HEALTHCAREWILL NOTREALIZEITSFULL POTENTIALUNLESS CHANGE-MAKING BECOMESANINTRISIC PARTOFEVERYONE’S JOB,EVERYDAY, INALLPARTSOFTHE SYSTEM.








QI leadership is demanding it requires navigating complexity, shifting mindsets, and fostering collaboration across levels Why It matters now
Co-production strengthens relevance and equity when patients, communities, and staff design care together, solutions are more sustainable
Kindness is a strategy,not a soft skill it improves psychological safety, builds trust, and drives better outcomes
Traditional,top-down approaches are not enough systems must support shared learning, humility, and relational leadership
CoproductionasaNewStandardforCare
Coproduction redefines the relationship between healthcare providers and users positioning both as equal partners in care design delivery and evaluation Bata den et al (2016) argue that health services are not simply delivered to pass ve recipients, but are co-created with people based on shared expertise, experiences, and goals In the African context where community engagement has long been centra to health programming coproduction offers a framework for deeper more equitab e collaboration
KindnessandCompassionasSystem-LevelImperatives
Kindness in healthcare is not just a virtue it is a strategic mperat ve for safety, wellbeing, and effectiveness Greco colleagues (2025) show that embedding kindness improves team function ng reduces staff burnout and enhances patient trust and outcomes In systems where healthcare workers often face emotiona fatigue and resource constraints compassion must be supported structura ly not just expected individua ly
SystemsThinkingtoNavigateComplexity
Health systems are complex adaptive systems where interventions often yield unexpected outcomes Peters et al (2014) stress the importance of systems thinking n eva uating the dynam c relationships and power structures that shape implementation This is especially critical in contexts where frontline healthcare workers, communities, and managers must continually adapt to changing needs and resources
Addressing Nonadoption and Sustainability
Despite significant investment in hea th innovat on many intervent ons struggle to scale or sustain impact due to ssues of nonadoption abandonment and m sa ignment with ocal systems (Greenhalgh et a 2020) This forum seeks to address these cha lenges
Across sub-Saharan Africa, health systems have made substantial progress in expanding access to essential services However, significant challenges remain in delivering care that is safe, compassionate, people-centred, and responsive to local realities Studies have shown that poor quality of care now contributes more to mortality than lack of access alone (Kruk, 2018), highlighting the need for a fundamental shift in how care is designed and delivered (Roberts et al , 2020)
To meet these challenges, this Forum focuses on coproduction, kindness, and systems thinking as transformative strategies for sustainable quality improvement
The 2025 ACQUIRE QI Leadership Forum is a unique opportunity to convene quality improvement champions from across the continent and around the world As countries move from pandemic recovery to long-term transformation, now is the time to reimagine care systems that are co-produced, compassionate, and rooted in equity and trust
RSVP and Next Steps: We look forward to welcoming you to Nairobi for the 2025 QI Leadership Forum To confirm your virtual participation, please fill out this registration form
TTo showcase models of co production in healthcare service delivery and improvement
To explore how kindness and compassion can be embedded at the heart of quality improvement
To examine the use of systems thinking in designing, evaluating, and sustaining change
To strengthen collaborative leadership and learning networks for QI across Africa
To elevate the voices of frontline workers and communit es as central actors in health system reform
A regional vision for co-producing safer, kinder healthcare in Africa
Strengthened understanding of how to apply systems thinking for sustainable QI
A shared platform for peer learning, resource exchange and innovation
New momentum for embedding compassionate care approaches in policy, training, and practice
Expanded ACQUIRE virtual community with over 1 000 active participants shaping the future of QI

















































Which seat are you picking for your next flight to the 2025 QI Leadership Forum? 1 2 3
































THE
Dr. Mary Adam
Ruthpearl Ng’ang’a
Dr. Lydia Okutoyi


Day 1
Thursday, July 10, 2025
Day 2
Friday, July 11, 2025
:30am
:00am 10:30am 11:00am
–
Tea/Coffee/Health Break
Session 2a – Co-Producing Safer Care: Voices from the Ground Patient and provider stories on cocreating safety
1:00pm
3:30pm
Session 3 – Incident Reporting Across Africa From Silence to Safety: Mapping African Incident Reporting
Session 5 –From Quality Assurance to Quality Improvement to CoProduction: A Journey Every Healthcare Worker Should Take
Tea/Coffee/Health Break Lunch Break
Session 2b – Co-Producing Safer Care: Practical Tools & Frameworks. How to design for co-production in real-world settings
Session 6 – Exploring Generative AI’s Role in Enhancing Quality of Care: Exploring How Technology is Enabling Human-Centered Communication, Consent, and Care Session 4 – Training Needs
Session 7 – Celebrating Frontline Innovation: Scientific Poster Presentations on Quality Improvement
+ End of Day Recap



Many health systems prioritise patient safety on paper, but few embed it into daily practice to reduce risk and harm.”
Sir Liam Donaldson


Date: Thursday, 10 July 2025 | Time: 9:00AM - 10:30AM EAT
Plenary Panel
The Global Patient Safety Action Plan (GPSAP) offers a powerful roadmap to eliminate avoidable harm, but translating it into action in African contexts requires tailored strategies This session explores how countries are adapting the GPSAP to local realities strengthening leadership, systems thinking, workforce capacity, data use, and patient engagement Through shared experiences and practical tools, participants will learn how to embed safety at all levels of the health system
Share real-world experiences from countries at various stages of GPSAP implementation
Provide a space for African stakeholders to benchmark progress and challenges
Foster cross-country learning and collaboration, with a focus on practical tools, systems, and leadership approaches
Encourage co-production with patients and frontline health workers in safety strategy design and implementation
While the Global Patient Safety Action Plan (GPSAP) provides a clear strategic framework, translating it into meaningful action remains a challenge in many African settings Health systems must adapt the plan to local realities, navigating barriers such as limited infrastructure, weak data systems, and undertrained workforces Effective implementation calls for strong leadership, systems thinking, and inclusive engagement of both healthcare workers and communities This session will showcase practical strategies and innovations that support countries in embedding patient safety across all levels of care
References
Patient safety is a global health priority and a cornerstone of effective, high-quality healthcare systems Despite advances in medical science and healthcare delivery, millions of patients continue to suffer avoidable harm during the course of their care According to the World Health Organization (WHO), unsafe care is among the top ten causes of death and disability worldwide (1)
The Global Patient Safety Action Plan 2021–2030 (GPSAP), launched by WHO, presents a bold and comprehensive strategic framework aimed at eliminating avoidable harm in healthcare Its vision is "a world in which no one is harmed in health care, and every patient receives safe and respectful care, every time, everywhere" (2) The GPSAP outlines seven strategic objectives, emphasizing the importance of policy leadership, safety culture, health worker capacity, patient and family engagement, data use, and system design for safety (3)
The relevance of the GPSAP is particularly urgent in low- and middle-income countries (LMICs), where the risk of adverse events is disproportionately high The Lancet Global Health Commission reported that poor-quality care causes more deaths than lack of access in many LMICs an estimated five million excess deaths each year are due to substandard healthcare (4) WHO's Global Patient Safety Report 2024 underscores these disparities, noting that while some progress has been made, many countries still face persistent challenges in operationalizing patient safety strategies (1)
WHO has issued global and regional calls to action encouraging Member States to adopt and adapt the GPSAP within their national health policies (5). Regional platforms such as the WHO Regional Committee for Africa have endorsed this approach, calling for context-specific solutions and sustainable implementation pathways (6)
1WorldHealthOrganization(2024)GlobalPatientSafetyReport2024https://wwwwhoint/publications/i/item/9789240095458
2WorldHealthOrganization(2021a)GlobalPatientSafetyActionPlan2021–2030:TowardsEliminatingAvoidableHarminHealthCare https://wwwwhoint/publications/i/item/9789240032705
3WorldHealthOrganization(2021c)GlobalPatientSafetyActionPlan2021–2030:AnOverviewhttps://appswhoint/gb/MSPI/pdffiles/2022/09/Item220-09v2pdf
4Kruk,ME,etal(2018)High-qualityhealthsystemsintheSustainableDevelopmentGoalsera:timeforarevolutionTheLancetGlobalHealth,6(11),e1196–e1252
https://doiorg/101016/S2214-109X(18)30386-3
5WorldHealthOrganization(2021b)GlobalActiononPatientSafety:WHA74(13)https://appswhoint/gb/ebwha/pdffiles/WHA74/A74(13)-enpdf
6WorldHealthOrganizationRegionalOfficeforAfrica(2020)RegionalCommitteeforAfrica:SeventiethSessionReporthttps://iriswhoint/bitstream/handle/10665/333998/AFR-RC70-14engpdf


The 2025 ACQUIRE Quality Improvement Leadership Forum Co-Producing Safer Care: Centering Quality and Kindness from the Start
Date: Thursday, 10 July 2025 | Time: 9:00 AM -- 10:30 AM
FORMAT Keynote
SESSION ONE LEAD:
Plenary Panel

KEYNOTE ADDRESS
Reflections
Dr. Lydia Okutoyi Director of Healthcare Quality, Kenyatta National Hospital (KNH), Kenya
SPEAKER PANELISTS
Country Perspectives; Reflections on Advancing GPSAP from a national and institution perspective “From Strategy to System: How the Philippines is Advancing GPSAP Implementation" --- Lessons on structure, leadership, stakeholder engagement, and patient inclusion

Reinavelle
Jeunesse Mateo Patient Safety Program Manager DOH PHILIPPINES
PLENARY REFLECTIONS
Open Mic: Reflections from participants: Where are we on the GPSAP matrix? What support do countries and hospitals need?


Irungu



Dr. Edwin


Dr. Eyobed Kaleb



Dr. Alphonce Chandika


Dr. Bongani Chikwapulo


Dr. Olanrewaju Olatunji Sulaimon
Many health systems prioritise patient safety on paper, but few embed it into daily practice to reduce risk and harm - Sir Liam Donaldson


















FORMAT Keynote
SESSION 2A
SESSION OBJECTIVES
Stories That Transform: The Power of Listening in Healthcare
Plenary Panel
Reflections
Dr. Peter Lachman
International Leader in Healthcare Quality & Safety | Advocate for Kindness in Care

To elevate patient and provider voices in co-production efforts, explore how trust and kindness influence safety perceptions, and inspire leadership cultures that embed listening and storytelling into quality improvement practice
LEARNING GOALS
Reflect on real-world experiences of patients and providers engaged in co-production efforts
Understand how relational factors like trust, kindness, and communication shape safety experiences
Identify strategies for embedding narrative-based approaches and empathetic listening into leadership practice
RATIONALE
Stories bring the human element of co-production to the forefront, challenging assumptions and reconnecting improvement work to the people it serves Patient and provider narratives illuminate blind spots and shift cultural norms that prevent authentic collaboration This session recognizes that co-production begins with listening to lived experiences of those who receive and deliver care Creating space for vulnerability and reflection helps leaders develop relational skills necessary for meaningful partnership
SESSION 2A : KEY POLL INSIGHTS
of respondents identified "assuming we know patients' needs" as Africa's top barrier to listening and 40% said time constraints. of respondents reported listening to patient feedback daily of respondents said, the thing that most influence a patients sense of safety is staff communication
Health systems often underrepresented voices of patients, families, and frontline providers in care decisions, despite evidence that these perspectives are essential for safe, respectful care (1) Co-production requires moving beyond tokenistic consultation toward genuine partnership where users define quality (3) Research shows that when healthcare embraces kindness as a strategic imperative, it creates psychological safety for patients and staff to speak up about safety concerns(2)
Studies across African contexts show that respectful, compassionate care impacts patient trust and care-seeking behaviour When providers feel heard and valued, they engage more in quality improvement efforts However, structural hierarchies, time pressures, and cultures of blame often limit meaningful engagement Evidence suggests that embedding storytelling into improvement work can bridge these gaps by creating emotional connections that motivate sustainable change (1)
Person-centered care requires understanding individual experiences and preferences, moving beyond standardized protocols to responsive, relationship-based approaches (5) Successful coproduction initiatives show that when patients and providers collaborate as partners, outcomes improve and satisfaction increases across all stakeholder groups (1,3,4)
There is clear momentum for systemic reforms, emphasizing leadership, institutional structures, and foundational education over isolated interventions


FORMAT Keynote
SESSION 2B
Plenary Panel
Session Objectives: To introduce practical frameworks and tools for operationalising co-production in resourceconstrained settings, highlight adaptable approaches from diverse African contexts, and strengthen participants' confidence to implement co-production in their organizations
Understand user-friendly models and engagement strategies that support meaningful patient and staff participation
Reflect on low-resource approaches for co-production in diverse African health system settings
Identify enabling conditions and entry points for implementing co-production efforts in participants' contexts
While co-production is widely endorsed as a principle, many health systems struggle to operationalize it due to structural hierarchies, resource constraints, and absence of practical frameworks Leaders need guidance that bridges theory and practice This session recognizes that co-production is a skillset requiring training, tools, and institutional support Moving from values to methods helps embed co-production into daily practice rather than leaving it as an aspirational concept 1
Reflections
Prof. Elizabeth Bukusi Global Health Leader, Expert in Research Ethics, Community Engagement & Implementation Science

Implementation science shows that successful adoption of new practices requires addressing both technical and adaptive challenges (1) Co-production represents a shift from providercentered to user-defined approaches, requiring new frameworks for engagement (2,6) Research across sub-Saharan Africa shows that community health programs succeed when they incorporate local knowledge and enable community ownership (3,4)
Studies of co-production in healthcare reveal that successful initiatives share common characteristics: clear roles, adequate time for relationship-building, training for providers and users, and organizational commitment to sharing power (2,6) However, many efforts fail due to insufficient attention to contextual factors, power dynamics, and sustainability planning (1)
Evidence from African health systems suggests that co-production approaches must be adapted to local contexts while maintaining core principles of partnership and mutual respect (3,5) Successful frameworks emphasize starting small, building trust gradually, and focusing on tangible improvements When users define quality in healthcare delivery, both processes and outcomes improve significantly (7)
The community values patient engagement and shows readiness for co-production, but time, assumptions, and leadership gaps hinder deeper implementation


Co-Producing Safer Care: Centering Quality and Kindness from the Start
Dr. Peter Lachman is a pediatrician and internationally recognized expert in healthcare quality and safety Formerly the CEO of the International Society for Quality in Health Care (ISQua), he has led global initiatives to embed compassion, co-production, and patient safety at the heart of health systems. A pioneer in positioning kindness as a strategic imperative, Dr. Lachman's work emphasizes that safe care cannot be achieved without psychological safety, empathy, and listening In this session, he will draw on decades of experience and the voices of patients and clinicians to demonstrate how storytelling and relational leadership can transform organizational cultures from the ground up
Prof. Elizabeth Bukusi is a leading researcher and implementation scientist with over 30 years of experience designing and evaluating community-engaged health interventions in Africa. She is a champion for ethical, inclusive, and participatory research and healthcare practices In this session, Prof Bukusi will bring her deep expertise in community partnership, co-design, and contextualized quality improvement to share practical tools and frameworks for embedding co-production in real-world health system settings Her approach bridges evidence and action, ensuring that co-production is both principled and practicable
International Leader in Healthcare Quality & Safety | Advocate for Kindness in Care
Bukusi Global Health Leader
Expert in Research Ethics, Community Engagement & Implementation Science
KEY NOTE SPEAKERS






Errors must be accepted as evidence of system flaws, not character flaws.
Dr. Lucian Leape


Date: Thursday, 10 July 2025 | Time: 2:00PM - 3:30PM EAT
Hybrid Panel Discussion
SESSION OBJECTIVE
To explore current incident reporting mechanisms across African healthcare systems, identify critical barriers and enablers to safe reporting, and map approaches that can transform medical error reporting from punitive silence to transparency
Share existing formal and informal incident reporting mechanisms from participants' contexts
Identify cultural, organizational, and structural barriers that inhibit error reporting
Map practical approaches for creating psychologically safe reporting environments
Building trust in incident reporting systems requires a shift from fear-based to learning-oriented approaches Cultures of blame and risk avoidance give us systems that try to control rather than learn This session recognizes that incident reporting is not just a technical tool it reflects organizational culture, leadership values, and the quality of relationships among providers, patients and institutions
Participant-generated inventory of current reporting mechanisms and gaps in their immediate contexts
Identification of 3-5 key barriers and enablers that resonate across diverse African healthcare settings
Participant commitments to explore learning approaches that build trust and psychological safety in their institutions
Medical errors represent a significant global health challenge, with the landmark "To Err is Human" report highlighting that healthcareassociated harm affects millions of patients annually (1) The WHO emphasizes that robust incident reporting systems are fundamental to achieving universal health coverage and quality care delivery (2,3) However, studies across Africa reveal significant gaps in reporting culture and infrastructure
Research from multiple African countries shows consistently low incident reporting rates In Nigeria, healthcare workers showed reluctance to report medical errors due to fear of punishment and lack of systematic feedback (8) Similar patterns emerge across Uganda (9), Ethiopia (10), and Kenya (12), where healthcare professionals cite fear of blame, inadequate reporting systems, and absent feedback mechanisms South African studies confirm these challenges, with emergency departments showing poor adverse event reporting despite available systems (15,16)
The barriers are multifaceted: psychological factors including fear of punishment and emotional impact on providers (17), organizational factors such as inadequate training and lack of anonymous reporting systems (18,19), and systemic issues including absence of feedback loops connecting reporting to improvement (20,21) Research from Kenya's Kenyatta National Hospital and national policy frameworks (22,23) illustrate attempts to address these challenges, yet implementation remains inconsistent
Aviation industry lessons show that shifting from punitive to learningoriented error management dramatically improves safety outcomes (5) Healthcare systems adopting similar approaches, emphasizing psychological safety and systematic learning from incidents, show improved reporting rates and patient outcomes (6,24,25) The evidence suggests that successful reporting systems require not just technical infrastructure, but cultural transformation toward transparency, and shared accountability (26,27)


The 2025 ACQUIRE Quality Improvement Leadership Forum
Co-Producing Safer Care: Centering Quality and Kindness from the Start
Date: Thursday, 10 July 2025 | Time: 2:00 PM -- 3:30 PM
FORMAT
Hybrid Panel Discussion
SESSION OVERVIEW This session explores the state of incident and medical error reporting across African healthcare systems Drawing on practical experiences from panelists and data collected through pre-conference polls, it aims to identify common systemic and cultural challenges and highlight practical steps to transform reporting cultures from fear-based to learning-oriented The discussion will center on how to build psychologically safe environments that encourage transparency, reflection, and improvement
PROGRAM AGENDA
KEY NOTE

Ronel R. Steinhobel
National Department of Health
PANEL DISCUSSION
SESSION MODERATOR

Dr. Rhoda Kalondu, Quality & Safety Lead, Ministry of Health,
GUIDING QUESTIONS
OPENING PRESENTATIONS
Incident Reporting in Africa –A Learning Imperative

Dr. Lydia Okutoyi Director of Healthcare Quality KNH
Insights from the Ground: Poll Results on the Status, Barriers, and Enablers of Incident Reporting




Esayas
What systems exist in your country/facility for reporting clinical incidents or medical errors?
How have these evolved – especially in terms of anonymous reporting?
SESSION 3 : KEY POLL INSIGHTS
Does your institution have a structured system for reporting medical errors or adverse events?
Can healthcare workers report errors anonymously in your institution?
Have you personally submitted an error or incident report?
Which format is used for reporting incidents in your facility?
Ruthpearl Ng’ang’a Pro-Founder ACQUIRE



What are the enablers and barriers to reporting at institutional and national levels?
What feedback mechanisms are in place to support learning from reported incidents?
Reporting without action is not enough: turn incidents into insight for safer care















“In time, QI should become a basic skill like cardiopulmonary resuscitation; one that all health professionals acquire early in their training”
Training


Date: Thursday, 10 July 2025 | Time: 3:30PM - 5:00PM EAT
Hybrid Panel Discussion
In the pursuit of safer, people-centered care across sub-Saharan Africa, strengthening the quality competencies of the health workforce is critical This session focuses on the role of Training Needs Analysis (TNA) in identifying, prioritizing, and addressing knowledge and practice gaps in Quality Improvement (QI) and Patient Safety (PS) training at multiple levels---pre-service, postgraduate, and in-service
Drawing from a Kenya multi-site study the session will showcase how training institutions, regulators, and ministries can work together to build a health workforce equipped to lead change.
Understand common gaps in QI/PS training across levels of the health workforce
Analyze real-world examples of multisectoral QI curriculum development and delivery
Identify action points for institutions and policy bodies to
Identify action points for institutions and policy bodies to strengthen QI training using Training Needs Analysis findings
High-quality health systems are essential for achieving universal health coverage and meeting the Sustainable Development Goals Yet, in many low- and middle-income countries, QI and patient safety are under-emphasized in medical and nursing education Health workers often enter clinical service with limited understanding of systems thinking, improvement science, or their role in improving care outcomes [1,2]
A 2017 sub-Saharan African study revealed students and faculty have limited exposure to QI frameworks or methodologies in pre-service curricula [3] This is concerning, given estimates that 1 in 10 hospitalized patients in developing countries suffers preventable harm during care [2]
In response, global actors have developed QI education strategies ranging from graduate medical fellowships [4] to junior doctor engagement models [5], with a growing emphasis on longitudinal, team-based, and workplace-integrated learning [6,7]
Despite these possibilities, challenges remain in identifying where the biggest gaps are, who should be targeted, and how to align QI education with real-world needs This session will present findings from a local Training Needs Analysis, and invite dialogue on policy, design, and implementation priorities The 2025
Despite global consensus on the importance of quality improvement (QI) and patient safety, these concepts remain underrepresented in pre-service health professional education across many low- and middle-income countries Health workers often enter clinical service without foundational training in systems thinking or improvement science, limiting their ability to contribute to safer, higher-quality care This session explores findings from a Kenyan Training Needs Analysis to inform targeted context-sensitive strategies for integrating QI education into health workforce development
Gain exposure to national and institutional QI training needs assessments
Learn from successful integration of QI into education pathways
Contribute to recommendations for policy and systems change in QI capacitybuilding
References
1 Armstrong M, Black D, Miller A Quality criteria for core medical training: A resume of their development, impact and future plans J R Coll Physicians Edinb 2019;49(3):230--6
2 Wilson R, Michel P, Olsen S, et al Patient safety in developing countries: Retrospective estimation of scale and nature of harm to patients in hospital BMJ 2012;344:20
3 Bowser, D, Abbas Y, Odunleye T, et al Pilot study of quality of care training and knowledge in Sub-Saharan African medical schools Intl Journal of Medical Ed 2017 8:276-282
4 Neumeier A, Levy AE, Gottenborg E, et al Expanding Training in Quality Improvement and Patient Safety Through a Multispecialty Graduate Medical Education Curriculum Designed for Fellows MedEdPORTAL 2020;16:11064
5 Mahalingam A, Groom K, Carter, B Lal, A A quality improvement (QI) initiative to increase junior doctor participation in QI Future Healthc J 2017;4(2)
6 Wong B, Etchells E, Kuper A, et al Teaching quality improvement and patient safety to trainees: A systematic review Acad Med 2010;85(9):1425--39
7 Jones B, Vaux E, Olsson-Brown A How to get started in quality improvement BMJ 2019;364


The 2025 ACQUIRE Quality Improvement Leadership Forum Co-Producing Safer Care: Centering Quality and Kindness from the Start
Date: Thursday, 10 July 2025 | Time: 3:30PM - 5:00PM EAT
SESSION OVERVIEW In the pursuit of safer, people-centered care across sub-Saharan Africa, strengthening the quality competencies of the health workforce is critical This session focuses on the role of Training Needs Analysis (TNA) in identifying, prioritizing, and addressing knowledge and practice gaps in Quality Improvement (QI) and Patient Safety (PS) training at multiple levels preservice, postgraduate, and in-service
Drawing from a Kenya multi-site study the session will showcase how training institutions, regulators, and ministries can work together to build a health workforce equipped to lead change
PROGRAM AGENDA
SESSION MODERATOR Peter Mutanda, Healthcare Quality Improvement Specialist International Rescue Committee (IRC)

PANEL DISCUSSION


OPENING PRESENTATION
Brief overview of current approaches to TNA in Kenyan multi-site study

GUIDING QUESTIONS
Does your institution offer formal training in quality improvement (QI)?
Who is targeted for QI education in your institution?
SESSION 4 : KEY POLL INSIGHTS of respondents reported that
How well does your institution train on kindness and patient safety? Somewhat briefly mentioned
Dr. Carolyne Mukuha, Independent Healthcare Quality Consultant

Peris


How well does your institution train on kindness and patient safety? Who Receives QI Training?
There is visible progress toward safety infrastructure, but digital transformation and standardization remain critical next steps














Co‑productionisaboutlevelling hierarchiesand…sharingriskand responsibility…Goodco‑production willalwayscontainelementsoflived experience…It’saboutsharingrisk andresponsibilityandlookingout foreachother.”

Anthony O’Connor, Patient Safety Learning consultant


Co-Producing Safer Care: Centering Quality and Kindness from the Start
Date: Friday, 11 July 2025 | Time: 9:00AM - 10:30AM EAT
Breakout / Interactive Conversation
SESSION OVERVIEW
BACKGROUND The 2025 ACQUIRE
Across Africa and globally, health systems have long relied on Quality Assurance (QA) to ensure compliance with clinical standards and protocols While essential for standardization, QA can often feel top-down and disconnected from frontline realities This session explores the evolution from QA to Quality Improvement (QI) a more participatory, team-driven approach and onward to Co-Production, where patients, families, and communities are recognized as partners in shaping care
While QA remains vital, it is often experienced as externally imposed and disconnected from the realities of patient care Many healthcare workers are familiar with "checking the box, " but less equipped or supported to make improvements or engage patients meaningfully
This session addresses the need to demystify QI and Co-Production, offering healthcare workers across all cadres accessible language, practical tools, and a supportive mindset shift It affirms that even the smallest actions when guided by curiosity, kindness, and partnershipcan lay the foundation for transformational change [1,2,4]
By recognizing the roles that all individuals play in quality, this session aims to equip participants to lead change from where they stand
Participants
Understand the distinctions between QA, QI, and CoProduction and how they relate to their own roles
Feel encouraged and capable of initiating quality conversations or changes, regardless of their position
Identify one testable change that fosters collaboration, safety, or kindness in their context
Engage peers or patients in small acts of co-production as part of daily improvement efforts
FACILITATOR Dr Oluwadamilola Matti & Dr Faith Leilei
Speaker: Dr Peter Lachman -- Former CEO,
Across Africa and globally, health systems have historically leaned on Quality Assurance (QA) to ensure compliance with standards, protocols, and guidelines QA has helped standardize care, but it often manifests as a top-down system of audits, inspections, and checklists that can feel burdensome to frontline health workers
As systems evolve, Quality Improvement (QI) introduces a proactive, participatory approach that empowers teams to identify challenges, test changes, and make data-informed decisions to improve outcomes and processes Building on QI, Co-Production represents a further paradigm shift positioning patients, families, and communities as partners and co-creators in healthcare service design and delivery [1,2]
This continuum from compliance (QA), to collaboration (QI), to cocreation (Co-Production) marks a cultural and operational transformation in how quality is understood, measured, and practiced [3,4] As healthcare workers face increasing demands with limited resources, embracing this journey offers not only efficiency and safety, but also meaning, compassion, and resilience in practice
Clearly distinguish the purpose and characteristics of Quality Assurance, Quality Improvement, and Co-Production using simple, real-life examples
Reflect on their current practice and identify where they are on the continuum of QA QI Co-Production
Recognize the role of kindness and shared decision-making in delivering safer, more compassionate care
Commit to a small, actionable change they can apply immediately in their clinical or administrative context
4


The 2025 ACQUIRE Quality Improvement
Co-Producing Safer Care: Centering Quality and Kindness from the Start
Date: Friday, 11 July 2025 | Time: 9:00AM - 10:30AM EAT
Breakout / Interactive Conversation
FIRESIDE CHAT
SESSION MODERATORS

Dr. Faith Leilei, Director Satellites AIC Kijabe Hospital
SESSION MODERATOR

Dr. Oluwadamilola Matti, Executive Manager Society for Healthcare Quality in Nigeria
GUIDING QUESTIONS
FIRESIDE CHAT MEMBER

Dr. Peter Lachman
International Leader in Healthcare Quality & Safety | Advocate for Kindness in Care
Key Questions:
What's the real difference between QA and QI?
Can small changes make a big impact?
Co-production sounds ideal but how do we start when we’re short on time, staff, or resources?
How do you measure kindness?
QA Lens: Describe early experiences with QA (audit systems, licensing, compliance); strengths and limitations.
QI Lens: Share how structured improvement methods (PDSA, root cause analysis, etc.) brought progress and where gaps remain.
Co-Production Lens: Describe movement toward partnerships with patients/families and what this looks like in action.
How would you describe your institution’s current approach to quality?
What is the biggest driver of quality efforts in your setting?
SESSION 5 : KEY POLL INSIGHTS
of respondents said their institution focuses on Quality Improvement using tools like PDSA and RCA, over compliancebased assurance or co-production approaches
identified internal QI data and audits as the strongest driver of quality efforts, ahead of accreditation or leadership mandates
cited staff training and understanding as the biggest barrier to embracing co-production, while only 19.2% said leadership buy-in was the issue.
What is the greatest challenge to moving toward co-production?
What support would help your team embrace co-production?
There is a strong foundation for quality improvement practices, but co-production remains limited by staff preparedness To progress, institutions need to invest in capacity-building and storytelling to inspire and guide inclusive, collaborative care models



“ThepromiseofAIin healthcareisnottomakeus superhumanbuttomakeus morehumanbyfreeingus fromtasksthatmachines candobetter.”



Date: Friday, 11 July 2025 | Time: 2:00PM - 3:30PM EAT
Breakout / Interactive Conversation
This session is designed to spark a grounded, interdisciplinary dialogue on the responsible and impactful integration of Generative AI in healthcare communication, particularly in under-resourced settings
It will center on how AI can support not substitute human relationships in care, especially in moments that require clarity, compassion, and collaboration
The conversation will focus on three core domains:
1 Strategic opportunities for AI deployment in LMICs, emphasizing tools that are appropriate, accessible, affordable, and scalable
2 Use of AI in enhancing communication, specifically in patient/doctor/next-of-kin conferences, health education, and informed consent
3 Ethical imperatives, including privacy, fairness, cultural appropriateness, and alignment with broader quality improvement (QI) and patient safety agendas
Real-world examples from clinical settings will be highlighted, alongside current implementation science research and field-based experiences from providers actively testing or deploying AI tools
By the end of the session, participants will:
Identify opportunities for the adoption of appropriate, accessible, affordable, and scalable AI solutions in health systems in low- and middle-income countries
Explore use cases where AI can improve communication, including its role in patient/family-provider conversations, health education, and informed consent
Examine ethical imperatives surrounding AI use in healthcare, with attention to governance, cultural relevance, privacy, and health equity
Participants will:
Recognize three practical ways AI can enhance communication and understanding between healthcare workers and patients
Appreciate the value of AI in supporting not replacing compassionate, respectful care
Understand the ethical frameworks required for the responsible deployment of AI in clinical settings
Be inspired to explore or pilot AI tools that improve care quality and safety in their own work environments
FACILITATOR Dr Oluwadamilola Matti & Dr Faith Leilei
Speaker: Dr Peter Lachman -- Former CEO,
Healthcare systems across Africa are increasingly committed to advancing safer, higher-quality, and more patient-centered care Yet despite these goals, systemic gaps in communication between providers, patients, and families persist In many clinical settings, time pressures, high workloads, language diversity, and low health literacy hinder effective engagement and understanding These challenges are particularly acute in low- and middle-income countries (LMICs), where the delivery of patient-centered care often lacks supportive infrastructure or tools
Recent advances in Generative Artificial Intelligence (AI) offer promising opportunities to address these communication gaps AI tools now have the capacity to generate tailored, accessible explanations of medical information; offer real-time translation for multilingual consultations; and facilitate the creation of visual and voice-based content that can support truly informed consent processes [1,2,3] These applications hold transformative potential for enabling patients and caregivers to better understand diagnoses, treatment options, risks, and responsibilities particularly in settings where human resources are stretched
However, the promise of AI must be carefully weighed against its limitations and ethical risks Questions related to privacy, bias, cultural sensitivity, algorithmic transparency, and the potential for dependency or harm remain at the forefront of implementation concerns [4,5] In LMIC contexts, where health systems are still evolving toward robust data governance and equity in service delivery, careful and context-sensitive deployment of AI is essential A human-rights based and quality-focused framework must guide the integration of AI into patient-provider interactions [6]
Dr Fred Mutisya Clinician and AI implementers (Kenya)
Prof Stephen Muhudhia Pediatrician and Founding Member, Bioethics Association of Kenya
Sarah Kiptiness and Rob Korom of Penda Health Storytelling on using AI as a diagnostic support tool in Kenya’s local healthcare setting


The 2025 ACQUIRE Quality Improvement
Forum Co-Producing Safer Care: Centering Quality and Kindness from the Start
Date: Friday, 11 July 2025 | Time: 2:00PM - 3:30PM EAT
FORMAT
Breakout / Interactive Conversation
PROGRAM AGENDA
SESSION MODERATOR

Mike Mulongo Credentials
PANEL DISCUSSION
SESSION MODERATOR

OPENING PRESENTATIONS
Session Overview & Objectives

Prof Stephen Muhudhia
Bioethics, AI, and patient dignity

Dr. Sarah Kiptiness
Penda Health, Organizational innovation with AI tools
GUIDING QUESTIONS
At what point do AI and QI intersect, and what is the value-add to frontline healthcare delivery? E g How can AI support meaningful informed consent---especially when time is short and literacy is low?
What are the most pressing ethical considerations for AI adoption in African healthcare contexts?
SESSION 4 : KEY POLL INSIGHTS
What AI tools have you used/encountered in your healthcare practice?
What is the greatest benefit of AI in Patient Safety & quality improvement?
What is your biggest concern about using AI in healthcare communication?
What do you suggest as essential for the adoption and use of AI in your healthcare context?
How can local governance frameworks and health worker training support safe, ethical AI use?
There is visible progress toward safety infrastructure, but digital transformation and standardization remain critical next steps













The 2025 ACQUIRE Quality Improvement Leadership Forum
Co-Producing Safer Care: Centering Quality and Kindness from the Start
Date: Friday, 11 July 2025 | Time: 3:30PM - 5:00PM EAT
FORMAT
Hybrid (Zoom/streaming + in-room facilitation)
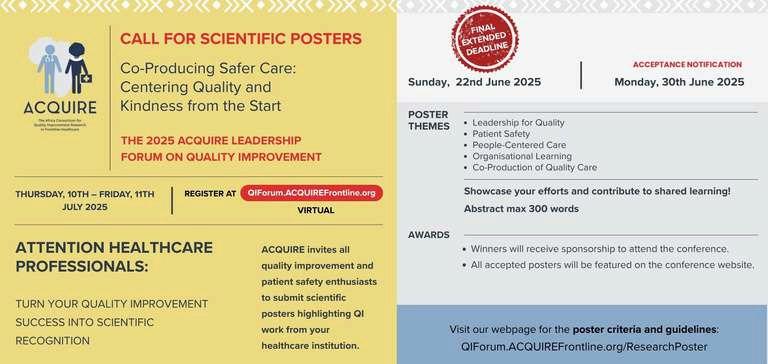
Poster Submission Deadline: Sunday, 15th June 2025
This poster session provides an inclusive and supportive space for healthcare professionals to:
Share their QI experiences, challenges, and lessons learned. Contribute to continental learning and build a repository of context-relevant innovations
Gain visibility, mentorship, and support in transforming implementation efforts into publishable science
Highlight the role of co-production, empathy, and organisational learning in building safer care systems
Recognizing and celebrating local solutions is essential to motivating improvement and sustaining momentum in health system transformation
This session aims to:
1 Showcase Frontline Innovations
Feature posters from healthcare workers and teams across Africa
Emphasize practical, scalable quality improvement projects. Highlight the intersection of kindness, safety, and co-production in practice
2 Encourage Scientific Rigor and Recognition
Provide a stepping stone toward peer-reviewed publication
Inspire attendees to document and disseminate their own work.
3 Foster Regional Collaboration and Learning
Facilitate conversations between institutions through poster themes. Enable attendees to explore diverse strategies in patient safety, leadership, and people-centered care
Create a virtual gallery and discussion space to sustain engagement beyond the event
Notification of Acceptance: Monday, 30th June 2025
Across Africa, healthcare workers are engaging in meaningful efforts to improve quality, safety, and patientcenteredness in care delivery. However, many of these initiatives remain undocumented, limiting shared learning across regions and systems Scientific poster presentations are a valuable mechanism to spotlight this work, encourage knowledge exchange, and foster a culture of inquiry and continuous improvement
The ACQUIRE Forum aims to provide a platform for professionals at all levels especially frontline implementers to transform their quality improvement (QI) and patient safety efforts into scientific recognition By elevating stories of innovation, kindness, and leadership, the forum helps bridge the gap between practice and publication
Visibility will be given to frontline QI projects that might otherwise remain undocumented
Participants will interact with real-world data on kindness, safety, and improvement interventions
Poster presenters will gain confidence and feedback to publish or scale their work


Enhancing Midwifery skills in reducing birth asphyxia at Reverend John Chilembwe Hospital formerly Phalombe District Hospital in Malawi
Veronica Likharuwe Makondetsa PHALOMBE DISTRICT HEALTH OFFICE
Effect of Appropriate Incident Management and Quality of Care: A Case Study of Likoni Subcounty Hospital
Monica N Munyendo
LIKONI SUBCOUNTY HOSPITAL MOMBASA
Scaling Patient Safety and Quality of Care in Rural Health Facility through SafeCare – The Lwala Community Hospital Experience
Sabina Nyaera Morang'a LWALA COMMUNITY ALLIANCE
Implementing Early Warning Score in Monitoring Clinical Deterioration and Escalation of Care
WINNIE WAMBUI KARUGA
MWAI KIBAKI REFERRAL HOSPITALOTHAYA, KENYA
A Continous Quality Improvement Approach to Reducing HIV Exposed Infant (HEI) Seroconversion by 50%,i e From 4% to 2% positivity by December 2023: A case for Kihara Sub County Hospital
Marion Njeri
KIHARA SUB COUNTY HOSPITAL
Postive change on QI leadership in healthcare: a look in kiambu County
Grace LVCT
KIAMBU COUNTY
Enhancing Positive Experience Among PrEP Clients Through the KUMBE Initiative at Likoni Sub-County Hospital
Increasing the number of ANC attendance and deliveries through Maternal and Newborn Health Training
Wambui Makobu AIC KIJABE HOSPITAL
Hospital-Wide Multicomponent Interventions to Improve Hand Hygiene Adherence Among Healthcare Workers in A Rural Hospital in Kenya: A Quality Improvement Program
Tabitha Muchendu KIJABE HOSSPITAL
Reducing patient waiting time at the Cardiology outpatient clinic of General Hospital, Odan, Lagos, Nigeria
ONALEYE SIMEON OMOTAYO
GENERAL HOSPITAL ODAN LAGOS
Enhancing Patient Satisfaction Through Improved Communication on Treatment and Aftercare instructions in Medical wards at Mwai Kibaki Referral Hospital
CYNTHIA NJERI IKUHA
MWAI KIBAKI REFERRAL HOSPITAL
Poor waste disposal by guardians on floor and windows at peadiatric ward, karonga Hospital
Christina Mlenga KARONGA DISTRICT HOSPITAL
Achieving 4 hour benchmark: Improving Emergency Room Efficiency and Patients Outcome
Adebayo Grace Dunsin DUCHESS INTERNATIONAL HOSPITAL
IMPROVING TB CASE IDENTIFICATION AT JUMUIA FRIENDS HOSPITAL FROM 45% IN JANUARY TO 97% BY 30TH SEPTEMBER 2024
VICTOR KIPLAGAT
JUMUIA FRIENDS HOSPITAL KAIMOSI
Bringing Safe Medicines Closer: Quality Improvement through Community-Based Dispensing in Marginalized Areas of Masai Mara, Kenya
Ndinda Damaris Kyalo COSMOS LIMITED
Quality Improvement in delivery of cancer care at Mbingo Baptist Hospital: Cameroon Baptist Convention Health Services
Lorraine Elit MBINGO HOSPITAL
Strengthening Maternal and perinatal death Respose and Surveillance in reducing maternal deaths
Veronica Likharuwe Makondetsa PHALOMBE DISTRICT HOSPITAL
Increasing Reporting of Medical Errors at an Urban Level 4 Hospital in SubSaharan Africa
Caroline Kendi Gichuru HALISI FAMILY HOSPITAL
Strengthening Pre-eclampsia and Eclampsia Care Through Quality Improvement at General Epe
David K Newton FEDERAL MEDICAL CENTRE EPE
Increasing Facility Deliveries at Ndilidau Dispensary in Taita Taveta through Community Engagement and Reliable 24/7 Maternity Service
Asha Abdi
NDILIDAU DISPENSARY TAITA TAVETA COUNTY
Successs story -Transforming Healthcare Quality through Health Service Delivery Awards (HSDA) in Nairobi County
Susan Omondi NAIROBI COUNTY HEALTH OFFICE
STRENGTHENING PRIMARY
HEALTH CARE SYSTEMS USING
KAIZEN APPROACH AT KAHAWA WEST H/C RUARAKA SUB-COUNTY, NAIROBI, KENYA
ESTHER SANKALE RUARAKA SUB-COUNTY
A Multi-Component Complex Intervention to Reduce Blood Culture Contamination Rates in A SingleCenter Rural Tertiary Teaching Hospital in Sub-Saharan Africa
Argwings Chagwira
KIJABE HOSPITAL
A 5-STEP ROOT CAUSE ANALYSIS MODEL FOR TEST OVERUTILIZATION: A STUDY ON ITS APPLICATION TO PLASMA TRANSFERRIN TESTING
Joel Mumo Musyoki LIFECARE HOSPITAL
Enhancing Patient-Centered Care: Findings from the Lamu County Referral Hospital Patient Experience Survey
Stephen Kizito LAMU COUNTY REFERRAL HOSPITAL
NICHOLAS OGOLLA
LIKONI SUBCOUNTY HOSPITAL DECREASED PERCENTAGE OF PREGNANT WOMEN TO START ANC DURING FIRST TRIMESTER
James Masanza MAJETE 1 HEALTH CENTER


The 2025 ACQUIRE Quality Improvement Leadership Forum
Co-Producing Safer Care: Centering Quality and Kindness from the Start

Quality improvement rooted in kindness can transform lives by centering human experience in systems change, particularly within healthcare ”
2025PlanningCommitteeMember AngelaDonelson,PhD
DonelsonConsulting

I’m looking forward to the 2025 QI Forum because the pace set by the ACQUIRE 2024 QI Forum is one that slowing down is not an option, standing still is unacceptable, and speeding up is an understatement
The QI Forum is a space for shared best practices It provides QI enthusiasts, champions and practitioners with the opportunity to not only showcase whats working, but to also explore how past successes are building blocks for future excellence

2025PlanningCommitteeMember BernardOmondi
QualityImprovementManager MetropolitanHospital Nairobi

If the patient was a relative pf a healthcare provider would the care have been the same?
DrElomOtchi
2025PlanningCommitteeMember
TechnicalDirectorfortheAfricaInstituteof HealthcareQuality,SafetyandAccreditation (AfIHQSA) (FISQua,MPH,MA(Org Devt),PGD,BSc) KenyattaNationalHospital
“The ethical use of AI in healthcare hinges on safeguarding patient dignity, using evidence to drive equitable, high-quality outcomes for all ”

MikeMulongo
2025PlanningCommittee,Member
DevelopmentPractitioner Unlockingsystembarriersthroughactionable evidenceforpolicyandpractice

We need evidence of impact in order to make a strong business case for QI, and only a robust learning system can provide this
This means that in addition to sharing our successes, we also need to talk about our setbacks
Please join us at the 2025 ACQUIRE QI Leadership Forum for the seventh session, a QI Work Poster Session with a "Fireside-Chat" reflection moment on these conversations’
Dr OduorOtieno
2025PlanningCommtteeMember
QualityImprovementAdvisor SYSTEMSEvaluationLtd

Seeing quality and safe healthcare services through the eyes of the healthcare user, will get us to coproducing safer care It's time to have patient representatives in the room where quality and safety matters are discussed ”
Dr SabelileTenza(PhD)
2025PannngCommitteeMember
Quality&SafetyResearcher North-WestUniversity SouthAfrica

Kindness in care is not optional It s the most human element of quality and it must be embedded in every protocol, every team, and every patient interaction from day one ”
Dr CarolyneMukuha
2025PlannngCommtteeMember
HealthcareQualityConsultant

Dr FaithLelei Co-production in healthcare means treating patients not as passive recipients, but as active partners in designing and delivering care that reflects their real needs This is our goal
2025PlanningCommitteeMember
Director,SatellitesAICKijabeHospital,Kenya
Moving from QA to QI to coproduction isn’t about changing frameworks it’s about changing mindset It’s about making quality make sense to the people who deliver care every day
When frontline workers feel equipped and patients feel heard, quality stops being a concept and becomes how we work, together
Dr OluwadamilolaMatti
2025PlanningCommitteeMember
ExecutiveManager SocietyforHealthcareQualityinNigeria

Patient safety isn t a checklist it’s a culture
Co-production means inviting patients, families, and staff into a system where kindness and dignity are just as important as outcomes ”
Dr RhodaKalondu
2025PannngCommitteeMember
HeadofthePatientSafetyUnitat KenyattaNationalHospital

Co-producing safer care requires more than protocols it needs the humility to listen to frontline workers and the courage to redesign systems around their realities Safety begins with shared ownership ”
PeterMutanda,BScN,MSc
2025PannngCommtteeMember
HealthcareQualityImprovementSpecialist
"WHAT IFA LEARNING HEALTHCARE SYSTEM IN AFRICA IS NOT JUSTA DREAM, BUT THE FUTURE WITHIN OUR REACH?"

