WINTER 2022 MATTERS at







































































































Dedication doesn’t pause for the festive period
CaringChristmas
Welcome to the latest edition of Health Matters. While most of the county is settling down with their families to enjoy the special time over Christmas, our frontline healthcare workers are at work looking after patients and making sure everyone is getting the best of care.


Some of the workers, from emergency call takers and paramedics, to staff on the ground in our hospitals, share their experiences of working over the festive season and what they do to make it special for themselves and their patients, both away from their homes and families.
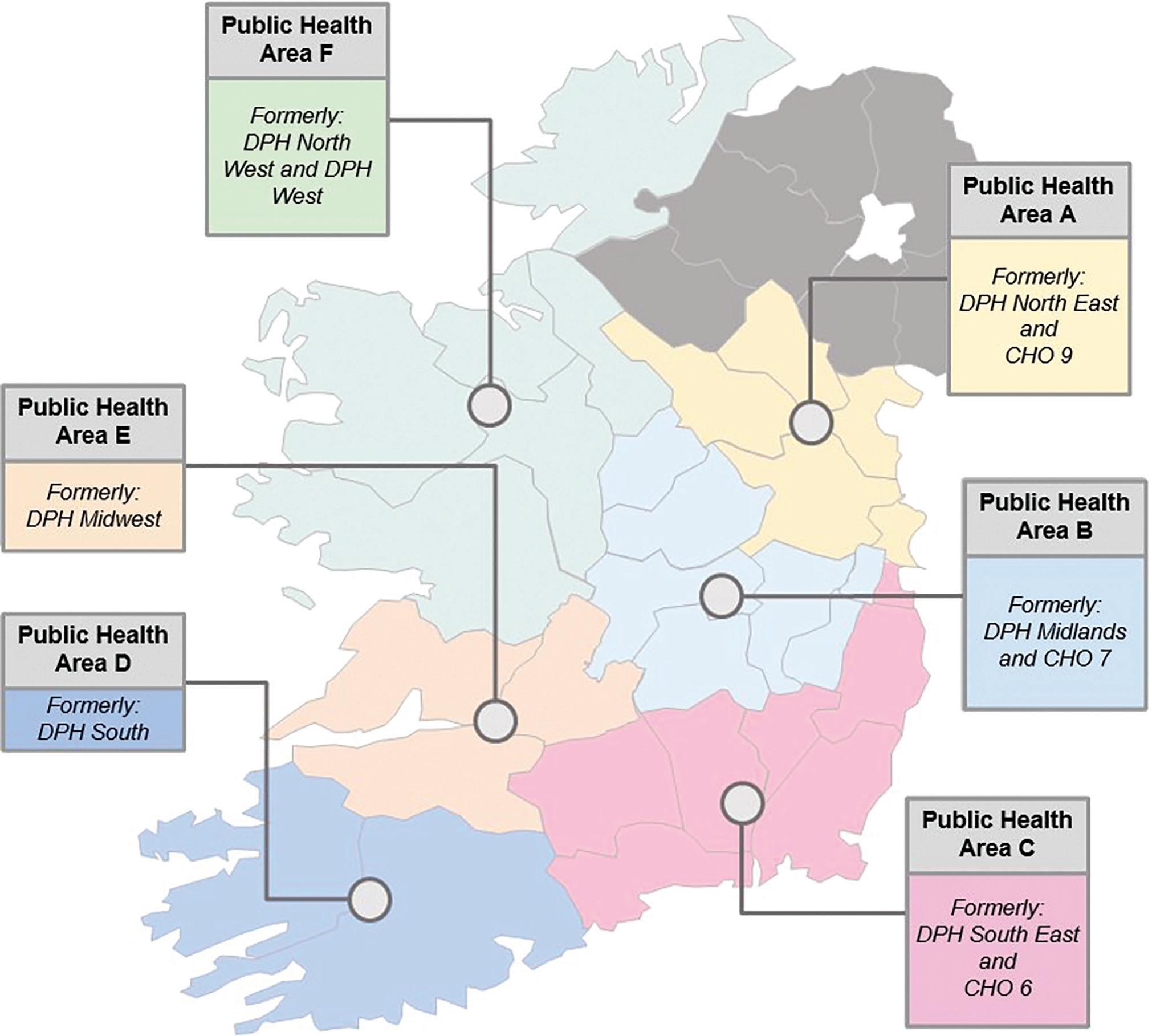
In this edition, we put the spotlight on Integrated Care and the new Regional Health Areas (RHAs), which will see most of our healthcare accessed in our communities. Acute hospitals and Community Health Organisations (CHOs) will be grouped together into six large regions called RHAs. The RHAs will be fully operational by January 2024.
It is all part of the Sláintecare vision of an integrated health system where a person can access high-quality healthcare from valued healthcare professionals, closer to their home, within a reasonable amount of time.
We also find out about the winners in this year’s Health Service Excellence Awards, which again received a massive number of entries.
The awards are an opportunity to showcase and celebrate examples of the great work that happens every day across our health service. But it also gives staff a chance to see what other teams around the country are doing and has led to much shared learning.
A sincere thanks to all those who have sent in contributions to this edition and I hope you find plenty of interesting reading in it.
Happy Christmas and a prosperous new year to all our readers.
Joanne Weston Editor
CONTENTS
CEO message
A frontline Christmas
Minister breaks ground on UHL bed block
Children’s therapy services in Cashel
House donation
New equipment for baby care unit
Moville craft fair
Barretstown fundraiser
Cappagh outpatient department opens
Vascetomy service
Nursing strategy launch
Intensive care wing unveiled
HPV catch-up service
Flu vaccine
Rose Room for bereaved families
EAP healthcare workers and grief
Winning midwife
A day in the life of Disability Case Manager
Audrey completes swim
UHL Launchpad for cycle
Diwali celebrations
Respiratory lifeline for children
Breastfeediing week
Vital support for local women
Making progress on Integrated Care
Enhanced Community Care
Pathfinder service
CAMHS physical health monitoring clinic
Nenagh Injury Unit
Integrated Care Hub
Nurse-led clinic in Letterkenny
Children’s Disability Network
My HSE Self Service
Organisation Development
Values in Action
Health Service Excellence Awards
Le Chéile staff disability network
Living Well programme
Men’s Shed support for dementia pgroamme
Dementia activity box
Webinar promoting culture of safety
Memory Technology Resource Room
Civil Registration Service
Laboratory Programme
Drug checking pilot programme at EP
HSE at the Ploughing Championships
Home STI test service
Cancer survivor writes fundraising book
BreastCheck
National Screening Advisory Committee second annual call
Support and guidance for AMS teams
Are you winter ready?
Every Smile Matters
Patient Partners
Advances in digital recruitment
Your Opinion Counts
Brand guidelines
Data breach notification
QPS TalkTime
Walk and Talk Improvement
HSeLandD sees rise in annual users
FunFit for kids
New walking initiative in Dublin
End stigma of obesity
Perinatal mental health day
HSE climate plans
CHI lead way in climate action
stars visit UHL
1
2
8
8
9
9
9
10
10
10
11
11
12
14
16
16
17
18
19
19
20
21
22
24
26
27
29
30
31
32
33
34
35
36
38
40
42
46
48
49
50
51
52
53
56
63
69
70
72
72
73
74
75
76
77
78
79
OUR
54
55
57
58
60
61
62
64
66
68
80 Hurling
A MESSAGE FROM
EDITOR
A MESSAGE FROM OUR CEO STEPHEN MULVANY MEET THE TEAM
As I write this, I am just at the start of my 3rd month as your Chief Executive O cer. I’m continuing my visits to services and am really enjoying getting to chat to sta and service users about what is working well and what we want to improve.
HSE

Head of Internal Communications
Internal Communications Team
Yvonne Costello
Ann McLoone
Amy O'Neill
Frances Plunkett
Shane Larkin
Paddy Crosse
Keeva Carpenter
It remains my view that our 2 key priorities in the months ahead are maintaining, and where possible, improving access to our services and improving our engagement with sta and with service users and their families, particularly those that may be struggling to access our services or may wish to share their views on how we can improve.
Many of our health and social care sta , and those of our s.39 and s.38 voluntary partners, are working in di cult circumstances, including sta in parts of our disability, child and adolescent mental health and Emergency Department services, as they try and do their best for patients, service users and families.
As is often the case, it may take time before things begin to improve. To all our sta , and particularly those working in di cult circumstances, I want to acknowledge all that you have done, are doing and will do over the coming months and I want to thank you for your service. The HSE Executive Management Team and I are committed to supporting you, including through our work with our CHO, Hospital Group and Department of Health colleagues.
At a specific and practical level, we know that the congestion in our Emergency Departments is a symptom of a wider problem which includes the imbalance between the number of patients who need to be admitted to our hospitals each day and the numbers being safely discharged, with our vulnerably elderly patients being most likely to be caught up in this.
As our winter plan sets out, we need to work together on three key areas i.e.
• Firstly, improving the level and pace of hospital planned and community supported discharge from hospital, preferably discharge home for further assessment
• Secondly, providing clinically appropriate alternative pathways that allow for a reduction in the numbers of vulnerable mostly elderly patients being admitted to hospital
ASHVILLE MEDIA GROUP Editor
Our aim is for each of our services to be supported to drive improvement and to demonstrate, with data, that they are doing the best they can with the resources they have, today. For 2023, we will place a significant emphasis on enabling local front-line teams to map their key process flows, assess, and take whatever steps are practical for them to mitigate any imbalance between demand and capacity. More and more we intend to link future investment, which we know is needed, to areas that can demonstrate this, rather than simply investing in problems such as waiting lists without checking whether resources are being utilised e ectively and e ciently.
• Thirdly, improving the flow through our hospitals so that average lengths of stay are reduced, in particular reducing the average lengths of stay for patients who stay for more than 10-14 days in our acute hospitals. For at least the next 14 weeks, if you’re a member of one our front-line teams that is involved in any of the three key areas above, I think it is important that you and your teammates can visualise, own, prioritise and work towards a very small number of key measurable goals. These measurable goals, such as delivering a certain number of supported discharge opportunities per week, should be such that, if achieved, will materially reduce the risk to your patients.
I would appreciate it if you can work on this within your teams and seek input and guidance from your local and regional management as needed. It is intended that having these specific measurable goals would help focus and motivate our e orts, including our collaborative problem-solving e orts. They should not be used as hard performance management targets that can de-motivate depending on how they are set and monitored.
Published by Ashville Media, Unit 55 Park West Road, Park West Industrial Estate, Dublin 12, D12 X9F9. Tel: (01) 432 2200 ISSN: 0332-4400
All rights reserved. Every care has been taken to ensure that the information contained in this magazine is accurate. The publishers cannot, however, accept responsibility for errors or omissions. Reproduction by any means in whole or in part without the permission of the publisher is prohibited.
© Ashville Media Group 2022.
As we look ahead to the period between now and the end of February, we have reason to be concerned. The operational system, particularly as viewed through the prism our Emergency Departments, has been under pressure for some months and this pressure has increased in recent weeks. This is the case even though RSV does not appear yet to have quite peaked, Flu and COVID are well away from their peak, and the weather has been unseasonably mild.
Given what we can see ahead, and the issues and risks that it may pose for our patients and sta , I don’t think we have the option of only doing what we are already doing. We need to ask ourselves are we fully satisfied that we have done everything that can be done to fully implement our winter plan, and are we convinced that we are making the best use of all the sta and patient energy and insight, relationships with our voluntary, primary care and private partners, information, sta time and other resources available to us.
Ultimately our goal, in the interests of our patients, service users and their families, is to allow each of us to be satisfied that we have done everything we practically can to alleviate ED congestion this winter while continuing as much as possible the good work already visible in the reduction to community and hospital waiting lists.
The reality is that the low level of COVID vaccination uptake amongst healthcare sta is very concerning while FLU vaccine uptake amongst our health care workers this season is behind what was achieved in recent years. None of us wants to bring COVID or FLU home to vulnerable members of our families, or to impact on our fellow workers who may have vulnerable family members, or to increase the risks already faced by vulnerable patients in our care.
I am urging all sta who are eligible but have not already done so to get vaccinated for COVID and Flu.
Finally, thanks, again to all of you for everything that you are doing and will do over the coming months. I would like to wish you and your family a happy Christmas and a peaceful new year.
| 1 HEALTH MATTERS WINTER 2022
Emma Finn
Joanne Weston Art Director
Áine Du y Creative Director
Jane Matthews
CHRISTMAS on the FRONTLINE
Staff go the extra mile to make it special
CHRISTMAS IS A SPECIAL TIME OF YEAR WHERE FAMILIES AND FRIENDS GET TOGETHER TO CELEBRATE. BUT FOR FRONTLINE STAFF IN THE HEALTH SERVICES, IT IS OFTEN JUST ANOTHER WORKING DAY, SPENT LOOKING AFTER PATIENTS AND MAKING SURE THEY STILL GET THE BEST OF CARE. STAFF FROM AROUND THE COUNTRY SHARE WITH US THEIR EXPERIENCES OF WORKING OVER THE FESTIVE SEASON AND WHAT THEY DO TO MAKE IT SPECIAL FOR THEMSELVES AND THEIR PATIENTS, BOTH AWAY FROM THEIR HOMES AND FAMILIES.
HEALTH MATTERS WINTER 2022 2 |
HOSPITAL TEAMS KEEP CHRISTMAS MAGIC ALIVE FOR CHILDREN
“Fun is a huge part of working in a children's hospital and my job as a music therapist is to help the child to navigate their hospital journey and cope with the experience as best they can,” explains Alison Sweeney.

Alison, from Co Laois, is Senior Music Therapist in Children's Health Ireland at Temple Street. She set up the Music Therapy service in Temple Street almost eight years ago and has been there ever since.
“I'm one of those lucky people who can honestly say, I love my job, and I wouldn't swap it for anything in the world,” she said.
Christmas time in the hospital is particularly special and the sta play a large role in creating a wonderful atmosphere.
“Going the extra mile at Christmas time is really important and, if I'm being honest, is something I see colleagues do every day of the year. Every team member does what they can when they can to make a child's hospital experience that little bit easier, that little bit more tolerable and that's what working in a children's hospital is all about. The smile and welcome that Martina and her team gives parents and sta in the canteen every morning, the chatter and banter from John, Graham, Alan and team in Portering, and, of course, the giggles with our specialist nurses as they carry out their role so diligently and with such kindness,” said Alison.
“There is huge anticipation in the run up to the big day. Our service is very child-led and young children often bring this excitement into the therapy space which can result in writing songs about Santa, or their Christmas wishes. For adolescents, it can be a challenging time knowing that their current experience doesn’t fit how they would wish to celebrate Christmas. For parents too, the run up to Christmas can be challenging and filled with anticipation of the road ahead. Whilst we know we can't replace home, we work very hard as a team to ensure that Christmas in any Children's Health Ireland hospital is every bit as special and magical as it should be.”
“Christmas day is my favourite day of the year in Children's Health Ireland. I'm not doing therapy sessions on Christmas morning, instead my role is to bring a little musical joy to the wards and families along with our Christmas Day team led by John and Emma. I arrive around 9am and head straight to the music therapy room to tune the hospital guitar, and pack together a box of musical instruments which we will play as we jingle jangle our way from child to child, ward to ward, listening
to children's stories of how the morning has gone and introducing them to the big guy - Santa Claus himself!” said Alison.
She described the mood in the hospital during the Christmas period as ‘magic’. “Our play team do an incredible job at decorating the hospital - they honestly turn it into a winter wonderland and it is so appreciated by patients, families and sta . It brightens everyone’s mood. We usually have a day of carol singing on the wards with some of the hospital team and we've got lovely feedback about that from families and sta too.
“The reality is, everybody wants to be at home on Christmas day but there are times when this simply isn't possible. One thing we can do is make sure that every child under our roof has a memorable Christmas with singing and laughter and presents and Santa and joy! That's one of the biggest lessons working in CHI at TS has taught me - there are always sparks of joy to be found and shared.”
Alison explained how music therapy is an evidence-based profession.
“We use music to address clinical goals. I work with children and young people at both a creative and therapeutic level. Many of the young people I meet can be quite traumatised following what may have been an unexpected admission to hospital. Life is turned upside down for these young people and I hold the privileged position of working alongside them, and supporting them throughout their hospital admission. It’s a really creative, interesting job and I love the fast-paced, high-energy work in the acute setting,” she said.
Alison said she is lucky to share in such happy memories at Christmas time and be able to spend time at home with her family.
"The memories I have from Christmas day in Children's Health Ireland at Temple Street are so special. There's such an energy and excitement in the hospital Christmas morning. These experiences are amongst those that make Christmas for me. Singing Christmas carols on the ward with the team-there is such a sense of togetherness in it,” she said.
“I don't want to paint us as martyrs. The reality is I get to go home and have Christmas dinner with my own family. Some of the team don't get to do that because they work all day and unfortunately some patients don't either. I'm very lucky I get to do both and spend time with my family in the late afternoon. And that for me is Christmas. After a challenging two years, I'm really looking forward to this one.”
HEALTH MATTERS WINTER 2022 | 3
Christmas feast makes day special at the Coombe
Babies famously don’t like to follow a timetable so the Coombe Hospital in Dublin is usually a bustling place on Christmas Day as the new arrivals keep coming.
While the new and expectant mums can’t be at home, the hospital’s catering sta have made it their goal to ensure that they still get a festive feast to enjoy.

Lisa Jones, catering supervisor at the hospital, explained that care and attention that the chefs put into the Christmas Day menu.
“The menus are planned weeks in advance. You have everything there – the turkey and ham, brussels sprouts, roast potatoes, all the veg you could want. And the desserts are as good as you would get in any restaurant and all handmade here – Christmas pudding, cheesecake, yule logs, bano ee pie. The chefs really go all out,” she said.
“We don’t treat the day di erently from any other when it comes to preparation – all the meals are made from scratch,
nothing is pre-prepared.”



As a maternity hospital, there is a special atmosphere in the Coombe, which only gets better during the festive period.


“There’s always a great sense of excitement with all the new babies arriving. At Christmas, it’s an extra special time. Obviously, the hospital isn’t quite as busy because there are no elective surgeries but the wards are still full and the babies keep coming,” said Lisa.
“Everyone is in a great mood despite the fact that they are at work. The Christmas tree and the decorations are up and the place looks great. People are walking around with big smiles on their faces and bits of tinsel hanging o them. It really is a wonderful atmosphere.”
The catering team ‘cater’ to all tastes and diets and make sure to keep the patients involved.
“There are patients of all nationalities coming in so we have to make sure we have food that they would like to eat. The chefs like to make some lovely Indian
dishes and make it as spicy at the patients are used to.
“The patient is at the forefront of all we do here in the kitchen. We ask them what they would like and do our best to accommodate. And especially at Christmas we like them to have a meal that is special.
“We also have dishes specially prepared for people on a special diet such as coeliacs, diabetics, vegans, vegetarians or if they need halal food.”
The sta are treated superbly too with a full Irish breakfast ready for them.
Lisa’s children are teenagers now but her family still rises from their bed early to make sure they get to celebrate with her before she heads o for work.
“I am due in work at 7am so everyone gets up at 6am in the morning and we exchange presents then. I get a half hour with them. When I get home after 7pm, I get to put my feet up and have my meal handed to me. That’s one of the best parts of the day,” she added.
HEALTH MATTERS WINTER 2022 4 |
Seated - Glenda Sarsfield and Fiona Fletcher, Ward Catering Assistants; Standing - Jake Stapleton, Darylene Boyle, Debbie Ryan, Megan McLoughlin, DIning Room Catering Assistants; and LIsa Jones, Catering Supervisor.
HOLLYBROOK LODGE RESIDENTIAL UNIT IS A 50-BEDDED RESIDENTIAL UNIT SITUATED IN INCHICORE, DUBLIN 8. IT IS MANAGED BY MEDEL (MEDICINE FOR THE ELDERLY) DIRECTORATE, ST JAMES'S HOSPITAL. NOEL GORMAN (CEO) IS THE REGISTERED PROVIDER REPRESENTATIVE AND SHANAZ NASHEER IS THE PERSON IN CHARGE FOR HOLLYBROOK LODGE.
A lighting ceremony in early December heralds the start of the festive season in Hollybrook Lodge.
Fiona McAuley, Activity Coordinator in the residential unit, is responsible for making sure that Christmas is as special as it can be for all the residents.
Fiona’s role and responsibilities extend to addressing individual needs and wishes through person centred care.
“In my role I am very privileged to follow the interests of the residents. The residents and I have talked about the activities and outings they would like for Christmas and among other things, they expressed an interest in seeing the Christmas lights in town and in the Zoo. We will do our best to facilitate both these.
“Following on from these chats we have put together a great programme of musical events which I know the residents enjoy.



For example, Marina Cassidy and Roisin Hayes, Music Therapists in St James’s Hospital, are doing a concert for us - hearing Marina play the harp is the only event one of our residents will go to in the whole year.”
Fiona, originally from West Cavan but now living in Co Meath, has worked in the role for a number of years and joined the Hollybrook team just over a year ago.
She explained that paying attention to the individual wants and needs of each resident is key to providing a home away from home. This is particularly true at Christmas time.
“On Christmas morning everyone wakes up to a gift. They get dressed up and are ready for their traditional Christmas dinner or whatever the resident’s choice is. Brenda, our catering manager, works hard to try to get it right for everyone, and spends time with the residents finding out what they like. Many residents go home or residents can choose to eat together, in their rooms or family can come in and eat with them."
Hollybrook is very festive at Christmas - the sta love putting up decorations - the whole place is full of lights and Christmas trees. You will hear Christmas music playing all the time and all the favourite Christmas movies are shown. The Occupational Therapists and Physiotherapists run Christmas-themed groups in their Reminiscence and Sensory groups.
There are Christmas parties on the wards - and Fiona will organise a Christmas party too.


“Traditionally Christmas is our most important family time. This is when people make the biggest e ort to return home from all around the world. Everyone has a place at the table."
The importance of family can also mean that Christmas is a mixed bag for many - it is when we remember times past and those who are not with us anymore,” she said,




“We know to be sensitive to people too that everyone has their own way of doing Christmas and that we can’t match and meet everyone’s expectations. I think what matters more is that we pay attention and we act on what we hear - this is how we show that we care – when we are there for our residents in the kindest possible ways.”

| 5 HEALTH MATTERS WINTER 2022
‘We show we care when we pay attention and act on what we hear'
No let-up in 999 calls on Christmas Day
No two days are ever the same at work for Robbie Walsh, a call taker at the National Emergency Operations Centre in Tallaght, and he expects his first Christmas Day shift to be just as unpredictable.

Robbie and his NEOC colleagues handle all 999 calls that come in. Christmas Day, while seeing a reduction in some types of calls, will bring an increase in others.
“It is still a very busy day for us. You never know what kind of calls you are going to get but we do expect the same kind of calls to come in on Christmas Day. You have families getting together for the first time in a while. Throw in some alcohol and you might get some disagreements that turn violent,” he said.
“You would have people su ering with their mental health. It’s a great time of year for many but it brings a lot of sadness for others. Many people are alone and Christmas can heighten that sense of loneliness.”









He explained that often that voice at the end of the phoneline can be vital for people experiencing mental health di culties.
“While we aren’t a counselling service, we would stay on the line with people and talk to them until we can get an ambulance to them, once we don’t have another call waiting. We always send a crew out to a mental health call to check on them.”
It will be Robbie’s first Christmas Day on duty at NEOC. He may be missing out on his traditional family Christmas celebrations but the NEOC ‘family’ make sure those rostered enjoy much of the festivities.
“I’ll be in from 7am to 7pm so I will miss out on the exchange of presents. I don’t think I could get my five-year-old to wait that long for his presents. I’m lucky that I live close enough in Clondalkin so my commute isn’t long,” said Robbie.



“But here at the o ce everybody will bring in some part of the Christmas dinner for us – one will bring in the spuds, another the desserts, and somebody would look after the turkey or the vegetables, and so on. So we should have quite the Christmas feast to enjoy. Hopefully we will get a chance to take a break and eat it.
“Apart from that, there’s always a great atmosphere over Christmas. There’ll be plenty of Christmas jumpers on show and some sparkly earrings I’m sure.”


HUSTLE AND BUSTLE MAKES WAY FOR QUIET CALM

A quiet calm descends on most hospitals on Christmas Day as it empties of the usual bustle of sta and visitors.
For John Kelly, the director of pastoral care at Tallaght Hospital, it is a profound experience to witness the generosity of spirit all around.

“It’s always such a special time here. There is so much activity in the hospital in the weeks leading up to Christmas, it is all hustle and bustle, and then it becomes so quiet. It is quite profound to see the calmness all around,” he said.
“The sta give of themselves fully over Christmas. No doubt everyone would sooner be at home with their families but sta do really extraordinary things to make the experience more meaningful for patients You see them going around with their flashing earrings or adding a bit of colour to their uniform, simple things to brighten up the day.
“We have so many sta here who are far away from home on Christmas Day, coming here from overseas. It is di icult for them but they give totally of themselves. They are mainly younger people and they bring a great energy and are very positive.”
John spends the day visiting patients at their bedsides and having a chat with them.
“Some patients prefer to have quiet time on the day, others want to celebrate the spirit of the day. Of course, people are still sick and many die on Christmas Day and that is very di icult in itself. There is so much emotion for people when their loved one are sick and in hospital at this time of year,” he said.
“My experience is that often the photographs that you take on Christmas Day are the last ones that you ever have together with your loved one. It is the day that you make time to take those special photographs. One family I remember was in and had a lovely photograph of their granny taken in front of the hospital Christmas tree and she passed away soon after. They will have that photograph forever to look back on.”
HEALTH MATTERS WINTER 2022 6 |
From Boston to Irish midlands for doctor Aoife
Laois isn’t the first port of call you think about when you are coming from Boston, but Aoife Raja is delighted to have joined the team at the Midlands Regional Hospital in Portlaoise and readying herself for her first Christmas in Ireland.
Aoife, a Senior House O icer (SHO) in the Medical Department of the hospital, said she is actually looking forward to her Christmas Day shift and insists that the holidays are an opportunity rather than a disadvantage.
“Christmas time is a lovely. It’s a very inclusive holiday. But it is also an extremely lonely time for a lot of people and I think doctors have a part to play in making a di erence. It is an opportunity for us to really be able to help. I am good at talking to people and listening so I think it will be great to have some time with the patients that need someone to talk to,” said Aoife.
“You know that if somebody is in a hospital over Christmas there really must be something wrong. It is a very lonely time and often our patients need more than just medicine. Between Christmas and New Year we see a lot of elderly patients ending up in hospital. I think it’s a privilege to have a chance to be there for them.”
Aoife came to Ireland from her native United States eight
months ago. Her unusual choice of destination was guided largely by the fact that her dad is a GP in Portlaoise.
“I have been in and out of Ireland for the past 30 years because my dad was living here. And, of course, it is great to be somewhere that everyone can pronounce my name,” she said.
Aoife said she is lucky to have been part of two brilliant teams since she arrived in Co Laois.
“I started o in paediatrics and joined such a great team. I loved it. In terms of community and support, they couldn’t have been any better. Then I made the transition to the medical team and am so lucky that I got another great team. They are all so supportive, not just when it comes to patient care, but in an all-round way, helping and co-operating with each other,” she said.

She said that she has no doubts that Christmas Day will be celebrated widely across the hospital.
“It is pretty festive in Ireland so I’m pretty sure that we will be able to feel the vibe of the holiday even when we are working. I’m really looking forward to it,” she said.



it’s hard, because my family don’t get the time to show o their happiness of having me around. Likewise I don’t get to celebrate this with them, my sons don’t get to celebrate and enjoy the fun of opening their presents with me there. My wife has to do all of this on her own,” he said.
“We are a family that enjoys large celebrations and having our family around is important. Both my wife and I are frontline workers. Melissa is in the gardaí and at times works shift, so we endeavour to spend as much time on occasions like Christmas together as a family.”
Working on Christmas Day can be quite a regular occurrence for emergency sta .
Greg Lyons knows that there won’t be a spare minute to celebrate during his Christmas Day shift as a paramedic but he and his colleagues at the National Ambulance Service will still go that extra mile to bring a bit of festive cheer to their patients.
“We are generally a jovial bunch of sta , unique for sure, so our personalities helps cheer up all our patients and their families that we encounter on the day,” explained the Swords man.
“On the build-up to Christmas, some of my colleagues are brilliant with getting into the spirit. Most patients we encounter are just happy that we are with them, and a lot express their thanks and gratitude knowing we are with them and away from our own families on this special day.”
Greg admits that it is very tough having to forego the traditional Christmas Day with his family. His wife Melissa is a detective garda sergeant so the two are used to having to work on special holidays. But they make sure that they make the most of every minute together as a family.
“If you ask my wife, she might say it’s easier without me, but I know
“It all depends on where you are stationed and what way the roster falls," he said.
Christmas Day is always a very busy day for the ambulance service. Greg said that while work-related accidents reduce, there are lots of homebased accidents, falls, motor vehicle-related incident and also some Christmas-related calls.



It means that there isn’t much time to sit down with colleagues and celebrate the day.
“With current demands no day is a slow day. I would expect all crews will be out the door as soon as they sign on with our colleagues in the National Emergency Operations Centre,” he said.
Greg, who joined the National Ambulance Service in 2013, paid tribute to his colleagues who, he said, makes the job so enjoyable.
“The best part of the job is meeting some of the kindest and most genuine people in the course of my duties, followed by working with some of the most dedicated people, who put their heart and soul into what the day might bring them, shift in, shift out, sometimes at the cost of their own personal commitments.”

| 7 HEALTH MATTERS WINTER 2022
‘MOST PATIENTS ARE JUST HAPPY THAT WE ARE WITH THEM’
MINISTER BREAKS GROUND ON NEW 96-BED BLOCK FOR UHL

WORK has commenced on the new 96-Bed Block at University Hospital Limerick, the next step in increasing acute bed capacity in the Mid West.
Speaking in Limerick as he broke ground on this important development, Minister for Health Stephen Donnelly said, “This new, state of the art extension represents a significant and much needed development for University Hospital Limerick and, more importantly, for the people of Limerick and the Mid-West. It also again underlines this Government’s commitment to investing in modern, fitfor-purpose infrastructure that is critically important for the delivery of high quality, safe care across our health service.”
Construction will take at least two years to complete and the new facility will then have to be equipped and commissioned before opening to patients. The project represents a total capital investment of in excess of €90 million.
The new 9,800 square-metre block will be built over the existing Emergency Department and Dialysis Unit and will consist of 96 en-suite single rooms over four floors. Approximately half of the beds will be new beds for inpatients while the remainder will be replacement beds allowing the hospital to close or refurbish some of the more outdated inpatient accommodation on the site. This will allow for greater compliance with national guidelines and international best practice on infection prevention and control.
During his visit to UHL, Minister Donnelly also officially opened a number of new developments that have recently opened at UHL and which have improved the patient experience and work environment.
These included the new 60-bed block, and the new 24-bed Ward 6B for haematology and oncology patients.
Children’s therapy services centre in Cashel launched


New chapters in the history, both of the St Patrick’s Hospital building and provision of disability services locally, were marked in Cashel recently when Chief Officer of HSE/South East Community Healthcare Kate Killen White visited the new Cnoc na Rí facility.
Cnoc na Rí has been developed as a children’s therapy services centre in specialist renovation works, conducted on parts of the main St. Patrick’s Hospital building left vacant following the transfer of its long stay older persons care residents to the nearby Our Lady’s Hospital building on the Cashel Health Complex in the summer of 2020.
An Assessment/Rehabilitation unit and a Day Hospital remain on site at St. Patrick’s. The more modern accommodation for long stay older persons’ care prepared at Our Lady’s was identified at the time in 2020 and going forward as safer in terms of infection control.
Cnoc na Rí will be the centre for the recently established Children’s Disability Network Team (CDNT) serving Cashel, Tipperary Town and surrounding areas.
Members of CDNTs work closely together to provide a wide range of services and supports for a child and their family. As part of its work, parents and other family members learn how to support their child’s development and can share their experiences with others. As each child and family has different needs, so too will they have their own individual plan.
Joining the Chief Officer in speaking at an occasion to mark the coming into operation of Cnoc na Rí were Mary Nugent, Project Co-ordinator for this refurbishment during her time as Acting CDNM Manager; Aoife Sweeney, Children’s Disability Network Manager/ CDNM; Ciarán Ruane, Estates Manager, HSE/South East; and Margaret Foley, Assistant Director of Nursing, SECH.

HEALTH MATTERS WINTER 2022 8 |
Minister for Health Stephen Donnelly and John Hanafin, chairman of the UL Hospitals Patient Council (front, centre), with (from left) Rozalind Murphy, O’Connell Mahon Architects; Prof Colette Cowan, CEO UL Hospitals Group; Marcus Carne, Managing Director, Sisk; and Joe Hoare, Assistant National Director, HSE Capital & Estates. Photo: Don Moloney
FIRST CRAFT FAIR TAKES PLACE AT CLARKE'S PLACE, MOVILLE
DONATION OF FAMILY HOME FOR FOUR RESIDENTS WITH INTELLECTUAL DISABILITIES
Minister for Disabilities Anne Rabbitte officially opened a four-bedroom detached house in Glenageary, South Co Dublin that will serve as a permanent home for four residents with intellectual disabilities.

The house was generously donated by the parents of one of the occupants, Teresa O'Hara and her late husband Tom, to the Department of Housing and the HSE. The newly refurbished house in Glenageary is funded from the National Service Plan 2021 Development Fund and will be operated by St. John of God Community Services. It will enable independent living, improved quality of life and easier access to the community for the residents living there.
Staff at Midland Regional Hospital Portlaoise (MRHP) are delighted to have been gifted a new ‘ound Ear monitor for their Special Care Baby Unit. The donation was made by the charity, Bikers Ride Out for Prems. Many of those involved in the group have had or were closely related to babies who needed specialist care, just after birth.
The new high-tech Sound Ear monitor (see pic) allows staff and parents to gauge their noise levels when they are in the Special Care Baby Unit (SCBU). It was accepted on behalf of the hospital by Claire Julian, the Nursing Site Manager on duty when the Bikers arrived at MRHP.
Yolanda Fennel, the Clinical Nurse Manager who runs the Special Care Baby Unit at MRHP, explained, “The Sound Ear monitor, which is actually in the shape of an ear, will be mounted

onto a wall. It measures decibels and lights up and flashes orange to remind parents or staff to be quiet, indicating that the room is getting too noisy. Reducing noise levels helps premature babies in terms of their brain and overall development. This is a fantastic donation from the charity Bikers Ride out for Prems.”
Ita Kinsella, Director of Midwifery at MRHP, said, “This equipment is a significant resource which we can use to monitor the recommended noise threshold for babies in the Special Care Baby Unit, particularly during medical rounds and at peak visiting times. I would like to thank the charity for its ongoing continuous fundraising efforts and support for the SCBU. It is very much appreciated and positively impacts the service provided to babies in the unit.”
The first craft fair has taken place at the Moville Residential Group Home, Clarke's Place. Ingredients for the produce were grown by the residents and with great care made into delicious produce and proudly put on display. Produce such as beetroot, jams, chutney and cordials were available to visitors to the centre. There were also vegetable stalls and wood crafts on offer.
There was more than just these delights to see on the day. There was an amazing Birds of Prey show and some home baking
available to the visitors. It was a very successful day for the residents and for staff who supported them.
When one resident was asked how they felt about people coming to view their gardens and to see their house, they said, “We really enjoyed people coming to our house and gardens and everyone saying how lovely it was. “ Another resident said, “We felt proud.”
Martin McNamee, manager of Moville Residential Group Home said, “It was a really good event and it was great to see
the self-confidence, self-esteem and pride in the residents as they engaged with the people who visited and explained all aspects of the facility and items on sale to them.”
Anita Gallagher, Disability Manager added, “As a service we are very proud of the resident’s work, supported by the staff, in Moville community home. The proactive way that the residents took on a challenge, engage with the community and enhance the lives of all they meet is an inspiration to us all.”
| 9 HEALTH MATTERS WINTER 2022
Special Care Baby Unit receives an important new piece of equipment
Ryan O'Hare cuts the ribbon at his house, with Stephen O'Connor, Michelle Thunder, CEO of the SJOG Housing Association, Ryan's mother, Teresa, and Minister Anne Rabbitte. Photo courtesy of the Irish Times
IEHG CORPORATE TEAM MEMBERS FUNDRAISE FOR BARRETSTOWN
Ireland East Hospital Group Corporate

Team members Asta, Mick, Jennie, Ciara, Noirin and Muireann were delighted to participate in the Domino Amazing Race fundraising challenge for Barretstown Children's Camp in September.

Team Iconic (as they named themselves) thoroughly enjoyed the fun activities and challenges involved and fundraising for such a worthy cause. Their supporters ensured they raised 202% above target and a grand total of €1,215!
Team Iconic would like to sincerely thank all their colleagues, family and friends for all their donations and support.
OFFICIAL OPENING OF NEW CAPPAGH CHILDREN’S OUTPATIENT DEPARTMENT

The National Orthopaedic Hospital Cappagh (NOHC) o cially opened a dedicated Paediatric outpatient department to assist Children’s Health Ireland (CHI) in dealing with increasing numbers of patients waiting for orthopaedic appointments and post-surgery reviews. The new and bright child-friendly department is a welcoming and inviting space for our ‘Cappagh Kids’. The unit was opened by the children of Ireland for the children of Ireland.
Angela Lee, CEO of the National Orthopaedic Hospital Cappagh, said, “It was a very exciting day for us, as we opened our new Cappagh Kids Outpatients Department. We recognise how di cult attending hospital is for children and their parents, and we want to do everything we can to make their experience as pleasant and manageable as possible.”
Surgeons at Cappagh Kids work across NOHC and CHI Temple Street; therefore seeing patients in Cappagh Kids for pre-op and post-op appointments frees up capacity in Temple Street to deal with other conditions.
In the past year there were 1,018 paediatric outpatient attendances at the hospital, a significant increase on the previous year.
The unit, which sees patients from aged two years upwards, has recruited a number of specialist-trained paediatric nurses and allied health professionals to cater to increased patient numbers.
The new Cappagh Kids facility includes consultation rooms, a staging area, a therapy gym, a MDT conference room as well as waiting areas and o ce space.
EXPANDED VASECTOMY SERVICE LAUNCHES IN COMMUNITY HEALTHCARE EAST
Following the recent retirement of the General Medical Services (GMS) vasectomist in Community Healthcare East, they are pleased to announce that they have reached agreement with two GP Vasectomists to continue service provision for GMS patients in the area.
The two clinics will o er free access to a permanent contraceptive solution for men who hold a GMS/GP card. The service includes an initial consultation with the vasectomist as well as a post procedure consultation and semen analysis.

O ering a community-led Vasectomy service reduces the need for vasectomies to be carried out in a hospital setting leading to reduced waiting times. Referrals can be made directly through a local GP and through the Healthlink referral system.

HEALTH MATTERS WINTER 2022 10 |
Asta, Mick, Jennie, Ciara, Noirin and Muireann.
Ministers Anne Rabbitte and Roderic O’Gorman TD with some of the children at the new Outpatient Department.
Some
Mental health nursing strategy launched
Galway Roscommon Mental Health Nursing Services Strategy (2022-2023); Leading the way forward: Advancing a professional co-produced recovery service has been launched.

This is the first co-produced mental health nursing services strategy and is informed by the views and opinions of nursing services staff and individuals who avail of the service. It is an important document as it provides a template for the future direction of the nursing services in Galway/Roscommon Mental Health Services.
The five-year strategy is underpinned by the five strategic priorities:
• Person-centred care
• Professional practice
• Continuous service improvement
• Planning and developing our workforce; and
• Staff health, wellbeing and resilience.
Each of the strategic priorities have statements and indicators which will be prioritised for implementation over the next five years.
Speaking at the launch of the Nursing Services Strategy, Helen Earley, Area Director of Nursing, said, “Our vision is that Galway/ Roscommon Mental Health Services will stand out among those that lead Mental Health Nursing Service into the future, clearly demonstrating how it can be done, as working together we achieve much more. We launch our strategy at a time of unprecedented challenge in the HSE and within Mental Health Services. We have been proactive in responding to these challenges and delivering care in new and innovative ways.
“Through the implementation of our strategy, our staff will feel supported, valued, and remain committed to working in Galway/ Roscommon Mental Health Services and view it as the employer of choice. Above all, they will take pride in the outstanding contribution they make in providing the highest possible quality care for the individuals who use our services.”
Following the launch, the Nursing Services Strategy Steering Committee were replaced with the Nursing Services Strategy implementation steering group.
NEW INTENSIVE CARE WING PROVIDES ACCESS TO THE MOST VULNERABLE PATIENTS

Tallaght University Hospital hosted a visit by Minister for Health Stephen Donnelly as he officially opened the hospital’s new 1,750 m2 Intensive Care Wing. The expanded space on the first floor of the hospital has 12 ICU beds, each of which are in a single room. The additional beds which provide care to the most critically ill patients are located across two zones, each with their own central nursing station.
The new ICU expansion represents a major service development for TUH and the Dublin Midlands Hospital Group (DMHG). The Critical Care Area in TUH caters for a catchment area of 650,000 people and prior to the opening comprised of nine Intensive Care Unit (ICU) beds, five Post Anaesthesia Critical Care Unit (PACCU) beds, which manage elective and emergency postoperative patients, and two High Dependency Unit (HDU) beds located in the coronary care unit. The additional beds will enable the hospital to continue to provide high-quality medical care to the

increasing numbers of critically ill patients.
Lucy Nugent, Chief Executive of TUH, said, “The opening of our new ICU extension is part of the hospital’s strategy to improve infrastructure with the priority of improving access for our most vulnerable patients and prepare the hospital for the increasing demands of serving a rapidly growing population.”
The additional beds will be supported by 146 whole time equivalent staff made up of nursing, consultant intensivists, registrars and Health & Social Care Professionals. The
recruitment for medical staff is completed, the recruitment of the additional Health & Social Care professionals are at the final stages of recruitment. Nursing recruitment is ongoing with 50 posts filled and the remaining staff being in place by January / February 2022. The existing ICU in TUH which is 24 years old will be refurbished between SeptemberDecember, the additional bed capacity will increase steadily from 12 to 21 beds from January onwards upon completion of the refurbishment programme.
| 11 HEALTH MATTERS WINTER 2022
members of the Galway/Roscommon Mental Health Nursing Services Strategy Steering Group.
Left: Professor Anne Marie Brady, Deputy Chairman of the TUH Board; Lucy Nugent, CEO of TUH; Minister for Health Stephen Donnelly TD and Maria Donnelly, Consultant Intensivist and Declan Daly, Chair of the TUH Patient Community Advisory Council Right: Clinical Facilitator at TUH ICU Shauna Delaney, Minister for Health Stephen Donnelly TD, Professor Peter Lavin, Consultant Nephrologist & Lead Clinical Director
LAURA'S MEMORY LIVES ON
HPV catch-up programme a ‘testament to Laura’s dedication’
The launch of the Laura Brennan HPV Vaccine Catch-Up Programme is ‘a comfort and a testament to Laura’s dedication to increasing the uptake of the HPV vaccine’, according to her family.

The programme, which will launch in early December 2022, will o er free HPV vaccines to all boys and girls in second level education who were previously eligible to receive the HPV vaccine and who have not yet, for whatever reason, received it.
Young women, up to the age of 25, who have now left secondary school, and who did not receive the vaccine, will also be eligible to receive the vaccine as part of the catch-up programme. The vaccine will be administered in clinics. The vaccine is administered as a single dose and is free of charge.
Mum Bernie Brennan said, “September just gone would have been Laura’s 30th birthday. The reality of living with cancer, and then life after cancer when someone passes away means that we miss out on milestone celebrations with our loved ones. To see the HPV Catch-Up Programme named in Laura’s memory is a comfort and a testament to Laura’s dedication to increasing the uptake of the HPV vaccine. I urge all parents to discuss HPV vaccination with their children and encourage them to take it – vaccines prevent cancer. Prevention is better than cure and prevention is definitely better than no cure.”
Dad Larry added, “It is lovely to see the HPV Catch-Up programme named after Laura. It is so important that this vaccine will be available free of charge and easily accessed for those who missed out on it in school, I hope this move increases uptake across the country. I would urge anyone who has any question about HPV vaccines to get your information from trusted sources like the HSE and the WHO. Increasing uptake of the HPV vaccine will protect women and stop them getting cervical cancer.”
Minister for Health Stephen Donnelly said, “Laura Brennan is the epitome of inspiration for all of us. Even when faced with a terminal diagnosis, Laura dedicated herself to promoting the HPV vaccine to ensure that as few families as possible would have to go through the rigours of cancer treatment and end-of-life care as she did.
“The Laura Brennan HPV Vaccine programme is a fitting tribute to the memory and the tireless e orts Laura made to encourage young people to take up this vaccine. Vaccines save lives and, through screening and vaccination, we are working to eliminate cervical cancer in Ireland – I really cannot think of a better way to remember Laura than achieving this goal through the programme named after her.”
HEALTH MATTERS WINTER 2022 12 |
Why is HPV vaccine important?
HPV virus causes 1 in 20 cancers worldwide.
The HPV vaccine protects against the types of HPV that cause 9 out of 10 cervical cancers.
A study published in November 2021 from England observed a substantial reduction in cervical cancer and incidence of severe cervical abnormality caused by HPV infection (CIN3) in young women after the introduction of the HPV immunisation programme in England, especially in individuals who were o ered the vaccine at age 12–13 years.
The study advises “the HPV immunisation programme has successfully almost eliminated cervical cancer in women born since September 1st 1995.”
In countries where the HPV vaccine is used, the number of cases of genital warts has decreased dramatically in both young women and men.
What HPV vaccine is used in Ireland?
The HPV vaccine used in Ireland is called Gardasil 9. It is produced by MSD Ireland (Human Health).
When did Ireland begin o ering HPV vaccine?
In line with Department of Health
Immunisation Policy, the HSE has had a school based immunisation programme since 2010.
When the programme was first implemented it was for females only, in 2019 immunisation policy was updated.
The HPV vaccine is now available each academic year to boys and girls in first year of second level school.
Over 500,000 people have completed their course of vaccination across Ireland.
Who is eligible for HPV vaccine?
The HSE vaccination programme is available to: School Programme
All students in first year of second level school are eligible to receive the HPV, Tdap and MenACWY vaccines through the HSE school immunisation programme.
Evidence shows that uptake of vaccines is much higher when vaccines are provided within the school setting and it provides equitable access across the population. The full support of all education settings has been vital for the success of the programme and is aiding Ireland to progress towards elimination.

Laura Brennan Catch up Programme
The HPV (Human Papillomavirus) catch-up vaccination is being o ered to:
• Females (2nd year – 6th year) who have not received the HPV vaccine
• Males (2nd year – 4th year/5th year if
they did not do transition year) who have not received the HPV vaccine
• Females who have completed second level school and are 24 years of age and younger
How many doses of HPV vaccine are needed for protection?
The National Immunisation Advisory Committee (NIAC) has recently issued updated advice about the number of doses of HPV vaccine needed.
NIAC now recommend:
• One dose of HPV vaccine for people aged 9-24 years of age.
• Three doses of HPV vaccine for people who are immunocompromised (weak immune system)
Why has the advice changed about the number of doses of HPV vaccine needed?
The NIAC changed their advice about the number of HPV vaccine doses needed because of recent scientific evidence. This evidence shows that in people aged up to 25 years old with healthy immune systems, there is no major di erence in the e ectiveness of the vaccine between people who get one, two or three doses of HPV vaccine.
Where can I find information about HPV vaccine?
Visit www.hpv.ie
| 13 HEALTH MATTERS WINTER 2022
“It is lovely to see the HPV Catch-Up programme named after Laura. It is so important that this vaccine will be available free of charge and easily accessed for those who missed out on it in school, I hope this move increases uptake across the country.”
GIVING IT THEIR BEST SHOT
Flu Champions on achieving highest health and care worker flu vaccine uptake
During the 2021/2022 flu season 15 long-term care facilities achieved 100% health and care worker influenza vaccine uptake.They took the top prize for the highest flu vaccine uptake among health and care workers in a long-term care facility (less than 100 patients) at this year’s Seasonal Influenza Vaccination awards organised by the HSE National Immunisation O ce. This is the largest number of long-term care facilities that have ever won in this category to date.
We spoke to Flu Champions from three of the winning facilities about their vaccination drive last flu season and the importance of healthcare worker vaccination: Amanda McCall, Clinical Nurse Manager at Manderely Lodge; Noeleen Cahill, Managing Director of Atlanta Nursing Home; and Emma Kiernan, Clinical Nurse Manager at Arus Bre ni Nursing Unit.
“It really came down to the compassion of our sta ,” said Amanda from Manderely Lodge, “they were committed to the protection of our residents and our services.” Manderely Lodge not only achieved 100% flu vaccine uptake among sta but also achieved the best improvement in health and care worker uptake for a long-term care facility (less than 100 patients). “Education was really central to our campaign –sta understood that they were not only protecting themselves getting vaccinated but also residents, and their own families,” said Amanda.
“Many of our health and care sta also live with or look after their elderly relatives. They don’t want to catch flu, spread it or bring it home,” said Emma Kiernan, Clinical Nursing Manager at Arus Bre ni Nursing Unit. Arus Bre ni Nursing Unit also achieved 2nd best improvement in healthcare worker uptake for a long term care facility (less than 100 patients). “We set up clinics early on and we got good feedback from sta . Our clinics operated flexible times and we also worked closely with a local pharmacy where a lot of our sta got vaccinated. People wanted to get it to protect the people they care for,” added Emma.

Health and care workers are up to 10 times more likely to catch flu, and 1 in 5 healthcare workers develop flu each season. Because the flu virus is transmissible before symptoms develop, this increases the risk of healthcare workers spreading the virus to patients, colleagues and their families.
By getting vaccinated, health and care workers can help prevent the spread of flu and protect those most vulnerable. Older people and at-risk patients may not get su cient protection from the flu vaccine themselves so they rely on healthcare workers to get vaccinated to keep them safe. “It was important we educated sta on how highly infectious flu can be and how there is a real risk of spreading it to residents. Some sta can also be very sick with flu and have to miss work, and they may also spread it to their co-workers.”
Arus Bre ni also saw the impact of sta vaccination with reduced incidences of flu-related illness, “we had less sta calling in sick with flu,” noted Emma.
Flu vaccination of health and care workers can result in an up to 40% reduction in flu-related patient deaths. In Europe, high health and care worker uptake rates have also been shown to lead to reduced rates of sick leave in health and care workers.
When Atlanta Nursing Home experienced an outbreak last season they responded swiftly with a ramp up in education and communications, explained Noeleen Cahill, Managing Director of Atlanta Nursing Home. “We produced weekly newsletters at first and then ramped that up to a daily issue when we had an outbreak. We gave clear, precise and sensitive information to everyone on the team, and this led to a high degree of trust between us”, said Noeleen. “This was a key component in ensuring that when the time came to get influenza vaccinations our residents and sta were fully informed of the benefits of vaccination and trusted vaccination to lead the fight in keeping influenza out of Atlanta.”
FLU CHAMPIONS’ TOP TIPS FOR IMPROVING FLU VACCINE UPTAKE IN HEALTH AND CARE WORKERS
• Communicate regularly with sta e.g. sta meetings, newsletters



• Accommodate sta e.g. flexible clinic times, consider linking in with local pharmacies giving flu vaccines
• Remind sta on how and where they can get vaccinated
• Educate sta and direct them to trusted information sources e.g. HSeLanD e-learning programmes, HSE website
Health and care workers can save lives and prevent the spread of flu by getting vaccinated. The flu vaccine is the best way to protect yourself, patients, colleagues and families from flu this winter.
If you work in health and care, you can get your free flu vaccine at a local peer vaccinator clinic, GP or pharmacy. Visit hse.ie/flu for more information.
HEALTH MATTERS WINTER 2022 14 |
THE BEST WAY TO PROTECT CHILDREN FROM FLU THIS WINTER
The nasal spray flu vaccine is the safest, most effective way to protect children and the rest of the family from flu this winter
As we head into winter, it is more important than ever that children are protected from flu. Flu can be dangerous in children, especially those younger, and the nasal spray flu vaccine will give children the best protection from flu, says Dr Aparna Keegan, Specialist in Public Health Medicine, at the HSE National Immunisation O ice. The flu vaccine will also help protect others, like siblings, parents, grandparents and those who are vulnerable.
All children aged 2 to 17 years can get the free nasal spray flu vaccine from participating GPs and retail pharmacies.
CHILDREN ARE TWICE AS LIKELY TO CATCH FLU AS ADULTS
“Flu is highly infectious, and anyone can catch the virus. However, we know that children are twice as likely to catch flu as adults and can be very sick with flu. Younger children, in particular, are at an increased risk of serious illness.”
While most children who catch flu have mild symptoms, flu can sometimes lead to serious problems such as pneumonia or bronchitis in some children. Children, especially younger children, are also more likely than adults to develop severe complications of flu.
Common symptoms of flu in children include high temperature, muscle pains, headache and fatigue.
APPROXIMATELY 1 IN 10 CHILDREN UNDER 15 ATTEND THEIR GP WITH FLU-LIKE ILLNESS IN A TYPICAL FLU SEASON.
“We tend to see the highest incidence rates in the younger age groups – this can often mean an increased pressure on our healthcare services. Approximately 1 in 10 children under 15 attend their GP with flulike illness in a typical flu season.”
Flu can cause serious illness in children. In the last 10 years in Ireland almost 5,000 children were admitted to hospital with complications of flu, almost 200 children had treatment in intensive care and 40 children died.
“Children and young people with long term health conditions are most at risk of the severe complications from flu and needing hospital treatment.”

CHILDREN SICK WITH FLU CAN MISS OUT
“Children who are sick with flu, even with mild symptoms, can miss days in crèche, childcare and school. They can also miss out on their usual activities such as hobbies and sports,” said Dr Keegan.
Children can catch and spread flu easily. Children can also carry the flu virus in their system longer than adults do. This means they can spread it easily to other children, like those in day-care centres and schools, and to older and vulnerable family members and people around them.
“Your child’s free nasal flu vaccine is













the best, most e ective way to prevent them from getting very sick from flu and help prevent the spread of the virus to others too”.
SAFE, EASY AND PAIN FREE
Getting the nasal spray flu vaccine is a safe, easy and a pain free way to protect your child from flu this winter. The GP or pharmacist will give the nasal flu vaccine by spraying it once into each of the child’s nostrils.
“The nasal spray flu vaccine is a very safe, e ective vaccine and helps your child’s immune system produce antibodies that fight infection. It cannot give your child the flu. If your child has had the flu vaccine and they come into contact with flu virus, these antibodies will help them fight the flu and reduce the risk of them getting sick or needing to go to hospital.”
“Other countries, including the UK, have been o ering flu vaccine to children for many years. Not only will the flu vaccine help protect your child against flu, it will also help protect more vulnerable family members. It is important that we all do what we can to avoid serious illness and hospitalisation this winter,” said Dr Keegan.
The nasal spray flu vaccine is the best way to protect your child and others from flu this winter.
Contact your GP or pharmacist today. Use the pharmacy finder on hse.ie/flu to find a pharmacy giving flu vaccines for your child’s free nasal flu vaccine.
For more information, you can also visit hse.ie/flu.

| 15 HEALTH MATTERS WINTER 2022
Rose Room
Anew room for bereaved families at Mayo University Hospital (MUH) Maternity Unit has been named the Rose Room in memory of baby Hope Rose Caulfield who sadly died in 2017 aged nine days old.

Hope Rose’s parents Sandra and Jonathan Caulfield from Kiltimagh have fundraised significantly for the renovation of this space which will support the hospital in providing comfort and solace to families dealing with loss. The Caulfield family have turned their personal experience of bereavement into an opportunity to help other grieving families by fundraising and supporting the hospital in providing a dedicated quiet space for bereaved families.
Sandra Caulfield said, “With great love comes great sadness and Hope Rose was one of my greatest loves. I will hold her forever in my heart until I hold her in my arms.”
Andrea McGrail, MUH Director of Midwifery, said, “On behalf of Mayo University Hospital I want to thank Sandra and Jonathan for their commitment to this project; for their fundraising and for engaging with the hospital so passionately to make the Rose Room such a beautiful place. It is a calm and quiet room, with a wonderful painted mural which depicts children releasing lanterns on a beach, evoking light and hope, and the forever bond of siblings.
“Unfortunately in the Maternity Unit, some families will experience pregnancy or infant loss and it is so important to have a quiet and comforting place in which families can prepare for the di cult journey they are on.
“We also want to say a huge thank you to the community of Mayo and further afield, who have contributed to the various fundraising initiatives to renovate the Rose Room.
“We wish to also acknowledge the incredible commitment our sta have shown to this project.”
EMPLOYEE ASSISTANCE PROGRAMME (EAP) – HEALTHCARE WORKERS AND GRIEF
Healthcare workers care for others. Looking after yourself, especially after losing someone close to you, is the self-care many forget.
Similarly, focusing on work can be very di icult after the death of a work friend or team member.
It takes time to readjust to the workplace without them. Grief is di erent for everyone. Acknowledge your feelings and reach out for support if you need to.
Working with the Irish Hospice Foundation and a range of partners, the HSE is promoting supports and services for healthcare workers who may be grieving, responding to loss or supporting those bereaved.
HSE sta can call the HSE Employee Assistance Programme (EAP) on 0818 327 327 to speak to someone who can help. This is a free and confidential service.
There is also new dedicated content at www.hse.ie/grief/ healthcare to increase knowledge about grief, bereavement and supports.
HEALTH MATTERS WINTER 2022 16 |
Bereaved families have space to grieve in newly opened room
Jonathan, Ava, Chloe, Sandra and Faith Caulfield in the Rose Room named in memory of their daughter and sister, Hope Rose.
Winning Midwife
Mairead donates prize money to fund resumption of water births
Senior midwife Mairead Martin, from Our Lady of Lourdes Hospital in Drogheda, has been awarded a €10,000 bursary to advance the care of expectant and new parents and their babies.
Mairead, who has cared for thousands of women and families over her lengthy career, was this year’s WaterWipes Pure Foundation Fund Ireland winner.
Having worked as a midwife for now 32 years, Mairead’s colleague Rachel Gallagher nominated Mairead for her outstanding care given to women and families across Drogheda. Commenting on her nomination, Rachel said, “To me; Mairead is the true meaning of a midwife. Mairead has an infectious personality, so you can't help but be drawn to her warm and caring nature. Mairead is heavily involved in providing education to women and families, and leads the way in all aspects of antenatal education, birth preparation, breastfeeding, and postnatal care.”
When asked how she felt about being nominated for this year’s Pure Foundation Fund, Mairead said “I was absolutely thrilled about the award, and humbled by the fact that not only Rachel, but so many other of my Midwifery and Healthcare Assistant colleagues had done so as well. The staff of the Midwife Led Unit, Our Lady of Lourdes Hospital, Drogheda, are an amazing team of midwives, healthcare assistants, and student midwives who go above and beyond every single day to provide the best care to women and their babies during the antenatal, intrapartum, and postnatal period.”
Mairead will be donating her prize money to fund a resumption of water births, in appropriate circumstances, in the Labour ward at Our Lady of Lourdes Hospital. She also plans to help fund essential training for midwives, to enhance the quality and scope of the care that they already give to women attending for the antenatal, intrapartum and postnatal continuum.
Alongside the overall Ireland winner
Mairead Martin, WaterWipes, INHA and INMO also recognised four runners-up for their amazing work and achievements.
Public health nurse Eimear Close was nominated by a colleague for being “an amazing nurse who goes above and beyond for all her clients. She currently works in a very underprivileged area working with the homeless and travelling community. If you asked any of her clients what she is like they will always sing her praise.”
Stephanie Hayes, a midwife at St Luke’s General Hospital, Kilkenny, was nominated by a colleague for going “above and beyond every single day to care for, guide, prepare, support, encourage, teach & empower women through their pregnancies, labour and postnatal journeys.”
Neonatal professional Karen Prunty works on the frontline with new babies and parents who require hospitalisation after they are born and was nominated by a colleague for her hard work in “making this as stress free as possible in a worrying situation”.

| 17 HEALTH MATTERS WINTER 2022
A day in the life of Disability Case Manager Ronan Halpenny

Ronan Halpenny still gets goosepimples as he recalls the time he informed a man, who had been in a nursing home for 17 years, who didn’t communicate verbally, and was a similar age to himself, that he was finally going to be given a house that he could call home. “It was definitely one of the highlights of my career,” he says, reflecting on a career in the Disability and Social Care Sector which has now spanned almost 20 years with the past two as a Disability Case Manager in CHO DNCC.
Based in the Nexus Building in Ballycoolin, Dublin 15, he handles cases in the North West region of CHO DNCC. The work of a Disability Case Manager is varied, challenging, and involves a lot of moving parts.
“As a Case Manger I’m involved in providing services to both adults and children with disabilities. We commission the services that people need from our o ce and ensure that they are receiving the care they need and in a timely fashion. In doing that, there is a huge amount of contact with the service user, their family members, the service providers, agencies within the HSE and external agencies,” says Ronan.
“Basically any person who has a disability is our responsibility. It involves a lot of problem solving, a lot of sign posting, making sure people are linked up with the right services – an awful lot of moving parts”
Ronan’s first foray into the Disability and Healthcare Sector was 17,000km away in Sydney, Australia where he worked as a Care Assistant in a Disability Service. On his return to Ireland in 2002 he had found his calling and pursued this by obtaining a Certificate in Counselling, Psychotherapy & Psychoanalysis and followed this up by completing a Bachelor of Arts (BA) in Social Care Practice.
Since returning from Down Under and continuing his education, Ronan has held a number of frontline and leadership roles within many of the organisations with which he now engages on behalf of CHO DNCC. Initially as a social care worker in Sunbeam House in Bray, Co. Wicklow, he then went on to hold leadership roles in Clann Mór Residential and Respite, Peamount Healthcare, The National Advocacy Service for People with Disabilities, Stewarts Care and more recently with St Michael’s House. It was in 2020 that Ronan joined CHO DNCC bringing with him a wealth of experience.
Expanding on the knowledge and background he brought to the role,
Ronan says, “There’s no questioning that my experience working with organisations such as St Michael’s House and Stewart’s Care are of huge benefit to my day-to-day work here in CHO DNCC. It has enabled me to see things from many sides and also allows me to draw on the network of contacts that I made while working in those organisations.
“Many days as Case Manager I am trying to resolve an immediate crisis or dealing with an ongoing complex case, so having that additional knowledge or knowing the right person to pick up the phone to makes a huge di erence.”
Away from the o ce, Ronan’s caring nature continues to shine through. Last year, his wife completed a 5k to raise funds for the Make-a-Wish foundation which prompted Ronan to become a volunteer in that organisation. A motorsport fan, Ronan also finds time to attend rally events across the country acting as part of a rescue and extrication team where his experience as Cardiac First Responder plays an important part.

To keep fit, and for enjoyment, Ronan plays tennis competitively in some local leagues which he really enjoys. “I’m very much an amateur but I really do enjoy it, it’s a great way to keep active and for socialising,” he says. When pressed on who his favourite tennis stars are, he gives a nod to the future in picking Spaniard Carlos Alcaraz, “The future Rafael Nadal,” he claims.
However, he is quick to add that the real star of the game at the moment is Serena Williams who is currently taking part in her final competition before retirement having won an incredible 24 career Grand Slams: “She’s not only a star of tennis, she’s a legend of sport,” he adds.
When asked for any parting words of wisdom or advice, Ronan again goes back to his career highlight. “This gentleman didn’t communicate verbally, we were communicating by writing notes in my diary. I told him verbally that he was going to get his own house and he simply wrote ‘Are you sure?’ and I wrote ‘Yes, with a smiley face’ – the joy in his eyes and on his face is something I’ll never forget.
"It’s for that reason that my parting advice to anyone, young or old, is if you want to make a positive impact on people lives, if you like working with people, and if you want major job satisfaction – consider a career in the Disability and Social Care sector, you really won’t regret it.”
HEALTH MATTERS WINTER 2022 18 |
‘You’ll never regret a career in disability and social care’
'The best decision of my life'
Public health nurse Audrey Burkley said taking up swimming has been ‘the best decision of my life’.
The Cork-based nurse has recently completed the Jersey to France relay in just nine hours and four minutes, just one of her many swimming accomplishments in recent years.
“I took up swimming later on in life as I was told by the orthopaedic consultant to give up weight bearing activities or else go for major hip surgery. I have congenital dysplasia of both hips which was not diagnosed as a child,” Audrey explained.
Through Facebook, she got to know well-known sea swimmer Sally Minty-Gravett, and Audrey completed the English Channel relay swim in July 2017. The following year she swam around Jersey. That year, 2018, she joined the Coco Channel team and completed the North Channel Relay. Next on the list was the Bosphorus, swimming from Asia to Europe in 6.5 kilometres of open water and the London docklands 10km swim. Then with the Coco Channel team she completed the swim from Catalina to the mainland in July 2019.
The next plan was to swim from Jersey to France in May 2019 but it only came to pass this summer after a number of setbacks, not least the COVID-19 pandemic, as well as one of her team being treated for breast cancer.
Two novice swimmers and breast cancer survivors Anne King and Angela Harvey-Jones joined the team - called Audrey’s Happy Mermaids. They raised money for breast cancer support in Jersey in honour of their team-mate.

“The forecast was meant to be for calm conditions one never knows with the sea. Sal was the first person to start o and she swam in very lumpy conditions and then I took over. I enjoyed the rolling seas but di cult to follow the route as the boat was been moved in the direction of the wind towards Les Ecrehous. The rotation was one hour intervals and Anne and Angela both swam extremely well and we had dolphins on route,” said Audrey.
“We were so excited we forget about the swimmer in the water and we all reached for our camera phone. Dee, our observer, gave us great encouragement and helped us getting back onto the boat each time. On the third hour the conditions totally changed to a beautiful silky calm and perfect visibility to see the large barrell jellyfish.
“On the ninth hour very close to France, the conditions changed very quickly and Sal had very tough choppy swimming conditions and plenty of jellyfish. It was amazing that no one got stung. The pilot Vic made a call that it was too dangerous for us all to swim to shore so the decision was for just Sal to swim to shore.
“When we arrived back in Jersey we were treated to champagne on ice by the team Jersey Long Distance Swimming Club.
“This is a swim I will always remember and a big thank you to Sal, Jenny and the club for making this swim possible. “
Delma
Practitioner, all set for the o in the 2022 Wild Myeloma Way Cycle, which departed UHL in September.

UHL IS LAUNCHPAD FOR TWO-DAY CYCLE TO RAISE AWARENESS OF MULTIPLE MYELOMA

University Hospital Limerick was the launchpad this September for the twoday Wild Myeloma Way Cycle in aid of Multiple Myeloma Ireland, the only Irish charitable organisation focused exclusively on Multiple Myeloma patients, their families and carers.
The event was a highlight of Blood Cancer Awareness Month in the MidWest. The cycle route traversed the stunning landscape of the Wild Atlantic Way, from Limerick to Spanish Point via the Cli s of Moher on day one and returning to Limerick via the coast on day two.
The participants were cycling in memory of Michael Fleming, who tragically lost his life in a road tra ic accident while training for the cycle.
Further information on Multiple Myeloma at https:// multiplemyelomaireland.org/



| 19 HEALTH MATTERS WINTER 2022
Audrey completes another awesome swim challenge
Hackett, Advanced Nurse
At University Hospital Limerick for the launch of the two-day cycle were (from left): Delma Hackett, ANP, UHL; Geraldine Daly, CNS, Haematology; Dr Denis O’Kee e, Clinical Director of Cancer Services, UHL; Dr Cian McEllistrim, Consultant Haematologist; and Dr Hilary O’Leary, Consultant Haematologist.
D I W A L I
The Contact Management Programme (CMP) continued its tradition of celebrating our cultural diversity with the celebration of Diwali in their HSQ location. Diwali is the Indian festival of lights that celebrates good over evil. All staff members got involved, decorating the building with lights and handmade decorations, cooking traditional food to share with their colleagues and sharing their knowledge and stories of the Diwali festival as well as showing off their dance moves with traditional music and dance.

Some of the staff expressed what Diwali means for them and why it was important for them to share the celebrations with their colleagues in the CMP.

“For me, Diwali means togetherness. It is a time when I spend quality time with my family, cooking delicious meals together and decorating my home with candles and lanterns. Diwali has always been the most anticipated time of the year. As this year, I am far away from home, I looked forward to sharing this special day with my HSQ family,” explained Josna Johny from India.
Mohan Raj, also from India, added, “For me, the best part of Diwali is lighting the crackers and watching the fireworks with my family. It is the most fun and exciting festival that I look forward to every year. And I have been waiting for this day to celebrate with different nationalities and I hope everyone loved and enjoyed it with us like a family.”
Ayesha Ahmed, from Pakistan, said, “Diwali is something that I have never experienced before but now I'm getting a chance to celebrate and enjoy this beautiful festival with my colleagues. Everyone took part in celebrating Diwali at HSQ and it was a lot of fun.”

HEALTH MATTERS WINTER 2022 20 |
Diwali celebrations light up working week at Contact Management Programme
Lifeline for Children



AConsultant Paediatrician with an interest in Respiratory and Allergy, Dr Muhammad Tariq took up his post in Midland Regional Hospital Portlaoise (MRHP) six years ago with a vision to develop a centre for respiratory and allergy services for the Paediatrics Department.
Nursing management in MRHP campaigned for funding for Respiratory and Allergy Advanced Nurse Practitioner (ANP) and Clinical Nurse Specialist (CNS) and the department has since grown to a full multidisciplinary team including Lisa Egan, RANP and Ally Russell, CNS. The cohort of patients that attend this service include infants and children with eczema, infants and children with food allergy and children with asthma, respiratory conditions and allergic rhinitis.
Since Lisa took up her ANP role, in collaboration with her clinical mentor, Dr Tariq, the department has had the continuous support of Sandra McCarthy, Director of Nursing; Maura Rice, Paediatric ADON; Fiona Moore, ADON Nurse Practice Development; and Michael Knowles, General Manager.

Lisa and Dr Tariq have successfully set up a skin prick allergy testing service, a food challenge service, a low-risk penicillin delabelling service, a sublingual immunotherapy service and incorporated the use of FeNO into the MRHP asthma service. The service was successful in winning the best poster prize for the food challenge service at the IPA in 2019 and Lisa was also awarded best poster prize at the TCD international nursing conference in March 2022 for her poster on the impact of Grass SLIT on the quality of life of children with asthma and allergic rhinitis.
Having been awarded an educational bursary from ANÁIL, a body that seeks to provide peer support to respiratory nurse specialists and respiratory advanced nurse practitioners, Lisa has just developed a series of four educational videos. This series is aimed at helping secondary care givers of children with asthma and allergies, such as, schools, crèches, grandparents, family members or anyone who wishes to refresh their skills on the basics of asthma and allergy care. These videos are available on the Midland Regional Hospital Portlaoise section of www.hse.ie/dmhg.
Ally Russell started in the role of CNSp in Paediatric Respiratory and Allergy this year. Ally was successful in winning a Spark Ignite Award for her initiative to have a child-friendly training doll to help educate children and their parents about the fundamentals of asthma and allergy care with the aim of reducing morbidity and mortality associated with asthma and allergies from childhood into adulthood. Andy Asthma has become a valued team member.
Ally has been instrumental in the introduction of CPAP skills and training on the Paediatric Ward at MRHP. The introduction of CPAP for infants with bronchiolitis will ensure prompt action and treatment when infants present to the Paediatric ED with respiratory distress as a result of Bronchiolitis.

The team carry out weekly oral food challenges to determine positive or negative food allergy, which is imperative in improving the quality of life in children and families with allergies. During the summer months the team obtained extra bed spaces and completed 55 low risk penicillin day case challenges over a summer time initiative to reduce the waiting list and were delighted to say that most (53) of the children were not actually penicillin allergic.
The team carry out a joint complex allergy clinic with their colleagues in CHI; where children with complex allergy cases are reviewed in MRHP with direct input from CHI consultant paediatric allergist via a video link to provide expert quality care to patients in MRHP.
A large part of the Paediatric Respiratory and Allergy team’s role is educating their peers and most importantly educating children and families to live well with their condition. They regularly work with the Asthma Society of Ireland to educate the wider community on good asthma management and control. Lisa and Ally were leads in updating the new HSELanD paediatric asthma module. They also organised a respiratory meeting in March 2022 with Respiratory Nurse Specialists from all over Ireland to help inform their colleagues of the National Clinical Programme for Respiratory in their e ort to update the end to end model of care for Paediatric Asthma.
| 21 HEALTH MATTERS WINTER 2022
Portlaoise paediatric respiratory team a lifeline for children with allergies and asthma
Lisa Egan, RANP Paediatric Respiratory; Laura Farrell, cANP Paediatric Neurodisability; Maura Rice, ADON ED/AMSAU & Paediatrics; Veronica Taylor, Senior Physiotherapist; Catriona Gowing, Chief Pharmacist; Sandra McCarthy, Director of Nursing; Dr. Muhammad Tariq, Consultant Paediatrician with an interest in Respiratory and Allergy; Ally Russell, CNSp Paediatric Respiratory and Allergy; Teresa Garrahy, Clinical Audit Facilitator; Judy Ennis, Dietitian Manager; Michael Knowles, General Manager; and Kathleen Bennett, Secretary to Dr Tariq.
Lisa Egan, RANP, with child Faye Hinc, and Andy Asthma, a child-friendly training doll to help educate children and their parents about the fundamentals in asthma and allergy care
BREASTFEEDING WEEK

Almost two-thirds of babies breastfed at first public health nurse visit
There was a 5% point increase in the number of babies breastfed at the first Public Health Nurse visit between 2019 and 2021, a rise to 59%, according to new HSE figures. The improvement was celebrated as part of this year’s HSE National Breastfeeding Week, with the theme this year ‘Expert Help for Every Step of the Way’.






The HSE has recruited 20 additional infant feeding and lactation posts within nursing and midwifery services to support breastfeeding parents. Midwives are the first to assist with breastfeeding and should mothers need more specialist support, all 19 maternity hospitals now have a specialist lactation support service available. More infant feeding/lactation posts are being recruited to ensure nationwide availability within primary care services. 110 breastfeeding groups have now resumed meeting in person providing important peer-topeer support for parents on their breastfeeding journey.
Laura McHugh, HSE National Breastfeeding Coordinator, celebrated the new posts and the importance of these growing supports. “While breastfeeding rates are increasing around the country, we want to continue to build on this progress by supporting every parent who may need help on their breastfeeding journey. I welcome our



colleagues taking up the new infant feeding and lactation roles around the country, and although not everyone will need their services, their support will make a big di erence for parents who do,” she said.






“As well as the new posts, we have breastfeeding preparation and antenatal classes, our midwives and public health nurses and a growing number of in-person groups resuming post pandemic. There are also a range of online resources such as virtual breastfeeding groups and mychild.ie, which has practical breastfeeding advice and the ‘Ask Our Expert’ live chat and e-mail breastfeeding support service, available seven days a week.



“Approximately six in every 10 babies are breastfed in the first week of life, and we have developed a holistic range of supports to help mothers and babies learning this new skill.”


Anne O’Malley, HSE Public Health Nurse, Community Healthcare Dublin North City and County, added, “Every breastfeed makes a di erence because any amount of breast milk is beneficial for mother and baby. If a mother can breastfeed for a short amount of time it will be helpful, and the longer you breastfeed the greater protection for mother and baby. We want every mother to know about all the free supports available to help her to breastfeed for longer if she wishes.”


HEALTH MATTERS WINTER 2022 22 |
MY TYPICAL DAY
6am
Wake up time. Breakfasts and lunches are prepared for my four children before I head out the door. My husband leaves for work at 6.30am so I’m lucky that my mother comes to bring the smaller three to school. I have a 30-minute commute to work in Tralee and my eldest travels to school with me. I generally work four days a week.
8am
On arrival, I check on messages and referrals, while reviewing notes on patients seen on the previous shift. My o ice is on the Postnatal Ward (PNW) so I check in with the shift leader there and the Special Care Baby Unit (SCBU) for any additional referrals, working out a planned schedule to review women and babies.
AS
INFANT FEEDING COORDINATOR / LACTATION SUPPORT
University Hospital Kerry – Mairead O’Sullivan

10am
I facilitate a post-natal infant feeding class for those due to be discharged, helping mothers with any breastfeeding concerns and advising them how to contact me after discharge. I then review patients on the wards.
1pm
At lunchtime, I provide a 15-minute workshop with colleagues, covering hand expression, colostrum harvesting, safe skin to skin, and attachment and electric breast pumps/milk storage.
2pm
After a quick bite to eat, I book moms into their appropriate online antenatal breastfeeding class, emailing links and additional information. I facilitate these classes twice a month.
4pm
I’m chair of our infant feeding committee where we have a multi-disciplinary influence. These meetings are held regularly and current items on the agenda include maternity plans for National Breastfeeding Week.
5.30pm
After supper break, I have an antenatal breastfeeding preparation class with 18 attendees booked in. Although facilitating these groups online has taken some readjusting, service user feedback is extremely positive.
8.30pm
I finish work after class feeling hugely satisfied. It’s been a busy day, but I love the job. By the time I’m home, my two younger kids are in bed and the older two will be going shortly, so I catch up on the day with them and my husband before heading to bed myself around 10.30pm.
| 23 HEALTH MATTERS WINTER 2022
Vital support for local women
Portlaoise hospital offers local women important new breastfeeding supports
Midland Regional Hospital Portlaoise (MRH) has introduced two new pieces of equipment to provide vital support to local women who may be having problems with breastfeeding.

The first, a therapeutic ultrasound, provides micro-massage and heat which treats mastitis by unclogging milk ducts, while also reducing pain and swelling. The hospital has also purchased a cutting-edge laser machine which greatly speeds up the healing of cracked skin.

Claire Fitzpatrick, a Clinical Midwife Specialist in Lactation at MRH
Portlaoise, explained, “The laser treatment is non-invasive, it emits no heat or sound and is not painful but it does speed up wound healing and reduces inflammation which is very useful for women who are on the verge of giving up breastfeeding due to the pain caused by cracked nipples. For some mums, it helps prolong breastfeeding.”
One local woman treated by the breastfeeding support team at MRHP said, “I had three laser treatments which has really supported my breastfeeding journey. The service is incredible
HEALTH MATTERS WINTER 2022 24 |
and made such a di erence to me. I can now feed without pain. The two Lactation Consultants at Midland Regional Hospital Portlaoise could not have been more supportive, accommodating and full of information. I can’t emphasise enough how important and valuable this service is.”
Women who attend MRH Portlaoise to give birth can now return to get breastfeeding support from a fully qualified Midwife Lactation specialist for up to six weeks after their baby is born. Also later this month a Parent Craft Co-ordinator will take up a position at the hospital to help women and their partners in preparation for birth and parenthood, which includes creating awareness of breastfeeding and empowering mothers to consider it as their first choice of infant feeding.

MILK FOR ANNIE HELPED ME DEAL WITH HER NICU STAY"
Dundalk mum Sarah Heaphey was in shock when she went into pre-term labour with her little girl. Baby Annie was cared for in the neonatal intensive care unit (NICU) for weeks. Sarah focused on expressing her breastmilk for Annie to help in the best way she could.
“While was pregnant I said ‘I’ll try breastfeeding and if it works brilliant but if not I would be open to pumping’. My sister-in-law Jean pumped the previous year so I was also familiar with this thanks to her. My plan was to try my best and hope the breastfeeding worked,” said Sarah.
“I was booked in for the antenatal class in the hospital in January at around 33 weeks, there I learned about breastfeeding, the early days of milk coming in, some challenges and much more and thankfully I did. I was there the Thursday and then had Annie on the Monday. It was very unexpected - she wasn’t due until March!”
Sarah said that it was a scary time as Annie was in the NICU and she didn’t know what she could do.
“A nurse said the best thing you can do for her at the moment is give her your milk. It was very overwhelming at the time along with my baby being unwell. Shineen, the clinical midwife, was so supportive, she got me a pump in no time and I was pumping straight away. I went into a pumping trance and was spending a huge amount of my time making sure I got as much milk as I could and establishing my supply.
“All the midwives were great, I got engorged and they really helped me through it. I was pumping every three hours 24 hours a day. My husband was a great support with this also as it can be a very lonely time when you’re up in the middle of the night and no baby there with you.”
She explained that baby Annie had quite a lot of complications.
“She had Grade 3 intraventricular hemorrhage on her brain, it was a whirlwind on top of the shock of such an early labour. We spent weeks in the hospital including surgery at 28 days old in Temple Street,” said the new mum.
“Shineen said our aim was to get Annie to suckle by her due date, but by then she was feeding properly and was doing so well. Her feeding came on no end after her surgery. The few days before going home, Shineen gave me a plan and cautioned that I’d be triple feeding for a while, it’s very easy to underestimate the amount of time that goes into that, between feeding her myself, doing top ups of breast milk in a bottle, pumping and sterilising.”
As Sarah was pumping for six weeks when Annie was in hospital, she ended up with a huge supply of extra milk and was able to donate over four litres of milk to the Human Milk Bank.
“I was so delighted to be able to do this, as I can only imagine the stress of a mother not being able to give her own milk under such di icult circumstances.




It was a di icult process as I had to get bloods done, and found it hard to find someone to do them so I reached out to the hospital who were really helpful with it. It was really nice to get a letter recently to say that my milk had been used for some vulnerable babies,” she said.
Annie is thriving now at 10 months after her tough start in life.
“When she was eight months old, we went to Temple Street. I had to bring an extra bag of food, and bottles and formula etc. but when I was breastfeeding it was just myself and her - it was so convenient! I’m delighted I did it for as long as I did, and I do think it benefited her no end. It gave me something to focus on, and was a major way to help her, while she was in hospital.

“My advice for any mums going through a di icult situation with breastfeeding is to link in with anyone who might have gone through something similar. I found it very helpful to talk to other people. I got great support on my journey and it helped me feed better and for longer,” added Sarah.

| 25 HEALTH MATTERS WINTER 2022
"EXPRESSING
Top: Margaret Sheeran, Clinical Midwife Specialist in Lactation; dad Mohana Vamsi Dintakurti, mum Sokimya Addapalli, with their baby Advika Vamsi Dantakurti; and Claire Fitzpatrick, Clinical Midwife Specialist in Lactation.
Bottom: Claire Fitzpatrick, Clinical Midwife Specialist in Lactation; Ita Kinsella, Director of Midwifery MRH Portlaoise; Margaret Sheeran, Clinical Midwife Specialist in Lactation.
RHA E
Limerick, Tipperary and Clare
Integrated Care and Regional Health Areas
RHA F
Donegal, Sligo, Leitrim, Roscommon, Mayo, and Galway
RHA D Kerry and Cork
RHA
A North Dublin, Meath, Louth, Cavan, and Monaghan
RHA B
Longford, Westmeath, Offaly, Laois, Kildare, and parts of Dublin and Wicklow
RHA C
Tipperary South, Waterford, Kilkenny, Carlow, Wexford, Wicklow, part of South Dublin
The Sláintecare vision for Ireland is to have an integrated health system where a person, throughout their life, can access high-quality health care from valued healthcare professionals, closer to their home, within a reasonable amount of time.
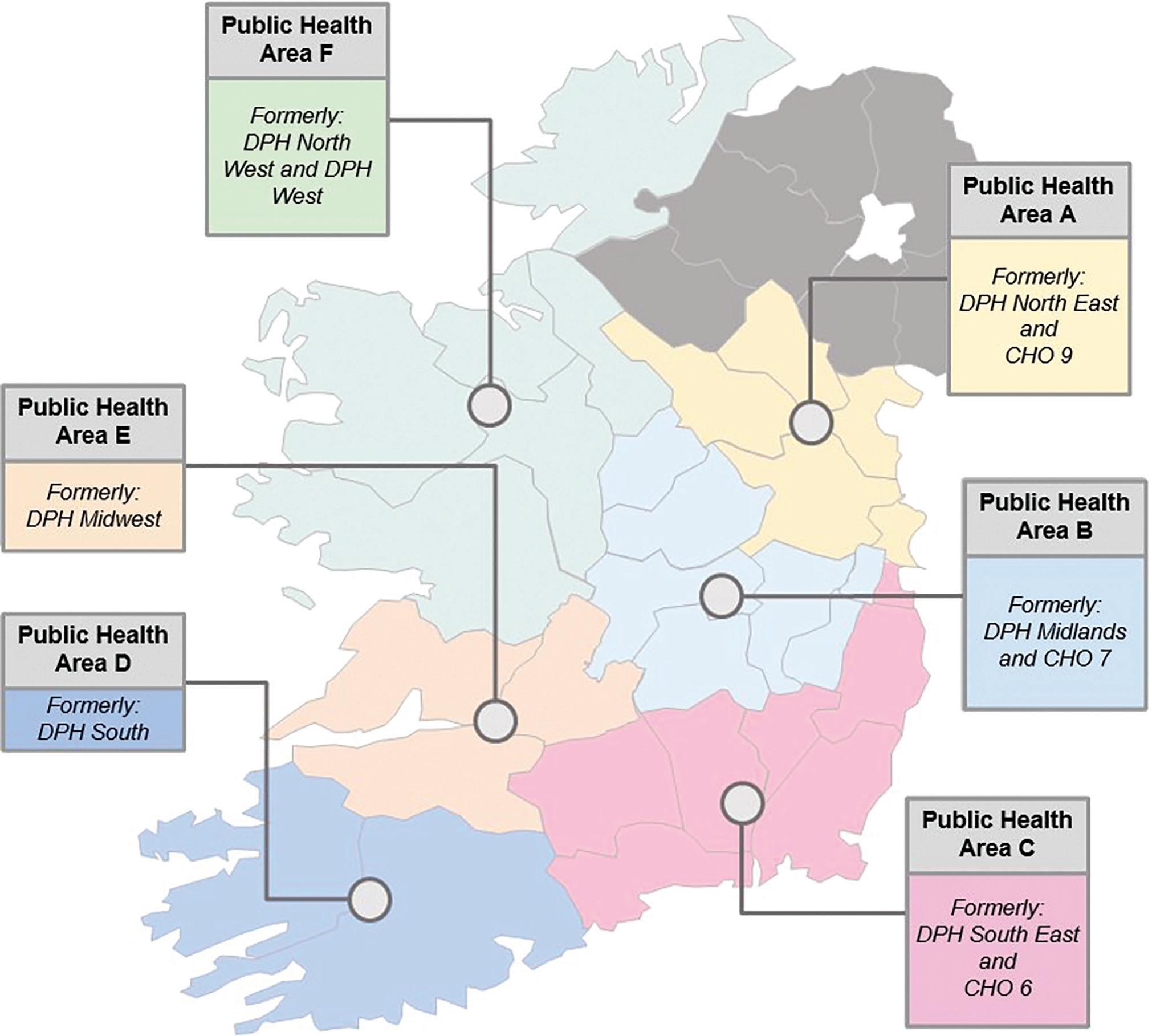
HEALTH MATTERS WINTER 2022 26 | Making Progress on Integrated Care
Enhanced Community Care modernising how we deliver care
The most significant expansion in primary care capacity in the last two decades
Healthcare in Ireland is facing many significant challenges such as a growing and aging population, and an overreliance on acute hospital care. Even good news stories that people in Ireland are living longer than ever before brings a need to plan and resource chronic disease and older person services.
Delivering more health and social care services in the community, closer to people’s homes, is the key to responding to these challenges.
The Enhanced Community Care (ECC) programme, a Sláintecare initiative, is doing just this by enhancing and increasing community health services and reducing pressure on hospital services.

At its core, the ECC is a programme of reform. With an investment of €240 million and 3,500 additional staff, it aims to increase overall levels of healthcare, with service delivery reoriented towards general practice, primary care and community-based services.
The ECC programme is enabling new ways of working, empowering local staff leadership to meet the needs of local communities and shift the focus away from acute hospitals.
Almost all of the 96 planned Community Healthcare Networks are now live. Each Community Healthcare Network serves a population of about 50,000 people and consists of between 4-6 primary care teams, with GPs involved in delivering services. CHNs are enabling decisions to be made closer to the point of care, and specific to population needs.
The CHNs are further supported by Integrated Care Programs for Older Persons (ICPOP) and Chronic Disease (ICPCD). These teams have shown that improved outcomes can be achieved when people are cared for in their own homes and communities. The teams will shift from the acute hospital towards general practice, primary care and a community-based home first service model.
When this new approach is fully embedded we will have fully developed integrated care pathways between acute and community sectors, improved outcomes for patient, a more efficient health service and a better service for staff to work in.
Change does not happen overnight, but significant progress is being made to reduce pressure on services and dependence on the hospitalcentric model of care.
We have already established 91 Community Healthcare Networks, 21 Community Specialist Teams for Older Person Services and 18 Community Specialist Teams for Chronic Disease Management. More than 2,300 out of 3,500 staff have been recruited. In addition, national coverage for the 21 Community Intervention Teams has been achieved and a volunteer-type model in collaboration with ALONE is being rolled out, with 6,000 people now supported through coordinated support.
| 27 HEALTH MATTERS WINTER 2022
A community first model of care
Regional Health Areas (RHAs) are a big part of achieving this vision. Acute Hospitals and Community Health Organisations will be grouped together into six large regions called RHAs. In each RHA services, resources, and governance will be co-ordinated around the needs of the patient across all care settings.
ECC can help ageing and vulnerable maintain independence
The HSE and the Department of Health hosted the first ever Enhanced Community Care (ECC) Conference 2022 at Dublin Castle.
The event brought together nearly 700 colleagues in person and online from all over the country to mark progress on implementing the ECC Programme.
Attendees heard from senior colleagues in the HSE, expert speakers working in integrated care, including the keynote speaker Professor Sir Chris Ham, former CEO of the Kings Fund UK. We heard from our HSE teams around the country about the programme’s latest developments, and the first hand experiences of people benefitting from this programme.
Speaking at the event, keynote speaker Professor Ham said, “Ireland’s ageing population and changing disease burden – with increased prevalence of chronic conditions such as diabetes
and asthma – requires care to be joined up around patients, especially those with complex needs.
“With Enhanced Community Care, Ireland has made an impressive start on this journey and is moving in line with international best practice. I commend the HSE on their work to date, especially against the backdrop of a global pandemic. The challenge now is to build on the foundations that have been laid and support health care staff in making services fit for the future.
“Providing more care in people’s homes or close to home will allow ageing and vulnerable populations to maintain their independence and live well in the community. Hospitals can then focus on providing specialist care for people with acute medical conditions as well as working more closely with general practices and community teams.”
Integrated care is where services, funding, and governance are co-ordinated around the needs of the patient, encompassing acute, primary and community care. Resetting how people understand healthcare and how to access it. Moving away from thinking we access healthcare through our hospitals first to understanding that most of our healthcare will be accessed in our communities - Department of Health Technical Briefing on RHAs to the Joint Committee on Health, November 2022
HEALTH MATTERS WINTER 2022 28 |
Progress
Integrated
Making
on
Care
a full ECC Conference recording, download or read presentations from expert clinicians and teams
Watch
at www.hse.ie/ecc
Pathfinder service expands delivering healthcare to older people in their homes
A National Ambulance Service (NAS) led service called Pathfinder, designed to safely keep older people who phone 112/999 in their own home rather than taking them to a hospital emergency department, went live in Limerick, Tallaght and Waterford this autumn.

Pathfinder improves outcomes for older people by providing safe alternative care at home rather than in hospital and is being provided by National Ambulance Service sta working with colleagues from HSE acute hospitals.
The service has already been working as a collaborative service between NAS and Beaumont Hospital Occupational Therapy and Physiotherapy Departments for more than two years.
Robert Morton, Director of the HSE NAS, said the expansion of the NAS Pathfinder Model is part of a plan to o er di erent groups of patients an alternative pathway other than presenting to a busy emergency department.
“NAS is delighted to be working with University Hospital Limerick, Tallaght University Hospital and the University Hospital Waterford who have agreed to support the expansion of the Pathfinder model to other parts of the country. NAS Pathfinder is improving outcomes for older people by minimising unnecessary ED attendances and o ering safe alternative care pathways for older people in their own homes rather than in hospital,” he said.
Welcoming the introduction of the


service to Limerick, Prof Colette Cowan, CEO of UL Hospitals Group said University Hospital Limerick was pleased to be able to o er this service to suitable older people in its catchment area.
“We know that the Pathfinder Model demonstrates that Pre-Hospital Services can help to safely keep older people, who have phoned 112/999, in their own home rather than transporting them to a hospital ED for assessment. Many older patients can be safely and appropriately managed in their own home rather than being transported to the ED when they dial 112/999 with low acuity complaints.”
Lucy Nugent, Chief Executive, Tallaght University Hospital said many older people in the hospital’s catchment area who dial 112/999 with non-urgent complaints will benefit from the Pathfinder care model.
“Pathfinder aims to reduce congestion in busy EDs and makes for a better environment for patients and sta on the floor whilst improving overall flow through the ED. The service enables increased ED capacity to care for other patients, by supporting this cohort of complex, frail patients at home.”
“The service is particularly welcome as we approach the winter, we know that our older citizens are particularly vulnerable to adverse events and poor outcomes during emergency department attendances and hospitalisation.”
Welcoming the new service to Waterford, Grace Rothwell, General
Manager, University Hospital Waterford said the hospital looked forward to collaborating with the National Ambulance Service for the benefit of older people in the area.


“Many patients who present to the emergency department have non-urgent care needs that could be treated elsewhere. Overall, Pathfinder has shown that it is a safe and acceptable service for older people who dial 999/112 with low acuity complaints.”
Pathfinder received initial funding from the Sláintecare Integration Fund to test the model in 2020 and has been operational since May 2020. The three new Pathfinder teams have been funded by the HSE.
The Pathfinder ‘Rapid Response Team’ respond to 999/112 calls for older people (65 years and older) in their homes. The older person is assessed by both an Advanced Paramedic and Occupational Therapist/Physiotherapist. Where safe, the team supports the older person at home rather than transporting them to an emergency department, by linking with a wide range of alternative hospital and community services. Pathfinder also operates a ‘Follow-Up Team’ (Physiotherapy & Occupational Therapy) which provides immediate home-based rehabilitation, equipment provision and case-management in the subsequent days following a 999/112 call.
On average two thirds of patients seen by Pathfinder following a 999 call have remained at home rather than being brought to the Emergency Department.
| 29 HEALTH MATTERS WINTER 2022
Top left: Blaithin Lally, Senior Physiotherapist; Linda O’Rourke, Advanced Paramedic; Nicola Donohue, Clinical Specialist Physiotherapist; Pat McCarthy, Advanced Paramedic; and Niamh Ganley, Senior Occupational Therapist. Top Right: Niamh Ganley, Senior Occupational Therapist; Pat McCarthy, Advanced Paramedic; and Nicola Donohue, Clinical Specialist Physiotherapist Inset: Nicola Donohue, Clinical Specialist Physiotherapist; and Pat McCarthy, Advanced Paramedic. Photos: Brian Arthur Photography
From CAMHS inpatient to CAMHS Connect providing step down care in
Galway and Roscommon communites
CAMHS team opens physical health monitoring clinic
Anew physical health monitoring clinic for young people with moderate to severe mental health difficulties has opened at Child & Adolescent Mental Health Services (CAMHS), Community Healthcare West (CHW).
Early intervention for psychosis has always been a priority for this service. In five years approximately 70 young people aged under 18 have been admitted to CAMHS Inpatient Unit Merlin Park, Galway for assessment and intervention for psychosis.
CAMHS Connect day hospitals in Galway city and Castlerea, Co Roscommon provide step-down care and intervention for those who are being treated in the Galway and Roscommon community settings, some under 14 years of age.
Dr Delia McGuinness, Clinical Lead CAMHS Connect, and Dr Catherine O’Brien, Clinical Lead CAMHS Inpatient Unit, have shared expertise to now develop an outreach service to support CAMHS outpatient teams in CHW in providing essential intervention for those young people with psychosis in the community setting.
Recently there have been concerns for young people in CAMHS nationally in regard to the provision of regular investigations for antipsychotic medication. As part of the physical health focus, it was decided to expedite the development of a physical health monitoring clinic in CHW in 2022.
Based in outpatient CAMHS, South Galway Clinic, Senior Registrar Dr Ronan Rice started a pilot project in physical health monitoring in the outpatient clinic and was also part of the CAMHS Connect/Outreach team bringing a particular focus there to development of assessment tools, physical health monitoring and assessment and lifestyle intervention pack.
The pilot project in the outpatient clinic centres on an audit of young people prescribed antipsychotic medication, which took place from January to June 2022 and Dr Rice carried this out with registrars Dr Margaret Gallagher and Dr James Duffy. During this pilot clinic, a
physical health review was offered to all young people prescribed antipsychotic medication attending South Galway CAMHS. Responsibility for physical monitoring was shared between South Galway CAMHS and patients’ GPs with an emphasis on improved communication and information sharing.
Looking at international practice, the CAMHS Connect/ Outreach team saw the very innovative service set up in Bradford UK by mental health nurse Kate Dale. Kate had also developed the Bradford tool - an electronic monitoring tool for the clinics there.
The CAMHS Connect/ Outreach team members Dr Emma Beatty, Senior Registrar; Dr Joanne Fallon, CAMHS Occupational Therapy Manager; and Mairead Doyle, Senior Dietetics Specialist/ Manager entered – and won - the SPARK Ignite Healthcare innovation competition to fund their adaption of the Bradford tool for an adolescent population in the physical health monitoring clinic.
"Our goal is that this electronic system will also provide reminders for physical health monitoring appointments as advised by best practice guidelines so that these crucial interventions are not missed. We plan to develop a GDPR compliant database of young people in the physical health monitoring clinic, to provide targeted group interventions such as dietary advice, exercise programmes and smoking cessation,” explained Dr Beatty.
The Outreach clinic commenced in CAMHS Connect Galway city in June 2022 and the plan is to extend to Roscommon and Mayo, with patients attending clinics in CAMHS Connect eHub Castlerea.

Clinical Nurse Specialist (CNS) Aoife Walsh is co-ordinator of the new physical health monitoring clinic, working closely with Dr Rice, Dr Sannie John and Dr Simon Munro, the CAMHS Connect Senior Registrars, and CAMHS outpatient clinics CNM3 Maurice Moloney. Aoife has developed a clinic pack consisting of referral forms for community CAMHS teams, consent forms, assessment forms and antipsychotic checklists, & dietetic weight monitoring forms.

HEALTH MATTERS WINTER 2022 30 | Making Progress on Integrated Care
CNS Clinic Coordinator Aoife Walsh; Senior Registrar Dr Simon Munro; and Dietetic Specialist and Manager Mairead Doyle in the physical health monitoring clinic. Outreach and CAMHS Connect team - Dr C O’Brien, E Howley, Mairead Doyle, M Morgan, Aoife Walsh, Dr D McGuinness
Primary and Praise for Nenagh
Reform Primaryofand Community Care






In the new integrated care model Enhanced Community Care will be at the centre of how we deliver healthcare. To the left of ECC, health promotion and public health services will help people to live well at home to prevent sickness. This will assist our acute care services, treating people with urgent care needs, ensuring they have the shortest stay possible in hospital to get them well and back home.
At a time when the Emergency Department at University Hospital Limerick is managing record attendances of very sick patients, UL Hospitals Group’s three Injury Units at Nenagh, Ennis and St John’s Hospitals are a fast, e ective pathway for thousands of people who su er sprains, cuts, breaks and burns, but do not need to attend ED for treatment.
The service is particularly useful for parents of young children who are all too prone to accidents arising from play. Scari mum-of-three Theresa Tierney-Bugler experienced at first hand the e ectiveness of the Injury Unit in Nenagh after her daughter Andrea took a tumble at a birthday party.

Theresa was at the time expecting the arrival of her third baby, and her husband was away on duty with the Irish Navy. She called the Injury Unit and speaks highly of the calm, professional manner in which the sta dealt with her concerns over the phone, and later on arrival at Nenagh Hospital.
“It was all a bit hectic as my husband was away, but we all went over, and the PALS [Patient Advocacy Liaison Service) volunteers were there to greet us at the door and get us to where we needed to go. Andrea was triaged very quickly. To be honest, I thought it was a sprain, but the doctor swiftly confirmed it was a break. So they brought her for an X-Ray, and then put her arm in a cast. We were in and out in under an hour,” she recalled.
The Injury Unit at Nenagh Hospital is sta ed by an expert team of three full-time Registered Advanced Nurse Practitioners and one trainee ANP, along with two registrars, administrative support and led by Dr Damien Ryan, Senior Consultant in Emergency Medicine. They provide timely treatment for injuries that are non-threatening to life or limb, but which still require expert and prompt medical attention.
Injuries like Andrea’s account for a significant volume of the work that’s done in the UL Hospital Group's Injury Units every year. In 2021, a total of 33,853 people attended the three Units, 13% more than the total for 2020.
In the Nenagh Hospital Injury Unit alone, a total of 9,971 patients attended for treatment, which is a 14% increase on the number for 2020, and almost returned to pre-pandemic levels of activity. In 2019, the last full year prior to the public health emergency, 10,025 patients used the unit in Nenagh Hospital.
Dr Damien Ryan, Consultant in Emergency Medicine and clinical lead at the Injury Unit in Nenagh Hospital, welcomed the increase in patients at the Injury Units over the past year, and he reminded people who su er injuries like Andrea's, not to delay seeking treatment for an injury that needs medical care. “Minor injuries may indeed be clinically minor, but that does not mean they are insignificant. If they are not treated early, these injuries can become more complex and di cult to treat, and perhaps lead to serious illnesses,” Dr Ryan said.
Dr Ryan and his colleague at Nenagh Hospital, Clinical Nurse Manager Catherine Quinn, said that while it is encouraging to see more people attending, it is still important for people to first seek out the most appropriate options for treatment.
Mum Theresa urged all parents, and all people who su er minor injuries, to first think about the Injury Unit rather than panicking and heading to the Emergency Department at UHL.
“People should definitely be using the Injury Units more. Compared to ED at a time when it’s so busy with emergency care, the Injury Units are very e cient and fast. I think there might be a lot of unnecessary trips to ED made by people who might not realise the Injury Units exist. I Googled them and called ahead, and I would urge anyone to do the same,” she said.
| 31 HEALTH MATTERS WINTER 2022
Mum of three praises Nenagh Injury Unit for treatment of daughter’s injury
Operating within the six new Regional Health Areas,
Enhanced Community Care will be made up of 96 Community Healthcare Networks (CHNs) with 3,500 new ECC staff, working across 30 new Community Specialist Teams for Older People and 30 CSTs for Chronic Disease
“It’s fantastic for patients – they access the service in their area and don’t have to come into hospital, so it’s a bit easier all round” – Rachel Anglin, Chief Respiratory Physiologist at St Vincent’s University Hospital described the benefits of the Integrated Care Hub in Bray where she works with a team of colleagues providing a comprehensive range of integrated services.
Included on the team is Joyce O’Hara, Specialist Respiratory Nurse, who explains that she started in her post last year as part of a Sláintecare project. “It was a new project to deliver specialist respiratory services within the community. Previous to setting up the service which includes a nurse, pulmonary function tests and specialist physiotherapist, patients would have to access acute hospital services – they would have to be referred by their GP to a hospital waiting list.
“Because of the Sláintecare project, we were able to commence
that service in the locality. That meant that patients could avoid hospital waiting lists and they were seen in a timely manner. So we very much run an integrated service – I work very closely with my colleagues in St Vincent’s University Hospital, with GPs, and with our Respiratory Consultant who governs the service and we all work quite closely together.”
Rachel added, “I run the Respiratory Service here in the Integrated Care Hub. It’s a fantastic service for the patients because they can have this specialist testing in their community, in their area and they don’t have to come into hospital.”
Joyce concluded that they can then follow up with their patients which she described as “more personal and individualised. Patients get regular follow up every two to three months. Because this is a chronic condition, it’s lifelong. So we get to build a relationship with these patients. And we can stay with them on their journey through their chronic disease.”
HEALTH MATTERS WINTER 2022 32 | Making Progress
Integrated Care
on
helps teams build a relationship with patients Progress is already being made in ECC So far we have • 91 out of the 96 CHNs set-up • 21 Community Specialist Teams for Older Person Services • 18 Community Specialist Teams for Chronic Disease Management • Over 2,300 out of 3,500 additional staff recruited
Integrated care hub
New Nurse-Led Wax Clinic introduced at Letterkenny University Hospital
Letterkenny University Hospital held the first nurse-led Wax Clinic in the Outpatients Department in September, freeing up doctors in the ENT for more complex clinical care.
Sta nurse, Bridgene Bonner introduced the new clinic following specialised training in London and at the Royal Victoria Eye and Ear Hospital Dublin. The clinic runs under supervision from Prof Nash Patil, Consultant ENT Surgeon from Sligo University Hospital as part of the satellite ENT Outpatient Service for Donegal.
Bridgene Bonner described her work in the ENT Clinics and said, “During the Wax Clinic I perform micro-suction of the ears which is a non-invasive method of treating impacted wax and otitis externa, a condition that causes inflammation of the external ear canal.

“In 2017 I attended a course on ear care and micro-suctioning and since then I have been working on further developing my skills in this area. Under the guidance and with support of the ENT consultants, I developed a policy to introduce a standalone Wax Clinic which was initially due to start in early 2020 but was put on hold because of the pandemic.
“The work I do in the Wax Clinic would previously have been carried out by the doctors in the ENT Clinic which means that I am able to free up their time for more complex clinical care. I have been able to work with many long term patients who come in for micro-suction and a lovely part of the job is seeing how they have been getting on especially the improvements from their first visit.
“This new nurse-led clinic will take place once a month and I will treat 8 to 10 patients in each clinic. When I am not running my own session, I work in the ENT Outpatient Clinic supporting patients through the Department, booking their procedures, managing files and reports and providing information to newly diagnosed patients, including post-op patients attending the department.”
RHA planning and design
Planning for the six Regional Health Areas began earlier this year. The Department of Health and the HSE are working together to develop a draft RHA design and implemantion plan by the end of the year.
An RHA programme team, co-chaired by the Department of Health and the HSE, is currently developing the design and implementation plan for RHAs under five separate work streams. These are:
1. Corporate & Clinical Governance & Accountability - examining the reform of organisational, clinical and corporate governance and accountability lines as part of RHA implementation.
2. Digital & Capital Infrastructure - planning for necessary capital infrastructure for RHAs; to identify the current and future capital infrastructure and IT requirements.
3. People & Development - assessing what and where our current and future sta ing needs and associated training requirements are.
4. Change, Communications & Culture - facilitating stakeholder engagement; to establish relationships with local leadership and planning the communication of the RHA vision and benefits to all stakeholders.
5. Finance including Population-Based Resource Allocation (PBRA) - examining the reform of the budgeting and financial management process with RHAs as operational delivery units enabling population-based approaches.
To inform the RHA programme team’s work, six regional events with senior leaders, clinicians, and their representatives from CHOs and Hospital Groups took place throughout September and October 2022. Almost 600 people participated across the six events. These are the first in a series of engagement events to take place with services over the coming months.
NEXT STEPS
Funding is now secured for RHA leadership teams and initial resources in Budget 2023. The RHA Implementation Plan is due to be finalised by the end of this year with implementation due to start in early 2023. More engagement sessions are planned with health and social care professionals to inform the implementation plan for 2023.
| 33 HEALTH MATTERS WINTER 2022
Bridgene Bonner has commenced a nurse-led Wax Clinic in the Outpatients Department of Letterkenny University Hospital, taking place once a month. From left: Bridgene Bonner, sta nurse Angela Hegarty; and Professor Nash Patil, Consultant ENT Surgeon from Sligo University Hospital.
Integrated care for children with disabilities
The Children’s Disability Network Team (CDNT) in Sligo South Donegal community care is an interdisciplinary team made up of psychologists, speech and language therapists, occupational therapists, physiotherapists, dietitians, social workers, community facilitators, management and administration staff. The team works together to meet the complex needs of children with disabilities through family centred practice in line with the Progressing Disability Services (PDS) programme. The team provides supports and therapeutic inputs to children as well as offering parent training and group sessions.
The team works with Sligo Sports and Recreation Partnership which organises activities and outings along with summer camp activities for children on the CDNT caseload. In addition, the team provides afterschool clubs in the Avalon Centre, Sligo Town, five afternoons per week for children with high priority complex needs attending a special school. The team also links with Family Carers Ireland to jointly provide a Saturday club every second Saturday to children with high support needs and physical disability.
The CDNT team members work together in a purpose-built facility, located in Nazareth House, Sligo that was recently renovated with €3m in capital funding. The building consists of bright modern clinical rooms, an observation room, a multisensory room, a paediatric room and large group rooms for group sessions and parent training.
The team works closely with Child and Adolescent Mental Health Services (CAMHS), GPs and Primary Care Services who are co-located within the building. The team also works with education services, Tusla Child & Family Agency, acute hospital and specialist health services in order to best meet the needs of children and their families.
Fionnuala O’Connell, whose daughter Luna requires the services of the CDNT, Sligo South Donegal spoke of her experience availing of the service for her daughter. “Having the service in Sligo, within the one building has enabled us to attend appointments across services within the one building on the same day. This has made our family life a lot more fluid. Not having to bring her to multiple different appointments to multiple different areas. She has benefitted hugely from the team as they work collectively together, sharing information and procedures with my daughter’s best interests at heart. This has ensured that she has got the best service possible from the team here in Sligo.”
Mary Durcan, Children’s Disability Network Manager, Sligo South Donegal, explained that the interdisciplinary team approach ‘has been
RHA Timeline
July 2019
RHA boundaries approved by Government
April 2022 Preferred RHA Model approved by Government. RHA Working Groups set up
March 2020
Options for regional structures evaluated
very positive for our team, encouraging excellent teamwork and effective communication’.
“The team works very closely with parents to meet the goals and needs of the children who access the service. Our service is always growing and we are constantly learning new things. We continually strive to meet the needs of children and families here.”
Debbie Ferguson, Community Facilitator, Children’s Disability Network Team, Sligo, South Donegal, provides support and advice to parents and children who access the team.
“We are very fortunate here in Nazareth House to have a purpose-built facility to accommodate the complex needs of the children who access our service. Having all disciplines under the one roof here in Nazareth House provides an excellent environment for good teamwork and effective communication. Part of my role is to co-ordinate the individual family support plan for the children and the families, who access our service. I thoroughly enjoy working as part of this team,” she said.
Aisling Dolan, Senior Physiotherapist, said, “We do a lot of our joint sessions in our multisensory room. I’m a physio and I work a lot with the occupational therapists and the autism therapists, and we would bring families and the children into this room and do our treatments sessions and interventions here.”
Dervla Kelly, Occupational Therapist, spoke about the soft play areas.
“This is where we run a lot of our group therapies. I work alongside the physiotherapists, the community facilitators, the autism therapists. We bring families in here to run groups where we look at fine and gross motor skills together. We ran a group called the PHYSI Group recently with the OTs and physios. It’s a great chance for clinicians to come together and share their experience and their knowledge but also for parents and families to come together to share their experience and their expertise.”
Head of Disability Services for Community Healthcare Cavan Donegal Leitrim Monaghan Sligo, Edel Quinn, explained that the establishment of Children’s Disability Network Teams has been ‘a very positive step forward in providing for the needs of children in our communities with complex needs and those of their families’.
“The Sligo South Donegal Children’s Disability Team is one of seven such teams in Community Healthcare Cavan Donegal Leitrim Monaghan Sligo. Ongoing investment in and development of children’s services is a key priority for the HSE,” she said.
December 2022 RHA Implementation Plan outlined
January 2023
Design and implementation continues May - December 2022 Working groups focus on RHA Governance, FInance, People, ICT, Capital, Change Communications and Culture. RHA design workshops take place around the country
January 2024
6 RHAs up and running
HEALTH MATTERS WINTER 2022 34 |
Making Progress on Integrated Care
My HSE Self Service
Integrated staff records and payroll for a modern health system
The National Integrated Sta Records and Pay Programme (NiSRP) will implement national sta records and payroll systems across the HSE and will support the needs of a modern health system employer, enhancing available workforce information for managers. The programme will modernise the way the HSE connects with sta , improving access for them to their sta record and pay details via online employee and manager self-service.
NiSRP is now available in HSE East, South East, Mid West, North West and Midlands. We asked some My HSE Self Service users about their experience of using the system.

you’re not relying on ‘did I send that email’, ‘has this person gotten back to me’, ‘I have to send this form to person A, this form to Person B’. It is really easy to track everything. My overall comment is that it is just easy to use and a huge timesaver. There is no risk of losing papers or annual leave cards. I would never go back to the paper way again”.
Donal O’Donnell, Sta O icer in University Hospital Limerick

‘No
more Leave Cards’
Maria
Whelan, Paediatric
Occupational Therapist working with the Primary Care Team in Mullingar
‘It’s just so easy’
“It is user friendly. There are nice ‘How to Use’ My HSE Self Service tools available that my manager gave me but actually if you just log on it’s not complicated. It’s not convoluted, it’s just straightforward, all the headings and boxes are so clear. It’s just so easy.”
‘It’s flexible’
“I have used it on occasions when I have been out with HSE friends and they are not working in areas with My HSE Self Service. They are envious as I can book my annual leave at any time from my phone. I was away on holidays recently and I was able to book some annual leave days from abroad on my phone. You’re not chasing your manager with your paper leave card for approval of annual leave, you just log on to My HSE Self Service, submit your leave request and it’s gone to your manager.”
‘It’s a time-saver’
“You know how much annual leave you have remaining, and you’re not again chasing your manager to find out how many hours/days you have left. It is all just really clear, you can see your calendar, you can see what has been submitted and what has been approved.”
‘It is so easy to get set up for expenses and also for submitting expenses’





“My HSE Self Service is so easy to get set up for and to submit expenses. You can see what you have submitted,
“The first major benefit is it has gotten rid of annual leave cards. Sta can log on themselves to the system and take control of their own annual leave, it takes it out of the manager’s hands completely and I find it really helpful in that regard. Before, you would have to dig out the annual leave card, get an email from the sta member, they would have to meet you to sign the annual leave card as some of them are on shift work, the manager would then have to manually deduct the correct amount of leave, that has now all been taken away because of My HSE Self Service.”
The benefits of the Leave Calendar
“Once I got all of my sta signed up on to My HSE Self Service they were all up on the leave calendar. I can get an overview of the entire month, I can see who is on annual leave, who is due to take annual leave, who is on sick leave, maternity leave, and everything is there on the calendar as soon as I log in.”
Emergency Leave Requests – A Substitute
“I also have a substitute set up for when I am o and it works very smoothly. If a sta member needs leave when I am o my colleague is set up to approve and it works absolutely fine.”
Speaking about the NiSRP implementation, the Programme Director said, “To date the NiSRP Programme has delivered for over 62,000 sta members across the East, South-East, Mid-West, North-West and Midlands. This number will grow to more than 80,000 when extended to sta in the South in just over 19 weeks’ time."
To get further support in using My HSE Self Service please use the following link: https://healthservice. hse.ie/sta /my-hse-self-service-support/
| 35 HEALTH MATTERS WINTER 2022
Advancing Organisation Development to Support Service Integration
Susan Healy, Comms and Digital Officer, Organisation Development, in conversation with Organisation Development Practitioners Lisa McDaid and Elaine Birkett
The HSE is an organisation embarking on a journey of planned change. With new Regional Health Areas (RHAs) emerging to enhance the delivery of integrated care, change is inevitable. Though it can be disruptive people and culture change is an integral part of delivering new models of care. To enable this, the HSE has been working to build capacity for change through Organisation Development (OD) resources and supports.
OD aims to support our organisation in thoughtful and practical ways. The focus is to help build readiness and the conditions for change. Supporting service teams through the challenges that change implementation brings to improve integration and collaboration.
We took 10 minutes with HSE Organisation Development Practitioners Lisa McDaid and Elaine Birkett to discover more about the role OD has in supporting leaders and teams across services, to achieve this evolving integrated service model. In 2022, Lisa and Elaine attended the Advanced Organisation Development practitioner programme at The King’s Fund in the UK. Here they share some insights into the impact OD can have for our organisation coupled with their professional experience in the health service.

What leadership style is emerging as the most needed in organisation transformation right now?
Lisa: New models of compassionate and collaborative leadership are needed to address the challenges of implementing an integrated care model. Our leaders need to develop strong networks, supportive alliances and trusting relationships within and across organisational, professional and geographical boundaries. We have a workforce of highly capable, committed and enthusiastic people, including skilled and dedicated leaders. Because our system is
changing we need to shift towards a new leadership approach, a leadership approach that moves towards collective leadership. It is a fluid approach enabling anyone with expertise for a particular task or situation to take responsibility when there is a need. This requires compassionate leaders who enable responsibility across all levels.
For RHAs and integrated care models to be realised, how can OD support that?
Elaine: People working in the organisation are already highly skilled in their specialism or professional practice. Where we add value as an OD team is in building internal capacity with leaders and teams to create a culture of being more ‘change able’ in the organisation. Bringing integrated care models to life requires people and culture
change skills and our role is to help services to adopt that approach, using sound methodologies like the Health Services Change Guide. In addition we continuously develop tools and resources for teams to use in a practical way. As a team we create connections across the organisation’s boundaries to promote more integrated supports for frontline teams, which is ultimately about ensuring the best outcomes for patients and services users.
What are the conditions needed to improve in areas such as quality, change and innovation?
Lisa: Creating a receptive environment to enable people to embrace the desired change is essential. The People and Culture Change Platform represented in the Health Services Change Framework identifies the
HEALTH MATTERS WINTER 2022 36 | Making Progress on Integrated Care
Lisa McDaid, Elaine Birkett, Organisation Development and Change Practitioners.
key priorities that shape culture, mobilise change and deliver better outcomes. The nine priority areas help create the conditions for change. We need to connect our e orts and attend to each element in more joined up ways. This will assist us to deliver integrated services.
Who are the change leaders in this organisation?


Elaine: It’s an interesting question in that it implies there is a specific group of change leaders. In the Change Guide we say ‘Change is everyone’s responsibility’. I’ve always liked that and continue to advocate for people to feel they have permission to innovate and bring about change. That is key for our health service to strive. Naturally, there are people with defined roles for delivering change but the pandemic shone a light on so many people as catalysts for change that may not have been obvious beforehand, we need to continue that opportunity for the greater good.
Is it important to understand the tools to influence the OD agenda at strategic level? Why is this?
Lisa: OD practitioners have many hats to wear in an organisation. They need to have strong networking and influencing skills. They must be able to align their work to meet the organisation's priorities. We work with many national and local programmes


to build internal capacity for change. We will be supporting the RHAs and the significant complexity of that – to ensure momentum and the right outcomes will need ‘investors for change’ and that is part of the role, to spark that buy-in and support a coalition for change that will enhance our health service. As a team we look forward to continuing to support those priorities.
Now that you have completed the King’s Fund Advanced OD Practitioner programme what insights are you bringing back to the team and service?
Elaine: It gave us a good sense that we are in the right place with the approaches we are taking as a team to build capacity for change skills across our organisation. We work hard to make sure that the OD resources we provide to leaders and teams on complex change are best practice and fit for their needs. Being on the programme validated that work, which was a rming.
Lisa: It is really important in our role to keep up to date in relation to the evidence on change and innovation. It provided useful insights about Organisation Development approaches to integrated care which were successfully deployed in the NHS and other similar sectors.
The King’s Fund programme is designed for experienced Organisational Development (OD) practitioners to develop and deepen their understanding of the possibilities for OD in current health and social care settings.













To support leaders in developing a systemic view in their work and to develop skills as a relational practitioner.
The programme o ers insights into engaging the frontline and experts in the field, creating the conditions for quality improvement and compassionate and collaborative leadership to enable and support growth.
Both Lisa and Elaine are Organisation Development Practitioners with OD, Change & Innovation.


Lisa has managed a number of large scale multiple site reform programmes and teams involving significant cultural change. Lisa uses her experience of leading transformation in complex environments to support those leading change and innovation, frontline teams and business support services to focus on people and culture and create the conditions for change.
Elaine has been in the Irish Health service for almost 19 years working across a range of locally led services initially and is positioned at a national level working with Organisation Development, Change and Innovation. Elaine brings a lens of Human Behaviour, Change Coaching & Mentoring and systems thinking to her work as an OD Practitioner, supporting leaders and teams navigate the complexity of people and culture change coupled with her organisational knowledge.
To find out more about HSE Organisation Development, Change & Innovation supports contact us on: Email changeguide@hse.ie Visit www.hse.ie/changeguide Follow us on Twitter @HSEchange_guide






| 37 HEALTH MATTERS WINTER 2022
I’ve always liked that and continue to advocate for people to feel they have permission to innovate and bring about change. That is key for our health service to strive.
a role model to my colleagues by genuinely living the behaviours’
Values in Action (ViA) was re-launched in Community Healthcare East (CH East) earlier this year. A shared learning and networking event for Champions took place at the end of September.

As part of this event Ellen Badal Tamayo, Clinical Nurse Manager 2 in Clonskeagh Community Nursing Unit (CCNU), shared her experience of being a Values in Action Champion and how the behaviours have supported her, her colleagues, and the residents in their home in the Nursing Unit.
ELLEN’S STORY
Ellen Badal Tamayo, Clinical Nurse Manager 2, Clonskeagh Community Nursing Unit

Iwas introduced to Values in Action by my colleague who came back from the launch of ViA in CH East way back in 2019. I immediately felt very committed to be part of this change.
Firstly, the 9 behaviours in ViA fully complimented the current change CCNU was undergoing at the time. We were changing from a Medical model of Care to a Social Model of Care which was called at that time Butterfly Household Model of Care. It gave strong emphasis that 'Feelings matter most'.
When I was reading about the 9 behaviours it made me feel that this is allowing me to be a better and kind person at work and that I could promote a positive work environment by living these behaviours. It allows me to look after myself, my colleagues and the service user.
Posters and information about ViA were put up here in CCNU. We were also involved in a focused week of ViA activity entitled ‘All in A Week’s Work’ which promoted one behaviour at a time. This week was great in getting other people involved. When we noticed somebody living one of the behaviours we acknowledged it with a sticker – it was funny some people by the end of the day had stickers all over their clothes – definitely living their values!
I genuinely believe though that the 9 behaviours helped sta to overcome challenges at the most di cult time in healthcare. Sta were there for each other and also did everything in whatever capacity they can to put a little normality and a smile back on our resident’s faces. Lastly, sta looked after themselves to ensure that they are healthy enough to come to work no matter how di cult the situations may be. Sta shone the brightest during that darkest time.
There is a positive work environment here in Clonskeagh. Sta are always willing to help each other and provide a positive lived experience for the people we look after. We still have a lot to improve and as a ViA Champion I endeavour to promote these 9 behaviours among sta . We have put back ViA posters again (all posters except IPC were removed) and will organise activities to promote the programme again.
However, I think the best promotion is through myself, being a role model to my colleagues by genuinely living the 9 behaviours. Championing the 9 behaviours is not always easy but what is good about this is that there are other colleagues in other areas we can ask for support. May we all continue to be an inspiration to others.
HEALTH MATTERS WINTER 2022 38 |
‘Being
Ellen with her colleagues Bindu George, Assistant Director of Nursing; and Rainu Ruth Raju, Sta Nurse, Clonskeagh Community Nursing Unit, at the recent ViA Champions event.
LEADERSHIP SUPPORT
Martina Queally, Chief Officer for Community Healthcare East
Martina Queally, Chief O icer for Community Healthcare East, also spoke at the recent event and emphasised the importance of a positive culture in supporting sta through significant change.
“When we talk about culture, unless we have some way of doing it, it’s like trying to catch smoke.
In finding some way of building that positive culture you need tools to help you, this is why ViA is valuable, it doesn’t just talk in theory, it’s practical,” she said.
Martina spoke about the complex changes facing community healthcare. “They require us to work together through radical
integration – planning together, bringing intellects and ambitions together to share resources to do things di erently… we will not do that unless we have a culture built on solid foundations of mutual respect and trust, and all of the actions in Values in Action are mission critical for us to do that.”
What’s next for ViA in CH East
The project team now plan to focus on supporting the community of Champions as they spread the behaviours throughout their workplaces across CH East. If you would like to hear more about Values in Action in CH East, please email ValuesinAction.CHEAST@hse.ie.
In the HSE we strive for a culture where sta feel valued and supported to be the best they can be where there is a common sense of purpose and pride in the team. Values in Action is about putting the values of care, compassion, trust and learning at the core of everything we do in the health service. As one of our Champions likes to say, ‘It’s for ourselves and it’s for our patients.’ Values in Action Champions are nominated by their peers to lead the social movement in their workplaces through living and spreading the 9 behaviours.
If you are curious about improving the culture in your own workplace; if you are interested in finding out how you can get involved with the Values in Action movement; or if you have a Values in Action story to share, feel free to email the ViA National Team at info.valuesinaction@hse.ie; and join the conversation on twitter @HSEvalues, using the hashtag #WeAreOurValues.

| 39 HEALTH MATTERS WINTER 2022
Caption - Martina Queally, Chief O icer; Achmat Isaacs, Network Manager CHN5, and ViA Project Team member; and Bronwen O'Donoghue, Admin Support, Community Healthcare Network 5 (CHN5), Community Healthcare East
CELEBRATING
Excellence
Excellence
Awards again showcase the great work happening across our health service
The Health Service Excellence Awards is an opportunity to showcase and celebrate examples of the great work that happens every day across our health service. The awards also promote shared learning for other teams through our awards success stories.
“The awards themselves are really about outcomes for patients, outcomes for the public, things that make people’s lives better. They might have different solutions. Some of them might be ICT, some of them might be patient fronting, but they are not about us celebrating ourselves, they are celebrating the experience of people getting better,” said HSE Acting CEO Stephen Mulvany.
Also in attendance was Minister for Health Stephen Donnelly, who added, “What really struck me was the energy, the passion, the pride. It’s incredible to see. Everyone here is an innovator.”
recognition and validation of what they’re doing every single day.” Kate Cassidy, whose project to help pregnant women and their family to quit smoking wwas the category winner in Excellence in Quality and Patient Safety, said, “it’s brilliant to have a day like this for sharing of ideas. Already we have spoken to teams that we definitely intend reaching out to and scaling up their projects in our own area.”
Donal Cassidy, category winner, Improving Patient Safety, with the rapid COVID-19 testing among the homeless in Dublin, said, “The importance of a day like this can’t be underestimated. It has meant so much to all of the staff that we’re working with, and the recognition has generated huge energy and goodwill and ongoing support. It has really re-energised all in our team.
“The importance of a day like this can’t be underestimated. It has meant so much to all of the staff that we’re working with, and the recognition has generated huge energy and goodwill and ongoing support. It has really re-energised all in our team."
Monica Clancy, winner in the Innovation in Service Delivery category, for the FEES speech and language project in the Midwest, said, “I think it is really important for clinical staff to get the opportunity to showcase the good work that they are doing. There’s lots of amazing work going on out there and it’s about encouraging people to bring their projects forward and have that
Laura Tully, winner in the Right Care, Right Place, Right Time category for the Student Sexual Health Service in TUS in Athlone, highlighted the benefits of the awards, “I feel very motivated today because we’ve just been in a room with people celebrating the good work that happens in our health service. And this is not the end of the road. I think people have kind of got a contagious passion and definitely a drive now and a motivation to keep moving forward and keep improving things for our patients.”
NON-JUDGEMENTAL SERVICE DELIVERS FOR STUDENTS ON CAMPUS
A pioneering nurse-led student sexual health, contraception and health promotion service located in the Technological University of the Shannon Midlands West (TUS) in Athlone has taken the Sláintecare Integration Award – delivering Right Care Right Place Right Time.
The service was funded through the Sláintecare Integration Fund back in 2020 and now will receive funding from the HSE.
“The reason we needed this service was unfortunately because there wasn’t
a service in the area and students were faced with barriers such as travel time, costs, stigma, embarrassment, so we’re really pleased now to have overturned that,” said nurse Laura Tully, Project Lead, CNM, Student Sexual Health Service, TUS and CHO8.
Dr Tom Walsh, GP, Clinical Lead, Student Sexual Health Service, TUS, explained, “It has led to a much higher level of consultation. It’s building all of the time and we’re seeing increasing numbers and a much higher rate of consultation relative to prior to this when
they had to use tertiary services.”
Saoirse Mulvihill, Vice President for Welfare, TUS Students’ Union, said the non-judgemental nature of the service is key to its success.
“It’s a really safe space here. It’s completely safe from judgement and it’s within the students’ comfort zone. Students come here, they are not going to be judged for any of their questions. They know Laura has heard it a hundred times before. From our feedback survey of people using the service, 100% of them would recommend it,” said Saoirse.
HEALTH MATTERS WINTER 2022 40 |
RAPID COVID TEST RESULTS FOR HOMELESS POPULATION SAVES TIME AND DISRUPTION
Rapid COVID-19 testing in the Dublin Homeless Services won the Improving Patient Experience Award for the HSE CHO9 Social Inclusion team.
Dr Austin O’Carroll, Clinical Lead, HSE Homeless COVID Response Team, explained, “One of the things we did during the COVID response was we isolated people from when they became symptomatic. We then had to wait for the test results. Most people, practically four-fifths of people that we moved into this isolation stayed for 48 hours and then tested negative and were able to leave. This meant that we had nurses, isolation specialists, key workers employed to
support a huge amount of people that didn’t need to be in isolation.
“This test produced huge efficiencies. It meant that we could save money because we didn’t have to staff the isolation unit for as many people. But it also saved on client time and disruption. They didn’t have to rush off and spend two days in a place they didn’t need to be.”
The testing machine is highly portable so they could bring the machine to the person either in their hostel accommodation or unfortunately if they were sleeping on the streets they could bring it to them there in the mobile health unit.
Donal Cassidy, General Manager, Social
Inclusion and Addiction Services, CHO DNCC, said that COVID has acted as a pilot for the testing regime and they are confident it can be used with a variety of other health conditions.
“We see that we can build upon this learning and the inter-agency approach, not just look at COVID, we’re now looking at many other health conditions. We’re working with the agencies around more effective case management in care and really when you look at the most vulnerable, the people who cannot navigate our system, who have poor levels of English, we cannot do any more than bringing the care to that person,” he said.
SPEECH AND LANGUAGE SERVICE BROUGHT FROM HOSPITAL SETTING OUT INTO THE COMMUNITY
The winning project in the category of Innovation in Service Delivery was a speech and language service usually delivered in a hospital, but through innovation was extended to the community in the Mid West.
The Mid West Community Healthcare (MWCH) Mobile Fibreoptic Endoscopic Evaluation of Swallowing (FEES) Service was the award winner for the Mid West Community Healthcare Speech and Language Therapy Services.


Paula Cregg, Speech and Language Therapy Manager, explained, “The project became a possibility when we recruited additional speech and language therapists in the Mid West in 2021. These therapists had the skillset and competencies to train other speech and language therapists and allow for the development of communitybased FEES services.”
Monica Clancy, Senior Speech and Language Therapist, said, “FEES is a very well established swallowing diagnostic
test. What’s novel and unique about this project is that we have taken FEES out of the acute setting and delivered it safely and efficiently in the community setting.
“It’s really exciting for us as a team to be at the fore of such an exciting movement within speech and language therapy. I think it will really change how we do our jobs.
“Up until now, FEES was only available for inpatients within UHL in Dooradoyle in Limerick. There was zero access for community-based service users to have a FEES locally and if they needed a diagnostic test like this, they would have had to travel on their own steam to a private provider in Dublin.”
The team have also liaised with the HSE Organisation Development and Design team and plan to use the Change Guide resource to document the stages of their project and demonstrate their capacity to change how they delivered their services and achieve sustainable service improvements for the people they serve.
| 41 HEALTH MATTERS WINTER 2022
lntegration Award: Dr Dominic Rowley; Sarah La Cumbre; Laura Tully, Project Lead; Paul Reid, HSE, Frances O' Connell; Dr Thomas Walsh; Audrey Doyle. Innovation in Service Delivery: Elaine Whelan; Elaine Kerins; Paula Cregg; Monica Clancy; Yvonne Traynor, HSE Board; Kate Hayes; and Sarah Curran.
QUIT PROJECT LIBERATES PARENTS FROM SMOKING
A non-judgemental quit smoking programme for pregnant women and their families has been hailed a huge success and earned the Health and Wellbeing team in CHO5 the Excellence in Quality and Patient Safety Award.
Kate Cassidy, General Manager, South East Community Health Care (CHO5) and Project Manager of ‘Supporting Pregnant Women and Extended Family to Quit and Stay Quit’, explained that the Sláintecare-initiated project which was a co-designed proposal which meant they involved pregnant women, all their integrated services around acute hospitals, and anybody who could
intervene with a pregnant woman.
“The endgame of this project was that we would intervene with every pregnant woman in the south east who was a smoker. And that we would do it in a very client-centred, non-judgemental way,” she said.
David Phelan, Health Promotion Officer, explained that they were able to get over 1,500 people referred into the project, way exceeding expectations.
“When I started I was sceptical myself. Would we even get the referrals? We set a target of 500 referrals within the year. We completely surpassed that. The nonjudgemental service delivered in the right
INFECTION MANAGEMENT SYSTEM KEY TO CONTAINING COVID ON BEAUMONT WARDS
An Infection Manager System has earned a team at Beaumont Hospital the top prize in the Engaging a Digital Solution to Provide a Better Service category.



Emma Ryan, ICT project manager and Project Lead, Beaumont Hospital, said the Infection Manager System meant that laboratory results were fed in real time into a database.
“Patients were flagged immediately throughout the hospital systems, information on infection status was available to everybody at point of use and then displayed on a dashboard,” she explained.
Eoghan De Barra, Consultant in Infectious Disease, said it was a great help for the staff during the COVID-19 pandemic.
“We integrated in the vaccination status, the national COVID testing, so we had everything we needed to know about a patient in one place electronically to decision-makers. So that speeded up those decisions,” he said.
“This can definitely be used for other infections. It was built out of the need for COVID but there are many other infections that pose similar challenges in a hospital environment. So the second generation of this has moved on to look at hospitalacquired bacteria, MRSA, CPE, C-diff, and indeed once monkeypox came along, we were able to plus that into it. So it’s an adaptable platform that can flex to whatever comes next.”
Shaini Gangadharan CNM3, Infection Prevention and Control, said the process became ‘really seamless’.
“The new system enabled us to generate the contacts of COVID-19 positive cases in real time just with a click,” she said.
Clockwise from top: Improving Patient Experience: Dr Gabriel Fitzpatrick; Brian Kirwan; Dawn Russell; Dónal Cassidy; Anne Marie Hoey, National Director, HR; Hannah Dineen. Excellence in Patient Quality and Safety: Dr Derval Howley; Mary O'Donnell; David Phelan; Kate Cassidy; Mark Brennock, HSE National Director, Communications, Colm O’Connor; Engaging a Digital Solution: Prof Karen Burns, Emma Ryan, Shaini Gangadharan, Dr Eoghan De Barra, Stephen Mulvany Chief Financial Officer, HSE, Ian O’Neill.
care, right place at the right time was the key to the success of this project.”
Kate Cassidy said the project has been hugely positive for participants.
“Once a parent achieves the ability to quit smoking, there’s a cascade model where it empowers them because they feel liberated. They feel they get back the control over their own life.
“We will continue to work with pregnant women because we know they need expert help to quit. The evidence is there that by doing this we provide a really quality service to the women of the south east and their extended family.”
HEALTH MATTERS WINTER 2022 42 |
Your Mental Health
health difficulties
One in two people in Ireland have experienced mental health difficulties and a new national campaign, responding to research findings, is highlighting the common signs to look out for and encouraging people to find help and support on yourmentalhealth.ie
Often when someone isn’t feeling themselves and this feeling persists, it can be hard to recognise what’s going on or they just accept it as part of their normal daily life. Ongoing stress, low mood anxiety or sleep problems, which are common mental health difficulties, can seem unconnected but they are part of our mental health and are telling us to seek support.
As well as personal support, research respondents were also interested in online, mobile apps and text supports, which are available or signposted on yourmentalhealth.ie/ The site has been re-developed to better meet the needs of people searching for self-help and other supports. These resources include:
• ‘Stress control’ a HSE sponsored online programme can help you to recognise stress, how it is affecting you and more importantly help you overcome these feelings.
• ‘Minding your wellbeing’ videos can help you develop a positive outlook using mindfulness, gratitude, self-care and resilience.
Online cognitive behavioural therapy can help you to change specific negative thoughts and behaviours that are causing current and ongoing stress and anxiety. HSE employees can access free counselling through the Employee Assistance Programme. Call 0818 327 327 to speak to someone who can help.
According to Mark Smyth, a senior clinical psychologist with the HSE, “Recognising common difficulties such as anxiety is an important first step in looking after your mental health. If you notice that you’re not feeling yourself and have ongoing stress, sleep problems or anxiety the best advice is to act sooner rather than later. Don’t wait for it to get worse. Being comfortable in talking to someone you trust or seeking support will make a difference. Whether it’s mindfulness,
taking part in a stress control programme, signing up for online cognitive behavioural therapy or trying online counselling, there are supports available that will suit you and how you’re feeling.”
Yvonne O’Neill, National Director – HSE Community Operations, added “We are encouraging people to reach out and find support that can help. The HSE partners with many different mental health organisations to provide supports to people of all ages with
different needs. More recently the HSE and its partners have made available a number of new digital health options including innovative online, text and phone supports. The re-development of yourmentalhealth.ie will make it easier for people to access these supports.”
Just not feeling yourself, ongoing stress, low mood, anxiety or sleep problems visit www.yourmentalhealth.ie to find support that can help.

| 43 HEALTH MATTERS WINTER 2022
New HSE campaign encourages people to find support that can help with common mental
LE CHÉILE
New staff network for HSE employees with a disability: the Le Chéile Network
The establishment of Le Chéile Network, the HSE’s first sta network for employees with disabilities, was marked with great enthusiasm and energy when the HSE sta network's first meeting took place.
Supported by the HSE’s Diversity Equality and Inclusion team, the Le Chéile Network aims to promote a positive working environment whereby all employees feel supported and valued. Le Chéile is an Irish word meaning “together”. For Network members, that means together they will work towards creating a positive and inclusive workplace culture where all individuals are treated with dignity and respect.

The term ‘disability’ is used to reference many di erent conditions that can be either visible or invisible. This may include visual, hearing, mobility, learning, speech, neurological and other types of disabilities. Di erent definitions of disability are used in di erent contexts, for example to set eligibility for services, or to outlaw discrimination on grounds of disability. There can also be a wide range of di erence between how individuals with a particular condition are a ected, ranging from mild to severe di culties.
Globally, it is estimated that 10% of the workforce has a disability. It is hoped that the creation of the Le Chéile Network will help HSE sta feel more comfortable disclosing information about a disability to managers and colleagues and raise awareness about the importance of disability inclusion across all parts of the HSE.
“The establishment of a network for sta with disabilities is an important step in engaging with employees and allies” said Maria Barry, Diversity Equality and Inclusion Manager in the HSE’s National HR division. “The Le Chéile network will act as a representative voice for sta with disabilities, a forum where sta can discuss experiences and share insights in a safe space, and a
resource on disability-related topics. It is estimated that 70% of us will be a ected by a disability at some point in our lifetime so it’s really important that we create a culture of disability inclusion and awareness in the HSE”.
The benefits of sta networks, also known as Employee Resource Groups (ERGs), have been well documented. Sta networks provide a forum to connect with other sta who may have similar experiences in the workplace and an opportunity for sta to contribute personal stories and experience into policy and practice. “I joined the network because I wanted to be part of a bigger group of people with disabilities who share similar experiences as myself,” said Kellie O’Farrell, Occupational Therapist and member of the Le Chéile Network. “I want to be part of a group where I can advocate for my rights to ensure that I am working in an inclusive, positive work environment”.
“There needs to be a group together to build this cohesiveness and there’s power in people with di erent experiences and levels within the HSE. You can be isolated with a disability so it’s nice to be able to share your experiences with others. It brings a bit of camaraderie and fun,” said Cathy Heely, Senior Social Worker, Family Therapist and Le Chéile Network member.
HEALTH MATTERS WINTER 2022 44 |
The new HSE Le Chéile Network team.
“The Le Chéile network will act as a representative voice for staff with disabilities, a forum where staff can discuss experiences and share insights in a safe space, and a resource on disability-related topics."
Networks also assist with raising awareness on issues to the wider workforce such as the importance of inclusive communications and the provision of workplace adjustments (or “reasonable accommodations”) for sta with disabilities. The Employment Equality Acts 1998 – 2015 oblige employers to consider appropriate measures which they could take to support a sta member to carry out their day-to-day duties. Reasonable accommodations take a variety of forms and can include adapting a workplace premises, providing equipment or assistive technologies or providing training or other supports that might help a sta member person carry out their work.
Managers play a key role in supporting sta with disabilities in the workplace.
“Inclusion and diversity modelled through compassionate leadership promotes comradery, teamwork, creativity and innovation,” said Dr Patricia Walsh, Consultant Psychiatrist/Clinical Lead for a Psychiatric MDT and Le Chéile Network member. “Managers benefit from leaning in, listening to and learning from the challenges of minority groups, whose voices may be quieter than others. Instead of seeing disability, I look for ability.” Patricia added, “The phrase ‘What we walk by we stand for’ reminds us that it is our responsibility to highlight discrimination and champion equality for all minority groups.”
Part 5 of The Disability Act 2005 places a duty on public bodies to recruit people with disabilities and provides for a target of 3% of the workforce with a disability. It also places a duty on public bodies to support access to services and facilities for people with disabilities.
Pat Fallon, Assistant Sta O cer and Le Chéile Network member, has said that, “The HSE, the largest public sector organisation, can be a leading light in relation to the employment of people with disabilities. Please see our ability not disability.”
The Le Chéile Network meets virtually, every two months. If you are interested in finding out more about the Network or would like to join, please contact diversity.HR@hse.ie
International Day of Persons with Disabilities (IDPD) is a United Nations day that is celebrated every year on December 3rd.
The day is about promoting the rights and well-being of persons with disabilities at every level of society and development, and to raise awareness of the situation of persons with disabilities in all aspects of political, social, economic, and cultural life.
The WHO joins the United Nations in observing this day each year, reinforcing the importance of securing the rights of people with disabilities, so they can participate fully, equally and e ectively in society with others, and face no barriers in all aspects of their lives.
ON STAMMERING
Stammering is a communication impairment that is widely misunderstood. Stammering, also known as stuttering, is a neurological disorder that a ects speech production. Because of the nature of this disability, the intensity of the stutter can vary. Depending on the day, a person’s stammer may appear seldom or may significantly a ect their daily interactions.
Sandra Kelly, who has been working in the HSE for 16 years, is based in the O ice of the Chief O icer for the Dublin South, Kildare & West Wicklow Community Healthcare Organisation and has a stammer. Sandra shared some examples of how stammering can a ect her day-to-day work.

“Due to my stammer, I may give a slightly delayed response during a meeting or when giving a presentation. Colleagues can sometimes misinterpret a Wstammer as being rude if I am delayed in saying “hello”, “good morning”, or responding to a question”. In 2020, Sandra did a live interview on one of Ireland’s most listened to radio programmes, the Ryan Tubridy Show, and shared some further examples of the impact of stammering on her day-to-day life outside of work.
Even though stammering is now widely recognised as a neurological disorder that can be acquired, people who su er from it still experience social stigma.
“A stammer has nothing to do with a person’s intelligence, people often misinterpret it as a mental health disorder. From my experience, people often do not see stammering as a disability; it’s not taken as seriously as other disabilities” said Sandra.
Managers can support sta members with a stammer by creating a safe space for individuals to share their experiences in the workplace and by providing them with the same opportunities for
development and learning.
The recently established sta network for employees with disabilities, the Le Chéile Network, can provide support and advice. “It gives people with disabilities the opportunity to discuss any workplace challenges with other members of sta with a disability,” said Sandra.
Sandra o ered some practical ways in which individuals can support a colleague with a stammer in the workplace.
“Give your colleagues time to finish their sentences without interruption. Interrupting someone can actually make a stammer worse. Include individuals with a stammer in conversations and don’t assume that just because they have a stammer, that they don’t want to contribute to a discussion.
Reasonable accommodations for sta members with a stammer can have a very positive impact on them and their work performance. By joining the Le Chéile Network, I can now share information and resources on stammering awareness with my work colleagues.”

International Stammering Awareness Day is celebrated annually on October 22nd and aims to raise awareness of the issues faced by individuals with a stammer.

If you would like to join the Le Chéile Network, contact diversity. hr@hse.ie

| 45
HEALTH MATTERS WINTER 2022
A SPOTLIGHT
LIVINGWELL

Living Well Programme empowers people to manage their long-term health condition



The Living Well programme began in 2019 as a Sláintecarefunded project in six Community Healthcare Organisations (CHOs) and has since developed into a HSE-funded programme, mainstreamed in these areas since January 2020. Furthermore, two more CHOs have started to deliver this evidence-based programme.
Since 2020, 253 programmes have been delivered to 2,700 participants across Ireland and their participation in the Living Well Programme has been either online or in person.





What is the Living Well Programme?









‘Living Well - A Programme for Adults with Long-term Health Conditions’ is an evidence based self–management programme. Over the course of six weeks, participants develop practical skills and confidence to better manage their chronic or long-term health condition. Workshops are delivered by two trained leaders, one or both of whom are living with a long-term health condition (peers).
Unlike clinical education programmes which may focus on education and clinical management, Living Well focuses on developing and enhancing the self-management skills of those who complete the programme. In this way, it complements regular treatment and structured patient education programmes.

The evidence for the Sláintecare-funded Living Well Programme in Ireland
By supporting people to self-manage, the Living Well programme aims to reduce unscheduled care admissions and can provide a suitable post discharge self-management programme to aid recovery, and in turn contribute towards a reduction in acute care re-admissions. The Living Well Report March 2022 demonstrates the value of the Living Well programme in supporting participants to become e ective selfmanagers and active partners in their healthcare.


WHO IS LIVING WELL FOR?
Living Well is for adults 18 years and over who are living with or caring for someone with a long-term health condition(s).
Living Well is not suitable for people with significant memory or learning di iculties.
HEALTH MATTERS WINTER 2022 46 |
I am a 48-year-old mother of five, ranging in age from 6 to 22, and I have su ered with Chronic Pelvic pain for 17 years following multiple pelvic surgical procedures. I continued with physiotherapy and Pilates workouts and I did manage to keep my symptoms from getting worse but I was never without pain in my pelvis.
After the birth of our fifth child, by C-section, I also began to have chronic bladder pain, pressure and discomfort. A combination of conditions and the pain caused by them has had a harrowing e ect on my relatively young life. I cannot sit for long periods, so driving, taking a flight or even going to the cinema is very hard for me. Intimacy has had many challenges and this has been so very di icult for myself and my husband. Exercise, shopping and most lively activities are not possible for me due to pain and incontinence. I cannot dance any more at weddings or family events and getting a good night’s sleep is a rare and precious gift.
My GP has been a great support to me and over the years I have come to rely on a routine of various medications and a Tens machine to help me get through my day. These treatments all come with their own side e ects, which also need to be negotiated to allow me to work and raise my family.
Chronic pain left me feeling depleted and defeated, I just wanted to cry and I decided I needed a di erent kind of help. A kind that would help me find
a way to cope. I took out my phone and typed “dealing with pain” into the search engine. I found the website of Chronic Pain Ireland who informed me about the Living Well programme with the HSE. It was a revelation and a truly life changing conversation. In that hour my life became mine again and after going through the resources that were recommended I came to realise that I was not just in Chronic Pain I had Chronic Pain. Chronic Pain Ireland sent a supportive email with links to the HSE Living Well programme. I called my local o ice and spoke with Áine and she was incredible. Before I knew it I was enrolled on the next available course and the course materials, including the “Living a Healthy Life with a Chronic Condition” handbook, were sitting on my kitchen counter. The course was delivered by webex and my employer was happy to allow me to take the time I needed to participate every Tuesday morning for 6 weeks.
The course was delivered by two wonderfully kind and e icient ladies who themselves su ered with chronic illnesses. I knew that I was truly heard and my issues were understood. It was reassuring to hear that the selfmanagement skills and tools, they were teaching us, that they were using them on a daily basis in their own lives. They were not just delivering the course to us, they were participating in it with us.
I learned techniques to use my mind and imagination to distract
me from my pain and help me relax. This helped to take the edge o flare ups. I learned to be kind and patient with myself and I learned ways to communicate to my family, how I was feeling and more importantly how to ask for help during flare ups, how to cope with feelings of low mood and di icult emotions. We were taught the importance of making good decisions and weekly actions plans and were instructed on how to follow through with these. The course included information on the importance of diet, movement and exercise.
During the six weeks I shared my life with others that were all su ering with various chronic illnesses and we had many tearful, serious and sometimes hilarious discussions that were hugely beneficial to me and gave me solid support to put the selfmanagement skills that I was learning into everyday practice.
After the six weeks were over, I was in a much better place. I felt more in control. I didn’t feel hopeless anymore and, most importantly, I accepted my condition would have good days and bad days. I had a new confidence within myself on how I was going to respond to the challenges that I would face in the future.
I only have one regret about this course and that is that I did not do it years ago. I hope more people get empowered and helped by this amazing Living Well Programme.
HOW DO I FIND OUT MORE?
For Information about the programme go to www.HSE.ie/livingwell Here you will find details of upcoming Living Well programmes and contact details for the Living Well teams.
People can self-refer or can be referred by a healthcare professional. Onward signposting to supports/resources/other programmes is key at end of programme
| 47 HEALTH MATTERS WINTER 2022
‘MY ONE REGRET IS THAT I DIDN’T DO IT YEARS AGO’
Ailish tells us what completing the Living Well programme has meant for her
Dementia: Understanding Together

Finding
companionship and understanding at your local Men’s Shed.
For people with dementia and their families it is often the small things that make a big di erence.
Dementia: Understand Together is tackling stigma and isolation by raising awareness for dementia and encouraging communities to take actions that will help to include and support those a ected by the condition.



The campaign is supported by over 40 partner organisations across Ireland ranging from retail, transport, banking, health, voluntary to community sectors who, together with over 400 community champions from all over Ireland, are leading the way in creating inclusive communities.
We know that people with dementia are more likely to experience social isolation. Staying socially connected and involved in their community is vital for a person’s health and wellbeing. Keeping socially engaged can also help to reduce the risk of developing dementia. Whether that’s simply meeting a friend for a co ee, taking part in a favourite hobby, or joining in with a community group like The Men’s Shed’s.
As a grassroots organisation, The Men’s Sheds believe strongly in the autonomy of each individual shed, in which Shedders have the opportunity to maintain and improve their well-being on their own terms and within their own communities. The Sheds are


HEALTH MATTERS WINTER 2022 48 |
“Like all Sheds, we aim to be respectful and welcoming to all Men in the community. When someone wants to join the Shed, we consider that person as an individual and each individual’s situation is different."
Mise



places of belonging, mutual respect, companionship and community for all Shedders regardless of their health status.
Each Shed o ers a range of activities from woodworking and metalcraft, to card games and gardening, and everything else in between. People interested in finding out what their local Shed has to o er are more than welcome to bring a friend or relative for the first few visits until they feel comfortable. Equally, if a person needs ongoing support, it is not a problem to bring a carer along.
TP O’Gorman, a Shedder and IMSA volunteer, shared his experience.
“Like all Sheds, we aim to be respectful and welcoming to all Men in the community. When someone wants to join the Shed, we consider that person as an individual and each individual’s situation is di erent. There is not a ‘one-size fits all’ approach when it comes to Sheds. The big thing for us is to try to ensure there is a good ‘match’ from the start and to try to balance the needs of new members coming in with those of existing members (and their capacities),” he said.
“We lost one of our Shedders who had dementia not that long ago, we really miss him. We are a Shed who loves music and he was a musician. He would come to the Shed (initially with a companion) to play and listen to music, and then we used to collect him sometimes to bring him. The balance worked – but we are aware from other Shed experiences that sometimes they worry about doing the wrong thing, and about risk and responsibility.
Understanding individual’s needs when they arrive at the door for the first time is so important, I know some have suggested extra training for Sheds might be useful to help awareness and understanding as we grow older and with all the age-related conditions coming down the tracks.”
If you’d like to check out the nearest Men’s Shed to you and to arrange a visit to find out more, see www.menssheds.ie







While the “Your Shed and Dementia” manual has been developed primarily for members of the Irish Men’s Sheds Association, anyone with an interest in dementia is welcome to check it out at www.understandtogether.ie/trainingresources/helpful-resources/publications



Portiuncula University Hospital (PUH), with support from the National Dementia O ce, has launched ‘Seo Mise - This is Me’, a quality improvement initiative developed by PUH’s occupational therapy and medical social work departments. It includes a Dementia Resource Pack which has been designed to empower patients and families to make e ective decisions and choices regarding their future care. The four medical and surgical wards at the hospital will also have access to a Dementia Activity Box suited to individuals requiring stimulation with therapeutic intervention.
Siobhan Coen, PUH occupational therapist, explained, “Approximately one in three patients aged 70 and older admitted to Irish hospitals have dementia and this figure will increase annually as the population ages. People living with dementia are among the most vulnerable patients in hospital. They are often older, frail, and very prone to delirium, falls, pressure ulcers, and malnutrition which are key safety issues in hospitals.
Another part of the initiative is the introduction of a Dementia Activity Box to enhance the patient’s experience at the hospital.
Speaking of the importance of the Dementia Activity Box, Siobhan said, “The Dementia Activity Box aims to promote a more cognitively stimulating environment for our patients with dementia. The box is equipped with a variety of both traditional and new technology products such as jigsaws, conversation balls and iPads which will be used to cognitively stimulate patients and hopefully better build relationships among sta and their patients. These products are evidence-based to facilitate engaging conversations, stimulate senses and promote reminiscence between patients with dementia, sta and carers. It will support optimum health and wellbeing during the patient’s hospital stay and help reduce the anxiety and confusion that can occur whilst in an unfamiliar hospital environment.”

| 49 HEALTH MATTERS WINTER 2022
Portiuncula hospital launches ‘Seo Mise - This is Me’ to enhance quality dementia care
Seo
Siobhan Coen, Occupational Therapist, Portiuncula University Hospital talks about the ‘Seo Mise – This is Me’ initiative and interacts with patient Edward Egan using the Dementia Activity Box – https://www.youtube. com/watch?v=BtoHLAjiYGo
Siobhan Coen, occupational therapist; and patient Edward Egan.
Webinar on ‘Promoting a culture of safety’
The HSE National Dementia O ce, together with the National Safeguarding O ce, hosted a webinar on non-cognitive symptoms of dementia to coincide with World Alzheimer’s Day. This webinar, entitled ‘A focus on non-cognitive symptoms of dementia: Promoting a culture of safety’, was targeted at sta within and outside the HSE, as well as people living with dementia and family carers of people living with dementia.
The webinar had almost 700 participants on the day and you can watch it back on the Dementia Pathways website: https://dementiapathways.ie/education-and-training-additional-educationresources/a-focus-on-non-cognitive-symptoms-of-dementia-promoting-a-culture-of-safety
Speaker presentations were followed by a moderated question and answer session with speakers where attendees were a orded the opportunity to raise questions with the panel of speakers. This facilitated an interesting discussion.
The majority of attendees were HSE sta but there were many from other backgrounds including private nursing homes and care providers, intellectual disability services, Alzheimer’s Society of Ireland, academia, people with dementia, and family carers of people with dementia.
This webinar formed part of the communication and engagement work package of the Implementation Programme for National Clinical Guideline No. 21 (Appropriate prescribing of psychotropic medication for non-cognitive symptoms in people with dementia). This two-year implementation programme commenced earlier this year.
New Module
New HSeLanD module on support pathways for people with non-cognitive symptoms of dementia
To keep up to date with progress of the implementation programme, see https:// dementiapathways.ie/ resources-for-practice/ implementation-ofnational-clinicalguideline-no-21
The National Clinical Guideline on ‘Appropriate prescribing of psychotropic medication for non-cognitive symptoms in people with dementia’ was published by the Department of Health in December 2019 to guide the appropriate use of psychotropic medication for non-cognitive symptoms being experienced by people living with dementia. The National Dementia O ice HSE is now rolling out the clinical guideline through a comprehensive implementation programme.
As part of the implementation programme a HSeLanD module has been developed. This module, called ‘Support pathways for people with non-cognitive symptoms of dementia’ is targeted at all healthcare professionals who provide care to people with dementia across all settings. The module aims to help the learner to determine the best person-centred supports for a person with non-cognitive symptoms of dementia and to recognise the risks of unnecessarily prescribing a psychotropic medication.
There are three core topics within the 30-minute module:
• Topic 1- Non-cognitive symptoms of dementia
• Topic 2- Tailored, person-centred support
• Topic 3- Risks of psychotropic medication
By the end of this module you will be able to:
• Explain the steps you must take to determine the best supports for a person with noncognitive symptoms of dementia.
• Describe how you can deliver a person-centred approach to dementia care.
• Summarise the types of non-pharmacological interventions that can support a person who is experiencing non-cognitive symptoms of dementia.
• Outline the risks you associate with psychotropic prescribing.
The module includes recorded scenarios, audio excerpts and an animated explainer. This module, which is now available on HSeLanD, forms part of a broader training and education programme which includes Facilitator education which will be rolled out in 2023.
50 | HEALTH MATTERS WINTER 2022
MEMORY TECH
Memory Technology Resource Room showcases assistive technologies for dementia
As part of International Dementia Awareness month, an open day was held in the Memory Technology Resource Room (MTRR) in St John’s Hospital, Sligo, which was launched during the summer on a pilot basis.

This is one of 28 such rooms nationally, all run by occupational therapists and all of which have achieved fantastic outcomes for the dementia and cognitively impaired client group over the last number of years.
The MTRR service is one that has grown nationally year on year, having started as an Assistive Technology Library pilot programme in Tipperary in 2011, to now having 28 permanent sites across Ireland. The service is supported nationally by the HSE and the National Dementia Office.
The MTRR is a practical resource for people with memory difficulties and dementia, and their families and friends to see and trial a wide range of assistive technologies to support memory, independence and safety. It is led by senior occupational therapist Kara Dolan who assesses where specific difficulties lie in relation to a person’s memory, and then advises on how best to support them with their memory problems in their day-to-day life.
Alongside the assistive technologies, the occupational therapist may provide individualised education, home-based memory programmes and / or practical strategies that aim to help people keep well and maintain their independence despite their memory problems.
The MTRR has a wide variety of assistive technology devices on display and available for clients, and their carers, to see and trial, under the assessment and guidance of an occupational therapist. These include orientation devices, safety devices, motion sensors, GPS tracker type devices, as well as many of the smaller and lower tech devices which often have the biggest impact. It also provides advice around adapting the clients existing technology (eg education for medication reminder apps on smartphones; etc to enhance daily living in the most cost effective way possible. All recommendations for the purchase of devices will only be made following thorough discussion and assessment by the OT of individual client needs.
The aim of the MTRR service is twofold:
• Firstly, it provides individualised OT assessment, advice and education around assistive technology devices which may be beneficial to the clients' specific areas of difficulty or concern. The success of this aspect of the MTRR has been largely due to the strong focus on the individualised, client centred OT assessment, and subsequent individualised OT advice.
Secondly, the service will also have a strong focus on client (and carer) education. This will include education and implementation of various cognitive and compensatory strategies, which aim to facilitate safety and independence, as well as improve the client's quality of life. It also includes education and assistance on navigating the wide range of smartphone apps and other services in the community which are now freely available.
The service is offered to any clients, over the age of 18 years, who have dementia or have memory/cognitive difficulties that are affecting their daily function and engagement. They must be living in Co Sligo, and in most cases be able to attend an appointment in the MTRR room in St John’s Hospital.
Home visits can be provided in certain cases where it is not feasible for the client to travel, or where the OT feels that it is relevant to complete the assessment in clients own home. Referrals can be accepted from any healthcare professional, and clients/families can also self-refer.
Ciara Connellan, OT Manager, Older Persons Services Sligo Leitrim, said, “I am so pleased that we are now in a position to offer this fantastic service to those in the Sligo area who experience memory deficits. This service will provide practical support to both clients and carers as they journey through life with cognitive difficulties. It is so beneficial that we now have a large variety of assistive technology products available and the expertise of a dedicated senior occupational therapist in Sligo to support those aged 18 years and over through their difficulties.”
| 51 HEALTH MATTERS WINTER 2022
Majella O’Donnell, CNS Dementia; Dr Ravi Prasad Prayaga, Community Geriatric Registrar; Dr Paula Hickey, Consultant Geriatrician; and Kara Dolan, Senior Occupational Therapist, MTRR.
How HSE staff turned around a Civil Registration Service at crisis point

The Civil Registration Service for births, stillbirths, marriages and deaths in the Eastern Registration Area covers the counties of Dublin, Kildare and Wicklow and comes under the regional management of Community Healthcare East. It serves the largest population base in the State and manages all national and international online certificate orders placed via the online certificate order portal.
A day in the life of a Civil Registration office is busy and diverse. While registering a birth or solemnising a marriage are in the main joyful occasions, the experience of registering a still birth or death is a very difficult and painful time for those impacted. Civil Registration staff are skilled in celebrating alongside clients during times of joy while providing support and compassion during times of grief.
The perfect storm
Towards the end of 2021, Civil Registration Services across the HSE faced a number of strategic and operational challenges. The cyber-attack on the HSE in May 2021 resulted in the complete outage of all civil registration operating systems in the Eastern Registration Area. Full system restoration took almost 10 weeks. Meanwhile orders made via the www.certificate.ie portal were not accessible during this time. The situation was exacerbated by an increased demand for certificates driven by Brexit. Concurrently, system outages and service delays resulted in a significant increase in calls to the service from members of the public, placing an additional pull on existing resources. Furthermore, temporary COVID-19 emergency legislation waiving the requirement for in-person appointments for the registration of life events came to an end in October 2021. However, the capacity of the service remained curtailed due to enduring COVID-19 social distancing measures which limited the number of in–person appointment slots available.
Combined, these factors caused a perfect storm resulting in significant disruption to Civil Registration Services and large backlogs in certificate orders. When systems were offline, back-up procedures were put in place where possible and staff worked overtime to help reduce backlogs and provide for the continuation of essential services. The endeavours and flexibility of staff enabled all marriages to be solemnised as planned despite the challenging circumstances. However, these efforts were not sustainable as a long term solution. Complaints from service users were increasing and the service was beginning to buckle under mounting pressures.
The solution
In order to address the service challenges presenting, a multidisciplinary project improvement team was established in November 2021. Led by Aisling Heffernan, Head of Service for Health and Wellbeing in HSE Community Healthcare East, the team comprised of Civil Registration staff, ICT, HR, Communications, staff from the Primary Care Reimbursement Service (PCRS) and Project Management support. The aim of the team was to oversee a coordinated and multifaceted approach to the recovery and restoration of Civil Registration Services disrupted by the cyberattack and altered workflows due to COVID-19 measures. In carrying out this work, the team embraced the opportunity to introduce a number of service improvement initiatives that would enable backlogs to be reduced and full services to be restored. In addition these initiatives would also improve the overall quality of the service for the public, restore confidence and create a more robust model of service delivery for staff.
Aisling reflected, “We recognised at the outset that we needed some breathing space to address increasing backlogs and so the facility to order a certificate online was temporarily paused. However during this time we ensured that certificates could continue to be requested locally from other Civil Registration offices. We thank our colleagues across the country for supporting this arrangement which gave staff the opportunity to reduce the existing backlog, refocus on how to address legacy issues from the cyber-attack and map out overall service improvements.”
Working together, the project team identified that adopting changes in work practices presented opportunities to improve efficiency and activity. One of the first tasks for the team was to review and improve the existing phone system which was inadequate for the high volume of incoming calls. As this work
HEALTH MATTERS WINTER 2022 52 |
‘At times it felt we were fighting a losing battle, it was one step forward, two steps back’
was being done, the PCRS managed all calls going to the Wicklow Office to allow Civil Registration Service staff the time to reconfigure the phone system and recruit additional staff. All calls to Civil Registration Staff are now being diverted to available staff and are answered in a timely manner.

In tandem with local service improvements and additional recruitment, the project team oversaw and led the roll out of a national eHealth project to utilise the Swiftqueue portal. This portal facilitates members of the public to book an appointment to register a birth or death at a convenient time and place. The introduction of this portal represents a step forward with ongoing efforts to make Civil Registration Services more accessible to the public. Resulting service improvement outcomes include increased capacity, reduced waiting times and enhanced service user experience.
Consistency and clarity of communications was an integral and critical component of the service improvement project. To ensure information on the HSE website on the registration process and appointment system for births and deaths was easy to access and understand, the project team worked closely with HSE Communications. This collaborative approach has led to a significant reduction in the number of telephone calls from the public looking for information, which in turn has freed up staff to focus on service provision.
The result
As a result of these initiatives, in just six months, staff in the Eastern Registration Area managed to clear a backlog of 19,000 certificate orders. In addition the waiting time for an appointment to register a birth or death has been reduced from up to 12 weeks to same day or next day in most cases.
The positive outcomes associated with the introduction of the Swiftqueue booking system has prompted its roll-out nationally on a phased basis.
Community Healthcare East's Chief Officer Martina Queally said, "The work completed in the Eastern Registration Area is demonstrative of the benefits of taking a multidisciplinary approach to problem-solving in HSE services and is yet another example of how dedicated, agile and responsive HSE staff can be to a crisis. I wish to thank all staff for their commitment and dedication in this regard."
Aisling concluded, “At times it felt we were fighting a losing battle, it was one step forward, two steps back. However, having come out the other side of this crisis, the team is now able to look back with pride at how it managed to, not only return an invaluable service to the public, but also improve it."
More information on Civil Registration Services can be found at https://www2.hse.ie/services/births-deaths-and-marriages/ or by searching online for HSE births, deaths and marriages.
LABORATORY PROGRAMME WILL ‘ADVANCE, STANDARDISE AND SUPPORT’ KEY ICT INITIATIVES
The Laboratory Programme, under the governance of eHealth, was established in 2021 following the cyber-attack, to advance, standardise and support key Laboratory ICT initiatives and to enhance integration of healthcare.
The aim of this Programme is to provide a framework for laboratory services to engage with HSE eHealth & Acute Operations.
The Laboratory Programme is comprised of a diverse team of experienced healthcare professionals including Medical Scientists, Clinical Scientists, Data Analysts, ICT Technical Experts, Project Managers and Project Officers.
Overall programme strategy includes:
• Aligning objectives and strategy
• Improving system resilience and streamlining processes
• Maximising & consolidating available resources
• Realising benefits of outcomes with a national perspective
• Exploring long-term benefits to the organisation
• Supporting innovations & new capabilities
Current key projects include:
• MedLIS National Laboratory Information System
• LIS & hardware stabilisation of current LIS systems
• Compliance Management System Procurement
• eOrdering for GPs
• Anti-Coagulant Monitoring System Procurement
MedLIS Update
The MedLIS programme was temporarily suspended following the cyber-attack in May 2021, while the National MedLIS Project team was re-directed to support the acute and immediate response to the attack on our healthcare systems.
The MedLIS server environment and infrastructure was also impacted by the events of May 14th 2021 and a decision was made to rebuild and host the application remotely in Sweden, in line with Cerner’s long term strategy. This will facilitate a code upgrade to the latest supported version, alignment with a Cloud first policy and a robust disaster recovery environment. The rebuild in Sweden will be complete by March 2023 to be followed by a 14-month project to deploy the MedLIS application at Beaumont Hospital.
Progress
A comprehensive project plan has been agreed in conjunction with our partners at Beaumont Hospital. The 14-month project includes additional build, testing and validation with a scheduled Go-Live date of Q2 2024.
Targets
MedLIS has experienced significant challenges and external shocks since the contract was signed with Cerner in 2015 but the vision remains the same in terms of paperless ordering and reporting, with a consolidated patient laboratory record, supported centrally by a dedicated National Support team.
The MedLIS team are happy to address any specific questions that our healthcare colleagues have on any aspect of MedLIS or the Laboratory Programme and appreciate your support.
Contact us
Laboratory Programme Manager Thomas Walsh, eHealth and Disruptive Technologies, St Patricks Hospital, Waterford, X91N977. Email: thomasw.walsh@hse.ie
| 53 HEALTH MATTERS WINTER 2022
First of its kind
Results from drug checking pilot at Electric Picnic published
The results of a ‘first of its kind’ pilot drug test programme at this year’s Electric Picnic festival finds high strength MDMA samples and a new substance 3-CMC not detected in Ireland before.
Taking place at Electric Picnic in September, the pilot involved festivalgoers anonymously putting drugs into HSE surrender bins at the HSE harm reduction tent and the festival medical tent. The substances were then moved by accredited staff members to our onsite portable laboratory and analysed by staff from the HSE National Drug Treatment Centre Laboratory using a Fourier Transform Infrared Spectroscopy (FTIR) machine. As part of the Safer Nightlife Harm Reduction Campaign, the pilot aimed to access, test and identify substances in a festival setting, alert the public, harm reduction services and onsite medics to any dangerous substances identified and gain insights on drug trends.

A total of 46 samples were received and tested in real-time at the event, with 42 samples seeing drug content found. The HSE issued three different risk communications relating to concerns around a particular MDMA product, high strength powders and crystals and the emergence of a new substance 3-CMC (a cathinone drug which can cause significant mental health problems). These risk communications were shared on social media, on the Electric Picnic app, on display screens located throughout the event and received significant attention across the mainstream media and on social media.
“While this report represents a relatively small number of samples numerically, we must recognise the importance of this pilot project and our findings,” commented HSE National Clinical Lead Addiction Services, Professor Eamon Keenan.
“The pilot is a real example of cross sectoral collaboration, where all agencies agreed on the need to collaborate to identify emerging drug trends, with an aim of protecting the health of people attending the event.
KEY FINDINGS:
• Drug content was identified in a total of 42 samples (91%) as part of pilot
• Four samples remain unconfirmed
• 19 MDMA samples were submitted (eight powders and 11 pills)
• Five MDMA powders tested as almost pure MDMA
• 'Ecstasy' pills ranged in strength from 36mg to 235mg of MDMA
• 12 New Psychoactive substances were submitted: seven tabs, four powders/crystals and one tablet
• Three of these new psychoactive substances identified had not been previously detected in Ireland (3CMC, 5-MAPB, 4-HO-MiPT)
• Three risk communications issued relating to a high strength 'MyBrand' purple skull MD MA pill, high potency MDMA powders and the emergence of 3-CMC (a cathinone drug)

“This programme is the first of its kind in Ireland, whereby the HSE accessed substances from people who use drugs to conduct real-time analysis for the purpose of sharing risk communications at a festival. As a result, the HSE were able to quickly share accurate information with the public to encourage harm reduction discussions both in person (HSE Volunteers were available throughout the venue) and online over the course of the event. We obtained quantitative estimates of MDMA being used in Ireland which we have never had access to before, while we engaged with hidden and niche user groups whom we otherwise would not have contact with through traditional addiction services.”
The project confirms for the first time that high strength MDMA products are appearing in Ireland similar to the rest of Europe, which significantly increases the risks for people. Five MDMA powders were confirmed as
almost pure MDMA which creates harm reduction challenges.
Emerging Drug Trends Project Manager at the National Social Inclusion Office, Nicki Killeen, said, “From a research perspective, it is extremely interesting that we accessed such diversity in the drug samples including very novel compounds. These results provide us with further insight on the changing drug landscape in Ireland. Based on this, it is clear that there is a need to further expand this approach to include more frequent analysis in new settings.
“As the drug market evolves, Ireland must prepare for possible changes and associated health threats with substance analysis having a central role in this process to help us identify concerns and respond at a faster rate to reduce harm.”
The report recommends a series of future actions such as engaging with the public to obtain feedback on the pilot and considering how the HSE can further access substances from people who use drugs for health purposes to expand on this approach.
Read the full report here: www.drugs.ie/features/feature/ results_from_irelands_first_back_of_house_drug_ monitoring_project
HEALTH MATTERS WINTER 2022 54 |
The Ploughing Championships return
HSE staff share expertise with public


After a two year hiatus, the National Ploughing Championships was back with a bang and a recordbreaking 277,000 people travelled to Ratheniska, Co Laois to soak up the experiences on offer at Europe’s largest outdoor event.
More than 80 HSE staff shared their expertise on a wide range of services and health topics over the three days. Staff came from all over the country, representing more than 12 individual health exhibitors which included the National Ambulance Service (NAS), Department of Vascular Surgery UHL, Sepsis, Emergency Medicine, Organ Donation and Transplant Ireland (ODTI), Public Health Area B, Diabetic Retina Screening Service and the START and QUIT health promotion campaigns.
HSELive staff were there each day to help people to access services including booking vaccinations, registering for screening services, applying for a medical card or the drugs payment scheme, and getting details on the Fair Play scheme. The HSE exhibition space was supported by Healthy Ireland.
Free health checks were the most popular offering and the queues of people provided an opportunity for meaningful engagement with people.
Blood pressure testing, offered by NAS and colleagues from Emergency Medicine, was in great demand.
availed of this which was far more than the
At the QUIT stand, many smokers took up the opportunity to have their breath carbon monoxide levels checked. Many also took up the offer of a free one-to-one stop smoking consultation with a HSE Stop Smoking Advisor.

The National Sepsis Programme team raised awareness of the fact that sepsis is a potentially life-threatening complication of an infection that can affect anyone.

On Wednesday, the Diabetic RetinaScreen programme was represented. People with diabetes types 1 and 2 were informed about the test on offer to them and how to register with the programme.
The Understanding Together (UT) Dementia team, walked the site raising awareness of the support and services available post diagnosis, both from health services and through social and community initiatives.
Representatives of Patients for Patient Safety attended. Sheila and Bernie’s passionate efforts to raise awareness of patient safety in general and the ‘My Medicines List’ was a strong example of the kind of practical and vital outreach which is perfect for the Ploughing.
On Tuesday, Organ Donation and Transplant Ireland (ODTI) donor co-ordinators highlighted the importance of having a discussion with family around one’s wishes to be an organ donor.
The Emergency Team raised awareness of the conditions for which people should attend their local Emergency Department or Injury Unit. The team also demonstrated basic initial treatment techniques. Many young children in particular enjoying seeing the team apply a splint or sling to ‘Mr Bones’, the model skeleton.

On the final day, health promotion experts at the START campaign stand offered practical advice and support on how to reduce treats for children’s health and wellbeing.
The Public Health Area B Team spread the word about VTEC/ STEC, potential health risks from private well water supplies, and preparing for a healthy pregnancy while farming.

| 55 HEALTH MATTERS WINTER 2022
The Vascular Surgery team offered at risk individuals the option of an ultrasound screen to identify Abdominal Aortic Aneurysm. 160 people
team had anticipated.
Home Testing
People living in Ireland aged 17 and older can now order an STI test kit online and carry out the tests at home
The HSE Sexual Health and Crisis Pregnancy Programme (SHCPP), Health and Wellbeing, have launched a free national online service which provides people living in Ireland aged 17 and older, the option to test for sexually transmitted infections (STIs) at home.
People aged 17 and older can order a free STI test kit on the online platform, which is delivered to their home by post. Users complete the tests at home and post the samples to the laboratory in the pre-paid envelope provided. Individuals receive their results by text or phone, and those who require further testing and treatment are referred to participating public STI clinics, ensuring a seamless individual experience.
This service is generally most suitable for individuals who do not have symptoms of an STI. Anyone who has symptoms of an STI is advised to attend an STI clinic or their GP for assessment. Users of this service are tested for chlamydia, gonorrhoea, syphilis, and HIV, with some users o ered a hepatitis B and C test as required.

The national service follows the highly successful pilot in Dublin, Cork and Kerry in 2021. The pilot evaluation found the home STI testing service to be feasible, impactful, and acceptable to service users and providers. The pilot served to increase STI testing capacity within the pilot counties, engaged new users and identified STIs among population groups known to be at risk of STIs. The service helped overcome the established concerns of embarrassment, stigma, and confidentiality that can serve as barriers to seeking STI testing within face-to-face settings. The full evaluation report can be found here: https://www.sexualwellbeing.ie/for-professionals/research/research-reports/
The HSE supported the launch with a digital, social media and outdoor campaign. A new ‘street art’ style creative designed by Joe Caslin was delivered as part of the national service. The campaign and promotional activity will help to raise awareness of the importance of accessing free STI testing for those who need it; and will help to normalise STI testing as being an important step in self-managing our overall health and wellbeing.

New posters and business cards are available to order from HealthPromotion.ie More information about the service is available at: www.sexualwellbeing.ie
PUBLICATION OF NATIONAL CONDOM DISTRIBUTION SERVICE – REPORT OF ACTIVITIES FOR 2021
The HSE Sexual Health and Crisis Pregnancy Programme published the National Condom Distribution Service (NCDS) Annual Report for 2021. The NCDS, established in 2015, distributes condoms at no cost to organisations working directly with individuals at increased risk of HIV, sexually transmitted infections (STIs) or unplanned pregnancy.

The report shows that the NCDS distributed 439,450 condoms and 259,603 lubricant sachets to 70 organisations between January 1st and December 31st 2021.
Organisations included public sector services such as public STI clinics; non-governmental organisations; and third level institutions. These organisations distributed condoms to groups including young people, gay, bisexual and other men who have sex with men (gbMSM), and migrant communities, among others. Demand was similar to 2020 as COVID-19 pandemic and public health restrictions were in operation for most of the first six months of 2021. Demand increased towards the end of 2021 as Government
To read the report, please see: www.sexualwellbeing.ie/for-professionals/ research/research-reports/ncds-2021_final.pdf To register for the NCDS please click here www. sexualwellbeing.ie/for-professionals/nationalcondom-distribution-service/
HEALTH MATTERS WINTER 2022 56 | 56
HSE launch free national home STI testing service
restrictions eased and university campuses reopened.
Maeve O’Brien, Interim Programme Lead, HSE Sexual Health and Crisis Pregnancy Programme; Justin Harbottle, Business Development Manager, SH:24; Minister Frank Feighan, Minister of State for Public Health Well-Being and the National Drugs Strategy; Professor Fiona Lyons, Clinical Lead HSE Sexual Health and Crisis Pregnancy Programme; Caroline Hurley, Project Manager, Sexual Health and Crisis Pregnancy Programme; Chris Howroyd, Chief Executive O icer, SH:24.
Midwife Cathy’s book gives back after cancer treatment

In January, 2021, Cathy O’Sullivan found a lump in her right breast and less than a month later she was diagnosed with breast cancer. Writing poems during appointments or other quiet times helped her cope with what she was going through.
“This cancer journey is unique to me as I am aware that everyone’s cancer journey is so di erent. My message to all reading this book is the importance of breast self-check. And maybe these words might provide some comfort or understanding for someone out there who is going or has gone through cancer,” she said.
Cathy wrote her first poem during her initial visit to Cork University Hospital, when she had an examination by a consultant, a mammogram, an ultrasound and biopsies.
“I wrote my first poem at that visit, as we all wore masks and were socially distanced in the waiting area, and there was no interaction with other women. Writing the poem was a form of distraction and passed the time for me,” she said.
“Prior to my diagnosis, life was busy both at home and at work. I worked as the Director of the Centre of Midwifery Education in Cork University Maternity Hospital where one day I was planning and organising education and working with a team, and the next day I was grappling with the fact that I was now on sick leave with a serious illness.
She admitted that starting chemotherapy was ‘scary’.
“I went through five months of intensive chemotherapy and then had a break of six weeks before surgery. To get through the discomforts of chemotherapy on Tuesdays, I used to drive to Garryvoe after my blood tests on Mondays for a walk with my sister-in-law. The view of Ballycotton Island and the sound of the waves were so calming. I used to make videos of the sound of the waves and play them during chemotherapy. I found nature, especially the sea, very therapeutic.
“I also found writing poetry helped me through chemotherapy and the whole cancer journey. I worked with a poet, Enda Wyley, who mentored me while writing the book. Enda’s encouragement kept me going when I would struggle with tiredness, side e ects and low energy, she did all this voluntarily as she believed in the book writing project and wanted to support the work of Cork ARC. Her generosity was remarkable.
“I found both writing and reading poetry very therapeutic and when I was writing I was totally distracted from worries.”
Cathy, whose cancer journey lasted 10 months, said the Cork ARC were a massive help.
“Cork ARC were a wonderful support and from the day I made the initial phone call to contact them until today, they have been brilliant. Diagnosis and treatment are di cult, but the limbo when it is all over
is challenging also. There are great after-supports in Cork ARC, including group sessions on how to adapt to life after cancer,” she explained.
“I found the one-to-one support and art therapy very helpful.”




Her goal now is to raise between €8,000-10,000 for Cork ARC. Since the launch, she has already raised more than €2,500 and it is growing daily. The book is €20 and is available on the Cork ARC website and online at Amazon and Book Depository.
“Thank you to Enda Wyley, my niece Maria Lynch, Rita Dineen, (cover illustration), and Orla Kelly for helping me get the book to publication stage.”
But her writing days are far from over.

“I have just finished a short story writing course with the Irish Writers’ Centre. I will enter the short story that I wrote into a few competitions and I will submit to journals for publication. I will continue poetry writing also. I will take time to relax and enjoy life,” she added.

To purchase the book, see https://corkcancersupport.ie/product/through-your-doors-again-by-cathy-osullivan/

| 57 HEALTH MATTERS WINTER 2022
A Cork midwife who charted her cancer journey through poetry has compiled her works into a fundraising book for the Cork ARC House.
BREAST CHECK
BreastCheck encourages uptake for Breast Cancer Awareness Month


BreastCheck marked Breast Cancer Awareness Month in October with a campaign encouraging women who have never had a breast screen to check the register and take up their invitations.














The campaign featured press and digital activity and was supported by new breast cancer detection and prevention leaflets and posters sent to every GP surgery across the country.
The breast cancer screening programme is delivered by the National Screening Service, and invites women aged 50-69 to have a screening test every two years.
Breast Cancer Awareness Month is an important opportunity to talk about the important role screening has in limiting the impact of this disease. Screening uses a mammogram (or x-ray) to look for abnormalities that could be cancer in women who have no symptoms - when cancer is still small. This means cancer is often diagnosed at a lower or earlier stage and it can be more easily treated or cured. A recent National Cancer Registry of Ireland report found that survival has improved for breast cancer, with the biggest improvements seen in the age-groups targeted by the national screening programmes.
Yet, while uptake of breast screening appointments among older women in the screening age range is strong, women in the younger age ranges - including those due their first screen - are a little less likely to attend for screening. Some women who don’t attend are fearful that a mammogram will hurt or of what screening may find.
The poster delivered to GPs outlines what happens at screening and reminds women who’ve never been screened to check they are on the register.
The leaflet entitled Breast cancer prevention and early detection information from BreastCheck, was developed in partnership with the National Cancer Control Programme and highlights the steps everyone can take to reduce their chance of developing breast cancer. Breast
cancer is the most common cancer in women in Ireland. Around 3,500 women are diagnosed with breast cancer each year and 1 in 7 women in Ireland will develop it in their lifetime.

It shows how some breast cancer risk factors can’t be changed, such as our age and our genes. While some risk factors we can change, including drinking alcohol, the types of food we eat, and how physically active we are.
It also outlines breast cancer symptoms and how to self-check. It highlights that women who are concerned about their breast health should speak to their GP rather than wait for screening.
There are about 2,500 General Practitioners, or GPs, in Ireland, working in group practices, primary care centres, single practices and health centres around Ireland. And recent HSE behaviours and attitudes research highlights the fact that GPs and practice nurses are the trusted source of health information for people in Ireland.
BreastCheck Programme Manager Suzanne Lynch said, “BreastCheck can help improve the outcomes for women by detecting breast cancer before women have symptoms. We’re keen to deliver good, trusted information to women where they are – and where better than their GP surgery or health clinic? The poster explains breast screening in easy-to-understand language, and prompts women to find out more.
“It’s our hope that women, especially those who have never had a screening appointment, will see it, talk to their GP about screening, and be empowered take the next step.
“I’d like to thank our general practice colleagues for their ongoing support in talking to their patients about screening once they are eligible. We’re keen to reach women who may be reluctant to come for breast screening. We want to let them know that screening is a positive, proactive step every woman can take to help protect their breast health.” If you would like a copy of the poster or leaflet contact communications@screeningservice.ie
HEALTH MATTERS WINTER 2022 58 |
NCRI REPORT SHOWS POSITIVE IMPACT OF CANCER SCREENING PROGRAMMES
A new report published by the National Cancer Registry Ireland (NCRI) shows the positive impact of BreastCheck, CervicalCheck and BowelScreen on cancer detection in Ireland. The report, titled Breast, cervical and colorectal cancer 1994-2019: National trends for cancers with population-based screening programmes in Ireland, shows a noticeable increase in earlier diagnosis, and a demonstrable reduction in mortality rates.



The overall key findings show:
• Cancers detected via screening were, on average, found at a much earlier stage in the screening age group than in the non-screening group

• Decreases in mortality rates for the three cancers were, in general, more substantial in the age-groups eligible for screening
• Survival is now higher and has improved more markedly in the screening age groups for all three cancers
• Population cancer screening in Ireland is e ective.


The trends for each programme detailed in the report reveal in more depth the positive outcomes of screening on each individual cancer type.
Chief Executive of the National Screening Service Fiona Murphy, said, “The NCRI report is the first of its kind to analyse the impact of population screening programmes on cancer trends in Ireland.

It is agreed that since the 1990s there has been a collective improvement in better awareness of cancer symptoms, new treatments, improvements in care, and changes in underlying risks for cancer which have all had a positive impact on improved survival.
“However, with the publication of this report and the detailed analysis of the various screened populations, we can now confidently say that a portion of that improvement is directly attributable to CervicalCheck, BowelScreen and BreastCheck.
The public can be reassured that our screening programmes are e ective.”












The report can be viewed at www.ncri.ie
BreastCheck held its Radiography Study Day in September; its first since the easing of public health restrictions. The day was organised by the programme’s clinical training team. It included seven talks with representatives from each unit. The event was held at the Catherine McAuley Centre on Dublin’s Eccles Street.
The first speaker was Georgie Crawford, host of one of Ireland’s most prominent health podcasts, The Good Glow. She talked about breast cancer care from the patient’s perspective and reminded those present to mind themselves so they can provide the best care to others.
Dr Laura Murphy, a consultant radiologist in the BreastCheck Eccles Unit, delivered a talk on the diagnosis and management of B3 lesions of the breast.
Galway radiographer Claire Ahern discussed her ‘AniMammo’ project that won the award for Best Innovation in Healthcare at the HSE Spark Ignite national final in 2021.

Dr Michael Click from the Galway Unit gave an overview of breast calcifications. He presented case studies that demonstrated the appearance of di erent types of calcifications found on mammograms and how these are formed.
Physicist Michael Manley from the BreastCheck Southern Unit explained the pros and cons of artificial intelligence across a broad spectrum of applications.
Radiographer Fiona Wilkins of the BreastCheck Southern Unit gave a talk on mindfulness and led a guided meditation with the group. She has completed a teaching diploma in mindfulness, meditation, and positive psychology at the Irish Mindfulness Academy.
The final speaker was Head of Strategy, Business and Projects Grace Turner who gave an update on the development of the NSS Strategy, outlining the work that has gone into the project so far.
“It was a very inspiring day,” said Kerry Lombard, national radiography services manager. “A lot of work went into making sure the day ran as smoothly as it did. A huge ‘thank you’ is due to the programme’s clinical training team who made it all happen.”

| 59 HEALTH MATTERS WINTER 2022
Chief Executive of the National Screening Service Fiona Murphy
BreastCheck hold first Radiography Study Day since 2019
Above: Kerry Lombard (left), Deputy Radiography Service Manager, Orla Mulhall. Below: Francina Mashigo (left), and Mamta Bhati, clinical trainers, BreastCheck Eccles Unit
Screening
National Screening Advisory Committee
launching its second annual call
The National Screening Advisory Committee (NSAC) is launching its second Annual Call seeking proposals on new screening programmes that may be introduced in Ireland, as well as suggestions for changes to five existing programmes: BreastCheck, CervicalCheck, BowelScreen, Diabetic RetinaScreen and the National Newborn Bloodspot Screening Programme.
The Annual Call will be open from mid-November 2022 to mid-January 2023 and will welcome proposals from the public and professionals.
Who are the NSAC?
The National Screening Advisory Committee (NSAC), which was established in 2019, is an independent committee which advises the Minister for Health and makes recommendations on the introduction of new screening programmes or changes to existing programmes relating to a number of conditions such as cancer, non-cancer and newborn conditions.
First Annual Call 2021
The committee’s first Annual Call, launched late last year, was very successful with a significant response received from
various sources such as members of the public, HSE, clinicians and anyone who had an interest in making a proposal. The committee has now considered the submissions from its first Annual Call and will publish its full work programme on its website www.nsacommittee.gov.ie.
Several decisions were made by the Committee during 2022 and one such decision was to make a recommendation to the Minister for Health based on a submission received via the Annual Call 2021 from BowelScreen. The recommendation was for the adoption of a clinical guideline that will ensure BowelScreen is aligned with current clinical practice across the symptomatic service in the HSE. The recommendation was subsequently approved by the Minister in March 2022 and is now being implemented by the HSE.
Following Annual Call submissions from several sources, including from BreastCheck, the Committee has decided to ask HIQA to begin looking at the evidence to extend the age ranges for breast screening. HIQA is also looking at evidence to extend the age range in Bowelscreen.
A ninth condition (ADA-SCID) was
added to the newborn bloodspot screening programme in May 2022, following a recommendation from the National Screening Advisory Committee. The Minister was pleased to see this new addition the NBS programme and appreciates the hard work of the HSE in implementing this recommendation. The NBS programme continues to be a priority, with a Health Technology Assessment (HTA) examining evidence for the addition of a tenth newborn condition currently underway by HIQA. A recommendation from the Committee to the Minister is expected before end 2022.
Please visit Committee’s website www. nsacommittee.gov.ie to learn more on the recommendations made by the Committee since its establishment.
Second Annual Call 2022
Second Annual Call of the National Screening Committee will be launched in mid-November. Detailed information on how to make a submission will be available on the NSAC website www.nsacommittee. gov.ie. If you have any questions on how to submit a proposal, please get in touch with the NSAC Secretariat by email NSAC_ Annual_Call@health.gov.ie.
HEALTH MATTERS WINTER 2022 60 |
Support and Guidance for AMS Teams
Antimicrobial stewardship guidance published


The AMRIC team were delighted to publish the HSE antimicrobial stewardship (AMS) guidance for all healthcare settings guidance in August of this year.

AMS is an integral component of patient safety as it promotes maximising the benefit of antimicrobials and causing the least harm for the individual service user. AMS programmes are delivered by a multidisciplinary team using a suite of strategies and interventions and operate within the governance structure of a healthcare facility. It is a vital approach in limiting and potentially reversing the development of antimicrobial resistance (AMR). As a healthcare worker we all have a role to play as an antimicrobial steward to curb, and hopefully reverse, this growing trend of AMR in order to have e ective antimicrobials to enable us to deliver an optimal level of healthcare. We need, as healthcare workers, to feel empowered to play our part by learning how to incorporate antimicrobial stewardship in our day-to-day practice.
The aim of the document is to provide support and guidance to AMS teams, healthcare facility managers, and the individual healthcare worker by providing the evidence, expert guidance, and tools they need to initiate and sustain AMS programmes and embed it in to routine work of each healthcare worker. The work of higher education institutions, professional colleges, and groups is central to the creation and delivery of AMS education. This document will provide guidance to the development of curricula, educational courses, and training programmes.
We would like to acknowledge the dedication and hard work of the working group in creating this document. The input and feedback of the AMS advisory group, and our key stakeholders in acute and community healthcare and in the higher education institutions made it into the informative and well-presented guidance resource it is. We are grateful to Professor Martin Cormican, former HSE Clinical Lead for AMRIC (2017- April 2022), Dr Colm Henry, Chief Clinical O cer, and the AMRIC Oversight Group for their review and approval of the guidance.
This AMS guidance will provide the base to enable many of the actions contained in the HSE AMRIC action plan 2022-2025 and Ireland’s national action plan for antimicrobial resistance 2022-2025.

The electronic version of this guidance is located on the newly refreshed AMS page on www.antibioticprescribing.ie This page contains other tools and resources to assist in the implementation of AMS.

| 61 HEALTH MATTERS WINTER 2022
Winter Ready
The HSE Emergency Management O ce updated the Severe Weather Planning Guidance document in October 2022, which will help HSE managers and sta to develop and update their local severe weather plans. It includes checklists and advice and you will find it on hse.ie at hse.ie/ emergencymanagement/severeweather
Given the reality of climate change and the risk of severe weather events, it is vital that HSE managers and all sta plan and prepare so that our ability to deliver health services during periods of severe weather is maintained and the e ects on service delivery kept to a minimum.
If you are a HSE manager please check the updated Severe Weather Planning Guidance document and:
• update your existing severe weather plans, include any learnings from 2021 to date and ensure all your sta are aware of them.
If you are a HSE sta member please ensure:
• you are familiar with severe weather plans for your area or department and discuss these plans with your line manager as needed.
HSE managers have to plan to ensure that all key services are resilient to severe weather and mitigate the impact that it may have on the day-to-day activities of the HSE. We must keep in mind that Severe Weather will not just impact HSE services; it will impact on other associated businesses - those providing service support, o site diagnostics, and dialysis as well as those in our supply chain, in Ireland and globally.
The format of the guidance is adaptable to the diverse range of HSE services and facilities. The document provides the individual manager with the flexibility to plan within his/her domain. Each manager is required to address the areas in the document and develop Severe Weather preparedness for his/her area of responsibility. New challenges exist such as dealing with infection prevention and control requirements, and plans now need to incorporate the associated constraints on service capacity during a severe weather event.
Guidance document
The Guidance includes checklists which are a practical way to support managers and sta to plan for a severe weather event. The detail covers a range of areas including;
• assessing your starting point
• carrying out a risk assessment
• communications
• preparing for the impact of an event on sta ng/patients/people who use our services
• estates and maintenance
• engaging with the Area Crisis Management Teams.
The HSE Severe Weather Guidance will assist individual managers to put in place appropriate measures to deal with the following during a Severe Weather event:
• Coordination of activities to minimise the e ect of Severe Weather
• Anticipating the impact of the requirements of COVID-19 on severe weather episodes
• Ensuring e ective communications systems are in place
• Maintaining the delivery of essential services
• The implementation of contingencies where necessary
• Monitoring and maintenance of adequate phased sta ng levels within all clinical and non-clinical areas, including the redeployment of sta to critical areas where required
• Ensuring sta awareness of its service’s contingency arrangements and those of other HSE services during a Severe Weather event.
The document comprises of two parts, a Checklist and Guidance. Neither are stand-alone and both documents are structured around planning, preparedness, response and recovery. The Checklist should be completed in association with the guidance provided. The Checklist and supporting documentation can be expanded to include each individual service’s criteria as appropriate. This document should be listed as an appendix to the service’s Major Emergency or Site Specific Emergency Plan and reviewed/updated accordingly.
HSE EMERGENCY MANAGEMENT OFFICES CONTACT DETAILS
HSE National Emergency Management O ice

Contact: Assistant National Director for Emergency Management Address: HSE National O ice for Emergency Management, Stewarts Care Limited, Stewarts Hospital, Mill Lane, Dublin 20, D20 XT80 Email: national.em@hse.ie Phone: 01 6201658
HSE East Major Emergency Management O ice Contact: Chief Emergency Management O icer East Region Address: Major Emergency Management O ice, Phoenix Hall, St. Mary's Hospital Campus, Phoenix Park, Dublin 20, D20 CK33 Email: emergency.planning@hse.ie Phone: 01 7959840
HSE South Emergency Management O ice
Contact: Chief Emergency Management O icer South Region Address: Emergency Management O ice - HSE South, Eye, Ear and Throat Hospital, Western Road, Cork, T12 WP62 Email: emo@hse.ie Phone: 021 4921622
HSE West Emergency Management O ice Contact: Chief Emergency Management O ice West Region Address: Regional Emergency Management Unit, Clinical and Administrative Building, Block A, Merlin Park Hospital, Old Dublin Road, Galway, H91N973 Email: emergency.managementwest@hse.ie Phone: 091 775933
HEALTH MATTERS WINTER 2022 62 |
Are you winter ready and have you updated your Severe Weather Plan?
All Area Emergency Management O ices are available to provide managers with support and advice to complete the process of updating existing severe weather plans.
Smile
Every Smile Matters initiative makes it all the way to Paris
Every Smile Matters (ESM), an e-learning programme, was launched in the spring of 2022 by Yvonne O’Neill, National Director - Community Operations. The programme was developed by the National Oral Health O ce in conjunction with our colleagues in the HSE Dental Service.


Every Smile Matters explores the oral health challenges of people in vulnerable groups and delivers user friendly evidence-based approaches with the aim to promote better oral health for everybody.
Every Smile Matters was developed to help primary care dental teams meet the diverse needs of these vulnerable people. It is also very relevant for healthcare teams providing oral care and is fully accessible to learners across the HSE and Section 38 & 39 organisations.
Six modules each of 30 minutes delivering didactic content and incorporating interactive screens and ‘Extend My Learning Content’ providing access links and also a full bibliography of referenced sources. Certification is available on completion of all modules within the full course. The programme fulfils the criteria for Irish Dental Council structured CPD accreditation.
Speaking at the launch, National Director Yvonne O’Neill explained, “Children and adults with intellectual disabilities, and vulnerable groups have increased risk of poor oral health and less access to oral healthcare. The underlying principle of Every Smile Matters is to incorporate the evidence based approaches to providing care used internationally, so that people with disabilities and people in vulnerable groups have better outcomes from interactions with the Irish HSE Dental Services. These outcomes include reduced need for advance restorations and reduced loss of teeth.”
Every Smile Matters is aligned to the International Association for Disability and Oral Health (iADH) curriculum, while incorporating it into the HSE setting through the use of highly relevant content set in an Irish context eg patient/parent stories, bespoke videos from HSE Dental Team members and sections on the Assisted Decision Making Act and its impact on informed consent for patients and clinicians.
The resources within ESM will support dental teams delivering services as envisaged in the National Oral Health policy ‘Smile Agus Sláinte’. Every Smile Matters answers the call for action to improve health and wellbeing for everybody in line with the Healthy Ireland Framework 2013-2025.
Every Smile Matters is a landmark piece of work for people with disabilities in Ireland and was presented at the international iADH conference in Paris, as an exemplar for up-skilling dental teams to meet the needs of the communities they serve.

The National Oral Health O ce recently held their regular ‘Community of Practice’ Special Care Study Day in Portlaoise, Co Laois. The HSE Special Care Teams present were invited to attend to become ESM
champions in their area and further embed the learning of Every Smile Matters through case study workshops and tailored presentations. The speakers on the day brought contributions from the National Rehabilitation Hospital and Dublin Dental University Hospital.
Every Smile Matters programme is now live on HSeLanD and can be located via the search bar and also under the Clinical Skills course catalogue.
To date, over 600 people have engaged with Every Smile Matters on HSeLanD.
| 63 HEALTH MATTERS WINTER 2022
Dr Myra Herlihy, Assistant National Oral Health Lead with Dr Mary Clarke, Specialist in Oral Surgery, Dublin Dental University Hospital at the ‘Community of Practice’ Special Care Study Day, Dr Myra Herlihy, Assistant National Oral Health Lead; and Róisín O’Murray, Head of Speech & Language Therapy Dept, National Rehabilitation Hospital at the ‘Community of Practice’ Special Care Study Day, Dr Claire Curtin, Senior Administrative Dental Surgeon, CHO 4; and Dr Myra Herlihy, Assistant National Oral Health Lead at the ‘Community of Practice’ Special Care Study Day.
PATIENT PARTNERS
Patient Partners give voice to patients, their families and the public
Patient Partners are members of the public who represent the views of patients, their families and the general public, and provide meaningful contributions to healthcare delivery.
Joan Johnston, a Patient Partner with the National Quality and Patient Safety Directorate (NQPSD), sat down with Sheema Lughmani to share how she became involved and her experiences with patient partnerships.

Why did you become a HSE Patient Partner?
Five years ago, my son Leo was born with Angelman syndrome, a rare neurogenetic condition. I found navigating the health system a bit challenging. It was made easier by my background as a physiotherapist, and knowing and understanding the clinical side of how the system worked, but ultimately I still found it challenging.

I volunteered to become a Patient Partner because I felt strongly that there’s a real opportunity to improve the system
from within and I think it’s important that people take up those opportunities when presented. During one of the long nights with Leo (he likes to get a jump on the day and so starts it at 3am) I was pondering why I suddenly found the system that I had worked in for many years challenging. I realised that on reflection, when I was on the service delivery side I thought I knew what my patients needed, when maybe sometimes I didn’t, or at least I didn’t know everything.
Now, being on the other side of it, I have a completely new perspective, giving me a unique bifocal insight. I feel it’s important for me to bring the benefit of that experience and knowledge to the system I now access as mum of a medically complex child. So now, anytime there is a request for a Patient Partner or somebody to feed into di erent projects with a patient’s perspective, I volunteer where I can.
Why do you think it’s important for Patient Partners to be involved in healthcare delivery?
I think it’s really important to get the patient’s perspective because you cannot know that you are meeting peoples’ needs without asking them, rather than asking them after the fact.
It’s important to have an element of co-design and full partnership from the beginning. No business would start up
HEALTH MATTERS WINTER 2022 64 |
without doing some kind of market research with service users telling them what they thought of their product, or how it could be adapted to better fit their needs. This applies to healthcare as well.
At the end of the day, sta in the health service may move posts or change careers. But the patients are the ones that will be there the longest. They continue to use the services and feel the impact of the delivery of those services long after individual sta have moved on. For me, I am going to be a lifelong user of these services for my son and our family. Many families like ours will feel the greatest impact of the delivery of those services.
What’s one thing you think healthcare colleagues should know about Patient Partners and their families?
As an ex-health care professional, I thought I was an expert on what people living with the condition I treated needed, wanted, or would benefit from. I thought I knew what value they placed on each of those things. But I didn’t. It wasn’t until I started working in my current role, where it is my job to ask
patients their needs that I really started to hear them. I know and understand so much better now that the things I think are important as a clinician may not be as important to the patient.
And the thing is, without asking someone living with the condition to give their perspective, we, as clinicians, are never going to fully understand if we are meeting patient’s needs or if we are simply meeting what we think are their needs.
How do you think we can get that insight into what a patient needs?

Having a Patient Partner whose perspective is valued, one who is given the space to be honest and can work with you to solve problems - that would be transformative in the health service, and a better way to gain an insight into patient’s needs. You would be surprised how much a patient is willing to share of their lived experience, especially if they feel they could make another patient’s journey a little easier. Your patients will be so much happier with the services being delivered and so much more satisfied knowing they had a key part in the design.
What have you learned through your experiences as a Patient Partner?
I’ve had a lot of Patient Partner experiences, particularly since I changed careers to patient support and advocacy. One of the things I’ve learned is that “patient engagement” and “patient partnership” are, for me, di erent.
Patient engagement has a much narrower scope. Patient engagement can boil down to something as simple as ‘Was there a patient in the room when something was discussed, and were they given an opportunity to say something?’ That doesn’t necessarily mean that particular patient had the relevant expertise or knowledge to be able to contribute to said discussion.
Patient partnership is completely di erent. When I started as a Patient Partner with the National Quality and Patient Safety Directorate, I was asked to join the management team. I was given a ‘seat at the table.’ I remember I was asked what was good and what was not so good about my past experiences. And that was a great way to start the conversation and partnership.
In my time with the National Quality and Patient Safety Directorate, I have felt an integral part of the team. Any opportunities that have come up, I have been asked if I’d like to participate. So it’s just not about sitting in on one discussion, but having that relationship with senior management and the decision makers. I feel comfortable enough in my value to the team to give open and honest contribution, revealing details I wouldn’t often share outside of family, all in the interest of helping those not on this journey understand it just a little better. It’s not just about helping my family but all families with medical needs. In that sense, NQPSD is one of the best in my experiences with patient partnerships.
In my experience with patient engagement versus patient partnership, I feel we need to avoid the ‘ticking the box’ mentality. It can’t be something as simple as having a patient in the meeting when the discussion was held especially if that patient can’t or doesn’t feel comfortable enough to speak to the lived experience of what’s being discussed. It doesn’t compare to a valued Patient Partner, one who has the relevant lived experience or represents a larger group of people with shared lived experiences of the matter at hand, who is part of your management team, or sits on your advisory board, a partner who is given that seat at the table.
Overall, I feel we are taking huge strides in the right direction of having meaningful, mutually beneficial patient contributions because, in the end, we all want a better health service.
| 65 HEALTH MATTERS WINTER 2022
“No business would start up without doing some kind of market research with service users telling them what they thought of their product, or how it could be adapted to better fit their needs. This applies to healthcare as well.”
Joan Johnston, a Patient Partner, with her son Leo.
Digital Recruitment
Digital improvements in the HSE Recruitment landscape



The HSE Digital Recruitment Improvements Programme has commenced to support the transition to the new Recruitment Operating Model, an ambitious endeavour which was highlighted in the Spring edition of Health Matters. We are pleased to share that in November we reached a key milestone for the Digital Recruitment Improvements Programme when the Recruitment Gateway went live.
The Recruitment Gateway
What is the Recruitment Gateway?

• The Gateway is a new online portal which has digitised the job order process for all services throughout the HSE Recruitment landscape.

• The Gateway will house a single, dynamic and intuitive digital job order form which will allow colleagues across the HSE to complete and submit accurate job order forms when recruiting new sta .
• The digitisation of the job order forms will increase e ciency, improve reporting and make the recruitment process more straightforward for everyone within the HSE.
What does the Gateway mean for you?

• The Gateway will speed up the recruitment process overall, which positively impacts sta teams on the ground and the individuals availing of HSE services.
• As well as the digitisation of the job order form itself, the related processes will also be digitised. This means that someone who has submitted a job order will be able to review the status of their job order, raise an amendment request or cancel the job order directly on the Gateway if required
• This will provide recruitment teams with greater oversight and autonomy on the job orders submitted for the area, which will ultimately increase recruitment timelines and fill necessary job posts in a more timely manner


What supports will be available?

Training supports are available on HSELanD. Those identified as requiring access to the Gateway received communications on how to access supports.
How do you access the Gateway?
• A process to identify Gateway users progressed throughout the year through a series of demonstrations to recruitment teams and individual sessions to collate user names and permission types
• Following go-live, new users are able to independently request access to the Gateway via a simple online form which Local HR teams will be able to support with
• The link for this form along with the Gateway URL can be found on the Recruitment Gateway page on the HSE sta site at www.hse.ie
Panel Digitisation within Local Services

• As part of the e ort to standardise the use of HR systems across local HSE services, work has begun to upgrade the systems used by recruitment teams to manage their panels
• Going forward, all existing and future panels within local services will be held on an intuitive, digital system called Microsoft Dynamics 365

• This system will allow for automated panel management, making it easier for recruitment teams to access and update their panels
• Panels will no longer be held on Excel documents. When an update is required to a panel on Microsoft Dynamics, recruitment teams will be able to complete this in a faster and more intuitive manner
• The Microsoft capability will enable services to link their panels to their job o er process however, this has not been included in this initial roll out but will be considered for future phases
HEALTH MATTERS WINTER 2022 66 |
Talent Pool
The Recruitment Reform and Resourcing team have commenced engagement with a service provider to develop a streamlined, candidate friendly digitised system which will:
• Provide an easily accessed system for potential candidates to register their interest in positions with the HSE.
• Capture basic data from potential candidates, including basic bio together with discipline, specialty, location choice, care setting and professional registration etc.
• Provide a simple landing page for potential candidates which can be promoted for various disciplines and can include various marketing material inclusion of videos etc.
• Invite all candidates who have been unsuccessful at interview, who have been placed on a panel, all graduates, professional registration bodies, job fairs, etc to register with the Talent Pool for notifications of future posts with the HSE.
• The Talent Pool will be open to anyone to register their interest in positions with the HSE and to receive notifications on same
• Enable e ective reporting and use of data to target and push notifications to this pool appropriate to specific jobs available across all of the HSE.
• Input is being gathered in relation to the requirement of this system from Recruitment Managers at present.
Reporting
National HR are working with the support of the eHealth & Disruptive Technologies team to progress current reporting from disjointed, unstructured, manual operational reporting to transition to robust analytics, adding value through insight.
The journey to a mature balanced reporting and analytics proposition is dependent on important foundations in structured, operational data, descriptive presentation of data and robust data governance.
Procurement Objectives
STEERING THE PROCUREMENT OF GOODS AND SERVICES ACROSS THE HEALTH SERVICE

The HSE Corporate Procurement Plan 2022-2024 sets out the key priorities to improve and enhance procurement activities within the health service.
The Corporate Procurement Plan is underpinned by analysis of procurement expenditure and supporting organisational structures. It is fully aligned with the overall HSE Corporate Plan 2021-2024 and will support the achievement of the organisational objectives and the National Service Plan.
The HSE is committed to achieving the priorities identified in this Plan and driving demonstrable procurement service improvements. Procurement will work with the OGP, the Department of Health and other public health providers to ensure a coordinated and integrated approach to implementing this Plan.
Digital Recruitment in the HSE
To support the delivery of health and social care services, the HSE, as the largest purchaser in the state, spends approximately €3.7bn on goods and services annually.
This ranges from items such as medicines, personal protective
equipment and medical equipment through to ICT systems. In addition, the HSE’s Capital Works Programme spends circa €1bn annually on healthcare-related construction activities that are subject to public procurement rules.
The HSE delivers services in a highly regulated environment with the emphasis on delivering e ective and safe patient care. HSE procurement activities also take place within a regulated environment underpinned by complex EU and national legislation. Cross-functional teams analyse markets, define products, agree specifications of requirements and evaluate tender responses.
The HSE is supported in transforming how services are delivered through continued
The work involved will:
• Examine, define and standardise data across disparate recruitment data sets and systems
• Design and build data integration and visualisation across the recruitment landscape
• Define a data governance approach to ensure data is maintained to a high standard, including any related security assessments
• Provide robust and insightful reporting on recruitment activities, processes and performance at a national level, with a view to progressing to similar reporting for individual HR teams in acute, community and national services.
If you require support or have a query on the Recruitment Gateway, please contact askNRS@hse.ie
strong engagement with current and prospective suppliers.
Stephen Mulvany, CEO, said, “Public investment in healthcare services focuses on delivering core services and supporting the resilience and preparedness of the health service to respond to urgent requirements. It also supports initiatives to advance health service transformation in line with agreed Sláintecare priorities. It is critical that procurement spend on goods, services and works is carried out in a transparent and e icient manner.”
The Corporate Procurement Plan 20222024 will steer the procurement of goods and services across the health service and is accessible on hse.ie
| 67 HEALTH MATTERS WINTER 2022
YOUR OPINION COUNTS
Majority of staff feel their work is making a real difference
The aim of the Health Service sta survey is to assess sta experiences in order to identify opportunities for improvement, which will help to build a better health service for all. The results from the 2021 sta survey highlighted that:
• Overall, sta are enthusiastic (even more so than in 2018), and highly motivated compared to other large organisations. The vast majority feel their work makes a di erence to patients and service users
• There is a strong sense of job security among sta
• There has been an increase in satisfaction with the level of care delivered since 2018, however, this is tempered by almost 4 in 10 saying that they feel the service delivered by their organisation is deteriorating
• Sta are more likely to believe their manager takes a positive interest in their health and wellbeing compared to 2018
• More sta say they are involved in decisions that a ect their work in 2021 compared to 2018
• The sense of recognition received for ones’ work was one of the lowest scoring areas in 2021, however, it has seen an increase since 2018
• Levels of employee satisfaction and optimism about working in the Health Service into the future have decreased since 2018
• Communication, perceptions of senior leadership, and work/life balance are areas that need more focus
• In 2021, the same number of sta report experiencing bullying from a colleague as they did in 2018
• Covid-19 has had a mixed impact on sta . The majority felt supported throughout the pandemic and one-third feel more positively towards the HSE since before the pandemic began. However, half feel there has been a negative change in their working environment
• The main suggestions to make the Health Service a better place to work in the future were; improving workplace culture, increasing frontline sta ng numbers and more flexibility in working conditions
National HR has put in place a reporting process to track the progression of actions arising from the 2021 Sta Survey across Hospital Groups, Community Health Organisations, and National and Corporate Services. A range of actions have been reported;
• Local sta recognition awards have been established across many services,

• Ongoing recruitment is taking place to build the workforce in line with the objectives of Sláintecare
• Improving local induction programmes for new sta and conducting exit interviews to identify needs and patterns in relation to sta turnover and identifying ideas to improve the work environment
• A range of measures to improve communication and information sharing, including sta apps, and HR drop-in clinics
• A range of supports and guidance on improving sta Health and Wellbeing e.g. EAP programme, wellness seminars
• Ongoing Learning & Development for sta
• The HR Engagement & Culture team are providing a range of initiatives designed to support organisations units, departments and teams to develop and improve workplace culture including the roll out of the refreshed Values in Action Programme Sta and managers are encouraged to continue to respond and action the results and recommendations from the survey.
In the upcoming sta survey, set to take place in 2023, we want to get sta feedback to identify opportunities to further improve and develop our Health Service. Sta feedback is key, ‘Your Opinion Counts’ and your participation will continue to be valued in 2023.


HEALTH MATTERS WINTER 2022 68 |
Brand Guidelines
A single coherent visual identity
In 2021, we updated and published the HSE’s Visual Identity Guidelines. In these guidelines, the HSE logo and visual identity has been simplified. The HSE logo is instantly recognisable and using the logo means patients and the public can easily identify and trust communications from the HSE. It’s important that we standardise how our communications look and feel and apply this in a consistent way in all our services.
A single coherent visual identity helps the public to understand and navigate their way around HSE services, and works to reduce confusion about service structures and care pathways. This means moving away from the creation and use of di erent logos to represent HSE o ces, teams and services.
Visual identity explained
Our visual identity includes the HSE logo, and fonts, colour palette and imagery styles that work together, helping us to communicate in a clear and reliable way for everyone. The guidelines show you how to use the visual identity in di erent types of communications and formats.
Using the visual identity guidelines
Please use the guidelines in any new communications. This might include stationery, internal reports, published documents, your email signature, advertising and marketing communications and information materials. Existing signage, uniforms or printed materials do not have to be changed to meet these guidelines.
Do not create any new logos or symbols for HSE services. Useful templates can be accessed at: HSE.ie/branding
If you have any queries, please contact a member of the communications business team at business.unit@hse.ie and 01 9213900

| 69 HEALTH MATTERS WINTER 2022
DATA BREACH NOTIFICATION
HSE begins data notification programme relating to cyber-attack
The HSE has started to notify patients and HSE sta by letter who had some of their personal information illegally accessed and copied duing the cyber-attack on the HSE. Due to the numbers of people involved, and the need to support each notification, this notification programme will continue in phases over the coming weeks and months. If you do not get a letter you do not need to contact the HSE or do anything. This is to help us to provide an e cient service to the people being notified in stages. It also means we can dedicate our support to people who have been notified. The process of notifying people began on November 29th 2022.
Joe Ryan, HSE National Director leading the notification programme, said, ‘From now and over the coming months, the HSE will be contacting approximately 113,000 people by letter to inform them that some of their personal data was illegally accessed and copied as part of this cyber-attack.
"As a result of our extensive monitoring and support from security services, we have seen no evidence that personal data relating to the HSE cyber-attack has been shared or used fraudulently.
"We are very sorry that this occurred and ask for people’s understanding as we work through this complex administrative process, in which we hope to support people and continue to answer their questions and requests. This notification process is an important duty for the HSE, as we held people’s personal data, and through this cyber-attack on HSE systems, that information was compromised.’
"In the letters to those a ected the HSE will be apologising to the people being notified that this happened. People being notified will receive a letter telling them what part of their personal information was impacted. The letter will also outline how, if they wish to do so, people can then request to view their exact documents which were illegally accessed and copied. This can be done via a portal on the HSE website at hse.ie/dataprotection or by post."
Joe Ryan continued, "The notification process will go on over the coming weeks and months, as we have to take great care in notifying people correctly and securely. The first group being notified includes approximately 850 HSE sta members. We are writing to them to notify them that data relating to their sta travel expense claims were illegally accessed and copied. This data contained some limited financial details."
He added, "We expect the notification process will take a number of months to complete, as we take the time to contact each person, ensure we have a secure communication with them, and go through the process of assisting them if they want to make a request to view their documents.
"Of the people being notified, 84% of our notifications relate to patient data and 16% to sta data. This means that over the coming
months we will be writing to approx 94,800 patients and around 18,200 members of sta . We anticipate we will have contacted everybody by April 2023 or sooner.
"We sincerely regret the impact this cyber attack has had on our health service, our patients and our teams nationwide. We have taken a thorough approach in responding, from the initial cyberattack to the lengthy period of data review and verification, and now the notification process."
RESPONSE TO THE CYBER-ATTACK
The health service was targeted by a criminal cyber-attack in May 2021. The aim of this attack was to disrupt our health services and computer systems by encrypting them, illegally access and copy data, and demand a ransom.
The cyber-attack was stopped once we became aware of it, and the HSE has worked with a range of state agencies to respond to it. No ransom was paid by the HSE or the State.
Specialist security partners of the HSE have been monitoring the internet including the dark web since the cyber-attack and have seen no evidence at this point that the illegally accessed and copied data has been published online (other than a small amount of data which was referred to in an article in May 2021 by the Financial Times and subsequently removed from the web) or used for any criminal purposes.
The HSE obtained a High Court order on May 20 2021 restraining any sharing, processing, selling or publishing of data illegally accessed and copied from our computer systems. This remains in place to prevent anyone using any of the illegally accessed and copied information. Our cyber security experts are continuing to monitor the internet and the dark web for illegally accessed information and the HSE will act immediately if they see any evidence of this.
ONGOING CRIMINAL INVESTIGATION
The information that was identifed as exfiltrated from HSE systems contained data that held information relating to individuals across the country. The cyber-attack on the HSE continues to be an ongoing criminal investigation which limits the amount of detailed information we can share in the public domain in relation to the data which was illegally accessed and copied, or the details of sites a ected. This is also to protect against the risk of sites being re-targeted or community based ‘phishing’ scams being mounted in those areas.
OTHER ORGANISATIONS AFFECTED
Due to systems that were shared with the HSE at the time of the cyber-attack, Tusla and Children’s Health Ireland were also impacted. Both Tusla and Children’s Health Ireland will be notifying people in the next phases of their respective processes.
HEALTH MATTERS WINTER 2022 70 |
TYPES OF INFORMATION
The health service data that was illegally accessed and copied have been thoroughly examined and validated. They are wide-ranging and include a mixture of personal information, medical information and internal health service data. The internal health service data includes documents such as HR forms submitted by sta in relation to leave and data relating to sta travel expenses.
For the most part, people are being notified that a limited amount of information relating to them was illegally accessed and copied. Personal information includes information on lists such as names, addresses, contact phone numbers, email addresses. Medical information can include some medical notes and correspondence with patients, some lists of patients receiving treatment, patient handover lists, notes, treatment histories and vaccination lists.
We will continue to liaise with the Data Protection Commission and to work closely with our technical experts, An Garda Síochána and the National Cyber Security Centre.HSE’s cyber security defences.
Since the incident we have:
• further strengthened our IT and cyber security
• increased our sta training about cyber security
• worked with international and national cyber security experts to protect against future attacks
For more information about our letters and people being notified, please see below or visit www.hse.ie/dataprotection
HSE SUBJECT ACCESS REQUEST PROCESSING ELEARNING TO SUPPORT ALL STAFF
The HSE’s Data Protection O ice is pleased to launch a new eLearning programme to assist and support all Subject Access Request (SAR) Decision Makers and sta who release personal data under the Data Protection Legislation. This new eLearning programme is part of a series of training, including the 'Fundamentals of GDPR' which should be completed before commencing this programme. Available now on HSeLanD, the new eLearning programme ‘Subject Access Request Processing’ is relevant to all sta who process personal data in their everyday work, and aims to enhance their knowledge of data protection.
It has been designed to provide SAR Decision Makers with the practical skills, critical thinking strategies and relevant knowledge to process data requests and the GDPR and the considerations when processing SAR requests.
The eLearning programme is organised in four distinct sections to aid the learner, followed by a separate assessment:
• Data subject rights
• Processing of SARs
• Restrictions fundamentals
•
SAR scenarios
It will take approximately one hour to complete and includes assessments and extend my learning pieces for those who wish to undertake further learning or who want practical activities to help transfer the learning into their local area of work.
Commenting on the launch of the new Subject Access Request Processing eLearning programme, Mary Deasy, Deputy Data Protection O icer, who led in the development of the programme (DDPO), said, “This programme is designed to assist and support all HSE sta who are involved in the release of personal data as part of their role. Learners will gain valuable knowledge and skills on the application of the provisions of Data Protection Acts and the GDPR to both straightforward and complex requests, by working through exercises and examples on realistic scenarios in the module.”
You can dip in and out of the eLearning programme at any time and can find it, by searching for ‘Subject Access Request’ in the search box or by visiting the HSE Compliance Courses catalogue.
| 71 HEALTH MATTERS WINTER 2022
It’s a Tuesday lunchtime, and through the halls, sta are hurriedly making their way from di erent departments to the meeting room. As they take their seats at the table and take a moment to say hi, one person is starting the online log in process. Sitting in their car, someone else opens their sandwich and hits the ‘Join' button. In other locations across the country and internationally, the co-hosts and guests begin the final countdown and so this session of QPS TalkTime begins.
So what is QPS TalkTime? It’s a fortnightly, one-hour, lunchtime webinar series, focused on improvement, with national and international speakers. It’s free, open to all and you can join yourself, with a group or listen back afterwards. Everyone joining has something in common, whether they are sta or patient partners, they all want to improve our health services for the people using and working in them. More importantly they want a chance to connect with others who have that same desire and with speakers who can share stories, learning and resources to help them on their journey.
Quality and patient safety is something we do every day as part of our work. However, we work in health services where complexity is the norm, where everything and nothing changes and where ultimately we just want to make a di erence. It can be the most rewarding of work and it can, as evidenced by the statistics on burnout and retention be hard. While QPS TalkTime is not a magic solution to the frustration, it’s a chance to hear from experts on a wide range of topics, from colleagues who have implemented improvements and to feel that sense of reassurance and optimism as you connect with others that you’re not alone in this work.
Feedback from participants is central to the design of the webinars and in 2022, we have included sessions on everything from partnering with patients, to psychological safety. We’ve also broadcast live from several conferences to bring the latest thinking to services across the country.
In the spring summer season, 96.5% of participants who took part in a survey said the sessions were excellent or good. Colleagues have described sessions as “Excellent presentation, very informative…” and when asked what was useful, one colleague told us, “Advice from those that had done it successfully before. Both of the projects were brilliant. They were simple ideas that could be easily implemented with great patient-centred results. I think it illustrates that it doesn't have to be complex.”
To register for the mailing list or access previous webinars, scan the QR code here. You can also follow @QPSTalktime or @NationalQPS for more information.


HAVE YOU HEARD OF WALK AND TALK IMPROVEMENT?



The National Quality and Patient Safety Directorate (NQPSD) invites you to have a listen to our new All-Ireland podcast Walk and Talk Improvement: Ideas for Safe Quality Care.


This podcast has been co-designed with patient partners, National Quality and Patient Safety Directorate and Health and Social Care Quality Improvement, Northern Ireland (HSCQI NI) team members.

OUR AIM
This All-Ireland podcast was developed to improve patient care by capturing the personal stories of people who work in and use our health services, and make these conversations available through a new communication platform. The initial project scope includes the development of six episodes based on the six commitments of the HSE Patient Safety Strategy 2019- 2024.
With this podcast, we aim to connect with people interested in quality and patient safety (QPS) across Ireland and bring the Patient Safety Strategy into the QPS conversation. Our ambition is to feature guests from Ireland and Northern Ireland to provide multiple healthcare perspectives from two health systems.
We launched the first four episodes on September 13th for World Patient Safety Day. The episodes are:
• Empowering and Engaging Patients: The role of patient partners


• Empowering and Engaging Sta : Stories, insights and learning from healthcare colleagues
• Reducing harm in healthcare: Recognising the deteriorating patient
• Using data to improve: No data without stories, no stories without data
• Leadership and Governance (in development)
• Human Factors (in development)


WHERE CAN I LISTEN?

We are delighted to say our episodes are available on Acast (scan the QR code), Spotify, Amazon, YouTube and Google podcasts. So if you’re interested in learning more about quality improvement and patient safety, have a listen to the personal stories that our colleagues and patient partners have shared with us in Walk and Talk Improvement: Ideas for Safe Quality Care. https://shows.acast.com/walk-and-talk-improvement/episodes
ACKNOWLEDGEMENTS
This project is the culmination of a wonderful partnership with teams in Ireland and Northern Ireland. We want to give a huge thanks to all involved for their tremendous e orts!
HSE, National Quality and Patient Safety Directorate team: Dr Mary Browne, Dr John Fitzsimons, Dr Maureen Flynn, Sheema Lughmani, Veronica Hanlon and Catherine Hogan.
Health and Social Care QI Hub Team, Northern Ireland: Levette Lamb, Cli ord Mitchell, David Mililiken, Tracey White, Chris McCann and Grainne Mackel.
HEALTH MATTERS WINTER 2022 72 |
HSeLanD: Building for the future
Annual users rise by over 50%
Alot has changed since the HSeLanD team first created its Development Roadmap.
COVID-19 heralded a significant growth in learners accessing HSeLanD, as well as increasing requests to support the design and development of learning resources.
From January 2020, annual users on HSeLanD have increased from 190,000 to 300,000 with over 8 million user log-ins, completing over 3 million eLearning programmes.
This massive surge in demand has led to updates to the HSeLanD Development Roadmap to meet the ongoing demand for this critical service.
Designed to support the rollout of the HSE’s People Strategy 2019-2024, the HSeLanD Development Roadmap 2020 – 2024 is also closely aligned with the work of other national health and social care agencies and key national policies, including Sláintecare and Our Public Service 2020.
The roadmap outlines how HSeLanD will continue to meet the changing needs of the health services, hospitals and linked healthcare agencies to deliver, manage and report on all learning, development, and training activities locally and nationally.



A variety of roadmap enhancements are being delivered across eight core themes:
• Personalised learning experience

• HeLM (Health eLearning Management) and classroom management implementations
• Device-agnostic learning experience

• Enhanced learning design options and mobile learning
• Capacity building
• Learning management and professional development planning (learning pathways)
• Integrated technical infrastructure (HSeLanD user authentication)

• Learning culture and engagement
In addition to improving technical hosting infrastructure for HSeLanD, exciting platform developments include the use of Single Sign-on, making it easier for learners to move seamlessly between the di erent areas of HSeLanD with a single user account. This will support further advancements in further personalising the learning experience based on a learner’s role, interests, and required training.
Direct course linking supports those looking to promote their HSeLanD learning resource by supporting the ability to link directly to any resource or course.


Another technical development is the introduction of Global Search, transforming HSeLanD into a single searchable solution through the use of course tags and new search filter options.

HSeLanD continues to enhance its mobile learning o ering so users can access the site and resources from any device. A first for HSeLanD

is a new HSeLanD mobile learning app that centres around the delivery of bite-sized learning pathways.

Tony Liston, General Manager, HSeLanD, explained, “Now more so than ever, sta across multiple disciplines have more control over their own learning and many more opportunities to develop their skills. The entire HSeLanD team look forward to continuing to work collaboratively with existing and new teams across the health services in 2023 and beyond to deliver a world-class L&D service with the HSeLanD Development Roadmap.”

| 73 HEALTH MATTERS WINTER 2022
'Now more so than ever, staff across multiple disciplines have more control over their own learning and many more opportunities to develop their skills.'
Making activity fun for children attending Community Paediatric Services
FunFit is a new and exciting physical activity programme for children with delayed gross movement skills that has been developed in response to a gap identified by physiotherapists working in HSE paediatric services in Cork.

For children, regular physical activity enhances and promotes the development of essential motor skills, bones and muscles as well as improving cognitive and social abilities. The World Health Organization recommends that all children get a minimum of 60 minutes moderate to vigorous physical activity every day for health benefits.
Unfortunately, Irish children are falling below the bar with only 17% of Irish primary school-aged children achieving this target. For children referred to community therapy services such as physiotherapy and occupational therapy, this figure is likely to be even less.
Currently, there are very little appropriate ‘organised’ activity options in local communities for these children to avail of. As children get older, mainstream sports clubs become less of a place of inclusion and fun and more of a competitive environment where children with movement difficulties get left behind. This results in children losing confidence, dropping out and often being wary of re-joining other clubs or programmes. There is also no referral mechanism to these clubs and no relationship or link to therapy programmes.
Recognising the need to fill this gap, staff in Cork Kerry Community Healthcare including Health Promotion Officers and Community Paediatric Physiotherapists have developed FunFit in partnership with local agencies such as Cork Sports Partnership and Leisureworld Cork.
FunFit is a community-based physical activity programme supporting children aged 8-12 attending HSE Paediatric Services to lead healthy, active lives in a fun, inclusive environment where the emphasis is on participation. The goal is to be the first step to long-term physical activity participation in activities of their own choice in their own communities. Access to the programme is through HSE therapist referral only.
The programme runs for one hour once a week for eight weeks. Children are grouped into 2 sessions according to appropriate age categories. Following training of suitable tutors, a pilot programme was delivered in April-June 2022 with a second pilot currently underway. Sessions are designed around fun games and activities which incorporate the key movement areas such as key fundamental movement skills, co-ordination, balance, propulsion and spatial awareness. Children are also encouraged to suggest and lead out on activities throughout the eight weeks. To date, almost 40

children have started a FunFit programme in one venue and the hope is to grow the programme including expansion to other areas.
Munster Technological University are also supporting the programme evaluation and initial data from Pilot Cohort 1 indicates significant improvements in key fundamental movement skills in just eight weeks. More importantly, however, is that FunFit provided a safe, fun space for these children to be active – their way. At their final session in June we asked children and their parents what were their thoughts on FunFit.
Programme Feedback Snapshot – Children
• Every part of it was my favourite. I loved it all.
I liked how we got to choose a game sometimes ourselves. That was a really good idea
• I really liked the instructors- they were kind ladies.
• My favourite was being outdoors – I didn’t like the time we were indoors
• I got to play with things I had sorta forgotten about like balloons and hula hoops.
Programme Feedback Snapshot – Parents
My daughter felt an equal to all the other participants, she was invited to make a suggestion on a fun game and she was listened to while she explained the "rules" of the game. Even if she wasn't the fastest or strongest, the effort she made was praised by the amazing instructors and her peers.
• It was good for him to see that others have some of the same difficulties as he does
Wish there was a program for them to keep going to every week
• It was very inclusive of all abilities
• My daughter would never be picked on a team in school and I wanted her to have a group where they could have fun and find encouragement and enjoyment.
HEALTH MATTERS WINTER 2022 74 |
Walk and Talk
Physical, social and mental benefits reported from ‘Walk & Talk’ initiative


Community Healthcare East Health & Wellbeing recently worked in partnership with Making Connections, a local charity providing befriending and wellbeing supports for older people, to deliver a ‘Walk and Talk’ programme in Churchtown, Co Dublin.


This new joint initiative was developed by a physiotherapist and occupational therapist in Churchtown Primary Care Centre, who identified a need to provide older service users with an opportunity to participate in physical activity while creating social connections with other people in the locality.
The overall aims of the initiative are to help older people reduce the risk of falling and to help keep bones strong while socialising with others. The benefits of the programme are captured through a physiotherapy assessment to record any improvements in strength. At the start of the programme, many participants had a lack of confidence in their ability to walk following a healthrelated issue or fall. In order to help build their confidence, group leaders walked with participants at their own pace and only to a distance they were comfortable with, while taking breaks as needed. Some of the group found it di cult to walk and talk at the same time as they were focussed on their walking, so the group went to a local cafe after each walk.
Participants in the programme reported that it not only increased their confidence in their ability to exercise and perform daily tasks like shopping, but it also reduced their fear of falling and improved their mental health. Many have also noted that they feel an increased connection with the local community and have developed new friendships.
“I’m now more confident to go out and do my weekly shopping.”
“I am able to go for longer walks since I started, I find it good for my mental health.”
“I would love to do the walks again at a later stage, I live alone and it is nice to have the company of other people.”
To find out more about the Churchtown Walk & Talk programme, email healthpromotioncheast@hse.ie.
GAA HEALTH AND WELLBEING BOARDS LAUNCHED IN WICKLOW

The launch of the GAA Health and Wellbeing Boards initiative was held recently at Wicklow's GAA Centre of Excellence. This initiative aims to raise awareness of mental health and wellbeing supports through the promotion of the 24/7 support and crisis helplines.
It was developed by a co-production group involving representatives from Mental Health Ireland, Co Wicklow GAA Health and Wellbeing, HSE Community Healthcare East Resource O icers for Suicide Prevention, Healthy Ireland - Wicklow, Wicklow Sports Partnership, HSE Mental Health Engagement and Recovery and the Wicklow Mental Health Association. The boards have been funded by the GAA clubs, the National O ice of Suicide Prevention and Wicklow Endless Opportunities. The boards also feature the ‘Five Ways to Wellbeing’, evidence-based actions we can do every day to improve our mental health and wellbeing – Connect, Keep Learning, Be Active, Take Notice and Give. Each board will include the club’s logo and eircode, as well as a Communications Toolkit to support each club’s roll out of the initiative.
Speaking about the initiative, Linda Moore, Head of Service for Mental Health, HSE Community Healthcare East, said, “Our communities play a vital role in creating, promoting, and protecting our mental health and wellbeing. By building awareness of how to look after your mental health and the services and supports that are available both nationally and locally, we are encouraging people to look after themselves and each other by reaching out for support when it is needed.”
Further information is available at: https:// o icialwicklowgaa.ie/supportsinwicklow/
| 75 HEALTH MATTERS WINTER 2022
Stigma around childhood obesity ‘must be broken’

Event aims to inspire best practice in care
The fourth annual ‘Overweight & Obesity… Let’s Talk’ event took place in October at the Royal College of Physicians, Dublin 2. This was a collaboration between the HSE, the Association for the Study of Obesity in Ireland (ASOI) and the Irish Coalition for People living with Obesity (ICPO).The event was attended in person with 60 guests and was also broadcast on-line, with over 1400 tuning in to watch this year’s event. The audience was made up of both healthcare professionals and members of the public. The strong attendance is a reinforcement of the interest for more information about obesity, with this year’s event focused on children and young people.
This event aimed to share the science behind obesity, to inspire best practice in obesity care, to break the stigma of obesity through sharing lived experiences and to explore conversations about growth, obesity and health.
There was a broad range of speakers, opening the event, Dr Ciara Martin, HSE National Clinical Advisor and Group Lead for Paediatrics, said, “2022 sees the continuation of implementation of the HSE Model of Care for the Management of Overweight and Obesity in Ireland. Specifically, two new multi-disciplinary community based services will be set up in CHO 5 and 7. These teams will provide specialist support for children and young people with overweight and obesity. The national specialist service in Children’s Health Ireland is also expanding to treat children and young people with severe and complex obesity.”
Some key information about obesity
• We need to improve the health and wellbeing of all children, irrespective of their body size or shape.
• The options and opportunities we all have available to us affect how healthy we can be, society is awash with unhealthy options and many of these have an impact on health and weight.
Childhood obesity is a chronic disease where excess weight affects health, this can include asthma, joint pain, type 2 diabetes, high blood pressure.
• Overweight and obesity affects children’s quality of life through social exclusion, higher risk of bullying and low self esteem.
• In Ireland, at least 1 in 5 children are estimated to have overweight or obesity as classified by BMI
• COVID-19 restrictions, reduced incomes and food insecurity have had an impact on weight related health behaviours including healthy eating, physical activity, sleep, screen-time and stress.
In the UK the prevalence of overweight and obesity in children increased by 5% between 2019 and 2021
Susie Birney, Executive Director ICPO, Patient Representative ASOI, spoke about the difficulty of raising the topic of obesity with family. “Parents are often blamed, and this can add to the stigma and lack of information about this disease. People want to know how to have the conversation and what support is available. It is clear that hearing the lived experience of those who live with obesity, combined with the science and the research, is an impactful approach for discussing health and weight and also towards addressing the stigma which comes with this disease,” she said.
Sarah O’Brien, HSE, National Lead, Healthy Eating & Active Living Programme, Health & Wellbeing, said, “Under our Healthy Weight for Children Action Plan we are working to support children, young people and families to adopt lifestyles and behaviours that promote health through initiatives like the START campaign (www.makeastart.ie), expanding community-based health promotion programmes such as Sláintecare Healthy Communities and providing training for healthcare professionals with initiatives such as RCSI’s Online Training Course available from www.childhoodobesity.ie.
“We know that our children, young people and families are living in a toxic environment flooded with cheap and intensely marketed energy dense foods. Irrespective of body size or shape, their opportunities to be healthy are being undermined every day. We need to set the stage for child health by working with government to address the big drivers through national policy and legislation that protects children and young people from these aggressive marketing practices.”
You can view a recording of the event on HSE Health and Wellbeing You Tube channel.
HEALTH MATTERS WINTER 2022 76 |
Perinatal Mental Health Service
Music star Emma shines for Perinatal Mental Health Service in first Wellness Day
Singer-songwriter Emma Langford was the special guest at a gathering of 74 Mid West mums in the Castletroy Park Hotel for a Wellness Day hosted by the Perinatal Mental Health Service team from University Maternity Hospital Limerick (UMHL).
The opening performance by the award-winning musician and songwriter was a major highlight of a day that saw the perinatal mental health team and their HSE Mid West Community Healthcare colleagues explore all aspects of wellness, including physical and mental wellbeing, and creativity.
It was the perfect curtain-raiser for an event that also marked the start of World Mental Health Week.
Event organiser Pauline Walsh, a candidate Advanced Nurse Practitioner (cANP) with the perinatal mental health team at UMHL, explained, “One of the main aims of this event is to reduce the stigma and explore the misunderstandings about mental health, and how to manage the challenges of childbirth, maternity leave and parenthood.”

The event included a workshop with art therapist Emilie Browne, while music therapist Pui Sze brought the occasion to a close with a musical performance that had all mums and staff participating.

The Specialist Perinatal Mental Health Service was established at UMHL in 2018, and is jointly governed by UL Hospitals Group and HSE Mid West Community Healthcare. It’s a referral service for women who experience mental health difficulty in pregnancy or up to the first year after birth.
Also part of the varied programme, Tracy Mahedy from Limerick Sports Partnership discussed the links between physical activity and mental wellbeing, while Marie Barrett, Community Dietitian, delivered a presentation on nourishing the body and the mind.
Claire Flynn, Regional Development Officer of the Mental Health Association spoke about the significance of hosting the event as part of World Mental Health Day. She then led a discussion on Managing Stress, and Clinical Psychologist, Dr Nodlaig Moore, introduced the gathering to the benefits of mindfulness and short meditation.
Members of the Specialist Perinatal Mental Health Service team at the Wellness Day in the Castletroy Park Hotel.
From left: Dr Niamh O’Dwyer, Senior Clinical Psychologist; Patricia O’Dea, Senior Social Worker; Aideen Higgins, Senior Occupational Therapist; Pauline Walsh, candidate Advanced Nurse Practitioner (cANP); Finola Roe, Clinical Nurse Specialist; Dr Mas Mahady, Consultant Perinatal Psychiatrist and Team Lead; Sheree O’Brien, Team Administrator; and Jenny Keane, Clinical Nurse Specialist.
Also promoted at the event was ARIES Mid West (Advancing Recovery in Ireland Education Service), the inspirational and inclusive educational programme on recovery and well-being, which is available throughout the region.
Dr Mas Mahady, Consultant Perinatal Psychiatrist and Specialist Perinatal Mental Health Service team lead, said, “We wanted to highlight the value of self-care and self-compassion at a time when a mother’s instinct is to put herself last. It’s important that we continue to acknowledge and respect the role of mothers, by supporting them and their mental health.”
Women can access the perinatal mental health service through their midwifery carers or consultants at UMHL, or through their GPs. See the HSE website for more, at Specialist Perinatal Mental Health - HSE.ie
| 77 HEALTH MATTERS WINTER 2022
Emma Langford provided the pitch perfect opening to the Wellness Day with her musical performance.
NET ZERO GOAL













The Governments Climate Action Plan 2021 sets targets for the Public Sector to achieve a 51% absolute reduction in energy-related Green House Gas emissions and a 50% energy e ciency improvement by 2030, and to achieve net zero no later than 2050.











The HSE recently published its Infrastructure Decarbonisation Roadmap to outline its approach to achieving the targets and the obligations set out in the Climate Action Plan. The Roadmap outlines the work undertaken by the HSE to date and our approach to continuing to reduce carbon emissions from our buildings and their operation.






The Roadmap will form an integral part of the HSE’s strategic approach to delivery of Capital and Property developments and progression of the HSE’s wider Climate Action and Sustainability agenda.
Peter Smyth, Assistant National Director, HSE Capital & Estates and Lead in the HSEs Climate Action & Sustainability O ce, explained, “The Roadmap builds on existing workstreams progressed by the HSE and its partners, particularly the Sustainable Energy Authority of Ireland (SEAI), to reduce the HSE’s existing energy usage and shift the HSE’s use of energy away from fossil fuels and towards renewable and carbon zero energy sources.”
HSE Capital & Estates have identified seven key action areas in the Roadmap to continue, enhance and expand on the work and progress made to date and outline how the HSE will achieve targets set by Government for the Public Sector.

For more information and to request a copy of the HSEs Infrastructure Decarbonisation Roadmap contact climate.action@hse.ie
ENERGY PERFORMANCE OFFICERS MEET TO HELP SAVE ENERGY






With the current energy crisis, increasing bills and accelerating climate action ambitions, energy e iciency and energy related CO2 emission reduction has never been more critical. The HSE and the Sustainable Energy Authority of Ireland (SEAI) are supporting Section 38 and Section 39 bodies to save energy now and plan strategically for the longer term emission reduction targets through a network of Regional Energy Bureaus.
The HSE Estates Climate Action O ice and SEAI hosted an event for Energy Performance O icers (EPOs) from Section 38/39 bodies. EPOs are a member of an organisations senior management team who has been nominated to DCCAE under the Public Sector Energy E iciency Strategy. They are accountable for energy management and performance in each Public Sector organisation.
At the event EPOs from various voluntary organisations met to gain a better understanding of current targets and requirements for public bodies, the benefits of strategic planning for decarbonisation to meet 2030 and 2050 targets, the HSE’s approach to date and supports available from the HSE and SEAI. Representatives from The National Orthopaedic Hospital Cappagh, Stewarts Hospital and Children’s Health Ireland CHI also shared their experiences of working in partnership with the HSE Estates Energy Bureau to achieve energy and carbon reduction targets for the Public Sector.
HEALTH MATTERS WINTER 2022 78 |
HSE unveils its climate plans to help achieve net zero goal
CHI
Climate Action
in climate action and sustainability
Children’s Health Ireland (CHI) recently held their Green Campus Awareness Week, supported by the HSE Estates Climate Action and Sustainability O ce.

In attendance alongside the CHI Climate O cer and HSE Sustainability o cers for the Dublin North and South regions were CHI’s waste partners Thornton’s (for recycling, domestic and food waste) and Stericycle (clinical waste mangers).
Each day of the week, sustainability was celebrated and discussed at each of CHI’s sites: CHI@Tallaght, CHI@Crumlin, CHI@ Connolly, CHI@Herberton and CHI@ Temple Street.
CHI o cially registered with the An Taisce Green Flag programme in September 2022 and are focusing on waste and energy consumption reduction. Stericycle and Thorntons educated sta across all sites on correct waste segregation and answered any queries that
they had in relation to waste management. The HSE Sustainability O cers advised on energy-saving initiatives and supports available from the Climate Action and Sustainability O ce. A fun quiz was shared with sta on the environmental impacts of healthcare, with spot prizes which were kindly donated to CHI. CHI’s Green Lead educated sta on the
correlation between climate change and health – described in the Lancet as ‘the greatest threat to public health of the 21st century’. The legal and moral responsibility of a paediatric healthcare provider to safeguard the future health of their patient cohort was discussed with sta and their suggestions and recommendations to improve sustainability were recorded. Sustainability initiatives already under way across CHI were highlighted, as well as advisement on how sta can become actively involved.
A beautiful art installation piece designed by CHI Commissioning Workstream Project Manager, Anne Dowling, utilising healthcare waste plastics was displayed to raise awareness of the environmental impact of care delivery within healthcare in Ireland. The piece was thought-provoking and got sta reflecting on the level of single-use items utilised in care delivery. Sta were challenged to consider their consumption and look to renewables where clinically appropriate. ‘Mr T’ the Thornton’s bin was around raising awareness with sta and patients at the Temple Street and Crumlin sites.
Great awareness was raised across all of the sites with some wonderful ideas shared between sta on the next steps in CHI’s sustainability journey. The events would not have been possible without the support of the HSE Climate Action and Sustainability O ce, Thornton’s and Stericycle.

| 79 HEALTH MATTERS WINTER 2022
lead the way
Cape made of plastics utilised in healthcare to raise awareness on the impact our consumption has on the planet. It was designed and made by Anne Dowling who works in the Project Management O ce in CHI. Figure 3 From left to right - Niamh Clonan from Thornton's; Robert Sweeney, HSE Sustainability O cer; Sonia O'Keefe from Stericycle; members of CHI@ Connolly's Green Team led by Annemarie Dowling, Assistant Director of Nursing, CHI@Connolly.
Stars visit UHL


Hurling team greeted by staff and patients












L imerick senior hurling stars Declan Hannon, Cian Lynch, Paul Kinnerk and William O’Donoghue, team manager John Kiely, and Limerick GAA County Board Chairman John Cregan visited University Hospital Limerick to meet patients and pay tribute to frontline sta for all their e orts to keep the Midwest public safe during the COVID-19 pandemic.
They were greeted by a large group of sta headed by John Doyle, Director of Scheduled Care, UL Hospitals Group, who applauded the All Ireland champions for the sheer pleasure they had generated throughout Limerick and the Midwest with their performances on the pitch throughout the darkest days of the pandemic.




Prior to the players and manager visiting wards in the hospital with the Liam MacCarthy Cup, Limerick GAA County Board chairman John Cregan presented sta with a signed and framed Limerick jersey as a token of appreciation for the dedication and hard work of all sta in UHL and all sites across UL Hospitals Group.


All pictures by Brian Arthur Photography


 Breda Duggan, General Manager, Cancer Services, UL Hospitals Group, with Limerick senior hurlers Paul Kinnerk, Cian Lynch, William O’Donoghue and team captain Declan Hannon. The hurlers are holding the signed jersey they presented to sta as a token of Limerick GAA’s gratitude to all sta of UL Hospitals Group.
Sta from University Hospital Limerick with members of the Limerick senior hurling team on their visit to the hospital.
Cian Lynch signs Danchelle Duhig’s plaster while team-mate Paul Kinnerk looks on
Fergal Archer gladly gives up his board-game to GAA county board chairman John Cregan for the chance to hold the Liam MacCarthy Cup and chat with William O’Donoghue (left) and Cian Lynch.
Limerick senior hurler William O’Donoghue signs the jersey of delighted hurling fan Cian Fitzpatrick
Cian Fitzpatrick with the Liam MacCarthy Cup and his sporting heroes William O’Donoghue, Cian Lynch and Declan Hannon
Breda Duggan, General Manager, Cancer Services, UL Hospitals Group, with Limerick senior hurlers Paul Kinnerk, Cian Lynch, William O’Donoghue and team captain Declan Hannon. The hurlers are holding the signed jersey they presented to sta as a token of Limerick GAA’s gratitude to all sta of UL Hospitals Group.
Sta from University Hospital Limerick with members of the Limerick senior hurling team on their visit to the hospital.
Cian Lynch signs Danchelle Duhig’s plaster while team-mate Paul Kinnerk looks on
Fergal Archer gladly gives up his board-game to GAA county board chairman John Cregan for the chance to hold the Liam MacCarthy Cup and chat with William O’Donoghue (left) and Cian Lynch.
Limerick senior hurler William O’Donoghue signs the jersey of delighted hurling fan Cian Fitzpatrick
Cian Fitzpatrick with the Liam MacCarthy Cup and his sporting heroes William O’Donoghue, Cian Lynch and Declan Hannon
| 80 HEALTH MATTERS WINTER 2022
Dan O’Brien was delighted to hold the Liam MacCarthy Cup and meet Limerick senior hurlers Declan Hannon, Cian Lynch, Paul Kinnerk and William O’Donoghue Libby O'Shaughnessy was delighted to get her hands on the Liam MacCarthy
Caoimhe Quaid with Limerick hurling stars Declan Hannon, William O’Donoghue and Cian Lynch
Young Peter O’Donnell gave the Liam MacCarthy Cup a very close inspection when he met Limerick hurler Paul Kinnerk
Baby Johnny Kingston and mum Maria with the Limerick hurlers (from left) Paul Kinnerk, Declan Hannon, Cian Lynch and William O’Donoghue
Sta from the Acute Medical Assessment Unit at University Hospital Limerick
Flu Vaccine for Healthcare Workers
It takes just a few minutes to protect yourself and the people around you.
You are 10 times more likely to get flu
Flu is serious
1 in 5 healthcare workers develop flu every year.
Up to 500 people die from flu every year in Ireland.
Flu causes pneumonia and bronchitis and can make chronic health conditions worse.
You can spread flu without knowing it
Your patients rely on you to protect them
You can protect your family and those around you
Flu vaccine is safe
Some people have no symptoms.
People with weakened immune systems or who have underlying health conditions rely on you to be vaccinated to protect them against flu.
Getting the flu vaccine also protects your family, your colleagues and the patients you care for.
It’s been given to millions of people for more than 60 years.
HEALTH MATTERS WINTER 2021 54 | Public Health Advice hse.ie/flu
Order Code: HN100467
If you work in healthcare, you are at increased risk of being exposed to COVID-19



It is important to keep up-to-date with your COVID-19 vaccines. This is because the protection you got from your previous vaccines or from a COVID-19 infection may weaken over time.



Protect yourself and the people you care for There is evidence that a second booster dose may reduce infection rates.


Get a COVID-19 vaccine at the same time as other vaccines You can receive your seasonal flu and COVID-19 vaccinations at the same time.
COVID-19 vaccines are free COVID-19 booster vaccines are available from CVCs and participating GPs and Pharmacies. You may be able to get vaccinated at your workplace.





Book an appointment at a COVID-19 vaccine centre near you at hse.ie or make an appointment with a participating GP or Pharmacy. Use the pharmacy finder at hse.ie to find a participating pharmacy.


HEALTH MATTERS WINTER 2021 54 |
#ForUsAll