

DEPARTMENT OF ANESTHESIOLOGY, PHARMACOLOGY & THERAPEUTICS



DEPARTMENT OF ANESTHESIOLOGY, PHARMACOLOGY & THERAPEUTICS
Full-time faculty - 26
Clinical Faculty - 568
Postdoctoral Research Fellows – 12
Research Associates – 6

Clinical Fellows - 16
Residents – ANAE – 95
Residents – FPA – 5
Residents – Pain Medicine - 5
Medical Students – 327
Pharmacology Graduate Program – 24
Pharmacology Undergraduate Program – 39
students / 47 with PCTH Co-op students included
CUPE 2950 Staff – 5
Non-Union Technicians/Research Assistants - 16
Management/Professional Staff – 18
Student Employees – 23
Adjunct Professors – 11
Affiliate Professors – 9
Emeriti Faculty - 30
Honorary Professor - 1



Dr. Peter Choi
“The 2024 calendar year was a relatively quiet year with a focus on preparation for new leadership in our department.”
One of the pressing human resource issues has been the hiring of a new department head. After a long search process, I am pleased to inform you that a new department head has been hired and he will start around mid-February 2025. This will bring much-needed long-term stability and a new vision to our department. I look forward to handing the reins to him. Dean Kelleher will announce the new department head soon.
In preparation for our new department head, our administrative staff and I have been reviewing the department’s terms of references, standard operating procedures, policies, and guidelines during 2024 to ensure they are up-to-date. Some guidelines, such the Academic Deliverables and Expectations for Academic Faculty Members, are new to ensure compliance with collective agreements. Others, such as terms of references
for various positions and processes for hiring clinical fellows, are updates to increase clarity and transparency regarding roles and processes for the new department head and our faculty, staff, and students.
In addition to the search for a new department head, we had a number of changes in our clinical education leadership during 2024. In the anesthesiology residency program, Dr. Abdulla Sadiq (BC Women’s Hospital) stepped down as the associate program director and Dr. Chris NixonGiles (Vancouver General Hospital) took over this role to support Dr. Zoë Brown (BC Children’s Hospital), who continues as the residency program director. Dr. John McAlpine (Lion’s Gate Hospital) has been renewed for another term as the FPA residency program co-director (urban community) and has been joined by Dr. Micaela Coombs (Whitehorse, YT) as the FPA residency co-director (rural community). Together, they are helping us address the shortage of anesthesia providers. Our pain medicine residency program also saw a transition in leadership with Dr. Michael Butterfield (Psychiatry) completing his term as residency
program director in 2024 and Dr. Audrey Chan (Physiatry) taking over in this role last summer. I thank all of our residency program leaders for their contributions.
There will be ongoing transition in 2025. Dr. Shelley Tweedle (Royal Columbian Hospital) has taken over the role of Faculty Development Lead in our department and will be working on determining our needs in 2025. As well, the department will be seeking a new Patient Safety Chair with the retirement of Dr. Malcolm Maclure in 2025.
Of course, the shortage of anesthesia care providers continues to be the major human resource problem in anesthesiology. The academic department continues to expand the training of anesthesia providers (see below) and work collaboratively with clinical departments in discussions with government and regulatory bodies for solutions to increase the number of anesthesia care providers in BC. This remains a work in progress and I am cautiously optimistic about these changes.
Our education programs continue to be excellent and highly desirable to leaners and I encourage you to read the reports for more details.
A number of our faculty members were recognized for their excellence in education. Dr. Richard Alexander (Royal Jubilee Hospital) received the Early Career Clinical Faculty Award for Excellence in Clinical Teaching from the UBC Faculty of Medicine. Dr. Laine Bosma (St. Paul’s Hospital) received the Certificate Merit from the Canadian Association for Medical Education for his many contributions to postgraduate education, especially in simulation. Dr. Jennifer Shabbits received the Dr. William Webber Award from the UBC Faculty of Medicine for her excellence in undergraduate medical education.

Dr. Tillie Hackett received the Michelle Harkness Mentorship Award for Mentoring ExcellenceInvestigator from the Allergies, Gene & Environment Network for her mentorship of graduate students and postdoctoral fellows. Drs. John Bowering and Anton Chau were recognized for their excellence by the Canadian Anesthesiologists’ Society, who awarded the Clinical Practitioner Award and John Bradley Young Education Award to Dr. Bowering and Dr. Chau respectively. Our residents also recognized 18 of our faculty for their teaching excellence (details in this report).
Thanks to the hard work of Dr. Zoë Brown, our anesthesiology residency program is at maximum capacity with the addition of three return-ofservice re-entry residents in addition to our usual entry cohort of 20 direct-entry residents. The pain medicine residency program expanded to include four of BC’s health authorities (FHA, IHA, VCH, and VIHA). The number of students enrolled in our PCTH graduate programs increased last year and our PCTH undergraduate program remains highly competitive and attractive to students. Unfortunately, our request for funding to expand our pharmacology learning space was declined in
2024 but Dr. Andrew Horne, vice-chair education, continues to look for possible solutions to allow us to expand our undergraduate enrolment. The Therapeutics Initiative continues to provide its highly successful education programs to clinicians across the province.
We resumed the annual Dr. Rudolf Vrba Memorial Lecture in Pharmacology with Dr. Paul Insel (University of California San Diego) as the Vrba lecturer in 2024. With funding from the family of the late Dr. Leonard Jenkins, a previous anesthesiology department head, we also started the annual Dr. Leonard Jenkins Memorial Lecture in Anesthesiology in 2024 with Dr. Susan Lee (Royal Columbian Hospital) as the inaugural Jenkins lecturer. The annual Dr. Jean Templeton Hugill Memorial Lecture also took place with Dr. Guy Weinberg (University of Illinois) in 2024.
The Faculty of Medicine Postgraduate Medical Education started changes to clinical fellowship programs at UBC in 2024 and these changes are expected to be finalized over the next year. Stay tuned for more information as these changes may have some impact on how we offer clinical fellowships in our clinical departments.
Our faculty and students continue to be successful in obtaining millions of dollars of research funding and I encourage you to read the research report for more details. Dr. Mark Ansermino received the 2024 J.S. Gravenstein Award from the Society for Technology in Anesthesia for his lifetime contributions in this field. Our department had substantial success in securing research funding in 2024. Three projects of Drs. Khaled Abdelrahman, David Fedida, and Tillie Hackett received almost $3 million of funding from CIHR. Dr. Catrina Loucks received a Michael Smith Health Research BC Scholar Award. Two of our postdoctoral fellows were recipients of postdoctoral fellowship awards. More awards were handed out at our Annual APT Research Day (see details in this report).
Please look at the list of publications to see the breadth and productivity of our department in research.

As we enter 2025, I look forward to stepping down as the interim head and working to support our new department head. I am grateful for the opportunity to be the caretaker of this department while we were in between department heads. I had hoped to maintain the status quo during my term but some changes were inevitable. Thank you to all of the individuals in this department, especially the administrative staff, who worked tirelessly and helped manage the changes that took place in 2024 – the Department would not have run without their hard work and strong support. Whatever positives resulted from the changes are shared among all of us. Whatever negatives occurred are owned by me.
Change can be hard and generate anxiety but it also offers an opportunity for reflection and renewal. For those of us who are more senior members of the department, it is an opportunity for us to hand over and let go, to make opportunities for our younger colleagues to direct our department, and to trust that those who come after us will excel and exceed us. For those who are just starting their careers or are mid-career, I hope that 2025 will be an opportunity for you to contribute and enact constructive change. I hope that you too will be able to realize the motto of UBC: Tuum est – it is yours.
With thanks and gratitude,

Peter Choi Professor & Interim Head

Dr. Zoë Brown Program Director
Dr. Christopher Nixon-Giles Program Associate Director
We are thrilled to welcome Dr. Chris Nixon-Giles as the new Associate Program Director. As the residency program continues to grow, Dr. NixonGiles will play an instrumental role in helping to shape its future. We are grateful for his leadership and dedication. At the same time, we bid a heartfelt farewell to Dr. Sadiq Abdulla, who has contributed immensely over the years, particularly with the CaRMS process. His hard work and commitment will be greatly missed.
Resident numbers continue to rise. As of December 2024, we have a total of 92 residents enrolled in the five-year Royal College of Physicians and Surgeons program. This year, we welcomed twenty new PGY1 residents, one program transfer, and three re-entry residents who have joined us for the final three years of their core training. A total of sixteen residents are set to complete their residency in the 2024/2025 academic year. The number of CaRMS positions for 2025/2026 will remain at 20, and we continue to attract a highly qualified pool of over 180 applicants.
The majority of the 2024 graduates have secured faculty positions at hospitals across British Columbia. Many are also pursuing exciting fellowship opportunities abroad. Our Exam Seminar Series, led by Dr. Katarina Kojic and Dr. Nav Chima, with support from many faculty members, remains a hallmark of our program. This initiative, along with the mock oral exam preparation days where faculty volunteer their time, has become a model for Royal College exam preparation.

The Resident Selection Committee, a subcommittee of the Residency Program Committee (RPC), plays a pivotal role in reviewing all applicants. Chaired by Dr. Chris Nixon-Giles, the committee includes 25 members representing major teaching hospitals across BC, as well as resident representatives. Dr. Nixon-Giles is excited to lead this committee and is focused on enhancing the selection process to align with his vision for the future of the program.
• Academic Day: The full-day academic program, which incorporates active participation from each of the teaching hospitals, has been highly successful. The Lead Residents have worked diligently to improve attendance and engagement, ensuring that the academic day remains a cornerstone of our training.
• Simulation Program: Led by Dr. John Veall and Dr. Taren Roughead, simulation remains a key component of our residency program. They deliver the Royal College CanNASc scenarios as required by the

curriculum, and ensuring each resident has the opportunity to attend two sessions per year. The success of this program is made possible by the tireless efforts of five simulation residents and numerous faculty members who generously volunteer their time.
• Journal Club: An integral part of our academic program, and an opportunity to get together with faculty. This is run by two residents who assist with the coordination and organization of sessions, supported by faculty at each site.
The clinical training program remains a strong pillar of our residency. Our residents benefit from comprehensive training in both core anesthesiology and subspecialties, with opportunities available at primary and secondary teaching sites across BC. The program continues to explore and implement new training experiences, with expanded opportunities



at Victoria, Nanaimo, and Royal Columbian Hospital. Plans are underway to further broaden subspecialty training at additional sites in the 2025/2026 academic year.
The success of our Anesthesiology Residency Program is driven by the dedication of our faculty members, who go above and beyond to support the education and development of our residents—whether in the operating room, during evening sessions, or on their days off. We are deeply grateful for their commitment.
As the program continues to grow, we must think creatively about how to deliver highquality training experiences whilst alleviating the pressure on our most saturated sites. It’s exciting to see the opportunities for residents to travel throughout BC and experience a variety of settings beyond the Lower Mainland.
The sense of camaraderie among our residents remains strong, thanks in no small part to the residents themselves who organize communitybuilding events and foster a supportive and collaborative environment.
Micaela Coombs & Dr. John McAlpine Program Directors
UBC FPA Enhanced Skills program’s mandate is to produce family physician anesthetists committed to providing a high standard of anesthesia care in rural British Columbia. It is a challenging and demanding 12-month program with a blend of tertiary center rotations in the lower mainland (adult, pediatric, obstetrical anesthesia, and critical care) for exposure to high volume and complexity and rural community rotations (including Whitehorse, Terrace or Campbell River, and an elective block) for exposure to the unique challenges associated with rural FPA clinical practice.
The UBC FPA Enhanced Skills program has 4 residents this academic year, with 4 incoming residents for the July 2025-2026 cohort.
We transitioned to a co-PD model this year with Dr. John McAlpine being joined by Dr. Micaela Coombs an FP-anesthetist (UBC FPA program 2020 graduate) and emergency physician from Whitehorse, Yukon. All UBC FP-anesthesia residents rotate through Whitehorse as one of the core rural rotations. We trust this partnership will add rural insight to the program and help strengthen relationships between its urban base and the rural communities it trains residents for.
The FPA residents participate in several unique educational activities including a seminar series focused on the unique challenges associated with rural anesthesia. Additionally, every year UBC’s FPA residents join FPA residents from across Canada to attend the Northern School of Medicine FPA Bootcamp. This is a week of intensive, high-fidelity simulation and is a highlight of the year.

Each November the annual UBC FPA Refresher Course is held with strong attendance from the BC FPA community and increasing attendance from other regions of the country. This conference receives tremendous support from the UBC Anesthesia faculty towards the academic content of lectures and workshops and is of great educational benefit to the BC FPA physicians.
Although the FPA program is an Enhanced Skills program within the Dept of Family Practice, it naturally has a very close relationship with the Royal College anesthesia program and some shared administration. We are grateful for the anesthesia department members who support our residents through direct teaching, shared educational opportunities, participation in our program committees, as site leads, and in other roles.
New Residents: The UBC Pain Medicine Program continues attract excellent applicants from a variety of specialties and once again this year the program matched two strong candidates. These were filled by Dr. Kiran Grant whose primary specialty is Emergency Medicine, and Dr. Frederic Turcotte whose primary specialty is anesthesia. Both individuals have already demonstrated and bring to the program their own specialty specific experiences in pain, and we look forward to having both individuals join our program.
Graduating residents: Dr. Sam Brophy and Dr. Noah Alexander successfully passed their Royal College Pain medicine exam and graduated from the program in Fall 2024. They will both be remaining in British Columbia to start their careers in pain medicine. Dr. Brophy will be working on the Island in tertiary care, and Dr. Alexander will be Vancouver in community outpatient clinics.
Program Director: Dr. Michael Butterfield’s 5-year term ended in October 2024. He was instrumental in continued accreditation of the program and the arduous task of implementing and educating the various pain specialty factions within the program on CBD. His energy, breadth of knowledge and skills will be missed. Fortunately for the program, he will remain a presence through participation in our competency committee and research advisor.
Dr. Audrey Chen, a physiatrist and previous UBC pain medicine graduate has taken over as program director. She currently works in a mix of community based pain practices: CPRI in Vancouver, Initium in Abbotsford, as well as the Transition Pain Clinic at VGH.
Competency By Design (CBD): Pain Medicine has fully transition to CBD and our residents Dr. Casey Wang and Dr. Shyama Das have continued their predecessors excellent work with implementation of CBD providing feedback for continued adjustments where needed. Both residents will be looking to complete their program in less than 2 years. Dr. Wang will be going on to complete an Orthopedics fellowship in Reconstruction of the Hip/Knee in Melbourne, Australia in February 2026 before returning to Canada to complete a hip/knee fellowship at the University of Toronto. Dr. Das plans to remain in Vancouver to further add to our growing pain medicine group.

We have continued to work with our wide variety of educational sites. These include the Bill Nelem’s Pain and Research Centre in Kelowna and the Central Island Pain Program in Nanaimo as part of our multidisciplinary pain clinic sites. With our group at St. Paul’s hospital, the team is working on adding more simulation training to the program. We recently acquired a phantom model to help with simulation and practice for interventional training.
• Ensure that the Competency by Design model is continuing to be seamlessly integrated into the pain medicine residency program.
• The team is currently working on a dedicated simulation program for managing emergencies that can occur when performing interventional procedures.
• Improve the research component of the pain medicine residency program.
• Increase resident engagement in leadership and community advocacy for individuals with chronic pain.
• Working on re-accreditation with UBC later this year.

2024 saw the culmination of UBC’s overhaul of their Integrative Renewal Program, drastically changing how administrative tasks related to teaching will be carried out. The aim of this project was to replace archaic software that was struggling to meet the modern-day demands of UBC faculty, staff, and students. September 2024 was the first academic term entirely run under this new system, and while there were steep learning curves and occasional hiccups along the way, by all accounts our department managed to weather the storm with minimal disruptions to Dr. Andrew Horne
Chair, Undergraduate Education Committee
our administrative tasks. Many thanks to Wynne Leung (our Staff LTL, or Local Transition Lead) for her tireless efforts in assisting faculty; as we continue to learn and transition our practices under this system, please reach out to her or Andrew Horne (Faculty LTL) for assistance in education-related tasks within Workday.
Beyond these behind-the-scenes updates, the Undergraduate Education portfolio for 2024 can be best summarized through discussion of each of the three 4-month academic terms:
Below is a summary table of courses offered in Term 2, along with course director and enrolment:
May 2023 saw 24 of our students graduate with their Bachelor of Science degree in Pharmacology. Pamela Bai was awarded the Prakash Gill Memorial Prize in Pharmacology and Therapeutics, as the Majors Pharmacology student with the highest
graduating average. The Esther R. Anderson Memorial Prize, awarded to the Honours Pharmacology with the highest graduating average, was not handed out this year. Congratulations to Pamela and our entire graduating class of 2024!
t
The Vancouver Summer Program is an offering for students attending international universities, where they can select one of many two-course packages from Faculties and Departments across UBC, and is a very popular program amongst students from southeast Asia. This year, we once again offered our course package titled Pharmacology and Literature Analysis in Science and Medicine. Kip Kramer and Paulina Scheuren took over as co-course directors for “Primary Literature Analysis in Science and Medicine”, while Joanne Leung continued on as director.
The Vancouver Summer Program is an offering for students attending international universities, where they can select one of many two-course packages from Faculties and Departments across
UBC, and is a very popular program amongst students from southeast Asia. This year, we once again offered our course package titled Pharmacology and Literature Analysis in Science and Medicine. Kip Kramer and Paulina Scheuren took over as co-course directors for “Primary Literature Analysis in Science and Medicine”, while Joanne Leung continued on as director for “Pharmacology Through Case Studies.” Enrolment was considerably lower than our historical average, which was attributed largely to higher-than-expected attrition from difficulties with students getting student visas, but we were still thrilled to be able to welcome 7 students to the department for this offering.
Many thanks to Joanne, Paulina, and Kip, as well as all of the other faculty, post-doctoral fellows, and graduate students who participated in instructional activities in support of this educational program!
In September 2024, we welcomed 29 students into the third year BSc Pharmacology program, and 12 students into the fourth and final year of the program; the latter is a combination of students advancing directly to fourth year from 2022W and those returning from 12-16 months of optional co-operative work experience. The balance of enrolment in our 400-level core courses were from students taking these courses as an elective or as part of their requirement for alternate BSc degrees such as Integrated Sciences. As previously mentioned, the course numbering for the 300-level courses has changed as of September 2023, with PCTH 301 (Term 1) and PCTH 303 (Term 2) replacing the co-listed PCTH 300/305 courses.
Enrolment in PCTH courses by students outside of the BSc Pharmacology specialization continues to be high, with many students taking PCTH 201 and PCTH 325 as breadth electives (though PCTH 201 is also a requirement of the BSc Pharmacology specialization), and high enrolment in PCTH 301 and PCTH 400 through students in the Integrated Sciences Program.
The following table summarizes the PCTH courses offered in Term 1 of 2024W, along with course directors and student enrolment:
course did not run in 2023W
As always, I want to offer my profound thanks to all course directors for their tireless efforts in organizing and facilitating delivery of our
undergraduate educational offerings, and for the faculty and adjunct faculty who contribute their time and expertise to content delivery within.
UBC medical students do a mandatory two week Anesthesia clerkship rotation as part of their Surgical and Perioperative Care Block in 3rd year. For many students this is their first exposure to Anesthesiology as a specialty. These two weeks give them an opportunity to learn many fundamental acute care principles and skills, including perioperative medical optimization of the severely ill patient, airway management, and a deeper understanding of cardiovascular and respiratory physiology and mechanical ventilation.
Generally, the Anesthesia rotation is one of the highest ranked among students. Students appreciate one on one time with staff, extensive teaching and hands on experience. During the SPC block, students also attend an Anesthesia Academic Day and a Trauma Academic Day. Both of these involve Anesthesia faculty and residents teaching. Depending on the site and resource availability, a variable amount of low and high fidelity simulation is used during these days.
Over the last year, new online learning modules have been added to supplement students’ learning resources and there are on-going efforts to make learning materials more accessible.

As part of the ICC stream, a number of students spend their 3rd year in a rural community where their clinical learning is integrated throughout the academic year and not separated into distinct specialty blocks. Their Anesthesia experiences are spread out through the year. Students are required to meet the same Anesthesia learning objectives and outcomes at the end of their clerkship year.
There is great demand for Anesthesia electives in 4th year as students prepare to make crucial decisions about what path to follow in their medical career. These electives can be two or four weeks in length depending on the site. There are Anesthesia electives throughout the province and we are constantly looking at ways to expand the availability given the high demand. Anesthesia electives are always highly rated by students.
As UBC MDUP undergoes expansion, there have been challenges with accommodating more students within our current system. We are grateful to all the dedicated clinical faculty whose willingness to share their time, knowledge and expertise make the Anesthesia clerkship rotation and electives such positive experiences for students.
Dr. Jennifer Shabbits Chair, Medical Undergraduate Program
Pharmacology teaching in the MD undergraduate program (MDUP) occurs primarily through lectures and case-base learning small group sessions in years 1 and 2, with a focus on mechanisms and foundational science principles at this introductory stage. Two new pharmacology resources were created in 2024 to aid students’ knowledge acquisition and self-assessment of pharmacology principles:
An Anki deck of several hundred open-source, spaced-repetition flashcards were created for each week of the Year 1 curriculum. A similar deck for year 2 will be developed in spring 2025.
A list of Therapeutics Initiative Letters relevant to the Year 1 curriculum was compiled, with hyperlinks to specific letters that relate to the topic of each week. A similar package will be prepared for Year 2 in spring 2025.
Additional resources are being developed in 2025 to help bridge the transition from pre-clinical (Years 1 & 2) to clinical (Years 3 & 4) learning. Pharmacotherapy becomes the focus in years 3 and 4, when students apply their foundational knowledge to patient care during clinical rotations.

Dr. Pascal Bernatchez Program Director
The Department of APT is honored to continue hosting the pharmacology and therapeutics (PCTH) training programs at both Ph.D. and M.Sc. levels, and delighted by our graduate trainees’ outstanding contribution to our department’s
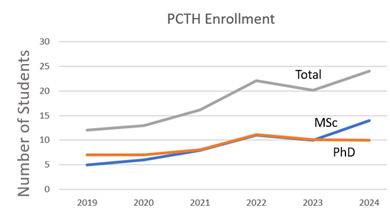
considerable research output. The 2024 PCTH graduate student enrollment reached a 7-year high, thanks to the relentless efforts by new and seasoned Faculty to secure the operating funds required to help support PCTH trainees.

Some of the key highlights from 2024:
Ten (10) new MSc students and 2 new PhD students joined our graduate program, for a total of 24 graduate students.
3 students graduated with a PCTH MSc degree, 3 with PCTH PhD degrees. Our most sincere congratulations!
3 MSc students transferred to our PhD program.
We have increased the annual minimal stipend of PCTH grad students to $25,000/ year – above the FoGS recommendation – due to continuous changes to student reality in Vancouver.
PCTH graduate students have been supported by a range of local, national and international awards including a UBC-sponsored 4-year fellowship, a Cmolik Alumni award, CIHR Canada Graduate Scholarship Master’s and Doctoral awards, a Canadian Lung Association Research award, a Matrix-N Cluster 23/24 Junior Scholars award, awards from Mitacs Canada and a China Graduate Scholarship award.
Dr. Tillie-Louise Hackett Professor, Vice Chair of Research APT Department
Canada Research Chair in Lung Pathobiology
The Department of Anesthesiology, Pharmacology and Therapeutics’ 2024 Annual Research Report is a snapshot of dedicated research efforts that advance Research, Clinical Practice, and Know Translation to enhance the Safety and Care of Patients. The research continuum of Anesthesiology, Pharmacology & Therapeutics spans across – acute and chronic pain, cardiopulmonary, clinical outcomes, equity in medicine, evidencebased medicine, intensive care, neurosciences, obstetrics, patient safety, pediatrics, peri-operative technology, pharmacoepidemiology, transplant and transfusion- throughout the human life time. At the core of this research are -our faculty, researchers, trainees, and support staff. Congratulations to everyone on your successes over the last year, please see some of the 2024 research highlights below.


Dr. Catrina Loucks
Assistant Professor, Grant Tenure Track
Michael Smith Health Research BC Scholar Award – 2024
Dr. Louck’s research is focussed on Improving pain management for children using patient-specific genetic information. In children, ongoing pain can interfere with brain development, disrupt behaviour and increase the risk of chronic pain. This can be particularly devastating in
children with high burdens of pain, such as children with cancer, many of whom experience highlydistressing pain requiring opioids. Providing timely and adequate pain treatment for these children is critical, yet it remains challenging to predict who will experience pain requiring opioids and how these children will respond to prescribed opioids. This is especially difficult in young children who cannot articulate their level of pain, limiting their ability to receive appropriate relief without harm. Dr. Louck’s research program is working to identify unique genetic signatures that predict how likely a child is to develop painful conditions, experience severe pain and respond to opioid-based pain relievers. This information will be used to develop predictive genetic tests to inform medication choices that will enhance the safety and effectiveness of pain management strategies for children. This work also has the power to combat the opioid crisis that continues to devastate British Columbians, where opioids can be restricted to patients most likely to benefit without harm.



Dr. Paulina Scheuren
Dr. Zishan Cui
Postdoctoral Fellow (Dormuth Lab)
Canadian Institutes of Health Research Postdoctoral Fellowship Award
3 year Postdoctoral Fellowship to support Dr. Cui’s research project entitled “Determine the optimal opioid treatment modality for patients with concurrent opioid and stimulant use disorder using populationbased data in British Columbia: A trial emulation)”.
Postdoctoral Fellow (Kramer Lab)
Canadian Institutes of Health Research Postdoctoral Fellowship Award
3 year Postdoctoral Fellowship to support her research project entitled “Spinal cord THERMOmetry as a novel measure of neuroinflammation after spinal CORD pathology (ThermoCORD)”

Canadian Institutes of Health Research Postdoctoral Fellowship Award
3 year Postdoctoral Fellowship to support her research project entitled “Spinal cord temperature as a measure of neuroinflammation in the human spinal cord”
Bluma Tischler Postdoctoral Fellowship Award
1 year Postdoctoral Fellowship to support her research project entitled “Spinal cord temperature as a measure of neuroinflammation in the human spinal cord”
APT Research Publications 2015-2024:
Since 2010, we have had a continual increase in the number of publications generated by the translational Research within the Department of APT.
Tri council Research Grants included: Canadian Institutes of Health (CIHR) Spring 2024 Project Operating Grants
Dr. Khaled Abdelrahman, Assistant Professor – was awarded a 5-year CIHR Project Grant ($803,250) to support his research on “The contribution of metabotropic glutamate receptor 5 to cerebral blood flow homeostasis in Alzheimer’s disease”
Dr. David Fedida, Professor – was awarded a 5-year CIHR Project Grant ($1,017,450) to support his research on “Mechanisms of potassium channel arrhythmias”.
Dr. Tillie-Louise Hackett, Professor – was awarded a 5-year CIHR Project Grant ($910,350) to support her research on “Integration of multi-resolution imaging to improve the diagnosis and treatment of fibrotic interstitial lung diseases”.
Department of Anesthesiology, Pharmacology & Therapeutics
Research Funding by Type, 2023/24 to 2024/25
3,500,000.00
3,000,000.00
2,500,000.00
APT Annual Research Day:
The APT Research Day is our annual event to showcase the Research excellence of fellows and trainees. This year marked the 18th Annual APT Research Day, held on May 14th 2024, at the BC Children’s Research Institute. The day was a great success thanks to the organizing committee led by Dr. Don Griesdale, Dr. John (Kip) Kramer, and Dr. Alana Flexman



Dr. Tillie Hackett
A Single-Cell Atlas of Small airway Disease in Chronic Obstructive Pulmonary Disease: A Cross-Sectional Study
Dr. Matthias Görges:
Dashboard of Short-Term Postoperative Patient Outcomes for Anesthesiologists: Development and Preliminary Evaluation
Objective: To review research currently conducted by graduate and post-graduate trainees and fellows in the Department of Anesthesiology, Pharmacology & Therapeutics at the University of British Columbia.
Winning Presentations:
Oral – Anesthesiology
Dallas Genereaux (Resident – Griesdale Lab )
Nicholas Ledlie (Clinical Fellow - BCWH)
Oral - Pharmacology & Therapeutics
Ryan Loke (Doctoral Student – Kramer Lab)
Lightning Talks
Ola (Alexandra) Lemanowicz – (Resident – Perry Lab)
David Olmstead – (Resident – Zoe Brown Lab)
Nikunj Patel – (Resident – Sekhon/Griesdale Lab)
Caelie Stewart – (Resident – Thornloe Lab)
Zeren Sun – (PCTH Graduate Student – Bernatchez Lab)
Innes Zuna – (Resident – Skelton Lab)
Dr. Colin Dormuth Co-Managing Director
The Therapeutics Initiative (TI) was established in 1994 at the University of British Columbia (UBC). The TI mission is to provide drug reviews, pharmacoepidemiological studies, as well as education and quality prescribing programs. It is supported by research grants, donations, an endowment and a shared cost agreement with the BC Ministry of Health (MoH) to the UBC.
Over the years, the TI has substantially enhanced its ability to assess the clinical evidence presented in published articles, meta-analyses by the Cochrane Collaboration and scientific material presented by the pharmaceutical industry. In pace with the extensive assessment of clinical evidence, the TI has also developed effective ways of knowledge translation and dissemination of this evidence to all active players involved in drug therapy: physicians, pharmacists, nurses, and drug policy at the MoH.
The TI is composed of 4 working groups that collaborate to prioritize topics, share in the assessment of evidence and disseminate findings. Activities of all TI working groups support priorities of the provincial Pharmaceutical Care Management Strategy and other health system objectives:
Drug Assessment Working Group (DAWG):
Assesses the clinical evidence of effectiveness and safety of new and existing drug therapies in the province and relate that evidence to the care of individual patients. This year the DAWG completed the following therapeutic reviews:

• GLP1a and SGLT2i for primary prevention of CVD in T2DM.
• GLP1a for alcohol use disorder and opioid use disorder.
• Triple therapy and dual bronchodilators as first-line therapy for COPD.
• Loop electrosurgical excision procedure (LEEP).
The DAWG provides problem-based learning opportunities regarding critical appraisal of clinical trials. Medical and pharmacy student trainees have attended the DAWG meetings where they learn to critically appraise systematic reviews and discuss the findings with the rest of the team.
Uses epidemiological methods to analyze linked administrative data to answer population-based questions which have not been adequately addressed in clinical trials. Projects include evaluation of drug policies and educational interventions, monitoring of drug utilization, and analysis of prescription drug safety and effectiveness. The PEG also helps design, deliver, and evaluate the Portrait program to improve the quality of prescribing in BC. Portrait provides primary care prescribers with a concise evidence overview, a comparison of their prescribing to peers or evidence-based targets, and advice about possible improvements to their prescribing.
In 2024, the PEG completed the following pharmacoepidemiological studies:
• Tafamidis effectiveness and safety realworld evaluation
• Paxlovid adverse drug events monitoring program analyses
• Smoking cessation program analyses
• Bisphosphonates utilization for primary prevention.
The PEG developed and distributed two prescribing portraits to physicians and nurse practitioners in BC:
• Thyroid lab testing
• Sedating medications
Provides health professionals with up-to-date, evidence based, practical information about rational drug therapy. The EWG held numerous educational events this year attended by over four thousand healthcare professionals in BC and across the world, highlights:
• BC Divisions of Family Practice in Comox, Nanaimo, and Langley.
• Vancouver Coastal Health- Mental health and substance Use Nurse Practitioners.
• Island Health Pharmacy Rounds.
• Peace Arch Hospital Grand Rounds.
• Bringing Best Evidence to Clinicians: Annual Therapeutics Initiative conference.
• BC Provincial Deprescribing webinar series to address undesirable polypharmacy effectively through responsible deprescribing.
• Best Evidence webinar series on various clinical therapeutics issues.
• Methods Speaker webinar series on topics related to systematic reviews, meta-analysis, methods and statistics in evidence synthesis.
The EWG also publishes the Therapeutics Letter that provides brief practical messages on how to deal with problematic therapeutic issues. All issues of the Therapeutics Letter are available on the TI website in English and Spanish.
Issue Number / Pub Date
TL 146 / February 2024
TL 147 / March 2024
TL 148 / April 2024
TL 149 / May 2024
TL 150 / July 2024
TL 151 / October 2024
Title
Apixaban is safer and more effective than rivaroxaban for nonvalvular atrial fibrillation
Screening to reduce fragility fractures: new trials, still ineffective
Rethink clindamycin for dental patient safety
How useful is Paxlovid in 2024?
Emergency contraceptives: Which pill will you recommend?
Minimizing harms of tight glycemic control in older people with type 2 diabetes
Website and Social Media: In 2024 the TI website received more than half a million visits, averaging 1,584 visits per day, with over 25 million “impressions” (number of times any page was viewed). The TI maintains Facebook and LinkedIn pages as well as two active X/Twitter profiles: TI (@DrugEvidence) and Cochrane Hypertension Group (@CochraneHTN) with a combined total of 13,488 followers. This year @ DrugEvidence has the most followers among all members of the International Society of Drug Bulletins
Prepares, maintains and promotes systematic reviews of the effects of healthcare interventions for hypertension. The scope of CHG includes randomized controlled trials of interventions evaluating blood pressure and clinical outcomes for the prevention and treatment of essential hypertension. Part of the international Cochrane Collaboration, the CHG published the following Cochrane systematic reviews in 2024:
Erviti J, Saiz LC, Leache L, Pijoan JI, Menéndez Orenga M, Salzwedel DM, Méndez-López I.
Blood pressure targets for hypertension in people with chronic renal disease.
Cochrane Database Syst Rev. 2024 Oct 15;10(10):CD008564.
doi: 10.1002/14651858.CD008564.pub3.
PMID: 39403990; PMCID: PMC11475354.
Wu C, Zhao P, Xu P, Wan C, Singh S, Varthya SB, Luo S-H. Evening versus morning dosing regimen drug therapy for hypertension.
Cochrane Review Update. Issue 2, 2024.
DOI: 10.1002/14651858.CD004184.pub3
Selected TI Publications:
Thompson W, Kim JD, Carney G, Otte J, Dormuth C. Changes in Sedative Use in British Columbia, Canada from 2012 to 2021: A Drug Utilization Study.
J Gen Intern Med. 2024 Oct 16.
doi: 10.1007/s11606-024-09065-2.
Epub ahead of print. PMID: 39414735.
Carney G, Maclure M, Patrick DM, Otte J, Ambasta A, Thompson W, Dormuth C. Pragmatic randomised trial assessing the impact of peer comparison and therapeutic recommendations, including repetition, on antibiotic prescribing patterns of family physicians across British Columbia for uncomplicated lower urinary tract infections.
BMJ Qual Saf. 2024 Oct 16:bmjqs-2024-017296.
doi: 10.1136/bmjqs-2024-017296.
Epub ahead of print. PMID: 39414374.
Wang Y, Spence L, Tung A, Bubbar CD, Thompson W, Tejani AM. Prescribing Portraits to Optimize Prescribing of Proton Pump Inhibitors in Long-Term Care: PPI-T STOP Study.
Can J Hosp Pharm. 2024 Mar 13;77(1):e3461.
doi: 10.4212/cjhp.3461.
PMID: 38482392; PMCID: PMC10914398.
Thompson W, McDonald EG. Polypharmacy and Deprescribing in Older Adults.
Annu Rev Med. 2024 Jan 29;75:113-127.
doi: 10.1146/annurev-med-070822-101947.
PMID: 37729029.
Ambasta A, Holroyd-Leduc JM, Pokharel S, Mathura P, Shih AW, Stelfox HT, Ma I, Harrison M, Manns B, Faris P, Williamson T, Shukalek C, Santana M, Omodon O, McCaughey D, Kassam N, Naugler C. Re-Purposing the Ordering of Routine Laboratory Tests in Hospitalized Medical Patients (RePORT): protocol for a multicenter stepped-wedge cluster randomised trial to evaluate the impact of a multicomponent intervention bundle to reduce laboratory test over-utilization.
Implement Sci. 2024 Jul 2;19(1):45.
doi: 10.1186/s13012-024-01376-6.
PMID: 38956637; PMCID: PMC11221016.
Pokharel S, Khawaja Z, Williams J, Mithwani AA, Strain K, Khanna P, Rychtera A, Kiryanova V, Tang K, Mathura P, Hylton C, Ambasta A. Patient perceptions of in-hospital laboratory blood testing: A patient-oriented and patient co-designed qualitative study.
Health Expect. 2024 Feb;27(1):e13880.
doi: 10.1111/hex.13880.
Epub 2023 Sep 26. PMID: 37751312; PMCID: PMC10726148.
Aeng ESY, Dhatt AK, Kim N, Tejani AM. Switching Topical Diclofenac from Higher to Lower Strength: Financial and Clinical Evaluation.
Can J Hosp Pharm. 2024 Jan 10;77(1):e3459.
doi: 10.4212/cjhp.3459.
PMID: 38204500; PMCID: PMC10754402.
Huyghebaert T, Svrcek C, Perry TL. How to navigate drug shortages with patients in primary care: Beneficial opportunities may exist beyond initial frustrations.
Can Fam Physician. 2024 Feb;70(2):85-86.
doi: 10.46747/cfp.700285.
The Chair is held by Professor Malcolm Maclure, ScD, a health services epidemiologist who uses BC’s population healthcare databases to improve prescribing safety and surgical safety.
As ex-officio member of the Council of Health Quality BC (HQBC), Dr. Maclure has witnessed how his development of metrics to support incremental improvements in rates of surgical site infections became temporarily out of alignment with the urgent needs of the BC healthcare system during the COVID-19 pandemic and afterwards, as the system struggled with staff shortages. At the same time, HQBC gave increasing attention to the harms of climate change on patient safety, such as wildfires threatening the city of Kelowna in 2023.
Following HQBC’s lead, Dr. Maclure pivoted in 2024 towards applying methods from the patient safety movement to the challenge of boosting climate action in healthcare and higher education systems. In preparation for a very active role as Emeritus Professor after June 2025, he began an international collaboration of academics
concerned about the unsustainability of those systems, with plans for a grant proposal to support action research on cutting emissions from flying.
He has maintained and will continue his participation in the Therapeutics Initiative, with special interest in its online confidential ‘Portraits’ of prescribing that compare individual prescribers’ personal patterns of prescribing, versus the average prescribing rates in similar practices. This is particularly relevant to patient safety in Dr. Dormuth’s grant proposal, “SelfAudit and Feedback using Electronic Records” (SAFER Rx), for which Dr. Maclure contributed to the resubmission.
In October, he completed the handover of the role of Co-Lead for the Patient Safety Theme in the Undergraduate Medical Curriculum, to a specialist in healthcare quality, supported by a patient safety activist who has built momentum into a restorative-justice approach to incidents of patient harm.

Publications:
Hallas J, Maclure M. Use of Point-in-Time or Window Approach in the Case-Crossover Design, Implications for Pharmacoepidemiologic Research Using Registries. Pharmacoepidemiol Drug Saf. 2024 Jun;33(6):e5850.
doi: 10.1002/pds.5850. PMID: 38887901.
Carney G, Maclure M, Patrick DM, Otte J, Ambasta A, Thompson W, Dormuth C. Pragmatic randomised trial assessing the impact of peer comparison and therapeutic recommendations, including repetition, on antibiotic prescribing patterns of family physicians across British Columbia for uncomplicated lower urinary tract infections.
BMJ Qual Saf. 2024 Oct 16:bmjqs-2024-017296.
doi: 10.1136/bmjqs-2024-017296. Epub ahead of print. PMID: 39414374.
Homayra F, Enns B, Min JE, Kurz M, Bach P, Bruneau J, Greenland S, Gustafson P, Karim ME, Korthuis PT, Loughin T, Maclure M, McCandless L, Platt RW, Schnepel K, Shigeoka H, Siebert U, Socias E, Wood E, Nosyk B. Comparative Analysis of Instrumental Variables on the Assignment of Buprenorphine/Naloxone or Methadone for the Treatment of Opioid Use Disorder.
Epidemiology. 2024 Mar 1;35(2):218-231.
doi: 10.1097/EDE.0000000000001697. Epub 2023 Jan 30. PMID: 38290142; PMCID: PMC10833049.
Lapointe-Shaw L, Salahub C, Austin PC, Bai L, Banwatt S, Berthelot S, Bhatia RS, Bird C, Desveaux L, Kiran T, Lofters A, Maclure M, Martin D, McBrien KA, McCracken RK, Paterson JM, Rahman B, Shuldiner J, Tadrous M, Terpou BA, Thakkar N, Wang R, Ivers NM. Characteristics of walk-in clinic physicians and patients in Ontario: Cross-sectional study.
Can Fam Physician. 2024 Oct;70(10):e156-e168.
doi: 10.46747/cfp.7010e156. PMID: 39406418; PMCID: PMC11477262.
Department Leadership
Peter Choi – Interim Department Head
Academic Leadership
Andrew Horne – Vice-Chair, Education
Alana Flexman – Vice-Chair, Equity, Diversity and Inclusion
Tillie-Louise Hackett – Vice-Chair, Research
Pascal Bernatchez – Basic Science Research Director
Don Griesdale – Clinical Research Director
Colin Dormuth – Co-Managing Director, Therapeutics Initiatives
Ken Bassett – Co-Managing Director, Therapeutics Initiatives
Stephan KW Schwarz – Dr. Jean Templeton Hugill Chair in Anesthesia (to 6/2024)
K Malcolm Maclure – BC Patient Safety Chair
Pascal Bernatchez – Director/Advisor, PCTH Graduate Program
Kalina Popova – Co-Director, Anesthesiology Undergraduate Education
Navraj Chima – Co-Director, Anesthesiology Undergraduate Education
Zoe Brown – Anesthesia Residency Program Director
Sadiq Abdulla – Anesthesia Residency Program Associate Director (to 2/2024)
Christopher Nixon-Giles - Anesthesia Residency Program Associate Director
Michael Butterfield – Pain Medicine Residency Program Director (to 9/2024)
Audrey Chen - Pain Medicine Residency Program Director
John McAlpine - Family Practice Anesthesia Residency Program Director
John Veall – Co-Director, Simulation Program
Taren Roughead – Co-Director, Simulation Program
Helen Parker - Faculty Development Chair
Paula Meyler – Visiting Professor & Continuing Professional Development Program Director
Su-Yin Macdonell and Sandra Kisilevsky - Whistler Anesthesia Conference co-chairs
Bali Dhaliwal – Clinical Faculty Advisory Committee Representative

Jens Lohser – Head, VGH/UBCH Department of Anesthesia & Perioperative Care
Jim Kim –Head, St. Paul’s Hospital Department of Anesthesia
Simon Whyte – Head, BC Children’s Hospital Department of Anesthesia
James Brown - Head, BC Women’s Hospital Department of Anesthesia
Kenneth Ryan – Head, Royal Columbian Hospital Department of Anesthesia
Feisal Mohamedali – Regional Head, Fraser Health Authority
Magda Lipowska – Head, Lions Gate Hospital Department of Anesthesia
Anup Navsarikar – Head, Richmond General Hospital Department of Anesthesia
Liz Chuah – Head, Burnaby General Hospital Department of Anesthesia
Mahalaxmi Iyer/Alex Vesely/Laila Karwa – co-Heads, Surrey Memorial Hospital
Parisa Soltani – Head, Chilliwack General Hospital Department of Anesthesia
Catherina Mattheus – Head, Abbotsford Regional Hospital & Cancer Centre
Desmond Sweeney – Head, Victoria General/Royal Jubilee Hospitals Department of Anesthesia
Duncan DeSouza – Head & Medical Director Kelowna General Hospital Department of Anesthesia
Willem Buys – Head, Vernon Jubilee Hospital Department of Anesthesia
Mark Edge – Head, Royal Inland Hospital Kamloops Department of Anesthesia
Andrea Steyn – Head, Penticton Regional Hospital Department of Anesthesia
Pal Dhadly – Head, University Hospital of Northern BC Department of Anesthesia
Division Heads
Alexander Wong – Division Heads, Regional Anesthesia
Juliet Atherstone – Division Co-Head, Cardiac Anesthesia
Anne-Marie Madden - Division Co-Head, Cardiac Anesthesia
Sandra Kisilevsky – Division Co-Head, Neuroanesthesia
William Rieley – Division Co-Head, Neuroanesthesia
James Brown – Division Head, Obstetric Anesthesia
Aaron MacInnes – Division Head, Pain Management (to 6/2024)
Simon Whyte – Division Head, Pediatric Anesthesia
Su-Yin Macdonell – Division Head, Perioperative Anesthesia
Chris Durkin – Division Co-Head, Thoracic Anesthesia
Travis Schisler – Division Co-Head, Thoracic Anesthesia

Dr. Siyana Kurteva
Assistant Professor, Tenure Track
Joined the Department – January 25, 2024
Serenity Aberdour – Clinical Instructor (Nanaimo Regional General Hospital)
Christie Addison – Clinical Instructor (Victoria General Hospital)
Colin Archer – Clinical Instructor (Royal Jubilee Hospital)
Juliana Barrera – Clinical Instructor (BC Women’s Hospital)
Garrett Barry – Clinical Assistant Professor (Royal Jubilee Hospital)
Shika Card – Clinical Instructor (St. Paul’s Hospital)
Jane Colish – Clinical Instructor (Nanaimo Regional General Hospital)
Michelle Correia – Clinical Instructor (BC Children’s Hospital)
Alexander Dotto – Clinical Instructor (Vancouver General Hospital)
Maurice Dunstan – Clinical Assistant Professor (Abbotsford Regional Hospital)
Joshua Frohlich – Clinical Instructor (Surrey Memorial Hospital)
Katrina Genuis – Clinical Instructor (North Island Hospital – Comox Valley)
Steven Green – Clinical Assistant Professor (Royal Columbian Hospital)
Cassian Horoszczak – Clinical Instructor (University Hospital of Northern British Columbia)
Kelly Heape – Clinical Instructor (Royal Columbian Hospital)
Stephen Ryan Heape – Clinical Instructor (Royal Columbian Hospital)
Talon Jones – Clinical Instructor (Penticton Regional Hospital)
Jiin Kim - Clinical Instructor (Surrey Memorial Hospital)
Naima Kotadia – Clinical Instructor (Vancouver General Hospital)
Katherine Lanigan – Clinical Instructor (BC Children’s Hospital)
Kaixuan Kate Liu – Clinical Instructor (Nanaimo Regional General Hospital)
Annabelle Mang – Clinical Instructor (Kamloops Royal Inland Hospital)
Jason McVicar – Clinical Assistant Professor (Kamloops Royal Inland Hospital)
Stephen Miazga – Clinical Instructor (Vancouver General Hospital)
Ibrahim Mohamed – Clinical Instructor (Abbotsford Regional Hospital)
Nicole Quigley – Clinical Instructor (Saanich Peninsula Hospital)
Ilana Sebbag – Clinical Associate Professor (BC Women’s Hospital)
Kamal Sidhu – Clinical Instructor (Surrey Memorial Hospital)
Drayton Trumble – Clinical Instructor (Vancouver General Hospital)
Mike van der Westhuizen – Clinical Instructor (Victoria General Hospital)
Benjamin Walker – Clinical Instructor (University Hospital of Northern British Columbia)
Lynne Williams – Clinical Instructor (Kamloops Royal Inland Hospital)
Cameron Williams – Clinical Instructor (Royal Columbian Hospital)
Kyle Wilson – Clinical Instructor (Nanaimo Regional General Hospital)
Cynthia Ming Wai Wong – Clinical Instructor (Royal Columbian Hospital)

In fond remembrance of the cherished friends and colleagues we mourned in 2024.



Promotion from Clinical Instructor to Clinical Assistant Professor
Young-Don Brendon Chung – Vancouver General Hospital
Mark Edge – Kamloops Royal Inland Hospital
Sherif Eskandar – Surrey Memorial Hospital
Claire Fast – Lion’s Gate Hospital
Julena Foglia – Vancouver General Hospital
Peter Gajecki – Surrey Memorial Hospital
Christine Marie Graf - Surrey Memorial Hospital
Asim Iqbal – Vancouver General Hospital
Elizabeth Jacobs – Kamloops Royal Inland Hospital
Michael Jew – St. Paul’s Hospital
Shamir Karmali – Vancouver General Hospital
Salma Ketabi – Surrey Memorial Hospital
Kelvin Kwan – Richmond Hospital
Aidan Lee – Surrey Memorial Hospital
Pawel Martinka – Royal Columbian Hospital
Disha Mehta – Surrey Memorial Hospital
Lelanè Mostert – Kamloops Royal Inland Hospital
Victor Tran – Vancouver General Hospital
Matthew Turnock – Royal Columbian Hospital
Charles Vincent Yu – St. Paul’s Hospital
Promotion from Clinical Assistant Professor to Clinical Associate Professor
Lynn Rudner Correll – BC Children’s Hospital
Kevin F. Froehlich – Vancouver General Hospital
Susan Lee – Royal Columbian Hospital
Kenneth Ryan – Royal Columbian Hospital
Teresa Skelton – BC Children’s Hospital
Promotion from Clinical Associate Professor to Clinical Professor
Chris Chin – BC Children’s Hospital
Yvonne Csanyi-Fritz – BC Children’s Hospital

Anesthesia Residents
Dr. Serenity Aberdour
Dr. Hamish Bodnar
Dr. Émilie Chan
Dr. Akal Grewal
Dr. Rachel Guo
Dr. Vivien Hu
Dr. Jack Huang
Dr. Talon Jones
Dr. Jiin Kim
Dr. Mario Kovacevic
Dr. Vlad Kovalik
Dr. Amir Siddiqui
Dr. Kamal Sidhu
Dr. Kresimir Ukalovic
PCTH Doctoral Students
Dr. Kingsley Okechukwu Nwozor
Dr. Elodie Sauge
Dr. Kauna Usman
PCTH Masters Students
Rishika Daswani
Yuxi Wei
Tony Zhou
Family Practice Anesthesia Residents
Dr. Ardalan Ahmadi
Dr. Kathryne DesAutels
Dr. Herman Johal
Dr. Nick Lyu
Dr. Manpreet Ruprai
Dr. Mario Rotundo
Pain Medicine Residents
Dr. Jeremy Murray-Guenther
PCTH Undergraduate Students
Parsa Alizadeh
Tejveer Atwal
Pamela Bai
Keren Chen
Tim Chin-Yueh Cheng
Eric Cheuk
Katherine Feng
Nathan Zai Yu He
Miyuki Hui
Roy Jui Yi Hung
Janell Ko
Henry Zi Han Li
Elaine Ling
Jessica Liu
Joshua Liu
Harsirat Naraina
Saina Nemati
Selina Eunyoung Park
Sabrina Rai
Xindi Wang
Catherine Xu
Eleen Qiuyu Yang
Jenicia Zhen

Dr. Richard Alexander – Clinical Assistant Professor Faculty of Medicine Clinical Faculty Award for Excellence in Clinical Teaching – Early Career for 2024
Dr. Mark Ansermino – Professor 2024 J.S. Gravenstein Award at the Society for Technology in Anesthesia
Dr. Laine Bosma – Clinical Associate Professor 2024 Canadian Association of Medical Education Certificate of Merit
Dr. John Bowering – Clinical Professor

VGH – Stephen Miazga
SPH – John Bowering, Trina Montemurro
RCH – Matthew Turnock; Shelley Tweedle
BCCH – Michael Barker
BCWH – Anthony Chau
Secondary Site: (Surrey) Aidan Lee, Christine Graf; (Victoria) Mark Vu; (Burnaby) Reza Faraji
Rural/Community – (Nanaimo) – Sarah Hall
Medicine – (Critical Care) – Donald Griesdale
Dr. Pieter Swart Resident Appreciation Award – John Veall
FPA Master Teacher Award – (Campbell River) Christopher Pollitt
FPA Master Teacher Award – (Terrace) Derek Sargent
FPA Master Teacher Award – (Whitehorse) Kathleen Dalinghaus

Anesthesiology Residents
Dr. Derek Daniel Wolney Prize for Clinical Proficiency – Jiin Kim
Dr. John A. McConnell Award for Academic Excellence – Kres Ukalovic
Dr. Jone Chang Memorial Award in Anesthesiology Excellence – Émilie Chan
Dr. Jone Chang Memorial Prize in Chronic Pain – Émilie Chan
Ken C.K. Wong Award for Clinical Teaching – Hamish Bodnar
UBC APT Advanced Simulation Training Program – Maya de Vos, Caroline Gardiner, Blake Birnie, Claire Moura, Brandon Evtushevski
Dr. Dimitri Giannoulis Memorial Award in Regional Anesthesia – Kimberly Li
Dr. Keith Mills Award for Excellence in Neuroanesthesia – Ben Chen
Dr. Keith Mills Bursary for Excellence in Neuroanesthesia Studies – Ben Chen
VGH Pieter Swart Award for Clinical Excellence and Collegiality – Robertson Venema
BCAS Resident Award for Physician Leadership – Émilie Chan
Dr. Anthony Boulton Award for FPA Clinical Excellence – Herman Johal
Dr. Paul Kliffer Golden Epidural Award – Kyra Moura (Jr. Resident); Amir Siddiqui (Sr. Resident);
Dr. Michael Smith Award for Pediatric Anesthesia – Mario Kovacevic


Esther Anderson Memorial Prize (highest graduating average in Honors Pharmacology)
No eligible PCTH student for award in 2024
Prakash Gill Memorial Prize (highest graduating average in Majors Pharmacology)
Pamela Bai
Thomas L. Perry Memorial prize in Medical Pharmacology
Shared by 5 Medical students (May 2024) – Nicka Kalaydina, Sarah Keyes, Hana Brath, Chiara Piccolo, Connor Harrigan
Pharmacology & Therapeutics Graduate Students
Sacks Prize (Best presentations)
Rishika Dawani (MSc student); Aileen Hsieh (PhD student) – May 2024
Leighton Pharmacology Graduate Award
Jia He Janet Zhang (MSc student); Aileen Hsieh (PhD student) – May 2024
CIHR-CGSM 1-Year Award
Jia-He (Janet) Zhang, MSc student (2023 Sept – 2024 August)
Jodi Anderson (2024 Sep – 2025 Aug); Raveen Badyal (2024 Sep – 2025 Aug)
CIHR-CGSD 3-Year Award
Aileen Hsieh, PhD student (2023 May – 2026 April)
