@aestheticsgroup
@aestheticsjournaluk
Aesthetics
aestheticsjournal.com
Treating Primary Hyperhidrosis Dr Rakesh Anand and Dr Emma Craythorne present an overview of the diagnosis and management of primary hyperhidrosis Hyperhidrosis is a common condition that can have a devastating impact on a sufferer. Not only is it underreported and underdiagnosed, but the significance and implications of the condition are often minimised.1,2 This article reviews the literature to help better guide healthcare professionals on the appropriate non-surgical approach to management, considering not only the location of involvement, but the individual as a whole.
Complications of hyperhidrosis Living with hyperhidrosis presents many challenges and impacts many aspects of daily life. The implications hyperhidrosis has on social and professional life, as well as mental and emotional health, cannot be underestimated. In addition, constant moisture from sweating can lead to chronic skin conditions.3,9,12 One study of 2,017 patients found the prevalence of anxiety and depression was 21.3% and 27.2% in patients with primary hyperhidrosis; higher than is reported in the general population.12
Definition Hyperhidrosis, or excessive sweating, is a common condition that can have profound psychological and social implications for the sufferer.3 It is defined by the secretion of sweat in amounts greater than is physiologically needed for thermoregulation. Sweat is produced by the eccrine sweat glands, which are distributed all over the body but are most numerous on the palms and soles.4 Hyperhidrosis can be classified by the presence of an underlying cause (primary or secondary) or by location (focal or generalised). Most commonly, hyperhidrosis is a chronic primary (idiopathic) condition; however, secondary medical causes or side effects of medications need to be excluded (Table 1).4
Prevalence and epidemiology The estimated prevalence of hyperhidrosis ranges from 1-5% of the population.5,6,7 The true prevalence of hyperhidrosis is unknown as it is often underreported by patients and underdiagnosed by healthcare professionals.1,2 The condition tends to start in childhood or adolescence but can occur at any age,8 and males and females are affected equally.9 Hyperhidrosis is uncommon in the elderly, reassuringly suggesting primary hyperhidrosis symptoms often improve with age.10
Some of the challenges and problems associated with hyperhidrosis include:11,13 • Effects on quality of life/impacts on activities of daily living – social embarrassment, relationship difficulties, impaired performance at work/school • Anxiety and depression • Bromhidrosis – unpleasant smell from by-products from bacteria living on the skin • Skin maceration with possible superadded bacterial or fungal infection • Pitted keratolysis – superficial infection on the soles of the feet characterised by pitting
Treatment Before selecting appropriate treatment, the practitioner must begin by considering the location of the sweating and combine this with factors such as the patient’s preference for treatment, as well as other factors such as availability, practicality, side effects, cost, safety, and efficacy. Table 2 outlines the suggested first and second-line therapies for hyperhidrosis dependent on location of involvement.13
Diagnosis Idiopathic hyperhidrosis that is localised to certain areas of the body is called primary focal hyperhidrosis. Primary focal hyperhidrosis (PFH) often affects the axillae, palms, and soles, but may also impact other sites, such as the face and scalp. It can also be multi-focal, affecting several sites of the body at the same, or alternating times. A consensus panel comprised of international practitioners suggested a diagnostic criteria for PFH.8,11 They proposed that the patient must display focal, visible, excessive sweating of at least six months duration without apparent cause, plus at least two of the following characteristics: • Bilateral and relatively symmetrical sweating • Interferes with daily activities • At least one episode per week • Onset before 25 years of age • Positive family history • Localised sweating stops during sleep
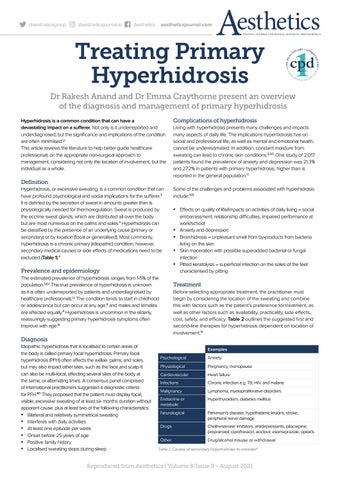
Examples Psychological
Anxiety
Physiological
Pregnancy, menopause
Cardiovascular
Heart failure
Infections
Chronic infection e.g. TB, HIV, and malaria
Malignancy
Lymphoma, myeloproliferative disorders
Endocrine or metabolic
Hyperthyroidism, diabetes mellitus
Neurological
Parkinson’s disease, hypothalamic lesions, stroke, peripheral nerve damage
Drugs
Cholinesterase inhibitors, antidepressants, pilocarpine; propranolol, ciprofloxacin, aciclovir, esomeprazole, opioids
Other
Drug/alcohol misuse or withdrawal
Table 1: Causes of secondary hyperhidrosis to consider4
Reproduced from Aesthetics | Volume 8/Issue 9 - August 2021