UAB alumnus/student/employee becomes patient following brain blood clot
Written by: Anna Waters
Media contact: Bob Shepard, bshep@uab.edu
Die-hard University of Alabama football fan Michel Thomas would not have missed the 2016 SEC championship game — the Florida Gators against his Crimson Tide for anything. Although he had spent the days before the game suffering from debilitating headaches and would spend the week after too nauseated to participate in final exams or project meetings with his classmates, Thomas made it to the Georgia Dome on Dec. 3, 2016, with his co-worker of 14 years, Tracy Taylor, R.N., nurse to UAB neurosurgeon Mark Harrigan, M.D.
Unbeknownst to both of them, Thomas attended

that game with a blood clot inhis brain,andHarriganwould later bethe one to remove it.
“I willsay I was pretty miserableduring thegame,” saidThomas, a business officer inthe UAB Department of Neurosurgery.“Iremember cheeringduringthefirstquarter during a turnover and thinking my head was going to explode.”
After nearlya week of constant headaches andnausea, Thomas — a UAB alumnus and a Master of Science inHealth Informatics studentinthe UAB School ofHealth Professions — finally sought treatmentat UAB Medicine UrgentCare for what he thought were common migraines.
“That Monday, after I quitthrowing up,I remember getting into the car to goto work, realizing I didn’t have my wallet, going backinside andthen going back to thecar just to realize I stilldidn’t have my wallet,”Thomas said. “By that point,itwas day five,and I was still having theseheadaches.Attheinsistence ofmyprimary care physician, Dr. Amy Lejeune,I decided to goto urgentcare,thinking that they would just giveme a migraine cocktail so I couldgoback to work and then gohome.”
Andrew Allen, M.D., thedoctor Thomas saw aturgentcare,says hecouldtellsomething was seriously wrong themoment hewalked in.
“Michel saidhewent to anAlabama footballgame the weekendbefore,and itseems likehis clot was expanding during thatgame,” Allen said. “He was complaining of a lot of intermittent headaches and vomiting,which wasa redflag for me.Initially,theintensity and localization of those headaches made meconcerned about an aneurysm.”
Allen immediatelysent Thomas to the emergency room,where a CTscan showed not ananeurysm but a blood clot. Thatnight,Thomas wasadmitted tothe hospital under thecare of Winfield Fisher, III,M.D., a UAB neurosurgeonwithwhom Thomas worked. Atthehospital, Thomaslearned that his most severe headaches andvomiting,as well ashis current, persisting symptoms,were due toa brain bleed anda blood clot inhis duralvenous sinuses,which drain bloodfrom the brain.Intracranial venous sinus thrombosis,as it iscalled, is a rare disorder that,inthiscase,was caused by a factor V Leiden deficiency,a hereditary hypercoagulability disorder.
“The symptoms of my condition were similarto thoseof an aneurysm; buta lot of people who have this kind of clot actually havestrokes, so I got lucky with a bleed instead,”Thomas said. “Eitherway,they’re bad; but the urgent care doctorgot meto the ER quickly.”
Angiogram images show blood vessels following thrombectomy and treatment with blood thinners.
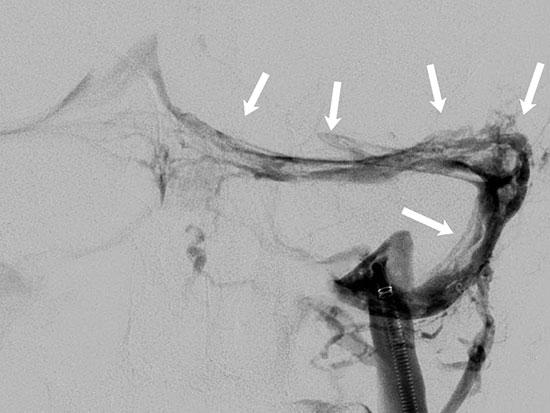
The arrows indicate scattered blood clots present throughout the venous system, which were diminished in size and extent after treatment.Fisher initially treated Thomas’ blood clots with blood thinners, hydration and pain
medication, which Fisher hoped would dissolve the blood clot and ease Thomas’ symptoms Because Thomas was in the hospital during finals, the School of Health Professions allowed him to take one of his finals on paper rather than on a computer screen, which caused him fewer headaches. However, even after he returned to work part time at the end of December, his headaches were still severe and frequent It was then that he went back to the ER and started to consider surgery to remove the clot.
The second time Thomas was admitted to the hospital, he was met by Harrigan, who suggested a thrombectomy, a procedure in which neurosurgeons lead a plastic catheter from the femoral vein in the leg to the venous sinuses in the head and then pull the blood clot out using a mechanical aspirator.
“This technique has come on the scene in the last six or eight years as a therapy for acute stroke, but we use it for intracranial venous sinus thrombosis as well,” Harrigan said “That system has certain design features that make it very useful for Michel’s condition.”
Thomas says his experience as a Department of Neurosurgery staff member helped him navigate the ins and outs of a neurosurgical procedure but didn’t prepare him for the experience of being the one in the hospital bed
“I already knew a little bit about the process from working in the hospital and directly with neurosurgeons, but it’s different when you’re the patient,” Thomas said.
Harrigan performed Thomas’ thrombectomy on New Year’s Eve, removing much of the blood clot and alleviating some of Thomas’ symptoms.

UAB neurosurgeonsWinfield Fisher and MarkHarrigan.
However, after three months,Thomaswasstillsufferingfrom severe,frequent headaches and light sensitivity that were interferingwithhis life.Part of theblood clot was still present inhisvenous sinuses, andthe samepainthat had followed him since December wasmaking it difficultfor him towork or gotoschool full time.When he discussed theseongoing symptoms withHarrigan, they began toconsider another thrombectomy to remove theremainder of the bloodclot.
“Wehave to relyon his opinion,”Harrigansaid. “In the old days,weused to reserve this for people who were getting really sick, like going into a comaorthingslikethat, and in that case,theneurologicchangeismore objective.But withthe bad headaches Michel was having,it’ssubjective.Wehad to relyon him totellushow bad his headaches were.”
Finally, Thomas’ second thrombectomy,onMarch 6, 2017, removed the entire clot and relieved mostof his symptoms.
“Weused thelargestof the catheters, called an ACE68,” Harrigansaid. “It’slikea great big straw, but bigger and longer.”
Thomassays hehas feltmarkedlybetter since his secondsurgery and has resumed his work and classes full time.
“I never fell behind in academics, thanks to the School of Health Professions, and I’m so grateful to them for working with me through all this,” Thomas said. “My co-workers were also just really supportive when I had to stay home or leave for doctors’ appointments, and I know that would have been the case even if I weren’t being treated by the faculty members in my department.”
Eta S. Berner, Ed.D., one of Thomas’ professors in the School of Health Professions, says she was impressed by his diligence in completing his coursework while he was in and out of the hospital.
“This is a disease that seems to affect younger people more than older people. We’ve done a lot of these procedures on people in their 20s or 30s”
“Michel was very conscientious in making up the work, even though he was still sick and had to manage the regular course workload as well,” Berner said “He did very well in the course, even with all that stress.”
While Thomas’ quality of life has been drastically improved, he still sees several UAB specialists to manage his headaches and is aware that this doesn’t mean he will remain blood-clot-free.
“He’s young; but he’s still at risk for recurrence of the blood clots in his head and for developing blood clots in other veins in his body, too,” Harrigan said. “This is a disease that seems to affect younger people more than older people We’ve done a lot of these procedures on people in their 20s or 30s.”
Harrigan explained that, while treating a co-worker is a different experience for him, he’s thankful to have had the opportunity to spend more time with Thomas during his recovery, and that Thomas has returned to work
“Because Michel is a colleague and friend, I see him a lot more frequently than I see other patients,” Harrigan said. “As his neurosurgeon, it is rewarding to see Michel successfully back in his daily routine.”
