



COMMON SENSE VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 3 MAY/JUNE 2023 President's Message: AAEM: The Champion of the Emergency Patient 2 6 Editor's Message: A Sincere Hello 10 Heart of a Doctor: Bad Company AAEM/RSA President's Message 2023 Match Editor's Message: AFond Farewell Page5 Celebrating 30 Years of AAEM at the Annual Scientific Assembly! Page 12
Officers
President
Jonathan S. Jones, MD FAAEM
President-Elect
Robert Frolichstein, MD FAAEM
Secretary-Treasurer
L.E. Gomez, MD MBA FAAEM
Immediate Past President
Lisa A. Moreno, MD MS MSCR FAAEM FIFEM
Past Presidents Council Representative
Tom Scaletta, MD MAAEM FAAEM
Board of Directors
Heidi Best, MD FAAEM
Laura J. Bontempo, MD MEd FAAEM
Kimberly M. Brown, MD MPH FAAEM
Phillip A. Dixon, MD MBA MPH FAAEM CHCQMPHYADV
Al O. Giwa, LLB MD MBA MBE FAAEM
Robert P. Lam, MD FAAEM
Bruce Lo, MD MBA RDMS FAAEM
Vicki Norton, MD FAAEM
Kraftin Schreyer, MD MBA FAAEM
YPS Director
Fred E. Kency, Jr., MD FAAEM
AAEM/RSA President
Leah Colucci, MD MS
Editor, JEM
Ex-Officio Board Member
Stephen R. Hayden, MD FAAEM
Editor, Common Sense
Ex-Officio Board Member
Edwin Leap II, MD FAAEM
Executive Director
Missy Zagroba, CAE
Executive Director Emeritus
Kay Whalen, MBA CAE
Common Sense Editors
Mehruba Anwar Parris, MD, Assistant Editor
Alessandra Della Porta, MD, Resident Editor
Stephanie Burmeister, MLIS, Managing Editor
Articles appearing in Common Sense are intended for the individual use of AAEM members. Opinions expressed are those of the authors and do not necessarily represent the official views of AAEM or AAEM/RSA. Articles may not be duplicated or distributed without the explicit permission of AAEM. Permission is granted in some instances in the interest of public education. Requests for reprints should be directed to AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202, Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
AAEM is a non-profit, professional organization. Our mailing list
Mission Statement
The American Academy of Emergency Medicine (AAEM) is the specialty society of emergency medicine. AAEM is a democratic organization committed to the following principles:
1. Every individual, regardless of race, ethnicity, sexual identity or orientation, religion, age, socioeconomic or immigration status, physical or mental disability must have unencumbered access to quality emergency care.
2. The practice of emergency medicine is best conducted by a physician who is board certified or eligible by either the American Board of Emergency Medicine (ABEM) or the American Osteopathic Board of Emergency Medicine (AOBEM).
3. The Academy is committed to the personal and professional well-being of every emergency physician which must include fair and equitable practice environments and due process.
4. The Academy supports residency programs and graduate medical education free of harassment or discrimination, which are essential to the continued enrichment of emergency medicine, and to ensure a high quality of care for the patient.
5. The Academy is committed to providing affordable high quality continuing medical education in emergency medicine for its members.
6. The Academy supports the establishment and recognition of emergency medicine internationally as an independent specialty and is committed to its role in the advancement of emergency medicine worldwide.
Membership Information
Fellow and Full Voting Member (FAAEM): $525* (Must be ABEM or AOBEM certified, or have recertified for 25 years or more in EM or Pediatric EM)
Associate: $150 (Limited to graduates of an ACGME or AOA approved emergency medicine program within their first year out of residency) or $250 (Limited to graduates of an ACGME or AOA approved emergency medicine program more than one year out of residency)
Fellow-in-Training Member: $75 (Must be graduates of an ACGME or AOA approved emergency medicine program and be enrolled in a fellowship)
Emeritus Member: $250 (Please visit www.aaem.org for special eligibility criteria)
International Member: $150 (Non-voting status)
Resident Member: $60 (voting in AAEM/RSA elections only)
Transitional Member: $60 (voting in AAEM/RSA elections only)
International Resident Member: $30 (voting in AAEM/RSA elections only)
Student Member: $40 (voting in AAEM/RSA elections only)
International Student Member: $30 (voting in AAEM/RSA elections only)
Pay dues online at www.aaem.org or send check or money order to: AAEM, 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 Tel: (800) 884-2236, Fax: (414) 276-3349, Email: info@aaem.org
Table of Contents COMMONSENSE AAEM-0723-131
is private. TM Upcoming Events 7 Foundation Contributions.............................................................................................................. 8 PAC Contributions 8 LEAD-EM Contributions 9 Wellness Committee: Wellness Committee Recap of AAEM23 in New Orleans! 24 Emergency Ultrasound Section: Emergency Ultrasound Section Recap of SA23 in New Orleans! 26 Pain and Addiction Committee: The Golden Hour: Buprenorphine Prescribing from the Emergency Department 32 Rural Medicine Interest Group: You Can’t Make This S--- Up 36 Social Service Resources in the Emergency Department: How We Can Impact Social Determinants of Health 38 Discovering the Awe in Medicine: Reigniting the Disillusioned 41 Women in Emergency Medicine Section: WiEM 2023: Looking to the Future 42 Medical Student Council Chair’s Message: Looking Back, Moving Forward 44 Critical Care Medicine Section: The Future of Fluid Resuscitation in Critically Ill Patients is Here. Or is It? 45 An Accidental Communiqué From the Future.............................................................................46 ABEM News: 2023 Recipients of ABEM 30-year Certificate 48 AAEM/RSA Resident Journal Review: Synovial Lactate in the Emergency Department Evaluation of Septic Arthritis 49 AAEM Job Bank 54
COMMON SENSE MAY/JUNE 2023
COMMONSENSE
Featured Articles

2
President’s Message: AAEM: The Champion of the Emergency Patient

In his President’s Message, Dr. Jones discusses the recent announcement of the bankruptcy and collapse of Envision and ponders if AAEM’s motto should be “Champion of the Emergency Patient” since everything AAEM does, believes in, and fights for is centered on the emergency room patient.
5
Editor’s Message: Farewell… and Hello!
In his outgoing message as Common Sense Editor, Dr. Mayer shares a quick look back as his time as editor (but reminds you that he’s really not going anywhere). Then, a bonus Editor’s Message from the new Common Sense Editor, Dr. Leap. Dr. Leap shares the path he took to Common Sense as well as his vision moving forward.
10
Heart of a Doctor: Bad Company
“In moments like this, I felt like I was taking on the role of the grim reaper.” In this issue’s Heart of a Doctor, Dr. Krishnamani recounts her treatment of a young gunshot victim and the heartbreak that follows.
12
Celebrating 30 Years of AAEM at the Annual Scientific Assembly!
The 29th Annual Scientific Assembly was held April 21-25 in New Orleans, LA. We had over 1100 attendees participate in this year’s educational offerings and social events. Thank you for coming!
27
Academic Affairs Committee: Confessions of Dr. Boomer
Dr. Boomer, ahem, I mean, Dr. Mary Claire O’Brien shares her words of Boomer wisdom and guidance to the younger Millennial Generation of doctors and makes a confession…she’s proud of you!
29
Social EM & Population Health Committee: An Unlikely Pairing: Gun Violence and COVID-19

34
What We Do Matters, But What We Say Matters Too
As EM physicians, we know that what we do matters, not just to our patients, but to our communities. Our choice of words matters too. This article discusses the use of stigmatizing terms and how those words can impact our beliefs, biases, and the care we provide.
43
AAEM/RSA President’s Message: 2023 Match
This article highlights and discusses the connections between the COVID pandemic and our country’s gun violence epidemic using example cases from U.S. cities.
“Well, this sucks.” After the competitive 2021 match for EM, Dr. Colucci was congratulated on her excellent match but also asked if she was done being “Chicken Little,” because the sky clearly was not falling. She really does not want to say she told them so, but…
VOICE OF THE AMERICAN ACADEMY OF EMERGENCY MEDICINE VOLUME 30, ISSUE 3 MAY/JUNE 2023
AAEM: The Champion of the Emergency Patient
Jonathan S. Jones, MD FAAEM

he American Academy of Emergency Medicine is the Champion of the Emergency Patient! While our motto actually is Champion of the Emergency Physician, everything we do, everything we believe in, everything we fight for is patient centered.
With the bankruptcy and collapse of Envision, the differing priorities of private equity backed corporate medical groups (CMGs) and our Academy cannot be more apparent.
Have you ever checked out Envision’s or another CMG’s website? They talk about “improving society,” “building teams,” and “providing compassionate care.” That sounds great. But developing a great sounding message is easy. Publishing flashy graphics is easy. Pretending to care is easy.
Do you know what else is easy? Firing physicians who have been forced to relinquish their Due Process rights is easy. Cancelling insurance contracts to ensure sick and injured patients receive large surprise medical bills is easy. Replacing board certified emergency physicians with non-physician practitioners and obfuscating the differences to patients is easy. Apparently running a successful company is not quite as easy. Perhaps they failed because they forgot what nearly every successful company in the world has not forgotten…that the customer matters. And that the employees matter too. Producing an excellent product and serving both employees and customers with respect usually leads to success. Treating
Temployees like replaceable commodities, providing substandard services by means of decreasing quality and volume of support, and by raising rates is usually a model for failure. In fact, I believe Envision made an even more egregious error than sacrificing their customers and employees. They failed in the most basic requirement of business. They didn’t even know who their customer was. In health care, there is one customer whose interests always rise above all others, that customer is the patient. Envision believed their customer was the hospital. In hindsight, it seems obvious that the situation would end this way. But enough about the bad guys. What about us. Are we really the Champion of the Emergency Patient? Yes, absolutely, and unequivocally. Every single action taken by our Academy is taken with the patient in mind. With the recent news of the demise of a large CMG, there is some media and public comments blaming the doctors for the problems private equity has caused to health care. This is a narrative that we must change. And while we change the narrative by providing full transparency to our goals and motives, we also could use some new PR. To that end, the Academy has recently contracted with an experienced marketing firm to help us get the word out about all that we do. When the discussions first started about increasing the resources spent on public relations, we discussed it in regards to attracting new members. And while this is absolutely a continuing goal, we will also strategically use similar messaging to reach out to patients and the media.
But we cannot simply delegate this task to our marketing firm and wonderful AAEM employees. Each of us must also tell our story. We must tell our personal stories about emergency medicine, but also tell the Academy’s stories. In thinking of my personal reason for dedicating time, effort, and resources toward the work for
the Academy, I thought not of a professional experience of mine, not of ways I have been denied due process, and not even of being replaced by a non-physician practitioner. No, when I thought of the reason I fight for the Academy’s beliefs, I think of patients, and specifically of my family.
Not long ago, my mother had to visit the ED with a life-threatening illness. We do not live in the same city and there was not very much that I could physically do to help. I obviously provided the best comfort and information which I could over phone and when I hung up, one thought hit me nearly immediately. That thought was that I sincerely hoped that the physician treating her was a Fellow of the American Academy of Emergency Medicine. While a myriad of factors determines the quality of care a patient receives, many of which are outside the direct control of the individual EM physician, fellowship in the Academy does help ensure a positive experience.
After some more internal deliberation, my thoughts on the topic coalesced into this top 10 list. Depending on the situation and audience, I often refer to this list to determine talking points and conversation starters.
>> AAEM PRESIDENT’S MESSAGE
COMMON SENSE MAY/JUNE 2023 2
[D]eveloping a great sounding message is easy. Publishing flashy graphics is easy. Pretending to care is easy…Apparently running a successful company is not quite as easy.”
Top 10 Reasons I Want My Family Member Treated by a Fellow of the American Academy of Emergency Medicine
1. My mom should be treated by an emergency medicine residency trained and board-certified doctor!
2. That doctor should treat her with respect and compassion.
3. That doctor should not be pressured to see more patients per hour or more high acuity patients than is safe.
4. That doctor should be protected in speaking out against unsafe practices in the ED or hospital.
5. That doctor should be personally healthy, well rested, and prepared to dedicate the time and effort to be fully involved in patient care.
6. That doctor should have a relationship with the hospital and the other medical staff and not simply be a replaceable warm body.
7. That doctor should value lifelong education and continuing certification.
8. That doctor should properly lead a multidisciplinary team in providing patient care which includes not simply signing protocols or assuming non-physicians have made the proper determinations.
9. That doctor should be the one determining and ordering tests and treatments.
10. That doctor should feel a sense of duty. Duty to the patient and profession.
The above statements are straightforward as far as I am concerned. Straightforward, but not necessarily simple or easy. And while simply being a member of the Academy does not ensure that the doctor values each of these statements, it would seem odd to me that a physician who disregarded or did not believe in these would go to the effort of joining AAEM.
Membership in the Academy is more than lending your voice to support our advocacy efforts or mission. Membership in the Academy is making a statement. It is making a personal statement as to the type of physician that you aspire to be. Fellowship in the Academy is a privilege and obligation. Listing FAAEM after your name singles your out. It not only signifies your qualifications but also espouses your beliefs. It invites inquiry and leads to expectations.
It is not to be taken lightly. Listing FAAEM makes a simple statement that I am good and that I will do good.
I am proud to be a Fellow of the American Academy of Emergency Medicine. And as in number 10 above, this imposes upon me a duty. Under the current circumstances, a duty which I feel heavy upon me is the duty to patients in general. You and I each know enough about the current realities of emergency medicine to ask tough questions when we or a family member happens to be a patient. But most patients do not.
I am proud of the work this Academy has done to strengthen the practice of emergency medicine. We should all be proud. But I also feel conflicted and have asked, myself, “Does good work matter if it happens in a vacuum?” In asking this, I do not think about our results or accomplishments, which while of course we strive for more, I think are quite profound. In
And so, if we really want to be the Champions of the Emergency Patient, there is one thing missing from our mission. And that is patient education. We must inform patients about the dangers of private-equity backed CMGs. We must ensure patients know to ask who is treating them. We must help patients ask the right questions to ensure the best care. We must provide resources for patients to take to their hospitals, communities, and legislators
Membership in the Academy is more than lending your voice to support our advocacy efforts or mission. Membership in the Academy is making a statement. It is making a personal statement as to the type of physician that you aspire to be…Listing FAAEM makes a simple statement that I am good and that I will do good.”
asking this, I think about the vacuum encompassing emergency physicians.
Which brings me back to my opening statement that AAEM is the Champion of the Emergency Patient. Are we the champions of the emergency patient? Mostly but not entirely as we have a few questions to ask. Does the work we do to ensure the highest standards of emergency care matter if the patient does not know? I am not thinking about receiving platitudes or even gratitude from patients. What I think about is would our work matter more if all patients knew the difference between an FAAEM physician and one who is not? Would patients receive better care if they knew about my top 10 list? Would they receive better care if they knew to ask the same questions any of us would ask? Undoubtably, I think the answer is yes.
to ensure they get what the need. We must exemplify all the attributes which go into creating a Fellow of the American Academy of Emergency Medicine.
As I finish penning this message, I am also preparing to work later this evening in the ED. While our work is not easy, every second of my shift I will strive to be the Champion of the Emergency Patient. And just as I will need your help and support to make this happen, know too that you have mine. And in those toughest of situations, I will remember that I chose this profession to do good, I will remember that my patient is someone’s mother, father, brother, sister, or child. I will remember that I asked for this great responsibility. And I will know that I am not alone. I will know that the American Academy of Emergency Medicine has my back!
>> AAEM PRESIDENT’S MESSAGE
COMMON SENSE MAY/JUNE 2023 3
How can you help?
Join your colleagues and make a gift or a pledge today.
Gifts at all levels can be paid in one year or pledged over two to five years. We encourage individuals, physician groups, and companies to help support the fight!
$50,000+ Champion Circle
$25,000 - $49,999 President’s Club
$10,000 - $24,999 Advocate
$5,000 - $9,999 Steward
$2,500 - $4,999 Ambassador
$1,000 - $2,499 Supporter
Up to $1,000 Friend
Donate Now
The AAEM Foundation
AAEM was established in 1993 to promote fair and equitable practice environments necessary to allow emergency physicians to deliver the highest quality of patient care. AAEM later established the AAEM Foundation to defend the rights of such care and the emergency physicians who provide it.
Recently, AAEM-Physician Group, a subsidiary of the American Academy of Emergency Medicine (AAEM), filed suit in the Superior Court of California against Envision Healthcare Corporation to avoid a takeover of an emergency department contract that was held by and independent group. Issues at stake include lay influence over the patient-physician relationship, control of the fees charged, prohibited remuneration for referrals, and unfair restraint of the practice of a profession.
Our specialty is in crisis. We cannot let these practices continue here and across the country.
AAEM is the only EM organization that speaks and acts against the harmful influences of the corporate practice of medicine.
Our Goal: $2.5 million by 2025
Gifts in Honor and Gifts in Memory
Gifts at all levels can be given In Honor Of or In Memory Of a program director, mentor, and/or colleague.
Notification of gifts made In Honor or In Memory will be sent to the honoree or their family and listed in our Annual Report.
Ways to Give
• Donate Online
• Scan QR Code
• Employer Matching Gift
• Return the Donation/Pledge Form
• Planned Giving
The AAEM Foundation gratefully accepts IRA distributions, contributions through donor-advised funds, planned gifts and bequests.
ACMS-0718-026
aaem.org/donate/aaem-foundation The AAEM Foundation is a 501(c)(3) non-profit organization. EIN: 20-2080841 American Academy of Emergency Medicine Foundation 555 East Wells Street, Suite 1100, Milwaukee, WI 53202 (414) 276-7390 • (800) 884-2236 • Fax: (414) 276-7390 25% 50% 75%
COMMON SENSE MAY/JUNE 2023 4
A Fond Farewell
 Andrew Mayer, MD FAAEM
Andrew Mayer, MD FAAEM
ell, it is time for me to retire as the editor of Common Sense. I have been the editor for several years and I feel that it is time for someone with a new perspective to take over and keep Common Sense fresh and relevant. My time as the editor has been very fulfilling. I have had the opportunity to interact with many interesting and talented emergency physicians since I joined the AAEM Board of Directors many
Wprocess rights just to name a few of our foundational causes. I believe that if AAEM did not exist the practicing emergency physician would be in a much worse position. AAEM has had to essentially shame other and larger emergency medicine organizations into dealing with the issues which most directly impact all emergency physicians. The value statement that “AAEM is the champion of the emergency physician” should be reflected on.
I want to thank all of the authors who have donated their time and talent to make Common Sense what it is today. I took over from Andy Walker who was the previous editor. He became “Old Andy” and I became “New Andy.” He has been a wonderful and insightful mentor and I appreciate all he has done to help me learn the job. I especially want to thank all of the staff at AAEM, especially Stephanie Burmeister, who really does all of the work. She has been committed to making Common Sense a great publication and her work is greatly appreciated. AAEM has been extremely fortunate in having Kay Whalen, Janet Wilson, and Missy Zagroba helping manage the organization through the years.
years ago. I have had the opportunity to meet and interact with every president of AAEM. I will always cherish the opportunities which AAEM has given me. I have grown and learned much as a person and as an emergency physician.

I hope each of you understands the impactful role which AAEM has had over the past years. AAEM has grown from a small rebel faction to a mature medical specialty society which has a seat at the table. I do believe that AAEM has been the “moral compass” of emergency medicine. AAEM has long led the fight against the corporate practice of medicine and restrictive covenants and for board certification and due
I want to thank AAEM and all of our members. This organization has given me many opportunities to try to fight for our specialty. My time with AAEM has been one of my main personal “Wellness” programs. Sitting and speaking with the leaders and members of our profession has been both enriching and inspiring. The small group discussion late into the night after board meetings and at the Scientific Assembly will always be especially cherished by me.
It is with great excitement that Dr. Ed Leap has been chosen as the next editor. He is a well-known writer in

emergency medicine circles. I believe that he is perfect for the job as editor of Common Sense. His writings have always felt straightforward, honest and meaningful to me. He seems truly excited about the opportunity and I stand ready to help him in any way to keep improving Common Sense and fighting for AAEM’s values.
I am not really going anywhere and I hope to see all of you at emergency medicine meetings in the coming years. Please consider becoming more active in AAEM and in organized medicine in general. Our specialty and our patients need your help.

EDITOR’S MESSAGE
AAEM has grown from a small rebel faction to a mature medical specialty society which has a seat at the table.”
COMMON SENSE MAY/JUNE 2023 5
My time with AAEM has been one of my main personal “Wellness” programs. Sitting and speaking with the leaders and members of our profession has been both enriching and inspiring.”
A Sincere Hello
Edwin Leap II, MD FAAEM
Here I am, writing my first column as the editor of Common Sense. I have been writing columns for various publications since 1995, when I first submitted a piece to the Greenville News, Greenville, South Carolina. Well, I think there was a letter to the editor in my high school paper, but we’ll leave that buried. Along with my early poetry. Nobody needs to see that.
The truth is that I have always loved books and writing. I was reading opinion columnists as a teen. In fact, I started college as a journalism major. My migration to medicine is beyond the scope of this piece, but in the end I circled back through medicine into writing. And now I find myself an editor. As my friend and mentor Howard says, “you just never know where these things will lead…”
Since my path has led me here, I need to explain my “vision” for this publication. I agreed to be editor because of my longstanding interest in the well-being of you, my colleagues in emergency medicine. You incredible physicians are my extended family.
I want this to be a publication where members can read articles that make them say, “oh, I’m not the only one who has experienced that!” And also, a publication that can be shared so that others, family, friends and other colleagues, can get an idea of what we deal with on a regular basis.

Common Sense must be inclusive, not just of nationality, race, ethnicity, gender or sexuality. It has to be inclusive of ideology. Medicine has become a very dangerous little echo chamber where politics and culture manage to poison free speech, free inquiry, and free thought. Over the past few years no small number of physicians have been afraid to voice their opinions for fear of censure, of ridicule, of loss of job or tenure.
Common Sense must be inclusive, not just of nationality, race, ethnicity, gender or sexuality. It has to be inclusive of ideology. Medicine has become a very dangerous little echo chamber where politics and culture manage to poison free speech, free inquiry, and free thought.”
we are feeling good or feeling bad, whether anxious, exhausted, broken, wounded, tearful, or burned out. That’s our common identity. And that’s what must bring us together in this organization.
My goal, as with every prior editor of Common Sense, is to offer a forum where AAEM can continue to highlight its amazing mission to advocate for our specialty. The work we do is important and is driven by people with uncommon creativity, passion and energy.
However, I also want to use Common Sense to offer a voice, to offer encouragement and to acknowledge the deep pain and daily difficulties the members of our tribe face every single day as we work to keep our patients safe and our sanity intact.
We have a big footprint and a huge impact on the health care system, but there aren’t all that many of us. We cannot afford to shut out or shut down our colleagues. We need everyone under the tent and for my purpose here, that tent is AAEM.
Emergency physicians may have many differences, but we are united by one really important thing. That is, when we go to work, when we stand at the bedside (or work at the computer more likely), when we use our education and skills to save lives, then we are one.

We are emergency physicians who stand ready day and night to “stand in the gap” for the patients who come to us. We do this whether
That being said, one of the reasons I was asked to consider this position was to identify and nurture new writers for Common Sense. And in order to do that I want you, the members, to send me your writing. Or if not, ask me if we can find someone to write about a topic that interests you.
Hopefully, those with a story to share, an axe to grind, a bone to pick, or any other old metaphor will see this publication as a potential showplace for what they have to say. I say this without fear and with absolute honesty. Common Sense has to be a publication that represents “all y’all” as we say in the South. If it doesn’t, then it won’t be as effective as it could be. If it does, then it brings us together and will attract new members, new creativity, new ideas, and new connections.
EDITOR’S MESSAGE
I agreed to be editor because of my longstanding interest in the well-being of you, my colleagues in emergency medicine. You incredible physicians are my extended family.”
>> COMMON SENSE MAY/JUNE 2023 6
I am honored, excited, humbled and not a little terrified to be the editor of Common Sense. And without doubt, I’ll make mistakes and missteps. But if you have ever read my previous work, you know that I speak for the physician, in the ED, doing one of the hardest jobs imaginable. I figure if I keep doing that, I’ll be on target.
Finally, to former editor Andy Mayer, AAEM President Jonathon Jones, and President-Elect, Robert Frolichstein. Your encouragement has been invaluable. Thank you all. Oh, and don’t worry, I’ll get you back…
Edwin Leap, MD
P.S. I’ll often send out some suggestions for submissions. Here are some things I’d be interested in seeing soon:
I’d love to see a column from a medical spouse on some aspect of how they see our work and the way it impacts them, or something they think we can do to be healthier and happier. This can be serious or humorous.
Tell me about your hobby and how it helps you to cope.
Send me something about how your 1) philosophy or 2) religious belief helps you with your work. This can be from atheist, theist or anyone in between—share the way you process this crazy world!
Upcoming Events: AAEM Directly, Jointly Provided, & Recommended
AAEM is featuring the following upcoming conferences and activities for your consideration. For a complete listing of upcoming conferences and other meetings, please visit: aaem.org/education/events
AAEM Events
September 13 & 14, 2023
Virtual Oral Board Review Courses aaem.org/education/events/oral-boards
7-10 September 2023
XIIth Mediterranean Emergency Medicine Congress (Rhodes, Greece)
November 29 & 30, 2023
Virtual Oral Board Review Courses aaem.org/education/events/oral-boards
Jointly Provided
Re-Occurring Monthly
Unmute Your Probe: Virtual Ultrasound Webinar Series
Jointly provided by EUS-AAEM aaem.org/eus
Re-Occurring Monthly Spanish Education Series*
Jointly provided by the AAEM International Committee aaem.org/get-involved/committees/committee-groups/international/ spanish-education-series
July 10-12, 2023
Joy & Wholeness Summit (Park City, UT)
Jointly provided by the Coalition for Physician Well-Being https://www.forphysicianwellbeing.org/2023-coalition-annual-conference
July 22-23, 2023
The Miami Beach Point-of-Care Ultrasound Conference (Surfside, FL)
Jointly provided by Miami Beach Ultrasound https://www.miamibeachem.com/mbpocusconferenceregistration/ miami-beach-pocus-conference-2023-registration
July 24-28, 2023
Essential Emergency Medicine: Can’t Misses in EM - Cardiac Misfortunes, Environmental Misadventures, and Unfortunate Misdiagnoses (Key West, FL) – Jointly provided by EssentialCMEhttps://www.essentialcme.com/conferences
September 19-23, 2023
UC Davis Emergency Medicine Hot Topics (Maui, HI)
Jointly provided by UC Davis https://ces-apps.ucdavis.edu/confreg/?confid=1257
October 16-20, 2023
Essential Emergency Medicine: Can’t Misses in EM - Cardiac Misfortunes, Environmental Misadventures, and Unfortunate Misdiagnoses (Lake George, NY) – Jointly provided by EssentialCME https://www.essentialcme.com/conferences
Recommended
Advances in Cancer ImmunotherapyTM https://www.sitcancer.org/education/aci
• June 27, 2023 - A Focus on Toxicity Management Part 2 (Virtual)
• August 17, 2023 - A Focus on Cellular Therapies and T cell Engagers (Washington, DC and Virtual)
• October 19, 2023 - A Focus on Hematologic Malignancies (Virtual)
The Difficult Airway Course: EmergencyTM https://www.theairwaysite.com/a-course/ the-difficult-airway-course-emergency/
• September 22-24, 2023 - San Diego, CA
• October 20-22, 2023 - Washington, D.C.
• November 17-19, 2023 - New Orleans, LA
Online CME
Recognizing Life-Threatening Emergencies in People with VEDS https://www.thesullivangroup.com/TSG_UG/VEDSAAEM/
EDITOR’S MESSAGE
COMMON SENSE MAY/JUNE 2023 7
AAEM Foundation Contributors – Thank You!
AAEM established its Foundation for the purposes of (1) studying and providing education relating to the access and availability of emergency medical care and (2) defending the rights of patients to receive such care and emergency physicians to provide such care. The latter purpose may include providing financial support for litigation to further these objectives. The Foundation will limit financial support to cases involving physician practice rights and cases involving a broad public interest. Contributions to the Foundation are tax deductible.
Levels of recognition to those who donate to the AAEM Foundation have been established. The information below includes a list of the different levels of contributions. The Foundation would like to thank the individuals below who contributed from 1/1/2023 to 5/1/2023. Please note any donations made during the 2023 Scientific Assembly will be reflected in our next issue..
Contributions $1000 and above
Algis J. Baliunas, MD FAAEM
David W. Lawhorn, MD MAAEM
Jonathan S. Jones, MD FAAEM
Kathryn Getzewich, MD FAAEM
Thomas R. Tobin, MD MBA FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Pedro I. Perez, MD FAAEM
Robert A. Frolichstein, MD FAAEM
Ronald T. Genova, MD
Contributions $250-$499
Alexander Tsukerman, MD FAAEM
Andrew Thomas Larkin, DO FAAEM
Ann Loudermilk, MD FAAEM
Arnold Feltoon, MD FAAEM
Barry N. Heller, MD FAAEM
Bradley Houts, MD FAAEM
Brian J. Browne, MD FAAEM
Brian J. Cutcliffe, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Bryan Knoedler, MD
Catherine V. Perry, MD FAAEM
Contributions $100-$249
D. Scott Moore, MS DO FAAEM
David R. Steinbruner, MD FAAEM
David Thomas Williams, MD FAAEM
David Wang, MD FAAEM
Donald L. Slack, MD FAAEM
Eric D. Lucas, MD FAAEM
Floyd W. Hartsell, MD FAAEM
Gary M. Gaddis, MD PhD MAAEM FAAEM FIFEM
H. Samuel Ko, MD MBA FAAEM
Jason M. Driggs, MD FAAEM
Jeffrey A. Rey, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Jenna Otter, MD FAAEM
Jessica Moore, MD
Kathleen Hayward, MD FAAEM
Katrina Green, MD FAAEM
Katrina Kissman, MD FAAEM
Kenneth Scott Hickey, MD FAAEM FACEP
Laura Richey, MD FAAEM
Marc D. Squillante, DO FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Ming-Jay Jeffrey Wu, MD FAAEM
Nancy Conroy, MD FAAEM
Nayla M. Delgado Torres, FAAEM
Neeharika Bhatnagar, MD FAAEM
Patrick B. Hinfey, MD FAAEM
Paul W. Gabriel, MD FAAEM
Philip Beattie, MD FAAEM
Piotr Jurgielewicz, MD
Renee Marie Nilan, MD FAAEM
Riley MW Williams, MD MBA
Robert Boyd Tober, MD FAAEM
Rohan Janwadkar, MD
Roland S. Waguespack III, MD MBA
FAAEM
Sameer D. Mistry, MD CPE FAAEM
Shane Coughlin, MD
Tim J. Carr, FAAEM
Timothy J. Durkin, DO FAAEM CAQSM
William E. Franklin, DO MBA FAAEM
Yeshvant Talati, MD
Contributions up to $99
Alexander J. Yeats, Jr., MD FAAEM
Alexander S. Maybury, MD FAAEM
Amie Rose
Benson Yeh, MD FAAEM
Caitlin E. Sandman, DO FAAEM
David C. Crutchfield, MD FAAEM
Edward T. Grove, MD FAAEM MSPH
Eric M. Rudnick, MD FAAEM
AAEM PAC Contributors – Thank You!
Ernest H. Leber Jr., MD FAAEM
Erol Kohli, MD MPH FAAEM
Everett T. Fuller, MD FAAEM
James P. Alva, MD FAAEM
Jason J. Morris, DO FAAEM
Joanne Williams, MD MAAEM FAAEM
Jonathan Y. Lee, MD FAAEM
Jose G. Zavaleta, MD
Joseph M. Reardon, MD MPH FAAEM
Kelly Dougherty, MD
Kenneth T. Larsen, Jr., MD FAAEM
Kevin C. Reed, MD FAAEM
Linda Sanders, MD FAAEM
Marianne Haughey, MD FAAEM
Michael Lajeunesse, MD
Om Pathak, DO
Peter H. Hibberd, MD FACEP FAAEM
Peter M.C. DeBlieux, MD FAAEM
Sachin J. Shah, MD FAAEM
Samuel M. Morris, MD
AAEM PAC is the political action committee of the American Academy of Emergency Medicine. Through AAEM PAC, the Academy is able to support legislation and effect change on behalf of its members and with consideration to their unique concerns. Our dedicated efforts will help to improve the overall quality of health care in our country and to improve the lot of all emergency physicians.
All contributions are voluntary and the suggested amount of contribution is only a suggestion. The amount given by the contributor, or the refusal to give, will not benefit or disadvantage the person being solicited.
Levels of recognition to those who donate to the AAEM PAC have been established. The information below includes a list of the different levels of contributions. The PAC would like to thank the individuals below who contributed from 1/1/2023 to 5/1/2023. Please note any donations made during the 2023 Scientific Assembly will be reflected in our next issue.
Contributions $500-$999
Mark S. Penner, DO FAAEM
Ronald T. Genova, MD
Contributions $250-$499
Bradley Houts, MD FAAEM
Fred Earl Kency, Jr., MD FAAEM
Joseph T. Bleier, MD FAAEM
Mark A. Foppe, DO FAAEM FACOEP
Michael L. Martino, MD FAAEM
Paul W. Gabriel, MD FAAEM
Thomas B. Ramirez, MD FAAEM
Tim J. Carr, FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Alexander Tsukerman, MD FAAEM
Brian J. Cutcliffe, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Bruce E. Lohman, MD FAAEM
Catherine V. Perry, MD FAAEM
David W. Lawhorn, MD MAAEM
Donald L. Slack, MD FAAEM
Garrett Sterling, MD FAAEM
Gary M. Gaddis, MD PhD MAAEM
FAAEM FIFEM
Jeffrey A. Rey, MD FAAEM
Jeffrey J. Thompson, MD FAAEM
Joseph M. Reardon, MD MPH FAAEM
Katrina Green, MD FAAEM
Philip Beattie, MD FAAEM
R. Lee Chilton III, MD FAAEM
Riley MW Williams, MD, MBA
Robert Boyd Tober, MD FAAEM
Robert M. Esposito, DO FAAEM
William E. Franklin, DO MBA FAAEM
Contributions up to $99
Alex Kaplan, MD FAAEM
Amie Rose
Brice Guy, DO
David L. Sincavage, Jr., MD FAAEM
David R. Steinbruner, MD FAAEM
Eric M. Rudnick, MD FAAEM
Erol Kohli, MD MPH FAAEM
Jason J. Morris, DO FAAEM
Kevin C. Reed, MD FAAEM
Linda Sanders, MD FAAEM
Marc D. Squillante, DO FAAEM
Om Pathak, DO
Peter H. Hibberd, MD FACEP FAAEM
Ruth P. Crider, MD FAAEM
COMMON SENSE MAY/JUNE 2023 8
LEAD-EM Contributors – Thank You!
The AAEM Institute for Leadership, Education & Advancement in the Development of Emergency Medicine, Inc. (LEAD-EM) was established after the tragic and unexpected death of AAEM president, Dr. Kevin G. Rodgers.
The Kevin G. Rodgers Fund and the Institute will LEAD-EM just like Dr. Rodgers did. The funds will support important projects such as development of leadership qualities, and clinical and operational knowledge of emergency physicians with a view toward improving and advancing the quality of medical care in emergency medicine, and public health, safety and well-being overall. LEAD-EM would like to thank the individuals below who contributed from 1/1/2023 to 5/1/2023. Please note any donations made during the 2023 Scientific Assembly will be reflected in our next issue
Contributions $1000 and above
Jonathan S. Jones, MD FAAEM
Contributions $500-$999
Fred Earl Kency, Jr., MD FAAEM
Contributions $250-$499
Dale S. Birenbaum, MD FAAEM
David W. Lawhorn, MD MAAEM
Mark A. Foppe, DO FAAEM FACOEP
Mary Ann H. Trephan, MD FAAEM
Contributions $100-$249
Alexander S. Maybury, MD FAAEM
Ann Loudermilk, MD FAAEM
Brian R. Potts, MD MBA FAAEM
Catherine V. Perry, MD FAAEM
Christopher Kang, MD FAAEM
David R. Steinbruner, MD FAAEM

Edward T. Grove, MD FAAEM MSPH
Gary M. Gaddis, MD PhD MAAEM FAAEM FIFEM
Joseph M. Reardon, MD MPH FAAEM
Kathleen Hayward, MD FAAEM
Kevin C. Reed, MD FAAEM
Paul W. Gabriel, MD FAAEM
Roland S. Waguespack III, MD MBA FAAEM
Contributions up to $99
Alicia J. Starr, DO
Erol Kohli, MD MPH FAAEM
Jose G. Zavaleta, MD
Marc D. Squillante, DO FAAEM
Om Pathak, DO
Richard G. Foutch, DO FAAEM
Samuel M. Morris, MD
COMMON SENSE MAY/JUNE 2023 9
Bad Company
Pavitra P. Krishnamani, MD MS
18-year-old male, coming in with a gunshot wound to the head, unresponsive with CPR started,” I was alerted one morning. I was perhaps two hours into my shift, but I had to take a moment to re-confirm.
“18 years old?” I asked, surprised by how young the gentleman was, “Is a parent coming in with him?”
“No, EMS said that family had been notified, but we’ll keep looking for a way to re-contact them,” the voice on the other end of the line said.

I had chills. We were mid-pandemic and on complete lockdown. Our policies didn’t allow for anyone other than medical staff to be with patients, even those who were unresponsive and in a critical care room. Family was allowed to provide collateral information but only in predesignated locations within the hospital.
As I prepared the room with my colleagues for the controlled chaos to come, I wondered what it would be like to stand at the head of the bed for the first time while taking care of a patient with a gunshot wound to the head.
“He’s here,” the lead nurse yelled out as a yellow and black stretcher wheeled an unconscious man into the room. The patient had regained pulses and was actively getting breaths with a bag-valve-mask device. As we moved the patient over to our ED stretcher, I noticed a trail of scant gelatinous whitish-pink material fall out of his skull. It wasn’t my first time seeing brain matter, but the sight was one that never sat well with me. I deftly checked the patient’s carotid arteries as my colleague wheeled over the nearby video laryngoscope, sincerely hoping that the boy had not lost pulses again. Hopes fulfilled, I signaled for EMS to start their sign-out.
“18-year-old found in the backseat of a friend’s car with a single GSW to the head. He’s in high school and was in a car with his schoolmates, who were playing with a gun when it accidentally went off. We lost pulses at the scene and they were regained around five minutes ago after about 15 minutes of CPR. Fluids running for persistent hypotension. Patient remains unresponsive.” EMS finished.
“Geez, these were his friends?” I asked, visualizing the young high schooler now on my stretcher getting a ride with his buddies and talking about his summer plans less than an hour ago before a gun went off, robbing him of hopes and dreams.
“Yeah, I know…bad company doc, baaad company…” the paramedic replied.
“Any prior medical conditions or allergies?” I asked.
“Not that we know of, but we contacted mom, who said she’s en route.”
The team started coalescing the patient. I checked on his breath sounds quickly before getting set up for an intubation while the blood pressure cycled. It was cycling for the second time, which generally portended an extremely low blood pressure. I called for a manual blood pressure to be measured and checked for a pulse again. As my fingers searched his carotid arteries once more, my breath caught.
“We’ve lost pulses again, let’s start CPR,” I called the team into action. CPR was started and when we checked for an organized rhythm, we saw none. The patient’s heart rhythm read asystole—after a difficult day, his heart had simply given up. We intubated him and gave him some epinephrine as we continued CPR for another round. “Let’s take a look with an ultrasound on pulse check!” I called.
His heart was at standstill. Asystole. No pulses. With severe intracranial injury and brain matter spilling out of his skull, the patient was unlikely to do well even if by a miracle he survived this code. But he was just 18—barely an adult. In front of us lay a boy who was supposed to have his whole life ahead of him. Our team members looked at one another before starting another round. An emergent blood transfusion along with intravenous fluids ran to support the patient’s blood pressure.
This high schooler was mere months away from graduating. I wasn’t sure what he had planned for the next phase of his life, but with every beat of CPR, those plans became increasingly unrealistic. Everyone in the room knew this. The trauma surgery and emergency medicine teams alike knew that this patient would not make it, but we hoped that with just one more round he might. Yet after a full resuscitation, we collectively made a decision to stop. It was time to let the youth before us go.
>> HEART OF A DOCTOR
COMMON SENSE MAY/JUNE 2023 10
“‘Geez, these were his friends?’ I asked, visualizing the young high schooler now on my stretcher getting a ride with his buddies and talking about his summer plans less than an hour ago before a gun went off, robbing him of hopes and dreams.”
His face was oddly still as he lay there, limp with his palms facing the sky as if to ask a higher power to take him. The toll of his premature passing rung in my mind and an eerie silence hung over the recently bustling room as our staff quietly dissipated.

“Hey, it looks like his mom just arrived, she’s so confused…says the kid never even liked guns,” one of our triage nurses walked over and told me as I was getting ready to leave the room. Time of death had been called and the trauma team had left. I took a deep breath and stared back at our nurses and techs getting ready to unzip the white bag in which this child’s thin lanky body would lay for some time before burial.
“Do you think his mom will be able to visit him here before we transfer his body?” I asked, my heart breaking for her.
“No, we can’t allow anyone back here right now, it’s policy,” the charge nurse said, empathizing with me.
I paused, “how about in the morgue?” I said more quietly. The charge nurse and I exchanged a despondent glance, knowing that this too would
be a challenge to accommodate during a time in which health care facilities, coroner’s offices, and funeral homes alike were in lockdown.

The patient’s body lay there, lifeless, and yet more disconsolate than the glassy aesthetic that had come over his eyes or the brain matter strewn across his stretcher was the fact that his mother may never be able to say goodbye to his flesh. Such was the cruelty of a pandemic that devastated in both life and death.
‘The kid never even liked guns,’ his poor mother had said to the triage nurse. Under my mask, my lips formed a pained expression and I brushed a single tear off of my cheek before taking a deep breath.
In moments like this, I felt like I was taking on the role of the grim reaper. I suppose it is possible to think of the steps I took towards the boy’s mom that day as steps towards relieving her bated breath. Somehow it felt different though, with every step reverberating an impenetrable whisper of woe as I walked towards a mother waiting to receive news that would devastate even the bravest of hearts.
HEART OF A DOCTOR
Tell Us Your Opinion! The editors of Common Sense want to hear from you! What articles did you like or which ones, not so much? Submissions are open for future issues. Please visit aaem.org/resources/publications/common-sense or contact cseditor@aaem.org for more information. This is where your voice can be heard! What stood out to you from this issue of Common Sense? Have a question, idea, or opinion? Edwin Leap II, MD FAAEM, editor of Common Sense, welcomes your comments and suggestions. Submit a letter to the editor and continue the conversation. Submit a Letter to the Editor Submit a Letter to the Editor at: www.aaem.org/resources/publications/common-sense/letters-to-the-editor COMMON SENSE MAY/JUNE 2023 11
I wasn’t sure what [the high schooler] had planned for the next phase of his life, but with every beat of CPR, those plans became increasingly unrealistic…Yet after a full resuscitation, we collectively made a decision to stop. It was time to let the youth before us go.”
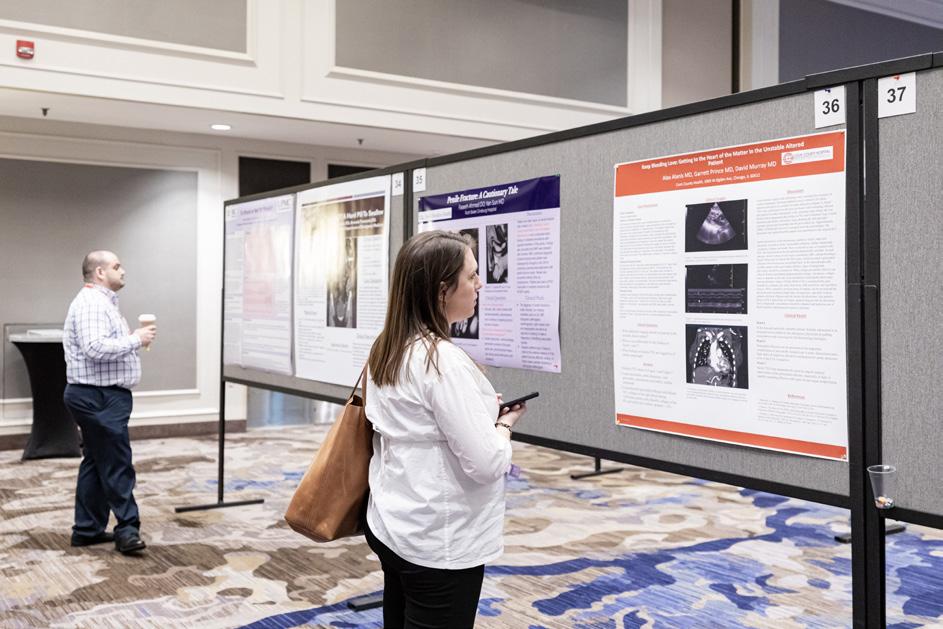
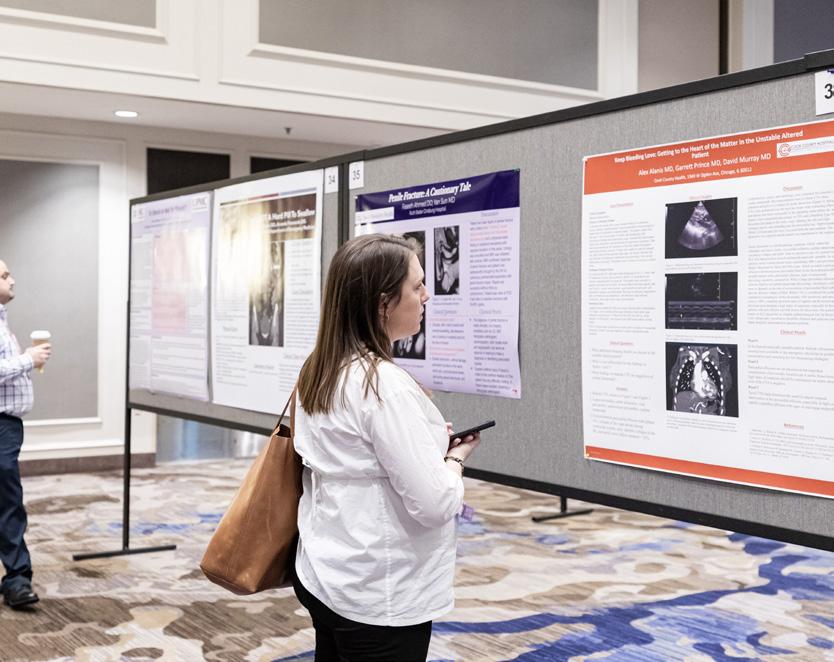
29th Annual SCIENTFIC ASSEMBLY
ANNUAL AAEM SCIENTIFIC ASSEMBLY: THANK YOU FOR JOINING US!

The 29th Annual AAEM Scientific Assembly was held in New Orleans, LA from April 21-25, 2023. With a focus on cutting edge clinical medicine as well as practical application to patient care, this event was one of the most anticipated academic conferences of the year. This year’s Scientific Assembly took an innovative and practical look at various topics within emergency medicine that are shaping our field of practice. We were excited to provide the opportunity to expand the conversation on the topics of cardiology, pharmacology, critical care, neurology, reproductive health, and many more. By combining discussion from leading scholars with innovative medical nuances, we were able to provide a resource to enhance the understanding of our beloved specialty.
Powerhouse plenaries included Drs. Amal Mattu (Cardiology), Brian Acunto and Kimberly Chernoby (Reproductive Health), Ilene Claudius and Mimi Lu (Pediatrics), Corey M. Slovis (EMS), and Michael Winters and Peter DeBlieux (Resuscitation / Critical Care.) The Addiction Medicine Panel, led by Dr. Jack Perkins, gave an inside view of the journey from active addiction to recovery. “Meeting of the Minds” also returned for a third year: Dr.
Justice, Equity, Diversity, and Inclusion movement in EM with panelists Drs. Cortlyn Brown, Italo Brown, and Mohamed Hagahmed, while Dr. Andrew Phillips questioned Drs. Bruce Lo and Danya Khoujah about the conflicting guidelines around dizziness in ‘To HINTS or Not to HINTS: A Tale of 2 Guidelines.’
This year’s keynote speaker, Dr. Rob Gore, grew up in Brooklyn and came full circle to practice emergency medicine at Kings County Hospital – SUNY Downstate. His dynamic keynote address, ‘Community Violence and the Emergency Physician’ drew on his personal experience to examine the physical and psychosocial trauma that go well beyond the injuries we see every day.
The ever-popular Breve Dulce sessions returned this year and continued to be some of the most attended sessions of AAEM23. The interactive Small Group Clinic sessions gave attendees hands-on practice in a variety of settings. The AAEM/RSA Resident Track - selected by residents, for residents - prepared students for their careers in emergency medicine with presentations on clinical topics, career success, and the role of residency unions in emergency medicine.
We had an energetic group of medical student ambassadors, who were omnipresent and ever helpful in keeping the conference going. Special educational sessions were targeted toward their benefit. Thank you, student ambassadors! There were also a wide variety of networking opportunities available at Scientific Assembly. Whether in the hallways, at receptions, or near the coffee stations during breaks, the level of interaction between attendees was high. The JEDI off-site reception, Women in EM networking lunch and Eid Dinner, and the RSA Party were all highly anticipated and attended. The newly revamped EngageEM! social was a novel and fun event for attendees to engage with the committees, sections, chapter divisions, and interest groups within AAEM. The Wellness Committee provided offerings such as Airway at AAEM storytelling, Paint ‘N Sip, a Fun Run, and the Wellness Room.
We sincerely hope that you enjoyed the Assembly this year. Our goal is to continue in the tradition of bringing in a combination of your perennial favorites and some new speakers to keep you educated, inspired, and coming back every year for more.
29 TH
Scientific Assembly Planning Work Group Co-Lead Christopher Colbert, DO FAAEM; Co-Lead Molly K. Estes, MD FAAEM FACEP; Co-Vice Lead Jason Hine, MD FAAEM; and Co-Vice Lead Julie Vieth, MD FAAEM
Preview of the Preview of the COMMON SENSE MAY/JUNE 2023 12
Preview of the Preview of the
29th Annual SCIENTFIC ASSEMBLY
Scientific Assembly Planning Work Group
Co-Leads:
Christopher Colbert, DO FAAEM
Molly K. Estes, MD FAAEM FACEP
Co-Vice Leads:
Jason Hine, MD FAAEM
Julie Vieth, MD FAAEM FACEP
Members:
Harman S. Gill, MD FAAEM
Michael Gottlieb, MD FAAEM
Siamak Moayedi, MD FAAEM
Jack C. Perkins Jr., MD FAAEM
Andrew W. Phillips, MD MEd FAAEM
Eric M. Steinberg, DO MEHP FAAEM
AAEM/RSA Representative:
David Fine, MD
Advisors:
Laura J. Bontempo, MD MEd FAAEM

Joelle Borhart, MD FAAEM FACEP
Christopher I. Doty, MD MAAEM FAAEM
Kevin C. Reed, MD FAAEM
Joanne Williams, MD MAAEM FAAEM
George C. Willis, MD FAAEM
Breve Dulce Work Group:
Jason Adler, MD FAAEM
Kimberly M. Brown, MD MPH FAAEM
Sarah B. Dubbs, MD FAAEM
Ryan C. Gibbons, MD FAAEM
Thomas P. Noeller, MD FAAEM
Sherri L. Rudinsky, MD FAAEM
Kathleen M. Stephanos, MD FAAEM
AD HOC Members
AAEM Board President:
Jonathan S. Jones, MD FAAEM
AAEM President-Elect:
Robert A. Frolichstein, MD FAAEM
AAEM Secretary-Treasurer:
L.E. Gomez, MD MBA FAAEM
AAEM Immediate Past President:
Lisa A. Moreno, MD MS MSCR FAAEM FIFEM
AAEM Past Presidents Council Representative:
William T. Durkin, Jr., MD MBA MAAEM FAAEM
Education Committee Chair:
David J. Carlberg, MD FAAEM
Education Committee Vice Chair:
Michael E. Silverman, MD MBA FAAEM FACEP
Education Committee Board Liaison:
Phillip A. Dixon, MD MPH FAAEM
Total Registered for AAEM23: 1163
Exhibitors: 43
Sponsors: 14
Number of speakers: 211
Number of posters: 274
Number of oral abstract presentations: 44
Number of awards awarded: 28
Number of Airways at AAEM attendees: 100

Number of WiEM lunch attendees: 77
Number of JEDI social attendees: 90
Number of Wellness Paint ‘N Sip participants: 20
Number of Fun Run participants: 15
Number of WiEM Eid Dinner attendees: 28
Oral Board Examiner Dinner attendees: 28

CCMS After Dark attendees: 25

engagEM attendees: 225

RSA Party attendees: 205
Anything But a Lecture attendees: 20
Section Leader Boot Camp participants: 35
Leadership Academy participants: 31
New Attendee Reception attendees: 60
Aging Well in EM Interest Group Breakfast attendees: 21
COMMON SENSE MAY/JUNE 2023 13
Annual SCIENTFIC ASSEMBLY
Preview of the
2023 AAEM Award Winners









Administrator of the Year
Seth Teigen, FACHE
Advocate of the Year
Julie Vieth, MBChB FAAEM
Amin Kazzi International Emergency Medicine Leadership Award
John Robert Acerra, MD FAAEM

David K. Wagner Award
Eveline Hitti, MD MBA FAAEM

James Keaney Award
Laura Bontempo, MD MEd FAAEM
Joanne Williams Award
Loice A. Swisher, MD MAAEM FAAEM
Joe Lex Educator of the Year Award
Mark I. Langdorf, MD MHPE FAAEM
Master of the American Academy of Emergency Medicine (MAAEM)
Leslie Zun, MD MBA FAAEM
Master of the American Academy of Emergency Medicine (MAAEM)
Mark I. Langdorf, MD MHPE FAAEM




Resident of the Year Award
Leah Colucci, MD MS

Robert McNamara Award
Marianne Haughey, MD FAAEM

Young Educator Award

Cara Kanter, MD FAAEM

Strategic Ally Award
Kay Whalen, MBA CAE




Preview of the
29th
COMMON SENSE MAY/JUNE 2023 14
Preview of the Preview of the
29th Annual SCIENTFIC ASSEMBLY
AAEM23 Competition Winners
Open Mic Competition Winner
Rebecca Raven, MD
Gregory Wu, MD FAAEM
YPS-AAEM Research Competition
1st Place: Jack Allan, MD
2nd Place: Benjamin Karfunkle, MD
3rd Place: Hazel Sanchez Baconga, MD
AAEM/JEM Resident and Student Research Competition

1st Place: Bailey Pierce, MD MBA

2nd Place: Dino Gutierrez
3rd Place: Thomas Porturas, MD PhD
AAEM/RSA & WestJEM Population Health Research Competition
1st Place: Anha Telluri
2nd Place: Erica Dunn, DO
3rd Place: Sean Eden
AAEM23 Photo Competition Results

1st Place: Quoc Vinh Tran, DO
2nd Place: Deanna Margius, MD
3rd Place: Michael D. Zwank, MD FAAEM
CCMS-AAEM Breveloquent Competition

1st Place: Rebecca Raven, MD
2nd Place: Kimberly Pistell, DO
3rd Place: Amina Ramadan, MD
SOCIAL MEDIA AT AAEM23
AAEM Twitter Impression: 76.8K
Twitter Mentions : 183
Instagram Impressions: 23.4K
Facebook Impressions: 14.4K
AAEM/RSA Twitter Impressions: 25.2K
Twitter Mentions: 183
Instagram Impressions: 16.0K
Facebook Impressions: 541
AAEM Social Media Impressions: 114,600
AAEM Twitter Mentions: 347
AAEM/RSA Social Media Impressions: 41,700

AAEM/RSA Twitter Mentions: 183
Social Media Impressions (Overall): 156,300
Twitter Mentions (Overall): 530 COMMON SENSE MAY/JUNE 2023 15
29th Annual
SCIENTFIC ASSEMBLY
Preview of the
AAEM/RSA at AAEM23
Almost 400 residents and medical students participated at AAEM23



Nearly 150 attendees went to Wellness Airway Storytelling Event
Five residents presented in the AAEM/RSA Breve Dulce Competition



Six lectures and a panel on residency unionization were presented during the AAEM/RSA Resident Track drawing resident, medical student, and attendings


Sixty medical students took in the lectures by engaging faculty speakers and panelists during the Medical Student Track
Sixty medical students took in the lectures and participated in hands-on suturing and Stop the Bleed workshops during the Medical Student Track
Twenty medical students competed in the first AAEM/RSA & EUSAAEM Sim Sono Sleuthing Case Challenge
2022-23
Award Winners
Student Committee Member of the Year
Zoë Cole
Midwest Regional Faculty Mentor Award
Kene A. Chukwuanu, MD FAAEM

Northeast Regional Faculty Mentor Award

Michael Galuska, MD FAAEM



Southern Regional Faculty Mentor Award
Loice Swisher, MD MAAEM FAAEM
Western Regional Faculty Mentor Award
Victor M. Cisneros, MD MPH CPH


Resident Committee Member of the Year
Alessandra Della Porta, MD

Faculty Mentor of the Year
Gus Garmel, MD FAAEM FACEP
Kevin G. Rodgers Program Director of the Year
Harsh Sule, MD MPP FAAEM
National Medical Student of the Year Scholarship Award
Robert G. Canning Jr.
International Regional Medical Student of the Year Scholarship Award

Tai Donovan

Northeast Regional Medical Student of the Year Scholarship Award
Chibuzo Opara
Midwest Regional Medical Student of the Year Scholarship Award

James Nardini
Southern Regional Medical Student of the Year Scholarship Award
Heather Pol
Western Regional Medical Student of the Year Scholarship Award
Mary Unanyan
International EMIG of the Year
Ross University School of Medicine
Regional EMIG of the Year
Howard University College of Medicine
Program Coordinator of the Year
Wanda Bailey Gregory
Preview of the
COMMON SENSE MAY/JUNE 2023 16
AAEM/RSA
President
Jonathan S. Jones, MD

FAAEM
New Board of Directors
AAEM is proud to welcome the newly elected board of directors!
President-Elect
Robert Frolichstein, MD FAAEM


Secretary-Treasurer
L.E. Gomez, MD MBA
FAAEM
Immediate Past President
Lisa A. Moreno, MD MS

MSCR FAAEM FIFEM
Past Presidents Council
Representative
Tom Scaletta, MD MAAEM
FAAEM
At-Large Director
Laura J. Bontempo, MD




MEd FAAEM
At-Large Director
Kimberly M. Brown, MD MPH FAAEM

At-Large Director
Heidi Best, MD FAAEM
At-Large Director
Phillip A. Dixon, MD MBA MPH FAAEM



At-Large Director
Al O. Giwa, LLB MD MBA
MBE FAAEM
At-Large Director
Robert P. Lam, MD FAAEM


At-Large Director
Bruce Lo, MD MBA RDMS FAAEM
At-Large Director
Vicki Norton, MD FAAEM
At-Large Director
Kraftin Schreyer, MD MBA FAAEM

YPS Director
Fred E. Kency, Jr., MD FAAEM
AAEM/RSA President
Editor, JEM
Leah Colucci, MD MS Editor, Common Sense

Ex-Officio Board Member
Stephen R. Hayden, MD

FAAEM
Edwin Leap II, MD FAAEM
Results that need to be added are:
AAEM23 Photo Competition Results
1st Place: Quoc Vinh Tran, DO
2nd Place: Deanna Margius, MD
OF
AAEM BOARD
DIRECTORS
COMMON SENSE MAY/JUNE 2023 17
Academic Affairs Committee
Chapter Division Committee
Clinical Practice Committee
Chair: Mary Claire O’Brien, MD FAAEM
Vice Chair: Sangeeta Sakaria, MD MPH MST FAAEM
Education Committee
Chair: Deborah D. Fletcher, MD FAAEM
ACCME Work Group
Vice Chair: Jeff A. Baker, MD FAAEM







Chair: Robert L. Sherwin, MD FAAEM
Vice Chair: TBD
Chair: David J. Carlberg, MD FAAEM
Vice Chair: Michael E. Silverman, MD MBA FAAEM FACEP

Virtual Oral Board Review Work Group
Lead: Sara A. Misthal, MD FAAEM

Vice Lead: Elisabeth Calhoun, MD FAAEM
Scientific Assembly Planning Work Group
Lead: Frank L. Christopher, MD FAAEM
LMS Work Group
Advisor: Michael C. Bond, MD FAAEM FACEP
Speaker Development Work Group
Advisor: Mitchell Goldman, DO FAAEM FAAP
Co-Lead: Christopher Colbert, DO FAAEM

Emergency Medicine Workforce Committee
Co-Lead: Molly K. Estes, MD FAAEM FACEP


Ethics Committee
Vice Lead: Jason Hine, MD FAAEM




Lead: Jason Hine, MD FAAEM
Lead: Kevin C. Reed, MD FAAEM
Chair: Joshua T. Bucher, MD FAAEM
Government and National Affairs Committee
Vice Chair: Deborah D. Fletcher, MD FAAEM


Chair: Al O. Giwa, LLB MD MBA MBE FAAEM
Vice Chair: Melissa Myers, MD FAAEM


Co-Chair: William T. Durkin Jr., MD MBA MAAEM FAAEM
Co-Chair: Greogry N. Jasani, MD FAAEM
Vice Chair: Anthony R. Rosania III, MD FAAEM


AAEM SECTION
LEADERSHIP Committee Leadership
COMMON SENSE MAY/JUNE 2023 18
International Committee
Co-Chair: Manish Garg, MD FAAEM
Co-Chair: Gregory M. Polites, MD FAAEM


Co-Vice Chair: Christine T. Knettel, MD FAAEM
Legal Committee
Chair: Melanie S. Heniff, MD JD FAAEM FAAP
Vice Chair: Malia J. Moore, MD FAAEM


Pain and Addiction Committee
Co-Vice Chair: Terrence M. Mulligan, DO MPH FAAEM FACOEP FIFEM FACEP FNVSHA FFSEM HPF


Membership Committee
Operations Management Committee
Chair: Shana EN Ross, DO MS FAAEM FACEP
Vice Chair: Frank L. Christopher, MD FAAEM

Palliative Care Committee
Chair: Anthony R. Rosania III, MD FAAEM

Vice Chair: Algis J. Baliunas, MD FAAEM

Section Leadership Committee
Chair: Zachary Repanshek, MD FAAEM


Vice Chair: Alexis LaPietra, DO FACEP FAAEM
Social EM and Population Health Committee
Chair: Jessica FleischerBlack, MD FAAEM
Vice Chair: Margaret Putman, DO FAAEM
Social Media Committee
Chair: Carolyn Kanter, MD FAAEM
Vice Chair: Allison Zanaboni, MD FAAEM




Chair: Faith C. Quenzer, DO MPH FAAEM
Wellness Committee
Vice Chair: Jordan Vaughn, MD
Chair: Matthew D. Zuckerman, MD FAAEM
Vice Chair: Danya Khoujah, MBBS MEHP FAAEM
Co-Chair: Al’ai Alvarez, MD FAAEM
Co-Chair: Neeharika Bhatnagar, MD FAAEM


Vice Chair: Jennifer Kanapicki Comer, MD FAAEM



COMMITTEE LEADERSHIP
COMMON SENSE MAY/JUNE 2023 19
Section Leadership
CCMS-AAEM Council 2023-2024
Section Chair: Elias E. Wan, MD FAAEM



Councilors:
Section Chair-Elect: David Hirsch Gordon, MD


Secretary/Finance Chair: Allyson M. Hynes, MD FAAEM
Section Immediate Past Chair: A. June Gordon, MD FAAEM
EMSS-AAEM Council 2023-2024
Section Chair: Bryan Everitt, MD



Councilors:
Chair-Elect: * Open Position
Secretary/Finance Chair: Christopher Hewitt, DO MPH FAAEM
Section Immediate Past Chair: C.J. Winckler, MD FAAEM


EUS-AAEM Council 2023-2024
Section Chair: Neha Bhatnagar, MD FAAEM


Councilors:
Chair-Elect: Alexis Salerno, MD FAAEM



Secretary/Finance Chair: Shawn Sethi, DO FAAEM
Section Immediate Past Chair: Allison Zanaboni, MD FAAEM






AAEM SECTION LEADERSHIP
Frederick Gmora, DO Neil Dasgupta, MD Jason Xu, MD Alex Yang, MD RSA Rep: Ava Omidvar, MPH FP-C
Katherine Raczek, MD FAAEM FACEP
Rachel Ely, DO FAAEM Ryan Newberry, DO MPH FAAEM
Craig Cooley, MD MPH EMT-P FAAEM
RSA Reps: Kayla Gordon, OMS III and James Nardini
Kendra Mendez, MD FAAEM
Patrick Kishi, MD FAAEM
Andrew Shannon, MD MPH FAAEM
Rebecca Theophanous, MD MHSc FAAEM
RSA Rep: Ochan Kwon, MD
COMMON SENSE MAY/JUNE 2023 20
Shadman Kabir
JEDI-AAEM Council 2023-2024
Section Chair: Cortlyn Brown, MD FAAEM


Councilors:
Section Chair-Elect: Kristyn Smith, DO
Secretary/Finance Chair: Alyssa Eily, MD
Section Immediate Past Chair: Italo Brown, MD



WiEM-AAEM Council 2023-2024
Section Chair: Danielle E. Goodrich, MD FAAEM



Councilors:
Section Chair-Elect: Molly Estes, MD FAAEM





Secretary/Finance Chair: Cara Kanter, MD FAAEM





Section Immediate Past Chair: Vonzella Bryant, MD FAAEM





YPS-AAEM Council 2023-2024
Secretary/Finance Chair: Nicholas Boyko, DO Fujimoto, MD FAAEM Councilors:
Section Chair: Moiz Qureshi, MD MBA
 Jordan Vaughn, MD Kristin Fontes, MD FAAEM
Kendall Moore, MD FAAEM
Valerie Pierre, MD FAAEM
Jordan Vaughn, MD Kristin Fontes, MD FAAEM
Kendall Moore, MD FAAEM
Valerie Pierre, MD FAAEM
AAEM SECTION LEADERSHIP
RSA Reps: Salma Yusuf and Asma Hashim, DO
Jennifer Rosenbaum, MD Michelle E. Romeo, MD Jack Allan, MD
Jennifer McGowan, MD FAAEM
RSA Rep (1): To Be Announced!
Sulynn Walker MD FAAEM
Jennifer McGowan, MD FAAEM
Mary McLean, MD
Elspeth Pearce, MD FAAEM
COMMON SENSE MAY/JUNE 2023 21
RSA Reps: Salma Yusuf and Jordan Eichelser
Interest Group Leadership
Aging Well in Emergency Medicine Interest Group
Geriatric Interest Group
Rural Medicine Interest Group
Simulation Interest Group
Co-Chair:
Marianne Haughey, MD FAAEM

Co-Chair: Gary Gaddis, MD PhD MAAEM FAAEM FIFEM
Chair: To Be Announced!
Chapter Division Leadership
California Chapter Division (CAL/AAEM)
President
Jesse Borke, MD CPE FAAEM
Vice President
Jennifer Kanapicki Comer, MD FAAEM
Secretary
Danielle E. Goodrich, MD FAAEM

Treasurer
Shahram Lotfipour, MD MPH FAAEM
At-Large Directors
Haig Aintablian, MD
Tom Dalton, MD
William T. Durkin, Jr., MD MBA MAAEM FAAEM
Jessica Munoz, MD
Faith Quenzer, DO
Associate Representative
Carl Preiksaitis, MD
Resident Representative
Cassie DeWitt, MD
Karen Chung, MD
Medical Student Representative
Yusuke Wakita
Capital Region Chapter Division (CR/AAEM)
President
Terrence M. Mulligan, DO MPH FAAEM FACOEP
FIFEM FACEP FNVSHA FFSEM HPF
Secretary/Treasurer
L.E. Gomez, MD MBA FAAEM
At-Large Directors
William Brady, MD FAAEM
Joel Clingenpeel, MD MPH MS MEdL FAAEM
William T. Durkin, MD MBA FAAEM
Bruce Lo, MD MBA RDMS FAAEM
Chair: Robyn Hitchcock, MD FAAEM
Co-Chair: Afrah Ali, MBBS FAAEM
Co-Chair: Rose V. Goncalves, MD FAAEM


Delaware Valley Chapter Division (DVAAEM)
President – Delaware
J. Daniel Hess, MD FAAEM
Director – Delaware
Eli Zeserson, MD FAAEM
President – New Jersey
Emerson R. Franke, MD
Director – New Jersey
John Genova, MD
President – Pennsylvania
Katrina Kissman, MD FAAEM
Director – Pennsylvania
Rebecca Mills, MD FAAEM
Florida Chapter Division (FLAAEM)
President
Steven Parr, DO FAAEM
Immediate Past President
Ramon Pabalan, MD FAAEM
Vice President
Michael Dalley, DO FAAEM
Secretary-Treasurer
Mark A. Newberry, DO FAAEM
Directors
Patrick Hughes, DO MEHP
Rian Pillitteri, MD FAAEM
Loice Swisher, MD MAAEM FAAEM
Alexandra Terskiy, MD FAAEM
Chair – FLAAEM Scientific Assembly Planning Committee
Michael Dalley, DO FAAEM
Resident Member Representative – South Florida
Daniella Lamour, DO
Resident Member Representative – North Florida
Morgan Sweere
Medical Student Member Representative
Rachel Shi
Great Lakes Chapter Division (GLAAEM)
President
Brady McIntosh, MD FAAEM
Immediate Past President
Sudhir Baliga, MD FAAEM
Vice President
William Boston, MD FAAEM
Secretary/Treasurer
Bob Zemple, MD MBA FAAEM
WI State Representative
Jon Rubin, MD FAAEM
OH State Representative
Eric Brader, MD FAAEM
MI State Representative
Larisa Traill, MD FAAEM
IA State Representative
Olivia Bailey, MD FAAEM
IN State Representative
Courtney Soley, MD FAAEM
Resident Representatives
Allyson Peterson, MD
Michael McGary, MD
AAEM SECTION LEADERSHIP
COMMON SENSE MAY/JUNE 2023 22
India Chapter Division (AAEMi)
President
John R. Acerra, MD FAAEM
Immediate Past President
S. V. Mahadevan, MD
Vice President
Terrence M. Mulligan, DO MPH FAAEM FACOEP
FIFEM FACEP FNVSHA FFSEM HPF
Secretary/Treasurer
Katherine Douglass, MD, MPH
At-Large Directors
George Abraham, MD
Kumar Alagappan, MD FAAEM FIFEM
Lingappa Amernath, MD
Joseph D. Ciano, DO
Ashes Mukherjee, MD
Pinaki Mukherji
Neeraj Patil, MD MBBS FRCS MRCS
Sohil Pothiawala, FAMS EM MRCSEd A&E
Louisiana Chapter Division (AAEMLa)
President
Deborah Fletcher, MD FAAEM
Vice President
Vanessa Piazza, MD FAAEM
Secretary-Treasurer
Christine Butts, MD FAAEM
Immediate Past President
Meredith Hall, MD FAAEM
At-Large Directors
LuAnn Barnett, MD FAAEM
Nicole McCoin, MD FAAEM
Britni Sternard, MD FAAEM
Resident Director – Baton Rouge
Mitchell Hymowitz, MD
Resident Director – New Orleans
Maria Arulraja, MD
Student Representative – Tulane
Mallory Kiefer
Student Representative – LSU
Marcelle Fournet
Missouri Chapter Division (MOAAEM)
President
Jennifer A. Cooper-Lewis, DO FAAEM
Immediate Past President
Michael J. Klevens, MD MBA FAAEM FACHE
Secretary/Treasurer
Gary M. Gaddis, MD PhD FAAEM FIFEM
At-Large Directors
Christopher Michael Allen, MD
Haley Rapp, MD FAAEM
New York Chapter Division (NYAAEM)
President
Lillian Oshva, MD FAAEM
Vice President
Nicholas A. Schwartz, MD FAAEM
Secretary/Treasurer
Dennis Price, MD FAAEM
Immediate Past President
Erol Kohli, MD MPH FAAEM
At-Large Board Members
Kathryn Getzewich, MD FAAEM
Leyam Kewson, MD FAAEM
Yuliya Pecheny, DO
Julie Vieth, MD FAAEM
Student Representative
Alex C. Sneddon
Texas Chapter Division (TAEM)
President
Jeffrey Pinnow, MD FAAEM
Immediate Past President
Liza Chopra, MD FAAEM
Vice President
Luke Berry, MD
Secretary
Rachel Metz, MD FAAEM
At-Large Directors
Brandon Browne, MD FAAEM
Alexandre Migala, DO FAAEM
Kenneth Nugent, MD FAAEM
Laura Pittman, MD FAAEM
Resident Director
Ali Mohammed, DO
Tennessee Chapter Division (TNAAEM)
President
James Parnell, MD FAAEM
Vice President
William E. Lummus, MD FAAEM
Secretary/Treasurer
Arthur Smolensky, MD FAAEM
Immediate Past President
Mary Jane Brown, MD FAAEM
At-Large Directors
Jacqueline Dovgalyuk, MD FAAEM
Edmund Hadley, MD FAAEM
Zachariah Ramsey, MD FAAEM
Pamela A. Ross, MD FAAEM
Andy Walker, MD FAAEM
Resident Representative
Corey McNeilly, MD
Student Representative
Anantha Singarajah
Uniformed Services Chapter Division (USAAEM)
President
Jacob Arnold, MD FAAEM
Vice President
Alexander F. Barbuto, MD FAAEM
Secretary-Treasurer
James Gragg, DO
Immediate Past President
Zachary J. Sletten, MD FAAEM
Air Force Representative
Josh Bukowski, MD FAAEM
Navy Representative
Sean Stuart, DO FACEP FAAEM FAWM
Resident Representative
Jessica Eker, MD
Medical Student Member Representative
Matthew Brown
CHAPTER DIVISION LEADERSHIP
COMMON SENSE MAY/JUNE 2023 23
Wellness Committee Recap of AAEM23 in New Orleans!
Neha Bhatnagar, MD, Al’ai Alvarez, MD, and Jennifer Kanapicki-Comer, MD

AAEM23 Wellness Events Highlights


5K Fun Run/Walk
We were thrilled to kick off our leadership roles with the Wellness Committee at AAEM23 in New Orleans! We thank Dr. Allie Min for her leadership as chair for the past two years, and we look forward to continuing this momentum!


As a quick recap of the last year, we shared the success of the #StopTheStigmaEM month-long campaign in collaboration with SAEM and other national and international organizations in EM. AAEM co-hosted the “Shadows and Light: A Physician’s Lens on COVID.” We also shared our continued efforts on National Physician Suicide Awareness (NPSA) Day in collaboration with CORD, championed by Dr. Loice Swisher. Another success is the efforts of AAEM-RSA on their Residency Wellness Instagram survey and the lovely gift boxes they put together for those who participated!
Ways to get involved with the Wellness Committee this year:
• Attend our monthly meeting: Second Tuesdays at 2:00pm CT. Please email Roxanne Dobbs (rdobbs@aaem.org) to be added to our calendar.
• Get Published: Submit an Article to Common Sense about important wellness topics that mean a lot to you!1
• Engage online via our MyAAEM discussions, social media posts, and emails for further details.
• Visit our webpage for more information by scanning the QR code or visiting aaem.org/get-involved/committees/committee-groups/wellness
What a beautiful sunrise run along the Mississippi River! Plus, three members beat AAEM President Dr. Jonathan Jones! We can’t wait to see the total donations the winners will make, knowing Dr. Jones will match them up to $1000.

New Attendee Reception
It was heartwarming to start Sunday morning with a big crowd of new attendees. The event was packed and highlighted the power of engagement efforts of the Wellness Committee. Bonus: celebrating the 5K Fun/Run in the Big Easy with New Orleans coffee and beignets!

Airways Storytelling
Thanks to Dr. Chris Colbert and Dr. Janae Hohbein for emceeing this year’s event. Another packed event of gathering, laughter, some tears shed, and even a Wayne Brady cameo! Brava, storytellers!
Paint’N Sip
The second year of this event was another smash! Held in our Wellness Room with a breathtaking 41st-floor view of Canal Street and the Mighty Mississippi! Attendees had a blast painting and conversing in this peaceful, creative space.

Yoga
Held on the 41st floor, we started the day with a scavenger hunt to find the session and tested our flexibility and endurance.
Dinner
Thanks to Dr. David Hoyer for leading a group to break bread and share experiences on wellness, and the impact of due process.
WELLNESS COMMITTEE
>> COMMON SENSE MAY/JUNE 2023 24
Here are some areas we plan to focus on for 2023:
• Develop a Mental Health Action Plan. How might we maximize our mental health?
• Find your Outlet. Learn ways to manage stress.
• Job crafting. How alignment with values can help us find professional fulfillment.
We look forward to working with you this year! Join the Wellness Committee for the fun events…Join us for the advocacy…Most of all, join us for the community. You don’t have to go through this alone!
References
*Co-chair, @nbhatnagar_md
†Co-chair, @alvarezzzy

‡Vice-chair, @kanapicki
1. For Common Sense deadlines and information visit: aaem.org/resources/ publications/common-sense/submissions
WELLNESS COMMITTEE
COMMON SENSE MAY/JUNE 2023 25
Emergency Ultrasound Section Recap of SA23 in New Orleans!


 Neha Bhatnagar, MD FAAEM FPD in US and Shawn Sethi, DO FAAEM
Neha Bhatnagar, MD FAAEM FPD in US and Shawn Sethi, DO FAAEM

collaboration with AAEM’s other five Sections, detailing Pregnancy Ultrasound in the case of a Septic Post-Abortion patient.
EUS leadership and members had a blast in the Big Easy this April, and we have lots to report back on all our projects!


First, we would like to thank our 2022-2023 Council and welcome new Council members! (aaem.org/get-involved/sections/eus/about/ leadership)

Our Section Meeting Meet & Greet had quite a turnout, and the engagEM social networking event was a hoot! Can’t wait to get these eager new members involved! There were over 30 Poster Submissions related to ultrasound, and your judges are hard at work deliberating who will win the top three prizes! Winners will be announced in the coming weeks. And there were nearly a dozen Breve Dulce talks related to ultrasound and/or presented by our EUS members!
Key EUS Member Benefits Unmute Your Probe
This Virtual lecture series is free to members, counts for CME, and includes the past two full years of lectures on both basic and advanced ultrasound topics, as well as this year’s more administrative and FPD-focused content. Check out the next lecture on June 21 at with Dr. Yash Chavda speaking on “Credentialing and Billing: How to credential your department and start a billing program”1
Speaker’s Bureau for Medical Student EM Interest Groups
We had a variety of fun events at SA, including our successful Sono Sleuthing medical student competition (held in collaboration with the RSA and Sim groups), our free open Hands-On Session, and multiple Small Group Clinics. The Section also commends the Ultrasound Pre-Conference team on yet another wonderful year for their courses! Our incoming Chair Dr. Neha Bhatnagar had a blast participating in the “Six Docs Walk into a Shift Show” lecture in
Submit a request and one of our qualified lecturers will give your group a talk on a topic of your choosing! We’ve already given five successful lectures with strongly positive feedback! Request a speaker at tinyurl.com/2w3xt3yd
Regional Courses
Are you practicing in the community where multiple docs at your site want more ultrasound training, but you’d rather not travel and pay thousands of dollars for courses at conferences or private teaching companies? Request a regional course, and the EUS leadership will bring the education course to you! Find out more at aaem.org/get-involved/sections/eus/ events/regional-us-course
Countinued on page 28 >>
EMERGENCY ULTRASOUND SECTION
COMMON SENSE MAY/JUNE 2023 26
Confessions of Dr. Boomer
Mary Claire O’Brien, MD FAAEM

Dear Dr. Boomer, In academic medicine, how do you tell your senior colleagues that medicine is changing, and they need to change with it? They just reminisce about the “old days.” How can I encourage my older colleagues to be flexible, without ticking them off? “Best,”
Frustrated Dr. Millennial
We simply do not understand one another. Because—for us Boomer Doctors, medicine is not like anything we have ever seen before.
The electronic medical record? We remember carbon paper, mimeograph machines, and microfilm. Typewriters. White out. Books! We remember going to the medical library and hoping there was a copy of Sir Robert Muir’s Pathology—all 1120 pages of it. As students we carried fat blue plastic notebooks in the pockets of our short white cotton coats. They were full of lists: the causes of heart failure, the names of all the bacteria with all their Gram stains, the procedure for how to do a Gram stain, algorithms for cardiac arrest, a diagram of how to put down a stomach lavage tube, the causes of hyponatremia.
Dr. Millennial, you should be so proud of me! When I hear “hyponatremia” these days, I just take out my phone and type it into Google! I get 12,840,000 results in 0.56 seconds. Who needs to memorize? Did you know that there are more than 60,000 drugs in the current United States Pharmacopeia? If I come across a new medication, I just “google” it. What, you don’t trust google for medical information? I thought that was your mantra, “If it’s on the internet, it must be accurate.”

Just teasing, Dr. Millennial.
Remember what my Boomer colleague Patrick says, “You find out who the real neurologists are when the electricity goes out.” Yes, Dr. Millennial, I am a Luddite. But I do not need an app to tell me what a heart murmur sounds like or how to use my clinical gestalt. You young folks will find out who the real doctors are, when the technology is not working!
Old Dr. Boomer has a few confessions to make.
Dear Dr. Millennial, You can’t! We are the most expe- rienced physicians in this practice paradigm! We have socks older than you whippersnappers. You can’t tell us anything. If there were a better way of doing things, we would have told you!
*Signed,*
Dr. Boomer
P.S. Did you just call me old?
I like you. You are so clever with technology! That fancy ultrasound machine of yours has revolutionized emergency medicine. Every time I figure out how to turn the dang machine on, you are making a podcast about a new indication. A podcast—or was it a blog or a Reddit? Who cares! No more DPLs! No more culdocenteses! No blind central lines! Gee, you’re even scanning eyeballs these days. Wonders never cease with you, Dr. Millennial. You are innovative.
You mention flexibility. The reason we Boomers prefer to do things the tried and true way is that we earned our wrinkles making bad mistakes. We hope you will avoid those same blunders by listening to our fascinating anecdotes. Yes, that means you have to stand still for 10 seconds. OK, 10 minutes. We have a lifetime of knowledge to share with you—not because we are smarter, but because we have been burnt, Dr. Millennial. We are also trying to build a relationship with you, one that does not involve social
ACADEMIC AFFAIRS COMMITTEE
The reason we Boomers prefer to do things the tried and true way is that we earned our wrinkles making bad mistakes.
>> COMMON SENSE MAY/JUNE 2023 27
media. Imagine! Ask our advice, Dr. Millennial. Mentoring is our superpower. If you listen to us, we will be much more likely to listen to you.
We were raised to respect hierarchy. We do not mind being criticized as long as it is our “boss” that is doing it. You are not our boss. You are the Trophy Kids! You do not like to be criticized. You expect praise simply for doing the job that you are paid to do. This baffles us Boomers.
We were raised to be competitive and individualistic. You think that life is a team sport and that the playing field is flat. Keep your guard up, Dr. Millennial. Big Brother knows all about your world view. He’s dangling those “bright spots” and “mindful moments” as if Corporate Medicine were all one big Kumbaya. Don’t believe him. It ain’t!
We were raised to be workaholics. You value—no, you insist upon—work life balance. You kids are right about that one, Dr. Millennial. Kill yourself at work and you are—dead. We wish we had figured that out before our knees got so creaky.
Many of us Boomers fought hard to be included in medicine, especially in leadership roles. Your generation trumpets diversity—keep pushing! Many wonderful professionals are still struggling to be included. Go make this messy world a better place, Dr. Millennial. Empower your patients. Be compassionate with your fellow clinicians.
In truth, I am a wee bit envious of you. And if some of my crotchety colleagues don’t appreciate your energy and creativity, Dr. Millennial, never you mind. I think you are just wonderful.
I’m proud of you.
Ways to get involved with EUS
• Join a Section Workgroup: Education, Communication, Social Media, and more!
• Get Published: Submit a thought-provoking article or interesting case to the POCUS Report and/or to Common Sense!2,3
• Become a Speaker for our Speaker’s Bureau. Sign up at tinyurl. com/bd5f8uyu
• Find out more about all of these offerings and more at our Emergency Ultrasound Section site, aaem.org/get-involved/sections/eus, or scan the QR code.
Watch out for our MyAAEM discussions, social media posts, and emails about upcoming virtual section meetings. The next one is planned for mid-late May, and it is not just for council—we welcome all our members to join and contribute their ideas!
We’re looking forward to an exciting year leading up to SA24 in Austin, TX!
References
*@nbhatnagar_md
†@shawn_sethi
1. aaem.org/get-involved/sections/eus/events/unmute-your-probe
2. For POCUS Report deadlines and information visit aaem.org/get-involved/ sections/eus/newsletter
3. For Common Sense deadlines and information visit aaem.org/resources/ publications/common-sense/submissions
ACADEMIC AFFAIRS COMMITTEE
EMERGENCY ULTRASOUND SECTION
COMMON SENSE MAY/JUNE 2023 28
Countinued from page 26>>
An Unlikely Pairing: Gun Violence and COVID-19
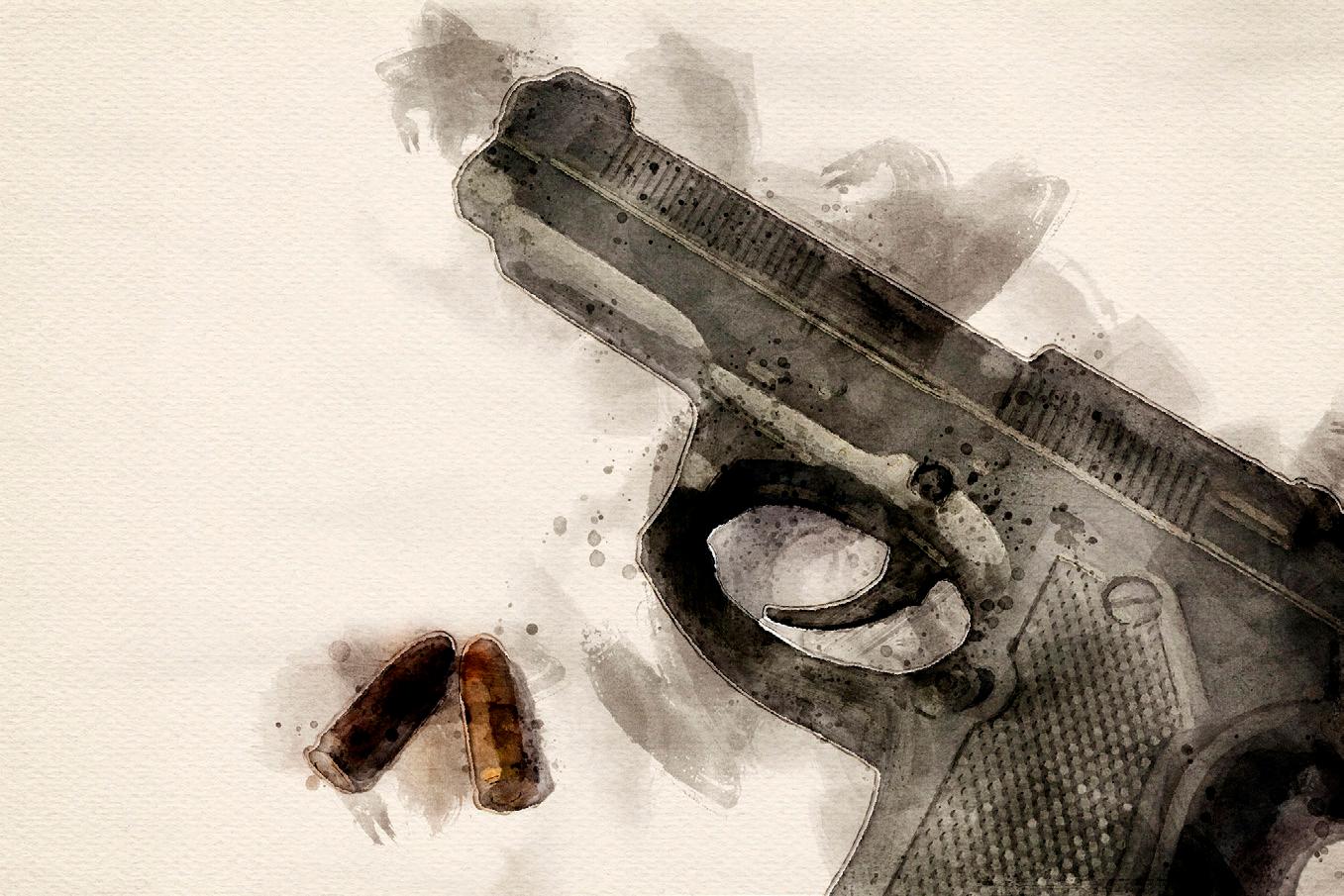 Brenda Arthur, MD* and Jada Watts, BS †
Brenda Arthur, MD* and Jada Watts, BS †

In May of 2021, my eighteen-year-old, younger brother was fatally shot and killed. It happened two days before he was supposed to play in his basketball state championship. He was an all-star basketball player. He was involved in his community. He had a 4.0.
My mom did everything right. He was in the wrong place at the wrong time.†
Gun violence takes the lives of numerous bright, young, talented people. It is closer to home than we realize.
The coronavirus pandemic has also taken many lives, all while wreaking havoc on our hospital systems and bringing to light inequities and injustices present in American society.
It has been three years since the World Health Organization announced the coronavirus pandemic. Firearm violence, the epidemic, has troubled this country long before COVID. It has risen in the shadows alongside the spread of COVID and its subsequent mandates and seems to be getting more lethal. Both homicides and unintentional shootings in the United States increased to record levels in 2020, the same year of the declaration of the COVID pandemic. 1 In this paper, we offer important, unseen connections between these parallel occurrences, using major cities in the United States as example cases.
Containment Policies
Philadelphia’s first COVID containment policies were implemented on March 16, 2020.2 This meant that all non-essential businesses were closed. On March 23, 2020, Philadelphia County began its first stay-at-home orders.2 The city was essentially shut down.
Weekly shootings in Philadelphia almost doubled in the weeks following these containment policies.3 Prior to March 16, the average number of individuals shot per week was 25. Afterward, that number almost doubled to 46.3 The rise in firearm violence coinciding with COVID containment policies is difficult to ignore.
Across the country, the Gun Violence
Archive notes that almost 20,000 homicides and accidental, fatal shootings occurred in 2020. This is a 25% inc rease compared to 2019, only one year prior.4 While the sharp increase in deadly shootings was not maintained, there has been a total increase in nonfatal firearm injuries since 2020.5 This increasing rate of firearm violence began right around the time when a large portion of the country was shut down.

Unemployment
The described COVID containment policies caused sudden changes in employment. Many businesses were forced to close, which resulted in 11.7% of Americans being laid off.6 The newly socially distanced country allowed for the success of industries contributing to virtual platforms while other industries dedicated to serving the public job market deteriorated. Different theories exist regarding the complex relationship between gun violence and change in employment rates.
On one hand, changes in financial security relating to unemployment often leads to increased financial stress. Stress is difficult to measure or study, but we suspect that this increased stress and financial burden in families may have led to increases in things like robbery or other acts of violence to maintain basic needs. In the first year of the COVID pandemic, New York City had a 22.4% increase in robbery rates when compared to the previous year. Chicago had a 10% increase in comparison to 2019.7 In general, time spent outside of the workplace or recreational pastimes leaves more time in the day for other affairs. With increased financial stress, some of the other may include violent activity. 8
John Donohue, a Stanford University law professor who studies gun violence, notes that periods of stress are associated with more shootings.4 It is easy to see how unemployment during the COVID pandemic may be linked to increasing rates of violence.
>>
SOCIAL EM & POPULATION HEALTH COMMITTEE
COMMON SENSE MAY/JUNE 2023 29
Firearm violence, the epidemic, has troubled this country long before COVID. It has risen in the shadows alongside the spread of COVID and its subsequent mandates and seems to be getting more lethal.”
Scarcity
Unemployment or changes in financial security described above can put humans in a state of scarcity. This may include trouble accessing food, essential living supplies, housing, or paying bills. The start of COVID not only brought changes in American employment, but also put many under duress of accessing those basic needs— remember when you could not find toilet paper in the stores? For some neighborhoods COVID only exacerbated preexisting resource scarcity.
Scarcity rewires our brains to decrease activity in the dorsolateral prefrontal cortex, the part of our brain that helps with goal-directed, logical decision making.9 When the focus shifts from goal-directed, critical decision making to survival or acquiring basic sustenance, consequences of violence may not be at the forefront of the mind.
The emotional tension of not having enough to support a family can lead to significant turmoil within a household and distress to the individual.8 This responsibility during COVID likely not only affected the parental figures of the family, but also may have pressured potentially younger members of the household to provide as well—shifting multiple generations in our country to think in survival mode, possibly affecting rates of violence.
Isolation
Mental health often comes up in conversations about violence and the coronavirus pandemic. Poor mental health has a complicated relationship with violence. While it is associated with an increased risk of violence, it is essential to note that this alone is usually not the cause of violent activity.10
Isolation during the pandemic was strange, in part related to the physical and social distancing that was government mandated; but also, the feeling of detachment from society, even if an individual was part of a household full of other humans. COVID containment policies and new online work platforms perpetuated feelings of isolation. Isolation has an extensive, largely negative effect on mental health and may have even been experienced as traumatic to some.11
Substance use, anger, and traumatic life events are all linked with violence, all things that the coronavirus pandemic may have amplified for some individuals.10
Further, isolation from society and a decline in mental wellness can reduce appropriate emotions and social cognition.12 The Journal of Psychiatry defines reduced empathic concern and reduced displays of right feeling as ‘callous-unemotional traits.’ These traits are associated with firearm violence.13
Isolation, and a disconnect from society, can be the start of someone having callous-unemotional traits, especially in our adolescent population whose minds are still developing.13 The forced disconnection from society during the COVID pandemic may have played a complex role in the increase in firearm violence at the time.
Increasing Gun Sales
More than 22 million guns were purchased in the United States in 2020. This is a 64% increase in purchases over 2019.4,8 While research does not explicitly state a link between gun sales and increased gun violence, we know that access to guns is a key risk factor for gun violence.10 With this significant increase in gun sales during the pandemic, our hypothesis is that more individuals had access to firearms. The United States was in a unique period of uncertainty at the start of the pandemic, with many people having new fears. About 110,000 California adults acquired a firearm in response to fears.4 Almost half of those adults were new firearm owners.
Having peers who carry guns is a significant risk factor for gun carrying and other violence.13 This likely perpetuates further the increase in gun sales and access to guns, as well as possible gun violence.
Structural Discrimination
The pandemic aggravated and exposed racial disparities in the United States. Black and Latinx communities were disproportionately affected by COVID. These are the same communities with the heaviest burden of gun violence in cities.1
Generations of systemic racial discrimination and inequities in health care, housing, education, jobs, green space, and other factors increase the risk of gun violence. These systemic inequities have also been shown to make individuals more vulnerable to COVID-19.2 Large scale disinvestment in communities of color strips these communities of resources and opportunity, causing structural vulnerabilities that translate to shouldering an unequal burden of any crisis, including both COVID-19 and gun violence.
One explanation for the rise in firearm violence during the start of the coronavirus pandemic is that the pandemic aggravated the structural factors that were already driving gun violence in this country.2,10

Conclusion
This paper has brought to light the complex relationship between the COVID pandemic and our country's gun violence epidemic. As emergency medicine physicians, we are experts in getting patients where they need to be to continue their care. Often, we are the first to catch a pulmonary embolism, diabetes, surgical pathology, or cancer. When this happens, we usually know the next steps to increase patients’ chances of long-term survival. In the same respect, we are often the first hospital contact for survivors of violence.
SOCIAL EM & POPULATION HEALTH COMMITTEE
>> COMMON SENSE MAY/JUNE 2023 30
Medicine, especially emergency medicine, goes against everything that firearms stand for…A firearm’s sole purpose is to cause harm.”
With firearm violence becoming the number one cause of death for young children in the United States, this is a problem that must be aggressively addressed and remedied. 14 The Johns Hopkins Center for Gun Violence Solutions describes a detailed public health approach to gun violence prevention, and even parallels it to motor vehicle safety.15 Their approach to addressing this epidemic has multi-level interventions ranging from individual interventions like counseling and education, to larger societal interventions to shape legislation and mitigate racism and inequities. It will likely take a multi-level approach like this one to begin to see meaningful decreases in rates of firearm violence.
Medicine, especially emergency medicine, goes against everything that firearms stand for. As an EM physician, it is my job to do my best to prevent future harm from reaching you once you enter my department.
A firearm’s sole purpose is to cause harm.
While guns on their own are inanimate objects, and I understand that they do not themselves cause violence, every day at work I see how guns make acts of violence deadly. I have trouble accurately putting together words to describe what working in a North Philadelphia ED is like. Michelle Romeo does a great job at the start of her Inquirer Piece, for those who are interested.16 I can say though, once again, that guns, in theory, are against everything that physicians stand for.
Do no harm.
We cannot get rid of firearms, as much as I would want to. They are numerous and now an integrated part of American society, in a disturbing way when you look at the numbers in comparison to other countries.17 As John Rich so beautifully describes in his book Wrong Place, Wrong Time, violence is evidence of a larger problem. 18 And we here in the United States have a problem.
Some of us feel the overwhelming effects of COVID-19 and gun violence more than others, but nonetheless I urge you to be motivated by the statistics presented in this paper.
We have lost so much already. We cannot lose anymore.*
Editor’s Note: The author’s wish to extend a warm thank you to Dr. Megan Healy for her constant support and assistance with this piece.
References
*AAEM/RSA Member - PGY2, Temple University Hospital Emergency Medicine Residency
†AAEM/RSA Member - MS3, Howard Medical School
1. Gun Violence and Covid-19 in 2020: A Year of Colliding Crises. Everytown Research & Policy. https://everytownresearch.org/report/gun-violence-andcovid-19-in-2020-a-year-of-colliding-crices/. Published March 11, 2022. Accessed February 13, 2023.
2. Timeline and updates: Managing Director's Office. City of Philadelphia. https://www.phila.gov/departments/covid-19-recovery-office/timeline-andupdates/#march-2020. Accessed February 13, 2023.
3. Temple-Led Research Team Finds Covid-19 Containment Measures in Philadelphia Associated with Increase in Firearm Violence in the City.
Temple Health. https://www.templehealth.org/about/news/temple-ledresearch-team-finds-covid-19-containment-measures-philadelphiaassociated-increase-firearm-violence-city. Accessed February 13, 2023.
4. Lenthang M. Why Experts Say Gun Violence Rose in 2020, Amid Pandemic Lockdowns. ABC News. https://abcnews.go.com/US/expertsgun-violence-rose-2020-amid-pandemic-lockdowns/story?id=80466932. Accessed February 12, 2023.
5. Kim D-Y, Phillips SW. When COVID-19 and Guns meet: A Rise in Shootings. Journal of Criminal Justice. 2021;73:101783. doi:10.1016/j. jcrimjus.2021.101783
6. Parkinson C. Are Temporary Layoffs Becoming Permanent During COVID-19?: Monthly Labor Review. U.S. Bureau of Labor Statistics. https://www.bls.gov/opub/mlr/2021/beyond-bls/are-temporary-layoffsbecoming-permanent-during-covic-19.htm. Accessed February 16, 2023.
7. Sutherland M, McKenney M, Elkbuli A. Gun Violence During COVID-19 Pandemic: Paradoxical Trends in New York City, Chicago, Los Angeles and Baltimore. The American Journal of Emergency Medicine 2021;39:225-226. doi:10.1016/j.ajem.2020.05.006
8. Beardslee J, Kan E, Simmons C, et al. A Within-Individual Examination of the Predictors of Gun Carrying During Adolescence and Young Adulthood Among Young Men. Journal of Youth and Adolescence. 2021;50(10):1952-1969. doi:10.1007/s10964-021-01464-6
9. Huijsmans I, Ma I, Micheli L, Civai C, Stallen M, Sanfey AG. A Scarcity Mindset Alters Neural Processing Underlying Consumer Decision Making. Proceedings of the National Academy of Sciences. 2019;116(24):1169911704. doi:10.1073/pnas.1818572116.
10. McGinty EE. Mental illness and Gun Violence: Disrupting the Narrative. Psychiatric Services. 2018;69(8):842-843. doi:10.1176/appi.ps.201800172
11. Necka EA, Rowland LM, Evans JD. Social Disconnection in Late Life Mental Illness – Commentary From the National Institute of Mental Health. The American Journal of Geriatric Psychiatry. 2021;29(8):727730. doi:10.1016/j.jagp.2020.08.013
12. Bland AR, Roiser JP, Mehta MA, Sahakian BJ, Robbins TW, Elliott R. The Impact of Covid-19 Social Isolation on Aspects of Emotional and Social Cognition. Cognition and Emotion. 2021;36(1):49-58. doi:10.1080/026999 31.2021.1892593
13. Blair RJ. Callous-Unemotional Traits and Gun Violence. American Journal of Psychiatry. 2020;177(9):797-798. doi:10.1176/appi.ajp.2020.20071041
14. Gebeloff R, Ivory D, Marsh B, Mccann A, Sun A. Childhood's Greatest Danger: The Data on Kids and Gun Violence. The New York Times. https://www.nytimes.com/interactive/2022/12/14/magazine/gun-violencechildren-data-statistics.html. Published December 14, 2022. Accessed March 3, 2023.
15. Public Health Approach to Gun Violence Prevention. The Educational Fund to Stop Gun Violence. https://efsgv.org/learn/learn-more-about-gunviolence/public-health-approach-to-gun-violence-prevention/. Published April 5, 2021. Accessed February 12, 2023.
16. Romeo M. ER Doc: America is Bleeding Out, and Philly is Ground Zero: Opinion. https://www.inquirer.com/opinion/commentary/gun-violenceemergency-doctor-philadelphia-new-york-20220519.html. Published May 19, 2022. Accessed February 20, 2023.
17. Giligan, C. How the U.S. Compares to the World on Guns. U.S. News. https://www.usnews.com/news/best-countries/articles/2023-01-30/howthe-u-s-compares-to-the-world-on-guns. Accessed March 4, 2023.
18. Rich, JA. Wrong Place, Wrong Time: Trauma and Violence in the Lives of Young Black Men. Baltimore: Johns Hopkins University Press; 2011.
SOCIAL EM & POPULATION HEALTH COMMITTEE
COMMON SENSE MAY/JUNE 2023 31
The Golden Hour: Buprenorphine Prescribing from the Emergency Department
Jessica Moore, MD

Timing is everything. In the emergency department, we are acutely aware of this concept. Sometimes, you only have a short window to intervene before you’ve lost the opportunity to change an outcome. Time is brain for stroke, and time is muscle for STEMI. You are familiar with the golden hour: the short period of time after traumatic injury during which your intervention is most likely to prevent death. Is there a similar window for the treatment of opioid use disorder?
We are all familiar with the opioid crisis that has been ongoing for decades. According to the CDC, over 91,000 people died from drug overdose in 2020, with just about 75% of those deaths involving an opioid. Between 2019 and 2020, we saw a 31% increase in the age-adjusted rate of overdose.1 In addition to the mortality burden, we also know that opioid use causes substantial morbidity related to nonfatal overdose as well as medical complications of use, namely infections. According to the Joint Economic Committee, when considering health care expenditure, loss of productivity, criminal justice involvement, and reduced quality of life, opioid use was estimated to cost the U.S. economy approximately 1.5 trillion dollars in the year 2020.2

Fortunately, we have medications that are proven highly effective for the treatment of opioid use disorder (OUD). Buprenorphine, a partial opioid agonist, is a medication which was approved by the FDA in 2002 for the treatment of OUD. Perhaps most commonly prescribed as Suboxone® (buprenorphine/naloxone combination product), it is associated with markedly decreased mortality as well as decreased illicit opioid use, rates of overdose, and rates of HIV when compared to abstinence-based treatments.3-6 Use of medications for OUD (MOUD) such as buprenorphine also increases likelihood of retention in care, which is linked to reduced criminal justice involvement and greater likelihood of employment.6-8
The evidence is abundant and clear: buprenorphine is safe and effective. You may be surprised to learn that buprenorphine’s number needed to treat for mortality benefit is smaller (better) than that for medications we consider some of the most highly effective in medicine today. As written by Dr. Elisabeth Poorman in a 2021 New England Journal of Medicine commentary: “In one study, buprenorphine treatment was associated with a 37% reduction in all- cause mortality during the year after a nonfatal overdose. This reduction is larger than the reduction in mortality associated with any blood-pressure medication, diabetic agent, or statin. It is larger than the reduction associated with aspirin after an ST- segment elevation myocardial infarction (STEMI).”9 A medication with such astounding mortality benefit, for any other less-stigmatized disease, would be given out like candy.
Historically, the prescribing of MOUD has been tightly regulated. The most highly regulated is methadone, which when used for the treatment of OUD, must be dispensed by a federally regulated opioid treatment program (“OTP” or “methadone clinic”). Buprenorphine, although somewhat less regulated, still had its own set of barriers which significantly limited its use. Until recently, providers were required to register for a Drug Addiction Treatment Act 2000 waiver (“DATA 2000 waiver” or “X-waiver”) in order to prescribe buprenorphine for the treatment of OUD. Additionally, constraints existed regarding the number of patients to which a single provider could prescribe buprenorphine, a DEA Schedule III medication. Ironically, no similar waiver has been required to write for other controlled substances considered to have higher misuse potential (think DEA Schedule II medications like oxycodone)—and no other medical condition has limits on the number of life-saving scripts that can be written by a single provider per given time frame. Could you imagine if we were constrained in the number of epinephrine autoinjector or antibiotic prescriptions we could write in a year? Surely, such a restriction would have long ago been abolished due to ethical concerns.
As of January 2023, Section 1262 of the Consolidated Appropriations Act, 2023 removed the federal requirement for practitioners to submit a Notice of Intent to prescribe DEA schedule III, IV, and V medications for the treatment of OUD. In other words, the bill eliminates the X-waiver requirement, effectively allowing any practitioner with a DEA license to prescribe buprenorphine for the treatment of OUD.10 It also removes prescribing limits. Medical societies across the country have applauded this change and count it as a monumental step in improving access to care for patients with OUD. This legislation has the potential to be practice-changing for many emergency physicians.
>> PAIN AND ADDICTION COMMITTEE
COMMON SENSE MAY/JUNE 2023 32
ED presentations are a type of golden hour for patients with OUD—a critical window of opportunity for initiation of evidence-based treatment.”
But why, you may ask, should I prescribe buprenorphine from the ED? First, it’s often where we find the patients who need it most.11 The patients with the most severe and unstable forms of their disease are those we see in emergency departments. Second, we see improved outcomes when treatment is started in the ED, when compared to delaying to outpatient follow up for initiation.12,13 ED buprenorphine prescribing has been shown to increase linkage to outpatient treatment and retention rates.14 While some may worry ED buprenorphine prescribing would lead to an increase in ED utilization, the opposite was shown to be true: those who get buprenorphine prescriptions from the ED have decreased emergency department utilization.15 Third, medications like buprenorphine are considered standard of care for opioid use disorder, and as such, should be provided whenever indicated, as is done for all other medical conditions. Patients with OUD can and do achieve remission, but only if they have access to treatment.
ED presentations are a type of golden hour for patients with OUD—a critical window of opportunity for initiation of evidence-based treatment. Patients presenting to the ED for opioid overdose in particular have high post-discharge mortality rates, with a significant number of deaths occurring in the first two days after discharge.16 If treatment is not started in the ED, there is a very real possibility the patient may have a fatal overdose before ever getting to an outpatient buprenorphine provider.
We, as emergency physicians, have always been the ones to adapt, innovate, and rise to the occasion for our patients. You may be the only doctor your patient is able to see. You have the incredible ability to immediately and substantially reduce that patient’s risk of mortality by prescribing buprenorphine when needed. Statistically speaking, it may be the most life-saving intervention you perform during that shift.
Emergency physicians are among the best-equipped doctors to intervene in the opioid crisis. Our specialty is one that is relatively quick to implement change in response to new and compelling guidelines, policies, and evidence. We are jacks of all trades, and if we can learn the basics (and more) of diverse specialties including cardiology, critical care, pediatrics, anesthesiology, radiology, palliative care, and OB/GYN, we can learn this one addiction medicine intervention too. Buprenorphine prescribing is within your scope of practice, and it is simpler than floating a pacer or determining the etiology of your patient’s nonspecific dizziness.
Without past restrictions on buprenorphine prescribing, we all now have the power to make a difference in so many lives, and for society at large. I hope that with this change, ED buprenorphine prescribing will continue to become more commonplace.
I am optimistic that, like me, you will view the removal of the X-waiver
as a long awaited and exciting opportunity for our specialty to be part of the solution to the opioid epidemic. May you be empowered to use buprenorphine as just one additional tool you have to save lives. After all, it’s what you already do best. For information and educational materials on treating opioid use disorder in the ED:
AAEM’s white paper: Management of Opioid Use Disorder in the Emergency Department: A White Paper Prepared for the American Academy of Emergency Medicine
SAMHSA: TIP 63: Medications for Opioid Use Disorder
NIDA: Initiating Buprenorphine Treatment in the Emergency Department
For outpatient addiction medicine resources in your area:
SAMHSA: Buprenorphine Practitioner Locator and Opioid Treatment Program Directory https://www.samhsa.gov/medications-substance-use-disorders/find-treatment
References
1. Centers for Disease Control and Prevention. Drug Overdose. June 2, 2022.
2. Joint Economic Committee. The Economic Toll of the Opioid Crisis Reached Nearly $1.5 Trillion in 2020. 2022.
3. Evans E, Li L, Min J, et al. Mortality among individuals accessing pharmacological treatment for opioid dependence in California, 2006-10. Addiction 2015;110(6):996- 1005. (In eng). DOI: 10.1111/add.12863.
4. Dupouy J, Palmaro A, Fatséas M, et al. Mortality Associated With Time in and Out of Buprenorphine Treatment in French Office-Based General Practice: A 7-Year Cohort Study. Ann Fam Med 2017;15(4):355-358. (In eng). DOI: 10.1370/afm.2098.
5. Sordo L, Barrio G, Bravo MJ, et al. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. Bmj 2017;357:j1550. (In eng). DOI: 10.1136/bmj.j1550.
6. The American Society of Addiction Medicine. Advancing Access to Addiction Medications.
7. Bukten A, Skurtveit S, Gossop M, et al. Engagement with opioid maintenance treatment and reductions in crime: a longitudinal national cohort study. Addiction 2012;107(2):393-9. (In eng). DOI: 10.1111/j.13600443.2011.03637.x.
8. Soyka M, Träder A, Klotsche J, et al. Criminal behavior in opioiddependent patients before and during maintenance therapy: 6-year follow-up of a nationally representative cohort sample. J Forensic Sci 2012;57(6):1524-30. (In eng). DOI: 10.1111/j.1556- 4029.2012.02234.x.
9. Poorman E. The Number Needed to Prescribe - What Would It Take to Expand Access to Buprenorphine? N Engl J Med 2021;384(19):17831784. (In eng). DOI: 10.1056/NEJMp2101298.
10. SAMHSA. Removal of DATA Waiver (X-Waiver) Requirement. 03/29/2023 (https://www.samhsa.gov/medications-substance-use-disorders/removaldata-waiver- requirement).
Countinued on page 37 >>
We are jacks of all trades, and if we can learn the basics (and more) of diverse specialties… we can learn this one addiction medicine intervention too.”
PAIN AND ADDICTION COMMITTEE
COMMON SENSE MAY/JUNE 2023 33
What We Do Matters, But What We Say Matters Too: How Stigmatizing Language Can Affect Our Patient Interactions in the Emergency Department, and Beyond
Rajitha Reddy, MD,* Amina Ramadan, MD,* and Shana Ross, MD*
As emergency medicine (EM) physicians and physicians in training, we know that what we do matters, not just to our patients, but to our communities. Our choice of words also matter, whether in patient interactions, professional discussion, or the electronic medical record. The use of stigmatizing terms, regardless of malintent, can impact our beliefs, biases, and the care we provide. Our hope is to empower physicians to have humility and recognize how our biases can lead to word choices which negatively impact patient care, and the physician-patient relationship.
Even in medical literature and publications, stigmatizing descriptors for patients have been used. Patients with Sickle Cell Disease (SCD) often are called “sicklers” which is associated with negative attitudes toward this population.2 This term, similar to other derogatory terms such as “alcoholic” and “CFer,” identifies the patient as the disease instead of the patient having the disease. Patients with SCD who experience discrimination have a higher likelihood of experiencing more pain.5 SCD predominantly affects the black population which further compounds the bias these patients receive. Black Americans who already have poor health outcomes in America and are less likely to be treated for pain.1
The impact of stigmatizing language is seen to affect care quality and continuity not just in patients with sickle cell anemia, but in many other conditions as well. Patients with opioid use disorders, particularly mothers of infants with neonatal abstinence syndrome, are known to avoid seeking treatment and be less likely to follow-up if they feel negatively stigmatized for their substance dependence during interactions with health care providers.8 Stigmatizing terms by nature conflate
a person with the negative aspects of their human experience and draw no distinction between them. Patients at risk for stigmatization typically bear a number of other social burdens, such as housing instability, single parenthood, and socioeconomic disadvantage, which come with their own sets of negative terms. This interplay of factors means that treating a patient’s presenting medical problem, whether or not it is substance-related, as separate from the patient themself, can be a small but critical step towards empowerment, respect, improved compliance, and better care. Approaches such as using “patient-centered language” have been shown to change not only patient attitudes but also those of health care teams.9 For example, a 2010 study by Kelly and Westerhoff showed that the term “substance abuser” provoked stigmatizing reactions in providers, and a 2019 study by Ashford et al showed that the use of
these terms may negatively influence medical decision-making.4
Similarly, obese patients are known to avoid health care appointments and follow-up care due to perceived stigma. Particularly among adolescents, use of preferred weight-related terms such as “unhealthy weight” and “plus size” over terms such as “large” and “fat” have been shown to contribute positively to the patient-provider relationship.7 High numbers of obese patients report avoidance of their physician if they feel weight-based stigma, many going so far as to find a new doctor. 6 These disruptions in care due to negative feelings can undermine our efforts to help our patients improve their health.
Literature on whether using patient-centered language and avoiding stigmatizing terms actually improves health care outcomes is >>
Patient trust and empowerment are factors that should matter to us, because providing high quality care is about more than just numbers—it is also about whether our patients feel cared for when they seek us out in their moments of vulnerability and need.”
COMMON SENSE MAY/JUNE 2023 34
sparse. This is understandable in the American health care system, where research funding is typically directed towards more concrete and measurable challenges than word choice. Additionally, modern emergency medicine is more focused on metrics than ever before, leaving qualitative research to fall by the wayside unless it contributes tangibly to hospital performance. Stigmatizing terminology can also be seen as a “soft” contributor to successful patient care, especially in a fast-paced field where there are higher-priority physiologic and pharmacologic elements to be urgently addressed. Multiple studies have, however, shown definitively that use of stigmatizing language erodes trust between patient and provider, resulting in less empathetic care, and patients who feel disempowered.10 Patient trust and empowerment are factors that should matter to us, because providing high quality care is about more than just numbers—it is also about whether our patients feel cared for when they seek us out in their moments of vulnerability and need.
Stigmatizing language in patient charts has been shown to impact the attitudes of physician trainees towards patients.3 Once this language becomes a part of a patient's chart it can multiply future bias. With the new CARES Act patients now have real-time access to patient notes. All providers despite their previous level of interest in word choice will be impacted. This extends the patient physician relationship usually confined to the emergency room.
Regardless, one thing remains certain, and that is that our words, as physicians, matter. They matter to our patients, who use our words as a gauge of whether they should trust and turn to us. They matter in our professional interactions, where they can either project culpability onto our patients for the conditions they endure, or the neutrality necessary to separate affliction from the afflicted.4 They matter to the larger communities within which our medical practices abide, where many social factors beyond our control contribute to our patients’ morbidity. We do not want our failure to perceive a patient as a human being with dignity, separate from their disease, and deserving of the most respectful terminology available, to be one of those factors.
Our first priority is to do no harm, but biases, which are the root of stigmatizing language, are instilled in us involuntarily, and in medical training, purely by virtue of the society we live in. By having humility, recognizing our own biases, and making the effort to improve, we can reduce the risk that patients we care for will experience stigmatization. Emergency physicians care for the most vulnerable in society, often those from marginalized communities who already face enough barriers to care. Today, we are many patient’s first, last, or only interaction with our health care system. It is more important now than ever that these patients feel they can trust us to care for them in our emergency departments.
References
1. *University of Illinois at Chicago Department of Emergency Medicine
2. Anderson KO, Green CR, Payne R. Racial and ethnic disparities in pain: causes and consequences of unequal care. J Pain. 2009 Dec;10(12):1187-204. doi: 10.1016/j.jpain.2009.10.002. PMID: 19944378. https://pubmed.ncbi.nlm.nih.gov/19944378/
3. Glassberg J, Tanabe P, Richardson L, Debaun M. Among emergency physicians, use of the term "Sickler" is associated with negative attitudes toward people with sickle cell disease. Am J Hematol. 2013 Jun;88(6):5323. doi: 10.1002/ajh.23441. Epub 2013 May 13. PMID: 23526459; PMCID: PMC5027173. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5027173/
4. Goddu A, O'Conor KJ, Lanzkron S, Saheed MO, Saha S, Peek ME, Haywood C Jr, Beach MC. Do Words Matter? Stigmatizing Language and the Transmission of Bias in the Medical Record. J Gen Intern Med. 2018 May;33(5):685-691. doi: 10.1007/s11606-017-4289-2. Epub 2018 Jan 26. Erratum in: J Gen Intern Med. 2019 Jan;34(1):164. PMID: 29374357; PMCID: PMC5910343. https://pubmed.ncbi.nlm.nih.gov/29374357/
5. Kelly JF, Westerhoff CM. Does it matter how we refer to individuals with substance-related conditions? A randomized study of two commonly used terms. Int J Drug Policy. 2010 May;21(3):202-7. doi: 10.1016/j. drugpo.2009.10.010. Epub 2009 Dec 14. PMID: 20005692. https:// pubmed.ncbi.nlm.nih.gov/20005692/
6. Mathur VA, Kiley KB, Haywood C Jr, Bediako SM, Lanzkron S, Carroll CP, Buenaver LF, Pejsa M, Edwards RR, Haythornthwaite JA, Campbell CM. Multiple Levels of Suffering: Discrimination in Health-Care Settings is Associated With Enhanced Laboratory Pain Sensitivity in Sickle Cell Disease. Clin J Pain. 2016 Dec;32(12):1076-1085. doi: 10.1097/ AJP.0000000000000361. PMID: 26889615; PMCID: PMC5045821. https:// www.ncbi.nlm.nih.gov/pmc/articles/PMC5045821/pdf/ajp-32-1076.pdf
7. Puhl R, Peterson JL, Luedicke J. Motivating or stigmatizing? Public perceptions of weight-related language used by health providers. Int J Obes (Lond). 2013 Apr;37(4):612-9. doi: 10.1038/ijo.2012.110. Epub 2012 Jul 10. Erratum in: Int J Obes (Lond).2013 Apr;37(4):623. PMID: 22777543. https://pubmed.ncbi.nlm.nih.gov/22777543/
8. Puhl RM, Himmelstein MS. Adolescent preferences for weight terminology used by health care providers. Pediatr Obes. 2018 Sep;13(9):533-540. doi: 10.1111/ijpo.12275. Epub 2018 Mar 24. PMID: 29573233. https://pubmed. ncbi.nlm.nih.gov/29573233/
9. Schiff DM, Halvorson AE, Dupont W, Davis MM, Patrick SW. Impact of stigmatizing language describing opioid-exposed mother infant dyads: A randomized case vignette study. Subst Abus. 2022;43(1):551-555. doi: 10.1080/08897077.2021.1975866. Epub 2021 Sep 29. PMID: 34586979; PMCID: PMC9644408. https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC9644408/
10. Traxler B, Nicks S, Puckett M, Dunn K, Croff JM, Hartwell M. The use of person-centered language in scientific research articles focusing on opioid use disorder. Drug Alcohol Depend. 2021 Nov 1;228:108965. doi: 10.1016/j.drugalcdep.2021.108965. Epub 2021 Sep 4. PMID: 34507010. https://pubmed.ncbi.nlm.nih.gov/34507010/
11. van Boekel LC, Brouwers EP, van Weeghel J, Garretsen HF. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013 Jul 1;131(1-2):23-35. doi: 10.1016/j. drugalcdep.2013.02.018. Epub 2013 Mar 13. PMID: 23490450. https:// pubmed.ncbi.nlm.nih.gov/23490450/
WHAT WE DO MATTERS,
IN
BEYOND
BUT WHAT WE SAY MATTERS TOO: HOW STIGMATIZING LANGUAGE CAN AFFECT OUR PATIENT INTERACTIONS
THE EMERGENCY DEPARTMENT, AND
COMMON SENSE MAY/JUNE 2023 35
You Can't Make This S--- Up
Robyn Hitchcock MD FAAEM
The local dialysis unit calls saying they have an agitated woman who ripped out her dialysis catheters and is talking about suicide because her dog was killed yesterday so they are sending her to the emergency department. Which I am super excited about because like most critical access hospitals, we do not have inpatient dialysis and I will not be able to complete this lady’s dialysis. If she has life-threatening electrolyte disturbances I can’t fix it, nor will I be able to send her anywhere to fix it. Happy Monday.

She gets into the emergency department and her vitals are normal. Her EKG is stable suggesting her potassium should be okay. But she is restless, angry, pacing the room and intermittently slamming the glass doors. We start our usual medical work up and call the psychiatric evaluation team who agrees with me that she really looks more angry than crazy. I had gotten the rest of the department settled down so I was able to tuck aside some time to sit down and really talk with her. I walk into the room and see a woman with pink hair, in the psych eval mandated blue paper scrubs, looking and acting really angry. I asked her if she wanted to talk.
“About what?” She says.
“Well, why don’t we start with what happened at dialysis. The nurses say you got upset and ripped out your catheters.”
“I might have ripped out the catheters but it was an accident. They always put the wrong kind of tape on me. My skin doesn’t like paper tape. So I was scratching my arm and the blankets might have come up and I guess the catheters came out but I didn’t mean to take them out and I certainly wasn’t trying to kill myself.”
Okay, that’s plausible.
“Do you want to talk about what happened to your dog, I heard you lost her yesterday and I’m so sorry.” I asked next.
“The woman across the valley poisoned my dog. I know it. There are at least six dogs on the property and none of the others are suffering at all. I know that bitch is responsible.”
“It sounds like you know this woman and there’s a history there. Do you want to talk about it?”
Here it comes…
“Ten years ago my son started dating this girl. She came to us one day saying that he was physically abusing her so we took her into our house to live with us.”
She pauses and stares directly at me saying, “Never take a snake into your home. Cut off its head and bury it under a rock.”

She then continues. “After she’d been with us a couple of weeks, I had to go to the coast. I asked my husband if he wanted to come, but he said he needed to stay at home and supervise the wood cutting so we’d have wood for the winter. I asked my son if he wanted to come, and he said he had to work on wood cutting as well. So I went down to the coast on my own.
“While I was gone, my husband was sleeping on the couch in the living room because we had ripped up the carpet in the bedroom. One night she came to him after he’d been drinking and had taken some pain pills, naked, while he was on the couch and he was too out of it to know what was going on so they had sex. I think she raped him. My son found out about it and tried to attack her but he found my husband, his father. He beat him up instead and killed him. So my husband is dead, and my son is in jail because of this woman.
“Several years ago I had to go to the hospital for a prolonged time over two and a half months. As a result of this I was going to lose my house because of hospital bills so I signed my property over to one of my nephews. He has since moved several families in and there are various shacks and RVs of some very undesirable people on the property now. I’ve tried to get them to leave but my nephew says it’s not my property so I can’t make anyone go.
“Between all of these people there are quite a few dogs. My beloved German Shepherd was the only dog that suddenly started experiencing symptoms of poisoning and died yesterday. I’m absolutely sure this woman is responsible and I’d like to take a gun to her head and kill her.”
RURAL MEDICINE INTEREST GROUP
>> COMMON SENSE MAY/JUNE 2023 36
She pauses and stares directly at me saying, “Never take a snake into your home. Cut off its head and bury it under a rock.”
We did our usual medical work up and fortunately her labs were pretty unremarkable. Her electrolytes were stable although her creatinine was elevated given that she was in renal failure. After a long discussion with her regular therapist, the police, and the psychiatric intake team all agreed that she was homicidal but she wasn’t crazy and homicidal. Psychosis was not making her homicidal—it was a social situation that was. She did not need psychiatric evaluation or hospitalization. This is a legal issue for the police, not a medical issue or a psychiatric one. After warning her potential victims and notifying the police, we discharged her because it was not a medical problem.
You can’t make this s--- up. Why do these things always end up in the emergency department? Sometimes it feels like a bad episode of Jerry Springer. Or a good one. Namaste.
11. Shastry S, Counts C, Shegog E, Loo G, Cowan E. Emergency Department Utilization Patterns in Patients with Opioid-Related Emergency Department Visits. Subst Use Misuse 2022;57(6):995-998. (In eng). DOI: 10.1080/10826084.2022.2046098.
12. Streck JM, Ochalek TA, Badger GJ, Sigmon SC. Interim buprenorphine treatment during delays to comprehensive treatment: Changes in psychiatric symptoms. Exp Clin Psychopharmacol 2018;26(4):403-409. (In eng). DOI: 10.1037/pha0000199.
13. Sigmon SC, Ochalek TA, Meyer AC, et al. Interim Buprenorphine vs. Waiting List for Opioid Dependence. N Engl J Med 2016;375(25):25042505. (In eng). DOI: 10.1056/NEJMc1610047.
14. D'Onofrio G, O'Connor PG, Pantalon MV, et al. Emergency departmentinitiated buprenorphine/naloxone treatment for opioid dependence: a randomized clinical trial. Jama 2015;313(16):1636-44. (In eng). DOI: 10.1001/jama.2015.3474.
15. Le T, Cordial P, Sankoe M, et al. Healthcare Use After Buprenorphine Prescription in a Community Emergency Department: A Cohort Study. West J Emerg Med 2021;22(6):1270-1275. (In eng). DOI: 10.5811/ westjem.2021.6.51306.
16. Weiner SG, Baker O, Bernson D, Schuur JD. One-Year Mortality of Patients After Emergency Department Treatment for Nonfatal Opioid Overdose. Ann Emerg Med 2020;75(1):13-17. (In eng). DOI: 10.1016/j. annemergmed.2019.04.020.
RURAL MEDICINE INTEREST GROUP
COMMON SENSE MAY/JUNE 2023 37
PAIN AND ADDICTION COMMITTEE Countinued from page 33 >>
Social Service Resources in the Emergency Department: How We Can Impact Social Determinants of Health
Madi McDole, OMS-III* and Kelsey Newbold, OMS-III*
hile emergency departments specialize in urgent and acute medical care, EDs often provide a general entry point for patients to gain access to health care and serve as a place that patients go to seek social services.1 Social determinants of health play a significant role in the physical, mental, and emotional health of patients, and basic health care needs go beyond simply treating physical ailments and disease. Emergency department providers and staff have a unique opportunity to intervene and assist patients by providing social service resources to those who may otherwise not have the knowledge of, or access to, such resources. Yet, looking from a bird’s eye view, emergency medicine as a whole seems to miss the ball on this opportunity. This is likely due to the fact that social service work is resource-intensive and time-consuming which is understandably challenging in an emergency department setting where life-threatening medical problems take priority. However, it is clear that investing time, funding, and resources into providing social services would ultimately and significantly improve the health and lives of our most vulnerable patient population. So, the question becomes, where do we start?
WCase Managers
This is the most well known and most used resource in the ED. Case managers are social service workers that have many roles, including facilitating the transition to post-hospitalization care, such as skilled nursing facilities and home health resources. Case managers also assist in connecting patients with resources available within the community including housing agencies, peer groups, food banks, and low-cost transportation.1 Utilizing social work services has been shown to have longterm benefits for patients.2 Children with asthma had lower incidences of exacerbations. Adolescent mothers had increased contraceptive use with a subsequent drop in teen pregnancies. Psychiatric patients had decreased suicide attempts. Immunocompromised patients had lower incidence of infections and decreased lengths of stay. Not only can the use of social workers improve quality of care, but it has also been shown to have financial benefits. One hospital saved nearly six million dollars in one year by initiating a case management program.3 Help patients and save money? Sounds like a win win!
Enrollment in Medicaid
There is a misconception that uninsured patients go to the ED at higher rates than their insured counterparts and use it “inappropriately” for non-emergent conditions. This isn't necessarily true. Research has


>> COMMON SENSE MAY/JUNE 2023 38
Social determinants of health play a significant role in the physical, mental, and emotional health of patients, and basic health care needs go beyond simply treating physical ailments and disease.”
shown that uninsured patients use the ED at the same rate as their insured counterparts, but they use other resources significantly less, including primary care offices and urgent cares. 4 Interestingly, patients enrolled in Medicaid had lower utilization of the ED than those who were uninsured and commercially insured. This suggests that enrolling uninsured patients in government insurance could decrease overall ED volume by increasing access to other health care resources. So, next time you have a patient without insurance, you or a case manager can educate them on Medicaid enrollment and benefits. They may be able to get coverage for that current hospital visit with presumptive eligibility.5 Unhomed patients can enroll without a permanent address as well!
Addiction Resources
As drug and alcohol use continues to rise, so do the number of patients coming to the ED with substance use disorders. In fact, this population made up 11% of all adult ED visits from 2016-2017.6 What can we do for these patients when detox centers or case managers aren't available? Alcoholics Anonymous, also known as AA, has resources that we can utilize. Each geographic area is split up into districts where there is a central intergroup office. You can contact that office to receive a “Where and When” pamphlet that gives times and locations for all the meetings in your area, as well as other informative pamphlets. Sometimes this patient population isn't ready to receive help yet, but we can give them the resources to use when they are ready. Each AA district also has a Hospital and Institution Committee where members can volunteer to provide comfort throughout a patient’s hospital detox. Additionally, there is a stigma of coming into the ED with a substance use disorder and these patients frequently leave feeling judged. Addiction is an illness. Kindness and compassion will always go further than placing blame.
Food and Clothing Resources
Food insecurity affects over 10% of U.S. households and is associated with many negative health care outcomes including increased risk for chronic diseases.7 The prevalence of food insecurity is higher among ED patients than the general public, and studies have found associations between food insecurity and more frequent ED utilization, especially among unhomed and low income patients. Let’s be honest, those turkey sandwiches we hand out are not cutting it. Resources can be provided to patients such as the USDA’s Hunger Hotline (1-866-3-HUNGRY or 1-866-348-6479) which is in place to provide information on meal sites, food banks, and other local services. However, some hospitals around the country are taking matters into their own hands by launching food pantries within their hospitals to provide patients with shelf-stable food and fresh produce.8 Additionally, many unhomed patients lack adequate clothing and may show up to our EDs without shoes, jackets, or with tattered clothing. Similarly to food pantries, some EDs around the country are starting clothing closets for discharged unhomed patients or those in need of clothing. While the hospitals that provide such food pantries and clothing closets are currently few and far between, wouldn’t it be great if this was more widespread and accessible to patients in EDs around the country?
Advocacy
It often feels like a lot of issues are out of our control. We can't materialize housing for our unhomed patients if shelters are full. We can’t force our patients to get life-saving drugs, such as Epipens and insulin, if they can't afford the steep price. We can’t provide medically necessary and lifesaving treatments if they become illegal. The list goes on. Health care policy changes need to be made and we can use our platform and experience to advocate for them. Call up your local congressman. Join an AAEM committee. Be involved in your hospital's administration. Help educate the next generation of physicians.
References
1. * Arizona College of Osteopathic Medicine, Midwestern University, Glendale, Arizona
2. American College of Emergency Physicians. Social Work and Case Management in the Emergency Department. Retrieved from https:// www.acep.org/globalassets/new-pdfs/preps/social-work-and-casemanagement-in-the-emergency-department.pdf
3. Steketee, G., Ross, A. M., & Wachman, M. K. (2017, December). Health Outcomes and costs of Social Work Services: A systematic review American journal of public health. Retrieved from https://www.ncbi.nlm. nih.gov/pmc/articles/PMC5731071/
4. Grover, C. A., Sughair, J., Stoopes, S., Guillen, F., Tellez, L., Wilson, T. M., Gaccione, C., & Close, R. J. H. (2018, March). Case management reduces length of stay, charges, and testing in emergency department frequent users. The Western Journal of Emergency Medicine. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5851494/
5. Zhou, R. A., Baicker, K., Taubman, S., & Finkelstein, A. N. (2017, December). The uninsured do not use the emergency department morethey use other care less. Health affairs (Project Hope). Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5754025/
6. Center for Disease Control and Prevention. Hospital Presumptive Eligibility. Retrieved from https://www.cdc.gov/phlp/docs/hospitalpe-brief. pdf
7. Zhang, X., Wang, N., Hou, F., Ali, Y., Dora-Laskey, A., Dahlem, C. H., & McCabe, S. E. (2021, August 19). Emergency department visits by patients with substance use disorder in the United States. The Western Journal of Emergency Medicine. Retrieved from https://www.ncbi.nlm.nih. gov/pmc/articles/PMC8463055/
8. Estrella, A., Scheidell, J., Khan, M., Castelblanco, D., Mijanovich, T., Lee, D. C., Gelberg, L., & Doran, K. M. (2021, July 14). Cross-sectional analysis of food insecurity and frequent emergency department use. The Western Journal of Emergency Medicine. Retrieved from https://www.ncbi. nlm.nih.gov/pmc/articles/PMC8328160/
9. Gany, F. M., Pan, S., Ramirez, J., & Paolantonio, L. (2020). Development of a medically tailored hospital-based Food Pantry System. Journal of Healthcare for the Poor and Underserved. Retrieved from https://www. ncbi.nlm.nih.gov/pmc/articles/PMC8073793/
PALLIATIVE CARE COMMITTEE
COMMON SENSE MAY/JUNE 2023 39
S I T C ’ s A d v a n c e s i n C a n c e r I m m u n o t h e r a p y
( A C I ) p r o g r a m s o f f e r f o c u s e d c l i n i c a l e d u c a t i o n o n a d i s e a s e s t a t e o r t o p i c a t n o c o s t f o r e m e r g e n c y p h y s i c i a n s . A t t e n d e e s o f t h e s e h a l f - d a y , i n n o v a t i v e p r o g r a m s g e t i n - d e p t h t r a i n i n g i n i m m u n o t h e r a p y t r e a t m e n t f o r a v a r i e t y o f t o p i c s f r o m e x p e r t s i n t h e f i e l d .
2023 PROGRAMS
ACI: A Focus on Toxicity Management
Part 2
June 27 | Virtual | Zoom Webinar
This program will cover etiology and management strategies for hepatic, GI/diarrhea/colitis, renal/nephritis, neurologic, pancreatic and ocular toxicities.
ACI: A Focus on Cellular Therapies & T Cell Engagers
Aug. 17 | Hybrid | Washington, DC & Virtual
Join SITC's panel of experts for an in-depth education on all aspects of cellular therapies & T cell engagers.
ACI: A Focus on Emergency Physicians



June 28 | Virtual | Zoom Webinar
Join SITC and AAEM for a CME certified course geared specifically for emergency physicians to better treat cancer patients receiving immunotherapy.




ACI: A Focus on Hematologic Malignancies


Oct. 19 | Virtual | Zoom Webinar

Gain leading industry insights on the clinical implementation of immunotherapy for hematologic malignancies.
The 2023 ACI series is jointly provided by the Partners for Advancing Clinical Education and the Society for Immunotherapy of Cancer in collaboration with the Association of Community Cancer Centers, the Advanced Practitioner Society for Hematology and Oncology and the Hematology/Oncology Pharmacy Association. These programs are provided in collaboration with the American Academy of Emergency Medicine
I N - D E P T H E D U C A T I O N F O C U S E D O N Y O U R S P E C I A L T Y R e g i s t e r a t s i t c a n c e r o r g / a c i | # L e a r n A C I C L I N I C A L E D U C A T I O N P R O G R A M S F O R E M E R G E N C Y P H Y S I C I A N S F R E E F O R H E A L T H C A R E P R O F E S S I O N A L S , S T U D E N T S , P A T I E N T S A N D P A T I E N T A D V O C A T E S . C M E , C N E , C P E A N D M O C C R E D I T S A V A I L A B L E .
™
SCAN OR VISIT SITCANCER.ORG/ACI TO LEARN MORE & REGISTER COMMON SENSE MAY/JUNE 2023 40
Discovering the Awe in Medicine: Reigniting the Disillusioned

 Shea McGrinder, MS3
Shea McGrinder, MS3
As a third-year medical student, recently coming off two weeks of an emergency medicine rotation, some might call me an expert in emergency medical care. Those “some” would be all my non-medical friends and relatives who continue to come to me with all their injuries, acute medical conditions, and any skin lesion introduced as “hey whaddya think this rash is?” These friends and family have no idea that the only diagnostic assertions I have provided fall along the lines of, “yep, that eye is definitely red.” Yet, despite my persistent deer-in-the-headlights expression, my accompanying timidity, and my fear of ascribing a two weeks to live prognosis to my friend’s hangover, I feel that my time on the rotation has made drastic improvements in my medical knowledge base and approach to patient care.
Over the rotation, I met some of the most enthusiastic practitioners that I have ever had the pleasure of slowing down to explain to me again why a paronychia is not at the top of the triage list for the night or why it is not worth running the expensive viral tests for every patient with a cough, even if I want validation for remembering that slide from a microbiology lecture. Unfortunately, however, I did meet another subset of practitioners during my time in the ER and actually in every one of my rotations— medical practitioners who regret their choice of specialty, who are disillusioned with the way the field of medicine is going, and in some cases, their decision to pursue medicine at all.
To their credit, medical schools and hospitals are trying to address the high rates of burnout with resiliency training aimed at teaching coping skills. However, these programs, when optional, will often go ignored and when mandatory, are greeted with skepticism and rolled eyes. Despite this cynicism of medical practitioners’ opinions on resiliency programs, a quick PubMed search does seem to support the efficacy of them to have a positive impact on practitioner outlooks on their careers. Unfortunately, despite the effort to help physicians cope with workplace stress, physician burnout is at its highest ever level.
The path to becoming a doctor is tough and long. The competition starts in middle school and continues throughout high school. Students must keep a near perfect GPA while taking every math and science AP course available. Then the undergrad years are spent taking myriad STEM courses deemed “weed outs” while simultaneously being expected to take on research and leadership roles to pad the resume. Many students then go to graduate school or work in medical fields to improve their medical school chances. Those that make it through this gauntlet and land in medical school then find themselves continuing to duke it out to get into a certain specialty, sometimes even vying for a field for which they had no real affinity. But they have come to a point that they have worked too hard, spent too much time, effort, and money in getting to where they are, that they feel they must go for the most prestigious or most highly compensated specialties. By the time they finally become full-fledged physicians, it is no wonder that they often feel exhausted and burnt out. However, burnout rates are not meant to be the topic of this essay. Instead, I want to revel in the good parts of being a medical student and ultimately a physician. The New York Times recently released an article titled, “How a Bit of Awe Can Improve Your Health” by Hope Reese, where the author explored the need to find awe in your daily life for the benefit of your mental health and to “improve psychological well-being.” When I read this article, I thought immediately that this is what stressed out, tired, disillusioned medical professionals need to read and practice. There is so much in medicine and medical training that can be a gut punch, but we must reflect upon and appreciate the vast knowledge we have acquired, the unbelievable work we get to do every day, and the positive effects we can have on others. When we end our shift, we have worked very hard but we have done really good work. So, my advice to my fellow medical students, residents, and attending physicians who have regrets or doubts about what they do is to put their inner deer back in the headlights that once let you gape in total amazement at a resident draining the priapism for 45 minutes at 2:00am.
I remember one patient that we had who had a recent dental procedure done but had been given too much local anesthetic. This resulted in a paralysis of the right lateral rectus eye muscle leading to an inability to move the eye to the right. She sat in a chair in the back of the emergency
Countinued on page 43 >> COMMON SENSE MAY/JUNE 2023 41
There is so much in medicine and medical training that can be a gut punch, but we must reflect upon and appreciate the vast knowledge we have acquired, the unbelievable work we get to do every day, and the positive effects we can have on others.”
WiEM 2023: Looking to the Future
Danielle Goodrich, MD FAAEM FACEP

Sheryl
Sandberg
once said, “leadership is about making others better as a result of your presence and making sure that impact lasts in your absence.” The Women in EM Section (WiEM) has had phenomenal leaders who have cultivated a network of strong women and men to create programs and opportunities for our members. As the incoming section chair for WiEM, I am grateful to have learned from the best and I am excited to take the reins and continue their legacy.
In the past years, WiEM has used the strength and passions of our members to develop programming to meet the needs of all our members. I am especially proud of our zoom panels and speaker series tailored to DO and international students through the EM Bound Osteopathic Student Webinar Series and the EM Bound IMG Student Webinar Series. It can be difficult to find mentors and these events provide students and residents with opportunities and information from those who have been there before. My hope is that other communities from different backgrounds will be represented in future programming. Our WiEM team has put together awesome programming at Scientific Assembly and we hope to continue to expand our presence in the coming years. Our WiEM luncheon has been a hit and our collaboration with the Muslim WiEM has created new traditions with an Eid al-Fitr dinner this year which celebrates the breaking of the month long fast of Ramadan. I hope to cultivate the same passions to create more opportunities that reflect the diversity and interests of all our members.
As an emergency medicine physician who works in a tertiary care center, though without a dedicated EM residency program, I have often suffered from imposter syndrome. However, AAEM and WIEM have provided me the opportunities to get involved and find a connection. I hope to do the same for others. While I encourage everyone to get involved, I especially hope to do more events with WiEM who work in the community to foster engagement and programming that meet their needs. AAEM is the champion of the emergency physician, no matter your practice style, we are here for you. What is in store for the coming year? Keep a lookout for our Women’s Wisdom Podcast.

Listen as Dr. Molly Estes interviews female leaders in AAEM and learns their secrets to their success. We will continue our zoom series and panels with new topics on the way including work/life balance, fertility, and more. We hope to continue to develop our mentorship program and create more programming for leadership development. Please join us for our monthly open council meetings to hear more about our upcoming events and get involved.
I am looking forward to a successful year, through our ongoing programming as well as developing new and impactful opportunities for our members.
WOMEN IN EMERGENCY MEDICINE SECTION
WiEM has used the strength and passions of our members to develop programming to meet the needs of all our members.”
COMMON SENSE MAY/JUNE 2023 42
Leah Colucci, MD MS
Well, this sucks.
A little over two years ago I expressed to a group of PDs that I was very nervous about the future of emergency medicine. I anticipated that our workforce issues and the independent practice/scope creep would make us less desirable to applicants. That group told me I was being influenced by the AAEM folk I had been hanging out with and things were not that drastic. After the 2021 match, one of those people reached out to congratulate me on my excellent match (shout out to my amazing program that I will forever be proud to call home). This individual highlighted how competitive 2021 was for EM and asked me if I was done being “Chicken Little,” because the sky clearly was not falling. I really do not want to say I told you so, but alas with over 500 open spots (the majority filling through SOAP) our problems are being exposed.
To those residents who SOAPed into emergency medicine: You are family now. You belong. Imposter syndrome is hard enough without you questioning if you deserve to be here or are wanted at your institution. The same goes for residents at CMG programs—I can only imagine how awful it feels to hear the negative chatter online or speculation about your institution. You deserve high quality training and support in your education just like anyone else. We want to protect you and your future career. So please know we fiercely represent all residents.
While the dirty laundry of our specialty is being aired, do not feel hopeless. There is so much that can be done and exposing these problems just means more people are acknowledging what our organization has been saying for a long time. More people are joining our mission.

We need to fight for due process on the hill. We need to address
Countinued from page 41 >>
room while waiting for it to resolve as it seemed likely to be a transient issue. All the residents and all the medical students fought over who would get to go perform her next neuro exam to see this eye not move, constantly having to remind ourselves that we would be freaking her out by swarming her all at once. It is almost comedic how excited we were to not see something happen, and yet it is exactly the kind of excitement and joy in what we are doing that I am pitching we all try to find in our work. It is imperative that we take an extra second to get excited about the culmination of all that hard work to be able to appreciate even such a minute detail of someone’s state of health.
workplace violence and security for our staff. We need to empower our nurses and stand with them, so they stay at the bedside instead of leaving to become NPs. We need to fight the expansion of scope of practice for mid-levels. We need to share resources on how boarding is being improved at different shops across the country. We need to encourage the highest standards of education at all of our programs to create the best and brightest physicians. You might just be one voice at your hospital, and maybe you will be called Chicken Little too, but one voice is better than none and one voice can make a difference.
AAEM/RSA wants you to join us in fixing the issues. Reach out. I have a spot for you, by golly, I have a leadership position for you! You can run one of our task forces, write a white paper, lead a committee. There are endless opportunities and I will find you a role that is the right fit. This is my call to arms.
Email: president@aaemrsa.org
2023 Match
AAEM/RSA PRESIDENT’S MESSAGE
While the dirty laundry of our specialty is being aired, do not feel hopeless. There is so much that can be done and exposing these problems just means more people are acknowledging what our organization has been saying for a long time.”
DISCOVERING THE AWE IN MEDICINE: REIGNITING THE DISILLUSIONED
The challenge I put forth to you is to remind yourself how incredible even the most mundane cases are, and how insane it is what you can do to better someone’s health. Every day, find that interesting detail in a case that years of study have allowed you to recognize and let that be a reminder of why you are doing this, and a motivation to keep pushing onward with an ongoing, renewed awe for medicine. It truly is an incredible field for incredible people, and I hope that you can find and maintain that medical student-level of fascination. COMMON SENSE MAY/JUNE 2023 43
Looking Back, Moving Forward
Mary Unanyan, OMSIV, AAEM/RSA Medical Student Council Chair

After years of hard work, the day has finally come, To graduate from medical school, and step into the sun, A journey that began with a single step, Is now a milestone we'll never forget.
The path was winding, but filled with power, A journey of growth, of learning and change, Of facing challenges, and embracing the strange. The endless hours of studying and exams, The sleepless nights and constant cram, The sacrifices made, the doubts and fears, The pressure to perform, all fade away as graduation nears.
We've learned so much, about the human form, From cells and organs, to disease and norm, We've witnessed life, from birth to death, And studied ways, to give it its best breath.
In those moments, we grew so strong, We learned to cope, to carry on, Developing a sense of right and wrong, To keep us headstrong as we wake each dawn. But it's not just about the knowledge we gained, It's about the compassion we've maintained, We sacrificed our time, our sleep, and our youth, To learn what it takes, to restore another’s truth.
So let's celebrate this momentous day, The end of one journey, the start of a new way, To a new chapter in our medical career, With gratitude and pride, and no hint of fear.
The pressure is high, the stakes are even higher, But we stand tall, in the face of every fire, For we are physicians, with a noble cause, To heal and to help, to mend all flaws.
It’s no longer about the grades we received, It's about the knowledge we gained, and the skills achieved, To diagnose and treat, to ease patients’ pain, To be the one they trust, never in vain.
So here's to us graduates, the doctors of tomorrow, As healers with a calling so true, May we use our knowledge with kindness, pride, and grace, To welcome each patient with a warm embrace.
And let's be proud, of all that we've become, Of the hard work and growth in battles won, Be brave and venture forward, on the journey anew, With a heart so full that nothing can undo.
To a life of service, of compassion and care, Aim to bring hope everywhere, For as long as there are lives to repair, We will be there to help and to care.
For the honor we hold, as physicians true, Is to make a difference, in all that we do.
MEDICAL STUDENT COUNCIL CHAIR
COMMON SENSE MAY/JUNE 2023 44
So here's to us graduates, the doctors of tomorrow... For as long as there are lives to repair, We will be there to help and to care.
The Future of Fluid Resuscitation in Critically Ill Patients is Here. Or is It?
Shadman Kabir, OMS-III, Elias Wan, MD, and David H. Gordon, MD
Fluid balance is a critical aspect in the management of critically ill patients. Maintaining the right balance of fluids in the body is essential for the proper organ and system function. However, critically ill patients often have fluid imbalances due to a variety of factors, such as injury, surgery, infection, or underlying medical conditions. Fluid overload in critically ill patients has been associated with increased mortality, longer length of stay in the intensive care unit (ICU), and a higher incidence of organ failure. Therefore, determining the most effective fluid balance control is essential for the management of critically ill patients.
The POINCARE-2 study is a recent stepped wedge cluster-randomized trial that evaluated the effectiveness of a protocol-based approach to fluid balance control in critically ill patients.1 Over the course of three years, from May 2016 to May 2019, the study enrolled critically ill patients in 12 intensive care units from nine hospitals in France. The inclusion criteria for patients included at least 18 years old, under mechanical ventilation, admitted to one of the 12 recruiting units for more than 48 and up to 72 hours, and expected to have a length of stay greater than 24 hours after inclusion. Out of 10,272 patients screened, 1361 met the inclusion criteria and 1353 completed follow-up. The POINCARE-2 intervention involved daily weight-based restriction of fluid intake, diuretic administration, and ultrafiltration in case of renal replacement therapy from day 2 to day 14 after admission. The primary outcome was all-cause mortality at 60 days. Intention-to-treat analyses were used for both cluster-randomized analyses (CRA) and randomized before-and-after analyses (RBAA).
The results indicate that there was a total of 905 patients included in the study, with 433 patients in the strategy group and 472 patients in the control group for the cluster-randomized analysis (CRA), and 643 patients in the strategy group and 718 patients in the control group for the randomized before-and-after analysis (RBAA). The mean age and weight at admission were similar between the two groups in the CRA. In the strategy group, 129 patients died compared to 160 in the control group, and the difference in 60-day mortality rates between the two groups was not statistically significant. The safety outcomes showed that hypernatremia was more frequent in the strategy group compared to the control
group. Similar results were obtained from the RBAA analysis. These findings suggest that the POINCARE-2 strategy did not result in a significant reduction in mortality compared to standard care. However, the use of the POINCARE-2 strategy was associated with a higher risk of severe hypernatremia, which has also been observed in an ARDS network trial and a protocoled diuresis trial for de-resuscitation in the ICU.2,3 Growing evidence suggests that iatrogenic hypernatremia leads to an increased risk of mortality, highlighting the importance of addressing this issue.4
In conclusion, effective fluid balance control in critically ill patients requires a multidisciplinary approach that includes nurses, physicians, and other health care personnel. Regular monitoring of fluid intake, output, and balance is essential for detecting and managing fluid imbalances. The POINCARE-2 strategy did not yield a statistically significant reduction in mortality; however, it did demonstrate an observational reduction in both 60 and 28 day mortality rates. Due to differences in current global clinical practice, reduced compliance, or contamination of data, it is imperative to conduct large, sufficiently powered trials to evaluate the clinical efficacy of the POINCARE-2 strategy in critically ill patients while monitoring & treating for hypernatremia.
References
1. Bollaert PE, Monnier A, Schneider F, et al. Fluid balance control in critically ill patients: results from POINCARE-2 stepped wedge clusterrandomized trial. Crit Care. Feb 21 2023;27(1):66. doi:10.1186/s13054023-04357-1
2. Bissell BD, Laine ME, Thompson Bastin ML, et al. Impact of protocolized diuresis for de-resuscitation in the intensive care unit. Crit Care. Feb 28 2020;24(1):70. doi:10.1186/s13054-020-2795-9

3. National Heart L, Blood Institute Acute Respiratory Distress Syndrome Clinical Trials N, Wiedemann HP, et al. Comparison of two fluidmanagement strategies in acute lung injury. N Engl J Med. Jun 15 2006;354(24):2564-75. doi:10.1056/NEJMoa062200
4. Lindner G, Funk GC, Schwarz C, et al. Hypernatremia in the critically ill is an independent risk factor for mortality. Am J Kidney Dis. Dec 2007;50(6):952-7. doi:10.1053/j.ajkd.2007.08.016
CRITICAL CARE MEDICINE SECTION
COMMON SENSE MAY/JUNE 2023 45
An Accidental Communiqué From the Future
Leonard Dunikoski, DO FAAEM

Salubrious salutations! As ever, we are pleased to present a bulletin of this week’s most relevant updates and news from the greater Proxima Centauri medical community!
The Geriatrician Council has released a position statement regarding care of our near field community elders. They confirm the statistical benefit of Voidronate® in preventing low-g related osteopenia and encourage clinicians to consider lifestyle associated measures. The esteemed Dr. Xaphod stated, “Although tailored molecular therapy is appealing, we encourage our colleagues to consider simpler preventative measures for our seniors who have decided to remain enmorteled instead of uploading to the binaric afterlife. Moving a patient’s living quarters as little as 15% closer to the axis of rotation in one of our orbital O’Neil Cylinder rest homes can significantly reduce gravity related trauma.”
Adjudicators in the 13th district have confirmed that the common practice of donating hypothalamic implants to family members pursuing medical training does violate the Nepotism Statutes. They have encouraged civically minded physicians to donate their used implants to the lottery so that all trainees have “...a right to equal educational opportunity, be they siliconate or carbonate.”
Tech Laboratist Theta Melissarian premiered the latest addition of vat-grown secondary lymphatic pumps for cervical implantation. New spacefarers have long experienced volume redistribution and associated venous thromboembolism during their first weeks in zero-g. The widespread adoption of the revolutionary biosynthetic implants made such pathology vanishingly rare. This follows the announcement of promising advancements in antiproton therapy to remove residual prion contaminants in the wildly popular Soylens Pay-It-Forward™ protein snacks.
Allegations of a pay-for-cryonic stasis conspiracy rocked the quadrant last year. Recently decrypted documents detail a well-established and funded confederation of off world clinics using voidcraft transit law to evade legal doctrines. Calling the practice “unconscionable,” Dr. I’leen Clawdius reaffirmed the “rights of all younglings, spawnlings, and siliconian offspring to exist within the uninterrupted flow of galactic standard time.” The Pediatric Conclave further affirmed that all little people should be allowed to become big people and received widespread public acclaim.
Medical licensees are reminded to update their genecode registration with any professional or personal alterations at their earliest convenience. Subsequent to several recent and highly publicized cases regarding noncompliants, the Medical Directorate has adopted a zero tolerance policy. All modifications that are anticipated to fall two standard deviations from Centauri baseline must have exception authorization from the Directorate or risk consideration for involuntary biomass reprocessing.
The Heme Syndicate has recalled their “Oh, Positive”© line of nanobot augmented low titer RBCs. Their direct to consumer marketing campaign had promised to make juvenile cohorts “Better, Faster, and Stronger.” Yet alarms were raised when patients began reporting feelings of mediocrity, lassitude, and melancholy. Fabricators knowledgeable of the matter suspect a hitherto unidentified cross reaction with illicit neural boosters.
The last remaining members of the American Academy and College of Emergency Medicine have completed their ambitious, multi-decade attempt at creating a shared gestalt consciousness. Dubbed “The Hive,” initial field reports describe near prescience, perfect diagnostic and predictive capability (within 24 to 72 hours of symptom onset), a 4.2% improvement in patient throughput, and immaculate satisfaction scores. A recent patient described the experience of emergency care as “being touched by the hand of the divine.”
Remember to register for our upcoming Pan-Galactic Scientific Assembly! Beginning on Centuari perihelion 3120 and lasting 6 full cycles, attendees will have full access to a host of the system’s top educators, influencers, and bio-savants, including:
“Silicates and other four dimensional life: the anatomy of resuscitation”Dr. Scotwine Garden
“Transactional bargaining in life and death: 20th century Terran medicine” - Reverend Samha Riss
“The failure of AI and confabulatory medicine” - Dr. GP Chatterjee
“Xenoform envenomations: lessons from a trans-dimensional career”Archonate Seen Nor’dt

“Beam me up, snotty: new frontiers in transport technology” - Mssr. Erwin S.
Dinger
“Matter - it’s what you do (a treatise on the ethics of care)” - Dr. Melher Bert
…and much more! Early corvid specials do apply. Register today!
COMMON SENSE MAY/JUNE 2023 46
Their direct to consumer marketing campaign had promised to make juvenile cohorts “Better, Faster, and Stronger.” Yet alarms were raised when patients began reporting feelings of mediocrity, lassitude, and melancholy.”
2023 Recipients of ABEM 30-year Certificate
ABEM recognizes physicians who, as of December 31, 2022, have marked 30 years of being board certified in emergency medicine. Because board certification is a voluntary process, this landmark accomplishment reflects a dedication to the specialty of emergency medicine, a commitment to continuous professional development, and the long-standing provision of compassionate, quality care to all patients.
To maintain their ABEM certification for 30 years, physicians must participate in continuing professional development and learning in the specialty. The ABEM continuing certification process assists certified physicians keep current on medical advances and provides opportunities for practice improvement.
ABEM salutes these physicians for their dedication to the specialty, their recognition of the value of board certification, and their commitment to caring for acutely ill and injured patients. ABEM-certified physicians are among the finest health care providers in the United States. Each of them exemplifies the ABEM mission, “To ensure the highest standards in the specialty of Emergency Medicine.”
AAEM CONGRATULATES the following AAEM members who have achieved this honor:
Beth Anne Lux, MD FAAEM
Carlos C. Huerta, MD FAAEM
Carol Lynn Clark, MD FAAEM
Charles D. Benham, MD FAAEM
Courtney Ann Bethel, MD MPH FAAEM FACEP
Craig B. Gerstenkorn, MD FAAEM
Daniel V. Girzadas Jr., MD RDMS FAAEM
David Anthony Hnatow, MD FAAEM
David Barcay, MD FAAEM
David Nathan, MD FAAEM
David R. Hoyer Jr., MD FAAEM
David W. Habenicht, MD FAAEM
Eric D. Lucas, MD FAAEM
Eric M. Kardon, MD FAAEM
Franklin Friedman, MD FAAEM
George Robert Woodward, DO FAAEM
Glenn S. Ekblad, DO FAAEM
Gus M. Garmel, MD FAAEM FACEP
Jeter P. Taylor III, MD FAAEM
Joanne Williams, MD MAAEM FAAEM
Jonas R. Salna, MD FAAEM
Jonathan S. Rubens, MD MHPE FAAEM
Kelvin L. Spears, MD FAAEM
Marc J. Dumas, MD FAAEM
Mark Erich, MD FAAEM
Mark O. Davis, MD FAAEM
Marty Bell, MD FAAEM
Michael C. Plewa, MD FAAEM
Michael M. Dickerson, MD FAAEM FAPWCA
Nina T. Gentile, MD FAAEM
Patricia Denise Baccash, MD FAAEM
Prentice Steffen, MD FAAEM
Richard E. Daily, MD
Robert Christopher Reiser, MD FAAEM
Robert W. Wilson, MD FAAEM
Ronald L. Pearson, DO MPH FAAEM
Ronald T. Genova, MD
Russ Braun, MD MPH MBA
Scott Westenberg, MD FAAEM
Shailendra Bhatnagar, MD FAAEM
Terry Kowalenko, MD FAAEM
Timothy D. Sturgill, MD FAAEM
Ulric A. Gilkes, MD FAAEM
Walesia L. Robinson, MD FAAEM
Wayne B. Cayton, Jr., MD
William B. Lovett, MD FAAEM
William T. Fisher, MD FAAEM
Willoughby S. Hundley III, MD FAAEM
Editor’s note: If you achieved your 30-year certificate from ABEM and are a current AAEM member and not listed here, please contact cseditor@aaem.org
ABEM NEWS
COMMON SENSE MAY/JUNE 2023 47
AAEM is the leader within our field in preserving the integrity of the physician-patient relationship by fighting for a future in which all patients have access to board certified emergency physicians and physician rights are protected.
Member Benefits
Publications
Free subscriptions to the Journal of Emergency Medicine and Common Sense
Education
Free registration to the Annual Scientific Assembly with refundable deposit and discounted registration for other AAEM events
Members-Only Section
Access the AAEM Job Bank, your Advanced Resuscitation Expertise Card (for Full Voting members), and other academic and career-based benefits
Learn more about these and other member benefits at www.aaem.org/membership/benefits
American Academy of Emergency Medicine 555 East Wells Street, Suite 1100, Milwaukee, WI 53202-3823 (800) 884-2236 info@aaem.org www.aaem.org
Membership Categories
Fellow and Full Voting – FAAEM
Dues: $525 Board certified in emergency medicine or pediatric emergency medicine
Associate
Dues: $250 Graduate of an ACGME or AOA approved emergency medicine training program and not yet taken or passed your EM board
Fellow-in-Training
Dues: $75 Graduate of an ACGME or AOA approved emergency medicine training program and currently enrolled in a fellowship
International Member
Dues: $150 Physicians with an interest in emergency medicine who practice outside of the United States or Canada

Emeritus Member
Dues: $250 Full voting member who has practiced emergency medicine for 30 or more years and has been a full voting member for a minimum of 10 years -or- at least 65 years of age and have been a full voting member for a minimum of 10 years
Special circumstances may lead to a request for emeritus membership and will be reviewed on a case-by-case basis. See www.aaem.org/membership for more information.
Learn more and join today at: www.aaem.org/membership
Group Membership
AAEM offers group memberships to allow hospitals/groups to pay for the memberships of all their EM board certified & board eligible physicians.
100% ED Group Membership
Criteria: All board certified and board eligible physicians at your hospital/ group must be members
Discount: 10% discount on membership dues
ED Group Membership
Criteria: Two-thirds of all board certified and board eligible physicians at your hospital/group must be members
Discount: 5% discount on membership dues
For group memberships, AAEM will invoice the group directly. If you are interested in learning more about the benefits of belonging to an AAEM ED group, please contact us at info@aaem.org or (800) 884-2236.
Join Today! www.aaem.org/membership 51 COMMON SENSE SEPTEMBER/OCTOBER 2021 COMMON SENSE MAY/JUNE 2023 48
Synovial Lactate in the Emergency Department Evaluation of Septic Arthritis
Authors: John B. Harringa, MD, Jonathan B. Hurst, MD, Stephanie Adjei, MD, and Kyle A. Glose, MD
Editors: Michael Bond, MD FAAEM, Kami M. Hu, MD FAAEM, and Donald Doukas, MD
Introduction
Septic arthritis is a highly morbid condition with potential to progress to sepsis or irreversible tissue damage leading to devastating loss of function. Timely confirmation of septic arthritis in the ED can be quite challenging however, with the diagnosis distracted by multiple mimics, namely crystal arthropathies, immunologic processes including rheumatoid arthritis and spondyloarthropathies, and reactive arthritis, among a smattering of rarer pathologies. The typical gold standard for diagnosis, synovial fluid culture, is generally irrelevant to the emergency physician given the delay in results. As such, ED decisions regarding antibiosis, hospital admission, and surgical consultation are necessarily made without complete information. A more reliable biomarker or clinical support tool would therefore considerably aid ED physicians in rapidly intervening on septic joints while facilitating antibiotic stewardship (and more targeted therapy) in non-infectious arthritides.
Synovial lactate has long since been suggested as a biomarker for septic arthritis with literature contemplating its use at least as far back as 1983.1 Since then, additional synovial biomarkers have been identified, such as interleukin-6 (IL-6) and fraction of D-enantiomeric lactate (produced almost exclusively by bacteria) relative to L- or racemic lactate, alongside traditional markers including synovial leukocytes (SyWBC) and glucose, as well as serum leukocytes (SeWBC), erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP). Newer technology to detect pathogens has also been trialed, such as PCR for bacterial and fungal 16S and 18S ribosomes. Despite these advances, differentiating between infectious and non-infectious arthritides in the ED remains a diagnostic challenge.
In 1976, Newman offered a definition of septic arthritis:2
Microorganism identified in affected joint -or-
Microogranism identified elsewhere (e.g. bacteremia) in the setting of a painful swollen joint -or-
Radiographic or histological evidence of infection in the setting of painful swollen joint -or-
Synovial fluid turbidity.
While a useful framework, these criteria become progressively more subjective. Modern algorithms rely primarily on synovial WBC count with variable thresholds, generally 50,000 but sometimes 20,000 or even 100,000 when specificity is the priority. Other factors include the presence of crystals on microscopy (which does not exclude infection), and gram stain and culture, in addition to serum markers. Gram stain has been demonstrated to miss as much as 78% of infected joints, and culture
results 48-72 hours after the fact have little bearing on ED management.3 As such, additional clinical tools and/or biomarkers with better diagnostic characteristics would facilitate rapid diagnosis and treatment and reduce associated morbidity, as well as allow for safer and more confident ED discharges in cases of non-infectious arthritis.
Questions
1. What is the role of synovial lactate in the ED diagnosis of septic arthritis?
2. Are other biomarkers useful in the ED diagnosis of septic arthritis?
Lenski M, Scherer MA. The significance of interleukin-6 and lactate in the synovial fluid for diagnosing native septic arthritis. Acta Orthop Belg. 2014;80(1):18-25.
Lenski and Scherer looked to evaluate the role of synovial lactate and IL-6 in the diagnosis of septic arthritis. This was a single-center, retrospective case-control study that compared several synovial inflammatory markers in patients with culture-verified native septic arthritis versus those with aseptic arthritis. 119 patients in total were included in the trial, 62 patients with culture-verified septic arthritis and 57 patients with acute aseptic arthritis. Patients were included if there was suspicion of septic arthritis and joint aspiration was performed. Patients with periprosthetic joint infections or culture-negative septic arthritis were excluded. The inflammatory markers of synovial fluid IL-6, total protein (TP), glucose, lactate, and WBC were examined. Statistical analysis calculated receiver operating characteristic (ROC) curves and their corresponding area under the curve (AUC), sensitivities, specificities, and likelihood ratios (LR) to determine each marker’s utility in the diagnosis of septic arthritis.
In this study, synovial lactate demonstrated the greatest difference between cases and controls, with an AUC of 0.864 (95% CI 0.785-0.942), sensitivity of 74.5% (60.5-84.8%) and specificity of 87.2% (73.3-94.4%). This was followed by synovial IL-6 with an AUC of 0.803 (0.702-0.903), sensitivity of 92.5% (80.1-97.4%), and specificity of 64.1% (48.4-77.2%). These were not statistically significantly different from SyWBC (AUC 0.782 [0.689-0.874]; sensitivity 71.2% [57.7-81.7%]; specificity 84.9% [73.0-92.2]. Using interval likelihood ratios, detection of synovial lactate greater than 10 mmol/L essentially confirmed septic arthritis (Interval LR=20.43). Alternatively, if synovial lactate was less than 4.3 mmol/L, septic arthritis was very unlikely (Interval LR = 0.21). This study also found that synovial IL-6 could have useful rule-out probability with a level below 7000 pg/ml which reduced the likelihood of septic arthritis (Interval LR=0.12).
>>
AAEM/RSA RESIDENT JOURNAL REVIEW
COMMON SENSE MAY/JUNE 2023 49
This was a retrospective single-center study with a relatively small sample size, bringing its validity and generalizability into question. It did not include those patients with concerns for periprosthetic joint infection due to the risk of false positives. Lastly, the authors remarked that all inflammatory biomarkers were not identified for each patient, although it is unclear if this could have biased results in any way. Within these limitations, this study found that synovial lactate and IL-6 have similar test characteristics to traditional biomarkers such as SyWBC and may thus offer some added value. At extreme values in particular, synovial lactate and IL-6 performed particularly well, although in such cases it is likely that traditional methods would also lead to less diagnostic uncertainty.
Shu E, Farshidpour L, Young M, et al. Utility of point-of-care synovial lactate to identify septic arthritis in the emergency department.3 Am J Emerg Med. 2019;37(3):502-505.
Based on their observation that synovial lactate seems a promising biomarker to discriminate between septic and aseptic arthritis, Shu et al. set out to examine the utility of a bedside point-of-care (POC) blood gas analyzer as a novel technique to rapidly assess synovial lactate levels. They prospectively enrolled patients at their facility who were undergoing arthrocentesis for the evaluation of a swollen or painful joint between October 2016 and April 2018. Trial inclusion did not dictate what studies were ordered; patients were enrolled if the treating clinician was able to obtain an extra 1mL of synovial fluid in a separate sterile syringe. Synovial lactate levels were analyzed using a POC blood gas analysis system (EPOC, Alere). Further variables were subsequently abstracted from the electronic medical record (EMR). As a reference standard, they defined septic arthritis as either a positive synovial culture, or a diagnosis of septic arthritis by orthopedists leading to operative intervention (e.g. washout) and intravenous (IV) antibiotics (even if cultures were ultimately negative).
In total, 40 joints in 39 patients (one patient was included twice with bilateral affected knees) were included in the study. The incidence of septic arthritis was 27.5% (11 joints), similar to other studies. The area under the receiver operator characteristic (AUROC) curve was 0.69, corresponding to a good model per standard definitions (e.g 0.5 as no better than chance, 0.8 as a strong model, and 1.0 as a model with perfect prediction). They reported there were similar or poorer C-statistics for other commonly used tests and physical findings used to assess for septic arthritis. Their AUROC suggested that in ideal cutoff of ≥ 10mmol/L for their data, at which point, sensitivity and specificity were 27% (95% CI 10-72%) and 97% (79-99%) respectively.
A major limitation of this trial is that the POC device was neither developed for evaluation of synovial fluid, nor compared to a validated laboratory standard, though this concern is mitigated to some extent by the agreement of these results with other studies examining test characteristics of synovial lactate as pertaining to septic arthritis. The authors freely admit this study was designed more as a proof-of-concept than to achieve full and untempered support for the clinical use of this device. Further, the inclusion of three cases of septic bursitis has unclear
relevance to the clinical question. Moreover, their isolated pathogenic organisms consisted of staphylococcus aureus and group B streptococcus, with one case of Escherichia coli. This relative homogeneity may bolster their results compared to a more representative sample including other pathogens with seemingly weaker correlations with synovial lactate, such as gonococcus.4 The post-hoc identification of synovial lactate threshold is also a limitation; a future study to validate this threshold would be stronger evidence.
The authors conclude that these results are comparable to those of using SyWBC alone, which is true in some studies and less so in others. Their results support an interesting proof of concept for rapid bedside analysis of synovial lactate, which may be particularly useful in places without the laboratory capacity to rapidly perform this test. Future studies are needed and would ideally include a laboratory reference standard to lend validity to the POC device results. With poor sensitivity, however, this study provides evidence against the ED use of POC synovial lactates to rule out septic arthritis.
Li Z, Li C, Wang G, et al. Diagnostic accuracy of synovial fluid D-lactate for periprosthetic joint infection: a systematic review and meta-analysis. J Orthop Surg. 2021;16(1):606.
In contrast to L-enantiomeric lactate, D-lactate in humans is produced almost entirely by bacterial metabolism. While synovial lactate has long been a target of research in the assessment of septic arthritis, given this method of production it stands to reason that D-lactate may be more specific for the presence of pathogens over the L- or racemic lactate assays. Li et al. conducted a systematic review and meta-analysis (SRMA) examining the diagnostic accuracy of D-lactate in the evaluation of periprosthetic joint infection (PJI), whether spontaneous or as a complication of surgery.
This SRMA utilized statistical methods consistent with the Cochrane Collaboration’s standard for assessing test characteristics, and results were reported according to the PRISMA criteria for SRMAs. Data were collected independently by two researchers, with disputes resolved via discussion and consensus. Potential articles for inclusion were identified via searches of PubMed, Embase, and the Cochrane Library in June 2021 using the search terms “periprosthetic joint infection” and “prosthesis-related infection” as the diagnosis of interest and D-lactate as the target index. To be included, articles required a population having undergone joint arthroplasty and diagnosis of PJI confirmed by Musculoskeletal Infection Society (MSIS), American Academy of Orthopedic Surgeons (AAOS), or European Bone and Joint Infection Society (EBJIS) guidelines, D-lactate analyzed on synovial sample, and reported data sufficient for the construction of a 2x2 contingency table. Case reports, reviews, expert opinions, and animal studies were excluded. Studies were also assessed for methodological quality and risk of bias via the QUADRAS-2 tool.
Ultimately, 169 unique potential inclusions were identified, of which 21 full-text articles were reviewed, and five met inclusion criteria. The
AAEM/RSA RESIDENT JOURNAL REVIEW >> COMMON SENSE MAY/JUNE 2023 50
included studies consisted of 1087 patients, among whom 253 (23.3%) had PJI. The risk of bias was generally low across the studies, with only one study deemed high risk of bias in one of seven domains (flow and timing). Pooled sensitivity and specificity of D-lactate for PJI were 82% (95% CI 70-89%) and 76% (69-82%), respectively. Pooled positive and negative likelihood ratios were 3.4 (2.4-4.8) and 0.24 (0.14-0.42), and the AUROC curve was 0.84 (0.8-0.87).
Strengths of this study included the rigorous SRMA methodology and resultant large patient population with a typical incidence of PJI. Limitations included a high I2 statistic for sensitivity and specificity values, indicating significant heterogeneity of included studies. A limitation as pertaining to our goal of assessing ED evaluation of septic arthritis is the focus on PJI, which is seen more often as a surgical complication than as a spontaneously occurring process, limiting generalizability to the ED population. While the AUROC of D-lactate demonstrated good to excellent diagnostic accuracy (typically defined as AUC>0.8), this value is comparable to that seen for L- or racemic lactate. Many facilities do not have the ability to assay D-lactate, and while it makes physicologic sense that a marker produced almost exclusively by bacteria would be more useful than non-specific L- or racemic lactate, the results of this SRMA do not bear this out. The authors conclude that D-lactate has the potential to add value to the evaluation of PJI, especially as pertaining to obtaining intra-operative or post-operative synovial samples, which may be true, but in the context of the other included studies, D-lactate seems unlikely to add value in the ED environment.
Carpenter CR, Vandenberg J, Solomon M, et al. Diagnostic Accuracy of Synovial Lactate, Polymerase Chain Reaction, or Clinical Examination for Suspected Adult Septic Arthritis. J Emerg Med. 2020;59(3):339-347.
This article describes a prospective, cross-sectional study comparing the diagnostic accuracy of physical exam and history, synovial L- and D-lactate and PCR, alongside SyWBC count and gram stain for the diagnosis of septic arthritis. The authors utilized a convenience sample, including patients greater than 18 years of age who presented to a single site (Barnes-Jewish Hospital in St. Louis, MO) with acute monoarticular knee symptoms judged to be concerning for septic arthritis by the ED physician. Other joints were excluded from the study due to difficulty obtaining a sufficient volume of synovial aspirate for study tests. Antibiotic use within the 72 hours preceding presentation was an additional exclusion criterion. The primary outcome measure was sensitivity of synovial lactate for the diagnosis of septic arthritis, defined as growth of bacteria on synovial fluid cultures that was ultimately treated as an infection as evidenced by consultation with orthopedic surgery or infectious disease specialists according to standard of care.
Prior to arthrocentesis, trained research assistants collected history and physical exam elements from included patients using a standardized instrument. They also obtained clinician’s gestalt estimates of the probability of septic arthritis both before and after laboratory studies were available for review. Synovial WBC, L-lactate and D-lactate were
measured; notably, the method for measurement of D-lactate had not been validated in synovial fluid, though had been validated for serum and urine specimens. Synovial PCR was performed to detect bacterial or fungal DNA. Synovial fluid was cultured on blood, chocolate, and MacConkey agar in a 5% CO2 atmosphere for three days, and anaerobically on Brucella blood agar for five days. If the sample volume was sufficient, a portion was also inoculated into blood culture media.
Between October 2013 and July 2016, 71 patients were enrolled in the study with a mean age of 58 years. A predominance of African American males was noted in the patient demographics. During this time, the investigators observed bacterial growth in nine cases, however, four of these were deemed to be contaminants resulting in a 7% (n=5) prevalence of septic arthritis in the study population. No single element of physical examination or history was accurate in the diagnosis of septic arthritis, nor was overall clinician gestalt, as all calculated likelihood ratios (LR) included one in the confidence interval. Synovial WBC count was available in 62 cases and was noted to have a LR of 0 when between 0 and 20,000 WBC/μL, 1.3 when between 20,000 and 40,000 WBC/μL, and 22.8 when greater than 40,000 WBC/μL. Gram stain had a positive LR (+LR) of 32 and a negative LR (-LR) of 0. Synovial L-lactate >5 mmol/L was found to carry a sensitivity of 60% (15-95), specificity of 78% (65-88), +LR of 2.7 (0.68-4.7), and -LR of 0.52 (0.09-1.1). Synovial PCR showed a sensitivity of 60% (15-95), specificity of 80% (68-89), +LR of 3 (1.3-7.2), and -LR of 0.50 (0.17-1.5). No samples were found to contain D-lactate.
A major limitation of this study includes the relatively small sample size and convenience sampling method as well as the 7% prevalence of septic arthritis in the study population, which the authors note is significantly lower than the 27% prevalence observed in prior studies. The authors also note that their +LR and -LR for both synovial lactate measurement and synovial PCR were much less impressive than previously described, though do note they are not the first investigators to report similar findings. Ultimately, the authors conclude that history, physical exam, synovial L-lactate, and PCR may be inadequate alone for the diagnosis of septic arthritis and that synovial white blood cell count and gram stain remain the gold standard tests for this diagnosis.
Berthoud O, Coiffier G, Albert JD, et al.
Performance of a new rapid diagnostic test the lactate/glucose ratio of synovial fluid for the diagnosis of septic arthritis. Joint Bone Spine. 2020;87(4):343-350.
In this cross-sectional study conducted at a single-center in France during 2015-2018, synovial fluid from adult patients presenting with acute (defined as onset within the past 30 days), atraumatic native joint effusions was examined to determine the diagnostic accuracy of synovial lactate, glucose, and the glucose/lactate ratio. Septic arthritis was defined in the study according to the Newman criteria, but the reference standard was the ultimate diagnosis as assigned by the treating physician. 2 Diagnostic performance of the various lab values was assessed via calculation of the AUROC for each, in addition to determination of sensitivities, specificities, and positive and negative likelihood ratios.
>>
AAEM/RSA RESIDENT JOURNAL REVIEW COMMON SENSE MAY/JUNE 2023 51
Ultimately, 233 aspirations from 226 patients were included in the study. The mean age was 62 years and 65% were males, the knee was the most aspirated joint (72%). Out of these, 25 patients were diagnosed with septic arthritis (10.7%). Demographics between groups were similar except for a significantly higher proportion of patients with cirrhosis in the septic group versus non-septic group (16 vs. 0.5%, p <0.001). Of note, 18.5% of the individuals received antibiotics prior to arthrocentesis. On average, synovial lactate was significantly higher in cases of septic arthritis (9.3 vs. 3.2mmol/L, p<0.001), as were synovial lactate/glucose ratios (3.7 vs. 0.60, p<0.001). The lactate/glucose ratio seemed to perform favorably to synovial lactate or glucose alone, but the differences were not statistically significant: AUROC was 0.86 (95% CI 0.77-0.95) compared to 0.80 (0.68-0.91) and 0.83 (0.74-0.93), respectively. Increasing the threshold of synovial lactate to 11.0mmol/L or higher increased specificity to 99.5% (97-100%), though predictably reduced sensitivity to unacceptable levels, stratifying 16/25 cases of septic arthritis as negative. A secondary objective of this study reviewed the diagnostic performance of utilizing urine test strips and glucometers on synovial fluid to aid in rapid clinical decision-making. There was a very strong correlation between synovial fluid glucose values obtained via glucometer compared to the laboratory, but only a moderate correlation was seen between urine test strips and laboratory values.
Potential confounders include the fact that almost 20% of patients had preceding antibiotic treatment, and many had inadequate volume aspirated or pathogen species less prone to biochemical alteration of the synovial fluid. The incidence of septic arthritis was also low compared to that of other published studies. Additionally, their laboratory was only able to assay for L-Lactate and therefore may have resulted in falsely low lactate levels despite the presence of D-lactate-producing pathogens. The authors concluded that synovial lactate/glucose ratio showed relevance in differentiating septic arthritis from other acute arthritis, and this ratio performance was stronger than each component individually. With that said, its independent use continues to have limited utility in the ED.
Coiffier G, Berthoud O, Albert JD, et al. Elaboration of a new synovial predictive score of septic origin for acute arthritis on the native joint (RESAS). Rheumatol Oxf Engl. 2021;60(5):22382245.
Utilizing the same cohort as the above study, Coiffier and Berthoud et al. subsequently conducted a multivariate analysis to construct a clinical decision support tool (CST), which they called the RESAS score (REnnes hospital Septic Arthritis Score).7 The score incorporates SyWBC, presence of crystals, synovial lactate, and synovial glucose, ranges from -4 to +13 points, and defines septic arthritis at a score of ≥ . It assigns +3 points for macroscopic purulence or SyWBC of ≥70,000 and subtracts 2 or 4 points for observed calcium pyrophosphate or monosodium urate crystals, respectively. Synovial lactate levels of 8.5-9.9mmol/L adds 2 points, 10.0-11.4 adds 4 points, and a value ≥11.5 adds 6 points. Synovial glucose levels of 1.1 to 1.9mmol/L also adds 2 points, and ≤1.0mmol/L or under adds 4 points. By weighting higher synovial lactate
levels and lower synovial glucose levels, they functionally include the synovial lactate to glucose ratio, as well as incorporating traditional SyWBC measures and the logical truism that in the presence of crystal arthropathy, a second concomitant diagnosis is less likely.
The investigators applied this score to their initial cohort for internal validation, yielding an AUROC of 0.93 (0.88-0.98), improving upon their initial results. They subsequently applied the score to 70 additional cases of acute arthritis, 12 with septic arthritis as per Newman’s definition (10 of the 12 bacteriologically proven). The AUROC for this external validation cohort was 0.97 (0.94-1.0). Moreover, in comparison to the performance of any sole biomarker, this composite score offered the best sensitivity and specificity at 91.7% (64.6-98.5%) and 98.3% (90.9-99.7%) respectively, with a +LR of 53.2 (7.6-373) and -LR of 0.09 (0.013-0.55), which the authors rightly conclude are extremely promising results, at least as compared with current standards of care.
Answers
1) What is the role of synovial lactate in the ED diagnosis of septic arthritis?
In isolation, synovial lactate has inadequate diagnostic accuracy to reliably differentiate infectious and non-infectious arthritides, potentially because of the inherent characteristics of different pathogenic organisms. Synovial lactate in concert with other markers, such as glucose, may add value to current frameworks which primarily hinge on SyWBC count.
2) Are other biomarkers useful in the ED diagnosis of septic arthritis? Synovial IL-6, glucose, protein, WBC, and serum WBC, ESR, and CRP have all demonstrated varying relationships with the probability of septic arthritis. Most individual biomarkers demonstrate poor sensitivity, significantly limiting their utility in the ED, where ruling out dangerous diagnoses is of paramount importance. Clinical tools that combine various clinical and lab findings, such as the RESAS score, show promising results.
The Bottom Line
While synovial lactate on its own lacks sufficient diagnostic accuracy to rule out septic arthritis in the ED, in resource-rich settings, literature suggests there may be added value to its inclusion in a comprehensive synovial fluid analysis, which should also include gram stain, culture, microscopy (crystals, organisms), SyWBC, and glucose. Synovial IL-6 may similarly add value and has theoretical potential as a therapeutic target. The RESAS score is a novel CST which incorporates these markers with promising results to differentiate septic from non-septic acute arthritis.
References
1. Curtis GD, Newman RJ, Slack MP. Synovial fluid lactate and the diagnosis of septic arthritis. J Infect. 1983;6(3): 239-246.
2. Newman J. Review of septic arthritis throughout the antibiotic era. Ann Rheum Dis. 1976;35(3): 198-205.
3. Gbejuade H, Elsakka M, Cutler L. How well does synovial fluid gram staining correlate with cultures in native joint infections? Orthop Rev (Pavia). 2019;11(4): 8156.
4. Gobelet C, Gerster JC. Synovial fluid lactate levels in septic and nonseptic arthritides. Ann Rheum Dis. 1984;43(5): 742-745.
AAEM/RSA RESIDENT JOURNAL REVIEW COMMON SENSE MAY/JUNE 2023 52

COMMON SENSE MAY/JUNE 2023 53
AAEM Job Bank Service
Promote Your Open Position

To place an ad in the Job Bank: Equitable positions consistent with the Mission Statement of the American Academy of Emergency Medicine and absent of restrictive covenants, will be published (upon approval). All ads run for a six month period or until canceled and will appear in the AAEM member magazine Common Sense and online. For pricing and more information visit www.aaem.org/membership/benefits/ job-bank.
Complete a Job Bank registration form, along with the Criteria for Advertising Section, and submit payment. If you are an outside recruiting agent, the Job Bank Criteria for Advertising must be downloaded and completed by a representative from the recruiting hospital/group.
Direct all inquiries to: www.aaem.org/membership/benefits/job-bank or email info@aaem.org.
Positions Available
For further information on a particular listing, please use the contact information listed.
Section I: Positions in full compliance with AAEM’s job bank advertising criteria, meaning the practice is wholly-owned by its physicians, with no lay shareholders; the practice is equitable and democratic; due process is guaranteed after a probationary period of no more than one year; there are no post-employment restrictive covenants; and board certified emergency physicians are treated equally, whether they achieved ABEM/AOBEM/RCPSC certification via residency training or the practice track.
Section II: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are employee positions with hospitals or medical schools and the practice is not owned by its emergency physicians. Thus there may not be financial transparency or political equity.
Section III: Positions that cannot be in full compliance with AAEM’s job bank criteria, because they are government or military employee positions. The practice is not owned by its emergency physicians, and there may not be financial transparency or political equity.
Section IV: Position listings that are independent contractor positions rather than owner-partner or employee positions.
SECTION I: POSITIONS RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK CRITERIA
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA (Below are hospitals, non-profit or medical school employed positions.)
SECTION TWO CONNECTICUT
Trinity Health Of New England seeks BC/BE EM Physicians to join our emergency medicine teams at Mercy Medical Center in Springfield, Massachusetts, Saint Francis Hospital and Medical Center in Hartford, Connecticut and Saint Mary’s Hospital in Waterbury, Connecticut. Our practice model empowers our physicians to work at their highest level, while allowing time for professional development and family life. Whether you are focused on providing outstanding patient-centered care or driven to grow into a leadership role, you will thrive at Trinity Health Of New England. To learn more, visit our provider portal at www. JoinTrinityNE.org (PA 1985)
Email: ndiehl@abccreative.com
Website: https://www.jointrinityne.org/Physicians
MayJun, JulAug, SepOct
LOUISIANA
Ochsner Health is seeking a board certified/board eligible physicians to join our Division of Pediatric Emergency Medicine at Ochsner Medical Center and Ochsner Hospital for Children.
Opportunity Details: • Employed physician group that offers competitive fair market compensation plus benefits • In House pediatric intensivist and hospitalist attendings 24/7 to assist with streamlined pediatric admissions and patient care. • All facilities utilize Epic electronic health records integrating care across the system and facilitating seamless multi-hospital practice • All specialties available for consultation and easy one-call transfer from our community emergency departments to our main campus Interested physicians should apply to: https://ochsner. wd1.myworkdayjobs.com/OchsnerPhysician/job/New-Orleans--New-Orleans-Region---Louisiana/Pediatric-EmergencyMedicine_REQ_00158668 (PA 1991)
Email: courtney.lawhun@ochsner.org
Website: https://ochsner.wd1.myworkdayjobs.com/ OchsnerPhysician/job/New-Orleans---New-Orleans-Region--Louisiana/Pediatric-Emergency-Medicine_REQ_00158668
MayJun, JulAug, SepOct
MICHIGAN
Medical Director of Emergency Medicine Research Corewell Health William Beaumont University Hospital (previously Beaumont Royal Oak) The Department of Emergency Medicine is recruiting a Medical Director of Research to lead a nationally recognized research program. The successful candidate will be an ABEM certified emergency physician who works clinically at University Hospital with academic appointment at Oakland University William Beaumont School of Medicine. Preference will be given to candidates with a record of extramural funding, success mentoring colleagues, formal academic research training, and experience managing research. The institution is seeking a broad and diverse candidate pool. University Hospital is a 1,100-bed referral center that has been recognized by U.S. News and World Report as one of the “Best Hospitals” for the past 26 years. In 2022, it ranked second statewide. The Emergency Department is the busiest center in Michigan with an annual volume approaching 120,000 visits. It has had an EM residency program for 30+ years and has Emergency Geriatric, Pediatric, Ultrasound and Medical Education fellowships. In 2021, ED faculty published 50+ papers; extramural support totaled over $550,000. MD or DO (PA 1979)
Email: kimberly.andrews@beaumont.org
Website: https://providers.beaumont.org/physician-resources/ physician-careers
MayJun, JulAug, SepOct
MISSOURI
Centerpoint Medical Center is seeking an Emergency Medicine Program Director for their new residency program in Independence, Missouri. Qualified Candidates: - Board certified in emergency medicine with a minimum of three years’ experience - Previous experience as an Associate Program Director, Core Faculty member, or Department Chair is requiredAvailable to begin work in spring 2023 - Ability to obtain Missouri licensure - Excellent interpersonal and communication skills Duties and Responsibilities: - Work on obtaining initial ACGME accreditation through submission of application. - Recruit and select candidates for the residency program through the National Residency Matching Program. - Provide accurate statistical and narrative information in accordance with the requirements of the ACGME and the ACGME’s Review Committee for Emergency Medicine. - Maintain current knowledge of the accreditation and
operational requirements of the residency program, including monitoring current trends and anticipating changes. - Assure that faculty meet research and scholarly activity requirements of the program. Incentive/Benefits Package: - Competitive W2 compensation - Robust benefits include medical, dental, vision and 401k - A-rated professional liability insurance (PA 1947)
Email: amie.murphy@hcahealthcare.com
Website: https://careers.hcahealthcare.com/jobs/10681698emergency-medicine-residency-founding-program-directoropportunity-in-independence-missouri
JanFeb, MarApr, MayJun
NEW HAMPSHIRE
Dartmouth Health and The Geisel School of Medicine at Dartmouth are pleased to announce a national search for the Chair of the Department of Emergency Medicine. This is an opportunity to lead an exceptional clinical department known nationally for providing outstanding patient care, fostering the medical and biomedical education of the next generation, and supporting innovative research. In this leadership role, the Chair of the Department of Emergency Medicine will have primary responsibility and accountability for the overall direction, operation, and management of the Department in accordance with the mission and goals of Dartmouth Health and The Geisel School of Medicine at Dartmouth. Qualified candidates will: hold a medical degree (MD, MD/MPH, MD/MBA, MD/PhD) or equivalent degree(s); qualify for rank of Professor or Associate Professor at the Geisel School of Medicine; be American board certified; and be a New Hampshire licensed physician or should be eligible for licensure in the state of New Hampshire. The preferred candidate will have five or more years of experience as a strategic leader with the ability to manage a substantial, complex, and evolving organization. All application material should be submitted to: Elizabeth Homsy Senior Associate, Healthcare Practice Korn Ferry elizabeth.homsy@kornferry. com Dartmouth Health is an equal opportunity employer, and all qualified applicants will receive consideration for employment without regard to race, color, religion, sex, national origin, disability status, veteran status, gender identity or expression, or any other characteristic protected by law. (PA 1966)
Email: elizabeth.homsy@kornferry.com
Website: https://www.dartmouth-health.org/ MarApr, MayJun, JulAug
None Available at this time. 54
NEW JERSEY
Opportunity: Chairman, Department of Emergency Medicine, Capital Health Systems Licensing and Education Requirements: • Board certified in Emergency Medicine • 5-10 years of clinical experience (preferred) • 5 years of group leadership (preferred) Responsibilities for this position include, but are not limited to:
1. Provider Management: a. Manage recruitment and retention of provider staff b. Maintain regular reviews and evaluations of providers c. Interview provider candidates d. Participate in on-boarding of new providers to ensure they have a full understanding of operational procedures e. Monitor the overtime rate of providers across the system to ensure department goals are achieved f. Create routine schedule, call schedule, and staffing models for the Capital Health Emergency Department
2. Clinical Workflow & Operations: a. Be accountable for the optimal operating efficiency of staff and develop/maintain a patient-centered approach to clinical care b. Develop and maintain a process to review note closure rates and plan to mitigate deficiencies across the system c. Meet with Utilization Review and Medical team leadership to identify opportunities for proper bed assignment and level of care d. Lead the ED Operations, ED leadership and ED Documentation meetings. Participate in other required meetings such as OBS Operations and CHMG Inpatient Operations e. Assist with implementation of Surge management f. Analyze metrics and review analysis with Senior Capital leaders g. Review clinical variation of practice and promote best practices h. Provide new disease management oversight i. Work in conjunction with emergency management systems to ensure emergency preparedness 3. Quality a. Keep abreast of local, regional and national trends in science and education as related to emergency medicine and communicate this information to staff, faculty and administration b. Liaison to committees such as Sepsis, AMI/CPC, stroke accreditation and Patient Satisfaction, Neuro Operations, Resuscitation, Maternal/ child, and Radiology c. Appoint committees and leadership roles as needed to further the goals and functions of the Department d. Address reported safety events, participate in adverse event review, and work directly with providers to ensure continued performance improvement 4. Residency a. Teaching b. Oversee development in conjunction with the Residency Director (PA 1959)
Email: apatel@capitalhealth.org
Website: https://www.capitalhealth.org/ MarApr, MayJun, JulAug
NEW YORK
Chair of the Department of Emergency Medicine at Glen Cove Hospital Glen Cove Hospital is a 216-bed community hospital with the resources to care for all types of patients. Glen Cove has a very supportive and pro-emergency medicine administration as well as a new ICU, CCU, Telemetry, and Brain Injury Unit. We also have a very active and supportive hospitalist program. As Emergency Medicine Chair, you’ll have complete operational and clinical oversight of the department. You’ll collaborate with our experienced service line leadership team in efforts such as recruiting, finance, business development, and more. You’ll also have the incredible opportunity to work with other healthcare professionals across Northwell Health’s extensive integrated network. Glen Cove Hospital has a full-service Emergency Medicine department. Some highlights include: • Approximately 20,000 annual visits • ED consists of 22 private rooms and 4 trauma/critical care beds • 18 ICU/CCU beds • Press Ganey Guardian of Excellence Award 2022 for patient experience • Our Geriatric Emergency Department has a Level 1 Accreditation from ACEP • Designated Primary Stroke Center by The Joint Commission • AHA/ASA Get with the Guidelines Stroke Gold Plus with Honor Roll Plus Award • ACEP Accreditation Bronze Level for PACED (Pain & Addiction Care in the ED) Submit your CV to: adaily@northwell.edu In addition to the listed responsibilities, this leader will promote a positive and inclusive organizational culture, play an essential role in creating and executing team member engagement initiatives, and champion and advance diversity, equity, and inclusion as central to the organization and its values system. (PA 1981)
Email: ppenso@northwell.edu
Website: https://jobs.northwell.edu/career-specialties/physicians/ MayJun, JulAug, SepOct
NORTH CAROLINA
Emergency Medicine – Site Medical Director (MD/DO) Wake Forest Emergency Providers We are seeking candidates with proven experience in leadership and clinical practice. This is a unique opportunity to lead a dynamic Emergency Medicine team with the support and backing of a large, regional, nonprofit, academic health system. In addition to practicing clinically, the selected candidate will also provide leadership in staffing, financial management, performance improvement, and quality and safety initiatives for their site. We offer a highly innovative model wherein our physicians have tremendous influence in their practice. This includes access to transparent financials and performance metrics and the ability to influence practice plans. With a lean administrative model and responsible staffing, our physicians have abundant resources at their disposal to improve outcomes for patients and lead care innovations. While our Medical Directors have autonomy to manage their sites, they also enjoy great collaboration and support with experienced peers, a strong Regional Director and a supportive President. This is an employed position with Wake Forest Emergency Providers About Wake Forest Emergency Providers Affiliated with Atrium Health Wake Forest Baptist (www.wakehealth.edu), Wake Forest Emergency Providers is a nationally recognized, 501c3 non-profit, proudly providing health care for all! We are contracted with select, partner organizations to provide staffing for Hospital Emergency Departments, Free Standing Emergency Departments, and Urgent Cares throughout the North Central and Northwest regions of North Carolina. Location Outdoor activities abound in the area with unrivaled hiking, road/gravel/ mountain biking, fly fishing, kayaking/rafting and rock climbing easily accessible. Public schools are among the top ranked in the state and the community is close-knit and supportive. Position Requirements: • Qualified Candidates must be Board Certified (or eligible) by the American Board of Emergency Medicine or equivalent, and licensed (or eligible) to practice medicine in the state of North Carolina. What We Believe When you join Wake Forest Emergency Providers, you will be welcomed into an inclusive culture that celebrates and respects the contributions a diverse team can make together. Practice where your voice is valued, your passion for advancing medicine is rewarded, and you get the resources and support you need to thrive personally and professionally. In our organization, you can work alongside the most advanced minds in medicine to improve medicine, elevate hope and advance healing—for all. Interested Candidates May Contact: Scott Dudley Atrium Health Wake Forest Baptist - Provider Recruitment 336-341-2631 sdudley@ wakehealth.edu (PA 1969)
Email: sdudley@wakehealth.edu
Website: http://www.wakehealth.edu
AprMar, MayJun, JulAug
NORTH CAROLINA
Duke Pediatrics is recruiting for a faculty member to join the Division of Pediatric Emergency Medicine. Duke Children’s is ranked among the nation’s finest for pediatric care and is #1 in NIH funding for pediatric clinical science departments. Ideal candidates will possess excellent clinical skills, a passion for education, and a demonstrated record of scholarly contributions. The Greater Triangle area of Raleigh, Durham and Chapel Hill is culturally diverse, economically resilient and nationally recognized as a great place to live and work. Interested candidates should submit CV and Letter of Interest via https:// pdc.dukehealth.org/physician-jobs (PA 1958)
Email: sherrod.basnight@duke.edu
Website: https://pdc.dukehealth.org/physician-jobs
MarApr, MayJun, JulAug
VERMONT
The Department of Emergency Medicine at The Larner College of Medicine (LCOM) at The University of Vermont (UVM) is seeking an Emergency Medicine Physician to fill the role of Associate Professor or Professor in the Clinical Scholar Pathway, commensurate with years of experience and accomplishments. The physician identified in this search will be provided the opportunity to serve as the Vice Chair of Academic Affairs (VCAA) of the Department of Emergency Medicine. The Department of EM provides clinical coverage at the seven clinical campuses of the University of Vermont Health Network in Vermont and upstate New York. Fifty academic faculty in the Department work with colleagues in community clinical practice to serve approximately 200,000 patient visits annually, and the Network hospitals serve a catchment of 40,000 square miles and 1.4M people. LCOM students and Emergency Medicine
residents train clinically in three of the network sites with elective rotations in multiple other sites. Our primary teaching campus is the University of Vermont Medical Center, the only level 1 trauma center in the greater region. The majority of academic faculty provide clinical coverage at multiple sites in Network, including our rural and critical access sites, underscoring our commitment to high quality rural acute care delivery. The Vice Chair of Academic Affairs (VCAA) will lead advancement of the academic components of the mission of the Department of EM. The VCAA will mentor faculty, fellows, and residents in their academic efforts and will lead the Promotions and Tenure Committee in advising the Chair on readiness for promotion. Recruitment and retention of faculty, fellows, and residents with a commitment to diversity, equity, and inclusion will remain a top priority. The VCAA will collaborate with colleagues locally at LCOM and nationally through organizations such as AAEM, SAEM, CORD, and the AAMC, providing networking opportunities, enhancing mentorship, incorporating innovative educational practices, and fostering faculty development. The VCAA will be provided with 30% nonclinical time to achieve the roles and responsibilities across the following domains: · Leadership and Strategic Planning · Faculty Development & Mentorship · Faculty Evaluation and Feedback · Diversity, Equity, and Inclusion · Faculty Recruitment, Retention, and Wellness · Scholarship Although all interested candidates are encouraged to apply, strong preference will be given to candidates with leadership experience in the educational, clinical, and research activities of academic emergency medicine. Consistent with all recruitments, we seek candidates that demonstrate empathy, humanism, and humility, and candidates must be comfortable with an environment that employs transparency to create faculty and leadership accountability. Candidates must commit to our core values of Professionalism at the Larner College of Medicine and are advised to review our Statement on Professionalism. Interested individuals should apply online at https://www.uvmjobs.com/postings/58864 (position number 00026358). Confidential inquiries to acquire further information about this position may be directed to Dr. Ramsey Herrington, Chair of the Department of Emergency Medicine at ramsey. herrington@uvmhealth.org (PA 1962)
Email: Ramsey.herrington@uvmhealth.org
Website: https://www.uvmjobs.com/postings/58864
MarApr, MayJun, JulAug
WEST VIRGINIA
The Department of Emergency Medicine at Charleston Area Medical Center is recruiting a pediatric emergency medicine physician to work at Women and Children’s Hospital located in Charleston, WV. This 120-bed dedicated Women and Children’s Hospital is a part of a large university-affiliated regional referral center with a drawing population of 562,000. We have in-house Neonatologist with 24/7 coverage in Level III NICU as well as a PICU with pediatric intensivists. Charleston Area Medical Center also sponsors an ACGME accredited emergency medicine residency program with 20 residents at present. Position Requirements: • MD or DO degree from an accredited university medical school • Completion of an Emergency Medicine Residency and a Pediatric Emergency Medicine Fellowship or completion of a Pediatric Residency and a Pediatric Emergency Medicine Fellowship • Board Certification or Board Eligible (ABEM or AOBEM) in Pediatric Emergency Medicine • Ability to achieve full and unrestricted hospitalist privileges at Charleston Area Medical Center • Eligibility for a West Virginia Medical License Benefits include: • Excellent benefits package • Competitive compensation • Affordable community • Extraordinary family environment • Unsurpassed recreational activities • Outstanding school systems About Charleston, West Virginia Charleston is the state capital and largest city in the state. We are proud of our diverse population, amazing outdoor activities, and excellent schools. We are centrally located to numerous major metropolitan areas in North Carolina, Ohio, Pennsylvania, Virginia and Washington, DC, and Yeager International Airport is just 5 miles from the hospital. In addition, Charleston offers a Downtown district filled with eclectic galleries, chic boutiques, and unique restaurants. The area boasts a vibrant academic and professional community that offers a balanced professional career and a fulfilling personal lifestyle. Come see what our community can offer you! (PA 1955)
Email: carol.wamsley@camc.org
Website: http://www.camc.org
MarApr, MayJun, JulAug
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
COMMON SENSE MAY/JUNE 2023 55
(Below are hospitals, non-profit or medical school employed positions.)
SECTION II: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA, CONTINUED
(Below are hospitals, non-profit or medical school employed positions.)
WEST VIRGINIA
The Charleston Area Medical Center Institute for Academic Medicine is seeking Emergency Medicine clinicians for academic positions as Core Faculty and Clinical Core Faculty. This regional, tertiary medical center sponsors an ACGME accredited emergency medicine residency program with 20 residents at present. Serving a multi-county area, the four Emergency Departments see over 130,000 patients per year and the following locations: CAMC Memorial Hospital - 30 beds with
4 assessment beds CAMC General Hospital – Level 1 Trauma Center with 26 beds and additional fast flow areas CAMC Teays Valley Hospital – 10 beds with 2 assessment beds CAMC Women and Children’s Hospital – 20 beds · Mid-level coverage
all sites · 24/7 Hospitalists Coverage · Complete specialty and surgical support · Strong Administrative Support (PA 1989)
Email: ryan.nagy@vandaliahealth.org
Website: https://www.camc.org/ MayJun, JulAug, SepOct
SECTION III: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
(Below are military/government employed positions.)
None Available at this time.
SECTION IV: POSITIONS NOT RECOGNIZED AS BEING IN FULL COMPLIANCE WITH AAEM’S JOB BANK ADVERTISING CRITERIA
FLORIDA
International Emergency Medicine Fellowship Opening at Global Physician Network, at Sarasota Memorial Health Care System, Sarasota, Florida A two (2) Year Fellowship Track Position for an ACGME Accredited Emergency Medicine Board Eligible / Board Certified Attending who will accomplish the Fellowship with a Fully Funded International Project Based Field Experience, MBA in Project Management, and Certification in Crisis Leadership. Located in Sarasota the Fellowship is home to the Florida State University College of Medicine Emergency Medicine Residency Program. Please contact forwarding a statement of interest and your curriculum vitae. Dr. Sagar Galwankar, International Emergency Medicine Fellowship Director Email: gcsagar@ yahoo.com (PA 1968)
Email: gcsagar@yahoo.com
Website: https://www.globalphysiciannetwork.com/ MarApr, MayJun, JulAug
FLORIDA
Join a democratic group in Cape Coral, FL established since 1985, partnered with Lee Health. An annual volume of 70k at a single community hospital site. Competitive pay and top-notch benefits including CME reimbursement, medical, 401k. Equal shift distribution averaging 14 shifts per month, 8-10 hours each, with only a few overnight shifts annually. Patient load of 1.5-2 per hour, with 24-hour physician and APP coverage. Epic with Dragon dictation. Opportunity to teach residents due to a new internal medicine residency. Enjoy a sunny coastal location, perfect for outdoor enthusiasts and families. (PA 1976) Email: tylerensley@gmail.com
Website: https://capecoralemergencyphysicians.com/ MayJun, JulAug, SepOct
MINNESOTA
Join Emergency Physicians Professional Association (EPPA)! -a physician-owned, independent, democratic group of over 220 physicians staffing multiple facilities throughout Minnesota. Currently staffing 7 Twin Cities metro hospitals, 1 central MN hospital, 5 regional/rural sites, and 3 Urgency Rooms. Patient volumes 9K-75K per year. Immediate openings for BC/BE, Emergency Medicine residency trained physicians in the St. Cloud, Wilmar, and Monticello, MN areas with significant financial advantages (Shareholder buy-in is waived). Shifts range from 8 hours (metro) to 12 hours (rural). Sites include Level 1-4 trauma centers in multiple hospital systems. EPIC EMR at all sites. Variable workload based on site, ranging from 1.2-2 patients per hour. W2 with multiple benefits: malpractice, health, dental, life, disability, personal umbrella insurance; 401k, pension and profit sharing. Competitive compensation for full-time contract (1600 hours/year) with average RVU productivity. Shareholder/ Ownership track available. Night, weekend, and holiday differentials. Nocturnist positions possible. (PA 1965)
Email: bleagjeld@eppahealth.com
Website: https://www.eppahealth.com
MarApr, MayJun, JulAug
NEW YORK
CityMD is a network of urgent care centers dedicated to setting an unprecedented standard of care for our patients and an edifying, intuitive work environment for our employees. We are looking for board-certified Emergency and Family Practice trained physicians who thrive in an environment surrounded by highly trained and motivated individuals and operate on one of the most advanced administrative systems in healthcare today. Your responsibilities will include the diagnosis and treatment of patients of all ages and interpreting and archiving medical information. We are hiring board-certified physicians who are Emergency Medicine or Family Medicine trained to work in our state-of-the-art urgent care centers. Our facilities are staffed with highly trained and motivated individuals who operate one of the most advanced administrative systems in healthcare today. Highlights • Scribes on staff. This allows you to focus your time on direct patient care. • Advanced imaging available on a routine and STAT basis, including CT, US and MRI. • Specialist consultation allows for 48 hour turn around and same day results for urgent cases. • State-of-the-art facilities, digital X-Ray, laboratory services with modern, clean and aesthetically designed work environments. • Dedicated physician led Aftercare team following up on all aspects of patient care.
• Integrated Electronic Medical Records across all CityMD locations. Our commitment to our patients and employees, along with our state-of-the-art personalized healthcare delivery system, has taken CityMD from one location on the Upper East Side to over 130 in the New York/New Jersey area including Northern/Central/Southern New Jersey and Manhattan, Brooklyn, Queens, Long Island, Rockland, and Westchester County. As a proud “People First” company, we are centered on the values of integrity, excellence, professionalism, and quality. Our Compensation package is broken down as follows:
• Competitive hourly rate plus performance-based bonus • 4 weeks of paid time off • $3000 annually in CME • 401K match is up to 4% of your bi-weekly pay up to annual IRS limits • Full medical, dental and vision benefits, as well as short term and long term disability benefits and company paid life insurance • Medical Professional Liability Insurance Covered • Holiday Pay & Extended Hour Site Differentials up to $45/hour on top of base • $120 - $185 per hour The provided compensation range is based on industry standards and salary determinations will be made based on numerous factors including but not limited to years of experience, individual performance, quality measures and location of position. (PA 1961)
Email: slameira@summithealth.com
Website: http://www.citymd.com MarApr, MayJun, JulAug
NORTH CAROLINA
More than 40 years strong, ECEP II, P. A. is seeking a full-time emergency medicine physician for our emergency medicine group serving the greater Wilmington, NC area. Our full-time physicians practice an average of 28 to 30 hours per week. Wilmington practice sites include New Hanover Regional Medical Center, a level II trauma center, treating an annual patient volume of 75,000, Orthopedic Hospital, a community hospital with an annual patient volume of 27,000, and Scotts Hill Emergency Department, a full-service standalone emergency department with an annual patient volume of 34,000. Our group also practices at Pender Memorial Hospital in Burgaw, a community hospital located just 25 minutes north of Wilmington with an annual patient volume of 17,000. ECEP offers competitive pay and an excellent benefits package. Live, practice and enjoy a great quality of life in an exceptional coastal community with beaches, golf, and a historic waterfront at your doorstep. (PA 1984)
Email: kskaggs@ecepnet.com
MayJun, JulAug, SepOct
TENNESSEE
Middle TN Emergency Physicians is a private, physician owned democratic group staffing seven hospitals of the Ascension St. Thomas Health system in middle Tennessee. After over 35 years staffing the core urban hospitals of Saint Thomas, the two premier private democratic emergency groups in the area merged with a shared vision of providing the highest quality emergency care in the dynamic middle Tennessee area centered around Nashville. Our success offered the ability to expand our vision to the four regional facilities further advancing opportunities for emergency physicians in the area. We are currently seeking motivated BC/ BE physicians to serve as independent contractors at the St. Thomas River Park, St. Thomas DeKalb, St. Thomas Highlands, St. Thomas Stones River and St. Thomas Westlawn hospitals. Highly competitive pay is commensurate with volume at each individual facility with a bonus of no state income tax. Send CV to MTEPJobs@gmail.com. (PA 1948)
Email: brad.w.russell@gmail.com
JanFeb, MarApr, MayJun
WASHINGTON
Emergency Physicians of Mason County are recruiting to add 1-2 partners to our LLC. We are an independent democratic group that staff a rural critical access hospital in the south Puget Sound. We have held the contract for over 30 years. Mason General Hospital in Shelton, Washington has an ED that sees approximately 20k patients a year. We have three daily shifts, 1112 hours each. No midlevels, and everyone is ABEM certified. 13 Bed ED. Excellent nursing coverage, often with 5 RN’s. General surgery and OB/GYN backup. Benefits: Competitive salary, malpractice paid by hospital (occurrence), 401-K, group health plan. Beautiful place to live. 1 hour or less from Olympic National Park. 2 hours to skiing. 2 hours from Seattle and Portland. Email rgbelville @ runbox.com. (PA 1982)
Email: rgbelville@runbox.com
MayJun, JulAug, SepOct
(Below are independent contractor positions.)
COMMON SENSE MAY/JUNE 2023 56
COMMON SENSE MAY/JUNE 2023 57
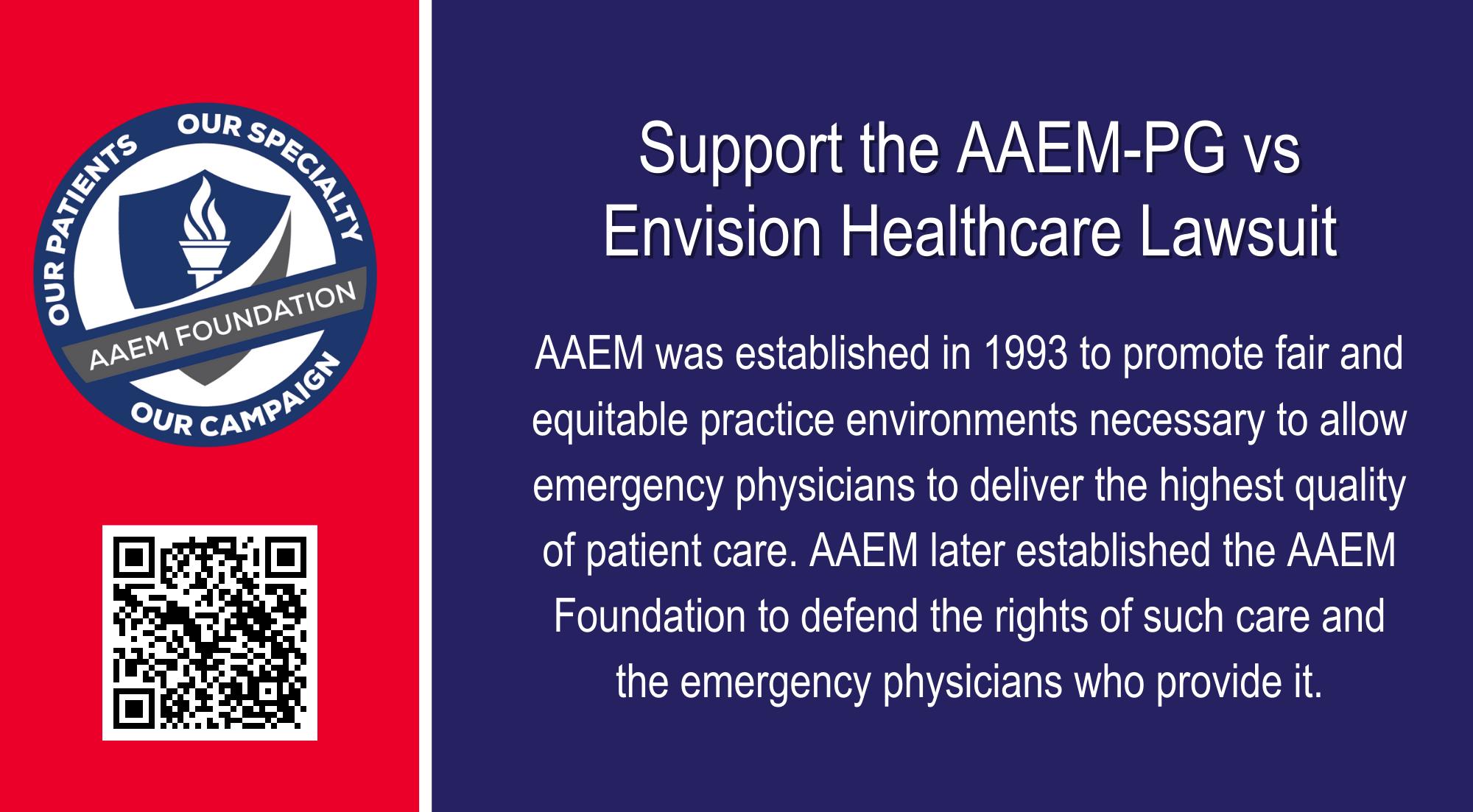
555 East Wells Street / Suite 1100 Milwaukee, WI 53202-3823 PRSRT STD U.S. POSTAGE PAID MILWAUKEE, WI PERMIT NO. 0188
COMMONSENSE














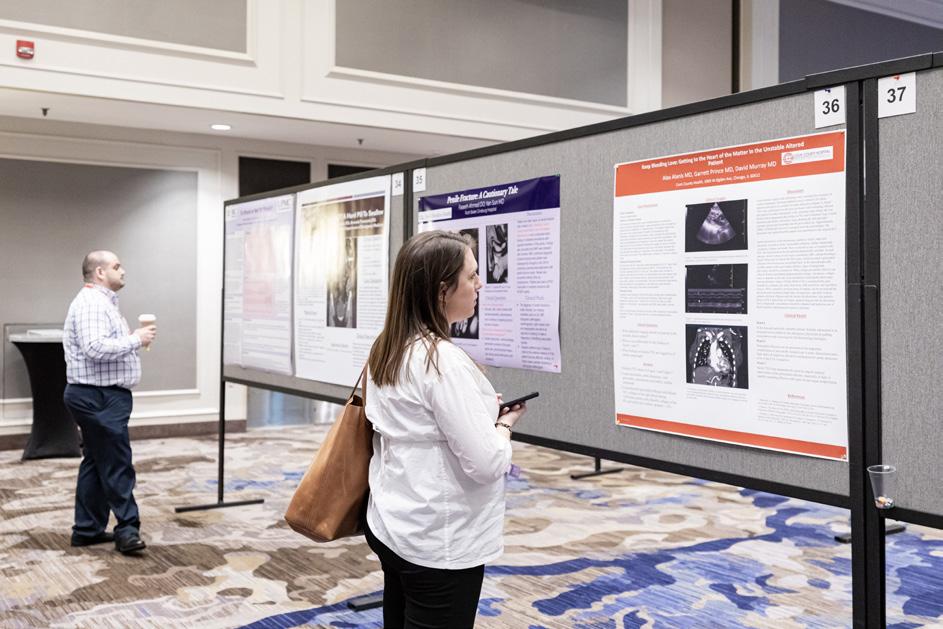









 Andrew Mayer, MD FAAEM
Andrew Mayer, MD FAAEM
























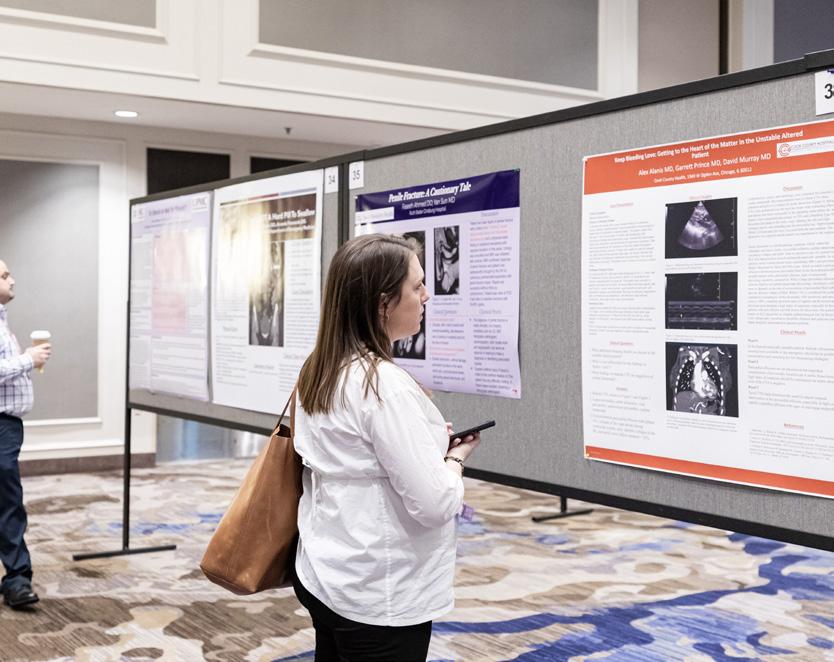










































































































































 Jordan Vaughn, MD Kristin Fontes, MD FAAEM
Kendall Moore, MD FAAEM
Valerie Pierre, MD FAAEM
Jordan Vaughn, MD Kristin Fontes, MD FAAEM
Kendall Moore, MD FAAEM
Valerie Pierre, MD FAAEM













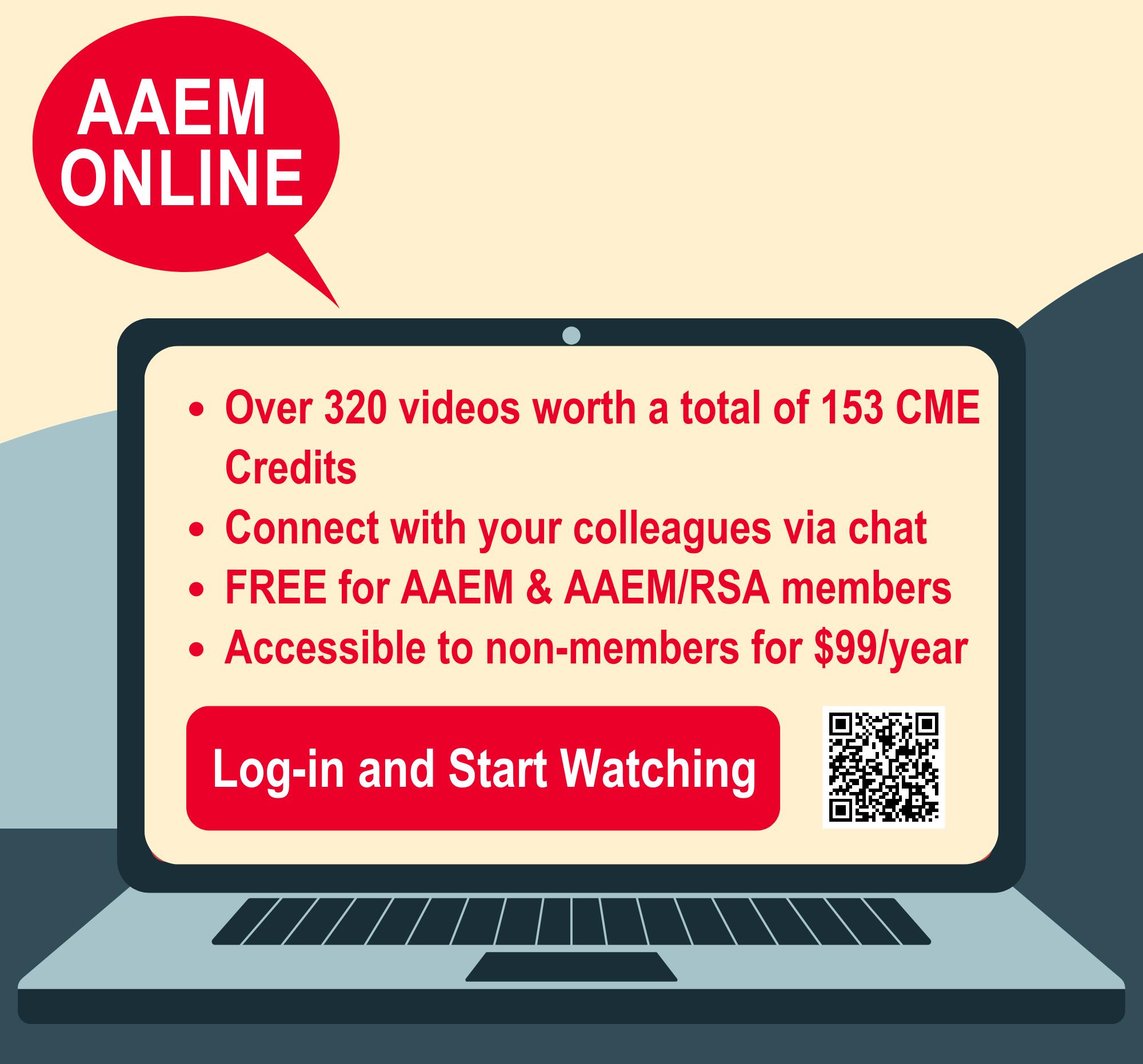


 Neha Bhatnagar, MD FAAEM FPD in US and Shawn Sethi, DO FAAEM
Neha Bhatnagar, MD FAAEM FPD in US and Shawn Sethi, DO FAAEM






 Brenda Arthur, MD* and Jada Watts, BS †
Brenda Arthur, MD* and Jada Watts, BS †







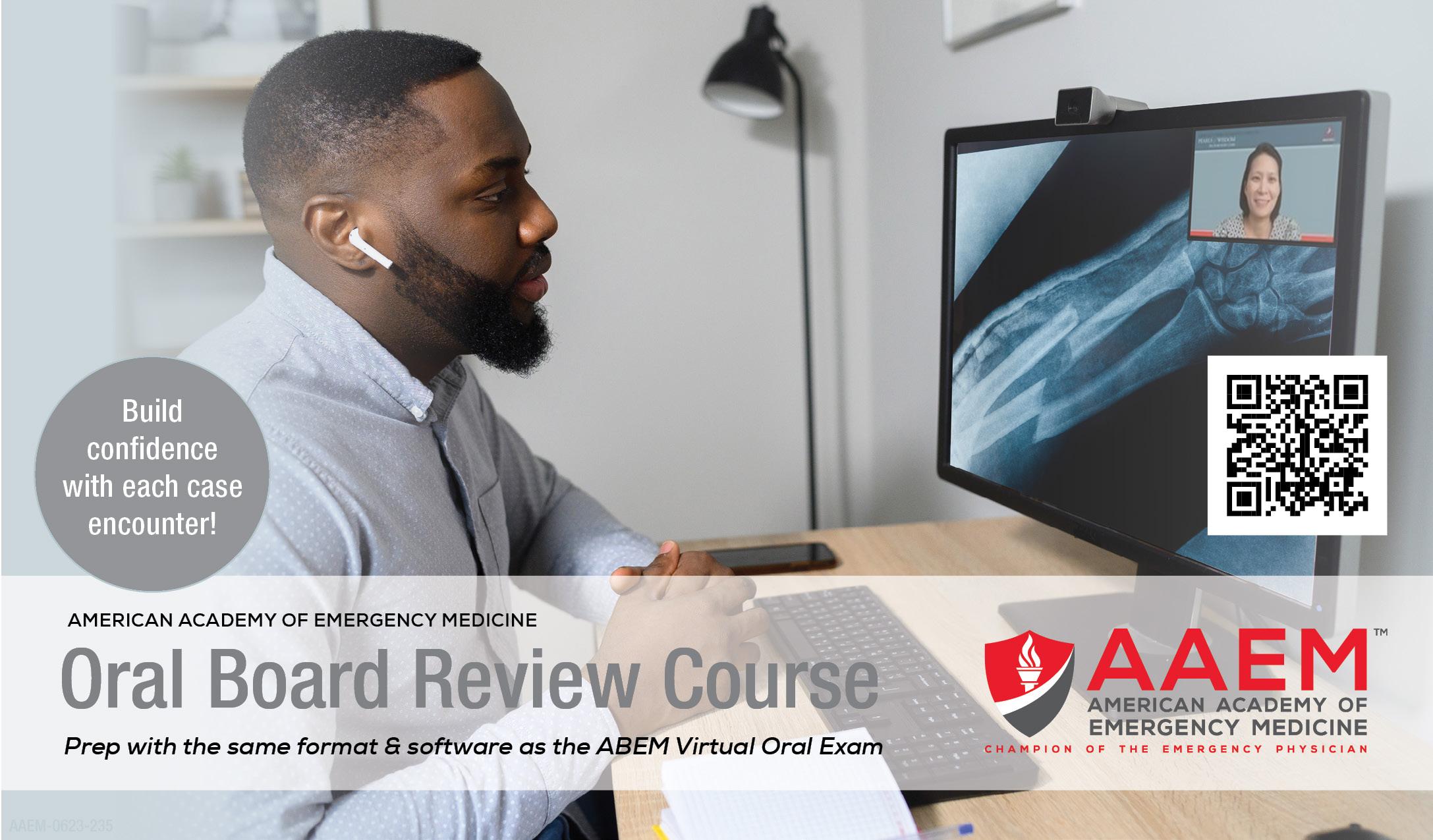













 Shea McGrinder, MS3
Shea McGrinder, MS3