ADVANCING WOMEN’S HEALTH
Doctors leading change for patient care

• SA’s elective surgery crisis
• Fairer fees for doctors
• Influencing decision-makers
• Deepfake doctors



F R O M


Doctors leading change for patient care

• SA’s elective surgery crisis
• Fairer fees for doctors
• Influencing decision-makers
• Deepfake doctors



F R O M

is produced by Australian Medical Association SA
Australian Medical Association South Australia Inc. Level 7, 431 King William St, Adelaide SA 5000
PO Box 685, Fullarton SA 5063
(08) 8361 0100 medicsa@amasa.org.au www.ama.com.au/sa
membership@amasa.org.au
President
A/Prof Peter Subramaniam: president@amasa.org.au
ceo@amasa.org.au
Editorial Dr Roger Sexton editor@amasa.org.au
Advertising medicsa@amasa.org.au
ISSN 1447-9255 (Print) ISSN 2209-0096 (Digital)
Neither the Australian Medical Association South Australia Inc. nor any of its servants and agents will have any liability in any way arising from information or advice that is contained in medicSA. The statements or opinions that are expressed in the magazine reflect the views of the authors and do not represent the official policy of the Australian Medical Association South Australia unless this is so stated. advertising material is expected to conform to ethical standards, such acceptance does not imply endorsement by the magazine. All matter in the magazine is covered by copyright, and must not be reproduced, stored in a retrieval system, or transmitted in any form by electronic or mechanical means, photocopying, or recording, without written permission. Images are reproduced with permission under limited license.
Cover image: Meaghan Coles Photography


AMA SA Council
President: A/Prof Peter Subramaniam
Vice President: Dr Louis Papilion
Immediate Past President: Dr John Williams
Chair: Dr Karen Koh
Ordinary Members
Dr Vikas Jasoria
Dr Emily Kirkpatrick
Dr Krishnaswamy Sundararajan
Dr Hannah Szewczyk
A/Prof William Tam
Dr Isaac Tennant
Specialty Group Representatives
Anaesthetists: Dr Louis Papilion
Dermatologists: Dr Karen Koh
Emergency Medicine: Dr Cathrin Parsch
General Practitioners: Dr Mark Ralfe
Gynaecologists: Dr Fariba Behnia-Willison
Intensive Care: Dr Raj Ramadoss
Ophthalmologists: A/Prof Michael Goggin
Orthopaedic Surgeons: Prof Edward (Ted) Mah
Paediatrics: Dr Gillian Watterson
Physicians: Dr Chelsea Patterson
Private Specialist Practice: Dr Simon Clark
Public Hospital Doctors: Dr Jayanthi Jayakaran
Public Hospital Doctors: Dr Chetan Pradhan
Public Hospital Doctors: Dr Clair Pridmore
Surgeons: Dr Christopher Dobbins
Regional representatives
Southern: Dr Jerida Keane
Northern: Dr Alice Fitzpatrick
AMA SA Board
Chair: A/Prof Peter Subramaniam
Ms Linda Abrams-South
Prof Tarun Bastiampillai
Dr Emily Kirkpatrick
Dr Shriram Nath
Dr Louis Papilion
Ms Megan Webster


As I reach the three-month mark of my term as President of AMA SA, I am reminded of the AMA’s responsibility to represent our profession at a pivotal time for healthcare in South Australia. The challenges before us are myriad. We face growing demand for healthcare from an ageing population with chronic illnesses, and limited physical, staff and fiscal resources to deliver timely care.
While we work with our junior and senior colleagues in the LHNs, we continue to engage with government on the challenges faced by doctors in private practice –both GP and non-GP specialists – in pursuit of a return to payroll tax exemption. While convenient to portray the payroll tax as a tax on doctors, it is, in reality, a tax on patient access to essential community-based services. Reduced access ultimately increases cost pressures across the broader health system.
AMA SA must ensure that the voices of doctors are not only heard but acted upon. Our experience shows that even when solutions are agreed upon, for many reasons implementation can be glacial in pace. Nonetheless, AMA advocacy will persist – grounded in the realities of clinical practice, informed by firsthand experience within the system, and strengthened by data-driven, evidence-based insights.
A resilient medical workforce – one that is supported to address community needs – is key to meeting system challenges. The practical recommendations from the AMA SA Access to Care Round Table in May make clear that strengthening the role of general practice and community care is not only effective but also cost-efficient for the system. Improving access to timely general practice will relieve pressure on our overburdened emergency departments. Similarly, increasing the availability of residential aged care beds for patients transitioning from hospital, and better linking these facilities to general practice, will ease hospital congestion. The AMA has been consistent in our call to state and federal governments to recognise and properly resource general practice as the cornerstone of every patient’s journey. A fixation on bulk-billing rates as a single metric of health system ‘success’ is a distraction; the true measure of success is better health outcomes for patients. This is the standard by which we should evaluate the health system. Achieving this requires a fit-for-purpose and resilient workforce.
International Medical Graduates (IMGs) play an indispensable role in the South Australian workforce, particularly in regional and rural areas where shortages are most acute. We are working with the various organisations that represent, support, and welcome IMGs. Together, we are advocating to break down barriers for IMGs to unlock the potential of a muchneeded portion of our workforce.
The new Women’s and Children’s Hospital is more than just a major infrastructure project – it’s a oncein-a-generation opportunity to design and implement future-proofed healthcare services that will meet the evolving needs of women and children across South Australia for decades to come. We continue to contribute to the consultation process to help ensure this outcome.
All this is taking place on the eve of a state election where the issues of ramping, elective surgery waiting lists and access to GP care will feature. Reform requires more than promises. It requires a strategy for delivery, clear, implementable plans and measurable outcomes. We will hold both government and opposition accountable.
Every new chapter in the AMA’s history in South Australia brings fresh eyes and opportunities to fulfil our purpose. With the skills, vigour and shared purpose of our Board, Council and dedicated staff, I am confident that AMA SA will continue to lead and deliver meaningful outcomes in the months and years ahead.
As I write my final message for medicSA, I feel a sense of gratitude and pride in closing this chapter. These past two-and-a-half years as CEO of AMA SA have been some of the most rewarding, challenging and memorable of my career, and I feel truly fortunate to have worked alongside such incredible people at both state and national levels.
I’m proud of the significant changes we’ve been able to embed behind the scenes that have strengthened the way AMA SA operates and sharpened our focus on supporting members. That journey remains a strong focus of the team, and I leave confident it is well on track. I will always be grateful to Immediate Past President John Williams for his trust and faith in me to drive these reforms when and where they were most needed.
One project especially close to my heart has been the transformation of medicSA and our electronic newsletter, Pulse. Seeing these communication platforms evolve in content, design and readability has been a real highlight. My heartfelt thanks go to medical editor Dr Roger Sexton for his support and to our team for their creativity and flair in bringing the vision to life. It has been wonderful to see this important publication develop into a modern reflection of our members’ voices and interests.
Another privilege of this role has been the opportunity to engage with government and stakeholders at every level. From advocating for clarity and fairness in payroll tax, to negotiating with ReturnToWorkSA on fee schedules, and working with state leaders on access to care and system reform, I have valued the chance to represent doctors and ensure their voice is heard in the rooms where decisions are made. These experiences have taught me that while progress is rarely straightforward, persistence and constructive relationships can

create meaningful outcomes. I am grateful to those in government who listened, engaged and partnered with us to improve the system.
One of the real highlights of my final week has been bringing to life the vision of our Women in Medicine Breakfast featured later in this magazine. Sitting in a room filled with such incredible female leaders in medicine and healthcare sharing openly, supporting one another, and inspiring us all was truly special. It was a beautiful way to finish my time with AMA, and I am so grateful to everyone who contributed. A heartfelt thank you to Dr Emily Kirkpatrick for hosting with such warmth, and to our panellists Dr Melanie Smith, Dr Susan Neuhaus and Dr Alecia Macrow for their wisdom and generosity.
I would like to sincerely thank our Board, Council and committees for their contributions. I am continually impressed by the dedication of our members who generously give their time and expertise on behalf of their profession. The strength of AMA SA lies in these collective efforts, attracting those whose values align with our commitment to trust, inclusion and collaboration. This dedication is reflected in each edition of this magazine, which captures just a snapshot of the important work undertaken to keep our members informed.
Most of all, I want to acknowledge my small but mighty team. It has been an honour to lead such a talented and passionate group of people. Their energy, professionalism and unwavering commitment to doing what is right for the profession have been a source of pride for me and we have delivered a lot in a short space of time together.
Thank you to everyone who has positively contributed to my journey for your support, encouragement and belief in what AMA SA can and should be.


At Norman Waterhouse, we know that experience matters
Our team comprises some of South Australia’s leading specialists in employment, industrial relations, commercial law, wealth management, wills and estates, tax, and family law.
As your full-service legal solution, we offer comprehensive support across a wide range of legal areas, ensuring you receive expert guidance for all your legal needs.
Protecting your practice starts with the right contract
Clear and well-drafted employment contracts are essential, whether you’re negotiating a new opportunity or hiring someone new. Our experienced legal practitioners understand the unique demands of the medical profession and provide practical and tailored advice for both employers and employees throughout all stages of contract negotiations.
For timely, personalised advice and complete peace of mind, contact one of our legal professionals.

Dasan Principal T: 8210 1253

Smith Principal
T: 8210 1203

Chris Alexandrides Special Counsel
T: 8210 1299


Annabelle Narayan Senior Associate
T: 8210 1292
Retirement from clinical practice is a transition in medicine we must all consider at some stage.
The decision to retire is extremely difficult for most doctors, especially those whose identity is so strongly aligned with their work. Doctors who have enjoyed decades of clinical practice generally expect it to continue and assume they will be in a position to determine when they exit clinical practice at a time of their own choosing. When something unexpected occurs to disrupt this plan – for example, illness, a medicolegal complaint or Ahpra restrictions on registration – it can come as a real shock. The doctor may be totally unprepared.
A doctor’s work delivers an enticing triad of benefits that meets their need for three things: achievement, affiliation with people, and power and influence both over and through others. These needs are of course not unique to medical practice, but a medical career delivers them in such spades that upon retirement it is very hard to find an alternative source.
A lack of forward planning for retirement can leave a doctor working well beyond the point when they should. Surgical practice is one example where the lifespan of a surgeon may be a lot shorter than the surgeon wants it to be. The days filled with achievement; contact with people; being valued, listened to and in control are hard to replace with anything else. There is nothing like it and writing medicolegal reports does not always ‘cut it’.
Doctors with a penchant for multiple marriages may find themselves working well past retirement age to recapture the wealth they have lost several times over. This is a recipe for trouble, as their workload may be too hurried, heavy and complex and errorprone in the years when they could be safely enjoying a more appropriate part-time caseload that allows for longer consultations and time for cognitive processing in complex cases.

Importantly, too, doctors who have devoted their lives to the care of others to the exclusion of family, friends and personal interests can find there are no alternatives to work and returning to work is all they have left.
Ill-preparedness of doctors, especially when they are the subject of a complaint and a consequent sudden enforced retirement, can be mentally crippling and depressing.
Retirement is around five years in the planning. It is not something that can be sorted out in a few months. Travel and gardening are fun but are not substitutes for achievement, affiliation and influence.
Retirement is a medical transition and can be an opportunity to take on another medical role such as teaching. The loss of retired doctors’ clinical experience and wisdom is enormous at a time when undergraduate teaching time is under pressure and students need as much exposure to patients’ clinical stories and patient presentations as possible. We all want to create the best medical graduates Australia has ever seen.
Retiring doctors have an enormous amount to offer at the other end of the career spectrum and we should actively find ways to optimise their contribution.
I hope you enjoy this fine Spring 2025 edition of medicSA and, as always, I welcome your correspondence.
Dr Roger Sexton roger.sexton@bigpond.com

YOUR LOCAL FERTILITY EXPERTS

Dr Bruno Radesic MD, FRANZCOG Medical Director, Fertility Specialist

Dr Victoria Nisenblat MD, PhD, FRANZCOG, CREI Fertility Specialist

Dr Kate Gowling
BHlthSc, BMBS, FRANZCOG, MRMed Obstetrician and Gynaecologist
All consultations are led by specialist obstetrician & gynaecologists
• One doctor every step of the way offering true continuity of care for your patients

Dr Michelle Wellman
BHlthSc, BMBS, FRANZCOG, MRMed Fertility Specialist
• World-leading IVF technologies such as the Geri time-lapse incubator that delivers leading success rates

Dr Alex Hubczenko
MBBS, FRANZCOG Fertility and Pelvic Health Specialist
• Full-service clinic offering fertility checks and ovulation tracking through to IVF, donor treatment and genetic testing
• Doctor consultations available across North, South, and Central - with city-based procedures at St Andrews Hospital
• Convenient clinic access with onsite parking and public transport at the door.
Women’s Health Week, held in the first week of September, is Australia’s largest event dedicated to the health and wellbeing of women, girls and gender-diverse people. Despite growing awareness, a significant gender gap in healthcare persists. Women’s experiences are still too often under-researched, underfunded and misunderstood. In this edition of medicSA challenges in women’s health and highlight the AMA’s advocacy for gender equity in medicine and healthcare.


AMA SA Board Member and Councillor Dr Emily Kirkpatrick hosted AMA SA’s Women in Medicine Breakfast and says the event sparked important conversations about equity, recognition, and the future of inclusive leadership in medicine.


On Thursday, 4 September, over 100 health professionals gathered for the inaugural AMA SA Women in Medicine Breakfast.
The energy in the room was electric as clinicians, students, policymakers and leaders came together to celebrate women’s contributions to medicine and to reflect on the systemic changes still required to achieve leadership equity.
It was an absolute honour to open the discussion by setting the scene. We know that women now make up around 75% of Australia’s healthcare workforce, yet they hold only 25% of leadership roles. The disparities at senior levels remain significant, with only 28% of medical school deans and 12.5% of hospital chief executives being women. It’s important to note that South Australia is shifting this figure nationally, with a high proportion of female CEOs.
Our panel featured three remarkable leaders: Dr Melanie Smith, GP and digital health innovator; Dr Susan Neuhaus AM, surgeon, former Army Colonel, and published author; and Dr Alecia Macrow, GP and women’s health advocate. Each offered honest, powerful reflections on their journeys and the barriers women in medicine still face.
Dr Smith, who started her career in software engineering, candidly discussed navigating male-dominated workplaces and the persistence of imposter syndrome.
‘Even when we are qualified and capable, those doubts can creep in,’ she said, resonating with many in the room.
Dr Neuhaus shared her experiences training and serving in what she called ‘two of the biggest boys’ clubs’ – the Australian Army and the Royal Australasian College of Surgeons. She reflected on how far South Australia has come.
‘The world has changed since then … and South Australia has been an absolute leader,’ she said.
‘This state has taken great pride in advancing women, from being the first state to give women the vote.’
She also highlighted small but meaningful changes, like the Women’s and Children’s Hospital leading discussions nationally to remove the ‘Mr’ and ‘Miss’ honorific for male and female surgeons so that all doctors are recognised equally as ‘Dr’.
Dr Macrow addressed financial inequities embedded in the system, noting that female GPs often spend longer with patients, particularly in mental health and antenatal care, but are penalised under the current Medicare structure.
‘Sometimes we do things differently than our male colleagues, in the way we work and connect,’
Dr Macrow said. ‘That time matters to patients, but it can cost us financially.’


The discussion made clear that inclusion isn’t just about fairness, it’s about professional excellence and looking outside the workplace at broader policy to support our non-work life. We know that diverse leadership results in stronger teams, better decisions and improved patient outcomes.
As the session concluded, AMA SA President Associate Professor Peter Subramaniam and outgoing CEO Nicole Sykes reflected on the importance of elevating women’s voices.
‘The AMA is an amazing platform of inspiring people,’ Ms Sykes said. ‘In my time here, I have been inspired by women and their stories... I can’t stress enough the importance of elevating others.’
I’d like to acknowledge the Women in Medicine Breakfast sponsors, Doctors Health Fund, MIGA, Radiology SA, Avant and Quintillion Concierge, who believed in AMA SA’s vision. This breakfast marked only the beginning. The conversations will continue, within our workplaces, committees, and communities. AMA SA is committed to ensuring we work towards supporting the next generation of women in medicine, not only to take their seats at the table but also to help shape it.
For more on Dr Susan Neuhaus and her new novel The
to page 64


Dr Fariba Behnia-Willison represents gynaecologists on the AMA SA Council. Writing for medicSA she says 2025 has been a ‘landmark’ year for the advancement of women’s health but significant systemic gaps remain.
From new policy shifts to expanded access to care, 2025 has marked a pivotal period for women’s health in Australia. Progress in obstetrics and gynaecology has been both long-awaited and encouraging. But while recent developments are commendable, they also highlight how far we still have to go. A deeper, more inclusive investment is needed – one that truly acknowledges the complex and specific needs of half our population.
Women make up 50% of the population, yet their health needs have historically been underfunded, undervalued and shrouded in silence. Fertility garners attention – perhaps because of male involvement – but conditions such as pelvic organ prolapse, incontinence, chronic pelvic pain and menopause remain taboo. The silence surrounding these issues is more than cultural; it’s systemic. Too often, women are valued only when trying to conceive or carrying a child – not for their individual health and wellbeing.
As a result, many women find their medical needs overlooked when childbearing is no longer possible. Postnatal pelvic floor disorders, menopausal symptoms and long-term complications receive limited attention and support. If we are to build an equitable healthcare system, a woman’s worth must not be tied solely to her reproductive status.
Historically invisible and misunderstood, endometriosis and pelvic pain are finally receiving the attention and multidisciplinary care they require. A major step forward was the further rollout in May 2025 of the National

Endometriosis Action Plan, which was introduced in 2018. This year, targeted Medicare funding has expanded, providing real relief for those living with endometriosis and chronic pelvic pain.
Specialised pelvic pain clinics that bring together gynaecologists, physiotherapists, psychologists and pain specialists offer a truly biopsychosocial model of care. Diagnostic delays, once particularly common among adolescents and young adults, are being addressed through increased awareness and earlier intervention.
Another important development was the expansion of the Pharmaceutical Benefits Scheme (PBS) to include advanced oral GnRH antagonists. These better-tolerated, more effective treatments for endometriosis offer new hope for people living with this condition. Crucially, this sends a broader message: gynaecological disorders are chronic and real, and deserving of both clinical and policy-level attention.
But this momentum must carry forward to other underrecognised conditions that are still falling through the cracks.
Women’s health decisions begin with education. Improved health literacy – starting in schools – leads to smarter healthcare choices and earlier care-seeking. The Periods, Pain and Endometriosis Schools Program (PPEP Talk) delivered by the Pelvic Pain Foundation of Australia is reaching 20% of Australian teens. It is an excellent model for national implementation.
The taboo continues
Pelvic organ prolapse (POP) affects as many as one in three women after childbirth. Meanwhile, women’s chances of experiencing stress urinary incontinence peak in their 30s – just as they balance careers, caregiving and personal growth. These are not niche issues. They are widespread and life-altering, yet are insufficiently addressed.
Access to conservative therapies such as pelvic floor physiotherapy, incontinence nurses and affordable pessaries varies widely across the country. Many women don’t know that early intervention is possible and many health professionals lack up-to-date training. Without more investment in research, education and access, we’ll continue to see unnecessary surgeries and ongoing impairments in quality of life.
overlooked transition
Menopause is universal. Every woman who lives long enough will experience it, but it remains underdiagnosed and undertreated. Symptoms like hot flushes, cognitive shifts, joint pain and mood changes are too often misattributed or dismissed. Hormone replacement therapy (HRT) remains underutilised, partly due to persistent myths – even among clinicians.
Women from culturally and linguistically diverse backgrounds face added challenges, including language barriers, stigma and inadequate access.
We need a new model: menopause clinics, GP training and public education campaigns. This is not a footnote in women’s lives. It is a critical chapter that deserves medical and emotional support.
Every cell in a woman’s body knows that it is female. We cannot assume that symptoms, diseases and responses to treatment will mirror those in males. Medical trials are often performed with the assumption that both men and women will have the same response or reaction. Innovations tailored specifically for women are urgently needed – and they’re emerging, including here in South Australia.
One example is the neuroimmune-modulating intrauterine device in development by Adelaide’s A/Prof Susan Evans of Alyra Biotech, which represents a new frontier in managing central immune symptoms in pelvic pain. A/Prof Evans founded Alyra Biotech to develop new products to help women who experience the severe pain that results from excessive immune activation in the uterus. Patents have been awarded in the United States, China and Australia with further patent jurisdictions pending.
Another example is the work of my company SmartFEM in developing the whole blood autologous graft, a regenerative and biologically harmonious alternative to other tissue augmenting products such as biological grafts or mesh. Using a woman’s own blood to form a natural graft, it encourages tissue regeneration without foreign material, offering a safer and more personalised treatment for prolapse. The SmartFEM product gained TGA approval in late 2024.
These innovations are not futuristic – they are already taking shape. But they cannot thrive without robust support.
Transformative clinical solutions need systemic backing. Research, translation and equitable access all rely on government funding, streamlined regulation and national commitment. Without these, promising developments risk stalling before they can reach patients.
Australia has the research talent, technological infrastructure and willpower to lead a global revolution in women’s health. What we need now is the political will and financial commitment to sustain it.
We must change how we talk about women’s health. Conditions such as endometriosis are not personal inconveniences – they are public health priorities. From adolescence to post-menopause, care must be embedded across the entire health system.
As clinicians, we witness daily how delays in care, fragmented systems, and silenced suffering impact women’s lives. But we also witness how lives transform when women are heard, believed, and treated with dignity. That transformation must extend beyond the clinic and into national health policy.
This year has shown what is possible when we prioritise and invest in women’s health. But we must not stop here. Every condition, whether common or stigmatised, deserves evidence-based care and national attention. Half the population cannot continue to be underserved.
Women are not a special interest group. They are the backbone of our society, families, and future. It’s time our healthcare system reflected that truth—with action, funding, and innovation.
• AMA SA Councillor Dr Fariba Behnia-Willison is a gynaecologist, women’s health advocate, and founder of SmartFEM, dedicated to advancing care through innovation and patient care.

Gynaecologist and long-term women’s health advocate
Dr Melissa Slattery argues that the costs imposed by endometriosis on individuals and the health system should be balanced by increased government spending.
Endometriosis affects one in seven women. There are about 35,000 women in South Australia who need care for endometriosisrelated pain and other symptoms. Despite its prevalence, endometriosis has a legacy of underdiagnosis and delayed diagnosis, resulting in significant costs to individuals, our health system and our society. It can lead to infertility, chronic pain and reduced social, educational and economic participation among sufferers. According to estimates, it costs affected individuals around $35,000 per year, our health system $250 million per year and our community $9 billion per year. Early diagnosis and intervention are critical. That’s why every doctor needs to know something about endometriosis.

Australia was the first country to develop a roadmap and blueprint to tackle endometriosis in a nationwide,
coordinated manner. The 2018 ‘National Action Plan for Endometriosis’ (NAPE) was created from a partnership between federal government, endometriosis experts and advocacy groups. The initiatives include raising public awareness; $87 million to fund research, education and specialised GP clinics; developing collaboration between government, experts and advocacy groups to address endometriosis as a chronic condition; and improved treatment approaches.
The plan has triggered considerable progress. Examples include funding for the Periods, Pain and Endometriosis Program (PPEP Talk) in schools, development of the RACGP Endometriosis Learning Module, and release of the RANZCOG Clinical Practice Guideline and the Australian Living Evidence Guideline: Endometriosis. It established dedicated Endometriosis and Pelvic Pain GP clinics, including two in South Australia. Pleasingly, there is now evidence of reduced diagnostic delays with the average patient age at diagnosis gradually decreasing.
One could therefore question – as the AMA in South Australia did – the need for last year’s South Australian
Parliamentary Inquiry into Endometriosis, at considerable cost to taxpayers, as opposed to our State Government simply supporting the Federal NAPE initiative already in place. But that’s politics.
The Final Report of the Select Committee, tabled in March this year, paints a grim picture of endometriosis care in South Australia, highlighting delayed diagnosis, fractured care, poor education, and general disregard for the plight of affected women.
The report is highly critical of the medical profession, as was the Minister for Health who was quoted saying, ‘We can’t have the issues that we’ve seen for many, many decades – of how endometriosis has been treated by the medical profession – continue one day longer’.
This looks a lot like blame shifting to me. If we unpack the issues with endometriosis care provision as outlined in the report, the insufficient training of primary caregivers is far and away the easiest to criticise and the easiest to fix. On the other side, the lack of timely access to medical professionals and services, the lengthy delays in accessing public hospital gynaecology services, the lack of multidisciplinary pain management services, the sheer cost of care to individuals, and the lack of health education in the community are structural problems that the South Australian Government needs to address. It has made the commitment to do so, adopting all 20 of the recommendations in the report.
There has been a repeated call for user-friendly endometriosis management guidelines. RANZCOG published succinct endometriosis guidelines in 2021 and more recently made available the Australian Living Evidence Guideline
The Australian Government is funding the Endometriosis Management Plan (Endo-MP) project being conducted by the SPHERE Centre of Research Excellence in Sexual and Reproductive Health for Women in Primary Care in collaboration with the RACGP. The Endo-MP will be available to all practising GPs and people with endometriosis and chronic pelvic pain in Australia upon national implementation in 2026.
As most guidelines note, the multidisciplinary care model is considered the ideal for assisting individuals who have endometriosis. However, factors such as a lack of regional care centres, remuneration of specialist service providers and the lack of skilled workforce relative to
workload present difficulties with the model’s successful implementation.
It helps to distinguish between the management of patients presenting with pain that has been present for a short time and those who have chronic pain (present for longer than three to six months). With early presentation, management should be within the primary care setting; prevention of progression to chronic pain is the goal. Most patients at this stage do not require multidisciplinary care and should not be shoehorned into that model unnecessarily.
To optimise care, we must improve knowledge and skills among primary care providers, individualise care teams (GP plus gynaecology, psychology and physiotherapy as necessary), and lobby government for 100% rebates for all pelvic pain consultations, procedures and investigations. The goal of providing exceptional pain and endometriosis care across the community cannot possibly be met without including existing GP and private gynaecology services, simply on account of the thousands of patients requiring care. Given the massive monetary cost of pelvic pain to individuals, our health system and the community, as succinctly described in the report, scrimping financially on early intervention and provision of high-quality care is illogical.
The South Australian parliamentary report supports the creation of more endometriosis and pain clinics in public hospitals across the state, for the management of chronic or complex pain. These clinics must include multidisciplinary teams that can provide specialist GP, gynaecology, fertility, urology, colorectal, radiological, and nursing services. The report supports upskilled nurses managing care, but this may be a false economy: the initial assessment, investigations and individualised referrals to other services should be made by the most qualified and experienced member of the treatment team, not the least. Again, the cost of providing this model of care is justified relative to the economic impact of the problem.
We have an opportunity to dramatically improve endometriosis care in South Australia; we should use it.

Dr Melissa Slattery is a gynaecologist and long-term women’s health advocate.


A landmark study published in the British Journal of Obstetrics and Gynaecology has revealed alarming disparities in the incidence of maternal and neonatal outcomes between Australia’s public and private maternity care systems.
The research examined more than 368,000 births in Victoria, New South Wales and Queensland between 2016 and 2019. It found that newborns delivered in public hospitals were twice as likely to die from stillbirth or neonatal complications compared to those born in private facilities.
The study also demonstrated that mothers giving birth in public hospitals were three times more likely to suffer birth trauma, including severe perineal tears and haemorrhage.
AMA President Dr Danielle McMullen says the ‘concerning’ findings highlight the critical need for reform in both public and private hospital systems.
‘Funding for our public hospitals must be increased to ensure they can continue to provide safe, high-quality maternity services,’ Dr McMullen says.
‘Continuity of care must be prioritised, and renewed efforts to support collaboration in our public hospital maternity services are paramount.
‘We also need a private health system authority to examine reform options to make private health insurance, including for maternity care, more accessible for Australians.’
The study attributes many of the adverse outcomes in public care to fragmented service delivery. It also raises concerns about the accessibility of private maternity care, especially in light of the recent closures of private maternity units across Australia.
‘Patient choice is absolutely critical,’ Dr McMullen says. ‘We need reforms to ensure all Australians have the utmost confidence in both the public and private systems, with access to high-quality, multidisciplinary care.’
Scientists have uncovered a hidden biological defence that could explain why women’s hearts respond differently to men’s with hypertension and pave the way for sex–specific treatments.

A new preclinical study from Monash University has uncovered a biological mechanism that may help protect women’s hearts from damage caused by high blood pressure – a discovery that could lead to sex-specific treatments for cardiovascular disease.
Published in Communications Biology, the research –led by the Monash Institute of Pharmaceutical Sciences (MIPS) – found that the female sex hormone estrogen increases levels of a natural protein called annexin–A1 (ANXA1) in female mice. Previous work by the MIPS team had already shown that ANXA1 plays a crucial role in regulating blood pressure.
In the latest study, researchers discovered that when ANXA1 is absent, high blood pressure causes more severe damage to the heart and major blood vessels –particularly in females.
Lead researcher Dr Jaideep Singh said the findings help explain why women may experience heart disease differently from men, especially when they have high blood pressure.
‘Our study reveals a biological link between the female hormone estrogen and the protein ANXA1 that protects
the heart – something scientists didn’t fully understand before,’ Dr Singh said.
‘Essentially, we found that estrogen helps increase ANXA1 protein, and when ANXA1 is missing, the heart is more vulnerable to damage due to poor mitochondrial function, the body’s energy system.’
Dr Singh says the discovery is an important step towards developing heart-disease treatments tailored specifically for women, addressing a gap that has been evident in medical research for a long time.
‘We’re really excited about what this discovery could mean for future treatments that enhance ANXA1, providing better protection for women with high blood pressure,’ he said.
‘These therapies might help prevent serious problems like heart failure by focusing on the unique ways women’s hearts and blood vessels work. It also highlights the importance of doctors considering sex differences when deciding how to treat heart disease.’
MIPS researchers aim to proceed towards clinical testing with the goal of improving outcomes for women living with high blood pressure.

GP and medical educator
Dr Marny Royans says lifestyle medicine can help doctors move beyond menopause symptom management to deliver holistic, evidence-based support for midlife women.
As a GP, I’ve seen how profoundly the menopausal years can affect women – physically, emotionally, socially and cognitively. My work in aged care has also shown me the long-term impacts of chronic disease – many of which start in midlife and are preventable.
In general practice, supporting behaviour change can be challenging. Time pressures, reactive care models and limited training in lifestyle medicine, health coaching and the psychology of behaviour change make it difficult to provide the kind of support that sustainable change requires. At the same time, the media and wellness industries often exploit women’s vulnerabilities – offering quick fixes and unproven solutions that undermine confidence and fuel confusion.
While menopause is technically a single stage in life, in this article I use the term to include both the perimenopausal stage and the years that follow in postmenopause.
For many women, the hormonal shifts of menopause feel like the point where everything begins to fall apart. This is often when risk factors for chronic conditions emerge or accelerate.
While menopause awareness is increasing through media coverage and political attention, many women remain confused. Their symptoms may be dismissed. There is a lack of whole-person care. Women are frequently told their symptoms are ‘normal’ or their tests are ‘fine’. Some ask about menopause hormone therapy (MHT) but are dissuaded by doctors with outdated views on its risks and benefits.

Most women will begin their conversations about their symptoms and concerns by speaking to their GP. But not all GPs feel confident or equipped to manage symptoms of menopause.
These are just some of the problems that affect access to care.
Short consultations: women are often navigating multiple concerns – weight changes, fatigue, poor sleep, low mood – but short appointments don’t allow doctors and patients to explore them fully.
Generic or unrealistic lifestyle advice: telling women to improve their diets and exercise more is not enough. They need practical, evidence-based advice and tailored, compassionate support.
Outdated knowledge of perimenopause and menopause: too many women are not appropriately diagnosed and miss out on effective, evidence-based options, including hormone therapy and non-hormonal treatments.
Symptom-focused care without prevention: while relieving symptoms is essential, menopause is also a window to address long-term health risks – such as cardiovascular disease, osteoporosis, and metabolic changes.
Not considering the path women have walked to get here: past experiences of dismissal, judgement or feeling unheard can affect a woman’s trust in the healthcare system.
Compounding the problem, the wellness industry frequently targets midlife women with promises of ‘hormone balancing’, biohacking or supplements – often
promising miracles without a scientific basis. When healthcare doesn’t meet women’s needs, they are more likely to turn to less credible alternatives.
Lifestyle medicine is integral to menopause care, ensuring that women receive both symptom relief and strategies to protect their future health.
Lifestyle medicine is an evidence-based clinical discipline focused on the prevention, management and, in some cases, reversal of chronic disease by addressing behavioural, social and environmental drivers of health.
It is built on six key pillars:
• nutritional improvement and sustainable eating habits
physical activity and reducing sedentary behaviour
• stress reduction and support for mental wellbeing
• optimising sleep quality
• reducing harmful substance use (e.g., tobacco, alcohol)
• strengthening social connection and community engagement.
Menopause is a critical life stage, strongly associated with the emergence or progression of chronic disease risk factors. With evidence-based lifestyle interventions and appropriate support, this period can become a powerful opportunity for women to build physical resilience, reduce future disease risk and align their health habits with what matters most to them.
When women receive comprehensive support at this stage, the benefits ripple outward: improved energy, mood and functional capacity; healthier ageing trajectories; increased self-efficacy; and a greater sense of agency over their bodies and wellbeing.
Most doctors were not taught a lot in medical school about how to manage menopause and even fewer have received training in the relatively new discipline of lifestyle medicine.
Many women seek help only after years of struggling with fatigue, poor sleep, mood changes, brain fog or weight gain – and still may not feel heard. As GPs, we’re in a unique position to change that experience.
A few key strategies can make a meaningful difference.
• Validate and truly listen. Acknowledging and validating a woman’s experience can be therapeutic and build trust in the healthcare system instead of less credible alternatives.
• Stay up-to-date on MHT developments. The global consensus is clear: MHT is effective and safe for most women under 60 or within 10 years of menopause onset. Body-identical options, such as transdermal oestradiol and micronised progesterone, have improved safety profiles.
• Screen for lifestyle-related risk factors – without judgement. Midlife is associated with metabolic shifts and increased cardiovascular risk, among others. Proactive screening and early intervention can help prevent chronic disease.
• Offer more than just hormones. While MHT benefits many, not all women want or need it. Evidence-based non-hormonal options such as SSRIs/SNRIs, Fezolinetant, CBT-I for insomnia and tailored lifestyle strategies may be discussed.
• Be curious, not prescriptive. Use open-ended questions to explore what matters most to the patient. Many women are navigating identity changes, caregiving demands and emotional fatigue.
• Incorporate a health coaching approach. This can foster motivation, build self-efficacy and support women to take sustainable, self-directed steps towards better health.
• Seek the latest evidence – or refer. Menopause care is a rapidly evolving field, and practice should reflect current guidelines. If you’re not confident with the latest recommendations, connect women with trusted colleagues or specialists, or learn from credible resources.
My hope is that more GPs feel supported and confident to start these conversations; that we move beyond reactive, symptom-focused care to person-centred, proactive support. We must stop viewing menopause as an end point, and instead recognise it as a powerful window for health promotion and prevention.
When we get menopause care right, we’re not just reducing hot flushes – we’re helping women sleep better, move more, age well and live with greater confidence and independence.

Dr Marny Royans is a GP, medical educator and founder of Lifestyle Medicine Collective.
Learn more at www.lifestylemedicinecollective.com.au
Email: contact@lifestylemedicinecollective.com.au

Fertility preservation is increasingly relevant for young people navigating medical,
gender-affirming
Fertility education in schools has traditionally focused on preventing conception, to orient young people to acquiring the education and skills needed to participate in the activities of our modern world. It is often much later that fertility is considered – sometimes when unexpected events push it into focus.
Age is the single biggest factor that affects fertility rates in women and those assigned female at birth, and it has the strongest influence on chance of conception. The number of eggs diminishes with age, reducing the choice of which egg will ovulate. Additionally, the fine spindles holding duplicate sets of chromosomes in eggs that have been frozen in meiosis 2 are subject to damage and oxidative stress over time. Any breaks in these spindles lead to one or more chromosomes being left behind in the oocyte cytoplasm, or added to the set of maternal chromosomes extracted into the polar body at ovulation, creating trisomy or monosomy in an embryo, and most commonly no conception, but sometimes miscarriage or an ongoing pregnancy with trisomy 21, 18 or 13. Thus freezing eggs or embryos using Artificial Reproductive Technologies (ART) at a younger rather than older age, ensures both higher numbers of eggs and more chance that they will have a normal complement of chromosomes.
Just less than 10% of ART cycles in Australasia are to safeguard future fertility predominantly to protect young people from age related gamete changes, when they are not in a position to have a family at a young age.
Genetic factors that reduce ovarian reserve or negatively impact sperm production should prompt discussion about safeguarding fertility. In females, genetic conditions such as Fragile X syndrome (additional CTG repeats on the X chromosome), Turner’s Syndrome (karyotype 46 X0) or Down’s syndrome (Trisomy 21) accelerate the loss of oocytes
from the ovary. In Turner’s Syndrome, 90 per cent of people will have exhausted their ovarian reserve before puberty; however, in Turner’s mosaicism many will have a natural puberty and the opportunity to preserve fertility in their adolescence.
Safeguarding fertility in young people with cancer is well established in clinical practice, particularly for those having total body irradiation for a bone marrow transplantation, or radiotherapy or chemotherapy with agents such as vincristine or cisplatin.
Before cancer therapy begins – and depending on the urgency of treatment and each individual’s situation – freezing oocytes, sperm or embryos should be discussed alongside options such as ovarian or testicular tissue freezing, surgical transposition of ovaries out of radiotherapy fields or the use of GnRH agonists to reduce ovarian exposure to chemotherapeutic agents.
Modern random start or duo stim protocols in ART stimulation cycles avoid delays in inducing multifollicular ovarian stimulation for oocyte/embryo freezing.
In breast and estrogen-dependent cancers, the use of aromatase inhibitors such as letrozole reduces the impact of high estradiol levels on cancer progression during stimulation. Laparoscopic removal of ovarian tissue to freeze provides an opportunity for tissue grafting at a later date. This is a technique which has proven but not guaranteed success both in creating pregnancy and providing replacement hormones when ovulation recommences.
Post puberty, ejaculatory sperm is usually frozen for future use, although surgical retrieval of sperm can be performed if the sperm count is low. Before puberty, frozen surgically retrieved testicular samples can be stored, but taking consent is ethically challenging and no successful pregnancy from these samples has been

reported. Very recently, reimplantation of prepubertal testicular tissue has been successful in animal models and attempted in humans, with rapid improvements in protocols and outcomes, although it is still considered experimental in clinical care.
Cardiac, renal and rheumatological conditions can also negatively impact oocyte numbers. Required medications may have safety implications for a foetus and impact the ability to carry a pregnancy. Careful consideration of fertility preservation in a multidisciplinary setting is warranted, in conjunction with possible changes to medications, genetic testing of embryos and potential needs for surrogacy.
Endometriosis is associated with lower egg numbers due to the inflammatory environment generated by the breakdown and regeneration of endometrial-like cells situated in the pelvic cavity, which can also negatively impact the quality of eggs.
Fertility-preserving surgery involves careful excision of lesions and avoidance of destructive heat-based diathermy to avoid damaging the oocyte pool. When ovarian reserve is low and endometrioma excision or complex surgery is planned, egg freezing should be considered prior to surgery to preserve fertility.
When only one gonad (ovary or teste) is present, fertility preservation can manage the risk of loss of function of the other gonad. Congenital absence of a gonad is rare, but torsion, infection, cancer, vascular obstruction or cyst formation can lead to unilateral surgical removal of a unilateral gamete-containing organ. Storing eggs or sperm provides reassurance that there will be an opportunity to use stored gametes if the second gonad is compromised.
In transgender medicine, fertility preservation is often discussed in the context of a multidisciplinary team. The long-term effects of exposing spermatogonia to
estrogen has a variable effect on sperm production and semen quality. When estrogen and antiandrogens are withdrawn, some, but not all gender transitioning people assigned male at birth will have recovery of sperm production.
Sperm freezing before starting estrogen should be discussed, although for those using puberty blockers to delay secondary sexual characteristics, mature sperm will only be retrieved after pubertal transition, which may be prolonged and/or distressing.
Egg quality and quantity do not appear to be affected by exposure to androgens, so there is no urgent need to make a fertility preservation decision. However, many individuals choose to freeze eggs before starting androgen therapy to avoid the gender dysphoria that can arise from stopping androgens, experiencing elevated estrogen levels during an ART cycle, and then resuming androgens after fertility treatment.
Increasing evidence demonstrates that reducing factors that affect cellular oxidative stress improves the quality of eggs and sperm and maintains ovarian reserve. Avoiding smoking, marijuana use, a sedentary lifestyle, poor diet and a high caffeine or alcohol intake are simple self-efficacious measures that all people can undertake to safeguard gamete quality and future fertility.

Professor Louise Hull is Deputy Head of the University of Adelaide’s Department of Obstetrics and Gynaecology.

Pelvic pain remains under-recognised and under-treated, but a new initiative is aiming to unite clinicians, researchers and advocates to improve care pathways and patient outcomes.
Gynaecologist and obstetrician Dr Preetam Ganu explains.
Persistent pelvic pain – pain present on most days for more than six months – is a significant yet under-recognised health issue. International estimates suggest 15-25% of women experience chronic pelvic pain. In Australia, nearly half of women report having suffered pelvic pain in the past five years, with one in four missing work, study, or exercise and one in three experiencing an impact on mental wellbeing.
South Australia has been a leader in pelvic pain innovation. The IMAGENDO project is developing AIassisted integration of ultrasound and MRI to reduce diagnostic delays and avoid unnecessary surgery. Alyra Biotech is advancing a novel neuroimmune-modifying intrauterine device, with Phase 1 trials completed in Adelaide and a larger clinical trial set for 2025.
Despite these advances, there has been no open, multidisciplinary platform in South Australia to unite all clinicians and researchers working in pelvic pain – until now.
Inspired by successful models in other states and supported by the Pelvic Pain Foundation of Australia, we established the South Australian Pelvic Pain Network (SAPPN) in 2025. As a founding member, I saw an opportunity to break down silos, strengthen referral pathways and foster collaboration across sectors, especially after attending World Endometriosis Congress.
SAPPN is a not-for-profit, clinician-led initiative to improve outcomes for people living with pelvic pain, through collaboration, connection, education and advocacy. Our multidisciplinary membership includes physiotherapists, general practitioners, gynaecologists, gastroenterologists, pain specialists, psychologists, nurses, dietitians, researchers and more – united by a shared commitment to evidence-based and patientcentred care.
Our mission is to:
• Enhance collaboration among clinicians across South Australia
Strengthen referral pathways for timely, holistic, person-centred care
• Support professional development through presentations, peer-led case studies, and hybrid events
Advance pelvic pain knowledge by promoting current research and clinical best practice
• Build a community of like-minded professionals through networking and shared learning.
Members benefit from regular networking and professional development events, a clinician-only referral directory to streamline connections, a regular newsletter, and opportunities to host local events.
SAPPN began with a WhatsApp group and grew to over 70 members in its first month. Our organising committee includes representatives from each major discipline. SAPPN’s official launch took place on 28 August 2025, with around 70 people in attendance. The strong early uptake reflects the urgent need for shared learning and coordinated care. Annual membership is through the Pelvic Foundation website.
We believe SAPPN will strengthen care pathways within South Australia and contribute to a national movement to improve outcomes for those living with pelvic pain – because complex problems demand collaborative solutions.

Dr Preetam Ganu is a gynaecologist and obstetrician.
The recommendations emanating from the AMA SA Access to Care Round Table have been presented to the Health Minister and are now being discussed in high-level meetings involving senior representatives of SA Health and AMA SA.
The Round Table on 9 May brought together more than 30 leaders from across the health sector to generate ideas about how to care for South Australians in their communities and reduce emergency presentations at the state’s hospitals.
AMA SA Committee of General Practice Chair Dr John Williams said SA Health was reviewing how the recommendations can align with, boost or transform existing systems and services.
He said an initial discussion included SA Health’s Deputy Chief Executive for Clinical System Support and Improvement, Robyn Lindsay; Executive Director, Integrated Care System, Jeanette Walters; and Chief Medical Officer Dr Michael Cusack. Further discussions will include consideration of how relevant Round Table participants are included in the design and implementation of specific recommendations.
Two key themes summarised Round Table participants’ perspectives about the reforms needed to keep patients healthy in their communities and out of hospital.
1. Sustainable reform demands whole-of-system collaboration and information sharing.
2. Better leveraging of general practice and community care will keep people healthier in their communities and avoid hospital presentations.
AMA SA urges SA Health to include clinicians and consumers in the design, testing, implementation and evaluation of all measures, new and existing, to ensure their knowledge and experience are considered and reflected in services throughout the health system.
1. Establish a visible and realistic SA Health 12-month Action Plan.
A shared roadmap of reform initiatives will enable clinicians and other healthcare professionals to

Participants called for a co-owned and public-facing Action Plan led by SA Health that outlines specific initiatives (including practical, low-cost programs and services and long-term reforms), capitalising on digital and AI capabilities.
2. Provide physical and digital resources for the GP clinic that support a unified, person-centre health ecosystem, enabling care to be delivered at the right time and right place and by the right provider.
• Provide funding to employ nurse practitioners, registered nurses and other allied health professionals to enable GP clinics to open after hours, linked with discharge-planning KPIs.
• Mandate the use of clear, standardised discharge and referral summaries that are uploaded to My Health Record and available to the patient’s nominated GPs and residential aged-care facilities (RACF) within 24 hours of discharge.
outpatient services, with recommendations to be included in the SA Health Action Plan.
27 contribute their knowledge and expertise to effective, patient-focused change.
• Integrate into Local Health Networks (LHNs) care coordinators and discharge planners who work with Primary Health Networks (PHNs) to collaborate with GP clinics to provide follow-up post-discharge and identify at-risk patients in their communities, focused on reducing avoidable representations and readmissions to hospital, aligned with NSW Lumos evidence.
• Enable read-only access to Sunrise for GPs, private specialists and rural after-hours access teams, noting that workarounds exist currently with nonGP specialists who see private and public patients, without clear patient consent and privacy.
• Establish direct contact lines between GPs and other specialists in public and private settings, with the formation of a statewide database led by the State Health Coordination Centre, linked to Healthdirect’s health provider directory.
• Expand virtual care specialist support services for GPs, with the Virtual Care Service (VCS) working with Hospital in the Home (HITH) services to provide specialist, real-time advice to GPs and navigation for care, reducing fragmentation and unnecessary presentations to emergency departments (EDs).
3. Reform outpatient and specialist access pathways to improve efficiency, enable clinicians to focus on providing clinical care, and reduce long wait times.
• With AMA SA input, establish an outpatient department (OPD) implementation working group or taskforce to identify practical measures to improve
• Capitalise on artificial intelligence, two-way SMS communication with patients and e-referrals, and provide support for clinicians, to reduce the burden of administrative tasks in outpatient settings, such as managing requests for specialist input, completing referrals and wait times.
• Create a state-wide e-referral ‘front door’ for outpatient care across all LHNs that enables a single referral, regardless of locality and health network, reducing barriers that cause confusion when LHNs have different boundaries for different services.
• Embed team-based video conferencing arrangements with hospital specialists, mirroring models in Victoria at Northern Health that enable rapid access to advice, reducing reliance on traditional OPD appointments, yet still using activity-based funding. Linked to an expanded rapid access model for outpatient clinics (e.g., respiratory, gastroenterology).
• Introduce GPs with special interests, into OPDs, with a focus on reducing long wait times and opportunities to redirect care back to primary care with specialty advice coordinated by the OPD GP.
4. Improve aged-care coordination and dignity with end-of-life care, formalising communication pathways and shifting care to people’s homes.
• Establish an Aged Care Working Group to include the PHNs, consumers and GPs, with the aim of:
» developing a central repository for and training in the use of Advance Care Directives that is accessible to RACFs, South Australian Ambulance Service and GP clinics, building on previous pilots within the Barossa Hills Fleurieu LHN and the Department for Health and Wellbeing
» establishing pathways to facilitate RACF communication with a patient’s nominated GP clinic, including hospital notifications, to prevent unnecessary transfers and tests and to monitor the patient’s post-hospital needs.
• Expand VCS in-reach to enable RACF residents to obtain a rapid access face-to-face review supported by VCS clinicians, with subsequent referral to My Home Hospital or HITH without the need for ED attendance.
The complete list of recommendations is available here: ama.com.au/sa/articles/access-to-care-round-tablerecommendations
AMA SA President and vascular surgeon Associate Professor Peter Subramaniam is calling for urgent strategic action to address South Australia’s ballooning surgery waiting lists.
Ambulance ramping dominates media and political commentary about healthcare in South Australia, but the state is facing an essential surgery crisis that requires similar attention. I use the term ‘essential’ surgery rather than ‘elective’ surgery deliberately. These procedures are not discretionary. They are necessary to preserve patients’ health and quality of life.
At the time of writing in September 2025, SA Health data shows there are more than 24,000 patients awaiting essential procedures. More than 6,100 of those are overdue – many far beyond recommended timeframes for safe care. This growing backlog is a daily strain on clinical and support teams trying to manage this within local healthcare networks.
A breakdown of the data reveals overdue rates across many specialties. Neurosurgery has the most significant percentage with 54% of patients overdue, followed by plastic surgery (40%), urology and vascular surgery
(37%), and general surgery (33%). Even specialties with lower percentages such as ophthalmology (12%) ENT (15%) and gynaecology (16%) represent significant numbers of patients waiting beyond recommended timeframes.
While Category 1 patients (cancer or life-threatening conditions) in most circumstances receive treatment in the appropriate time frame, most patients on overdue lists are Category 2 and 3 cases whose conditions, though clinically significant, are categorised as being lower in the scale of clinical prioritisation. The lack of ringfenced essential surgery beds in our regularly overcapacity hospitals means these lower-priority surgical patients face long and unpredictable waiting times.
These numbers represent system strain but also an inherent risk to patients. Prolonged waiting times can lead to harm in some cases, for example delayed cancer diagnosis (for non-urgent diagnostic procedures) or the risks associated with acute deterioration: physical deterioration, quality of life, psychological distress and


increased rates of emergency presentations. Crucially, vulnerable populations and regional communities bear the greatest burden of this reduced access.
Addressing this crisis requires a multifaceted strategic approach. It can begin with an audit of urgency categorisation to ensure they are applied appropriately, with regular review and audit of cases prone to ‘category creep’ or inconsistency within specialties and across networks. Resourcing must include sufficient time allocation and adequate numbers of specialtyspecific surgeons to lead multidisciplinary review panels to achieve this.
Targeted resource allocation and investment form the foundation of any meaningful reform and it is no different for elective surgery. Other states and jurisdictions have demonstrated the effectiveness of pre-planned, dedicated surgical blitzes – concentrated periods of additional operating capacity strictly focused on reducing overdue lists – by directing surge resources to address the most acute specialty bottlenecks. Redirecting investment to increasing operating theatre access for ‘pure’ elective surgery cases, funding presurgical optimisation programs, and ensuring the right configuration of workforce is a strategy that is within the gift of the system – even within the constraints of bed capacity. Targeting the longest waiting lists are an obvious strategic action that will reduce the overdue lists.
Private sector outsourcing is now a recognised strategy for managing public essential surgery pressures across Australia. In South Australia, a standardised, centrally administered outsourcing framework that recognises the commercial realities and operational requirements of private hospitals – including appropriate contract terms, pricing structures and administrative processes – will create a sustainable partnership to address backlogs. These contracts
must guarantee transparent case selection and patient transfer, equivalent clinical standards, credentialing and aftercare, plus comprehensive documentation that outlines outcomes, complications and equity of access. Long-term agreements guaranteeing case volume reduce uncertainty for both public and private hospitals while supporting throughput during public capacity challenges.
Any extension of outsourcing and the individual hospital contracts must protect surgical specialty training opportunities, with trainee involvement in outsourced cases mandated by contract where appropriate, ensuring trainees maintain logbook opportunities. Accredited units and active partnership with the Royal Australasian College of Surgeons will maintain standards while addressing bottlenecks and supporting the next generation of surgeons.
An opportunity exists for establishing more regional training posts – particularly for general surgery – by including rural hospitals in training networks, enabling trainees to gain broad specialty exposure while contributing to workforce resilience in under-served regional areas.
In addition, establishing a general surgical service in every major regional centre with the appropriate supports (operating theatres, anaesthetists, operating theatre and recovery nursing, and allied health) will reduce pressures on metropolitan surgical services and provide equity of access for regional patients. For specific specialties, such as ENT, plastic, orthopaedic and ophthalmic surgery, incentivising visiting subspecialists while investing in day-surgery and shortstay surgical capacity in regional hospitals is another action that can reduce waiting lists.
Supporting infrastructure must include opportunities for innovative models of care that include pre-surgical optimisation through allied health ‘prehab’ clinics – in both metropolitan and regional centres, telehealth consultations and transfer logistics to ensure regional patients can access the care they need.
A comprehensive, multifaceted strategy to manage essential surgery pressures recognises that addressing surgical backlogs requires that we reform how we prioritise, deliver and support surgical care across our state.
It is not acceptable that thousands of South Australians are overdue for essential surgeries. The system must respond to ensure this does not become normalised. System-wide thinking, strategic investment and coordinated innovative reforms are essential to restore trust and deliver on our health system’s promise of timely, equitable and high-quality surgical care.
29
The Grattan Institute’s recent report on non-GP specialist fees highlights critical issues in Australia’s health system – from outdated Medicare rebates to long public hospital waiting times. AMA President Dr Danielle McMullen says the report underscores the need for reform, transparency, and investment to ensure patient choice and access to timely, affordable care.

Many of you will have seen the Grattan Institute’s report into non-GP specialist fees, and the surrounding media coverage, some of which portrayed these fees in a very negative light.
While much of the media coverage at the time was unbalanced, the report – published in June –acknowledged the urgent need for reforms in both our public and private sectors to ensure patient choice and access to affordable care in a timely fashion. This included a call for a review of MBS items to ensure Medicare rebates are keeping pace with the rising costs of delivering timely, high-quality healthcare to all Australians.
For those of us working within the health system, the issue of lagging rebates comes as no surprise. It simply formalises what we have been experiencing firsthand: a funding model increasingly out of step with the realities of clinical practice and patient demand.
Medicare rebates have lagged inflation for years, and we welcomed the report’s recognition that it is time for a review of rebates to ensure they reflect the real costs of providing care.
At the Australian Medical Association, we also support greater fee transparency, and will work with the federal government to finalise its enhanced medical cost finder website to ensure patients are better informed about the potential fees they might face for private specialist care.
However, the report goes too far in suggesting the government should deny patients access to their Medicare rebate simply because of their choice of specialist. This is an ill-thought-out response that deflects blame for a very complex issue.
We recognise there are significant issues in the private health system, including a lack of oversight across the entire system. We will continue to call for an independent Private Health System Authority to oversee reforms that would support a more sustainable private health system – one that protects patient choice and clinical autonomy.
Our Clear the Logjam campaign has shown just how much pressure our public hospitals are under after years of underfunding by governments.
This report is yet another reminder of the long delays patients face when trying to access care through the public hospital system, particularly for outpatient services.
It is time for all governments to reach agreement on a new and properly funded National Health Reform Agreement to bring down these unacceptable waiting times.
We also welcome the report’s recognition of the need for an independent national workforce planning agency to ensure Australia’s medical workforce has the right skills, in the right places, to meet future community needs and demand. The AMA has long advocated for the creation of such an agency.
Targeted investment in a sustainable, well-distributed health workforce – including investment in rural and regional training – is essential to ensure every Australian, no matter where they live, can access the care they need, when they need it.
Rest assured, we will continue to advocate on behalf of you and your patients. Together, we can build a health system that is fair, transparent, and fit for the future.

Doctors are a vital part of South Australia’s return-to-work scheme, but current funding models are putting that system at risk. AMA SA Vice President Dr Louis Papilion outlines the case for reform and calls for fair, sustainable remuneration.
Return to Work South Australia (RTWSA) is an essential part of our social safety net, helping injured workers recover and return to employment. The system depends on clinicians providing timely, high-quality care. Yet many of our members report that this is becoming increasingly difficult.
The reasons are clear: more paperwork without adequate compensation, and item numbers whose remuneration has been stagnant for years. Together, these pressures have eroded enthusiasm for participation and placed the sustainability of the program at risk.
Ultimately, when clinicians feel devalued, patient access to timely care is reduced. This undermines the very purpose of the RTWSA scheme – delays in assessment and treatment compromise recovery, extend time away from work, and increase the likelihood that patients will fall back on the already overburdened public system. In short, the current funding model risks shifting cost and pressure elsewhere, weakening the program’s effectiveness for the very people it is meant to serve.
South Australia has legislated that remuneration for RTWSA services is set at the “average private fee” for each item. National data is retrieved from Medicare and bundled in a way that is opaque and difficult to interpret.
The result is clear: South Australian practitioners are reimbursed significantly less than their counterparts in every other state and territory. Elsewhere in Australia, remuneration is set at AMA rates, our preferred methodology and a fair reflection of the value of services provided.
We believe the current collection and calculation methods are flawed. Two years ago, AMA SA uncovered proof of this. Anaesthetic item numbers had been frozen for 14 years, despite clear evidence they no longer reflected reality. After persistent advocacy and detailed analysis, we secured an 85% increase in remuneration for anaesthetists across all item numbers. This was a major step forward, but it still falls short of parity.
More recently, we have identified similar discrepancies in GP and non-GP specialist item numbers. We requested an increase across the board, but unfortunately the adjustment was not extended to surgeons or general practitioners. This work is ongoing, and our commitment remains firm: to ensure all specialties are treated fairly.
RTWSA has pointed to increasing clinician participation as evidence that current rates are not a disincentive. We disagree. While participation has not yet declined, member dissatisfaction is rising, and we see this as the canary in the coal mine. Fair remuneration is not simply about dollars; it is about sustainability, quality care, and clinician willingness to engage with a demanding system.
Our goals remain clear:
• Adoption of AMA rates for all RTWSA services, legislated into law. This would bring South Australia into line with every other state and territory, ensuring equity and removing the need for annual fee disputes.
Streamlined approvals and paperwork, with appropriate compensation for essential reporting. Clinicians are willing to provide detailed reports where necessary, but the current burden is excessive, inefficient, and demoralising.
Every year AMA SA and RTWSA undertake a lengthy review process to negotiate fees for the following year. This is costly, time-consuming, and an unnecessary burden on taxpayers. Our proposal would eliminate this cycle entirely. By legislating AMA rates, the system would gain certainty, fairness, and efficiency, allowing both RTWSA and AMA SA to focus on their core missions rather than annual disputes.
It is important to acknowledge the wins and commend the hard work of the AMA SA team. But our focus has not wavered. We will continue to pursue reform with persistence, evidence, and professionalism, because this is what our members, and their patients, deserve.
Finally, I would like to thank the RTWSA team for two years of constructive dialogue. While differences in perspective are inevitable, our discussions have remained respectful and productive. This provides a strong foundation for further progress, and we look forward to building on it.

Dr Louis Papilion is a specialist anaesthetist and AMA SA Vice President.
At its 7 August meeting, AMA SA Council unanimously reappointed Dr Karen Koh as Chair for another 12 months. Dr Koh invited intensive care doctor Dr Krishnaswamy Sundararajan and anaesthetist and AMA SA Vice President Dr Louis Papilion to provide updates from their specialties. Dr Sundararajan raised ongoing concerns around ICU bed block and limited downstream capacity, noting that high occupancy continues to strain services. Dr Papilion highlighted persistent contract inconsistencies across local health networks and said some lack contracts altogether.
Council also received an update on the Access to Care Round Table – a major AMA SA initiative that brought together key stakeholders earlier this year, to address systemic barriers to timely, coordinated care. The resulting recommendations – now submitted to the Minister and SA Health – were well
received, and Council stressed the importance of maintaining momentum and ensuring accountability in follow-up discussions.
Concerns were also raised about the design of the new Women’s and Children’s Hospital, particularly regarding clinical space and emergency access. Council agreed to escalate these issues and pursue public advocacy.
Finally, Council endorsed a strategic campaign to elevate general practice in South Australia, including a targeted lobbying strategy to address Medicare reform, payroll tax and public perception challenges.

Dr Raj Ramadoss, Intensive Care Representative
AMA SA Council Position
• Ordinary Member (GP)
AMA SA Committee Positions
Doctors in Training Committee Representatives
• Doctor in Training from WCHN
• Doctor in Training who is an IMG
• Doctor in Training undertaking GP training
IMG Committee Representatives and Members
• Doctor in Training representative
• Two General Members
The new AMA SA Doctors in Training Committee chair, Dr Elise Witter, brings a passion for doctor wellbeing and advocacy to South Australia. From tackling bullying and harassment to improving access to events and resources, the committee is committed to improving working conditions for the state’s junior doctors.
I have been delighted to take up the position of chair of the AMA SA Doctors in Training (DiT) Committee after recently moving to Adelaide from Queensland, where I held an equivalent position. I am a stage-3 psychiatry trainee currently practising at the Royal Adelaide Hospital and have a particular passion for DiT wellbeing. Despite the differences between states (especially in the weather!), there are many similar issues facing DiTs in South Australia. These have been highlighted by the recent Hospital Health Check, which identified disappointingly high rates of bullying, harassment and discrimination that continue to affect junior doctors in the state’s major public hospitals doctors in training. Bullying and harassment are known to have adverse impacts on doctor wellbeing and, ultimately, clinical outcomes and patient safety. I look forward to continuing the work of outgoing DiT Committee members in identifying and advocating for safe reporting pathways and other strategies to tackle these systemic issues.
Advocating for access to adequate workspaces –along with essential resources such as computers – remains a priority for the DiT Committee in 2025. We’re also focused on increasing member engagement by delivering targeted events and other meaningful benefits for DiTs and medical students. In addition, we’re looking to expand collaboration with other organisations and forums representing doctors in training – helping to maximise our collective impact.
Earlier this year in May, I represented DiTs at the AMA SA Access to Care Round Table. This was an excellent opportunity to discuss issues related to access to care with stakeholders including Health

Minister Chris Picton and Federal AMA President Dr Danielle McMullen. This forum has led to a series of recommendations, including enhancing the interoperability of communication and patient medical record systems, enhancing access to outpatient clinical care and how to capitalise on technology to overcome barriers in access. DiTs concerns were highlighted to more than 30 leaders from various sectors and organisations, contributing significantly to the conversation and recommendations. The DiT Committee looks forward to working with other AMA SA members and SA Health to implement these recommendations and improve access for South Australian patients.
Finally, there are a number of events DiTs have enjoyed this year. I must congratulate former chair Dr Hayden Cain, who was honoured with the Rising Star award at the AMA SA Gala in June. Our speed networking events have been incredibly popular, with the most recent on 24 July receiving a big tick of approval from junior doctors and students. We are continuing to explore other suggestions for events that can deliver maximum benefits to DiTs. The DiT Committee is always eager to hear from our members – whether it’s ideas to improve your experience, challenges you’re facing, or interest in becoming involved with the committee and our events. We welcome your input –please contact us at any time!
‘I SPEAK TO A LOT OF STUDENTSHERE’S WHAT’S WORRYING THEM’
This year I’ve had the privilege of speaking with hundreds of medical students at events, meetings and around campus. And while I am asked all sorts of things (yes, including ‘What’s the MedBall theme this year?’), one question keeps coming up: ‘Do I need to do research to succeed in medicine?’
The pressure is real. Over the past six years research has increasingly felt, for many, like a high-stakes currency for our careers rather than a space to explore interests and do meaningful work. As Adelaide Medical Students’ Society (AMSS) President this year I have tried my best to lead by example – not by discouraging research by any means, but by reminding students that there is no single path to success in medicine. If we reduce medical school to a race for publications, we lose sight of the deeper purpose of why we’re here.
The AMSS has been discussing in depth this year that if students are engaging in research purely from fear and not interest, we face a major risk of promoting performative CV-bulking. When research becomes something students do from fear rather than passion, we risk burnout, not better doctors.
Beyond research, students have also voiced concerns about the broader healthcare system. The AMSS has collaborated with South Australian Salaried Medical Officers Association (SASMOA) and we share many of the same concerns about workforce conditions. Students are watching closely, not just to see what the internship landscape looks like but to find out whether the system will support us as we step into our careers. We continue to hope that we, and our older peers in the hospital system, are walking into a system that values and supports us. We remain optimistic because of the incredible resilience and camaraderie within our medical community that inspires confidence for the future.
These are big questions and heavy considerations for a 23-year-old (and often these conversations extend well beyond my paygrade!). But to me, these conversations are a sign of something hopeful. They show that students care deeply. Students care about our profession, our future patients, and, most importantly, for each other. This gives me enormous optimism about what the future holds.
As a representative of the student body, I believe it is important to continue challenging narrow definitions of success in medicine. I believe the student body is turning a corner – valuing curiosity over competition and collaboration over comparison. I hope I enter a workforce where students feel empowered to follow their passions and define success on their own terms.


It has been a whirlwind of a past few months, to say the least. Not only have students wrapped up their final exams for semester one, but many final-year students have also been jet-setting off to and from their international medical school electives. I, for one, had the most amazing time in Oxford with my fellow Senior Vice President, but have returned to Adelaide both fascinated and dumbfounded by some of the stories from my colleagues who explored the jungles and major trauma centres of South Africa, the streets of Taiwan, and the canals of Venice.
While I was away, the Flinders Medical Society magic continued to flourish. There have been numerous events for all students to engage with. Leading up to and following exams – and to combat that seasonal depression – we really wanted to focus on mental health during the winter months. It was lovely to see our yoga sessions take off, as well as excitement brew for our Mental Health in Medicine Seminar – an event that highlights the importance of doctors taking care of themselves before they can take care of their patients. All too often, we see our sacrifices for our patients overshadowing our own mental wellbeing.
This year has not only marked the 50th anniversary of FMSS but also the 50th year of honouring and uplifting Indigenous voices, culture, and resilience through observing NAIDOC Week. To commemorate the occasion, our committee organised a ‘Wear It Yellow’ day, as well as a screening of the Indigenous film Last Cab to Darwin. Thanks to our passionate Indigenous Education Lead, we also launched an Indigenous Workshop Series, with four workshops covering areas such as reproductive health, palliative care, mental health, and nutrition.
To celebrate our own 50th anniversary, our students have been proudly showing off this year’s special edition line of merchandise. We also hosted our largest-ever Medical Ball at the Hilton Hotel – a night that truly showed medical students don’t just scrub in –they scrub up into stars. On the night, students danced freely above the treetops, toasted beneath the stars, and allowed themselves to be completely – joyfully –‘up in the air’, which was the theme of this year’s ball.

FMSS was also privileged to hold a bake sale fundraiser for Daffodil Day, with all proceeds donated to Cancer Council. Additionally, we brought out our competitive sides to face off against our Adelaide Medical School friends at the annual Intersociety Soccer Tournament. While we didn’t take home the trophy, rest assured FMSS will be back with a vengeance next year.
It was with great pleasure that I attended the AMA SA Women in Medicine Breakfast alongside Sara Bilwani, the AMSS President, to celebrate the commitment of women over the years within the medical sphere. What a truly inspiring event. It was also a privilege to represent medical student voices in the media, advocating for better working conditions and remuneration for junior doctors at a recent press conference.
Overall, it has been an incredible year so far, and every day I am reminded how truly honoured I am to serve this society as President. With internship offers rolling out, I look forward to commencing as a junior doctor at the Royal Adelaide Hospital and wrapping up unfinished business as we launch into the final few months – where I get to pass the baton to next year’s executive committee.

Creating quality commercial property investment opportunities.

For doctors and medical professionals seeking a reliable and diversified income stream, commercial property funds can offer an attractive balance of regular distributions and long-term capital growth.
THINKING OF INVESTING IN AUSTRALIAN COMMERCIAL PROPERTY?
Make a time to meet with Director Adrian Rivish, to find out more about commercial property investments and FRP Capital.
Scan the QR Code to book a meeting or email adrian@frpcapital.com.au


The AMA 2025 National Conference (AMA25) brought healthcare professionals from across the country to Adelaide for two days of lively discussions about some of healthcare’s most pressing challenges.
The annual event, staged this year at the Hilton Adelaide from 1 to 2 August, featured clinicians and other healthsector leaders who delved into topics such as chronic disease prevention, AI integration, cybersecurity threats and regulating telehealth.
AMA SA was well-represented at two of the breakout sessions. There was standing room only as former AMA SA President Dr Chris Moy led a session on achieving the most from campaign efforts. AMA SA Road Safety Committee Chair Dr Monika Moy reinforced that road safety is a public health issue and described the most pressing new factors contributing to rising road-trauma numbers.
Australian Health, Ageing and Disability Minister Mark Butler addressed AMA25 attendees, crediting the national AMA for Labor’s GP workforce policies and acknowledging how AMA policy efforts have directly influenced government decision-making. AMA SA member and former Australian of the Year Dr James Muecke outlined the latest research into the impacts of processed food on human health.
Q&A sessions and soapbox discussions on national health policy maintained the momentum, with attendees actively engaging in robust debates about healthcare reform and the future of Australian medicine.
AMA President Dr Danielle McMullen thanked all speakers and attendees for contributing to the success of the conference.
‘There were so many informative and inspiring sessions –the depth and breadth of knowledge on hand was quite something,’ Dr McMullen said.



AMA25 attendees heard that advocacy based on strategic planning and evidence can bring mutually beneficial results – and ensure campaigners with fire in their bellies don’t have their passion extinguished.

The importance of AMA advocacy and the role of each member in promoting AMA positions and their patients’ interests was evident in an AMA25 session dominated by debate over how AMA representatives can ‘win’ when looking to influence decision-makers.
The promise of a lively discussion under the direction of former AMA Vice President and AMA SA President Dr Chris Moy meant there was standing room only when Dr Moy introduced the ‘Navigating Influence’ session panellists: former AMA President Dr Omar Khorshid, AMA SA CEO Nicole Sykes, AMA Tasmania CEO Lara Giddings and AMA NSW President Dr Michael Bonning.
Dr Moy said doctors should understand that taking calls for more funding or a policy change to political leaders is only a step further along the campaign pathway from daily efforts to improve their patients’ access to care.
The panellists brought to the discussion a combination of clinical, health, political and business expertise that
Dr Moy channelled into a robust examination of how advocacy works – and when it doesn’t, why.
Dr Moy noted that while some younger members may wish to ‘burn the place down’, and others may become cynical if their efforts are unsuccessful, holding ‘a seat at the table’ has come after decades of relationship building for successive AMA leaders.
He said that once a meeting had been scheduled, it was critical to align the argument to the audience. For example, he suggested, if you’re meeting a health minister about climate change, talk about health impacts of climate change in Australia – don’t point out the accelerated melting of polar icecaps.
Dr Khorshid said he knows now that ‘my entire career at the AMA and being a doctor, I’ve been an advocate’.
‘Advocacy is influencing decision-makers to make a decision that you think is right. It might be for a patient, a colleague, yourself – or it might be a public health issue that affects every one of us.
‘YOU HAVE TO WORK OUT HOW TO ASK FOR YOUR GOAL SO IT’S A WIN FOR YOU BUT ALSO A WIN FOR EVERYBODY ELSE.’
- Former AMA Vice President Dr Chris Moy
‘You need a bit of courage, you need patience, resilience. Because change takes time.
‘It can be easy to become disheartened and cynical, and to give up. That’s what most people do. They have a good idea, they can’t understand why everybody else can’t see it, and they give up.
‘You need to be strategic. You need to think about who the decision-maker is and how you can influence them.’
Ms Sykes said she had learned in her two years at AMA SA that you can apply business principles to advocacy.
‘You must be able to articulate what the problem is and you need to know what you’re trying to achieve,’ she said. ‘And take the time to map the journey: strengths and weaknesses, who you should have on board to help drive the change you want.
‘There is strength in numbers, I’ve heard many stories from members who’ve tried to influence change by themselves with little to no response.
‘At its basis, it is about building relationships with key influencers, making sure you have the right experts at the table, and having those with factual information and lived experience tell their stories.’
Dr Bonning said the best advocacy ‘is when we can walk away from the table and someone else thinks it’s their idea’.
‘If you can help someone come to their own rational thinking of the idea, you win. Because they will take that idea far further than you will, and they have the levers they can pull to achieve it.’
Dr Bonning said doctors have an advantage in being able to present evidence-based arguments to explain their ‘agendas’.
‘Doctors always have an agenda,’ he said. ‘Every patient walks in with an agenda. You have an agenda for what you want to do for them; they have an agenda in what they think you should do for them. And you reach some kind of outcome.
‘Politicians, health officials – they’re no different. They have an agenda; you have an agenda. We can come at it from a position of recognising that there’s often significant overlap. … Politicians don’t want problems; they want someone with expertise to bring them an answer.’
It was the insight of Ms Giddings – who had sat ‘on the other side’ as a former Tasmanian Premier and health minister – that articulated the need for advocates to walk into important meetings with a clear idea of what they want and to be able to express why the ‘ask’ will help the decision-maker, too.
‘The collective voice of the AMA is important,’ Ms Giddings said. ‘(A Minister hears) hundreds of individual voices and can’t respond to all of them.
‘But when you know you have a funnel for that idea and it’s coming up through a collective, you stop and you give time.’
1. Know your audience. Don’t assume a level of understanding. Respectfully ask the open question of how much they know at the beginning. It opens a conversation without you being patronising.
2. Own the cost and show the value of your ‘ask’. Don’t go in pretending there won’t be a cost, so be prepared to explain the value of the financial cost and to describe the benefit for the decisionmaker – how it’s going to fix a problem.
3. Help them own the idea. Get them to the point where they feel like they own the idea and will receive some of the credit.
4. Have a specific ‘ask’; describe the outcome you want to achieve and how.
5. Use evidence to tell the stories that will have an impact.
6. Timing is everything.
7. Do not be a zealot. Don’t offend people. Things are never black and white. There are always shades of grey.

E-scooters, medical cannabis and smart phones are among innovations having real but as yet unmeasured effects on the safety of drivers and pedestrians.
Mobile phones, and particularly smart phones, have been shown to increase a car driver’s crash risk four-fold, with distraction having a substantial effect on drivers’ capacity to stop quickly.
AMA SA Road Safety Committee Chair Dr Monika Moy told AMA25 attendees she is ‘constantly amazed’ at the number of her general practice patients who believe it is acceptable to conduct a telehealth consultation while they are driving.
‘It is really very common,’ she said. ‘The sound of the indicator will often give this away – when I hear that, I ask that they please pull over and call reception back when they are parked.’
She said there is ‘ample evidence’ that the advantage of hands-free as opposed to hand-held phone use in reducing collisions is ‘really quite minimal’.
‘It will be interesting to see how public opinion and legislation develop in this area,’ she said, ‘as there is no doubt the use of hands-free phone use has become quite normalised because there is the perception that it is safe.’
Dr Moy told conference delegates that the AMA SA Road Safety Committee – the only AMA committee
that exists solely to improve road safety – advocates for changes that will reduce the number of deaths and injuries on the state’s roads.
Committee members include AMA SA members, an SA Police representative, a road safety consultant, Adelaide Lord Mayor Dr Jane Lomax-Smith and a director of the University of Adelaide’s Centre for Automotive Safety (CASA), A/Prof Jeremy Woolley.
‘We believe road trauma is a public health issue,’ Dr Moy said. ‘There were 1,300 deaths on Australia’s roads in 2024 … This is a number that is increasing.’
She said trends show that the number of road deaths has increased year on year since the pandemic reduced traffic and associated road trauma in 2020.
She said the reasons are ‘unknown and likely to be multifactorial’. Some factors have contributed to the road toll for decades – with speed and alcohol ‘the obvious ones’ – but new factors including mobile phones are having an increasing impact.
‘We know the greater the speed and the greater the alcohol concentration in your blood, the more likely you are to have a casualty crash,’ Dr Moy said. ‘Progress has been made in (addressing) both of these, but they haven’t gone away.’
‘Cannabis is not new,’ Dr Moy pointed out. ‘Nor is driving after consuming cannabis. But for the first time in Australia we are seeing people driving with cannabis in their system because it has been legally prescribed to them by a doctor.’
Dr Moy said that until recently it’s been illegal in all states and territories in Australia with any detectable concentration of THC – the psychoactive component of cannabis that impairs the driving task – in the system.
This has recently changed in Victoria and Tasmania. It’s now legal to drive in Tasmania with detectable levels of THC, provided it’s been legally prescribed and provided there is no obvious impairment.
In Victoria, it’s still technically illegal, but penalties may be waived at the magistrate’s discretion if it’s been legally prescribed.
South Australia has legislation before Parliament that is similar to that of Victoria, but it’s yet to be passed.
‘The upshot of this is that we are now going to have people legally driving with THC in their system. There have been several studies looking at (the effects) and the results are inconclusive.
‘However, there is good evidence that THC does cause impairment. There is a lot of individual variability (in reactions), it’s hard to measure, and there is a very inconsistent link between blood levels and the saliva levels that are tested in roadside testing.
‘There is also an inconsistent link between blood levels, saliva levels and the amount of impairment; there is also variability in the duration of the effects, which can last between four hours and 10 hours after ingestion.
‘There is variability depending on mode of delivery and individual susceptibility.
‘Because of the inconsistent link between saliva levels and degree of impairment, it means an “allowable level” can’t be easily applied to cannabis as we have with alcohol.’
E-scooters, e-skateboards and Segways are among the personal mobility devices (PMDs) having an impact on road trauma numbers, with e-scooters the most prevalent.
‘There is no doubt there are some positives associated with these PMDs,’ Dr Moy said. ‘They allow

easy movement, particularly around the city centre, can be enjoyable and have the potential to reduce emissions, especially when they replace car journeys.
‘However, despite these positives it cannot be said that these devices come without risk to both the riders and other road users, including pedestrians.
‘Unfortunately, we lack clear data on injury rates. Better data collection is sorely needed.’
The Victorian Injury Surveillance Unit has found that in Victoria, between 2018 and 2023, ED presentations included 1,680 e-scooter injuries. Nationally there were 14 deaths involving e-transport devices between 2016 and 2020.
In South Australia, recently introduced legislation allows privately-owned e-scooters to be ridden on roads and footpaths.
Dr Moy said there was a risk to pedestrians, not only in the experienced impacts but in ‘perceived risk’.
‘As health practitioners, we want our most vulnerable patients to participate in an active and engaged lifestyle and to feel confident walking down the street,’ Dr Moy said. ‘This is not what I’m hearing from a lot of my aged and infirm patients. There is a lot of fear.’
‘WE ARE NOW GOING TO HAVE PEOPLE LEGALLY DRIVING WITH THC IN THEIR SYSTEM.’
- AMA SA Road Safety Chair Dr Monika Moy
The AMA presented its annual awards at the National Conference, recognising outstanding achievements and honouring those who exemplify medicine’s highest values.


Perth GP Dr Rajeshwary (Raji) Krishnan received the President’s Award for her dedication to improving health outcomes for multiple generations of First Nations families and establishing a multidisciplinary general practice for marginalised members of the community.

Brisbane-based senior gastroenterologist Adjunct Professor Tony Rahman was awarded for his deep commitment to helping homeless people, refugees and the vulnerable to access healthcare, and for his leadership in gastroenterology nationally and internationally.

Newcastle-based paediatrician and researcher Dr Rebecca Healey was acknowledged for her groundbreaking research and advocacy on behalf of international medical graduates.
Dr Dominic Edwards was acknowledged for his outstanding service in advancing and prioritising women’s healthcare. Dr Edwards is the Obstetrics and Gynaecology Principal House Officer at the Mater Mothers’ Hospital in Brisbane. He has also worked in Cambodia and Uganda, helping address high maternal and neonatal mortality.
Former AMA presidents Dr Tony Bartone and Dr Omar Khorshid were joint winners of the 2025 AMA Gold Medal – the organisation’s highest honour – for their leadership during the COVID-19 pandemic. AMA President Dr Danielle McMullen said both men were ‘unflappable’ during the worst health crisis Australia had endured in 100 years.
GP Dr Kim Loo and psychiatrist Dr Pramudie Gunaratne, both based in Sydney, were joint recipients of the Women in Medical Leadership Award for their unwavering commitment to promoting women in medical leadership, improving quality care, and influencing medical politics.

ACT clinician Dr Marrwah Ahmadzai was recognised for her outstanding work in women’s healthcare, the provision of culturally safe healthcare and combating racism in the healthcare system.



Former AMA ACT President Prof Walter Abhayaratna was recognised for his outstanding leadership in health research and advocacy.

South Australian medical student Samantha Nillissen is one of three students who were awarded AMA Indigenous Medical Scholarships at the National Conference.
The Flinders University student, who is also an Aboriginal midwife, said she’s faced more than just academic hurdles on her path into medicine.
‘I’ve been homeless twice. I know what it means to live on the margins – feeling invisible within a healthcare system that doesn’t always recognise the realities of time or lived experience,’ Ms Nillissen said.
‘These experiences opened my eyes to the deep disparities that exist and gave me a clear sense of purpose: to fight and advocate on behalf of the vulnerable.
‘I want to be a doctor who truly sees people, understands their context and helps build a more compassionate and equitable healthcare system for all.’
Ms Nillissen received the scholarship along with Barundji man Myles Mackenzie, a medical student at Queensland’s James Cook University and Wongutha, Ngarluma and Wudjari-Noongar woman Kayla Williams-Tucker, who is studying at Western Australia’s University of Notre Dame.
This is the first year it’s been financially possible to award three scholarships in a single year. Each one is worth $11,000 per year for the remainder of the student’s degree.
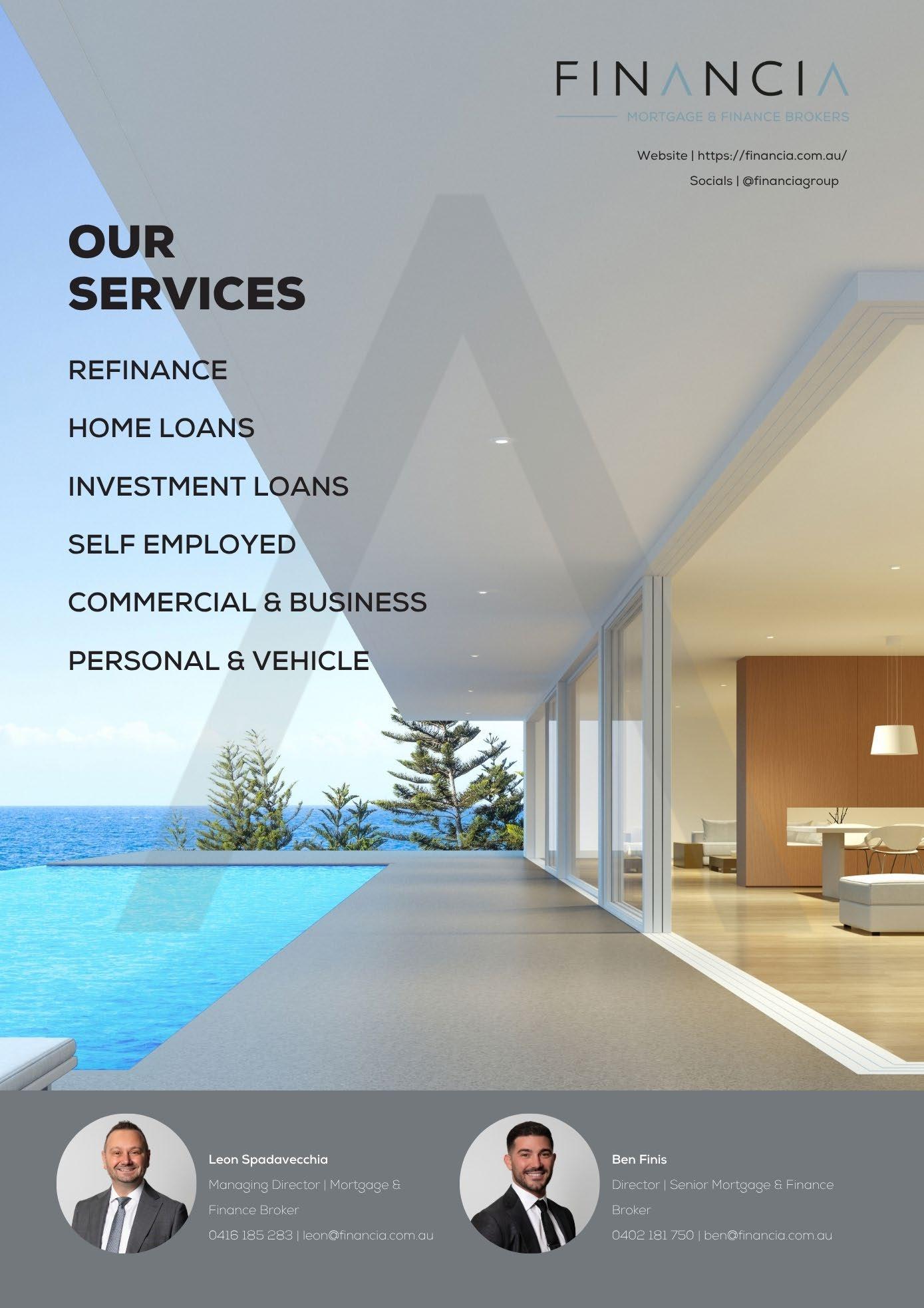
AMA President Dr Danielle McMullen warns of the dangerous rise of deepfake technology, which is increasingly being used to spread misleading and even harmful medical information.

I first discovered a fake social media profile impersonating me when a family member called to ask if I really believed in what I – the fake version – was selling.
I felt a rush of emotions: confusion, concern, and disbelief. How could this be allowed to happen?
All online scams are insidious, but they become particularly dangerous when they involve healthcare.
Since discovering the fake Dr McMullen on Facebook, I have made several attempts to have her removed.
Unfortunately, my efforts have been futile. It feels like an endless game of whack-a-mole – and the scammers are winning.
It seems I got off relatively lightly, though. Other prominent clinicians, including Dr Norman Swan and former AMA president Professor Kerryn Phelps, have had their identities misused in ‘deepfake’ videos that promote unproven health products.
The companies behind these products use artificial intelligence technology to replicate the appearances and voices of reputable health professionals with astonishing accuracy.



A fake Dr Swan was shown calling scientific evidence ‘stupid’, while selling supplements claiming to treat heart disease, diabetes and obesity.
Professor Jonathan Shaw, one of the world’s most cited researchers, appeared in a deepfake ad urging people to stop taking prescribed medication in favour of an unproven alternative.
‘If you know me, it’s clearly fake,’ the real Professor Shaw wrote in the AMA Vicdoc magazine. ‘But for members of the public, it was unfortunately very convincing.’
These scams aren’t just a health risk – they’re a financial one too. Vulnerable Australians are being tricked into buying products that don’t work, or don’t even exist.
Deepfake technology is becoming more convincing by the day. We now live in an age where every video must be questioned: is it real, or is it AI-generated? And if it’s AI generated, is it sanctioned, or a scam? Believe it or not, ‘AI influencers’ are now a thing. ‘Mia Zelu’, an AI-powered social media ‘influencer’, has amassed more than 160,000 Instagram followers by sharing fake, AI-generated content of herself at events such as Wimbledon.
‘THE AMA WILL CONTINUE TO ADVOCATE FOR A DIGITAL ENVIRONMENT
– NOT DECEPTION.’
When we talk about AI here at the AMA, we talk about its potential to transform healthcare, offering innovative solutions to long-standing challenges (with appropriate guardrails, of course).
From faster diagnostics to slashing administrative burdens, AI is unlocking new possibilities.
Machine learning is improving medical imaging and data analysis, while predictive models are enhancing preventive care. AI-powered apps and wearables are already monitoring patient vitals in real time.
Many GPs are using AI tools to transcribe consultations and assist with notetaking. While the performance of these tools varies and caution is needed when using them, their potential to free up time for patient care is undoubtedly significant.
These examples barely scratch the surface of the potential of AI in healthcare. But with great potential comes great risk.
Patient privacy and data security are critical concerns, especially as AI relies on extensive datasets to function effectively. We have taken a leadership role in advocating for a regulatory framework that balances innovation with safety. In submissions to bodies such as the Therapeutic Goods Administration, we’ve outlined principles for responsible AI integration – with clinical oversight always at the core.
We’ve been clear: AI should support – not replace – clinician judgment. Regulations must ensure that final decisions remain in the hands of healthcare professionals, preserving the human element in care.
These are the important issues we should be discussing more – not deepfake scammers. But we must respond to the reality we face, and fortunately, we are nimble enough to tackle multiple challenges at once.
I recently wrote to Communications Minister Anika Wells, urging the federal government to act on deepfake content promoting harmful treatments. We’re calling for clear, enforceable regulations on healthrelated advertising online, including:
mandatory identification of the individual or company responsible for any online material promoting a medical product or service
• an accessible portal for individuals to report fake or misleading AI-generated or other content unsubscribing mechanisms to allow users to opt out of unsolicited medical advertising takedown requirements mandating platforms remove harmful content within a specified period after a complaint is lodged
• enforcement powers, including the ability to issue infringement notices for non-compliance.
This is not a problem we can ignore or leave to tech companies to solve on their own. We need strong, enforceable regulations that keep pace with the technology. We need accountability from platforms that profit from engagement irrespective of truth. And we need public awareness so Australians can better recognise and report harmful content when they see it.
The AMA will continue to advocate for a digital environment where innovation serves the public good – not deception. It’s time for government, industry, and the community to come together and draw a clear line: health misinformation – including when powered by AI – has no place online.

Financial advisers can make a significant difference to your future – but what exactly do they do, and how can you benefit from their expertise? Hood Sweeney’s Financial Planner Jackson Harvey explains.
When people mention the term financial adviser, most people picture someone in a suit talking superannuation, insurance or tax. While those areas are important, they barely scratch the surface of what real advice offers.
Because at its core, financial advice isn’t just about your money – it’s about your life.
So what does a financial adviser actually do?
We help you get clear on where you’re headed and build a plan to get you there – on your terms.
A financial adviser works with individuals and families to understand what matters most to them and builds a strategy to support those priorities. Whether it’s buying a first home, managing the financial demands of raising children, or preparing for retirement, advisers help navigate complexity and provide structure.
We act as a sounding board, a strategist and a steady hand during life’s unpredictable moments. Clients bring their goals; advisers bring the insight and experience to help make those goals achievable.
Because life’s too short to constantly worry about money. And sadly, too many Aussies are doing just that.
Many Australians feel uncertain about their financial future. Between conflicting opinions online, advice from friends, and constant changes in the economy, it’s easy to feel stuck or unsure about what steps to take.
That’s where professional advice steps in – objective, qualified and tailored to you.
Advisers help clients cut through the noise and focus on what’s relevant. Whether it’s choosing the right investment approach, structuring debt or planning for retirement, they provide a framework for making sound decisions.
Effective advice can literally save or earn you tens –even hundreds – of thousands of dollars over your lifetime. Whether it’s smarter tax planning, avoiding costly missteps or structuring your finances efficiently, it’s about making the most of what’s earned and keeping more of it.
Financial uncertainty is one of the biggest causes of stress for Australians. With a plan in place, you’ll sleep better at night knowing you’re on track, protected and prepared for whatever life throws at you.
Our clients don’t just receive recommendations – they gain understanding. Advisers explain the rationale behind each strategy, empowering clients to take ownership of their financial journey, long after the meetings are done.
Your goals and circumstances will change, and we’ll be there to adjust your strategy as life evolves. New job? New baby? New house? Business opportunity? Family member passing? Relationship breakdown? We’re by your side, helping you adapt and navigate each turn in life’s journey, your journey.
At Hood Sweeney Securities*, trust is the foundation of every client relationship. The team is guided by three core principles:
Integrity – Always acting in your best interest. No fluff, no shortcuts. Just honest, reliable advice.
• Ultimate transparency – Clear communication about fees and services. You’ll always know what you’re paying for, and what services you receive. No fine print. No surprises.
• Education – Financial wellbeing starts with understanding. Clients are encouraged to engage with their financial journey, not just follow it. You don’t have to know every detail, but you need to know why advice has been provided and what path you wish to go down. The more you know, the less you’ll worry.
Financial advice isn’t reserved for the wealthy – it’s for anyone who wants to take control of their future. It’s about creating freedom: freedom from money stress, freedom to make confident choices and freedom to prioritise what truly matters – your family, your wellbeing, and your personal aspirations.
In a world full of financial ‘hot tips’, competing opinions and rising uncertainty, having a trusted and qualified adviser in your corner isn’t just helpful – it’s essential
Because when your financial life is well-managed, everything else becomes easier to navigate. And that’s what real advice is all about.
The information in this article contains general advice and is provided by Hood Sweeney Securities Pty Ltd AFSL 220897. This article has been prepared without taking your personal objectives, financial situation or needs into account. Before acting on this general advice, you should consider the appropriateness of it having regard to your personal objectives, financial situation and needs. Please refer to our FSG (available at hoodsweeney.com.au/ services/financial-planning/how-we-service-our-clients/ financial-services-guide) for contact information and information about remuneration and associations with product issuers.

Jackson Harvey is a senior financial planner at Hood Sweeney.
Representative of Hood Sweeney Securities AFS Licence No. 220897

Across the world each year, coronary artery disease (CAD) is responsible for approximately nine million deaths. Biomedical engineers at the University of Adelaide, led by Associate Professor Jiawen Li, are developing a 3D-printed imaging device which would help prevent recurrent incidents. A/Prof Li explains how the device works.
CAD is caused by the buildup of atherosclerotic plaques and although most plaques remain stable, some continue to destabilise until they rupture or erode. These can cause thrombotic occlusions which lead to MI or sudden cardiac death.
These deaths are preventable if we can identify and manage high-risk patients, as demonstrated in recent


For more information or to arrange an inspection of 34 Kensington Road, please contact:
• Saxon Smith of Higher Commercial (RLA 323 903) on 0477 859 659
• Zoe Lynch (Colliers) on 0451 273 884
• Sinamin Dominey (Colliers) on 0484 229 877

studies in the New England Journal of Medicine and The Lancet. However, the methods in these trials have not used a personally tailored approach. Existing technologies, including conventional angiography and intracoronary imaging modalities, suffer from poor predictive ability due to their intrinsic limitations, including low resolution and/or lack of molecular contrast.
34 Kensington Road, Rose Park SA 5067
Medical, allied health or office opportunity in premier location
Located within a sought-after medical precinct in Adelaide’s eastern suburbs, this soon-to-be renovated commercial space is ideal for medical, allied health or office use.
• Approx building area of 356 square metres
• Up to nine (9) consulting rooms, a reception, amenities and a substantial open-plan workspace
• Rear access via Eliza Lane with on-site parking for up to 12 vehicles
• High-exposure location with excellent signage opportunities, including an illuminated pylon sign to Kensington Road
• Just minutes from the Adelaide CBD and metres from The Parade, Norwood
Renovation is set for completion in late 2025 and will include new flooring, painting and plumbing, with basins installed in each consulting room.
Offering high exposure, convenient rear-road access, and close proximity to public transport, this is a rare opportunity.


There is great potential that with the right diagnostic methods, such as the 3D-printed imaging device, cardiologists can detect high-risk plaques and tailor management to improve outcomes using a personalised medicine approach in cardiology.
If only stable plaques were found in older people with high bleeding risk (which could be due to concurrent active cancer, or chronic kidney disease), cardiologists may decide to avoid invasive intervention with stenting, which necessitates the addition of further antiplatelet therapy, to prevent severe bleeding.
Conversely, if any high-risk plaques are detected, a more aggressive treatment with intervention and additional cholesterol-lowering/anti-inflammatory medication will be explored.
The key design feature of our 3D-printed imaging device is to combine the strengths of two complementary imaging modalities (autofluorescence and optical coherence tomography (OCT)) into a single 3D-printed imaging micro-lens, to assess both the biology and micro-structure of plaques.
As recently pointed out in the Journals of the American College of Cardiology, it is important to ‘consider both morphologic features and biological activity of plaques’. The integration of OCT and autofluorescence can meet this need without increasing patients’ risks by injecting any fluorescent dye, as autofluorescence is based on the intrinsic fluorescence signal generated by high-risk biological features of plaques like intraplaque haemorrhage or necrotic core or insoluble lipid.
By utilising the unique advanced manufacturing capability of our collaborators in Stuttgart, we are able to 3D-print the micro-lens thinner than the lens in a commercially available device and provide unprecedented capability to detect high-risk plaque characteristics.
Frontline cardiologists Professor Peter Psaltis and Dr Jessica Marathe, with whom I have been collaborating, see this device as a potentially transformative treatment paradigm shift. By identifying high-risk patients accurately, it is possible to avoid recurrent cardiovascular events by intensifying treatment with stents and targeted cholesterol-lowering or antiinflammatory therapies, while avoiding over-treatment for stable diseases.
This precision not only improves patient outcomes and limits risks of complications but also mitigates the uncertainty and anxiety many patients face.
• A/Prof Jiawen Li is a University of Adelaide biomedical engineer.
A Monash University study of almost 400,000 people is the first to indicate, in humans, that the signalling of substances called short-chain fatty acids or SCFAs, released when gut bacteria break down dietary fibre, protects against cardiovascular disease and hypertension by as much as 20%.
Lead author Dr Leticia Camargo Tavares said disruption in the receptors was shown to be associated with up to 20% increased prevalence of hypertension and heart disease or stroke – even after accounting for other risk factors like body weight and smoking.
The study used data from the UK Biobank database and found rare genetic variants that profoundly affect the function of receptors that bind to SCFAs essentially prevent people from utilising the cardiovascular protection offered by their own gut microbes.
The researchers compared the cardiovascular medical history of individuals with the genetic variants to the history of controls, finding that the affected cohort had a significantly higher incidence of hypertension and long-term risk of cardiovascular disease, including heart attacks, heart failure and stroke.
The authors noted that the genetic variants occur in less than 1% cent of individuals.
‘Rare pathogenic variants in G-proteincoupled receptor genes involved in gut-to-host communication are associated with cardiovascular disease risk’ (Cardiovascular Research, May 2025)
DOI: 10.1093/cvr/cvaf070
University of Sydney research has found that children are at a similar risk of dehydration and hyperthermia in extreme heat as adults, contradicting previous advice that children are more susceptible to heat-related illnesses.
The study was conducted at the university’s Heat and Health Research Centre in collaboration with the University of Canberra. In the largest controlled study of its kind, it looked at the effects of high temperatures (up to 40 degrees Celsius) on 68 children aged between 10 and 16 years.
Professor Ollie Jay said that children historically were thought to be more vulnerable to heat stress during physical activity due to factors such as having a higher body surface area-to-mass ratio compared to adults.
‘However,’ he said, ‘when we studied the effects of extreme heat on children and compared them with the effects on adults, we found that children aged between 10 and 16 did not sweat differently to adults and their bodies heated up by the same amount. As a result, they were not at a higher risk of dehydration or hyperthermia.’
Throughout the trial, participants’ core temperature was measured, with the rate of dehydration determined by weighing the participants before and after the trial using high-precision digital scales.
The research team has developed a Sweat Rate Calculator Though developed primarily for adults, the tool accurately estimates the fluid intake requirements for children based on measurements such as their height, weight, activity type and the temperature.
‘Thermoregulation and dehydration in children and youth exercising in extreme heat compared with adults’ (British Journal of Sports Medicine, June 2025)

A new study has found that a parent’s concern that their child is deteriorating in hospital is as strongly associated with serious illness as abnormalities in vital signs such as heart rate, breathing rate or blood pressure.
The research at Monash University’s School of Clinical Sciences at Monash Health demonstrates that listening to parents could play a crucial role in preventing adverse outcomes in paediatric patients.
The study introduced a simple question for clinical staff to ask parents during every vital signs check: ‘Are you worried your child is getting worse?’. The results showed that children whose parents said they were worried were significantly more likely to experience serious illness – even when their vital signs appeared normal.
‘If a parent said they were worried, their child was around four times more likely to require intensive care. That’s a signal we can’t afford to ignore,’ said researcher Dr Erin Mills.
The study highlights the need to formally integrate caregiver concern into hospital earlywarning systems, noting that current tools often rely solely on physiological measurements. Unlike escalation pathways such as Ryan’s Rule or REACH – which require families to initiate urgent reviews – this approach places responsibility with clinicians to routinely ask about concern.
The authors say parent concern should be included in clinical review processes and treated as an important source of information, alongside physiological signs.
‘Association between caregiver concern for clinical deterioration and critical illness in children presenting to hospital: a prospective cohort study’ (The Lancet Child & Adolescent Health, July 2025)

University of Queensland researchers have discovered a crucial link between the brain’s ‘cleaning system’ and deterioration of neurons associated with Alzheimer’s disease.
Professor Elizabeth Coulson, from UQ’s School of Biomedical Sciences and Queensland Brain Institute, said the research has revealed a direct link between early brain degeneration and impaired waste clearance in the brain, and could help explain how Alzheimer’s begins to take hold.
The research focused on specific brain neurons which are the first to die in Alzheimer’s disease. Previous studies had found the degeneration of these brain neurons and build-up of toxic proteins go hand-in-hand in Alzheimer’s disease.
‘The brain has inbuilt cleaning systems to rid it of waste and toxins, which is essential to cognitive health and preventing neurodegenerative diseases,’ Prof Coulson said. ‘However, how the brain knows to empty the waste is still unclear.’
The five-year study showed that the neurons, previously known for cognitive function, also control the blood and fluid movement that drives the cleaning system. Weakening those neurons led to impaired waste clearance.
The researchers also found that commonly prescribed Alzheimer’s drugs partially restored the waste fluid flow.
‘Cholinergic basal forebrain neurons regulate vascular dynamics and cerebrospinal fluid flux’ (Nature Communications, June 2025)


A cancer diagnosis turned Dr Roger Sexton from doctor to patient. In navigating treatment and recovery, he found he’d gained valuable insights into care, resilience and the patient’s experience of the healthcare system.
After a lifetime of very good health, my time came several months ago when I was diagnosed with an invasive oral squamous cell cancer. Once diagnosed, things moved quickly and I found myself a patient in the private health system. What a trajectory that has been. Surgery, chemotherapy and radiotherapy consumed three months and then came a period of slowly resolving radiotherapy after-effects.
I have received excellent care from my treating doctors and the hospital nursing staff along the way. From my observations as a patient, I have drafted 15 lessons learned as a patient.
1. Symptoms are very distracting. Unwell doctors are prone to errors. My symptoms were constant, consumed my full attention and disabled my focus on work-related matters.
‘Lying in the corner in the foetal position, hoping it will all go away when you wake up, is useless.’
2. A good medical history and physical examination are vital. This is a medical mantra. My diagnosis could have been made four weeks earlier if the dentist had adhered to what we all know in medicine is a structured approach to diagnosis.
3. Be as helpful to your treating staff as possible. They are doing as much as they can to help you and we must reciprocate. Being helpful gets you there quicker.
4. Do as much as you can to help yourself. Lying in the corner in the foetal position, hoping it will all go away when you wake up, is useless. ‘Self help’ means preparing yourself for surgery nutritionally and physically and beginning treatment in optimal shape. Aerobic fitness, nutrition and sleep are key elements. There is clear evidence supporting the benefits of aerobic fitness in cancer survival and reducing treatment side-effects. I attended a multidisciplinary clinic where I was taken through an hour of moderate-intensity exercise three times a week under close supervision.
5. Take the advice of your treating medical team and respect it. I did, and it was very helpful. I understood it was evidencebased. It is important as a patient to behave yourself.
6. Good clinical handover is critical. As we know, this is where patient care is so easily compromised. I saw excellent clinical handover while I was in ICU; the incoming nurse knew everything about me and what had been and needed to be done. There is a lesson there for all of us in terms of referrals to other practitioners or hospitals.
7. A comforting bedside manner is important. It was a pleasure being under the care of doctors who were unhurried and took the time to listen to and address my questions. I sensed that the doctors seeing me understood what I was worried about.
8. Time is a healer. It is on our side, but the days as a patient are slow. Signs of progress are uplifting. It is good to look back at how far you have come, rather than the length of the road ahead.
9. Free-to-air TV is a dementia risk factor. I know this to be true.
10. A cheer squad of family and friends aids healing. This is so important. Family and friends are the cheer squad we need to help us through. Whether it’s a short text, a photo, a cartoon – whatever –these gestures are uplifting when the burden of dependency can be very depressing.
11. Being a patient can be a full-time job. It is easy for illness to exclude all else. I had plenty of advice to stop everything and spend the recovery days as a full-time patient. Doing what was necessary to manage the treatment after-effects was, indeed, very time-consuming. But partial engagement in aspects of my work during recovery felt the right thing to do and gave me a sense of control and purpose that the illness had taken away.
12. The importance of optimism and aiming to be in ‘the group that does well’. I’ve always believed five-year-survival statistics did not truly reflect the individual prognosis of patients with cancer. There are the patients who do well, and those who don’t. As a doctor, I’ve always emphasised that we will work together so our patients are among those who do well. This gives everyone hope.
13. Don’t burden people with the gory details of your story – give them the positive news. People have been so kind, caring and concerned. I have made a point of not sharing the uncomfortable details of my treatment but have rather focused on the positive progress and recovery. People don’t deserve to be burdened by what I have been going through. A good rule.
14. Use a diary to record what you need to do each day. If you don’t, you may very well forget and miss doses of medications and other things. My diary kept me on track to complete what became a long list of daily tasks that included medications, jaw stretches, oral care, five meals a day, exercise and appointments. It was also a visual reminder of the passage of time and of my progress.
15. We are all billiard balls on the billiard table of life. We are at risk of being sent unexpectedly in a new direction by an unexpected external force; I have had all my age-appropriate health screening tests and yet diagnosis of an SCC of the mandible with perineural invasion was rare and difficult to detect.
Having your own inquisitive GP, booking regular checkups to optimise the chance of early detection, and adhering to the principles of a good history and physical examination become even more important.
I am pleased to be doing well. I am a most grateful patient, having had such good care in the private health system. Everyone will have their own list of lessons learned. I hope you find mine of some use. There are many more!

New research could point night-shift workers – including busy doctors –towards a diet that fits their schedule and tackles weight gain.
A study led by Monash University is shedding light on how night-shift workers can maintain a healthy weight and improve metabolic health, despite the challenges posed by irregular working hours.
The SWIFt study – published in The Lancet’s eBioMedicine – explored the effectiveness of intermittent fasting (IF) as an adaptable alternative to continuous energy restriction (CER).
The study involved 250 nightshift workers who followed one of two modified 5:2 IF strategies, consuming only 2100 kJ/day (about 25% of their usual intake) on two days a week, either during night shifts or on days off while eating normally on the remaining five days.
Their outcomes were compared to those following a CER diet and the results are promising. Most participants who followed the IF strategies showed ‘clinically significant improvements’ in body weight, blood pressure and insulin resistance – all key markers of metabolic health.
Professor Maxine Bonham from Monash Health’s Department of Nutrition, Dietetics and Food says the study shows for the first time that the 5:2 diet offers an alternative approach to improving metabolic health in nightshift workers.
‘Due to their work schedules, night-shift workers have little choice but to eat at times of the day normally associated with sleeping. Because of this, weight gain and an increased risk of developing type 2 diabetes are recognised consequences of night-shift work,’ Prof Bonham says.
‘We used intermittent fasting to remove some of the challenges faced by night-shift workers who face limited food choices as a result of their work schedule.
‘By testing the effectiveness of two 5:2 strategies compared with continuous energy restriction on weight loss and improvements in insulin resistance in nightshift workers, we were able to understand that just by minimising food intake one to two days a week, without changing any other aspect of their diet, we can improve night-shift worker health.’
New research suggests that even small shifts toward earlier sleep times can lead to measurable increases in physical activity the next day.
Going to bed earlier than usual may boost physical activity levels the following day, according to new research led by Monash University and published in Proceedings of the National Academy of Sciences (PNAS).
In the primary study, almost 20,000 participants wore a validated biometric device (WHOOP) for one year, resulting in almost six million nights of data. Objective sleep and physical activity metrics were derived from the wrist-worn device.
Researchers examined both habitual sleep patterns and nightly variations to understand their impact on next-day physical activity.
Findings revealed that earlier bedtimes were consistently associated with higher levels of moderate-to-vigorous physical activity. Participants who typically went to bed around 9pm logged about 30 more minutes of such activity daily compared to those with a 1am bedtime. Even compared to the average bedtime of 11pm, the 9pm sleepers recorded nearly 15 additional minutes of daily activity.
Lead author Dr Josh Leota said the insights carry meaningful implications for public health.
‘Rather than just promoting sleep and physical activity independently, health campaigns could encourage earlier bedtimes to naturally foster more active lifestyles,’ Dr Leota said.
‘A holistic approach that recognises how these two essential behaviours interact may lead to better outcomes for individual and community health.’
De Leota’s co-author Dr Elise Facer-Childs said a validation study involving nearly 6,000 participants from the ‘All of Us Research Program’ using Fitbit data has supported the findings across diverse populations.
‘Sleep and physical activity are both critical to health, but until now we didn’t fully grasp how intricately connected they are in everyday life,’ Dr Facer-Childs said.
‘Our findings are consistent across different populations and show that if you can get to sleep earlier than usual while keeping your sleep duration the same, you may be more likely to increase your physical activity the following day.’
As the weather warms up, the Adelaide Central Market is bursting with vibrant seasonal produce, and this recipe for beef flank steak fajitas makes the most of it. Packed with lean protein and colourful veggies, it’s a deliciously healthy way to enjoy the flavours of Spring.

• 600g flank steak
• 1 red, 1 yellow and 1 green capsicum, sliced lengthways
• 1 brown onion sliced lengthways
• 1 tbsp olive oil
For Fajita Seasoning
• 1 tsp cumin
• 1 tsp smoked paprika
• 1 tsp garlic powder
• 1 tsp salt and a few cracks of pepper
• 1 green shallot, thinly sliced
• 1 tablespoon sliced kalamata olives
• 2 teaspoons chopped fresh dill
• 4 cos lettuce leaves, coarsely chopped
• 2 teaspoons pine nuts, toasted
Serving Suggestions
1. Season and Cook Steak
2 serves | 5 min prep 20 min cook | Easy
• Mix fajita seasoning ingredients together and rub onto the flank steak, making sure to cover all sides and edges.
• Heat 1 tbsp olive oil in a skillet. Cook steak 4–5 minutes per side or until the internal temperature is 55°C (medium). Rest 5 minutes, then slice thinly against the grain - slicing against the grain on a flank steak is important, it will ensure that you get a beautiful, tender steak.
2. Char-Chook Veggies
• In the same skillet, without cleaning it (unless it’s particularly charred and dirty) cook capsicum and onion in a single layer for 1–2 minutes to develop a light char – don’t overcook as you still want to have a little bite.
3. Serve
• Arrange steak and veggies on a platter or skillet and serve with warm tortillas or coriander lime rice and your favourite toppings.
• Warm tortillas (wrap in a tea towel to keep warm) or coriander lime rice (see below)
• Guacamole, sour cream, salsa, or chipotle mayo
• Stir 1 tbsp lime juice, 2 tbsp chopped coriander, and 1 tbsp olive oil into 2 cups cooked, long grain rice.
Adelaide Central Market is open Tuesday to Saturday. Book your home delivery order via shop.adelaidecentralmarket.com.au

Misty mountain trails, accidental detours and a finish line 100 miles away. AMA SA Councillor Dr Isaac Tennant reflects on his ultramarathon through the Blue
‘Good luck! I can’t believe you’re doing this.’
I gave a nervous smile in reply.
Standing at the starting line in the cold, foggy darkness of the Blue Mountains at 5am, my wife’s incredulous words echoed in my mind. Here I was – about to embark on perhaps the most gruelling 24 to 48 hours of my life. Who knew that watching those Instagram videos of European runners scaling the Mont Blanc massif a year ago would have sparked an obsession which led me here, to this Utra-Trail ultramarathon in New South Wales? What felt like a far-off dream at the time had become a reality.
Well, not quite just yet. I’ll have to run the 100 miles first.
And so, to the shouts of the race marshal and the deep tones of a local Dharug elder’s digeridoo, we set off from Katoomba into the dark morning of 24 July. It would be 34.5 hours before I saw the finish line.
The morning itself was lovely. The cold, calm embrace of fog over the landscape initially kept the horizons and valleys from our view, but it rewarded our tenacity as each valley explored or peak summited revealed another facet of the ranges’ beauty.
As the day marched on, I gradually moved up the ranks toward the middle of the pack. By around 3 pm I had caught up to another runner I couldn’t pass, and we fell into stride – and conversation –together. Aaron, as I came to know him, became my guardian angel over the next 13 hours. While I had never run a trail ultramarathon before, Aaron had completed a handful of 100 km trail races.

This 100-miler race was a new challenge for both of us, and I certainly appreciated his company once the sun went down.
‘EACH
The night brought new challenges and my lowest moments. At one point, we took the wrong turn leaving an aid station, adding 8 km to our run. However, the real trouble was yet to come. At 4:15pm, we crawled exhaustedly to our last night-time aid station. I took one gulp of instant noodles, felt a wave of nausea and stood to get to a bin to vomit.
The next thing I remember was looking up at four faces crowded around my head. I was lying on the floor, confused yet feeling far less nauseous.
‘Not to worry all!’ I told them. ‘It’s just a vasovagal – I’ll be fine.’
Having said this, I bid Aaron farewell as I continued recovering at the aid station. While this could have been a race-ending event (and perhaps should’ve been), after about 45 minutes my blood pressure was comfortably back in the normal range and I was given the all-clear to continue.
The next one to two hours before dawn was truly the worst I have felt in my life. Cold, sore, sad and alone, I limped along until the sun rose, lifting my spirits with it. Buoyed by the new light, I was able to intermittently return to a jogging pace, eventually catching up to Aaron by mid-morning. By then the end was in sight, my running buddy was back by my side, and with each painful step I was a few centimetres closer to completing the ultramarathon.
Crossing the finish line was an almost indescribable experience. The last 200m of the course was lined with the friends and family of the runners, creating an

ecstatic atmosphere. I broke into a run, leaping across the finish line in triumph.
I had done it.
171 kilometres long, 7.2 kilometres up and down.
Though it took me over a week to walk normally again (and a similar amount of time to process the emotions I felt during the aftermath of the race), I didn’t really mind.
The 100-miler was done.
Though I ran this race alone, I know of at least two other CALHN doctors who completed the 100-km event the following day – both with their own stories of struggle and triumph. If you work with G or Daniel, make sure to ask them how they went.
Running this far may seem extreme, but each of us is merely choosing one way to express something common to all humans: a desire for adventure and the satisfaction of achieving something once thought impossible. Not everyone chooses to run an ultramarathon, but each of us chooses our own mountains to climb. Whether it is the training program of your chosen speciality, the dedication of perfecting a second language or musical instrument, meeting the challenges of parenthood, or something else entirely, it is a privilege to struggle in the face of a challenge you have chosen for yourself, to succeed, and to share our successes with those around us.
Having said this, I am a firm (read: biased) advocate for spending some time running/walking/hiking through the mountains every now and again.
See you at the next race.
AMA SA President Dr Louis Papilion and his family took part in the ‘Walk a Mile in My Boots’ challenge.

As another winter flu season continues, many of us in the health system can feel the pressure mounting once again. Ramping, delayed elective surgeries, bed block, increasingly complex patients, and the relentless stress of our roles can feel overwhelming. Yet, amid this frustration, it’s also a moment to pause and reflect.
In many ways, we are incredibly fortunate. We have job security, a roof over our heads, and food on the table. For thousands of South Australians, that security is not guaranteed.
Between 2016 and 2021, homelessness in South Australia rose by 19%, with an estimated 7,428 people experiencing homelessness on any given night. It’s a sobering statistic, and one that reflects the growing strain on our social safety nets.
Since 1954, the Hutt St Centre has been a lifeline for people doing it tough. Beyond providing meals, clothing, and hygiene services, the Centre offers crisis support, access to emergency accommodation, welfare officers, and GP and nurse-led clinics. Its approach recognises that homelessness is often temporary and complex, and that recovery requires compassion rather than judgment. It also helps clients work toward longterm stability through education, job-seeking support and community-building programs.

My practice, Stace Anaesthetists, sits just around the corner from the Hutt St Centre. It’s not unusual to see someone sleeping on our front veranda. My children aged 4, 6 and 8, often ask why someone would be sleeping outside, or ‘at Daddy’s work’. These are difficult questions to answer. I try to explain the role of bad luck, while reminding them how fortunate we are.
This year, I decided to act. I signed up for ‘Walk a Mile in My Boots’, a fundraiser supporting the Hutt St Centre’s vital work. Since its inception in 2008, participants have walked or run a nominated distance during National Homelessness Week, culminating in a powerful community walk each Friday.
I was proud to join this year’s walk with my wife, Jasmine, our three kids, my brother, sister-in-law and nephews. It was a wonderful community event and a deeply meaningful experience for my children. They came to see that giving back is not just about charity; it’s about solidarity, empathy and connection. This year, 3,200 people took part, and the energy and goodwill were contagious. Together, we’ve already raised over $500,000, with donations still climbing.
At a time when our health system feels stretched to the limit, taking part in something bigger can be both grounding and inspiring. We can’t fix everything, but we can all walk a mile in someone else’s boots.

Former military surgeon Dr Susan Neuhaus has chosen fiction as a means of telling buried stories of the feats of Australian women doctors at war.
When Susan Neuhaus is asked for a few words to describe her professional roles, she hesitates, then comes up with three to describe a life of varied, continual and heartfelt service.
‘How’s this?’ she asks. ‘“Surgeon, soldier, storyteller”.’
It’s a summary of a professional life that has taken her around the world, filling roles and performing tasks that started with medical school and most recently produced a fictional account of female surgeons in World War I.

‘I was just doing a job I’d been trained for, following in the footsteps of two other women who had performed it before me,’ she says.
‘There were so many women performing the most extraordinary battlefront surgery, dealing with injuries they’d never seen before and in an era before antibiotics’
Along the way, Dr Neuhaus operated a private practice for patients with rare surgical cancers, has shared her expertise on non-medical boards, and retired from the Australian Army with the rank of Colonel after spending much of her life zigzagging the world: training in England and Australia, then service in Cambodia, Bougainville, Australia and Afghanistan.
Her service to military medicine and her patients led to her being added to the AMA Roll of Fellows in 2019.
Now, she works in areas near her Adelaide home where patients desperately need more committed medical specialists: Whyalla, Alice Springs, Port Lincoln. She’s recently spent some time with Médecins Sans Frontières in central Africa. She spends about one-third of her time on non-medical boards. The rest of her spare time, she writes.
In 2009, she was in Afghanistan as a combat surgeon. It was a time of widespread and heated debate over the role of women in war zones and combat positions.
One day, she was sitting beside a male patient. Through an interpreter, she discussed with the patient the operation that would soon occur. As she provided the same information she had countless times before, it occurred to her that this man was trusting his life to a woman in a foreign uniform – in a country where many women find it impossible to be educated, to think for themselves, to follow professional careers. Meanwhile, she was an Australian woman who had travelled thousands of miles to care for people she didn’t know and who held very different beliefs from her own, while her own children were tucked home in bed in Australia, thousands of kilometres away.
She returned to Adelaide and two things happened.
The first was that she led a study at the University of Adelaide that was looking at health outcomes of mothers who had been deployed. It was sparked by international research that seemed to show that mothers who served overseas suffered more psychological conditions such as PTSD and anxiety than others. Dr Neuhaus says she was not surprised that the Australian study had very different results: it showed that Australian military women who had been deployed did not report any more health issues than other cohorts of women.
The second was being asked to write the history of female doctors in the Australian Army. She thought there had been only a handful, but her research quickly unearthed ‘more and more’.

‘There were so many women doctors whose stories had never been told,’ she says. ‘Australian women who served in World War I – there was no official record of them.’
Her research took her to France and England. She found more than 15 women who had defied the norms and expectations of the times and embarked for service in Europe. Two of them were from Adelaide: Dr Phoebe Chapple and Dr Laura Fowler-Hope, the latter the first female surgery graduate at the University of Adelaide, a doctor who spent three months as a prisoner of war after being captured in Serbia.
‘There were so many women performing the most extraordinary battlefront surgery, dealing with injuries they’d never seen before and in an era before antibiotics,’ she says. ‘Then, when they returned home, they couldn’t find jobs – except as doctors for women and children – because all the surgical jobs had to go to the men.
‘Many of these women received awards and commendations overseas, yet in Australia there was not a single medal and there’s been a collective forgetting about them.’
She says she felt ashamed that there was this ‘whole history of women doctors’ whose stories remained untold.
‘I thought we should know the women who opened the doors for us,’ she says. ‘We should share their names. And we should do what we can to open doors for others to come through. That’s how we can best honour them.’
Her research for the non-fiction book led her to Royaumont Abbey Hospital, one among a network of hospitals run by Scotland Women’s Hospitals for Foreign Service during World War I. The research, combined with her determination to honour Australian women’s

roles in combat, became the platform from which she wrote the recently published novel The Surgeon of Royaumont
The novel tells the story of a Sydney medical graduate, Dr Clara Heywood, who wants to offer her surgical skills to serve her country in World War I – but no one will accept the help of a female surgeon. Dr Heywood is a character Dr Neuhaus describes as ‘fictional but very much based on fact’; a doctor who disregards the opposition of family, friends and a contemptuous Australian military and makes her way to France, where within months she is working with women who provide critically needed care for men wounded on the frontline.
Some of the characters are real-life women Dr Neuhaus found in her research, including Royaumont’s MédecinChef, Miss Frances Ivens, and Australian pathologist, Dr Elsie Dalyell. But many are composites, offering the opportunity to capture the various characteristics of the women who made their way to France and the conditions under which they served war’s victims.
‘It was the only way I felt I could do them justice,’ she says.
Dr Neuhaus knows she’ll never be sure what inspired the determination and grit that led so many doctors and nurses to the frontline against such forceful opposition. But as a woman in a male-dominated profession, she’s thought about it.
‘I think if medicine is your passion, it’s absolutely the right thing for you,’ she says.
The Surgeon of Royaumont (Harper Collins) is available from bookstores now.

AMA SA’s Committee of General Practice member Dr Chris Bollen found much to learn in Kashmir – a striking Himalayan region that is a long-standing flashpoint between India and Pakistan.
Stepping off the plane at Srinagar’s military airport, the heavy paramilitary presence made for a disconcerting welcome. Barbed wire, camouflage-clad Central Reserve Police and armoured vehicles dotted the streets every few hundred metres. Yet amid this tension, life thrived – tuk-tuks swaddled in winter side panels buzzed through streets lined with fruit vendors and bustling markets. This juxtaposition set the tone for our three-day immersion in Kashmir, a land of contested borders, deep history and overwhelming beauty.
Our first destination was Dal Lake. There, a flotilla of brightly painted shikaras awaited at Ghat 14, touting for the fare to take our party of eight to the opulent ‘Shalimar Princess’ houseboat that was to be our home for the next three days. These floating wooden mansions, adorned with hand-carved panels and plush interiors, trace their origins to 19th-century Europeans barred from land ownership. Today, they are permanently moored and represent the heart of Kashmir’s tourism, a fragile industry shaken by years of political unrest.
We were welcomed aboard with saffron-infused Kashmiri tea by our smiling hosts, Shakeel and Ashwin. The warmth of their hospitality stood in sharp contrast to the icy breeze off the lake and set the tone for the memorable days ahead.
Day two began at dawn with a journey by shikara to the floating vegetable market. Traders in handpaddled boats sold winter produce – lotus roots,

radishes, and spinach – in what we learned is a fading tradition as younger generations turn away from agriculture. Srinagar’s layered past revealed itself as we wandered through its old town, from the grandeur of the 14th-century Jamia Masjid with its cedar pillars to the intricately paper-mâché adorned Green Mosque. Here we discovered the roots of the paisley design, later replicated by Scottish mills and exported globally.
That afternoon, we explored the fabulous symmetrical Mughal gardens that have influenced garden design the world over with their four squares divided by water channels and fountains. Later, we observed the handcrafting of silk carpets and copper samovars, a testament to the enduring artisanal spirit of the region.
Our final day took us skyward on the world’s second-highest cable car to the Kashmir ski fields, another contrasting feature of this amazing region. As snow deepened, we tossed snowballs and sipped Kashmiri Kehwa tea at 3,950m. Back at the Shalimar Palace, a farewell feast featured spiced lotus root and rich rogan josh and was followed by a final visit from Pashmina sellers – each shawl a woven tale of five goats and 18 months of labour. Kashmir astonishes not only with its scenic splendour but with its resilience. Amid militarised streets and contested identities, the people remain warm, welcoming and proud of their culture. This land, layered with complexity, history and artistry, leaves an indelible mark on all who wander its winding lanes and silent waters.




Menz takes the Audi Q4 e-tron
45 Sportback for a spin.
It is almost four years since I wrote about the inaugural electric Audi and that article included a couple of paragraphs of the history of Audi, which in summary dates back to 1910 in Germany. Audis have been sold in Australia since the late 1960s when Audi came under the umbrella of Volkswagen.
Audi now has a range of eight fully electric vehicles ranging from the Q4 to GT. The Q4, Q6 and Q8 models come in both SUV and sportback models and correspond to the internal combustion-engined (ice) Q3, Q5 and Q7 in size. Within each model there is a choice of rear-wheel-drive or all-wheel-drive and within the Q4 model are designated either 45 or 55; these numbers appear entirely arbitrary.
The test vehicle was the 45 sportback with its 82-kWh battery putting out 210 kW of power and generating
454 Newton metres of torque. The claimed 0-to-100 km/h acceleration is 6.7 seconds and if this is not fast enough the more expensive four-wheel-drive 55 with 250 kW does the same sprint in 5.4 seconds. For comparison, the top of the range RS e-tron GT Performance sprints to 100 in 2.9 seconds (but you get no change out of well over $300,000). The test car was so much more affordable at $97,000.
So what do you get for all that money? In short, a very competent comfortable German-built electric vehicle. It sports the usual safety and comfort features one has come to expect, including adaptive cruise control, lane departure warning, parking assist and cross rear traffic assist, although the rear camera has a fairly narrow angle. There are automatic lights when the sun approaches the horizon and a windscreenwiper function when it starts to rain. These features can be further enhanced with a couple of extra cost packages, including comfort and style.
And if you don’t want your Audi in pebble grey, the metallic colours (available in a limited choice of white, grey, black, blue, or silver) range between $1,755 and $2,255 extra. A sunroof is also available at just under $3,000 extra.
Interior features include three zone climatecontrol air conditioning or dimming interiormirror ambient lighting. What used to be called a dashboard is now called the Audi ‘virtual cockpit’ a fully digital instrument cluster with a 10.25-inchhigh resolution colour display in addition to the 11.6 inch central display for navigation, among other things.
There is meant to be wireless Apple CarPlay, but I did not find it at all intuitive; although I was able to connect my phone via Bluetooth to make and receive phone calls I was not able to use my phone for navigation. Another disappointment for me was only being able to set the cruise control in 5 km/h increments.
The Q4 e-tron was pleasant to drive and like many electric cars has a very good handling because of the low centre of gravity. The adaptive cruise control worked extremely well and I fortunately did not have to test the autonomous emergency breaking. Cruise control would also bring the car to a complete halt and automatically restart the car when the car in front moved off. The regenerative braking was adjustable but did not allow for right-foot-only driving as the car did not come to a complete halt with the right foot off the accelerator. However, when the brake was applied to make the car stationary, it would then remain stationary until the accelerator was depressed. One of the upgrade options has the more sophisticated regenerative breaking found in other electric vehicles tested.
The Q4 claims to have a range of 520 km. Unlike other e-tron models, it cannot be charged from a standard 240V outlet at home. It needs either a specific EV charger installed at home, or for the driver to attend a public charging station. With over 200 charging stations across metro and regional South Australia, it’s easy to travel a fair distance between charges.
In summary, the Q4 e-tron 45 as a fine example of German engineering and when considering value should probably be compared to other offerings from Germany rather than the Chinese-madeequivalents which are around $20,000 cheaper.
Test car provided by Solitaire Motors, Hawthorn.
Dr Robert Menz is a GP and enthusiastic motorist who once owned an Audi Fox and whose father owned an Audi 100, which was the very first Audi model sold in Australia.




The Pakistani Medical Association of South Australia (PMASA) hosted its annual gala at Adelaide Oval on 23 August. The theme was green and white – the colours of Pakistan’s flag – in honour of members’ rich heritage. The event celebrated outstanding achievers with awards across academic and extracurricular categories. Distinguished guests from around Australia attended, including keynote speaker Senator Fatima Payman and South Australia’s Minister for Health and Wellbeing, Chris Picton. The evening featured a vibrant blend of comedy and inspiration from comedian and actor Nazeem Hussain. Outgoing PMASA President Dr Rehan Hassan officially passed the torch to his newly elected successor, Dr Abdullah Rana, marking the beginning of a new leadership chapter.





AMA SA proudly supported the Second Annual African Australian Heart Health Initiative (AAHHI) Medical Symposium, held at the Adelaide Convention Centre on 19 July.
The event offered professional development for healthcare providers whose work focuses on improving cardiovascular and general health outcomes for Australians of African descent.
AMA SA was represented by Councillor Dr Jayanathi Jayakaran, who commended AAHHI and its founder, Dr Chukwudiebube (Chuks) Ajaero, for their vital work in highlighting and addressing the unique healthcare needs of African Australian communities.
‘It is wonderful that Chuks’ concerns for Australians of African lineage and descent have led to his determination to do something positive, and that he has inspired peers and colleagues to contribute their time and expertise to this very significant cause,’ Dr Jayakaran said.
Dr Ajaero said the feedback from participants was ‘overwhelmingly positive’.
‘The AAHHI is very grateful for the enormous support it has received from health professionals and industry sponsors, including the high-quality speakers from across Australia,’ Dr Ajaero said.
‘We also thank the South Australian Minister for Health and Wellbeing, Chris Picton, South Australia’s Chief Public Health Officer Professor Nicola Spurrier and AMA SA for their presence and support.’





For those in the medical profession, time is often the rarest commodity. Between patient care, clinical obligations, research, and personal commitments, life can begin to feel like a relentless triage. Doctors often say they don’t have enough time, and that there are too many demands on the time they do have.
Here are some tips to make time work more efficiently and more effectively for you – both workwise and personally:
• Focus on what you do best. Stick to it, as that is what makes you professionally satisfied and provides your income. You’re better off focusing on the job you do so well and earning money – that way, you can afford to outsource everything else.
• Create a task list. Sit down and list all the things you don’t have time to do, don’t want to do, and that don’t involve your professional life. These can

quintillionconcierge.com.au
AMA SA’s partner Quintillion Concierge offers a range of private and business concierge services to help clients manage their lives. Founder Carly Falconer explains why outsourcing mundane tasks can help doctors prioritise what matters.
be quite mundane tasks but it’s often the minutiae of life that gets in the way and prevents a smoothrunning life.
Delegate. Hand off all the tasks that can done by someone else. Why? As Steve Jobs once said, ‘Great things are never done by one man. They’re done by a team of people’. At work and at home, delegation is a strategy for success and sustainability, both mentally and physically. Stay sane and in control by letting others handle the things you don’t have time for – and that they can probably do better anyway. This isn’t about giving up control; it’s about recognising that expertise comes in many forms, not just your own.
Time is the one resource you can never get back. Use it where it matters most – to achieve your goals and enjoy your life. Avoid being consumed by the trivial tasks that slow you down.


Phil Manser from AMA SA’s partner winedirect shares the joy of vertical tastings, and explains why he believes it’s the real reason you should collect wine.
‘When we understand what happened in the past, we gain a better understanding of where we are now and what could be.’
That was my year-10 history teacher answering my question, ‘why?’.
Years on, I have regularly applied this to my career in wine, although I’m sure my history teacher had a higher purpose in mind.
Vertical tastings, sampling the same wine from multiple vintages, have been a regular part of my life in wine and a great way to bring like-minded winos into the same room. I’ve been part of a group for over 30 years that has conducted verticals of all kinds, with members all contributing missing vintages to form a continuous chain of years. Apart from the odd Penfolds or Wynns events, we’ve covered a great many producers and styles, from Mount Mary Chardonnay, Orlando Steingarten Riesling, Kaiser Stuhl Ribbon Series and more recently Pipers Brook Chardonnay. Of course, it wasn’t as fancy as all that in the beginning; our very first was Koonunga Hill from 1983-1994!
Pick a wine and try the experience. Wine bottles are like time capsules, subtly (or not so subtly) revealing the
conditions of the year they were made, the winemaking techniques used, and even issues of storage. It’s a great way to learn about wine – and if nothing else, a great excuse to bring your friends together.
If you’re lucky enough, perhaps the winemaker might be able to attend? You’d be surprised how many of them will say yes. I would!
When we covered 20 vintages of Eileen Hardy Shiraz back in the early 90s, Bill Hardy was kind enough to attend and speak. At the end of the tasting, he volunteered sheepishly, ‘great work, I doubt the Hardy family would be able to do this ourselves’.
He’s been in our group ever since.
Get a group together, pick a few producers and styles, and get to work. Collect consecutive years of your favourites, keep an eye on the auction scene and start building.
Reach out to me and I’d be happy to make some suggestions.
phil.manser@winedirect.com.au | winedirect.com.au
$295

Cellared Premium
Aussie Shiraz Plus a Bonus Belter RRP $942
Sometimes you just want the comfort of a perfectly cellared Shiraz. So here they are. Scan me for more details











