





MATTERS AUTUMN 2023 GET YOUR FLU AND COVID-19 VACCINES Protectyourself Protectothers
A MESSAGE FROM OUR EDITOR
Welcome to the newly revamped Health Matters. We have added some new features that we hope you will enjoy as we continue to showcase the exemplary work that is being carried out across our health service. We put the spotlight on climate change and the role the Irish health service can play in helping Ireland meet its climate targets in the coming years.
The HSE Climate Action Strategy outlines how the organisation will reduce emissions and become a more sustainable healthcare service. And, of course, we all have a part to play in its success. Little actions can have large impacts.
In this edition, as National Breastfeeding Week nears, we chat to teacher Laura Tighe about her experience breastfeeding her twins. She shares some great insights for mums and expecting mums.

In our new What Is section, we take a close look at social prescribing to find out exactly what it is, how is works, and the impact it can have on its service users across the country. As we move towards Sláintecare and trying to keep people well and out of hospital, the concept of social prescribing is such an important one.
One of our Hot Topics is the recent availability of free fertility treatments for eligible couples. It will make a huge difference to men and women who are eager to become parents but have been unable to afford private fertility treatment.
They are just a small number of the many stories we have for you this edition.
Once again, a big thank you to all the teams around the country who have submitted their initiatives and programmes. It is great to be able to showcase the amazing work being done to make life better for people who use our services.
Joanne Weston Editor
CONTENTS 1 Consultant fundraises in memory of sister-in-law 2 VR used to treat phobia of dogs 3 The Wagon Project 4 Talking Point : Climate change 6 Hot Topic: Fertility treatment 7 Spotlight on: Flu vaccine 8 Mum Laura talks about breastfeeding her new twins 11 Pain-breakthrough in Galway 12 Spotlight on: Community Inclusion Hub 13 Hot Topic: Healthy Ireland plan 14 What is: social prescribing 16 Community Connector 17 Day in the Life 18 Severe asthma clinic 19 Hot Topic: Drug checking 20 Teleatherapy in Laois/O aly 21 Spotlight on cancer in young adults 22 Kathleen's mission to build dementia inclusive communities 26 Health regions in focus 28 Lymphoedema clinic 29 COPD pilot initiative 30 National Clinical Surveillance Infection Control System 30 Nurse-led oncology service 31 Change Guide 32 Hot Topic: ADHD Changing Lives programme 33 Spotlight on: the Health Passport 34 Reablement getting people back to their homes and lives 36 Spotlight on: Telehealth 37 Tobacco free campus visit 38 Hot Topic: Assisted DecisionMaking Act 39 Supporting self-management 40 Meet the Team: Community Intervention Team 42 News part 1 44 Steps to Health 46 Awards and accolades 48 Team providing psychological support for refugees 50 Spotlight on: Screening 52 Diversity eLearning programme 53 Clinical audit study in Our Lady of Lourdes Hospital 54 Migration to HealthIRL 54 Evaluation Framework 55 Walk and Talk podcast 55 Benefits of using Project Management O ce 57 Creative reflection for nurses and nursing students 57 World Patient Safety Day 57 Walk and Talk podcast 58 New cancer research clinic in Tallaght 59 Maternity Bereavement Survey 60 News part 2 62 HSE Annual Report and Financial Statements 2022 64 National Policy for Consent in Health and Social Care Research 65 Mental Health Crisis Resolution Service Model of Care 65 80% of sta using NiSRP 66 New care pathways across acute and community settings 68 Hepatitis C home testing 68 Patient Safety Act 69 Reform of Home Support Services 69 Controls Assurance Review Process update 70 Caru end-of-life project 71 IFMS launch 72 First Patient Partnership Forum to be held 73 National Travel and Subsistence Unit 73 MN-CNS project expands 74 Events 78 Health and wellbeing 80 Way to Unwind: Make self-care a priority
The climb

Consultant climbs 32 peaks in a week for hospital fundraiser

During the seven-day trek with colleague and friend Professor Richard Greene, the pair climbed a combined altitude of 16,000 metres, which is almost twice the height of Mount Everest.
Richard, who has previously climbed Africa's tallest peak, Kilimanjaro, tripled the initial target of €10,000, with more than €30,000 coming in from supporters at home and overseas.
During the seven-day trek with colleague and friend Professor Richard Greene, the pair climbed a combined altitude of 16,000 metres, which is almost twice the height of Mount Everest.
Ahospital consultant has climbed the highest peak in every county in the country within a week to fundraise in memory of his sister-in-law.

Dr Richard Horgan, a consultant obstetrician and gynaecologist based in Cork University Maternity Hospital (CUMH), completed the challenge almost ve years after the death of his wife's sister, 38-year-old Orla Gosnell. All the money raised will go to creating dedicated spaces for patients and staff at CUMH.
Orla, a social care worker, died in December 2018, ve months after giving birth to her fth child at CUMH.

Richard took the nal steps of the challenge in mid-July after completing an average of four to ve peaks per day.

As he descended the nal peak, 918-metre tall Galtymore on the Limerick/Tipperary border, he said, “I am overwhelmed by the love and respect for Orla, the support for Richard Greene and I, for CUMH, and I am humbled by the generosity and support of so many,” he said. Richard was joined by Orla’s husband Robert, her mum Myriam and dad Kees on his nal descent.
The challenge began in Cork on Sunday, 16 July and the climbers revealed they slept for little more than four hours per night. They travelled more than 2,000km around the country and slept overnight at the base of the following morning's peak.
He said he hopes the new space will include a symbol speci cally remembering Orla and her experiences in CUMH.
“What has always been to the forefront in my work is the patient's experience, the mother's experience - even in bad outcomes - and to make the experience as positive as we can. When I walk into the maternity hospital, there are magni cent glass corridors and there's an opportunity to install seats. We have three oors to work with and could do it on all oors. It is simply somewhere patients, their partners and staff can sit, take a moment, have a chat, take a phone call - have those few minutes,” said Richard. HM
MY STORY
Dr Richard Horgan after he reached the nal peak of his week-long fundraising challenge
Orla Gosnell, who passed away ve years ago. The fundraiser was in her memory.
| 1 HEALTH MATTERS AUTUMN 2023 MY STORY
Team uses virtual reality to help children overcome fear of dogs
A team in Clare have piloted a unique programme aimed at helping children overcome their fear of dogs.

The Clare Primary Care Psychology team work with children whose fear was getting in the way of their enjoyment and participation of everyday activities. They built a partnership with a number of key services in the community who each contributed a key ingredient to the intervention which was named ‘Brave with Dogs!’ It was then piloted with a small number of children and their parents.

The participating families described the impact of dog phobia on family life and the child’s social activities.
Exposure therapy is the treatment of choice for overcoming a fear. The child is supported to face their fear in small steps whilst feeling safe and in control. Instead of using a real dog, the team used the next best thing – Virtual Reality (VR)!
dogs. In this way, the children
A company called oVRcome provided the children with VR goggles and an app for viewing VR footage of dogs. In this way, the children could feel like they were interacting with a live dog and could complete exposure steps both in the clinic and at home.
As well as learning to understand dogs, another important component was teaching children how to keep themselves safe and prevent any unwanted attention from a dog. They learned to do the ‘X-Factor’. This is where you stand still with your arms crossed at your chest and look away from the dog.
“All of the children reported signi cant progress with their goals of being able to visit friends who have dogs; play out in the local area with the neighbouring children; and feel more comfortable going to the beach, park or sports grounds when dogs were around,” said Susan Quain, Psychologists Assistant.
aspects of the pilot intervention that helped to achieve these goals: Parents learned how best to support their child by being a calm, steady presence when their child’s anxiety was heightened.
“The children themselves learned to understand dogs better which helped to lower their fears. They also learned strategies for protecting themselves if they felt threatened in a situation with a dog. Virtual Reality also played a useful role for some of the children. However, some children required real-life experience with dogs as well to progress. All of these elements worked together to reduce the children’s fear and enhance their quality of life.” HM
FEATURE 2 |
The Clare Primary Care Psychology team: Melissa Garrihy, Psychologists Assistant; Eliza Walsh, Psychologists Assistant; Dr Suarla Deane, Clinical Psychologist. Missing from photo: Susan Quain, Psychologists Assistant.
HEALTH MATTERS AUTUMN 2023
Dawn Kavanagh from Dogs Trust demonstrating the X-Factor.
The Wagon Project
supports Traveller men to take pride in their culture

Institute of Art, Design and Technology (IADT).







Based at Hazel House, Tribadden, Co Dublin, the aim of The Wagon Project was to promote positive mental health among Traveller men and young Travellers through culturally appropriate means. In essence, it revolved around the promotion of physical, emotional and cognitive health in a social and culturally-speci c environment that encourages stewardship.
The Wagon Project was instigated by two Traveller men who wanted to pass on the custom of building a traditional barrel top, old-style Wagon to the younger generation. Led by Southside Traveller Action Group (STAG) through a Men’s Shed programme, the project developed into a thriving cross-community initiative with many services coming together to offer their support and expertise. These included HSE Community Healthcare East, Connecting for Life, Healthy Ireland, Tusla, Dún-Laoghaire Rathdown County Council, CYPSC, Hazel House Café and Woodwork School in Tribradden, and the
Area Lead for Mental Health Engagement, HSE Community Healthcare East, Andrea Koenigstorfer, said, “I’d like to give a special acknowledgement to the interagency Working Group who helped provide a platform of support for Traveller Men to take pride in their heritage and culture through this project. The project not only supported Traveller men to come together to showcase and share their skillsets to future generations, but it also resulted in a range of physical, mental and social bene ts for the participants”.
The Men’s Shed participants ‘Shedders’ described their experience of the Wagon Project as a celebration of Traveller culture. The ‘Shedders’ have also spoken of the joy they felt in working together, as well as the pleasure and pride they took in everything they achieved, saying “It’s a live museum”; “Did you see the shelves in the Wagon?... I made them!”; “It’s peaceful here, we’re focused when we’re here, and busy”; and “There’s no distractions and I love it.”
Moving forward, the Traveller Men’s Shed are going to help restore two old wagons that are in Hazel House, and the Working Group is looking at recommendations for how the project can build on its initial success and continue to be supported. HM


FEATURE | 3 HEALTH MATTERS AUTUMN 2023
HSE Climate Action Strategy will ensure more sustainable healthcare service

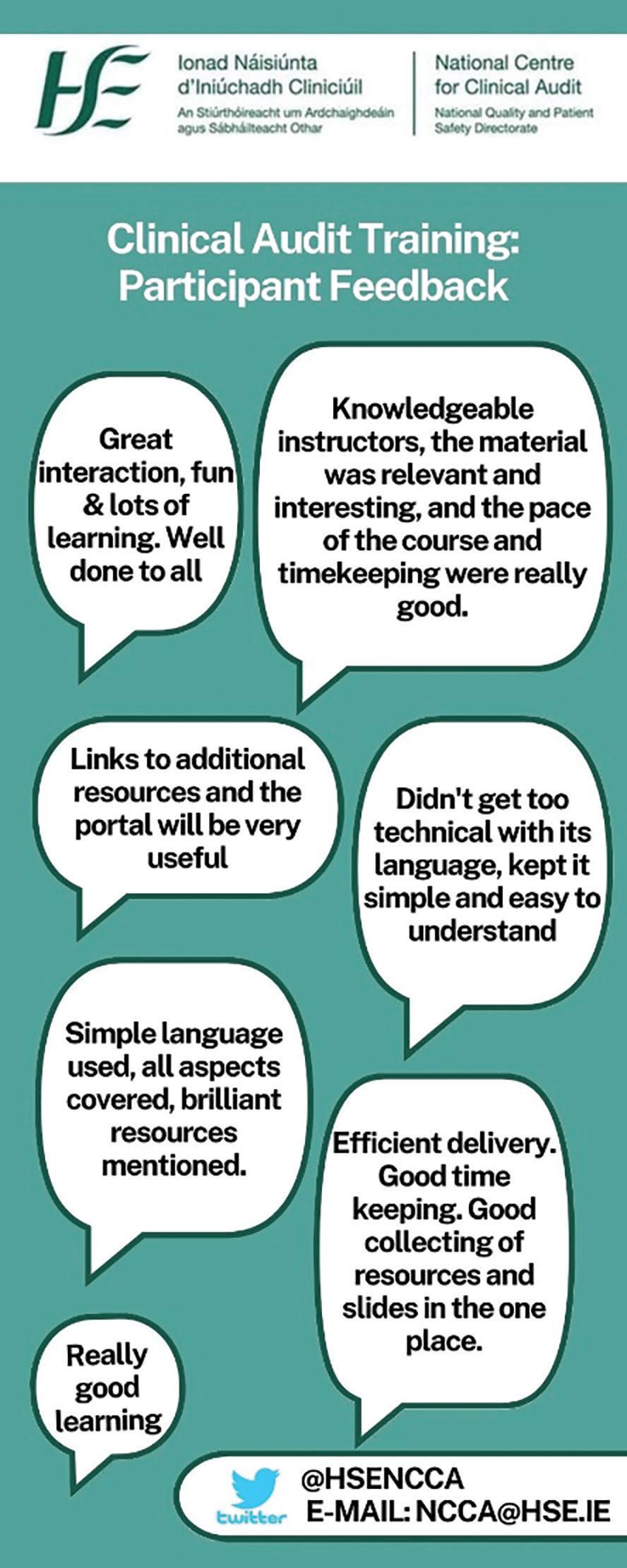
The climate crisis “T


he reality is that the climate crisis is a health crisis and the healthcare sector is a considerable contributor to net global emissions, estimated to be between 5 and 15%.”
That was the simple facts behind the newly published HSE Climate Action Strategy, outlined by Dr Philip Crowley, HSE National Director for Strategy and Research.
The HSE aims to deal with the growing health impacts of climate change by reducing emissions and becoming a more sustainable healthcare service. The HSE Climate Action Strategy will help us achieve this goal.
THE CLIMATE ACTION STRATEGY


FOCUSES ON SIX MAIN AREAS:
• Sustainable buildings and the green environment
• Transport and mobility
• Sustainable procurement
• Greener models of healthcare
• Water and waste management








• Adaptation and resilience
BUILDING ON EXISTING WORK WITHIN THE HSE
The recently published HSE Climate Action Strategy builds on ongoing work within the HSE led by Peter Smyth, Assistant National Director, HSE Capital and Estates and his team in the Capital and Estates Climate Action and Sustainability Of ce.
TALKING POINT
HEALTH MATTERS AUTUMN 2023 4 |
Delivering this Strategy requires urgent and collaborative action with staff, service users, partners and communities. As a leading Public Sector Body, we must align with the Government Climate Action Plan which means by 2025, we will help to:
• achieve the buildings and retro tting targets laid out in the Public Sector Climate Action Mandate
• carry out and review the Public Sector Climate Action Mandate every year
By 2030, we will help to:
• reduce greenhouse gas emissions from the public sector by 51%
• improve energy ef ciency in the public sector by 50%
WHAT WE’RE DOING

Work is already under way to reduce our carbon emissions and become a health service that leads by example on climate action. As part of this work, we have:
• set up working groups to deliver on our 10 objectives within the strategy
• begun to set up structures to help us implement climate action initiatives at local level ef ciently and effectively
• begun developing an online Sustainability Assessment Tool for smaller healthcare sites, providing support and guidance on energy, carbon, water and waste reduction


• started to roll out water conservation and waste prevention training through the Green Healthcare Programme
• put over 100 energy teams in place at our largest energy user sites
• supported these sites with dedicated energy of cers
• started carrying out shallow energy retro t and deep energy retro t programmes
• applied an energy-ef cient and carbon-zero design approach to all of our capital works
MOVING FORWARD
Moving forward we want to support and promote a positive cultural change. We will make sustainability core to our future decisions and ensure that it is embedded into our everyday ways of working and culture. In order to do this we will:


• continue to raise awareness and drive climate action through a communications campaign

• support staff service users and communities to act as sustainability and climate action activists by providing national guidance, tools, support and measures to track improvements

• continue the ongoing focus on prevention and social prescribing, as the best way to improve patient care is to prevent illness
We recognise and appreciate the important role we’ll play in tackling the climate crisis. The strong alignment between caring for the health of environment and caring for the health of our patients should motivate us all to action in this space ensuring that we protect the health and wellbeing of future generations. HM
TALKING POINT
Kevin Sheridan, HSE Estates Manager; Helen Maher, HSE Estates Manger; Cathryn Buckley, Of ce Manager HSE Capital and Estates; and Dr Philip Crowley, National Director, Strategy and Research, HSE. Back: Ken Hyland, Sustainability Of cer; Neil McManus, Energy Of cer; and Roisin Breen, Climate Action, Programme Lead.
| 5 HEALTH MATTERS AUTUMN 2023
THE HEALTHCARE SECTOR IS A CONSIDERABLE CONTRIBUTOR TO NET GLOBAL EMISSIONS, ESTIMATED TO BE BETWEEN
HSEFUNDED FERTILITY TREATMENT SERVICES
HOT TOPIC 74%
The HSE has introduced publicly funded fertility treatment services from September 2023. This includes treatments such as IVF, IUI and ICSI for people who meet the access criteria. The service will initially be provided by approved private providers on behalf of the HSE, while the HSE over time builds up a network of public capacity to deliver the service directly within the public health system.
People who are experiencing fertility issues can be referred by their GP to their local regional fertility hub, where they can expect to avail of a wide range of investigations and interventions including: relevant blood tests, semen analysis, fertility-related surgeries and medical management of fertility challenges including ovulation induction with follicle tracking. If further advanced treatment is recommended and the patients meet the access criteria, the hubs will refer patients to a HSEapproved private provider of their choosing. HM
OF THE PUBLIC SUPPORT PUBLICLY FUNDED FERTILITY TREATMENTS TO HELP PEOPLE CONCEIVE
THERE ARE SIX REGIONAL FERTILITY HUBS WITHIN PUBLIC MATERNITY HOSPITAL NETWORKS ACROSS THE COUNTRY THAT ARE ALREADY PROVIDING SERVICES TO PEOPLE EXPERIENCING FERTILITY ISSUES.
There is no cost to patients for the recommended treatment through the private providers.
“We are delighted to see investment in this area to ease the nancial burden for public patients and it will signi cantly increase access to services for many. We have designed caring and ef cient pathways for patients, ensuring a safe and quality service, so that fertility issues are addressed through the public health system at the lowest level of clinical intervention necessary”
Dr Clíona Murphy, Clinical Director, HSE NWIHP
THE HUBS CURRENTLY RECEIVE APPROXIMATELY
150
ON A
BASIS
HOT TOPIC
HEALTH MATTERS AUTUMN 2023 6 |
NEW REFERRALS
MONTHLY
Vaccines for healthcare workers
Protect yourself. Protect others.
Although the COVID-19 pandemic is no longer a public health emergency, vaccination will still play a vital role in keeping u and COVID-19 at bay this autumn and winter.

Getting your recommended u and COVID-19 vaccines in the autumn will help protect you, your family, colleagues and patients throughout the winter months.















As a healthcare worker, you are at higher risk of being exposed to u and COVID-19 so it is important to keep up-to-date with your vaccines.

WHERE YOU CAN GET A FLU OR COVID-19 VACCINE?
You can get your u and COVID-19 vaccines at work from early October, and also from participating GPs and pharmacies. These vaccines are free for healthcare workers. It’s safe to get both vaccines at the same time, you will get one vaccine in each arm.
TRAINING ON HSELAND
‘Flu and COVID-19 Vaccines for Healthcare Workers–protect yourself, protect others’ is a 15-minute online course designed to educate and inform healthcare workers about the vaccines. Go to hseland.ie and search for it.







FIVE THINGS YOU SHOULD KNOW













1 VACCINATION IS THE BEST PROTECTION AGAINST VIRUSES LIKE FLU AND COVID-19
To prevent the spread of u and COVID-19, it is important to follow infection prevention and control procedures such as good hand hygiene. However the best way to protect yourself from catching these viruses is by getting the vaccines.


2 EVERYONE IS AT RISK OF BECOMING SICK FROM FLU OR COVID-19
Even in healthy young people, u and COVID-19 can cause fever and fatigue. The risk of serious illness is higher in people over 50 and those with a weak immune system.
3 IMMUNITY FROM INFECTION WEAKENS
Getting the COVID-19 vaccine will top-up your immunity against COVID-19 for the months ahead. The u vaccine helps your immune system produce antibodies to ght infection.
























4 IT IS EASY AND FREE TO GET VACCINATED
You do not need to travel far to get the vaccines and the vaccines are available free of charge at a local participating GP or pharmacy.
5 THE VACCINES ARE SAFE AND EFFECTIVE
The HSE only uses vaccines when they meet the required standards of safety and effectiveness and after the European Medicines Agency (EMA) has licensed them. Vaccines offer strong protection, and effectiveness can vary from person to person. However, if vaccinated people do get sick, they are likely to have milder symptoms. HM
| 7 HEALTH MATTERS AUTUMN 2023
SPOTLIGHT
ON
LAURA'S STORY
Nationwide breastfeeding supports available
The number of babies breastfed in Ireland is increasing, with an 8% increase in the number of babies breastfed at the rst public health nurse (PHN) visit in the last seven years (from 54% in 2015 to 62% in 2022).
31.5 new lactation and infant feeding posts have been recruited in the last three years. There are now 56 lactation and infant feeding posts available nationwide to ensure that all maternity and PHN services have specialist support available. They provide complex support for some mothers and babies, and support ongoing skills development of other frontline colleagues within midwifery and nursing services.
An updated infant feeding education programme is now being rolled out nationally. This programme focuses on standardising the delivery of breastfeeding education and
skills training. It maximises blended learning and ensures midwives and PHNs are up to date with emerging evidence. HM
Over 150 breastfeeding groups run by HSE and HSE-funded volunteer breastfeeding organisations are available, with groups in every county. Find your local group on www.mychild.ie
HSE staff are entitled to https:// healthservice.hse.ie/staff/leave/ breastfeeding-breaks/" breastfeeding breaks at work up until their child’s second birthday. New legislation was introduced in July 2023 which extends this entitlement to all mothers in employment.
Popular online resources include virtual breastfeeding groups and the HSE’s mychild.ie website www2.hse.ie/services/ask-our-breastfeeding-expert, ‘ask our expert’ live chat and e-mail breastfeeding support service available seven days a week.
HEALTH MATTERS AUTUMN 2023 8 |
Laura Tighe, mum to twins, Neasa and Culainn, who were born on 6 January in Sligo University Hospital at 37 weeks and five days, shares her experience.
The Sligo mum had always planned to try breastfeeding her daughter and son (7 months) but was initially worried, like any new mum is. Speaking about her journey, Laura said, “Having done some research, breastfeeding was always something I wanted to do because of the bene ts of it. Being a rst time mum, I looked then into what was available in Sligo and I attended antenatal classes, some of which were speci c to twin mums.
“I am a huge advocate for breastfeeding. As a PE teacher with an interest in health and lifestyle, I understand the importance of good nutrition. I knew there were huge bene ts to breast eeding my babies.

“Eventually, I was able to tandem feed the twins….. which was lovely. But of course, I had some concerns. Like other mums, I worry and aone of the worries I had was whether the babies were getting enough milk. You can’t measure it so you don’t know how much your babies are getting, and this is worrying for a rst-time breastfeeding mum."
Lynn was a huge support because if you questioned yourself she confirmed that you were doing the right thing and she would give you advice on how to do it better.
was going to be the case," explained Laura.
Laura met Lynn Cunningham, the Infant Feeding and Lactation CNS at Sligo University Hospital, before her twins were born, which the Sligo mum found of great support to her, particularly in the beginning.
“I told her I wanted to be able to express milk too and she [Lynn] would advise me on products that worked well. She guided me through colostrum harvesting and was always available for advice when I needed it. She would say to me ‘your body knows that you have had twins, so it will produce enough milk for two babies. I had to trust that this
“Lynn was a huge support because, if you questioned yourself, she con rmed that you were doing the right thing and she would give you advice on how to do it better. There was huge bene ts to having her in the hospital. She made it all easier.
“Many people thought that it wouldn’t be possible to breastfeed twins and most encouraged me to bottle feed but I knew what was best for the babies and I wanted to try my best to do it. I was conscious it may not have worked out for me for multiple reasons, for example, if the babies had to go to NICU or the babies wouldn’t take to
INTERVIEW | 9 HEALTH MATTERS AUTUMN 2023
breastfeeding or it was too sore, I did not have the supply and so on."
Speaking openly about her journey, Laura encouraged all mums to try breastfeeding.


“You hear about many women who attempt breastfeeding and they might stop between six and eight weeks. I really feel if you can keep going for another couple of weeks it becomes so much easier, I can’t even describe how much easier. It goes from being tough, where you are sleep deprived, you’re worried and a little bit stressed whether they are getting enough milk to much easier. After you pass that six to eight-week mark, all that hard work pays off and all of a
sudden you are not worrying about your supply and you can go anywhere and give them the best food that you could give to your baby on tap with no organisation or prep work prior to leaving the house. It becomes much easier.
“It also creates these intimate moments with your baby that I can’t even explain and it’s just a really lovely connection. You become so proud of yourself, you are literally their lifeline. It’s so special and it’s not going to last forever and, in the grand scheme of things, it is a short amount of time.” Laura is returning to work as a PE teacher, and is looking forward to continuing to breastfeed her twins, with support from her workplace. HM
A key priority for us at the Rotunda is supporting our staff in their breastfeeding journey. We have a dedicated breastfeeding room equipped with a multi-user electric breast pump, fridge and comfortable seating. We subscribe to the recent Work Life Balance Act 2023. This legislation entitles women to breastfeeding breaks from what was previously six months to two years.
HEALTH MATTERS AUTUMN 2023 10 | INTERVIEW
Geraldine Gordon, Clinical Midwife Specialist in Lactation at the Rotunda Hospital
Pain blockers
University Hospital Galway becomes first centre to introduce revolutionary nerve-blocking probe
University Hospital Galway (UHG) has become the rst centre in Ireland to introduce a nerve blocking probe which uses liquid nitrogen to freeze nerves and remove pain post-surgery.

The CryoNerve blocking probe delivers liquid nitrogen at a temperature of around -190 degrees from the tip of the device during invasive surgery.
I can honestly say that I have had zero pain since my surgery in this area on my back, which I affectionately call my shark bite.
This device is applied to the nerve underneath each rib, freezing it and temporarily stopping its conduction. These nerves are one of the main sources of pain after chest surgery, and cryo nerve block helps by temporarily shutting off the nerve.
Once frozen, it thaws over a period of months, reducing pain for patients recovering from major surgery.
Dr Alan Soo, Consultant Cardiothoracic Surgeon, UHG, who has introduced the technology to Ireland for thoracic surgery, explained that the device also has the potential to be rolled out to cardiac surgery.

“Evidence has shown that this is effective in
reducing pain and does not cause permanent damage to the nerves and surrounding structures. In UHG, we have been designated as the rst centre to introduce this device. We have since employed this device in around eight patients. All patients who received this treatment on top of their usual analgesic strategy had dramatic improvement on their post-operative pain and reduction in length of stay. We aim to introduce this strategy to patients receiving cardiac surgery soon,” he added.
Sligo woman Imelda Ryan-Jones was the rst person to avail of the device in Ireland. Imelda underwent surgery in February during which the device was used on the nerve endings in her back.
“I can honestly say that I have had zero pain since my surgery in this area on my back, which I affectionately call my shark bite,” said Imelda.
“I have had severe pain around my front ribs, as they were moved so much during surgery, but much to my relief, my shark bite has de nitely been pain-free. I practically forgot it was there and it has healed tremendously well too. I highly recommend this new innovative procedure and it was my pleasure to participate.” HM
| 11 HEALTH MATTERS AUTUMN 2023
Dr Alan Soo and Imelda Ryan-Jones
Dr Alan Soo and Imelda Ryan-Jones
Community inclusion

Hub helps connect young service users with their community
Inclusiveness and building relationships are at the heart of the newly opened Community Inclusion (CI) Dungloe Hub in Donegal. It is a HSE-run school leaver service for young adults who have an intellectual disability transitioning to adult services. The young adults who attend will have recently nished school or other education and training programmes.


Our central location is accessible to all and gives a great feeling of inclusiveness. We have a real sense of connection with the community around us.
The Hub works closely with the young adults to build independence, set personal goals, and support them to live their life in the way that they want, with the support of the HSE day service co-ordination team and the guidance of cers within that team. The role of the guidance of cers is to work with each individual to identify strengths and support needs and guide them to the service that will best meet those needs and wishes.
It is part of Donegal Community Inclusion Training Services (DCITS), a HSE day service provider which delivers services for adults between the ages of 18 to 65 years with intellectual disabilities across the county. DCITS’
aim is to ensure that people using the service are at the heart of everything they approach. This is a process that involves listening, thinking, sharing ideas and providing supports so that those using the service are at the centre of the decisions which relate to their lives.
Deborah Smith, CI Dungloe Hub Co-ordinator, said, “Our central location is accessible to all and gives a great feeling of inclusiveness. We have a real sense of connection with the community around us. Our proximity to the town has helped the service users integrate within the local community and build relationships with the fantastic local businesses, community groups and people around us.”
Service user Paul McFadden from Gweedore said he is thrilled to be attending the Hub.
“I like the big open space, the staff, my friends and the routine. One of my biggest achievements so far is my work experience placement in SuperValu – this was a big goal for me. My keyworker helped me with it. My job in SuperValu is stacking the shelves, and I like helping the customers to nd what they are looking for and having the craic with them,” he said. HM
HEALTH MATTERS AUTUMN 2023 12 |
Minister Rabbitte with staff and service users at the of cial opening of Community Inclusion Dungloe Hub
Minister Rabbitte with service users at the of cial opening of Community Inclusion Dungloe Hub
SPOTLIGHT ON
HEALTH SERVICES HEALTHY IRELAND IMPLEMENTATION PLAN
2023–2027


HOT TOPIC
The Healthy Ireland Implementation Plan 2023-2027 was unveiled recently, highlighting four priority areas and identifying a suite of actions and measures of success for each strategic area. The roll-out and implementation of this plan will align with the transition to HSE Health Regions. HM
FOUR PRIORITY AREAS
1. Embedding health and wellbeing in health service delivery



2. Strengthening partnership and community working
3. Supporting healthy behaviours from childhood through to healthy ageing
4. Supporting staff personal health and wellbeing
OF HOSPITAL BEDS ARE FOR CHRONIC DISEASES AND 80% GP VISITS
“It represents another important milestone in our effort to remain focused on prevention as well as treatment. It gives direction to promote health and wellbeing and prevent chronic disease in health services and further strengthens partnerships as we work together to improve the health of our growing population.”
KEY PRINCIPLES
• To promote and support healthy behaviours across all age groups
• Promote the Healthy Ireland vision as part of our partnership work with voluntary, statutory, and other organisations.
• Support people to improve their health and wellbeing, and work to reduce health inequalities.
• Demonstrate our commitment to tackling climate change and promote sustainability by recognising that climate change is having a direct effect on our health and wellbeing, and on the environment



































• Maximise the benefits of digital technology to support people’s health and wellbeing.
• Provide a working environment that supports staff in their own health and wellbeing, demonstrating that we care about them by providing positive working environments where staff feel respected and valued.
Approximately 1.3 million people in Ireland are living with chronic conditions such as asthma, chronic obstructive pulmonary disease (COPD), diabetes, and cardiovascular disease
| 13 HEALTH MATTERS AUTUMN 2023 HOT TOPIC
– Bernard Gloster
80% of cases of coronary heart disease, 90% of type 2 diabetes cases, and ONE-THIRD of cancers can be avoided by adopting healthy lifestyle behaviours
WHAT IS...
Social prescribing
Social prescribing off ers a non-medical link to better health
Social prescribing is a way of linking people with non-medical, or complementary, sources of support within their communities. It recognises that health is heavily determined by social factors such as poverty, isolation and loneliness.
The emphasis is on the concept of community referral to avoid being limited by the medical model of prescription. The service provides GPs and other healthcare professionals with nonmedical referral options to improve health and wellbeing. Self-referral is also encouraged.
Social prescribing is available in over 30 locations nationwide to address health and wellbeing through engagement in social activities and community participation. These services are delivered in partnership with community and voluntary organisations .
According to the National FRC Mental Health Promotion Project Health and Wellbeing Community Referral Bi-annual Report 2022, social isolation (25%) was the most common reason for referral to the project, followed by loneliness at 11%. Other mental health issues were also commonly reported by service users, including depression (10%) and grief (5%). In total, 62% of those referred to the service were referred for support around their mental health.
Other concerns reported by service users include nancial stress, unemployment, retirement, mobility issues, insecure housing and poor health. A GP or other practitioner can refer their patient
to the Community Referral service, or an individual can make contact themselves. Initial contact is made - either through a meeting in person, on the phone, or online - to assess whether or not the service is appropriate.
Actions taken following acceptance of a referral depend on the needs of the service-user. It may be just one-off information or advice needed, a signpost to other services, or a referral to a communitybased activity or group. Care plans are coproduced between the link worker and service user, where social supports, groups, activities and community assets or resources are mapped out. Walking groups, social groups, support groups and exercise groups are the most popular referrals.
Some people nd it very dif cult to take that initial step alone. The link worker can even accompany them to the activity for the rst session/class or two.
The link worker can meet with the client for six to eight sessions. This time given to the client is important; the message conveyed is that the person is important and of value. This can improve self-worth and support self-advocacy.
Cork and Kerry Regional Social Prescribing Co-ordinator Rita Bevan said, “We all go through
HEALTH MATTERS AUTUMN 2023 14 | WHAT IS
of referrals are due to social isolation followed by loneliness at
periods in our lives where we can feel a little down, perhaps feeling somewhat alone, disconnected and disengaged. We can feel stuck in this state, wondering what is missing in our lives and what we can do about it. Sometimes, we might go into a downward spiral and it can seem very dif cult to navigate the way out.
“Together, you and the link worker can explore what might support and assist you to improved wellbeing; perhaps a greater sense of connection and purpose - navigating your way to less distress and have an enhanced experience of life.
“If we tend to our physical health can we do the same for our emotional or mental health? One way to do this is by speaking to a social prescribing link worker and navigating how to improve our emotional health and wellbeing.” HM
CLIENTS REPORT IMPROVED EMOTIONAL, MENTAL AND PHYSICAL HEALTH
Social participation:
“I wouldn’t have known what to do with myself when my husband died if I hadn’t met you, it was always me and him, I’m so thankful for you”
(service user, 78)
Mental wellbeing:
“This has benefitted my mental health. I feel like this has done me the world of good.” (Service user to Link worker)
Service users have reported a general increase in wellbeing, improvement in the ability to be around and interact with people, increase in security knowing they can re-engage if things are not going well, increase in self-belief, self-esteem, and self-respect.
Quality of life:
“My service users have informed me many times of the life-changing and hugely beneficial experience they have had since engaging with social prescribing. (link worker)
To make a referral or to self-refer to a service, contact your local social prescribing service directly. See allirelandsocialprescribing.ie for a list of social prescribing services and their contact details across the country.
PRINCIPLES OF SOCIAL PRESCRIBING:
• Focuses on the individuals’ needs in a holistic way
• Individuals are empowered to become coproducers of their health and wellbeing
• Takes into consideration the wider determinants of health, including environmental, social and economic factors
• Increased focus on early intervention and prevention
• Emphasis is placed on building social connections and forging social capital
• Utilises the support and services provided by the community, voluntary and private sectors
DID YOU KNOW?
Social prescribing can include physical activity initiatives like parkrun, walking groups, reading groups/books for health, library services, stress prevention/management programmes, self-help, adult education, men’s sheds, community gardening, arts and creativity and many more.
KEY PRIORITY GROUPS INCLUDE:
• those who are experiencing low mood, anxiety, depression, or mental health and wellbeing issues
• people who have health challenges
• family carers
• people who have experienced bereavement
• those who are in any way disadvantaged, or at risk
• those who are members of marginalised groups, such as ethnic minorities, members of the Travelling community, asylum seekers, refugees, migrants, and members of the LGBTQ+ community
• people who feel disempowered through life experiences, such as people who have/are experiencing homelessness, drug/alcohol misuse, contact with the criminal justice system and those who have experienced abuse
PROJECT TARGETS:
• Better quality of life
• Improved health behaviours
• Reduced healthcare resources
| 15 HEALTH MATTERS AUTUMN 2023 WHAT IS
Community Connector
A specialist social prescribing service for older people
Anew role has been created in Community Healthcare East to provide a specialist service to older people in the community.
Community Connector Tina Hannan took up her post in April. Her role is similar to social prescribing but with a focus on people aged over 65 who have more complex care needs. This HSE pilot programme, implemented across all CHOs, will be an integral part of the Integrated Care Programme for Older Persons (ICPOP) Service in Community Healthcare East.
The programme goes a further step forward to providing personalised health and wellbeing plans to our older population to reduce unnecessary visits to hospital. The ICPOP provides the only referral pathway for patients to be referred to the Community Connector. After they have engaged with the Community Connector Service, clients can be referred back into the community to the social prescribing services that are available across Community Healthcare East.
Tina’s role centres around supporting older individuals who may have dif culties accessing activities and interests that they may have previously enjoyed or have always wished to try but never have.
Tina said of her new role, “I feel privileged to hold this role and believe very strongly that all older members of our community have a right to be able to access limitless activities and supports that they hold as important to them and being supported to do so each step of the way by the Community Connector.”
ICPOP, now up and running as part of Sláintecare, is a
specialist multi-disciplinary service primarily targeting and managing the complex care needs of the older person. The service covers Dublin South East with Helen O’Riordan as the operational lead of the team.
Health and Wellbeing provide a grant aid agreement to Southside Partnership, which directly employs and hosts the Community Connector.
Lisa Sieger-Jamison, Social Prescribing and Wellbeing
Project Leader at Southside Partnership DLR, supports the implementation of the Community Connector programme, which will work alongside other Southside Partnership wellbeing supports. These include the DLR Social Prescribing Programme for Health and Wellbeing and the Living Well with Dementia Programme, also funded by the HSE.
“Having a specialised social prescribing service for older community members linked directly with the Integrated Care Hub is providing a non-medical intervention straight after discharge to support people to stay well in their own community,” said Lisa. HM

HEALTH MATTERS AUTUMN 2023 16 | FEATURE
Helen O’Riordan, ICPOP Operational Lead, and Tina Hannan, Community Connector from HSE Community Healthcare East, with Lisa Sieger–Jamison, Social Prescribing & Wellbeing Project Leader, Southside Partnership DLR.
6am – Wake-up time. I usually exercise, get ready, and grab a coffee before the children wake up. My son, Matthew, is aged three and my daughter, Anna Rose, is just eight months old.
7am - The children go to the childminder and I drive to work at the Mercy University Hospital, listening to a podcast or audiobook on the way.
7.45am - At the hospital, I check my daily schedule and prioritise the most important tasks. I also check and respond to emails.
8.15am - I attend Journal Club where the most up-to-date literature on in ammatory bowel disease (IBD) and gastroenterology is presented and discussed.
DayLıfe A in the of












9.30am- 1pm - In the outpatient department, I review patients at the IBD clinic in collaboration with gastroenterology medical colleagues. Patients attend my advanced nurse practitioner clinic for review and follow-up. I have also established and implemented a preconception education clinic, which IBD patients attend for preconception counselling.
1pm - Lunch and catch-up with colleagues.
1.30pm - I attend the weekly IBD multidisciplinary team meeting where colleagues and I present and discuss complex cases and action individualised care plans, in close collaboration with the patients.
3pm - Catch up with emails and patient calls.


4pm - In my role as education of cer for the IBD Nurses Association of Ireland, I spend time organising keynote speakers for upcoming seminars and study days. This role also involves ensuring continued professional development opportunities for IBD nurses.
I conduct research as part of my new role as IBD nurse lead for the national clinical programme in gastroenterology and hepatology. I am leading a research and development project for an IBD model of care in collaboration with colleagues. The aim is to improve access to care for IBD patients and standardise their care nationwide.



5pm - Home to spend quality time with my family.
 Sarah Gleeson advanced nurse practitioner in inflammatory bowel disease, Mercy University Hospital, Cork
Sarah Gleeson advanced nurse practitioner in inflammatory bowel disease, Mercy University Hospital, Cork
HEALTH MATTERS AUTUMN 2023 | 17
Asthma
Asevere asthma clinic in Donegal has brought dramatic improvements to the lives of many of its patients.
The clinic run by Letterkenny University Hospital (LUH) offers novel therapeutics and treatment for people in the region suffering from severe asthma. The treatment involves an injectable biological infusion which dramatically reduces the symptoms of the condition in some patients.
Dr Olga Mikulich, Respiratory Consultant at LUH, introduced new biological infusion therapies for patients in the north west in 2018.

“Not everybody will be suitable for this injection but if you find the right patient and start them on this treatment the effect is so transformational. They still need to take their preventative medication including their inhalers but they have their lives back,” she said.
“We can estimate that based on national average there are about 25,000 patients in Donegal living with asthma; 2,500 of them suffer from severe asthma, again based on national and international estimations. We followed about 800 patients in our severe asthma clinic and there are 34 patients on biologic agents for their asthma, out of them 20 are on new biologics.”
Traditional treatment for severe asthma includes
25,000
THERE ARE ABOUT PATIENTS IN DONEGAL LIVING WITH ASTHMA
2,500 ARE SEVERE
Severe asthma clinic continues to transform lives of patients
oral steroids. However, frequent courses of oral steroids that are needed to control symptoms can carry a high toxicity risk. This infusion treatment provides monoclonal antibodies (lab-made proteins) which target the specific cells responsible for asthmatic inflammation in the body. Suitable patients receive the infusion once a month or once every two months depending on need.
“This has revolutionised severe asthma treatment and in patients own words ‘gave them their lives back’,” said Dr Mikulich.
65-year-old Bernadette McCafferty developed severe life-threatening asthma in recent years. As a result of the condition, she was hospitalised on a number of occasions and faced long recovery periods.

“You would be sitting quite well one minute and then it would be like the flick of a switch. It was scary because you’re opening your mouth and there is absolutely nothing going in. Nothing,” she said.
“I had several spells in hospital with really long recovery periods so I just thought there is no way I can see old, old age with this.
Since she began taking the infusion, Bernadette’s life has changed dramatically. “I’ve just had an art exhibition and I’ve just taken up cold water swimming and dipping, which I couldn’t do before because of the asthma. I am now back to where I was,” she added. HM
FEATURE HEALTH MATTERS AUTUMN 2023 18 |
Dr Olga Mikulich, Respiratory Consultant at Letterkenny University Hospital, introduced the new biological infusion therapies for patients in the north west in 2018.
Patient Bernadette McCafferty from Castlefin, Co Donegal with Respiratory Advanced Nurse Practitioner Patricia McLaughlin at the asthma clinic, LUH.
HOT TOPIC 97
The presence of the HSE Safer Nightlife programme at the Body and Soul Festival, Life and Electric Picnic, have been a success, according to Prof Eamon Keenan, HSE National Clinical Lead for Addiction Services. Designed as a drug harm reduction programme for summer festivals, the Safer Nightlife project proved successful as a pilot scheme when rst introduced at the Electric Picnic Festival last year. HM
SAFER NIGHTLIFE SUCCESS AT SUMMER FESTIVALS







Plans for 2023 include distributing resources at the various festivals, recruiting and training volunteers and expanding testing. This is a health-led initiative – no judgement.

samples of drugs surrendered over three days of Life Festival including ketamine, MDMA and cocaine.
Volunteers engage with people, talking to them about drugs. There were two surrender bins, one in a HSE tent and the other in a medical tent. People were encouraged to surrender drugs into those bins.
The Safer Nightlife and Festivals - HSE Pilot Drug Monitoring and Information recently won a PRCA PR award for ‘Best Public Information Campaign’.
A drug called 3CMC, a cathinone or a stimulant drug, is a new psychoactive substances that had never been identified in Ireland. It carries risks associated with mental health problems, psychosis, and suicide ideation and as a result we were able to put information out about that.

Health risks associated with these substances were communicated in social media alerts via the website drugs.ie and by drugs.ie volunteers on the ground.
“Looking to the future, our Safer Nightlife programme has a central role in reducing drug-related harms at events and in the nighttime economy.”
Nicki Killeen, HSE Project Manager, Emerging Drug

Trends


Goto drugs.ie/festivals formoreharm reduction information

HOT TOPIC
HEALTH MATTERS AUTUMN 2023 | 19
New digital therapeutic set to transform Parkinson’s speech therapy
Speech and Language Therapists (SLTs) in Laois/Offaly have been piloting Teleatherapy’s innovative solution to aid providing speech therapy to people with Parkinson’s disease through the Health Innovation Hub Ireland.

In early 2023, HSE SLTs began trialling Teleatherapy with their clients with Parkinson’s disease. Teleatherapy is a platform which allows SLTs to prescribe therapy exercises to clients and monitor their progress. Clients use the Teleatherapy app to guide them through their therapy and measure their speech over time.
Aoife Carolan, SLT Lead on the pilot at CHO8, has been on board since 2022 to help trial Teleatherapy in her department. Aoife was excited at the opportunity to bring innovation to CHO8 when asked about using
Teleatherapy to date.
“I have noticed that clients are more motivated to practise consistently as they know their HSE clinician is monitoring the quantity, quality and frequency of their practice at home – with obvious results evident in terms of their speech function and less need for face to face routine reviews,” she said.
It also helps with therapists’ caseload management.
“There is good potential for waiting list reduction with an initiative of this nature. It also means there is more time during face-to-face sessions to focus on more complex or bespoke issues, outside of the daily therapy which we now know is being completed well and consistently with the aid of this app and the feedback it gives us,” said Aoife.
Health Innovation Hub Ireland (HIHI) works with a number of
companies each year to trial their innovations in the HSE. Dr Tanya Mulcahy, Director of HIHI, explained, “This pilot has not only demonstrated the value of the Teleatherapy voice therapy to patients but has also identified how the online platform provides added benefits to patients, their carers and healthcare staff. This is a great Irish product with the potential to impact Parkinson’s patients globally.”
Clare Meskill, CEO and cofounder of Teleatherapy, founded the company in 2020. When discussing the pilot with CHO8 to date, Clare said, “It’s great to be collaborating with SLTs in the HSE, to build and improve the platform as we learn together. Their enthusiasm and dedication has been fantastic. We at Teleatherapy are really grateful to both the SLTs and the HIHI.” HM
HEALTH MATTERS AUTUMN 2023 20 |
Eamonn Keenan Enhanced Community Care Network Manager; Jean Durkin, Emma Gonoud SLT Manager III; Clare Meskill and Dave Calnan Co-founders of Teleatherapy; Danny Owens; Frank Durkin; Martin Kelly; Michael Jones; Aoife Carolan and Aine Shaw, Speech and Language Therapists, HSE; Jane O’ Flynn and Michael Twomey, Health Innovation Hub Ireland
SPOTLIGHT ON
Cancer care
Developing Psycho-Oncology Services for children and young people with cancer in Ireland: A blueprint for the next decade
Every cancer experience is as unique as the person going through it. Cancer is challenging for every age group but for children, adolescents and young adults (CAYA), this can be a particularly daunting life event due to their developmental stage and the many changes they have to negotiate.
Receiving a potentially life-threatening diagnosis of cancer at a young age (0 to 24 years) is a major life stressor found to be universally distressing and potentially traumatising. It is associated with a range of physical, psychological, emotional and social dif culties and understandable levels of distress for patients and their families.
Psychosocial concerns include but are not limited to anxiety, depression, post- traumatic stress, family problems, social isolation, fertility considerations, transition to survivorship care, feelings of isolation, fear of recurrence, impact on education and other issues that sometimes only emerge once active treatment has nished.
Recognising that having cancer as a CAYA has several features that make the management of the disease more challenging than cancer at other ages, the HSE’s National Cancer Control Programme (NCCP) and Children's Health Ireland (CHI) at Crumlin launched the Model of Care for Psycho-Oncology services for patients aged 0 to 24 years and their families.
DID YOU KNOW?
Each year in Ireland, around 200 children up to the age of 16, a further 69 adolescents between the ages of 16 and 19, and 111 young adults between the ages of 20 and 24 are diagnosed with cancer.
The primary aim of the Model of Care is to provide a blueprint for the provision of psychosocial and psychological support services for CAYA with cancer. Based on national and international best practice, it will provide guidance for the delivery of an accessible, exible and appropriately skilled response via Psycho-Oncology hospital-based services. It will also provide a range of community and primary care supports, tailored to the needs of the individual.
The new Model of Care are will mean PsychoOncology services for all 0 to 15 year olds will be delivered within the National Paediatric PsychoOncology (NPPO) service in the CHI at Crumlin, while AYA (Adolescents and Young Adults) PsychoOncology services (for 16 to 24 year olds) will be delivered within the recently developed AYA cancer service network, which incorporates CHI at Crumlin, Cork University Hospital, University Hospital Galway, and St James’s Hospital, Dublin.
Dr Chiara Besani, who is co-chair of the CAYA Psycho-Oncology Model of Care working group, stressed that for those involved in delivering care, their role is to “ensure that we support each family in coping and adjusting to the incredibly unfair and dif cult journey they face. In clinical practice, we are delighted to see many developing posttraumatic growth and we aim for our patients to achieve their goals.” HM

| 21 HEALTH MATTERS AUTUMN 2023
Kathleen's mission
TO BUILD DEMENTIA INCLUSIVE COMMUNITIES
Kathleen Farrell is from Dublin. She is living with Lewy Body Dementia – with a big emphasis on living.
Kathleen is determined to empower others like herself to live the best life possible and has become a vocal advocate for people with dementia and their families. She is also the face of a new campaign to make our communities more dementia inclusive.
“Since diagnosis in 2021, it’s been a bit of a whirlwind but thank God, I have been blessed with support from my family and later, when I was stronger, I got involved with the Irish Dementia Working Group,” she explained.
The Irish Dementia Working Group (IDWG) are a group of people living with dementia who advocate for better services, supports and policies in Ireland. The Alzheimer Society of Ireland (ASI), who are also a partner of the Dementia: Understand Together campaign, supports IWDG members to build their capacity and con dence and to use technology to engage in advocacy and awareness work, both online and in person.
“I could say I never felt better but that would be a step too far. I certainly feel empowered to deal with my situation and help as many people with dementia to live a better life and feel better about themselves as possible,” she said.
Kathleen was involved in the Dementia: Understand Together campaign’s development of the dementia

inclusive community symbol, which is being rolled out nationally as a sign of solidarity and support for people with dementia and their families.
“Joining the Dementia: Understand Together working group has been so important to me as I’m passionate about staying active in my community,” she said.
“We have been involved every step of the way in developing the inclusive community symbol. I was impressed with the way the Dementia: Understand Together campaign team were so willing to support us and they understood that this was so meaningful for people living with dementia. The IDWG met with the campaign team on many occasions to discuss the symbol from start to nish, design, layout, colours etc.
“At the second meeting, everything we had recommended had been acted upon. ‘Nothing about
HEALTH MATTERS AUTUMN 2023 22 | INTERVIEW
INTERVIEW
Kathleen being interviewed on Virgin Media
us, without us’ is how we like to describe it. For me, I was so mindful that it wasn’t just talk, this was actually happening. It gave me hope and a clear understanding I wasn’t on my own. My life wasn’t over, it was just a new chapter but a different chapter that needed support."
Kathleen explained that it is why she wanted to put her face and words to the new poster and symbol.
“I knew it would help to make people living with dementia feel good about themselves,” she said.

“I got involved in making the poster for the campaign and it was the most incredible day. There were three models and we were treated like royalty. Everyone was so supportive and friendly at the photoshoot, it really was one of the best days of my life.”
She said spending the day with the crew was ‘amazing’ and the photographer made sure they were comfortable.
“Niamh from ASI was supporting me on the day and she was unbelievable. At all times I was being looked after, and at no stage was I scared or worried that I might get lost or wander off,” Kathleen joked.
“I had not laughed so much in such a long time. I forgot about the Lewy Body Dementia for the few hours. For me it was the best day since I was diagnosed. I couldn’t believe how my life had changed. I felt brilliant! I felt like a model, and I felt alive, the old me was back, she’s never been gone, just hiding!”
She explained that the symbol will enable people to engage in their own communities safely.
“I am only recently diagnosed with Lewy Body Dementia and I have occasionally given the cashier my wallet instead of my card. I now know that when I see this symbol, the cashier will be patient and understanding. I can feel safe and not embarrassed,” said Kathleen.
Kathleen is actively speaking to people about how they can also get involved in the campaign and display the symbol. A key part of the campaign is encouraging and working with community champions and organisations, such as Boots, Irish Rail, AIB, the Irish Museum of Modern Art, Actavo, the National Transport Authority and many more to take part in dementia awareness training. HM
For more information, training opportunities and to order your dementia inclusive community toolkit and symbol, visit www.understandtogether.ie/get-involved If you have any questions about the campaign, the IDWG or ASI, please email understandtogether@hse.ie
INTERVIEW
"Already the posters are opening up a new awareness in our communities,” she said. “I have spoken to my local chemist, hairdressers and beauticians which is very important to me. This means that I will be able to engage meaningfully in my local community. They are willing to walk the walk and not just talk the talk."
| 23 HEALTH MATTERS AUTUMN 2023
New Model of Care gives people living with dementia timely and equal access
The HSE Enhanced Community Care (ECC) Programme has launched a new Model of Care for Dementia to set out care pathways to ensure people living with dementia are at the centre of care practices and service design.

With over 64,000 people currently living with dementia in Ireland, it is a life-changing condition.
This model of care provides an integrated framework to bring together a wide range of services for people living with dementia and is underpinned by the following:
• People living with dementia are at the centre of considerations relating to service design and recommendations related to care practices
• They receive timely and equitable access to assessment, diagnosis and post-diagnostic support regardless of the location of a service, the type of dementia they have, their age, their ethnicity, any other disability or co-morbidity, or their gender.
• The Dementia Model of Care provides for a diagnostic model utilising three levels of assessment:
• Level 1 - Primary Care GP

delivered assessment: This may include support and information from any of the ECC programme services; Community Health Networks/Primary Care Teams, Community Specialist Teams for older people, Community Specialist Teams for chronic disease and Community Intervention Teams (CITs).
• Level 2 - Memory Assessment and Support Service (MASS): People 65 years or over with a typical and clear presentation of dementia will predominantly be assessed and supported in a Level 2 MASS (or/other specialist service). The person with dementia will be offered relevant supports in their geographical area. As of May 2023, nine MASSs have been funded in Donegal, Sligo, Cavan/Monaghan, Mullingar, Limerick, Kerry,
Mayo, Wexford and Waterford. Funding for additional MASS sites will be sought in future National Service Plan (NSP) estimates bids.
• Level 3 - Regional Specialist Memory Clinic (RSMC): People 65 years or under with a suspected dementia, or those with atypical or unclear presentations that require a more detailed assessment, will predominantly be assessed and supported in a Level 3: RSMC. However, they may utilise the post-diagnostic support services that are local to where the person with dementia lives. As of April 2023 four RSMCs have been funded, located in the Mercy University Hospital, Cork, Galway University Hospital, Tallaght University Hospital and St James’s Hospital, Dublin.
The Dementia Model of Care is
HEALTH MATTERS AUTUMN 2023 24 | INTERVIEW
Paul Maloney, Programme Manager; Dr Mairéad Bracken-Scally, Project Manager; Fiona Foley, Project Manager;Mary Butler TD; Sinéad O’Reilly, Project Of cer; Kate Brennan, Project Manager; Janette Dwyer, AND, Older People, Change and Innovation; Marie Scanlon, Project Manager; Dr Seán O’Dowd, Clinical Lead.
the culmination of signi cant engagement, investment and collaboration of a broad range of expert stakeholders across community and acute HSE services, voluntary services, Third Level education sector, clinical and executive leadership within the HSE and the Department of Health. The HSE will continue to work closely with new and existing partners to continuously enhance the lives of people with dementia, their families and other supporters.

Charlie Drake, a person living with dementia, explained, “The Model of Care is based on the principals of citizenship and personhood and it will put the person with dementia at the centre as they live and journey on their road with dementia.
"It will give us a voice and a say in how we would like our dementia to be managed.” HM
DID YOU KNOW?
It is estimated that for every one person with dementia, there are three others supporting those living with the condition and providing care.
Supportive Memory Guide empowers people early into their dementia diagnosis

The Supportive Memory Guide is an online eBook designed for people early in their dementia diagnosis, which aims to empower the reader with technology focused advice to implement rehab and protective strategies. This eBook was developed as part of the mPower programme, a Dementia Initiative in CHO1, which targets digital resources for People Living with Dementia and support community services.
This project was a collaborative venture between Kate Hanlon of eHealth Communications, and senior occupational therapists Kerri Malone, Orla McDonnell and Emma O’Brien. Orla and Kerri work in primary care in Co Louth. They both recognise that early intervention is essential with this client group, and promote the importance of services and resources without which can lead to a more rapid deterioration in the condition.
Emma works specifically with people living with dementia and their families at the Memory Technology Library in South Tipperary, and is national lead for the Memory Technology Resource Rooms. Emma’s service provides demonstration of a wide range of assistive technologies and provides practical advice and solutions to support continued engagement in activities.
Kate was responsible for the graphic design of the eBook, as well as the supporting technology resource videos. This meant arranging the content in a way that was practical and easy to use for people living with dementia, as well as making conscious design choices with the client in mind, for example bright, high-contrasting colours, easy navigation and larger font size.
The eBook covers a range of relevant areas; Routines and Habits, Scheduling and Planning, Supportive Home Environments, Managing Medication, Simple Home Technologies, Smart Home Technologies, Smart Phones, Keeping Active and Engaged. The mPower programme highlighted the important role technology can play to help maintain independent living following a diagnosis of dementia. This eBook focuses on the use of technology, is a practical resource with education resources, everyday advice and tutorials for helpful assistive technologies.
The book was drafted with the help of healthcare professionals and a focus group of people living with dementia organised by the Alzheimer’s Society of Ireland. Their valuable input provided positive feedback and helpful advice. HM
| 25 HEALTH MATTERS AUTUMN 2023 INTERVIEW
SUPPORTIVE MEMORY GUIDE Empowering you with practical tips and useful technologies eHealth and Disruptive Technologies Occupational Therapy
"It will give us a voice and a say in how we would like our dementia to be managed.”
Health regions
Moving to a new structure with six health regions
HSE West and North West: Donegal, Sligo, Leitrim, Roscommon, Mayo, and Galway
HSE Dublin and North East: North Dublin, Meath, Louth, Cavan, and Monaghan
HSE Dublin and Midlands: Longford, Westmeath, Offaly, Laois, Kildare, and parts of Dublin South and Wicklow*
HSE Midwest: Limerick, Tipperary and Clare
HSE Dublin and South East: Tipperary South, Waterford, Kilkenny, Carlow, Wexford, Wicklow, part of South Dublin
HSE South West: Kerry and Cork
HEALTH MATTERS AUTUMN 2023 26 | Making progress on Sláintecare and
integrated care
WHAT WILL THIS DO?
Our health service is being reorganised into six HSE Health Regions, which will allow us to:
• deliver more integrated care closer to patients’ homes by bringing hospital and community services together
• plan and deliver services around the needs of local populations
• improve governance and accountability at all levels
• strengthen local decision-making
• provide consistent quality of care across the country
Restructuring the HSE into 6 Health Regions will take some time and to support this, an implementation plan has been published.
The plan sets out a high-level programme of work to establish Health Regions from February 2024. It includes key actions and timelines throughout 2023 and into 2024.
WHAT HAPPENS NEXT?
THE KEY ACTIONS FOR 2023 ARE GROUPED INTO THE FOLLOWING FOUR THEMES
Leadership, Vision and People Health Regions will have the power to develop their own workforce. the structures, roles and responsibilities of Health Region teams will be finalised throughout 2023 and into 2024.
Model of Integrated Care and Healthcare Governance
Health Regions will be accountable and responsible for understanding the needs of their local populations and can plan services in response to these needs, and they will be held accountable for the health outcomes.
Planning and Finance Health Regions will have authority and flexibility to manage finances at a regional level. Over time, the population needs in each region will inform their budget.
Infrastructure including Capital, ICT and Supports
Investing in modern technologies and maintaining facilities and equipment, will mean better quality care and improved patient outcomes.
A number of core infrastructure activities will happen throughout 2023 and into 2024. The capital arrangements, digital requirements and physical infrastructure needs of each Health Region will be finalised.
• A detailed plan for 2024 and beyond will be completed during 2023.
• Throughout the remainder of 2023, the responsibilities and boundaries of HGs and CHOs will be brought in line with the new Health Region structures.
• Health Regions will be set up from February 2024. They will be led by six newly approved Regional Executive Of cer posts. By the end of 2024, the existing HG and CHO structures will be stood down as the new Health Regions structures are established.
• Integrated care allows patients and service users to access health services more easily, no matter where they live. It also makes it easier for our staff to respond to patients’ needs and make improvements to care. It is a system of care where patients’ needs come rst.
• Health regions are a crucial step in reducing barriers to integrated care and improving health outcomes for everyone.
| 27 HEALTH MATTERS AUTUMN 2023
Making progress on Sláintecare and integrated care
A new specialist clinic in Summerhill Primary Care Centre in Co Meath is providing high-quality, comprehensive services for all lymphoedema and lipoedema patients.
Mum-of-three Sarah Lane was diagnosed with melanoma skin cancer six years ago.
“I had a spot on my upper back that was removed and the results came back as malignant melanoma. It spread to some lymph nodes and more surgery was carried out. In the space of eight months the cancer had returned, requiring more surgery and 35 rounds of radiation – all contained in that area under my armpit.”
A hairdresser, Sarah said she was told of the risk of lymphoedema developing as a result. Three years ago, she noticed swelling in my arm. It felt heavy and the skin felt tight – it was the start of lymphoedema.
“I had a couple of appointments to try and address it, but it got worse. Even little things like drying my hair were tough and I had to get my wedding bands sized up because of it. I’m a hairdresser and having lymphoedema in my arm forced me to retire. At 39 I’m too young to retire and hairdressing is all I know,” she said.
However, earlier this year when she was attending an appointment for blood tests, Sarah, who is continuing to receive treatment for melanoma, explained how a nurse told her about the new Specialist Lymphoedema Clinic.

New lymphoedema patient information leaflets on reducing your risk of lymphoedema after cancer treatment are now available on hse.ie/lymphoedema
The new leaflets explain what lymphoedema is and what to do to reduce your risk of developing lymphoedema if you have had treatment for
“She explained that I just needed to be referred by my GP. She gave me a lea et and then helped me ll in the forms. I got a call the next day and made an appointment,” said Sarah.
“I met Thelma Dunne, a lymphoedema therapist, at the clinic and we had a very long chat about the condition and how serious it is. The reality of it, particularly that it will never go away, can be quite upsetting. But I felt Thelma listened to me and understood how it made me feel. She advised that the treatment plan I was given would help keep it manageable.”
Kay Morris, Project Manager for Lymphoedema Services, explained there are three specialist clinics providing high quality, comprehensive services for lymphoedema and lipoedema patients in Clare, Meath and Donegal. There is hope to expand on the number of specialist clinics upon receipt of funding. HM
"I’m a hairdresser and having lymphoedema in my arm forced me to retire. At 39 I’m too young to retire and hairdressing is all I know,” she said."
cancer to your lower body, head and neck or your upper body.
To order leaflets search lymphoedema on www.healthpromotion.ie
For more information contact: Kay Morris at Kay.Morris@hse.ie
HEALTH MATTERS AUTUMN 2023 28 |
‘Lymphoedema is an awful side effect from cancer treatment but this service really helps’
Donegal HSE pilot scheme awarded European prize
DID YOU KNOW?
Chronic Obstructive Pulmonary Disease (COPD) is a disease that makes it hard to empty air out of your lungs. This is because the airways get smaller leading to airfl ow obstruction. This can result in shortness of breath or tiredness because you are working harder to breathe.
Apilot initiative has been giving support to people living with Chronic Obstructive Pulmonary Disease (COPD) in their own homes and keeping them out of hospital.
The Community Virtual Ward provides an alternate pathway to hospital-based COPD care through the bespoke platform. The platform was developed during the COVID-19 pandemic to look at respiratory rate trends and to look at the use of technology to monitor and explore the feasibility of further use in the clinical setting.
The service was offered to 10 people between May and August last year to evaluate the rate of admission from COPD and the bene ts of inclusive selfmanagement of this chronic disease.
The 10 patients, known to specialist respiratory services with COPD, were selected and admitted to the Community Virtual Ward for remote monitoring and optimisation of the existing care plan. The results showed early identi cation of exacerbation of the

medical condition through respiratory rate monitoring. The patient started treatment sooner, as they had improved access to prescriptions for antibiotics and steroids which was organised with relevant GPs, resulting in a signi cant reduction in hospital attendance and admission
A signi cant increase in patients' ability to manage their health was displayed and the feedback indicated that patients loved this new care pathway and they displayed increased knowledge and understanding of their condition and con dence to manage it.
Such was its success that it has been awarded the European Federation of Allergy and Airways Diseases Patients’ Associations (EFA) Patient's Prize for Digital COPD. This pathway will be further explored having secured funding to extend the programme in the wider Donegal area, and if successful will be an exemplar model of pathway management of those living with COPD within the ECC Chronic Disease Programme. HM
| 29 HEALTH MATTERS AUTUMN 2023
Maura Gillen, General Manager, HSE Primary Care Services Donegal; Antoinette Doherty, Advanced Nurse Practitioner in Respiratory Integrated Care; Claire McRory, Operational Team Lead for CDM Donegal; and Des O’Toole, HSE Digital Clinical Innovation Lead.
Making progress on Sláintecare and integrated care
Thousands of cancer patients avoiding ED admission thanks to nurse-led oncology service
Cancer patients’ attendance at the Emergency Rooms across the country have been massively reduced due to new National Acute Oncology Nursing Service.
The Limerick team leading the Acute Oncology Nursing Service at UHL has managed approximately 2,000 calls from unwell patients attending haematology and oncology services, and helped them to avoid the ED pathway at the hospital.
UHL-based clinical nurse specialists Anne Ryan and Susan Nagle are among 26 Acute Oncology Nurses in hospitals nationwide funded by the HSE National Cancer Control Programme (NCCP). The service, established in response to the COVID-19 pandemic, enables patients undergoing active cancer treatment who become ill at home to contact the Acute Oncology Nurses via a dedicated phone service instead of ending up in the Emergency Department.

The specialist nurses assess the patient’s symptoms
Making services safer: introducing the new National Clinical Surveillance Infection Control System
HSE Acute and Community services, eHealth and AMRIC are working together to introduce a National Clinical Surveillance IT System for Infection and Prevention Control.
The introduction of this software will help support surveillance of HCAI will play a key part in control of healthcare associated infections (HCAIs). It is estimated that about half of HCAIs can be prevented.
The system ICNET will be available across all acute and community services. It will deliver signi cant bene ts to the patients, service users and staff.
IPC teams will now have access to a one-stop-shop for all their IPC information in relation to their patients or service users. Having everything in the one system means that the IPC teams have fast access to all the
using an evidence-based tool and advise on the most appropriate care and management required.
Joan Lube, a patient from Newbridge, Co Kildare, who attended the service at Tallaght University Hospital, said, “I needed to contact the triage service on two or three occasions since commencing my cancer treatment, and I have always been amazed by the direct access to the team rst and foremost, and the prompt response to any issues or concerns that I had. I knew I was not alone during treatment and I could always ask for help and advice. Receiving a phone call has been so reassuring and has made my cancer journey much easier.”
A national audit of the December 2022 calls (1,383) received by Acute Oncology Nurses during the 8am to 4pm service showed that 84% of patients with cancer who contacted the service did not require Emergency Department attendance or admission. HM
information they need to deliver care that is appropriate and timely which reduces the number of HCAIs. The system assists staff in the timely management of outbreaks. It signi cantly reduces the administrative burden on these teams and has additional features such as clinical audit.
Deirdre Mullins, Project Manager with AMRIC, said the system also has comprehensive reporting capabilities which can be con gured to support local needs. It delivers enhanced workforce productivity due to greater ef ciencies in obtaining patient information, record keeping, and administration. There are a number of hospitals which already have clinical surveillance systems in place for Infection Control.
A national eHealth project team is now in place and Informatics Nurse posts (CNM2) are being appointed in each Hospital Group to support implementation of this system. It is planned to implement this system progressively commencing in Q4 2023. HM
HEALTH MATTERS AUTUMN 2023 30 |
Clinical Nurse Specialists Susan Ryan (left) and Anne Ryan, who lead the Acute Oncology Nursing Service at University Hospital Limerick.
Driving forward for change with the Health Services Change Guide in Action



In order to handle change in their services, busy healthcare professionals frequently seek assistance but they just don’t know where to turn outside formal third-level education or a senior mentor in their eld.

The good news is that our national HSE Organisation Development and Design team offers all staff members the chance to take part in a virtual session designed to acquaint you with and inform you of the theory of change we employ in the health services.

The Change Guide in Action virtual workshop was designed and introduced in 2022 to support teams who are working to implement change in their service.












With the aim of supporting the implementation of Sláintecare, this workshop can help to strengthen the ability of services to meet the dif culties of ongoing development. Services can then embrace the change challenges for service improvement and excellence.
Ultimately, it enables services to improve their readiness for change in preparation for the development of the new health regions.
The two-hour virtual session is interactive and allows you to ask questions and also have some time to review aspects of the Change Guide with other health service colleagues. Staff that have used the Health Services Change Guide have been interviewed and their learning is shared at the workshop.
Marie Boyle, Community Healthcare Network Manager in Limerick CHN6, shared her experience of using the Change Guide to steer her practice as she led her team through the early implementation phase of Community Healthcare Network / Enhanced Community Care. “It was a very engaging process because it allowed staff time to engage with each other and it allowed all of the ideas to come from the room,” she said.
Since its inception, feedback from those that have completed the virtual workshop indicates how much they have appreciated the shared experience and opportunity to discuss their own change challenges with their peers. HM























































If you wish to attend a workshop please email changeguide@hse.ie | Change Guide in Action Workshops take place online monthly. You can view the dates by visiting www.hse.ie/changeguide
| 31 HEALTH MATTERS AUTUMN 2023
HOT TOPIC
An innovative new early intervention programme which bene ts families affected by Attention De cit Hyperactivity Disorder (ADHD) was rolled out recently to parents in Louth and Meath. Changing Lives, delivered by community organisation Archways and funded by HSE Mental Health Services, is closely linked to a number of recommendations relating to ADHD support under Sharing the Vision, Ireland’s national mental health policy.
The programme is targeted at families with children aged three to seven years who are demonstrating behaviours consistent with ADHD but are often too young to receive a formal diagnosis. Potential families are identi ed through health, educational and community services, or can selfrefer to the programme. HM
CHANGING LIVES PROGRAMME FOR FAMILIES AFFECTED BY ADHD
“The strategies that we as parents were given within the programme had such a massive and positive impact on our lives at home that it gave me hope again as a mum.”
Mum Siobhán Haughey, Duleek, Co Meath
The Changing Lives Initiative Programme was initially delivered and evaluated as part of a 3.5 year EU-funded project which ended in 2021. The evaluations demonstrated the programme’s ability to significantly reduce ADHD-related behaviour in young children as well as other emotional and conduct problems.
As well as working with families the Changing Lives initiative provides training on ADHD for those working with young children, in particular teachers and early years professionals.
“This is a great example of the HSE working with service providers to bring about real change in people’s lives.” Emer Clarke, Senior Project Manager, HSE Mental Health Operations.
Early intervention is essential for children experiencing behaviours consistent with ADHD. The programme provides an invaluable support at a crucial time.
Further information on how families can avail of the programme is available at www.changinglivesinitiative.com
HOT TOPIC
HEALTH MATTERS AUTUMN 2023 32 |
SPOTLIGHT ON
The Health Passport
Passport gives people with a disability control over their healthcare
The HSE Health Passport is a tool that allows people with an intellectual disability to be the custodian of their own health information as well as providing health care providers with accurate and essential information about their individual health and needs. It is available as an App or as a paper version.
The Health Passport has been piloted in St Michael’s House (SMH) respite services since September 2022 with the direct support of two designated project co-ordinators. The overall CREATE team in SMH was devised with funding received from the national HSE CREATE initiative, with a speci c focus on Digital Assitive Technology.
The core CREATE team comprises Anne Spencer, CNM2 Co-Project Lead; Ann Hunt, CNM1- Respite Liaison Nurse; and project coordinators Emma Irvine Maguire, CNM1, and Christine Kiernan, Social Care Worker. An internal advisory group and working group were devised with key stakeholders from within SMH represented. Both groups afford the core CREATE team invaluable support and guidance.
The needs of people with an intellectual disability are often not wholly understood when attending a healthcare setting. This is primarily due to a lack of awareness and information about that individual and what supports they may require.

The Respite Liaison Nurse within SMH identi ed a gap in service user information when they attended respite services and believed the HSE Health Passport could assist
in bridging that gap. With the funding from the national HSE CREATE project scheme, the team focused on introducing the passport to service users who avail of respite – the two project coordinators have been providing direct supports to service users, staff in day services and families of service users who attend respite to introduce the passport to them.
Enda Finneran is one of the service users who has enjoyed the process of completing his Health Passport App on his tablet.
Enda can now share his passport digitally with healthcare providers so that they are aware of what is important to him and what support he may need during his care. Having the Health Passport in his possession at all times will ensure the information is readily available whether his family or a carer is supporting him with appointments.
The project co-ordinators have been working with 140 respite service users, their families and SMH staff for the duration of the project to date. Overall they have received positive feedback.
An elderly parent caring for their son/daughter have reported the passport to be a great tool for them. It allows them to have all of the necessary information about their son/daughter at hand should they be admitted to hospital without an advocate or attend an unfamiliar locum GP appointment. HM
| 33 HEALTH MATTERS AUTUMN 2023
Renewed confidence
Reablement offers a roadmap for independent living
Grace McAuliffe recently celebrated her 92nd birthday while living independently and safely at home. However, she suffered a fall in midApril and was admitted to Cork University Hospital. She was then faced with a fractured hip, a fear of falling and a loss of her independence.

Following her surgery and brief rehabilitation in South Infirmary Victoria University Hospital, she was referred to the Reablement team by her occupational therapist.
“Only for the care I received, I wouldn’t be where I am today. The team explained everything and listened to my worries. They were excellent. They gave me confidence to try more things. I am so grateful, they really encouraged me every step of the way,” said Grace.
This new Cork Kerry Community Healthcare Reablement pilot initiative is a therapy-led
HEALTH MATTERS AUTUMN 2023 34 | MY STORY
Grace (92) has renewed confidence
programme, designed to facilitate independence and rehabilitation. It aims to empower participants and promote their self-sufficiency in daily activities after a period of deconditioning, illness or hospitalisation.
The programme focuses on helping individuals regain essential skills for everyday living, such as personal care, mobility, meal preparation, household tasks and social engagement. By building strength, confidence and problemsolving abilities, participants can gradually reduce their reliance on assistance and regain control over their lives.
Grace’s Reablement goals included increasing independence with washing and dressing, improving confidence and independence with outdoor mobility, improving bed mobility and regaining independence with kitchen tasks.

The Reablement team provided regular encouragement, support and some aids and appliances to help Grace regain her independence with everyday activities. Grace is making significant progress with the support of her Reablement team. She can dress independently using the sock aid and she is gaining confidence with showering. Many sessions have focused on improving outdoor mobility by going for walks in Grace’s locality. It is expected that she will regain her full independence and not require home supports.
Skilled therapists work closely with each individual to develop a personalised care plan that is tailored to their unique needs and goals. Máire Caulfield, Senior Occupational Therapist, who works on the Reablement Team in Cork, said she is delighted to be part of the team.
“Reablement is a fantastic service because we can provide prompt support when clients can really benefit and make gains that are sustainable into the future. The feedback from clients and their families is very rewarding,” she said.
“It’s fantastic to see clients do so well, get back to doing things they love and know that we played a part in supporting that,” said Audrey Kavanagh, Reablement Assistant in the North Kerry area, describing the benefits of working with the Reablement Service and more recently with Mary Daly from Scartaglen, Co Kerry.
Mary recently celebrated her 91st birthday and was referred to Reablement by her public health nurse following a fall at home, which required admission to University Hospital Kerry and convalescence in Killarney Community Hospital.

“After my fall, I was so nervous and I had lost confidence in myself. Reablement gave me the encouragement I needed to gradually get back to doing things for myself,” said Mary.
Fiona Geary, Clinical Project Lead, explained the community benefits also. “Reablement is resulting in a 66% reduction of dependency levels, a significant improvement in the client’s well-being and an increase in their quality of life. The service has the potential to sustain service users’ independence for longer, while also having an immediate impact on waiting lists in home support and community services.” HM
DID YOU KNOW?
Skilled therapists work closely with each individual to develop a personalised care plan that is tailored to their unique needs and goals.
| 35 HEALTH MATTERS AUTUMN 2023
The programme focuses on helping individuals regain essential skills for everyday living.
Mary Daly Scartaglen
Grace McAuliffe
SPOTLIGHT ON
Telehealth
Telehealth can shape the future of healthcare
It is envisaged that telehealth will become the norm in the next 10 years with all healthcare staff capable of caring digitally and providing blended care models of in person and telehealth interactions. The eHealth National Telehealth Programme and the National Digital Health Clinical Of ce organised a Consultation Day to explore the present and future of HSE Telehealth - using ICT to deliver healthcare services remotely when patients and providers are separated by distance.
The past three years have seen signi cant adoption of telehealth solutions in healthcare, accelerated by the pandemic's distancing requirements. These solutions include telephone and video consultations, remote monitoring of health conditions, and online access to validated health-related information, self-help tools, and peer/ person-to-person supports.
Support for telehealth development is evident within government and organisational strategy which emphasise its role in enabling care delivery closer to home, reducing hospital visits, improving access to services, and lowering healthcare associated carbon emissions.
The insights gained from the Consultation Day will contribute to the development of a comprehensive HSE Telehealth Roadmap by the National Telehealth Steering Committee. Sheilagh Foley, a patient managing multiple chronic conditions, emphasised the patient
For more information visit:
experience perspective and her hopes for telehealth in the future, while HSE Chief Operations Of cer Damien McCallion and Prof Richard Greene, Chief Clinical Information Of cer and Chair of the National Telehealth Steering Committee, highlighted the signi cance of telehealth within the organisational context.
Four key categories emerged from round table discussions among attendees:
• The importance of education and training to empower patients and healthcare staff and promote valuable telehealth use.
• Recognising the need for investment in equipment and infrastructure including consideration of ongoing developments and advances in technology.
• Identifying the need for improved governance, regulation, and data collection to ensure safe scaling of telehealth services.
• The expectation that telehealth will become the norm and improve links between community and acute healthcare sectors.
The Telehealth Consultation Day successfully fostered collaboration, inspired innovation, and provided valuable insights into the potential of telehealth to revolutionise patient care. By continuing the dialogue and sharing knowledge, we can collectively shape the future of healthcare and improve the lives of patients and service users. HM
https://www.ehealthireland.ie/news-media/news/2023/telehealth-consultation-day.html
HEALTH MATTERS AUTUMN 2023 36 |
Tobacco free
Tobacco Free Campus: CHO DNCC lead the way globally
The work of teams across CHO Dublin North City and County (CHO DNCC) on implementing Tobacco Free Campuses (TFC) was highlighted recently.

The Chair and Vice-Chair of the Global Network of Tobacco Free Health Services (GNTH) Susann Koalick and Laura Antón, alongside Martina Blake, Pauline Kent and Edward Murphy of Tobacco Free Ireland (TFI), visited Grangegorman Primary Care Centre to witness a TFC in practice.
They were met by Ellen O’Dea, Head of Service for Health and Wellbeing, staff from CHO DNCC and members of the Grangegorman Tobacco Free Campus working group, Roisin O’Neill and Jackie Brady who led the site visit.

TFC policies are evaluated on eight standards based on international best practice, which align with the GNTH model. Grangegorman PCC was one of 40 sites from CHO DNCC to have been awarded a TFC bursary recently from TFI in 2023. The site visit incorporated a walk around the campus to observe some changes the
campus have made over the last year as part of their Quality Improvement Plan.
Changes made by the TFC working group in Grangegorman demonstrates their commitment to the health of their service users and staff in promoting a tobacco free environment and healthy image in the community. The successful implementation of their policy this year also demonstrates the proactive support of service managers and all staff in Grangegorman.
During the visit, Stop Smoking Advisor for the Grangegorman 1:1 Stop Smoking Clinic, Susan MacNicholas, conducted a round table discussion with two of her clients who have successfully quit with her guidance and support. The discussion was a great opportunity to celebrate the success of their quit journey and to get feedback of their experience engaging with the Stop Smoking Service. A bene t of the 1:1 clinic on site is that it has allowed successful links and referral pathways with other services to have been established.
The Stop Smoking Clinic has helped Grangegorman improve on its identi cation, diagnosis and treatment of any tobacco users on site, a key component of its TFC policy. HM
MY STORY
| 37 HEALTH MATTERS AUTUMN 2023
FEATURE
Grangegorman Primary Care Centre Tobacco Free Campus site visit.
Staff from Tobacco Free Campus sites in CHODNCC collecting their awards.
ASSISTED DECISIONMAKING

HOT TOPIC
The Assisted Decision-Making Act 2015, recently introduced, gives a person the right to be assisted to make decisions with legally recognised supports. This is regardless of disability or any condition which may affect their decision-making capacity. The Act recognises each person’s right to make autonomous and independent decisions for as long as possible. HM
What does it mean?
A core principle of the Act is that each person is presumed to have capacity to make their own decisions, being supported to make their own decisions as far as is possible. The Act emphasises minimal restriction of a person’s rights and freedoms and the importance of respect for the person’s will and preferences.
The three levels of supports available for people requiring support with making decisions are decision-making assistants, co-decision-makers and decision-making representatives. Decision supporters will likely be someone that the person knows and trusts, such as a family member or a close friend.
A plain English guide to the codes is available together with informational videos on each code. Accessible guidance documents for people who want to enter a decision support arrangement and/or use other DSS services; an easy-read guide to the 2015 Act and the DSS; and materials setting out approximately 60 different scenarios to help to explain how each code could apply in real-life are also available. These supports can be accessed on www.decisionsupportservice.ie.
Three eLearning programmes
1. Guidance for Healthcare Workers
2. National Consent Policy 2022
3. Supporting Decision Making in Health and Social Care Available on www.assisteddecisionmaking.ie
13 CODES OF PRACTICE
The DSS has published 13 Codes of Practice for decision supporters, interveners and relevant professionals, providing guidance for their functions and responsibilities.
Decision Support Service (DSS) is responsible for a range of functions including promoting awareness of the Act, registering and regulating certain decision support arrangements, supervising the actions and activities of decision supporters; and investigating complaints made under the Act
HEALTH MATTERS AUTUMN 2023 38 |
Living support
Supporting self-management is key to keeping people well
Every day, people living with chronic or long-term health conditions perform tasks and make decisions related to their health. This is known as self-management. Such tasks may include:
• recognising and dealing with symptoms
• monitoring one’s condition such as checking blood glucose levels or measuring peak ow
• taking medication(s)
• managing other treatments
• attending various appointments and communicating with healthcare professionals
• making and maintaining lifestyle changes
• coping with the emotional effects of the condition
How effective this is depends on the support they receive and their level of con dence and skill to manage tasks that are sometimes quite challenging, especially for those with multiple conditions, explained Maeve Carmody, SelfManagement Support Co-ordinator, Cork Kerry Community Healthcare.
“Self-management support is the help given to people living with chronic conditions to enable them to manage their health on a dayto-day basis. It expands the role of healthcare professionals beyond delivering information to include helping patients build con dence, develop skills and make choices that lead to improved self-management and better outcomes,” said Maeve.
“Effectively supporting self-management requires a collaborative, partnership approach.”
How can self-management support be put into action?
• Condition specific education programmes such as cardiac rehabilitation, pulmonary rehabilitation and diabetes education programmes, which provide people with invaluable information about the management of their condition.

• Living Well - A Programe for Adults with Long-term Health Conditions: This free group HSE self-management programme supports people to develop the skills and confidence to manage their health. For more information go to www.hse.ie/LivingWell





• Action and self-management plans: Resources such as the COPD communication card, asthma action plan and heart failure self-management plans. These plans help patients to manage their condition when they are well, and to be aware of the warning signs of an exacerbation or flare-up.
• Skills training: Learn new skills such as motivational interviewing and reflective listening. https://www.hse.ie/ eng/about/our-health-service/healthcare-communication/
• Literacy and communication guidelines: The information we provide needs to be in a format that the person can understand and is appropriate for different cultural and health literacy levels. Support is available from HSE Communications and www.nala.ie. HM
For more information go to
www.hse.ie/selfmanagementsupport
“Self-management support goes beyond the healthcare setting. Community and voluntary organisations provide invaluable support to people with chronic conditions. By being aware of and referring to these community resources, we can help our patients to engage with them. These include healthy cooking and exercise group programmes."

MY STORY
| 39 HEALTH MATTERS AUTUMN 2023
The self-management support room in Cork Kerry Community Healthcare
Community intervention
Providing your healthcare in your community
In a leafy green suburb, close to the north of Dublin city, the Community Intervention Team in Ballygall, Glasnevin provide a range of enhanced services, or as their name suggests, ‘interventions’ in the ‘community’ to make life easier for patients and help avoid unnecessary attendance in acute care. They support oncology patients as well as providing home care to those who need it.
The range of services provided by this nimble, experienced team is extensive and growing. Working with colleagues in the Mater Hospital, Beaumont Hospital, and Connolly Hospital, they facilitate early discharge from hospitals and help others avoid hospital, in addition to supporting people to live well with a chronic illness at home.


With ample parking, and easily accessed from across the region, Noeleen Sheridan, Clinical Nurse Manager 3, heads up the Community Intervention Team with an agile team of specialist nurses who provide a range of services to make life better for a wide range of people living in Dublin North City and County, letting them access specialist health interventions quickly at a time that suits them.
This example of Sláintecare integrated healthcare in action in Dublin North City and County, shows the value of providing specialist care for people who need a defined short period
of enhanced services or acute intervention.
Bernadette, who has just had her last infusion last week, said, “I just would walk straight in and it’s done in 10 or 15 minutes, the women are lovely and it saved me queuing in the hospital. It was so convenient because I could just leave work, go and get it done and be back to work in 45 minutes.”
Noeleen gets great satisfaction from her work. “I see how patients respond to the treatment in the community, having trained experienced team minding them in the community. We discuss their concerns and they feel listened to. In many cases they can go about their jobs,
HEALTH MATTERS AUTUMN 2023 40 |
Top left: L-R Laura Flanagan and Angela Henry, Home Service RGN
M EETTHE TE AM
Above: L-R Dara McDonald, Clinic Administration; Caroline Grehan,Clinic CNM2; Noeleen Sheridan, CNM3; Maria Smith, Clinic RGN.
mind their young families and enjoy life more when their treatment is provided locally at a time that suits them.
“The team I work with are fantastic, they’re always looking to make life easier for people. As well as in the clinic we provide services to appropriate patients in their home. It’s a wide range of interventions, from administering IV antibiotics to monitoring others on coagulation treatment in their home.
“If someone needs fluids we might provide this at home, or an elderly person might have their blood test taken at home where they might not be able to attend a hospital. If a person has a urinary catheter which is blocked, we can do this at their home, out of hours.”
There’s a real focus on provision of oncology services.
“If someone lives in our area and attends any hospital and have a chemotherapy infuser, a chemo pump or a portacath, they can come to us to have the pump disconnected or their portacath flushed,” she said.
This can have a hugely positive impact on a person’s quality of life and timing, as Noeleen, who has extensive experience managing a Day Oncology Ward, explained.
“In hospital people might have to wait a few hours, but in our service we can flush their portacath in minutes, and they are free to go about their business. We have a specialised oncology satellite clinic from the Mater Hospital, the only one of this nature in Ireland. It’s great to see other Community Intervention Units starting to do some of this work. Everyone here has worked in oncology and has experience and training in this specialised area.”
Having specialist nursing in the community has facilitated a more holistic approach to patient care.
“We talk with our patients, we can take the time to see what’s going on in their lives and have the links in the community. That means we might be able to enable and empower them to take a move to support their overall health,” she said.
"One patient wanted to go holidays when on chemotherapy tablets and was not due in outpatient clinic for four months. When it was discussed by her multi-disciplinary team, her consultant agreed that she could go and we could check her bloods before and on return from her holiday, patient felt heard, we were able to reassure her it was fine to go on a much needed holiday with her family."

Aoife, a former patient of the CIT, said, “I got to know the team and they were so supportive and friendly. Caroline would ring to update me and answer any questions I had. The appointments were always on time.
"From a professional perspective, their medication management and enhanced nurse monitoring made my life easier at a time when I really needed this.”
The Community Intervention Team in Ballygall is one of a number of specialist, health professional teams across Ireland who provide rapid and integrated responses for patients with an acute episode of illness who require enhanced services/acute intervention for a defined short period of time. This may be provided at home, in a residential setting or in the community as deemed appropriate, thereby avoiding acute hospital attendance or admission, or facilitating early discharge. HM

MEET THE TEAM | 41 HEALTH MATTERS AUTUMN 2023
We talk with our patients, we can take the time to see what’s going on in their lives and have the links in the community.
Outside Community Intervention Team clinic
Geraldine Workman, Home Service RGN.
Prof Risteárd Ó Laoide, National Director, HSE National Cancer Control Programme; Frances Crowley, member of the Pat Smullen Pancreatic Cancer Fund Committee, and widow of champion jockey, Pat Smullen; Prof Ray McDermott, UCD/St Vincent’s University Hospital and Clinical Lead, Cancer Trials Ireland; and Eibhlín Mulroe, CEO, Cancer Trials Ireland.
Cancer Trials Ireland announces creation of Pat Smullen Chair in Pancreatic Cancer
Cancer Trials Ireland has announced the creation of the Pat Smullen Chair in Pancreatic Cancer at University College Dublin (UCD). The new position will anchor expertise in pancreatic research in Ireland with the ambition of creating a global centre of excellence for treatment and research of this form of cancer, which has one of the poorest outcomes.
“The position will receive €900,000 in funding over ve years from Cancer Trials Ireland’s Pat Smullen Pancreatic Cancer Fund with matching funding for the role from the HSE National Cancer Control Programme (NCCP),” says Eibhlín Mulroe, CEO of Cancer Trials Ireland. “UCD will then take over Cancer Trials Ireland funding contribution to continue the partnership with the HSE NCCP.”
The new Chair will share their time between their clinical work as a treating physician at St Vincent’s University Hospital – the national surgical centre for pancreatic cancer – and their research work at UCD School of Medicine.

The Health Service Leadership Academy was delighted to hold a Graduation Ceremony for the MSc in Leadership in Healthcare Cohort 5 and the Professional Diploma in Management in Healthcare Cohort 4 in June 2023.

Graduates from these programmes had to overcome particular challenges to graduate. They commenced their programmes during the Covid-19 pandemic while the health service was working to respond to the demands of resuming normal services while also responding to the challenges of both the pandemic and the cyber-attack at that time. Bernard Gloster, CEO, and Anne Marie Hoey, National Director of HR, attended the ceremony.
Twice as many treated for opioid abuse than any other drug
The National Social Inclusion Office has launched this third report on Drug Treatment in Ireland Key Patterns and Trends: 2014– 2021.
Dr David Evans, Research and Data
Officer, National Social Inclusion
Office, said, “By combining data from two sources, the report shows that approximately twice as many people are treated for problem opioid use than any other drug. This is a significant level of service provision and has implications for future resource allocation.”
Professor Eamon Keenan, HSE National Clinical Lead for Addiction Services, said, “I am pleased to be able to present this third Drugs
Insight report that provides clear information on the number of people receiving treatment for drug-related problems in Ireland. We hope to produce such a report on an annual basis and will work with the HRB to progress recommendations in the report.”
On 1 March 2023, a re on the roof of Wexford General Hospital forced the full evacuation of the hospital. HSE Capital and Estates were on the scene within hours and have been assisting the management and staff of the hospital ever since. Electrical and other life
safety systems such as oxygen and re detection systems were repaired within days to allow the return of services, such as maternity, as a priority.
These past few months have seen a number of works packages delivered at an accelerated pace. These include
HEALTH MATTERS AUTUMN 2023 42 |
NEWS PART ONE
Full report is available on the publications section of hse.ie
HSE Capital and Estates overseeing the reinstatement works at Wexford General Hospital
Patient journey video to encourage students into health careers
Secondary school students curious about a career in healthcare are being invited to accompany a heart attack patient on a virtual journey from his 999 call, through a life-saving intervention in the cath lab at UHL and on to rehabilitation and recovery.
The interactive educational video, an initiative of the Junior Health Sciences Academy (JHSA), has been launched at UHL with the help of TY students from Coláiste Chiaráin, Croom; Gaelcholáiste Luimnigh; Thomond Community College and Castletroy College.

The result is the “STEMI: Patient Journey” video now available as an educational resource on the website of the Health Sciences Academy.
Filmed in Limerick with staff working in their actual environments, this interactive video follows a patient who experiences chest pain, through to his transfer via ambulance to UHL cath lab for stenting of the artery, to the coronary care unit and nally to cardiac rehab. The video has numerous information points, staff role information and course information on where to study.
modular build temporary on-call accommodation, a mobile endoscopy unit linked to the hospital, reconstruction of the hospital roof and the refurbishment of the Special Care Baby Unit, Maternity, St Mary’s and St Patrick’s Wards; all of which were water
At the launch of the STEMI Patient Journey video at the Clinical Education and Research Centre at UHL were Coláiste Chiaráin students Grace Wall, Darragh Enright, Sean Kennedy and Aoife O’Connell with Jennifer McGrath, Clinical Nurse Manager 1,Cardiology; Mary McCarthy, Clinical Nurse Manager 2, Cardiology; and Cliodhna Roche, Cardiac Rehab Physiotherapist, UHL
DOMESTIC, SEXUAL AND GENDER-BASED VIOLENCE SURVEY
47.57% of respondents stated that people accessing their service had requested support
55% of respondents weren’t familiar with their local DSBGV services
21.8% had a lack of information, knowledge and/or experience, lack of screening tools, or need for training/ education
damaged following the re. The hospital looks forward to the full reopening of its Emergency Department following the restoration of these wards.
The coming weeks and months will see the refurbishment of St Catherine’s
First cohort of Hibernia student nurses arrive

The RCSI Hospital Group were pleased to welcome the first cohort of Hibernia College student nurses who have begun specialist placements at Our Lady of Lourdes Hospital, Drogheda and Cavan and Monaghan Hospital as part of their BSc (Hons) in General Nursing degree. This new undergradate nursing programme, developed by Hibernia College, provides alternative routes for people who wish to undertake a full-time Level 8 Degree Programme. The RCSI Hospital Group is delighted to enable these students gain the required clinical experience in their jourmey towards nurse registration while supporting the local and national agenda that seeks to grow the number of registered nurses and midwives to meet increasing healthcare sector demand.
and St Gabriel’s Wards followed by be the reconstruction of the On-Call accommodation and Education Centre, both of which were badly damaged by the re. Finally, the endoscopy service will return to its refurbished location later in the year.
| 43 HEALTH MATTERS AUTUMN 2023 NEWS
Watch the video here
Photo: Brian Arthur
Hibernia College student nurses on placement in Cavan and Monaghan Hospital, Bernadette Grif n, Fisola Akinfenwa and Htoo Htoo Lar.
Steps to Health
Staff walking challenge is improving fi tness levels and connecting colleagues
Steps to Health 2023 nished on a high with 880 teams and 6,631 participants registered for the challenge. With over 60% of teams registered logging their steps and participating in the leader boards, 405 teams completed the challenge logging in their nal step counts in week ve.
The challenge is part of the staff health and wellbeing programme in the HSE encouraging staff to get up, out and move more especially during the workday. It aims to help staff connect with colleagues and overall improve their health and wellbeing by being more active. Steps to Health encourages staff to not only take part but also to look at their activity levels and increase their physical activity beyond the ve weeks of the challenge.
Anne McNally, Director of Nursing, HSE National Infectious Diseases Isolation Facility, and Helen Stokes, Facility Manager, HSE, were both part of The Isolators, a team of 10 based on St Ita’s Campus in Dublin. The Isolators stepped up a whopping 7.3 million steps throughout the challenge – the equivalent of walking from Ireland to Uzbekistan!
In 2022, a group from the Wexford Vaccination Team called the Jabbing Joggers started a walking group for the Steps to Health challenge. After successfully completing the challenge, the group stayed together and continued walking, and planned to walk the Camino in Spain. This year the group completed the Camino walking 117km from Sarria to Santiago de Compostino over ve days. Arriving at the Cathedral on day ve, Ciara Doran, a Jabbing Joggers team member, said, “We each had an
emotional moment, maybe the sheer achievement of walking all day for the last ve days.”
EVE-GHIs Team, called the Grasshoppers, in Dublin 8 were very committed participants this year. Iwona Kolinska, Supervisor, explained, “Our Steps to Health Challenge was a ve-week journey where staff members and students joined their efforts to improve physical tness.

HEALTH MATTERS AUTUMN 2023 44 |
Anne McNally and Helen Stokes from The Isolators during one of their daily walks on the cliff walk at St Ita’s Campus, Portrane.
“At the very beginning we kept motivating each other to go out for a walk, but over time, walks became an important part of our daily routine. We quickly realised how bene cial they are. Students and staff members were looking forward to having a break from prolonged sitting in front of computer screens. We could relax and enjoy beautiful weather.”
She said their daily adventures allowed them to get to know each other better.
“We had many interesting conversations about current sport events, Irish history, art, people that inspire us or places we'd like to visit. During those veweeks we had an opportunity to explore the local area. Our walks became cultural endeavors when we visited places such as the Museum of Modern Art or St Patrick’s Park. Steps to Health not only helped us to increase our physical activity, but also had a positive impact on our mental health. We are very grateful we had a chance to be a part of this great initiative and we are looking forward to joining the challenge next year.”
The Steps to Health Team would like to thank all the staff, teams and co-ordinators who took part in this year’s challenge and look forward to our 2024 challenge! They also would encourage staff to get up and moving and keep stepping throughout the year ahead. HM

Visit www2.hse.ie/living-well/exercise/

MY STORY HEALTH MATTERS AUTUMN 2023 | 45
The Jabbing Joggers, who walked the Camino in Spain.
The Grasshopper Team Wall which motivated the team to keep walking every week and to get their activity up and logging their weekly step count.
"We quickly realised how beneficial they
are.
Students and staff members were looking forward to having a break from prolonged sitting in front of computer screens."
for more information on being active. OUR
Prestigious design award for HSE Ardee ambulance base


An ambitious new HSE building in Co Louth has won a prestigious design award. Ardee Ambulance Base was nominated for and subsequently won in the RIAI (Royal Institute of the Architects of Ireland) category for Healthcare & Wellbeing buildings at the recent 2023 RIAI awards.
The building which was delivered by the HSE Capital and Estates Team sits on the northern edge of St Brigid’s Hospital Campus in Ardee. The new facility caters for the staff and vehicles with the provision of staff of ces, rest rooms and kitchen, changing areas and showers.
Moloney O Beirne Architects were appointed design lead, while the HSE Capital and Estates team were led by Selina Kavanagh, Estates Manager, John McCrea, Project Manager, Tom Connor and Marc McHugh, Site Clerk of Works, assisted by John F Shevlin, Ambulance Of cer.
Winners announced in second NCHD research competition
The National Doctors Training and Planning (NDTP) Training Leads for Dublin Midlands Hospital Group (DMHG), Prof Robert Eager and Dr Darragh Shields hosted their second NCHD Research Competition earlier in the summer. The NDTP Training Leads play an important role in supporting the wellbeing, education, and training of NCHDs across the DMHG.
This yearly competition is a great opportunity for NCHDs to showcase their hospital-nominated projects on original research, a completed audit cycle, or a quality and improvement project. The competition allowed NCHDs to demonstrated their research skills, represent their respective hospitals and win prizes.

The competition consisted of five oral presentations and a NCHD poster competition. Participants displayed exceptional skills, and the event provided a platform for them to showcase their research and gain recognition. Guest speakers David Mockler and Nicola Fay also gave informative presentations on systematic reviews and searching the literature, adding value to the event.
Jessie Elliott won the first prize of a €1,000 gift voucher in the oral presentations, representing St James’ Hospital. Dr Christopher Fenelon and Dr Darren Moloney, representing Midlands Regional Hospital Tullamore, came second and received a €500 gift voucher. Dr Guhan Rangaswamy, representing St Luke’s Radiation Oncology Network, won the poster competition and received a €250 gift voucher. The judges commended all participants for their impressive work.
HEALTH MATTERS AUTUMN 2023 46 |
AWARDS
Dr Darren Moloney, MRHT; Dr Christopher Fenelon, MRHT; Dr Conor Costigan, TUH; Dr Jessie Elliott, SJH; Dr Jill Nicholson, SLRON); Dr Myles Flitcroft, CWIUH.
Paul Moore Photography - Ardee Ambulance Base
Heroes Ignite Innovation
The HSE Spark Summit 2023 took centre stage in Dublin recently, showcasing the extraordinary ideas and breakthrough innovations generated by healthcare workers. The event, which celebrated the spirit of innovation and ignited a passion for creativity, provided a dynamic platform for healthcare professionals to address the challenges they encounter in their clinical practice and spearhead transformative solutions.
During the summit, innovative projects that received support through the HSE Spark Innovation Programme were showcased and duly acknowledged.
Dr Patsy Lenane's project, Skinnovate, won the
Saolta celebrates incredible nursing and midwifery mentors
Saolta University Health Care Group is celebrated recognising the contribution of our nursing and midwifery mentors in supporting new colleagues.
The Saolta Preceptor Recognition Awards is an initiative to publicly acknowledge and thank the nurses and midwives who made such a huge impact on our new recruits.

Preceptorship is the term given to a structured, supported period of learning where experienced nurses take on the role of mentoring newly appointed nurses and helping them to adapt to their new positions. Since 2022 over 550 new overseas nurses and midwives joined the Saolta group and benefited from an adaptation and preceptorship programme.
Sligo University Hospital winner: Maeve Dolan
Roscommon University Hospital winner: Gráinne Keaveney
Galway University Hospitals winners: Therese Prendergast and Soumya Rajan
Letterkenny University Hospital winner: Manjumol Thomas
Mayo University Hospital winner: Chelsea Bourke
Portiuncula University Hospital: Diane Fitzgerald
CEO's Choice Award for Best Hospital and Community Integration Project. It involves using lifelike skin models to aid GPs in managing routine skin conditions.
Dr. Petya Bogdovana-Mihaylova led a project at Tallaght University Hospital (TUH) that won the HSE Bright Spark Award for Best Admissions Avoidance Project. The project aimed to optimise the management of headache patients in the emergency department to prevent hospital admissions


Siobhan Meany's 'Constant Pressure Device' was named as victor of the HSE Spark Ignite Competition. The award was presented by Minister Ossian Smyth.

| 47 HEALTH MATTERS AUTUMN 2023 AWARDS
Jared Gormly, Ossian Smyth, Siobhán Meaney and David Pollard.
Dr Patsy Leanneand Bernard Gloster., Dr Hannah O'Keefe, Dr Petya Bogdanova-Mihaylova and Jared Gormly.
Support for refugees
The Psychology Service for Refugees and Asylum Seekers (PSRAS) turned 30 last year, coinciding with a huge increase in applications for international protection. To reflect on the past 30 years and the evolution of the service, psychologists, support staff and service users shared their experiences with Dr Amy Moriarty, Senior Clinical Psychologist for PSRAS.

PSRAS is currently based in Balseskin Reception Centre, which provides accommodation, food and onsite medical care to approximately 500 international protection (IP) applicants also known as asylum seekers.
“In addition, our service also provides off-site psychological support to other accommodation

HEALTH MATTERS AUTUMN 2023 48 | FEATURE
Dr Amy Moriarty talks about the experience of working in the Psychology Service for Refugees and Asylum Seekers
Dr Amy Moriarty (centre) with Jessica Cooper and Caitriona McKeown, both social workers with the service.
centres in CHO9. PSRAS provides short and medium-term interventions as well as traumafocused groups and workshops,” explained Amy.
The residents of these centres arrive from many war-torn or corrupt countries and enter into a process of waiting for interviews, transfers and outcomes regarding refugee status. Some people may also come as programme refugees. They are selected while overseas, and given refugee status, allowing somewhat easier access to supports on arrival.
It was for programme refugees that PSRAS was originally set up. In 1992, Brian Glanville, then Director of Psychology for the Eastern Region Health Authority, set up a new specialist service for refugees displaced by the Bosnian war.
“Over the next 20 years, approximately five psychologists worked hard to maintain
The management and shape of the service changed over the following years, and in 2012 it had reduced from five psychologists to one. In 2015 Graham Connon took over as principal of the service and remains in this position. In the last eight years the management structures have changed and PSRAS is now under the governance structure of social inclusion and caters specifically for CHO9. There are now two full-time senior posts, one staff grade post and trainee placements.

and build the service, including Liliana Morales, who is still with the service today. A designated psychologist was also hired to support young unaccompanied minors arriving alone to Ireland,” said Amy.

“An interpreter who currently works with PSRAS came as an unaccompanied minor and spoke of many challenges at the time, particularly the fact that asylum seekers could not work, which contributed to a range of social and mental health problems. A positive change since then has been that the right to work after six months. One former service user reported a very positive experience with PSRAS but felt that stigma was a barrier for many cultures in accessing psychology. Thankfully, many PSRAS psychologists have done huge work to teach cultural competence to trainees to increase cultural awareness and understanding.”
“What was remarkable in my conversations with some of the psychologists who have worked here was that almost everyone said one of the greatest positives of working with this population group was the bountiful gratitude received for minimal input. This in turn seemed to make the work rewarding for many, and even sustaining,” said Amy.
“One recalled the pride and humility they felt when a former client made contact years after discharge to interview them for their thesis. It seems the impact of human connection in the face of such displacement and disconnection can be profound and memorable for clients as well as staff.”
When asked about the challenges of working in this area, Amy said that many mentioned resource challenges and difficulties navigating complex and fragmented systems as well as the need for a unified national approach to supporting this population.
“The need for boundaries, self-care, supervision and support to prevent burn-out was often referenced. Working with different cultures and languages can also pose challenges related to communication and understanding and there may be challenges when working with interpreters. However, overall, enthusiasm for diversity and difference was a striking theme,” she said. HM
FEATURE | 49 HEALTH MATTERS AUTUMN 2023
The original home of the service at Grangegorman.
"It seems the impact of human connection in the face of such displacement and disconnection can be profound and memorable for clients as well as staff.”
Liliana Morales who works with PSRAS.
SPOTLIGHT ON
Screening Services
Capturing real-time feedback from people who take part in bowel screening
The National Screening Service rolled out a novel digital approach to gather real-time feedback from screening participants, to explore people’s experiences of BowelScreen, the national bowel screening programme, in 2022.
The online survey was sent to a selection of BowelScreen participants by text message. The digital survey helped the programme capture and analyse responses quickly and easily.
The results of the digital survey were positive: 89% of respondents rated BowelScreen as ‘good’ or ‘very good’. Overall, BowelScreen participants reported high levels of satisfaction with the programme. It achieved a net promoter score – a measure used to gauge participant loyalty, satisfaction and enthusiasm - of over 73%, a score considered exceptional.
Research
The National Screening Service (NSS) is researching people’s attitudes to self-sampling for cervical screening. Some countries have started using self-sampling as part of their cervical screening programmes. In 2022 the NSS started assessing how useful self-sampling might be for the Irish cervical screening programme; what people think about it; how reliable it is as part of a screening programme;

The results show how participants feel about communications from the BowelScreen programme and have given the programme feedback on the services provided, and where improvements can be made.
The response rate to the survey of between 42 and 49% is considerably higher than traditional paperbased surveys, showing it to be an effective and innovative way to capture real-time patient experience.
Given the success of the project, the NSS is replicating this digital real-time methodology for BreastCheck in September 2023 for all women who have a BreastCheck mammogram and receive a normal result. The survey results will be used to improve BreastCheck and learn from women’s experiences. HM
and the ways it might be added to the CervicalCheck programme in the future. The NSS is also evaluating new international research as it is published, and talking to colleagues in other countries where self-sampling is being offered in cervical screening programmes.
The research will aim to find out if self-sampling would appeal to under-screened and never-screened groups of people. It will ask what kinds of support and information people might need to take a self-sample correctly, such as talking to their GP or practice nurse, an explanatory video, or a leaflet with pictures; and whether people would be happy to receive a self-sampling kit in the post or if they would rather collect it from their GP or pharmacist. HM
HEALTH MATTERS AUTUMN 2023 50 |
examining the potential role of self-sampling in cervical screening
CervicalCheck programme providing personal cervical screening reviews
For more information, visit cervicalcheck.ie. Participants can request a review by emailing review.request@ screeningservice.ie.
Launch of new pregnancy eye screening initiative
Further information visit diabeticretinascreen.ie, or Freephone 1800 45 45 55. Healthcare professionals can make referrals via pregnancyeye@ screeningservice.ie.
CervicalCheck has introduced a new review process for women who have had screening and subsequently develop cervical cancer, called personal cervical screening reviews. The reviews are available on request for all women who have had a CervicalCheck screening test in the 10 years before a diagnosis of cervical cancer. Women will have a personal contact person throughout the review process.
The aim of a review is to help women or their families if they are looking for answers or ways to understand how and when their cancer developed. Reviews will provide women with an opportunity to ask questions about their screening journey, using a restorative approach tailored to each person’s circumstance.
The process was designed with input from women who participated in CervicalCheck and subsequently received a cervical cancer diagnosis. There was oversight by a multi-disciplinary implementation committee with representatives from the NSS’s patient panel, the Irish Cancer Society, clinical experts, and communications and programme staff. HM
A new screening initiative for women who have diabetes and become pregnant has been launched. The risk of diabetic retinopathy may increase during pregnancy and through this new initiative, the National Screening Service’s Diabetic RetinaScreen programme is working with maternity units and other healthcare professionals, to provide sight-saving screening during pregnancy.

Diabetic RetinaScreen Clinical Director Professor David Keegan spoke about his clinical experience of working with women with diabetes, and the potential impact of pregnancy on the eyesight of a woman who has diabetes.
Patient advocate Vicky Doyle, who is attending for more frequent diabetic retinopathy screening through the initiative, shared her experiences. She told Minister Donnelly that the new system gives her “a sense of being minded”. She said the efficiency and regularity of the service “is good; you get the appointment, test, and your results arrive very soon after your test. It’s a joined-up service and there’s a continuum of care.” HM
‘Talking Health & Wellbeing’ podcast
Putting people at the heart of the National Screening Service’s (NSS) new five-year strategy was the subject of the HSE’s ‘Talking Health & Wellbeing’ podcast. In the podcast episode, ‘#ChooseScreening’, Fergal Fox interviewed NSS Chief Executive Fiona Murphy, and Patient and Public Partnership (PPP) representative Grace Rattigan. Available on all podcast platforms.
| 51 HEALTH MATTERS AUTUMN 2023
DRS Programme Manager Helen Kavanagh; Karen O’Connor of the Mater Misericordiae University Hospital; NSS Chief Executive Fiona Murphy; Consultant Endocrinologist Assoc Prof Mensud Hatunic; Minister for Health Stephen Donnelly; patient advocate Vicky Doyle; and DRS Clinical Director Prof David Keegan.
Better ways to work
In this section we look at...........
New Diversity, Equality and Inclusion eLearning programme available
The HSE Diversity, Equality and Inclusion team has launched a new eLearning programme called Diversity, Equality and Inclusion in the Workplace. This programme aims to support all staff members across the Health Service to apply the principles of diversity, equality and inclusion to our working environments and teams.
“We wanted to develop a useful and practical learning resource for staff members,” said Maria Molony, Diversity, Equality and Inclusion Manager. “We designed this programme to provide information and guidance on some of the most common types of enquiries that our team receives from staff on topics relating to diversity,
equality and inclusion in the workplace.”
• The eLearning programme has been developed with support from the three HSE Staff Networks:
• The Cultural Diversity network for employees from diverse ethnic and cultural backgrounds and their allies
• The Le Chéile network for employees with disabilities and their allies
• The Reach Out network for lesbian, gay, bisexual, transgender, queer, intersex and asexual (LGBTQIA+) staff and their allies. The eLearning programme is available on HSeLanD and consists of three modules. You can nd the programme in the Human Resources course catalogue, or by searching for each module name in the HSeLanD search engine. HM
If you have any feedback on the eLearning programme or if you would like further information or guidance, please contact diversity.hr@hse.ie
HEALTH MATTERS AUTUMN 2023 52 |
Clinical Audit Case Study: Our Lady of Lourdes
How do you know you and your team are providing the best care possible to your patients? Think about the structures, processes and outcomes of care where you work.
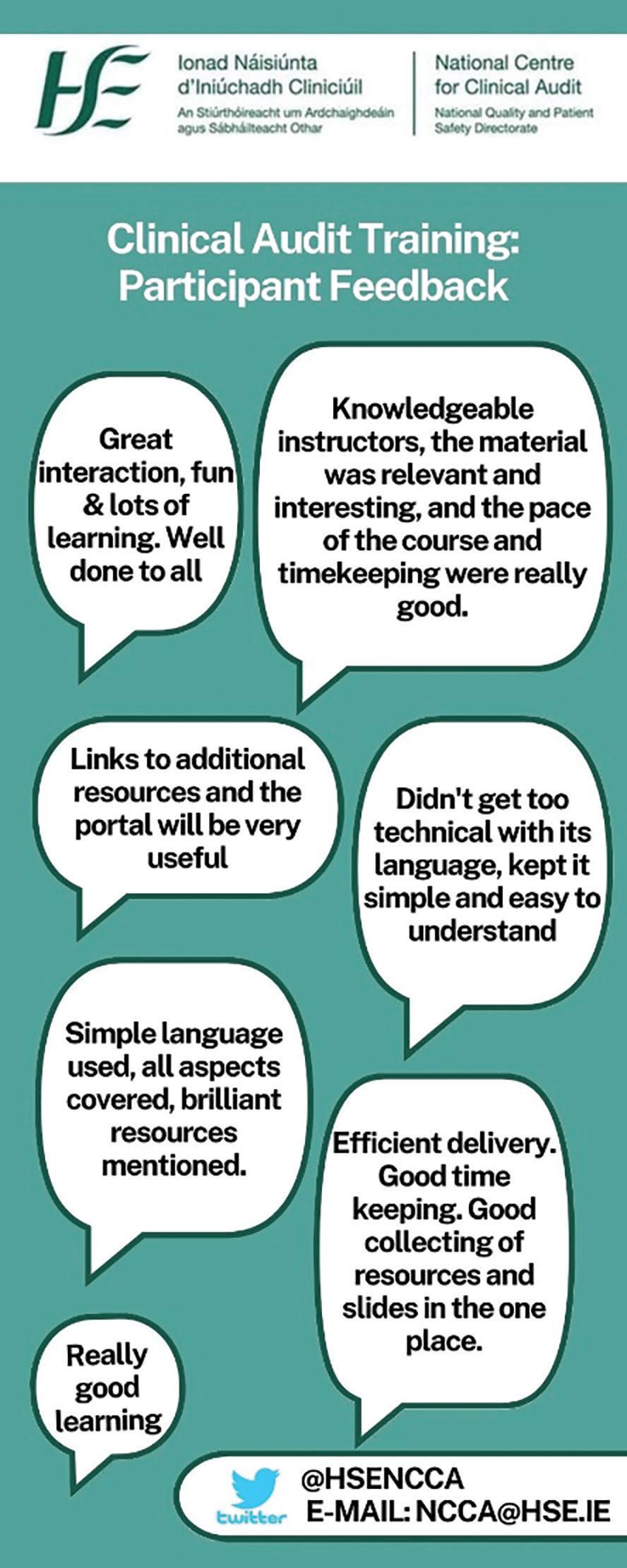
Local clinical audit provides the ability to improve the quality of care in individual healthcare settings in a collaborative and systematic way. When clinical audit is conducted well, it enables the quality of care to be reviewed objectively within an approach that is supportive, developmental and focused on quality improvement.
Mark Knipe and Elaine Conyard from the Pharmacy Department in Our Lady of Lourdes Hospital, Drogheda recently provided an example of the bene ts of local clinical audit. They conducted a clinical audit with the aim of improving medications management for inpatients with Parkinson’s disease.
As Mark and Elaine explained, patients with Parkinson’s disease (PD) require timely administration of medications to control their symptoms and admission to hospital can cause a disruption to their medication routine. This can result in adverse effects for them, such as; the loss of symptom control and permanent reductions in a patient’s baseline condition.
Having identi ed opportunities for improvement with an initial audit of 24 patients, Mark and Elaine introduced the pharmacist-led interventions of staff education, priority medicines reconciliation and stock optimisation.
Post implementation re-audit of 30 inpatients with PD demonstrated improved results. For example, the percentage of patients receiving pharmacist medicine reconciliation increased from 79% to 97%, the average delay in administration of 1st dose medication following admission reduced from 14 hours to four hours, and the percentage of patients who experienced increased rigidness during admission decreased from 54% to 7%.
In order to plan this effective clinical audit, Mark and Elaine, followed the best practice guidance in the seven stages of clinical audit included in Clinical Audit: A Practical Guide 2023, which has recently been published by the HSE National Centre for Clinical Audit. HM
receiving
medicine reconciliation increased from 79% to 97%, the average delay in administration of 1st dose medication following admission reduced from 14 hours to four hours, and the percentage of patients who experienced increased rigidness during admission decreased from 54% to 7%."
BETTER WAYS TO WORK | 53 HEALTH MATTERS AUTUMN 2023
"The percentage of patients
pharmacist
Measuring progress with Evaluation Framework
Mindful of the need for continuing reflective practice in a changing environment, the Health Promotion and Improvement (HP&I) team in HSE Community Healthcare East are developing a service-specific Evaluation Framework.
There are many benefits to this framework but primarily it ensures that the team is consistently evaluating different aspects of its service, and using this to identify where further resources or targeted work may be necessary.
In conjunction with using Health Atlas to embed health needs assessment in their planning and service delivery, the team envisages this framework will enhance their understanding of how their practice meets the diverse, complex and changing needs of the local population.
The objective of this project is not to duplicate existing evidence underpinning their programmes, but rather to assess the local context for implementation and produce practice-based evidence to complement it, using a pragmatic approach, explained a team spokesperson.
This project has almost reached completion and it should lead to greater focus on service users’ expressed needs and continuous reflective practice leading to greater value for money. HM
Moving all staff users and devices to HealthIRL a key priority
User accounts, devices and mailboxes will be moved from our eight legacy regional domains to a single domain in the HealthIRL migration programme. Migrating to HealthIRL is essential for cloud and cyber security, and a key recommendation in the HSE cyber-attack post-incident review report.
HealthIRL is a secure modern platform, supporting best practice identity management, resilience and security. With HealthIRL you can access cloud-based systems and get a single view of the organisation. It simpli es collaboration and means you use one account as you move throughout the organisation.
Bene ts of HealthIRL and why you need it
• Must be on HealthIRL to access Microsoft Teams, Of ce 365 and Exchange Online
• Ability to access cloud-based systems such as HPVP, single sign-on (SSO), Trendcare, and others
• Locate any HSE staff member in a single email directory
• Share calendars with colleagues across all locations
• Login from any location, on any HSE device
• Keep the same login if you relocate between HSE regions
• Access national applications and shared folders from any location
• Reset expired and forgotten passwords using self-service
• A more connected and standardised user experience
Every HSE building, department and staff member will move to HealthIRL. Users at every level of the organisation should prioritise HealthIRL migration when in your area.HM
For more information on this contact
Louise.Tully@hse.ie
For general enquiries and notifying us if you have not been migrated yet, contact Healthirl.migration@hse.ie
HEALTH MATTERS AUTUMN 2023 54 | BETTER WAYS TO WORK
Project Management Offices (PMOs) are a relatively new function in HSE organisations. The role of a PMO is to provide a range of expert support and change management services to aid the successful planning, implementation and delivery of new HSE projects and initiatives.
PMOs play an integral role in increasing capability to deliver service improvements and organisational change through staff training and support in project management,” explained John Nwobo, General Manager and Portfolio Lead, Project Management Office, HSE Community Healthcare East.

“They facilitate the delivery of benefits to service users and value to the public by managing change
well, enabling benefits realisation management and service improvement evaluation processes. PMOs also enable strategic alignment of projects to ensure that investment is provided to the right service improvement projects - those that contribute to an organisation’s strategic priorities.
“The PMO approach involves using standardised methodology, tools and templates to ensure optimal development, collation and analysis of project data, while also identifying and helping to mitigate project risks and issues.
Project Management support is widely available across Community Healthcare Organisations and Hospital Groups. Reach out to your local office to find out more about training opportunities and how taking a project management approach could help you with your next service improvement project. HM
| 55 HEALTH MATTERS AUTUMN 2023 BETTER WAYS TO WORK
The PMO approach to delivering successful new healthcare initiatives
John Nwobo
“They facilitate the delivery of benefits to service users and value to the public by managing change well, enabling benefits realisation management and service improvement evaluation processes."
Creative reflection initiative expanded to registered nurses at Connolly Hospital
Creative re ection sessions have proven such a success with student nurses that the initiative has been extended to registered nurses at Connolly Hospital Blanchardstown (CHB).
The programme has provided student nurses and registered nurses with an opportunity to express themselves by re ecting on experiences through alternative methods of representation. Nursing students and registered nurses have engaged in wonderful examples of poetry, drawings, pictures and mind maps to demonstrate their learning and understanding on speci c experiences and topics. This has led to the initiation of valuable group discussions on experiences/topics, which has subsequently enhanced the learning for all involved
The use of these sessions were predominantly initiated in CHB for student nurses. However, with such positive feedback received from student evaluation, its use has also been incorporated into a variety of educational programmes for registered nurses attending the Regional Centre for Nursing and Midwifery Education, Dublin North (RCNME DN). Using an active teaching strategy during re ection sessions has led to a greater enthusiasm within the cohorts of nursing students/registered nurses to participate in critical re ection, which has enhanced their ability to apply and integrate their own meaning and understanding of experiences leading to the promotion of future learning opportunities.
The rst creative re ection session was piloted in January 2022 with a group of third year DCU student nurses. Following positive student feedback from the rst session, the use of creative re ection sessions have now been implemented throughout all year groups of DCU nursing students by CPCs from the NPQD Connolly Hospital.
The use of re ection speci cally within undergraduate nurse education is imperative, as it allows students to examine their own experiences, analyse their feelings and re ect on their own actions with the aim to acquire new knowledge and understandings of situations and concepts. Furthermore, re ection provides student nurses and registered nurses with an opportunity to explore practice experience, and integrate existing knowledge with new insights and understanding.
CHB CPC and Student Allocation Liaison Of cers (SALO) are currently part of a working group in DCU reviewing the facilitation of re ective practice for undergraduate student nurses. The plan going forward is to incorporate more structured creative re ection facilitated by both CPCs and Higher Education Institutes combined with independent re ection learning to enhance critical thinking, leadership and professional development. HM

HEALTH MATTERS AUTUMN 2023 56 | BETTER WAYS TO WORK
The latest episode of the All Ireland podcast series Walk and Talk Improvement is now available. The aim of this series is to improve patient care by capturing the personal stories of people who work in and use health services. Episodes feature guests from across Ireland, Northern Ireland and the UK.

Episode 7, hosted by Dr Maureen Flynn, Director of Nursing, ONMSD, features leaders in nursing and midwifery from Ireland and Northern Ireland working to make healthcare safer for everyone. Our guests share their journeys and experiences as leaders in nursing and midwifery. As a listener, you will learn about their:
• solutions, innovations and strategies used to improve patient and staff safety
• their clinical experiences and how this has shaped their leadership roles
• tips for how you can oversee and implement patient and staff safety improvements in your service and,
• their inspirations and experiences along the way.
If you’re looking for inspiration and insights in your patient safety, nursing or midwifery work, tune in to hear the insightful stories shared in this episode. HM
Webinar series shares learning and experiences
The National QPS Directorate provides a regular lunch time one-hour webinar series focusing on quality safety and improvement. Running approximately every two weeks in term time, it is open to all those interested in improving quality and patient safety across our healthcare services. Join individually or together as a group to assist in building your own local QPS networks.

THE WEBINARS AIM TO:
• connect people interested in QPS


• share learning and experiences of improvement. HM
You can watch back previous QPS TalkTime episodes on the NQPSD YouTube Channel. Follow us on Twitter to stay up to date
@QPSTALKTIME
BETTER WAYS TO WORK | 57 HEALTH MATTERS AUTUMN 2023
the QR Code below to register
Scan
‘The patient today could be you tomorrow’
Survivorship
An important new Cancer Research Clinic, the rst and only one of its kind in Ireland has been established at Tallaght University Hospital (TUH). The new Testicular Survivorship Clinic is conducting research to try and discover new treatments for patients, who have had the disease.
Those centrally involved in this important new clinic at TUH include Dr M Raheel Khan, Research Registrar; Prof Ray Mc Dermott, Medical Oncologist; and Advanced Nurse Practitioner in Oncology Patrice Sheehan. The team started work on the clinic back in September 2022 and saw their rst patient in October 2022. To date, they have seen around 75 patients.

So far, medical staff involved in this trial at TUH have met with patients to examine them, take blood tests and get them to ll in a targeted questionnaire. If anything suspicious arises out of this initial screening then further tests, scans and if necessary follow-up treatment can be arranged. The team behind this new development are hoping this clinic will improve morbidity and mortality for patients with testicular cancer. Medical oncologists around the country are very keen to replicate this model in other centres.
Testicular cancer is typically diagnosed in a young male population (15 to 35 years) and has a cure rate of 95%. This means there is a big cohort of patients who are survivors. Recent studies have shown a very high incidence of second cancers, cardiovascular events and psychological issues, resulting in higher rates of early deaths, suicide, unemployment and disabilities. To help them and
intervene early if these other complications arise, numerous medical studies including this one at TUH are being conducted in the US, UK and Scandinavian countries. In March 2023, at a stakeholder meeting of Cancer Trials Ireland, it was agreed to establish similar clinics nationwide. A central registry will be maintained in the Trials Unit of TUH. As a result, the TUH Cancer trials team will collect and maintain data on patients from all over Ireland.HM

HEALTH MATTERS AUTUMN 2023 58 | FEATURE
Important new Cancer Research Clinic set up at Tallaght University Hospital
Dr M Raheel Khan, Research Registrar; and Advanced Nurse Practitioner Oncology, Patrice Sheehan.
Eye Suite
Improving Access to Outpatient and Day Case Ophthalmology Services
New outpatient and day case services are now available at Nenagh Hospital with the opening of the Eye Suite.
Located in the €1.5 million outpatients extension at Nenagh and building on the designation of Nenagh as a centre for cataract surgery since 2018, this new development expands outpatient ophthalmology services and means patients can for the first time have their eye injections in Nenagh.
Until now, ophthalmology services within UL Hospitals Group had been principally delivered at University Hospital Limerick. The relocation of part of this service is in line with the Group’s objectives to expand activity in model 2 hospitals and also sits well within the framework of Slaintecare and the National Eye Care Plan developed by the Irish College of Ophthalmologists.
The new service in Nenagh is led by consultant ophthalmologist Mr Conall Hurley. New treatments available to adult patients in Nenagh include intra-vitreal injections (IVTs) for conditions such as diabetic retinopathy, retinal vascular occlusions and wet agerelated macular degeneration. The new suite is also equipped with a range of modern ophthalmic lasers for the treatment of post cataract surgery capsular changes, retinal vascular diseases and uncontrolled glaucoma. The existing cataract surgery service will continue in Nenagh.
“Since 2018, almost 5,000 patients have had their cataract surgery performed in Nenagh. In view of the success of the cataract service here, hospital management concluded that it would be complementary to have an expanded ophthalmology service located on the Nenagh campus. This would allow delivery of both outpatient clinics as well as appropriate treatments on the Nenagh campus as well,” he said.
Mr Hurley added he was pleased to be now be heading a team delivering an expanded range of appropriate services in Nenagh while maintaining the delivery of his ophthalmic emergency services in UHL.
SINCE 2018 ALMOST
5,000
PATIENTS HAVE HAD THEIR CATARACT SURGERY PERFORMED IN NENAGH

That multidisciplinary team comprises medical and specialist nursing staff, including advanced nurse practitioners (ANPs); an optometrist; allied health; administrative and support staff.
Mr Hurley noted that such integrated eye care teams working closer to the patient’s home is envisioned in the National Eye Care Plan. It is expected that candidate ANPs currently training under his supervision will ultimately be delivering services directly to patients in Nenagh with the expanded scope of practice including eye injections and screening patients for conditions such as cataract, glaucoma and diabetic retinopathy. HM

MY STORY
Top: Thomas Barton from Castletroy in Limerick celebrating with Nenagh Hospital staff after he was the first patient to have an eye injection at the new Ophthalmology Suite at Nenagh ABOVE: Ailish O’Callaghan, Clinical Nurse Specialist, Ophthalmology; Bernie Nolan, Assistant Director of Nursing; Mary McCormack, Staff Nurse; and Deirdre Grace, Candidate Advanced Nurse Practitioner Ophthalmology.
HEALTH MATTERS AUTUMN 2023 | 59
Elevating the voice of patients
Did you know one in three people in Ireland have trouble reading, understanding and using health information to manage their treatment and care? People accessing our health services as both patients and family advocates will struggle with information that is essential to good health and patient safety. Poor literacy also impacts the capacity of patient partners to truly get involved in the design of health care.
This year’s World Patient Safety Day took place on Sunday, 17 September. The HSE partnered with Patients for Patient Safety to develop and signpost helpful resources for staff and patients. The theme is ‘Elevate the voice of patients and patient safety through health literacy’. We want to recognise the important role of patients in healthcare delivery by elevating their voices. We need to collectively identify their needs and work to address them.

To get you started, a useful resource is the Ask Me 3: Good Questions for Your Good Health as a prompt for patients or a prompt when explaining materials to patients.
• What is my main problem?
• What do I need to do?
• Why is it important for me to do this?
https://www.ihi.org/ resources/Pages/Tools/ Ask-Me-3-GoodQuestions-for-Your-GoodHealth.aspx
You can also access resources through the National Adult Literacy Agency website.
Innovative Infographic unveiled in TUH ICU

An innovative infographic has been unveiled at the Tallaght University Hospital (TUH) ICU Wing. Sponsored by the Adelaide Health Foundation Innovation Fund, the simple, colourful and clinically accurate infographic will be on display in the waiting area for families. The ICU wing at TUH is the first hospital in the country to display this type of informative infographic.
The infographic, which has been developed by an expert hospital design company enables family members to familiarise themselves with the key ICU equipment they will find at their loved one’s bedside. The display will ‘demystify’ the very clinical and often daunting nature of the ICU for families.
“It is well established that families experience significant levels of stress and distress during the admission of a loved one to ICU. For most of our families, the sudden and unexpected admission of their loved one will be their first (and possibly only) experience of the world of ICU,” said Dr Melanie Ryberg, Principal Clinical Psychologist and Clinical Neuropsychologist in ICU.
HEALTH MATTERS AUTUMN 2023 60 |
NEWS PART TWO
Caption: Dr Natalie Cole, Head of Innovation at Innovate Health at TUH; Dr Melanie Ryberg, Principal Clinical Psychologist and Clinical Neuropsychologist in ICU; Lisa Dune, CNM3 ICU; and Niamh Gavin, CEO of the Adelaide Health Foundation.
HSE surveying people aged 65 and under living in Nursing Homes and Older Persons Services
The HSE is carrying out a national online survey of people aged 65 years and younger who live in registered public, private and voluntary nursing homes, and older person services.
There are approximately 1,300 people aged 65 and under living in nursing homes and services for older persons who may have an acquired brain injury, a neurological condition, a complex physical and intellectual disability or a complex medical diagnosis. The information collected in the survey will be used to establish a database that will;
• help to identify people with a disability who may be inappropriately living in nursing homes and older persons services.
• help to ensure that the most appropriate health and social care supports are provided in the most appropriate setting.

• help to identify and plan the resources the person needs to live the life they choose, in their current service or in a home in the community.
• enable the HSE and service providers to plan services and ensure the needs of people with disabilities are being met.
Ukrainian Community Centre opens in Bray

HSE’s Community Healthcare East’s Social Inclusion team were delighted to be part of the official launch of the Ukrainian Community Centre Bray and North Wicklow which took place in June in St. Andrew’s Presbyterian Church Hall, Bray.

Bray Area Partnership led the event with Minister for Community Development and Charities, Joe O’Brien, and the Ambassador of Ukraine to Ireland, Larysa Gerasko among more than 100 invited guests. The event provided a great opportunity for various organisations that have come together to support Ukrainians seeking temporary protection in Ireland to reflect on the amazing work that has been done over the last year in this regard.
Lee Collins, Social Inclusion Manager, and Tetyana Dmytrash, Ukrainian Outreach Worker from HSE Community Healthcare East, pictured above, were on hand to highlight the GP and primary care services provided by Edoc in Bray.
| 61 HEALTH MATTERS AUTUMN 2023 NEWS
The resident online survey can be accessed here https://surveys.hse. ie/s/U65-ResidentSurvey or by scanning the QR code.
There were great celebrations in Tallaght University Hospital (TUH) recently as it celebrated its 25th anniversary. Back in 1998, 115 patients were transferred from the base hospitals of the Meath, Adelaide and National Children’s Hospitals with 1,500 staff to TUH. The hospital now employs over 3,000 staff with over 60 nationalities represented in its workforce and is one of the largest employers in the Tallaght area.
Lee Collins, Social Inclusion Manager, and Tetyana Dmytrash, Ukrainian outreach worker, from HSE Community Healthcare East.
The HSE Annual Report and Financial Statements 2022
The Health Service Executive Annual Report and Financial Statements 2022 was published on 4 July 2023. The Annual Report is an instrument of accountability that provides a range of detail re ecting the dynamic and complex delivery of a nationwide health and social care service. It includes an overview of governance and accountability within the organisation and provides detailed nancial information about our organisation through the Annual Financial Statements.
In his review, the Chief Executive Of cer highlighted that “Since 2020, health services have faced extraordinary challenging times with the impact of COVID-19 and the criminal cyberattack, and with how the world has fundamentally changed for all of society in terms of the war in Ukraine and demands for international protection. In the face of these signi cant challenges, new services have been developed and improvements to existing services have been achieved. It is our people, the staff of the HSE and our many partner professionals and organisations who have made this possible.”
Living with COVID-19
2022 was the third year of COVID-19 but the rst full year of our transition to living with the virus. In the rst ve days of 2022 we had more con rmed COVID-19 cases than in all of 2020, and by March we had more hospitalised cases than in the 14 months prior to that point. Despite a reduction in the prevalence of COVID-19 within the community, it is clear that COVID-19 continued to have a signi cant impact on our health and social care services in 2022.

Waiting lists and access to care
Increased and sustained unscheduled care demand (unplanned / emergency care) was a signi cant challenge in 2022 across all acute hospitals. While considerable progress was made during the year, the most critical health priority as we move into 2023 is to ensure the full delivery of the Waiting List Action Plan which will include short-term
measures to address acute scheduled care and community waiting lists backlogs, as well as longer-term reforms to enhance capacity.
Performance and key achievements
In our commitment to deliver upon the vision to transform Ireland’s health and social care services, including mental health, disability and older persons’ services, work continues to ensure equitable access to integrated services, organised around people’s needs.
• 20 Sláintecare Healthy Communities were established across the country, in areas of highest disadvantage, to provide the following services: Stop Smoking, Parenting Programmes, Healthy Food Made Easy, Making Every Contact Count (MECC) and Social Prescribing.
• Community Intervention Teams (CITs), who provide a rapid and integrated response where enhanced services / interventions are required for a de ned short period of time, achieved national coverage during the year, receiving almost 84,000 referrals in 2022 (30% higher than expected activity).
• Over 1.1m contacts were made with general practitioner (GP) Out of Hours services during the year (23.8% ahead of the 2022 target and 8.8% higher than the number of contacts in 2021).
• Over 8,100 people were removed from waiting lists as a result of community wait list initiatives. Approximately 6,300 of these were children and young people in orthodontics, primary care child psychology, counselling in primary care, and child and adolescent mental health services.
HEALTH MATTERS AUTUMN 2023 62 |
• Almost 21 million home support hours were delivered to almost 75,000 older people during the year. This was an additional 320,000 home support hours compared to the previous year.
• Work continued on strengthening the 91 Children’s Disability Network Teams which offer multi-disciplinary, child-centred and family-focused care. A new integrated assessment of need tracking system for children and adults was also progressed.
• Almost 390,000 emergency ambulance calls were responded to in 2022, with over 1,000 air ambulance calls completed and over 2,000 specialised unit transfers undertaken by the National Ambulance Service critical care retrieval service and children’s ambulance service.
• The number of people waiting over 18 months for outpatient services reduced by 38%, while the number waiting over 12 months for inpatient services reduced by 23%
• 157 additional permanent acute beds were delivered.
• To support cancer patients and their families at all points in the cancer journey, a model of care for Psycho-oncology was launched, setting out how supports will be developed over the coming years.
• All 19 maternity services are now providing midwifery-led care in the supported care pathway for normal risk women. HM
Financial management
The HSE is committed to its obligation to protect and promote the health and wellbeing of the population while making best use of the resources available to it. We are continuing to work with all services to ensure core financial management controls are operating effectively and to secure greater efficiencies in the use of the totality of resources available to us. In 2022, the HSE continued to operate in an environment challenged by on-going funding and expenditure pressures caused by the COVID-19 pandemic. Revenue and capital funding of €23.5bn was received from the Department of Health, including €1.9bn which was provided on a once off basis in relation to the HSE’s COVID-19 strategy. The overall revenue expenditure reported for 2022 was €23.4bn which is 8% higher than the expenditure in 2021. Acute hospitals and the National Ambulance Service represented 38% of overall expenditure, with 47% of expenditure in community services. Work continued on the development of the integrated financial management system (IFMS) to support improvements in financial reporting, including analysing and forecasting.
1.35
54,500 3.37 103 million new Emergency Department attendances
births in 2022 million home support hours delivered to persons with a disability
new emergency places provided to people with a disability
157,000
(almost) women in the eligible population had a complete mammogram
6,300 smokers received online cessation support services
4,000 people accessed specialist inpatient palliative care beds within 7 days
21 million home support hours provided to elderly
| 63 HEALTH MATTERS AUTUMN 2023 REPORT
Stay updated
All the latest developments and changes from across the HSE
HSE National Policy for Consent in Health and Social Care Research






The HSE and Tusla are delighted to announce the publication of the latest version of the HSE National Policy for Consent in Health and Social Care Research, which has been updated to re ect the commencement of the Assisted Decision-Making (Capacity) Act 2015 as amended by the Assisted Decision-Making (Capacity)(Amendment) Act 2022.


The policy builds on the work completed in 2022 by the National Of ce for Human Rights and
Equality Policy in publishing the updated version of the HSE National Consent Policy (which is now also undergoing revision in light of the commencement of the Act).







The policy provides guidance for healthcare services hosting research, for research ethics committees in the HSE and its funded organisations, as well as for internal and external researchers who want to conduct research within the service. HM

Please find more information herehttps://hseresearch.ie/consent/ and/ or contact ResearchAndDevelopment@hse.ie

HEALTH MATTERS AUTUMN 2023 64 |
Mental Health Crisis Resolution Service Model of Care brings supports to the community

The new HSE Crisis Resolution Service Model of Care aims to provide mental health intensive supports in individuals' homes or communities as an alternative to hospital admission. It wants to provide more accessible and personalised support to individuals with mental health dif culties, empowering them on their recovery journey and offering an alternative to hospital admission when appropriate.


There are two key service components in Crisis Resolution Services:
• Crisis Resolution Teams will play a vital role by providing intensive mental health interventions and support in the patient’s home and the community as an alternative to a hospital admission. The team will use the skills of the multi-disciplinary team to assess the service user’s needs and to develop an individual care plan that supports the individual service user on their recovery journey.
• Crisis Café teams will provide an out-of-hours friendly and supportive community crisis prevention and crisis response service in the evenings and at weekends in a café style/non-clinical safe environment. The café service, Solace Café, will support individuals and their family members/carers to manage their mental health and well-being by providing clear supports and effective signposting to services.
It will be piloted across ve pilot learning sites in Community Healthcare Cavan, Donegal, Leitrim, Monaghan, Sligo, Midwest Community Healthcare, Cork Kerry Community Healthcare, South East Community Healthcare, and Community Healthcare Dublin South, Kildare and West Wicklow. There will be an independent evaluation undertaken of the pilot implementation of Crisis Resolution Service over the pilot testing phase of 18 to 24 months. HM
80% OF STAFF NOW USING NISRP

At the conclusion of the implementation of National Integrated Staff Records and Payroll (NiSRP) in the Southern region, it is a pleasure to consider what has been achieved already in 2023, said Ivan McConkey, NiSRP Programme Director. With the addition of the 18,500 employees in the South, approximately 80% of all HSE personnel and management teams nationally are now experiencing the power and benefits of this integration work.
“While the NiSRP team moves on, full steam ahead, with our colleagues in HSE West, we are very grateful and we will not forget the positive attitude, diligence and effective collaboration with us by all our colleagues in HSE South,” he said. HM
For further information about NiSRP and how to get started on HR and Payroll Self Service (if live in your area), please visit www.hse.ie/nisrp
Follow NiSRP on twitter
@NiSRP_HR

FEATURE | 65 HEALTH MATTERS AUTUMN 2023
Care pathways



Healthcare professionals across acute and community settings team up to establish new care pathways
have been approved by the Department of Health and the HSE for rollout in acute and community settings across Ireland in 2023. Of these 36 pathways, the priority for 2023 is to fully implement seven modernised care pathways for a variety of conditions including virtual fracture assessment clinics, male lower urinary tract symptoms (LUTS), continence, haematuria, paediatric eye care, medical retina concerns, and cataracts. In May and June 2023, a total of 7,932 new patients were managed within the nine sites that had these pathways up and running.
Deirdre McNamara, Director of the Strategic Programmes Of ce (SPO), Of ce of the Chief Clinical Of cer, who is leading this work, said, “The implementation of modernised care pathways is central to transforming the delivery of scheduled care services and reducing waiting lists. These new pathways will improve access time to service, enhance patient care and give
Healthcare professionals working within hospitals and community settings around the country are joining forces to deliver newly reformed or modernised scheduled care services for patients experiencing a wide range of health concerns, from impaired vision to the management of chronic disease conditions.

These new care pathways will create new points of access to healthcare for conditions with some of the longest waiting lists, ensuring that patients can be seen faster and progress through a simpli ed journey towards de nitive treatment – in many cases with fewer overall visits and without having to go to hospital.
Some 36 new modernised care pathways, which were developed by the National Clinical Programmes based on international evidence and best practice based guidelines,
7,932 IN MAY AND JUNE 2023, A TOTAL OF NEW PATIENTS WERE MANAGED WITHIN THE NINE SITES THAT HAD THESE PATHWAYS UP AND RUNNING
HEALTH MATTERS AUTUMN 2023 66 |
Liam Woods, National Director RHA Implementation; Dr Colm Henry, HSE Chief Clinical Of cer; Ewout van Ginneken, Berlin Hub Coordinator, European Observatory on Health Systems at the workshop.
patients a better experience, while alleviating pressures on hospitals.”

The new pathways are achieving these goals by embracing advances in e-health and supporting the establishment of consultant-led multi-disciplinary teams, which enable health and social care professionals and nurses to deliver advanced clinical care at the highest level of their licence. Patients who can be treated at home or in the community will now be able to avail of that option, reserving specialist consultant care for those who need it most.
In addition to improving access to care for service users, the modernised care pathways are also creating new opportunities for a wide range of healthcare professionals to work within the health service. Recruitment to ll a large number of posts is under way at hospitals and community sites across the country, with approximately 400 whole-time equivalent posts on offer at present.
Transforming health care services towards delivering more integrated care is not without its challenges. Among these are recruitment, retention and training, the need for technological infrastructure and equipment upgrades, and changes to the way data is collected and interpreted.
In May 2023, the SPO hosted an implementation workshop in the Royal College of Surgeons in Ireland, which was attended by over 160 healthcare professionals


from around the country and senior HSE leadership. The event featured talks and panel discussions with those who had already begun the work of establishing some of the new pathways, providing valuable opportunities for peer-to-peer learning and networking. Work to make all of the modernised care pathways fully operational in their respective community and hospital sites around the country is ongoing, and will continue through 2024. HM
If you would like to know more about the modernised care pathways, you can reach out to the SPO team at StrategicProgrammes.CCO@hse.ie.
| 67 HEALTH MATTERS AUTUMN 2023
Damien McCallion, HSE Chief Operating Of cer; Dr Colm Henry. HSE Chief Clinical Of cer; Ita Hegarty, Pathway Lead; Deirdre McNamara, Director Strategic Programmes; Ewout van Ginneken, Berlin Hub Coordinator; European Observatory on Health Systems; and Liam Woods, National Director RHA Implementation.
FEATURE
Dara Meldrum, Physiotherapist; Breda Kenny, Physiotherapist; Shane McMahon, Chief Audiologist; Sara Brennan, Speech and Language Therapist; and Prof Michael Walsh, National Clinical Advisor in ENT, National Clinical Programme for Surgery at the Modernised Care Pathways Implementation Workshop.
Hepatitis C home tests for thousands at risk
Almost 4,000 at-home hepatitis C testing kits have been ordered and delivered since the HSE home test service went live in April. Thousands of people at risk of hepatitis C are now able to order a test to their home, as the HSE steps up its bid to eliminate the deadly disease.
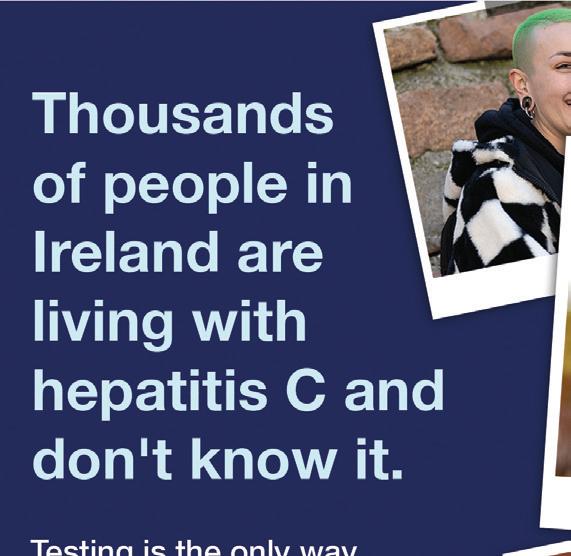
The discreet, at-home testing kits are free to order online from hse.ie/hepc as part of the HSE’s Hepatitis C Treatment Programme, which has already treated over 7,000 people, 95% of whom are now cured. The new home testing kit could help people unknowingly living with hepatitis C to get a life-saving diagnosis and treatment sooner. The new self-testing kits aim to reach people who may not be engaged with other services such as drug and alcohol support, as well as people who may have potentially been exposed to the virus in the past. HM

Patient Safety Act embeds culture of open disclosure
Being open, honest and compassionate with patients/service users or their relevant person when a patient safety incident occurs where the patient/service user was harmed is essential in our response to such events.
To help embed a culture of open disclosure across the Irish healthcare sector there have been significant developments with the Patient Safety (Notifiable Incidents and Open Disclosure) Act 2023 and the National Open Disclosure Framework.
The Act provides a legislative framework for a number of patient safety issues, specifically:
• mandatory open disclosure of a list of defined patient safety incidents that must be disclosed to the patient and/or their relevant person by law (for example where a patient died following a medication incident or a patient died following wrong site surgery).
• a requirement to report such incidents to the Health Information and Quality Authority (HIQA), Chief Inspector and/or the Mental Health Commission (MHC) using the National Incident Management System (NIMS).
• mandatory disclosure to the patient the outcome of a cancer screening review undertaken on their request. It extends HIQA’s regulatory remit to private hospitals.
• legal protection for the conduct of open disclosure in line with the legislation.
The commencement date of the Act is yet to be confirmed. The HSE has established an implementation group to oversee its implementation and make the required changes to our policies, technical system (NIMS), training, etc.
There is no change to our HSE Open Disclosure Policy for now. Regular updates will be provided. HM
HEALTH MATTERS AUTUMN 2023 68 |
Reform of Home Support Services and new Statutory Home Support Scheme






The reform of home support services and the development of a statutory home support scheme will provide equitable access to high-quality, safe, and regulated home supports for service users with assessed needs. It will also provide the standardisation and quality assurance required to support the recruitment and retention of home support care workers into this essential service. The Department of Health is establishing the new scheme to fund, license and regulate home support services.
The new regulations for home support providers will set out the minimum requirements needed to get a license to provide home supports to people. HIQA are developing corresponding National Standards for Home Support to guide providers on evidence-based, high quality, effective and consistent home support service delivery.
The HSE, as a major provider and funder of home support services nationally, is leading on preparing the health system and implementing this signi cant national change process in partnership with our key stakeholders.
Given the scale and complexity of the work required, the HSE has established a National Programme to lead on and monitor progress towards the embedding of the future home support service. Important achievements to date include extensive stakeholder engagement via workshops and established fora, a gap analysis of the existing ‘As Is’ home support service and preparations for the procurement of IT solutions.





Implementation of the new Home Support framework will continue over the next two years. It is planned that the new legislation and regulations for home support providers will be nalised by the end of 2023. HM
Controls Assurance Review Process update

The Controls Assurance Review Process (CARP) is a tool that assists the HSE in the review of the effectiveness of the organisation’s system of internal controls. It allows us to highlight the strengths of our controls environment and to identify activities which may require further improvement and support.
Final reports, including findings based on the 2022 responses and development, Action Plans were issued to each CHO, Hospital Group and Corporate Division. Progression of these action plans has been monitored over the last few months and we will continue to work with each area on this.
Following the launch of our new National Financial Regulations (NFRs), the Governance and Compliance Team has completed NFR training across all CHOs and Hospital Groups and have developed various online resources to support staff.
In addition, preparation for the 2023 CARP process has commenced. The CARP training programme will run for the month of October and early November. Training dates will be issued to CARP participants as per the eligible staff listings received from each CHO, Hospital Group and Corporate Division. HM
The 2023 CARP will open on 31st October 2023 for a six-week period. If you would like to learn more about CARP or if you have any internal control related questions, please contact Govn.Compliance@hse.ie
FEATURE | 69 HEALTH MATTERS AUTUMN 2023
Room to improve
Maternity bereavement survey fi ndings will help shape future care

National survey of maternity bereavement care in Ireland shows most parents were positive about the care they received, but some areas can still be improved.
The results of the rst National Maternity Bereavement Experience Survey have been published. It is the rst ever national survey of maternity bereavement care in Ireland asked women and their partners about the bereavement care that they received in an Irish maternity hospital or unit following a pregnancy loss or perinatal death.
The aim of the survey was to learn from the experiences of bereaved parents in order to improve the standard and quality of maternity bereavement care in Ireland. Women and their partners who experienced a second trimester miscarriage, a stillbirth or the early neonatal death of a baby in one of Ireland’s 19 maternity units or hospitals between 1 January 2019 and 31 December 2021 were invited to participate in the National Maternity Bereavement Experience Survey.
Participants shared their experiences of the care they received, from communication and information at the time of antenatal diagnosis, through to labour and birth, postnatal and bereavement care, neonatal care, investigations, discharge home, follow-up care and care in the community.
WOMEN AND PARTNERS OR SUPPORT PERSONS TOOK PART IN THE SURVEY.
The ndings show that 74% of participants rated their overall care as ‘very good’ or ‘good’, and 26% rated their care as ‘fair to poor’.
Participants praised staff for their caring and sensitive attitudes, with numerous comments mentioning
The findings show that 74% of participants rated their overall care as ‘very good’ or ‘good’, and 26% rated their care as ‘fair to poor’.
midwives and chaplaincy staff in particular. They identi ed areas where care can be improved, particularly in relation to information and support relating to grieving, physical recovery, and mental health after leaving hospital. Participants expressed a desire for dedicated spaces in hospitals for grieving parents; more consistent communication across services involved in their care; additional supports for physical and mental health; and more support for partners.
The survey showed that ‘care after birth and meeting your baby’, rated as the highestscoring stage of care. 82% of participants said that their baby was presented in a respectful and sensitive manner, and participants felt that they could spend as much time as they wanted with their baby.
The lowest-scoring stage of care was ‘discharge’, with 47% of participants saying that they were not given information about changes they might experience to their mental health before they were discharged from hospital. HM
FEATURE
655
232 IN TOTAL
HEALTH MATTERS AUTUMN 2023 70 | SURVEYS
Go-live
First go-live for IFMS, a major transformation programme for the Irish health service
The single Integrated Financial Management and Procurement System (IFMS) went live in July, as planned, for the rst of ve Implementation Groups. The rst Implementation Group included HSE East, Shared Services, the National Distribution Centre, Primary Care Reimbursement Service, National Ambulance Service, HSE National and Corporate Services, and Tusla. This rst go-live represents a signi cant milestone in what is a major transformation programme for the Irish health service. The transformation will bring about changes to our nancial management and procurement systems and processes, involving new ways of working for our staff.
Preparations for go-live involved:
• the establishment of local change networks, led by full-time local staff.
• the development of a detailed implementation plan for each service area, taking account of local operations and users. The plan covered change management, stakeholder engagement and communications, business readiness assessment, testing, end user training and data migration activities.

• the establishment of a local working group for each service area, supported by the IFMS Project Team, chaired by a senior leader sponsor and comprising mainly of nance and procurement leadership. It was tasked with the delivery of the local implementation plan. Progress was overseen by IFMS Project governance.
• the development of detailed cutover plans for each site in preparation for go-live.
To ensure a controlled start-up of the system, priority was given to key users who accessed the system from Monday, 3 July, with the balance of almost 4,000 users granted access from Tuesday, 4 July. This is the rst of ve Implementation Groups for IFMS, with Implementation Groups 2 to 5 scheduled to go live at approximately half-yearly intervals to achieve the target of having the entire HSE, and 80% of the expenditure of the Irish health service, transacted on IFMS by the end of 2025.
Hypercare Support for IG1 areas commenced on 3 July. This is a concentrated level of additional functional, technical and project support provided to users of IFMS over a de ned period post go-live, including onsite support for users on key sites. The objective is to proactively seek and identify issues so that disruption to operations is minimised by resolving any teething issues quickly. This period of Hypercare also allows for completion of knowledge transfer prior to transition to business as usual support.
Dedicated IFMS Helpdesks are in place to support HSE and Tusla staff, patients, and suppliers who are impacted by IFMS. Key lessons learned have been captured from this rst implementation so that they can be used to inform the approach to Implementation Groups 2 to 5. HM
| 71 HEALTH MATTERS AUTUMN 2023
FEATURE
Partner with patients
Ireland’s First Patient and Public Partnership Conference to be held
The HSE’s Operational Performance and Integration Directorate and the HSE National Patients’ Forum is hosting Ireland’s rst Patient and Public Partnership Conference in Dublin’s Convention Centre on 12 October 2023.
This conference, which is one of the rst of its kind, will focus on and look at how the HSE works in partnership with patients and members of the public to design and deliver person-centred care. Conference participants will explore how co-design, co-decisionmaking, co-implementation, and co-evaluation can take place. They will discuss how HSE services can partner with patients and the public to ensure they can in uence decisions on the design, delivery and evaluation of services.

There will be discussions on how this can start at the national level and lter down to the regional and local levels. Partnering with patients and the public calls for patient representatives on boards, advisory panels, strategy working groups, project teams, and hospital councils. It is about demonstrating how HSE services and staff can listen to the patient and public experience voices and how we can collaborate with those with this experience. This conference is about focusing on building better, together.
HSE National Director Operational Performance Integration Joe Ryan said, “We know that working in
partnership with patients and the public ultimately delivers better health outcomes. The HSE is fully committed to partnering with patients to ensure they can in uence decisions on the design, delivery and evaluation of health services. We know we have a way to go to achieve all of our aims but this conference is an important opportunity for discussion and debate. I am delighted this event is taking place and look forward to taking part and, ultimately, to working with colleagues on the next steps needed to realise our vision in this area.” HM

HEALTH MATTERS AUTUMN 2023 72 | FEATURE
Joe Ryan
THE NATIONAL TRAVEL AND SUBSISTENCE UNIT
The role of the National Travel and Subsistence Unit (NTS) is to review and analyse claims in line with policy, including running of reports. Where applicable, engage with employees and managers on travel and subsistence expense claims submitted through Employee Self Service (ESS) to query discrepancies and make retrospective xes.
Top tips for employees submitting travel and subsistence expense claims
• Familiarise yourself with National Financial Regulations NFRB4 https://www.hse.ie/eng/about/ who/ nance/nfr/nfr-docs.html
• All employees must have prior approval to travel.
• Ensure your Travel Privilege record is valid and that your correct vehicle details and documents are uploaded to HR and Payroll Self Service
• Submit all expense claims within one month of the expense date or at the very latest within 3 months.
• The date of your claim must accurately re ect the date the journey was taken or expense incurred.
• Start and end times must also accurately re ect the time away from home or base.
• Location travelled to, please ensure to enter the full destination travelled to.
• Purpose– You must enter a valid reason / purpose for your journey
• Upload receipts where possible.
Top tips for approvers of travel and subsistence expense claims
• To ensure an expense claim is fully compliant with NFRB4 requirements, each claim submitted for approval must accurately re ect the journey taken or expense incurred and the above tips for employees must be adhered to. As an approver of staff expense claims, please ensure each expense claim is fully compliant with NFR B4 before approving for payment.
• Expenses incurred should be as low as possible.
• As approver, you can reject a claim if you feel there is inadequate information or incorrect information submitted. When you reject a claim, you also have the opportunity to return a comment / reason for rejecting the claim to the employee. The employee can then carry out the correction required and resubmit for approval. HM
MEDICATION SAFETY
The MN-CMS Antenatal Visit (ANV) Medication Inbound Messaging Project has optimised the MN-CMS Electronic Health Record (EHR) by developing automated, clear, relevant and timely communication of medication and vaccine information between GPs and the EHR, leading to an improvement in medication safety at transitions of care.
This quality improvement initiative was achieved under the leadership of Emma Flaherty, Senior Informatics Pharmacist, and Eileen Burke, Senior Project Manager, in collaboration with hospital pharmacists, GPIT, GP vendors, the Healthlink team and Cerner.
It was built on the foundation of a previously successful pathfinding project, which enabled the bi-directional exchange of clinical information for ANV Shared Care messages between MN-CMS sites and GPs in structured electronic format, via Healthlink. The medication information has advanced from a baseline of non-standardised format and inconsistent approach from multiple GP vendor systems, to a clear and standardised format with defined headings and structure to medications, which the GP has prescribed or discontinued and vaccines administered in the previous 12 months.
Through successful implementation, the following benefits have been realised:
• Enhanced communication
• Medication Reconciliation Efficiency
• Standardised data entry
• Improved data quality and innovation
• Scalable potential
This project is a pathfinder, it is the first project, nationally, to develop a process for standardisation of medication-related information between GP systems and an EHR and it is a building block of Irish Summary Care Record development, as envisaged by Sláintecare.
This project was shortlisted for Public Sector Digital Transformation Project of the Year.
Our contact details are NTS.service@hse.ie For all NiSRP relation queries contact support.nisrp@hse.ie
| 73 HEALTH MATTERS AUTUMN 2023 FEATURES
Senior Researcher in the Department of Pathology in Hvidore, Denmark, Dr Jesper Bonde; retired Consultant Gynaecologist Prof Gráinne Flannelly; CervicalCheck Clinical Director Prof Nóirín Russell; and Business Intelligence Analyst with the National Screening Service Micheál Rourke
Annual colposcopy conference
The National Screening Service (NSS) CervicalCheck programme held its annual colposcopy conference on 12 May in Athlone, titled ‘A New Era for Colposcopy Services’.
NSS Chief Executive Fiona Murphy paid tribute “to all our nursing colleagues in screening who support our participants every day with care and compassion”.
HSE Chief Clinical Of cer Dr Colm Henry delivered the opening address, discussing the effects of the pandemic on cancer screening, and acknowledging and applauding the resilience of the CervicalCheck team.
CervicalCheck Clinical Director Professor Nóirín Russell gave an update on the programme.
Two international speakers delivered presentations on the day: Dr Jesper Bonde, a senior researcher from the Department of Pathology in Denmark presented about persistent HPV infection; and Dr Matejka Rebolj, a senior researcher with the Cancer Prevention Group at King's College London, gave a presentation on the value of including HPV self-sampling in screening.
Insights
Cork University Hospital hosted their 12th annual Child and Family Nursing Conference, ‘Sharing Insights and Empowering Excellence'. Helen Cahalane, Director of Nursing, opened the conference with a lovely welcome address. There was a very large attendance at


Conference talks of turning tide in nursing
Cork University Hospital held its Annual Nursing Conference with the theme ‘A Turning Tide: Nurses Influencing the Future’. The keynote speakers captured this theme by sharing their insights with the delegates. Geraldine Cunningham, Organisational Development Consultant, described how to influence a better future for nurses with kindness and compassion to the fore; Dr Jolanta Burke, RCSI, demonstrated how nurses can flourish even in challenging environments; and Sheila McClelland, NMBI, outlined how regulation and nursing standards can guide this pathway into the future.
Nurses in a diverse number of roles presented initiatives being implemented nationally across all disciplines.
the conference which included children’s nurses and allied health professionals from around Ireland.
Keynote speakers included Professor Donal O’Shea, HSE National Lead for Management of Obesity who presented on the Model of Care, sharing new
HEALTH MATTERS AUTUMN 2023 74 |
EVENTS
Siobhan Scanlon, ADON CUH; Susan Jacob, CNM2, CUH; Sheila McClelland, CEO NMBI; Sinead Favier, Paediatric CPC Children’s/General Integrated Programme; Helen Cahalane, Director of Nursing CUH; Ann Marie Galvin, ADON Nurse Practice Development Coordinator, CUH.
shared at child and family conference
Healthy Ireland conference
‘The Time is Now – Act today to shape a Healthier Tomorrow’ was the theme of the rst Healthy Ireland conference held in The Convention Centre, Dublin recently.

Sarah McCormack, HSE National Lead for Healthy Ireland, welcomed the over 400 delegates, and spoke of how this conference was continuing the implementation of the Healthy Ireland Framework and how each of us can play a signi cance role in building healthier environments and helping people to adopt healthy behaviours.
A highlight of the conference was the launch of the Health Services Healthy Ireland Implementation Plan 2023 – 2027 by HSE CEO Bernard Gloster. He welcomed the plan seeing it as another key step forward for achieving the goals of Healthy Ireland while recognising the challenges that it will bring to achieve its implementation. He asked for a united effort from all to play their part in its implementation and to unite in one year to demonstrate the achievements in that rst year of implementation.
A certi cate was presented to the HSE for the planting of 36 trees the calculated number of trees to offset the conference carbon emissions.
Letterkenny staff showcase their talents at variety performance
The very talented staff of Letterkenny University Hospital hosted a variety show at An Grianán Theatre in May. The concert brought together the best of LUH’s actors, musicians, performers, singers and dancers for a night of entertainment and laughs. The famous LUH choir led by renowned choral director Veronica Mc Carron opened and closed the concert. The staff variety show is a long-standing tradition in Letterkenny but was on pause for the last four years due to the pandemic and staff were delighted to hit the stage again.
Throughout the two nights nearly €7,000 was raised for charity and cheques were recently presented to representatives of the various organisations involved; Donegal Down Syndrome was presented with €2,922, Féilecáin, the Stillbirth and Neonatal Death Association of Ireland received €2,922 and the Friends of LUH were presented with €1,060.
Members of LUH choir and Hospital Show Committee with representatives from Friends of LUH, Féilecáin and Donegal Down Syndrome

insights in healthcare weight management practices; and Dr Eoin McNamara, Disability, Integration and Youth Research Analyst, who shared interesting acumens from the Growing up in Ireland Study and the trends in physical activity and adolescence to adulthood
screen time behaviours. Clinical presentations throughout the day validated excellent leadership and teamwork in children’s nursing in our Health Service, demonstrated by wonderful nurse led innovations.
Poster presentations on the
day provided an excellent opportunity for attendees to view initiatives which incorporated the conference theme, and the winning poster was awarded to Sinead Maher, CNS Sexual Assault Forensic Examiner, South In rmary Victoria University Hospital.
| 75 HEALTH MATTERS AUTUMN 2023 EVENTS
CHO DNCC Health Promotion and Improvement Of cers also found the event useful for networking and exploring the barriers and opportunities to promote and implement this key chronic disease prevention programme. To avail of the online training go to hseland. ie and log on the makingeverycontactcount.ie to get details of your local MECC Programme Lead for workshop information
A Making Every Contact Count (MECC)
Champions Event was organised by Community Healthcare Organisation Dublin North City and County (CHO DNCC) recently.
Amongst the nine recommendations in the Making MECC Work research to enhance the implementation of MECC is to have local Champions to model best practice and share experiences. This timely event was a huge success with 29 out of 35 Champions recruited attending on the day representing all 12 CHOs.
Brid Greenan, MECC Programme Lead for CHO DNCC, commended the "great enthusiasm on the day from all attendees, with one Champion coming straight from the airport after their holiday in South Africa.”
The aim of the event was to promote, support and mobilise the implementation of Making Every Contact Count - our key chronic disease prevention programme. It was an opportunity for new Champions to hear how this key priority programme started in North Dublin Mental Health Services.


Connecting skilled talent at Construction Jobs Expo
There will be a follow up webinar on Monday, 16 October for HSE staff. This time the webinar will focus speci cally on menopause and our mental health. To nd out more email healthpromotioncheast@ hse.ie or visit our Twitter account @CH6East.
Let’s talk about the menopause
HSE Community Healthcare East Health and Wellbeing Head of Service, Aisling Heffernan with Loretta Dignam from the Menopause Hub pictured with the Community Healthcare East Health and Wellbeing's Menopause Working Group.
Health and Wellbeing Community Healthcare East hosted a webinar for staff around the topic of menopause. Loretta Dignam from the Menopause Hub presented the webinar. The aim of the event was to begin to raise awareness of the topic, and to break down the taboos that surround menopause; thus providing a more supportive environment for those experiencing menopause. This introductory webinar covered a vast range of information for staff. Loretta shared tips and resources for navigating this challenging and transitional stage of life; including what to expect, symptoms and what you can do to alleviate some of those symptoms. Loretta also addressed the myths and taboos around menopause. A recorded version of the webinar is available on our Community Healthcare East YouTube page https://youtu.be/jngPWBB-iIA
HSE Capital and Estates is committed to creating a high quality physical environment that will enhance wellness for patients, service users and staff wellbeing – and as a result are always looking for the most highly skilled workers in the industry.
The recent Construction Jobs Expo in Dublin’s RDS was a unique, one-day event focused on connecting skilled talent with employers seeking to ll key job vacancies. HSE Capital and Estates had a strong presence on the day, alongside other industry
HEALTH MATTERS AUTUMN 2023 76 | EVENTS
‘One conversation really can change a life’
HSE National Midwifery Conference

Midwives from around the country came together in Dublin for the second National Midwifery Conference co-hosted by the Of ce of the Nursing and Midwifery Services Director (ONMSD) and the National Women’s and Infants Health Programme (NWIHP).
The conference encompassed an ‘All Ireland’ approach with the theme ‘Honouring midwives’ crucial care contribution to mothers and newborns’. The atmosphere was one of celebration and acknowledgement of the key role that midwives have in providing safe, highquality care to mothers and babies. Over 170 attendees were treated to a programme of renowned international, national and local speakers with topics spanning global midwifery, innovation, workforce, student midwife experiences and self-care.
A key theme for discussion at the conference was progress made in relation to Ireland’s National Maternity Strategy (2016-2026).
The range of topics on the programme also included:reducing midwife burnout at organisational level - midwives need time, space and a positive workplace culture;midwifery students’ experiences of their clinical internship placement during the COVID-19 pandemic in Ireland; breastfeeding snakes and ladders; and NWIHP update of progress and projects.
National Education Day for staff supporting self-harm programme
Mental health teams from across the HSE that are implementing the National Clinical Programme for Self-Harm and Suicide-related Ideation in the emergency departments and across primary care attended the National Education Day.
The event was hosted by the NCPSHI, HSE and was the first in-person event for the programme since the pandemic, with over 80 professionals attending.
leaders. Attendees were able to discuss employment opportunities with Dorota Nieznanska, Director of Estate, Ireland East Hospital Group and Michael Bermingham, Assistant National Director, HSE Capital Property, HSE Capital and
Further details of the programme and the revised model of care 2022 can be accessed at https://www.hse. ie/eng/about/ who/cspd/ncps/ self-harm-suiciderelated-ideation/
Estates, along with other senior members of the team about the great variety of roles available within HSE Capital and Estates. Several contacts were made which will hopefully result in the further strengthening of the HSE Capital and Estates team.
The education day promoted the programme’s key pillars; that people who present to the health service following self-harm or with suicide-related ideation should receive brief interventions in the form of empathic, validating, compassionate and traumainformed responses; a timely expert biopsychosocial assessment and intervention, including a written emergency safety plan and follow up and linkage to next appropriate care. Everyone that attended was eager to learn and share knowledge about the topics that were identified for the day.
| 77 HEALTH MATTERS AUTUMN 2023 EVENTS
Margaret Quigley, National Lead for Midwifery ONMSD; Clare Kennedy, Project Of cer, NWIHP; Dawn Johnston, Director of Midwifery, NMBI; Angela Dunne National Lead Midwife, NWIHP.
SPOTLIGHT ON
Health and wellbeing
Hospital garden club partners with Sligo Leader and the Organic Centre
Sligo University Hospital (SUH) has partnered with Sligo Leader and the Organic Centre to introduce a year-long Garden Project involving some minor gardening work throughout the hospital. This project is part of the hospital’s Green Campus Programme and will focus on increasing biodiversity on the site as well as enhancing outdoor spaces at the hospital.
This project is one of a number of initiatives undertaken by the hospital’s Green Campus Committee. This project in SUH is already delivering bene ts to the participants, staff, patients and visitors who are enjoying the beautiful green areas in the hospital.
It consists of approximately 15 community
Traveller Men’s Health Day
Traveller Men’s Health Day, which took place recently, focused around a soccer tournament with teams of Traveller and Roma men from around the country competing. This was the first year that the HSE entered a team, and although they didn’t win, a very enjoyable day was had by all.

The day is a cross-community initiative that brings various healthcare support services together to engage with the Traveller community to help break down the stigma around talking about physical and mental health.
“Mental health is a huge issue for Traveller men with a suicide rate that is seven times
volunteers. The volunteers undertake various gardening activities such as planting, weeding, pruning, and preparing planter boxes for winter. The project is funded by the HSE’s Climate Action and Sustainability Of ce and Sligo Leader Partnership Company. HM


higher the national average,” said Pa Reilly, Eastern Region, Traveller Health Unit Mental Health Initiative.
“Creating spaces where Traveller men can talk about mental health and move away from any stigma is crucial.” HM
HEALTH MATTERS AUTUMN 2023 78 |
The HSE football team at the Traveller Men’s Health Day tournament
Men's Health Week gets moo-ving
There was more than cattle on offer at Kenmare and Caherciveen Marts this June when they hosted free men's health awareness days, as part of Men's Health Week. There were also free health checks on offer at local pharmacies in Caherciveen, Kenmare, Waterville and Sneem.

Over 155 men attended the free mart events and health checks, organised by the Health Promotion and Improvement Department in the HSE, in partnership with local community groups.

Project lead Michelle Foley, Health Promotion and Improvement Of cer with the HSE, said, “This was a wonderful opportunity for men in South Kerry to meet with a range of health and community professionals in a one-stop-shop. The focus of this event was health awareness, prevention and increasing access to health and community services.” HM
Recovery in Colour boosting creativity and mental health
Recovery in Colour is a creativity and mental health recovery education course co-produced by HSE Community Healthcare East and Advancing Recovery in Community Healthcare East Services (ARCHES) Recovery College, and delivered in Clonskeagh Hospital Dublin and Bray Primary Care Centre, Wicklow.

The course supports people to use ‘art journaling’ - creating a personal visual journal, painting, drawing, colour and collageto explore the meaning of mental health recovery, self-care and to help articulate future plans and ambitions.

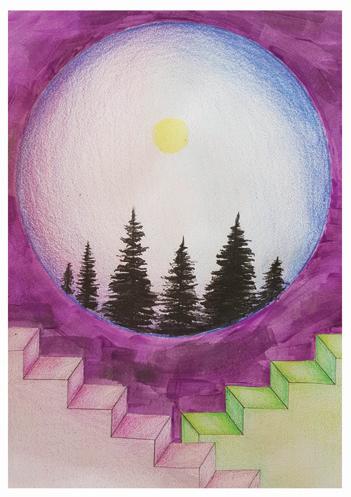

The co-production of the course was led by Recovery Education Facilitator, Cathy Doyle who developed the idea for Recovery in Colour from her own mental health lived experience.
Feedback from ARCHES Recovery College students who have participated in the course suggests that Recovery in Colour helps people in their own recovery journey by creating a safe space to discuss and make sense of psychological distress, providing an atmosphere of encouragement and respect and making people feel at home and valued. HM
| 79 HEALTH MATTERS AUTUMN 2023
Recovery in Colour artwork by ARCHES Recovery College students
A WAY TO
Unwind
MAKE SELF-CARE A PRIORITY DURING THE WINTER MONTHS
As the shorter, darker days come in, it is easy to stop doing the things that can boost our health and wellbeing and push them off until the spring comes around again. With good mental health, we feel happier, we enjoy life more and we look forward to the future. We then become more resilient and able to cope with the challenges that life can throw at. That is all the more important in the long winter months. Self-care means prioritising taking care of ourselves every day in different ways and we can do that by building self-care into our day and creating our own self-care toolkit.
Good self-care habits
• Get active - Any kind of movement that makes you physically active every day such as walking or gardening
• Be balanced – Have a look at what you eat, your consumption of alcohol and tobacco. Maybe try to eat more fruit and vegetables or cut back on the number of drinks you may have.
• Be kind – It is important how we treat ourselves. We should be kind to ourselves when we make mistakes or mess up and understand that you don’t have to be perfect.
• Rediscover old hobbies or interests - They give us time out from the routine of day-to-day life. Rediscover old interests.
• Manage your stress - A lot of us experience stress in different ways and cope with it in different ways. Ask for help when you need it. You can’t do everything alone. Look for the support of family and friends, or sometimes it may be professional help. It might just be asking someone to give you a hand and knowing when you are becoming overwhelmed.
The Minding Your Wellbeing programme has been adapted from a face-to-face programme into a series of free online videos. The programme consists of five 20-minute video sessions which are available via yourmentalhealth.ie. The content focuses on: practicing self-care; understanding our thoughts; exploring emotions; building positive relationships; and improving resilience; all of which are important for mental health and wellbeing.
• Get good sleep – Get into a regular bedtime routine so your body gets used to learning how to relax and unwind and you get a better night’s sleep.
Tips for self-care
• Pause. Pause before you say yes. You may need to say no. It is a really valuable tool to have in your self-care toolkit.
• Make a list but keep it short. If it is too long, it can seem overwhelming and put you off doing anything.
• Praise yourself. tell yourself well done if you did something dif cult.
• Don’t put things off, get the things you want to do the least out of the way rst.
• Take short breaks.phone a friend, take a quick walk, stretch at the desk, have a cup of tea. This will all give your mood a boost until you have a proper break.
Self-care at work
COVID-19 has changed a lot for many of us, whether we are working from home, in the office or on the frontline. Maintaining social distancing has made it hard to ‘connect with others’ which is a key self-care strategy. Managing stress has been more difficult as staff are re-deployed and often working in highly stressful situations. However, if ever there was a time for managers to promote good self-care among teams it is now.
Two important ways to do this are:
• Be a good role model yourself by demonstrating good self-care
• Adding it as a standing agenda item at staff and individual supervision meetings. Ask staff how they’re doing with their self-care and genuinely listen to their response.
HEALTH MATTERS AUTUMN 2023 80 |
HealthIRL is a secure domain that allows users to:





• Access Microsoft Teams, Office 365 and cloud systems
• Login from any location on any HSE device
• Keep the same login if you relocate between HSE regions

If you have not been migrated yet contact:

Healthirl.migration@hse.ie








Flu & COVID-19 vaccines Have you topped up your winter protection yet? Your flu and COVID-19 vaccines help protect you from serious illness. So give your immune system a top-up this winter. See what vaccines are recommended and book your appointment today. Visit hse.ie Call HSELive 1800 700 700
























































































































































































 Sarah Gleeson advanced nurse practitioner in inflammatory bowel disease, Mercy University Hospital, Cork
Sarah Gleeson advanced nurse practitioner in inflammatory bowel disease, Mercy University Hospital, Cork