ACG MAGAZINE



T ACG A C ﹕
B/F C A A
This award recognizes an ACG Member who has provided distinguished contributions to clinical gastroenterology, including: (a) clinical medicine, (b) technology application, (c) health care delivery, (d) related factors such as humanism and ethical concern. It is not intended that this award be given in honor of one’s laboratory research accomplishments.
C S A
This award is bestowed upon an ACG Member who has initiated or has been involved in numerous volunteer programs/ activities, or has provided significant volunteer service post-training. The service must have been performed on a completely voluntary basis and not for the completion of training or position requirements.
D M T A
This award recognizes an ACG Member who has provided meaningful and sustained contributions to trainees/colleagues in gastroenterology. Such contributions could include mentorship or teaching to help develop the mentees’ career, clinical practice, research or academic practice.
D NP/PA T A
This award recognizes a distinguished nurse practitioner or physician assistant who is an ACG Member and has shown long-standing contributions to educating and mentoring NPs/ PAs in the field of gastroenterology and hepatology (GIH). Meaningful contributions in teaching include demonstrating mentorship, preceptorship, curricula development and/or other activities that have an impact in educating and developing future NPs/PAs in the field of GIH.
D﹐ E I A
This award recognizes an ACG Member whose work in the areas of clinical practice, research, teaching and/or leadership has demonstrated an emerging or sustained commitment to the values of diversity, health equity and inclusion.
I L A
This award is given to an ACG Member in recognition of outstanding and substantial contributions to gastroenterology, to the College, and to the international gastroenterology community.
M A C
G
Masters of the College of Gastroenterology shall have been ACG Fellows who, because of their recognized stature and achievement in clinical gastroenterology and because of their contribution to the College in service, leadership, and education, have been recommended for designation as Masters.
NP/PA A C E
This award recognizes a distinguished nurse practitioner or physician assistant who is an ACG Member and has shown longstanding contributions to advancing clinical practice in the fields of gastroenterology and hepatology. Substantial contributions to GI practice include demonstrated practice expertise, leadership, mentoring and collaborative activities that have an impact at the state, regional, national or international level.
S S﹒ W A
This award is given to an ACG Fellow or Master in recognition of outstanding service to the American College of Gastroenterology over the course of an individual’s career.
﹕ A ﹐
S ﹕ ﹒/---
Nominations for all awards must:
• Be accompanied by two le ers of recommendation (three for the NP/PA Awards)
• Include the nominee’s CV
• Conform to the specific nomination requirements
• Be unsolicited by the nominee
Nominations must be submi ed online: gi.org/acg-award-nomination-form
Nomination requirements: gi.org/award-nomination-guidelines
Actress and anal cancer survivor Marcia Cross implores GI physicians to actively screen for an underdiagnosed condition
PAGE 21

TRAINEE HUB
Dr. Katie Dunleavy recounts her experience training GI fellows in Rwanda through GI Rising, Inc.
PAGE 15
ACG PERSPECTIVES
Dr. Colleen Kelly shares her decision to donate a kidney to her Brown University colleague Chuck Hampton
PAGE 35 COVER STORY




“ Speaking about the embarrassment around this issue, it's time that we really end the stigma of the anus because I have fallen in love with mine.”


—Marcia Cross, “Shame Buster Marcia Cross De-Stigmatizes Anal Cancer” PG 21

Dr. Jonathan Leighton on being "all in," participating actively in the GI community
Newly named Leonidas H. Berry Health Equity Research Award, recent publications: ACG Microbiome Monograph and the Endoscopy Unit Orientation Manual, in memoriam for Dr. Eugene Bozymski and ACG past president Dr. Arvey Rogers & more
Dr. Patrick Young's photo "A Study in Blue" of Lháxten/Cerise Creek Conservancy in British Columbia, Canada
Dr. Katie Dunleavy on her experience providing GI training in Rwanda with GI Rising, Inc.
SHAME BUSTER MARCIA CROSS
DE-STIGMATIZES ANAL CANCER
Actress and anal cancer survivor Marcia Cross shares her experience with the underdiagnosed condition
27 CULINARY CONNECTIONS
Three culinary enthusiasts discuss how food is part of their identity and share healthful recipes
31 CONVERSATIONS WITH WOMEN IN GI
Dr. Jill Gaidos in conversation with Dr. Bincy Abraham, an early adopter of intrabdominal ultrasound in IBD
35 MY DECISION TO DONATE A KIDNEY
Dr. Colleen Kelly shares her decision to donate a kidney to her colleague at Brown University
37 IBD 101
A look at the IBD 101 course which gives fellows comprehensive training in IBD diagnosis and management
46 AJG
New ACG Guideline on Alcohol-Associated Liver Disease by Jophlin and Singal, et al
46 CTG
Clinical Long-Term Outcomes of PatientReported Outcomes in the Prospective Real-World Tofacitinib Response in Ulcerative Colitis (TOUR) Registry by Herfarth, et al
46 ACGCRJ
Unusual to “Bee” in the Colon: A Rare Finding on Screening Colonoscopy by Yousaf and Bechtold
PATIENT HANDOUT: ALCOHOL-ASSOCIATED LIVER DISEASE
A patient handout about alcohol-associated liver disease and alcohol use disorder, based on the new ACG Clinical Guidelines on ALD
Executive Director
Bradley C. Stillman, JD
Editor in Chief; Vice President, Communications
Anne-Louise B. Oliphant
Manager, Communications
Becky Abel
Art Director
Emily Garel
Senior Graphic Designer
Antonella Iseas
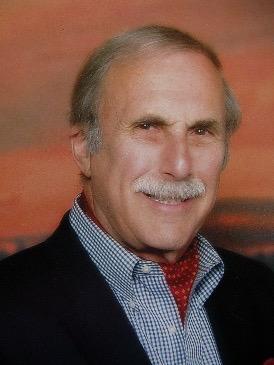
President: Jonathan A. Leighton, MD, FACG
President-Elect: Amy S. Oxentenko, MD, FACG
Vice President: William D. Chey, MD, FACG
Secretary: Nicholas J. Shaheen, MD, MPH, MACG
Treasurer: Costas H. Kefalas, MD, MMM, FACG
Immediate Past President: Daniel J. Pambianco, MD, FACG
Past President: Samir A. Shah, MD, FACG
Director, ACG Institute: Neena S. Abraham, MD, MSc, MACG
Co-Editors, The American Journal of Gastroenterology:
Jasmohan S. Bajaj, MD, MS, FACG
Millie D. Long, MD, MPH, FACG
Chair, Board of Governors: Dayna S. Early, MD, FACG
Vice Chair, Board of Governors: Sita S. Chokhavatia, MD, MACG
Trustee for Administrative Affairs: Irving M. Pike, MD, FACG
Jean-Paul Achkar, MD, FACG
Brooks D. Cash, MD, FACG
Jill K. J. Gaidos, MD, FACG
Seth A. Gross, MD, FACG
David J. Hass, MD, FACG
James C. Hobley, MD, MSc, FACG
Aasma Shaukat, MD, MPH, FACG
Neil H. Stollman, MD, FACG
Renee L. Williams, MD, MHPE, FACG
Patrick E. Young, MD, FACG
youtube.com/ACGastroenterology
facebook.com/AmCollegeGastro
twitter.com/amcollegegastro
instagram.com/amcollegegastro
bit.ly/ACG-Linked-In
CONTACT
We'd love to hear from you.
Send us your ideas, stories and comments. ACGMag@gi.org
CONTACT ACG
American College of Gastroenterology 11333 Woodglen Drive, Suite 100 North Bethesda, MD 20852 (301)263-9000 | gi.org
DIGITAL EDITIONS
GI.ORG/ACGMAGAZINE




American College of Gastroenterology is an international organization with more than 18,000 clinician members representing some 86 countries. The College's vision is to be the pre-eminent professional organization that champions the evolving needs of clinicians in the delivery of high-quality, evidence-based and compassionate health care to gastroenterology patients. The mission of the College is to advance world-class care for patients with gastrointestinal disorders through excellence, innovation and advocacy in the areas of scientific investigation, education, prevention and treatment.

Bincy P. Abraham, MD, MS, FACG
Dr. Abraham is the Fondren Distinguished Professor in IBD and Professor of Clinical Medicine at Houston Methodist-Weill Cornell and Program Director of the GI Fellowship Program at the Lynda K. and David M.Underwood Center for Digestive Disorders. She is a member of the ACG International Relations Committee.

Asmeen Bhatt, MD, PhD
Dr. Bhatt is Assistant Professor in the Center for Interventional Gastroenterology at UTHealth (iGUT), at the University of Texas Health Science Center at Houston. She is a member of the ACG Educational Affairs Committee.

Marcia Cross
Marcia Cross is a co-founder of HPV Cancers Alliance and is a stage II anal cancer survivor. Professionally, she is a Golden Globe and Emmy Award-nominated actress known for such shows as Desperate Housewives, Melrose Place, and the critically acclaimed Everwood

John A. Damianos, MD
Dr. Damianos is a first-year GI fellow-in-training at the Mayo Clinic in Rochester, MN. He completed an internal medicine residency at Yale-New Haven Hospital. His clinical interests include gut microbiome therapeutics, nutrition, IBD, and disorders of gutbrain interaction

Katie A. Dunleavy, MB BCh BAO
Dr. Dunleavy is a third-year GI fellow at Mayo Clinic Rochester. She is editor of the Trainee Hub section of ACG MAGAZINE and is a member of ACG’s Digital Communications and Publications Committee.

Jill K.J. Gaidos, MD, FACG
Dr. Gaidos is a Trustee of the College and former chair of the ACG Women in GI Committee. She is Associate Professor at the Yale School of Medicine Section of Digestive Diseases and Director of Clinical Research for the Yale IBD Program. She serves as ACG Governor for Connecticut and is a member of ACG’s Digital Communications and Publications Committee.

Colleen R. Kelly, MD, FACG
Dr. Kelly is a gastroenterologist at The Brigham and Women’s Hospital, and member of the faculty in the Department of Medicine at Harvard Medical School. She previously was Associate Professor of Medicine at Brown University. She currently serves on ACG’s Research Committee.

Lillian Kreppel
Lillian Kreppel is a co-founder of the HPV Cancers Alliance and is a stage II anal cancer survivor. She is a public speaker, entrepreneur, marketing strategist, and public relations expert, and serves as a patient advocate for the Rectal-Anal Task Force for the National Cancer Institute.

Jonathan A. Leighton, MD, FACG
ACG President Dr. Leighton is Professor of Medicine at Mayo Clinic Arizona and is the Medical Director of the Office of Mayo Clinic Experience there. He also chairs Mayo Clinic Arizona’s Office of Joy and Well-being.

Lisa B. Malter, MD, FACG
Dr. Malter is Professor in the NYU Grossman School of Medicine, Director of Education at the IBD Center of NYU Langone Health, and Director of the IBD Program at Bellevue Hospital Center. She is a member of the ACG Educational Affairs and Training Committees.

Bryan G. Sauer, MD, MSc (Clin Res), FACG
Dr. Sauer is Associate Professor of Medicine and Medical Director of Endoscopy at the University of Virginia. He currently serves as chair of the ACG Practice Parameters Committee.

Patrick E. Young, MD, FACG
Dr. Young is a Trustee of the College, formerly serving as Chair of the ACG Board of Governors. He is Professor of Medicine at the Uniformed Services University of the Health Sciences where he serves as Director of the Digestive Health Division. He is an interventional endoscopist at Walter Reed National Military Medical Center.

Kelly Issokson, MS, RD, CNSC
Kelly Issokson is an IBD-focused registered dietitian and director of the Advanced Dietary IBD Education and Training (DIET) Program at Cedars-Sinai in Los Angeles.
WE HAVE SO MUCH TO BE THANKFUL FOR AS GASTROENTEROLOGISTS but at the same time, the delivery of healthcare has become challenging. Peter Drucker, a well-known management consultant, has described medical facilities as the most complex of organizations. We not only have to manage inpatient and outpatient environments and ensure “hard skills” such as the use of technology and procedural expertise, but we also require “soft skills” which encompass teamwork, empathy, and communication to improve patient outcomes. On top of that, we must understand that we often interact with our patients during some of their worst life events. As leaders in healthcare, we have to be “all in” if we are going to make a difference in the future. But, how do we best do that?
Jackie Robinson, the great baseball player, once said, “Life is not a spectator sport. If you’re going to spend your whole life in the grandstand just watching what goes on, in my opinion, you’re wasting your life.” I happen to agree wholeheartedly, and it is one of the reasons I joined the ACG. I was especially reminded of this a few weeks ago at the 2024 ACG Board of Governors/ASGE Best Practices Course in Las Vegas. What a wonderful event to participate in! The Board of Trustees (BOT), Board of Governors (BOG), and other leaders and members had the opportunity to collaborate, create, and have fun. Seeing the BOG and BOT in action also reminded me that the combined wisdom of all of us is greater than that of any one individual or group. We can do
so much more through teamwork and collaboration, and that is what I love about the ACG. Networking allows us to exchange ideas, build connections, and form new relationships while enhancing career development, expanding knowledge, and fostering new opportunities. It is the way to get things done!
The BOG is an amazing group of individuals, unique to ACG, coming together to inspire, engage, inform, and influence. They co-directed the Best Practices Course with ASGE at the weekend meeting. This alone is a great collaboration of two societies in the interest of their members to deliver a high-impact course. The Governors are representatives throughout the United States and abroad who bring knowledge of challenges and legislative issues from their respective regions. I had the unique opportunity to meet with them and listen to their major issues, including workforce shortages, anesthesia issues, and ongoing concerns about Board certification. I was overwhelmed by the dedication of this group of concerned colleagues, and also incredibly moved by the cross-pollination and collegiality between the BOG and the BOT. This exchange of ideas and close collaboration is just what we need to inform the College’s policy priorities and promote change for the better. Grassroots feedback from our Governors is essential in shaping the strategy and direction of our Legislative & Public Policy Council. The day ended with the BOG and BOT participating in a dinner celebration that included a performance by the Official Band of the ACG, The Beacons, as well as some simply amazing karaoke performances! Yes, we are a talented group in so many ways.
It is also an honor as ACG President to lead my friends and colleagues on the BOT. I may be biased, but this is a wonderful group of diverse and talented individuals from private and academic practice with a broad
“As leaders in healthcare, we have to be ‘all in’ if we are going to make a difference in the future.”
range of talents and experiences. We are also a group who understands the importance of self-reflection and the need to understand our strengths and weaknesses. Through input from our members, it is our priority this year to understand what we can do even better to represent our members, and not rest solely on the successes of the past. To that end, I am delighted to announce plans to analyze and update our current Strategic Plan to better reflect the needs of the College and its members moving forward.
I also want to also acknowledge the great work of the Educational Affairs Committee and the Research Committee, two pillars of our organization. Working tirelessly over that same weekend in January, the Ed Affairs committee developed an impressive agenda for the 2024 Annual Scientific Meeting. Please join me in Philadelphia for ACG 2024! Dedicated members of the Research Committee reviewed and recommended the “best of the best” research grants for funding by the ACG Institute in 2024. I am so proud of the contributions of these two committees!
Looking ahead to April and ACG Advocacy Day, AKA the Washington, DC, “Fly-In,” I will join the Governors as well as members of the ACG Institute’s Emerging Leaders Program to represent clinical gastroenterology before legislators and regulators. The intent is to ensure that Members of Congress are keenly aware of the issues plaguing those of us in GI and hepatology, and ultimately to influence positive change. The Emerging Leaders cohort will engage with the Governors in meetings on the Hill so that they can become the influential leaders of tomorrow.
This is an exciting time for the field of GI and hepatology as well as ACG, and yet I also know there are challenging times ahead. If we all get involved and don’t stay in the “grandstands,” we can do so much together. The ACG is an exciting community of leaders who want to make a difference. Please join us today!
 —Jonathan
—Jonathan
GASTROENTEROLOGIST Leonidas H. Berry, MD, MACG has been honored by naming the ACG Health Equity Research Award as a tribute to his life, work, and leadership in fighting discrimination in medicine.
ACG’s Monograph on Microbiome Therapeutics offers succinct summaries of the very latest science on the human gut microbiome in a concise and clinically relevant resource with expert insights on this rapidly evolving field.
New from the ACG Membership Committee, the Endoscopy Unit Orientation Manual is a thorough and informative volume written in clear and accessible language for the benefit of both clinical and non-clinical staff to provide a comprehensive understanding of GI endoscopy, procedures, equipment, processes, and the roles of team members.
Read more in the pages of Novel & Noteworthy for College news, kudos, and a new podcast from the Women in GI Committee!

UPPER JOFFRE LAKE AND MATIER GLACIER, NLHÁXTEN/CERISE CREEK CONSERVANCY, BRITISH COLUMBIA, CANADA.Patrick E. Young, MD, FACG
Equipment: iPhone 11, panorama mode.
What captured my attention: Mountain lakes are among my favorite places in the world! There may be a physical cost to getting there, but the reward is often a serene and majestic vista, as we see here. In this case, my wife and I hiked roughly 5 kilometers uphill from the base to arrive at the Lake. While there were numerous gorgeous sights along the way (including the lower and middle lakes), we really did not stop to reflect and absorb it all until we reached the upper Lake. Once we did, we were struck by the beautiful blue hue of the glacial lake (the reflection from the rock silt)

as well as the tranquility and grandeur of the surrounding mountains. Feeling small in the vastness of the world has a wonderful way of re-centering us and reminding us that we are just a tiny part of an amazing creation.
Technical Challenges: Given the time of day and sun angle, most of my initial attempts at photographing the scene were washed out. Fortunately, there were a few low-lying clouds passing through. By capturing this image when the sun was partially covered, I was
able to get a good image of the mountains and lake, with a few inspiring beams of light as a bonus.
Thoughts on photography: While I do not consider myself a photographer, per se—I wouldn’t know an f-stop from a bus stop—I have tried to acquire a photographer’s eye. I love how they study the world, taking the time to notice the beauty “hidden” around them. While life is rife with challenges, there is beauty almost everywhere, and in everyone, if we make the effort to find it.

About Dr. Young is a Trustee of the College, formerly serving as Chair of the ACG Board of Governors (2020-2022). He is Professor of Medicine at the Uniformed Services University of the Health Sciences in Bethesda, Maryland, where he serves as Director of the Digestive Health Division. He is an interventional endoscopist at Walter Reed National Military Medical Center.

The ACG Institute is proud to announce that the Health Equity Research Award is now named in honor of the life and legacy of Leonidas H. Berry, MD, MACG. The College and the ACG Institute recognize his many contributions to gastroenterology, and his tireless efforts to end discrimination in medicine and medical schools.
Dr. Berry was a pioneering gastroenterologist, inventor of the Eder-Berry biopsy attachment for the Eder gastroscope, and President of the National Medical Association from 1965 to 1966, among many career distinctions. He joined the College in 1946 and was ACG’s first African American member. ACG bestowed its first Clinical Achievement Award to Dr. Berry in 1987. He was named a Master of the College (MACG) in 1990 in the inaugural cohort of members honored with this distinction.
Tips for Applying for the Leonidas Berry Health Equity Research Award
This two-year award, with funding of up to $75,000 ($50K year-one, $25K year-two based on progress), supports actionable science that will translate to reducing health and/or healthcare disparities.
Applications for ACG Institute Research Awards, including the Leonidas Berry Health Equity Research Award, will open this fall. Look for more information this summer or read last year’s grant announcement: gi.org/research-awards

[MEXICO]
THE COLLEGE SPONSORED TWO FACULTY to travel and participate in the Mexican GI Association Annual Meeting in November in Cancun as part of a symposium on the “Impact of COVID-19 on the Digestive System.”


[GIQUIC NEWS]
[JOY & WELLNESS]


INCREASING JOY AND WELLNESS in
GI was the topic of a virtual grand rounds by Richard S. Bloomfeld, MD, FACG, Chair of ACG’s Professionalism Committee, moderated by ACG President Jonathan A. Leighton, MD, FACG that featured valuable insights on burnout and professional satisfaction as well as actionable strategies to foster a culture of wellness in GI practice.
WATCH: bit.ly/acg-vgr-wellness-bloomfeld

THE GI QUALITY IMPROVEMENT CONSORTIUM (GIQUIC) registry has once again been approved as a Qualified Clinical Data Registry (QCDR) for reporting to the Merit-based Incentive Payment System (MIPS) for the 2024 reporting year.
The QCDR reporting mechanism is a dynamic reporting option that allows providers to report on Quality Payment Program and QCDR measures that are meaningful to their specialty practice and foster improvement in the quality of care provided to patients. The 2024 GIQuIC QCDR is approved to report for individual eligible providers, groups, and virtual groups to the Quality, Promoting Interoperability, and Improvement Activities performance categories.
[PREGNANT PAUSE]
THE ACG WOMEN IN GI COMMITTEE has launched a new podcast series featuring interviews with authors of ACG's Monograph on GI Diseases and Endoscopy in Pregnancy and Postpartum Period.
Each episode of the “GI in Pregnancy Monograph Podcast” includes great conversations. The first two episodes have dropped with more in production!

IBD and Pregnancy with Sunanda V. Kane, MD, MSHS, FACG
Hyperemesis Gravidarum and Nutritional Support with Linda Ahn B. Nguyen, MD, FACG
More topics coming soon!
LISTEN to Podcasts: gi.org/gi-in-pregnancy-monograph-podcast
READ the Pregnancy Monograph: bit.ly/ACG-Pregnancy-2022
LEARN MORE about GIQuIC: giquic.org
LEARN MORE about Medicare’s Quality Payment Program: qpp.cms.gov
community to connect and keep learning with weekly lectures. Since then, experts have delivered hundreds of lectures. A new milestone was reached at the end of 2023, when over 80,000 participants enjoyed ACG Virtual Grand Rounds.
[KUDOS]
THE COLLEGE CONGRATULATES
ACG staff members Claire Neumann, Neen LeMaster, and Morgan Huntt on publishing a scholarly article in CSE Science Editor, a publication of the Council of Science Editors. Their study, “Weighing the Cost: Open Access Article Publishing Charges, Waivers, and Society Membership,” examined the relationship between waiving open access publishing charges for
members and the number of publications submitted to ACG Case Reports Journal by ACG members. They found noticeable increases in the proportion and number of published manuscripts from members and new members, suggesting that individuals were incentivized to join the College in lieu of paying article processing fees. They previously presented this paper as a poster at the 2023 Council of Science Editors annual meeting in Toronto, ON, Canada.


[REQUIRED READING]

–Seven chapters covering the latest scientific insights into the microbiome, featuring concise, clinically relevant summaries with an emphasis on the rapidly evolving therapeutic armamentarium.
READ: bit.ly/ajg-microbiome-monograph
Editors: Neil H. Stollman, MD, FACG and Colleen R. Kelly, MD, FACG.


Ari Grinspan, MD, FACG and Olga Aroniadis, MSc, FACG provide a clinically oriented introduction to the human gut microbiome.



The ACG Membership Committee published a comprehensive manual for the orientation of lay personnel, office desk staff, and ancillary support staff in the endoscopy unit to allow them to navigate the world of GI endoscopy confidently. Co-Editors Nikila Ravindran, MD, FACG, Dayna Early, MD, FACG, and Tauseef Ali, MD, FACG along

FACG
with expert editors and authors have produced a thorough and informative volume with clear and accessible language for the benefit of both clinical and nonclinical staff. The manual introduces endoscopic procedures, equipment, and processes, and outlines the roles of different team members. It is meant to complement existing institutional policies and orientation processes and serve as an essential resource for integrating new staff into your endoscopy unit.
READ: bit.ly/acg-endoscopy-unit-manual
Co-Editors


Dayna S. Early, MD, FACG
Cynthia Ko, MD and Alexa Weingarden, MD, PhD explore non-prescription therapeutics including probiotics and prebiotics.


The monograph covers two new prescription agents: the whole-stool based RBL enema is reviewed by Sahil Khanna, MD, FACG and Caterina Oneto, MD, and


Paul Feuerstadt, MD, FACG and Kerry LaPlante, PharmD review the pillbased Firmicutes spore product, VOS.


Tauseef Ali, MD, FACG
Monika Fischer, MD, MS, FACG and Arnab Ray, MD, FACG elaborate on future therapeutics on the near- and longer-term horizon.


Jessica Allegretti, MD, MPH, FACG and Kira Newman, MD, PhD review the current status of biome therapeutics in IBD, IBS, and other conditions.


Jasmohan Bajaj, MD, MS, FACG and Patricia Pringle Bloom, MD present the emerging and exciting data on the biome and liver health and disease.


[IN MEMORIAM]
EUGENE M. BOZYMSKI, MD, MACG (SEPTEMBER 29, 1935 – FEBRUARY 14, 2024)

With deep sorrow, the College notes the death of Eugene M. Bozymski, MD, MACG of the University of North Carolina, Chapel Hill. Dr. Bozymski was an outstanding teacher and clinician who was the 2020 Samuel Weiss Awardee for his extensive and longstanding service to ACG.
Dr. Bozymski was a tireless and hardworking member of six ACG committees over the years, including the Research Committee, Educational Affairs Committee, and Nominating Committee, and had a tenure as chair of both the Awards Committee and the Practice Parameters Committee. Dr. Bozymski served two terms as the ACG Governor for North Carolina, from 1996 to 1997 and then from 2002 to 2005. As an ACG Governor, he was very much a visible advocate for both his colleagues and patients. Because of his service to the College and his standing in the GI profession, the College recognized Dr. Bozymski as a Master in 2007.
Although his work as Governor and his work on the multiple ACG committees is impressive, his major impact and

Bryan G. Sauer, MD, MSc, FACG Professor of Medicine, University of Virginia, UVA Health; Chair, ACG Practice Parameters Committee
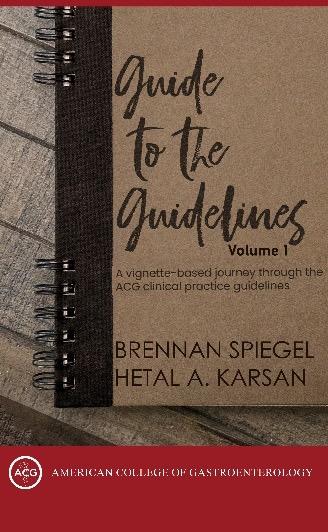
The Guide to the Guidelines, Volume 1, written by Brennan Spiegel and Hetal A. Karsan is a “vignettebased journey through the ACG Clinical Practice Guidelines.”
After seeing the advertisements for this much-anticipated book at ACG conferences, I was excited to get it in my hands.
We all know that the ACG Practice Guidelines are a wealth of knowledge
contribution to the College was as an educator who participated in numerous ACG national postgraduate and regional courses. He is remembered for his lectures which set a standard for clarity and exposition, reflecting the depth of his knowledge and passion for education.
Dr. Bozymski was Emeritus Professor of Medicine at UNC School of Medicine where he served as Head of Endoscopy for many years. A recognized expert in the field of esophageal diseases, disorders of esophageal motility, and therapeutic endoscopy, he played a pivotal role in establishing the Endoscopy Center and the Motility Center at UNC and assisted Duke University in establishing their unit.
In 2007, his trainees and colleagues established the Eugene and Mary Kay Bozymski and William and Linda Heizer Distinguished Professorship at The University of North Carolina, a position now held by Dr. Nicholas Shaheen, the Secretary of the College and past Director of the ACG Institute for Clinical Research & Education.
A graduate of John Carroll University, Dr. Bozymski received his medical degree from Marquette University School of Medicine/Medical College of Wisconsin. He completed a rotating internship at Scripps/Mercy Hospital in San Diego and a 3-year medical residency at Marquette University School of Medicine/Medical College of Wisconsin interrupted by a
written by some of the most prominent content experts in their specific areas. They are a great resource for clinical medicine, and even board studying, as they present recommendations based on the current evidence. But sitting down to read a guideline can be an arduous (dare I say sometimes boring) process and in our ever-distracted world is challenging. In addition, doing so for 70+ guidelines is an unattainable goal for most.
Most importantly though, the best way to understand the content of a practice guideline is through a casebased approach whether it be an actual patient in your clinic or a clinical vignette. The principle applied here (and in life) is “context matters” – the context of how we read the guidelines matters as to how we understand and apply these guidelines.
2-year stint in the U.S. Army. He then did his Gastroenterology Fellowship at the University of North Carolina at Chapel Hill from 1966 to 1968, at which time he joined the faculty. He served as Chief of Endoscopy in the GI Division for 25 years and as Co-Chief, Division of Gastroenterology for 4 years at Chapel Hill, where he established the Motility Center.
“Dr. Bozymski’s impact on medicine, education, and patient care is immeasurable, and his absence leaves a void that cannot be easily filled. As we remember and honor his remarkable life, let us reflect on the invaluable legacy he leaves behind—a legacy of compassion, dedication, and excellence that will inspire generations to come,” remembers Dr. Shaheen, a mentee and colleague of Dr. Bozymski at UNC Chapel Hill.


The beauty of the Guide to the Guidelines book is that it puts into context the recommendations presented in ACG Practice Guidelines by using a vignette-based approach to facilitate understanding and application of these guidelines. This framework helps highlight key aspects of the guideline through real-life scenarios encountered in clinical medicine.
The information presented is easy to read and insightful, with “call-out” boxes to stress the most relevant points (including ones that “cannot be missed.”) This is not just a book that collates the recommendations of each practice guideline, rather it asks the reader to consider a case and how they would proceed, then suggests, “What do the guidelines say?” as the case is worked through.
For example, the vignette-based approach to the recently published
The ACG Institute for Clinical Research & Education sponsors the Edgar Achkar Visiting Professorship (EAVP) program to bring distinguished faculty to GI training programs for clinical education, mentorship, and networking opportunities. Within EAVP, the Visiting Scholar in Equity, Diversity & Ethical Care is an initiative of the ACG Institute’s Center for Leadership, Equity & Ethics that aims to create awareness around the issues and challenges of delivering equitable care, respecting diversity, and instilling ethical decision making.
*CHRISTOPHER D. VÉLEZ, MD: VISITING SCHOLAR IN EQUITY, DIVERSITY & ETHICAL CARE, ATRIUM HEALTH CAROLINAS MEDICAL CENTER, CHARLOTTE, NC, JANUARY 18-19, 2024
“We at Atrium Health particularly appreciated the DEI aspect of Dr. Vélez’s talk about research and clinical care. We often do not appreciate the DEI nuances in the interaction with patients or research subjects, such as culturally appropriate language to use in

GERD guidelines presents three clinical scenarios: 1) uninvestigated GERD, 2) GERD symptoms non-responsive to PPI, and 3) antireflux procedures for GERD. The vignettes allowed the practice guideline information to be easily digestible (pun intended) and provided a framework through which to understand the recommendations and apply them to an everyday patient population. Logistically, it took about 15-20 minutes to work through each case including some time to look at the figures in the actual practice guideline.
Overall, the case scenarios provide an excellent understanding of the practice guidelines – and best practice may be to utilize both the Guide to the Guidelines book with the actual practice guideline (which are downloadable for free via the ACG website at gi.org/guidelines!)
Volume 1 has just been released and includes topics labeled “Bread and Butter” in which common luminal topics are

SATISH S.C. RAO, MD, PHD, FACG: CREIGHTON UNIVERSITY – ST. JOSEPH MEDICAL CENTER, OMAHA, NE, FEBRUARY 1, 2024 (AWARDED IN 2023)
“The ACG Edgar Achkar Visiting Professorship is an outstanding and a noble service gift from ACG to both the institution that has significant gaps and unmet needs in education and training and a most rewarding and personally inspiring experience for the professor.” —Satish
S.C. Rao, MD, PhD, FACGdiscussed. The first chapter is “Gut Feelings” – neurogastroenterology and motility conditions including IBS, SIBO, and anorectal conditions amongst others; Chapter 2 is “Down the Hatch” – esophageal conditions; and Chapter 3 is “Lumps and Bumps” including luminal tumors such as colorectal cancer. The next volume will tackle GI infection, inflammation, and bleeding covering many topics such as C.difficile colitis, Helicobacter pylori, IBD, and GI bleeding. Finally, Volume 3 will be devoted to liver disease, pancreas, and biliary. And by the time that is published, it will be time to revamp Volume 1!
In summary, I recommend this book with highest recommendation. I think the best way to understand and apply the ACG clinical practice guidelines is through a case-based approach, and this offers just that – a way to structure
our understanding and application of the guidelines through cases that ring true in clinical medicine.
Place orders in the U.S. via ACG’s online store: bit.ly/GtoGvol1-purchase
For international deliveries, please order via Amazon.

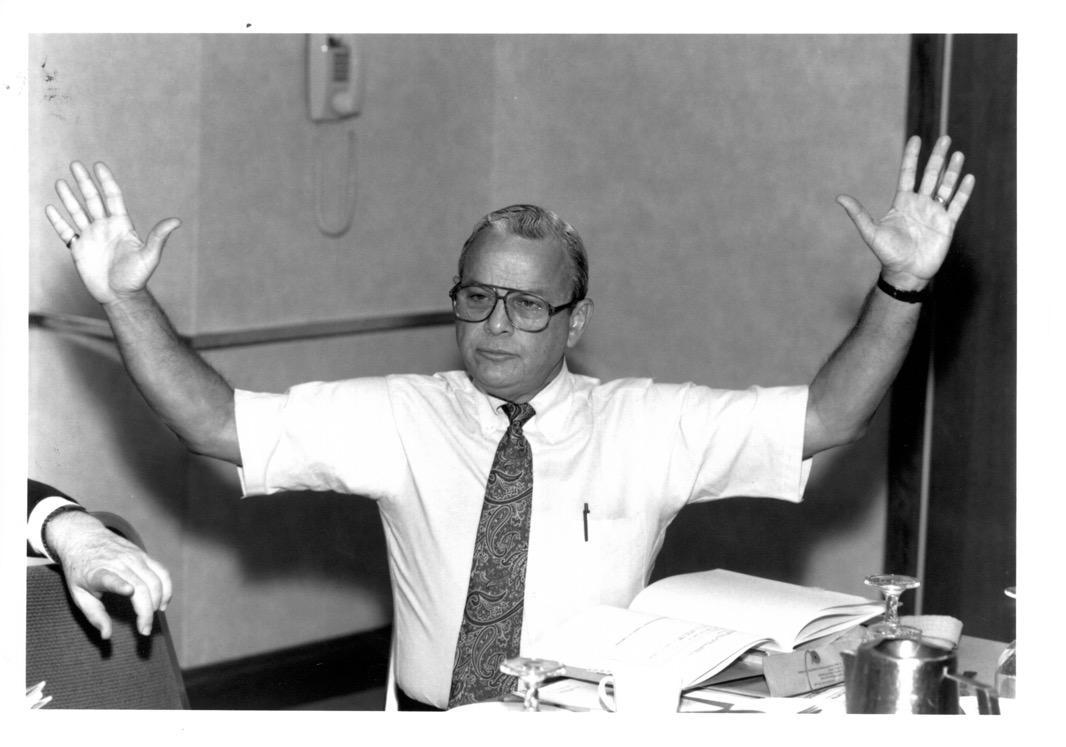
ARVEY I. ROGERS, MD, MACG (DECEMBER 8, 1934 - DECEMBER 22, 2023)
The College celebrates the life of ACG Past President Arvey I. Rogers, MD, MACG of the University of Miami who died on December 22, 2023. “He was a gentleman and a scholar, and the world was a better place for having him in it,” reflected Lawrence J. Brandt, MD, MACG, ACG Past President (1994-1995).
Dr. Rogers joined ACG in 1980 and was elected Trustee of the College in 1984. In 1987, he became an officer of the College, serving as Secretary, and was ACG President in 1992-1993. He was named a Master of the College in 1994. His ACG service includes the Awards Committee (1996 to 2005) and the Archives Committee (2004 to 2010). Over the years, he remained engaged with the College, invested in its success, and deeply connected within ACG through his many longstanding friendships.
Born in Chicago, Illinois on December 8, 1934, Dr. Rogers grew up in Beaumont, Texas. He graduated from Lamar University at 19 and medical school at UT Galveston at 23. After his internship at Philadelphia General Hospital, he moved to Miami where he did his residency in internal medicine and infectious diseases at Jackson Memorial Hospital, and his fellowship in gastroenterology at Jackson and the VA Hospital. In Miami, he met and married his first wife Susan, who was in nursing school at Jackson.
In 1962, he joined the University of Miami Medical School faculty, becoming among the first members of the Department of Gastroenterology. Dr. Rogers served as GI fellowship training Program Director from 1964 through 2001; Chief of the Division of Gastroenterology from 1994 to 2001; Section Chief of Gastroenterology at the VA Medical Center from 1964 until 1999; and Director of Postgraduate Education from 1992 through 2001.
In 2001 when his wife Susan faced a terminal illness, Dr. Rogers retired so that they could spend more time together until her death in 2008. Dr. Rogers was blessed with not just one love of his life, but two. In 2010, he married Joan Rosenberg and returned to UM as Assistant Dean of Continuing Medical Education. One of the last programs he coordinated was one of the first to train medical professionals in the importance of discussing end-of-life care with patients and their families.
A gifted educator, Dr. Rogers loved training residents and fellows in the art of becoming a physician, including what it means to truly listen. Dr. Rogers was a prolific writer who published articles, poetry, and other expressions of mindfulness and humanity in the practice of medicine. In Spring 2018, Dr. Rogers reflected on his patient care philosophy in an article in ACG MAGAZINE
that he co-authored with his son Scott, “Mindfulness and Medicine: The Healing Capacity of Genuine Listening.”
All who had the honor to know Dr. Rogers will long remember his smile, his humor, and his enormous capacity for empathy, kindness, and compassion.
Dr. Robert Kravetz Remembers His Friend Dr. Arvey Rogers
Long-time friend and fellow member of the ACG Archives Committee Robert E. Kravetz, MD, MACG remembers Dr. Rogers’ medical humanism and respect for the history of the College: “Arvey and I go back much further than anyone who knew him at the College. We interned together at the Philadelphia General Hospital from 1958 to 1959 when we were paid $2 per day and worked 24 hours on and 12 hours off. He was one of the outstanding interns in a group of 100 and we all knew that he had a bright future in academics. I kept in contact with him all of these years since we both were gastroenterologists and had a special interest in medical humanities.
We worked closely together as editors of the book celebrating the 75th anniversary of ACG in 2007 (The American College of Gastroenterology 1932-2007: Seventy-Five Years of Commitment to Clinical Gastroenterology, Gastroenterologists, and Patient Health). He knew how important it was for the younger generation of gastroenterologists to be familiar with the College’s history and pay homage to those upon whose shoulders our specialty has been built.”



Katie A. Dunleavy, MB, BCh, BAO, Mayo Clinic, Rochester, MN
WORDS CANNOT CAPTURE THE BEAUTY OF RWANDA AND ITS PEOPLE. Ernest Hemingway’s travel through East Africa described the green rolling hills, rich in flora and fauna, and my experience traveling in Rwanda felt both familiar and unknown. I do not attempt to paint imagery of my experience as magnificent as it felt, but I hope to inspire physicians to consider traveling to become globally minded gastroenterologists.
GI Rising, Inc.
Six years ago, ACG MAGAZINE highlighted the first Rwanda Endoscopy Week (REW) organized by Steve Bensen, MD; Fred Makrauer, MD; and Vincent Dusabejambo, MD (Bensen S, Makrauer F., Giving Rise to GI in Rwanda. ACG Magazine. 2018; 2(2):26-36). This exposure attracted the annual participation of other North American gastroenterologists and the creation of GI Rising, Inc., a non-profit organization dedicated to bringing sustainable gastroenterology and endoscopic care to the people of Rwanda, a small country of 14 million in sub-Saharan East Africa. (They even took their name from the ACG Magazine article title!)






ACG MAGAZINE GIVING RISE MEMBERS. MEDICINE. MEANING. to GI in RWANDA

GI Rising, Inc., is led by Dr. Bensen (Dartmouth-Geisel Medical School), Dr. Makrauer (Harvard Medical School), and board members including Don Duerksen, MD; Matt Smith, MD; Rebecca Laird, MD, MPH; Lisa Rubenberg, CRNA; and Kene Chudy-Onwugaje, MD (Dusabejambo V, Walker T, Makrauer FL. Reply. Gastroenterology. 2020 May; 158(6): 1844-1845). Their close ‘grassroots’ partnership with pioneering Rwandan physicians such as Dr. Dusabejambo and the Rwandan Ministry of Health has led to the creation of Rwanda’s first postgraduate training program.
In 2022, the first class of GI fellows was recruited to The University of Rwanda’s Fellowship in Gastroenterology and Hepatology. This program is thought to be Africa’s first sustainable GI fellowship and a model for the country’s efforts to restore physician capacity after the 1994 Genocide. In many ways, Rwanda’s partnership with GI Rising, Inc., planted the seeds for this growth and development of internal medicine subspecialty programs in Rwanda.
Any program director in North America knows the immense work it takes to develop a new fellowship and this challenge was compounded by limited resources, and lack of in-country specialists. Hanna Aberra, MD, PhD, completed her training in Ethiopia and was recruited as the first GI Fellowship Program Director. She is a phenomenal educator, advocate, and leader in a field where few women are empowered to make change. Interestingly, I found the differences in gender inequality less prevalent among Rwandan physicians, with many women holding leadership positions, and three of the first four GI fellows being women.
In collaboration with GI Rising, Inc., and the Medical College of Wisconsin, international faculty members from all over the world travel to Rwanda each month to collaborate with local faculty in the education and training of their fellows. In 2023, two university hospitals in Kigali, the capital of Rwanda, were recognized as World Endoscopy Organization Centers of Training, a distinction acknowledging the excellent quality of endoscopic
education. The heart of this fellowship program remains its self-sustainability with strong local buy-in and Rwandan-directed development. With the advent of hybrid digital education, mentorship and training continues long after faculty leave Rwanda, allowing for an enduring connection.
Rwanda is a country rebuilt with strength and resilience following the 1994 Genocide when a 100-day period of widespread ethnic cleansing accounted for the death or displacement of 1 million people. This genocide was deeply personal, rooted in ethnic hatred and propaganda arising from over a century of European colonization. Neighbors killed neighbors, families were displaced, and the survivors were faced with the enormous responsibility of forgiveness. In the face of this destruction, the Rwandan economy and health care system was decimated, with the loss of 90% of physicians and health care workers who sustained the country’s poor health care system. Now a new generation of physicians are being trained in Rwanda, and as the best and brightest from their communities, they represent a new era of hope, as many are first-generation physicians guided by the intention of giving back to their communities.
Over the last 30 years, Rwanda has made inspiring strides to reimagine health care. From 2012 to 2019, the Rwandan government led the Human Resources for Health Program (HRH Program), a bold initiative to allow international physicians to help fill the shortage of health professionals. During this time of rebuilding, Rwanda made the intentional decision to provide universal health insurance to all citizens. With this innovation, strides have been made across the health care sectors, with community health partnerships decreasing the access time for rural villagers, with impressive increases in life expectancy and deaths in children under age 5. Universal health care grew from a pilot project of health insurance funded by the Ministry of Health, called Mutuelle de Sante, providing free care to the poorest 25% of Rwandans. To this end, less than 10% of all Rwandans are uninsured today.
There are four national referral hospitals in Rwanda: Kigali University Teaching Hospital (CHUK), King Faisal Hospital Kigali, Rwanda Military Hospital, and Butare University
Teaching Hospital. Currently, the GI fellows spend time providing care and performing endoscopy at CHUK and King Faisal Hospital. The notable limitation is that access to GI care outside of Kigali is limited. During my time in Rwanda, I met patients who traveled by foot, motorcycles, and buses to reach a doctor’s appointment. Four GI fellows are prepared to graduate in 2024 and have committed to remaining in Rwanda to become faculty and provide patient care. Over the next 5-10 years endoscopic care will continue to expand from the main teaching hospitals in Kigali to district hospitals to improve access.
Rwanda Endoscopy Week (REW)
In 2016, the Rwanda Society for Endoscopy was formed with a group of North American faculty and local Rwandan internists. In 2017, the first REW was held, and the following year GI Rising, Inc., was created. Today, REW has become a yearly collaboration between GI Rising, Inc., the Rwanda Society for Endoscopy, and the University of Rwanda to increase access and knowledge of GI diseases. During REW gastroenterologists, GI fellows, CRNAs, anesthesiologists, endoscopy technicians, nurses, and biomedical engineers travel from around the world to Rwanda to provide high-level patient care while teaching Rwandan physicians. Through fundraising, grant applications and donations, GI Rising, Inc., has been able to outfit the various sites with endoscopic equipment and consumable devices allowing for development and delivery of endoscopy services in urban centers and remote district hospitals.
In 2017, they performed 250 procedures at four sites, and by 2023 expanded to 1,069 procedures at ten sites. As the number of procedures has increased so has access to anesthesiasupported sedation. Lisa Rubenberg, CRNA, has led initiatives to create a sustainable education for Rwandan nurse anesthetists. Similarly, Conrad Worrell, RN, and President of the American Board of Certification for Gastroenterology Nurses has been dedicated to helping nurses obtain the
skills they need to assist in procedures and care for endoscopic equipment. The cultural implications of sedation for a medical procedure are far-reaching and as GI Rising, Inc., works to increase access to endoscopy, they believe ongoing collaborations with Rwandan health care professionals are essential.
In October 2023, I traveled to Rwanda for a month-long clinical elective planned to coincide with Rwanda Endoscopy Week (REW). Every day in Rwanda was a new adventure filled with opportunities for direct patient care, teaching, and connection. The first week of REW was a conference led by Rwandan physicians to provide case-based teaching to the forty-two internal medicine residents and five GI fellows. During the second week, I traveled to Butaro District Hospital with Conrad Worrell, RN, (Brigham & Women’s Hospital) and Don Duerksen, MD, (University of Manitoba). As we traveled on the unpaved roads from Kigali to Butaro, I felt nervous, alone with my thoughts and uncertain of what we would encounter, though somehow freer having left the chaotic city of Kigali. We arrived as the sun set with rain teeming from the skies, but the significance of our arrival was palpable. In the next week we would perform the first endoscopic procedures at this site.
Butaro District Hospital is a unique 240-bed hospital and cancer center developed in collaboration with Dr. Paul Farmer, Partners in Health, and the Rwandan Ministry of Health. Patients from East African countries travel to seek specialized cancer care. This is a special place deep in the rural green hills of Rwanda; a peaceful land of healing and caring for the whole person. After only a few minutes on campus, it was easy to see how Dr. Paul Farmer had chosen this location and spent his final hours here before his passing in 2022. Currently, patients with suspected GI malignancy are referred to Kigali for diagnostic endoscopy, increasing patient burden of travel, finances, and timeto-diagnosis, which limits treatment options. Over five days, about 200 patients were self-referred for evaluation

and we performed 81 unsedated EGDs with indications ranging from epigastric pain to weight loss. While most patients had nonulcer dyspepsia with a normal endoscopic assessment, five patients had masses concerning for malignancy.
This pilot project demonstrated a significant demand for GI endoscopy in rural Rwanda, which could only be achieved with the support from Butaro Hospital physicians, staff, and administrators. We stayed on campus at the enchanting University of Global Health Equity (UGHE) located within walking distance of the hospital. UGHE has created an innovative medical university focused on delivering high-quality health care by addressing social and systemic inequities in health care delivery. Watching the sun rise as the mist lifted over a nearby volcano is a memory I will cherish forever.
Solange Mukanumviye (’24), Shikama Felicien (’24), Dynah Nyampinga (’24), Zainab Ingabire (’24), Cedric Kwitonda (’25)
During my time in Rwanda, I cultivated a love for teaching students and trainees, and as a first-time endoscopy instructor, I mirrored techniques used by my valued mentors. During my last two weeks in Rwanda, I spent as much time as I could getting to know the GI fellows who sacrificed to pursue this sub-specialty training. A generous donation from a gastroenterology consultant at Mayo
Clinic helped provide the fellows with new iPads, which will be essential to providing access to online textbooks, GI fellowship curriculum, and board review. Most importantly, these iPads will provide a direct link to continue our friendship and mentorship from afar.
I witnessed the direct impact of medical education as lessons taught were applied to patient care in the moment. Patients were correctly diagnosed or medically managed because of teaching and mentorship. When I spent an afternoon in GI clinic with a fellow, one patient stood out to me because it was so clear how a lack of locally available GI training had directly impacted her care. Although a young woman, after the pregnancy of her last child she started noticing bleeding per rectum. She was treated with cycles of antibiotics for over nine months before being referred to the teaching hospital in Kigali. She traveled to the capital with her husband and a backpack, unclear of when or if she would return home. A simple digital rectal examination had never been performed, though within minutes of her physical examination a rectal tumor was found. Days later, following urgent colonoscopy with biopsy she was diagnosed with a new unresectable rectal cancer. One of the GI fellows hopes to use this experience to teach community health workers the value of physical exam to help expedite patient care.
Amidst much uncertainty, and my limited understanding of the national language, Kinyarwanda, I quickly
learned that the Rwandan GI fellows are exceptional. As individuals they are compassionate, curious, and intelligent, but as a collective they are the future leaders and a symbol of hope for their country. There were times during my stay I felt powerless because the medicine I knew could help treat the diseases of poverty and social exclusion were out of reach. In these moments, I looked across the exam room and saw faith in the fellows’ eyes. I’m confident that their optimism, drive, and unique understanding that health is impacted by social circumstance will empower change in Rwanda.
Already, Rwandan physicians are providing trauma-informed care as they work to understand the impact of collective trauma on health disorders. I will never forget the moment I realized that chronic epigastric pain in Rwanda may be a symptom of distress relating to the aftermath of the genocide. When seeing a patient in Butaro Hospital with a wonderful Rwandan physician, Ruth Mukeshimana, MD, the patient described how her abdominal pain started when she was little girl hiding in the forest. The physician explained to me that this is how many people refer to their time trying to escape during the genocide. Following this patient’s normal endoscopy, we spent time discussing and drawing the gut-brain interaction. While the stressors of life may be different in Rwanda, I learned not to overlook the connection between social circumstances and physical symptoms.
Reflection
It is difficult for me to describe how this adventure began, but I am hopeful that it is not yet at its end. Ernesto ‘Che’ Guevara may have expressed this best in The Motorcycle Diaries when he said, “The first commandment for every good explorer is that an expedition has two points: the point of departure and the point of arrival. If your intention is to make the second theoretical point coincide with the actual point of arrival, don’t think about the means – because the journey is a virtual space that finishes when it finishes, and there are as many means as there are different ways of ‘finishing.’ That is to say, the means are endless.”
I am appreciative for the travel grant from the Mayo International Health
Program that made this trip possible. When I see the sacrifices the Rwandan GI fellows have made to become leaders of GI in their country, I feel so proud to be a small part of their journey. I now recognize that no matter where my path leads me in academic medicine, I must always have a space in my heart for global health work. Dr. Paul Farmer was right when he said, “with rare exceptions, all of your most important achievements on this planet will come from working with others—or, in a word, partnership.”
Returning home to finish my final year of GI fellowship at Mayo Clinic has made me count my blessings. I was honored to be offered a position on the Board of Directors for GI Rising, Inc., and hope that this is the beginning of a long-enduring relationship. In the future, I hope the Rwandan GI fellows can be afforded the opportunity to visit international institutions just as I was afforded the opportunity to learn from them. I enthusiastically encourage all GI fellows to participate in a global health experience (Luft S, Makrauer F. How (and Why) to Get Involved with Global Health as a GI Fellow. Dig Dis Sci 2022 Aug;67(8):3485-3486. doi: 10.1007/s10620-022-07577-7). A huge thank you to the incredible people I met during REW who traveled across the world to take part in this enriching experience! I learned to triage patients with unfamiliar and advanced pathology in a resource-limited setting as I navigated language and cultural barriers. There is no doubt that I returned to the States a better person, physician, endoscopist, and educator.
1. Connect with GI Rising, Inc., at our website: gi-rising.org or email us for more information.
• Dr. Katie Dunleavy: Dunleavy.katie@mayo.edu
• Dr. Steve Bensen: Steve.P.Bensen@hitchcock.org
• Dr. Frederick Makrauer: fmakrauer@bwh.harvard.edu
2. Donate at gi-rising.org/about-5 All funds support fellowship education, maintenance of endoscopic equipment, medical non-physician professionals and scholarship support for Rwandan physicians to travel to conferences.
3. Educate and mentor GI fellows and internal medicine residents.
4. Volunteer to travel to Rwanda as faculty for the GI Fellowship program or during Rwanda Endoscopy Week. We would love to see more GI faculty, fellows, residents, students, and non-physician medical professionals join us! It is vital to have partnership with nursing, endoscopy technicians, IT support, BioMed, anesthesia, surgeons, etc.
5. Partner with GI Rising, Inc., to enlist support from private and industry donors.















(1) Katie Dunleavy, Donald Duerksen, Ruth Mukeshimana (Rwandan resident), Conrad Worrell, and Jean Leonard Mugisha (Rwandan nurse) perform the first EGD at Butaro Hospital in November 2023.
(2) L-R: Conrad Worrell, Alex Zhornitskiy, Joseph Romine, Beth Pflanz, Kristin Sprenger, Lisa Rubenberg, Arlina Aviles, Michelle Kennett.
(3) Katie Dunleavy and Steve Bensen celebrating a successful 6th Annual Rwanda Endoscopy Week! Steve Bensen, Kuldeep Tagore, Erik von Rosenvinge.
(4) Patient physical examination prior to endoscopy shows significant nutritional decline and wasting due to lack of medical access. Patient permission obtained.
(5) Erik von Rosenvinge, Rukaiya BashirHamidu, Vincent Dusabejambo (Rwandan gastroenterologist), and Kuldeep Tagore at Charite Digestive Clinic in Kigali, Rwanda.
(6) The beautiful and transformative University of Global Health Equity Butaro Campus.
(8) Second-year GI fellow Shikama Felicien performing endoscopy with nursing team at CHUK hospital.
(10) The new endoscopy unit supported by The Ministry of Health and hospital administration at The University Teaching Hospital of Kigali.
(13) Collaboration of medical students, GI fellows and gastroenterologists at the 6th Rwanda Endoscopy Week. L-R: Peter Bensen, Shikama Felicien, Matt Bryan, Rukaiya Bashir-Hamidu, Ivy Riano Monsalve, Hanna Blaney, Katie Dunleavy, Steve Bensen, Kuldeep Tagore, Erik von Rosenvinge.













Each chapter of the Guide to the Guidelines series includes carefully selected vignettes designed to illustrate key concepts from the guidelines, followed by a conversation-style discussion written to keep you awake and alert. The authors highlight noteworthy points and provide multiple-choice questions to test your knowledge of the material. Using their combined experience of managing GI and liver patients in both academic and private practice settings, they can help you provide high quality care to your patients. Brennan



MARCIA CROSS IS A WORLD CLASS SHAME BUSTER AND A STIGMA BASHER. She took her experience with a diagnosis of HPV-related anal cancer and used it to fuel her advocacy and leadership to educate and empower others. I could not be more impressed with her role in co-founding the HPV Cancers Alliance or grateful that she agreed to deliver the Emily Couric Memorial Lecture at the Annual Scientific Meeting in October 2023 during my presidency.
Ms. Cross spoke straight from the heart, courageously sharing the personal details of her diagnosis and treatment for anal cancer. In her address, Ms. Cross was honest, vulnerable, and incredibly straightforward in speaking about anorectal symptoms and her respect and admiration for the anus. She was charming in making jokes and proudly declaring her love for the anus but, in all seriousness, her unique brand of plainspokenness is absolutely necessary to counter the stigma and shame that these diagnoses induce for many people. But not for Marcia Cross.
Ms. Cross took her surprising and devastating diagnosis and found her voice as a patient advocate and nonprofit leader. She used her celebrity, her elegance, her Juilliard training as an actress, and her public persona, and she decided to speak the truth to help others.
As a truth-telling champion of health, who “names names” when it comes to the anus and anal cancer, Ms. Cross strikes me as being a force for good in the world. She eschews embarrassment and proudly called on her audience at ACG 2023 to, “Love your anus. It’s the key to your health, freedom, and dignity.”
Being a public figure who talks openly about the anus and anal cancer is neither an easy nor a comfortable role. Many celebrities support excellent causes, but few speak as honestly and fearlessly as Marcia Cross. Seeing her in action delivering the Couric Memorial Lecture was a profound and inspiring experience. Her vision and generosity
in delivering this high-profile lecture at the ACG Annual Scientific Meeting will now reach an even larger audience through the pages of ACG MAGAZINE.
Thanks to her efforts, dedication, and partnership with Lillian Kreppel, the HPV Cancers Alliance is making a difference in the care of patients facing diagnoses and educating policymakers, health care providers, and the public about the facts of HPV and the risk of cancer. My deepest gratitude goes to Ms. Cross for delivering the Couric Memorial Lecture and for fighting shame and stigma as a vocal champion for the health of the anus and the prevention of HPV-related cancers.
“I want to thank the American College of Gastroenterology for having me here to speak to you today. I am incredibly grateful for this opportunity and want you to know that I am deeply in awe of what you all do. I've been asked to tell you about how I came to be an advocate about HPV and the cancers it can cause, and to offer some thoughts on how we can improve early detection of those cancers.
I'll start with my story. Six years ago, during my very busy life with work and young kids, I needed a prescription from my gynecologist. I had been seeing her for many years, but the office said they would not give it to me and that I needed to come in for an appointment.
I was thinking, I was just there! But time is elusive in my mind, and she was correct. I was six months overdue for my annual checkup.
Dr. Nancy Goldman, who I had great respect for and liked personally, was chatting pleasantly as she always did during my examination. She was masterful at making me feel calm as she went from getting a Pap smear to then performing a digital rectal exam. I had been through this many times before and didn't think anything of it. When she left the room, I got dressed and was ready to get back to my busy day. But after a quick knock on the door, she came in and said she wanted me to see another doctor down the street, that she'd already called, and I should go there now. Honestly, I was somewhat annoyed, because that meant I was going to miss my daughter's basketball game. I was clueless. Nothing was on my radar. I don’t even remember wondering why I was going there.

After that doctor examined me, she said, well, whatever it is, it's curable. An immediate colonoscopy was scheduled and then I drove off to the basketball game in a state of complete shock that wouldn’t lift for many months.
And so began my journey with anal cancer. The treatment is quite gnarly, but it is an endurable one. And yes, it was, at least so far, knock on wood, curable. But only because it was caught early by Dr. Goldman who performed that digital rectal exam. By the way, I did not come in with any symptoms nor had I ever tested positive for HPV. I am so lucky that she was close to retirement age and had been trained at a time when doing a DRE was the norm and her professionalism and rigor had never waned.
Cut to a year later, post-treatment. I had no intention of going public with my story, but what I found in my continual deep dive on the internet during my ordeal was this pervasive ignorance and deep shame pertaining to all things HPV. So, despite my being largely an introvert (yes, I'm sort of an extroverted introvert), I could not stay silent when people were dying needlessly because of this virus and the stigma and shame surrounding it.
Since that time, anal cancer thriver Lillian Kreppel and I formed the HPV Cancers Alliance. For the last five years, it has been our mission to educate the public about HPV and the cancers it can cause. Though we have had great success in some areas, we find ourselves facing huge roadblocks in others. The first is that there is a serious lack of education about HPV for populations that came before the vaccine. Patients in their forties, fifties, and above. And in terms of anal cancer specifically, most cases occur in post-menopausal women like myself who are told not to even bother seeing their gynecologists anymore.
According to the CDC, in the U.S., there are currently 80 million people infected with HPV and HPV is the cause of over 37,000 new cases of cancer each year. Anal cancer, in particular in postmenopausal women, continues to be on the rise. Oral pharyngeal cancers are on the rise as well and are the most common HPV cancer among men. From 2019 to 2022, 31,284 deaths of women were attributed to HPV-associated cancers.

“There are currently 80 million people infected with HPV and HPV is the cause of over 37,000 new cases of cancer each year. Anal cancer, in particular in postmenopausal women, continues to be on the rise. Oral pharyngeal cancers are on the rise as well and are the most common HPV cancer among men... There is so much shame associated with having the virus that many people fighting for their lives are suffering silently!”
There is so much shame associated with having the virus that many people fighting for their lives are suffering silently! One woman confessed that she had a hysterectomy because of HPV and went through it alone because she was ashamed to tell her family. I was shocked and deeply upset. Others lied about what cancer they had and hid it from other family members. Having a virus is nothing to be ashamed of it. It makes battling it that much more fraught. I heard firsthand from anal cancer patients that they lied to friends and family about what cancer they had due to their deep feelings of shame about it being in their anus. I did not, nor do not judge, as we are still in a time where our seemingly last bodily taboo is the anus.
Years ago, Katie Couric put the colon on the map when she went public with her husband’s cancer battle. Now, no one thinks twice talking about the colon. Decades before that, in 1972, Betty Ford went public with her breast cancer and began dismantling that taboo; shocking to think that breasts were a taboo to talk about. But times were different. What seems to be the last bodily taboo is the anus. And to hammer home our need to neutralize that word, I will be saying it a lot today, to you, the fellow leaders of this cause. One question that Lillian and I found ourselves asking again and again about the anus is:
We naively thought that once we got to ACOG (the American College of Obstetricians and Gynecologists), we could persuade them to make digital rectal exams part of regular checkups. After all, this three-minute exam saved my life. Nope, not their department

they told us. And no, they were not interested in implementing or even discussing our suggestion, even for certain at-risk patients. We were, and continue to be, shocked.
Okay, we thought, so It's not their department. Is it the gastroenterologists’ domain? When I went public with my cancer story, I did an interview with physician Dr. Jon LaPook. He said to me that many times when a colonoscopy is performed, the scope goes through the rectum and anus and doesn't include them in the exam. They're missed. Deeply confused, I looked up the gastroenterologist’s scope of practice and read, “a gastroenterologist is a specialist with expertise in the disorders and diseases that affect the digestive system. Which includes the gastrointestinal tract, esophagus, stomach, small intestine, large intestines, rectum, and anus as well as the pancreas, liver, bile ducts, and gallbladder.” Why did he tell me to make sure to tell the doctor to turn the camera around? So, I looked up what the colonoscopy was supposed to examine, and I found that during routine colonoscopy screenings for colon cancer doctors are looking for abnormalities or diseases in the colon, and don't usually examine the anus. I was stunned. What?! So where does that leave us? Or rather, the neglected anus? My hope today is that you will take on this fight for the anus and give it the attention it deserves.
Next little section is about, when is a hemorrhoid not a hemorrhoid? I have, since my diagnosis, had too many conversations with people who were not as lucky as I was. Their cancer was not diagnosed in time for it to be curable. Usually, the reason is this:
“Speaking about the embarrassment around this issue, it's time that we really end the stigma of the anus because I have fallen in love with mine.”
— Marcia Cross
The patient has bleeding, itching, or discomfort, or feels something is not quite right. They wait a bit to see if it's going to go away.
Finally, they call a doctor for an appointment. That can take weeks or even months, depending on many factors: work schedules, insurance, fighting through the embarrassment, and then, finally, a patient speaks to or sees a doctor. The doctor says, almost without exception, that it is a hemorrhoid. The patient is relieved, lives with the symptoms, and hopes that the doctor is right. More time passes, and it's not going away, and now the patient has to call again. Hope to get an appointment, take more time off from work, pay another bill, again. Wrestle with shame, and, again, this takes time. And, finally, the patient sees the doctor and, hopefully, if it is cancer, it's found. But by then their once curable cancer has now spread and they're fighting for their lives. By the way, we often hear from our patient community that a digital rectal exam or other exam was not performed at the initial visit.
So, here's a possibility to the solution. The doctor says, “I think it sounds like a hemorrhoid,” or looks at it. “If the symptoms do not change in X number of days, call and tell my staff that I asked to see you right away.” Or even better, why don't you make an appointment for the patient for two weeks out, and if the patient's symptoms go away, the patient can just cancel the appointment. But if it has not, they already have an appointment scheduled. That might go a long way toward helping patients get a more timely diagnosis. Because this hemorrhoid thing, I'm sure most of the time it is a hemorrhoid, thank God, but it's the thing that we hear about the most in terms of why something took so long to get diagnosed.
Let's talk about the digital rectal exam. Because of the stigma around the anus, many doctors are reticent to do these exams and, of course, patients are embarrassed about having them. Upon talking to a brilliant, insightful gastroenterologist, one thing he does is he lets the patients know exactly what's happening. For example, explaining the automatic muscle reactions by the sphincter during the exam. So that all those sort of feelings and things that
happen while it's going on, he kind of normalizes it so that it takes off the embarrassment and makes it normal.
I remember something he said to me, “and make sure you wipe off the jelly.” That's what he said that someone taught him, and that it was an important part.
I know this all sounds maybe simple, and maybe you all do it, but for some reason—and again, it comes back to that body part of ours, the anus—these things don't happen. They don't happen. They don't happen with gynecologists. They don't happen in other doctors’ offices.
Speaking about the embarrassment around this issue, it's time that we really end the stigma of the anus because I have fallen in love with mine. In fact, I now know that the anus, or as it is commonly referred to, the asshole, is one of the most beautiful of God's creations. Without the brilliance of its opening and closing and the glorious undulating of the anus, we would all be up shit’s creek without a paddle.
Love your anus. It is the key to your health, freedom, and dignity. I love and deeply appreciate mine. I'm making jokes here, but it's actually true. I mean, you can lose a finger, a hand, maybe a breast. But I don't think anybody here really wants to lose the ability to go to the bathroom when they need to travel the world, be not dependent on something else.
I really do believe that it's time to end that stigma and I'm going to try to enlist you all in this process. So, I know that hopefully after this talk all about the anus and the rectum and the colon, that you're all going to go off to hopefully a fabulous dinner. But I challenge you, somewhere in the next few days, to use the word anus in a sentence. Maybe you can even talk about how wonderful they are. I certainly wouldn't want to be without mine. And I am hoping that in the future you will join the fight to recognize HPV-related cancers and be advocates for diagnosing them in the most timely manner possible.
I'm so grateful to be here because I know that you guys are on the front lines, and that you deal with all of this,
and so many more issues every day. And I meant what I said, that I am in awe of you and I had a wonderful gastro—and it's the hardest word to say. And my husband had the nerve to say to me, “There's not an N in there.” And I said, “Yes, there is, darling.” But, it's such an intimate and personal and important specialty, and I hope that this conversation will help you to pay more attention to possible signs of anal cancer.”
Delivered each year at the ACG Annual Scientific Meeting, the Couric Memorial Lecture honors the life and work of Emily Couric, who died of pancreas cancer at age 54 in 2001 while serving as a State Senator in the Commonwealth of Virginia. The lecture was established by ACG in 2006 and endowed by the Virginia Gastroenterological Society and the Old Dominion Society of Gastroenterology Nurses and Associates in honor of Senator Couric, sister of journalist and media executive Katie Couric. Senator Couric was a strong advocate for health care issues, particularly in her instrumental work to pass the nation’s first legislation


During the summer of 2017, HPV Cancers Alliance
Co-Founder Lillian Kreppel began having concerning bowel symptoms—intense itching and bleeding while going to the bathroom. After seeing her gastroenterologist for a digital rectal exam and sigmoidoscopy, she received the difficult news: she had a cancerous tumor, specifically, stage II anal cancer. She completed chemoradiation therapy to treat the cancer, and her prognosis was good.
This experience spawned a new mission—to talk about anal cancer and HPV, which she had been diagnosed with years before, especially since symptoms of itching mean that so often people mistake anal cancer for hemorrhoids. Never afraid to tell it like it is, Lillian became an advocate to raise awareness of anal cancer and other HPV-associated cancers, as they are rarely discussed due to social stigmas. Her iron-clad determination and energy fueled her to bring this advocacy to a larger scale.
Lillian, Marcia Cross, and businessman Dan Lifton formed the HPV Cancers Alliance in 2019. The Alliance is dedicated to educating the public about HPV-related cancers, engaging with physicians to increase HPV-associated cancer screening and HPV prevention, and advocating for legislation to support HPV vaccination nationally. The Alliance also empowers patients to be their own best advocates, encouraging them to step up and ask for what they need.
Lillian recently reached her 5-year cancer-free mark and now considers herself an “anal cancer thriver.”
Website: hpvca.org
Twitter/X: @HPVAlliance
LinkedIn:
linkedin.com/company/hpv-alliance
Facebook: facebook.com/HPVCancersAlliance

ACG Weekly Virtual Grand Rounds
ACG Weekly Virtual Grand Rounds
2024
2024
2024 ACG’s IBD School & Eastern Regional Postgraduate Course
2024 ACG’s IBD School & Eastern Regional Postgraduate Course
June 7–9, 2024
June 7–9, 2024
The Capital Hilton, Washington, DC
The Capital Hilton, Washington, DC
2024 ACG’s Hepatology School & Midwest Regional Postgraduate Course
REGISTER NOW: GI.ORG/ACGVGR
REGISTER NOW: GI.ORG/ACGVGR
ACG VGRs are offered TWICE each Thursday, with a live broadcast at noon (ET) followed by an 8:00pm (ET) rebroadcast!
ACG VGRs are offered TWICE each Thursday, with a live broadcast at noon (ET) followed by an 8:00pm (ET) rebroadcast!
2024 ACG’s Hepatology School & Midwest Regional Postgraduate Course
August 23–25, 2024
August 23–25, 2024
Radisson Blu Mall of America, Minneapolis, MN
Radisson Blu Mall of America, Minneapolis, MN
2024 ACG’s Functional GI & Motility Disorders School & ACG/VGS/ODSGNA Regional Postgraduate Course

2024 ACG’s Functional GI & Motility Disorders School & ACG/VGS/ODSGNA Regional Postgraduate Course
September 6–8, 2024
September 6–8, 2024
Williamsburg Lodge, Williamsburg, VA
Williamsburg Lodge, Williamsburg, VA
ACG 2024 Annual Scientific Meeting and Postgraduate Course
October 25–30, 2024
ACG 2024 Annual Scientific Meeting and Postgraduate Course
October 25–30, 2024
Pennsylvania Convention Center, Philadelphia, PA
Pennsylvania Convention Center, Philadelphia, PA
2024 ACG’s Functional GI and Motility Disorders School & Southern Regional Course
December 6-8, 2024
2024 ACG’s Functional GI and Motility Disorders School & Southern Regional Course
Renaissance Nashville, Nashville, TN
December 6-8, 2024
Renaissance Nashville, Nashville, TN


YIKES, IT’S SPRING ALREADY???
If you’re slacking just like us and wondering if it’s too late to start making those small healthy changes, don’t miss a beat because the #ACGfoodies have your back!!!
Check out reflections from #ACGfoodies Dr. John Damianos, Dr. Asmeen Bhatt, and clinical dietitian Kelly Issokson – who proclaims she is “a foodie first and a registered dietitian second.” They share their culinary journeys along with recipes close to their hearts, sure to fill our guts with goodness.
— Alex, Christina, and Vani
 JOHN A. DAMIANOS, MD
JOHN A. DAMIANOS, MD
G
I Fellow, Mayo Clinic, Rochester, MNRaised in a Greek household, I grew up on a Mediterranean diet. Early on, my parents instilled in me that no meal is complete without a salad, and my nightly chore was to make the family salad. I discovered young that cooking brought me joy, and much of that joy came from experiencing others savor something I had crafted for them.
I am also the son of a gastroenterologist, so the notion was engendered in me that food is fuel, and what and how we eat directly impacts our gastrointestinal and, thereby, systemic health. It was only natural then that in medical school I would be so drawn to our lectures on the gut microbiota. Following one of our first lectures on the topic, I bounded to the podium, pointed to the slide projected on the screen, and declared, “I want to do that.”
Ingredients:
Salad
• 3 large leaves of kale, chopped
• 1/2 medium-sized red onion, finely chopped
• 1 large garden cucumber, finely chopped
• 1 large heirloom tomato, diced
• 1 large bell pepper (color of your choosing!), finely chopped
• 1 handful of sliced Kalamata olives
• 2 handfuls of walnuts
• 3 Tbsp ground flaxseed
• 1 tablespoon of Nigella sativa seeds
• Optional: 7 oz. imported Greek feta cheese
My research in residency concerned diet in inflammatory bowel disease. In fellowship, I particularly enjoy untangling the multiple contributors—diet included—to a patient’s gastrointestinal symptoms and collaborating on how to restore health. From a research standpoint, I am immersing myself in the complex and controversial world of microbiome therapeutics. And in my spare time, I am cooking—always devising new concoctions with my favorite organ, the microbiome, in mind.
Over the years, I tinkered with my childhood salad recipe to get to what is now a near nightly staple for me. Friends have deemed it my “super salad,” and often request it for parties and get-togethers. In addition to bursting with flavor, I love how it is rich in so many vegetables and herbs, and includes fiber, polyphenols, omega-3 fatty acids, good bacteria, and numerous other nutrients
to support a diverse and healthy microbiome. It pairs particularly well with homemade hummus (my wife’s is unsurpassed!) and multigrain bread. Don’t forget to sop up the leftover dressing at the end with some bread, the Greek tradition of papara.

Dipl. of ABOM, University of Texas Health Science Center at Houston
Food is as integral a part of my identity as is my age, gender, ethnicity, and profession. It is what uniquely distinguishes me as an individual. My food choices have evolved and grown with time and experiences. As a child growing up in the cosmopolitan city of Bombay (now Mumbai), India, I was blessed to be surrounded by fantastic
Dressing (makes 1 liter)
• ¼ liter of fermented balsamic vinegar
• ½ liter of Greek extra virgin olive oil
• ¼ cup ground black pepper
• 1/3 cup dried Greek oregano
• 1/3 cup of dried rosemary
• 1 Tbsp dried basil
• 1 Tbsp sumac
• 1 tsp of dried thyme
• 1 tsp turmeric powder
• 1 large garlic clove, crushed
(To make the dressing, add all ingredients to a 1-liter container and shake well.)
Steps:
1. Add all vegetables (kale, onion, cucumber, tomato, bell pepper, and olives) to a large salad bowl
2. Mix in walnuts, flaxseed, and Nigella sativa seeds
3. Crumble feta (omit for vegan option)
4. Shake the salad dressing well and drizzle as much as desired
5. Toss the salad
6. Enjoy!





harmony of spices and fresh ingredients yet were identifiably “Indian.”
My family hails from the state of Assam in Northeast India which is famous for its tea plantations and cultural influences from Southeast Asian countries. The matriarchs in my family introduced me to my roots and taught me the makings of Assamese food. However, in Mumbai, I had a constant exposure to Marathi, Gujarati, Udupi, Punjabi, Parsi, Gomantak, Malayali, Bengali, Mughlai, and countless other cooking styles, which ultimately shaped what I call my “Indian” food.
I moved to the United States nearly 25 years ago, which opened a whole new world of gastronomy for me. The U.S. is truly a melting pot of cultures and food sits in the heart of it all. Wandering through farmers’ markets and hole-in-thewall restaurants throughout this country, I took to international cuisines as a fish does
to water. Living in Houston – which is truly a gold mine for foodies –makes relishing different cuisines an actuality for me.
Travels around the world have also shaped my culinary journey. I seek out authentic restaurants and food experiences in different cities and often will rate my travel based on the foods that I have eaten in every location.
It is vital to understand that the food we consume often defines our health. One’s dietary decisions should be based on food allergies and must include foods that boost our immune system and those that are required for bodily functions.
As a gastroenterologist and obesity medicine specialist, I educate patients on the importance of their dietary choices and portion
control. A healthy body and mind are the best medicine a physician can prescribe. I encourage people to cook meals at home with fresh ingredients, use healthy cooking techniques, and meal plan to avoid uncertainty around their meals during a busy work week. I advise moderation in eating calorie dense foods and focus on eating nutrient rich foods that appeal to an individual’s taste buds, cultural background, and health needs.
I present to you a vibrant, colorful, and nutritious crockpot recipe, “Slow-Cooked Vegetable Curry,” that is perfect for spring. As a busy professional and a mom, cooking large batches of scrumptious nutritious meals saves time and keeps my family happily fed. I hope I have inspired you as a reader to begin or expand your own culinary journey—go forth and conquer it!
Ingredients:
• 2 Tbsp vegetable oil (canola, sunflower, peanut etc.)
• 2 medium onions, finely chopped
• 4 garlic cloves, minced
• 1-inch piece of ginger, minced
• 2 tsp cumin seeds
• 2 tsp cilantro powder
• 1/8 tsp turmeric
• 1 tsp red chili powder (or cayenne pepper or paprika)
• 3 tsp curry powder
• 3 Tbsp canned crushed tomatoes
Steps:
1. In a large skillet, heat oil over medium heat
2. Add cumin seeds, allow them to sputter, about 1 minute
3. Sauté onions until soft and lightly browned, 5-7 minutes
4. Add garlic and ginger and cook for another minute
5. Add the ground spices and stir for 1 minute
6. Stir in crushed tomato; cook for 1 minute
7. Transfer to a 5- or 6-quart crockpot or slow cooker
8. Mash 1 can of garbanzo beans until smooth; add to slow cooker
9. Add vegetable broth, coconut milk, salt, and pepper
10. Add potatoes and cook, covered on high heat, for 1 hour
11. Add cauliflower, carrots, and the second can of garbanzo beans
12. Cook, covered, for another hour on high heat and then add the peas
• 2 cans (15 oz.) garbanzo beans/chickpeas, rinsed and drained
• 1 1/2 cups peeled potatoes cubed into 1/2 inch pieces (about 1/2 pound)
• 2 cups fresh cauliflower florets (~8 oz.)
• 1 cup carrots cut into 1/4-inch pieces (2 medium carrots)
• 1 1/2 cups frozen green peas
• 2 cups vegetable broth
• 1 cup coconut milk
• 1 tsp salt, to taste
• 1/2 tsp pepper
• 2 Tbsp minced fresh cilantro to garnish
• 1 lime, cut into wedges
13. Cook, covered, on low heat until vegetables are tender, another 2 to 2 1/2 hours
14. Sprinkle cilantro to garnish
15. Serve with cooked brown or white rice along with lime wedges and plain yogurt, if desired








 KELLY ISSOKSON, MS, RD, CNSC, Clinical Dietitian, CedarsSinai Medical Center, Los Angeles, CA
KELLY ISSOKSON, MS, RD, CNSC, Clinical Dietitian, CedarsSinai Medical Center, Los Angeles, CA
I consider myself a foodie first and a registered dietitian second. This is why I felt it crucial to have received formal training in Culinary Arts before I went on to pursue my dietetics career. Why eat if you’re not going to enjoy the experience? We know that the foods we eat play a significant role in mental health, physical health, and chronic disease prevention (cancer, heart disease, diabetes). We also know that including more plants in our diet correlates with better health and gut function and is a sustainable and eco-
I’m sharing my lentil soup recipe because it is easy to make, plant-based, contains >10 different plant foods, is high in fiber and protein, cheap, and so, so good. While you prepare this recipe, I also invite you to take note of the different textures of the ingredients (crunchy celery and soft mushrooms), the way they are prepared (carrots diced, mushrooms sliced), the way the ingredients change once heated (onions go from opaque to translucent, spinach wilts down to nearly nothing!), the different aromas and how they build over the course of preparing this soup (sautéing mirepoix vs. adding tomatoes and herbs). Being mindful while preparing food and while eating helps make the whole experience so much more enjoyable. Leave out the red pepper flakes if you don’t like it spicy. Serve with warmed crusty bread and some heart
healthy EVOO (extra virgin olive oil) to make it even more hearty. Buen provecho!
LENTIL SOUP — COOKING TIME: 30 MINUTES | SERVING SIZE: 2 CUPS | SERVINGS PER RECIPE: 3-4
Ingredients & Equipment:
Ingredients
• 1 Tbsp olive oil
• 1 medium carrot
• ½ onion
• 1 celery stalk
• 2 cloves of garlic
• 8 oz. crimini mushrooms
• 4 medium tomatoes (or one 28 oz. can of diced tomatoes)
• Spices/herbs: ½ tsp salt, ¼ tsp pepper, 2 tsp dried oregano, 2 tsp dried thyme, 1 bay leaf, 1 tsp red pepper flakes
• 5 cups water
• 1 cup dry red lentils (rinsed)
• 1 bunch spinach (rinsed) or any other leafy green!
• Garnish: fresh parsley, 2 Tbsp nutritional yeast
Equipment
• 2 small prep bowls (for olive oil, nutritional yeast)
• 3 medium prep bowls (for mirepoix, mushrooms/garlic, and tomatoes)
• Soup pot
• Spoon
• Sharp knife
• Cutting board
• Measuring cups and spoons
Steps:
1. Mise en place:
a. Measure out olive oil into small prep bowl
b. Dice carrot, onion, celery (mirepoix) into small pieces (approximately ¼”) and add to medium prep bowl
c. Mince garlic, slice mushrooms, and combine into other medium prep bowl
d. Dice tomatoes and place them (along with juice) into separate medium prep bowl
e. Gather spices/herbs and combine into medium prep bowl with tomatoes
f. Rinse lentils, add to tomato and spice/herb prep bowl
g. Rinse spinach, set aside
We would like to hear from you if you have personal connections with GI & gastronomy. Contact ACG magazine staff by email at acgmag@gi.org to share your story with the ACG community. You can also tweet using #ACGfoodies to connect with the community.
h. Rinse parsley, then finely chop
i. Measure out nutritional yeast into small prep bowl
2. Warm a pot over medium-low heat
3. Add olive oil and carrot, onion, celery – sweat for about 3-5 minutes or until onions are translucent
4. Add garlic and mushrooms and cook for another 10 minutes
5. Add tomatoes, spices, herbs, lentils, and water
6. Bring to boil, then reduce to simmer. Simmer for ~15-20 minutes
7. Turn off heat; stir in spinach
8. Once spinach is wilted, serve soup
9. Garnish with freshly diced parsley, nutritional yeast. Enjoy!

Recipe is gluten free, vegan, high in fiber and iron.
Nutritional Breakdown Per Serving:
If 4 servs, each serv = 258 kcals, 5g fat, 41 g carb, 9g fiber, 363 mg sodium, 16 g protein
If 3 servs, each serv = 344 kcals, 7g fat, 55 g carb, 11 g fiber, 484 mg sodium, 21 g protein


Dr. Bincy Abraham on “Innovations in Clinical Care: Incorporating Intestinal Ultrasound in the IBD Clinic”
Jill K. J. Gaidos, MD, FACG in Conversation with Bincy P. Abraham, MD, MS, FACG


BINCY P. ABRAHAM, MD, MS, FACG, is the Fondren Distinguished Professor in Inflammatory Bowel Disease, Department of Medicine; Professor of Clinical Medicine, Academic Institute in the Academic Division of Gastroenterology and Hepatology at Houston Methodist – Weill Cornell, and Program Director of the Gastroenterology Fellowship Program, Lynda K. and David M. Underwood Center for Digestive Disorders, Houston Methodist in Houston, Texas. Dr. Gaidos had the opportunity to interview Dr. Abraham while at Houston Methodist for hands-on intestinal ultrasound training.
Jill Gaidos: You were the first person that I heard in the U.S. who had started using intestinal ultrasound (IUS) in your inflammatory bowel disease (IBD) clinic. What interested you about intestinal ultrasound to want to learn it and begin using it in your clinical practice?
Bincy Abraham: We had a visiting professor from Australia who came to give a talk for our local GI society and he came to visit us at our institution. He was not doing bowel ultrasound, but his colleague was. He was
“The nice thing about IUS is that it’s an adjunct test. If you have any concerns, you can always order a CTE or MRE if needed.”
—Dr. Abraham
more of a functional GI doctor. He found out that my practice is focused on inflammatory bowel disease and he said, “Bincy, you have to learn how to do intestinal ultrasound.” I had heard about it a bit from a presentation by Dr. Kerri Novak in Calgary, but I didn’t know all the details. So, I reached out to Kerri initially and she introduced me to the Intestinal Bowel Ultrasound Group (ibusgroup.org) and told me to submit an application. I applied and I didn’t get in that first round; I initially got waitlisted but then an opening became available and started training. It was Thanksgiving weekend in 2019 when I did Module 1 in Copenhagen. I remember we took the kids because it was their break too. In the application, you had to talk about what equipment you are getting. I learned about the equipment from the visiting doctor from Australia whose colleague raved about his equipment, “You have to get the Canon i800. It’s the best machine in the world.” I reached out to ultrasound reps and had several vendors come in with their equipment, top of the line stuff. Every clinic day I had one or two vendors each and I would compare the images between the machines. I fell in love with the Canon and the GE but ultimately made the decision to get the Canon machine. I ordered it, went to the course, and came back and started practicing in clinic. I then went to Milan in early 2020 and did 99 ultrasounds there for Module 2 and then went to the European Crohn’s and Colitis Organisation meeting for Module 3 in Vienna. This all happened peri-COVID. Literally, I had taken the last train from Italy to Vienna before Italy shut down. I went to the ECCO meeting, passed my test, and got certified. When I got back, everyone was talking about COVID and how Milan was at the epicenter and I was like, “Oh my gosh!” I think I missed the whole thing by just a few days. And, I came back and started doing ultrasounds and it’s really changed how I practice.
JG: One of the challenges with implementing IUS in practice is the cost of the machine. A lot of sites are using donations and philanthropy
funds to pay for the ultrasound machine. How were you able to get your ultrasound machine funded?
BA: I was lucky enough to get department funding for my equipment. It is the best opportunity if you can utilize philanthropic funding because you can actually show value to those who provided the funds and how it is changing the practice of medicine. For centers who don’t have the opportunity to use philanthropic funds or have saved budget to purchase a machine, you can eventually break even with normal reimbursement of performing the exams. In our article
“Integrating Intestinal Ultrasound into an Inflammatory Bowel Disease Practice: How to Get Started” published in Crohn’s and Colitis 360 (Abraham BP, Reddy D, Saleh A.Integrating Intestinal Ultrasound into an Inflammatory Bowel Disease Practice: How to Get Started. Crohns Colitis 360. 2023 Aug 7;5(3):otad043. doi: 10.1093/crocol/otad043.
PMID: 37719309) we have provided a formula to calculate how long it will take you to pay off your machine. The formula includes the number of ultrasounds you do with the average reimbursement for the insurance companies in your area to calculate how long it would take to recoup the cost of the machine. You can use that information to tell your institution or administrators, “If we get this machine now, we can break even in X number of months.” It will vary depending on the number of procedures that you do and the number of providers who do it at your site. Fortunately, the maintenance of the equipment is of low cost. I’ve had my machine since 2019 and as long as you take good care of it, that is, don’t drop your transducers, do annual maintenance through the manufacturer, it will last you for years and years. And, once you break even, the rest is profit. Some sites bill for a facility fee. We do not bill for a facility fee at our site.
JG: Another challenge is taking the time away from your clinical practice to complete the multiple training sessions.
BA: Practitioners have to spend one month away from their clinical practice to complete the hands-on session which can be a struggle to arrange. The time is typically divided up into two-week blocks. But it’s important to get adequate practice at an expert center to be comfortable obtaining and interpreting these images.
“For centers who don’t have the opportunity to use philanthropic funds or have saved budget to purchase a machine, you can eventually break even with normal reimbursement of performing the exams.” —Dr. Abraham
JG: Did you have support from your hospital leadership to implement IUS or did you have to convince your administration that this would be useful?
BA: In Texas, we are not employed by the hospital, but we are under the physician organization of Houston Methodist. So, our hospital is different from the clinic practice. Our GI section is very big and we are ranked in the top five in the nation for GI and GI surgeries based on this year’s U.S. News & World Report, so there is a reputation to do what is important to advance medicine. I never received any pushback from radiologists or our leadership but, in fact, encouragement to learn this point-of-care imaging. At our referral center, patients can have very complex disease, so I still order MRI Enterographies (MRE) on them if needed. Especially if I am not sure of a finding on IUS. Until my surgeons feel comfortable with just IUS imaging, I don’t prevent them from ordering additional imaging such as CT or MRIs especially if they feel it is needed to obtain cross-sectional assessment prior to a major surgery.
JG: Right, you don’t want to miss anything. BA: I feel better, the patient feels better when there is confirmation with another type of assessment. So, no real pushback. I think everyone has seen the benefit. The other part of it is I’ve been here at my institution for 10 years, so being a bit established and having seen me grow the practice helped a lot. I also applied for an institutional grant that is available for those who want to learn a new technique or skill that is not available at my institution. I received the grant funding to learn IUS with approval from my Chief of GI who was quite supportive of me doing this additional training.
JG: Was it easy to implement IUS into clinic logistically? Did you just watch to see how others did this during your training or was it trial and error?
BA: It was trial and error because no one else in the U.S. was doing it so I didn’t know who to ask. Because I was learning, and I didn’t want patients to be delayed in clinic I set aside one day to do IUS; Tuesdays were my IUS days. I made sure
I had one hour per patient because I was doing the full clinic visit, doing the ultrasound, the report, and the billing. I wanted to make sure I had time to see everything and not feel rushed to find stuff quickly while the next patient is waiting. So, I initially set aside one full hour (30 minutes for clinic visit, and 30 minutes for IUS) to do all of it including documentation and orders. I thought that was great because, even though I was seeing fewer patients, I felt more comfortable and used that as investment time to learn how to implement IUS into clinic correctly. But, once I became more comfortable, I was able to shorten the visits to 45 minutes (15 minutes for IUS), then 40 minutes total. I have my APP help me in clinic too; we tag team. I start the ultrasound, getting the history while she is typing in the note and ordering labs. When I’m done with the ultrasound, I already know the management plan for the patient. Since I know what their disease activity is based on the IUS, I either continue therapy, do therapeutic drug monitoring and adjust the dosing of their therapy, change to new therapy, schedule for additional tests like a colonoscopy, or order additional imaging, if needed. We have a plan in place before they leave, so I don’t have to wait for a calprotectin to come back or wait for an imaging order to be scheduled or wait for the colonoscopy to provide a plan of care. So, it just makes the flow of assessment and management so much quicker. Right then and there, we know what to do and we can schedule the appropriate follow-up based on if they are in remission or if they have active disease. The whole management part of the patient visit is simplified. Now, I do IUS on essentially every IBD patient that comes for an in-person visit.
JG: How long do you think it took you to get comfortable? I know you did 99 cases during your Module 2 training. So, when you came back, were you comfortable with everything you saw on the intestinal ultrasound?
BA: Absolutely not. It’s a lot like GI fellowship when you learn
colonoscopies. You may be very good, but if you can’t get through a tight curve or can’t get into the ileocecal valve, you have an attending backing you up. But when you leave fellowship, you don’t have that backup anymore. Similarly, when you are done with your training and you are doing your own ultrasounds, there isn’t anyone there to say, “Oh that’s right,” or, “you measured that correctly.” So, there was a time period for building up of your confidence. The nice thing about IUS is that it’s an adjunct test. If you have any concerns, you can always order a CTE or MRE if needed. I’m not saying I ended up ordering MREs on every patient I did IUS on, but more for those with complex disease. Also, with IUS, you can reassess them at any time; you know your own schedule. You always have the back-up of additional testing if you need to. I can’t give you an exact number that I did before I felt better, but I would say probably another 50 to 100 or so. I think the hardest ones are the normal ones because it’s harder to find normal bowel. The other thing that is more challenging are the patients who have had surgery because their anatomy is different. There are a lot of things that you worry about such as missing any critical findings or especially early on, mixing up the stomach for part of the transverse colon or using the incorrect probe and missing findings deeper in the abdomen. Similar to colonoscopy, when you know to look behind all the folds to try not to miss a small polyp or something. You learn more from experience and learn tips and tricks as you go along. Also, staying involved with IBUS and their meetings definitely helps. Just hearing others talk about how they do ultrasounds, their data, and seeing their images are quite reassuring and you think, “OK, I’m doing it right,” or, “That’s a good tip,” and I’ll keep that in mind when I’m doing my next pouch patient or a patient with a stoma, etc.
JG: So now that more U.S. sites are getting involved in IUS, do you think this will lead to changes in our guidelines for IBD management?
BA: I’m actually excited that most of the IBD centers are learning it because I think IUS is the most amazing tool. I can’t believe we have gone so many years without using it. I think it’s just fantastic. Now,
the question is, could every single gastroenterologist be able to learn this now? Probably not the existing general practice GI doctors. But, since it’s such an impactful tool, I think we are starting out correctly by using this at IBD centers. My hope though, as we are talking about the future, is to train all GI fellows in abdominal and intestinal ultrasound. It’s useful to distinguish IBD from IBS. We would do a colonoscopy for these patients, but there are some patients who are low risk and may not warrant an invasive procedure. We could use adjunct markers such as fecal calprotectin, but for those patients who have more abdominal pain and less diarrhea, the stool marker may not be as useful, whereas the IUS would be beneficial. I have a patient who has IBD in remission but has terrible constipation. We saw her entire colon filled with stool. She wanted me to change her IBD medications when really it was due to delayed transit constipation. We put her on constipation medication, and she improved clinically. But I had to show her that there was no bowel wall thickness. We could actually see her bowel wall beautifully because everything was filled with stool, and we could see all her normal bowel wall layers. She then understood that we needed to treat the constipation. I think it can be hugely beneficial. In the future, I think we should be training our GI fellows in this, starting them really early. Now our internal medicine residents are being trained in pointof-care ultrasound, not just for GI but for heart and lungs and other organs too. Future generations of GI fellows should get trained in ultrasound, not just intestinal but abdominal too. That would be my hope.
Regarding guidelines for IBD, in our STRIDE 2 guidelines we talk about the informal recommendation for transmural healing in Crohn’s disease. I think STRIDE 3 guidelines would need to include that as a formal target. Now that we are doing more IUS, we have more data on the benefit of transmural healing over just endoscopic healing. With endoscopic healing, you are
just looking at the mucosa. But we all know that Crohn’s is a transmural disease, so we need to know about the submucosa and the other layers. We can also look at extramural complications with IUS. I think we are going to change our guidelines for disease assessment and our long-term goals for histological and transmural healing. Especially now that we have more treatment options.
JG: One of the things I commonly find is that women tend to compare themselves to other women, particularly related to their accomplishments. You are someone who does a lot! As the director of your IBD program, the program director for the fellowship program, you are the PI on multiple clinical trials, you give a ton of talks. How do you find time to do all that you do?
BA: It’s all about looking good on the outside (laughing)! Internally though, my brain may be going a little bit crazy. Reading a lot of time management books has helped. Setting up boundaries has also helped.
I gave a talk at the ACG Women’s Leadership Conference in 2020 about setting boundaries and no one had really talked about exactly how to do that previously. I found this amazing article that talked about what is your boundary style. If you know that, then you can set the appropriate boundary. That really opened my eyes. We always read articles that suggest you need to manage your time, but how do you do that? Yes, you make to-do lists, but when you get 200–300 emails a day you are never on top of everything. Or “do your priority activities first.” But, in medicine, everything is a priority. So how do you even distinguish what is a priority?
JG: Everything is an emergency.
BA: Everything, it seems. One thing that has really helped was knowing what my boundary style is. There are two major boundary styles: a separator vs. an integrator. When I did the quiz, I found out I’m a huge separator. Meaning, that when I’m at work, I
prefer to focus on work only. When I’m at home, I prefer to focus only on home and family. If anything gets disrupted, I feel out of balance; I feel stressed. What I used to do was work until about 6 p.m. I would take home all the stuff I hadn’t finished. Once my kids were in bed, I would go back to finish the work. But I noticed that 80-90% of the time, I didn’t get that work done because I was exhausted, especially when my kids were little. I don’t know what I was thinking. Unless it was a major deadline, then I drink as much coffee as possible to get it done. But, when I found out I was a separator, I realized why I was feeling so out of control. So what I ended up doing was staying a little bit later at work, finishing the work. Then when I get home, I can spend time at home with the family and not stress out about going back into work mode.
JG: Not thinking about all the things you didn’t finish at work.
BA: Yes! Similarly, when I’m at work and I’m getting a call about home stuff or something about the house, I get so stressed because I’m not there to fix that or help them out. My husband knows not to call me at work unless it’s a true emergency. If there are any home issues, he will wait until I get home and then we can discuss it then. Unless it’s a true emergency, of course, like a kid who is ill and someone needs to pick them up from school/daycare, etc. That happens as a working mom, but I’m always hoping my husband can go pick them up, especially on my scope days when you can’t leave.
JG: Exactly. Nobody get sick today!
BA: I just find I do so much better that way compared to someone who is an integrator. They do well integrating work and home life stuff easily. They can schedule an appointment for their kid at the pediatrician or schedule the plumber to come to their house while they are at work. Then when they get home they can do work-related calls or emails and still be there doing their home stuff. I just need to mentally separate.
JG: I can already tell just by what you are saying, I am absolutely a separator.
BA: This article was amazing; I think everyone should read it. [Kossek, Ellen E. 2016. Managing work–life boundaries in the
digital age. Organizational Dynamics 45(3): 258-270.] Finding out that I am a separator really helped, but it was also critical to incorporate the basics of time management. Not everything is a priority; some things can wait. You do as many of the urgent and important things as possible, like putting together the slides for upcoming presentations. I put deadlines on my calendar and block off time to work on those. I tell my administrator not to schedule any meetings during those times. For the most part, I make myself stick to it. Sometimes, it takes me less time than I expected, but 90% of the time it takes longer. I read somewhere that you should allot 50% more time than you think you will need. Delegating as much as possible is also important. We have issues delegating things because we have been doing these things for so long, so we think we are the best at it. But, unless you allow someone else to do something for you, you will never let go. One of the classic examples is letting the kids wash the dishes. Sure, they may leave a few crumbs here and there, but if they never start, and we never delegate, then I will end up doing the dishes for the rest of my life. You also need to know how much time you need for yourself to recharge. Depending on how much time you need, you should schedule it. I am an introvert, so at conferences, I spend a lot of time with other people, but I have to include time to go back to my hotel room, taking time for myself alone so I am recharged for the next day.

Jill K. J. Gaidos, MD, FACG
Dr. Gaidos is Associate Professor of Medicine at the Yale School of Medicine Section of Digestive Diseases and Director of Clinical Research for the Yale IBD Program.

Bincy P. Abraham, MD, MS, FACG
Dr. Abraham is the Fondren
Distinguished Professor in IBD and Professor of Clinical Medicine at Houston Methodist-Weill Cornell and Program Director of the GI Fellowship Program at the Lynda K. and David M. Underwood Center for Digestive Disorders.

REFLEXIVELY, WITHOUT THINKING. Others you carefully consider, weighing risks and reaching a logical conclusion. My decision to donate a kidney to a 72-yearold man who wasn’t a relative, or even a close friend, was both. I am aware that to many people it seems a bit crazy, but it made sense to me. He needed one, I had two, the data on long-term outcomes for living donors is reassuringly excellent, and I would get four weeks off work around the holidays to recover.
Chuck Hampton is an unbelievably kind and positive person, beloved by students, staff, and generations of Brown alumni. He is employed at the athletic facility, working the early morning shift at the welcome desk, greeting members as they swipe ID cards, eager to chat for a few minutes about your kids or weekend plans, while offering a fist bump to every student athlete arriving for morning practice. I had known him for about seven years, since I joined a running club that uses the facility for practice. When he told me his kidneys were failing and rolled up his left sleeve to reveal the fistula, he didn’t seem too worried. He planned
“...[I]t wasn’t so much a choice as an obligation to a fellow human being, whose kindness represents the best of what we can all be.”
—Dr. Kelly
to get listed for transplant and felt confident things would work out. My reaction was immediate, kind of like when someone needs a pen to sign something and you hand them yours. I knew that I would give him one of my kidneys. I am blood type O negative, and a colleague and running club friend, who also happened to be Chuck’s transplant surgeon (Rhode Island is like that), was pretty confident that I would be a match.
To be clear, I didn’t offer right away. Instead, I spent time researching and discussing it with family and close friends over the next few months. The reactions were mixed, but mostly supportive, and those who weren’t happy about it (i.e., my dad) knew well enough that it wasn’t possible to talk me out of something I had decided to do. As the path forward opened in front of me, with a few encouraging signs, if you believe in that kind of thing, it became apparent that not to donate would be turning away from a calling. For me, it wasn’t so much a choice as an obligation to a fellow human being, whose kindness
represents the best of what we can all be, and who deserved more time.
In the United States, over 100,000 people are on the waiting list for kidney transplant, yet only about 25,000 transplants are performed annually. With waits as long as five years, most die waiting. If one out of every 10,000 healthy Americans donated, then many dialysis centers would close. Encouragingly, more and more people are joining the living donors club; there is even a Facebook group with over 9,000 members. Few express any regrets and most describe it as one of the most meaningful things they have ever experienced. Kidney exchanges or chains are another innovative way that more patients have been matched with a suitable donor.
Payment is an issue that is controversial and opposed by many ethicists. Today, donors are prohibited by law from being paid or reimbursed in any way (though, full disclosure, I did get a color photo of my kidney taken by the surgeon just before its laparoscopicallyguided removal, as well as a mug, a water bottle, which I promptly lost, and a boxy oversized T shirt with a giant green ribbon on the back that I will likely never wear). However, there is reasonable argument that financial incentives for donors are not different from compensating an egg donor or pregnancy surrogate and could be conceived in a way that would prevent exploitation of the socioeconomically disadvantaged. Safeguards such as built-in waiting periods and delayed compensation, with payments spread over 10 years or given in the form of school vouchers, retirement savings, or other longterm government benefits would prevent vulnerable persons from donating out of immediate financial desperation. Compensating donors would shorten the waiting time and save the health care system billions of dollars annually. For now, the only permissible donor benefit occurs if a previous donor needs a kidney
“In the United States, over 100,000 people are on the waiting list for kidney transplant, yet only about 25,000 transplants are performed annually.”
—Dr. Kelly
transplant: allocation regulations for organs from deceased donors give priority to candidates on the waiting list who have given whole or segments of organs, so I’ve got that going for me.
It's been a little over a year now since our surgeries. My creatinine has settled at a new baseline of 1.3, I feel well and am back to running, with a 2-inch scar just to the left of my belly button. It makes me really happy to see Chuck back at work, spending time with friends on campus and cheering on the teams. Personally, I feel proud that I had the courage to do this (I was TERRIFIED the morning of my nephrectomy) and can attest to the truth of the statement that the most meaningful things in life are those that require sacrifice.
We are all interconnected, and doing for others leads to deepest joy and fulfillment. As physicians, we know that unpredictable and tragic things happen to people all of the time, and I don’t believe in living my life in a calculated way to try to outsmart the inevitable. Odds are that my remaining kidney won’t fail and that I will be fine and die of something completely unrelated when my time comes. I’m not worried about it.

INFLAMMATORY BOWEL DISEASE (IBD) TREATMENT HAS BECOME INCREASINGLY COMPLEX. IBD education varies across fellowship programs. IBD 101 is a novel program that was designed to provide introductory level IBD exposure to first-year gastroenterology (GI) fellows in order to provide a common baseline understanding of the disease complexity and management strategies, and to review the opportunities for supplemental IBD education during or following GI fellowship. The program utilizes experiential learning and group observed structured clinical exams (GOSCEs) to teach the basics of diagnosis and management of IBD. In 2019, a cohort of fellows participated in a one-day course with small group learning and GOSCEs. Findings from pre- and post-course surveys reveal that IBD 101 was associated with increased comfort managing IBD with a durable benefit independent of individual access to IBD education. This article reviews highlights and offers perspectives from IBD 101 faculty and the takeaways of several participating GI fellows.
“The basics matter in IBD. It’s important to understand how to diagnose a patient with IBD and know that with this discussion you will be beginning a lifelong relationship with your patient.”
—Dr. Katie Dunleavy, 2021 Participant

Lisa B. Malter, MD, FACG Professor of Medicine, NYU Grossman School of Medicine; Director of Education, Inflammatory Bowel Disease (IBD) Center, NYU Langone Health
COURSE CO-DIRECTORS

David H. Hudesman, MD, FACG Professor of Medicine, NYU Grossman School of Medicine; Co-Director, Inflammatory Bowel Disease Center at NYU Langone Health


Sunanda V. Kane, MD, MSPH, FACG Professor of Medicine, Mayo Clinic Rochester, MN
David T. Rubin, MD, FACG
Joseph B. Kirsner Professor of Medicine; Chief, Section of Gastroenterology, Hepatology and Nutrition, University of Chicago Medicine
What Is Known:
• IBD care is becoming more complex and evolving rapidly
• There is variability in IBD education and exposure amongst U.S. gastroenterology training programs
What Is New:
• A one-day educational program, “IBD 101: Physicians and Patients Providing Pearls and Perspectives,” was held by NYU Langone Health on September 14, 2019
• This novel educational program for first-year GI fellows was well received by attendees and faculty
• Use of GOSCEs featuring standardized patients was a practical education tool
• Attendees had increased comfort managing IBD three years later compared to peers
• The program has run each fall since 2019 and in collaboration with the ACG has expanded to offer programming to all North American GI fellows
own diversity in patients, local physician expertise, and educational opportunities. Access to patients with IBD and to gastroenterologists who subspecialize in IBD is not guaranteed. Comprehensive and effective education in IBD has become increasingly complex to provide as the field has undergone and continues to undergo rapidly evolving changes related to emerging therapeutic options and treatment endpoints.
While there are numerous IBD educational offerings available to fellows at various time points during GI training, they vary in availability depending on location, the ability to leave one’s home institution, and the home institution’s resource pool. None of these other regional or national opportunities for fellow education have been available during the first year of training in GI and this, therefore, delays and potentially minimizes their understanding and interest in IBD.
IBD 101 was designed to address these challenges.
Structure of IBD 101
Rationale for IBD 101
With an increased prevalence of IBD, shifting demographics, continued evolution of treatment targets for IBD patients, and a rapidly changing therapeutic armamentarium, it is increasingly important to ensure that all GI fellows are adequately educated about IBD to meet the needs for greater expertise. It has been demonstrated that patient care varies by center, with evidence to support superior IBD-related care being delivered at higher volume centers. Patients with Crohn’s disease followed at an academic center are more likely to achieve steroid-free remission and a better quality of life.
Moreover, training in IBD diagnosis and management during GI fellowship is not uniform across academic institutions. Each hospital system serves a unique population with its
Course objectives include: (1) provide an educational opportunity for the firstyear fellows to learn basic, introductory information on the diagnosis, treatment, and management of IBD; (2) offer fellows exposure to the subspecialty of IBD early in their fellowship, to allow them to make more informed career decisions; and (3) inform fellows about other educational opportunities in IBD.
Components of IBD 101 include: (1) small group didactics on basic IBD topics; and (2) clinical case simulation rotations, demonstrating basic conversations about managing aspects of IBD care. The simulation portion of the program utilized standardized patients (SP) to play the role of a patient with IBD who suffered from a focused aspect of their disease that required clinical management and discussion. In this portion of the program, fellows rotated in groups of five, observing the GOSCE sessions, with each session featuring one of the faculty discussing a specific aspect of IBD care with the SP during a twelve-minute simulated clinical
scenario. For each GOSCE session, at the completion of the simulation, the fellows had 20 minutes to review the case with the faculty member and to ask questions.
Specialized training in the diagnosis and management of IBD during GI fellowship is desired by trainees and may enhance patient outcomes. The results of IBD 101 demonstrate the benefit of this introductory exposure for GI fellows and the demand for the course has grown and persisted in subsequent years. We intend to offer this programming for the foreseeable future to meet the future needs of our field.
A Sample Case from IBD 101
The scene: A 58-year-old man with a diagnosis of longstanding ulcerative colitis with inadequate treatment due to reluctance to start a stronger therapy who is admitted to the hospital with worsening of his condition. He has been treated with intravenous steroids but is having a suboptimal response and warrants an alternative approach.
The objectives of the expert clinicians’ discussion with the patient:
1. Review the current state of the patient's disease
2. Address appropriate considerations in management at this time
3. Answer any questions the patient has regarding his condition and recommended treatment options
The goals for the trainee:
1. Summarize the clinical case
2. Review the treatment options offered by the physician
3. Ask questions about what was recommended
4. Ask questions about why this course of action/therapy is best
5. Ask questions about how this was portrayed to the patient
6. Clarify anything that remains unclear
In 2019,
100%
55 FELLOWS from 32 ACGME-ACCREDITED GI TRAINING PROGRAMS completed pre- and post-course surveys (89%)
fellows reported:
INCREASED COMFORT managing IBD patients
98% of fellows reported increased interest in exploring IBD during fellowship
completed surveys in 2022 of whom 58% WERE IBD 101 ATTENDEES
18 IBD experts from 8 academic institutions in the U.S.
11 faculty completed post-course surveys
IMPROVEMENT IN UNDERSTANDING of supplemental opportunities to learn about IBD during fellowship
96% would strongly recommend IBD 101
COMPARED TO NON-ATTENDEES, those attending IBD 101 reported:
• Higher levels of comfort managing IBD
• Higher global competence after adjusting for presence of a local IBD specialist, number of IBD patients per month, and rotation through an IBD service
100% of faculty:
• agreed that both the didactic and GOSCE formats were effective teaching tools.
• would recommend the course to other first-year trainees
Key Take-Away: IBD 101, an introductory course for first-year GI trainees, was associated with increased comfort managing IBD with a durable benefit independent of individual access to IBD education.
About The Survey: Fellows completed a pre- and immediate post-course survey to provide a measure of the program’s ability to meet its objectives and assess improvement in comfort levels with various aspects of IBD care. Three years after the inaugural IBD 101 course, in May 2022, email surveys were administered to third-year GI fellows from programs that participated in the course including those fellows that attended the course as well as those who did not. It is important to note that the cohort of GI fellows who participated in the program in 2019 had their training interrupted by the COVID-19 pandemic, which may have impacted their uptake of the IBD materials, and their educational intentions and career plans.
During the COVID-19 pandemic we pivoted to a virtual format for our 2020 program. While still maintaining small group learning in a Zoom format, we were able to continue the course and grow the program during subsequent years as well as fully collaborate with the ACG starting in 2021. Our largest program hosted over 400 North American GI fellows in 2022 with a faculty including over 40 IBD experts from all over the U.S. The program will return to its original live format with a program to be held on September 14, 2024 in Washington, DC.
Read More about IBD Training:
Malter LB, Israel A, Rubin DT. Proposal to Update the Curriculum in Inflammatory Bowel Diseases for Categorical Gastroenterology Fellows. Inflamm Bowel Dis. 2019;25(9):1443-1449. doi:10.1093/ibd/izz107
Wolff MJ, Balzora S, Poles M, Zabar S, Mintah A, Wong L, Weinshel E, Malter LB. Objective structured clinical examination as a novel tool in inflammatory bowel disease fellowship education. Inflamm Bowel Dis. 2015 Apr;21(4):759-65. doi: 10.1097/MIB.0000000000000317. PMID: 25633560.
Kahn SA, Rubin DT. Can we improve on the "see one, do one, teach one" paradigm in training fellows to care for patients with inflammatory bowel disease? Inflamm Bowel Dis. 2015 Apr;21(4):766-7. doi: 10.1097/MIB.0000000000000337. PMID: 25719529.
Malter L, Hong SJ, Lopatin S, Murphy M, Hudesman D, Kane S, Rubin DT. Increasing Exposure to Inflammatory Bowel Diseases Education in Gastroenterology
Fellowship: The Pilot IBD 101 Experience. Inflamm Bowel Dis. 2024 Jan 13:izad311. doi: 10.1093/ibd/izad311. Epub ahead of print. PMID: 38217539.
Learn more About IBD 101: gi.org/trainees/ibd101
This program was generously supported by unrestricted educational grants from Pfizer and Takeda Pharmaceuticals and sponsorships from AbbVie, Janssen, and Prometheus Labs. The organizers would
With a group observed clinical "examination" or GOSCE, examination is in quotes as no one is in the hotseat for these since IBD 101 is geared for early GI trainees who are NOT yet knowledgeable about IBD. The NYU Grossman School of Medicine has been using simulation with observed standardized clinical exams (OSCEs) in GI fellowship since 2006. These OSCEs include scenarios designed by medical educators in GI in order to provide fellows the opportunity to role play with a standardized patient. In 2013, the IBD-specific OSCE at NYU was created to assess fellows' ability to discuss complicated aspects of IBD management during second- or third-year GI fellowship. However, the intensive nature of standard OSCEs led to the inability to scale the program to larger groups. That is what led to the development of this program utilizing a group format. GOSCEs were first reported back in the 1990s and provide an opportunity for more learners to experience the educational tool in a cost-effective manner as well as provide an opportunity for idea sharing between the learners. The use of standardized patients in a modified OSCE format significantly enhances the exposure of IBD compared to didactics and case-based learning alone while having the unique opportunity to watch experts in the field conduct the visit.
like to thank medical educators Dr. Elizabeth Weinshel and Dr. Sondra Zabar and standardized patient expert Ginny Drda and the NYSIM team for their expertise in the program development; Dr. Mark Pochapin and Tamar Wallace for their support in the course development; Danielle Seabron for her support in the course management; and Dr. Sarah Lopatin and Dr. Simon Hong for the data analysis.

Katie A. Dunleavy, MB, BCh, BAO, Mayo Clinic, Rochester, MN, 2021 Participant
1. What were the two or three most critical take-aways from IBD 101 program and why did they resonate with you? The basics matter in IBD, it’s important to understand how to diagnose a patient with IBD and know that with this discussion you will be beginning a lifelong relationship with your patient. With new treatment options, patients have a higher chance of achieving remission, but treatment must be personalized to the individual. Goal setting is key in IBD; you cannot choose a treatment until you and the patient have decided on a shared goal for achieving success.
2.IBD 101 has a unique offering with clinical case simulations. What benefits and insights did this part of the program provide?
Personally, I believe clinical case simulations are very important for new GI fellows. It can be hard to imagine a scenario of a patient with IBD outside of a textbook or board review question. Having the opportunity to work through detailed personal cases allowed the patient to have a space in our learning. Similarly, seeing experts having difficult patient conversations in the GOSCE gave me the words and the confidence to do the same in my own practice.
3.This program had powerhouse faculty. What was the most surprising/ intriguing advice you heard at IBD 101? I particularly enjoyed hearing from Dr. Susie Kane about her experience discussing pregnancy and fertility risks with patients. This is a nuanced discussion that requires both confidence in facts and humility in demeanor. It was fantastic to see her model this discussion and show us the power of listening with intent.
4.What advice do you have for first-year fellows who might be considering IBD 101?
Just do it! If you are interested in IBD, or eager to learn more, sign up and get
ready to be amazed. This program is geared towards first-year fellows and really covers the basics of IBD, and the nuances to taking care of patients with IBD. The faculty is incredible and kind. I had the opportunity to attend the IBD 101 Happy Hour at ACG 2022 and it helped lead to career advice and mentorship.
5.Anything else to add — insights, gratitudes, “aha” moments?
A huge thank you to Dr. Malter for making this program possible. I hope we can continue to have IBD 101 reunions at ACG each year. It is a wonderful and low-key way for fellows to meet their IBD heroes in real life.
 Omar Jamil, MD, University of Chicago, 2022 Participant
Omar Jamil, MD, University of Chicago, 2022 Participant
1.What were the two or three most critical take-aways from IBD 101 program and why did they resonate with you?
Sometimes we get so caught up in the care of complex patients that we forget the basics of outpatient management of mild disease. The course did a great job of building foundational knowledge in the management of mild to moderate disease, which is important to solidify before getting into the weeds of understanding new agents and new treatment strategies.
2.IBD 101 has a unique offering with clinical case simulations. What benefits and insights did this part of the program provide?
I really enjoyed this. IBD affects every component of a patient's life and requires empathic care. The simulations were common, but important, index cases that not only established key principles in basic care, but also put on display the importance of bedside manner and attention to detail.
3.This program had powerhouse faculty. What was the most surprising/intriguing advice you heard at IBD 101?
I always enjoy watching Dr. Rubin
interact with patients. In the course, he acts as the clinician in one of the patient simulations. He is empathic but definitive, he is economical with his words and precise when he speaks. Seeing experienced providers in the patient cases is fun and aspirational; I think we can always pick up small gems to improve outpatient interaction skills.
4.What advice do you have for first-year fellows who might be considering IBD 101?
The learning curve in the first year of fellowship is steep, and in the hospital there sometimes is not time to ask questions with all the work that needs to be done. The course offers an opportunity to ask everything and anything you want to know about IBD and will give you the confidence you need to triage problems and provide basic care as a first-year fellow.
5.Anything else to add — insights, gratitudes, “aha” moments?
All of my favorite attendings are the ones who have no problem with being vulnerable, admit when they don't know something, and ask questions. This course is an opportunity to sit down and just learn from the experts; it's a rare and unique opportunity and the break-off groups create small spaces so that you can interact with faculty in a smaller setting.

Megan Murphy, MD Johns Hopkins Medicine, Sibley Memorial Hospital, 2019 Participant
1.What were the two or three most critical take-aways from IBD 101 program and why did they resonate with you? Managing IBD is complicated and care is rapidly evolving. There are several new treatments on the market today that weren’t available back in 2019 when I attended the inaugural IBD 101. Understanding resources on where to keep up with the latest in IBD is helpful. IBD 101 provides not only in-depth education that day but also reviews other learning opportunities going forward for trainees. Second, the patient perspective is so important. IBD can have a dramatic impact on someone’s quality of life, and, often in young people, for many years. It can
be easy as a trainee to get caught up in learning drug mechanisms of action or cancer screening protocols, but at the end of the day you have to understand how this disease is impacting the patient’s quality of life in order to best care for them. IBD 101 uniquely had real patient discussions in addition to standardized patient encounters. Lastly, the academic IBD community is filled with incredible clinicians, researchers, and educators. It is an engaging and approachable faculty; trainees should take advantage of any opportunity to learn from and interact with this group of physicians.
2.IBD 101 has a unique offering with clinical case simulations. What benefits and insights did this part of the program provide?
The group OSCE, where learners observe faculty work with a standardized patient in a clinical vignette, is one of the highlights. First, it takes the pressure off the learner to perform an OSCE so you can really sit back and take it all in. Second, you are learning from the absolute best in the country. I was able to watch Dr. David Rubin and Dr. Corey Siegel, leaders in the field at institutions far from my own training site, talk with patients about starting a biologic or thinking about a colectomy. These were invaluable experiences and aid in teaching the intangibles, nuances, and style you can’t learn from a textbook.
3.This program had powerhouse faculty. What was the most surprising/intriguing advice you heard at IBD 101?
I wouldn’t call it “advice”, but what surprised me the most was how approachable, collaborative, and enjoyable the faculty was. I was blown away by the quality of clinician educators that were there. Witnessing the leaders in the field interact like old friends and passionately teach about IBD was both refreshing and inspiring. I knew at that time I wanted to set myself up professionally so I could one day be part of that circle.
4. What advice do you have for first-year fellows who might be considering IBD 101?
Go! Even if you do not plan to pursue a career in IBD, as a general gastroenterologist, advanced endoscopist, or hepatologist, you can’t escape seeing IBD in your patient population. It’s a concentrated high-yield learning experience with the ability to network with faculty and fellow trainees from across the country. Especially for first-year fellows who may be undifferentiated as to their future career path or have lower volumes of IBD at their training institution, you may realize IBD is the career move for you! Early in your training is the optimal time to explore.
5. Anything else to add — insights, gratitudes, “aha” moments?
I am grateful to my general GI program director, Dr. Mark Mattar, for supporting me in attending the inaugural IBD 101 back in 2019. It really sparked my academic interest in IBD and gave me the roadmap to begin exploring a career in IBD. By attending IBD 101, I had exposure to other IBD learning opportunities to pursue throughout my general GI training and an introduction to Dr. Lisa Malter. Dr. Malter ultimately became my program director during my advanced IBD fellowship at NYU. I am so grateful to Dr. Malter for her personal mentorship during my training and so impressed by her for building and expanding this program which will continue to educate trainees and open doors for them early in GI fellowship, as it did for me.
 Siri A. Urquhart, MD Mayo Clinic, Rochester, Minnesota, 2021 Participant
Siri A. Urquhart, MD Mayo Clinic, Rochester, Minnesota, 2021 Participant
1. What were the two or three most critical take-aways from IBD 101 program and why did they resonate with you?
The IBD 101 program introduced me to the breadth and depth of IBD clinical care, research, and educational opportunities available to trainees in gastroenterology. With the intimate
and interactive format, including use of small group discussions, I learned that the care of patients with IBD is truly an art. The diversity of IBD faculty and national leaders from across the country provided me with a unique insight and perspective on how to best care for my patients with IBD. The IBD 101 Fellows Mentorship and IBD Circles provided a unique interactive, virtual space to share complex cases and receive advice from world experts in IBD!
2. IBD 101 has a unique offering with clinical case simulations. What benefits and insights did this part of the program provide? The clinical case simulations offered the opportunity for in-depth discussion on the variety of ways with which we as gastroenterologists can approach the care of patients with IBD. It was truly a wonderful experience to see, hear, and participate in these discussions, ultimately learning that there are a variety of options with which to approach the care of patients with IBD.
3. This program had powerhouse faculty. What was the most surprising/intriguing advice you heard at IBD 101?
The IBD faculty who participated in the IBD 101 program were very approachable and friendly. Participating in this program as a first-year gastroenterology fellow allowed me to form initial connections with faculty whom I now get to see and interact with at meetings and conferences throughout the year!
4. What advice do you have for first-year fellows who might be considering IBD 101? I would strongly encourage first-year fellows to participate in IBD 101. This program provides the opportunity to learn basic, introductory information on the diagnosis, treatment, and management of IBD, exposure to IBD as a subspecialty early on in fellowship to make career decisions and mentorship connections and learn about other educational opportunities in IBD.
5. Anything else to add — insights, gratitudes, “aha” moments?
I am very grateful to have participated in the IBD 101 program. The IBD community is welcoming, friendly, and supportive
and the IBD 101 program brings these qualities to life in a fun, interactive format for trainees!

Muhammad Nadeem Yousaf, MD, University of Missouri, 2022 Participant
1. What were the two or three most critical take-aways from IBD 101 program and why did they resonate with you?
One of the most critical takeaways from IBD 101 was the emphasis on a holistic approach to patient care. The program highlighted the importance of considering not only the evaluation of complexity of IBD but also the psychological and emotional impact it has on patients. Understanding this multidimensional aspect of the disease resonated with me deeply because it reinforced the significance of empathy and compassion in providing comprehensive care to my IBD patients. Learning about novel treatment modalities, ongoing clinical trials, and emerging research gave me a sense of optimism and renewed motivation to contribute to the ongoing efforts in improving patient outcomes. The program highlighted the importance of staying updated with the ever-evolving landscape of IBD management, instilling in me a commitment to lifelong learning.
2. IBD 101 has a unique offering with clinical case simulations. What benefits and insights did this part of the program provide?
The clinical case simulations offered by IBD 101 were undoubtedly one of the most beneficial aspects of the program. These simulations and small group round table discussion with outstanding faculty provided a realistic and immersive learning experience, that allowed a small group of fellows in each breakroom to apply their knowledge gained during didactic sessions. By engaging in interactive discussions and problem-solving exercises, we developed essential skills in diagnosing and managing complex IBD cases with a methodical approach. These simulations not only deepened
our understanding of the disease but also honed our critical thinking abilities, preparing us to navigate realworld challenges with confidence.
3.This program had powerhouse faculty. What was the most surprising/intriguing advice you heard at IBD 101?
The IBD 101 program boasted a faculty of exceptional expertise and experience. Interaction with Dr. Malter, Dr. Rubin, Dr. Kane, Dr. Regueiro, and many more during IBD 101 course as well as at the IBD 101 reception at the ACG Annual Meeting was amazing and provided me the opportunity to learn from their experience and gather useful tips and tricks. One particular piece of advice that stood out to me was to individualize a treatment plan that best fits the patient based on their disease severity, comorbidities, and preferences. This could be achieved by building a strong provider-patient relationship, and fostering a multidisciplinary approach among gastroenterologists, surgeons, dieticians, primary care, and mental health providers to address all aspects of IBD patient care. In the management of complicated difficult patients, if you don’t know what the next step in the management is, you are not alone. IBD 101 experts across the country are reachable for discussion of your case and guide you by providing their opinion.
4.What advice do you have for first-year fellows who might be considering IBD 101?
For first-year gastroenterology fellows considering IBD 101, I highly recommend seizing this invaluable opportunity. This program offers a comprehensive foundation in IBD, equipping participants with essential knowledge and skills during didactics and round table discussion with IBD experts. By attending IBD 101, fellows can enhance their understanding and management of complex cases. This is a great opportunity for networking with fellows and faculty and to discuss
your difficult cases with IBD experts. The program also offered guidance for fellows who are interested in IBD fellowship and funding opportunities for those who want to pursue their career in clinical or translational research. After attending IBD 101, be prepared to embark on a transformative journey that will positively shape your career in gastroenterology.
5.Anything else to add — insights, gratitudes, “aha” moments?
Attending the IBD 101 program was an enlightening experience that left me with numerous insights and "aha" moments.
I am immensely grateful to ACG, NYU Langone Health, course director Dr. Malter, and the faculty for organizing such a comprehensive and impactful course for first-year gastroenterology fellows. Throughout the program, I developed a deeper appreciation for the challenges faced by IBD experts in managing their difficult patients and for the advice they provided to us from their lifetime experiences. The knowledge gained from IBD 101 has not only broadened my understanding of IBD but also instilled in me a sense of purpose and dedication to making a meaningful difference in the healthcare of my patients. I am truly inspired and motivated to continue my journey in gastroenterology, armed with the valuable lessons learned from IBD 101.

Adam S. Cheifetz, MD, FACG Professor of Medicine, Harvard Medical School; Director, Center for Inflammatory Bowel Disease; Medical Director, Infusion Services; Beth Israel Deaconess Medical Center
It is my pleasure to have been involved with IBD 101 since its inception. It is a wonderful program that allows the fellows to closely interact with faculty from all over the United States. IBD 101 is a fantastic introduction to IBD and the importance of patient interactions and shared decision making. The clinical case simulations are a unique and wonderful part of this program. Watching how faculty are empathetic and how they speak with patients and explain complex
issues is something everyone could benefit from. Though this is great for all first-year fellows, it is a must for anyone considering IBD as a specialty. The interactions with faculty and connections the fellows can make cannot be overstated. I wish they had a program like this when I was a fellow. I would be remiss if I did not recognize what an amazing job Dr. Lisa Malter has done conceptualizing and developing IBD 101. She has really spearheaded this fantastic program.
 Sunanda V. Kane, MD, MSPH, FACG Professor of Medicine, Mayo Clinic Rochester
Sunanda V. Kane, MD, MSPH, FACG Professor of Medicine, Mayo Clinic Rochester
1.What are the two or three most critical benefits from the IBD 101 program and why do they matter for GI fellows?
The strengths of IBD 101 are the ability to learn in small groups from national and international IBD experts, and a full day focused on a single topic designed for the level of a very new GI fellow.
2.IBD 101 has a unique offering with clinical case simulations. What are the benefits and insights for this part of the program?
Many people learn best from a case/ patient. Having actors serve as patients, fellows can learn not only the facts surrounding the clinical situation, but also how to talk to patients about sensitive or complicated topics.
3.What advice do you have for firstyear fellows who might be considering more training in IBD or making this a major focus of their practice?
Take advantage of the exposure to over 20 faculty at your disposal during the day. Fellows can be provided with faculty emails, so reach out! We don’t know if you are interested if you don’t tell us. At the end of the day, Dr. Malter summarizes all the opportunities available to fellows for additional IBD training as well.
4.Anything else to add about the
importance of the IBD 101 experience?
IBD care has become complex, given the number of approved therapies, and the technology available for diagnosis and monitoring. If a fellow does not have adequate exposure to enough patients, there is no way they would feel comfortable or competent in caring for these patients. The feedback we get is tremendously helpful for improving the course every year so that it remains relevant to every fellow regardless of their interest in a future career in IBD or not.
 David H. Hudesman, MD, FACG Professor of Medicine, NYU Grossman School of Medicine; Co-Director, Inflammatory Bowel Disease Center at NYU Langone Health
David H. Hudesman, MD, FACG Professor of Medicine, NYU Grossman School of Medicine; Co-Director, Inflammatory Bowel Disease Center at NYU Langone Health
1. What are the two or three most critical benefits from the IBD 101 program and why do they matter for GI fellows?
As part of IBD 101, first-year fellows are learning from leading experts in the field from across the country, not only in terms of an introduction to IBD diagnosis, treatment, and care – but also in how these specialists interact with their patients. This is a prime opportunity for trainees to learn early in their fellowships about IBD care and even consider whether they may want to subspecialize in IBD down the line. It’s also an excellent opportunity for fellows to network and build relationships with GI leaders and other fellows from across the country, regardless of the area of GI they ultimately choose to pursue.
2. IBD 101 has a unique offering with clinical case simulations. What are the benefits and insights for this part of the program?
With the inclusion of the group objective simulated clinical exams (GOSCEs) as part of the course, fellows can learn not only about IBD management, but also to experience first-hand how GI leaders from around the country interact in a professional, patient-centered manner when discussing IBD care and utilizing shared decision-making with their patients.
3. What advice do you have for first-year fellows who might be considering more training in IBD or making this a major focus of their practice?
The best advice I can give is to ask the IBD specialists at your institution, or even faculty from the IBD 101 course early on, if you can spend time with them in IBD clinic or collaborate with them on IBD research or educational projects.

David T. Rubin, MD, FACG, Joseph B. Kirsner Professor of Medicine; Chief, Section of Gastroenterology, Hepatology and Nutrition, University of Chicago Medicine
1. What are the two or three most critical benefits from the IBD 101 program and why do they matter for GI fellows?
IBD as a subspecialty has made tremendous progress in management goals and treatment options, but with this progress has come increasing complexity and challenges to keep up with. The IBD 101 program provides first-year fellows with solid fundamentals and a foundation for their ongoing learning about IBD through their fellowship.
2. IBD 101 has a unique offering with clinical case simulations. What are the benefits and insights for this part of the program?
The point of IBD 101 is to teach clinical care and the approach to this wonderful and challenging patient population. Case presentations are the best way to engage clinical thinking and cement new learning.
3. What advice do you have for first-year fellows who might be considering more training in IBD or making this a major focus of their practice?
This program will introduce fellows to the field, but also introduce them to many faculty members who are, to a person, willing and able to mentor and welcome them to learn and even visit their programs.

Adam S. Cheifetz, MD, FACG Professor of Medicine, Harvard Medical School; Director, Center for Inflammatory Bowel Disease; Medical Director, Infusion Services; Beth Israel Deaconess Medical Center

Sunanda V. Kane, MD, MSPH, FACG Professor of Medicine, Mayo Clinic Rochester

David H. Hudesman, MD, FACG Professor of Medicine, NYU Grossman School of Medicine; Co-Director, Inflammatory Bowel Disease Center at NYU Langone Health
David T. Rubin, MD, FACG
Joseph B. Kirsner Professor of Medicine; Chief, Section of Gastroenterology, Hepatology and Nutrition, University of Chicago Medicine

Katie A. Dunleavy, MB BCh BAO Gastroenterology Fellow, Mayo Clinic, Rochester, MN

Omar Jamil, MD Gastroenterology Fellow, University of Chicago

Megan Murphy, MD Assistant Professor of Medicine, Johns Hopkins Medicine, Sibley Memorial Hospital

Siri A. Urquhart, MD Gastroenterology Fellow, Mayo Clinic, Rochester, Minnesota

Muhammad Nadeem Yousaf, MD Gastroenterology Fellow, University of Missouri
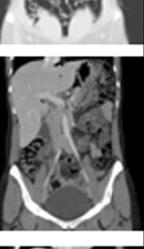


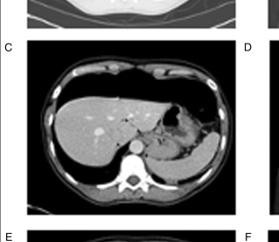

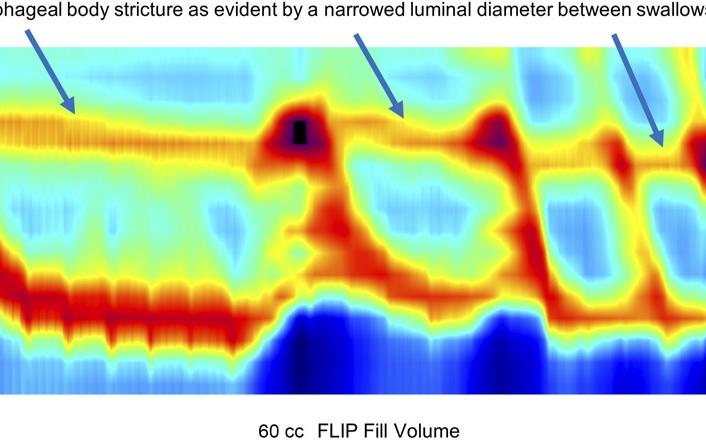

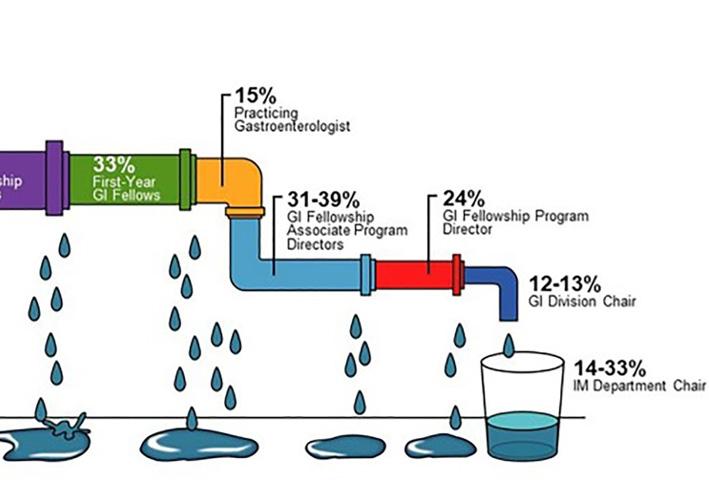
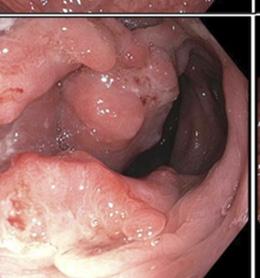





THE NEW ACG CLINICAL GUIDELINE on Alcohol-Associated Liver Disease by Jophlin and Singal, et al., in the January 2024 issue of The American Journal of Gastroenterology covers the diagnosis and treatment of alcohol use disorder as well as the management of alcohol-associated liver disease, alcohol-associated hepatitis, and considerations for liver transplantation.


For a special issue of the Red Journal slated to publish this fall, Co-EICs Dr. Jasmohan Bajaj and Dr. Millie Long have issued a call for papers that contribute to advancing understanding of inflammation’s role in digestive health and pave the way for improved clinical practice. The deadline is July 1st.
The pages of Clinical and Translational Gastroenterology include reports of results from the Prospective Real-World Tofacitinib Response in Ulcerative Colitis (TOUR) Registry by Herfarth, et al
To bee or not to bee, that is the question raised by an unusual endoscopic finding in ACG Case Reports Journal
Loretta L. Jophlin, MD, PhD*; Ashwani K. Singal, MD, MS, FACG*; Ramon Bataller, MD, PhD, FACG; Robert J. Wong, MD, MS, FACG; Bryan G. Sauer, MD, MSc, FACG; Norah A. Terrault, MD, MPH, FACG; Vijay H. Shah, MD, FACG. The American Journal of Gastroenterology 119(1):p 30-54, January 2024. | DOI: 10.14309/ajg.0000000000002572

New ACG guidelines on the management of patients with alcoholassociated liver disease (ALD) include a review of epidemiology, risk factors, diagnosis and management, and policy and prevention. The authors offer evidencebased recommendations on pharmacotherapy for alcohol use disorder (AUD) including baclofen, acamprosate, naltrexone, gabapentin and topiramate. They recommend integrated multidisciplinary care models that incorporate behavioral interventions and/or pharmacotherapy for those with ALD and AUD. The guidelines review referral for liver transplantation, when appropriate.
READ: bit.ly/AJG-EtOH-Guideline
LISTEN: bit.ly/ajg-podcast-vijay-shah
The American Journal of Gastroenterology seeks papers which critically examine the role of inflammation in various digestive disorders, providing insights into the challenges faced by clinicians from diagnosis to treatment.
DEADLINE: JULY 1, 2024
LEARN MORE: gi.org/call-for-papers
Muhammad Nadeem Yousaf, MD & Matthew L. Bechtold, MD, FACG. ACG Case Reports Journal 11(2):p e01260, February 2024. | DOI: 10.14309/crj.0000000000001260
A 78-year-old man was referred for a screening colonoscopy by his primary care physician. In addition to a 7mm polyp in the cecum, the authors discovered a honeybee in the descending colon. Despite upper GI enzymes, a clear liquid diet, and bowel preparation, the honeybee remained intact. The patient reported that he likely swallowed the bee while biking and eating grapes before beginning his bowel prep.
READ bit.ly/acgcrj-colon-honeybee
Hans H. Herfarth, MD, PhD, FACG; Anita Afzali, MD, MPH, MHCM, FACG; Monika Fischer, MD, MS, FACG; David P. Hudesman, MD, FACG; Maisa Abdalla, MD, MPH; Robert McCabe, MD; Benjamin L. Cohen, MD; Ryan C. Ungaro, MD, MS; Will Harlan, MD; John Hanson, MD; Gauree G. Konijeti, MD, MPH, FACG; Steven Polyak, MD; Timothy Ritter, MD; Bruce Salzberg, MD, FACG; Jennifer Seminerio, MD; Emily English, BA, MSW; Xian Zhang, PhD; Millie D. Long, MD, MPH, FACG. Clinical and Translational Gastroenterology, December 22, 2023. DOI: 10.14309/ctg.0000000000000669
The authors assessed patient-reported outcomes (PROs) and predictors of success during tofacitinib maintenance therapy. TOUR included 103 patients with refractory ulcerative colitis (UC); 67% had failed ≥ 2 biologics. Of 103 patients, 82.5% entered the maintenance phase and 43.7% remained on tofacitinib at week 52. Tofacitinib de-escalation to 5 mg BID occurred in 15% of patients. At week 52, 42.7% and 31.1% of all patients reported a simple clinical colitis activity index (SCCAI) <5 and SCCAI ≤2, respectively. Normalization of bowel frequency, rectal bleeding, and urgency occurred in 79%, 61%, and 48% of patients remaining on maintenance therapy. Social satisfaction improved significantly (p<0.001), while anxiety and depression scores only numerically improved. No consistent predictors for tofacitinib long-term treatment efficacy were identified, and safety findings were consistent with the known safety profile of tofacitinib.
READ bit.ly/bit.ly/ctg-TOUR-registry


Clinical take-aways and evidence-based summaries of articles in GI, Hepatology & Endoscopy.
EVIDENCE-BASED GI (EBGI) evaluates new research articles published across leading general medicine, GI and Hepatology journals.
ACG Editors identify the highest quality studies published on important topics and create structured abstracts summarizing the study for quick reference and provide commentary on how the data is applicable to clinical practice.
Editors record audio summaries for easy listening on the go.
EBGI on Twitter for weekly tweetorials @ACG_EBGI













What is Alcohol-Associated Liver Disease (ALD)?
ALD is a liver disease in which your liver is damaged due to heavy alcohol use, and the liver is unable to completely perform its functions. ALD is one of the main causes of chronic liver disease worldwide and is the leading cause of preventable liver-related death in the United States.
What does your liver do?
Your liver filters your blood and breaks down, balances, and creates nutrients you need. The liver helps to digest food, remove harmful or unneeded parts of what you consume, and make clotting factors that keep your blood flowing well. It also processes several prescription and over-the-counter medications.
Alcohol Use Disorder –Alcohol-associated liver disease is most often related to alcohol use disorder (AUD), harmful drinking which negatively affects your health and often your personal and/or work life.
Over the last 10 years, alcohol use has increased in the United States, especially among younger adults, women, and minorities. Stress, anxiety, and isolation from the COVID-19 pandemic made this problem worse.
WOMEN: 2 OR MORE drinks per day or 14 OR MORE drinks per week
Stages of ALD – Excessive alcohol consumption can contribute to three stages of liver disease:
• Fatty/steatotic liver disease,
• alcohol-related hepatitis, and
• cirrhosis (severe scarring of the liver)
In serious cases, the damage to your liver may be too severe and you may need a liver transplant.
MEN: 3 OR MORE drinks per day or 21 OR MORE drinks per week
ALD is Preventable – The most effective way to prevent ALD is to stop drinking entirely. Reducing your alcohol use can also lower your risk for developing ALD. Some people who drink heavily may need medical assistance with stopping alcohol use because suddenly stopping can cause severe withdrawal symptoms such as seizures or death.
• Your doctor can help you find a counselor and there are behavioral therapies and medications that may help you reduce your drinking or stop entirely (baclofen, acamprosate, naltrexone, gabapentin or topiramate).
• You can seek help from your gastroenterologist, primary care physician, or a therapist as a first step.
• People with obesity, diabetes, hepatitis C, or hepatitis B should avoid alcohol.
• Heavy alcohol users should abstain from tobacco because it can increase the risk of cirrhosis.
• People who drink heavily should seek medical care for stopping drinking.

Learn from successful GI innovators and unpack learnings and pitfalls
Demystify the process of developing new technology
Explore ideas and apply the innovator’s mindset to your everyday practice


