

State of health
The benefits and barriers of rural medicine



Our new Patient Portal, sharing a clearer picture.
Introducing our Patient Portal. Patients can now access scans and reports at their convenience and share them securely with others.
Key features:
• Immediate access to images post-appointment.
• Reports available 7 days after delivery to referring doctors.
• Secure sharing with friends, family, and health professionals.
This service does not impact report delivery to referring doctors. Critical findings will continue to follow our usual process.
This initiative is in line with the National MyHealth Record (MHR) requirements. Our clinics enable report integration with MHR.
Patient access via our website or SMS invitation following their appointment.

AMA(SA) members’ campaign for blanket gambling TV
Cybersecurity, IT and legal experts provide tips to keep medical businesses and their data safe from


medicSA
is produced by the Australian Medical Association (SA)
Australian Medical Association (South Australia) Inc.
Level 1, 175 Fullarton Road, Dulwich SA 5065
PO Box 685, Fullarton SA 5063
Telephone: (08) 8361 0100
Email: medicsa@amasa.org.au www.ama.com.au/sa
Membership: membership@amasa.org.au
EXECUTIVE CONTACTS
President
Dr John Williams: president@amasa.org.au
CEO Nicole Sykes: nsykes@amasa.org.au
medicSA
Editorial
Medical Editor: Dr Roger Sexton
Editor: Karen Phillips editor@amasa.org.au
Advertising medicsa@amasa.org.au
Design & Layout
Olivia Fantis
ISSN 1447-9255 (Print) ISSN 2209-0096 (Digital)
DISCLAIMER: Neither the Australian Medical Association (South Australia) Inc. nor any of its servants and agents will have any liability in any way arising from information or advice that is contained in medicSA. The statements or opinions that are expressed in the magazine reflect the views of the authors and do not represent the official policy of the Australian Medical Association (South Australia) unless this is so stated. Although all accepted advertising material is expected to conform to ethical standards, such acceptance does not imply endorsement by the magazine. All matter in the magazine is covered by copyright, and must not be reproduced, stored in a retrieval system, or transmitted in any form by electronic or mechanical means, photocopying, or recording, without written permission. Images are reproduced with permission under limited license.
AMA(SA) COUNCIL & EXECUTIVE BOARD
President: Dr John Williams
Vice President: A/Prof Peter Subramaniam
Immediate Past President: Dr Michelle Atchison
Chair: Dr Hannah Szewczyk
Ordinary Members
Dr Vikas Jasoria
Dr Emily Kirkpatrick
Dr Bridget Sawyer
Dr Nimit Singhal
Dr Krishnaswamy Sundararajan
Dr Hannah Szewczyk
A/Prof William Tam
Dr Isaac Tennant
Specialty Group Representatives
Anaesthetists: Dr Louis Papilion
Dermatologists: Dr Karen Koh
Doctors in Training Representative: Dr Hayden Cain
Emergency Medicine: Dr Cathrin Parsch
General Practitioners: Dr Chris Moy
Intensive Care: Dr Raj Ramadoss
Ophthalmologists: A/Prof Michael Goggin
Orthopaedic Surgeons: Prof Edward (Ted) Mah
Paediatricians: Dr Patrick Quinn
Pathologists: Dr Shriram Nath
Physicians: Dr Andrew Russell
Psychiatrists: Prof Tarun Bastiampillai
Surgeons: Dr Christopher Dobbins
Regional representatives
Southern: Dr Jerida Keane
Northern: Dr Alice Fitzpatrick
Public Hospital Doctors Representative: Dr Clair Pridmore
Student Representatives
Adelaide University: Hannah Kieu
Flinders University: Lydia Smalls
AMA(SA) Executive Board
Dr Michelle Atchison, Dr Guy Christie-Taylor, A/Prof William Tam, Ms Megan Webster, Dr John Williams (Chair), A/Prof Peter Subramaniam
SA members of AMA Federal Council
Dr Michelle Atchison
Prof Edward (Ted) Mah
Dr Clair Pridmore
Dr Hannah Szewczyk
Dr John Williams
President’s Report
Dr John Williams
There was a catchcry that went viral during the early months of the pandemic: Not all heroes wear capes. It wasn’t new, but it caught on in 2020 because it so accurately recognised that lives were being saved by amazing people – doctors, nurses and other health practitioners - doing amazing things in our hospitals, surgeries, vaccination clinics and other health settings.
I remembered that saying, and that period, as I watched athletes from around the world extend and exceed our understanding of what the human body can achieve during the Games of the XXXIII Olympiad in Paris.
I also joined audiences – television, radio, online and digital – in being astonished at the grace and humility some of these champions demonstrated in managing victory, defeat and what must sometimes be crushing fandom, all before several billion of their closest friends around the world. There were no capes in Paris, but many, many feats of super-human effort and endurance.
And that led me back to medicine. Physically, most of the Olympic athletes are closer to Superman than most of us doctors. But despite the provenance of their name, rarely does an Olympian have to make the decisions that could

determine a person’s capacity to live a healthy life. We doctors do that on a daily basis – and, as with the most awe-inspiring athletes – it’s the manner in which this super-power is offered and enacted that makes all the difference. In recent weeks, the AMA has named the newest members of its Roll of Fellows – those members whose actions and service have earned them the privilege of being Fellows of the AMA. I was overjoyed when I learned that our own AMA(SA) Council member and Committee of General Practice Chair Dr Bridget Sawyer was to be added to this elite fraternity. On behalf of AMA(SA) members I congratulate Bridget and all new Fellows. Similarly, we must congratulate those members who received awards at the AMA National Conference. No capes, but super indeed.
On a sadder note, it was distressing to hear of the death of another ‘super’ doctor, Dr Michael Mosley. In our Autumn 2024 edition, this magazine featured an interview with the British doctor- turned-science communicator, who was promoting his latest television documentary series. Dr Mosley’s super-power was his capacity to translate complex medical terms into language that people without medical training could understand. Most importantly, he acted like a Pied Piper, bringing them along for a ride that increased their knowledge about science and medicine and encouraged them to adopt behaviours that would improve their health and mental wellbeing. He will be missed. president@amasa.org.au
More than halfway through his term, AMA(SA) President Dr John Williams takes stock.
You began your presidency promising to be the voice of AMA(SA) members. How important is that voice?
Our members are our most valuable resource – they’re both our strength and our purpose. As president of the AMA in South Australia it’s a privilege to listen to our members and amplify their voices. Their insights shape and motivate my advocacy work so when I meet with health decisionmakers like the Premier and the Health Minister I can be confident that I’m speaking on their behalf.
What are your most satisfying achievements?
Negotiating the rural GP agreement with the Rural Doctors’ Association of SA has significantly improved conditions for more than 330 rural GPs and GP registrars. It’s also a crucial step in establishing and retaining the clinical workforce we all need to deliver world-class care.
Another success story is what’s happening in the Riverland, with the Riverland Academy of Clinical Excellence and the single employer model (SEM). I’m pleased the SEM will be rolled out to other regional Local Health Networks.
What are your priorities for the remainder of your presidency?
I have been a vocal advocate for more investment in general practice and this will continue. Current Medicare funding arrangements are out of date and made worse by inadequate indexation of the Medicare rebate and a previous Medicare freeze. We need to put general practice on a more sustainable footing, capable of delivering the type of care that many patients now need.
How can the crisis in South Australia’s hospitals be fixed?
This is one of the outcomes of years of neglect of general practice. The failure is felt most by our most vulnerable: the aged, people with mental health issues or chronic disease, and in our Indigenous communities.
Healthcare is often seen as a cost to be managed. I believe we should view it as an investment in our community and an essential part of building a thriving economy.
We need smarter investment to increase capacity across the system. That includes more public hospital beds, more aged-care beds and greater capacity for NDIS and other levels of community care. We need the state and Australian governments to stop the blaming and handballing of responsibility and work out how to work together to deliver world-class primary and tertiary care.
How is AMA(SA) helping?
By leveraging the expertise of our membership we are better placed to advocate for the right type of change.
Much of our advocacy happens through direct communication with health decision-makers. Our trusted reputation gives us a seat at their tables, and we work hard to maintain constructive relationships to ensure our views and evidence are heard. And when necessary, or asked, we advocate through the media.
Is the fight against payroll tax lost?
It’s disappointing and frustrating that the State Government has set the tax in motion, but our advocacy continues with rigour. AMA(SA) remains at the table with RevenueSA making sure the perspective of practice owners is at the forefront of how the tax is rolled out. A legal challenge is likely, and we will consider the AMA’s next steps then.
We continue to raise our members’ concerns with the Health Minister and other health decisionmakers.


Medical Editor
From the Dr Roger Sexton
was reflecting recently on my time as a ‘projector monitor’ at school and how much I enjoyed setting it up in readiness for the class to watch a documentary.
It was very satisfying installing the full roll of film at one end of the projector and watching it feed automatically through the very complex sequence of rollers to finally emerge at the other end and roll itself onto the empty spool.
When it worked, it was a joy to watch and see everything work as it was intended. It was seamless and very satisfying to watch the film arrive exactly where it was meant to go.
There were times, however, when during this loading process the film became stuck and required extrication of the film by reversing the whole process and starting again.
This struck me as a metaphor for the current woes of the health system.
As people enter the health system, they need a clear and unobstructed pathway towards the help they need. This should be efficient and seamless. It should guide patients through the various twists and turns of the complex health system and allow them to reach their destinations: the care they need and the health outcomes they seek.
However, we are now seeing many patients become stuck in the health system ‘projector’ at one or more of the many points along their paths.
This manifests in so many ways, such as difficulty accessing GP and other primary care, extended waiting times for preventive health care, specialist appointments, elective surgery, overcrowding in EDs, ramping, and delayed or premature discharge from hospital. There are many examples.
These show that the health system is not necessarily designed to facilitate the efficient
movement of individual people through it. As doctors, we know there are blockages and barriers that are difficult to overcome – but we also know that one of the ways to minimise and even remove those barriers is to support general practice.
The critical role of general practice in providing accessible and affordable care for patients must not be allowed to remain undervalued.
General practice is a filter the state hospital system badly needs, but it has been denied the opportunity for a range of reasons.

The AMA continues to advocate at state and federal levels for health system reform. Standing with the Colleges, especially those representing general practice, can add real weight to the arguments for such reform.
We all have roles to play in becoming involved and supporting the AMA to restore the power and centrality of general practice in the health system. It is worthwhile to consider how each of us can do this.
‘We are now seeing many patients become stuck’
I hope you enjoy the articles and stories from our many contributors in this edition of medicSA. I’m now settling down to watch a movie – with not a projector in sight. I welcome your correspondence.
roger.sexton@bigpond.com
Join the AMA(SA) Community and Make a Difference in Healthcare
AMA(SA) is seeking dedicated individuals who share our commitment and passion for driving positive change in the healthcare sector.
We’re excited to offer a range of positions that will help us achieve better outcomes for patients and doctors.
Both online and in-person attendance options are available.
AMA(SA) is stronger, louder and more effective when doctors stand together. Explore our open positions and learn how you can make a genuine impact.
1. International Medical Graduate (IMG) Committee - NEW COMMITTEE
The International Medical Graduate (IMG) Committee is a new committee which will serve as a strategic advisory body to the AMA(SA) Council, dedicated to identifying barriers of entry and establishing support systems for IMGs entering and practising in South Australia. The committee aims to advocate for the best interests of IMGs and facilitate their integration into the healthcare system.
We are seeking multiple members to establish this Committee with backgrounds in general practice and specialties, representing a range of experiences from new arrivals to Australia to those with over 5 years of experience working in Australia.
The IMG Committee will play a critical role in supporting and advocating for IMGs, recognising their importance to the Australian healthcare system. We are seeking multiple members for this committee.
2. Doctors in Training Committee – Member
• Central Adelaide Local Health Network (CALHN).
• Women’s and Children’s Health Network (WCHN).
• International Medical Graduate (IMG).
The AMA(SA) Doctors-in-Training Committee aims to identify and act on matters affecting the professional and personal lives of junior doctor members. We are looking for dedicated representatives from each of the following groups: Commitment
• 6-8 meetings annually.
• Pre meeting preparation.
Essential Requirements
• Member of AMA(SA).
Commitment
• Quarterly meetings.
• Pre-meeting preparation.
Requirements
• Open to all AMA(SA) members with a vested interest in the success of IMGs.
5 positions available
3. Committee of General Practice –Regional Member
We have a vacancy for a rural General Practitioner to join our Committee of General Practice. This position plays a pivotal role in providing a platform to influence and support general practice in regional areas.
Commitment
• 6-8 meetings annually.
• Pre-meeting preparation.
Essential Requirements
• Working as a rural GP.
Application Deadline 25 October
How to Apply
If you are motivated to contribute to any of these roles, please express your interest by sending your application to abrown@amasa.org.au
If you would like more information, please contact our CEO Nicole Sykes at ceo@amasa.org.au or our President Dr John Williams at president@amasa.org.au
CEO
From the Nicole Sykes

Over the past few months, AMA(SA) has achieved several significant milestones that reflect our unwavering commitment to supporting our members and the broader medical community.
Our campaign to minimise the impact of new interpretations of payroll tax on doctors and your patients have led to us securing crucial concessions from the Treasurer, including an amnesty that offers retrospective protection for non-GP medical specialists in private practice.
The Treasurer has also confirmed that GPs paid from rural hospitals will be exempt from payroll tax, a significant win for our rural practitioners.
We continue to work closely with Treasury, RevenueSA and RACGP to define how the legislative changes are being applied, ensuring that the finer details are clear and beneficial to our members. These ongoing efforts are crucial in safeguarding the interests of private practices across the state.
In addition to our advocacy efforts, we have been electing new leaders and strengthening our governance processes. We are pleased to welcome four new board members:
WE ARE COMMITTED TO SUPPORTING OUR MEMBERS AND THE BROADER MEDICAL COMMUNITY.
Dr Bridget Sawyer, Dr Shriram Nath, Professor Tarun Bastiampillai and Professor Ted Mah. All longterm AMA(SA) Council members, their expertise and dedication will undoubtedly contribute to
the achievement of our strategic initiatives in the coming years.
Our broader commitment to transparency and good governance includes a comprehensive review of many documents that underpin how AMA(SA) operates, capitalising on the efforts of a large group of volunteer members who work with our secretariat. We have updated many documents, including our Board charters, volunteer recruitment policy and committees’ Terms of Reference.
One pivotal development has been the establishment of a committee focused on international medical graduates. This is a significant step in our efforts to support this vital group of professionals. We are advertising to fill positions on this committee, and I encourage anyone interested to submit an expression of interest.
Our commitment to engaging with members across the state remains strong. The third leg of the President’s rural engagement tour was particularly productive, offering us the opportunity to meet established members and new acquaintances. A highlight was our visit to Mount Gambier and Districts Hospital, where we received a warm welcome and were inspired by the team’s vision to enhance medical services in this beautiful region.
These achievements would not have been possible without the small, dedicated team behind AMA(SA). Their efforts to deliver member value and respond to member requests have been instrumental in our refreshed approach and I thank each member of the team for their hard work and commitment as we embark on the important objectives of our new Strategic Plan
These efforts and achievements underscore our mission to support and advocate for the medical profession in South Australia. We look forward to continuing this important work in the months ahead.
Local and systemwide issues were the focus of meetings during the Limestone Coast stop on the AMA(SA) regional tour.
AMA(SA) President Dr John Williams is in the driver’s seat on his way to the Limestone Coast, the third stop on his rural tour of the state.
The trip from Adelaide to Mount Gambier takes about four and a half hours – plenty of time to reflect on his rich and varied career.

locations, mostly in general practice.
As the car zips past silo art and through the vineyards of Coonawarra, Dr Williams recounts his years working in London, at hectic innercity hospitals and poorly resourced GP clinics where he refused to stick to seven-minute appointments.
He also chats about the months he spent in the notoriously violent Highlands region of Papua New Guinea and his narrow escape from a rather unusual bus hijacking.
Dr Williams talks, too, about his time in South Australia – his home state. He’s worked in

As he speaks, it’s clear patient care has always been Dr Williams’ main concern. It’s what motivated his rural tour in the first place.
‘MY RURAL TOUR IS AN OPPORTUNITY TO LISTEN TO RURAL DOCTORS.’
‘As a GP based in Port Lincoln, I know first-hand that rural and regional healthcare isn’t always given the focus it deserves,’ Dr Williams says.
‘The voices of country doctors aren’t always heard as loudly as they should be when our leaders are making important healthcare decisions. I’m trying to change that.
‘My rural tour is an opportunity to listen to rural doctors, so that when I meet with the Health Minister or speak at a press conference, I can be confident that I’m speaking on their behalf.’
President’s priorities
Dr Williams visited the Limestone Coast on Thursday 29 August. His first stop was the Mount Gambier and Districts Hospital for a meeting with Limestone Coast Local Health Network (LCLHN) CEO Emma Poland and her colleagues, Executive Director of Medical Services Dr Sue Abhary and Director of Medical Services Dr Hemant Diesh.
Later the same evening Dr Williams hosted a dinner with local doctors and LCLHN representatives at The Barn in Mount Gambier.
Dr Williams told gathered health professionals that the fragile parts of South

Australia’s health system are suffering – including aged care, Indigenous health and rural health.
‘More than 20% of people in South Australia live in rural or regional areas,’ Dr Williams said.
‘We need our leaders to view healthcare as a basic part of infrastructure – like our roads. Proper investment is needed in every corner of the state.’
Dr Williams outlined two priorities in fixing the health system’s woes.
‘The first priority is improved data collection, he said. ‘More data is needed to understand where and why patients are sick and to inform decision-makers about what is and isn’t working.
‘The second is greater connectivity in the system. We need to leverage hospital and GP data to better connect general practice with tertiary care.’
Supporting junior doctors
GP anaesthetics registrar Dr Vienna Tran, who has been working in Mount Gambier for three years, said more efforts are needed to attract and retain junior doctors in South Australia.
‘A region’s medical workforce is only as strong as its junior doctors,’ Dr Tran said. ‘We’re energetic, enthusiastic, we’re willing to learn and work hard – we keep the wards going.
‘In a place like Mount Gambier that’s expanding, we need junior doctors more than
PRESI D E N T ’S
NE COAST RURAL TOUR
LIMESTO
“WE NEED OUR LEADERS TO VIEW HEALTHCARE AS A BASIC PART OF INFRASTRUCTURE – LIKE OUR ROADS.”

Hemant Diesh, Sue Abhary, Dr Williams, Emma Poland, Ms Skyes
ever. We need to make sure they don’t feel isolated or alone.’
Ms Poland, who stepped into the LCLHN CEO role in January, said she’s committed to trying new ways to make the region a place doctors want to work.
‘Being a healthcare professional is more than just a job,’ Ms Poland said. ‘It’s important to create a culture that supports doctors. We need to make this a safe place for workers and patients.
‘We also need to look at education and partnerships that will allow us to expand our research capabilities.’
Dr Williams said the single employer model (SEM), which has boosted the recruitment and retention of regional doctors in the Riverland, is due to be rolled out to all other regional areas in the coming months.
He also spoke of his work with the Rural Doctors’ Association of SA to negotiate a new pay agreement for more than 330 rural GPs and GP registrars.
‘If we want to keep doctors working in rural areas, at very least we need to make sure they’re remunerated properly,’ Dr Williams said. ‘The GP agreement is a crucial step in establishing and retaining the clinical workforce we all need to deliver world-class care.’




THEROAD AHEAD
We still have some ground to cover and look forward to upcoming visits to Kangaroo Island , the Iron Triangle, Port Lincoln, Murraylands, Victor Harbor and Clare.
Dr Williams is encouraging clinicians to join events scheduled during his visits.
‘There are many issues rural doctors are dealing with and it’s really important I support them as they work their way through these minefields,’ Dr Williams says. ‘For the doctors themselves, this is an important opportunity to showcase their regions and help shape my important advocacy work with health decision-makers.’
Rural Tour Events
Kangaroo Island
Tim Hall (Avant) & Dr Williams
Lisa Hickey & Helen Hadjisavva (Hood Sweeney)
Off-key: payroll tax harmony still lacking

In March 2007 state and territory treasurers across Australia announced a common goal: overhaul payroll tax arrangements to achieve greater harmonisation across the country.
While all jurisdictions have taken steps to align payroll tax provisions – South Australia, New South Wales, Victoria, Tasmania and the Northern Territory have even adopted identical legislation – payroll tax rates and thresholds vary and there are different
AMA(SA)’s advocacy has achieved several important outcomes not attained in other jurisdictions.
interpretations and applications of the law. For many private medical specialists in South Australia, the lack of harmony has fuelled confusion, anxiety and anger. Over the past 12 months AMA(SA) president Dr John Williams has advocated against payroll tax, describing it as an unacceptable burden on the health system. AMA(SA)’s advocacy has achieved several important outcomes not attained in other jurisdictions and Dr Williams and AMA(SA) CEO Nicole Sykes remain at the table with RevenueSA, Treasury and RACGP to ensure the perspectives of general practice owners are considered as part of legislative change.
States out of sync

*Final negotiations are still occurring in some states at time of publication.


On the record
Dr John Williams’ advocacy work as AMA(SA) President takes many forms and includes frequent media appearances. He’s a regular contributor on TV, radio, print and digital platforms and has helped government, the media and audiences understand many issues affecting patients and doctors.
System in crisis
July’s ambulance ramping figures were the worst in South Australia’s history. Public hospital patients spent a record 5,539 hours waiting outside hospitals for emergency care. When the figures were released on 2 August, hundreds of essential surgeries had been postponed due to a code yellow across public hospitals that started on 30 May.
Dr Williams appeared on ABC Radio Adelaide on 5 August to express his concerns and those of AMA(SA) members. He told Mornings presenter David Bevan that all sides of government, at both the state and federal levels, must work together to protect the fragile parts of our health system - Indigenous health, aged care and mental health. He also emphasised that general practice is the long-term rescue for the health system and questioned why the South Australian Government is ripping money out of GPs in the form of the payroll tax.
Hotel healthcare
Dr Williams was asked about a new State Government plan to establish a 25-bed ‘ready-made’ health facility – possibly within a hotel – to care for patients who are medically ready to leave hospital and are occupying beds.
The ABC’s Liz Rymill interviews
Dr John Williams in Mount Gambier on 30 August
Dr Williams told The Advertiser and ABC News that AMA(SA) would welcome the additional system capacity but said the state government must make sure all beds are properly staffed with enough trained professionals to ensure patients receive the best care.
He also stressed the need to ensure the facility is fully connected with the rest of the health system and that acute care can be obtained immediately in an emergency.
GP shortage
The Department of Health and Aged Care’s ‘GP Workforce’ report released on 5 August confirmed that South Australia’s GP shortfall is likely to grow over the coming decade to 584 fulltime equivalent positions by 2033.
Dr Williams told The Advertiser, ABC Radio Adelaide, fiveAA Radio and Southern Cross Media that the state and federal governments must work strategically and cohesively to find long-term solutions to improve access to GP-led care for patients, including in rural and remote areas.
He said there must be more opportunities for doctors to experience general practice early in their careers, and policy that ensures the number of GP training places each year is based on community need.
He also reiterated AMA(SA) members’ concerns about the payroll tax and the risk that some practices may be forced to close down due to the additional financial burden.
Media queries and statements in recent weeks related to:
The impacts of payroll tax
The President’s rural tour
Essential surgery waiting lists
State Government ‘ummm-ergency’ campaign
Using botox for jaw injuries
The IV fluid shortage
Commencement of work at Modbury Hospital
Access to care at Clare Hospital
Access to specialist services at Wallaroo
Vaping legislative changes and impact of vaping on young people.
August 2024
Doctors in Training Representative
AMA(SA) Council met again on Thursday 22 August, with many areas of governance and advocacy discussed and actioned. While the meeting was chaired by AMA(SA) Vice President A/Prof Peter Subramanian, Dr Karen Koh was elected as the future chair, replacing Dr Hannah Szewczyk who was thanked for her excellent service.
Continuing the theme of governance the Council then voted to appointment four new AMA(SA) ordinary Board members. I would like to congratulate Professor Tarun Bastiampillai, Dr Shriram Nath, Dr Bridget Sawyer and Professor Ted Mah on their appointments.
A large part of the subsequent meeting was spent discussing international medical graduates (IMGs) working in South Australia and ways they may be supported to ensure they can live and work to their full potential in Australia. We heard that the accreditation process for specialist IMGs is currently quite arduous and convoluted and can lead to highly skilled doctors not being able to work to their full scope of practice despite shortages and public demand. It was noted that demand must be weighted against the need to ensure a safe standard of practice is upheld in Australia.
We also discussed the need to aid the integration of new IMGs, especially solo-practising GPs, into our health care system; this can be incredibly complicated even for doctors trained in Australia or who have practised here for years. Due to these and many more issues Council agreed to a proposal for AMA(SA) to establish an IMG committee, to work in tandem with the recently formed federal AMA working group, to address the concerns.
During the meeting we also discussed the new joint medico-legal joint statement that has been developed with the Law Society of South Australia and its implications on fees that doctors may charge for legal reports, the on-going issues and concerns regarding CPD homes, payroll tax implementation, ambulance ramping and the elective surgery log jam.
President Dr John Williams highlighted the recent incredibly successful AMA National Conference, AMA24, during which Dr Danielle McMullen and A/Prof Julian Rait were elected as president and vice-president of AMA Federal respectively, and our very own Dr Bridget Sawyer was admitted to the AMA’s Roll of Fellows!
Dr Hayden Cain is Chair of the AMA(SA) Doctors in Training Committee


Gambling ad ban must ‘put the people first’
A partial ban on gambling advertising on television is not enough to stop the damage triggered by the ads, write AMA(SA) members Professor Malcolm Battersby and Professor Michael Baigent.
The House of Representatives inquiry into online gambling, ‘You win some, you lose more’, concluded what we had feared: ‘Gambling advertising and simulated gambling through video games, is grooming children and young people to gamble … It is manipulating an impressionable and vulnerable audience to gamble online’.
Despite this conclusion, reports suggest the federal government in its response is proposing a watered-down version of the 31 recommendations from the inquiry.
As gambling addiction specialists, we are deeply concerned about the proposed rejection of a complete
advertising ban in place of a partial ban on free-to-air live TV advertising that appears to support the objectives of major sporting organisations and media businesses rather than the health and wellbeing of Australian citizens.
Advertising profits, divided among the industry, sporting codes and media outlets, derive from those who lose their income gambling. We are very concerned that those who gamble are being manipulated to act on their urge to gamble. In addition, younger people who are being exposed to relentless advertising around the sports they follow are being groomed into believing gambling is a natural component of elite sport.
The numbers show how prevalent it is. In the 12-month period 2022-2023, Australian metropolitan TV broadcast 504,100 gambling ads (average of 1,381 spots per day) and on regional TV 338,600 (average of 928 per day).
The state of play
The current rules are that gambling advertising is prohibited from five minutes before the start of play until five minutes after play for live sporting events between 5 am and 8.30 pm. Between 8.30 pm and 5 am, gambling advertising is allowed during commercial breaks and before and after any game, but not during play.
Gambling advertising is also prohibited between 5 am and 8.30 pm during programs ‘principally directed’ at children.
Reports of the proposed changes indicate they will ban gambling advertising during children’s programming, live sports broadcasts and an hour either side, and limit advertising to two an hour in general TV programming. This is a partial ban that will not stop the effects of this advertising on gambling addiction.
Gambling’s real damage
Minister Shorten has been quoted as saying he doesn’t think gambling is as severe as tobacco addiction. But a critical difference between gambling and alcohol or tobacco addictions is that the bottle or cigarette packet doesn’t chase you down the street. Gambling advertisements and the gambling app are on phones being used and accessed 24 hours a day. You just cannot escape reminders, inducements or triggers for gambling anywhere in your life.
A 2023 Australian Institute of Family Studies report highlights that exposure to gambling advertising had the greatest impact on people aged 18 to 34 years and people at risk of gambling harm. One in five young women (19%) and one in seven young men (15%) bet for the first time after seeing or hearing an ad on TV.
Among adolescents who were at risk of gambling harm, 40% bet on impulse in response to seeing or hearing betting advertisements.
We know that children and adolescents, particularly males, have not yet fully developed executive cognitive functions and are vulnerable to gambling advertising messages that suggest winning is easy, winning is frequent and gambling is a quick way to get rich.
Gambling addiction no longer affects just a few isolated individuals. Research shows that 7.9% of Australian adults (1,659,000) have one or more gamblingrelated problems and at least 1% (210,000) have gambling disorder. Recent evidence shows that 4.2% of all suicides in Victoria are gambling related, which extrapolated nationally would be 136 of 3,249 suicides annually (2022). Of these, 8% (10 people) are significant others whose lives are destroyed by their partner’s gambling.
Consistent research shows that for every problem gambler at least six others are directly affected, mainly through the financial consequences but also the ‘absent parent’, depression, anxiety and the loss of employment that affects all the family.
Every day in our clinic and our in-patient service we see the devastating effects of gambling, not only on the gambler but also their families, friends and colleagues. Our patients are diagnosed with gambling disorder – and at that point, they can no longer stop and require specialised treatment. Sadly, people only seek help in
a crisis, as a last resort because of shame and stigma. By then, lives may be destroyed with loss of relationships, divorce, loss of the family home, cultural harm, people resorting to criminal behaviour, and ultimately suicide attempts and suicide.
Our research has found that excitement caused by intermittent rewards or near misses provided by pokies and betting apps become paired with or linked to images, sounds, the venue itself, the sight of money or looking at the phone, creating an overwhelming urge to gamble. Our patients tell us how gambling advertising acts as a trigger to this urge to gamble, despite them not wanting to. In our service, some 80% of patients report suicidal ideation and 30% have attempted suicide in the 12 months before they seek help.
“We don’t advertise vaping for the sake of our young – why allow gambling ads to continue?”
In published studies we have shown that approximately 50% of male prisoners in South Australia had a lifetime gambling addiction. This state’s government recognised the importance of addressing the devastating impact of gambling disorder on individuals in the criminal justice system and funded our Statewide Gambling Therapy Service to provide a court diversion program. This has been successful in keeping well over 50 people from prison since it began. It is clear that the government and magistrates recognised that, as for other addictions, gambling disorder is a psychiatric illness, not a greedy or wicked character disorder. The magistrates have embraced this sentencing option because they understand that most people who come before them are not habitual criminals and are often people who had never gambled in their lives before they started playing the pokies or placed a bet on sports betting app.
We don’t advertise vaping for the sake of our young - why allow gambling ads to continue?
In letters to the Prime Minister and other parliamentarians we have urged the importance of action that prioritises the health and safety of Australians above the financial status of multi-million-dollar sports and media organisations. We reject any suggestion that gambling ads are necessary for the viability of these businesses and ask that our governments put the people first.


Prof Michael Baigent
Prof Malcom Battersby
HOW WE CAN ASSIST WITH YOUR BIGGEST CHALLENGES
CYBERSECURITY

The healthcare industry is especially susceptible to cyberattacks due to the volume of personal & protected health information.
Orlo One (Hood Sweeney’s Technology Services division) work with many medium to large healthcare businesses across South Australia to protect them against cyberattacks and data breaches.
Contact Orlo.one to discuss your cycersecurity needs.
COMPETITION & GROWTH ADVISORY



IMPORTANT PAYROLL TAX UPDATE
Are you aware of the recent shift in interpretation of payroll tax legislation by RevenueSA?
Brick-and-mortar medical practices increasingly face competition and disruption. Standalone urgent care clinics are growing in popularity
due to their convenience, often staying open longer than typical doctor’s offices.
Practices with long wait times may struggle to compete with clinics offering extended hours or home visits. This is where Blue Jam, Hood sweeney’s Growth Advisory, steps in, offering strategic facilitation and growth strategies tailored to your needs.
Blue Jam provides comprehensive solutions to help your practice thrive in this competitive landscape offering marketing as a service, technology integration, and people & culture strategies.
Contact bluejam.com.au to discuss how we can help your business not only compete but thrive.
The classification of independent contractors as employees is changing, and it’s crucial to stay informed and be prepared.
Medical Professionals have recently been granted an amnesty to protect them from retrospective payroll tax assessments. This may shift the planning you have been doing with your financial advisors. Do you know how the amnesty works and how to ensure you are covered by it?
Lisa Hickey, Director and Head of the Health team at Hood Sweeney has been working closely with the AMA(SA) throughout this process and is up-to-date with the most current information coming out of Revenue SA and what is being worked on behind the scenes in this evolving tax landscape.
Given the potential financial implications for patients and practices alike, Lisa Hickey, Director and Head of the Health Team at Hood Sweeney, is offering a Payroll Tax Assessment to ensure your practice is fully compliant.
To book a payroll tax assessment for your practice, please contact Lisa on 1300 764 200 or lisa.hickey@hoodsweeney.com.au

Safe and secure
Recent breaches have reinforced the importance of strong, pre-emptive action to prevent the damage cyber-attacks and hacking can inflict on businesses in 2024.
In our special feature, national anti-hacking experts and local specialists outline what every health business should do to protect your operations and your patients’ data.






Standing guard against risks

The health sector is a prime target for cyber criminals - and is vastly underprepared for attacks.

Healthcare providers topped the list of sectors reporting notifiable data breaches to the Office of the Australian Information Commissioner in 2023, with incidents rising from 63 in January-June 2023, to 104 in the second half of last year.
Research shows that only a third of Australian healthcare organisations embed cyber security awareness and training in their organisational policies and procedures.
The Australian Government has joined an industry
Recent cybersecurity breaches affecting health providers have been a ‘real wake-up call’ for private practitioners, says Partnered Health Medical Centres Chief Medical Officer Dr Shirley Fung.
It was while working at a small private GP clinic that Dr Fung sought cybersecurity training from Cyber Wardens. She completed the free 45-minute online training in June.
‘We are so dependent on technology in every aspect of running a practice, whether it is our practice management software, booking platform, accounting software or emails,’ Dr Fung says. ‘A breach to any of these systems would cripple business operations, leading to significant financial impacts and the risk of leaking patients’ personal and sensitive data.

alliance led by Telstra, CommBank and the Australian Cyber Security Centre to help protect Australia’s 2.5 million small businesses from online threats.
It is offering a free, CPD-accredited online training program through Cyber Wardens, a national initiative of the Council of Small Business Organisations of Australia (COSBOA). The training is accredited by the Australian Medical CPD Standard (AMcpdS) and available from the AMA’s CPD catalogue.
‘It’s no longer just IT experts who are responsible for cyber security — it’s critical that doctors and practice staff are trained in the basics to help fight attacks,’ says COSBOA CEO Luke Achterstraat.
MediSecure falling victim to cybersecurity breaches despite having extensive resources, it’s a real wake-up call for the entire health industry which handles highly sensitive data.’
‘CYBERSECURITY DOESN’T HAVE TO BE COMPLEX & EXPENSIVE.’
‘With large health related companies like Medibank and
Dr Fung says the online course emphasised the value of small steps: automatically updating software, enabling multifactor authentication, improving password strength, identifying scam messages, backing-up data and installing antivirus software.
Dr Fung says it is important that health practitioners and businesses are aware is that it is their responsibility to protect their patients’ data.
‘The most surprising thing I learned was that many small actions can be protective and are well within the capability of small private businesses,’ she says. ‘Cybersecurity doesn’t have to be complex and expensive.’
Cyber Wardens training ‘graduate’
Dr Shirley Fung



MALWARE
Cyber-crime’s most wanted

‘Malware’ is short for ‘malicious software’, and is a constant threat for computer users. These programs can wreak havoc on your device, stealing data, encrypting files, and disrupting your online experience.
Among the most common types of malware are:
• Viruses - digital parasites that attach themselves to legitimate programs and spread by replicating themselves
• Worms - similar to viruses, worms exploit vulnerabilities in software to spread rapidly across networks, often consuming resources and slowing down systems
• Trojan horses - disguised as legitimate software or files, Trojan horses trick users into installing them. Once inside, they unleash their payload, which can include stealing login credentials or installing other malware.
• Scareware - programs that bombard you with alarming pop-ups claiming your computer is infected with viruses or compromised. They pressure you to purchase fake security software or ‘fix’ the non-existent problem for a fee.
PHISHING

Phishing is when cybercriminals impersonate a person or entity to trick a victim into handing over sensitive information. A phisher poses as a legitimate company, such as a bank, and tries to trick you into divulging personal details such as your username, password or account details. They may contact you by phone, email, SMS or on social media, using tactics such as malicious links that install tracking software on your computer.


The telltale signs of a phishing email or message include poor spelling and grammar, a sense of urgency, unformatted text, and links to fake websites with slightly different addresses.

RANSOMWARE
Ransomware is a type of malware that encrypts your files, rendering them inaccessible to you.
As the name suggests, hackers demand a hefty ransom, usually in cryptocurrency, to unlock your data. It’s essentially a digital kidnapping scheme.
There are a number of ways ransomware attacks can happen.
• Phishing scheme - often starts as an email pretending to come from a legitimate source, such as a bank or a delivery company
• Drive-by downloads – by simply visiting a compromised website, malware can automatically sneak onto your device
• Exploiting vulnerabilities – hackers constantly scan for weaknesses in outdated software or unsecured networks.
MULTI-FACTOR AUTHENTICATION
Strong and unique passwords are a great way to avoid being targeted by cybercriminals, but they are not failsafe. Multi-factor authentication (MFA) is an additional layer of security to help verify you and protect your accounts from fraud.


Turning MFA on for your accounts is like turning on a digital ‘alarm system’.
MFA can work in various ways to verify your identity. You can receive a code via SMS or a secure notification in a free security app such as Google Authenticator.
MFA means that even if someone does obtain your password, they won’t be able to access your account, because only you will have the ability to complete the additional verification process.


- Definitions courtesy Cyber Wardens







Cyber-breaches – what we’ve learned

Details of the MediSecure cyberattack released in May reinforced the need for healthcare providers to protect their data, writes Orlo One’s Adrian Crossing.



In 2023, Australian prescription delivery service provider MediSecure experienced a ransomware attack that compromised the sensitive personal and health data of millions of customers. The compromised data included contact details, Medicare card numbers and expiry dates, prescribed medications and reasons for prescriptions. This incident –just one of many happening every day to individuals and businesses of all sizes – underscores the critical need for health providers to have the systems in place to protect data and be prepared for when the worst happens.
01
The
MediSecure data
Take proactive cybersecurity measures – Regular security assessments of your systems and processes and robust access controls can mitigate the risks of a cyberattack.
Train staff to detect potential threats – The most common cause of ransomware cyberattacks are emailbased and malicious links. Don’t leave cybersecurity to your IT expert - ensure all staff using your devices are educated and security aware. Security awareness training may cover email scams, Malware, password security, removable media, social networking dangers, safe internet habits and clean desk policies.
Implement a disaster recovery and incident response plans – These will map your response to and expediate a quick recovery and resumption of operations after a cyberattack, data breach or any event that takes your business offline, including natural disasters and failed software updates such as the CrowdStrike issue in July that shut down computers around the world.


breach highlighted the vulnerabilities that exist for the healthcare industry, which collects and stores some of the most sensitive personal information from millions of people. The lessons include: What did we learn?
Encrypt your data – Encryption protects sensitive data from unauthorised access. One of the most immediate and effective things a medical business can do is to deploy multi-factor authentication (MFA). MFA combines two or more independent credentials: what the user knows, such as a user name and password; what the user has, such as a security token; and what the user is, ascertained by biometric verification methods. MFA creates a layered defence that makes it more difficult for an unauthorised person to access a target, such as a physical location, computing device, network or database. If one factor is compromised or broken, the attacker still has to breach at least one or more barrier before breaking into the target.

Maintain personally identifiable information – Regularly purge unnecessary sensitive information and review access to data.
Back up your records – Copy essential data to a password-protected external drive such as a USB stick to ensure data can be restored after a data loss, malicious or accidental.




Why business continuity planning is essential

Rapidly developing technology has provided peace of mind for medical practices by increasing efficiency and offering secure data storage and recovery solutions. However, no one can predict when or where a disaster might strike. A carefully considered business continuity plan and working with your IT experts on a disaster recovery plan can ensure everyone knows what to do when things go awry.


The healthcare industry is subject to stringent privacy regulations, and non-compliance can result in reputational damage, legal action, and hefty fines. Effective disaster recovery solutions enable the restoration of medical data and resumption of daily operations with minimal downtime and minimise the panic when something goes wrong.

Healthcare-specific recovery planning
Healthcare organisations face a unique set of challenges for data protection and business continuity. From the need to be operational at all times to the highly sensitive nature of electronic health records (EHRs), medical organisations encounter various requirements for data protection and business continuity.
Non-compliance with The Privacy Act 1988 rules and regulations can result in significant reputational damage, legal action, and hefty fines. However, digital health records are inherently more efficient and less prone to errors. The guidelines were established to reduce instances of lost records, human error in medical transcriptions, and other issues that medical organisations faced before a central standard was implemented.
The downside is that on-premise disaster recovery solutions can quickly become very expensive.

An alternative is to use the security provided by managed services such as hosted disaster recovery and backup services.

- Technology business, Orlo One is a specialist branch of AMA(SA)’s preferred supplier of financial advice, Hood Sweeney.




Challenges in the era of virtual care
The explosion in the use of digital technologies for medical consultations during the pandemic has created risks and fears about privacy and security of patient information, writes Dr Emily Kirkpatrick.

The rapid adoption of digital technologies within the healthcare sector in Australia has fundamentally transformed the delivery of medical services, mainly through the introduction of virtual healthcare. South Australia has emerged as a pioneer, establishing the State Health Coordination Centre and the co-located Virtual Care Service.
These initiatives integrate specialist general practitioners (GPs) and non-GP specialists to support residential aged care facilities and regional hospitals, as well as escalated calls from HealthDirect. In addition, the Child and Adolescent
Virtual Urgent Care Service (CAVUCS) within the Women’s and Children’s Health Network sets national benchmarks for virtual emergency department care for children. However, this wave of digital innovation has been accompanied by a corresponding rise in cybersecurity challenges, particularly concerning remote working, telemedicine platforms, and consumer-operated health applications and devices.
Dr Emily Kirkpatrick
Healthcare Executive & Specialist General Practitioner
BALANCING ACCESS AND SECURITY
The surge in telehealth consultations, especially during the COVID-19 pandemic, highlighted virtual healthcare’s benefits and vulnerabilities. Telehealth offers increased accessibility and convenience for patients, yet it also introduces significant cybersecurity risks. A key concern is the secure transmission of patient data across the internet.
In Australia, telehealth platforms must adhere to stringent regulations, such as those mandated by the 13 Australian Privacy Principles (APPs) under the Privacy Act 1988 (Cth), which demand rigorous protection of patient information. Under APP 3.3, a practitioner must not collect sensitive information unless reasonably necessary.
Considerations include whether it is essential for
a clinician to transcribe all content within a virtual consultation, retain asynchronous messages if not clinically related or gather pre-appointment survey data. If data is retained, healthcare entities should be aware of how it is stored and for what time frame, whether it is stored on Australian servers, and if and how it is transferred into the medical record.
Under APP 11.1, the practitioner must also take reasonable steps to protect personal information from misuse or unauthorised disclosure.
It can be confusing with multiple platforms exchanging and storing data, including information sent via email; ensuring the practice or practitioner has a cyber protocol with encryption and secure authentication mechanisms is important.
THE BYOD DILEMMA
The increasing reliance on personal devices by healthcare professionals, commonly referred to as Bring Your Own Device (BYOD), adds another layer of complexity to the cybersecurity landscape.
Personal devices typically lack the extensive security measures of hospital-provided equipment, rendering them more vulnerable to cyber-attacks. When healthcare providers use their smartphones, tablets, or laptops to access patient records or communicate with colleagues, they risk exposing sensitive data to unauthorised access. Implementing MFA to strengthen the security of systems and applications, including email, will help reduce the likelihood of unauthorised access.
Anti-virus and anti-malware software should be installed on all devices, especially if uploading PDFs in medical software. Another factor is when patients use their own devices for sending information to a practice, such as ECG recordings, ensuring there is a process for email monitoring of attachments.
In parallel, practices and healthcare institutions should offer clear guidelines and comprehensive training on secure device usage, ensuring everyone is aware of the importance of protecting patient information.
HOME SECURITY INSURING AGAINST THE RISK
The shift towards remote work has blurred the lines between professional and personal environments, creating new cybersecurity challenges. Home networks are typically less secure than hospital networks, making remote access to medical records and systems a potential target for cybercriminals. In this context, using Virtual Private Networks (VPNs) is crucial.
A VPN establishes a secure, encrypted connection between a healthcare professional’s device and the hospital network, protecting data from interception. This is achieved by masking the user’s IP address and encrypting data traffic.
VPNs play a vital role in ensuring the confidentiality of sensitive information. Healthcare professionals should utilise VPNs consistently when accessing patient records or hospital systems remotely, thereby upholding data security and privacy aligned to the APPs.
Given the increasing frequency and sophistication of cyberattacks, including in health, practices should consider cyber insurance coverage. It is becoming more common as a contractual requirement for healthcare entities that are delivering sub-contracted health services to have coverage, often for a small fee, to enable coverage for up to $2 million liability.
When taking out insurance, the providers will typically provide organisations with a gap analysis of where weaknesses lie, including email and website risks.
The integration of digital technology in Australian healthcare has elevated the importance of cybersecurity. From a clinician perspective, it’s essential to consider the broader impact on delivering safe patient care.
If practitioners and practices adopt and adhere to robust cybersecurity practices, clinicians can continue to deliver high-quality care while safeguarding the confidentiality and integrity of patient data.

Under (digital) lock and key
Medical practitioners in private practice must implement policies and procedures that ensure the safety and security of their patients’ sensitive information, in compliance with the Australian Privacy Principles.
Norman Waterhouse Lawyers commercial and taxation law specialist Marissa Mackie says she is aware of an increased regulatory focus on the adequacy of data protection measures including cyber-security measures being implemented by businesses.
‘An entity has an obligation to take “active measures” to ensure the security of personal information it holds and “reasonable steps” to protect the information,’ Ms Mackie said.
practitioners to access records of another’s patient,’ she warned.
‘It is a timely reminder for practitioners and practices to review their data collection and privacy policies to ensure compliance with the rapidly-evolving expectations of the Office of the Australian Information Commissioner and to ensure they consider insurance coverage for instances of cyber-security breaches.
’Australian Digital Health Agency privacy director Oscar Bem says protecting patients’ privacy is not about hiding health information but enabling it to be used productively and ‘empowering consumers to make informed choices’.
‘ALL STAFF MUST BE AWARE OF THEIR PRIVACY RESPONSIBILITIES AND FOLLOW BEST PRACTICE’
‘What “active measures” and “reasonable steps” mean may vary from business to business.
‘The health information held by a medical practice or practitioner about their patients carries a higher level of privacy protection than other personal information, and practitioners are held to a higher standard with respect to the measures taken to ensure the protection of it.’
Ms Mackie said the practice’s obligations are not limited to taking steps to mitigate the risk of cybercrime.
‘Obligations may extend to addressing vulnerabilities within an entity’s record management systems, where an entity simply acts as a service provider for independent practitioners, and the ability for
‘All staff must be aware of their privacy responsibilities and follow best practice,’ he said. ‘Patients must be provided with clear and accessible information about how an organisation will manage their personal and health information and how their privacy choices will be supported.’
Mr Bem said practices should be aware that they are ultimately responsible for the security and privacy of patients’ information, even when third-party services or platforms are used.
He said privacy policies must be:
• clear – explaining how personal and health data is collected, used, disclosed, stored and disposed of
• accessible - clearly displayed on a practice website, in a waiting room, or on request
• tailored – customised to a practice’s specific needs
• updated – reviewed and revised when necessary.
Top privacy tips
Inform your patients about how you handle their health information and respect their choices
Use the health information lifecycle model, which begins with the collection of information and ends with its disposal, to guide your privacy policies and procedures
Check the privacy settings and terms of your software tools and applications
Ask for more information or clarification from your vendors or providers if you have any doubts or concerns
Design offices, clinical areas and waiting rooms to prevent health information from being overheard or seen by unauthorised people
Ensure storage and disposal methods for hardcopy and electronic documents are secure
Check computer systems and devices have appropriate access controls and passwords
Only share health information when necessary and with consent of authorised individuals, in accordance with a practice’s privacy policy.
Visit the Australian Digital Health Agency’s website at www.digitalhealth.gov.au to learn more about how to manage privacy and cybersecurity effectively.

Strengthening health’s ‘cyber posture’
Digital services, platforms and infrastructure must remain fit for purpose and user-friendly as rapid change occurs in the cyber-threat environment, says Australian Digital Health Agency chief information security officer Danielle Pentony.
‘Collective effort and innovation from leaders are important as we work towards a more secure, resilient and trustworthy digital future,’ Ms Pentony said.
Ms Pentony – who represented the agency in a panel on cybersecurity and data protection at the AMA National Conference – said healthcare providers, health technology partners and patients have come to trust and rely on digital platforms to store and access health information.
In a sector undergoing massive and accelerated change, she said, it is important that ‘any digital tool, system or process is scalable, interoperable and user-friendly, with a strong emphasis on data security and privacy’.
‘Human factors and technologies can inadvertently create vulnerabilities or introduce security risks,’ Ms Pentony said. ‘Human factors can include staff mistakes that may put their organisation’s data or systems at risk. Mistakes may be accidental, or come from a lack of required training, and at times could occur with malicious intent.’
She said cyber-criminals exploit weaknesses by targeting system vulnerabilities. Recent cyber-attacks have revealed that attackers are often driven by the potential for financial gain, she said, with the healthcare sector particularly
‘COLLECTIVE EFFORT AND INNOVATION FROM LEADERS ARE IMPORTANT’
attractive to cyber-criminals due to the potentially sensitive nature of patient data.
Ms Pentony said such cyber-attacks may lead to:
• data breaches, through the loss or theft of sensitive information
• service disruptions or significant interruptions to healthcare service delivery
• reputational damage
• a loss of trust and decreased consumer confidence in the organisation’s ability to protect data.
‘Effective cyber security is important to not only safeguard sensitive patient information but to deliver the best possible patient outcomes,’ Ms Pentony said.
The agency is working with the digital healthcare sector to meet the requirements of the Cyber Security Strategy 2022-2025 and the National Digital Health Strategy and Framework for Action
‘A core part of this strategic direction is increasing cybersecurity awareness across the healthcare ecosystem so we can adapt to changes in the threat environment and support the secure evolution of digital health,’ Ms Pentony said.
The agency is providing a range of training programs to heighten awareness and help health providers protect themselves and their patients’ data.
• Digital Health Security Awareness – a fivemodule online course to help staff improve cyber security awareness and behaviours
• Cyber Security Alerts – monitors and alerts health providers to new risks and threats, including those possibly affecting medical practice, allied health practitioners, software developers, pharmacies, aged care facilities and disability services
• Cyber Champions Network – doctors can apply to join a new community of health professionals working to strengthen Australia’s defence against and response to cyber threats to the health sector.
‘It is only by working together that the agency and the Australian health sector will be able to continue strengthening our individual and collective cyber posture for a truly resilient healthcare ecosystem,’ Ms Pentony said.
The Australian Digital Health Agency’s Danielle Pentony (centre) with Daryl Pereira of Google Cloud and the National Office of Cyber Security’s Xavier O’Malley at the AMA national conference
Private practice
Australian patients harbour serious concerns about how their personal general practice data is collected and shared, according to recent research into community attitudes.
A mixed methods research study supported by the Digital Health Cooperative Research Centre examined the views of a broad cross-section of the Australian population during late 2021 and early 2022.
90 per cent of respondents said they supported sharing their general practice information to directly support their care, but fewer than half felt comfortable with their data being used for secondary purposes like research and health service planning.
Professor Annette Braunack-Mayer from the Centre for Health Engagement, Evidence and Values co-authored the study and says respondents expressed a range of concerns.
‘Patients are worried about whether the “data custodians” are trustworthy,’ Professor Braunack-Mayer says.
‘They’re concerned about how they manage the data, who they might release it to and under what conditions. They’re concerned about personal harm relating to privacy breaches and discrimination and they’re also worried about third parties profiting off their data.’
GP information is increasingly being used for quality assurance, evaluation, health service planning and research.
The study findings suggest that patients are more concerned about sharing general practice data than they are about sharing data collected in other healthcare settings like hospitals.
‘My take on this is that general practice relationships of all the healthcare relationships are the most personal ones – they’re deeper, often more longstanding and more wholistic’ Professor Braunack-Mayer says.
‘People are telling their GPs things that are more personal and may therefore be more worried about the likelihood that their data is shared.’
Dr Carolyn Adams is a senior lecturer at Sydney’s Macquarie University and an expert in privacy law in healthcare settings. She says even though patients view GPs and other healthcare settings differently, the same laws apply when it comes to how data can be shared.
‘Some GP data is shared under legislative authority,’ Dr Adams says. ‘In relation to Medicare for example, doctors
‘WE HAVE TO TAKE THIS REALLY SERIOUSLY.’

are required by legislation to send that information to Medicare. They’re not breaching confidentiality because the sharing of data is required by law
‘Data can also be shared on the basis of express or implied consent. If data is going outside the practice and there is no legislative authority, you would be more inclined to ask for express consent.’
Dr Adams says the other way practices legally share data is through deidentification.
‘In the past that has been fine, because if you strip enough of the personal information off each record you could generally say it would not be possible to identify the individuals,’ Dr Adams says.
‘But as our technical capacity to reidentify information increases, the reliance on deidentification is increasingly coming under the spotlight.’
Both experts agree more must be done to educate patients about how their data is being used.
‘What we know based on the research we’ve done is that many people do not know to what extent their information is being shared outside the practice for purposes that are not related to their clinical care,’ Professor Braunack-Mayer says.
‘They’ve told us they want to know how the practice uses their data and they want that information to be accessible. That means it will need to be available in multiple languages and to suit different literacy levels.
‘We need resources for the community, we need resources for GPs and we probably need legislative change.’
Dr Adams agrees regulatory changes are needed and says GPs also have a responsibility to educate their patients better.
‘We have to take this really seriously. The reason that obligation of confidentiality exists between a doctor and a patient is because that relationship is based on trust,’ she says.
‘ If that trust is compromised then the therapeutic relationship is compromised, and that’s clearly not in the interests of patients, GPs or the community.’


On the national stage
The Federal AMA annual conference on the Gold Coast provided a platform for discussions about exciting and educational reforms in medicine and health care. It was also an opportunity for AMA(SA) leaders to embrace the new AMA ‘Vision for Australia’s Health’ and meet their interstate peers in an environment all agreed met the brief of ‘inspiring every doctor, every moment’.

A ‘formidable’ team
Federal AMA is welcoming a new President and Vice President, and for many members AMA24 offered an opportunity to learn more about the incoming leadership team.
Former Vice President Dr Danielle McMullen was confirmed as President in July after running unopposed. Associate Professor Julian Rait, who led AMA Victoria from 2018 to 2021 during a large part of the COVID-19 pandemic, was elected as Vice President at the conference.
Current President Professor Robson congratulated the pair.
‘I am delighted to be handing over the reins to Dr McMullen, who has proven her mettle in her vice-presidential role for the past two years and as President of AMA NSW before this period,’ Prof Robson said.
She said she was looking forward to representing all doctors and understands the strain being felt across the health system, including in general practice, public hospitals, mental health and in the private health sector.
‘There is an urgency and a readiness to take the best bits of our healthcare system and strengthen them, to support our excellent doctors and other health workers, to invest in prevention and early intervention, and to invest in general practice so that Australians have ready access to their doctor when they need them,’ Dr McMullen said.
‘Our first priority must be boosting investment in general practice. It’s the cornerstone of our healthcare system, with our GPs looking after Australians from birth to death and through all the ups and downs in between.’
A/Prof Rait echoed the need for urgency.
‘There is plenty of work ahead of us as we seek to address the many challenges, and seize on the many opportunities, across the Australian health system,’ he said.
GENERAL PRACTICE… IS THE CORNERSTONE OF OUR HEALTH SYSTEM
‘She and A/Prof Rait will make a formidable team and lead the AMA with great distinction.’
Dr McMullen assumes the presidency in October.
‘The vice presidency of the AMA is one of the most important health leadership roles in the country, and I am incredibly honoured to be elected to this position.’
‘I am looking forward to working with Dr McMullen, an extraordinary GP who will be a fantastic President of this organisation.’
Photo: New AMA President Dr Danielle McMullen and Vice President A/Prof Julian Rait, with outgoing President Prof Steve Robson
A VISION WITH PURPOSE
AMA’s new ‘Vision for Australia’s Health 2024-2027’ (the Vision) is the blueprint for a healthcare system that values prevention as much as treatment – one designed to ensure equitable access to healthcare for all Australians.
Launching the document during the national conference, AMA President Professor Steve Robson said a collective effort is needed to ensure Australia’s healthcare system is maintained as one of the best in the world.
‘In developing the ‘Vision for Australia’s Health’, we heard from doctors that the biggest challenges facing the profession are the things that impede timely and equitable access to care,’ Prof Robson said.
‘We heard about long waiting lists for appointments, workforce shortages, public hospitals that are over capacity, the increasing costs of healthcare, and inadequate supply of services in many areas of Australia.
‘Meanwhile, we have a lack of investment in preventive health — with growing rates of chronic disease further burdening the system.’
The Vision sets out five pillars to guide healthcare investment:
• a sustainable and thriving general practice at the heart of primary care
• public hospitals that are funded to provide high-quality and timely care
• a sustainable private health system
• public health that empowers communities and improves health outcomes
• a health system prepared for the challenges of tomorrow.
Prof Robson told members the AMA wants to create a health system that is responsive, efficient, and centred on the needs of those it serves.
‘The road to a healthier Australia will need to be paved with more than just plans – it will require purposeful action,’ he said.
‘The AMA stands ready to act and is uniquely positioned to leverage the expertise of our broad member base in shaping policy and driving change.’

‘Becoming a registrar in obstetrics and gynaecology is my greatest achievement.’
AMA24: Igniting inspiration
The AMA24 national conference on the Gold Coast coincided with the halfway point of the Paris Olympics, so it was fitting that one of the first speeches was presented by Olympian and clinician Dr Jana Pittman.
Dr Pittman was the first woman to represent Australia in both a Summer and Winter Olympic Games, taking up bobsledding when persistent injuries ended her athletics career.
She described her story as ‘a roller coaster of triumph, defeat, failure, and success’ and explained how throughout her life she’s harnessed fear to achieve greatness.
Despite winning four Commonwealth Games gold medals and two world title crowns, she told AMA members that becoming a registrar in obstetrics and gynaecology is her greatest achievement.
‘I was very lucky to compete for Australia for almost 25 years, but I have to say my transition into medicine is the best thing I’ve ever done,’ she said.
The theme of AMA24 was ‘inspiring every doctor, every moment’ and Dr Pittman’s speech set the tone.
During the three-day event, which started on 2 August, members were introduced to AMA’s new “Vision for Australia’s Health” and a new Federal leadership team. There was also an address from Australia’s Health Minister Mark Butler, who praised AMA’s role in healthcare reform and its strong relationship with the federal government.
AMA(SA) President Dr John Williams described the conference as a wonderful opportunity to connect with like-minded colleagues and learn from other industry leaders.
‘I was proud to lead a strong contingent of South Australian doctors at the conference,’ he said.
‘It was fantastic to catch up with old friends and form new relationships with fellow members who share a passion and dedication for the AMA and the important role it plays in building a better healthcare system for our country.’
AMA 2024
Leading by example
A desire to ‘give back’ has driven the very successful career of new AMA Fellow Dr Bridget Sawyer.
Adelaide GP and AMA(SA) Councillor Dr Bridget Sawyer isn’t someone who seeks awards or acknowledgement. For her, the work itself is the reward.
Sitting in AMA(SA)’s Dulwich headquarters just days after being admitted to AMA’s Roll of Fellows at the AMA national conference, she recalls a recent conversation with one of her long-term patients.
‘She said to me, “I came to see you, Bridget, because you’re my voice of reason – you keep me on track”,’ Dr Sawyer recalls.
‘And that gives you a bit of a shiver. It’s touching to see the respect that patients have for how I can help them.’
Dr Sawyer says helping patients and trying to improve their wellbeing has been the main motivator throughout her career.
‘If you’re healthy everything goes along with it,’ she says. ‘If you lose your health that’s when you fall into a hole, whether that’s emotionally or financially.
‘We need to be able to look after everybody better.’
Dr Sawyer says she’s felt the need to ‘give back’ because of the educational opportunities she was afforded while growing up in England. Her academic grades earned her a fee-free education at grammar school and then university.
‘My family never would have been able to afford to
AMA names new Fellows
Dr Bridget Sawyer was one of seven members inducted into the AMA Roll of Fellows at the national conference.

send me to uni,’ she says.
‘I was the first one in my family to go to university. I’m very grateful for the opportunities I’ve had and it’s always been important to pass that on.’
Dr Sawyer describes her career as ‘peripatetic’ – one spanning broad areas of medicine and geography.
She completed her training in general practice in the UK in 1987, after time spent working in rural New Zealand. In 1990 she moved to Australia for a role with the Royal Flying Doctor Service in Broken Hill, NSW.
‘I went from Manchester to Tibooburra (in far-west NSW) in five days, which was quite an eye-opener,’ she recalls.
‘Working for the Royal Flying Doctors was quite possibly the best job I’ve had.’
In the following decades Dr Sawyer’s focus shifted to
Dr Annette Barratt
Dr Barratt’s distinguished medical career spans more than four decades and her leadership roles at the state and federal levels have helped shape healthcare policies and initiatives. As Vice President of AMA Tasmania, she advocated for the profession and patients alike.
Dr Fred Betros
Dr Betros is a general surgeon with public and private hospitals in Western Sydney. A powerful advocate for patients and doctors, he joined AMA NSW Council in 2014 and has served on the Board since May 2016.
Dr Bridget Sawyer receives her Roll of Fellows certificate from AMA President Prof Steve Robson
general practice and then sports medicine. She was President of the SA Sports Medicine Association from 2011 to 2013 and has worked with elite athletes in netball, basketball and cycling.
I’VE LEARNT TO BE QUITE TOUGH
Dr Sawyer says working at Paralympic HQ for the Rio Games was a professional highlight. She also notes her work as race doctor at this year’s World Cup Para Cycling event in Adelaide and her time as women’s race doctor for the Tour Down Under.
‘I was there since the event’s inception and one of the best parts was witnessing the change in attitude toward women’s cycling. It was seen to be just as successful as the men’s,’ she says.
Dr Sawyer has been an AMA(SA) Councillor for seven years and Chair of the AMA(SA) Committee of General Practice (CGP) for six years.
In the latter role she has been a strong advocate on many issues, including the need for evidence-based policies during the COVID-19 pandemic. She was also asked by the South Australian Health Minister to join his Ambulance Ramping Taskforce.
AMA(SA) President Dr John Williams says Dr Sawyer’s admission to AMA’s Roll of Fellows reflects her dedication to developing and promoting AMA’s advocacy and initiatives.
‘I’ve had the privilege of working with Bridget for several years and have seen firsthand her impact across the medical profession here in South Australia,’ Dr Williams says.
‘This prestigious honour recognises her tireless efforts to improve the standing of both AMA(SA) and the Federal AMA and the work she has done advancing the role of women in medicine.’
Dr Sawyer acknowledges being a female doctor has had its challenges.
‘I’ve learnt to be quite a tough professional. I used to get a bit cross when people would think I couldn’t do something
Dr John Saul
Dr Saul was President of AMA Tasmania during the COVID-19 pandemic. His leadership during that period and his advocacy for essential reform underscore his dedication to advancing health on the state and federal levels.
Associate Professor Ines Rio
Associate Professor Rio’s distinguished career is marked by significant leadership roles and exemplifies an unwavering commitment to advancing the medical profession. Her leadership in women’s health, maternity care, mental health, aged care and primary care in Victoria has promoted AMA policy and enhanced the delivery of healthcare, outcomes and equity.

because I’m a woman,’ she says. ‘If I’ve made a difference to the women coming behind me then that’s fantastic, but I didn’t set out to do that – I was just doing my job.’
‘There are things I do now that I wish I’d known about when I was 30 because I think it would have changed the trajectory of my career, but that’s what experience is all about. You evolve with what you do.
‘I think that’s part of what motivates me is sharing what I know now, so people behind me can benefit. We all learn from people who are ahead of us.’
Dr Sawyer says her hope for the future is that she can help the broader community understand the importance of having a GP.
‘It’s such a hard thing to nail down everything we do as GPs – you can’t. And I think we’re disregarded a bit and not seen to be of value.
‘That-long term relationship we have with our patients is so valuable. I hope we can get the community to realise that.’
Associate Professor Jeffrey Looi
Associate Professor Looi’s service to the AMA has been characterised by academic rigour and a keen sense of justice, bridging the gap between policy development at a national level and advocacy for colleagues in the workplace. He was first elected to the AMA Federal Council in 2014 and has served with distinction on several committees.
Professor Anthony Lawler
Professor Lawler is the Deputy Secretary of Health Products Regulation at the Department of Health and Aged Care. He has served as the Tasmanian Chief Medical Officer and Deputy Secretary of Clinical Quality, Regulation and Accreditation. He’s been an active member of the AMA for 30 years, holding a number of leadership positions.

The 2024 AMA award recipients reflected the composition of the association’s membership and an increasingly diverse professional community.
AMA 2024 Best and brightest
The AMA presented its annual awards at the AMA national conference, honouring those who exemplify medicine’s highest values and recognising outstanding achievements that improve the health of all Australians.
GOLD MEDAL
The AMA’s 2024 Gold Medal was awarded to Professor Caroline de Costa (Qld) — a Professor of Obstetrics and Gynaecology and a clinician to 2016 — for her leadership in reproductive health, Pacific health and Indigenous health in regional Australia.
AMA President Professor Steve Robson described Prof de Costa as a ‘trailblazer who has shown in her work an absolute commitment to ensuring everybody, even in the most remote parts of the country, has access to the highest quality reproductive healthcare.’

PRESIDENT’S AWARD
Associate Professor Suzi Nou (NT) was awarded the AMA 2024 President’s Award for her outstanding advocacy work on private practice.
‘Associate Professor Suzi Nou is an exceptional anaesthetist who is highly respected by her colleagues,’ Professor Robson said.
‘We honour Suzi for advocating strongly for specialists to maintain their independence for public patients in private hospitals, amid the looming threat of bundled and managed care in the private sector.’
INDIGENOUS MEDICAL SCHOLARSHIP
University of Queensland medical student Kealey Griffiths (Qld) received this year’s Indigenous Medical Scholarship.
Professor Robson said Ms Griffiths was an impressive medical student ‘who has all the makings of a fantastic doctor and psychiatrist, where she will have a very important role in assisting Aboriginal and Torres Strait Islander communities.’


EXCELLENCE IN HEALTHCARE AWARD
Anaesthetist, researcher and teacher Professor Andre Van Zundert (Qld) was awarded the Excellence in Healthcare Award in recognition of his commitment to medicine, research, teaching and volunteering.

DIVERSITY IN MEDICINE AWARD
Dr Clara Tuck Meng Soo (ACT) and Dr Dinesh Palipana (Qld) were each awarded AMA’s Diversity in Medicine Award for their outstanding contribution to advancing diversity, equity and inclusion in the medical field.
Dr Soo, a Canberra-based general practitioner known for her dedication to the LGBTIQ+ community, has been instrumental in promoting the rights and well-being of transgender and gender diverse people.
Dr Palipana is an emergency doctor living with quadriplegia. He was the first quadriplegic medical intern in Queensland and the second person to graduate medical school with quadriplegia in Australia.



WOMEN IN MEDICAL LEADERSHIP AWARD
Professor Helena Teede and Dr Sarah Whitelaw were awarded the Women in Medical Leadership Award in recognition of their influence on national health policy by promoting gender equity and diversity as fundamental pillars of healthcare.


WOMEN’S HEALTH AWARD
Dr Keeth Mayakaduwage (Vic) was presented with the Women’s Health Award for his extensive research that has significantly advanced Australia’s understanding of the complexities of stillbirth and the importance of evidencebased practices.

DOCTOR IN TRAINING OF THE YEAR AWARD
AMA’s Doctor in Training of the Year Award went to Dr Amireh Fakhouri (NSW) for taking a courageous and principled stand for fairness and the rights of doctors in training.

Standing up for international medical graduates
A new AMA group aims to help international medical graduates of today and tomorrow, writes Dr Maha Selvanathan.
Many years ago, after completing my medical studies in Russia and my internship in my home country of Malaysia, I took the path of many other overseas-trained doctors by moving to Australia.
As I had already completed my training, I thought the hard part was over. What I thought would be a reasonably straightforward process of gaining employment as a doctor in Australia turned out to be anything but that.
I was faced with bureaucratic hurdles and red tape, I had to make several trips back home to complete various paperwork, and I endured many setbacks.
In the decade-plus since I started working as a doctor in Australia, I have seen very few, if any, improvements to the visa and employment processes for international medical graduates (IMGs).
And that is just the process of becoming a doctor. Overseas-trained doctors also face many challenges in the workforce, including exploitation, discrimination and difficulties establishing themselves in the community without a support network.

net they can fall onto. IMGs are often placed into jobs in communities with no orientation or guidance, and it can lead to burnout.
The AMA has long advocated for IMGs, but this working group will ensure this support is solidified and that new policies and reforms will be pursued. It demonstrates that overseas-trained doctors in Australia are valued and that someone is looking out for us.
‘Overseas
trained doctors
face many challenges’
In response to these challenges, the AMA has created an IMG Working Group, and I am proud to have been elected as chair after the group’s inaugural meeting in June 2024. There are major issues that must be addressed, and the AMA’s IMG Working Group is dedicated to unearthing and pursuing solutions to these problems.
Australia is an attractive destination for IMGs. Generally speaking, being a doctor in Australia provides great job satisfaction, better pay and conditions compared with other countries, and there are many opportunities to continue learning and improving.
It is also suffering a considerable workforce shortage – especially in rural areas, such as Armidale where I have worked as a GP for a decade. In many cases, IMGs are highly sought after to help address doctor shortages in these areas.
But while Australia depends on overseas-trained doctors to fill workforce gaps, there’s no support system or safety
Reforming the pathways to employment for overseastrained doctors is an obvious place to start. All too often I hear about the red tape preventing IMGs from starting a career in Australia, and I’ve experienced it myself. I have a friend who is trained as a neurosurgeon but is currently working at a supermarket. These kinds of stories are all too common. Visa processes and employment practices must be reviewed and efforts must be made to ensure IMGs have equal opportunities that lead to long-term employment, particularly in rural areas. Resources must be made available for IMGs to assist them when seeking work. Primary health networks (PHNs), general practices, medical colleges, local governments and other medical stakeholders all have important roles to play.
We want to ensure that once overseas-trained doctors arrive in Australia, they stay here and enjoy their time here. In Armidale, we had at least six doctors leave town two years ago, and this gap has not yet been filled.
Australia can be a fantastic destination for overseastrained doctors. I look forward to improving outcomes for all of us. I want to encourage more IMGs to engage with the AMA at state, territory and federal levels to ensure we can create a better system for all.
Dr
Maha Selvanathan is the chair of the AMA’s IMG Working Group

Fairer fees for parents
Federal and state AMA campaigns to have Ahpra review fees for doctors on parental leave have attracted wide support from the nation’s health ministers.
Acampaign led by AMA Victoria President Dr Jill Tomlinson calling for fairer Ahpra registration fees for doctors on parental leave is gaining national attention after strong support from South Australian Health Minister Chris Picton.
A petition created by AMA Victoria and backed by the Federal Australian Medical Association, as well as the AMA in South Australia, Queensland, New South Wales, Northern Territory, ACT and other associations across Australia, quickly gathered about 3,000 signatures.
The petition highlighted inadequacies in the current Australian Health Practitioner Regulation Agency (Ahpra) fee structure that asks health workers on parental leave to pay a full year’s registration fee – which has recently increased to $1,027 for 2024-25 - even if they work only one day of that year.
After requesting support from AMA(SA) President Dr John Williams, Mr Picton issued a media release in which he committed to raising the issue with his state and federal counterparts at the Health Ministers’ meeting in Sydney on 16 August.
At the meeting, the ministers noted that Ahpra is reviewing registration fee arrangements for practitioners taking parental leave and has agreed to report back to health ministers as a priority.
AMA members have been told the problem has implications for more than 877,000 Australian healthcare workers, who are a diverse and predominantly female workforce. Implementing a fee reduction or a specific registration category for those on parental leave would demonstrate a commitment to gender equity and support for the predominantly female workforce in the healthcare sector.
The petition explains that Ahpra and the 15 national boards do not lower fees or provide any proper mechanism or registration fee category to help healthcare workers who take parental leave.
There is a provision for an annual non-practising registration fee of $192. However, any healthcare professional resuming practice within the 12-month registration period must pay the full $1,027 registration fee, regardless of when they return in the annual registration cycle.
The issue was raised by Victorian oncology registrar and mother of two Dr Belle Sasse, who has argued there should be a pro-rata option. Dr Sasse was looking to return to work in mid-July after taking parental leave and was told she would have to pay the full fee to cover the two weeks
until the new Ahpra year began in August.
Dr Williams welcomed Mr Picton’s action to rectify what Dr Williams described as ‘a flawed and inequitable registration fee-setting process’.
‘At a time when we desperately need more doctors, we must help and support the ones we have,’ Dr Williams said.
‘The AMA in South Australia and around the country wants a fair, equitable and sensible fee-setting structure that recognises the practicalities of working as a health practitioner in this country.
‘Doctors working part-time or on parental leave – most of whom are women – should be able to have their Ahpra fees reduced or forgiven so returning to their roles, when they are ready, is simple and cost-effective.’
Mr Picton said it was vital to have a more equitable system that accounts for the need for maternity leave, given the vast majority of the health workforce is female.
‘Doctors, nurses and other health workers deserve parental leave like anyone else and they shouldn’t be disadvantaged for taking it,’ he said.
‘At the meeting, other Ministers from around the country were supportive of me raising this issue with Ahpra and they have now committed to working on this issue and formulating a plan to address this inequity.’
Mr Picton thanked the AMA and Dr Belle Sasse for their advocacy and said he was hopeful of positive action from Ahpra to address the current inequity.



GRIP is a specialised hand and wrist surgery practice for adult and paediatric patients. With onsite, experienced hand therapists, we offer streamlined operative and non-operative care of the highest standards.
GRIP Surgery
Dr Paul van Minnen and Dr Nicholas Smith are Plastic and Reconstructive Surgeons who dedicated their private practice to hand and wrist surgery of all complexities.
Our hand surgeons diagnose and treat conditions involving the hand, wrist and forearm with the aim to restore function and form.
GRIP Hand Therapy
Our hand therapists provide occupational and physiotherapy services, exclusively dedicated to the care and rehabilitation of the hand and wrist.
GRIP Hand Therapy is available at 4 convenient locations: Adelaide, Beverley, Hope Valley and Morphett Vale. A GP or Specialist referral is not required.




New focus on African Australian heart treatments
The inaugural Symposium on the Cardiovascular and General Health Profile of Australians of African Descent offered new and thought-provoking insights into conditions with particular significance for an oft-overlooked sub-group of the Australian population, writes Dr Chukwudiebube Ajaero.

‘Is it all in the genes?’
That’s the question that started the first Symposium on the Cardiovascular and General Health Profile of Australians of African Descent, hosted by the African Australian Heart Health Initiative at the Adelaide Convention Centre on 27 July 2024.
Dr Rodney Mbizvo, cardiologist and Interventional Cardiology Fellow at Central Adelaide Local Health Network, asked the question to introduce a presentation in which he noted that there is little or no data on African cardiovascular health derived from the African Australian population.
He emphasised the need for dietary discretion and physical activity for African Australians and pointed out the importance of hypertension in the aetiology of hard cardiovascular endpoints of Africans, especially regarding strokes.
many cases of atrial fibrillation are asymptomatic.
Prof Ganesan emphasised that the prevalence of atrial fibrillation has been noted to increase when Africans migrate from rural to urban areas, which can be extrapolated to increased prevalence of this condition in Africans who migrate to industrialised economies such as Australia.
Dr Jude Chapman-Wardy, head of obstetrics and gynaecology at Modbury Hospital, told the audience that pregnancy-induced hypertension occurs with greater severity and frequency in Africans. Treatment modality may be different from non-pregnant hypertensive cases, so medications such as alpha-methyldopa, hydralazine, labetalol and Calcium channel blockers can be helpful.
Other presentations included a report from neurologist and nuclear physician Dr Wilson Vallat on mitigating stroke risk in Africans, GP Dr Geeta Trehan’s discussion of gender and gender-specific screening and psychiatrist Professor Scott Clark’s detailing of the links between mental illnesses and poor cardiovascular outcomes.
“Dr Rodney Mbizvo emphasised the need for dietary discretion and physical activity for African Australians due to the lack of data on their cardiovascular health.”
Dr Mbizvo was followed by Northern Adelaide LHN nephrologist Dr Chiang Sheng Lee, who explained to participants that Africans generally have low renin hypertension, so calcium channel blockers and diuretics are preferred to ACE inhibitors as the first treatment options.
In his report, Professor Anand Ganesan detailed the racial and ethnic differences in atrial fibrillation concerning Africans. Prof Ganesan said evidence from multiple studies suggests there is a lower prevalence of atrial fibrillation in black people, but that this may be due to a possible ‘atrial fibrillation paradox’ – that is, that it is due to the underreporting of atrial fibrillation cases, especially as
During the symposium, the AAHHI launched the Evaluation of Metabolic and Psychosocial Interactions in African Australian Heart Study (EMPATHY), to be steered by Dr Chukwudiebube Ajaero, Prof Clark, A/Prof David Ogunniyi, Dr Azmeraw Tayelgn Amare, former AMA(SA) President Dr Peter Joseph, Distinguished Prof Vasso Apostolopoulos, A/Prof Lillian Mwangi and Dr Jocelyne Mulangala,
The study will assess interactions between metabolic and psychosocial factors towards cardiovascular disease in African Australians.
We look forward to providing an update at our next symposium in July 2025.
Dr Chukwudiebube Ajaero is Chair of the African Australian Heart Health Initiative. He is also a cardiologist and electrophysiologist with SA Heart and affiliate Senior Lecturer with the University of Adelaide.

RESEARCH BRIEFS

Astronaut aroma study may improve nursing home menus
RMIT University Scientists have led a worldfirst study on common food aromas that may help explain why astronauts report meals taste bland in space and struggle to eat their normal nutritional intake.
The research, published in the International Journal of Food Science and Technology, has implications for improving the diets of isolated people, including nursing home residents, by personalising aromas to enhance the flavour of their food.
The team had noted that how people perceive vanilla and almond extracts and lemon essential oil changed from normal environments on Earth to the confined setting of the International Space Station (ISS), which was simulated for participants with virtual reality goggles.
Lead researcher Dr Julia Low said vanilla and almond aromas were more intense in the ISS-simulated environment, while the lemon scent remained unchanged.
The team found a particular sweet chemical in the aromas of vanilla and almond, called benzaldehyde, could explain the change in perceptions, in addition to an individual’s sensitivity to the particular smell.
‘One of the long-term aims of the research is to make better tailored foods for astronauts, as well as other people who are in isolated environments, to increase their nutritional intake closer to 100%,’ Dr Low said. ‘The results of this study could help personalise people’s diets in socially isolated situations, including in nursing homes, and improve their nutritional intake.’
Research finds new way blood vessel growth is controlled
Scientists at La Trobe University and the Phillipps-University of Marburg in Germany have discovered how a peptide called Apelin regulates blood vessel growth, creating avenues of research for cancer treatment, organ regeneration and tissue engineering.
The study, published in Science Advances, revealed that when Apelin is produced by selfrenewing stem cells in the nervous system called ‘neuro progenitor cells’, it regulated the signals to the body that coordinate how blood vessels grow. The researchers observed that Apelin stimulates and regulates new blood vessel growth.
The research team observed the blood vessel development in living zebrafish, which are transparent as embryos and while young.
La Trobe University researcher Dr Kazuhide Shaun Okuda, whose zebrafish research and imaging expertise played key roles in the study, said the discovery could lead to new therapeutics to regulate blood vessel growth in diseases like cancer.
‘Apelin stimulates and regulates new blood vessel growth.’
The discovery is important for the burgeoning research areas of organ regeneration and tissue engineering, both of which need blood vessels to promote growth and deliver nutrients.
‘There’s research that suggests that it can help with cardiac regeneration, for example,’ Dr Okuda said.
Alzheimer’s discovery could improve medication
A significant discovery by Australian scientists has the potential to improve the effectiveness of drugs currently used to manage cognitive decline in patients with Alzheimer’s disease.


Alzheimer’s disease is the most common form of dementia, which is the second-leading cause of death in the country. About 250 Australians are diagnosed with dementia every day.
The CSIRO-led study compared data from 475 people with varying levels of cognitive impairment.
The scientists looked at the level of amyloid plaques in the brain, the atrophying or shrinking of the basal forebrain, and cognitive decline (memory and attention).
Dr Ying Xia, researcher at CSIRO’s Australian e-Health Research Centre and lead author of the study, said the results show how the atrophying of the basal forebrain, a key brain region for learning and memory and part of the cholinergic system, could indicate the presence of the disease well before symptoms occur.
‘Our research suggests an important link between brain structure, in this case shrinkage, and the way the brain functions during Alzheimer’s disease progression.’
The findings may help in the ongoing development of drugs to reduce the decline in the brain function seen in patients with Alzheimer’s disease. This could include work with drugs currently undergoing regulatory approval, which clear amyloid plaques from the brain, to amplify their cognitive effects.
Dr Xia said new drugs to clear amyloid plaques hold promise, but that it is not yet known whether targeting these plaques will address the underlying causes of memory and attention decline.
‘Currently, drugs available to manage cognitive decline in Alzheimer’s are only effective in up to 30% of cases,’ said Dr Xia. ‘We think we can improve on that figure, by increasing our understanding of the role played by the system targeted by the current drug treatment regimes.’

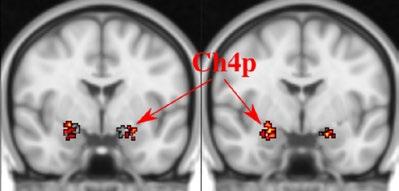
Designing healthier cities with good bacteria
The urbanisation of towns could be contributing to poor health outcomes in our communities, research from the University of Adelaide and Flinders University has found.
In the narrative review, published in the journal Environmental Research, researchers highlight the good bacteria that have been produced in well-designed cities, urban landscapes and buildings, which can help our immune systems to function properly.
The inclusion of large green spaces that consider conservation, environmental, social and public health outcomes in developments, as well as building designs with windows that open and indoor plants, are critical, the researchers said.
‘Exposure to many bacteria in the environment is actually good for us’, said lead author Kate Matthews, a University of Adelaide graduate and Flinders PhD student. ‘Our bodies are adapted to dealing with a diversity of bacteria in our environment, providing the “training” that teaches our immune system not to overreact to everyday exposures.’
The researchers found that as humans have become increasingly removed from nature, the diversity of microbes in the green spaces they have been exposed to has decreased. This can mean immune systems may overact and make allergies, asthma and autoimmune diseases worse.
‘As the percentage of the world’s population living in urban environments, increases (68% by 2050), so it becomes more important to design our urban environments to promote human exposure to diverse microbiota, with the potential to improve health outcomes,’ Ms Matthews said.
Leader of the University’s Environmental Allied Health group Dr Jessica Stanhope said that unlike other approaches to alter the human microbiome, such as diet and exercise, changing the design of the environments people are exposed to means that individuals do not have to make changes to their behaviour to improve their health.

Helping support your business everyday
Make Officeworks your partner in business. We’re here to support AMA SA members with our trusted range of over 40,000 products, business services and specialist advice to keep your business running smoothly and help you get back to what you do best.
Register for a free Officeworks 30 Day Business Account to access your exclusive member business pricing on a select range of everyday office supplies, print, furniture and tech.
Along with your 30 Day Business Account you can also enjoy additional benefits to help you get on with business.
30 Day Business Account.†
Buy everything you need today and pay in 30 days. Use multiple cards linked to one account or a digital card in the Officeworks App to manage it all in one place.
Easy online ordering.
Shop the way that works for you with secure, 24/7 online ordering from wherever you are.
Flexible Delivery.
^‡Our flexible delivery options include 2 hour, same day and next day delivery within eligible metro areas.
Large store network.
When the unexpected happens, there’s always an Officeworks close by with 165+ stores across the country.
Click & Collect.
Save time by shopping online with free 2-hour Click & Collect# on stocked items in store.
To register for a
or for

Doctors should ensure they are paying attention to their ‘operating manuals’ as the first step to peak performance at home and at work, writes Dr Roger Sexton.
TPillars of healthy performance
here are three pillars of doctors’ health that need our collective attention.
The first is our obligation to come to work in as healthy a state as possible. This is a professional obligation. Our existence needs – sleep, sunlight, exercise, hydration and good food – are too often ignored in the pursuit of a busy, time-pressured working week.
Our personal ‘operating manual’ – how we live our lives – is a common source of trouble. For example, there are many examples of doctors who are poor moneymanagers, always running late and managing time poorly. They may be unable to say ‘no’ and not manage the ensuing excessive workload. They test the tolerance of family members by coming home late and playing the ‘committed doctor’ card too many times. This empties the domestic ‘emotional bank account’. A holiday in Hawaii is nice but does not top it back up again. Compounding this is a sense of immunity to illness and a lack of attention to preventative health checks and good lifestyle habits. The second is when we come to work. All too often,
There can be an immediate sense that control has been lost
there can be an immediate sense that control has been lost over how, when, where and with whom we work. Time pressure can become immediate and last all day, and taking work home and remotely logging in to finish it off is the answer. This is the new work, health and safety issue facing GPs in particular.
Self-employed doctors may sense this, too. Despite owning their practice, they may outsource too much to their practice manager and end up marching to the beat of the receptionists’ drum. Working ‘on’ the practice and the workplace is always time well spent. Sharing ideas and improving ways of working can resonate positively with everyone. This starts with departmental or practice meetings and identifying what would make the working day better. A stronger culture of prioritising healthy staff and work environments will bring out the best in doctor and staff.
Third, the accreditation process for doctors in training can drive positive changes by embedding staff wellbeing in work practices and workplaces. There needs to be a minimum standard of care for staff. This is starting to happen and Colleges can drive this.
The importance of doctors’ health in our personal lives as well as our professional work remains as important today as ever. It affects recruitment, retention, clinical care, medicolegal costs and, of course, our precious personal and family lives that all too often take second place.
Dr Roger Sexton is the medical director of Doctors’ Health SA.
Riding the ED rollercoaster
Public hospital emergency departments demonstrate the best and the worst of Australian healthcare, writes intern Dr Isaac Tennant.
Another season goes by, as our third internship rotation (of five in total) draws to a close. Although the unwelcome voice of imposter syndrome still occasionally mutters in the back of my mind, I now find myself possessing a greater degree of confidence in my ability and an understanding of my limits. Though each coming day brings opportunities for learning new clinical, procedural and interpersonal skills, ongoing positive interactions with fellow staff members and patients have built a body of evidence that testifies to my usefulness (at least most of the time) as a health worker. To echo the experience of many of my fellow junior medical officers (JMOs), it has been great to find my feet as a doctor.
levels. My regular medical and nursing team of previous rotations has been exchanged for shift work with an array of new colleagues, and together we have participated in the move from the old QEH ED to the new ED building. It has been exciting to be involved in this change and to be part of the last rotation of junior doctors to work in the old ED. But the new building’s increased bedspace, staffing and natural light are certainly improvements on the old department.
Although initially I lamented the change in staffing and working environment, I have grown to appreciate the equity of interdisciplinary and intra-disciplinary interaction exemplified by the ED. In such a hierarchical field as healthcare, it is refreshing to see every doctor exhibit genuine interest in and respect for our nursing colleagues, paramedics and administrative staff. It is a telling and positive sign when the most junior doctors and nurses feel safe to raise concerns with the medical consultant. In this perhaps I am largely indebted to the hard work and positive role model of Dr Michael Edmonds – head of the QEH ED – along with his fellow consultants and leadership team. Leading by example is the most powerful form of leadership and the examples they set reaffirm the importance of exemplifying the sort of workplace culture that junior doctors will want to be a part of.
IT HAS BEEN GREAT TO FIND MY FEET AS A DOCTOR
In the past few months I have left my home base at the Royal Adelaide Hospital to undertake an emergency department (ED) rotation at the Queen Elizabeth Hospital (QEH). ‘Change’ has certainly been the mantra of this period, both on personal and corporate



Alongside the new collaborative working relationships I have developed with many of the ED nurses, I have enjoyed meeting a diverse range of international medical graduates (IMGs) working in the ED. Working alongside colleagues from Southeast Asia, South America and Western Europe has fostered an appreciation of the impact of IMGs on our medical system and the important role they play in our workforce. And they have such fascinating tales



of travel and practising medicine abroad!
Still, while I have gained many benefits from this rotation, it has been impossible to escape the constant signs of an overburdened health system. The hybrid inpatientoutpatient responsibilities of the ED enable me to see both the mounting lists of patients waiting for treatment while concurrently being struck by the degree of bed block preventing admitted patients leaving the ED. Though the new department’s physical and administrative structure is more conducive to patient flow than some other EDs I have worked in, it is clear that the growing population and under-supported general practice sector (to name only

two of the important contributing factors) are having an impact on the patient care experience - plus ça change, plus c’est la même chose.
Having said all this, I remain thankful for the healthcare opportunities and relative equity provided to our wider population. No health system is perfect – evidently ours is not – but we do have a lot to be thankful for here in Australia. Having recently returned from travel to Southeast Asia, I have been struck by the privilege we have as Australian citizens or residents. There aren’t that many other countries where one would be entitled to such quality healthcare, provided primarily through the Medicare levy. In addition, Australia’s private health system enables us to avoid some of the inflexibilities and inefficiencies of other fully-public systems elsewhere in the world.
However this praise is no reason to give up our commitment to improving the medical system we work in and benefit from. In a year during which some reports suggest the Australian life expectancy has fallen for the first time since the mid-90s, continued advocacy by AMA(SA) and other organisations is critical in guiding our policy makers to make expert-informed decisions to improve the structure and delivery of our nation’s healthcare.
I finish this rotation reminded of the necessity of this large-scale change, but also importance of the small things: treating fellow healthcare workers with respect and showing genuine interest in their lives. Let us all work together to create a system and a culture where every patient – and every healthcare practitioner – can thrive.
Dr Isaac Tennant Medical intern, Royal Adelaide Hospital


Intern Dr Isaac Tennant celebrating one of the last days of the old Queen Elizabeth Emergency Department with paramedic intern Ethan Harithupan
Student news Flinders University
Younger students learning from their peers
The Flinders Medical Student Society (FMSS) has been busy filling the 2024 calendar with a range of events and advocacy efforts. As we pass the halfway point of the academic year, I extend my heartfelt thanks to our committee members for their ongoing dedication and hard work. We are honoured to continue serving our members and strengthening our relationship with Flinders University.
In June and July we hosted a variety of successful events, addressing both academic and social interests. Our first-year medical students enjoyed bonding during the ‘Backup Plan’ pub crawl, when they reminisced about their potential career paths. Meanwhile, our third years had the opportunity to hear from their peers about their elective term experiences. Thanks to MIGA, we were able to help students envision possibilities for their own elective terms next year.
Our annual Mental Health in Medicine night was a standout and sellout event. With support from the Psychiatry Interest Forum (PIF), we highlighted the importance of mental wellbeing. Dr Gareth Furber and Dr David Coyte shared their valuable insights, urging us to support ourselves and our peers, not only during medical school but throughout our careers as health professionals. Dr Furber works for the Health, Counselling and Disability services at Flinders, a vast resource of wellbeing support for all our university students. His blog and teaching focuses on supporting students to be productive, happy and feel that they belong, and has a strong emphasis on self-care and behaviour change. Dr Coyte is a South Australian-based psychiatrist

with training in adult and child and adolescent psychiatry. He discussed the effects of stress on the body and mind and how this manifests in mental illness. Both encouraged us to notice signs of stress early and to recognise the various pathways for help, including FMSS, university services and organisations including the AMA, and our training colleges further in our career.
On the advocacy front, FMSS was thrilled to attend the AMSA National Conference in Melbourne (M24). Our presidents, AMSA representative and several other members participated as delegates in this five-day event. We engaged in academic talks with professionals such as Dr Lewis Potter and Dr Shewit Belay, who shared their unique journeys and special interests in medicine. We also had the chance to network with sponsors such as ACRRM and eTG. Dr Potter talked about the development of his business, Geeky Medics, and how he balanced this with medical school and training. We heard about the importance of continual professional development and understanding when to ask for help. Dr Belay showed us that a career in medicine can be beyond what we imagine. Working as a locum while auditioning for musicals, she encouraged us to follow our medical and non-medical passions.
‘WE HEARD ABOUT … WHEN TO ASK FOR HELP’

As I write this, we are excitedly anticipating our Annual Wright Evans Med Ball and our collaborative Inter-Society soccer match with the University of Adelaide. This year’s ball, themed ‘The Most Magical Night of Your Dreams,’ promises an evening of drinks, dancing, and fun. In a few months, we look forward to honouring our committee members at our annual retreat, where we will express our gratitude with a night of food and drinks. We are also excited for Gradweek, which will feature events to honour our deserving graduating class.
I’m eager to see how the rest of 2024 unfolds.
Grace
Mackenzie

FMSS Senior Vice President and AMA(SA) Council representative Lydia Smalls, Geeky Medics founder Dr Lewis Potter and President Grace Mackenzie
FMSS President 2024
FMSS President Grace Mackenzie and the 2024 Junior Committee

Mixing business and pleasure
The Adelaide Medical Students’ Society (AMSS) and the medical students from the University of Adelaide have enjoyed a much-needed break after sitting their exams following the Winter edition of medicSA.
Since you have last heard from us, the AMSS has held our annual International Food Fiesta (IFF) and PubCrawl, had 60 of our members go to the AMSA National Convention in Melbourne, and began rehearsals for our medical student play MedRevue.
I want to say a special thank you to our international officers Ganesh Venkatesh and Rithiha Balu for their amazing work with the IFF this year. This year the IFF was brought to the main campus of the University of Adelaide as we celebrated Australia’s multiculturalism and diversity. We also collaborated with YouX and other international student societies, leading to this year’s IFF being the largest we’ve staged.
I also want to thank our Vice President of Education Jock Duncan and our Team Education for their work in completing the AMSS’s Australian Medical Counsel report. The AMC report is one of the most important documents the AMSS produces each year and takes months of hard work. It allows the society to gather opinions and feedback from the student body about their experiences in medical school and use that information to work collaboratively with the university to improve the program.

Coming up soon we have our second Inter-Society Soccer tournament against the engineering, law and dentistry students and Flinders Medical Students’ Society. Last year the AMSS took home the cup, but I hear the other societies have been training hard to turn the tables this year.
The day after the tournament we have our members suit up for this year’s MedBall, with the theme being ‘Med Gala’, taking inspiration from the Met Gala. This year’s MedBall will no doubt be vibrant and glitzy, to say the least!

Soon after MedBall we head into September, when our Annual General Meeting (AGM) is held, and the current AMSS passes the torch to tomorrow’s AMSS. This is always an exciting time for our society. During the AGM we have the opportunity to thank this year’s committee for their service and usher in the next bright-eyed committee, which we are confident will give back and continue the cycle of service to our fellow students and the community.
Laura Kelly AMSS Acting President 2024

(From top) The 2024 AMSS Committee
‘Best stall’ winners at the International Food Fiesta, AMSS representatives at the International Food Fiesta
Medicinal magic
The 2024 Flinders Medical Students’ Society (FMSS) Wright Evans Medball was a roaring success, fitting this year’s ‘The Most Magic Night of Your Dreams’ theme. With more than 250 attendees and the beautiful National Wine Centre as the venue, it was magical indeed. Everyone who attended will have wonderful memories of a highlight of their medical education in 2024.
A special thanks to our sponsors, Wright Evans Partners, without whom this event would not have been possible.
FMSS President Grace Mackenzie





FMSS External Vice President Syme Aftab and Internal Vice President Le Jiang
Isabella Wang, Emily Middleton, Aislin Forrest
Gabriel Tramaglino and Hannah Davidson
Lydia Smalls, Amy Tregenza, Adele Czechowicz and Grace Mackenzie
FMSS Senior Vice President and AMA(SA) Council student representative Lydia Smalls and FMSS President Grace Mackenzie

Culture on show
Topics ranging from dermatology in general practice to doctors’ financial ‘health’ captured the interest of attendees at the South Australian Indian Medical Association (SAIMA) Annual Scientific Meeting and Charity Gala on 29 June.
Members welcomed representatives from government and corporate partners at the dinner, staged at the Adelaide Entertainment Centre. The evening was an extravaganza, showcasing Indian music and dance, highlighting the achievements of the Indian medical community, and raising funds for the Cancer Care Centre.
SAIMA would like to thank all their sponsors, without whom the SAIMA ASM and Charity Gala Dinner would not be possible.
- SAIMA President Dr Jaiveer Krishnan



Professor Nicola Spurrier presenting the President’s Award to Professor Renuka Visvanathan for her contributions to medical research
Dr Vidya Bhushan Chadha receiving the Lifetime Achievement Award for his service to ophthalmology from Multicultural Affairs Minister Zoe Bettison
SAIMA Committee (From left) Mrs Julie Boultby, Dr Chetan Pradhan (seated)
Dr Pravin Hissaria, A/Prof Venkat Thiru, Dr Jaiveer Krishnan, Dr Neeraj Gupta (seated), Dr Kamban Babu, Dr Sanjeev Sabharwal, Mr Rudraksh Gupta, Mrs Reeba Mathew (seated).
(From left) Mr Rudraksh Gupta, Dr Kamban Babu, Mrs Reeba Mathew, A/Prof Venkat Thiru, Dr Pravin Hissaria, Dr Jaiveer Krishnan, Dr Chetan Pradhan, Dr Neeraj Gupta

We recently travelled to the southwest of Ireland with an active walking group to experience the unique geography, history and culture of the ‘Emerald Isle’.
The long history of Ireland is evident everywhere, with carbon-dating indicating neolithic settlement from 6000 BC and the discovery of ritualistic burial sites pointing to evidence of social organisation and burial beliefs and customs.
It was in 500 BC that the Celts arrived from India via mainland Europe. They ruled the land of Ireland through the centuries, including the long periods of Viking and Norman settlement, right up to the 16th century AD when the British took control.
Interestingly, the Romans never occupied Ireland, considering it too cold and hostile to bother with. Their name for it, Hibernia, reflected their less than fond regard for it as a cold, wintry and undesirable place. So, no
TREADING ANCIENT PATHS
Medical editor Dr Roger Sexton found fascinating history lessons at every turn when touring southwest Ireland.
cobbled streets!
The history of British rule over Ireland and the mistreatment of the Irish is a common theme at visitor destinations and in guide commentary. The passion for Irish independence and unification is palpable and promulgated through some of their catchy and emotional folk music. This was evident at the atmospheric pubs to which we had the pleasure of going.
The Irish rebellion in 1916, the Irish War of Independence barely five years later and then the Irish Civil War not long after that set the scene for ‘The Troubles’ to come.
But it’s easy to forget the centuries of turmoil during a quick stop in the rural areas of south-west Ireland. The geography is so pleasant and green, with sheep-studded paddocks bordered by stone walls and hedgerows and little villages full of well-maintained houses as pretty as pictures.
Neat gardens and baskets of petunias adorning houses, bridges and windowsills were a colourful feature
‘Ireland’s
everywhere.
We walked the unique countryside, from the limestone Burren country to the mountainous areas and lakes near Killarney, to the western coastal Cliffs of Moher.
We boated along lakes and rivers to our mountainous destinations. The remote Blasket Islands off the Dingle peninsula were a highlight, not only for their history of human survival and cultural and literary development but also the whale-watching nearby.
The mid-summer weather was in our favour but was always somewhat unpredictable. We had heard ‘Ireland is either wet or very wet’ and we must have been lucky. Still, taking clothing to cover all eventualities was essential.
It was surprising to see surfers in the water along the west coast taking advantage of the big swells from the Atlantic moving onto the shore. The warmer gulf stream from the Caribbean also moderates the Irish climate quite favourably when compared with Scotland.
We stayed in lovely hotels and guesthouses and found the hosts, the meals and accommodation all to a high standard.
The Irish economy is now the second best-performing in Europe, having been a ‘basket case’ not so long ago. The “I” in ‘PIGS’ stood for Ireland. The signs of prosperity were evident everywhere we went. Euros are the Irish currency and this made for a more favourable currency exchange compared to the British pound.
South-west Ireland offered us a most memorable travel experience, made all the better for travelling with 24 outgoing walking friends with the same attitude to travel and adventure and an appreciation of a good evening’s dining and entertainment.
This is a safe, most interesting and highly recommended travel destination.




X-TRAIL ON THE ROAD AGAIN
The force is with Nissan’s new-look e-Power SUV, writes Dr Robert Menz.
This edition of medicSA gives me the pleasure of introducing to you the facelifted Nissan X-Trail, just in time for Spring. Although the X-Trail has been around for more than two decades, neatly filling the medium SUV space for Nissan, it is now available for the first time as a hybrid.
Nissan has some experience in the electric vehicle space, with the Leaf having been the first commercially available fully electric vehicle when it was released in 2009, just before the Mitsubishi MIEV. Nissan has also this year released an e-POWER version of its Qashqai compact SUV. The main competition for X-Trail would be Toyota’s RAV4 hybrid (if you don’t mind a two-year wait) and Mitsubishi’s PHEV Outlander, although plug-ins do require topping up with electricity to maximise their efficiency.
$49,990 for the X-Trail ST-L e-POWER for 2023-built vehicles only, while stocks last.
YOU ONLY NEED TO USE THE BRAKES FOR RAPID BRAKING
X-Trail is a four-model series ranging from the basic ST listed at $37,750 MRP to the top-end Ti-L at $53,990; the test car was the ST-L, available for $50,490 in the e-POWER model. However, at the time of writing Nissan was advertising a special driveaway price from
So, what is e-POWER, I hear you ask? Conventional hybrid engines use either internal combustion or electric engines to power the wheels. e-POWER technology uses a high-output electric motor to exclusively drive the wheels, with the petrol engine generating the required electricity. The result is a smoother and more responsive driving experience. e-POWER uses a 1.5 L three-cylinder petrol engine to charge the battery and that alone drives the electric motors, powering all the wheels. In addition to the petrol engine, e-POWER uses regenerative braking to help keep the battery topped up. This means you only need to use the brakes for rapid braking or to bring the car to a complete halt.
X-Trail is also available with a conventional 2.5 L four-cylinder petrol engine, with two electric motors producing a combined total of 157 kW. The basic X-Trail has two-wheel drive with all-wheeldrive available across the range. The e-POWER X-Trails
are all-wheel drive, and Nissan calls this e-4orce.
The basic ST is very well equipped with an extensive range of safety equipment but also includes Apple CarPlay touchscreen and folding, heated, door mirrors. TI includes extra features such as 18-inch alloy wheels with tyre pressure monitoring climate control and heated adjustable power seats for the driver. The top range X-Trail features a larger 12.3inch touchscreen display, wireless CarPlay, satnav, sunroof, electric tailgate, and heating for the second row of seats and the steering wheel.

Driving the X-Trail was very straightforward. The only problem that your reviewing driver had was being unable to safely overtake because the car would not exceed 100 kph. I eventually realised that instead of activating the cruise control, I had inadvertently activated the speed limiter. Once sorted the X-Trail became much more driveable.
During a short testing period I did have the opportunity to drive a car full of gentlemen to the recently opened Ondeen Restaurant at Verdun. We had a very pleasant
lunch in the wintersunfilled sunroom overlooking the small vineyard, with its resident kangaroo grazing between the vines.
On another day, there was no problem accommodating my bicycle when I put down both rear seats. On this occasion the senior cycling group, having been successfully caffeinated at the Loose Caboose, rode to Port Adelaide on a wet and windy Monday morning. We much appreciated shelter and delicious morning tea in Pancakes At The Port while waiting for the showers to abate.
In summary, the Nissan X-Trail ST-L e-POWER with e-4orce is a competent, comfortable and accommodating midsized SUV.
Vehicle supplied by Nissan Australia.
Dr Robert Menz is a GP and enthusiastic motorist, who is happy to discuss sharing the vehicle testing responsibilities with any AMA members who might be interested.
Hamilton House Plastic Surgery
RICHARD HAMILTON MBBS, FRACS, Plastic Surgeon, wishes to notify colleagues that his private clinic Hamilton House Day Surgery is fully accredited under the rigorous Australian National Standards (NSQHS) for health care facilities and also by QUAD A (American Association for Accreditation of Ambulatory Surgery Facilities, inc.) (www.quada.org).
Richard Hamilton continues to practise Plastic and Reconstructive Surgery at Hamilton House; 470 Goodwood Road, Cumberland Park, with special interests in skin cancer excision and reconstruction, hand surgery and general plastic surgery.
He also welcomes patients considering cosmetic surgery, who now by government regulation, require a referral from their General Practitioner.
A “See and Treat” service is also available for urgent skin cancer patients and patients travelling from rural areas, with convenient, free, unlimited car parking at the premises.
Richard also consults fortnightly at Morphett Vale, and monthly at Penola and Victor Harbor. He is available for telephone advice to GPs on 8272 6666, and readily accepts emergency plastic and hand surgery referrals.
Referrals can be faxed to 8373 3853 or admin@hamiltonhouse.com.au For all appointments phone Richard’s friendly staff at Hamilton House on 8272 6666 www.hamiltonhouse.com.au

RESPECTED AND ADMIRED
Dr Ross Treloar Wishart Reid
MBBS MD MRCAP
1925 – 2024
Ross Reid was born in Adelaide to John Tennyson Reid, a solicitor, and Irene Mildred (née Treloar) and, apart from stints overseas for professional development, he lived his entire life in the city. After schooling at Prince Alfred College and a discussion with his father about what profession he might follow, he chose medicine and won a Commonwealth Scholarship to the University of Adelaide. This was critical as his father died two months after he began first year of medicine and his mother was in no position to support her son for six years of university training.
After winning the Lister Prize for proficiency in practical surgery in 1945, Ross graduated in 1947 and proceeded to junior positions at the Royal Adelaide Hospital (RAH) and the Adelaide Children’s Hospital before joining the Institute of Medical and Veterinary Science in 1950 as a junior assistant clinical pathologist.
At the same time, he became a lecturer in pathology at the University of Adelaide, and in 1957 became a reader in the Pathology Department, a role he held until 1964. Concurrent with these positions was his role of honorary assistant pathologist at the RAH. He performed many autopsies and had the privilege of being taught by and working with Professor Sir John Cleland.
Ross lived with his parents at their home in Collinswood until his marriage on 11 December 1948 to childhood sweetheart and near neighbour, Muriel Vera Fricker. The 1950s were an eventful time for the young couple with Ross’s busy professional life and the arrival of five children within 10 years. Muriel was a physiotherapist but stayed at home with the children before taking up part-time work when her youngest son went to school.
UK and US research opportunities
During this time Ross completed an MD thesis, conferred in 1956, on the relationship between kidney disease and diabetes. He was also awarded a Nuffield Dominion Travelling Fellowship in 1956 to undertake research in London and Chicago, and was accompanied by his wife and two young sons. In London he worked in Professor Payling Wright’s Department of Pathology at Guy’s Hospital. His research there focused on the chemistry and cytology of myelin development, specifically the relationship between glial cell proliferation and myelin sheath formation in the spinal cord of chick embryos. A highlight of Ross’s sabbatical was five days at Oxford University, where he met Sir Howard Florey and visited the laboratories of the Sir William Dunn School of Pathology.
In Chicago, Ross worked with Professor Robert Kark of the College of Medicine at the University of Illinois. There he set up a section cutting department to examine material from patients with nephrotic syndrome as part of a wider study of kidney disease by means of percutaneous renal biopsy, including biopsies using electron microscopy.
In 1963 Ross used a Harkness Travelling Award to study the teaching of pathology in North American medical schools.
Returning home
In 1965 he joined Gribble and partners (‘Gribbles’), then the only private pathology firm in South Australia. Ross joined Drs Michael Gribble and Ruth Osmond in their rooms in Gawler Chambers on North Terrace as a tissue pathologist. Other partners joined the firm, including lifelong colleagues and friends, Dr Phil Hodge (senior lecturer in the Pathology Department at the University of Adelaide), Dr Ian Robertson and Dr Doug McGill (senior pathologist at the IMVS). Ross was a dedicated and skilled medical teacher and, with his three colleagues, resumed teaching medical students on a voluntary basis in the 1970s.
As the Gribbles’ practice expanded, new rooms were built in Ward Street at North Adelaide. Later the firm moved to the corner of Goodwood and Greenhill roads. We well remember our father leaving home in Marlborough Street, College Park, earlier and earlier each year in the 1970s to beat the crosstown traffic. Ross ceased working with the Histopathology Department of Gribbles Pathology in 1988. He continued working as a tissue pathologist with other firms, including Clinpath, before retiring in 1996.
New interests in retirement
Like many other South Australian medical practitioners before him, in the late 1960s Ross became interested in bird watching. Over the next 50 years he and Muriel travelled through much of South Australia and beyond pursuing their passion for birds and nature. They purchased a bush block at Inman Valley in the 1970s and enjoyed showing the property to friends and fellow birdwatchers.
When not working or chasing birds, Ross and Muriel could be found at Adelaide Oval watching Test and Sheffield Shield matches. They had their special seats and were surrounded by friends and fellow cricketwatchers with whom they shared companionship and afternoon tea treats. One of Ross’s treasured possessions was a 1997 letter from Sir Donald Bradman, in response to a letter asking why Bradman had kept wickets for South Australia. Sir Don explained that during a match at the Sydney Cricket Ground, their wicketkeeper suffered a broken finger, so he had volunteered to wear the gloves for the rest of the match.
While a self-confessed poor athlete, Ross supported the Norwood Football Club. For some years in the 1960s he joined his good friend and GP, Dr Brian McCarthy, as club doctor and he was often to be found watching matches on a Saturday afternoon.
Ross was a proud Prince Alfred College graduate and great supporter of the school, sending his four sons there. One of the highlights of his last years was the arrival of the Princes Record, which we would read to him as his eyesight failed.
Ross and Muriel were proud that their eldest son studied medicine, moving into general practice, and the dynasty continues with two grandchildren becoming medical practitioners. After moving into aged care in 2015, Ross and Muriel celebrated their 70th wedding anniversary before Muriel’s death in late 2019. Ross continued to receive family and friends until the end of his long and productive life.
The family has a letter dated 24 April 1996 from Mark Coleman of the Royal College of Pathologists of Australasia (SA branch) acknowledging a letter from Ross about his retirement. Ross noted that he was ‘saddened by the prospect’ of retirement from pathology. Mark had some very kind words to say about Ross and his contributions when he was a trainee at the IMVS (1974–77) and the monthly case meetings of all Adelaide pathologists. ‘I developed then a respect and admiration for your wisdom and experience which remains to this day,’ he wrote.
A private memorial service was held in August to celebrate Ross’s life and times.
- Dr Mark Reid, Penelope Paton, Emeritus Professor Nicholas Reid and Dr Julian Reid
Medico of merit

Sir Joseph Cooke Verco
MB LRCP FRCS BS MD 1851 - 1933
A highly renowned physician, administrator, naturalist and philanthropist, Sir Joseph Cook Verco was a foundation member and later President of the South Australian branch of the British Medical Association (which later became the AMA in South Australia) and, with Edward C Stirling, a founder of the University of Adelaide’s medical school.
His tenure as President of the BMA(SA) was extraordinary: his two terms were 30 years apart and the second lasted an unsurpassed five years and spanned World War I.
Apart his other positions and interests, Sir Joseph was a renowned conchologist and malacologist and President of the Royal Society of South Australia from 1903 to 1920. The Royal Society established the Sir Joseph Verco Medal in his honour in 1928. It is awarded for distinguished scientific investigations carried out by a member of the Society.
For more about the history of AMA(SA) and the medical profession go to the AMA(SA) History Committee’s website at https://amasahistoricalcommittee.wordpress.com/
MRCS
J C Verco in 1919 From a framed photograph in the archives of the University of Adelaide captioned ‘Dean of Dental Faculty, Adelaide University 1920-1928’


Reality check
Is the wine you’re buying from a real winery?
The wine industry has gone through some dramatic change in recent years and the retail landscape has had the biggest shake up of all. Where once the local bottle shop or independent chain was where most of retail wine was sold, we now have a market dominated by two major players through a series of aggressive acquisitions. This has led to a dramatic reduction in the number of independent wine retailers. Many commentators are reluctant to use the ‘d’ word but duopoly is very close to the mark.
What does It mean for the buyer?
For some consumers this is a bonanza. Big wine brands are discounted to a level where in many cases they are being sold at or near cost price to influence you to reach for your wallet. So, where is the margin recovered for these companies?
The official term is ‘buyer own brands’, a concept born of collaboration between a retailer and existing winery,
a relationship both parties were proud to support and acknowledge. It creates a special bottling of a wine made for that retailer, bearing the winery’s name. Sadly, however, this concept has gone down a disturbing road where biblical volumes of bulk wine are being passed off as wine brands that exist from companies you’ve never heard of before, or, worse, companies that haven’t existed for years. At $10 or less for a bottle, consumers are prepared to take a punt and in many cases the margin made on these wines are bigger than a restaurant mark up. Yes, you’ll see an address on the label somewhere – it’s the law – but look up the address and in many cases it either leads to the same refinery or a registered address nowhere in cooee of a winery. Don’t get in your car to visit the cellar door – it’s not there and never was.
None of this supports the wine industry, the growers, the vineyard contractors, the rural towns that support these people. The ‘beveragitisation’ of the wine industry remains a big challenge for wine producers and legislators alike. The next five years will be a critical time in an industry that’s been under siege since ‘the wine glut’, prolonged by the global financial crisis and parity with the US dollar (not to mention China).
As consumers of wine, you can do your bit by buying what’s real. When you’re pondering your next wine purchase, ask your wine merchant about the providence of your wine. In our case, we continue to champion wineries that do exist, that have a destination or family-owned vineyard. There’s enough variety and value out there without making it up. - Phil Manser



Have you recently changed your:
• Contact information
• Payment details
• Place of work
Scan the QR code, or log in to the Member Portal at ama.com.au/sa
Update your details under settings
For any enquiries, please contact AMA(SA) at membership@amasa.org.au or 8361 0108.
medicSA is produced quarterly. Published in print and digital formats, and strongly supported by social media channels, medicSA ensures your message resonates far beyond its pages.
2024 Advertising Bookings
We take pride in delivering exceptional value to our advertisers, ensuring your brand receives the recognition it deserves.
Publication:
Booking Deadline:
Artwork Deadline: Summer 2024 30 October 2024 13 November 2024
2024 Editorial Submissions
Please submit your editorial request or your article for consideration by these dates:
Publication: Submission Deadline: Summer 2024 21 October 2024
For all advertising & editorial enquiries, please contact: medicSA@amasa.org.au

AMA is the sole leading advocate representing doctors from all specialties.
Join AMA(SA) to play a crucial role in shaping a healthcare landscape prioritising the well-being of both medical practitioners and the South Australian population.

ADVOCACY
On a comprehensive range of topics important to our members such as payroll tax, regional contracts, and single employer models.
PROFESSIONAL SUPPORT
Including networking events and committee participation, access to AMA fee guidelines, subscriptions to the MJA and medicSA, and an upcoming mentorship program.
Join us and use your voice to strengthen ours.
*Membership fees are tax deductible.
EXCLUSIVE MEMBER BENEFITS
Increasingly exclusive offers including car dealerships, gym memberships, financial advice, loans and lifestyle activities.

