ACG MAGAZINE
MEMBERS. MEDICINE. MEANING.




ACG Weekly Virtual Grand Rounds
ACG Weekly Virtual Grand Rounds
2024
2024 ACG’s IBD School & Eastern Regional Postgraduate Course
2024 ACG’s IBD School & Eastern Regional Postgraduate Course
June 7–9, 2024
June 7–9, 2024
The Capital Hilton, Washington, DC
The Capital Hilton, Washington, DC
2024 ACG’s Hepatology School & Midwest Regional Postgraduate Course
REGISTER NOW: GI.ORG/ACGVGR
REGISTER NOW: GI.ORG/ACGVGR
ACG VGRs are offered TWICE each Thursday, with a live broadcast at noon (ET) followed by an 8:00pm (ET) rebroadcast!
ACG VGRs are offered TWICE each Thursday, with a live broadcast at noon (ET) followed by an 8:00pm (ET) rebroadcast!
2024 ACG’s Hepatology School & Midwest Regional Postgraduate Course
August 23–25, 2024
August 23–25, 2024
Radisson Blu Mall of America, Minneapolis, MN
Radisson Blu Mall of America, Minneapolis, MN
2024 ACG’s Functional GI & Motility Disorders School & ACG/VGS/ODSGNA Regional Postgraduate Course

2024 ACG’s Functional GI & Motility Disorders School & ACG/VGS/ODSGNA Regional Postgraduate Course
September 6–8, 2024
September 6–8, 2024
Williamsburg Lodge, Williamsburg, VA
Williamsburg Lodge, Williamsburg, VA
ACG 2024 Annual Scientific Meeting and Postgraduate Course
October 25–30, 2024
ACG 2024 Annual Scientific Meeting and Postgraduate Course
October 25–30, 2024
Pennsylvania Convention Center, Philadelphia, PA
Pennsylvania Convention Center, Philadelphia, PA
2024 ACG’s Functional GI and Motility Disorders School & Southern Regional Course

December 6-8, 2024
2024 ACG’s Functional GI and Motility Disorders School & Southern Regional Course
December 6-8, 2024
Renaissance Nashville, Nashville, TN
Renaissance Nashville, Nashville, TN


PUBLIC POLICY
A recap of ACG's 2024 Advocacy Day, featuring ACG Governors and Early Career Leadership Program participants meeting with Members of Congress on Capitol Hill.
PAGE 23
With massive advancements in AI rapidly influencing almost every aspect of healthcare, what does this mean for the future of gastroenterology? The answers may be surprising.
26
CONVERSATIONS WITH WOMEN IN GI Dr. Jill Gaidos in conversation with Dr. Sara Horst on EMR optimization and improvement.
PAGE 37

ACG members and GI practices continue to face mounting financial and reimbursement pressures. Complex coding and documentation requirements only add to these burdens. The ACG Practice Management Committee is pleased to announce the new member benefit: professional coding and documentation assistance for ACG members, tailored to your individual practice’s questions and needs.

Arlene Morrow, CPC, CMM, CMSCS, is now available to answer your questions!
ACG members will receive an answer and guidance within a few business days.


“Ironically, in an era of AI-enabled gastroenterology, there has never been a greater need to learn and perfect an age-old technique: laying hands on the patient.”
—Brennan Spiegel, MD, MSHS, FACG, “AI in GI: Navigating the New Frontier of Digestive Health” PG 26
6 // MESSAGE FROM THE PRESIDENT
Dr. Jonathan Leighton on facing headwinds and being prepared for what's to come in GI
7 // NOVEL & NOTEWORTHY
CRC Awareness Month highlights, recent leadership and mentoring programs, a tribute to the late Rep. Donald Payne, Jr. (D-NJ), ACG member accomplishments & more
8 // GI EYE
Dr. Alan Sloyer's photo "Balloon Over Bagan" sharing his view while floating over Myanmar
15 // TRAINEE HUB
Dr. Katie Dunleavy interviews colorectal cancer survivor, educator, and patient advocate Allison Rosen
19 // GETTING IT RIGHT
Dr. Jose Nieto on GI locum tenens opportunities, pearls, and pitfalls
23 // PUBLIC POLICY
Highlights from ACG's 2024 Advocacy Day on Capitol Hill
26 // COVER STORY
AI IN GI: NAVIGATING THE NEW FRONTIER OF DIGESTIVE HEALTH
Dr. Brennan Spiegel on the exponential growth of artificial intelligence and its role in GI
33 // ACG PERSPECTIVES
33 CULINARY CONNECTIONS
Culinary Connections section editors provide recipes to start your summer
37 CONVERSATIONS WITH WOMEN IN GI
Dr. Jill Gaidos in conversation with Dr. Sara Horst on EMR optimization and improvement
41 VIRTUAL HAPPY HOURS IN GI FELLOWSHIP RECRUITMENT
A reflection on Mayo Clinic's virtual happy hours for GI fellowship recruitment
45 TRAIN THE TRAINERS
Dr. Vivek Kaul, Dr. David Dulaney, and Dr. Shivangi Kothari on the recent Train the Trainers program in Kolkata, India
49 // INSIDE THE JOURNALS
50 AJG
From Shadows to Spotlight: Exploring the Escalating Burden of Alcohol-Associated Liver Disease and Alcohol Use Disorder in Young Women by Danpanichkul, et al
50 CTG
Clinical Outcomes Before and After Prucalopride Treatment: An Observational Study in Patients with Chronic Idiopathic Constipation by Lembo, et al
50 ACGCRJ
Progesterone-Only Contraceptive-Induced Ischemic Colitis by Rajamanuri, et al
51 // REACHING THE CECUM
51 PATIENT HANDOUT: BARRETT'S ESOPHAGUS
A patient handout about Barrett's esophagus from the ACG Patient Care Committee
52 ACG GUIDELINE HIGHLIGHTS: ACUTE PANCREATITIS
A visual summary of ACG's 2024 Clinical Guidelines on Acute Pancreatitis
Executive Director Bradley C. Stillman, JD
Editor in Chief; Vice President, Communications Anne-Louise B. Oliphant
Manager, Communications Becky Abel
Art Director Emily Garel
Senior Graphic Designer Antonella Iseas
President: Jonathan A. Leighton, MD, FACG
President-Elect: Amy S. Oxentenko, MD, FACG
Vice President: William D. Chey, MD, FACG
Secretary: Nicholas J. Shaheen, MD, MPH, MACG
Treasurer: Costas H. Kefalas, MD, MMM, FACG
Immediate Past President: Daniel J. Pambianco, MD, FACG
Past President: Samir A. Shah, MD, FACG
Director, ACG Institute: Neena S. Abraham, MD, MSc, MACG
Co-Editors, The American Journal of Gastroenterology:
Jasmohan S. Bajaj, MD, MS, FACG
Millie D. Long, MD, MPH, FACG
Chair, Board of Governors: Dayna S. Early, MD, FACG
Vice Chair, Board of Governors: Sita S. Chokhavatia, MD, MACG
Trustee for Administrative Affairs: Irving M. Pike, MD, FACG
Jean-Paul Achkar, MD, FACG
Brooks D. Cash, MD, FACG
Jill K. J. Gaidos, MD, FACG
Seth A. Gross, MD, FACG
David J. Hass, MD, FACG
James C. Hobley, MD, MSc, FACG
Aasma Shaukat, MD, MPH, FACG
Neil H. Stollman, MD, FACG
Renee L. Williams, MD, MHPE, FACG
Patrick E. Young, MD, FACG
youtube.com/ACGastroenterology
facebook.com/AmCollegeGastro
twitter.com/amcollegegastro
instagram.com/amcollegegastro bit.ly/ACG-Linked-In
IDEAS & FEEDBACK
We'd love to hear from you. Send us your ideas, stories and comments. ACGMag@gi.org
CONTACT ACG
American College of Gastroenterology 11333 Woodglen Drive, Suite 100 North Bethesda, MD 20852 (301) 263-9000 | gi.org
DIGITAL EDITIONS
GI.ORG/ACGMAGAZINE


American College of Gastroenterology is an international organization with more than 18,000 clinician members representing some 86 countries. The College's vision is to be the pre-eminent professional organization that champions the evolving needs of clinicians in the delivery of high-quality, evidence-based and compassionate health care to gastroenterology patients. The mission of the College is to advance world-class care for patients with gastrointestinal disorders through excellence, innovation and advocacy in the areas of scientific investigation, education, prevention and treatment.

David T. Dulaney, MD
Dr. Dulaney is Director of the Gastroenterology Fellowship Program at San Antonio Uniformed Services Health Education Consortium (SAUSHEC) at Fort Sam in San Antonio, TX. He currently serves on ACG’s Training and Educational Affairs Committees.

Katie A. Dunleavy, MB, BCh, BAO
Dr. Dunleavy is a third-year GI fellow at Mayo Clinic Rochester. She is editor of the Trainee Hub section of ACG MAGAZINE and is a member of ACG’s Digital Communications and Publications Committee.

Jill K.J. Gaidos, MD, FACG
Dr. Gaidos is a Trustee of the College and Associate Professor at the Yale School of Medicine Section of Digestive Diseases and Director of Clinical Research for the Yale IBD Program. She is a member of ACG’s Digital Communications and Publications Committee.


Khushboo Gala, MBBS
Dr. Gala is Chief GI Fellow at Mayo Clinic Rochester. She currently serves as Co-Editor-in-Chief of ACG Case Reports Journal
Sara N. Horst, MD, MPH, FACG
Dr. Horst is Assistant Vice Chair for Digital Health Operations for the Department of Internal Medicine and Health IT Clinical Director for Vanderbilt University Medical Center. She currently serves on ACG’s Women in GI Committee.

Vivek Kaul, MD, FACG
Dr. Kaul is the Segal-Watson Professor of Medicine at the University of Rochester Medicine in Rochester, NY. He is currently Secretary General of the World Gastroenterology Organisation and serves on ACG’s International Affairs Committee.

Shivangi T. Kothari, MD, FACG
Dr. Kothari is Associate Professor of Medicine and Associate Director of Endoscopy at the University of Rochester Medicine in Rochester, NY. She currently serves as ACG Governor for Northern New York and on ACG’s Awards and Educational Affairs Committees.


Jonathan A. Leighton, MD, FACG
ACG President Dr. Leighton is Professor of Medicine at Mayo Clinic Arizona. He also chairs Mayo Clinic Arizona’s Office of Joy and Well-being.
Jose M. Nieto, DO, FACG
Dr. Nieto is a gastroenterologist at Digestive Disease Consultants in Jacksonville, FL. He currently serves as ACG Governor for Northern Florida and on ACG’s Legislative and Public Policy Council and Membership Committee.






Vani Paleti, MD, Dip ACLM, Dip ABOM
Dr. Paleti is a gastroenterologist at Baylor, Scott & White Health in Killeen, TX, with a special interest in lifestyle and obesity medicine.
Alexander Perelman, DO, MS
Dr. Perelman is a gastroenterologist at Vanguard Gastroenterology in New York City. He currently serves on ACG’s Professionalism Committee.
Allison Rosen, MS
Allison Rosen is a stage 2C colorectal cancer survivor and fierce patient advocate. She is the Director of Project ECHO at the American Cancer Society, focusing on colorectal cancer prevention.
Douglas A. Simonetto, MD
Dr. Simonetto is GI Program Director and Associate Professor of Medicine at Mayo Clinic Rochester.
Alan F. Sloyer, MD, FACG
Dr. Sloyer is Associate Professor of Medicine at the Zucker School of Medicine at Hofstra/Northwell and a founding member of North Shore Gastroenterology Associates in Great Neck, NY.
Brennan M.R. Spiegel, MD, MSHS, FACG
Dr. Spiegel is Director of Health Services Research for Cedars-Sinai, Director of the Cedars-Sinai Master's Degree Program in Health Delivery Science, and Assistant Dean of Clinical and Translational Science in the David Geffen School of Medicine. He is a past Co-EIC of the Red Journal.




Christina A. Tennyson, MD
Dr. Tennyson is a gastroenterologist at Augusta Healthcare in Fishersville, VA, with expertise in integrative, lifestyle, and culinary medicine.
June Tome, MD
Dr. Tome is a GI fellow at Mayo Clinic Rochester. She currently serves on ACG’s Training Committee.
Elida Voth, MD
Dr. Voth is a GI and hepatology fellow at Mayo Clinic Rochester.
Xiao Jing “Iris” Wang, MD
Dr. Wang is Associate GI Program Director and Assistant Professor at Mayo Clinic Rochester. She currently serves on ACG’s Educational Affairs and Training Committees.
I HOPE YOU ALL ARE HAVING A WONDERFUL SPRING, WHEREVER YOU ARE! I am still enjoying the success of our ACG Fly-In and Advocacy Day that was held in Washington, DC, on April 18 and 19. The ACG Board of Governors, under the leadership of Dr. Dayna Early and Dr. Sita Chokhavatia, joined by Dr. Louis Wilson, Chair of our ACG Legislative and Public Policy Council, and the Early Career Leadership cohort under the leadership of Dr. Elizabeth Paine and Dr. Allon Kahn met with Members of Congress. The ACG Fly-In and Advocacy Day is a good example of how we all can work together and speak with one voice. ACG’s tremendous potential was unleashed on Capitol Hill in a powerful show of what we can all do together if we set our minds to it. I invite you to read more about this meaningful experience on pages 23 to 25.
Declining reimbursement, increased regulation, prior authorization, noncompete clauses, workforce shortages, and increasing consumer demand – to name a few – are the headwinds facing our profession. Waste in the U.S. health care system is enormous and accounts for 25% of health care spending. Physicians are reacting to this economic reality. This in turn has led many gastroenterologists into early retirement, locum tenens, or exploring a variety of other practice models including hospital-based systems and private equity.
Burnout among U.S. gastroenterologists and fellows is significant, with an overall prevalence of 49%. This has been documented in academic institutions as measured by Intention to Leave. Factors include lack of professional fulfillment, the electronic health record, patient-related
work after hours, busy inpatient consult services, and hospital call. All of these issues are exacerbated if there are children at home and vacation time is not taken. Studies show that there are both personal and system-based factors that play a role and all of these need to be addressed in a comprehensive approach.
This comprehensive approach starts with taking care of ourselves and our loved ones. I am reminded of the prediction in 1930 by the economist John Maynard Keynes that in 100 years his grandchildren would only need to work 15-hour weeks because of advances in science, technology, and compound interest. He believed our biggest problem would be how to use this leisure time. His prediction, unfortunately, does not appear to be accurate. Research suggests that leisure time is dwindling as people work harder to make ends meet and cell phones and laptops make it nearly impossible to escape work. Even though there is evidence that time off from work improves productivity and reduces burnout, this appears to be happening less in many situations. Chris Murphy and Tim Ryan, two U.S. Congressman, describe it as, “America is facing a spiritual crisis: a lack of meaning, identity, and belonging.” We have to fix this as quickly as possible. In our practices, we must optimize employee well-being. Leonard Berry, Professor of Marketing at Texas A&M, said it eloquently, “Generosity is a service organization’s most powerful opportunity to excel. Being generous with employees strengthens their sense of community, security, loyalty, and trust, and inspires them to go the extra mile to serve others.” It is critical that we improve employee experience, improve the
“...[W]e must understand that what made us successful today may not be enough to keep us there tomorrow.”
patient experience, simplify, and make efficient workflows and processes. I believe it is the moral obligation as an employer and it is critical to support leadership objectives. There are financial benefits to this as well. For our trainees, the future of our profession, it is critical that they get involved in their national societies, such as the American College of Gastroenterology. The opportunities are endless in terms of networking, mentorship, education, leadership, and advocacy. There are also opportunities for scholarship, training, and skill advancement, building your community, and just having fun!
In addition to taking care of ourselves and our staff, we must create an environment of innovation to improve productivity and we need to develop highly functioning care teams to support each other. We also need to address issues around sustainability and reducing waste in our practices.
Moreover, we must understand that what made us successful today may not be enough to keep us there tomorrow. We will need to respond to the changes ahead of us. With regard to an evolving workforce, we will need to prepare ourselves for workforce shortages, more flexible schedules, more mobile employees, and an increasingly fragmented workforce. A new “people strategy” will be imperative and our healthcare environment will need to be flexible and nimble to meet the changing needs. Finally, with technology advancing at warp speed, we will need to adjust to a bionic workforce and expect skepticism about the risks and benefits of this technology. We must always realize that healthcare is deeply personal, medicine will always be an art, and we must ensure that we as medical professionals do what only humans can do.
The future is exciting, and we must look at the challenges ahead as opportunities to improve. Together we can do so much to create a healthcare system that is lean, innovative, and patient-centered. I look forward to seeing you all soon!

SPRING IS A BUSY SEASON FOR ACG with March Colorectal Cancer Awareness Month and ACG Advocacy Day in Washington, DC. The ACG Board of Governors were joined by participants in the ACG Institute’s Early Career Leadership Program for a day on Capitol Hill. Read more about Advocacy Day on PG 23. N&N celebrates the accomplishments of the ACG family and recognizes professional achievements and contributions to the College, to gastroenterology, and to the world. Send your news to acgmag@gi.org
A short caption about the location:
Bagan is an ancient city and a UNESCO World Heritage Site in the Mandalay Region of Myanmar. Bagan is famous for its historical monuments and houses, with around 2,000 monuments from different periods. It is the most important historical site in Myanmar and it is awe-inspiring, especially from the air.
What equipment did you use?
Sony A7R4 Mirrorless Camera, Sony FE4/24-105 lens. The image was processed in Adobe Lightroom and Photoshop.
What captured your attention?
Many varieties of Buddhist temples close together in a magical setting.
Any technical challenges? It is hard to get sharp images from a moving object such as a hot air balloon.
Discuss the personal significance of this photo or photography in general, reflecting briefly upon why you pursue photography as a hobby and personal passion: I have been extremely fortunate to have had opportunities to travel around the world to unique destinations and have experienced adventures in more than 75 countries, on all seven continents, over the past five decades. I enjoy travel,

landscape, and street photography. I have been fortunate and blessed to have the opportunity to travel and learn and interact with the people inhabiting the wonderful world around us. It seems trite, but one constant throughout all the locations and years of travel is that no matter where we live or how we look, we are all the same.
My photos have appeared in
many notable publications, including The New York Times, New England Journal of Medicine, Photoshop User Magazine, Chronos, Annals of Internal Medicine (cover photo), and Shutterbug magazine.

I am an Associate Professor of Medicine at the Zucker School of Medicine at

Hofstra/Northwell and a proud founding member of North Shore Gastroenterology Associates, a private gastroenterology practice in Great Neck, New York, for more than 30 years. We are now a division of Allied Digestive Health, an integrated network of gastroenterology care centers of almost 200 physicians in New York and New Jersey.
I have been a member of the ACG for almost 40 years and I am a strong advocate for screening and early detection of colon cancer. A few years ago, I received a SCOPY award for work done to raise money and awareness for colon cancer screening during 10 years of Spinathon events on Long Island. I applaud the ACG for all
the work you have done in this area over the years, as well as for being a pragmatic and progressive platform for education and advocacy of gastroenterology and for us as gastroenterologists.
I have a photography website at sloyer.com and can be followed on Instagram at instagram.com/alansloyer
[BOOK REVIEW]
 Reviewed by Jill K. J. Gaidos, MD, FACG
Reviewed by Jill K. J. Gaidos, MD, FACG
I am always looking for ways to practice mindfulness but have never been successful at meditation. I can’t turn off the noise in my mind long enough to experience the peace that meditation is said to provide. That is where “The Art of Stopping” comes in. Dr. David Kundtz highlights that this practice is “contemporary contemplation, designed for those too busy (or maybe moving too fast?) to formally sit and meditate; it’s a way to care for the soul for those who wouldn’t otherwise do it, even though they might really want to.
The author introduces three levels of stopping: Stillpoints, Stopovers, and Grinding Halts. A Stillpoint is a quick stop where you take a few seconds to a few minutes (while waiting for your lunch to heat up in the microwave or while brushing your teeth) to focus just on breathing (there’s even a chapter teaching the breathing technique) and recenter yourself. Stopovers last from an hour to a few days (a quiet morning or weekend away) as a mini vacation for the soul. Grinding Halts can be a week or longer and only happen a couple of times in most peoples’ lives at times of major transitions.
This book provides an overview of the importance of taking time in our lives to reassess our purpose and our path toward that purpose. There are many examples included on how to incorporate stopping into your daily, life starting today. Incorporating stopping into my daily life has helped to bring some peace and clarity into the daily chaos.

[KUDOS]

ACG Past President Sunanda V. “Susie” Kane, MD, MSPH, FACG, started a new role as Chief Patient Experience Officer for Mayo Clinic in March, succeeding current ACG President Jonathan A. Leighton, MD, FACG, who served in this role at Mayo for the past seven years.
Dr. Kane joined Mayo Clinic in 2007 as a Consultant within the Division of Gastroenterology and Hepatology. In 2009, she became the Associate Practice Chair for that division and, two years later, transitioned to the Chair of Quality, a role she held for a decade. She is the Associate Chair of Patient Experience and Satisfaction and was a physician representative to the Department of Medicine Patient Experience Committee from 2013 to 2015.
[IN MEMORIAM]

ACG mourns the loss of a renowned champion of colorectal cancer screening in the U.S. House of Representatives, The Honorable Donald M. Payne, Jr. (D-NJ), who passed away on April 24, 2024, at the age of 65. Rep. Payne, Jr., served the 10th Congressional District of New Jersey since 2012, the same year that his father, Rep. Donald M. Payne, Sr., passed away from colorectal cancer. Rep. Payne, Jr., championed colorectal cancer-related causes as the Co-Chair of the Congressional Colorectal Cancer Caucus. He was a lead sponsor of the “Removing Barriers to Colorectal Cancer Screening Act” that passed the U.S. House of Representatives on December 9, 2020, and was included in COVID-19 relief legislation that cleared Congress on December 21, 2020. Rep.
[NACGF]
ACG has sponsored The North American Conference of GI Fellows (NACGF) since 1990. The strengths of this conference include its small size, and the opportunity for GI fellows to present their research to colleagues in a less pressured environment than at national meetings, while also receiving coaching on presentation skills from experienced faculty. Congratulations to the 2024 NACGF Distinguished Achievement Awardees, Ramzi Hassouneh, MD; Catherine Mezzacappa, MD, MPH; and Raseen Tariq, MD. These fellows presented at the conference in March and were scored highly by the faculty on their presentation skills, including confidence while presenting, clear and concise slides, and ample time allowance for Q&A from the audience. The winning presenters received a $1,000 travel stipend to attend ACG 2024 in Philadelphia, PA.



Payne, Jr., worked tirelessly to promote awareness of colorectal cancer and the importance of early screening, particularly among underserved communities in his Newark, NJ, congressional district and nationally.


[BRAINSTORM]
The American Journal of Gastroenterology (AJG) team gathered for an editorial board retreat in New Orleans, LA, on March 2, 2024. CoEditors-in-Chief Millie D. Long, MD, MPH, FACG, and Jasmohan S. Bajaj, MD, MS, FACG, led Associate Editors in evaluating published special issues and invited articles, editorial and reviewer policies, and discussed new collection ideas. Editors collaborated within their specialty groups to brainstorm new topic ideas and propose authors for invited review articles and Red Section pieces.
Working with the Journal’s publisher, Wolters-Kluwer, two new collections will be catalogued on the Red Journal’s website this summer: Diversity and Inclusion, and Artificial Intelligence. The next AJG special issue on Inflammation in Digestive Diseases is open for manuscript submissions through July 1, 2024. Looking forward to 2025, the Red Journal team plans to publish a patient-centered special issue focusing

ECLP at ACG Advocacy Day – The 2023-2024 cohort of the Early Career Leadership Program (ECLP) of the ACG Institute for Clinical Research & Education gathered with the ACG Board of Governors for Advocacy Day on Capitol Hill on Thursday, April 18, 2024. The group stayed in DC for a didactic session on April 19, highlighted by inspiring talks by ACG Trustee Patrick E. Young, MD, FACG, and ACG Governor for the District of Columbia, Aline Charabaty, MD, FACG. The ECLP program directors are Allon Kahn, MD, FACG, and Elizabeth R. Paine, MD, FACG – both of whom are alumni of the Institute’s Young Physician Leadership Scholars Program, which evolved into the ECLP. Dr. Paine coordinated the ECLP Washington, DC, program with a visit from ACG President Jonathan A. Leighton, MD, FACG.
Clockwise from top: (Top left) Aline Charabaty, MD, FACG, dropped some pearls and practical strategies for ECLP participants in her talk, “Time Management/Burnout Prevention.” (Top right) Patrick E. Young, MD, FACG, gave a deep dive in his talk for the ECLP program on “Mentoring, Coaching & Sponsoring,” sharing insights on being both a great mentor and great mentee/protegé. (Bottom) ECLP 2023-2024 Cohort in Washington, DC, April 19, 2024. First Row: Danny Issa, MD; Catherine T. Hudson, MD, MPH; Jennifer Ray, MD; George Cholankeril, MD. Second Row: Samuel Schueler, MD; Viveksandeep Thoguluva Chandrasekar, MD; ECLP Co-Director Elizabeth Paine, MD, FACG; ACG President Jonathan A. Leighton, MD, FACG; Alexandra Strauss, MD, PhD, MIE. Third Row: Lauren Feld, MD; Trisha Pasricha, MD, MPH; Sudha Pandit, MD; Galen Leung, MD; Ngozi Enwerem, MD, MPH; Allison June Kwong, MD; Simon Jinwha Hong, MD; Hassan Siddiki, MD, MS, MEd. Fourth Row: Sergio Sánchez-Luna, MD; Noemi J. Baffy, MD, MPH; Justin Brandler, MD; Kirk B. Russ, MD. Fifth Row: Jared Magee, DO, MPH; Jeffrey Berinstein, MD, MSc; Chamil C. “Don” Codipilly, MD.
Apply for an Edgar Achkar Visiting Professorship (EAVP) at your institution! A distinguished speaker will deliver grand rounds and engage with trainees. An option for EAVP is to request a Visiting Scholar in Equity, Diversity & Ethical Care, a project of The ACG Institute's Center for Leadership, Equity & Ethics. Speaker travel costs and honoraria are covered. The application portal opens July 22, 2024 and closes August 21, 2024.
Learn more: gi.org/eavp
[SUMMER
The Summer Scholars Program is an initiative of the ACG Committee on Diversity, Equity & Inclusion that pairs medical students from groups underrepresented in medicine with mentors for a research project and provides a stipend of $5,000. The Committee believes that a formalized mentorship and clinical research program is one pipeline to increase representation of underrepresented groups in medicine in academic gastroenterology careers. The program is an 8-10 week structured clinical research experience for medical students in the U.S. who are paired with research mentors sharing similar clinical research interests in the fields of gastroenterology and hepatology. At the end of the program, the students are required to submit a progress report and an abstract to a local, regional, or national conference.










March Colorectal Cancer Awareness Month puts the spotlight on prevention and brings attention to the importance of quality screening for colorectal cancer (CRC). ACG’s goal is to inspire, uplift, and celebrate our members in their efforts to increase visibility of CRC prevention while providing educational resources, tools, messaging, and graphics to support their efforts with patients and in their communities.
For 2024, the College’s CRC Month celebration featured advocacy, music, physical activity, patient education, and kicked off with an invitation to the larger GI community to show their true colors by wearing blue – the signature hue of CRC awareness – for “Dress in Blue Day” on Friday, March 4, 2024.




On March 12, 2024, on the National Mall in Washington, DC, ACG President Jonathan A. Leighton, MD, FACG, represented the College at the “United in Blue” rally and installation organized by the advocacy group Fight Colorectal Cancer. ACG is proud to be part of a coalition of organizations standing with CRC patients, survivors, and caregivers who gathered to visit with legislators and bring attention to colorectal cancer, the trends in young-onset disease, and to demand that the U.S. Congress prioritize CRC research and screening. A dramatic installation of 27,400 blue flags near the U.S. Capitol was a powerful visual representation of those younger than 50 who will be diagnosed with colorectal cancer in 2030, unless we do more to educate, screen, and raise awareness.

ACG offers an array of patient education handouts and resources for community education events and social media through its CRC Community Education Toolkit which can be accessed at bit.ly/ACG-CRC-toolkit. ACG also has an informative infographic about CRC translated into 11 languages, now including Arabic, which can be downloaded at bit.ly/CRC-Infographic-Translations

An evening of musical inspiration marked the end of CRC Month when Benjamin H. Levy, III, MD, of the ACG Public Relations Committee organized a virtual concert featuring artists from a wide array of musical genres who donated their time and performances. ACG’s Tune It Up Virtual Concert to Raise Awareness of Colorectal Cancer included performers such as Lisa Loeb, Rufus Wainwright, violinist Hilary Hahn, the Cincinnati Pops Orchestra, the Knights Chamber Orchestra, and many more! You can listen to a recording of this impressive program at gi.org/concert.

Bridging Medicine & Music was a colorectal cancer education program and concert organized by ACG Governor for Northern California Ronald K. Hsu, MD, FACG, and featured international celebrity electric violinist Mark Wood in person at Davis Senior High School in Davis, CA, on March 22, 2024. ACG was a promotional partner for this event and many ACG leaders contributed to a video with key messages about CRC prevention.

In honor of March CRC Month, the ACG Board of Trustees shows its dedication to colorectal cancer screening for average-risk individuals starting at age 45. Back
Left to Right: Dr. Aasma Shaukat, Dr. Jill Gaidos, Dr. Renee Williams, Dr. Irving Pike, Dr. Jean-Paul Achkar, Dr. Brooks Cash, Dr. Patrick Young, Dr. Seth Gross, Dr. Samir Shah, Dr. Millie Long, Dr. David Hass, Dr. Neil Stollman, Dr. Jasmohan Bajaj. Front
Left to Right: Dr. Costas Kefalas, Dr. William Chey, Dr. Jonathan Leighton, Dr. Amy Oxentenko, Dr. Nicholas Shaheen, Dr. Neena Abraham.







Each chapter of the Guide to the Guidelines series includes carefully selected vignettes designed to illustrate key concepts from the guidelines, followed by a conversation-style discussion written to keep you awake and alert. The authors highlight noteworthy points and provide multiple-choice questions to test your knowledge of the material. Using their combined experience of managing GI and liver patients in both academic and private practice settings, they can help you provide high quality care to your patients.



IN 1910, DR. WILLIAM J. MAYO PUBLICLY ENDORSED THE LEADING PRINCIPLE OF THE HOSPITAL, “THE NEEDS OF THE PATIENT COME FIRST.” While we can all agree that patientcentered care leads to improved outcomes for patient safety, faster diagnoses, and personalized treatment plans, the role of the patient voice in education has been varied. In the 1960s, the concept of standardized patients was first introduced by Dr. Howard Barrows, allowing medical students to practice history and physical examination skills on trained actors who graciously help prepare students for clinical encounters.
As trainees, we learn from all our patient interactions, but we only see our patients for a moment in time. Even in chronic illness, the person we witness on our exam table is one small snapshot of the full life that is experienced outside our office. Although we may learn about the impact of socioeconomic factors, gender biases, financial hardship, and stigma of disease, we are not there to witness it. Equally important is the impact of illness on relationships, family members, and personal identity – all principles which are not easily taught in a classroom. In Spring 2023, I set out to interview patient advocates with a variety of gastrointestinal

illnesses, to see how the voice of the patient advocate could help provide perspective and education to GI fellows. I had the privilege of interviewing Tina Aswani Omprakash, Jessica Caron, Erica Dermer, Ryan Piansky, Jeffrey Roberts, Alison Rothbaum, Melissa Adams VanHouten, Allison Rosen, and Brad Swiftney. I am forever grateful to these wonderful patient advocates for sharing their expertise and candid experiences in healthcare.

After this article was published, my program director, Dr. Douglas Simonetto, reached out to discuss how we could incorporate the patient voice at our GI Fellowship at Mayo Clinic. I emphasized that an invited speaker needed to be appropriately compensated for her time and given a center stage to share her voice. I was delighted to learn that Dr. Darrell Pardi, Chair of the Division of Gastroenterology & Hepatology at Mayo Clinic, agreed to have Allison Rosen visit as our first ever patient advocate to present at a Gastroenterology Grand Rounds.
In March 2024, Allison Rosen ventured to Rochester, MN, where she was welcomed to the podium to share her story with all of us. The audience was diverse – GI fellows, faculty, endoscopy staff, ostomy nurses, administrators, nurses, oncology fellows, and colorectal surgery fellows – as it was important to us to have her message heard broadly. Her timing was especially impactful, as it was Colorectal Cancer Awareness Month, so our audience and speaker #DressedinBlue for the occasion. Here we highlight some feedback and reactions to Ms. Rosen’s visit and ideas for future collaborations at GI fellowship programs across the country.

• Darrell S. Pardi, MD, MS, FACG, Chair, Division of Gastroenterology & Hepatology, Mayo Clinic: “It is so important to include the voice of our patients and their caregivers in our educational activities and medical decision-making. I appreciate Ms. Rosen being the first patient advocate to speak at Mayo Clinic GI Grand Rounds. Her presentation was very well received, and we look forward to having additional patient advocate presentations to follow.”
• Xiao Jing “Iris” Wang, MD, Associate Program Director, GI Fellowship, Mayo Clinic: “Having the patient voice as part of not only fellowship training, but part of our divisional, local, and national meetings is incredibly important for us as physicians. At Mayo, our guiding star is ‘the needs of the patients come first,’ and it is only by truly listening to our patients that we understand their needs. This
guides our research direction and our clinical focus. Our patient stories, particularly in their voices, remind us why we do what we do, and give meaning to the everyday. They teach us empathy, therapeutic alliance, and humility. I am so grateful to all our advocates who are so generous with their time and courage to share their journeys with us.”
• Krystal Mills, MD, First-Year GI Fellow, Mayo Clinic: “I truly enjoyed the opportunity to meet and learn from Allison Rosen during her visit to Mayo Clinic. As a physician, I gained a greater appreciation for the experiences of patients as they navigate the healthcare system. My understanding of how patients can be best supported was expanded and I look forward to strengthening my approach to patient-centered care.”
• Caroline L. Matchett, MD, First-Year GI Fellow, Mayo Clinic: “Having patient advocate Allison Rosen share her journey during our grand rounds was deeply inspiring and grounding. Her poignant story reminded us of the real-life impact of our work and the significance of patient-centered care. Through her advocacy, Allison has illuminated the path towards greater empathy and understanding in our practice. Her presence reignites our passion and commitment to excellence in gastroenterology, reaffirming our purpose: to empower and uplift those entrusted to our care.”
• Kathryn A. Schmidt, MD, SecondYear GI Fellow, Mayo Clinic: “Having Allison visit Mayo Clinic provided invaluable insights into the patient experience and highlighted the importance of advocacy in navigating healthcare. Her perspectives shed light on the challenges patients face, from diagnosis to treatment, and emphasized the need for personalized care and support. In addition to the unique education we gained from her visit, Allison was so enjoyable to speak with and learn from. I was very grateful for the opportunity to connect with such a passionate patient advocate.”
• Shuji Mitsuhashi, MD, First-Year GI Fellow, Mayo Clinic: “Our GI fellowship’s grand rounds with the patient advocate, a colorectal cancer survivor, was not just educational, but also eye-opening! Her stories had us on the edge of our seats, reminding us why we’re in this field, and to always bring a smile to our patients!”
• Jean C. Fox, MD, Consultant Gastroenterologist, Mayo Clinic: “Ms. Allison Rosen’s visit was indeed a memorable experience. Ms. Rosen boldly and eloquently provided a lens to the complexity of the lived experience of the person given the diagnosis of colorectal cancer (CRC). She enabled us to see the full humanity and complexity of the person sitting before us with a new diagnosis of colon cancer. The body changes of treatment are not limited to the GI tract. Going forward I will be certain to inquire about sexual and pelvic floor function. With the rise of CRC in young patients, preservation of fertility is a concern. We must all do better to have conversations with our patients before they start treatment or refer to someone who can. We have much to learn from patient advocates in all aspects of GI health and it is my hope that her visit is the first of many.”
“As a passionate patient advocate, it was a true honor and privilege to be invited to share my personal cancer journey as a part of GI Grand Rounds at the Mayo Clinic. Growing up, I always heard my dad talk about giving Grand Rounds (he is a physician) and assumed this was specific for high profile clinicians and researchers, so imagine my surprise when an invitation was extended to me to do this very thing. I applaud the GI Department at Mayo for their dedication to patient centricity and embracing the patient voice. The whole experience was truly amazing. From giving my presentation,
“ When advocates and healthcare systems partner, I genuinely believe lives can be saved.” —Allison Rosen
1. Invite a patient advocate to speak to your GI fellows or entire GI department! Be sure to give them an appropriate setting to share their story and respectfully compensate their time and work.
2. When designing clinical studies, ask for feedback from patient advocates as early as day one of the proposal. Patient advocates can help identify barriers to recruitment or study design, which helps to optimize outcomes for all parties involved.
3. Encourage GI fellows to listen to patient advocate podcasts, webinars, or tweetorials!
4. Work with GI societies to create workshops at national conferences to provide an opportunity for GI fellows and patient advocates to interact and learn meaningfully from each other. (Then be sure to schedule their talk on the main stage, not on the last slot of the conference, to optimize attendance.)
5. Consider implementing feedback from patients regarding communication skills and patient engagement.
to speaking with various faculty members, to getting a tour of the campus, I not only have a new-found admiration for everyone at the Mayo Clinic, but I learned how they operate as a multidisciplinary team seamlessly and plan to empower others to follow their lead. As I was experiencing some of the toughest years of my life fighting cancer 12 years ago, I would have never imagined that one day I would be traveling to tell my story to a room full of healthcare professionals who help save lives like mine every day. This opportunity was truly one of the highest honors as an advocate I have experienced. I plan to encourage every institution, big or small, to incorporate patients and survivors in opportunities like this. When advocates and healthcare systems partner, I genuinely believe lives can be saved.”

Rosen, MS
Ms. Rosen has deliberately and consciously chosen to dedicate her life – in and outside of her employment – to use her voice and platform to educate, advocate, and continuously learn how best to represent the collective cancer and ostomy community. She is a patient, community, policy, and research advocate. She has worked in the world of oncology for over 18 years in cancer research and cancer health disparities. On June 7th, 2012, at the age of 32, after years of struggling with Crohn’s disease, her life was totally disrupted when a colonoscopy revealed Stage 2C colorectal cancer. She has now been cancer-free for over 11 years and volunteers her time on committees for young adult and colorectal cancer patients, with groups working on effective patient experience, social media, and outreach initiatives. She is a public speaker, board member, and volunteer for local, regional, and national organizations and non-profits. Ms. Rosen has experience on both sides of the fence and works to bridge the gap between the healthcare system and the communities that it serves.

Katie A. Dunleavy, MB, BCh, BAO, is a third-year gastroenterology and hepatology fellow at Mayo Clinic, Rochester, who plans to stay at Mayo Clinic for an Advanced IBD year. She received her medical degree from the Royal College of Surgeons in Ireland and completed her internal medicine residency at Icahn School of Medicine at Mount Sinai Hospital in New York. Her areas of clinical interest include the overlap of inflammatory bowel disease and neurogastroenterology, ergonomics in endoscopy, and clinical trials research. She is a former coloratura soprano and is passionate about global health and medical education.
Weekly on Thursdays at 12 pm and 8 pm ET
Live Presentation by an ACG Expert Plus Q & A #GIhomeschooling
Even as all aspects of practice have changed due to COVID-19, your need to stay up to date on clinical GI does not stop. ACG is committed to your professional education. Our goal is to help the GI community embrace #GIhomeschooling with quality speakers and presentations.
ACG has launched Virtual Grand Rounds weekly on Thursdays at 12 pm and 8 pm ET. Each week an expert faculty member will present live on a key topic followed by Q & A.
Learn More and Register: GI.ORG/ACGVGR
Locum tenens is a Latin term meaning, “to hold the place of,” referring to physicians who temporarily substitute for another physician. Locum tenens assignments offer flexibility to physicians who may prefer short-term work or want to experience working in different healthcare settings or locations. It can be an attractive option for doctors who are recent graduates, in between permanent positions, retirees who want to continue practicing parttime, or those seeking a change from their routine or to increase their income. The duration of a locum tenens assignment can range from a few days to several months, depending on the needs of the healthcare facility and the availability of the locum tenens physician.
Like any other employment option, locums work has advantages and disadvantages. The advantages include schedule flexibility, allowing you to choose your schedule and work on your terms. You can decide when and where you want to work, allowing you to balance your personal life, pursue other interests, or take time off for personal reasons. This flexibility can lead to a better work-life balance and prevent burnout.
There are many work opportunities available through locums, which can include both inpatient and outpatient work. These assignments can give you exposure to a range of healthcare settings, such as hospitals, outpatient clinics, and endoscopy centers, as well as rural areas and underserved communities. This diversity allows you to broaden your clinical experience, gain exposure to different patient populations, and enhance your medical skills. Additionally, working in new environments and adapting to different healthcare systems that use varied resources and electronic medical records can be professionally enriching and intellectually stimulating.
It also offers networking and professional growth. Working as a locum doctor provides you with opportunities to network with professionals in various healthcare settings. You can learn from experienced physicians, collaborate with multidisciplinary teams, and develop valuable relationships within the medical community. This networking can lead to future job opportunities, referrals, and collaborations. A unique advantage is that it allows you to help in addressing community healthcare needs. Locums work can play a crucial role in addressing healthcare gaps in underserved areas or communities experiencing physician shortages. By temporarily filling staffing vacancies, you ensure that patients continue to receive necessary medical care. Your presence can alleviate the burden on permanent healthcare providers and improve access to healthcare services for individuals who might otherwise face challenges in receiving timely treatment.
It also exposes you to cultural exchange and global health. Locum opportunities are not limited to a single geographic location. You can choose

to work as a locum doctor in different regions or even different countries. This allows you to experience diverse cultures, understand global health challenges, and contribute to improving healthcare access and quality in underserved areas worldwide.
“Locum tenens work contributes to your personal and professional development by requiring adaptability, resourcefulness, and the ability to acclimate to new environments quickly.”
There are also many financial benefits. Locums work often offers competitive compensation, including higher pay rates and additional benefits. This can be particularly advantageous for doctors looking to supplement their income, pay off student loans, or save for their future. The pay differs based on institutional need, endoscopist procedural experience, and if it’s holiday coverage. The pay scale varies, but is negotiable. Payment includes a predetermined 8-hour minimum guaranteed fee, a negotiated hourly rate, and a beeper coverage fee. Physicians are reimbursed for their meals, travel expenses, car rentals, air transportation, state licenses, application fees for hospital privileges, and malpractice insurance. As a 1099 employee, it may be beneficial to consider forming an LLC/SCORP to optimize your tax advantages. I recommend consulting with your CPA to determine whether an LLC or S-CORP is the best option for you.
Locum tenens work contributes to your personal and professional development by requiring adaptability, resourcefulness, and the ability to acclimate to new environments quickly. It can help you develop essential skills such as effective communication, problem-solving, and cultural competence. These skills can benefit you not only in locum assignments but also in your long-term medical career.

Some disadvantages of locum work include distance away from your home or family for as long as two weeks to several months depending on your assignment. Although the pay is very competitive, there are no healthcare insurance coverage or retirement contribution plans provided. Sometimes, you may find yourself working on a job that isn't the best match, but you may be contracted to do so for a few weeks or months. In most cases, you can cancel the assignment with more than 30 days notice without any consequences. These assignments can vary in difficulty, and having a team with a diverse range of expertise is very important. There might be situations where certain specialties aren't available at the medical facility.
Choosing the right locums company is very important. You want to build a good relationship with your recruiter, who has your best interest. A good company will do what is in your best interest (negotiate higher pay rates, get your first choice of work days, and find a desirable area/hospital to work at). The best way to evaluate a company is through word of mouth from other physicians since it's dependent on the locums representative and not entirely the company. Typically, the locums companies get your state license, credentials, and pay your malpractice insurance with tail coverage. Companies typically provide $1-3 million in malpractice coverage with the exception of Virginia, which requires higher coverage. The malpractice insurance and tail coverage depend on the facility and locum company. For instance, Locum Company #1’s policy doesn’t pay out for a malpractice that happened under an assignment with Locum Company #2. Each locum assignment has specific malpractice insurance coverage with tail for the hospital assignment. Therefore, if you have three hospital assignments, you will have three different malpractice with tail coverage policies.
The companies charge the hospital a fee based on the amount of coverage that you provide for their hospital. It is common practice to work with different locum companies, which will give you more access to jobs. A good synergistic relationship with the locum company is important when trying to obtain more desirable locum opportunities, such as higher paying jobs that are geographically favorable to you.
It is important to ask other locum providers about pay rates to ensure you are receiving fair market value. It's also essential to offer competitive rates to have access to more opportunities, but don't undersell yourself. If you specialize in ERCP or EUS, you can demand higher pay due to a shortage of physicians. When choosing an assignment, consider the pay rate ($3,000-4,000 for 8 hours, $300-500 per hour for overtime), work hours (4-12 hours), location, facility work volume (2-10 new consults, 5-20 follow-ups, and 1-10 procedures per day), facility electronic medical record program, multidisciplinary

faculty, and facility equipment. There is comparable liability as a locum to private practice in a group. If a liability issue arises with a patient at a facility, the covering physician and the facility (risk management) will usually contact the physician to discuss and review the case.
Higher Rates – Locums is a lucrative part-time or full-time option which often pays higher rates than full time staff positions.
Flexibility – Locum providers often experience a higher level of autonomy in choosing their schedule and locations to practice.
Focus on Medicine – Experienced locum providers can focus more on patient care while avoiding reimbursement issues or facility internal politics.
Travel – Providers get to see the country and benefit from the flexibility to try new geographic locations and practice settings.
Overall, locum tenens provides a temporary staffing solution for healthcare facilities and allows physicians to maintain their professional practice while accommodating their personal needs and preferences. Locum tenens positions play a crucial role in maintaining healthcare services by ensuring that patients continue
to receive medical care even when regular physicians are unavailable. Many physicians find this role very satisfying because it offers flexibility and allows the physician to help communities in need of a gastroenterologist.
RESOURCES:
1. locumtenens.com/ppc/sign-up-tosearch-jobs/?gad=1
2. comphealth.com/locum-tenens
3. sbghealthcare.com


ON THURSDAY, APRIL 18, 2024, 100 College leaders met with House Representatives and Senators. Across more than 200 meetings, ACG’s tireless advocates expressed the continued challenges facing gastroenterology, while highlighting key legislative opportunities that would benefit GI patients and practices.
The highlight of the day was the annual luncheon, where seven Members of Congress offered a wide array of perspectives. Collectively, they addressed the relevance of physician advocacy on Capitol Hill and shared their personal experiences with cancer and the importance of preventive screenings.
ACG is grateful to U.S. Sen. Bill Cassidy, MD (RLA), an ACG Fellow and hepatologist, Rep. Mark Green, MD (R-TN), Rep. Kim Schrier, MD (D-WA), Rep. Andy Harris, MD (R-MD), Rep. Debbie Dingell (D-MI), and Rep. Debbie Wasserman Schultz (DFL) for their time.
Above all, the focus of the 2024 ACG Advocacy Day was reminding each Member of Congress that they are essential in supporting physicians and protecting patient access from the many harmful forces at play – from insurers and their burdensome utilization management requirements to everdecreasing Medicare physician reimbursement. The hope is that the frustration we conveyed, as well as the legislative opportunities discussed, have laid the groundwork for meaningful progress.


ACG’S KEY MESSAGES AND SPECIFIC LEGISLATIVE REQUESTS:
• Support the Safe Step Act (S. 652/H.R. 2630)
This popular, bipartisan bill has more cosponsors than ever before and was also introduced in the Senate for the first time. It would require many employer-sponsored health plans to implement a clear and transparent process to request an exception to a step therapy protocol. On Thursday, legislators and their staff remained broadly supportive of the bill, and recently, it has been included in broader reform packages that Congress will consider later in 2024.
• Support the Reducing Medically Unnecessary Delays in Care Act (H.R. 5213)
This legislation would require all Medicare plans to have only medically-necessary prior authorization policies for both prescription drugs and services. It also requires all appeals and peer-to-peers to be conducted by a doctor in the same specialty as the patient's condition.
• ACG's New 'Principles of Medicare Reform' New for 2024, our advocates shared ACG's principles that should guide any Medicare reform. We were grateful to have the opportunity to meet with staff for four members of the new Senate Medicare Payment Reform working group, as well as Finance Committee staff from both the House and Senate.
• Champion efforts to require insurers to correctly classify surveillance colonoscopy a preventive service Building on recent interest, we reminded Congress that with colorectal cancer cases among young Americans increasing at a staggering rate, now is the time to act. We hope to have more advocacy opportunities for you on this issue soon.
As always, we are grateful to the College's leadership, to ACG President Dr. Jonathan Leighton, to Dr. Louis Wilson, Chair of the Legislative & Public Policy Council, as well as everyone who dedicated time and effort to the success of our 2024 Advocacy Day!
—Dr. Dayna S. Early, Chair, ACG Board of Governors & Dr. Sita Chokhavatia, Vice Chair








Harris (R-MD) was not part of our an essential part of Harris, MD




U.S. Rep. Troy Carter (D-LA)
"When that engine light comes on in our car, we respond. When our bodies send us a signal, we push through and think it'll go away. I know I'm preaching to the choir, but sometimes the choir needs rehearsing, too."— Rep. Troy Carter




own Dr.

Dr.
 U.S. Sen. Cory Booker (D-NJ) greets New Jersey’s
Sita Chokhavatia and
Adam Elfant
(R-MD)
Dr. Louis Wilson, Dr. Dayna Early, Dr. Jonathan Leighton, Dr. Costas Kefalas, Dr. Pierre Hindy; ACG’s Brad Stillman
Dr. Sergio Sánchez-Luna; ACG’s Vaidehi Gajjar-Mehta; Dr. Elizabeth Paine; Dr. Lauren Feld; Dr. Trisha Pasricha; Dr. Danny Issa
(D-LA)
Dr. Bara El-Kurdi; Dr. Ngozi Enwerem; Dr. Harish Gagneja; U. S. Rep. Beth VanDuyne (R-TX); Dr George Cholankeril; Dr. Jay Yepuri
U.S. Rep. Debbie Wasserman Schultz (D-FL) and Dr. Lauren Feld
Dr. Chamil Codipilly; Dr. Pooja Singal; U.S. Sen. Tina Smith (D-MN); Dr. Nayantara Coelho-Prabhu
Dr. Samir A. Shah; U.S. Rep. Gabe Amo (D-RI); Dr. Alyn Adrain
U.S. Sen. Cory Booker (D-NJ) greets New Jersey’s
Sita Chokhavatia and
Adam Elfant
(R-MD)
Dr. Louis Wilson, Dr. Dayna Early, Dr. Jonathan Leighton, Dr. Costas Kefalas, Dr. Pierre Hindy; ACG’s Brad Stillman
Dr. Sergio Sánchez-Luna; ACG’s Vaidehi Gajjar-Mehta; Dr. Elizabeth Paine; Dr. Lauren Feld; Dr. Trisha Pasricha; Dr. Danny Issa
(D-LA)
Dr. Bara El-Kurdi; Dr. Ngozi Enwerem; Dr. Harish Gagneja; U. S. Rep. Beth VanDuyne (R-TX); Dr George Cholankeril; Dr. Jay Yepuri
U.S. Rep. Debbie Wasserman Schultz (D-FL) and Dr. Lauren Feld
Dr. Chamil Codipilly; Dr. Pooja Singal; U.S. Sen. Tina Smith (D-MN); Dr. Nayantara Coelho-Prabhu
Dr. Samir A. Shah; U.S. Rep. Gabe Amo (D-RI); Dr. Alyn Adrain

With massive advancements in AI rapidly influencing almost every aspect of healthcare, what does this mean for the future of gastroenterology? The answers may be surprising.
Brennan Spiegel, MD, MSHS, FACG, Cedars-Sinai, Los Angeles, CA
THE CHIEF RESIDENT BEGAN MORNING REPORT IN A CONFERENCE ROOM FILLED WITH ANTICIPATION, presenting a patient case to the collected team of internal medicine trainees—a 62-year-old woman suffering from persistent diarrhea and abdominal pain. As the mentor overseeing this teaching session, my role was to guide the residents through the diagnostic process, encouraging them to explore the patient’s symptoms and lab results and, ideally, uncover an underlying condition.
"The patient first noticed the symptoms about eight months ago," the Chief Resident began. "There is no correlation with food intake, and the pain is diffuse, not localized to any specific area." There were also reports of neuropathic symptoms, shortness of breath, weight loss, and other seemingly diffuse symptoms.
The room was filled with 20 residents, each one seeking to unravel the mystery. They delved into the patient’s history, asking pointed questions. When did the diarrhea start? Were there any triggers? Alarm features? What was the nature of the pain? The usual questions.
As the case unfolded, the presenter shared some lab results that caught everyone’s attention. The liver enzymes were slightly elevated, and the creatinine levels were marginally high. "Additionally," the Chief Resident added, "the patient exhibited mild anemia and an elevated sedimentation rate, suggesting an inflammatory process.”
The trainees kept at it, their minds working to piece together the puzzle. They considered a wide range of conditions, including gastrointestinal infections, inflammatory bowel disease, celiac sprue, and autoimmune syndromes, among many other potential diagnoses. Each hypothesis was discussed and debated in depth as the conversation continued.
Meanwhile, unbeknownst to them, I was conducting an experiment of my own. I had been quietly entering all the case data into the Chat GPT-4 large language model, an artificial intelligence (AI) program, curious to see how its
conclusions would compare to the collective intelligence of the room. I didn’t expect much from the AI, but around 12 minutes into the discussion, with a hypothesis forming in my own mind, I prompted the computer for a differential diagnosis.
The AI’s top suspicion was systemic amyloidosis. And indeed, I was thinking the same thing. Not only did the computer pinpoint amyloidosis, but it also provided an elaborate explanation, aligning the symptoms and lab findings with the pattern typical of the disease. Though it listed several other potential diagnoses, including everything else mentioned by the residents, its priority on amyloidosis was notable.
Back in the conference room, the brainstorming continued. The residents considered and discarded various possibilities, mulling over the evidence, demonstrating their impressive knowledge and capacity to examine a complicated case. But it wasn’t until 44 minutes into the discussion that the word "amyloidosis" finally emerged from the group, suggested with some hesitation as a potential diagnosis. The revelation that systemic amyloidosis was indeed the correct diagnosis, albeit not the group’s primary suspicion, was a key moment for me. Remarkably, the AI had arrived at the correct diagnosis 32 minutes earlier than the doctors.
My initial skepticism of using AI for medical decision-making was not unfounded. Upon the release of Chat GPT-3.5 in late 2022, I put it through a rigorous test, utilizing my own book, "Acing the GI Board Exam," to pose questions that might appear on an accreditation exam. The results were underwhelming, to say the least. The AI struggled with basic diagnostics, recommended treatment paths that veered into the dangerous, and lacked the nuanced understanding of a seasoned physician. It was clear that AI had a long way to go.
But that changed fast. With the advent of GPT-4, I subjected it to the same battery of questions, less than a year after the first assessment. The transformation was remarkable. This time, the AI performed with near-perfect accuracy, not only identifying the correct diagnoses but also providing detailed, thoughtful explanations that mirrored the depth of understanding
one would expect from a highly trained doctor. This leap in proficiency within just one year is a testament to the exponential growth of AI capabilities, a concept that many of us find hard to grasp. And here’s the thing—this is the worst AI will be for medical decisionmaking. We expect it will get better and better, and do so faster than most anyone imagined it could.
This massive leap reflects the kind of exponential growth that Gordon E. Moore predicted would occur nearly six decades ago. Moore, co-founder of Intel, articulated this idea in 1965 as “Moore's Law,” describing a trend where the number of transistors on a microchip doubles approximately every two years, reducing costs while increasing computing power. Moore's prediction of massive growth in computing power has been borne out, underpinning the rapid advances we witness in AI.
Separately, futurist Ray Kurzweil introduced the concept of "The Singularity” in 2005, which he described as a point in time when machine intelligence will surpass human intelligence, resulting in a transformative and perhaps unfathomable shift in our society.
Kurzweil posited that at this juncture, which he predicted would occur by 2045, the progress in technology will become so rapid and profound that it will rupture the fabric of human history. Just try to wrap your mind around that! The implications of The Singularity are vast, suggesting not only an integration of AI in everyday life but a fundamental change in our understanding of existence, as machines could potentially improve and replicate themselves autonomously.
Kurzweil's timeline, pointing towards the mid-21st century for this event, places us on the brink of what will be the most significant period in technological advancement. Looking at our current trajectory with AI, where systems like Chat GPT demonstrate understanding and problem-solving at near-human levels (or, in some cases, beyond human levels), it seems we may be on schedule, if not ahead, for this unprecedented era. The Singularity
isn't just a distant myth; it's a foreseeable pivot point for human civilization, increasingly anchored in our reality by the continuous, exponential advancements in computational power and AI sophistication.
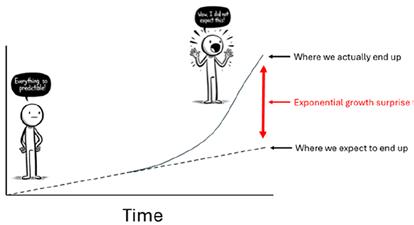
As gastroenterologists, it’s critical that we adjust our mindset from a linear to an exponential model of thinking to ensure we keep up with the times. This is not easy to do, in part because it’s hard to think exponentially. Our predisposition for linear reasoning served us well in the past, but the future demands that we anticipate changes not as they have occurred, but as they will occur, at rates far surpassing our previous experiences. To echo the famous insight from sports legend Wayne Gretzky when asked how he is so good at hockey, we need to "skate to where the puck is going to be, not where it has been." Today, the puck is accelerating at an unprecedented speed, propelled by advances in AI and computational power. To understand what’s going on, consider the image in Figure 1
This is a model of how progress in technology changes over time. Initially, the path seems linear and predictable—akin to the expected trajectory of a puck gliding across the ice in a straightforward direction. The figure confidently assumes their journey will continue along this gentle incline, believing they can predict where they’ll be in the future. But then, the path jolts upwards in a steep ascent—the signature of exponential growth. This sharp rise represents the “surprise factor” of technological advancements, like a hockey puck that has suddenly been smacked by a powerful swing, changing its course dramatically. The figure, taken aback by this unexpected turn, finds themselves propelled into a future far beyond their linear predictions, echoing the idea that we must aim to “skate” not to where we think the puck will be, but to where it is actually going—which, due to the nature of exponential growth, is a point much further ahead than our instincts might suggest.
To remain at the forefront of our field, and to harness the full potential of AI in improving patient care, we must prepare ourselves for where the technology is headed, not just where it stands today. The example of the morning report is a glimpse of what’s possible when we combine the depth of human medical expertise with the analytical powers of AI. As the technology continues to evolve, so too must our approach to integrating it into
“To remain at the forefront of our field, and to harness the full potential of AI in improving patient care, we must prepare ourselves for where the technology is headed, not just where it stands today.”
our practice, ensuring we are always moving towards the future of gastroenterology, ready to meet it with open arms.
AI has permeated every domain of medicine, and gastroenterology is no exception. Figure 2 displays the outcome of a PubMed search for publications that intersect "gastroenterology" with "artificial intelligence." The histogram illustrates not just growth, but an exponential surge, from 1986 to 2024, underscoring the accelerated pace at which technological advancements are being integrated into gastroenterological research and practice.
An entire textbook could now be dedicated to the impact of AI on the field of digestive diseases, given the breadth and depth of its influence. In fact, I assume such a book is already on its way, if not already published. AI is revolutionizing the way we approach diagnostics, treatment, and patient management in gastroenterology and hepatology, and its applications are proving to be as diverse as they are transformative. In the realm of endoscopy, AI has been employed to detect colorectal polyps during colonoscopies. Advanced algorithms analyze video feeds in real-time, identifying polyps with a level of precision that rivals—and sometimes surpasses—the trained eye. Recent studies suggest that AI assistance can substantially improve unaided adenoma detection rates, which is crucial for early intervention and cancer prevention.
But the applications of AI extend far beyond polyp detection. For example, AI systems are now being developed to assess the severity of inflammatory bowel diseases and other forms

of colitis. By analyzing endoscopic images, histopathological data, and clinical parameters, AI can provide gastroenterologists with detailed severity scores with potential to refine treatment plans or predict disease progression.
Barrett's esophagus is another area where AI is proving useful. Through the analysis of endoscopic images, AI can detect subtle histopathological changes that might escape even the most meticulous endoscopist or pathologist. Its applications are similarly groundbreaking when it comes to diagnosing and staging gastrointestinal malignancies, with machine learning models offering remarkable accuracy in interpreting radiologic, endoscopic, and histopathologic images, potentially catching cancers earlier and informing more precise interventions.
In the brief span since I begin writing this article about a week ago, the landscape of digestive diseases literature has burgeoned with over 100 new papers on AI applications. That’s just astonishing to me. To maintain currency with this ever-expanding body of knowledge, I leveraged GPT-4 to devise a PubMed search strategy, a task I might have traditionally reserved for a consultation with a biomedical librarian. While expert input remains invaluable, the AI solution was remarkably straightforward: I requested GPT-4 to generate a search strategy, and it promptly delivered. The strategy it proposed, captured in Figure 3, demonstrates AI’s utility not just as a subject of study but as an active tool in managing the deluge of academic output about AI itself.
Just a glance at the array of topics identified by the search strategy over the last month reveals the staggering scope of
“Ironically, in an era of AI-enabled gastroenterology, there has never been a greater need to learn and perfect an age-old technique— laying hands on the patient.”
AI’s reach into digestive disease. The breadth of research ranges from neural networks that offer prognostic insights for pancreatic ductal adenocarcinoma to deep learning models scrutinizing liver tumor images, and sophisticated algorithms aimed at early detection of esophageal cancer. One study explores the use of AI to quantify histologic features of ulcerative colitis in biopsy samples, proposing a novel metric for clinical trial outcomes. Another raises a concern on whether AI's interpretation of abdominal CT scans could inadvertently magnify healthcare disparities.
Continuing through the PubMed list of recent articles, the innovations continue to unfold: machine learning is being harnessed to refine the assessment of hepatic fibrosis; AI is playing a role in the nuanced diagnosis and management of appendicitis; and deep learning is being employed to enhance the interpretive accuracy of capsule endoscopy images. Each paper not only contributes to the wealth of knowledge but also exemplifies the profound and multifaceted ways in which AI is redefining the field of gastroenterology. In our research at Cedars-Sinai, we are also exploring the utility of AI applications in gastroenterology and beyond. For example, our team developed an AI-powered tool designed to offer mental health support through natural language processing. Initially, the concept, suggested by a psychiatry colleague, struck me as overly ambitious. The intricacies of talk therapy, traditionally a deeply human interaction, seemed beyond the reach of a machine.
At the outset, the AI's performance was far from satisfactory. It struggled to build rapport with patients, often leapt to premature conclusions, and provided advice that lacked nuance. However, informed by these early shortcomings, we continued to refine the system. We incorporated insights from behavioral health specialists, fed it expert
(("Artificial Intelligence"[MeSH Terms] OR "Machine Learning"[MeSH Terms] OR "Deep Learning" OR "Neural Networks" OR "AI" OR "computational models") AND ("Gastroenterology"[MeSH Terms] OR "Hepatology"[MeSH Terms] OR "endoscopy" OR "colonoscopy" OR "liver diseases" OR "gastrointestinal neoplasms" OR "gastrointestinal diseases" OR "hepatic" OR "esophageal" OR "pancreatic")) AND (English[lang] AND "last 10 years"[PDat])
dialogue, and adjusted its responses to align with established psychological practices.
After about three months of intensive refinement, the AI began to demonstrate a level of conversational ability that was, frankly, unexpected. Feedback from patients was illuminating; some reported a preference for the AI system over human therapists, citing feelings of being less judged and perceiving the AI to be more attentive. It offered advice unfettered by bias and seemed impervious to the patient's background. We even tested to see if its advice varied by patient demographics—a form of implicit bias known to occur with human clinicians—but we were unable to find objective evidence of systematic variations in performance.
Currently, our team is conducting several IRB-approved clinical trials, applying this AI therapy in contexts as varied as chronic pain management, post-bariatric surgery recovery, and support for liver transplant candidates maintaining sobriety. The journey of this project offers just one more example of the potential for AI to become an adjunctive role in patient care.
With massive advancements in AI rapidly influencing most every aspect of healthcare, what does this mean for the future of medicine in general, and the future of gastroenterology, in particular? What will be our role, as GI doctors, when AI systems can effortlessly conduct a high-quality patient interview, generate an accurate and complete differential diagnosis through multidimensional inputs, and even send prescription, imaging, and procedural orders through the electronic health record? While current AI systems do not physically perform procedures such as colonoscopies or ERCPs, it's not outlandish to think such capabilities might emerge. For now, the immediate imperative for non-endoscopic gastroenterology is for us to thoughtfully determine how we will adapt and shape our roles within this evolving landscape.
What about the physical exam? While AI has yet to cross the threshold into this hands-on aspect of medicine, it can access and interpret imaging studies such as abdominal CT scans, potentially identifying conditions that may elude the probing fingers of even the discerning clinicians. However, it's neither practical nor economically sensible to rely on an AI's analysis of CT scans for every case
“It's more apt to consider AI as 'augmented intelligence' rather than purely 'artificial,' emphasizing collaboration with technology to enhance—not replace—our diagnostic and therapeutic skills.”
of abdominal discomfort in the hopes that it will identify the issue. Take, for example, a patient suffering from chronic myofascial abdominal wall pain. A normal CT scan won’t reveal the problem, and without integrating the results of a physical test like the Carnett maneuver, an AI system would miss the diagnosis. And what about a patient with rectal bleeding? A thorough rectal examination is still indispensable. To date, human clinicians are required to assess for hemorrhoids and, when appropriate, perform anoscopy. We don't have robots that can undertake these tasks, and it doesn't seem likely that we will in the foreseeable future (one hopes...).
Ironically, in an era of AI-enabled gastroenterology, there has never been a greater need to learn and perfect an ageold technique—laying hands on the patient. This foundational aspect of patient care has, regrettably, seen a decline in practice. I've encountered cases where trainees presented patients without having conducted a physical exam at all—a startling omission. The rectal exam, for example, is often overlooked in many clinics, and the nuanced techniques of abdominal palpation and percussion are not as commonly practiced among trainees as they should be.
Now, more than ever, there is a pressing need to reinforce these essential skills. AI systems may be capable of suggesting the need to check for a Carnett sign in someone with positional abdominal pain, perform a rectal examination in the setting of GI bleeding, inspect for aphthous oral ulcers in a patient at risk for IBD, or assess lunula size in the nail bed of someone with cirrhosis, among hundreds of other overt and subtle physical exam maneuvers. Yet, it remains the domain of human clinicians to actually perform these examinations. As AI assumes a more significant role in diagnostic reasoning, the value of physical examination skills paradoxically increases. Gastroenterology training programs must prioritize and invest in teaching the art and science of the physical exam. This approach will not only enhance patient care but also ensure that clinicians can provide the comprehensive data AI tools require to support and extend their diagnostic capabilities.
We must also remain vigilant in overseeing AI systems for potential errors. Despite the inevitable improvements that will come over time, the risk of inaccuracies and misjudgments persists. It's more apt to consider AI as "augmented intelligence" rather than purely
"artificial," emphasizing collaboration with technology to enhance—not replace—our diagnostic and therapeutic skills. This partnership mandates that we develop new educational approaches, teaching medical students and trainees to harmonize their clinical judgment with AI's capabilities. The ideal practice will find its equilibrium between human intuition and machine precision.
A prevalent belief underscores that AI will not simply replace doctors; however, those adept at leveraging AI will advance quicky beyond their peers who do not. We may soon enter an era where excluding AI from the diagnostic process could even be viewed as a form of malpractice. Yet, the indispensable human element remains paramount. The amalgamation of our cognitive faculties with AI's analytical power requires deliberate practice and training—a process that needs to commence now. Professional bodies like the American College of Gastroenterology (ACG) are pivotal in crafting best practices and curricula that guide clinicians in incorporating AI into their practice. This integration aims not only to preserve but to enhance our innate diagnostic capabilities through AI, all the while remaining acutely aware of its limitations.
Furthermore, accelerating research into AI's application in digestive diseases is imperative. Our investigative efforts must expand to encompass a broad spectrum of concerns. This includes safeguarding patient privacy and security, establishing ethical guidelines in collaboration with GI professional societies, addressing and mitigating biases related to race, ethnicity, and gender, and ensuring robust governance and transparency of AI systems. These critical areas should be a focal point for leading research institutions, and a source of robust funding from bodies like the NIH and its National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Additionally, training programs are in a prime position to encourage their most promising talents to pursue AI research, thereby shaping a future in which AI fully complements and enhances the fields of gastroenterology and hepatology.
As we navigate the exponential emergence of AI in healthcare, it's vital to remember that our deep-seated need for human connection, shaped by millennia of social evolution, cannot be fully replicated by technology. For now, at least, and probably for a long time to come, patients will still turn to human doctors to help guide them through the most vulnerable moments of their lives. While AI can attempt
“AI will serve as a powerful ally, amplifying our capabilities in data analysis and knowledge application, but the core of our practice will ultimately depend on wisdom.”
to simulate empathy and forge connections with increasing efficacy, the complexity of the human brain, with its intrinsic design for social interaction, transcends mere computation. In this new era, the role of doctors will shift from traditional knowledge keepers to curators of deep empathy and wisdom—traits that I believe remain distinctly human.
The future will continue to see machines handling data storage, processing, and knowledge management, allowing us human doctors to focus on applying wisdom in our practice. Despite advancements that enable AI to exhibit traits resembling wisdom, the essence of being human—our ability to empathize, to understand others on a root level, and to partake in shared decisionmaking—remains our unique domain.
We must refine our capacity for genuine human interaction, from the simplicity of eye contact to the complexity of understanding others' inner worlds. The essence of medicine— comforting touch, clear communication, shared decision-making, attention to the patient's broader social context—will rely on our wisdom honed over years of dedicated practice. AI will serve as a powerful ally, amplifying our capabilities in data analysis and knowledge application, but the core of our practice will ultimately depend on wisdom.
Embracing this challenge presents an incredible opportunity to redefine our roles and excel in ways previously unimaginable. Ultimately, AI's emergence challenges us to become the best versions of ourselves, heralding a future where human insight, empathy, and clinical know-how meld with machine intelligence to elevate the art and science of medicine.
Author’s note: I wrote this article myself using good old-fashioned human intelligence. After writing the text, I employed Chat GPT-4 to help copyedit certain passages. I believe it remains important that humans—not computers—primarily write for other humans, but also recognize benefits of AI to support editing of original text written by humans. After all, that would be practicing what this article intends to preach.

Brennan Spiegel, MD, MSHS, FACG
Dr. Spiegel is Director of Health Services Research for Cedars-Sinai, Director of the Cedars-Sinai Master's Degree Program in Health Delivery Science, and Assistant Dean of Clinical and Translational Science in the David Geffen School of Medicine.
WHEN THE COVID PANDEMIC STARTED, many of us gastroenterologists felt isolated, but we were able to connect virtually with friends and colleagues locally and afar. A group of us interested in both food and medicine started to regularly share our culinary creations via Twitter (now X) and Instagram. We found connections, developed a supportive community, and many friendships were created as a result. We started the Culinary Connections as a regular column in ACG MAGAZINE approximately three years ago! We have been delighted to share the experiences,
achievements, and recipes of so many diverse members of the College.
The column has featured fellows, gastrointestinal dietitians, and attendings from all over the country who have introduced us to delicious plantforward cuisine and new foods. The College also supported the publication of two e-books, Gastronomy and GI: The Culinary Connections Collection, Volume One and Volume Two. Thank you for your support and interest in this collaboration. In the future, we hope to share practical techniques and tools
combining both gastroenterology and culinary medicine for the members of the College. We would appreciate hearing what you would like to see in future issues and what could impact both your personal wellness and your patient care. As we enter the summer season, this issue incorporates a refreshing fruit and vegetable salad, seared steak with tangy chimichurri sauce, and steamed lobster. We hope you enjoy and have a great summer!
— Alex, Christina, and Vani

Baylor, Scott & White Health, Killeen, TX
It’s summer, and what’s better than a refreshing seasonal salad. I live in Texas where summers are blazing hot; I bet you wouldn’t want to get slow roasted in the kitchen cooking. I'm presenting to you a salad featuring a medley of seasonal fruits and vegetables that is delightfully refreshing and cooling for the summer. This salad can be served fresh or refrigerated to be served later!


Augusta Healthcare, Fishersville, VA
As a physician, my medical professional life, including medical school, residency, fellowship, and 10 years of employment, had been entirely in urban areas. I received excellent training and worked at prestigious institutions, but never worked or lived in a rural area. I never saw this as a drawback in my medical training or experiences. Several years ago, I had the opportunity to work as a locum tenens gastroenterologist in a small town in Maine.
Gastroenterologists are fortunate to work in our field, but also fortunate to collaborate with fantastic people. While providing a service to the area, I received valuable lessons in return from the individuals I met along the way, including physician colleague, Dr. Kirk Bernadino. My experience in Maine helped me gain a new perspective on community, health care, and living, while also teaching me how to cook lobster!
Ingredients:
• 2 medium-sized green mango, peeled and grated
• 1 large red bell pepper, finely diced in cubes
• 1 cup raspberries
• 1 medium-sized red apple, grated
• 2 medium-sized cucumber, peeled, seeded, finely diced
• 2 small Mandarin oranges, peeled
• Few sprigs of basil, finely chopped
• Few sprigs of fennel, finely chopped
• Few sprigs of dill, finely chopped


Maine is known for its natural beauty, coastline, and people. Maine’s jagged coast is larger than California’s, and the state is filled with vast areas of wilderness. Many people in Maine can trace their heritage for generations and are referred to as Mainers. Mainers are resilient, hardworking, and have a unique connection to the land and sea. In Maine, if you are not born there, you are “from away.” These are lessons I learned as a doctor “from away”:
1. Get outside. Spending more time outdoors has been associated with being less sedentary, more time involved in moderate to vigorous physical activity, and having a lower risk of chronic disease. Mainers spend more time in nature than most of us, and they are outside, whatever the weather. There is an appreciation of all four seasons. Maine is known as “Vacationland” as tourists come in droves during the summer months, which are typically cooler than the rest of the country and filled with sunshine. But Mainers still find plenty to
1. Mix all ingredients.
2. Add salt and pepper to taste (could use Tajin for that extra kick).
3. Serve fresh or chilled.
Note: Other ways to enjoy this delightfulness—
• Add a dollop of yogurt (dairy or dairy-free) to make yummy wholesomeness.
• For tacos: served on warm tortilla with drizzle of lime juice and sour cream.
• Serve with slices of avocado, nasturtium leaves, and edible flowers for Sunday brunch.








quickly, Mainers also prepare better for what nature has in store. Preparation and investing in proper gear make a huge difference.
2. Appreciate the dark and quiet. Living in New York City, the din of traffic and the glare of lights felt normal. I did not realize the noise and light pollution I was accustomed to and forgot what a starry sky looked like. Although uncomfortable at first, I became more accustomed to the darkness and quiet of Maine and grew even to value it.
the local community worked together to help save the Polkys' boat when it was severely damaged. The Polky family hosted our family and endoscopy staff on their lobster boat to give us a glimpse of what lobstering involves. This included filling bait bags, measuring lobsters, putting on the bands, and hauling traps.
past by triggering memories, enriching the present with time shared together, and creating impressions for the future.
My locum tenens experience in Maine taught me a lot and one of my most memorable meals was learning to cook lobster in the Polky kitchen with Bobby Joe and Elaine. I hope you enjoy it as much as I do and make it this summer.

Vanguard Gastroenterology, New York, NY
Living in an apartment, I don't have a grill, but I have perfected reverse searing to the point that I prefer it over other cooking methods. Start with a good marbled steak about 1 to 1.5 inches thick; here, I used ribeye. I prefer to dry brine a day before, but a few hours is enough. To do this, place the steak on a baking rack and salt generously on all sides. Place it in the fridge uncovered. You will see some fluid drawn out in a few hours; don't worry and don't wipe it away. It will reabsorb into the meat. When it's time to cook, preheat the oven to 225°F. While it's heating, remove the steak from the fridge. If there is still some moisture on it, pat it dry. Sprinkle with garlic powder and pepper. Place it in the middle rack for 30-45 minutes. After that, remove it and pat it dry again. Let it rest for 10 minutes while you get a cast iron skillet ready. Once the skillet is ready, I like to start by cooking the fatty edge to
3. Community. Strong social connections have been associated with increased longevity and protection against dementia, inflammation, and depression. There is a strong sense of community in Maine. Mainers work together for common goals and are remarkably resourceful. Lobstering is a good example. Most would agree Maine has the most delicious lobster, but most outsiders do not realize the challenges the men and women who work in lobstering face. While performing endoscopy, I learned about the international trade tariffs, bait and staff shortages, warming waters, challenging weather, and changing regulations facing the lobster industry from Elaine Polky, an endoscopy technician whose husband Bobby Joe is a lobsterman in Tenants Harbor. Recently during a winter storm,
Ingredients:
• 4 lobsters (1 ¼- 1 ½ pounds each)
With the heat of summer approaching, the siren song of grilling season is calling. The ACG Foodies have always preached a plantforward approach, but I admit that, for me, there's nothing better than a good steak. The key, as with all things, is moderation. Red meat and the grill are special to me, as recollections of my father standing in the yard grilling my favorite meals are ingrained in my memories. To this day, I host a barbecue for his birthday to celebrate his life, although this year will be 12 years since his sudden passing. Food is special that way; it connects us to the

1. Fill a large lobster pot with 2 inches of water. Add salt and stir.
2. Bring water to a boil.
• 1 Tbsp sea salt


3. Add lobsters, return water to boiling, and steam for approximately 12 minutes. If you have a steamer basket, you can add it to the bottom of the pot. If not, just add the lobsters on top of each other in the pot as the Polkys do.
4. The lobsters should turn bright red. If not red, steam for a few minutes more. When red, you can check for doneness by pulling on the antenna. It should come off easily.
5. Serve with a side of melted, salted butter, lemon wedges, and corn on the cob.





 Dr. Tennyson with endoscopy tech Elaine Polky and Dr. Kirk Bernadino in Maine.
Dr. Tennyson with endoscopy tech Elaine Polky and Dr. Kirk Bernadino in Maine.
render some fat for the skillet. Once it's smoking a little, place the steak down for ~60 seconds, turn it, and go back and forth every 30 seconds until the desired crust and temperature are achieved. I stop at an internal temperature of 120-123°F, as residual cooking will get it to 130°F, which is medium rare. Once ready, place the steak on a cutting board, season with cracked black pepper (the prior pepper likely burned off), and cover loosely with a foil tent for a 10-minute rest. Cut against the grain and add a sprinkle of flaky finishing salt. Serve and enjoy!
For modifiers, I sometimes add butter to the pan with garlic to baste
I also love a tangy chimichurri sauce with my steak. For the chimichurri, use 1 bunch of cilantro, 1 bunch of parsley, ~1/3 of a shallot, and a few garlic cloves. Mince them finely with red pepper flakes (for extra kick, you
Ingredients
• 1 to 1.5 inch thick ribeye or other well-marbled steak
• Kosher salt
• Garlic powder
• Black pepper
• Flaky finishing salt (like Maldon)
• Food thermometer
Steps:
1. Dry brine the steak for few hours, up to 1 day ahead by placing it on a baking rack, salting generously all over, and refrigerating uncovered on a cooling rack.
2. Preheat oven to 225°F. Remove steak from fridge, pat dry, and season with garlic powder and pepper.
3. Bake steak for 30-45 minutes.
4. Remove from oven, pat dry again, and let rest 10 minutes.
5. Heat a cast iron skillet over high heat until smoking. Render some fat from the steak edge in the pan.
6. Sear steak for 60 seconds per side at first then flipping every 30 seconds, until desired crust forms.
7. Transfer to cutting board, season with cracked black pepper, tent loosely with foil, and rest 10 minutes.
8. Slice against the grain, sprinkle with flaky salt, and serve.


We would like to hear from you if you have personal connections with GI & gastronomy. Contact ACG magazine staff by email at acgmag@gi.org to share your story with the ACG community. You can also tweet using #ACGfoodies to connect with the community.
Ingredients

• 1 bunch cilantro
• 1 bunch parsley
• 1/3 shallot, minced
• 2-3 garlic cloves, minced
• Red pepper flakes
• Salt
• Olive oil
• Red wine vinegar or lime/lemon juice
Steps:
1. Finely mince the cilantro, parsley, shallot, and garlic.
2. Add red pepper flakes and salt to taste.
3. Stir in olive oil and red wine vinegar or lime/lemon juice to reach desired consistency.
4. Serve chimichurri sauce alongside reverse seared steak.





Jill K. J. Gaidos, MD, FACG in Conversation with Sara N. Horst, MD, MPH, FACG
asynchronous care models like eVisits or eConsults. I also want to help with education around how to help people do their daily work a little bit better through the EMR because it’s such a big part of our lives.
JG: One of the challenges for physicians is that IT is not a comfortable space for us. We figure out how we interface with the EMR the least amount possible to get our work done, close the chart, and walk away. So, how do you educate clinicians or get people comfortable making changes to the EMR, opening their eyes that charting and placing orders can be completed more easily?

DR. SARA HORST IS THE ASSISTANT VICE CHAIR FOR DIGITAL HEALTH OPERATIONS for the Department of Internal Medicine and Health IT Clinical Director for Vanderbilt University Medical Center.
JG: What are the duties associated with your titles? What are your job responsibilities at Vanderbilt?


SH: For the Department of Medicine Digital Health Operations position, this is really a place where I can work on everything associated with the electronic medical record, both on the patient-facing side and on the clinician-facing side. I am excited our hospital system is supporting administrative infrastructure around health IT implementation. When a physician wants to change something in the EMR, even with a robust health IT infrastructure, it can be difficult sometimes to interface and even understand what to ask for. I am tasked with trying to improve this clinician experience with the EMR. I’m also spending a lot of time trying to think of innovative ways for us to deliver care through telehealth, through
“I believe having physicians involved in health IT decisions is imperative as we understand the operational downstream effects in patient care.”
—Dr. Horst
SH: I definitely do not have all the answers, but I am excited to be in a space to think about how to help. As a busy clinician, you often figure out one way to do something, even though it may not be the easiest way to do something, and habits form. So, I am trying to tackle it in little pieces. We implemented Epic in 2017, and I saw a lot of potential for improvement after the initial implementation, so I became an Epic Physician Builder. This is a program that allows physicians to learn more about the build foundation background of the EMR and even implement some health IT build. Now, when someone comes to me with a problem, I can say, “OK, I see your problem. There is no perfect solution, but here are some ways we can make this a little bit better.” It’s really satisfying to make an EMR improvement that makes things simpler for workflows, and also allows for measurement of outcomes. This is how we can make improvements in system-based patient care as there is so much power in data. I believe having physicians involved in health IT decisions is imperative as we understand the operational downstream effects in patient care.
JG: How did you get interested in this pathway? We all know this is needed, but not all of us are going to volunteer to help implement changes to the EMR.
SH: I take care of IBD patients, and I was in this nice clinical research space and had figured out how to efficiently pull data from our prior EMR. It was fun, and I was working to expand these projects. But when we implemented Epic in 2017, I realized that data extraction was going to be much different and likely more difficult.
JG: Yes, it’s a complex process!
SH: I actually got pretty frustrated and discouraged, but interestingly I also had just taken part in a women in GI leadership course. Something that really resonated with me in the course was the advice: “Don’t just complain. You should come up with a solution.”
JG: (Laughing) Right!
SH: As this is happening, I heard about the Epic Physician Builder program that was starting at my institution and so I volunteered myself. I knew I needed to understand the background of the EMR to see if I could help make changes. At that point, I was just interested in clinical research and data extraction, but then I started to get into the building piece and really enjoyed it. I started to work on improvements for our clinic and I could see the potential for helping clinicians’ daily lives. Because I had gained interest and knowledge, I started to be asked to be on committees around EMR workflows. I said yes a lot because it was interesting to me, and it just kept building. This was definitely not a career path that I was originally planning. If you had asked me 10 years ago if I was going to be a Clinical Health IT Director and Assistant Vice Chair of Digital Health Operations, I would have said, “What are you talking about?” (Laughing)
JG: (Laughing) Exactly!
SH: It kept me going and the passion was there. I would stay up until midnight trying to work something out in Epic. Once you do that, you realize it’s probably a direction you need to keep pushing.
JG: Yes, absolutely. I have been working with our Epic people to try to facilitate some of the health maintenance documentation for my IBD patients and they were more focused on the fact that our notes are already too long as it is and I shouldn’t include that information. There is clearly a disconnect between IT, practitioners, and the billing office.
“It’s not easy, and, in the end, will still require individual and organizational 'buy-in.' However, even these beginning attempts will help others understand the art of the possible.”
—Dr. Horst
SH: There are actually some solutions that I have come up with, but none are perfect. If the “data in” isn’t good, the “data out” is not going to be good for you. We are still very limited by the inability for EMRs to truly share data elements, such as a DEXA scan from an external location that is scanned in. Am I ever going to find that for you easily in our current EMR infrastructure? No. But I’ve worked through some things to more easily gather data into easily accessible locations in Epic—for us, this is called “Synopsis and Snapshot.” Because I am really passionate about this, I currently sit on the National Epic GI Steering Committee, and I am working to try to implement some of these things that could be put into Epic Foundation and allow more organizations with the same EMR to access it. I think these are the kinds of strategies that we as leaders, and maybe even societies, need to be thinking about a little bit more. It’s not easy, and, in the end, will still require individual and organizational “buy-in.” However, even these beginning attempts will help others understand the art of the possible.
JG: There is so much information in the EMR that you just can’t easily tap into. SH: Now, this is where things get tricky. Our current infrastructure often still requires you to click a button or put it in a flow sheet, which is just not easy for a clinician to do in a busy workday. It’s possible that AI or easier access to natural language processing could take a free form note that you write and turn it into an actual standardized data element that we could use for clinical research and data evaluation. But these strategies are time intensive and expensive currently. How institutions are going to weigh the risks and benefits of this, I don’t think we know the answer to that yet. But there is opportunity there.
JG: That is really interesting. There are quite a few studies showing that women spend more time in the EMR in general, including getting more inbasket messages, spending more time on documentation (Rotenstein LS, Fong AS, Jeffery MM, et al., Gender Differences in Time Spent on Documentation and
the Electronic Health Record in a Large Ambulatory Network. JAMA Netw Open. 2022;5(3):e223935. doi:10.1001/ jamanetworkopen.2022.3935). Do you see a gender difference among the people that you help to optimize their Epic use?
SH: That’s a really interesting question and I don’t know the answers to this completely, and I don’t believe it’s just women who struggle with this. There was a really interesting study out of Mayo Clinic recently (Bali AS, Hashash JG, Picco, MF, et al., Electronic Health Record Burden Among Gastroenterology Providers Associated with Subspecialty and Training. Am J Gastroenterol 2023. DOI: 10.14309/ ajg.0000000000002254), where they looked at clinicians in gastroenterology and found that time in the EMR was specialty driven. So, chronic disease state specialists (such as inflammatory bowel disease and hepatology) spent more time in the EMR. Non-physician providers (NPPs) also spent more time in the EHR. In some clinical infrastructures, it may be that these NPPs are required to take on more day-to-day care in patient calls and message baskets. Primary care clinicians in particular are getting overwhelmed by extra-clinical time duties.
JG: Our primary care doctors are struggling with this increased demand as well.
SH: If you want to see the burden across our institution, primary care is really bearing the brunt. Across health care, we have rapidly changed to giving asynchronous care more. When you look during the COVID pandemic, one study showed that EMR in-basket message volume doubled (Holmgren AJ, Downing NL, Tang M, et al., Assessing the Impact of the COVID-19 Pandemic on Clinician Ambulatory Electronic Health Record Use. J Am Med Inform Assoc. 2022 Jan 29;29(3):453-460. doi: 10.1093/jamia/ ocab268). Suddenly, patients were getting onto the portal because they had to; there was no other way for them to get their care. And then there was the 21st Century Cares Act which requires that all results go to the patient immediately. Our institution found that turning this on immediately doubled messages (Steitz BD, Sulieman
“I find when I am asking for something, I set up a meeting to physically show them exactly what is happening and ask them for an idea around what is a better workflow.”
—Dr. Horst
L, Wright A, Rosenbloom ST. Association of Immediate Release of Test Results to Patients With Implications for Clinical Workflow. JAMA Netw Open. 2021;4(10):e2129553. doi:10.1001/ jamanetworkopen.2021.29553). We have a lot of unintended consequences around trying to get better access to care that our clinicians and teams are feeling. We need to right the ship a little bit, and I don’t think we know exactly how to do this yet. There is a lot of interest. For example, one idea is to use AI to generate draft in-basket messages. This typically works best for the less complicated questions and not as well for the more complex questions or concerns.
JG: Such as the messages that end up in our in-baskets.
SH: Right. Also, institutions are increasingly billing for patient portal messages. Our institution implemented this in 2023. I think this is important, as we are providing more asynchronous care, and we need to start framing this better for patients. There is a lot of time and effort for the clinician to give care over the patient portal even if the patient is not directly in front of them in clinic. Also, patients don’t always want to come to clinic, and I understand that completely.
JG: You highlighted a few of the key strategies for setting boundaries around MyChart messaging in your ACG Magazine article, “Embracing Access to Physicians and Establishing Boundaries,” (available at https://issuu.com/amcollegegastro/ docs/23acgmag-summer-web/29) as well as providing specific criteria for billing for MyChart messages. One of the things that I thought was very interesting is that you have to have permission from the patient to bill them for MyChart messaging. When you are rolling this out, do you tell this to patients in clinic or how do you frame it?
SH: It is so key. I do think that for any of these care options, the patients need to say, “Yes, I want this.” Or they can say, “No, I want to come to clinic instead." Or “I’m going to go to a walk-in clinic.” We had to think a lot about this, and nationally people are handling this differently at every institution. We put together a strategy that is consistent across our institution such that when a patient goes into MyChart, they see the possibility of an eVisit as soon as they enter the portal and give consent. When another institution
implemented a similar strategy, they ended up having < 1% of their MyChart messages as billable visits, and decreased the number of messages that came in by 5-10% (Holmgren AJ, Byron ME, Grouse CK, Adler-Milstein J. Association Between Billing Patient Portal Messages as e-Visits and Patient Messaging Volume. JAMA 2023;329(4):339–342. doi:10.1001/ jama.2022.24710).
JG: One of the challenges with managing the in-basket message is that it’s care on top of care that we already providing. Sometimes patients don’t get that. I have patients who send messages saying, “I need to talk to Dr. Gaidos right now.” But I’m scheduled to be in endoscopy or clinic all day and can’t do a telephone visit while simultaneously doing all my other clinical duties.
SH: We have done such a good job of asynchronous care that it is causing a lot of pressure on our clinical teams to try to do this on top of what we are doing all day in clinic. This is creating a very difficult system to sustain.
JG: Absolutely. Patient questions are just one piece of the Epic in-basket and if all I had to do was keep up with that, it would be relatively manageable. But, we also have lab results that come in as the results are available (so 10 labs ordered for one patient may come in as 10 messages), and staff messages that need to be addressed as well.
SH: Yes, patient messages and calls occur in addition to all the prior authorizations, denial letters, peerto-peers, an outside physician is calling you, or infusion centers are calling. We have not enhanced the infrastructure around the support for that to measure up to the volume of messages that physicians are getting. And, as healthcare costs are higher and margins closer, our ancillary teams are getting tighter. There is nowhere for this work to go. And frankly, a lot of EMRs always just push the messages up to the top which may
be the clinician. It would be advantageous to think about how we can get ancillary teams to work to the top of their license and take some of this work so it would not even make it to the physician. These are difficult workflows to implement, and they require a lot of health IT support and operational buy-in. I don’t believe our message baskets are facile enough quite yet to do that, but I’m hopeful that over the next three to five years, this will get better.
JG: Are there resources for people who are interested in learning more about how to optimize their EMR? Any other training you would recommend?
SH: This is a place where it gets tricky because everybody’s EMR is a little bit different. The rules around what is accessible to clinicians to work on at each institution level are a little bit different. I think we need to start from the ground up. Some of the things I have been doing is talking to fellows. “Hey, when you go out to your practice, these are a few EMR workflows that you need to implement right away to make your life easier in five years.” It’s probably not a bad idea to start enhancing this education all across GI. There are things like the “community library” in Epic. If you can get access, it has a lot of great enhancement ideas, but a busy clinician doesn’t always have time. At an institution level, we have customer care support specialists who can work with clinicians and spend an hour of your time trying to improve your daily clinical care. We need to be better about this, but the time investment is difficult to do.
JG: I definitely want to understand Epic a little bit more, not that I want this to be my full-time job. There is a language barrier when I am trying to ask for things from my Epic team which leads to 10 emails back and forth just to get across the specifics of what I want. How would you recommend someone communicate with their health IT team when having issues with the EMR?
SH: A health IT analyst may not understand the clinical workflow enough to best help you. I find when I am asking for something, I set up a meeting to physically show them exactly what is
happening and ask them for an idea around what is a better workflow. Those have usually been the most successful conversations because even screenshots a lot of the time don’t get to the point of “these are the 15 clicks that I am doing for this.” It’s not always easy to make those conversations happen so I would reserve them for really important, bigger obstacles that you are coming upon. Once you have figured out a workflow change that happens in one area, I have realized that I can actually use that in other areas. I think if you are interested in learning more, little pieces can be helpful like “Smartphrases,” “Smartlists,” “Smartlinks," and “Letter Templates” in Epic. Often these can be shared with your teams, and starting here can be an entry into bigger and better things!

Jill K. J. Gaidos, MD, FACG Dr. Gaidos is Associate Professor of Medicine at the Yale School of Medicine Section of Digestive Diseases and Director of Clinical Research for the Yale IBD Program.


Sara N. Horst, MD, MPH, FACG
Dr. Horst is Assistant Vice Chair for Digital Health Operations for the Department of Internal Medicine and Health IT Clinical Director for Vanderbilt University Medical Center.

The coronavirus-19 (COVID-19) pandemic has left a lasting influence on fellowship recruitment. This has impacted both applicants and programs. In 2023, the Association of American Medical Colleges (AAMC) continued to recommend virtual interviews for training programs. Hybrid options where interviewees can select either in-person or virtual interview options within the same program are largely discouraged. Cited concerns for hybrid interviews include the risk of emphasizing inequities for applicants from disadvantaged backgrounds and the potential for bias in interviewer evaluations.
We have developed a variety of strategies to help highlight our program’s strengths using the virtual interview format. One of these strategies is to offer virtual happy hours. Prior to the COVID-19 pandemic, invited applicants would meet with current fellows at our program during an in-person happy hour including food and drinks. We have adapted to the virtual platform by attempting to replicate this experience. At Mayo Clinic, we first started hosting virtual fellow-only “Happy Hour” sessions as part of our gastroenterology virtual recruitment in 2020.
The intent of these happy hours is to help applicants learn about the culture of our program in a low-stakes environment. We hope that these
“Virtual happy hours show the collegiality among fellows and give insight into the inner workings of a program.”
social events are useful for providing a glimpse into the camaraderie among our co-fellows. Importantly, these sessions are not part of our program’s formal evaluation process.
Our program’s goal is to create a structured and engaging applicant-fellow virtual session in a relaxed setting. Current trainees volunteer to attend these virtual sessions with roughly five fellows per 10 to 12 applicants at each event. We intentionally invite a diverse group of fellows from different stages of training and career interests. This provides applicants with a range of views and perspectives. No faculty or program leadership are present.
Each happy hour takes place the evening prior to the interview day. A chief GI fellow serves as the moderator and host for the evening. We emphasize that the session is not recorded or used for the purposes of any evaluation. Applicants are reminded that the virtual happy hour is a risk-free environment and are encouraged to be open with their questions. Each session begins with an overview of the happy hour, including the structure of breakout rooms. We start with an easy and fun icebreaker question (e.g., what is your favorite ice cream flavor?). Current fellows
also share their background, interests, and favorite things about the fellowship program and the community. The introduction is followed by small breakout sessions each lasting about 20 minutes. Afterwards, applicants switch to another breakout room with a new group of current fellows. We finish each happy hour with a full group wrap-up to answer remaining questions and provide follow-up contact information.
We wanted to learn more about applicants’ overall experiences with these virtual happy hours during the GI fellowship application process, as well as whether they influence ranking of programs. We also asked for feedback regarding our specific program to improve these applicant-fellow virtual sessions in the future.
During the 2022 GI fellowship match cycle (2023 appointment year), we reached out to everyone who applied to our fellowship program to participate in a short, emailed survey. The survey took no longer than five minutes to complete. Applicants who interviewed at our institution were sent additional questions specific to our virtual happy hour. All responses were anonymous, and we asked a combination of multiplechoice and open-ended questions.
We learned that at least half or more of GI programs offered a virtual, fellow-only session during the past interview season. Applicants attended these sessions for most interviews. Importantly, we learned that most applicants considered these sessions to be a valuable part of their interview experience. Almost half reported these sessions altered their ranking decisions for GI programs.
Applicants enjoyed a variety of aspects of the virtual happy hour experiences. Recurring themes include significant cost savings, decreased use of vacation days, and overall usefulness of the sessions.
A particularly candid moment was when current fellows offered their endoscopy suite playlists. The virtual sessions are not without obstacles; it is difficult to replicate in-person dynamics via Zoom. Some applicants also find that the virtual setting does not give a full picture of the program.
Positive comments about having a fellow-only virtual social event:
• “I found the virtual happy hour extremely helpful!”
• “Really enjoyed the range of fellows present from first- to third-year fellows and enjoyed the small breakout rooms.”
Comments highlighting areas for improvement:
• “…transitioning to a ‘second look’ in-person happy hour, it would be great to get to know the program culture better in person.”
• “Think [break out room] has to be the ‘right size.’ Too small will lead to a lot of awkward pauses, awkward silence, etc., whereas very large breakout rooms will be hard to manage, and certain voices can get lost or important opinions do not get heard.”
Overall, virtual social events are a valuable part of the interview process. Most applicants attend these sessions as part of their evaluation of fellowship programs. Virtual happy hours show the collegiality among fellows and give insight into the inner workings of a program. Happy hours are also a fun opportunity for current fellows to expand their peer network. In our experience, planning a fellowonly virtual happy hour requires little administrative work, yet these sessions considerably impact applicants’ perception of a program. We have found that virtual social events can even influence applicants’ ranking decisions.
We continue to offer and improve these sessions as an important part of our virtual recruitment process. In a post-pandemic interview environment, virtual platforms are likely here to stay. Virtual social events are a powerful tool to highlight current fellows in a lowerstakes setting and show life outside the program. Future ideas are to also offer an in-person Second Look visit, ideally occurring once program ranking lists are submitted and before applicants’ lists are due. We hope that by sharing our
experience, we can empower other GI programs to use a virtual happy hour to help attract qualified, diverse candidates.
 Gianna L. Stoleru, MD
Gianna L. Stoleru, MD
University of Virginia Second-Year GI Fellow
How did the virtual social hours enhance your overall fellowship interview experience?
While different than in-person social hours, the virtual social hours allow for more one-on-one time to ask fellows specific questions. The virtual social hours also give a glimpse into how the fellows at an institution interact with each other. I tried to take note of things such as whether or not the fellows were having fun together during the social hour, and how easy or not it was to keep conversation flowing. To me, it was a good sign if we could have a fun, easy flowing conversation virtually – I believe this is more difficult to do online than in person and was reassuring when it occurred.
How do the virtual social hours compare to in-person sessions you may have had during residency recruitment prior to COVID-19? In-person social sessions prior to COVID-19 allowed for more organic socialization but also an opportunity to see the city/town where a program is located. I often enjoyed exploring a new place on my way to the social hour, and once at the designated meeting point, many residents would point out other nearby things to see or do. Virtual social hours are more for information gathering and observation than socialization, in my opinion.
What were the most effective ways a virtual social hour with current fellows allowed you to get a sense of the program’s culture?
I preferred social hours where the fellows were together in a group, rather than individually on computers at various locations. This helped with
making observations about the group dynamic. Scheduling the social hour on the same day as the interview also was most efficient from the interviewee standpoint. This is in comparison to inperson interviews, where the social hour usually occurred on the evening before the interview day.
Could you provide some tips to future applicants as to how they should conduct themselves and interact during these sessions?
It is very noticeable when certain interviewees are engaged and asking questions whereas others will not un-mute themselves the entire session. My best advice is to participate, keep your camera on, and try to engage as much as possible. This is the way to get the most out of your virtual social sessions. If you are someone who struggles with socializing over the internet, make sure you're paying attention to how fellows interact with each other so that you can still gain valuable insight from the session.
Could you provide some tips to program directors and coordinators on how to improve this process?
Something that our program has done over the last few years is to standardize our virtual social sessions, and ensure that we have fellows available to participate ahead of time. We utilize the same set-up that has been optimized for the interviewee experience (room layout, camera, and microphone positions, table positions) and participate as a group each time. It is important as an interviewee to see the diversity in a program as well, so knowing who will represent your program at each session ahead of time is something to put thought into. This also ensures you have an adequate number of available fellows to participate. The more the merrier!
 Vibhu Chittajallu, MD
Vibhu Chittajallu, MD
University Hospitals Cleveland Medical Center
Third-Year GI Fellow
How did the virtual social hours enhance your overall fellowship interview experience? It provided an opportunity to ask questions to current trainees that may
be more specific to life outside of the hospital, such as where do most trainees live, fun activities available in the area, and the camaraderie of the program.
How do the virtual social hours compare to in-person sessions you may have had during residency recruitment prior to COVID-19?
Virtual social hours are substantially less interactive than in-person sessions due to the inherent difficulty of being able to interject or have more than one conversation at a time. I recognize that it was a necessary adjustment during the pandemic and has at least partially accounted for the benefits of an inperson social hour.
What were the most effective ways a virtual social hour with current fellows allowed you to get a sense of the program’s culture?
I felt social hours with fewer interviewees and more current trainees allowed for better interaction and was easier for interviewees to be given a chance to ask questions more seamlessly.
Could you provide some tips to future applicants as to how they should conduct themselves and interact during these sessions?
This is your opportunity to clarify questions regarding the structure of a program and to gain better insight into the program through the lens of a current trainee rather than faculty. Please utilize the social hour as an opportunity to also learn more about the fellowship culture both inside and outside of the hospital.
Could you provide some tips to program directors and coordinators on how to improve this process?
Provide social hours with good ratios of current trainees to interviewees and potentially adjust the model entirely to being one current trainee to one interviewee so it can be a straightforward conversation instead.
 Smit Sunil Deliwala, MD Emory University School of Medicine
Smit Sunil Deliwala, MD Emory University School of Medicine
Second-Year GI Fellow
How did the virtual social hours enhance your overall fellowship interview experience?
Gave me a better understanding of the fellows and a chance to talk to them in a relaxed atmosphere.
How do the virtual social hours compare to in-person sessions you may have had during residency recruitment prior to COVID-19? Comparable hours.
What were the most effective ways a virtual social hour with current fellows allowed you to get a sense of the program’s culture?
Group discussion. No PowerPoints.
Could you provide some tips to future applicants as to how they should conduct themselves and interact during these sessions?
Semi-formal session, relaxed, have fun, and network. It’s also a good chance to meet other applicants.
Could you provide some tips to program directors and coordinators on how to improve this process?
Let interviewees know about the social hour when they receive their interview email. Important to create a relaxed and fun vibe, so interviewees can talk carefree. Do not recommend faculty in this process.
 Rebecca R. Yao, MD Mayo Clinic Rochester
Rebecca R. Yao, MD Mayo Clinic Rochester
Third-Year
GI FellowHow did the virtual social hours enhance your overall fellowship interview experience?
The virtual social hours offered a more casual look into programs and were a really valuable way to ask about the fellow experience – especially to ask questions that are practically relevant such as day-to-day logistics, but don’t
significantly influence personal ranking and are not as meaningful for interview day discussion. Being just an hour on the evening prior to the interview, the social hours also served as a way to get a feel for the culture and the collegiality of the program.
How do the virtual social hours compare to in-person sessions you may have had during residency recruitment prior to COVID-19?
As part of the first year of virtual residency interviews in late 2020, I actually never experienced in-person residency recruitment myself. I can imagine that in-person sessions offer more of the intangible “feel” of a program, and physically seeing the hospital campus and city in which one may live for the next three years is also important. And certainly, there’s an inherent amount of awkwardness and uncertainty that arises any time in a new setting with strangers on a virtual call, that probably would not be the case in person. Regardless, I feel as though virtual sessions still provide important insight into a program and its culture, and are an important feature of the virtual interview process.
What were the most effective ways a virtual social hour with current fellows allowed you to get a sense of the program’s culture?
Paying attention to how the fellows interact with each other and with the applicants was one of the most important and effective aspects for me. If you can envision yourself amongst the fellow group you’re with, that’s a great sign.
Could you provide some tips to future applicants as to how they should conduct themselves and interact during these sessions?
Be engaged – I still struggle with Zoom anxiety at times, especially pre-interview, but speaking up and asking a few questions really benefits yourself, the other interviewees, and the fellows who graciously take the time to hold the sessions. It is also helpful to ask about the strengths of the institution from the fellow perspective since this can inform one’s understanding of the program during the interview and the areas the institution
chooses to highlight. Could you provide some tips to program directors and coordinators on how to improve this process? Having some amount of structure to the virtual social hour is helpful. An hour of free rein questioning can potentially be tedious; thus, separating the hour into breakout rooms with smaller groups (which lowers the social barrier to asking questions), or adding in time for an icebreaker can make the sessions flow better. Ultimately, I believe trainees invest as much into the recruitment process as a program invests in them, and continuously seeking feedback from fellows throughout the year and incorporating positive change will pay dividends for everyone, including future applicants.
 Raseen Tariq, MD Mayo Clinic Rochester Third-Year GI Fellow
Raseen Tariq, MD Mayo Clinic Rochester Third-Year GI Fellow
How did the virtual social hours enhance your overall fellowship interview experience?
The virtual social hours significantly enhanced the fellowship interview experience by providing an accessible way to interact with current fellows prior to the actual interview day. This allowed for a relaxed setting to ask candid questions and gain insights into the fellowship program without the stress of formal interviews. These sessions also saved travel time and expenses, making it easier to participate in multiple programs.
How do the virtual social hours compare to in-person sessions you may have had during residency recruitment prior to COVID-19?
Compared to in-person sessions during residency recruitment prior to COVID-19, virtual social hours lack the physical presence and direct personal interaction, which can sometimes limit the depth of connections made. However, they do offer greater accessibility and convenience. The ability to join from anywhere reduces logistical challenges and allows candidates to engage with more programs than might be possible in-person.
What were the most effective ways a virtual social hour with current fellows allowed you to get a sense of the program’s culture?
The most effective aspect of virtual social hours was the informal interaction with current fellows. Hearing firsthand experiences and observing the demeanor and enthusiasm of the fellows provided valuable insights into the program’s culture. Breakout rooms with smaller groups were particularly useful for asking specific questions in a more intimate setting, making it easier to gauge the collegiality and support within the program.
Could you provide some tips to future applicants as to how they should conduct themselves and interact during these sessions?
• Be prepared with questions that are meaningful to you and reflect your interest in the program.
• Engage actively by participating in discussions and showing enthusiasm.
• Keep your video on, when possible, to create a more personal connection.
• Be mindful of your body language and professional appearance, even in a virtual setting.
Could you provide some tips to program directors and coordinators on how to improve this process?
• Ensure a stable and user-friendly technology platform to avoid technical difficulties.
• Provide a clear structure for the session, but also allow for spontaneous interaction and questions.
• Consider hosting multiple small sessions to facilitate more meaningful interactions rather than one large group.
• Provide information ahead of the session, such as program highlights or fellow profiles, to facilitate more informed discussions.
• Follow up with participants to gather feedback for continuous improvement of the virtual experience.

In February 2024, the Indian Society of Gastroenterology (ISG) hosted the World Gastroenterology Organisation's Train the Trainers (TTT) program in Kolkata, India. This intensive workshop, held from February 8-10, marked a significant opportunity for GI educators globally to convene and enhance their teaching and training abilities. The ACG sponsored Vivek Kaul, MD, FACG, as a TTT faculty member, and supported travel for two participants, Shivangi T. Kothari, MD, FACG, and David T. Dulaney, MD.
“The participants who attend TTT are now well aware that we do not teach gastroenterology but introduce them to educational techniques of how to teach gastroenterology.”
—James Toouli, MD, MBBS, PhD, FRACS 2013-2015 WGO President Adelaide, Australia
Since its inception in 2001, TTT has traversed the globe, hosting over 20 workshops, each tailored to cultivate the pedagogical prowess of its participants. Limited to 50 nominees from the various GI societies, the workshops not only offer educational modules but also integrate team-building activities, fostering camaraderie among attendees. The hallmark of TTT is its commitment to refining teaching methodologies and fostering a vibrant worldwide community dedicated to advancing GI education.

Shivangi T. Kothari, MD, FACG
Associate Professor of Medicine, Associate Director of Endoscopy University of Rochester Medicine, Rochester, NY
Shivangi T. Kothari, MD, FACG
“This was my first TTT workshop and I can say that TTT Kolkata organized by the WGO and Dr. Geoffrey Metz and Dr. Kelly Burak was an amazing and unique experience. It was an honor to be selected by the ACG to participate in the course. This is a unique, one-of-a-kind interactive workshop focused on training the next generation of GI educators. The training sessions focused on team building projects, conflict resolution, providing feedback, understanding study designs and statistics, and endoscopy teaching, to name a few. It was inspiring to meet peers from around the world, network, and share experiences and knowledge. Dr. Mahesh Goenka, Dr. Govind Makharia, Dr. Mathew Philip, and the team of the Indian Society of Gastroenterology did an outstanding job hosting the workshop and I truly had a memorable time.”

David T. Dulaney, MD
Program Director, San Antonio Uniformed Services Health Education Consortium (SAUSHEC) Gastroenterology Fellowship, Fort Sam Houston, TX
David T. Dulaney, MD
“The WGO Train the Trainers was an invaluable experience that empowered me to become a more wellrounded educator. As a young faculty and newly appointed program director, the lessons in hands-on endoscopy teaching, curriculum design, and scholarly activity will allow me to develop into a master educator for my fellows. I'm thankful to the ACG for the opportunity to learn so much at TTT and to the WGO and ISG for developing such an amazing program.”

Vivek Kaul, MD, FACG
Segal-Watson Professor of Medicine, University of Rochester Medicine, Rochester, NY; Secretary General of the WGO; faculty member for the Kolkata TTT Course; Dr. Kaul is an alumnus of the TTT program (ACG-sponsored attendee of TTT Taiwan, 2015)
Vivek Kaul, MD, FACG
"This was a high-impact educational and training event with renowned national and international faculty engaging with attendees from 11 countries. Such focused, high quality, interactive programs have a transformational impact for the attendees and open new doors for networking and collaboration for the next generation of physician educators.”





Clinical take-aways and evidence-based summaries of articles in GI, Hepatology & Endoscopy.
EVIDENCE-BASED GI (EBGI) evaluates new research articles published across leading general medicine, GI and Hepatology journals.
ACG Editors identify the highest quality studies published on important topics and create structured abstracts summarizing the study for quick reference and provide commentary on how the data is applicable to clinical practice.
Editors record audio summaries for easy listening on the go.
Follow EBGI on Twitter for weekly tweetorials @ACG_EBGI
Member benefit!
Watch for the eTOC delivered in your inbox monthly!

EBGI has Podcasts Too! Read. Listen. Learn.
Stay up to date on notable studies in major medical journals with ACG’s latest publication, Evidence-Based GI edited by Philip S. Schoenfeld, MD, MSEd, MScEpi, FACG.

Full issue download available as PDF: gi.org/ebgi
























OVER THE PAST DECADE, the global burden of alcohol-associated liver disease (ALD) and alcohol use disorder (AUD) among women aged 15 to 49 years has increased, according to a large-scale study using the Global Burden of Disease Study 2019 database and published in The American Journal of Gastroenterology in May 2024. These escalating trends mirror global increases in alcohol consumption that detrimentally affect young womens' health, and which are important predictors of alcohol-associated complications at later stages of life and afflict maternal and fetal health.


In Clinical and Translational Gastroenterology, Lembo, et al. report on clinical outcomes for prucalopride in chronic idiopathic constipation. A case of ischemic colitis after taking progesterone-only contraceptives for two months is featured in ACG Case Reports Journal
Pojsakorn Danpanichkul, MD; Cheng Han Ng, MBBS; Mark Muthiah, MBBS; Kanokphong Suparan, MD; Darren Jun Hao Tan; Kwanjit Duangsonk, PhD; Banthoon Sukphutanan, MD; Siwanart Kongarin; Nateeluck Harinwan, MD; Nuttada Panpradist, PhD; Hirokazu Takahashi, MD, PhD; Takumi Kawaguchi, MD PhD; Polathep Vichitkunakorn, MD, PhD; Nathorn Chaiyakunapruk, PharmD, PhD; Surakit Nathisuwan, PharmD, BCPS; Daniel Huang, MBBS; Juan Pablo Arab, MD; Mazen Noureddin, MD, MHSc; Jessica Leigh Mellinger, MD, MSc; Karn Wijarnpreecha, MD, MPH. The American Journal of Gastroenterology ():10.14309/ajg.0000000000002642, March 2024. | DOI: 10.14309/ajg.0000000000002642
Over the past decade, the global burden of alcohol-associated liver disease (ALD) and alcohol use disorder (AUD) among women aged 15 to 49 years has increased.
Alcohol-related complications significantly affect the health of young adults, including liver and psychiatric complications.
Young women exhibit higher susceptibility to these complications compared with men.
We quantify the global burden of alcohol use disorder, alcohol-associated cirrhosis, and liver cancer from alcohol in young women.
Our study highlights Europe's high burden of alcoholassociated cirrhosis and alcohol use disorder and Highincome Asia Pacific's pronounced burden of liver cancer due to alcohol in young women.
Trend analysis shows a decreased impact of alcohol use disorder but an escalated burden of alcohol-associated liver disease in young women over the past decade.
READ: bit.ly/ajg-danpanichkul-et-al
[CLINICAL & TRANSLATIONAL GASTROENTEROLOGY]
Anthony Lembo, MD; Brooks D. Cash, MD; Mei Lu, MD; Emi Terasawa, PhD; Brian Terreri, PharmD; Shawn Du, PhD; Rajeev Ayyagari, PhD; Paul Feuerstadt, MD; Baharak Moshiree, MD; Ben Westermeyer, BA; Selina Pi, BSE; Mena Boules, MD
In a comparison of constipation-related symptoms and complications before and after prucalopride initiation in adults with chronic idiopathic constipation (CIC), this study found that constipation-related symptoms decreased six months after prucalopride initiation (abdominal pain, abdominal distension, and nausea). Overall constipation-related complications also decreased six months after prucalopride initiation (intestinal obstruction, hemorrhoids, and rectal bleeding). Their findings suggest that
Epidemiological research on these issues remains insufficient. [ACG CASE REPORTS JOURNAL]

prucalopride may be associated with improved constipation symptoms and complications over a six-month period.
READ: bit.ly/ctg-lembo-et-al

Medha Rajamanuri, MD; Meher Garg, AS; Harris Siddiqui, MD; Sreeram Pannala, MD. ACG Case Reports Journal, April 2024. | DOI: 10.14309/crj.0000000000001313
This study shares the case of a 30-year-old woman who developed ischemic colitis after taking progesterone-only contraceptives for two months. She was treated with a dose of intravenous ciprofloxacin and metronidazole for possible infectious colitis, followed by a colonoscopy which showed segmental erythema and ulceration of the descending and sigmoid colon. The authors reported that her symptoms improved over a period of two weeks after stopping use of her contraceptive medication.
READ: bit.ly/acgcrj-rajamanuri-et-al


Diagnosis and Initial Assessment

Scott Tenner, MD, MPH, JD, FACG; Santhi Swaroop Vege, MD, MACG; Sunil G. Sheth, MD; Bryan Sauer, MD, MSci, FACG; Allison Yang, MD, MPH; Darwin L. Conwell, MD, MSc, FACG; Rena H. Yadlapati, MD, MHS, FACG; and Timothy B. Gardner, MD, FACG
Ultrasound patients with acute pancreatitis (AP).

Etiology In absence of gallstones or ETOH use, evaluate serum triglyceride level (>1000 mg/dL more suggestive)

The most common etiologies of AP are gallstones (40-70%) and alcohol (25-35%)

Monitor patient closely the first 6-12 hours while checking vitals, BUN/HCT to assess fluid needs.
LR preferred
Moderately aggressive hydration is most important the first 6-12 hours.
Moderately aggressive hydration is of little benefit after 24-48 hours— continue to monitor the patient closely during this time.
Reserve CT for uncertain diagnosis or failure to improve in 48-72 hours. Consider repeat US, MRI, and/or endoscopic US for idiopathic AP.
Reassess volume status within first 6 hours with goal of decreasing BUN

Concern for pancreatic tumor is highest for those aged 40+ with no clear etiology of AP
No antibiotics unless concern for infection.
Risk factors for severe disease:
• SIRS
• High/rising BUN
• High/rising HCT
• Obesity

• Extra-pancreatic collections, pleural effusions or infiltrates
• Altered mental status
• Older age and comorbidities
CCY recommended in those with 2nd episode of AP with no cause.
In mild disease, early oral feeding with low fat solid diet (within 24-48 hours) as tolerated.
Avoid parenteral nutrition if possible

If infected necrosis is suspected (typically after 10-14 days), use antibiotics that can penetrate: (1) Carbapenems (2) Quinolones (3) Cephalosporins (4) Metronidazole
In moderately severe or severe disease consider NG for enteral feeding (NG>NJ preferred)
Add small peptide-based medium chain TG oil for tolerance
Continuous feeding > cyclic or bolus
Acute Pancreatitis citation Tenner, Scott MD, MPH, JD, FACG; Vege, Santhi Swaroop MD, MACG; Sheth, Sunil G. MD; Sauer, Bryan MD, MSci, FACG; Yang, Allison MD, MPH; Conwell, Darwin L. MD, MSc, FACG; Yadlapati, Rena H. MD, MHS, FACG; Gardner, Timothy B. MD, FACG. American College of Gastroenterology Guidelines: Management of Acute Pancreatitis. The American Journal of Gastroenterology 119(3):p 419-437, March 2024. | DOI: 10.14309/ajg.0000000000002645
ERCP within 24 hours if complicated by cholangitis
Consider rectal indomethacin, pancreatic duct stent, and hydration to avoid post ERCP pancreatitis
CCY preferably before discharge in mild acute biliary pancreatitis
In stable pancreatic necrosis – wait 4-6 weeks for surgical, radiological, and/ or endoscopic interventions.
Understanding Barrett’s Esophagus: Information for Patients and Caregivers from the ACG Patient Care Committee
OVERVIEW: WHAT IS BARRETT’S ESOPHAGUS?
Barrett’s esophagus (BE) is a condition where the lining of the esophagus (swallowing tube) is damaged and normal tissue is replaced with cells similar to the small intestine. Patients with BE are at a slightly higher risk than the general population for a rare cancer called esophageal adenocarcinoma.
While there are no symptoms specific to Barrett’s, chronic acid reflux or gastroesophageal reflux disease (GERD) are common in these patients.
GERD can be a trigger for the development of BE.
However, not all patients with BE experience GERD.
Not all patients with GERD will develop BE.
An upper GI endoscopy with tissue samples is required to make the diagnosis.
Tests are recommended for those with over 5 years of GERD symptoms PLUS any 3 of the following risk factors:
• male sex
• age over 50 years
• white race
• tobacco smoking
• obesity
• family history of BE
• esophageal cancer in a first-degree relative (parent, sibling, child)
ACG Patient Information: gi.org/topics/barretts-esophagus
Some medications used for GERD may reduce the risk of developing dysplasia (precancerous cells) and esophageal cancer in patients with BE. Endoscopic treatments are the main way to manage BE and early esophageal cancer. Your doctor will give advice on monitoring BE with follow-up endoscopy.
Read the 2022 ACG Guidelines: Diagnosis and Management of Barrett’s Esophagus: bit.ly/acg-barretts-guideline

Learn from successful GI innovators and unpack learnings and pitfalls
Demystify the process of developing new technology
Explore ideas and apply the innovator’s mindset to your everyday practice


ABSTRACT CATEGORIES
• Biliary/Pancreas
• Colon
ABSTRACT CATEGORIES
• Colorectal Cancer Prevention
• Biliary/Pancreas
• Colon
• Endoscopy Video Forum
• Esophagus
• Colorectal Cancer Prevention
• Functional Bowel Disease
• Endoscopy Video Forum
• Interventional Endoscopy
• Liver
• Obesity
• Pediatrics
• Interventional Endoscopy
• Liver
• Practice Management
• Obesity
• Small Intestine
• Pediatrics
• Stomach
• Practice Management
• General Endoscopy
• Esophagus
• GI Bleeding
• Functional Bowel Disease
• IBD
• General Endoscopy
• GI Bleeding
• IBD
• Small Intestine
• Stomach
• Clinical Vignettes/ Case Reports
• Clinical Vignettes/ Case Reports