doctor doctor








KATE BENSON
It’s been a challenging and heartbreaking start to 2025 in health.

Public hospitals are struggling with inadequate budgets, and exhausted health workers are being forced to do more with less. Demand for services is only growing while staffing levels are constrained to 2018 levels.
The crisis in public psychiatry has been deeply distressing for doctors, highly vulnerable patients and their loved ones, and has caused a level of despair and consternation not seen in this state in decades.
Marshmallow-gate created an inferno of fury among junior doctors, while health staff across the board were left reeling at the antisemitic behaviour of two nurses –originally purporting to be doctors - at Bankstown Hospital.
I’m pleased to say AMA (NSW) got out on the front foot fast and publicly took a strong stand against these issues.
Backed by the board and council, president Dr Kathryn Austin and vice president Dr Fred Betros spoke vehemently against the devaluation and disrespect of medical professionals, and the disturbing damage to

The Australian Medical Association (NSW) Limited
ACN 000 001 614
STREETADDRESS
69 Christie Street
ST LEONARDS NSW 2065
MAILINGADDRESS
PO Box 121, ST LEONARDS NSW 1590 Telephone (02) 9439 8822
Outside Sydney Telephone 1800 813 423
Email magazine@amansw.com.au members@amansw.com.au www.amansw.com.au
The NSW Doctor is the quarterly publication of the Australian Medical Association (NSW) Limited.
all in the health system created by hate-fuelled rhetoric.
There is still much work to be done in these areas, but, as always, AMA (NSW) is taking it on through expert advocacy, lobbying, networking and a collaborative, forward-thinking approach.
In this edition, we showcase the excellent work done by AMA (NSW) on increasing access to safe, free abortion care across the state and we feature four fresh-faced interns embarking on their careers in NSW hospitals.
We cover the debate over health checks for doctors aged over 70 and we celebrate the importance of rural health.
We also feature opinion pieces from Dr Kean-Seng Lim on why we should be investing in general practice and championing the importance of primary care, and JMO Devin Deo channels Bob Dylan to call for change for his colleagues.
Thanks for reading. www.facebook.com/amansw magazine@amansw.com.au
Views expressed by contributors to The NSW Doctor and advertisements appearing in The NSW Doctor are not necessarily endorsed by the Australian Medical Association (NSW) Limited. No responsibility is accepted by the Australian Medical Association (NSW) Limited, the editors or the printers for the accuracy of the information contained in the text and advertisements in The NSW Doctor. The acceptance of advertising in AMA (NSW) publications, digital, or social channels or sponsorship of AMA (NSW) events does not in any way indicate or imply endorsement by the AMA.
AMA(NSW)BOARD
Dr Kathryn Austin, President
Dr Fred Betros, Vice President
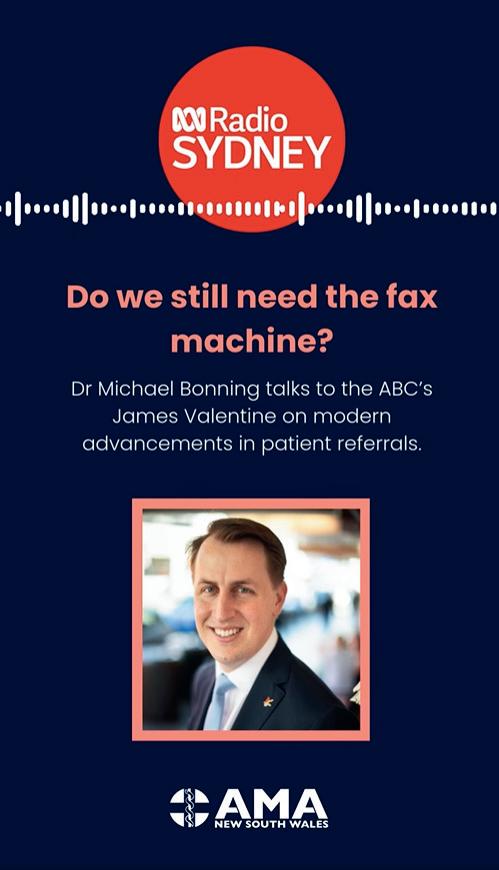
Dr Michael Bonning
Dr Costa Boyages
Dr Brian Fernandes
Dr Amandeep Hansra
Dr Jacqueline Ho
Dr Theresa Ly
Dr David Malouf
SECRETARIAT
Chief Executive Officer, FionaDavies Director, Workplace Relations DominiqueEgan Director, Membership Engagement and Commercial Partnerships GaryWhite
Editor
Kate Benson kate.benson@amansw.com.au
StaffWriters
Ally Chandler
Ally.chandler@amansw.com.au
Isabella Angeli Isabella.angeli@amansw.com.au
Design
Design Bees
Advertisingenquiries
Ally Chandler ally.chandler@amansw.com.au
I sincerely hope all our members were able to take some time to rest, reflect and connect with loved ones over the Christmas/New Year period.

It is an incredible honour and a privilege to be a doctor, but often, medicine takes us away from our family and friends for life’s important occasions. Taking time to recalibrate and make memories with those we value is vital to delivering good patient care. As they say, you cannot pour from an empty cup.
This year has started with the heartbreaking mass resignation of psychiatrists working in the public system. And we have had junior medical officers expressing grave concern over an email labelling them as “marshmallows”.
Both are the result of an underfunded, under-resourced health system forcing everyone to do more with less. We will continue fighting for increased funding and staffing to ensure all health staff are supported in the incredible work they do.
In recent weeks, we launched our VMO survey, run by ORIMA Research, to canvass the views of Visiting Medical Officers working in public hospitals.
The survey results will be used as evidence when we go to arbitration this year and I look forward to effecting real change for VMOs – and ultimately all doctors – by ensuring working conditions are updated for the first time in any meaningful way since 2007.
Last year was fruitful and exciting for AMA (NSW) and I am proud that we achieved so much for our members and the generations of doctors to come.
We made a pre-budget submission to NSW Treasury, focusing on budget and activity levels of local health districts, and funding modern workplace arrangements.
We also developed a model of care that can deliver safe, equitable and free abortion services in public hospitals and primary care, and we were proud to be the first state to provide legislated relief for GPs from payroll tax.
In our meetings with the Minister and Shadow Minister, we highlighted the value of investment in general practice because we understand the power of a robust primary care system, and the pressure it alleviates across our public hospitals.
With our private health system in crisis, we supported Federal AMA’s long-standing call for a new independent authority to oversee private healthcare and this will remain one of our highest priorities.
Not surprisingly, a special highlight for me last year was the NSW Legislative Council Select Committee on Birth Trauma as it gave us the opportunity to advise on ways physical and psychological trauma can be eliminated or reduced for women in labour, and how we can support mothers, their families and those working within the system to ensure our workforce remains stable and committed to delivering excellent care.

Thank you for your ongoing support and engagement. I look forward to a very fruitful 2025.

Over the past few months, there has been a growing sense of despair from those working in our health system in NSW.
The despair is manifesting in doctors walking away, in the frustrations being ventilated in the media and online and in the discussions we are having at AMA (NSW) over and over again.
While it is most prevalent for those working in the public hospital system, it is coming across from those in general practice and other specialities, from rural doctors to city practices.
The challenges are evident. Insufficient budgets in our public hospitals, escalating burdens of disease leaving patients older and sicker than ever before. The long term underfunding of general practice making it harder and harder to provide quality care without increasing gaps. A fear about the medico-legal environment and the raising pressure on indemnity.
For those working in our public hospitals, particularly our doctors in training, the grinding despair of an award that is generations out of date. For our public sector psychiatrists, watching in their under-resourced hospitals as the sickest and most marginalised patients are forgotten.
It feels like the words of 2025 are despair and outrage.
Despair and outrage are understandable words and understandable feelings. I have seen a lot of it in my many years with AMA (NSW).
It was only a few short decades ago that NSW Health was overwhelmed with a similar sense of outrage and despair. In the early 2000s, our hospitals were in crisis. Not a day went by without a crisis headline. Doctors and nurses were spat on and abused by patients. A major medical indemnity provider went into administration and doctors
had to pay an additional year of premium. There was inquiry after inquiry, the Walker Inquiry, the Royal North Shore Inquiry, the Garling Inquiry and so on. A lack of investment in health was a key driver for so many of our crisis issues, something which feels remarkably relevant today.
None of this reminiscing is intending to be a “back in my day”.
As I was observing to AMA (NSW) council recently, things are as bad now as I have ever seen. However, I also do not want despair and outrage to feel like powerlessness because powerlessness is the worst feeling of all.
As we celebrate the 145th birthday of AMA (NSW), I would like to encourage everyone to focus on action, on the incredible work which has delivered us this health system and the work we are all doing at AMA (NSW) to support doctors and patients. The work of fighting for health is not easy. It takes skill, patience and most of all hard work. It is uncertain and not always fair. However, in representing doctors, we represent the hardest working, most expert profession so we know we are up to the task.
fiona.davies@amansw.com.au
www.facebook.com/amansw

The NSW health system is in a state of despair not seen in decades. Doctors are walking away; industrial unrest abounds and patients are the collateral damage. How did we get here and how do we revive a dying health service?

Devastating.Deadly. Heartbreaking.
These are some of the words used to describe the ongoing crisis in public psychiatry, a shocking impasse which has left doctors reeling and thousands of vulnerable patients facing uncertainty.
The stand-off will now go to the Industrial Relations Commission, but the distrust between doctors and the NSW Government may never be repaired.
This month, junior doctors also
expressed outrage over an email inadvertently sent from an administrator likening them to marshmallows for allegedly choosing life over work.
And, doctors across the public hospital system have reported being ordered by local health district managers to work to 2018 budget and staffing levels, despite demands for services soaring in the past seven years.
These are all by-products of a health system under enormous budgetary strain; an exhausted and stressed workforce and an alarming
“This damaging rhetoric and devaluation of medical professionals must cease.” Dr Fred Betros, vice president, AMA (NSW).
devaluation of the medical profession.
As we know, the 2024-25 health budget was a serious blow to the state’s ailing system.
While the NSW Government announced areas of investment,
“I am concerned about NSW losing its appeal for medical professionals. When politics filters through clinical autonomy and governance, it deters employees.” Specialist.
there was failure to deliver resources to fix the most significant holes in the NSW health system.
Demand for services is only growing, as supported by data from the Bureau of Health Information, which showed presentations to emergency departments across NSW reached 787,590 between July and September this year - a 2.1 per cent increase on the same quarter last year, with triage 2 and 3 presentations the highest of any quarter since the BHI began reporting in 2010.
AMA (NSW) also expressed concern that during this reporting period 67,737 people left an emergency department before treatment began or was completed - up 9.8 per cent on the same quarter a year earlier.

This is yet more evidence of an exhausted system unable to meet the needs of its patients.
The budget also failed to address critical issues around conditions for doctors working in public hospitals. NSW doctors are now among the lowest paid in Australia, with little done to attract and retain them, particularly given incentives offered by other states.
Rural and regional communities have also been let down with limited support for already stretched local health district health budgets and no effective incentives to retain doctors in these regions.
“The healthcare system in NSW has earned consistent recognition as one of the top-performing in Australia, largely due to the commitment and skill of doctors and healthcare professionals working to support it ”says AMA (NSW) president Dr Kathryn Austin.
“It feels like we’ve been demoted; we are different to ‘health’; we are speaking to someone with less power.” Psychiatrist.
“Yet, despite its many strengths, the system faces the very real risk of losing its status unless efforts to recruit and retain medical staff are strengthened.”
According to the Australian Bureau of Statistics, the population of NSW stood at a little over 8 million 2021. By 2023, HealthStats NSW estimated it had grown to 8.2 million, and by 2043, it is expected to hit more than 10 million.
Yet, the NSW Health budget increased by 0.8 per cent in 2023 and 2.97 per cent in 2024 – against a backdrop of 5 per cent inflation.
Demand for services is soaring with no relief in sight.
“The current NSW Health budget is not sufficient, resulting in frustrated and stressed staff trying to do more with less.” Dr Kathryn Austin, AMA (NSW) president.
In the period between April and June last year, there were almost 800,000 attendances to emergency departments across the state – up more than 25,000 from the same quarter in 2023. And many were very ill, with those in triage categories one, two and three at the highest level since the BHI started reporting in 2010.
Anecdotal reports suggest most local health districts in NSW are running between $6 million and $200 million over budget, while an announcement in December stated more than 400 jobs would be axed at Sydney Local Health District alone.
“We’ve had reports from a staff specialist who spent four hours of his time trying to purchase a whiteboard because he has no admin staff to assist and had to complete a learning module before being allowed to make a purchase, ”Dr Austin said.
“In the end, he was told the hospital couldn’t afford the whiteboard. His time would have cost them about $600 with no outcome.”
This year, AMA (NSW) will go to arbitration to modernise conditions for Visiting Medical Officers, creating a fairer playing field for doctors wanting to work in NSW.
“We are seeing a real devaluation of doctors across NSW – both in terms of their pay and conditions, and in their treatment by the NSW Government – and this is highly concerning,” Dr Austin said.
“Doctors dedicate many years of their lives training and skilling up to care for others. They bring a level expertise to the health system which cannot be replaced by other health practitioners.
AMA (NSW) is calling on the NSW government to ensure the 2025-26 health budget matches or exceeds health inflation and can meet Federal Government activity

“We also want a focus on funding remuneration increases and improved conditions. It is time doctors were appropriately valued for the incredible work they do.”
"We're fed up because when we talk to our interstate colleagues and we say we work in NSW, they say, 'I'm so sorry.'” Emergency medicine doctor.
In an age where online reviews influence public perception, doctors must carefully navigate both negative and positive feedback.
Doctors have professional obligations which must guide how and when they engage with a review, be the review positive or negative.
acknowledged promptly, even if a substantive response cannot be immediately provided. Ensuring a patient’s concerns are heard can reduce the risk of a negative online review.

When a patient posts a negative review, it’s important to consider the pros and cons of engaging, particularly if you engage online. Sometimes engaging may only escalate an issue, even where you do so with the best of intentions.
While it is human nature for us to concentrate on the negative, always remember that for each negative review there are often many more positive reviews. It is not possible to eliminate the possibility of negative reviews, but you can ensure that if a patient raises a concern with the practice, the concern is at least
If a review raises concerns, whether clinical or non-clinical, you may wish to respond. Remember that your professional responsibilities extend to your online presence. Ensure your responses are respectful, considerate, and in line with the Medical Board’s Code of Conduct and the privacy legislation. If you are unsure of how or if you should respond, contact the AMA (NSW) Workplace Relations team.
If you choose to respond to a negative review, ensure you do so carefully. If you do wish to respond
to a clinical review do so off-line. Remember, even if the author of the review identified themselves as a patient, you must not breach their privacy and confidentiality by confirming that they attended your

practice and sought treatment or advice.
When responding to the negative clinical review, you should respond in the same manner as you would if responding to a com-plaint made to the practice or a regulatory body. AMA(NSW) recommends that you seek advice before sending your response from your professional association or medical defence organisation.
If the review concerns non-clinical issues, such as waiting times, customer service, or administrative processes, a brief, professional response may be effective. You may choose to respond online and respond with a simple comment, for example:
“Thankyouforyourfeedback.We arecommittedtoimprovingthe patientexperienceandhave takenyourcommentsinto consideration”.
Alternatively, there is no obligation to respond and you may choose not to do so.
Certain public review platforms prohibit hate speech, abusive language and defamatory comments. If you receive a review that violates the rules of engagement of the platform, you may request that the review be removed. Be sure to check the platforms’ specific policies for reporting inappropriate content before making a request.
There may be some reviews that give rise to defamatory imputations. Defamation law is a very technical area of the law, and if action is being considered, advice should be sought from a lawyer with expertise in defamation law.
Reviews about clinical care, treatment effectiveness or medical outcomes must not be solicited. Additionally, doctors are prohibited from offering rewards or incentive like discounts or preferential treatment in exchange for positive reviews.
Doctors can invite patients to leave a review online relating to nonclinical matters only, such as the patient’s experience at the practice. The invitation for a review must be made in a neutral and non-coercive manner and patients should never feel pressured or expected to leave a positive (or negative) review.
Usingpositivereviewsin advertising
While positive reviews can be beneficial for your reputation and that of the practice, you must be careful when it comes to sharing them publicly to advertise your services.
Under the Health Practitioner Regulation National Law, you are prohibited from using testimonials that discuss the clinical services. A testimonial is any review that includes comments about your skills, diagnosis, treatment, or patient outcomes. This means that even positive feedback

related to clinical care cannot be shared on your website or your social media platforms.
You should ensure that your social media accounts, and website (if there is provision for reviews to be left) are regularly reviewed and any reviews that may contravene advertising laws are removed. You are not responsible for what is posted on third party sites and accounts, but you are responsible for what is posted on your site and accounts.
Non-clinical reviews, such as those commenting on the friendliness of your staff, the efficiency of your practice, or the
overall patient experience, may be left on your website or social media platforms.
Editing a patient review has the potential to be misleading and/or deceptive as doing so means it may no longer accurately reflect the patient’s feedback and would breach the advertising requirements of the Health Practitioner Regulation National Law.
If you decide to invite patients to leave reviews, ensure you do so in line with your professional standards.
Ifyouneedassistancein managingeithernegative orpositivereviewsonline, contacttheAMA(NSW) WorkplaceRelationsteam forspecificadvice.Youcan contactourteamon(02) 94398822orvia
workplace@amansw.com. au


Addressing psychosocial hazards in medical practices is important as it can impact the wellbeing of your employees and the quality of care provided to patients. It can also result in employee absenteeism, staff turnover and declining performance.

Statistics from Safe Work Australia reveal a significant rise in psychological injuries related to workers' compensation claims, with a 36.9 per cent increase from 2017-18 to 2021-22. This highlights the growing importance for employers to effectively manage these risks.
The Work Health and Safety laws requires employers to eliminate or minimise workplace psychosocial risks as far as reasonably possible.
Whatarepsychosocial hazards?
Psychosocial hazards are defined by Safe Work Australia as being “from or in relation to the design or management of work, the working environment, or workplace interactions that may cause psychological or physical harm”.
These can include (but are not limited to):
Harmful behaviours such as bullying or sexual harassment. Low job control where workers have little say on how and when the work is performed.
Job demands that are either high or low and can be physical, mental or emotional.
Lack of role clarity.
Poor change management practices.
Inadequate reward and recognition.
Implementing internal policies and displaying signs in the practice that make it clear unlawful behaviours, such as bullying or sexual harassment by employers, employees or patients, will not be tolerated can help create a safer environment by setting clear expectations for both staff and patients.

Engaging with employees about any challenges they face in their roles in regular catchups, while offering them autonomy in managing their workflows and flexibility in processes, can foster a sense of control.
Providing support such as backfilling roles when an employee (such as a receptionist or nurse) is on extended leave and having appropriate systems and processes in place for employees to complete the required tasks can help to alleviate any added pressure in their roles.
Up-to-date position descriptions clarify role expectations and establish clear reporting lines. Providing clear instructions for new tasks and communicating priorities can further enhance job clarity and increase engagement.
Involving employees in change management processes by seeking their input on organisational or role changes that may impact them can help reduce fear and uncertainty through open and consistent communication.
Acknowledge and reward achievements in a way that resonates with the employee, ensuring recognition of both individual and team contributions for positive performance. This can be achieved by simply discussing with the employee whether they prefer recognition to be private or public for example, while also considering their personality. Providing mental health support and resources to employees, including employee assistance programs, counselling services, and training to management staff members to recognise psychosocial hazards will help reduce the risk of mental health issues eventuating or escalating.
Psychosocial risk management should be an ongoing process, and the practice should continuously assess the effectiveness of the measures in place.
Employers are required to consult employees on decisions that may affect their safety. This can serve as an effective way to gather valuable insights, as they bring knowledge and experience from both their role and the wider team.
AMA (NSW) can provide policy templates and help assist you in your understanding your employer obligations regarding providing a safe work environment.
JoanneChoo.
TheAMA(NSW)WorkplaceRelations teamcanprovidesupportonmanaging employeeswithmaybeimpactedby psychosocialhazardsandotherpeople managementmatterswithtailored adviceandtemplates.Pleaseemail workplace@amansw.com.auorcall (02)94398822forassistance.
Abortion was decriminalised in NSW five years ago, but equitable access to safe, free, timely care remains challenging for so many women across the state. AMA (NSW) has developed a model of care to change this.

For so many at the Parliament House funding call for abortion services to be embedded across NSW public hospitals, it was deeply personal.
For Independent MP Alex Greenwich, who spearheaded the decriminalisation of abortion in the NSW parliament five years ago, it was his grandmother’s letters to former US president George H. Bush pleading for women to have the right to choose.
For Jozefa Sobski, from the Women’s Electoral Lobby, it was the abortion she underwent frightened and alone in a Sydney apartment at the age of 21, coupled with distressing stories from her mother of terrified women seeking pregnancy terminations in German labour camps during the war.
And for AMA (NSW) councillor and obstetrician Dr Felicity Park, it was the teenage refugee who fell pregnant
after a sexual assault and desperately wanted a termination so she could complete her high school education and choose her future path in a new country.
Thanks to a decades-long campaign by so many people across NSW, abortion is no longer a criminal offence in this state, but equitable access to this vital healthcare service is still not widely available.

AMA (NSW) has worked with Family Planning Australia to develop a model where additional funding and resources would be provided to existing maternity and gynaecology services to embed termination of pregnancy care within existing service pathways.
Based on a similar successful program in Hunter New England Local Health District, it would utilise existing multi-disciplinary teams of doctors, nurses, midwives, psychologists and social workers, requiring modest funding from local health district budgets.
This model demonstrates the importance of embedding abortion services into routine healthcare pathways. This not only builds capacity but places abortion services as routine reproductive healthcare.
Greens MP and former regional GP, Dr Amanda Cohn, has introduced a private members’ bill calling for abortion law reforms. It focuses on obliging local health districts to ensure abortion services are provided to public patients; allowing nurse practitioners and midwives to prescribe medical abortions;
removing mandatory reporting requirements for providers; and requiring practitioners with a conscientious objection to refer patients on.
AMA (NSW) is opposed to the provisions in the Cohn Bill related to seeking to force doctors to be involved in abortion care.
President Dr Kathryn Austin said the Bill would potentially undermine the work AMA (NSW) and Family Planning Australia have done to develop a comprehensive clinical model which focuses on both primary and tertiary level care access. The focus should be on enabling those who require this form of reproductive care equitable access, not mandating all doctors provide the service.


Last year, the Medical Board of Australia caused a stir with the announcement that it was considering introducing mandatory health checks for doctors over the age of 70.
Dr Anne Tonkin, the Board’s chair, explained the motivation behind this proposal, stating:
“We are looking for effective and practical ways to support latecareer doctors in staying in safe practice, through health checks that will identify and enable doctors to address any risks that come with increasing age.”
At the heart of the proposal was a request for feedback from the medical community and the public as to which of the following three options would be the most appropriate in supporting late career medical practitioners;
Those options were: Keep the status quo and do nothing extra to ensure late career doctors are healthy and able to provide safe care;
The Board’s preference leans towards option 3, proposing that doctors between the ages of 70 and 80 undergo health checks every three years, with annual checks for those over 80.
Feedback was open for submission until early October and is currently under review.
At the time of announcement, AMA federal president Dr Danielle McMullen said to the Medical Republic:
3.
1. Introduce an extensive and detailed ‘fitness to practise’ assessment for all doctors aged 70 and older, to be conducted by specialist occupational physicians, or; 2. Introduce general health checks with a GP for late career doctors aged 70 and older, to support early detection of concerns with the opportunity for management before the public is at risk.
The proposal was sparked by data from the Australian Health Practitioner Regulation Agency which showed that doctors over 70 are 81 per cent more likely to be the subject of complaints, regardless of impairment.
“What we don’t support are processes that resemble revalidation or mandatory retirement of older doctors, nor do we support a complex fitness for practice assessment’’.
In September, AMA (NSW) sought feedback from its members regarding the proposed health checks.
The most common concerns voiced by members were:
Ageismanddiscrimination: Many feel the proposal unfairly targeted older doctors.
Exploitationofthemedical profession:
There were comparisons made to other professions, such as public servants, who are not subject to similar health check requirements.
One member wrote: “I think it is outrageous (and) offensive in the extreme and represents (and is) yet another aspect of medical regulatory bodies effectively attempting to subjugate (thus far too successfully) the medical profession”.
AMAstandpointandadvocacy:
For more than a decade, the AMA has been engaged in significant policy discussions regarding this issue. In 2017, the AMA worked closely with the Board and the Expert Advisory Group (EAG) to champion a process that respects the contributions of late-career doctors.
The AMA firmly supports doctors remaining in practice beyond the age of 70. The introduction of mandatory health checks for late career doctors, however, could create a major disincentive for them to continue working, potentially depriving patients of experienced healthcare providers and preventing younger doctors from accessing valuable mentors.
The AMA’s advocacy aligns with the Board’s preferred option, option 3, which calls for regular health checks. However, the AMA emphasises that the focus should be on supporting doctors who wish to continue practising, rather than penalising them for their age. This support, the AMA argues, should include significant engagement with the profession, as well as education and resources for doctors to manage their health and wellbeing.
It is essential to recognise that doctors who continue to practice beyond the age of 70 often do so
with considerable skill and judgment, adjusting their scope of practice, workload, and procedures to mitigate risks. The AMA urges the Board to acknowledge the autonomy and value of these doctors, while also ensuring patient safety.
The AMA supports regular health checks for all doctors and initiatives such as the “I Have a GP” project, which highlights the importance of every doctor having access to their own healthcare provider.
Throughout this consultation process, the AMA advocates for the Board to prioritise practitioner wellbeing in decision-making.
While the AMA recognises the Board’s concerns, the feedback from members is clear: any introduction of mandatory health checks must be structured to support, rather than penalise, late-career doctors.
The AMA recommends that the Board refine its proposal to have doctors undergo health checks with their own general practitioners, a model that would underscore the objective of safeguarding the doctor’s health and wellbeing, rather than enforcing a bureaucratic process.

Medical Board can be accessed through the following QR code.
https://www.ama.com.au/articles/ ama-submission-medical-boardconsultation-health-checks-latecareer-doctors
In a discussion with the Medical Republic, AMA federal vicepresident Professor Julian Rait said:
“Generously, many older doctors returned or at least deferred retirement [during Covid], much to the gratitude of the country and the community, and now that gratitude seems to have waned.
To that end, the association has questioned the Board on whether its proposals represent a form of ageism.We’re concerned, as I’m sure many older doctors are, about whether this might cross a line into age discrimination, and we’ve encouraged the board to seek legal advice and explain whether or not some of their models might be a form of discrimination”.
AMA (NSW) will continue to update its membership as this process progresses. But it is clear, any introduction of mandatory health checks must reflect balance to avoid alienating an experienced and valuable portion of the medical workforce.
IsabellaAngeli
We’re committed to helping advance our members in private practice, whether they are established or just starting out. In this edition, we highlight Dr Rebekah Hoffman, a general practitioner from Sydney’s Sutherland Shire. Dr Hoffman purchased a practice in Kirrawee in 1994 and last year expanded to Woolooware.
Canyoutellmeaboutstarting fromscratchinWoolooware?
We decided to branch out to Woolooware because the majority of our patients were travelling to see us from this postcode. We had the lovely problem of having lots of GPs that wanted to work with us and having no more space for them, no more rooms to put them in. So, we decided we’d be better off expanding. A site came up that we were interested in and we went for it. The building was previously a chiropractor, and it was already DA approved for health services which meant we didn’t have to go through council again, and that was a really attractive option.
Whatwouldyousaythe biggestchallengeinstarting fromscratch?
It was something that I’d never had to do before. I’m not a builder, electrician, accountant or a handy technician at all. GPs are exceptionally good at multi-tasking, however, this was a completely different process. I am completely capable of managing patients’ problems and medical diagnoses, but having to juggle finances around what ended up being an almost completely new build was a lot.
Areyouabletocomparethe challengesyouexperiencedat buyingintoanestablished practiceatKirrawee?
The situations were completely

different. When you buy into an existing practice, you’re buying into all the decisions they have already made with IT, computer software, staffing, contracts and pay. Some of those decisions you agree with and some you wouldn’t have made yourself.
The relationships are important to consider, as well, such as making sure the person you’re buying in with has the same vision and mindset as you. In the first instance, the person I bought in with unfortunately didn’t have the same mindset as me.
That became very difficult, two different people trying to run a business. My current business
partner and I are similar ages, same gender, similar aged kids and we are much alike in our values and what we want for the business, so that has been an easier ride.
Howhaveyoufoundyour practicesrewarding?
I really get a lot of value out of being a business owner. Yes, it’s about community but for me it’s more about the GPs. I want to run a business where they want to come to work and that I want to work at myself. We’ve all worked at rubbish practices that don’t value the doctors, and that’s not what I wanted. I wanted a practice where people say, “yep I want to work there’’.
Some of my doctors travel a long way to work here. I want them to feel safe, trusted, supported and that’s what we offer. We can offer a flexible, family friendly practice that will hopefully be their forever practice.
Whatwouldyousaytoa doctorstartingtheirown practice?
It depends on what day you talk to me. Some days I would say don’t do it, are you insane, it is so much easier just to find a good practice and be a contractor, and some days that’s true.
But easy is not always fun. The decisions that you make are really
important for how the business is run and structured, and what are seemingly simple decisions can really change outcomes significantly.
The business aspect of the two practices has taught me so much, and seeing the growth and the value of the practice is rewarding as well.
What’ssomethingreally simplethatyou’velearnt inthisprocess?
So much. I outsource everything now. I know I don’t need to be the expert on everything, and it’s ridiculous for me to try. If I can get my accountant to do it I will, if I can get my gardener to do it, I will. I am far more valuable doing the things that I am good at, and you end up saving much more money and getting a better job done if you outsource it.
The other really big one is that you can do it. I bought into my practice when I was 34. It was hard and I was young. I would like to think I’m still young, but there’s no age, gender or personality that can or can’t run what is now a medium to large business. You
j work you don’t have to keep doing it. You can try something else. We’ve tried lots of things and failed

miserably. We stopped and tried something else, and that’s completely fine as well.

When former AMA (NSW) president and dermatologist Saxon Smith was nine, he was writing letters as a “medic from the Western Front” for school history projects.
As a Nipper and young surf lifesaver on the Northern Beaches, he was lathering on sunscreen daily, no matter the season.
And at the age of 14, he declared he would cure skin cancer.
Tragically, Saxon lost his life to sarcoma earlier this year at the age of 47, but his ground-breaking research into sunscreen usage, published in the American Journal of Clinical Dermatology in 2015, has played a pivotal role in educating the public and medical practitioners on ways to prevent his deadly cancer.
Saxon’s research showed that Australia lagged behind many countries, including Switzerland, Austria and Denmark, for sunscreen usage – shocking in a country with the highest skin cancer rates in the world.
His research also showed that many people had no idea sunscreen had an expiry date, that it needed to be stored under 25 degrees to remain effective and that about two tablespoons were required to cover the whole body.
About 17,000 Australians are diagnosed with melanoma every year – that’s one person every 30 minutes. It is the third most commonly diagnosed cancer after prostate and breast, but 90 per cent of melanomas can be cured if treated early.

The co-medical director of the Melanoma Institute of Australia and co-Australian of the Year, Professor Georgina Long, recalls Saxon as an “incredible person and much loved in the medical community”.
“He was a dedicated clinician and was loved by his patients, students and colleagues. He wanted to make a difference, particularly through medical education.”
Professor Long said Saxon’s research ensured that the medical curriculum included educating the next generation of doctors on the causative links between UV and skin cancer.
“He conducted a breadth of research on the topic of prevention, including medical students’ attitude to tanning and sunscreen usage. The latter resulted in an important change in language and targeted education regarding the correct storage and application of sunscreen.”
Late last year, we kicked off a Sun checks for Saxon campaign aimed at reminding the public to check their sunscreen regularly and wear it every day.
“Prevention is better than cure,” says Professor Long.
“UV causes skin cancer, and you can prevent it. Be sun safe – wear a hat, sunglasses and clothes, and put on your sunscreen – properly.”
For Camille and son Elliot, 13, the profound loss of Saxon will be felt forever, but they value keeping his memory alive through his passionate quest of sun safety.
“He would be very pleased with this campaign. He always said we were never designed to live in Australia, but he definitely practised what he preached – rain, hail or shine.”

Our campaign launch in December last year.
Store sunscreen below 25 degrees
Always check expiry dates and discard if out of date. Use two tablespoons to cover your body
More than 1000 medical interns have recently started work in NSW hospitals. We talk to four with big plans for their careers.

Sabrina Bilston-John with partner Byron Northernlightsattract Sabrina Bilston-John has just started her internship at Lismore Hospital but already has plans to buy land in the Northern Rivers of NSW and settle down forever.
Originally from Perth, she completed a degree in biochemistry and was offered a Juris Doctor placement at the University of Western Australia.
While it was tempting, the lure of a practical career involving her passion - science - proved too much so she moved to Sydney to study medicine,
electing to spend the last two years in Lismore.
She’s a long way from home with her parents living in Melbourne and Shanghai, but she’s fortunate to have her partner Byron starting his internship alongside her at the same hospital.
“Thejuniorsarereallywell supportedatourhospital,but thefirstfewweekswillbea hugestepup.It’snoughtto100. Wearethesmartestwehave everbeeninourlives,butwhat ifIamaskedtodosomethingI don’tknowhowtodo?”
Sabrina feels certain surgery and psychiatry are not for her but is prepared to “fullyembrace” each rotation.
“I’mveryopentofindingwhereI fitbest.”
The people of Lismore are still rebuilding their town after catastrophic floods swept through in 2022, but their resilience and community spirt have left a mark on Sabrina.
“Almosteverypatienthasa floodstory.Itispartofwhothey are.Andthisishomeforusnow. Weabsolutelywanttostayin theNorthernRivers.”
Abigail Leeder had an interesting start to her medical career.
The youngest of nine, she attended a small religious school where science was not on the agenda, leading her to an arts degree in policy and Arab/Islamic studies.
That took her into policy roles with the Federal and NSW governments and the RACGP, but after meeting her husband, James, a psychiatry registrar, Abigail decided to take the plunge and study medicine.
Now in her early thirties with a toddler named Matilda, she’s recently started her internship at Royal Prince Alfred Hospital in Camperdown and is hoping she can become “a safe pair of hands” for her colleagues.
“I’mexcitedtobeembeddedina team.Whenyouareastudent, youspenttwotofourweeksin eachplacementsoI’mlooking forwardtofollowingpatients through.”
Abigail took a year off her in the middle of her studies after having Matilda, a move which she says meant she was refreshed and ready to tackle year four – the toughest year of the degree.

Husband James has also been working as a locum to give him more time to be with their baby, and Abigail’s huge family has “an army of involved aunties” who will provide support.
“Thekeyformewillbehonestyin navigatinganydifficulties.Ineed torecognisewhenIneedtolean onthemforsupportbeforeitgets toomuch.”

International student Emily Lee has an ace up her sleeve for her intern year at Wollongong Hospital.
Her boyfriend, Alex, has just finished his internship at the same hospital and will be able to share any “tipsandtricks” she may need.
They met last year and will be living together this year in Wollongong –a move which will provide her with welcome support given her family resides in Malaysia.
She keeps in regular contact with them and has developed a strong social network since moving to Australia in 2017 to study psychological science at university in Adelaide, but “havingapartner whounderstandexactlywhatit’s like” will provide a solid foundation.
“I’mexcitedtopractisemedicine aftersomanyyearsspent watchingothers.ButI’malso worriedaboutmakingsilly mistakesandnotbeinggood enough.I’llberesponsiblefor many,manypatientsonceIstart.”
Emily has no firm plans on a speciality as yet, but palliative care, obstetrics, medical oncology and paediatrics have piqued her interest and she’ll use her intern year to get a “solidfeel”on where she best fits.
She plans on keeping active outside of work and when the stress mounts.
“I’lldebriefwithAlex.AndIcan alwayssitbythebeach.Wollongong hassomanybeautifulbeaches.”
Lookingtothestars
Pravind Easwaran was headed for a career in global health policy when a part-time job in aged care during the pandemic sparked his interest in medicine.
Now, the 25-year-old University of Sydney student has started on the wards of Dubbo Hospital - and is both nervous and excited about the year ahead.
“Everyonesaysthefirsttwoweeks areroughbecauseyouonlyhavea buddyforthefirstweekandyougo fromthelearningstagestraightinto keepingupwiththerestofyourteam. Suddenly,it’sallonyou.”
But Pravind has plenty of strategies in

By Theo Clark
Country doctors can inevitably be more in tune with the seasons than their city counterparts. Up, over and beyond the ranges, the contrasting heat of summer or frosts of winter herald changing rounds of activity in communities dependent on gathering harvests.
Some seasons bring bounty and some seasons bring want, but in recent years there’s been a dependable seasonal event for all rural health professionals to look forward to, regardless of flood, fire or pandemic.
Since 2020, November has been known as ‘Rural Health Month’, an opportunity for a multidisciplinary ‘coming together’ of the rural health community for a series of educational and networking events with a ‘rural positive’ focus.
“2024 is the 5th year of Rural Health Month,” says Rural Doctors Network (RDN) CEO Richard Colbran.
“Back in 2019, RDN conceptualised the development of a celebration for rural health and thought ‘why shouldn’t the month of November be the time to celebrate and think positively about all the great attributes of working and living in rural and remote Australia?’ It’s fantastic to see how many organisations are now supporting and celebrating the idea of Rural Health Month, but also the notion of ‘rural positive’.”
This year, RDN’s Rural Health Month activities began with the hosting of the National Rural and Remote

Health Awards, at the Press Club in Canberra, by Rural Health Pro, a social enterprise of RDN.
The Awards were inaugurated last year but grew out of RDN’s #RuralPositive campaign of the COVID-19 era, which aimed to express gratitude for the service and dedication of rural health professional - the doctors, nurses, allied health workers and organisations who so often embody the best characteristics of service, compassion, innovation and resilience, whether it be serving and learning in remote Aboriginal or Torres Strait Islander communities, working at the cutting edge of technological innovation for long-distance health care provision, or just ‘being there’
in rural and remote communities, helping to build greater access.
This year’s finalists were honoured by the attendance of the GovernorGeneral Sam Mostyn at the Awards.
“Healthcare is so much more than just about treatment. It is education, it's prevention and management, it's project planning and execution, it's communication and collaboration, innovation and so much more," the Governor-General said in her address to finalists at the awards night.
"Yours are not just jobs, but vocations of care. Your work is essential to the wellbeing of all Australians and the prosperity and progress of our nation."
Nominations flowed from all around Australia - from Norfolk Island to WA.
From New South Wales, the Southern NSW Local Health District, Hunter New England Local Health District, Royal Flying Doctor Service South Eastern Section, and Macksville Medical Centre all had representatives honoured with awards on the evening.
“It’s wonderful for that acknowledgement and recognition for our rural, regional and remote areas,” said Casey Shorter, Practice Manager at Macksville Medical Centre, who won the Rising Star in Rural/Remote Health Award.

“It’s a far cry from what is experienced in the city, and it’s nice to have that acknowledgement and understanding from people that don’t quite always experience what we do.”
Later in November, activities shifted to the Manly Pacific Hotel in Sydney for the Rural Allied Health Conference, Rural GPs Conference, Medical Student Rural Inspiration Conference and Rural Practice Managers Conference amongst other events such as the Rural Medical Service Awards.
The presence of 13 veteran doctors attending to receive their 35 years+ long-service awards and mixing with future doctors from the student conference was a poignant highlight
“We gathered for our 36th annual Rural GPs Conference, and it was one of the highlights to also have 180 medical students coming for the Medical Student Conference and to engage with the rural network of doctors and other clinicians,” said Richard Colbran.
We’re celebrating 35 years of the Rural Resident Medical Cadetship
Program and launched an alumni program. The Cadetship program is administered by RDN on behalf of NSW Health and has seen over 400 future doctors participate. In 2012 an Indigenous Cadetship program was added.
“Our 35-year evaluation has shown that that Cadetship program overall has been incredibly significant, with over 60% of those graduates still practicing in rural and remote Australia, which is outstanding.”
This year, the conferences also drew participants from the wider Asia
Pacific, with a delegation from the University of Pattimura presenting on healthcare access in remote Indonesia.
“RDN believes in the strength of rural and remote communities and health services working together,” says RDN Chief Operating Officer Mike Edwards.
“Studying the commonalities between the remote island health care experiences of Indonesia and the remote outback experiences of Australia has highlighted for us the benefits of pooling collective wisdom - of sharing, understanding and adapting for local context, successful approaches to the challenges of rural and remote healthcare. That’s what this month is all about,” Mr Edwards said.
For rural practitioners, a sense of togetherness can be a source of inspiration every bit as important as the heartfelt gratitude of the country communities they serve. In the calendar of country seasons, November now sits as a permanent reminder that, no matter the challenges a doctor may be facing in rural practice, they need never feel “alone”.

Devin Deo Paediatric registrar, NSW
Recently, I saw the movie A Compete Unknown in cinemas, covering part of the life of famous singer songwriter Bob Dylan.
Among the many songs played, one particular favourite of mine featured - The Times They Are AChangin.
Dylan recalled writing the song as a deliberate attempt to create an anthem of change for the moment. How ironic then that it was playing in the background as I wrote this article.
Against the backdrop of mass resignations of NSW psychiatrists, and the more recent, marshmallow -gate, where a Junior Medical Officer mistakenly received an email from management critical of choosing life over work, it is a volatile time where the calls for change now come with renewed strength and urgency.
It is no secret that the system has come under immense strain with the ever-growing weight of more patients presenting more unwell where much of the medical workforce is burnt out and exhausted after dealing with the pandemic.
Marshmallow-gate started a firestorm within the NSW medical workforce, the fallout of which continues with calls for strikes among junior doctors.
It is, however, a symptom of a greater issue.

Premier Chris Minns was unaware of hospital staff rostered for 10hour, back-to-back night shifts. This is the sort of ignorance that has left many JMOs exhausted, burnout and unappreciated.
To be labelled “clinical marshmallows” despite the hard work and persistence for duty of care of patients is frustrating to say the least.
“The marshmallows are spending most of their shifts running from patient to patient, and ward to ward with barely time to catch their breath.”
The marshmallows are fighting to have a bite lest they were to faint due to the lack of a proper meal or snack between clinical duties.
The marshmallows are enduring the mental and bodily stress of consecutive shifts, a rotation and mix of days, evenings and night shifts, sometimes all in the same fortnight, enduring the whiplash to their circadian rhythm while sometimes forgetting what day it even is.
The marshmallows are bearing the brunt of frustrated and angered patients yet holding themselves together to deliver the best care possible for their patients.
The marshmallows are getting paid 30 per cent less than their interstate counterparts and seeing many of their colleagues leaving for other interstate opportunities.
JMOs deserve better from the health system that they serve.
It is time for the anthem of change to be carried out and for reform so we can deliver safe and quality healthcare to our patients.
We want doctors to be supported, appreciated and appropriately compensated.
The Times They Are A-Changin. We must change and that time is now.

Mt Druitt GP, past president AMA NSW
General Practice has a problem. In a world where we focus on short term results and visible achievements, the best of General Practice will never be seen.
The strength of quality General Practice is prevention, early intervention and improving health. It’s about the small steps of improving exercise, diets, blood pressure, weight, smoking cessation, being on the right medications or well-timed counselling to improve wellbeing. It’s about the many small steps to reduce the risk of heart attacks, strokes, cancers or hospitalisations. We will not see the results because these things don’t happen. We will not see the heart attacks or strokes that either don’t happen or are reduced. We will not see the cancers that are prevented. We will not count the times where a person does not go to hospital.
Australian lifespans are among the highest in the world – thanks to our robust health system. But that could change where general practice has been allowed to decline.
Studies have consistently shown that countries with good primary care systems have better health outcomes at lower costs.
In the US, where there were well recognised shortages of general practitioners, targeted programs to invest in improved models of
general practice demonstrated, & have continued to demonstrate, massive returns.
The Oregon Patient Centred Primary Care Home Program demonstrated an average return of $13 on every $1 spent through reduced hospital utilisation and overall costs, with benefits continuing to go up year on year in the three years of its evaluation.
Even in our existing system in Australia, evidence has shown that general practices that follow up their patients more intensively have lower hospitalisation rates across the board and that every dollar spent in general practice leads to $1.64 saved.
General practice of today is not the general practice of previous generations.
Today’s practice is more likely to consist of integrated multidisciplinary teams of health workers. This allows the provision of proactive, digitally enabled, comprehensive and co-ordinated care. Teams of doctors, nurses, pharmacists and allied health workers can co-ordinate to their top of scope where the whole is greater than the sum of its parts.
In the practice in which I work, we can identify the percentage probability of unplanned hospitalisation for every patient who attends.
We can identify each individual who may benefit from changes in
medications when new agents become available.
When a new cholesterol lowering agent became available, we were able to identify patients who would likely benefit and take appropriate action – reviewing files, recalling patients and liaising with cardiologists to discuss these changes.
The practice team monitors the data regularly to ensure that patients meet these cholesterol targets, with the dietitian and pharmacist looking at those who are not on target. This is what happens “behind the scenes”. The benefits are clear, but who sees the heart attacks that never happen? It is easy to focus on immediate problems such as elective surgery waiting lists because these are visible. Fewer patients on these lists give the appearance of a solution. But these problems could be solved much earlier, in a much more cost-effective way with far less of a toll on patients with greater investment in general practice.
The evidence is clear that good general practice underpins a good health system.
Ironically, the percentage of the total health care expenditure spent on general practice has continued to fall from just over 7 per cent in 2013-2014 to 5.7 per cent in 2021-22. Other countries are aiming to spend 10 per cent or more.
All this makes it harder to actually do good general practice and is contributing to the closure of many clinics.
Ultimately, the price is paid by patients and the rest of the system – both financially and in health terms. In a system which looks at measures of ill health and sickness, this is where the focus will be.
If we want a health system instead of a sickness system, we need to commit to managing illness early and comprehensively.
Sometimes you don’t know what you got until it’s gone.
Every year, more than 1000 Australians with blood cancers or blood disorders search for a stem cell transplant match. Only about half find a suitable match, and more than 80 per cent of those end up matching with overseas donors because there are not enough local donors available.
Stem Cell Donors Australia, previously known as the Australian Bone Marrow Donor Registry or Strength to Give, manages the registry of available donors in Australia, and searches databases both here and around the world to give patients the best chance of recovery post-transplant.
The matching process is heavily linked to the Human Leukocyte Antigen, one of the most variable gene systems in the human genome.
Patients will likely find their match with donors from a similar ethnic background.
This causes issues when we factor in the lack of diversity on the Australian registry, and global registries in general. Patients from minority ethnic backgrounds are severely underrepresented on the registry, meaning their chances of finding a match are reduced.
Many Australians have unique ancestries that are linked to our specific region of the world. Patients of Indigenous or Pasifika backgrounds, for example, rely heavily on the Australian donor pool to find their match.
To provide all patients with the hope for a second chance, there is an urgent need to recruit more donors, especially donors from ethnically diverse backgrounds.
Theregistrationprocess
To join the registry, recruits can visit stemcelldonors.org.au and follow the enrolment process to sign-up via mail-delivered cheek swab.
From these swabs, the registry will then test HLA-type, ABO-group and Cytomegalovirus-status, which are all important in the will then test HLA-type, ABO-group and
Cytomegalovirus-status, which are all important in the donor-patient matching process.
From there, recruits become available on the Australian registry and could become the life-saving match for a patient anywhere in the world. Recruits must be aged between 18 and 35 when they join the registry but can remain on the registry after the age of 35. There are several ways you can help promote Stem Cell Donors Australia.
Reach out to info@stemceldonors.org.au to request posters or organise events to promote donation.

Daniela, pictured with her husband Brendan, has been a mental health nurse in Sydney for more than 20 years. Her compassion, leadership, and mentoring skills have helped to shape mental health nursing in Australia.
In May last year, she was diagnosed with acute lymphoblastic leukaemia and will most likely need a blood stem cell transplant this year.
By increasing the number of donors on the Australian registry, hundreds of thousands of patients like Daniela are given hope that they will find

Since 1896, the Medical Benevolent Association of NSW-ACT (MBA NSW-ACT) has provided confidential support to doctors and their families in times of hardship or adversity.
Doctors seek assistance for challenges including illness, accident, grief, work stress, addiction, sudden loss of income and mental health concerns.
Often, these difficulties also lead to financial strain, with two thirds of doctors needing our support to help cover everyday essentials like accommodation, food, utilities and medical registrations, while they work through the underlying issue.
Through our support services delivered by senior social workers, we provide professional counselling, information and advocacy, and always emphasise the critical, yet often neglected aspect of doctors' wellbeing: having their own GP.
Despite the clear benefits of developing a GP relationship, only about half of the doctors who contact us in an adverse situation have a GP, and of these, many admit they are “well overdue” for a consultation.
One doctor MBA NSW-ACT supported recently demonstrates another reason why doctors need their own GP. She was facing a complex medical crisis and hadn’t worked in months. She had income protection, but the claim could not be approved without a medical certificate verifying her incapacity to work.
She did not have her own GP, so she had to have three different specialist consultations, just to complete this work capacity documentation.
These appointments were expensive, physically difficult for her to attend, hard to schedule due to limited availability, and delayed the approval of her claim which
added to her already high stress levels.
During this period, her savings had dwindled to the point that she needed MBA NSW-ACT’s support for essentials like rent, groceries, and household bills.
Our team also provided her with the contact details of a few GPs within her area that were experienced in working with doctors. About a month later she confirmed she “felt cared for” and that the GP had been proactive in their care which had “eased her mental load.”
In our work, MBA NSW-ACT stress that having a GP is akin to "putting on your oxygen mask first.” A doctor cannot provide optimal care to patients without prioritising their own health.
At MBA, we want you to make your health a top priority - find a GP and cultivate this vital professional relationship. It’s an investment in your future and the care you provide to others.
To help MBA NSW-ACT continue their vital work of supporting doctors experiencing adversity or hardship and to make sure the message gets out that all doctors need to have their own GP, please support our current appeal – details and QR code below.
Doctors prioritise their patients’ needs, but when it comes to their own health, they can sometimes hesitate.
So, when is the right time to see a GP? There’s never a wrong time.
Whether you’re feeling fine, managing ongoing health issues, or facing new concerns, maintaining a relationship with a GP you trust is essential.
Many doctors take a DIY approach to their health, and that’s understandable. We’re trained to problem-solve and assess risks. But, like a home renovation, there are limits to what you can, or should, tackle on your own.
Some issues require objectivity or expertise that’s not possible to provide for yourself. That’s where a GP comes in, offering a perspective that’s invaluable for addressing routine and more complex concerns.
Callers to the Doctors’ Health NSW 24/7 phone line often say “I do have a GP, but I don’t talk to them about this sort of thing”.
Whether “this sort of thing” refers to mental health, stress, or personal challenges, it highlights the need to find a GP you feel comfortable talking to about anything. Your GP should be someone you trust with the full picture of your health, not just physical symptoms.
Seeing your GP when you’re well for a preventative health “check-up”

can help establish that trust. It’s an opportunity to build a relationship, ensure compatibility, and create a baseline for your overall health. Having that foundation in place can make a big difference when unexpected issues arise, allowing you to focus on care rather than worrying about how to start the conversation.
A GP is more than someone who treats illness. They can act as a partner in your health, helping with preventive care, identifying risks you might not notice, and offering guidance tailored to your needs. This is especially important for doctors, who are often juggling high levels of stress, long hours, and demanding roles.
Many doctors delay seeking care for themselves. We know the risks of delayed presentations, yet it’s easy to fall into the trap of “not having time” or assuming it’s “not that serious.”
Having a GP who knows you and your history helps address issues early, before they escalate into something more difficult to manage.
A GP isn’t just there for emergenciesthey’re a resource for managing the everyday and staying on track. Making time for your own health isn’t indulgent; it’s practical and ensures that you can continue to provide good care to others.
The Doctors’ Health NSW 24/7 phone line (02)94376552 is here to support all doctors and medical students to prioritise their own health. Whether you need advice on finding the right GP or simply someone to talk to, calling Doctors’ Health NSW can be a first step towards better self-care.
Dr Kathryn Hutt Medical Director – Doctors’ Health NSW
















It was a busy start to 2025 with our team out meeting interns across NSW hospitals and sharing information on the career-long benefits of joining AMA (NSW).









DR DANIELLE MCMULLEN
AMA PRESIDENT
With an ageing population and rising rates of chronic disease, our primary care system has never been more crucial.
Yet, Medicare is failing to provide enough support for patients when they need to see a GP, particularly for more complex health needs.
Medicare was revolutionary when it was introduced in the 1980s, but that was when people had one or two simple health problems and didn’t need more than a few minutes with their GP.
Now, people suffer from more chronic health issues and require more mental health treatment. Making matters worse, we’ve had decades of poor indexation and a freeze on Medicare rebates that lasted several years.
Medicare rebates have fallen critically behind the cost of providing high quality care, creating more financial pressure for doctors and their patients.
The Productivity Commission’s latest Report on Government Services showed Commonwealth spending on general practice per person has declined since 2018–19, and more patients are delaying GP visits due to cost.
The health of these patients continues to decline, leading to increased emergency department presentations and more pressure on our public hospital system.
At the AMA, we have a plan to revolutionise Medicare rebates for all Australians and to address the critical workforce shortage in general practice.
We sought our GP-member views on how Medicare could be reformed, and developed a model that
supports longer, more comprehensive care. This model gives GPs and patients more options. It will help our doctors deliver more care, in a more sustainable way, through an increase in the patient’s Medicare rebate.
The model proposes a new seventier standard consultation item structure that will support patients to spend more time with their doctor by significantly increasing funding for the longer consultations that today’s patients need.
Costed at $4.5 billion, the model was developed over 18 months and was based on consultation with our members, analysis of available GP consultation time data, detailed economic modelling, consideration of the impact of different assumptions and scenarios, and testing against data provided by members.
We are also calling on the government to tackle workforce challenges and encourage a more multi -disciplinary approach to general practice healthcare where teams work together, under one roof.
We are proposing an extra 500 prevocational training rotations in general practice for early career doctors as well as an additional 500 GP training places as part of efforts to address the AMA’s predicted shortfall of 10,600 GP specialists by 2031-32.
To make sure we fill these extra training places we also need to fix the inequality in pay and leave entitlements for GP trainees compared to their hospital-based counterparts. While we’ve been encouraged to see trials of single employer models to address this inequity, we need to see a national approach to help encourage doctors into general practice specialty training.
We would also like to see the government provide more funding to support the employment of more nurses and allied health professionals in general practice. This will improve the capacity of general practice to provide the care that patients need within a well-coordinated GP-led model of care that is crucial to delivering improved patient outcomes.
In recent years we have seen the government invest in bulk billing incentives and we have welcomed that investment. But, as Health Minister Mark Butler has acknowledged, more is needed.
Many of our patients and families can’t access these incentives, leaving them out-of-pocket and deferring care. More of the same measures will help some - but not all - and will mean governments continue to delay helping many.
Our Modernise Medicare reforms provide a way forward. We are urging the federal governmentand all politicians - to support these reforms in the lead-up to the next federal budget and election to restore Medicare for all Australians.

Abbreviation often seen in medical documentation describing something seen at time of review 22.
Medical term for hair loss 24.
Paired bone of the pelvis 25. The final section of the small intestine
A contagious respiratory virus, often seasonal 26. 27.
The state of being able to find joy in things one would usually enjoy
Greek physician, writer, and philosopher who first described the four humours the ice bucket challenge was started to raise money for research into this condition
5.
Chronic skin infection caused by Treponema pallidum pertenue, characterised by papillomas and ulcers
6.
Sudden, involuntary, painful skeletal muscle contraction
7.
10.
A fear of this is called aviophobia or aerophobia
The animal found on the Caduceus
X-ray imaging technique used to screen for breast cancer
Substance produced by the choroid plexus
Viral infection that causes a painful rash of blisters
Diaphoretic (colloquial)
The junction between two neurons that allows them to communicate with each other
Type of fracture with a break in the skin
Surgical procedure that removes plaque from a blocked or narrowed artery
The white, fibrous tissue that covers most of the outside of the eye
Steatosis colloquially (_____ liver)
25 across and 26 across are bones that form this
Fungal infection of the lungs that occurs in people with weakened immune systems.
11. 12. 14.
Abbreviation for the condition described in 17 down
Medical suffix that that means to cut or make an incision into a part of the body, dervived from the Greek word tomos
Anatomical term referring to bundle of nerve fibers or a series of organs collectively providing a common function
15.
Condition defined by signs and symptoms such as mutism, waxy flexibility, catalepsy, echolalia or stupor
17.
Autoimmune condition associated with a malar rash, and almost never the diagnosis on House
18.
20. 23.
Medical term for an opening, hole, or passage, especially in a bone
The largest bone in the hip and pelvis Pyrexia, colloquially
Find the answers on page 43
You can find a comprehensive list of benefits and more information at www.amansw.com.au or email members@amansw.com.au


























As an AMA (NSW) member, for every new member you refer, we’ll reward you with a gift card. The more people you refer, the more gift cards you’ll receive.