The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.

Implemented by: Partner:






The project is being implemented with the support of UNICEF Ukraine and with financial support from the Government of Norway.

Implemented by: Partner:





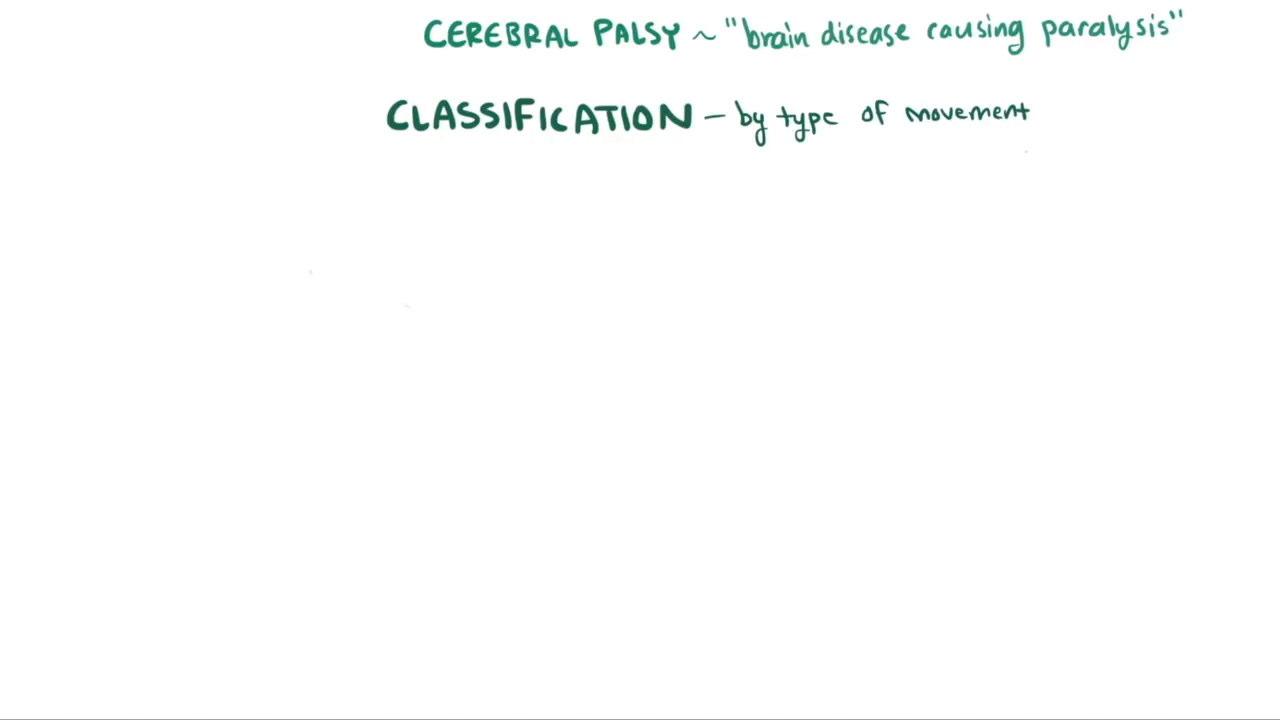
Agroup of permanent disorders in the development of movement and posture causing activity limitation, attributable to a permanent (non-progressive) injury that occurred in the developing fetal, neonatal, or infant brain. The motor disorders of CP are often accompanied by sensory, perceptual, cognitive, communication, behavioral disorders, epilepsy, and secondary musculoskeletal problems. (Rosenbaum et al., 2006).
Main limitations of the definition:
It does not refer to the pathogenesis of brain damage. The definition of non-progressive damage is hypothetical. The age limit is ambiguous (covering approximately 3 years).
The lower severity limit for diagnosing Cerebral Palsy (PCI) is not defined.










Spinal cord injury
Multiple Sclerosis
Cerebral palsy
Stroke
Brain or head trauma
Amyotrophic lateral sclerosis
Hereditary spastic paraplegias
Metabolic diseases (adrenoleukodystrophy, phenylketonuria, krabbe disease )

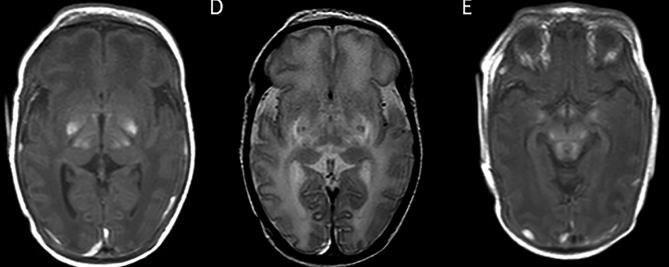
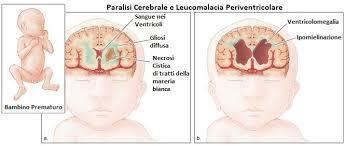
Germinal matrix-intraventricular haemorrhage (GMH-IVH)


Focal infarction




White matter injury
Global injury from hypoxic-ischaemic encephalopathy (HIE)












Quadriplegia
Involvement of all four limbs
Difficult somatic growth Mental retardation and associated disorders

Unilateral involvement Reduced motor repertoire on one side Presence of "Synergies"
Predominant involvement of lower limbs Difficulty with balance control Upper limbs generally functional





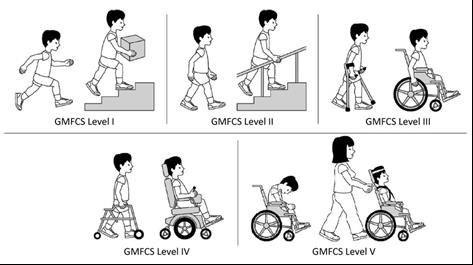
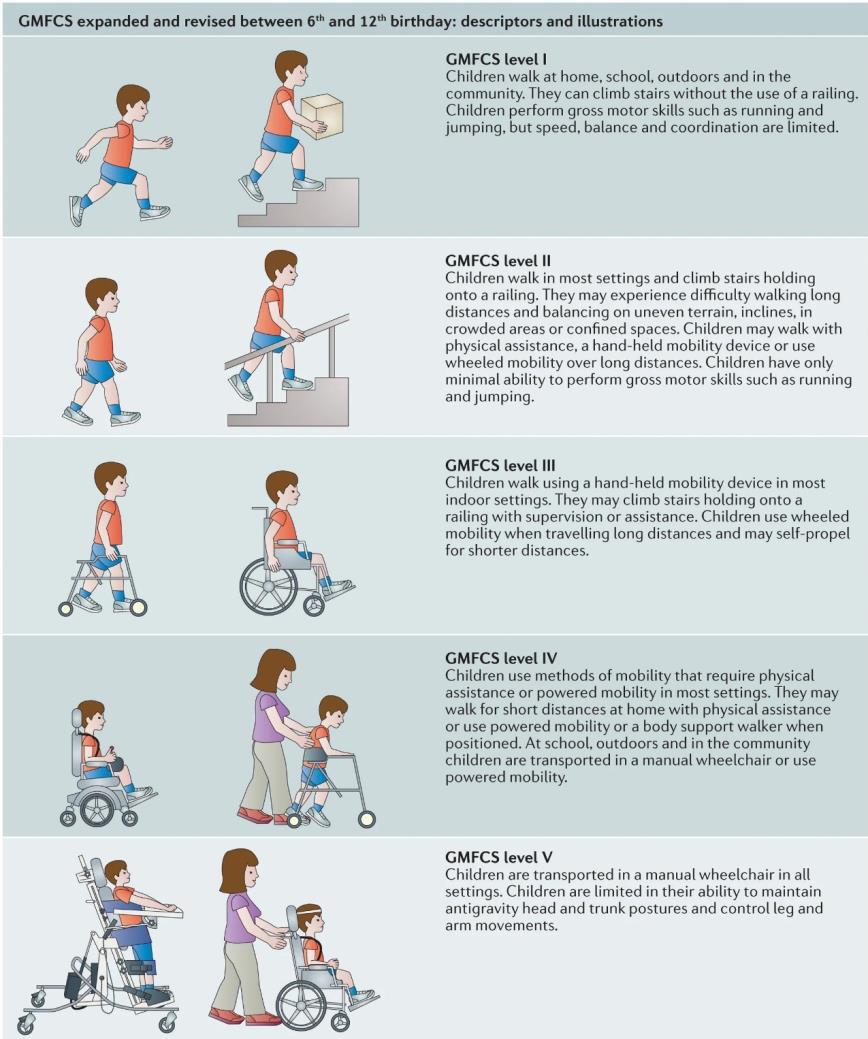
The Gross Motor Function Classification System (GMFCS) has become the gold standard to classify motor function in children with cerebral palsy




- stiff muscles (spasticity)
- uncontrollable movements (dyskinesia)
- poor coordination (ataxia)
- Mixed
- Spasticity is the most common movement disorder, affecting approximately 80% of children with cerebral palsy

CP (Cerebral Palsy): complex pathology

"...assuming it is possible, even temporarily, to eliminate antigravity hypertonia (spasticity), the child affected by CP would still appear to us with a seemingly only motor disorder, expressible as clumsiness or awkwardness. In truth, this "executive" disorder is nothing more than the result of the sum or interference of various "executive" and "cognitive" disorders at a high level of integration, similar to apraxia and agnosia."
G.SABBADINI - M.M. PIERRO
Even if a limb appears healthy, there may be a difficulty in controlling movement.
"Therefore, competence in manipulation does not always mean a secure acquisition of good autonomy, because the results achievable through good motor control may remain unattainable due to the presence of dyspraxic and disperceptive problems.
“
E. FEDRIZZI
•Alterations present in specific competencies and abilities (disorder profile)
•Developmental level achieved in various competencies (developmental profile)
•Compensation strategies activated
•Communication and relational competencies
•Potential area of development

NATURAL HISTORY
COMPLEXITY
DEVELOPMENT APPOINTMENTS
SEMEIOTICS
ATYPICAL DEVELOPMENT
RESOURCES LEARNING MODIFIABILITY
DEVELOPMENT PROFILE
TYPICAL DEVELOPMENT
A "developmental appointment" refers to a scheduled meeting or visit with a healthcare professional (such as a pediatrician, developmental specialist, or therapist) to assess and monitor a child's development. These appointments are crucial for:
•Tracking progress: Observing a child's growth and milestone attainment.
•Early identification: Detecting any potential delays or disorders in their physical, cognitive, social, or emotional development.
•Intervention and support: Planning and initiating appropriate interventions or therapies if developmental concerns are identified.
Milestones, in the context of a "developmental appointment" and the broader evaluation of a child's development, refer to specific functional skills or agespecific tasks that most children can do by a certain age.
These milestones cover various areas of development, including:
•Gross motor skills: Sitting, crawling, walking, running.
•Fine motor skills: Picking up small objects, drawing, using utensils.
•Language/communication skills: Babbling, speaking first words, forming sentences, understanding instructions.
•Cognitive skills: Problem-solving, learning colors/shapes, imaginative play.
•Social/emotional skills: Smiling, making eye contact, playing with others, expressing emotions.
Developmental appointments often involve checking a child's progress against these milestones to ensure they are developing typically and to identify any potential delays that might require further assessment or intervention.
•If a function is not acquired within the time period during which it is emerging, that function will be stably altered.
•The loss of the functional appointment leads to greater difficulty and requires longer acquisition times.
















Facilitate and promote, through the use of specific techniques, the development of competencies that allow the child to achieve maximum autonomy and socialization.
The success of the treatment is based on a realistic and achievable definition of objectives.


Objectives, evaluation, and framing

Functions in development
Different age groups

Heterogeneous clinical pictures


Disorders associated with other developmental areas

Disorders that stabilize quickly

Disorders that change over time
This transformation concerns both functional deficits and the atypical behaviors that result from them
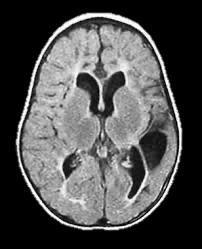

The study of brain connectivity can produce biomarkers of damage and functional recovery in Cerebral Palsy (CP).
Patients with spastic and dystonic CP have different structural connectivity maps.



Patients with CP show different motor functional connectivity maps, with reduced interthalamic connectivity.
Functional recovery following rehabilitation shows correlations with functional connectivity [Bleyenheufl et al., 2015] and structural connectivity [Eglander et al., 2015].


Kleim JA, Jones TA (2008)
J Speech Language Hearing Research, 51:225-239
Neural plasticity is the capability of the cerebral cortex to alter its functional organization as a result of experience
Nudo RJ (2006) J Am Soc Exp NeuroTher, 3:420-427

✓ Enriched environment The timing of rehabilitation intervention is fundamental - Early treatment Training improves motor performance Training intensity is a key element for rehabilitation effectiveness Plasticity induction requires sufficient repetition Training experience must be sufficiently salient Continued practice of motor skills is fundamental for maintaining optimal motor performance Taskspecific training can lead to functional recovery even in untrained functions Training the less affected side is maladaptive for the outcome
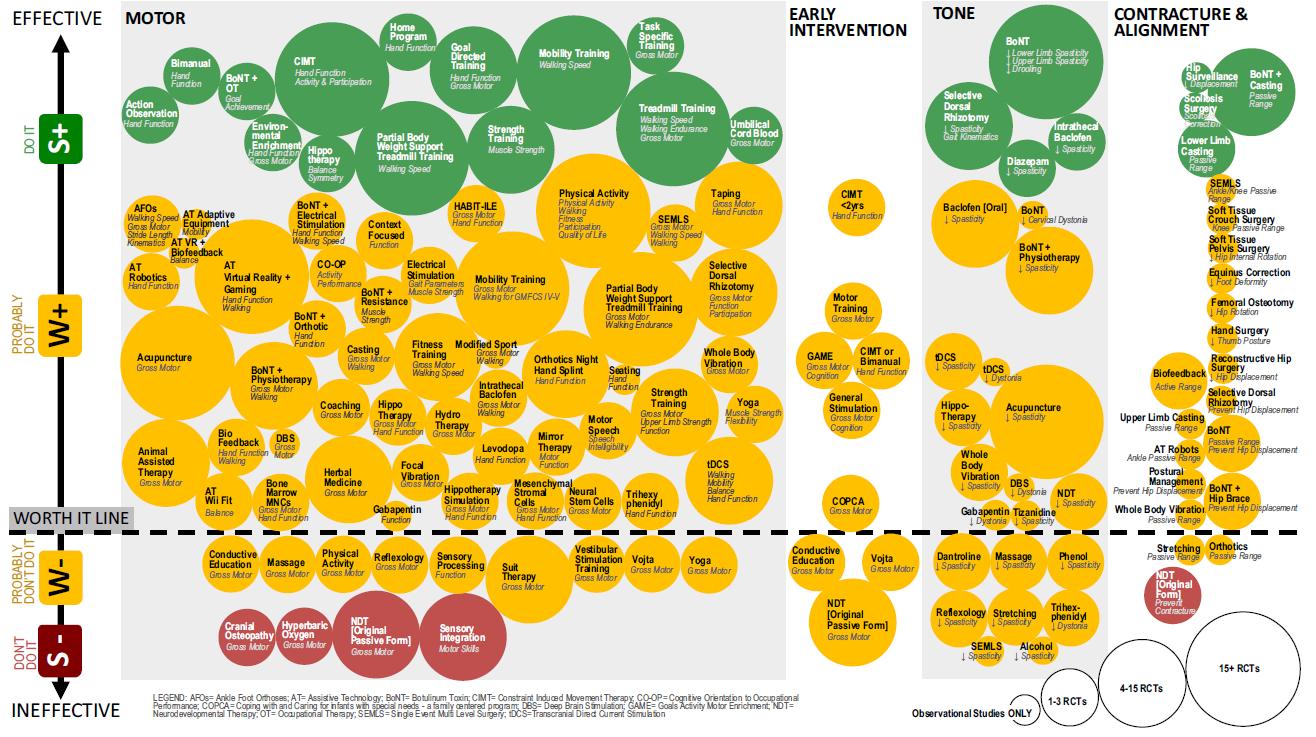
Iona Novak. Evidence-Based Diagnosis, Health Care, and Rehabilitation for Children With Cerebral Palsy.
J Child Neurol 2014 29: 1141.
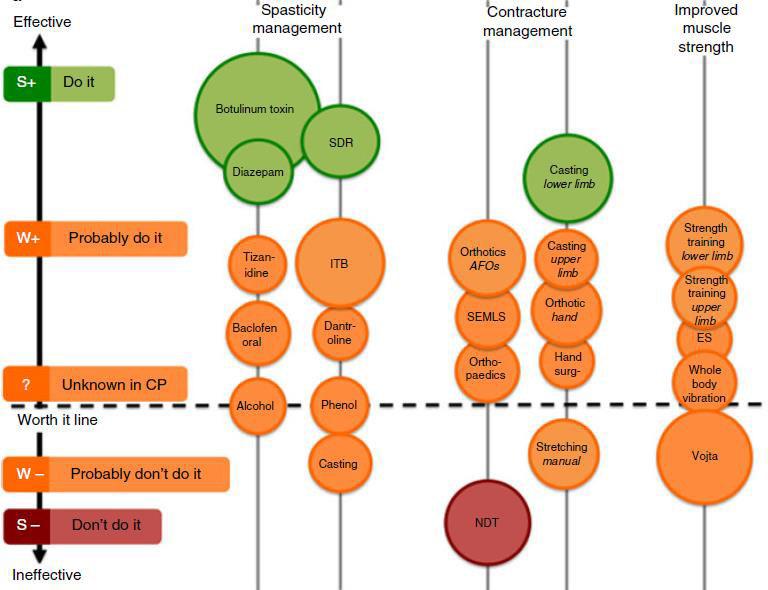
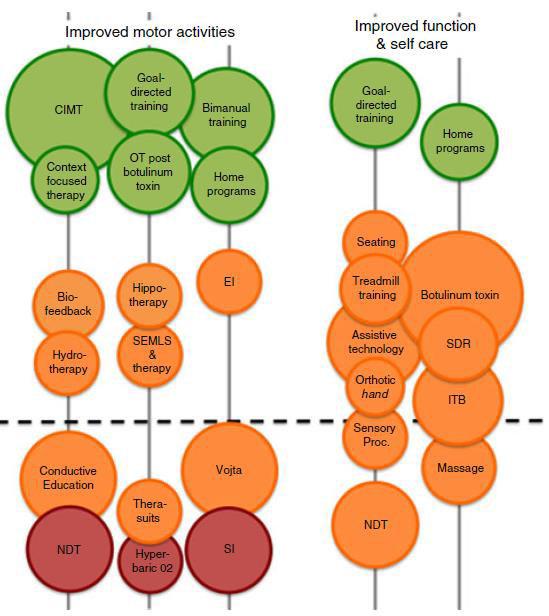


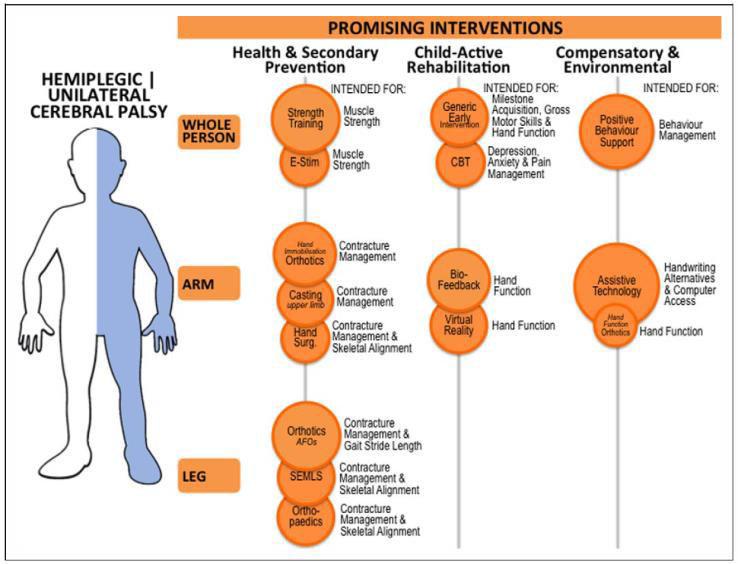
Iona Novak. Evidence-Based Diagnosis, Health Care, and Rehabilitation for Children With Cerebral Palsy. J Child Neurol 2014 29: 1141.
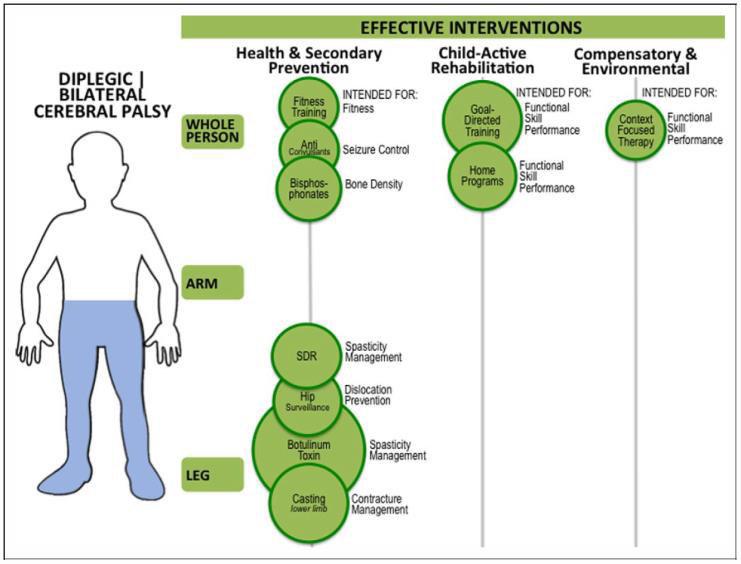
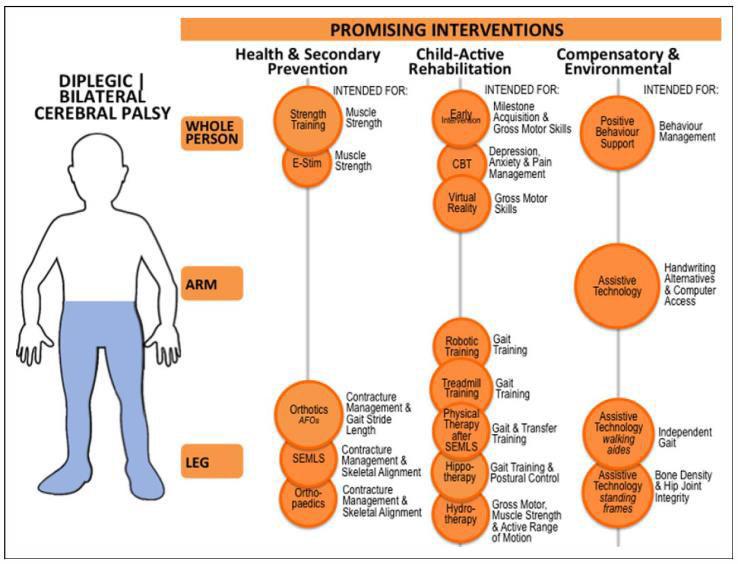
Iona Novak. Evidence-Based Diagnosis, Health Care, and Rehabilitation for Children With Cerebral Palsy. J Child Neurol 2014 29: 1141.

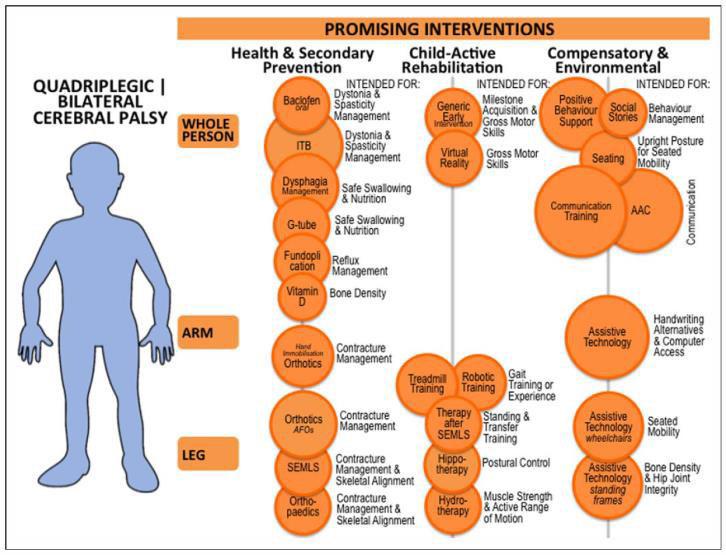
Iona Novak. Evidence-Based Diagnosis, Health Care, and Rehabilitation for Children With Cerebral Palsy. J Child Neurol 2014 29: 1141.







































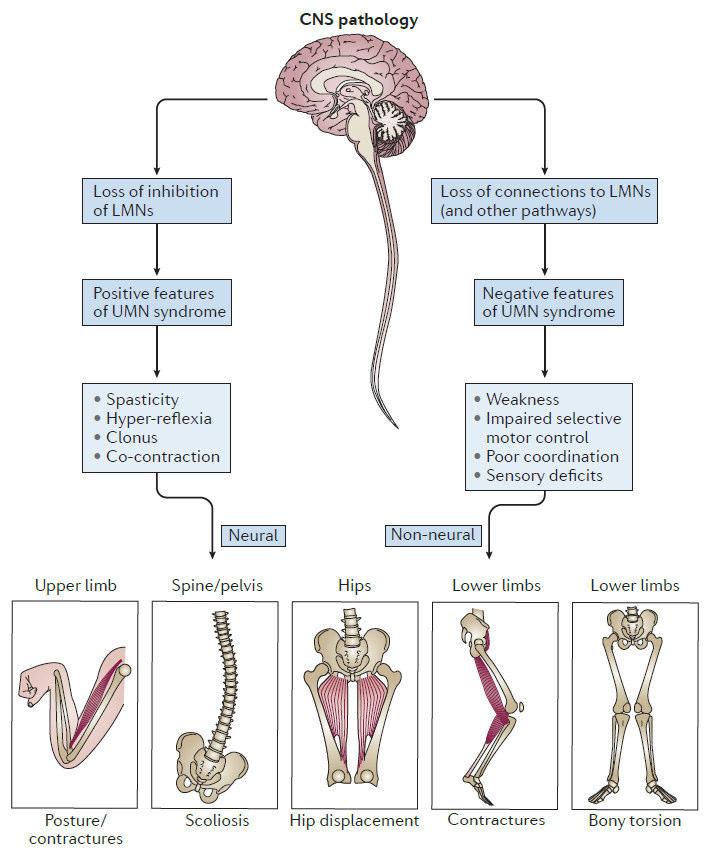
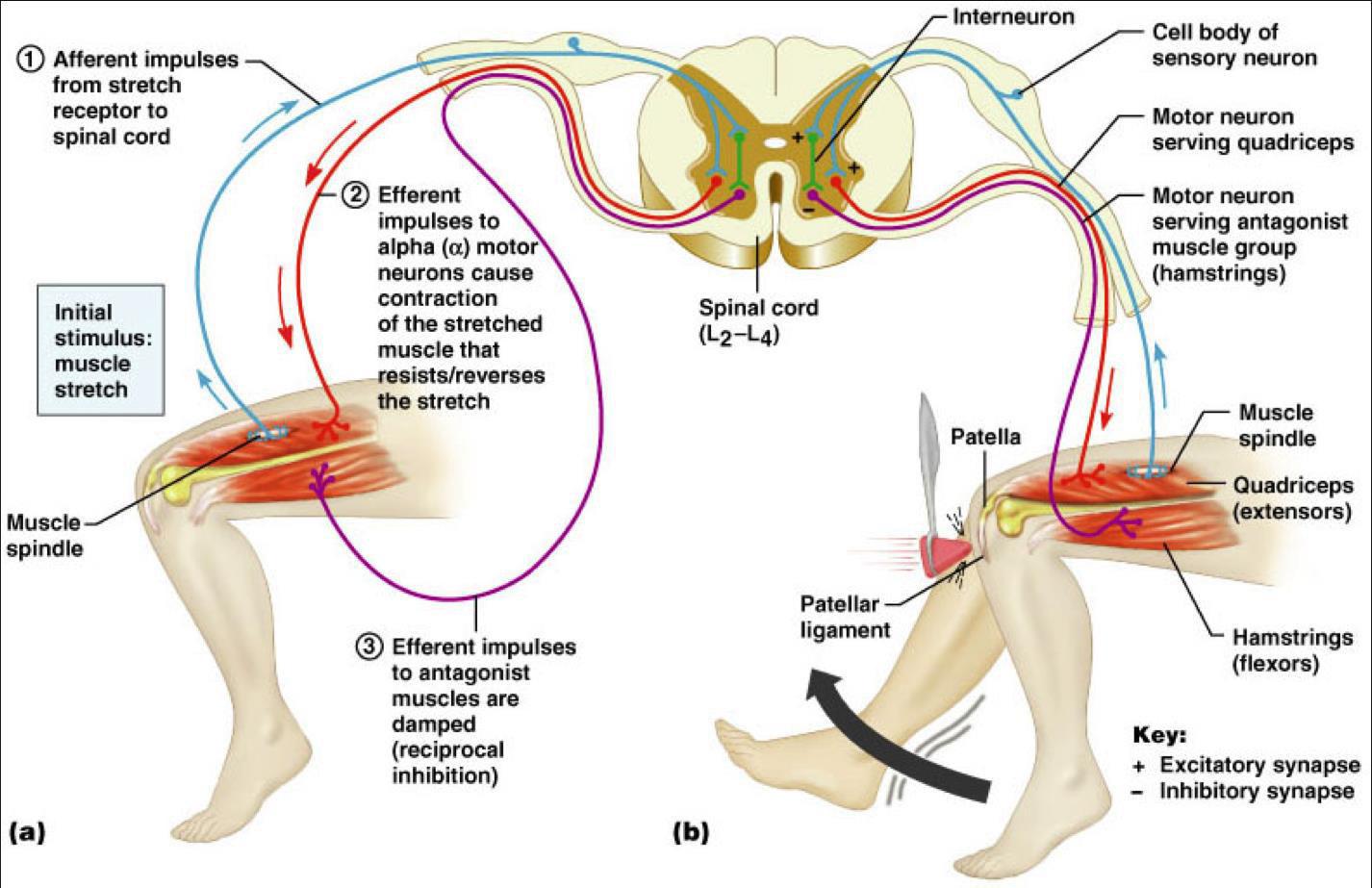
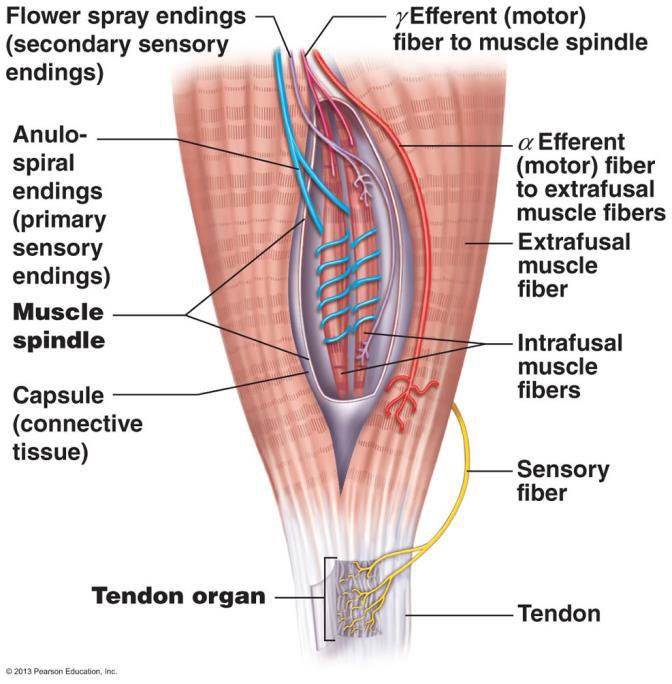
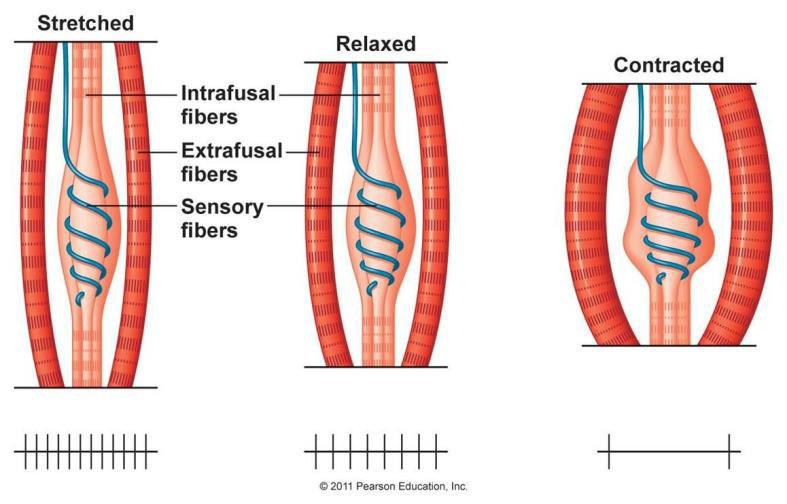
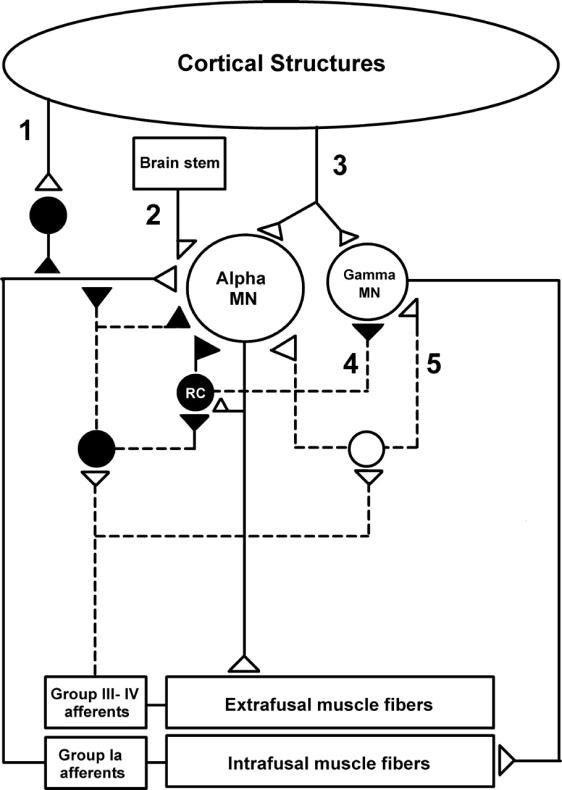
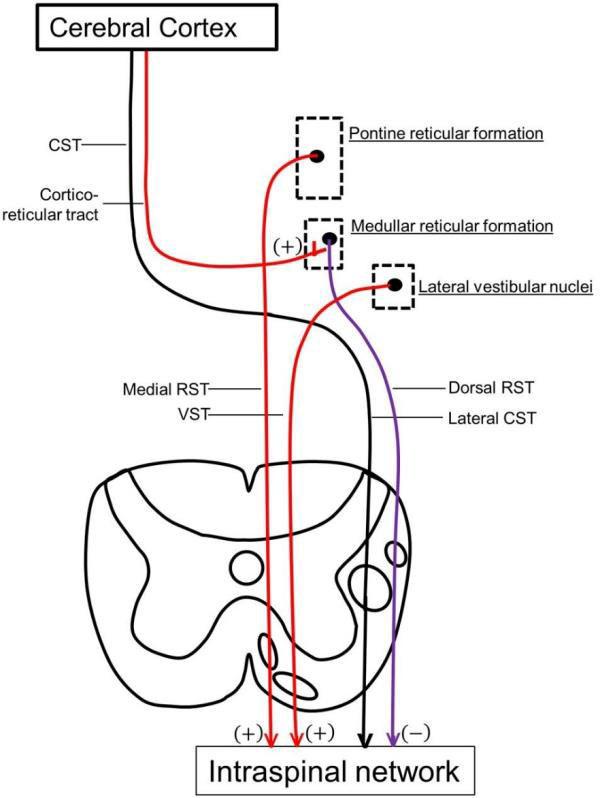
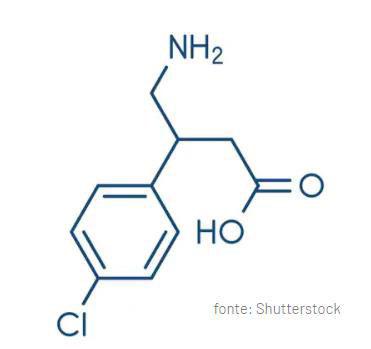
Spasticity: a motor disorder characterized by a velocity dependent increase in the tonic stretch reflexes (muscle tone) with exaggerated tendon jerks, resulting from hyperexcitability of the stretch reflexes as one component of the upper motor neuron (UMN) syndrome (Lance, 1980).
Dystonia: sustained or repetitive involuntary muscle contractions that produce abnormal but patterned postures and movements of different parts of the body.
Contractures and spasms: changes in passive components of muscle or muscle activity elicited by sensory triggers.

UMN: upper motor neurons
LMN: lower motor neurons





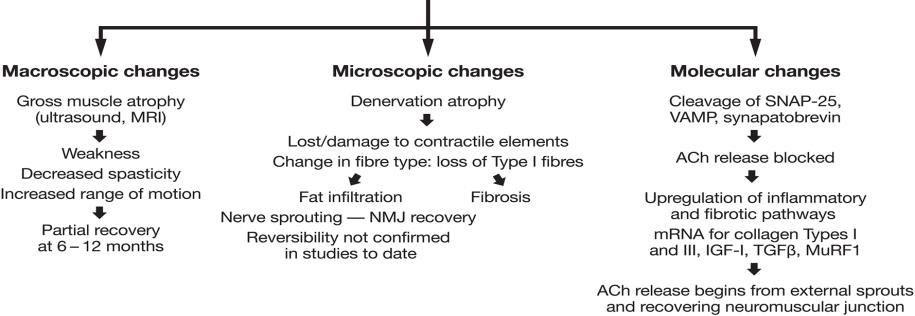
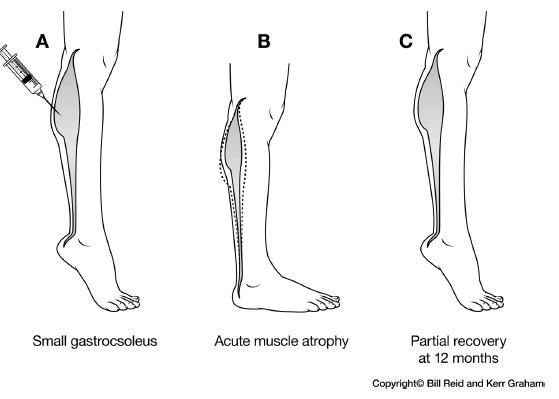
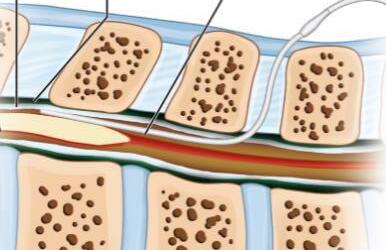
Muscles from children with CP are shorter and smaller and contain fibres of reduced diameter, which leads to a muscle with smaller forcegenerating area, partially explains decreased strength.

Sarcomeres are added in series as the bone grows, and therefore the ankle retains full range of motion


In a child with CP that sarcomeres are not added in series and thus, as the bone grows, the ankle is forced into plantar flexion

*Reduced muscle volume is observed in the spastic muscles of children with cerebral palsy (CP) as early as 15 months of age.
*Muscle thickness and cross-sectional area are decreased →→ reduced muscle production capacity →→ reduced strength.
The muscle-tendon unit length is compromised →→ reduced strength.
*Muscle weakness, impaired ability to generate or maintain force levels →→ gait deficit. Muscle weakness →→ reduced range of motion (ROM) of the hip, knee, and ankle →→ unfavorable levers for walking.

Co-activation of antagonists is more pronounced in patients with CP →→ necessary for joint stability →→ increased joint stiffness.
The stiffness of muscles and connective tissue increases due to spasticity →→ changes in the mechanical and biological properties of the muscle, stiffness of myofibers →→ alter the quantity and orientation of connective tissue structures.
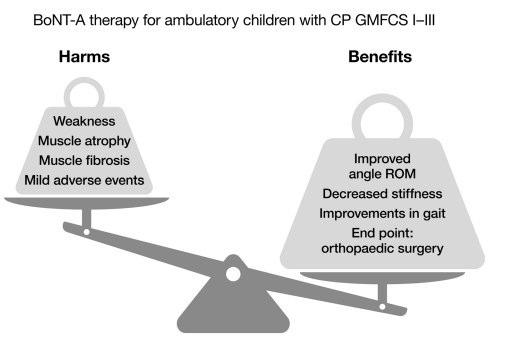
Patient Selection and Treatment Timing are Critical
I. Patient Selection:
Careful selection of the right patient ensures that botulinum toxin is used effectively and safely, maximizing benefits and minimizing potential risks.
Diagnosis and Indication:
Accurate Diagnosis: The patient must have a confirmed diagnosis for which botulinum toxin is an approved or an evidence-based treatment (e.g., spasticity, dystonia, chronic migraine, hyperhidrosis). Misdiagnosis can lead to ineffective treatment and wasted resources.
Type of Spasticity/Dystonia: Botulinum toxin is most effective for focal or multifocal spasticity/dystonia. It's less suitable for generalized spasticity, which might require oral medications or intrathecal baclofen.
Absence of Fixed Contractures: While botulinum toxin can prevent or reduce the progression of contractures, it generally cannot reverse established fixed contractures or structural changes in muscles, joints, or bones. In such cases, orthopedic surgery might be a more appropriate intervention.
Functional Goals: The patient and care team should have clear, realistic, and measurable functional goals. Botulinum toxin is a tool to facilitate functional improvement (e.g., improving gait, enhancing hygiene, reducing pain, facilitating dressing) rather than a standalone cure.

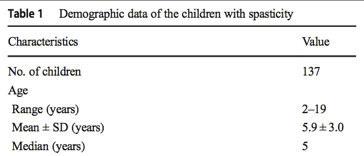
Treatment is recommended between 2 and 5 years of age, when motor development is evolving and motor patterns are modifiable →→ possibility of altering the disease course.
Improve motor function impaired by hypertonia.
Leverage the induced effect on the reorganization of nerve signals in untreated muscles.Improve sitting posture. Facilitate orthosis use. Prevent compensations and musculotendinous retractions. Reduce pain.
Improve personal hygiene.Delay the need for functional orthopedic surgery.

of focal spasticity in patients > 2 years of age (use in children < 2 years is off-label).Can also be used for focal dystonias.







• Lack or Reduction of Effectiveness:

• Development of Intolerable or Unexpected Side Effects

Disease Progression or Change in Clinical Picture
Need for a Multimodal Approach




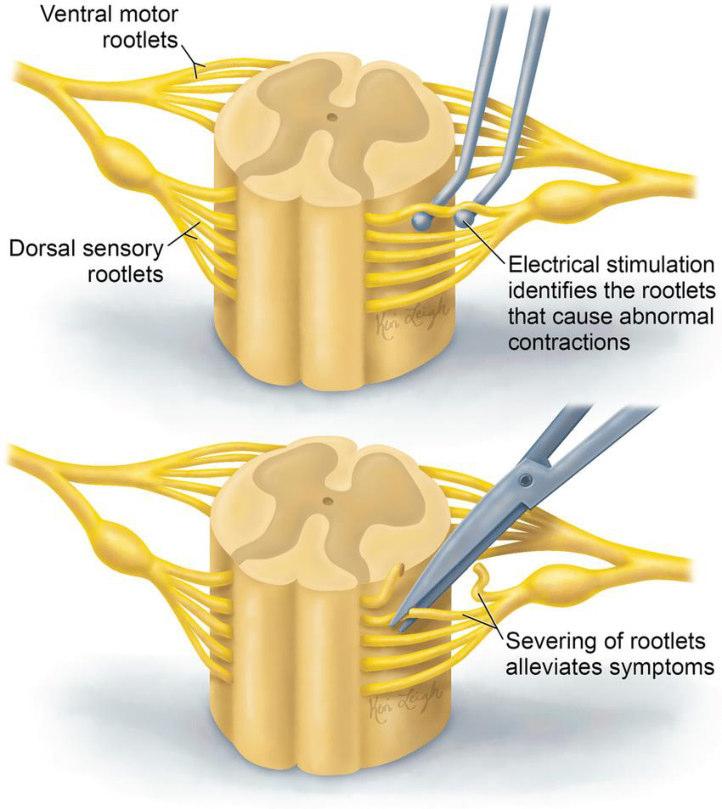

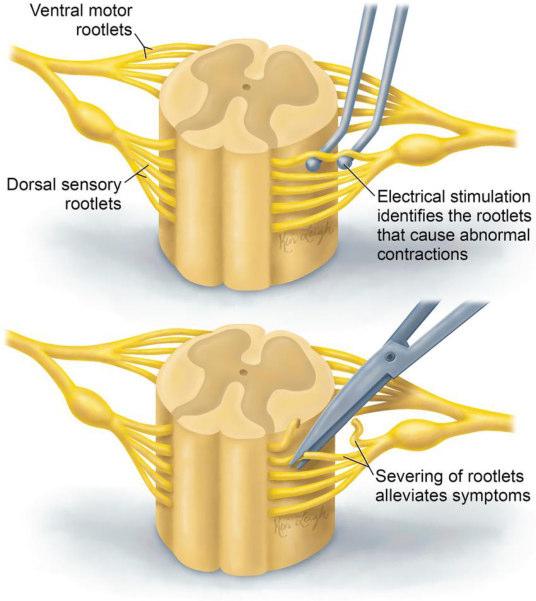
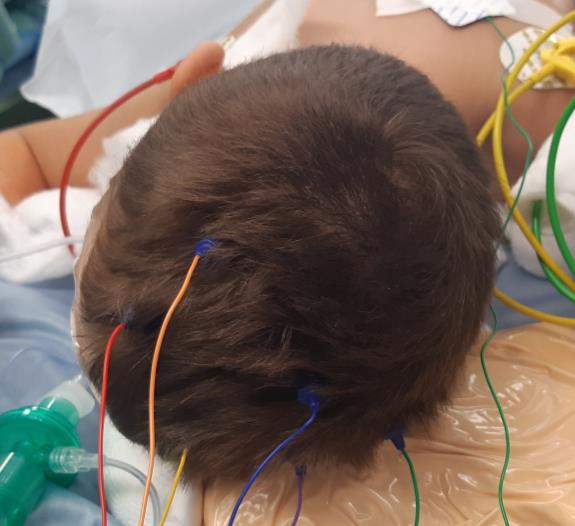
Transcranial Motor Evoked potentials (TcMEPs)
Somatosensory Evoked potentials (SEPs)
Bulbo-cavernosus reflex (SEPs)
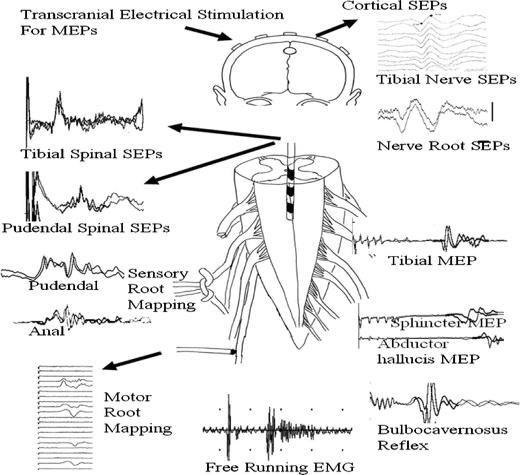

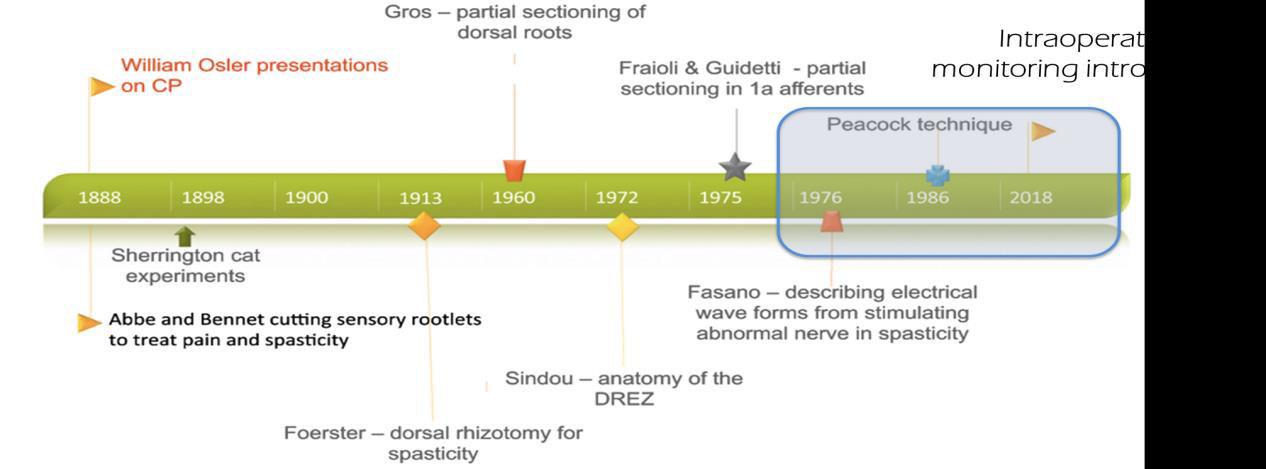
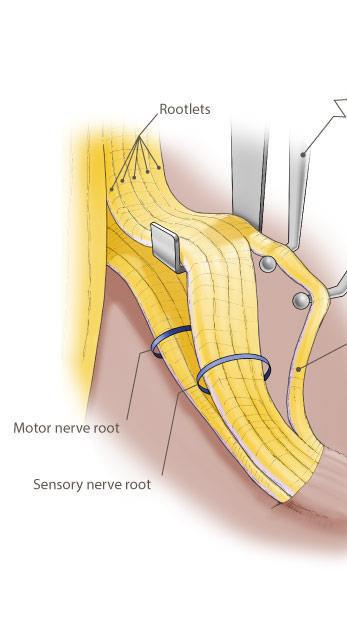
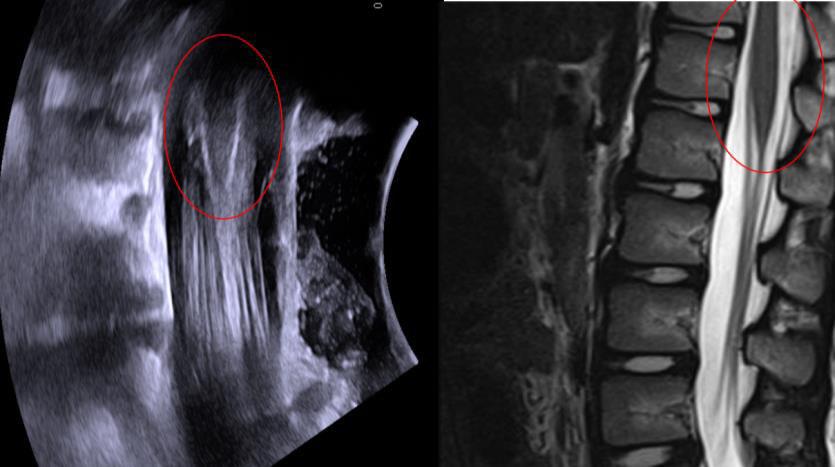
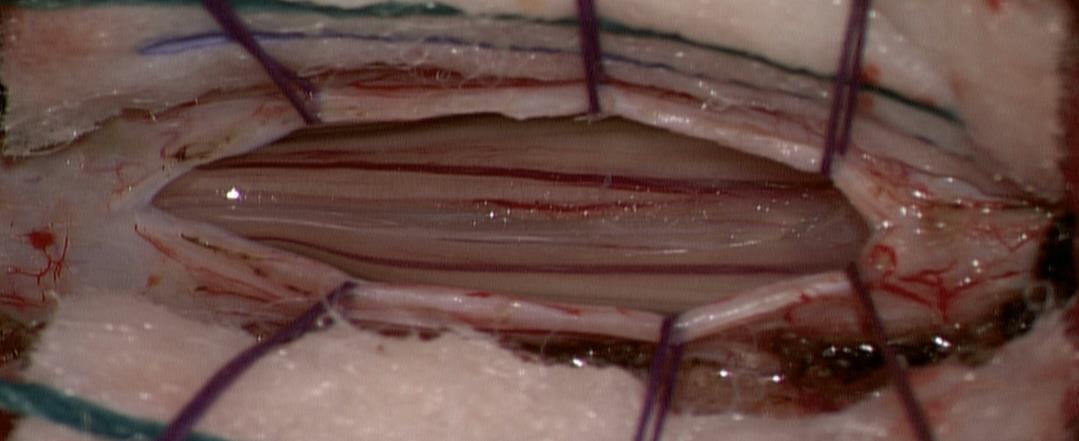
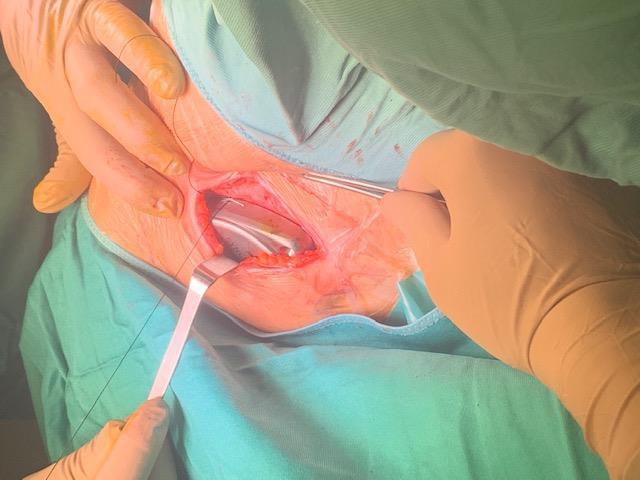
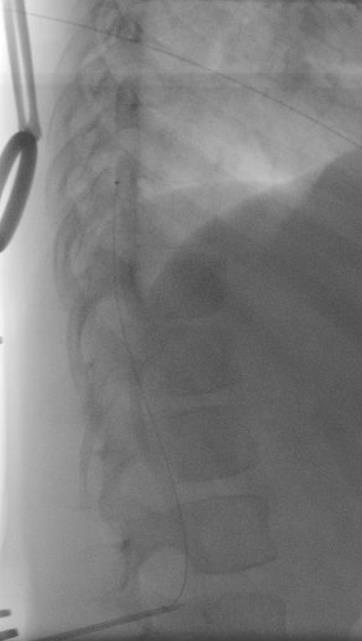
SDR involves surgically accessing the spinal cord (typically in the lumbosacral region, L2 to S1 or S2).The dorsal (sensory) nerve roots are carefully identified and then divided into smaller bundles called rootlets.


Reduces spasticityReduces painful spasmsImproves motor functionsEnhances autonomyImproves ADLs (Activities of Daily Living)Improves sleepImproves strength and endurance

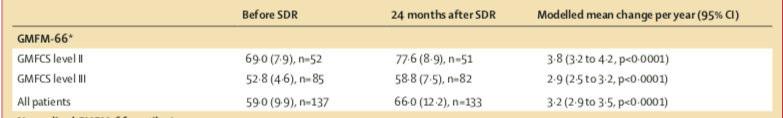
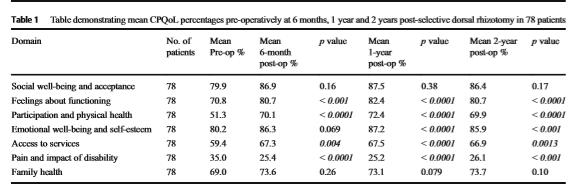
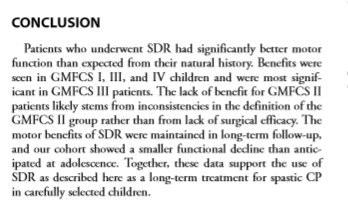
The observed benefit of SDR among children in this study exceeded the expected function without SDR

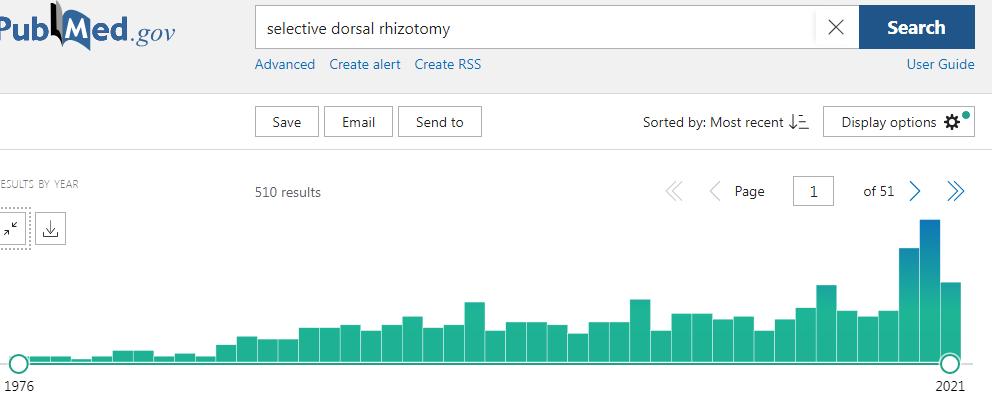
The objective of this review is to analyze the evidence supporting selective dorsal rhizotomy (SDR) for the treatment of spastic cerebral palsy (CP). We reviewed 85 outcome studies from 12 countries between 1990 and 2017. The published results are overwhelmingly supportive of SDR, and 39 studies form a basis for this review. Also included is some of the clinical experience of the senior author.






Effects of SDR on gross motor function in two years
Effects of SDR on rate of orthopedic surgery
Effects of SDR on hip subluxation
Effects of SDR on bladder function
Spinal deformities after SDR via multilevel laminectomy and laminoplasty
There is sufficient evidence supporting the short and long-term benefits of SDR. The evidence indicates that SDR can reduce spasticity permanently and eliminate neurological complications in patients with spastic CP.


Patients who underwent SDR had significantly better motor function than expected from their natural history. Benefits were seen in GMFCS I, III, and IV children and were most significant in GMFCS III patients. GMFCS II patients experienced different evolution based on their age at the time of surgery.



Functional mobility level and baseline gait quality are both important factors to predict gait outcomes after SDR. If candidates are well selected, SDR can be a successful intervention to improve gait both in children with spastic diplegia.
SDR improves dynamic muscle forces and leads to less gait pathology,as shown in the improvement in joint kinematics and joint kinetics. Individual muscle force analyses using the Muscle-Force-Profile extend standard joint kinematics and joint moment.

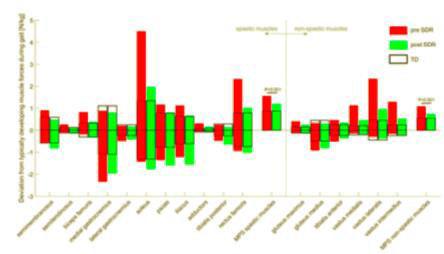

This study showed that selective dorsal rhizotomy improves dynamic muscle forces in children with cerebral palsy as shown in the improvement in joint kinematics and joint kinetics. SDR normalizes spastic muscle forces during walking in children with CP. SDR does also normalize non-spastic muscles forces during gait.




Adductor Longus L2, L3
Vastus Lateralis L3,L4
Tibialis Anterior L4, L5
Peroneus longus L5, S1
Gastrocnemius S1, S2
Abductor hallucis S1, S2
Sphincter S2

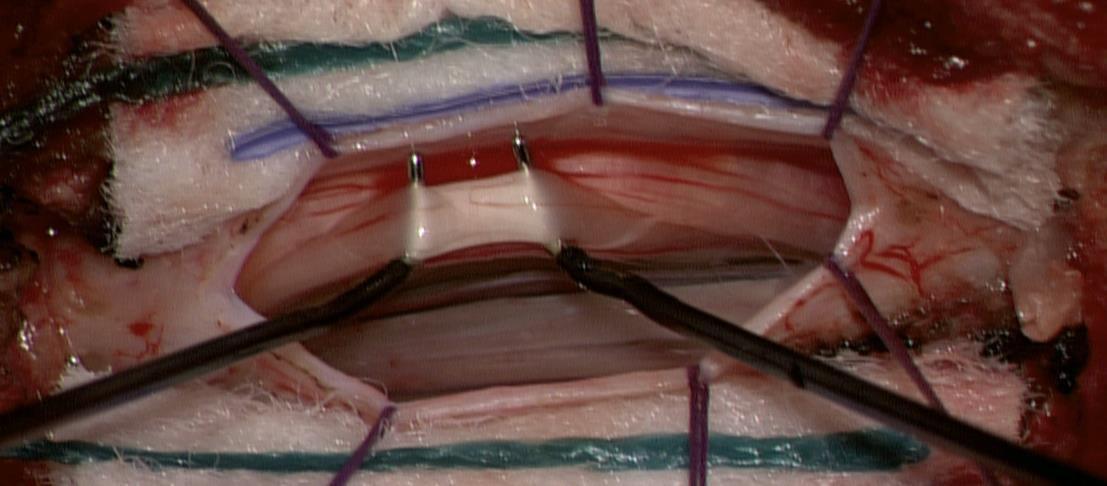
0 Unsustained or single discharge to train of stimuli
1+ Sustained discharge of appropriate muscle group. Ipsilateral response
2+ Sustained discharges of adjacent muscle groups, Ipsilateral
3+ Sustained discharges of distant muscle groups, Ipsilateral
4+ Sustained discharges of contralateral muscle group(s), with or without ipsilateral muscle group involvment










Muscle tone reduction
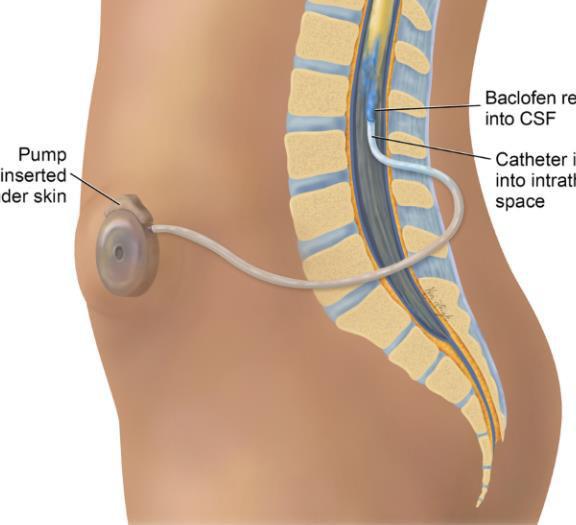
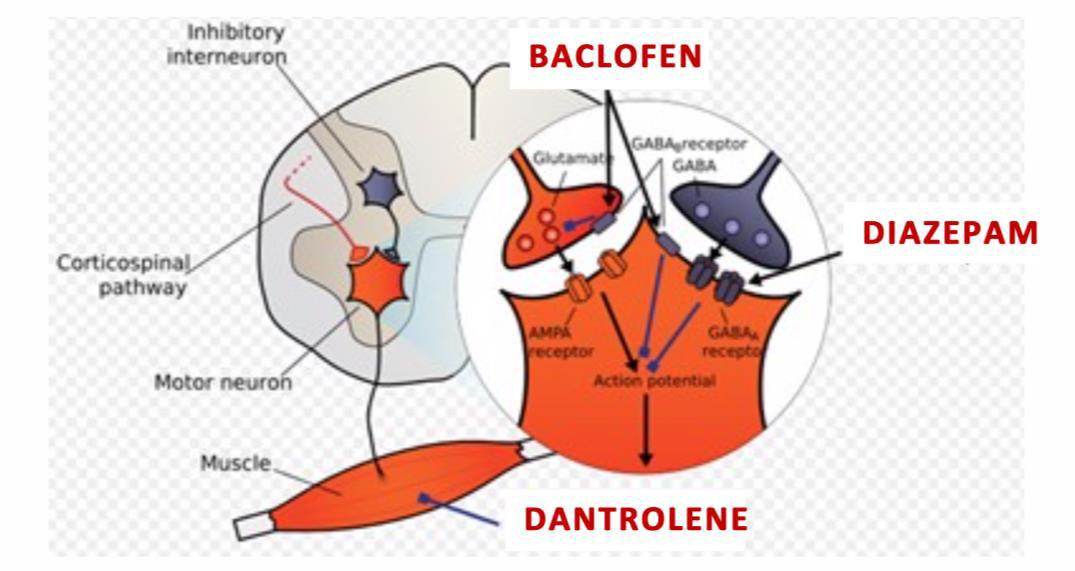
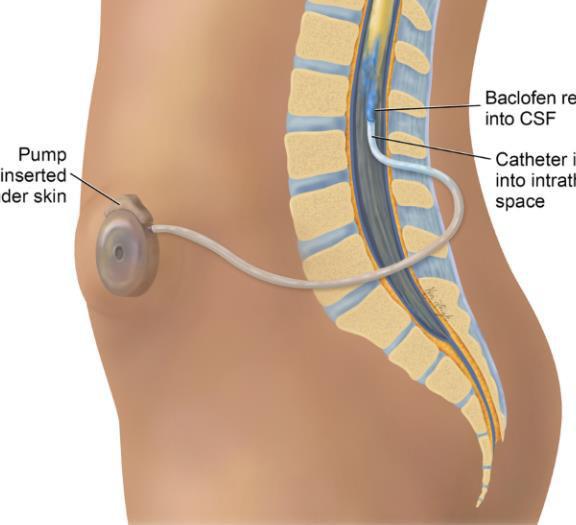
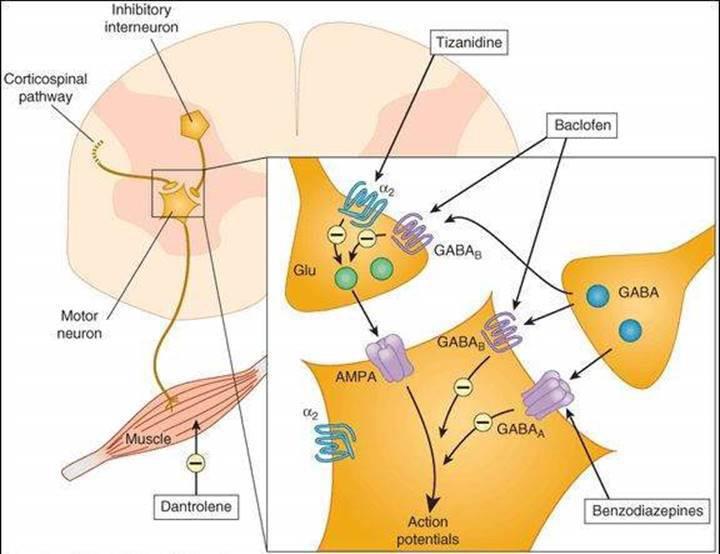
• Structurally similar to the neurotransmitter GABAAgonist action (GABAb receptor)Main action on primary afferent neurons of the spinal cord, possible action on cerebral 5MA receptors

Stretch reflex inibition
Lower spasticity


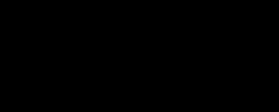
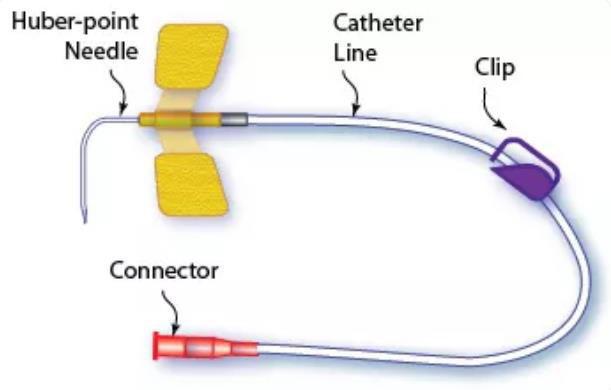
• Hydrophilic drugDaily dose 60-120mgSide effects at low plasma levelsBBB blocks passage (30-60mg oral = 12–
96 mg/ml CSF)Response to oral therapy not predictive

• High CSF concentration (501500 mcg/day = 30-1240 ng/ml CSF)Steady state in 24-48hLow plasma levels (5 ng/ml)Half-life
180 minutesHigher concentration at lumbar level (lumbar:cisterna magna = 4:1)Effective dose 100-1000 times lower

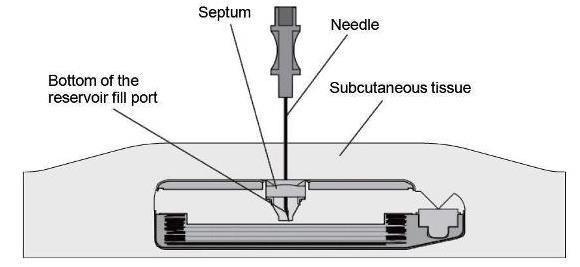
Age > 4 yearsAdequate body weight > 20kgAdequate
subcutaneous tissue












Thirty-one children (31/313 = 24%) had a VP shunt as part of the management of hydrocephalus. Five children (5/31 = 16%) had infection in 1 of their systems






• Increased seizures
• Worsening of scoliosis
• CSF leak (25%)InfectionsCatheter malfunction and dislocation
• WithdrawalOverdose



















T10–12 spastic diplegia
C5–T2 spastic quadriplegia
C1–C4 secondary generalized dystonia
Wound check / Wound care / Oral medication
weaning
Orthosis check and modification 20% increments every 24/48 hours
Monitor for early complications


5 days restNo trunk rotations
Orthosis to maintain knees in extension and ankle at 90 (TT likely refers to tibiotarsal joint/ankle)


No hip flexion beyond 80
Passive mobilizations of hip, knee, and ankle (TT) according to tolerance
Rehabilitation program at 1 week
Passive and assisted active mobilizations
Stretching
Standing with orthoses and standing aids (+ 1 hour standing frame with parent)
Assisted ambulation if possibleSelective activation of muscle groups
Rehabilitation program from Week II onwards
Passive and assisted active mobilizations
Standing with orthoses (+ 1 hour/day standing frame)
Assisted ambulation if possible
Selective muscle controlIncrease in muscle strength
Progressive increase in weight-bearing and ambulation times
2 X sessions daily
Reducing infection risk through strict aseptic technique
The refill interval depends on drug consumption, with a maximum interval of 6 months
In a multidisciplinary outpatient clinic



6 weeks before surgery Before surgery

5 weeks after surgery

6 months after admission

12 months after



2 years after 1 month in rehabilitation Every month in joint DH until the first refill Every 6 months or as needed (increments, orthotic changes, wound assessment)




Once a year: rx rachis




Functional measures
•GMFCS
•GMFM 66/88
•6 minute walk test
•10 meters walk testest
•Functional mobility scale
•Gillette
•Video Gait / Gait analysis
Quality of life measures
•Care and comfort hypertonicity questionnaire (CCHQ)
•CP child (CPQoL)
•Wee-FIM
•AbilHand
Expectations with result of procedure
VAS Individualised goals using a visual analogue scale