefits of occupational therapy for people working to improve their mental health and wellbeing through a focus on the everyday activities that bring meaning and purpose to life.
‘Introducing Occupational Therapy for Mental Health Recovery’ is an informative, interactive resource devised collaboratively by Mid West ARIES (Advancing Recovery in Ireland) and the HSE Mid West Mental Health Occupational Therapy Service.
The new guide is the first of its kind in the country, deftly deploying a range of IT tools to raise awareness of how Occupational Therapy (OT) works, including video testimonials, interactive quizzes and live online links to community-based support services, all easily accessible on a laptop, PC or smartphone.
This guide is free and available at https:// tinyurl.com/OT-Introduction
“This is a unique online education resource,” explained Mike O’Neill, manager, Mid West ARIES. “It fulfils all aspects of our mission to identify gaps in people’s knowledge of mental health services and supports, and to deliver innovative solutions that tangibly make a difference to people’s lives. It's enhancing access for
Áine Frawley, OT, Limerick; and Eithne Kennedy, OT Manager, Limerick and North Tipperary Adult Mental Health Service, the new guide is a great enabler for people attending mental health services, and for their families and loved ones.
Mike O’Neill, Manager, Mid West ARIES with Margaret Keane, Education, Training and Development Officer.
people to get the support they need as conveniently as possible.”
The ‘Myth Busting’ section of the resource, engagingly gamifies the educational process through a simple True/False quiz. That then shows the user, for example, that OT is not ‘talk therapy’ or counselling, but a practical therapy focused on the activities a person does in their everyday lives; or that it is not what you seek when you are sick at work (that’s Occupational Health). Incorrect responses to the questions prompt you to have another go, before delivering the correct answer.
Video is also used to show people how OT works from the perspective of the service user and the practitioner.
Eithne Kennedy, OT Manager, Limerick and North Tipperary Adult Mental Health Service, described the guide as “a great enabler” for anyone attending mental health services, and for their families and loved ones.
“By understanding what a profession can offer, people are empowered to request the kind of input they think will be of benefit. Many people who have informally fed back on our services have said that if they’d known previously what OT was, they would have requested it much earlier in their recovery," she said.
Sheena Cadoo and team in North Cork with the ASI information unit and Kevin Quaid and Charlie Drake, who are both living with dementia.

The Dementia: Understand Together campaign are delighted to share some wonderful initiatives that HSE teams have been working on alongside the community and voluntary sector to support people living with dementia and their families.
In Wexford, the NoBrainers group for people with young onset dementia was formed through collaboration between the HSE and The Alzheimer Society of Ireland, who are part of the Wexford Dementia Alliance. The NoBrainers, aged between 58 and 65, came together in January 2024. Emer Finn, an occupational therapist (OT) at the Wexford Memory Technology Resource Room, and Sally Veale, a social worker from the Memory Assessment Support Service, have been involved in setting up and supporting this innovative group. Activities included taking part in an arts programme through Wexford County Council, with their work featuring in the ‘NoBrainers Exhibition’ at Wexford Arts Centre recently.
In North Cork, Sheena Cadoo, OT at the Memory Technology Resource Room, and Margaret McEntee, Dementia Services Co-ordinator, have been delivering information and advice about dementia to people across the community. They were joined by Kevin Quaid and Charlie Drake, who are both living with dementia, and Amy Murphy, the Dementia Advisor covering North Cork. The team have encouraged numerous businesses and individuals to get involved and support their communities to become dementia inclusive.
In our last edition of Health Matters, we shared how Jennifer Manning, Clinical Nurse Manager from the Community Hospital of the Assumption, and the team in Tipperary have been helping to create an awareness raising video for dementia and inclusive communities.
The video features the Thurles Memory Cafe and Marguerite Keating, who is living with young onset Alzheimer's. You can watch the video via the QR code.
The campaign is always looking for opportunities to share projects that will improve the lives of people with dementia. Please sign up to receive our updates at understandtogether.ie/get-involved or email the campaign team at understandtogether@hse.ie









































A new study has found a strong link between using pornography and sexual behaviour and wellbeing among young adults.
The HSE Sexual Health Programme commissioned the Economic and Social Research Institute's Prof Emer Smyth and Prof Anne Nolan to better understand young adults' use of pornography in Ireland. Over 4,500 young people aged 20 years, who participate in the Growing Up in Ireland (GUI) study, were the focus of this research study. GUI is a powerful survey in that it captures information on children and their families at points throughout their development.
Often considered a taboo subject, this is the first study that collects data on young people's pornography use and examines its links to young people's sexual health.
The study found, firstly, pornography users were significantly less likely to use condoms every time they had sex compared to those not using pornography. Pornography frequently portrays sexual encounters without the use of


“This study comes at an important time in our understanding of young people's sexual health. There were significant increases in 2023 compared with 2022 in sexually transmitted infections and rates have continued to increase through 2024."
condoms, and therefore young people may perceive this as common and normative.
Secondly, users of pornography had poorer wellbeing, particularly amongst young men. The authors suggest this might be explained by anxiety about body image and sexual performance, increases in relationship dysfunction and greater isolation and lower self-esteem.
64% of young men and 13% of young women reported use of pornography. Men from more advantaged backgrounds were more likely to report using pornography, but amongst women, use didn't vary by social background. Pornography use was not influenced by migration status, having a disability, or being brought up in a rural or urban area. However having a religious affiliation
or where there was greater parental monitoring in adolescence were linked to lower porn use. Having received sex education at school made no difference in relation to young adults' use of pornography. This research was commissioned by the HSE Sexual Health Programme in late 2022. The pornography report is the first of three reports on young people's sexual health. This study comes at an important time in our understanding of young people's sexual health. There were significant increases in 2023 compared with 2022 in sexually transmitted infections (STIs) and rates have continued to increase through 2024, a trend observed across the EU. The overall STI rate in young people aged 15-24 years increased by 38% compared to 2022.
Evolution of exciting roles within the Public Health Nursing service and community nursing teams present an opportunity to make a difference.
The Public Health Nursing service aims to deliver safe, quality and person-centred community nursing care and is committed to promoting health and wellbeing, and enabling people to live healthy and fulfilled lives.
The aim of Sláintecare is to help people maintain their health in their homes and communities by expanding primary and community care services available to them.
Skilled nursing teams provide care in their communities while empowering patients to manage their health and promote independence, which aims to reduce hospital admissions and facilitate earlier discharges.
The Public Health Nursing service and the Community Nursing team offers holistic nursing care in various settings, reflecting Sláintecare's goal of shifting from hospital-based to community-based care. This has created significant career development opportunities in community nursing.
Acknowledging that there are a number of nursing teams working in the community, here we are focusing on Community Nursing teams within the Public Health Nursing service.
The nursing grades in the Public Health Nursing Service include:
• Public Health Nurse (PHN)
• Student Public Health Nurse
• Staff Nurse General Community
• Clinical Nurse Specialist (CNS)
• Candidate Clinical Nurse Specialist (cCNS)
• Advanced Nurse Practitioner (ANP)
• Candidate Advanced Nurse Practitioner (cANP)
• Clinical Nurse Manager 1 (CNM1) and Clinical Nurse Manager 2 (CNM2)
• Assistant Director of Public Health Nursing (ADPHN)
• Director of Public Health Nursing (DPHN)
Gemma Donegan, Clodagh Brackett, Aine Walton

We spoke to a cross-section of nurses working in the community from around the country to discover the difference they are making to patients and to our health service.
Aine Walton
Aine Walton is a registered general nurse working in the community based in Urlingford, Co Kilkenny. It’s a 25-minute drive from her home and Aine really appreciates the work/life balance the role gives her and the opportunity to see family and friends regularly.
Aine started her nursing career in St Luke’s Hospital in Kilkenny and worked for three and a half years, mainly caring for older people. During this time, she collaborated closely with public health nurses, physiotherapists, continence advisors, home support workers and occupational therapists.
“People don’t realise how much goes on in the community. We are linking in all the time with other professionals suchas general practitioners, public health nurses, dieticians and speech and language therapists for example. They may not be in the same building but they are part of the team. We are helping people stay at home in their own environments by providing continuous care."
Clodagh Brackett
Clodagh Brackett, Student Public Health Nurse, is based in Blackrock in Cork city and is attending UCC. Clodagh joined the
Don’t miss out
Find out more about the PHN Sponsorship Programme at bit.ly/PHNsCRGNs
If you would like to work in one of our community nursing teams based all over the country keep an eye out for opportunities by regularly visiting our careers page at hse.ie/jobs
To ensure that you are informed of all vacancies please register at careerhub.hse.ie for weekly job alerts.
If you are living abroad and would like to learn more about the HSE you will find information about living in Ireland here at careerhub.hse.ie

Student PHN Sponsorship Postgraduate programme in September and is due to complete the course in June 2025.
Clodagh gained experience of working in both the hospital environment and in the community while completing a Graduate Nurse Rotation Programme.
“When I complete the PHN course, I’m hoping to work in South Lee, close to where I grew up. There’s a great variety of work in the community and you get lots of support from PHNs and from RGN colleagues who are always willing to help. I enjoy the autonomy in the job. You have your own caseload and there is continuity of care for the patients.”
Gemma Donegan
Gemma Donegan is a public health nurse working in the Primary Care Centre in Shannon, Co Clare. Prior to becoming a public health nurse, Gemma worked for four years as a midwife and for three years as a general nurse.
“Becoming a public health nurse was always on my radar. When I was completing my undergraduate studies, I spent two weeks on community placement. I got to shadow a PHN and it was inspiring to see how she was integral to her local community. She knew her community and her caseload and was self-motivated and driven," she said.
“I wanted that for myself. Now that I am working as a public health nurse, I find the staff I work with really supportive. There is always someone to connect with and my manager is really accessible”
Gemma said there is a huge variety in her workdays, from assisting new parents during the postnatal period to caring for patients on their end-of-life journey and everything in between.
“It’s very dynamic who you are seeing and where you are seeing them. Every day is a new challenge. There’s variety in what you do but it’s not overwhelming. There is great job satisfaction. You are helping people to achieve a better quality of life and you are not just looking after the patient but their family as well. You are very much at the centre, bringing everyone together.”
HSE DUBLIN AND NORTH EAST REGIONAL EXECUTIVE OFFICER
As we approach the end of this year, I want to reflect on our journey over the last eight months since I took up my role of Regional Executive Officer in HSE Dublin and North East.
We have seen significant change as we move to the health regions and the integrated healthcare areas (IHA) structure. We now have three of our four IHA Managers in place and most of our regional management team. The move to the interim structure which came into place on 1st October will give us time to implement the new structures for the entire region. These interim structures will allow the integration of hospital and community services across our region and will see all our services work much more closely.
The vision to provide integrated care is not just a reorganisation, it’s a shift in how we serve our patients and the people who need our services, and how we support one another.

I understand that this transformation means change, and with it, challenges. Staff may have concerns about how they will be impacted by the changes. I want to reassure you all that while we implement these changes, your day to day engagement with patients remains the priority. For most staff, the only significant change might be a change in the person to whom you report. Your roles and responsibilities will not change. This new structure will also open a new chapter where we are more connected, aligned and equipped to deliver improved
health outcomes for the people of Dublin and North East.
Since I came into this role, I have had the privilege to meet many of you to understand your perspectives, hear your ideas and learn about the experiences that make our health community so strong. These conversations have been invaluable to me as I familiarise myself with the people and services in the region. I am committed to continuing this dialogue with you.
As we head in to 2025, I invite you to stay engaged with this process. Share your insights, bring forward your questions, and continue to support each other through these changes. This is a time for us to work together, to deliver integrated care.
“Since I came into this role, I have had the privilege to meet many of you to understand your perspectives, hear your ideas and learn about the experiences that make our health community so strong. These conversations have been invaluable to me as I familiarise myself with the people and services in the region.”
Thank you for your hard work, your commitment to our patients, and your resilience throughout this year of transition. I am deeply grateful to each of you and look forward to all that we will accomplish in 2025.

Dolores Donegan and Catriona McCahey were honoured to represent the menopause champions of Our Lady of Lourdes Hospital at the Menopause Workplace Excellence Awards recently.
The Menopause Workplace Excellence Awards are organised by Menopause Hub Academy and Great Place to Work and were held at Dublin’s Royal College of Physicians in October.
The HSE Menopause Policy which was launched in 2024 provides a blueprint for organisations to create HSE work environments that are supportive of staff going through the menopause. Our Lady of Lourdes Hospital in Drogheda have taken this a step further and selected 20 menopause champions across the various departments of the hospital. The menopause champions are working across the hospital to support their colleagues.
Dolores Donegan, Programme Manager, said, “Feedback from the menopause champion programme has been excellent. We have run many menopause programmes over the years but this has been the most effective, it is giving staff permission to support one another by having a person knowledgeable on menopause close by, to listen and support staff through this difficult transformation.”

The paediatric department in Cavan General Hospital officially launched its new Cubbie sensory pod recently.
The Cubbie was purchased in 2024 with monies fundraised by various individuals and groups and donated to The Friends of The Children’s Ward.
The Cubbie uses Personalised Sensory Regulation (PSR) to effectively regulate people with autism and sensory needs. It offers an easy to use, immersive, safe personal space of sound and vision to help support the sensory needs of users.
Dolores Donegan and Catriona McCahey representing Our Lady of Lourdes Hospital Menopause Champions at the Menopause Workplace Excellence Awards 2024.
The Cubbie also helps manage stress and anxiety and can be used to help with mindfulness and prevent overload. Therefore it can be used by all children attending the Paediatric Services in Cavan General Hospital and may also be used by parents and staff as needed.
Triona Boylan and Noeleen Smith from Cavan General Hospital's Paediatric Department.
Traditional sensory rooms do not offer the adaptability or ever changing sensory experiences delivered by the Cubbie. The children themselves can select from a huge variance of programmes to suit their current feelings. To help energise when under-stimulated and to calm when over-stimulated, matching each individuals needs every time.
The Paediatric Department would like to take this opportunity to thank all their fundraisers who contributed to this investment. It will benefit many children and families for years to come.

Beautiful Esme entered the world at Our Lady of Lourdes Hospital recently, the 100th baby to be born in one of the hospital’s birthing pools since water births resumed there in May 2023.
Midwives and local women celebrated the return of water births as a birthing option last year. Previously the birthing pools were allowed during labour but not for births.
The Drogheda hospital became the third hospital to re-introduce the option, along with the Coombe and Wexford.
Fiona Molony, CMM2, manager of the hospital’s Midwifery Led Unit (MLU), said, “The introduction of a water birth service at Our Lady of Lourdes Maternity Unit marks a significant advancement in maternity care, driven by a midwifeled initiative to re-establish a service discontinued in 2006.”
Over the course of a year, the team sat down with women to see what they wanted.
“The desire of women for the return of water births drove this project. This initiative underlines the therapeutic benefits of water
“I just trusted my body and when I felt I needed to push, I pushed. Within three pushes, Esme was born. Her cord stayed connected to her for about 20 minutes after birth. I then stayed
in the pool for about an hour afterwards doing skin-toskin with Esme. The experience from start to finish was amazing.”
during the birthing journey such as pain relief, relaxation, and increased satisfaction, offering another calming option for childbirth,” she said.
Amy Murtagh was delighted to give birth to the 100th baby in the Lourdes birthing pool since the resumption, although she didn’t originally plan to give birth in the water.
"As my labour progressed, my midwife asked if I wanted to get into the water to help ease the contractions. Within two and a half hours, Esme was born right there in the pool," she said.
Amy had her second son in July 2023 with an epidural but suffered badly from the side effects and was extremely sick, having to stay in hospital for three days separated from the baby. It made her determined to have a natural birth when she became pregnant with her third child.
“The water birth experience was amazing, I am so happy I gave birth to Esme in the pool. The room was dark and calm. When my contractions started to intensify, I got into the pool with my partner’s and midwife’s help. I rocked on all fours in the pool and took deep breaths for my contractions, I was so calm in the pool I was even falling asleep at 10cm dilated,” she explained.
“There was no checking of how dilated I was, I just trusted my body and when I felt I needed to push, I pushed. Within three pushes, Esme was born. Her cord stayed connected to her for about 20 minutes after birth and then my partner cut it. I then stayed in the pool for about an hour afterwards doing skin-to-skin with Esme. The experience from start to finish was amazing.”
service in the hospital.
“It involved a multidisciplinary approach, incorporating feedback from service users and collaboration across various hospital departments including midwifery, obstetrics, paediatrics, anaesthesics, infection control, clinical engineering, and maintenance,” she said.
Guidelines were put together following a review of what was in place in Wexford General Hospital and the Coombe – the other two units offering water births – as well as by examining international guidelines and research.

Partnerships extended beyond the hospital, engaging with counterparts in Northern Ireland for expertise and clinical experience using the Cooperation and Working together initiative (CAWT).
Staff also went to Royal Jubilee Maternity Hospital in Belfast for training.
Since the service’s relaunch in May 2023, over 100 water births have been successfully conducted, with feedback from both midwives and clients overwhelmingly positive.
The reintroduction of the water birth service at Our Lady of Lourdes Maternity Unit illustrates the power of dedicated teamwork, innovative problem-solving, and the pivotal role of incorporating service user feedback in healthcare delivery.
The initiative not only restored a valued birth option but also set a new standard in maternity care that emphasises woman-centred practices, safety, and satisfaction.
It is available in both the MLU and the consultant-led unit so no mums have to miss out if they want a water birth.
Amy said she would ‘100%’ recommend a water birth to other women.
“The warm water really helps with the pain of the contractions and puts your body and mind at ease. Esme is a very calm baby I am convinced it is from how she was born in the water,” she said.
MLU manager Fiona explained the methodology employed by the team as they examined how they might reintroduce the water birth
The Lourdes midwife team welcomed Katherine Robinson and Hannah McCauley from the Home from Home unit in the South Eastern Trust in Craigavon.
“Katherine is the midwifery manager for the unit and Hannah is a consultant midwife. Both midwives have a huge amount of experience with water births and made a wonderful presentation to our staff, as well as a question and answer session,” said Fiona.
Earlier this year, an accelerated plan for the national roll-out of the Integrated Financial Management System (IFMS) was agreed by the HSE. IFMS is the new single integrated financial management and procurement system for the health sector and is initially being rolled out across the entire statutory sector.
A HSE Dublin and North East Regional IFMS Implementation Team has been established to manage the roll out of the new system which has
Christine McGeough, Assistant Director of Midwifery, said there was a huge interest in the water births.
“People are very interested in learning about water births and many are making the choice to labour in the pool and even give birth in there. Water immersion has a great pain-relieving effect and it leads to a very calm birth,” she said. “There was great excitement waiting for the first baby to be born in the birthing pool. Now we are up past 100.”
a Go-Live date of 1st July 2025. This team will be led by Petula Clarke, Regional PM, together with Simon Hurl from the Systems Integration Partners, IBM, who are supporting the roll out of the new system across the HSE.
Oversight of this strategic project in the Dublin and North East health region sits with an IFMS Regional Working Group, which is chaired by Gráinne Hannon, Regional Director of Finance and includes members of the Dublin and North East Senior Leadership Team and other key stakeholders.

Minister of State for Disabilities Anne Rabbitte cuts the ribbon to officially open Castlewood House, a new children's respite service.

Rainbow Lodge Chidren’s Respite Centre in Urbalkirk, Co Monaghan, and Castlewood House Children’s Respite Centre in Trim, Co Meath have just been opened.
The benefits of a respite break for children, parents and families are well known. Respite services provide an opportunity for parents and families to recharge and attend to other matters in their lives. At the same time, the child with the disability is given an opportunity to engage with other children and to participate in fun activities which increases the child’s well-being, social skills, confidence, and independence.
HIQA. The property includes a studio style apartment with separate entrance and a ground floor bedroom which is wheelchair accessible. There is a further wheelchair accessible bedroom downstairs whilst upstairs the property has a further three bedrooms as well as a relaxation/play room.
Both respite services will operate seven days/nights per week on 360 days of the year and will offer up to 1,800 respite bed nights each year.
“I know the service will provide much needed and very welcome respite breaks for children and their families."
“I know the service will provide much needed and very welcome respite breaks for children and their families,” said Minister for Disabilities, Anne Rabitte.
Having had funding confirmed for the respite development, a procurement process was completed by HSE Disability Services and the Talbot Group was awarded the contract to deliver these children’s respite services in Monaghan and Meath.
The Talbot Group sourced a property for the Monaghan service, approximately 8km from Monaghan town, and then progressed the necessary works to ensure the property was redesigned to the specification agreed with the HSE and to the standards required by
The number of breaks offered to children and their families will vary depending on the assessed needs of each individual child.
Edel Quinn, Head of Service for Disability, HSE Community Services Cavan, Donegal, Leitrim, Monaghan, Sligo, said, “It has been a pleasure to work with the Talbot Group to bring a much needed children’s respite centre to the Monaghan area. Respite care is such an important support to families who are caring for children with additional needs.”
Mary Gorman, Head of Service for Disability, HSE Community Services Louth, Meath, Westmeath, Longford, Laois, Offaly, said, “HSE Disability Services were delighted to be allocated the additional funding required to progress the respite service that will be delivered at Castlewood House.”

Éist is a HSE-funded training programme developed by HSE speech and language therapists (SLTs) in Meath and Wexford, and people with communication difficulties/differences.
The goal of Éist is to raise awareness of communication difficulties/ differences and help businesses to understand the simple ways they can make it possible for “everyone to order a cup of coffee”.
People with experience of communication difficulties/differences are central to this programme and take the role of Éist Partners. They deliver the training alongside HSE SLTs. The training is free for participating cafés.
The first training session was in Leon’s café in Navan, Co Meath recently. It was attended by café owner Leon, café staff, Éist partners and spouses, HSE Meath Primary Care SLTs, and the HSE Meath SLT Manager.
The evening was a great success. The highlight was hearing the stories of people who experience difficulties when communicating. The main take home message was that “the simplest of things can make a huge difference”.
The National integrated Staff Records and Pay (NiSRP) programme team are working closely with colleagues in HSE Dublin and North East and continue to hold engagement and information sessions with management and staff.
NiSRP Project Leads are in place and play a crucial role in both collecting local information and processes along with communicating any change impact on staff. A key focus in recent weeks was on the first phase of testing.
All staff in Louth, Meath, Cavan and Monaghan will receive access to HR and Payroll Self Service. This Self Service system is an online tool that allows all staff to view payslips, update certain personnel information, apply for leave, submit travel and expense claims and view various reports. Managers can review and approve leave requests, travel and expense claims along with access to a team calendar and reports.
Programme Director, Ivan McConkey, said, “The team have already had positive engagement with staff and management in the region. I am confident that with continued close collaboration with our colleagues in HSE Dublin and North East, SAP HR and Payroll will be successfully implemented in 2025.”

The daughter of a Dublin woman who attends a new HSE centre for chronic disease in the Phoenix Park, has praised the clinic, saying: “They gave me back my mam.”
Cuan Aoibheann is HSEintegrated, with patients referred to the care centre by their GP, where they receive tests and meet with a consultant and their team.
It’s the first centre to offer a respiratory/cardiology clinic, which provides a unified approach to managing cardiopulmonary disorders.
COPD patient Beatrice Lyons, from Dublin 15, attended Cuan Aoibheann after she contracted a serious respiratory infection.
“Last November, I contracted an SRV. I ended up in Connolly hospital for two weeks, unable to breathe.
"After I came home, I just got worse. My daughter Samantha called the COPD nurse, and she quickly made an appointment at Cuan Aoibheann and from there, everything began to get better.
“It’s a wonderful place, because you get to know the people there and they get to know you. You meet the same nurse, the same doctor, the same everything, every time, instead of in a hospital, it can be anyone.
“They all know my name. I know their names, and they don’t have to go through everything with you, because they've already done that. There’s less stress on the patient."
The Health Service Executive Annual Report 2023 serves as both an instrument of accountability and provides insights into the workings of the HSE. The report also provides detailed financial information about our organisation through the Annual Financial Statements.
In his review, the Chief Executive Officer highlighted, “Structural change is not the main goal of this reform. We are doing this to ensure that people experience just one health service, which provides whatever care they need at the right time and in the right place.
“While we continue to face significant challenges, there have been many achievements in 2023. While more patients have come on waiting lists as anticipated, we also took far more people off than we had targeted to do. By the end of the year, we reduced the volume of the waiting lists by approximately 2.7%, and the average length of wait was brought down to seven and a half months.”
In 2023, we made significant progress on change and reform in the health service.
Restructuring the HSE into six operational regions is a key enabler for the wider introduction of universal healthcare and Sláintecare to deliver services that are:
• integrated, locally planned and delivered
• easier to access and navigate for patients and their families
• available closer to patients’ home when they need them
– right care, right place, right time.






We continued to see a reduction in waiting lists for scheduled and unscheduled care, despite increased presentations, by implementing the Waiting List Action Plan. The Urgent and Emergency Care Plan saw a reduction on the numbers of people on trolleys (down 8% on 2022 and down 22% during the second half of the year) despite unscheduled care presentations increasing from 1.25 million to 1.69 million, an increase of 35%, since 2017.
The Annual Report and Financial Statements 2023 is available at: bit.ly/HSEAnnualReport2023

• It is estimated 5.3 million people live in Ireland; this is an increase of over 97,000 people in 12 months
• There were 54,493 births in 2023
• The most recent estimate of life expectancy in Ireland is 80.5 years for males and 84.3 years for females
• According to the Healthy Ireland Survey 2023, 86% of the population said that their quality of life is good or very good, with just 5% of the population saying that their quality of life is poor or very poor


• 3.65 million new and return outpatient attendances - this is 7% above 2022 activity and 8% above 2023 target
• 1.36 million new ED attendances – this is in line with 2022 activity and 1% above 2023 target
• 1.7% of surgical re-admissions to the same hospital within 30 days of discharge – this is in line with 2022 performance and 15% above 2023 target
• 86.6% of people waiting <15 months for first access to Outpatients Department Services
• 95.9% of all attendees at ED who are in ED < 24 hours
The HSE was allocated a budget of €21.6bn for 2023, an increase of approximately €1bn on the previous year. The capital budget allocated to the HSE in 2023 was €1,157m of which €140m was reserved specifically for ICT projects.
• 1.61 million persons covered by medical cards as of 31st December – this is 3% above 2022 activity and 1% below 2023 target
• 95,962 total Community Intervention Teams referrals – this is 14.5% above 2022 activity and 18% above 2023 target
• 45,424 day-only respite sessions accessed by people with a disability – this is 60% above 2022 activity and 86% above 2023 target
• 89.4% of children aged 24 months received measles, mumps, rubella (MMR) vaccine –in line with 2022 performance but 6% below 2023 target
• 3.54 million home support hours delivered to persons with a disability, 5% above 2022 activity and 13% above 2023 target
• 92.8% of urgent referrals to Child and Adolescent Mental Health Teams responded to within three working days
In 2023, we expanded our workforce with a further 8,240 WTEs. Medical and dental staff levels increased by 1,064 WTEs, the number of nursing and midwifery staff increased by 2,628 WTEs and the number of health and social care professionals increased by 1,064 WTEs. Meanwhile, the number of staff working in other patient and client care increased by 1,213 WTEs.
The updated HSE National Consent Policy and its new Easy to Read version demonstrate the practical benefits of making information accessible.
In order to bring the Easy to Read Consent Policy document to life, Elaine McCaughley, Programme Lead, approached St Michael’s House to try to find out what service users thought of the Easy to Read resource, whether it was useful to them, and to hear their thoughts on consent in health and social care.
Róisín O’Neill, Quality and Risk Manager, St Michael’s House, said the invitation to support the launch of the Easy to Read Consent policy was very welcome.
“Supporting individuals with intellectual disabilities to explore a topic such as consent, and decisionmaking can be a daunting task for many staff. All too often the lack of available resources or accessible material can impact on getting the conversation started,” she said.
“Within St Michael's House, we often find that we are constantly trying to adapt and develop information into a format that makes sense to the people we support.
“Past experience had been that when policies are updated, despite having a real impact on the lives of those we support, there were no accessible format or resources available. As a service, we work to

develop resources that will support individuals to understand the concepts and to begin discussions about what this might look like in their life.”
They arranged a peer-to-peer workshop in July, where a group of five individuals, supported by staff, met weekly to consider the Easy to Read Consent Policy and explore ways that the document could be used to strengthen understanding about consent and decision-making.
“Having a policy in an easy read format is one piece of the puzzle, a useful one that we can refer to on a regular basis to start conversations and influence practice as we uphold the rights of those supported across this disability service,” Roisin added.

The updated HSE National Consent Policy 2022 and the Easy to Read document of the Policy are available on www.hse.ie/nationalconsentpolicy
The HSE National Office for Human Rights and Equality Policy hosted an event recently to celebrate the end of Year 1 of the HSE Assisted Decision Making (ADM) Mentorship programme.
Mentors and mentees, along with guest speakers, focused on Year 1 of the programme coming to a close and highlighted key learning and insights from participants.
The ADM Mentorship programme was launched in September 2023 to assist staff in effectively implementing changes mandated by the 2015 Act over a 12-month mentorship process. This programme was launched with over 500 participants organised into 45 mentorship sets. Sets included staff from the HSE, Section 38 and 39 organisations, and spanned acute hospitals and community sectors across Ireland.
The ADM mentorship programme aims to:
• build confidence and competence at a local level
• provide targeted support and resources to healthcare workers
• help solve common issues arising in practice
• develop a mechanism for escalation of issues which cannot be resolved at a local level
• capture and record solutions and case studies
Information and data will be used for future training and to address broader systems issues that may arise.
Speaking at the event, Caoimhe Gleeson, General Manager from the HSE National Office for Human Rights and Equality Policy, told the mentees, “You have told us that the ADM mentorship programme enhanced your knowledge, skills and competence and gave you a safe space to talk through your issues and concerns about how to uphold a person’s human rights in difficult and complex circumstances.”
Amanda Casey is the first Chief Social Worker for the HSE. She is an experienced social worker with a strong interest in promoting human rights across all health and social care services.

One of the Chief Social Worker’s main priorities will be to transform how we safeguard adults at risk of harm or abuse.
This includes:
• reducing harm
• promoting and protecting the rights of the people we care for
• empowering them to make choices
• considering the person and their family first when harm does occur
As staff members, we can safeguard those who use our services by:
• knowing what abuse and harm looks like
• knowing what to do if we have concerns
• getting training and support to manage concerns and complex situations
Protecting adults at risk is everyone’s responsibility, but it should be led by social workers with expertise in managing and reducing risk across a person’s life. Amanda will be contacting important stakeholders to progress this work.
The creation of this role demonstrates our commitment to person-centred, rights-based health and social care in Ireland. It will provide a strong organisational structure to support consistent adult safeguarding across our health regions.
If you want additional information on the HSE ADM Mentorship Programme, please contact adm.mentorship@hse.ie
Find out more about safeguarding vulnerable adults at bit.ly/SafeguardingVulnerableAdults
The Adult Safeguarding in Ireland review is our roadmap for this change. Access it here bit.ly/AdultSafeguardingInIreland
HSE
WEST AND NORTH WEST REGIONAL EXECUTIVE OFFICER
Over the past number of months, significant work has been undertaken across the country and regionally in setting up the new structures.
1st October was a really an important date for us as we stood down the existing CHO structures and the existing hospital group structures and the Regional Health Area Management Teams took over responsibility for the delivery of public health services in those geographies.
But it's important to bear in mind that these are just milestones and it's a journey that we're still on and will be for some time. There is still a lot of work to do in order to fully realise and develop the regions.

“The delivery of networks of care that stretch across our whole region is a priority for me. These are clinical structures that will be very important both in terms of knitting our region together and achieving a greater level of integration across our region."
While we now have significant autonomy and the ability to make decisions that are directly relevant to our own population, we are also cognisant of the fact that decisions that we take within our region can have implications across the whole country. So we work and co-operate closely with the other regions as part of the national HSE as well.
While we have made good progress in rolling out our structures, we must now focus on further embedding the structures that support the delivery of care.
The delivery of networks of care that stretch across our whole region is a priority for me. These are clinical structures that will be very important both in terms of knitting our region together and achieving a greater level of integration across our region. They are crucial in terms of the quality of the care that we provide and in terms of patient safety.
Instilling the importance of ownership of our health services is another priority and we will focus on a devolved approach which allows the regional healthcare management team to take ownership of the services. But we must also ensure our structures allow service users to feel ownership of their services.
Over the next couple of months, we will see structures developed within the region that allow us to engage
systematically and in a very functional way with service users to inform our planning and our delivery of care.
It's important that we all remember that while we are making these changes, care continues to be delivered at the highest possible level. It's not enough to be saying to our patients that when we have our new structure sorted, everything will be fine. We must continue to do the best that we can every single day while we're making these changes.
I'm really conscious that we're undertaking these changes at a time when we know that our hospitals and emergency departments are going to become busier, particularly during the months of December and January. Consequently, all of the health services will be focused on ensuring that patients are kept safe. Developing these new structures while we're also keeping an eye on that is really, really important.
One way we can all support our service and our colleagues is keeping up to date with our vaccines. We know that this will make a real difference and I would ask all of you to get your vaccine this winter.

Atlantic Technological University (ATU) and the HSE celebrated National Breastfeeding Week in a unique and impactful way by unveiling a striking new mural on the ATU’s Sligo campus, dedicated to promoting and supporting breastfeeding.
The initiative makes ATU the first higher education institution in Ireland to feature a large-scale exterior mural designed to encourage conversations and raise awareness of the importance of breastfeeding amongst all members of society.
The project team was headed by Fiola Murphy, HSE Child Health Programme Development Officer for Community Healthcare in Cavan, Donegal, Leitrim, Monaghan, and Sligo, along with Margaret McLoone, SFHEA, Programme Chair and Lecturer in Health Promotion at ATU. Their joint effort highlights the mural’s broader mission to serve as a reminder of the significance of breastfeeding and to promote healthier infant-feeding practices throughout the region.
Located on the wall of the Student’s Union building, the mural is the creation of renowned artist Marian Noone, also known as Friz. The mural depicts the artist’s niece being breastfed, a scene inspired by the observation of the tender moments between mother and child in the early days of the baby's life. The design focuses on the baby, and highlights the profound bond established as a mother breastfeeds her baby.

Head of Health and Wellbeing, HSE Community Services Cavan, Donegal, Leitrim, Monaghan, Sligo, Cara O’Neill, speaking at the launch of the breastfeeding mural.
Portiuncula University Hospital (PUH) recently appointed Siobháin Kiernan to the role of Advanced Nurse Practitioner (ANP) in General Paediatric Integrated Care. Speaking about the role, Siobháin said, “The key focus of this particular role was to identify patients with low acuity and common childhood conditions who were on wait lists for conditions that could be easily treated with timely intervention, significantly improving the quality of life for patients and their families.
“Unlike other advanced practice posts in areas of specialties, defining a patient cohort for the general paediatrics was the biggest challenge and after reviewing the most common referrals received to general paediatric outpatients, we defined the patient cohort to include constipation, recurrent abdominal pain in childhood, eczema, asthma, and coeliac disease.”
Siobháin Kiernan with eight-yearold Niamh Carolan from Monksland, Athlone.
The General Paediatric Clinic receives new patient referrals from general practitioners and review referrals from paediatric consultants as well as nursing staff. In addition, an outreach clinic is held once a week in the Primary Care Centre in Monkland, Athlone to integrate treatment into the community and provide patients and their families with care as close to home as possible.

Taoiseach Simon Harris has officially opened a new 50-bedded ward block at Portiuncula University Hospital (PUH). The project is a €35 million capital investment for the hospital site.
This new development delivers inpatient single room accommodation in line with all current, modern-day standards.
The project consists of a two-storey building and is linked to the existing
hospital. The Orchard and Garbally Wards, each comprise of 25 single rooms with ensuite facilities, include two dedicated negative pressure isolation rooms on each floor.
The new development will facilitate the relocation of two existing wards from the main hospital building which are outdated.
The design and layout of the new wards will deliver a patient-centred approach, improve patient
experience and comfort while ensuring privacy and dignity for all patients, particularly for those who are requiring end-of-life care.
Single room accommodation will also reduce patient exposure to possible infections while in hospital. These new wards will improve the patient’s journey, reduce length of stay and reduce the number of in-house patient transfers between wards.
The Palliative Care Week national campaign took place in September. The week provided an opportunity for people to talk to their family and friends about what their understanding of palliative care is.
There are many misconceptions about palliative care, such as it is only about end-of-life care. In reality, palliative care is about supporting and enabling people to live through their life-limiting illness.
Providing palliative care is the responsibility of all healthcare professionals. However, over the course of someone’s illness, they may require referral to the specialist palliative care services, known by many as the hospice service.

The theme of this year’s Palliative Care Week was ‘You, me and Palliative Care’. With this in mind, North West Hospice hosted two information stands at Sligo University Hospital and in the foyer of Markievicz House, where specialist palliative care staff provided information.
Staff at the Palliative Care stand in Markievicz House.

Donegal patient Francis Hegarty became the 50th patient to undergo the Renal Denervation (RDN) procedure at Galway University Hospitals (GUH); a minimally invasive procedure to help treat high blood pressure in patients who have not responded to medications and lifestyle changes.
GUH were the first in the country to carry out the RDN procedure, and the first internationally to offer RDN as a day-case surgery. This means that patients arrive at the hospital in the morning, have their procedure, and then return home the same day.

“Renal denervation is indicated for very high-risk patients with uncontrolled blood pressure or resistant hypertension. First line of treatment is lifestyle changes and adherence to blood pressure medications. If these measures are insufficient to control the blood pressure or the patient has intolerance to blood pressure medications, then RDN may be considered. The treatment is optional and is offered to patients who fit the criteria,” explained Prof Faisal Sharif, Consultant Interventional Cardiologist at GUH and University of Galway.
“Providing this approach as day case procedure has significant benefits for patients in terms of reduced disruption to their lives, recovery at home and we are not dependent on the availability of beds for an overnight stay which can be a challenge with the current demands on inpatient care, added Prof Sharif.
Karen Brennan, who underwent the RND procedure during the initial clinical trial five years ago, said, "This procedure has been a life changer for me; it saved my life. Five years on and I’ve never felt as good. My blood pressure remains normal, and I cannot thank Prof Sharif and his team enough for all they have done for me.”
Karen Brennan from Moylough in Co Galway and Prof Faisal Sharif, Consultant Interventional Cardiologist at GUH and University of Galway. Karen underwent the renal denervation procedure during the initial clinical trial.
Francis Hegarty from Teelin in Co Donegal with Prof Faisal Sharif, Consultant Interventional Cardiologist at GUH and University of Galway.
Falls prevention initiative leads to physical and mental health improvements
A HSE physiotherapy-led, integrated falls prevention initiative was piloted for community-based older adults in north Roscommon and east Galway in November 2023.
This joint initiative was made possible by the collaboration of physiotherapists from North Roscommon and East Galway Primary Care Community, Roscommon/ East Galway Integrated Care of the Older Person (ICPOP) and the Frailty Intervention Team in Roscommon University Hospital (R-FIT).
The programme was six weeks in duration and included balance training and strengthening exercises, as well as demonstrations of how to safely get up from the floor after a fall.
Therese Quinn, Senior Physiotherapist, North Roscommon and East Galway Primary Care Services; Theresa Drury, Senior Physiotherapist in ICPOP; Hazel Cooney, Senior Physiotherapist, R-Fit Frailty Team, Roscommon Hospital and Geraldine Gormley, Physiotherapy Manager, North Roscommon and East Galway Physiotherapy Services.
The overarching aim of the initiative is to promote active and independent living in older adults, and enable their successful ageing within their own communities. Participants thoroughly enjoyed the programme, which saw significant improvements in physical and mental health outcomes. It also provided a welcomed source of connectivity and companionship for older adults in Roscommon. The positive outcome of this initiative is undeniable.


A group of volunteer islanders received Emergency First Responder Certificates and Emergency Services Driving Certificates from the National Ambulance Service (NAS) at a special presentation held at the Community Hall, Árainn/Inis Mór, off the coast of Co Galway, recently.
The group of volunteers, co-ordinated by Rónán Mac Giollapháraic, recently completed the Emergency First Responder (EFR) course and Level One of the Emergency Services Driving Certificate and were presented with their certificates by John Joe McGowan, NAS General Manager Operations – West and Tony Canavan, Regional Executive Officer (REO), HSE West and North West.
The event also marked the delivery of a new ambulance vehicle to the island to replace an older vehicle. The new vehicle was supplied by NAS which has made a significant investment in training and equipping the islanders as part of planning for medical emergencies.
Tony Canavan, REO, HSE West and North West, said, “This is an example of how our health services can achieve progress; when hospital, community and the national ambulance services come together and work with the broader community to provide healthcare at the right time and in the right place.”

John McShane, Community First Responder Officer; Irene Scully, Assistant Staff Officer; Brian Crammer, Training Officer; Johnny Dicker, Head of Service Fleet and Assets; Gabriel Glynn, Operational Support and Resilience Manager; Bridin McGowan, Ambulance Officer; JJ McGowan, General Manager Operations – West; Tony Canavan, REO, HSE West and North West; Christine Boyle, Business Support; and Ivan O’Grady, Training Officer
JJ McGowan, General Manager Operations –West; Rónán Mac Giollapháraic, Árainn accepting the keys to the new vehicle; Tony Canavan, REO, HSE West and North West.
More than eight patients have undergone hip replacement surgery as a day-case procedure in Sligo University Hospital (SUH) over the past three months. This surgery is based on the Direct Anterior Muscle Sparing Minimally Invasive approach and SUH is currently the only public hospital in Ireland providing same day hip replacement using this technique.
This approach for hip replacement surgery was introduced in SUH in June and it carries a multitude of benefits for patients.
Patients experience less pain, have quicker recovery, a shorter hospital stay, less blood loss during surgery and better mobility postoperatively. When compared with traditional hip replacement surgery this new technique results in significantly shorter rehabilitation time, allowing patients to get back on their feet quickly and return to their normal pain free life.
Graham Kelly, Orthopaedic SHO; Joey Coyne, Consultant Anaesthesiologist; Gay Devaney, patient; Ruth McManus, CNM 2 Pre-Admission Clinic; and John Kelly, Consultant Orthopaedic Surgeon.
John Kelly, Consultant Orthopaedic Surgeon in SUH, said, “There are significant benefits for patients with this surgery; they can arrive in the hospital in the morning, have the procedure and are able to return home the same day with a new hip. I’m delighted that we can now offer this as a surgical option to patients in Sligo University Hospital.”


The Frailty Intervention Team Clinic in Roscommon University Hospital is successfully diagnosing Idiopathic Normal Pressure Hydrocephalus (iNPH) via the combination of multidisciplinary team assessment, CT brain imaging and lumbar puncture. Early identification and appropriate onward referral of iNPH has the potential to improve cognition, mood and mobility for service users, with knock-on impact of significantly reducing the care burden for families and carers.
The Frailty Intervention Team is a multidisciplinary team comprising a consultant geriatrician, advanced nurse practitioners, clinical nurse specialist, senior physiotherapist, senior occupational therapist, senior dietitian, and senior speech and language therapist. They assess people over the age of 65 who are living at home and may be falling or living with frailty. It is an outpatient service with access to a geriatrician and rapid diagnostics as needed. People may be referred to this service by their GP or any other member of the multidisciplinary team. The service is free of charge and accessible to a wide catchment area, as there are very few similar models of service available throughout the country.
In one of the team’s cases, a 74-year-old female presented for a Comprehensive Geriatric Assessment (CGA) with a history of three unexplained falls in six months, resulting in two hip fractures. A diagnosis of iNPH was made and a successful lumbar puncture (LP) was performed with onwards referral for Ventriculo-Peritoneal (VP) shunting. She went from a score that was indicative of dementia to one of mild cognitive impairment. It was a very successful outcome, resulting in meaningful improves to her quality of life.

Patients in the west of Ireland are accessing medical care from home as part of a virtual healthcare initiative being rolled out by Galway University Hospitals (GUH) in collaboration with Community Healthcare West.
The Roscommon Frailty Intervention Team with an award they received for their work from the Irish Gerontological Society.
While the patients remain under the care of their treating doctors and medical team this new programme allows them to receive monitoring of their ongoing care from home.
The initiative will also reduce the need for hospital attendance and is expected to save hundreds of bed days per year.
Emma Burke, ANP in Respiratory at GUH and Virtual Care Lead for the Galway City Integrated Care Hub, with Galway patient Frank O'Connell.
The programme’s digital platform is delivered through mobile health apps, which help patients track key health metrics and monitor symptoms from home. A clinician dashboard displays real-time information on a patient’s condition, alerting medical professionals to changes so they can detect deterioration early and deliver timely care.
The programme has had a successful trial in the Galwaybased Chronic Obstructive Pulmonary Disease (COPD) service. Since the introduction of the service in April, 30 episodes of care have been delivered via the pathway, saving just over 205 bed days with the average length of stay in virtual care now at eight days, a 35% improvement on the length of stay compared to the inpatient national average.

A new HSE report shows that more than half of patients assessed by GPs under a new chronic disease programme are at high risk of cardiovascular disease or diabetes, and are now receiving medical intervention.
The first report on the Opportunistic Case Finding (OCF) programme, published at the 2024 ‘HSE Integrated Healthcare: Advancing Health Service Reform’ conference, shows that since its launch in 2022, GPs have assessed nearly 200,000 patients under the programme.
Of these, over 105,000 were found to be at high risk of cardiovascular disease or diabetes, and there were a further 6,000 previously undiagnosed cases of chronic disease.
One in seven of those assessed under the programme (26,000 people) were identified as having undiagnosed chronic kidney disease, almost 2,000 of which were severe cases.
HSE Lead Dr Orlaith O’Reilly said one-third of people with chronic diseases are undiagnosed.
“With one-third of chronic diseases often undiagnosed, early detection is crucial. The OCF programme allows GPs to identify patients at high risk when they visit the surgery for other reasons. These patients are now benefiting from timely intervention and treatment, preventing the disease from progressing or, in some cases, enabling patients to reverse their diabetes,” she said.
You can read the report here: about.hse.ie/publications/opportunistic-case-finding-programme/
Pat Healy, National Director, National Shared Services and Schemes; Dr Sarah O’Brien, National Clinical Group Lead; Bernard Gloster, HSE CEO; Dr Orlaith O’Reilly, HSE Clinical Lead; Minister for Health, Stephen Donnelly; and Dr Shane McKeogh, ICGP/HSE Clinical Lead for Adult Respiratory Disease.
The National Cancer Control Programme (NCCP) has collaborated with the Irish Institute of Pharmacy (IIOP) to develop the IIOP Cancer Care Hub. This is an online information resource hub for pharmacists, which is focused on care of patients with cancer.
The IIOP Cancer Care Hub, which is intended to be a resource for all pharmacists, and one that is hoped will be especially useful to community pharmacists.
We know that the pharmacist’s role, in particular the community pharmacist, is evolving due to increasing numbers of patients on systemic anti-cancer therapy (SACT) who receive their supportive care medicines from their community pharmacist, and also due to the
increased use of oral anti-cancer medicines, which are largely dispensed in the community.
The hub has been designed to be an easily accessible single location where pharmacists can find information resources relating to cancer care.
The content within the IIOP Cancer Care Hub has been organised into six main pillars which reflect the cancer care continuum, from prevention and detection, through to treatment and management of side effects, and then on to palliative care and survivorship. Within each pillar, resources have been organised into three categories:
• Pharmacist information (immediate)
• Pharmacist further education
• Information for patients
The IIOP Cancer Care Hub was officially launched on World Pharmacist Day on 25th September and can be found here: iiop.ie/content/cancer-care-hub
IFMS, the single national Integrated Financial Management and Procurement System for the entire health sector, went live on schedule in July 2023 in the first of three implementation groups. These include HSE East, HSE Corporate and National Services, the Primary Care Reimbursement Service, and Tusla.
IFMS is used by staff involved in ordering or paying for goods and services for the HSE.
IFMS is replacing multiple, non-standard legacy finance systems with one organisation-wide solution and is part of the wider Finance Reform Programme to deliver better value to users of the Irish Health Service. Many of the benefits of IFMS, such as five-day month end close and report, increased procurement compliance, and streamlined invoice processing have been achieved for the first wave of users of IFMS. Additional benefits will be realised when the entire organisation is live on this single national system.
The HSE is developing Community NeuroRehabilitation Teams, to help people after serious neurological illness or injury to improve health outcomes, reduce disability and improve quality of life.
We are recruiting Senior and Clinical Specialists, Health and Social Care Professionals and other roles for Community Neuro-Rehabilitation Teams in HSE Dublin and Midlands, HSE South West, HSE West and North West, HSE Dublin and South East.
Register at www. careerhub.hse.ie to be notified of these jobs.
The roll out of IFMS to all HSE users will be completed in two waves:
· Implementation Group 2 (IG2): HSE Mid West and HSE West and North West, for go live on 1st April 2025
· Implementation Group 3 (IG3): HSE Dublin and Midlands, HSE Dublin and North East, HSE Dublin and South East and HSE South West, for go live on 1st July 2025
A dedicated IFMS Regional Implementation Team for each Health Region is focused on helping those impacted by IFMS to prepare for the changes that it will bring. IG2 users will be trained on IFMS during February and March 2025, with IG3 users trained in May and June 2025.
Please visit the HSE finance staff intranet to see our Frequently Asked Questions.
Find out more at hse.ie/translated-health-info

At the recent HR Summit, Bernard Gloster, HSE CEO, complimented the National integrated Staff Records and Pay (NiSRP) Programme team on their excellent work.
NiSRP is working to extend SAP HR and Payroll to Section 38 Agencies. Having all Section 38 agencies on one system will provide staff with a fully integrated SAP HR and Payroll solution on a digital platform including access to an extensive range of HR, Payroll and Finance reports.
The online HR and Payroll Self Service system also allows staff to view and update their own employee information and perform common HR-related tasks. The range of benefits with the integrated system also provides greater efficiencies, allowing resources to be deployed where they are needed most.
The NiSRP announced an updated certified eLearning course for HR and Payroll Self Service on HSeLanD.
Ivan McConkey, Programme Director NiSRP, explained, “We would encourage all colleagues across the HSE to complete the updated eLearning course for HR and Payroll Self Service on HSeLanD and view recent enhancements to the system and excellent functions that are available to all staff and managers.”
The National Dementia Services have recently launched a number of infographics for staff providing care to people with dementia across all settings. These specifically relate to the appropriate prescribing of psychotropic medications for noncognitive symptoms of dementia. Psychotropic medications are medications capable of affecting the mind, emotions and behaviour through an effect on the chemical makeup of the brain and nervous system.
There are a number of different categories of psychotropic medications including antipsychotics, antidepressants and hypnotics.
You can access these infographics and other relevant resources and information here: bit.ly/NationalClinicalGuideline21
There is clear evidence that shorter waiting times to access post-acute rehabilitation services correlates directly to improved patient outcomes, lessens disability and improves service efficiency.
Projected population growth and longer life spans will result in increased demand for rehabilitation within Ireland.
To date, there has been no clear national picture of the range and scope of existing post-acute inpatient rehabilitation services. A project team was established in 2023, with broad representation from national clinical programmes and oversight from the HSE’s Chief Clinical Officer. The project identified and mapped the scope of post-acute adult inpatient services, funded by the HSE and providing dedicated multidisciplinary rehabilitation.
The report provides a comprehensive overview of the availability and scope of HSE funded post-acute in-patient rehab services, and contains recommendations to support their further development.
This survey identified 43 healthcare facilities providing post-acute inpatient rehab, with a total of 1336 beds identified across a range of acute and community settings.
It provides an in-depth analysis of the availability of beds at a health region level and the criteria for accessing these beds.
This report is available at bit.lyHSERehabilitation

The Making Every Contact Count (MECC) programme is a vital initiative empowering frontline healthcare professionals to engage patients in supportive conversations about lifestyle changes, addressing the prevention and management of chronic disease.
The MECC Training Programme is standardised training for healthcare professionals, aimed at developing brief intervention skills to support lifestyle behaviour change in patients and service users. MECC training is a blended learning course, consisting of eLearning and a follow on ‘Enhancing Your Skills’ workshop. The workshop supports participants to build confidence in developing brief intervention skills and offers the opportunity to learn alongside peers. Delivered by expert trainers, MECC training ensures healthcare professionals are equipped to provide effective brief interventions.
At the heart of MECC is the principle that every healthcare interaction is an opportunity to promote positive health choices with patients and service users. The MECC programme places a strong emphasis on comprehensive and standardised training. One of its key components is the Training for Trainers (T4T) initiative, which equips healthcare professionals with the skills and knowledge to train their colleagues in delivering impactful MECC brief interventions.
A successful T4T event was conducted in September, resulting in 22 new trainers joining the MECC trainer pool. The trainers will go on to deliver the ‘Enhancing Your Skills’ workshop in health regions. The trainers who participated in the T4T event came from a range of health promotion backgrounds, including both community and acute care settings. This diversity in experience is crucial, as it ensures that MECC can be tailored to various patient needs and healthcare environments. These trainers are now an additional resource to support the implementation of MECC in each of the health regions.
It is planned to review and revise the existing MECC blended learning training programme in 2025 to ensure it is up-to-date and fit for purpose for the next phase of implementation.
Injury Units (IUs) offer an important service for patients who have injuries that are neither life-threatening nor limbthreatening such as minor fractures, sprains, and wounds. In 2023 there were over 161,000 attendances at IUs.
In 2024, the Emergency Medicine Programme (EMP) carried out a review of out-of-scope presentations to IUs and identified some challenges and opportunities for these healthcare services. One key finding was that while the inclusion and exclusion criteria are available and clear, there was inconsistency in how out-of-scope presentations are recorded across different IUs. This inconsistency highlights the need for standardisation in data recording, as accurately capturing these occurrences is essential for improving patient safety and care pathways.
Of the 161,000 attendances in 2023, 15,494 were classified as out-of-scope - the patient’s complaint was not appropriate for care in an IU. These cases place an additional strain on IU resources, particularly nursing staff, who are responsible for assessing patients, explaining the criteria, and redirecting them to appropriate services. Despite this, patient feedback indicated high levels of satisfaction with IU services.
Subject matter experts reviewed the out-of-scope cases, finding that three patients initially deemed inappropriate for IUs were actually suitable. This suggests that IU staff apply the criteria very effectively. Ongoing training and support are important to maintain this.
Key recommendations from the audit include standardising the recording of out-of-scope presentations, allocating sufficient nursing resources, and developing clear protocols for handling these cases. Additionally, expanding public education through media campaigns could further reduce inappropriate IU visits, ensuring that patients receive the right care in the right place. As IUs continue to expand, maintaining high standards will be critical to their ongoing success.
Climate Action Week highlights simple
The HSE has partnered with An Taisce for Climate Action Week as part of the HSE Climate Action strategy and focus on priority areas.
Simple actions and behavioural changes that each one of us can make, either individually or collectively, as part of our team or community, were shared over the week. These included buying seasonal or local produce, choosing to reuse, stopping food waste and cycling more.
In the 2023 HSE Your Opinion Counts Survey, 60% of staff respondents indicated an interest in being involved in positive Climate Action activities.
An Tasice runs a Climate Ambassador Programme. HSE staff who wish to become Climate Ambassadors can apply online: climateambassador.ie/apply-climateambassador/
A wildflower meadow sown by staff and service users at St Joseph’s Care Centre Longford (SJCCL) is bringing joy to those who visit it and is a vital boost for local biodiversity.
SJCCL is one of 10 pilot sites in the HSE Capital and Estates Green Space Pilot Project. Through the pilot project, HSE Capital and Estates will develop guidance for healthcare facilities who want to improve their green spaces. In the Dublin and Midlands region, Green Teams meet regularly outline and enact climate action and energy initiatives within the Community Nursing Unit (CNU).
SJCCL’s Green Team planted 460m2 of wildflower seedlings with the staff and service users
on the campus getting involved.

The purpose of the project was to boost biodiversity on the hospital campus, particularly attracting pollinators.
“The planting of large areas of native wildflowers onsite has had a hugely positive impact on the lives of residents, staff, visitors and the local community,” explained Karen Johnston, CNM2, SJCCL.
“These beautiful areas have become a focal point both visually and communicatively for all. Residents are now spending more time outdoors viewing the flowers and hand-picking some for their individual use.”
We are all aware of the slogan ‘reduce, reuse, and recycle’ and National Reuse Month in October focused on spreading awareness of reuse. This means taking products that would otherwise be discarded and using them again, either in their current form or with a few repairs or changes.
To raise awareness among healthcare staff, a special webinar was held, which included speakers on the following topics:
• HSE donating equipment overseas
• HSE aids and appliance cleansing and recycling service
• Bio systems
• Reusable sharps containers for healthcare risk waste in acute hospitals
• UCD’s experience with Warp It, the reuse platform
The webinar was delivered as part of the HSE's Green Healthcare Programme which is funded by HSE Capital and Estates.
We also run regular online training for staff on waste reduction, food waste reduction and water conservation technical training.
Contact sustainable. infrastructure@hse.ie for more information.
New Patient and Public Partnership representatives
The National Screening Service (NSS) has welcomed new Patient and Public Partnership representatives, following an extensive recruitment campaign.
Dympna Cremin, aged 66 from Limerick, was diagnosed with breast cancer following a BreastCheck mammogram in 2021. Having just retired as a Special Educational Needs teacher, she felt that the cancer “initially hijacked her retirement plans”, but thankfully her follow-up treatment has been successful, and she has now joined the Patient and Public Patient Partnership.


Dympna shared her story as part of Breast Cancer Awareness Month as a way of encouraging others to “avail of their opportunity to go for screening”. She will also bring her professional expertise in intellectual disability to “advocate for the use of clear language in health service communications that everyone can understand”.
Dr Frozan Sarwari dedicated much of her career as a gynaecologist in Afghanistan to improving women’s health at community level. Now living in Ireland, Frozan wants to use the chance to promote screening to similar communities here. Her expertise will help encourage people who may not ordinarily attend screening.

Mum-of-two Vicky Doyle is one of the hundreds of women with a diabetes diagnosis who took up the invitation to have additional screening while pregnant, from Diabetic RetinaScreen (DRS).
We screened 432 pregnant women for eye changes caused by diabetic retinopathy in 2023. In the first six months of 2024, 254 women with diabetes had priority eye screening through the initiative – including women who have never taken part in our screening programme.
“I felt I was a priority,” said Vicky, who has type 1 diabetes and is mum to Chloe, 3, and baby Ellie. “If an appointment didn’t suit it was rescheduled straight away. That was great as I had Chloe at home and I was working, so juggling my antenatal care was a challenge.”
The initiative was developed in with maternity units around Ireland to ensure women have a seamless route to follow-up eye testing and care if needed.
Kara Madden has worked with patient advocacy groups since their inception. Her experience has cemented her belief that “partnership is the best way to bring about change in the health services”. Kara was recently involved in the organisation of the HSE’s second Patient and Public Partnership conference.

I want to start by acknowledging the great work happening across the region and thank you most sincerely for your support and co-operation in these last eight months.
I spoke at the national HR Conference in September about leadership and reform. I had an opportunity to reflect on the lessons learned within our own organisation and internationally. There is a wealth of knowledge that must be incorporated into our approach in Ireland. Such as the significance of staff experience with change and the necessity of constructing our services in collaboration with and for our patients and service users. I had a couple of key messages at the HR summit that I would like to share with you.
“Be courageous in the pursuit of a good and positive culture, always ask the question who is the decision maker and in what governance structure is that decision being made. Communicate, communicate and communicate and always, say what you mean, and mean what you say!”


This message applies to all staff, including our Regional Leadership, as we lead by example.
Regional Leadership Team
I'd like to formally welcome the four Integrated Healthcare Area Managers who started in their posts on Tuesday, 1st October. Trevor O’Callaghan, IHA Dublin South City and West; Orlagh Claffey, IHA Dublin South West; Mary O’Kelly, IHA Kildare West Wicklow; and Carole Broadbank, IHA Midlands, have held key senior leadership positions in our region and their appointments provide stability as we plan how we can put the region on a sustainable footing while collectively developing our strategy for growing the region to be the best place to live in, to grow in and to work in.
I will work closely with our IHA managers, wider RLT to ensure integrated care is enabled in an organised manner across the region, and each IHA will closely work with all levels of staff and within our communities to ensure we continue to deliver the same level of services.
We are all progressing through a period of change, and I am confident that this time of change will lead us to a stronger place. Teams are restructuring, some are moving into new roles with new teams, and some have new management structures. During this time, it is imperative that we continue to focus on our activity and maintaining services for our patient population. Our focus is on integrating our services and ensuring our patients experience timely access to high quality services, improved waiting times and timely access to health and social care services. Above all, we must make sure our services continue to be delivered under strong clinical and business governance systems and that we provide a good culture in HSE Dublin and Midlands so, every one of us has to both set and show actions that support a positive culture.
I’d like to reference the ‘Supporting Transformation in Adult Safeguarding’ Conference, an event organised by the HSE

Kate Killeen White alongside the Regional Leadership Team: Robert Forde, Dr Sharon Sheehan, Trevor O’Callaghan, Martina O’Byrne, Paul Flood, Carole Broadbank, Dr Fionnuala Cooney; Mary O’Kelly, Joseph Campbell and Orlaigh Claffey.
National Safeguarding Office. It was a great honour and privilege to deliver the opening address at this event. I was heartened by the commitment and dedication demonstrated by colleagues to ensuring the safety, protection, and well-being of every vulnerable individual in our care. I have seen first-hand the profound impact of strong safeguarding policies and practices. It is our responsibility to not just respond to incidents but to be proactive to ensure that the systems and structures we build prevent harm before it occurs.
The winter vaccination programme for staff in our region is well underway. We have made good progress since our regional campaign kicked off on 1st October.
As of 10th November, we have reached 39.3% staff uptake of flu vaccination and 16% uptake of COVID-19 vaccination across the region, excluding some key data from GP, pharmacy and section 38 services. In this same period, integrated winter vaccination teams have organised 305 flu clinics and 437 COVID-19 clinics across the region for healthcare workers.
As we approach the Christmas period, I hope that that you can take some well-earned time to rest and if you are working over the period, thank you. If you require support in this time of year or any time of the year, please know that the HSE Employee Assistance Programme is free and available to all HSE staff. Finally, I know times of change can be challenging and I accept that we have a lot to do as we continue to develop the HSE Dublin and Midlands. I ask for your patience and commitment to delivering the highest quality and safe patient care.
Nollaig shona dhaoibh!
Midland Regional Hospital Portlaoise (MRHP) has officially launched two new designated areas in the hospital that will enhance quality of care for people living with dementia in this setting.
A new five-bedded Dementia Friendly Bay in the Emo Court Ward was opened to enhance supports for inpatients living with dementia, as well as a new dementia friendly area in the Emergency Department.
The new areas include:
• technological support, such as TV streaming system with amplifiers
• radio/music player and headphones help to optimise sensory stimulation, reduce sensory overload and minimise non-cognitive symptoms
• meaningful activities boxes, that can be tailored to each individual to promote independence, engagement and participation
• different colour schemes and contrasting colours to promote wayfinding, minimize confusion and make the environment more person-centred for people with dementia and their families
• orientation clocks introduced to support awareness of time, month, date and day
• blue-coloured handrails fixed in the Dementia Bay toilet for better navigation, safety and independence.
Olivia Lafferty, Director of Nursing, MRHP, said, “Providing person-centred care in a supportive physical and social environment can enhance the experience and wellbeing of patients with dementia during their acute hospital journey. We are committed to providing ongoing evidence-based high-quality person-centred care for patients living with dementia during their acute hospital stay.”
The funding of resources for this area was provided by the Nursing and Midwifery Planning and Development Unit and MRHP.

Smitha Joy, CNS in Dementia Care, MRHP; Dr Taiwo Popoola, ED Consultant, MRHP; Finola Gill, NMPDU; Tanya McGahey, OT, MRHP; Maura Rice, ADON, ED and Paediatrics Services, MRHP; Laura Dunne, Frailty Intervention Team Physiotherapist, MRHP; Fiona Moore, ADON Practice Development Department; and Claire Walsh, CNM 3, Emergency Department, MRHP.
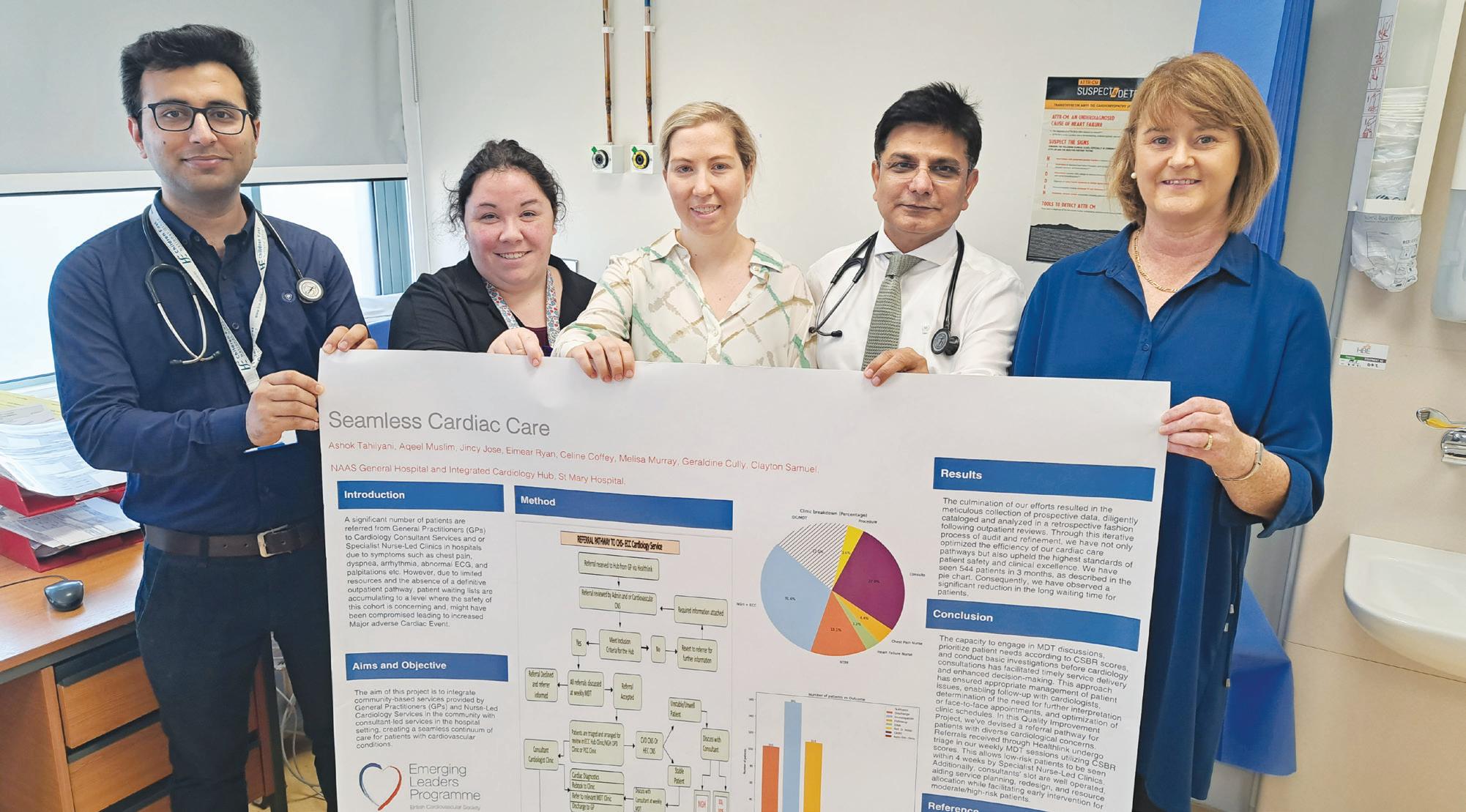
The integrated multidisciplinary cardiology team from Naas General Hospital (NGH) and Community Healthcare have been recognised at the British Cardiac Society (BCS) Annual Conference for innovating to reduce waiting time for patients.
The goal was to connect community-based services – like those provided by GPs and nurse-led cardiology services – with consultant-led services in the hospital.
This work has led to quicker patient care and a significant reduction in waiting times, from 48 to 52 months down to six to nine months.
Their international recognition reflects the hard work, dedication and innovation of their consultant and nursing teams.
One of the key highlights of the team’s presentation at the conference was the implementation of the Enhanced Community Care (ECC) post. This initiative, along with the new
streamlined cardiology work patterns, has greatly improved how patient care is managed.
Three members of the team work exclusively in community healthcare settings, ensuring patients receive care that extends beyond hospital walls: Eimear Ryan, Clinical Nurse Specialist (CNS); Melissa Murray, Projects Officer; Geraldine Cully, Operational Lead.
Working solely at NGH, there are members of the team who are at the forefront of providing specialised care to patients within the hospital setting: Aqeel Muslim, Registrar; Celine Coffey, Cardiac Physiologist; and Clayton Cully, Clerical Officer.
Two members of the team split their time between community healthcare and NGH, demonstrating the importance of integration across services: Jincy Jose, Clinical Nurse Specialist; and Professor Ashok Tahilyani,
Consultant Cardiologist.
Reflecting on his time at NGH, Professor Tahilyani emphasised the importance of teamwork.
“Success in medicine isn't defined by individual achievements; it's built on the strength of our team. I joined Naas General Hospital just over two years ago, and the welcome and support I received taught me the true value of teamwork. This success shows what we can accomplish when we truly work together as a team and as one health service,” he said.
In addition to his clinical work, Professor Ashok has started a running club that is open to patients choosing to make healthy lifestyle changes.
Each Thursday, they gather and run, walk, or run-walk around the beautiful lakes next to the hospital. This initiative not only promotes health but also fosters connections within our community, truly making every contact count.
Tallaght University Hospital (TUH) was delighted to host the Ricciotti ensemble as they visited Ireland on their Shamrock Shuffle tour. The Ricciotti ensemble is a street symphony orchestra from the Netherlands. The orchestra is made up of 43 young musicians, professional and amateur.

The musicians performed in the main atrium of the Hospital, the Vartry Renal Unit, Oncology Day Ward and the William Stokes Unit. This was followed by a final performance for staff at lunchtime at the rear of the hospital canteen. The visit was facilitated by the Arts and Health Team at TUH.
For many years, Naas General Hospital (NGH) has facilitated the clinical placements of many nursing students from a variety of disciplines. Recently, however, the hospital welcomed its own group of nursing students for the first time.
In partnership with Trinity College Dublin, NGH has been designated as an Academic Nurse Teaching Hospital. This means that NGH will serve as one of the main clinical bases for nursing students pursuing the Bachelor of Science in General Nursing.
Some 12 students will begin their clinical placements at NGH, gaining hands-on experience in a wide variety of healthcare settings across Kildare and West Wicklow. These placements will include rotations in areas such as the Emergency Department, Operating Theatre and Care of the Elderly (COTE), as well as in specialised units like the Coronary Care Unit, Intensive Care Unit and Day Care Services, which include Oncology and Haematology.
Séamus Hickey, violinist with the orchestra, who performed in the Oncology Day Ward. The NGH Care Cart in action.

Naas hospital unveils its Care Cart for staff
Naas General Hospital has launched a Care Cart, an initiative designed to support the spiritual and emotional wellbeing of staff.
Sara O’Brien, Clinical Placement Coordinator; student nurses Kumashe Femi-Oluyede, Sorcha Lynch, Kamila Merenkova, Aubrey Gamutan and Holly McDermot; Elaine Harris, Practice Development Coordinator; Siobhan Ryan; and Anne Murphy, Director of Nursing. Not pictured: Student nurses Emma Riley and Lucy Keogh

In other hospitals, the Care Cart has helped reduce staff burnout and turnover while indirectly improving patient care outcomes. The Care Cart promotes care, compassion, trust and learning - core values of the HSE and Naas General Hospital.
The Cart, devised by the Pastoral Care Team, will visit different wards and departments weekly, at convenient times, offering a space where staff can gather for snacks, encouraging material and supportive conversations. Staff can also grab a snack on the go without any obligations.
The cart offers a variety of drinks like Lipton tea and Innocent smoothies, and snacks catering to different dietary needs, including gluten-free, dairy-free, and vegan options. It also carries materials like advice cards, prayer cards from different traditions, and wellbeing tips.
The Care Cart aims to create a supportive environment where staff can simply ‘be’ and connect with each other, enhancing their emotional and spiritual wellbeing.
The residents, staff and management of Cluain Lir Community Nursing Unit (CNU) in Mullingar have been engaged in a flurry of creative activity in recent months as they aim to promote projects with a strong community focus.
Cluain Lir is home to 44 men and women who avail of full-time care alongside a Daycare Service providing support for the wider community.

In 2023, the CNU received Creative Ireland funding, with the support of the Westmeath Arts Office, to collaborate with photographic artist Emma O’Brien to highlight the unique personalities and stories of residents living with dementia. The resulting exhibition, entitled ‘Inside Out’, was a sensitive portrayal of the lives of residents and day service users.
This year, again with assistance from Creative Ireland and the Westmeath Arts Office, the show ‘Inside Out 2024’ has evolved somewhat into a format suitable for touring, and reached further into the community with an exhibition in the atrium of Belvedere House and Gardens in September.
In another coup for this energetic group of residents and staff, a garden entitled ‘Forget Me Not’ was selected to show in the Postcard Garden category in Bord Bia Bloom in the Phoenix Park in June. This garden was designed by the group under the guidance of staff member Carol Hayden.
Following the exhibition, the garden was returned and reassembled in Cluain Lir for residents to continue to enjoy for years to come.
Cluain Lir Resident Artist Lucy Tormey, who works closely with Activity Co-ordinators Karina Browne and Ruth Donoghue in the Unit, said it was wonderful to see the fruition of the efforts to maintain meaningful links between the residents and the communities they have come from.
The team from MRHT who represented Ireland at the EUSEM International SIM Wars.
Cluain Lir resident Michael Ward with his artwork.

Midland Regional Hospital Tullamore’s Rapid Access Frailty Team colleagues scooped the Multidisciplinary Team of the Year Award at the recent Hospital Professional Honours 2024 in The Dublin Royal Convention Centre.
The Honours promote excellence, dedication and innovation within the hospital sector and represent a celebration of all hospital healthcare teams who were working tirelessly on the frontline.

The Emergency Department Simulation Team from Midlands Regional Hospital Tullamore (MRHT) represented Ireland at the prestigious European Society for Emergency Medicine (EUSEM) International SIM Wars in Copenhagen in October. As the winners of the Irish Sim Wars at Irish Association for Emergency Medicine 2023, this dynamic team competed against international counterparts, tackling complex clinical scenarios designed to test their medical expertise and teamwork.
Facing environmental, physical and mental challenges, the team needed to demonstrate their ability to deliver high-quality care in a range of simulated patient emergencies. Their participation highlights their commitment to excellence in emergency medicine and positions them on the global stage in simulationbased medical education. The team would like to thank Dorothy Niall and the Midlands Nursing Midwifery Planning and Development in particular.
Congratulations from all your colleagues in MRHT.

Midland Regional Hospital Tullamore (MRHT) held its inaugural GP Study Day in the Education and Research Centre in the hospital recently. The event was a great success, with over 40 GPs attending from Offaly and Laois. The study day was chaired by Dr Joanna McGlynn, Medical Clinical Director and Consultant Physician in Geriatric Medicine, MRHT.
The study day provides a time for GPs and hospital colleagues to meet in person and discuss and learn about relevant topics of interest, such as care of older persons, emergency medicine, surgery, haematology and palliative care.
It also provides an opportunity for the health professionals to share information on the referral pathways into the hospital and provides a forum to learn about common GP scenarios across the various specialities.
Speaking about the event, Joanna said, “Events such as this evening provide an excellent opportunity for informal interaction between primary care practitioners and hospitalbased specialists.”
Shirley Keyes, Operations Manager, MRHT, added, “The GP Study Day is an important opportunity for the hospital to engage with our GP colleagues. We intend to make this a quarterly event and look forward to continuing our work for the benefit of patient care as we strive, in collaboration with our GP facilitators, to optimise the educational value of sessions like this.”
Professor AnneMarie Brady, Chair of TUH and Lucy Nugent, Chief Executive of Tallaght University Hospital.
Back: Dr Gerard Crotty, Consultant Haematologist; Dr Michael Cushen, Consultant in Palliative Medicine; Mr Yasir Bashir, Consultant Surgeon. Front: Dr Carla Hopper, Consultant in Emergency Medicine; Dr Anna Moore, Consultant in Emergency Medicine; Dr Joanna McGlynn, Medical Clinical Director and Consultant Physician in Geriatric Medicine; Dr Teresa Donnelly, Consultant Physician in Geriatric Medicine.

Organisers of the event from the Midland Regional Hospital Tullamore would like to thank all those who attended and facilitated on the day. 12% reduction in Tallaght wait lists

Over 40 GPs attended the event including Dr Muireann Leonard, GP; Shirley Keyes, Operations Manager, MRHT; Dr Michael Cushen, Consultant in Palliative Medicine; Dr Sohail Rasool, Irish Prison Service; Catriona McDonald, General Manager, MRHT; Dr Joanna McGlynn, Medical Clinical Director and Consultant Physician in Geriatric Medicine, MRHT.
There was a 12% reduction in waiting lists at Tallaght University Hospital (TUH) during 2023, according to figures in its 2023 Annual Report. The report has also revealed that 84% of patients were waiting three months or less for surgery. This is a significant achievement considering the increased activity levels and demands on hospital services during 2023.
One of the best indicators of the growth in the hospital's workload is the number of patients who attended the Emergency Department (ED) at TUH during 2023. For the first time, over 55,000 attended the ED.
On average, it took 32 minutes for patients to be triaged on arrival and most were seen by a doctor within four hours and 29 minutes.
Looking ahead, TUH CEO Lucy Nugent said, “Incredible efforts were made by teams across the system to reduce waiting times for outpatient appointments, and this has resulted in a 12% reduction in our waiting lists. There is still more work to be done in this area but we are hopeful that, as more space becomes available in the hospital and as paediatric services move out, we will be able to expand the number of clinics we can offer and further reduce waiting times for patients.”





Dungarvan Community Hospital in Co Waterford was the venue for the recent launch of the Making Safeguarding Personal (MSP) toolkit of resources.
Developed by the HSE’s National Safeguarding Office, MSP will serve as a reference point for advancing a person-centred and outcome-focused practice in adult safeguarding screenings and plans in place across the HSE and HSE-funded services.
The MSP practice tools give guidance to staff that advances person-centred and rights-based practice, in line with the principles of assisted decision making legislation. The tools are designed to advance empowerment, choice and control by persons using the HSE’s services and those supported by it.
Presentations at the launch acknowledged that safeguarding is a very challenging area of work and that everyone has a part to play in preventing abuse and in responses to it if it occurs.
National Sharing Day 2024 was the fifth annual event of its kind, hosted by Disability Quality Improvement and presented by disabled people on their lived experiences.
There were seven presentations from people who shared their experiences of making decisions about their finances, where they live, hobbies and future plans. They outlined their supports, which included their staff, family, friends and some of the challenges they have faced.
Bernadette Finnegan shared her story of moving from the Magdalene Laundries to a nursing home and then recently to her own home, where she finally has gained her sense of independence.
Shannon O'Farrell Molloy described the support of her family which has enabled her to live a life of her choosing and now she looks forward to being an honorary lecturer, and continuing travelling all around the world.





Assistant
The recent National HR Summit provided a chance to acknowledge and embrace the significant HSE restructuring, along with the opportunities and challenges arising from it.
The conference, entitled ‘Leading Our People Through Change’, also celebrated the strong foundations that HSE HR are working within during this period of organisational change.
Anne Marie Hoey, Chief People Officer, opened the summit welcoming the delegates and set the stage for CEO Bernard Gloster to deliver his address ‘The People Ask’.
The morning session, moderated by Enda Maloney, Saolta University Health Care Group, provided presentations from Kate Killeen White, Regional Executive Officer, HSE Dublin and Midlands Health Region, who shared her expertise on ‘Leading Large Scale Health System Transformation and the Lessons Learned’, emphasising two key effective practices - governance and decision-making within the new structures.
This was followed by HR Strategic Workforce Planning’s Dr Philippa Ryan Withero and Dean Grennan
demonstrating insights and uses of HSE workforce data, while Assistant National Director Eithne Fox outlined the actions to attract, recruit and, crucially, retain staff.
Declan Hynes moderated the mid-morning session with Professor Michael West talking about the evidence to support the positive impact of a compassionate approach in the workplace. Mary Connaughton, Director of CIPD, followed with her presentation ‘Delivering Change as a People Professional’ and the mid-morning session concluded with Dr Abigail Ruth Freeman, Research Ireland, emphasising that change does take time and co-creation is a key to success.
The afternoon session, moderated by Margaret Sorohan, showcased an overview and participant experience in the Health Service Leadership Academy delivered by Dr Louise Doyle, Prof Jane McGrath and Rose Shivmangal.
The day concluded with an excellent presentation from Audrey Cahill, Director General, Work Relations Commission, on ‘Workplace Relations in an Era of Radical Change’.



Top: Prof Michael West, Professor of Organisational Psychology, Lancaster University, Mary Connaughton, Director CIPD Ireland, Declan Hynes, Moderator, and Dr Abigail Ruth Freeman, Director Science Foundation Ireland. Middle: Bernard Gloster, CEO HSE. Above: Anne Marie Hoey, Chief People Officer, HSE.
The conference programme provided an opportunity for the delegates to reflect and build on their roles in HR at this time of organisation change. It also offered information on practical supports, overviews of new directions in culture development, attraction and retention strategies.
Delegates benefitted from opportunities to visit the HR stands hosted at the summit.


hears how we are ‘changing patient outcomes: one partnership at a time’

Patient partners and advocates highlighted the welcome progress and the evolving collaboration with the HSE in the development of the new health regions and their partnership structures at the recent HSE Patient and Public Partnership conference in Dublin Castle.
The second annual event was organised in partnership with patient partnership groups, including the HSE National Patients’ Forum. The theme was ‘Changing patient outcomes: one partnership at a time’.
Sharing an insight into why she got involved, patient partner and disabilities advocate Joan Johnston said, “As a patient partner, it is rewarding to see my voice reflected in service improvement and the changes that have been made. I feel that I am helping to change the perception of patient partners and the unique capacity and drive we have to work across the health system to improve the experience of those who come after us.”
Looking ahead, HSE CEO Bernard Gloster explained the next partnership priorities.
“A key focus of the HSE in 2024 has been the development and approval of patient partnership structures as part of the health regions. A partnership proposal was developed by patient representatives in collaboration with HSE staff which sets out what should be happening around patient partnership in each HSE region. The focus is now on working with the six HSE Regional Executive Officers to implement this proposal, and embed partnership in the functioning of the new health regions," he said.
Patient partner and disabilities advocate Joan Johnston; Laura Kavanagh, IPPOSI; HSE CEO Bernard Gloster; patient partner and rare disease advocate Anne Lawlor; and HSE National Director Public Involvement, Culture and Risk Management Joe Ryan.
Patient partner Aileen Killeen, Irish Heart Foundation patient partner Pauline O’Shea; and Regional Executive Officer, HSE Dublin and North East, Sara Long.

Speaking about her work on the health regions partnership structures, Laura Kavanagh, Irish Platform for Patient Organisations, Science and Industry, said, “The health regions programme teams have been great. They have sat, listened, convened workshops, drafted and redrafted proposals, and a whole partnership ‘blueprint’ has been developed which sets out what should be happening at a regional and national level.”
HSE National Director, Public Involvement, Culture and Risk Management Joe Ryan added, “We are committed to changing and improving how we involve patient partners in co-designing health service projects to improve services. As part of this work, we are developing internal policies to give life to the Partnership Strategy, including guidance on when patient partners are included and how partners are identified, selected and supported. We are fully focused on listening to the patient experience and partnering with those with this experience.”


On World Mental Health Day in October, the Central Office of Mental Health Engagement and Recovery (MHER) hosted the first International Individual Placement and Support (IPS) Learning Set in Ireland. The theme for the event was 'Being Together, Learning Together, Doing Together’
The event was specifically designed to inform and support those who are involved in various aspects of IPS, including service planning, programme delivery and partnering for future IPS growth. The event included a wide variety of workshops that covered various aspects of IPS, some of which included IPS in Ireland, which highlighted the employer and service user perspective, Learning by Data and a workshop on IPS Fidelity Evaluation.
Una Twomey, Strategy Lead for MHER, welcomed the Minister Mary Butler, who opened the Learning Set.
“The theme of this year’s World Mental Health Day is ‘Mental Health at Work’, and I want to highlight how important it is that we ensure that we foster workplaces that are supportive and free of mental health stigma. By doing this we can all support those who may have mental health difficulties to find work, to remain in work, and benefit from the fulfilment, well-being and sense of purpose that can come with employment,” said Minister Butler.

“That is why I am proud to support excellent initiatives such as the Individual Placement Support, an internationally recognised, evidence-based programme to support people with mental health challenges returning to or commencing work which is operated by the HSE.”


The event closed with a handover to Finland, who will host the next IPS Learning Set in 2025.


Minister Mary Butler with some of the event organisers at the IPS Learning Set.
Over 1,000 health professionals, policymakers, and patient advocates gathered both in person and online for the recent inaugural Integrated Healthcare: Advancing Health Service Reform conference. The event focused on key initiatives designed to tackle the most pressing challenges in Irish healthcare, such as expanding primary care, reducing waiting lists, modernising care pathways and implementing digital innovations.
Kate Weeks, one of the seven poster winners, receives an award from HSE CEO Bernard Gloster, with Aisling Heffernan, Chief Officer, Community Healthcare East, and Roseanne Killeen, CEO, Ireland East Hospital Group.
The conference received overwhelmingly positive feedback from senior leadership, colleagues and staff. Bernard Gloster, CEO of the HSE, highlighted the progress made in patient care through regional reform and other innovations, while acknowledging ongoing challenges like growing demand and the need to integrate care locally.
The conference explored themes such as improving productivity, enhancing the service user experience and advancing integrated and community care. Breakout sessions provided insights into the ongoing transformation and reform of healthcare delivery across primary, community and acute care.
One of the conference highlights was the presentation of over 100 posters developed by staff showcasing initiatives aimed at improving patient care. These posters showcased the continuous improvement efforts by staff across the health service, benefitting people who use our services. Seven outstanding poster presentations were recognised during the event, with Bernard Gloster awarding each of the winners for their innovative approaches to healthcare delivery, focusing on new ways of working, service improvements and multidisciplinary team efforts. The posters are available to view online and are also now on temporary display in Dr Steevens’ Hospital.

To access the posters, presentations and video recordings, visit hsenationalconference.com

The HSE, Department of Health, and Patients for Patient Safety Ireland collaborated with key stakeholders on the development of a suite of resources for patients as part of World Patient Safety Day, which this year focused on diagnostic safety.
The resources aim to continually improve communication between people using health and social care services and healthcare professionals. In one, ‘My Health, My Voice’, people are encouraged to share any symptoms they have and ask three questions. 1. What do I need to know now? 2. What do I need to do next and why? 3. What can I expect?
Dr John Brennan, GP and Lead Faculty for the Royal College of Physicians Ireland Postgraduate Certificate in Quality Improvement and Leadership in Healthcare, said, “Some diagnoses can be reached quickly often just in one visit, while others
World Mental Health Day was marked by a tree planting ceremony at the St Stephen's Hospital campus, in Glanmire, Co Cork.
Cork heritage specialist Ted Cooke captivated his engaged audience with his boundless knowledge of horticulture and local heritage. The campus community, staff and service users then bedded a variety of trees, enriching the already beautiful grounds.
The trees were being funded by the HSE Sustainability Office and will greatly enhance the campus environment and have positive effects on the mental and physical wellbeing of staff and service users.
This event was the latest of many organised by a very established Wellness @ Work Committee over the years.
Horticulturalist Ted Cooke planting with the Wellness@Work committee for St Stephen's: Aisling Hassett, ADON; Cornelia Holland, Nurse Planner; Conor Long, ADON; Cathal Keohane, ADON; Laura Garvey, CNM3; David Coakley, ADON; Sheila White, ADON; Catriona Canty, Mental Health Lead, Healthy Ireland; and Richard Browne, Catering Officer.
can take longer, requiring several visits, further tests or even a visit to a consultant.
“The ‘My Health, My Voice’ leaflet is very useful in helping to guide and shape conversations around the diagnostic process. I would encourage patients to try the leaflets and if unsure during a consultation, please ask the questions. We want each of our patients to fully understand their diagnostic journey and feel confident in the care they receive.”
Bernie O’Reilly, Chair of Patients for Patient Safety Ireland, who co-chaired the working group, said, “Not all patients feel as comfortable asking questions, and this leaflet helps provide a structure to appointments and points to suggested questions to ask. It also provides links to trusted sources of information and a very useful medicines list template.”




Sepsis is a life-threatening condition requiring urgent medical attention. When untreated or delayed, it can lead to tissue damage, organ failure, and death. Early recognition and intervention are critical to saving lives, as sepsis progresses rapidly and can become fatal within hours.
The eighth National Sepsis Summit took place recently with the theme focused on how ‘early treatment saves lives’ to address the crucial role of early intervention in improving patient outcomes.
“Early recognition and prompt treatment of sepsis can sometimes mean the difference between life and death. We know that timely intervention reduces mortality and minimises long-term complications for sepsis recovery. By simply asking ‘could it be sepsis?’ at the first sign of infection, we can save lives,” said Dr Michael O’ Dwyer, Clinical Lead, HSE Sepsis Programme.
Recognising the role of the patient experience in shaping the future of sepsis treatment, the 2024 summit also featured a speciality workshop designed for advocates, sepsis survivors and family members who are now involved in patient advocacy work. The workshop provided a unique opportunity for patient advocates to have a voice in shaping the future of sepsis treatment.
Also featured was a patient story from Yvonne Young, who shared a personal account of her son’s experience of sepsis. Between 2020 and 2023, there have been 117 deaths among children from sepsis with 2,891 cases.
“Have no regrets, ask 'could it be sepsis?' Don’t be afraid to ask, advocate for your loved one, advocate for your family,” she said.
Opportunities for cohesion across the new health regions through clinical leadership was among the topics up for discussion at the recent National Clinical Programmes (NCP) Conference.
Dr Siobhán Ní Bhriain, National Clinical Director Integrated Care, was on hand to welcome delegates to the event. The opening address from Dr Colm Henry, Chief Clinical Officer, emphasised the role of the NCPs in enabling and supporting integrated care in the new health regions through the design and implementation of modernised care pathways and modes of care.
Tony Canavan, Regional Executive Officer, HSE West North West Health Region, discussed the opportunities for cohesion, and the morning session concluded with a lively panel discussion on equity in decisionmaking and resource distribution across the health regions.
The focus then shifted to how clinical design can enhance care transitions. Nuala Ward, Director of Investigations at the Ombudsman for Children’s Office, provided a compelling presentation rooted in the real-life experience of a young person transitioning from paediatric to adult healthcare services.
Dr Ciara Martin, National Clinical Advisor and Group Lead (NCAGL) for Children and Young People, presented findings from a Your Voice Matters survey. Dr Emer Ahern, NCAGL for Older Persons, highlighted the need to have an age-friendly health system.
The afternoon sessions focused on the tools and services to support clinical design and the critical role that accurate data plays in informed decision-making.
For those of you who would like more information on the conference including some of the presentations from the day, please visit bit.ly/NCPConferenceDay2024

The HSE Health and Wellbeing Annual Report for 2023 shines a spotlight on the progress we've made in promoting healthier communities across Ireland. Our mission – to create a system that prioritises prevention, reduces health inequalities, and empowers individuals to manage their own health – has seen significant strides during 2023.
The cornerstone of our work in 2023, as always, was the emphasis on prevention. The Making Every Contact Count (MECC) programme has continued to expand, ensuring that every interaction between healthcare professionals and patients is an opportunity to promote healthier lifestyles. By equipping healthcare professionals with the tools to encourage behaviour change, we are embedding a culture of prevention that will benefit individuals and the healthcare system as a whole.
Participants attending a workshop to demonstrate the functions and uses of the Acorn Age Friendly Tablet
A total of 327 older people across Ireland have been presented with special tablet devices as part of the Healthy Age Friendly Homes Programme to reduce incidents of social isolation and to open them up to a new world of technology and communication. This Sláintecare Integration-Funded Project aims to promote social engagement of older citizens and reduce levels of social isolation through the use of Acorn Age Friendly Tablets. The Acorn Computer Tablet is a specialised tablet, tailored to address the needs of older people in a closed secure network. It opens up a world of relevant online content, encouraging users to engage and interact at both social and commercial level. The interface has clean lines, is simple to navigate, provides easy access to a help button, and provides remote technical assistance when required.
A key function of the Acorn Age Friendly Tablet is to help older people connect digitally by accessing information on services and local activities; stay in touch with family using videocalls; book online transport; use social media; access online library service and HSE Healthy Ireland’s My Health functionality on the tablet. Through an existing working relationship between Age Friendly Ireland and HSE Healthy Ireland, a collaboration was formed for this project to develop and implement the My Health functionality of the tablet with the developer Origin Care Group. This newly developed section on the Acorn Tablet includes free exercise videos led by health professionals; minding your wellbeing programmes; and health promotion information around mental health, healthy eating, quitting smoking and reducing alcohol consumption.
One of the most significant achievements outlined in the report is our work through the Sláintecare Healthy Communities initiative. This programme specifically targets the root causes of health inequalities, focusing on areas of deprivation where people are at greater risk of developing chronic illnesses due to factors such as smoking, poor diet, alcohol use, and physical inactivity.
Collaboration is at the heart of many of our successes this year. By working closely with organisations such as Tusla, Sport Ireland, and the community and voluntary sectors, we’ve been able to support local initiatives that encourage healthy behaviours, improve access to services, and empower communities to take control of their health.
The 2023 report also showcases how digital health innovations are transforming the way we deliver care. Online resources like Quit.ie, MyChild.ie, AskAboutAlcohol.ie, MyOptions.ie, Man2Man.ie, Sexualwellbeing.ie and Healthpromotion.ie have been critical in providing accessible advice and tools that help people manage their health independently.
To join our mailing list, email Healthandwellbeing. communications@hse.ie





















































If you work in healthcare, you are at increased risk of being exposed to flu and COVID-19


Vaccines are safe and effective and provide the best protection from flu and COVID-19.
You can get both vaccines at the same appointment.


Vaccines may be available at work and are also available free of charge from GPs and Pharmacies








Visit the HSE website for vaccine information and resources

