Designing Mental, Behavioral and Specialized HEALTHCARE FACILITIES

Delivering Solutions for Success
Vanir’s experience in the healthcare field goes back to the mid-1980s when we were awarded a contract with the California Department of Mental Health to manage more than $180 million in fire, life and safety improvements at five of its hospitals—a program that quickly grew to more than $500 million.
As a national leader in program, project and construction management and real estate development, Vanir has ranked as a top PMCM firm by Engineering News-Record for more than three decades. Serving markets throughout Arizona, California, Colorado, Georgia, Illinois, Texas and Washington, we have delivered $30.8 billion in construction value to hundreds of clients nationwide. Throughout every phase of planning, design, construction and start-up, our specialized teams will work with you to address your unique needs in an ethical, creative and cost-effective manner.






A/E/C
Architectural, engineering, interiors and design firm
Spiezle Architectural Group Inc. announced the addition of Associate Principal Damian Huneycutt, AIA, ACHA.
Based in the firm’s Charlotte, N.C., office, Huneycutt brings more than 20 years of healthcare design experience, guiding complex projects from concept to completion while exploring construction innovation, prefabrication strategies and alternative delivery methods. Huneycutt is certified by the American College of Healthcare Architects (ACHA) for his specialized experience and knowledge, and his commitment to transforming healthcare through better built environments. He holds a Bachelor of Arts in architecture and Bachelor of Architecture with a focus on daylighting design from the University of North Carolina at Charlotte. He is a member of the National Council of Architectural Registration Boards and the American College of Healthcare Architects.

shaping academic health sciences environments, White brings a visionary approach to designing immersive, future-ready learning spaces that bridge pedagogy and practice. Her work supports advancement across campuses nationwide in allied health, nursing and dental programs. Through high-fidelity simulation labs, interprofessional education hubs and advanced training spaces, she helps institutions reimagine student engagement with real-world clinical scenarios. White’s portfolio includes work with leading colleges and universities across the country, where she has helped develop strategic frameworks for interdisciplinary health education facilities. Prior to joining Kahler Slater, she led the Health Sciences market at Ayers Saint Gross.
specialty walls, and exterior metal solutions, has acquired Geometrik Manufacturing Inc. Based in Kelowna, British Columbia, Geometrik is a leading Canadian designer and manufacturer of wood acoustical ceiling and wall systems made from multiple wood species. Geometrik has built a broad portfolio of wood ceiling and specialty wall solutions using a variety of wood species along with various stains, perforations, shapes and sizes. The company currently offers nine different wood products across several types of acoustical ceiling and wall systems and a curated palette of 12 standard and custom wood finishes. These offerings bring a wide range of Western Hemlock solutions to Armstrong’s Architectural Specialties portfolio.


DesignGroup announced the appointment of Travis Tyson, AIA, ACHA, NCARB, as Principal and Healthcare Market Leader. Tyson brings nearly two decades of experience from Cleveland Clinic, where he most recently served as director of the Healthcare Design Studio, overseeing hundreds of projects ranging from small renovations to major new hospital construction. Tyson will build upon DesignGroup’s 53-year legacy in healthcare design with a focus on strengthening existing client relationships and forging new connections across the Midwest. Tyson’s tenure at the Cleveland Clinic included leadership roles on notable projects, including the Avon Hospital and Richard E. Jacobs Health Center and the Mentor Hospital, designed as a highly efficient, modular facility that could be replicated across multiple sites. He also spearheaded the development of enterprise-wide design standards for the Cleveland Clinic, ensuring consistent branding and functionality across the renowned health system.
Kahler Slater, an awardwinning international architecture, interior design, environmental branding and strategic advisory firm, announced the addition of Laura White, AIA, LEED AP, WELL AP as Academic Health Sciences Program Strategist and Associate Principal. With experience
CALENDAR

Global design firm HKS announced that Brian Zeallear, AIA, DBIA, NCARB, has joined the firm as a Principal and Health Studio Practice Leader. Based in the firm’s Seattle office, Zeallear brings three decades of experience leading complex healthcare projects and building high-performing teams across the West Coast and internationally. A recognized leader in healthcare design, Zeallear is known for his servant-leadership style and deep commitment to human-centered architecture. Throughout his career, he has championed design strategies that not only support operational excellence but also promote healing, connection and community wellbeing. As Studio Practice Leader, Zeallear will focus on growing HKS’ health practice in the Pacific Northwest and collaborating with firmwide leaders to drive innovation and deliver meaningful outcomes for health systems, providers and patients.
COMPANY NEWS
Yellow Brick Consulting has joined CannonDesign’s consulting platform, further strengthening the firm’s ability to drive impact for the nation’s leading healthcare organizations. This acquisition bolsters CannonDesign’s growing suite of consulting services and, together with the expertise of Blue Cottage of CannonDesign, establishes the largest and most experienced healthcare transition and activation consulting team in North America. Moving forward, Yellow Brick will retain its name and remain focused on bringing its renowned clinical expertise and services to clients globally. Kelly Guzman, Yellow Brick founder and CEO, will continue to lead the nearly 70-person transition and activation team. Since 2018, Yellow Brick has built a portfolio in transition and activation planning. Together, the team has guided hundreds of health systems through every phase of activation for new or renovated facilities. From early planning through construction, staff preparation, patient safety protocols and a seamless transition into fully operational healthcare environments, Guzman and her team have championed industry standards and knowledge sharing.

Apogee Architectural Metals has named Brandon Ellison as a Regional Sales Manager responsible for four independent sales agencies in the Southeast that represent EFCO, Tubelite and Wausau Window brand products. Previously, Ellison worked as part of the EFCO direct projects team before joining Advanced Window Inc., in Frederick, Md., where he most recently worked as a senior project manager. With 11 years of industry experience, he is known for his strong client relationships and problem-solving skills. Ellison earned an master’s degree in business administration with an emphasis in project management from Missouri State University.
Armstrong World Industries Inc., a leader in the design and manufacture of innovative interior and exterior architectural applications including ceilings,
Architecture and engineering firm Goodwyn Mills Cawood (GMC) is expanding its healthcare expertise through the strategic acquisition of Cassetty Architects in Nashville, Tenn. Founded in 1998 by Clint Cassetty, the firm specializes in healthcare architecture, having worked in hospital systems and healthcare corporations throughout the country. Bringing Cassetty on board fortifies GMC’s healthcare architecture team and enhances the firm’s expertise in the market. GMC’s in-house services include architecture, interior design, civil engineering, environmental services, landscape architecture, planning, transportation engineering, coastal engineering, geotechnical engineering, mechanical, electrical and plumbing engineering and disaster recovery. GMC is currently working on several significant healthcare projects throughout the Southeast, including a new surgery and bed tower expansion at Health First Palm Bay Hospital in Palm Bay, Florida, an emergency department and bed tower expansion at Southeast Health in Dothan, Alabama. Recent notable projects designed by the Cassetty Architects team include the Advanced Surgery Center of Sarasota, Fla., and the Orlando Ophthalmology Surgery Center. The Cassetty team has relocated to GMC’s Nashville office located in West End.
Association of Medical Facility Professionals Healthcare Design Conference + Expo
Oct. 25-28 | Kansas City
National Conference on Correctional Health Care 2025
Nov. 1-5 | Baltimore
Next Generation Patient Experience Conference Nov. 17-19 | Palm Springs, Calif.
Smart Healthcare Facilities Convention 2025
Nov. 19-21 | Miami
Rensa Filtration, a manufacturer and distributor of consumable, mission-critical air filtration products, has acquired IREMA-Filter GmbH of Germany and its U.S. subsidiary Aeolus Filter Corporation. IREMA is an innovator in filtration media and pleating technologies. Its U.S. subsidiary, Aeolus Filter, provides filters using IREMA’s advanced media platforms for critical applications in healthcare and data centers. Together, the companies bring decades of expertise in microfiber and nanofiber depth loading media that enhance dust-holding capacity, energy efficiency and filter service life.
Spotlight a person by contacting us at hco@wmhmedia.com
Huneycutt
White
Tyson
Zeallear
Ellison

Spotlighting Mental and Behavioral Healthcare Facilities
Welcome to the 2025 Annual Issue of Healthcare Construction + Operations News. This extended digital issue showcases the incredible work happening in an important and growing sector of the healthcare industry: mental health and behavioral healthcare.
The need for these specialized spaces is clear. Ninety percent of U.S. adults believe that the country is experiencing a mental health crisis. Data from the Substance Abuse and Mental Health Services Administration found that 1 in 5 adults, adolescents and youth experienced a behavioral health issue between 2019 and 2020, and in many communities, there are not enough healthcare facilities or beds equipped to support this urgent need.
However, the passion to better serve people experienceing mental and behavioral health challenges — and to invest in modern, safe and patient-centered spaces — is evident. Healthcare providers are partnering with design, construction, technology and manufacturing professionals to bring innovative projects to life, while technology is filling critical safety, security, capacity and access gaps. For example, flip to page 15 to learn how Bicycle Health is changing opioid recovery though virtual care — or turn to page 16 to see how Santa Clara’s new Child, Adolescent and Adult Behavioral Health Services Center prioritizes patients’ humanity while ensuring staff feel safe and supported. Additionally, HCO News was proud to join manufacturer Construction Specialties in recognizing an outstanding new healthcare facility, the University of Washington Medicine’s Center for Behavioral Health, which you can learn more about below.
These efforts represent just a sliver of the groundbreaking projects and solutions that are in development across the country, so watch the HCO News website for weekly coverage on projects, products and progress. While addressing the country’s mental and behavioral health challenges won’t happen overnight, investing in forward-thinking facilities, technologies and ideas will all move the needle toward building healthcare systems equipped to meet patient needs and help communities thrive.
Lindsey Coulter, Editorial Director
Construction Specialties, HCO News Honor Healthcare Excellence
The University of Washington Medicine’s Center for Behavioral Health and Learning is designed to foster hope and healing
By Lindsey Coulter
Healthcare Construction + Operations News was proud to partner with Construction Specialties — a provider of architectural louvers, screens, doors, flooring, expansion joints, privacy curtains and wall protection — to shine a spotlight on healthcare facilities that are committed to excellence in service and patient care.
To show appreciation for the work of these critical facilities, Construction Specialties sponsored the recent Healthcare Spaces Design Contest, which drew nominations of outstanding hospitals, clinics and specialized facilities from across the nation.
And the Winner is...
The University of Washington Medicine’s Center for Behavioral Health and Learning (CBHL) in Seattle!
In appreciation for the life-changing work and unique collaborative mission of the CBHL, Construction Specialties is donating a variety of architectural products to help improve performance, longevity and safety. Construction Specialties will work with the CBHL team to determine how the company’s products can best serve the facility and contribute to a better patient experience.
Inside
the Center for Behavioral Health and Learning
The six-story, 184,000-square-foot facility officially opened in May and includes 150 behavioral healthcare beds serving long-term civil commitment patients, geropsychiatry patients and acute-care medical and surgical patients who also have mental health challenges.

The facility supports a full continuum of behavioral health services: a crisis stabilization unit, modern neuromodulation treatments, transition support to community-based living, and 24/7 telepsychiatry consultation that allows UW experts to consult with primary care, community hospital, and emergency room providers across the state. It also integrates an interdisciplinary training and workforce development program focused on preparing and supporting the next generation of behavioral health providers. The CBHL is the first of its kind to combine mental health care, integrated medical care and workforce training for this much-needed, in-demand specialty practice.
UW Medicine partnered with SRG + CannonDesign to envision the CBHL facility as a fully integrated, welcoming and healing center, and an example of positive transformation for the State of Washington’s entire behavioral health system. According
to the architectural team, the new CBHL is an expansion of the existing hospital, designed with attention to scale, articulation, openness and warmth to reinforce the vision for a new standard of behavioral health care.
“We gave considerable thought to designing rooms that would be conducive to the care and safety of our patients. Our goal was always to create an open and welcoming environment that would not have an institutional look and feel,” said Ryan Kimmel, MD, chief of psychiatry for UW Medical Center.
Here, patients with mental or behavioral health disorders benefit from “whole person” care, including medical conditions or physical illnesses. The center was also designed with in-house medical and surgical spaces to improve partnership and collaboration between specialists and behavioral health experts.
To further improve the patient experience, the facility maximizes access to daylight and views, while assuring privacy, dignity and safety.
University of Washington Medicine’s Center for Behavioral Health and Learning Project Team:
Owner: University of Washington Medicine
Architect: SRG + CannonDesign
General Contractor: Clark|Abbott Joint Venture, Clark Construction Group, Abbott Construction
Glazing Contractor – Behavioral Care
Windows: Benson Industries
Manufacturer – Behavioral Care Windows: Wausau Window and Wall Systems, part of Apogee Enterprises Inc.
Aluminum Finishing Services – Behavioral Care Windows: Linetec, part of Apogee Enterprises Inc.
Supporting the project’s multiple goals, the architectural team selected Wausau 4000iDT Series aluminum-framed, high-performance windows. Engineered for behavioral care settings, these windows withstand high impacts from the interior. This ensures they are suitable for containing patients, restricting their passage to unauthorized areas, or delaying and frustrating escape attempts.
“The design of the building is rooted in the belief that the environment can significantly impact healing. We wanted to create spaces that feel safe, welcoming and uplifting, with plenty of natural light and access to nature. We also aimed to reduce the sense of isolation often felt in mental health facilities and promote a sense of community and support among patients,” said SRG + CannonDesign’s health care practice leader, principal and senior project planner, Lori Epler, AIA.
She added, “While this building is highly specialized, it’s truly remarkable how welcoming and therapeutic it feels. It’s an inspiring space designed to foster hope in patients on their healing journey and to motivate students to reach their full potential as practitioners.”


Construction Specialties will work with the CBHL team to determine how the company’s products can best serve the facility and contribute to a better patient experience.
Photo Credit: Wausau Windows
The CBHL is the first of its kind to combine mental health care, integrated medical care and workforce training for this much-needed, in-demand specialty practice. Photo Credit: CannonDesign
Healthcare Facilities Symposium and Expo Showcases the Latest Innovations in Treatment, Design
By Charlie Lange
Representatives from architecture, construction and engineering firms, healthcare networks and government agencies gathered in San Diego recently for the 38th annual Healthcare Facilities Symposium and Expo.
The event, held Sept. 24–26, featured an array of sessions on the design of mental health and wellness spaces, touching on how biophilic elements, sustainability and functional art can help contribute to healing environments.
Modern Healthcare Architecture
Before considering present and future developments, it’s sometimes necessary to look at the past. Speaker Francis Murdock Pitts, FAIA, FACHA, OAA, a Principal with firm Architecture+, did just that.
Pitts authored a chapter titled “The Architecture of a

Modern Psychiatric Facility” in the latest edition of the book, Redesigning the US Mental Healthcare System. In a presentation at the event, Pitts centered on how the country’s mental healthcare model has been pieced together since “asylum times” and has often failed to meet patient needs.
Pitts also touched on the earliest acknowledgements of environment’s role in mental healthcare and recovery and the emergence of modern design of treatment settings. He mentioned how some large hospital facilities found inspiration from studying the planning of villages and towns and creating common areas where patients can receive care and socialize outside of a strictly clinical setting.
Pitts encouraged the audience to take a humancentered approach to designing facilities “for the person, not the system” and creating environments that encourage healing and change. He also stressed that designers honor the five key pillars of resilience — nutrition, art, social connections, mindfulness and movement — and keep them at the front and center of their design processes.
“How can we make architecture enable human experience, with the understanding that space and form must be accessible, purposeful, resonant and generative?” Pitts asked.
Design for Health: Witnessing a Breakthrough in Prince Edward Island
Barbara Miszkiel and Brian Giebink of HDR, together with Bill Saul of architecture firm SableARC, presented on a new mental health facility project in Prince Edward Island (PEI), Canada.
As Canada’s smallest province, the area was originally a small fishing outpost and has grown into a community
Whitney Fuessel and Hector Covo of design firm HKS, along with Lindsay Davis of Davis Cohen Art Consulting & Appraisal and Carrie Henderson with the Harris Health System, discussed an art program that is part of the ongoing Lyndon B. Johnson Hospital campus expansion project. The hospital is in an urban area, and more than half of its patients are uninsured. The area has also been dubbed a “cancer cluster” as a nearby railroad and industrial sites have contributed to high rates of
“How can we make architecture enable human experience, with the understanding that space and form must be accessible, purposeful, resonant and generative?”
– Francis Murdock Pitts, FAIA, FACHA, OAA, OAA, Principal, Architecture+
of more than 200,000 residents in recent years. With that growth came strain on the province’s existing hospital, which struggled to accommodate an increasing need for mental health treatment.
In response, the provider worked with the HDR team to develop the Hillsborough Mental Health & Addictions Centre. Miszkiel said that while the existing building had design issues, staff and patients shared mostly positive stories about their experiences. In response, HDR worked to enhance the existing processes and use evidence-based design to integrate new ideas into the mental health treatment cycle, from intake to exit.
“We’re talking about the mental health evolution that’s happened there,” said Miszkiel. “It’s not just about the building, but about the whole system that the province took on and decided to really change the way we think about mental healthcare as a paradigm.”
The HDR team took inspiration from facilities across the globe, including one in Copenhagen, Denmark, that features courtyards and open sightlines to the surrounding nature to create a calming environment. For the PEI project, HDR sought to infuse the building’s interior with natural light and views of the surrounding rural setting, including a river and walking trails, to create nature-centered calming areas for not just patients, but also staff.
For patients to maintain a sense of agency within the facility, the design includes adjustable blinds, temperature controls and other customizable settings. Open spaces offer patients a variety of areas to read or rest, offering varying degrees of desired privacy. To add a regional flair, designers incorporated natural colors representing the sun, ocean, plants and other elements local to PEI, along with sustainable building materials.
The end result will be a more functional but also welcoming facility, where patients don’t feel locked in and have the resources and space to heal at their own pace. Construction is ongoing and is expected to be complete between 2026 and 2027.
Artful Healing: Transforming a Healthcare Campus Through Community and Creative Engagement
Another session highlighted how a local art program is being practically applied to enhance the care environment as part of a large-scale hospital campus renovation in Houston.
HFSE 2026 will be held at the Charlotte Convention Center, Sept. 28–30, 2026.
cancer in the community. Historically, the relationship between the community and the hospital has been marked by skepticism and distrust, and Fuessel said that one of HKS’s goals in taking on the project was to help rebuild that trust, promote equity and inclusivity and reinforce a communal sense in the hospital.
“This new facility is going to be a catalyst within the neighborhood, and we hope that it continues to ripple and uplift the people that are there,” said Fuessel.
To achieve this ambitious goal, the design team involved community consultants to garner support for the project and hear ideas on how to transform the hospital into an inviting and inclusive environment. During this process, the stakeholders established an art program to be incorporated into the project, featuring only local artists representing different backgrounds and professional levels.
Davis and Henderson noted that art can play a valuable role in healthcare design. Art projects and

installations can provide a meaningful experience that supports patients and families and uplifts staff. Additionally, it can create a sense of calm, support wayfinding efforts and distract from pain and discomfort.
Throughout the project, the team sought to incorporate art into not only open spaces, but into the very fabric and function of the buildings. For example, the hospital’s new parking garage, which required a jump-preventive façade, was an opportunity to utilize a printable high-density mesh material to display a massive mural on the side of the garage. This high-profile art installation will serve as one of the first sights visitors see when coming to the facility and will set a positive tone for the rest of their stay at the hospital.


The 2025 Healthcare Facilities Symposium and Expo featured more than 60 educational sessions, case studies and panel discussions over three days.
Photo Credit: Healthcare Facilities Symposium and Expo
From left: Barbara Miszkiel of HDR, Bill Saul of SableARC and Brian Giebnik of HDR spoke about an ongoing mental healthcare facility project in Prince Edward Island, Canada, at the 2025 Healthcare Facilities Symposium & Expo.
The HFSE exhibit hall featured more than 100 companies showcasing their products and services in the healthcare facilities market.
Photo Credit: Healthcare Facilities Symposium and Expo

National Conference on Correctional Health Care Hosted in Baltimore Nov. 1-5
By Kim Sterling
BALTIMORE — The National Commission on Correctional Health Care (NCCHC) will host its flagship National Conference on Correctional Health Care from November 1-5, 2025, in Baltimore. The conference brings together thousands of physicians, nurses, mental health professionals, administrators and custody leaders committed to improving care behind bars. It showcases the latest research, proven practices and emerging challenges in the field, offering a rare opportunity for multidisciplinary collaboration.

NCCHC CEO Deborah Ross emphasizes the importance of the event: “Correctional health is a team effort, and it relies on the many disciplines and custody working together to be successful. As the largest conference in the field for correctional health professionals, it offers critical knowledge across a range of topics, including suicide prevention, chronic care and behavioral health management. This shared knowledge strengthens collaboration between security and health care teams, reduces institutional risk and ultimately makes facilities safer for both staff and incarcerated individuals.”
Standards, Safety and Quality Improvement
The foundation of correctional health care begins with strong standards and oversight. In-depth seminars on NCCHC’s new 2026 Health Services and Mental Health Standards will help prepare facilities for updated requirements. Sessions on quality improvement provide practical strategies to identify gaps and enhance outcomes, reinforcing accountability and constitutionally adequate care.
Addressing Critical Health Risks
Correctional populations face heightened risks for serious and chronic conditions. Sessions on tuberculosis, hepatitis C and HIV will equip participants with best practices for containing and treating communicable diseases in secure environments. Chronic care and women’s health are also prioritized, with case-based discussions that emphasize evidence-based interventions to reduce mortality and improve outcomes.
Mental Health and Suicide Prevention
Mental health remains a pressing concern in correctional environments. The conference features suicide prevention strategies, mentorship in behavioral health, and effective approaches to care in restrictive housing. Presentations on dual loyalty examine the ethical complexities of serving patients while working within correctional systems.
Legal, Ethical and Professional Development
The legal landscape is continually evolving. A mock deposition session will prepare attendees for courtroom testimony, while ethics-focused sessions encourage reflection on dilemmas providers often face. Additional presentations highlight professional mentorship and workforce development, offering tools to support staff and reduce turnover.
Building the Future of Correctional Health
The conference underscores that correctional health care cannot succeed in isolation. From methadone program partnerships to collaborations with public health organizations, the agenda demonstrates how institutions and communities can work together to address substance use disorders, reduce recidivism and improve reentry outcomes.
With more than 100 sessions, extensive networking opportunities and a robust exhibition hall, the National Conference on Correctional Health Care is the premier event for advancing the profession. Participants — including clinical staff, administrators and custody leaders — will leave with actionable strategies to strengthen their facilities and contribute to a safer, healthier correctional system nationwide. For more information, visit www.ncchc.org/national-conference.
University of New Mexico Hospital Opens 570,000-Square-Foot Critical Care Tower
By Lindsey Coulter
ALBUQUERQUE, N.M. — The University of New Mexico Hospital officially cut the ribbon Oct. 1 on its new Critical Care Tower, a 570,000-square-foot facility that represents the largest expansion of the hospital in 15 years.
The tower, which welcomed its first patients Oct. 5, adds significant capacity to the state’s only Level I trauma center. The expansion includes a 68-bed Adult Emergency Department, 96 intensive care beds, a second helipad and 18 new operating rooms.
“The UNM Hospital Critical Care Tower is the instrument for making sure that we have good rural health care delivery,” said Gov. Michelle Lujan Grisham at the ceremony. “Whatever emergency comes our way, this campus, this university, this state will be ready.”
First proposed in 2015, the project required years of planning and construction. Hundreds of engineers, tradespeople, and hospital staff contributed to the facility’s completion, which combines advanced medical technology with spaces designed for patients, families and health education.
“It’s been incredible to see all the pieces of the CCT come to life — from the installation of high-tech medical equipment to the hanging of beautiful art pieces

that now brighten up the walls,” said UNM Hospital CEO Kate Becker. “The opening of the Critical Care Tower is possible because of your commitment to improving health care services for all.”
The facility also features The Sky Campus, a dedicated fourth-floor space designed for medical education, training, and staff support. The area includes private rest rooms for residents, secure lockers, eating lounges, and meeting rooms.
UNM Health System Chief Executive Officer Mike Richards, M.D., said the new tower will not only expand clinical care but also enhance the university’s role as a teaching hospital. He emphasized that the facility will serve as a hub for the UNM School of Medicine, as well as pharmacy, nursing, and public health programs.
UNM President Garnett S. Stokes said the opening marks a milestone for both patient care and education. “This is a special place, the embodiment of the kind of health care providers and educators we are — as well as the kind we still aspire to be,” Stokes said.


Kim Sterling is Vice President of Professional Services for NCCHC.
The tower includes a 68-bed Adult Emergency Department, 96 intensive care beds, a second helipad and 18 new operating rooms.
Photo Credit: Allan Stone and HSC Communications
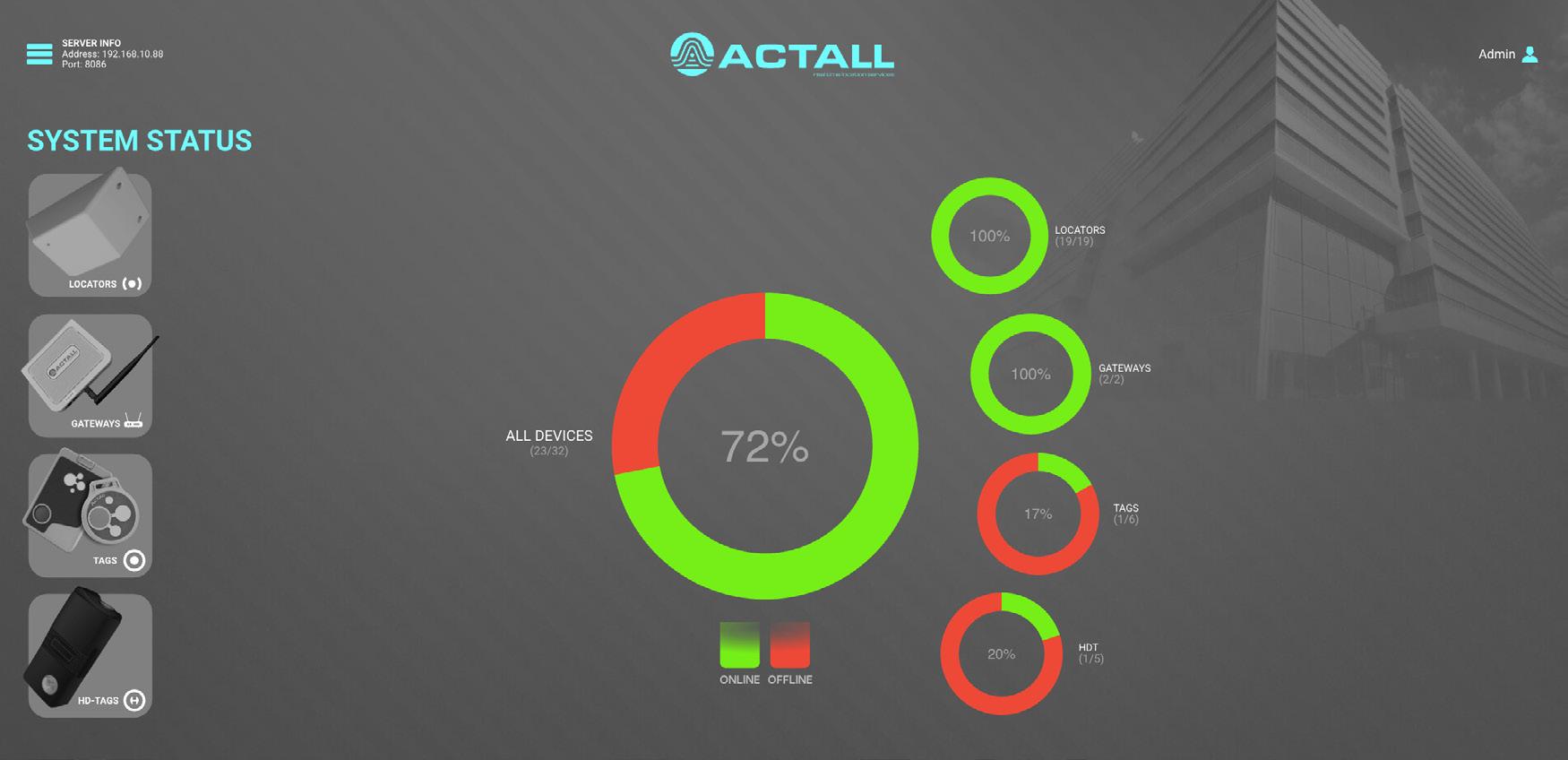
Extending the Life of RTLS How Actall can help healthcare providers avoid costly full-system replacements
By Lindsey Coulter
Real-Time Location Systems (RTLS) play a critical role in healthcare facilities. Healthcare providers across the spectrum and across the globe rely on the technology, which provides the real-time location of objects, people or assets within a specific area via tags, sensors and software. These systems are a critical component to ensuring staff safety, asset management and operational efficiency.
Thousands of hospitals and health systems worldwide long relied on Bosch RTLS technology, but the company’s unexpected exit from the market left facilities with significant investments in hardware tied to now-obsolete software. Actall, a Denverbased company already known for its RTLS work in corrections and behavioral health, responded to this need by developing a solution that helps healthcare providers extend the life of existing Bosch systems while modernizing for the future.
Actall’s HubSens 5.0 Fills the Gap
When Bosch discontinued its RTLS systems, many hospitals suddenly found themselves with significant investments in unsupported software. Additionally, the technology’s head end ran only on Windows 8, which was long past its support life and often created IT headaches. Replacing these systems wholesale would mean enormous costs — estimated at tens of millions for some health systems.
“That left [providers] with gear that still works just fine, but there is no way to manage it. That’s the problem Actall is fixing,” explained Bob Hampe, the company’s president and chief operating officer.
Actall has invested the past year engineering a specific solution to extend Bosch installations. In June, the company debuted HubSens 5.0, the latest version of its real-time location engine, now with full support for Bosch Security Escort field hardware. This solution enables control, telemetry and location processing and publishes results using the existing Bosch Security Escort remote control protocol. HubSens 5.0 was developed after lengthy interviews with Security Escort installations to determine their pain points and triage that listing into real priorities.
zonal solutions that offer more actionable location information in staff-duress scenarios. For hospitals, zonal tracking generally means faster, clearer communication during emergencies, according to Hampe.
To ensure flexibility, however, HubSens 5.0 allows hospitals to keep Bosch field hardware in place while layering in Actall products, such as PALS (RF Zonal), PALS Sentry (Ultrasonic Zonal), or the forthcoming PAKLS Escort (Coordinate). Migration can happen incrementally, with no downtime. The financial and operational impact of RTLS replacement can be immense.
“You can continue to operate your old system and improve on your new system, and it all works together,” Hampe said. “We’re not asking clients to throw away what they’ve already paid for. We’re giving them options to extend, adapt and modernize at their pace, while preparing for the future.”
A Trusted Partner in Complex Environments
Actall’s core strength is making RTLS work in architecturally dense healthcare spaces, which are often composed of concrete, steel, drywall and brick. These materials can affect duress or location signal propagation by deflecting or containing signals, or by allowing too much signal to bleed through.
Additionally, many healthcare facilities span multiple floors, with complex layouts that can impede or confuse RTLS signal transmission, and many hospitals struggle with signal interruptions from MRI machines and X-ray rooms. In many of these spaces, a Wi-Fibased RTLS system isn’t ideal for security purposes. Even in challenging spaces, Actall’s RTLS solution gets signals from a nurse’s duress button to a head-end monitor in three seconds or less.
Case Study: Victoria, Australia

“Actall’s approach to create a hybrid system that can integrate with the existing Escort hardware and expand with the new Actall devices is unprecedented for the industry with regards to supporting existing customers and their budget,” said Greg Cliff, Senior Project Manager and Engineer with CHA. “This unique approach will allow customers to utilize their investment of their system and evolve into the new Actall platform as their system expansion requirements occur and incorporate new system operation enhancements.”
“We’re providing a pathway, not just a product,” Hampe added. “Hospitals can take their time, continue running Bosch devices, and then migrate piece by piece into Actall technology without tearing out their infrastructure.”
Additionally, HubSens 5.0 is fully compatible with PrismUI, Actall’s Windows-based administration tool, which enables site personnel to manage devices, generate reports, configure alarms and notifications and integrate with I/O systems — delivering a rich ecosystem for operational continuity and future system expansion.
Choosing the Right Solution
Actall focuses on environments where radio frequency (RF) is difficult and staff safety is paramount — and where Wi-Fi-based solutions may not be ideal.
Instead of recommending a suite of solutions that might be more excessive than a client truly needs, Hampe works to zero in on the security and operational needs of each individual facility, understanding that hospitals don’t always need room-level precision or feature-heavy middleware. Instead, they most often need reliable safety and asset tracking that works in complex spaces.
When it comes to choosing the right RTLS solution, companies generally offer either zonal or X/Y systems. Zonal RTLS identifies an asset’s general area, while X/Y RTLS calculates its specific coordinates. In certain environments, XY-coordinate RTLS systems are appropriate, but for healthcare clients, Actall tends to recommend
In Victoria, Australia, Bosch systems were widely deployed in healthcare facilities. When Bosch pulled support, the Victorian government faced a dilemma: replace every system at once or find a bridge. By working with Actall, Victorian officials were able to extend Bosch systems while developing a staged migration plan. HubSens allowed them to maintain staff duress coverage immediately, buying time to plan a sustainable, multi-year modernization strategy.
Case Study: Whitby, Ontario
In Whitby, Ontario, a healthcare facility confronted the same issue: a Bosch RTLS system was tied to the now-unsupported Windows 8. Actall’s HubSens allowed the facility to keep staff duress protection online while introducing new Actall hardware. This approach let Whitby manage budgets and operational risk more effectively, while avoiding disruption to patient care.
Future-Forward Solutions Today
For healthcare facilities, Actall can offer more than just technology — it offers continuity, flexibility and the ability to solve complex problems in an easy and costeffective manner. Without a reliable RTLS system, the loss of high-value equipment, tools and medications can quickly trickle down to less efficient and effective patient care. It can also have a profound impact on a facility’s bottom line, meaning the potential of RTLS to transform the hospitals and healthcare facility operations is profound, but that transformation can’t happen on yesterday’s technology. Facilities struggling to find a sustainable RTLS solution, or grappling with the transition away from outdated systems, have options.
“If you have an existing Bosch system that provides staff duress in your healthcare facility, we can help you today,” Hampe said. “We can maximize your investment and manage your budget.”


HubSens 5.0 is fully compatible with PrismUI, Actall’s browser-based administration tool, which enables site personnel to manage devices, generate reports, configure alarms and notifications, and integrate with I/O and facility management systems — delivering a rich ecosystem for operational continuity and future system expansion.
Photo Credit: Courtesy of Actall
The 37,000-square-foot unit serves adults, providing both geriatric psychiatric care and dual diagnosis (psychiatry/addiction) services. This two-project, multi-phase expansion has also improved facility workflow, enabling them to accommodate more patients.
Best Practices in Lighting and HVAC for Behavioral Health Facilities
Understanding the nuances of this unique setting can dramatically
affect patient outcomes

By Patricia Rizzo and David Goldberg, PE
According to the American Society for Health Care Engineering (ASHE), nearly half of the specialty hospital projects under construction over the next three years will be behavioral health centers or psychiatric hospitals. In these facilities, safety and healing are of utmost importance.
Behavioral health facilities have come a long way from the sterile, institutional hospitals of the past. Architects and engineers collaborate with providers to meet the unique needs of their patient population. Purposeful interior design can have positive effects on mental and behavioral health. Offering patients autonomy in their surroundings — such as the ability to control lighting, and heating, ventilation and air conditioning (HVAC) systems — may help regulate their sleep, which could reduce stress levels.
Best practices for treating and housing patients with mental illness have shifted from custodial care to person-centered recovery. Understanding the role environmental factors and ambient comfort play in behavioral health is key to improving outcomes.
Ensuring Safety
Federal and The Joint Commission policies about patient safety, and accompanying considerations about security, are an imperative driver for facility design and operations. To that end, lighting for these spaces must be sufficiently robust to support patient and staff safety, while still providing suitable illumination and comfort.
Unique Needs of Behavioral Health Settings
As the design of behavioral health environments continues to evolve, lighting must benefit the diverse needs of populations across a multitude of spaces — from EmPATH units (Emergency Psychiatric Assessment Treatment and Healing), which are behavioral health units embedded in hospital emergency departments, sharing ED resources while providing a calm, therapeutic environment — to outpatient and residential facilities treating a range of diagnoses. Each facility has lighting requirements that are unique to the diverse population it serves. In addition to supporting patients’ health and wellbeing, these facilities must also ensure the safety of patients, caregivers and visitors. Luminaires with polycarbonate lenses and tamper-resistant fasteners and frames discourage damage to, and weaponization of, the luminaire. Ligature-resistant lighting — from luminaires to wall switches — removes hard edges, corners and entry points from the product, thereby reducing the opportunity for self harm.

The $24 million, 81-bed inpatient unit advances Carrier’s and RBMC’s commitment to delivering accessible, compassionate, quality care.

Healthcare facilities are difficult places for patients to maintain proper sleep hygiene. The lack of sleep, in many cases, can negatively impact healing, thereby lengthening the time a patient spends in the facility. Techniques to support circadian entrainment, such as modulating intensity from day to night via dimmable lighting, or including the enhanced features offered by tunable white or biodynamic lighting, can help preserve normal sleep/wake cycles and maintain hormonal balance.
In addition to providing daylight and views to nature, recent studies on health, performance, and comfort suggest that the ability to tune the color temperature of light (or even introduce color changing from pastels to saturated colors) based on application, need or occupant preference yields significant benefits. Personal control over room lighting can positively influence mood and support a patient’s feeling of independence, perhaps the most important benefit of all.
Physical Comfort Enhances Emotional Equilibrium
Studies indicate that extreme temperatures can exacerbate stress and anxiety, while a comfortably maintained environment fosters calmness and mental clarity. In addition to temperature, the quality of the air is important. Poor ventilation can lead to a build-up of pollutants and allergens, contributing to cognitive fog, lethargy and even long-term neurological impacts. In contrast, well-ventilated spaces with optimal air quality can enhance focus, boost mood and even improve sleep.
Similar to lighting, HVAC equipment in patient areas needs to be ligature- and tamper-resistant, preventing any potential for self-harm. In addition to HVAC, the electrical systems are another vital requirement. Like other healthcare environments, behavioral health facilities have unique electrical needs, including emergency power backup systems. Compliance with all the mechanical, electrical and plumbing (MEP) requirements ensures the facility operates efficiently, meets regulatory standards, and promotes the well-being of patients and healthcare professionals.
Excessive noise can be stressful for patients and hinder their recovery process. Strategic placement of loud MEP equipment can help create a quieter environment, promoting healing and rest.
Best Practices in Action
The 26-bed Center for Living in Meridian Health’s Raritan Bay Medical Center (RBMC) in Perth Amboy, N.J., has been treating behavioral health patients for decades and was in much need of an expansion and overall upgrade. To facilitate this and meet the ever-growing need for behavioral health services, Hackensack Meridian Health embarked on a partnership with Carrier Clinic, a leader in behavioral health, and retained NK Architects for the project.
The $24 million, 81-bed inpatient unit advances Carrier’s and RBMC’s shared commitment to delivering accessible, compassionate, quality care. The 37,000-squarefoot unit serves adults, providing geriatric psychiatric care and dual diagnosis (psychiatry/addiction) services. This two-project, multi-phase expansion has also improved facility workflow, enabling the provider to accommodate more patients.
The engineering team faced many challenges tying the new construction into the 100-year-old facility. Since the Center for Living continued operating during the renovation, the team had to keep the HVAC, electrical, medical gases, and water working throughout the renovation, and also provide temporary MEP systems and phased construction to prevent downtime in critical areas. The limited workspace and the need to install new infrastructure systems alongside existing ones without causing any major disruptions was also challenging. Additionally, conducting surveying in particular behavioral health areas limited the engineers’ access unless they were properly escorted by security.
Considering the unique protocols of a behavioral health setting, Johnson & Urban specified and designed all the equipment in the patient care areas to be ligature- and tamper-resistant. Tying into an existing facility is always challenging from a technical standpoint, in addition to the important consideration of patient wellbeing. However, working on a behavioral health project also required a particular focus on safety. Every detail — from screws to lighting — mattered.
Effective, Healing Lighting
The upgraded facility includes enhanced open day/dining and group spaces with both natural and color-tuning LED luminaires. This type of lighting design facilitates the entrainment of the body’s circadian rhythms, while also encouraging a warm, comforting, healing environment. Adjusting lighting from warm white to cool white can evoke a range of behaviors, from calm to alert, providing a holistic approach to treating psychological disorders.
The luminaires installed are robust to withstand abuse while still providing maximum visibility, wayfinding, glare reduction to support behavioral health and wellness. Every patient room features Kenall’s high-abuse luminaires, which includes 6-inch behavioral health downlights. Other areas of the clinic feature the company’s two-foot by two-foot recessed ambient troffers, and 4-inch-wide behavioral health SafeSlot™ luminaires.
Patient-Centered Expansion
The new facility also features inspirational artwork, modern decor, large-screen TVs in every room, and an abundance of natural light from oversized windows, including a relaxing sunroom. Every detail was designed to create a uniquely tranquil, comfortable, and safe environment for patients, visitors and team members. Show that applying practical, effective and patient-centric design — including the use of tunable white lighting and attention to physical comfort — can significantly impact patient outcomes.
Patricia Rizzo is the Senior Healthcare Product Marketing Manager for Kenall Manufacturing and may be reached at patricia.rizzo@kenall.com.
David Goldberg, PE, is a Senior Electrical Engineer, Johnson & Urban, and may be reached at DGoldberg@johnsonurban.com.
Photo Credit (all): Kenall, Johnson & Urban
The interiors include kid-sized wall graphics centered on the healthcare system’s friendly mascot, Choco the Bear, and interactive waiting areas where children can play and learn about topics such as circulation, nutrition and bone health.

Designing for Delight
Inside the playful architecture and precise construction of the Children’s Hospital of Orange County’s specialty outpatient facility
By Lindsey Coulter
When families step inside the new Rady Children’s Health outpatient facility in Orange County, Calif., they encounter a facility designed to transform how children experience healthcare. The nine-story, 300,000-square-foot outpatient building consolidates a wide range of pediatric services under one roof, streamlining care for families who often need to see multiple specialists.
The tower is the product of a multi-year collaboration between CannonDesign and McCarthy Building Companies and project manager Jacobs. Together, the team delivered a facility that is as technically advanced as it is imaginative.
“This facility provides specialty care,” said CannonDesign Interior Designer Hilary Thomas-Herd. “There are patients who need to see various specialists, so this is sort of a one-stop shop for seeing those types of caregivers.”
The new tower centralizes five floors of specialty clinics and offers a comprehensive imaging center, oncology infusion services, a research institute floor for clinical trials and pediatric research, and other family-centered amenities and resources.
By consolidating diverse services, the facility reduces stress on families while fostering collaboration between providers. It also expands Rady Children’s Orange County campus, complementing the Bill Holmes Tower, completed in 2012 — another product of the partnership between CannonDesign, McCarthy Building Companies and Jacobs.
Dynamic Inside and Out
Anchoring a visible corner in Orange, Calif., the tower was designed to be both a civic landmark and a welcoming destination for children receiving care. The building’s curved shape and red-and-silver façade with solar fins set it apart, but the fins are more than simply decorative. Dynamic integrated lighting creates a shimmering, kinetic effect that is most dense at the primary corner and tapers at the edges, giving the building a sense of motion.
to where you need to be. The curves within this building reinforce that concept.”
Wellness, Rendered Playfully
The graphics and branding program, led by Chris Hayes of CannonDesign, anchors the building in Rady Children’s wellness philosophy.
“The whole building is centered on the science of wellness and the five pillars of health: movement, sleep, nutrition, mental health and relationships,” Hayes explained. “We wanted people to learn through play, without knowing that they were learning. It’s all about informing families what your body needs every day to be healthy. While it’s definitely for kids, we made sure families can learn and benefit, too.”
These organic learning moments occur through kid-sized wall graphics (centered on the healthcare system’s friendly mascot, Choco the Bear), multi-lingual illuminated niches, and interactive waiting areas where children can play and learn about topics such as circulation, nutrition and bone health — without ever realizing they’re in an educational setting.
Other features include life-sized light-bright walls where children can create shapes and patterns as well as shadow-play walls for movement-based interaction. Custom cloud lighting in exam rooms creates calming ambiance, while immersive murals inspired by Southern California’s natural landscapes enhance dedicated play areas and help to reduce stress.


A landscaped terrace follows the building’s curvature, reinforcing the sense that the tower rises organically from the surrounding environment.
That curvilinear approach continues within the facility as well.
“Inside you’ll see a lot of curves on the floors, ceilings and the walls,” ThomasHerd said. “The basis of that is the idea that the healthcare journey, the journey toward wellness, sometimes it’s not always a straight line. Sometimes you have to veer off a path or take a different path to get

Toys, Nostalgia and a Mattel Partnership
One of the most striking design moves is the integration of Mattel toys into shadowboxes across elevator lobbies on floors four through nine.
“Every floor has a wellness theme like ‘let’s discover’ or ‘let’s enjoy the moment,’” Hayes said. “Our initial concept was to inspire children but also bring in nostalgia for families. This takes Rady Children’s ‘Long Live Childhood’ mantra to the next level. We had this idea of the arcade claw game that drops down and you try to pick up your favorite toy. It grew from there.”
Inspired by the project, Mattel donated a variety of Hot Wheels, Polly Pocket, UNO, Little People, Barbie and Thomas the Tank Engine toys to the project. The company also aimed to design the displays and toys to reflect the experiences of the children coming to the building, including one with a cochlear plant, and some with prosthetic limbs.
“Kids obviously gravitate to the displays because they’re toys, but even parents can get engaged. It’s super fun,” Hayes said. “That one idea that we drew evolved into something that, I think, will be unique to this hospital.”
Inclusive Wayfinding for a Diverse Population
Recognizing the region’s cultural and linguistic diversity, developing a solid wayfinding plan was key to the interior program. CannonDesign ultimately developed a wayfinding system that offers support in 28 languages.
“This whole system was designed to be diverse, with the three primary languages being English, Vietnamese and Spanish,” Hayes said. “We were trying to be very
Photo Credit (all): Laura Peters/CannonDesign
The graphic program was about encouraging kids to have fun, explore and engage with their surroundings.
Large expanses of glass are one example of biophilic elements that were intentionally incorporated throughout the building.


inclusive and very diverse, to the point where some kiosks feature Spanish as the primary language, whereas the one next to it is English or Vietnamese.”
Even the backdrop graphics embed the organization’s inclusive values, offering welcome messages in dozens of languages. That required a significant research effort from the design team, ensuring all translations were properly vetted and approved.
To ease navigation throughout the tower, CannonDesign paired these welcoming messages and graphics with a variety of natural elements and textures.
“We tried to really bring in the look of the natural environment, reflecting the feel of the sun and great colors that are in Southern California,” Thomas-Herd said.
“There is a moss wall in the lobby area and lighting with stretched fabric that makes it feel like you are looking at the sky. They’re bringing in a lot of branding … with Choco Bear guiding [visitors] into the building.”
Durable
Materials with a Natural Touch
Given the curious and tactile nature
of the building’s primary users, material choices balanced durability, infection control and child friendliness.
“Many of the graphics are actually sheet-wall protection, so, they’re serving two purposes,” Thomas-Herd said. “The flooring, depending on the space, is seamless sheet vinyl in infusion and imaging areas, LVT in clinical exam rooms and terrazzo in lobbies to have that seamless, elevated feel.”
Additionally, the team incorporated solid surfaces for added durability and ease of maintenance wherever possible, including in seating niches, walls and counters.
“That durability standpoint was critical, because this building should be here for a long time, but kids need the ability to be playful. The materials need to support that as much as possible,” she added.
Natural touches — such as terrazzo flooring, wood-look textures and large expanses of glass — reinforce the calming environment to bring healing biophilic elements to the space.
Level Nine: Research and Discovery
The tower’s top floor is devoted to pediatric research, but rather than keep this space separate from more patient-centric spaces, research was put on display in an effort to spark children’s curiosity about science.
“The client really wanted to get the kids excited about science and research and learning,” Thomas-Herd explained. “When families and visitors arrive on that floor, there is a makerspace where the kids can see into the research areas and watch what the scientists are doing inside. They can actually see into the lab through big windows at their level, and then after they observe the research, there are tables set up where kids can play and pretend like they’re scientists.”


The nine-story, 300,000-square-foot outpatient building consolidates a wide range of pediatric services under one roof, streamlining care for families who often need to see multiple specialists.
Recognizing the region’s cultural and linguistic diversity, the wayfinding system offers support in 28 languages.
example intentionally building.

PROJECT DATA
Project Name: Rady Children’s Health Tower
Location: Orange, Calif.
Size: 300,000 square feet
Project Type: Children’s Outpatient and Research
Project Delivery Method: Design-Assist
Owner: Rady Children’s Health
Architect: CannonDesign
General Contractor: McCarthy Building Companies
Construction Manager: Jacobs
Building and Safety Inspection: Smith-Emery
Civil Construction: Castle Contracting
Concrete: Dean Visosky Contractors, Penhall Company
Construction: Costa Azul Contracting Group
Electrical: Berg Electric Corp.
Excavation: Nolan Excavation
Finish Carpentry: Roy E. Whitehead Inc.
Fire Protection: Kimble and Company
Grading: Southern California Grading
Landscape Contractor: Pierre Landscape
Lifting and Hoists: Tractel Inc.
Masonry: Masonry Concepts
Mechanical Contractor: Murray Company
Medical Equipment and Specialties Construction: Seamless Care Inc.
Painting: Johnson & Turner Painting Co.
Roofing: Danny Letner Inc.
Steel Fabrication: Sanie Manufacturing, Schuff Steel, CMC Steel Fabricators
Surveying: IMEG, Pfeiler and Associates
Terrazzo Contractor: Corradini Corp.
Tile Contractor: Charles McCandless Tile Contractors
Traffic Control: RCS Safety LLC
Waterproofing and Concrete Restoration: Courtney Inc.
PRODUCT DATA:
Architectural Woodwork: ISEC Inc.
Curtainwall and Glazing: Tower Glass Inc., Giroux Glass
Doors: McKendry Door Sales
Elevators: Mitsubishi Elevators
Fire Doors and Shutters: McKeon Door West
Flooring: Signature Flooring
Foodservice Equipment: TriMark West
Building and Construction Execution
McCarthy Building Companies was brought on early as a designassist partner, which supported real-time information sharing in collaboration with Jacobs and CannonDesign, and allowed the team to make more informed design and budget decisions.
McCarthy broke ground on the tower in 2022, leading a construction effort that spanned just over two years. To deliver the project on a compressed timeline, significant planning was required in the preconstruction phase to allow for long-lead procurement materials such as metal panels, curtainwall, electrical gear and mechanical equipment, explained Cameron Kilar, McCarthy Project Director.
“This plan took significant coordination between the design team, Rady Children’s and McCarthy to ensure all design items were completed, and material ordered to support the schedule installation dates,” Kilar added. “Credit to all of the craft workers that spent some long hours and weekends working on the project to deliver this project on time.”
McCarthy also emphasized safety, precision and innovation throughout the project, coordinating closely with CHOC and CannonDesign to integrate complex MEP systems, high-performance materials and infection-control features while still delivering vibrant, family-centered spaces. However, the small site footprint made construction logistically challenging. In addition, during a large portion of the construction, McCarthy was constructing the parking structure expansion on the same site, which added complications.
The project was fully modelled in BIM, with utilities installed using Trimble. The majority of plumbing and HVAC systems were prefabricated by Murray Companies, which ensured efficient installation and facilitated just-in-time deliveries. To achieve accuracy in the building’s curvature, McCarthy used detailed 3D modeling and detailed surveying to ensure that the slab edge was accurate to receive the glass curtainwall panels.
Evaluation and Legacy
The Tower officially opened earlier this summer, and the post-occupancy evaluation will be completed in 2026. The evaluation will focus on durability but also how users of all ages are responding to the building, how it supports patient flow and its overall success in meeting its mission.
For Hayes, the project represents a career milestone. “This project is a one-ofa-kinder right now, but hopefully it becomes the norm,” he said. “I’ve designed several children’s hospital experiences, but this one, especially coming right after [the COVID-19 pandemic], was about encouraging kids to have fun, explore and engage with their surroundings. It’s kind of like an exhibit you would find at a children’s museum or Legoland, but in a healthcare setting.”

Lab Furniture and Fume Hoods: MottLAB
Operable Walls: L2 Specialties
Parking and Traffic: Myers & Sons Hi-Way Safety
Pneumatic Tube System: TransLogic Corp.
Signage: CA Signs, Signs and Services Company
Steel and Architectural Metals: Bapko Metal Inc.
Wall Systems: The Nevell Group
Window Treatments: Phillips Draperies & Curtains Inc.

Thomas-Herd agreed: “When we first showed the images with the spheres that are hanging from the ceiling, I don’t think it was a fully baked idea. But the leadership really latched onto this and felt like it was a symbol of the joy of childhood and were elements to make [healthcare] less scary.”
From its shimmering solar fins to its toy-filled shadowboxes, Rady Children’s new specialty care tower offers a new way of imagining and delivering pediatric healthcare design; balancing clinical excellence with joyful, playful and inclusive environments, supporting the mantra: Long Live Childhood.
As Hayes put it: “It’s designed to emotionally transport a child and take away all the anxiety of being in a hospital. While it can’t compare to Disneyland, but we’ve created that kind of experience where you’re in a fun space, not a traditional healthcare space.”


Mattel donated Hot Wheels, Polly Pocket, UNO, Little People, Barbie and Thomas the Tank Engine toys.
By consolidating diverse services, the facility reduces stress on families while fostering collaboration between providers.


Designing for Dignity Why treatment environments matter
When we talk about behavioral health care, especially in correctional and juvenile facilities, the conversation often starts with staffing, security and programming. But what’s just as critical — and too often overlooked — is the environment where treatment happens.
Deanna Dwenger, Psy.D., knows this reality intimately. With more than 12 years of experience in correctional psychology — both on the clinical floor and in leadership roles — she’s seen the consequences of spaces that strip away autonomy, natural light and dignity.
“People disengage. They shut down,” she says. “Or worse, they escalate. Self-harm. Aggression. Antagonism.”
These behaviors don’t arise out of nowhere. They’re shaped by the surroundings. When a room feels hostile, confusing or sterile, it reinforces a sense of being unsafe. And when people don’t feel safe, they don’t heal.
The High Cost of the Wrong Environment
In facilities with harsh lighting, loud echoes, blank walls and few personal touches, Dwenger saw patterns:
· Disorientation and distress from lack of natural light
· Increased self-harm and use of restraints in chaotic or cold spaces
· Antagonism and resistance in environments designed purely for control
· Disconnection and reduced staff safety, especially when there was no effort to make spaces feel welcoming or humanizing
It’s not about luxury. It’s about respect. As Dwenger puts it, “People need spaces that affirm their autonomy, reflect their dignity, and allow them to be seen as more than a diagnosis.”

doesn’t just benefit the patient. Safer environments also protect the providers working within them.
What Healing Can Look Like
That’s where CareAffirm comes in.
Traditional construction can take years to complete — time that communities don’t have.

CareAffirm prefabricated behavioral health rooms are designed to replace hostility with humanity. Featuring natural light, calming finishes, built-in sound therapy systems and privacy-conscious layouts, each unit creates an environment that supports emotional regulation and meaningful engagement.
CareAffirm solutions address the very deficits Dwenger has encountered for years:
· Natural light for orientation and circadian regulation
· Sound therapy systems to reduce agitation and promote calm
· Soft finishes and thoughtful furniture that feel safe — not institutional
· Safety features that protect both patients and providers
· Modular construction that opens faster, with customizable, trauma-informed layouts
Environments That Reflect Worth
Dwenger emphasizes that for healing to take root, individuals must believe their life has value. When environments remove the shame and sterility so often baked into institutional settings, something shifts — both consciously and subconsciously. The message becomes clear: Your progress matters.
That’s the power behind every CareAffirm build. These aren’t just prefabricated rooms — they’re environments crafted to affirm autonomy, dignity and the inherent worth of each person inside. Because growth doesn’t happen in a vacuum. Especially in mental health care — and particularly for justice-involved populations — progress depends on a space that makes healing feel possible.
CareAffirm’s environments do exactly that. They offer more than functionality. They offer a chance to be seen, to feel safe and to move forward.
Explore how CareAffirm environments create space for healing at www.careaffirm.com


Dwenger highlights how creating environments “that respect autonomy and dignity actually improves engagement in care.” In her experience, even simple changes — spaces that allow personal items, soothing colors or soundscapes — can dramatically reduce incidents of self-harm or aggression. And that
These aren’t just prefabricated rooms — they’re environments crafted to affirm autonomy, dignity and the inherent worth of each person inside.
Featuring natural light, calming finishes, built-in sound therapy systems and privacy-conscious layouts, each unit creates an environment that supports emotional regulation and meaningful engagement.
CareAffirm prefabricated behavioral health rooms are designed to replace hostility with humanity.
Photo Credit (all): CareAffirm
STANDOUTPRODUCTS

Durable, Tamper-Resistant Waste Bin
SPOTLIGHT PRODUCT
Behavioral Health Furniture
Elevate behavioral health spaces with the Summit Series, a thoughtfully designed collection of dining, accent, and lounge chairs, paired with tables in a variety of heights as well as stools. This collection offers the innovative Veldura finish for a soft, calming feel while ensuring lasting durability and easy maintenance. Each piece is crafted to support safety, comfort and therapeutic care.
To enhance the collection, we’ve introduced a new table top design, the Delta. The Delta top brings both style and versatility, offering a fresh alternative to traditional table top options. This collection will be available in six new colors as well as the standard 12 and can be customized with any laminate selection. The Summit Series can adapt to any design vision.
Cortech USA www.cortechusa.com
SafeBin delivers a smarter, safer way to handle facility waste. Built from durable rotationally molded construction with no metal hinges, it’s engineered to withstand heavy use while eliminating common safety risks. The tamper-resistant chute keeps bag liners out of reach, while the integrated lock (compatible with the master key systems) adds an extra layer of security.
Designed for efficiency, the SafeBin features a 35-gallon interior that works with or without liners, a sloped base for easy cleaning and drainage, and flexible options to bolt it securely to floors or walls. Available in a wide array of colors with a sleek black top, it blends seamlessly into any environment while upholding the highest standards of safety and hygiene. The SafeBin makes waste disposal easier, cleaner, and more secure. Protecting both staff and residents, every day.
Cortech USA
www.cortechusa.com
Patient-Room Lighting
Nightingale, a patient-centered, designforward lighting brand for healthcare environments, has unveiled the Attend™ sconce luminaire, a versatile new lighting solution that offers quiet yet functional illumination. Attend offers sufficient nighttime illumination to support medical staff in performing routine checks without disrupting patient rest. It’s designed to consider the needs of patient families, offering an optional task light and integrated local controls. These features enable family members and caregivers to read, work or relax comfortably while staying nearby. The luminaire drew inspiration from hospitality design rather than traditional institutional fixtures, bringing a more comforting aesthetic to the patient room. It is available in a range of finishes — including antimicrobial white, black, brushed metal, three wood grain options, and custom colors — for seamless integration with various interior palettes. Nightingale
www.nightingalelighting.com


Slip-Resistant Flooring
Mannington Commercial delivers a suite of performance-driven products enhanced with on-board technologies designed to cultivate healthier environments with lasting beauty and less maintenance in one of the harshest flooring environments. As health and wellness facilities are not “one product fits all” places, the company incorporates evidence-based design to create flooring that fits the unique needs of healthcare spaces. The company’s BioSpec line includes BioSpecArmor® for superior performance in demanding health and wellness environments, BioSpec® SR for slip resistance or BioSpec® MD for best-in-class abrasion resistance with more than 68 color options. Patterns and palettes are designed to work together seamlessly to craft a coherent design while tailoring spaces to fit functional needs.
Mannington Commercial www.manningtoncommercial.com

How Bicycle Health is Changing Opioid Recovery Through Virtual Care
By Lindsey Coulter
Bicycle Health has quickly become a leader in addressing one of the nation’s most persistent public health crises: opioid use disorder. As the largest medical group in the U.S. providing virtual Medication for Opioid Use Disorder (MOUD) treatment, the company combines evidence-based care with technology to deliver best-in-class outcomes at scale.
Addressing the Pain of Addiction
Founder Ankit Gupta established Bicycle Health after seeing how opioid addiction often began after a patient was legally prescribed medication for pain, and that few effective treatment options were available. His vision was to expand access to highquality, integrated medical and behavioral healthcare through a virtual model that reduces stigma and logistical barriers.

limited treatment access — including transportation, stigma and long intake processes.
“It’s as simple as a phone call,” Tomlin said. “You can be seen within 24 hours by a provider. You’ll have the support of 100 providers across the country, peer recovery coaches, peer support specialists, all on an app. If you don’t have a phone, we can get
The company’s model also leverages certified peer specialists, many of whom bring
“The peer specialists can meet clients where they are and walk them through the recovery piece,” Tomlin said. “It’s not psychotherapy, it’s talking to someone who’s been
This virtual, patient-centered and individualized model, which literally places MOUD at a patient’s fingertips, allows flexibility for patients to engage on their own schedules.
Sessions can be scheduled or accessed on demand, with patients able to message their recovery coach or provider as needed. The company’s national network of providers and staff makes it possible to match patients with specialists regardless of geography.
Rapid Response is Key
Overdose risk is 8–40x higher post-release
Studies across multiple states show that the risk of overdose is extremely high in the two weeks following release.

The ability to engage patients quickly is critical, and Bicycle Health strives to narrow the window between seeking and receiving care.
“We try to see individuals within 24 hours, because we know when someone seeks help, they want help then. They’re not going to wait.”
Patients are then assessed, prescribed medication and connected with local pharmacies. Drug screenings are handled virtually, when possible.
Bicycle Health is also actively growing its network by embedding services in emergency departments to offer support for patients immediately after overdose. The same model is being extended to correctional settings, allowing treatment to continue seamlessly as patients transition back into the community from detention or

“If you look at persons going back from recent incarceration, they are 40 times more likely to overdose in the first two weeks than the general population,” Tomlin said. “So can we provide a seamless continuum of care for them.”
Building Momentum in Criminal Justice Health Care
Tomlin joined Bicycle Health after a decades-long career in addiction treatment and recovery within the criminal justice and corrections system and has a keen understanding of the unique needs of people who are experiencing opioid-use addiction while in custody. His role now focuses on building awareness of Bicycle Health’s services and expanding partnerships with sheriffs, departments of correction and federal reentry programs. He is also leading efforts to extend these services to justice-involved populations — some of the most underserved and at-risk individuals in the country.
“Just within the Bureau of Prisons alone, 4,000-plus individuals have been treated by Bicycle Health at residential reentry centers,” Tomlin said. “Of those 4,000 there have been over 29,000 encounters, groups, sessions and one-on-ones. So, criminal justice is not new to Bicycle Health, but growing the spectrum of services and broadening the footprint is my goal.”
Bicycle Health began in 2017 at a single clinic in Redwood City, Calif., but Gupta quickly recognized that the brick-and-mortar model alone could not meet the scale of need. In 2020, Bicycle Health launched its virtual care platform, which provides empathetic, affordable, person-to-person care at scale. The app gives patients access to a coordinated model of MOUD that includes medication management, behavioral health treatment, support groups and care coordination.
The company’s full-time medical team of physicians, physician assistants and nurses is licensed across 32 states, with insurance contracts covering nearly 120 million lives.
From Startup to Industry Leader
Since its founding, Bicycle Health has treated more than 40,000 patients, with about 15,000 currently active, making it the country’s largest telehealth provider of MOUD. Its outcomes reflect the strength of its model: 80% of insured patients remain in care at 90 days compared with an industry average of 44%, and 95% report no withdrawal symptoms at seven days. Half remain in recovery after six months — a success rate 40% higher than most in-person clinics.
The company’s approach is designed to reduce barriers and expand access to treatment at a time when the opioid crisis continues to devastate communities.
“Recovery is a lifelong process,” said Steve Tomlin, Senior Vice President of Business Development, Criminal Justice. “Our retention numbers are better than most inpatient clinics: 86% of patients stay for a month, 72% stay for three months, 58% are still enrolled at 12 months.”
Additionally, roughly 30% of Bicycle Health patients are new to Suboxone (buprenorphine/naloxone) treatment, underscoring the company’s role in expanding access to people who may not otherwise begin recovery.
Meeting Patients Where They Are
A hallmark of Bicycle Health’s model is addressing the barriers that have historically

The company is also building partnerships with organizations such as CorrHealth and the Larimer County, Colo., Sheriff’s Office. Larimer County Lieutenant Staci Shaffer, MCJ, says the collaboration has been instrumental in expanding access to quality medical and behavioral health care for those experiencing incarceration.
“We try to see individuals within 24 hours, because we know when someone seeks help, they want help then. They’re not going to wait.” – Steve Tomlin, Senior VP of Business Development, Criminal Justice
“This collaboration bridges gaps in treatment, improves continuity of care and ultimately supports better outcomes for the individuals,” Shaffer said. “Working with these two organizations has reinforced the importance of innovation and teamwork in jail healthcare.”
A Mission-Driven Approach
Tomlin said his decision to join Bicycle Health was rooted in the potential to reach more people with effective treatment and remove the barriers that too often prevent recovery. While brick-and-mortar facilities are critically important and are key partners for Bicycle Health, the organization can help fill capacity and geographical gaps. That ability to offer easy and direct access, especially for patients with fewer physical options for treatment, reduces or eliminates many of the challenges that keep people from seeking or continuing care.
“The opioid crisis may not be front page news as it once was, but the issue is no smaller than it was when it was making daily headlines,” Tomlin said. “There’s billions of dollars in opioid settlement dollars out there available to treat individuals, and we have to look at every way we can to support people in their recovery.”

Elevating Behavioral Health Design
Santa Clara’s new Child, Adolescent, and Adult Behavioral Health Services Center prioritizes visibility, humanity and access
By Lindsey Coulter
Across the country, communities are prioritizing behavioral health services to address a spectrum of patients and needs. While research from the American Hospital Association shows that many providers are integrating behavioral health services into existing acute, primary and emergency services and facilities, many other communities are developing purpose-built hospitals and clinics to meet this growing need.

The Child, Adolescent, and Adult Behavioral Health Services Center at Santa Clara Valley Medical Center (SCVMC) is a prime example of a facility designed specifically to address the healthcare needs of all community members. When it opens in 2026, the three-story, 207,000-square-foot facility will consolidate and expand the county’s behavioral health services.

The project will create Santa Clara County’s first inpatient psychiatric facility specifically for children and adolescents, while also increasing adult inpatient capacity and replacing aging facilities. The design introduces co-located services in one building, including inpatient units, outpatient urgent care, emergency psychiatric services (EPS), administrative offices, an outpatient pharmacy and a pedestrian bridge connecting to the adjacent emergency department, allowing safe, secure, and private transport of patients between hospital departments and services.
HGA’s San Francisco office led the design in collaboration with research and behavioral health experts across the firm. The contractor team includes Webcor Builders, SBay Construction, and Thompson Builders, with Arup, Sandis, TEECOM, RHAA, and others providing engineering and specialty services. The project is targeting LEED Gold certification.
A First-of-Its-Kind Facility
For HGA Principal and Senior Project Manager Craig Blackhurst, the new center (the first ground-up project of its kind designed to the new OSHPD-5 standards) represents a major step forward in how the state approaches behavioral health design — but the project wasn’t without challenges. In addition to design intricacies and an ambitious delivery timeline, the development process coincided with the COVID-19 pandemic, which forced HGA’s team to rethink collaboration.
“We were designing this literally from our own homes and experiencing our own
challenges during that time,” Blackhurst said. “We realized through the empathy that we hold so dear in our guiding principles at HGA that we’re not all in the same boat, but we’re being tossed about on the same stormy sea. In many ways, these shared
“We
–
wanted to bring more nature and humanity into design to make patients feel like they could be sitting in a park.”
Craig Blackhurst, HGA Principal and Senior Project Manager
experiences brought our team closer together even though we were apart.”
To keep the project on track, HGA, California’s Department of Health Care Access and Information (HCAI, formerly OSHPD) and the county established a strategy of collaborative, incremental reviews.
“We partnered with regional leaders from HCAI and did a collaborative, integrated review,” Blackhurst said. “We were on [Microsoft] Teams meetings with them about every three weeks going through their comments in real time. We could respond to review comments much more rapidly than we could in a typical project,” Blackhurst said.
That process allowed early package approvals, allowing construction to begin sooner. “We broke the construction documents up into multiple increments and were able to get the packages approved earlier and the county found a contractor who was very motivated to go quickly,” Blackhurst said.
Program Development and Site
The impressive speed to construction was also an indicator of the county’s fervor for the project. The comprehensive program that combines inpatient, outpatient and emergency psychiatric services in one building has long been needed.

“We give a lot of credit to the client and the health center operators. They were very passionate about what they wanted to provide,” Blackhurst said. “[The county] doesn’t currently offer adolescent or children’s mental health services. So, they said, why can’t we just combine these and make it a more efficient facility, maintain separate patient populations but provide a one-stop shop?”


The comprehensive program that combines inpatient, outpatient and emergency psychiatric services in one building has long been needed. | Photo Credit (all): HGA
The third floor is divided between 21 beds for adolescents on the west wing and 14 beds for minors on the east wing. Secure outdoor courtyards with high walls, translucent glass, and visible landscape areas beyond were also integrated to provide daylight and views while

The facility’s site is adjacent to the county’s existing emergency department, a location that improved operational efficiency and reinforced the building’s focus. A new service tunnel and a patient transport bridge connect the BHSC to the existing facility.
“These features allowed us to reduce what’s in our building associated with other medical care and focus entirely on acute psychiatric care and outpatient services associated with psychiatric care,” Blackhurst said.
Layout and Flexibility
The building is organized with outpatient and administrative services on the ground floor, including EPS and secure outdoor courtyards for both patients and staff. Inpatient units for 42 adults occupy the second floor, while adolescents and children are on the third, with isolation and accessible rooms and outdoor spaces in each unit.
“The second floor is all adults, with two separate units. The great thing about that is they can have two equal acuity units, or if they have some patients with higher acuity,

they could split them and have the lower acuity and higher acuity unit,” Blackhurst said. “They might have 42 adults that are moderately acute in one scenario. They might have another scenario where 21 people need to be elevated. So, they have that flexibility.”
Meanwhile, the third floor is divided between 21 beds for adolescents on the west wing and 14 beds for minors on the east wing,
“Even that arrangement offers flexibility; if [the facility] doesn’t happen to have any minors at a given time, and they have more adolescents; they can split them and move them.”
Safety, Access and Nature
Visibility, safety and access to nature were central to HGA’s design approach. Patient units, especially on the second and third floors, are organized north to south, but the staff spaces are oriented east-west. The nurse stations intersect the patient units at the middle, allowing a full view across the entire unit in both directions with a clear line of sight to every single patient bedroom. Additionally, the HGA team designed staff spaces and access to the units to be compact and efficient to reduce staff fatigue.
Secure outdoor courtyards with high walls, translucent glass and visible landscape areas beyond were also integrated to provide daylight and views while maintaining privacy and supporting de-escalation.
“We wanted to bring more nature and humanity into design to make [patients] feel like they could be sitting in a park,” Blackhurst said.
Structural and Code Requirements
The facility was designed under California’s new OSHPD 5 standards, which falls between traditional hospital and standard building requirements. Blackhurst explained that an OSHPD 1 acute care hospital carries its importance factor of 1.5, while acute psychiatric under the new requirements is 1.25.
“It’s more than a standard building. It is still a shelter-in-place facility, but [codewise] not quite as much as a full hospital,” Blackhurst said. “It is actually more resilient than is required by code. For example, the backup generators will run longer than are typically required [for a psychiatric hospital].”
Broader Impact
For Blackhurst and the HGA team, the project is part of a larger shift in how behavioral health facilities are conceived and built, as behavioral health is an issue that touches every community.
“We present our design solutions a lot, and oftentimes we ask, ‘Who in the room has been touched by mental health care?’ Every hand goes up every time,” Blackhurst said. “Elevating the importance of designing spaces like this for this type of patient also helps to eliminate the stigma around mental healthcare; because mental healthcare is healthcare.”

The building is organized with outpatient and administrative services on the ground floor, including emergency psychiatric services and secure outdoor courtyards for both patients and staff.
When it opens in 2026, the three-story, 207,000-square-foot facility will consolidate and expand the county’s behavioral health services.
DESIGNER ROUNDTABLE




Environments That Heal
Three leading healthcare designers on how the right design choices can protect, support and empower patients while also easing the burden on staff
By Lindsey Coulter
The design of mental and behavioral health facilities is undergoing a transformation. For decades, these specialized spaces were built primarily for safety and control, often resulting in stark, institutional environments. But today, designers, clinicians, and healthcare leaders are pushing toward a different vision — one that balances safety with dignity, compassion and healing.
To explore this shift, Healthcare Construction + Operations News spoke with three leaders shaping the field: Tiffany Kalloor, associate principal and director of interior

design at Hoefer Welker’s Dallas office; Rachael Rome, studio practice leader in mental and behavioral health at HKS; and Marvina Williams, RN, associate principal at Perkins&Will. Their combined expertise spans architecture, interior design, clinical operations, and psychology, offering a rich look at the challenges and opportunities in behavioral health design.
Kalloor, Rome, and Williams shared their insights on guiding principles, patient dignity, staff well-being, community connections and the future of behavioral health facilities. Each emphasized the importance of evidence-based design while tailoring solutions to the unique needs of patients, staff, and care models. They discussed strategies such as trauma-informed environments, graded socialization and community integration.
While each brings a unique approach and perspective to their work, they all agreed on one central point: The environment is not just a backdrop to care but an active partner in healing. The right design choices can protect, support, and empower patients while also easing the burden on staff.
Q: What design principles or evidence-based strategies guide your approach to creating behavioral health facilities?
KALLOOR: At Hoefer Welker, our architects and interior designers ground every project in evidence-based design principles, drawing on proven outcomes and best practices to inform each decision. We collaborate closely with healthcare clients and clinicians to understand their key performance indicators and measures of success, ensuring those priorities are embedded throughout the design.
In mental and behavioral health facilities, safety is always paramount. Our team continually researches new products and innovations to incorporate the most effective, reliable solutions for protecting patients and staff. At the same time, we emphasize strategies that foster healing, promote community, and reduce isolation — helping create environments that support recovery as well as overall well-being.
By combining rigorous evidence with deep client collaboration, we deliver behavioral health environments that balance safety with compassion and community.
ROME: My primary guiding principle is that the environment itself can be a therapeutic agent; it’s something that shapes behavior, it fosters incremental progress, it supports recovery all through the environment. Drawing from both clinical psychiatry
and evidence-based design, I see spaces not just as the container, but as an active participant in care. The environment itself can extend that care.
One of the key strategies we use is something we call graded or incremental socialization. When patients are arriving in crisis, they really need and ask for privacy and safety and calm. So, as recovery progresses, the built environment can gently invite patients into greater connectivity with others through what we call environmental incentives. That can look like private rooms that open onto sunlit shared day rooms. It could be a cozy alcove that bridges solitary retreat from group interactions and group therapy spaces or other. It could be courtyards that encourage quiet meditative space adjacent to peer engagement through things like pickleball courts. The kind of staged exposure really mirrors the therapeutic models of gradual reintegration.
I am a designer by trade, but I also studied counseling and psychology. So, we try to mimic what that therapeutic model renders and allow patients to practice autonomy while still feeling supported. There’s also a lot of evidence that points to choice and control and agency. Architecture can obviously reinforce those things by offering patients choices on where to fit or how to engage with daylight or views or move to quieter spaces. In psychiatry, we know that healing is not necessarily linear. It happens with steps and setbacks and accelerations, and all of that is totally contingent on the person on the day at the time what the environment is, but by creating environments that really scaffold socialization.
WILLIAMS: At Perkins&Will, our approach to behavioral and mental health design is guided by a profound commitment to evidence-based practices, holistic well-being, community integration, client collaboration and leveraging the built environment to build brain capital. Evidence-based design goes together with a passion for innovation and data-informed design. We leverage the latest research and technological advancements to create environments that not only meet current clinical standards but also anticipate future needs. This involves considering how the built environment impacts health and well-being and designing spaces that contribute positively to patient outcomes. Evidence-based design strategies incorporate healing design, such as access to nature and calming interior design. We view behavioral and mental health through a holistic lens, recognizing that the mind, body and spirit are interconnected. Our designs go beyond clinical functionality, incorporating elements that nurture cognitive, emotional, psychological and physical well-being.

Q: How do you design spaces that promote dignity, autonomy and recovery for patients?
KALLOOR: We focus on creating spaces that honor the dignity of patients by feeling welcoming and familiar, rather than institutional. We intentionally avoid environments that appear overtly “behavioral health,” instead designing spaces that look and feel like any other medical setting — warm, familiar and comfortable — to reduce stigma and promote a sense of normalcy.
Supporting autonomy is equally important. Within the boundaries of safety requirements, we introduce innovative solutions that provide patients with a greater
KALLOOR ROME WILLIAMS
Perkins&Will renovated and expanded Lancaster General Hospital’s Emergency Department, allowing for increased patient capacity and an expansion of services.
Photo Credit: Courtesy of Perkins&Will
A patient room designed by Hoefer Welker at UT Southwestern Medical Center, Clements University Hospital psychiatric unit.
Photo Credit: Dror Baldinger
sense of control over their environment. For example, at UT Southwestern Medical Center’s Clements University Hospital Psychiatric Unit, our team developed a foam door pad attached with Velcro — a simple yet effective approach that gave patients more privacy than a completely open doorway, while maintaining necessary safety standards.
Ultimately, our goal is to create environments that feel comfortable, familiar, and supportive of recovery; spaces that foster dignity and empower patients on their healing journey.
ROME: We’ve invested in designing with empathy; designing for dignity, autonomy and recovery. We’ve written and designed to support dignity through normalization, understanding that patients deserve environments that express and extend care for them. We use materials that are warm to the eye and comforting to the touch, employing lighting that honors the natural circadian rhythms and private rooms that embody rest and respect. We believe that when a patient feels that the space is honoring their humanity, especially in moments of great vulnerability, it quietly reinforces their worth.
For autonomy, we try again to foster patient choice and control in our design. We know patients might be enduring a lot of shame or disorientation or even nausea from new pharmacological treatments. So, we look for opportunities within the bedroom space to design for gentleness with warm lighting. We try to put a sprinkling of small comforts that really reduce anxiety and support self-regulation.
WILLIAMS: Trauma-informed design is reshaping how we think about our built environment, prioritizing respect, safety, dignity and community. Innovative designs promote a sense of connection, allowing facilities to become a source of comfort and support.
Trauma-informed design is a powerful tool for alleviating the effects of trauma and promoting healing. Respecting patient privacy and dignity is fundamental to ethical and
WILLIAMS: Effective spatial planning is critical for behavioral health facilities to support the delivery of care while ensuring patient privacy, dignity and safety. Flexible and adaptable floor plans are essential to accommodate diverse treatment modalities and patient needs. Considerations should include designated areas for therapy, group activities, quiet reflection and outdoor spaces for recreation. Additionally, the layout should facilitate easy navigation and minimize the risk of patient agitation or elopement. Ensuring the safety and security of patients, staff and visitors is paramount in counseling behavioral health designs. Design strategies to mitigate risks include controlled access points, clear sightlines for supervision and secure areas for patient observation, and restraint, if necessary. Incorporating anti-ligature fixtures, tamperresistant materials and robust electronic surveillance systems, AI can further enhance safety measures.
Q: What’s one design decision you made in a mental health or behavioral healthcare project that had a bigger impact than expected?
KALLOOR: One of the most meaningful design decisions I’ve been part of came through the UT Southwestern Psychiatry Unit project. From the start, hospital leaders were intentional in their directive: The psychiatry unit should not look or feel any different than the other inpatient floors.
As a result, the unit was designed with the same high-quality finishes, expansive windows, and patient-centered elements as the rest of the hospital, rejecting the stripped-down, institutional aesthetic so often seen in behavioral health environments. Backed by the hospital’s commitment to fund this vision, the decision sent a powerful message: Psychiatric patients deserve the same level of dignity, care and positive experience as any other patient.

humane behavioral healthcare. Private rooms with
bathrooms offer patients a sense of autonomy and control over their environment.
Q: How do you create environments that support both patient privacy and staff visibility?
KALLOOR: We use a zoned approach to thoughtfully balance patient privacy with staff visibility. In high-visibility communal areas — where patients engage with care teams and peers — we design open, welcoming environments that incorporate color, artwork, patterns and amenities. These elements create warmth and help foster connection and community.
In more private spaces, such as individual patient rooms, safety and durability are the top priorities. Here, we are more intentional with finishes and details to ensure the environment remains secure while still supporting comfort.
This layered approach allows us to deliver environments that feel open and inviting, where interaction is encouraged, while still prioritizing privacy, protection and healing in more personal settings.
ROME: We use zoning strategies that allow staff to maintain passive observation without compromising patient privacy. Examples could be observation corridors that integrate borrowed light into patient spaces, while also offering staff the opportunity to check in while they’re walking as well as distributed team bases for staff to engage with patients that are outside of the typical, more conservative staff hub.
We also try to create barrier-free sight lines or nested sight lines, and we work closely with our audio/visual teams to create placements for discrete cameras. We integrate a lot of technology, but our team strives for the architectural choreography of each of these divisions within the space to make sure that everything is done without compromising the patient’s wellbeing.

That impact was felt not only by patients and staff, but also by the broader community. One of the unit’s largest donors was a family personally touched by mental health struggles, who recognized the importance of creating a space that normalizes behavioral health care.
For me and our team, the choice to design without compromise proved far more powerful than expected. It elevated the patient experience, reinforced dignity, and helped set a precedent for how behavioral health environments can and should be approached.
ROME: The smallest decision that had a massive impact was at San Antonio State Hospital. During a site visit, I had a forensic patient approach me and asked if she could show me her favorite part of the new facility. So I walked with her and a staff member to the end of the wing where the old building had been removed and there were a bunch of trees that had just been planted that were still low. There was a built-in bench at the end of the corridor, and I assumed she liked it because it created a more social spot for people to sit, but she went on to explain that it was her favorite place because everybody could gather there to watch the fireworks. Her birthday was on the 4th of July, and she said she never thought I would ever see fireworks again. Apparently on New Year’s Eve, people had all gathered there to watch the fireworks and celebrate their fresh starts, and she was counting down to her birthday. It was just a bench at the end of a corridor, but it had such an impact.
WILLIAMS: One design that had a major impact was in a behavioral health module in a busy trauma center. We were able to place the module on an outside wall that allows clearstory windows for the behavioral health emergency room patient. Many times, these patients are in the ED for several hours to several days waiting for placement. Just being able to know what time of day it is makes a huge difference for these patients. The effects of this on their circadian rhythm are influenced by the environment, and disruptions can lead to various other health problems.
ensuite
The UT Health Science Center - San Antonio State Hospital designed by HKS. Photo Credit: Joe Aker/HKS

Safeguarding Patients and Simplifying Compliance
Why healthcare organizations are turning to integrated Computerized Maintenance Management Systems and Enterprise Asset Management platforms
By Margaret Nardini
Unsafe care contributes to more than 3 million patient deaths annually, with roughly 1 in 10 harmed during healthcare delivery, according to the World Health Organization. While clinical errors often take the spotlight, operational failures like a missed HVAC alert in a surgical suite or a delayed repair on a sterilizer can be just as dangerous.
Yet many hospitals still depend on outdated systems and manual processes to manage maintenance, inspections and safety-critical assets. In a world of shrinking margins and rising complexity, that approach isn’t sustainable. Forward-looking healthcare organizations are turning to integrated Computerized Maintenance Management Systems (CMMS) and Enterprise Asset Management (EAM) platforms to close the gap between risk and response.
The role of facilities and clinical engineering has shifted from behind-the-scenes to mission-critical. When you’re managing assets in a high-risk environment, response time and documentation aren’t just operational metrics — they’re imperative for patient safety.
Detecting Safety Risks in Real Time
Hospitals can’t afford delays when something goes wrong. Integrated CMMS and EAM systems combine asset health data, accurate documentation and smart alerts to detect issues early, preventing them from escalating into critical events.
Whether it’s a sensor detecting a leak near sensitive equipment or an HVAC anomaly triggering an alert, integrated platforms can generate a work order instantly and route it to the right technician. With asset risk scores baked into the system, teams can prioritize responses based on severity.
For example, a hospital can identify a water leak in a critical unit via sensor, triggering an automatic alert and dispatch. The issue can be resolved in minutes, not hours, minimizing the risk of contamination and care disruption.
When CMMS and IoT systems are working together, facilities move from reactive to predictive. Facilities teams aren’t waiting for a complaint to know something’s wrong. Instead, they’re utilizing IoT sensors to detect performance anomalies and receive notifications that a failure may occur before it happens. This allows issues to be proactively resolved before clinical teams even realize a change in their environment.
Simplifying Compliance and Audit Readiness
Hospitals operate under intense regulatory scrutiny from The Joint Commission to CMS and ISO standards. Preparing audits with legacy systems often requires digging through binders, spreadsheets and fragmented logs.

logged with a timestamp, technician ID and electronic signature. Procedure management ensures staff follow the correct protocol, while
dashboards offer audit-ready reports on demand.
Preparing audits used to require days or even weeks of gathering documentation, reconciling maintenance logs and validating compliance records. With the right CMMS, that burden is drastically reduced. Facility and clinical engineering teams gain instant access to complete maintenance histories, inspection outcomes and compliance actions. All of which are organized, timestamped and searchable.

This level of transparency helps not only with audits but also with internal accountability and continuous improvement. Facility and clinical engineering teams can spot documentation gaps before regulators do and can address them proactively.
Mobilizing Maintenance to Match the Pace of Care
In healthcare, delays are costly. Closing a single patient room due to equipment failure can cost upwards of $20,000 an hour. Modern CMMS platforms help avoid this by providing technicians with mobile access to real-time data, work-order prioritization, standard and default procedures, and simplified documentation tasks.
Instead of waiting for paperwork or manual routing, technicians can respond to alerts instantly, scan equipment barcodes to access service history, and update tasks in real time.
Mobility isn’t a nice-to-have; it’s essential in environments where seconds count. Technicians can respond faster, document work accurately and keep clinical staff in the loop. That improves uptime, compliance and trust.
Beyond the immediate impact on safety and efficiency, mobile tools also support workforce agility, which is critical as many healthcare systems face staffing shortages and high turnover across facility maintenance and operations teams.
Raising the Bar on Safety Through Integration
Patient safety starts long before a clinician enters the room. It begins with properly functioning equipment, safe environments and well-documented protocols, which all require the right operational systems behind the scenes.
By integrating CMMS and EAM platforms with powerful monitoring and reporting capabilities, hospitals can move from reactive maintenance to a more proactive, datadriven model. The results can be faster response times, stronger compliance posture and ultimately, better care outcomes.
As the healthcare landscape continues to evolve with stricter regulations, rising operational costs and greater scrutiny over patient outcomes, the importance of responding quickly is no longer optional. Facilities, clinical engineering and IT teams are no longer operating alone, they’re sharing systems, data and assets for better outcomes.
Investing in an integrated infrastructure is an investment into safety, trust and futurereadiness. When maintenance teams are equipped with real-time insights and intuitive, automated tools, they can address problems as needed and prevent future issues. In healthcare, prevention isn’t just good practice — it’s a lifesaving imperative. When systems are connected, teams are empowered. Integration helps healthcare organizations respond with confidence, stay ahead of risk and focus on the patient.
Modern CMMS platforms streamline the entire process. Every maintenance action, inspection and calibration is
Margaret Nardini is the Healthcare Product Manager for Accruent.
Integration helps healthcare organizations respond with confidence, stay ahead of risk and focus on the patient. | Photo Credit (all): Accruent
Instead of waiting for paperwork or manual routing, technicians can respond to alerts instantly, scan equipment barcodes to access service history and update tasks in real time.
The Transformative Power of Trauma-Informed Design
Offering more supportive, therapeutic environments is essential for justice and recovery
By Felice Upton
Creating environments that heal rather than harm transforms outcomes for individuals, staff and communities. To create a trajectory to end incarceration, communities and providers must address underlying issues, not just presenting problems. One critical pathway is trauma-informed design.
The design of prisons and mental health facilities for both adults and youth profoundly determines whether the facility perpetuates cycles of trauma or create pathways to healing. After leading women’s prisons, and then youth facilities, over the course of many years, I’ve witnessed how environmental design either retraumatizes vulnerable populations or supports genuine rehabilitation. The stakes are enormous both for the individuals being served and the staff working in these facilities.
Why Trauma-Informed Design Cannot Wait
Nearly all incarcerated individuals have experienced some type of trauma, many of them significant trauma. Research consistently demonstrates that additional trauma exposure increases recidivism and future system involvement, yet traditional correctional environments often have harsh lighting, institutional colors, constant noise and sterile odors. These environmental characteristics can trigger hypervigilance and retraumatization, impacting not only residents but also staff.

patterns that provide clear sight lines, comfortable gathering areas and private spaces for difficult conversations contribute to environments where conflicts resolve before escalating.
Four Transformative Projects: Evidence in Action
The Family Visiting Revolution:
The Washington Corrections Center for Women partnered with a design student to reimagine family visits. Rather than assuming children would be traumatized by correctional settings, the team asked: How can we create spaces where families connect meaningfully? Over months of testing colors, textures, toys and games with mothers and children, the team developed design principles prioritizing warmth, safety and connection. The model maintains crucial family bonds during incarceration, which often prove critical for reducing recidivism and supporting successful reentry. After years of advocacy, the original vision was finally brought to life.

We’re witnessing a crisis reminiscent of mental hospital deinstitutionalization. Without trauma-informed alternatives to traditional carceral housing, people are recycled through systems that exacerbate harm rather than heal. Some states focused on real change are shifting toward smaller, therapeutic environments where thoughtful design is prioritized and takes into account the physical and mental health needs of staff and residents.
The evidence is unequivocal: Environments designed to increase hypervigilance and maintain cold institutional atmospheres actively sabotage rehabilitation goals. When spaces feel punitive rather than restorative, that undermines the objectives of reducing recidivism and promoting public safety, instead increasing risk, costs and turnover and reducing opportunities for healing and desistance.
The Science of Healing Environments
Environmental psychology research demonstrates that exposure to natural light, plants and outdoor views reduces cortisol levels, improves cognitive function and decreases aggressive behaviors. Access to nature isn’t luxury; it’s medicine. Gardens, calming plants like lavender and calendula, and outdoor views create measurable improvements in emotional regulation and behavioral outcomes.
Multisensory Design for Recovery:
Every sense contributes to either healing or retraumatization. Color psychology reveals that warm, natural palettes reduce anxiety and promote emotional stability. Acoustic design profoundly impacts behavior — low, soothing sounds improve sleep quality and reduce agitation. Even carefully considered scents, moving beyond sterile institutional odors toward pleasant, natural aromas, create environments that support rather than undermine mental health.
Intentional Flow Patterns:
How people move through space affects emotional states and interpersonal interactions. Deliberate flow
The Echo Glen Library Revolution: When I became superintendent at Echo Glen Children’s Center, we had a library but not one that was fully funded. It was not bright, colorful or engaging. There was no qualified librarian nor a book selection tailored specifically for our population. We rectified all of those deficits, and the resulting transformation created a bright, airy, cheerful space that fundamentally changed how youth interacted with learning. There is now a full-time librarian who ensures the space remains safe, so that young people can access age-appropriate books that make them feel valued. This project likely altered these youth’s lifelong relationship with education — a profound intervention with lasting impact.
Healing-Centered Mental Health Units:
The most complex project involved redesigning a locked mental health unit using experiential design principles. Working with researchers and designers, we interviewed residents about sensory needs during crisis periods, collaborated with nurses and psychiatrists about therapeutic goals, and developed protocols for safely incorporating calming design elements. The reimagined unit supported stabilization and recovery rather than simply containing the crisis.
Gardens for Healing:
At Echo Glen Children’s Center, community volunteers also created garden beds outside each unit. The garden beds helped ensure incarcerated people could engage in activities that remind them they are human. Having access to living things they can nurture and grow promotes both rehabilitation and healing. Working in soil, caring for living things and creating beauty provides therapeutic benefits extending far beyond the garden itself.
environments that promote dignity and create hope. When people feel human rather than warehoused, they engage more in programming, develop positive relationships and make changes that support successful reentry.
For Staff: Employees in healing environments experience reduced stress, fewer workplace injuries and increased job satisfaction. When physical environments support rather than undermine therapeutic goals, staff focus on rehabilitation rather than crisis management, which leads to lower turnover, reduced workers’ compensation claims and more effective interventions.
For Communities: When correctional facilities successfully reduce recidivism through trauma-informed design, communities benefit from increased public safety, reduced crime rates and lower costs from repeated incarcerations. Additionally, family bonds are more likely to remain intact when visiting environments designed to support rather than strain relationships.
For Society: Broader benefits include reduced correctional costs, decreased healthcare expenses from trauma-related conditions, increased productivity from successful reintegration and stronger communities overall.
Designing for Complex, Overlapping Needs
Modern correctional facilities must serve increasingly complex populations.
Gender-responsive design recognizes that different trauma experiences require different environmental supports. Mental health accommodations, modeled after those in psychiatric facilities, reveal that creating calming environments supports stabilization. Substance-use disorder considerations require thoughtful environmental design that supports recovery and reduces fear of withdrawal. Cultural competency ensures access to indigenous medicines, herbs and spiritual practices. ADA compliance creates truly inclusive environments. Behavioral management incorporates design elements that de-escalate rather than inflame situations.
The Imperative: Design as Strategic Intervention
Evidence overwhelmingly supports trauma-informed design as both a moral imperative and practical strategy for achieving correctional goals. When facilities create environments that reduce trauma, support mental health, and maintain human dignity, they’re not just being compassionate, they’re being strategic about public safety and cost-effectiveness.

This transformation requires courage from corrections and mental health professionals to advocate for facilities that truly serve rehabilitation goals.
It demands collaboration between designers, clinicians, security staff, and residents. Most importantly, it requires recognizing that how people are housed profoundly shapes who they become and whether they will be able to successfully reintegrate.
The choice is clear: continue building facilities perpetuating cycles of trauma and recidivism or create spaces truly serving justice and healing. The evidence, outcomes, and our shared humanity point toward one conclusion: It’s time to build environments that heal rather than harm.
Transformative Benefits Across All Stakeholders
For Individuals: Trauma-informed design directly supports rehabilitation by reducing retraumatization, improving emotional regulation and creating
Felice Upton is the founder of Just Us by Felice Upton Consulting LLC and the former Assistant Secretary of Juvenile Rehabilitation, Washington State Department of Children, Youth, and Families.
Echo Glen Children’s Center
Photo Credit: Courtesy of the Washington State Department of Children, Youth, and Families
Wisconsin’s Jonathan Delagrave Youth Development and Care Center Photo Credit: Treanor

Wellness Through Technology, Infrastructure and Operational Efficiency A win for correctional healthcare’s future
By Helen Hanks
Modern healthcare is experiencing an unprecedented transformation due to rapid advancements in technology. Nowhere is this shift more vital, and yet more challenging, than within the realm of correctional facilities. Prisons and jails have unique healthcare needs stemming from high rates of chronic illness, mental health and substance-use disorders, and infectious diseases among the incarcerated population. Correctional facilities continue to be the largest provider of mental health services in any community, with rates of mental health disorders higher than that of the community. With resources often stretched thin, budgeting challenges, aged infrastructure and security taking precedence, the deployment of efficient, innovative technology has become essential for bridging gaps, improving outcomes and upholding the fundamental right to health for inmates. Correctional healthcare infrastructure and operations leadership must continue to focus and examine opportunities beyond the right paint colors on the walls to affect mood or murals of inspiration in therapeutic communities, to advocate for implementation of innovation through technology:
· Spaces designated for telemedicine and remote care
· Data-driven healthcare management informed by electronic health records and other software tools
· Health solutions such as wearable health technology
· AI-powered mental health care augmentation and tablet access to Cognitive Behavioral Treatment programs
· Other smart designs that keep line of sight, digital visual resources, and radio frequency identification or facial recognition as part of the efficiency of operations
Correctional Healthcare’s Unique Challenges
Healthcare delivery in correctional facilities is shaped by a combination of logistical, ethical and resourcebased challenges. Correctional agencies have struggled to recruit and retain the qualified, diversified healthcare staff necessary to meet care needs. This became even more evident during and after the COVID-19 pandemic, when healthcare professionals were fatigued and left their professional fields, reducing an already finite recruiting pool. Additionally, recruiting and retaining new healthcare professionals in correctional facilities, in competition with community-based healthcare employers, has proven to be difficult, as they are often asked to work in aging facilities with limited resources, where security protocols can impede timely access to care.
The incarcerated population is also disproportionately affected by conditions such as hepatitis, HIV/AIDS and mental health disorders, with a high prevalence of substance-use disorders.
Examining the combination of staffing challenges and the depth of healthcare needs of those incarcerated, technological innovations offer a lifeline by streamlining processes, amplifying limited resources and enhancing both the quality and reach of healthcare services. Keeping technological innovations at the forefront when the opportunity exists during a physical plant renovation or other capital budget project will promote designing for efficiency and improving quality.
Teleservices Bridge Distance, Expand Access and Improve Community Reintegration
One of the most significant technological advancements in correctional healthcare is the adoption of telemedicine. Telemedicine uses digital platforms to connect inmates with off-site medical professionals, reducing the need for costly and logistically complex transports to external clinics or hospitals. This

technological advancement offers other benefits across a correctional system by rethinking the space set aside or designed for telemedicine as a teleservices space instead. These teleservices spaces can be more versatile designed
and built to meet healthcare needs and other legal needs such as contact with guardians, family visits, court hearing and other legal consultation.
By establishing dedicated spaces in housing units for secure video conferencing (teleservices) that are within line of sight and on video surveillance of corrections officers, people incarcerated can consult with specialists in fields ranging from psychiatry to dermatology, cardiology and infectious diseases. These pre-scheduled contacts can be monitored by the department’s healthcare team from a different location to ensure any recommended next steps are scheduled or managed locally.
In addition, creating teleservices spaces empowers incarcerated people to take action in their lives and rehabilitation planning by being more in control and responsible for being present at their appointments. Teleservice spaces within housing units not only improve access to timely care but also address safety and security concerns associated with moving high-risk individuals.
The implementation of teleservices, especially telemedicine, results in a reduction in off-site trips translating into fewer security incidents, lower transportation expenses and a more efficient allocation of staff resources.
Electronic Health Records Offer Efficiency, Accuracy and Continuity
The implementation of electronic health records (EHR) is another cornerstone of technological efficiency in correctional healthcare. EHR systems enable seamless documentation, retrieval and sharing of patient information across different providers within the correctional system.
With frequent transfers of people between facilities, traditional paper records pose significant risks for errors, omissions and delays. EHRs mitigate these risks by ensuring that critical health information — medication histories, allergies, chronic conditions and previous treatments — travels with the patient. This not only enhances the quality of care but also reduces redundant tests, adverse drug interactions and miscommunication.
EHR platforms tailored for correctional settings often include modules for mental health, dental care and substance use, reflecting the comprehensive needs of the incarcerated population. Furthermore, integrated reporting tools help administrators track health trends, manage outbreaks and comply with regulatory requirements efficiently. Partnering with an EHR company that has integrated artificial intelligence algorithms within their product will help data-driven correctional healthcare administrator and providers better understand and predict healthcare trends, ensure clinical decision and supportive documentation is in the record, individualized treatment planning and comparative growth, and the streamlining of scheduling, coding and

Telemedicine utilizes digital platforms to connect inmates with off-site medical professionals, reducing the need for costly and logistically complex transports to external clinics or hospitals.
Photo Credit: Broomfield Detention Center
Mobile apps and dashboards improve insights into detainees or inmates’ wellness.
Photo Credit: 4Sight Labs
billing. With many states engaged in Center for Medicaid and Medicare Services 1115(a) Re-entry Waivers to promote successful community reintegration, an effective EHR is key to CMS billing, community partner information sharing and tracking post-release outcomes.
Remote Diagnostic Tools and Mobile Health Technologies
In addition to telemedicine and EHR, correctional healthcare has benefited from the rise of remote diagnostic tools and mobile health (mHealth) technologies. Digital stethoscopes, otoscopes, and portable ultrasound devices allow healthcare providers within facilities to capture high-quality diagnostic data. These data can be transmitted to specialists for
through virtual counseling, remote psychological assessments and digital cognitive-behavioral therapy (CBT) platforms.
Telepsychiatry enables mental health professionals to conduct evaluations and follow-ups efficiently, even when resources are scarce. Digital CBT programs, available via secure tablets or dedicated kiosks, provide ongoing support and skill development for people incarcerated managing depression, anxiety or substance abuse. These platforms can be tailored to meet specific linguistic, cultural and literacy needs, further enhancing engagement, responsive to accessibility and efficacy.
Moreover, secure tablets or dedicated kiosks can help staff proactively communicate with their incarcerated patients and vice versa to be proactive in reducing mental
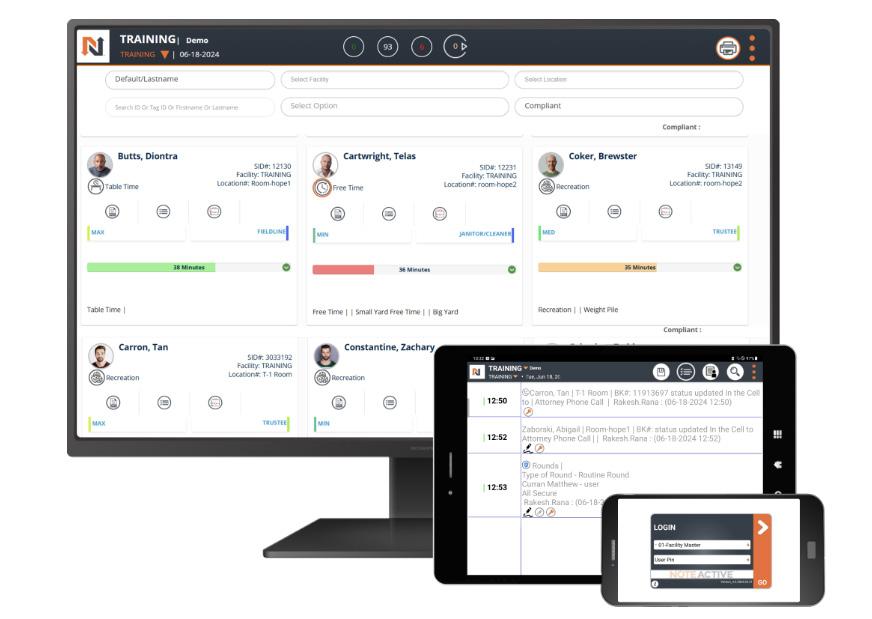
evaluation, expediting diagnosis and treatment without necessitating travel.
These mHealth solutions, such as secure tablets or kiosks, empower people incarcerated to engage with health education, report symptoms or even request appointments. The self-service approach not only promotes health literacy and personal responsibility but also streamlines administrative workflows for staff. By reducing paperwork and automating appointment scheduling, reducing requests for copies of health records, these tools free up valuable time for direct patient care. Correctional healthcare facilities can use kiosks for check-in stations just like community healthcare with the
health crises, enabling earlier intervention and reducing the risk of suicide or self-harm.
Infection Control and Population Health Management
Correctional facilities are particularly vulnerable to outbreaks of infectious diseases due to high population density and limited infrastructure. Technology plays a pivotal role in infection control, from automated tracking of immunizations and testing to digital contact tracing during outbreaks.
EHR systems can alert staff to vaccination gaps,
“Telepsychiatry and digital CBT programs can be tailored to meet specific linguistic, cultural and literacy needs, further enhancing engagement, responsive to accessibility and efficacy.” – Helen Hanks, Former Commissioner, New Hampshire Department of Corrections
use of radio frequency identification (RFID) and facial recognition technology, a person can check in at a kiosk instead of needing an officer to process the why they are there. This information is then relayed to the corrections officer on post and the healthcare staff awaiting their patients.
Leveraging Technology for Timely Support
Mental health disorders are highly prevalent among incarcerated individuals, yet correctional facilities have long struggled to provide adequate mental health services. Technology has begun to narrow this gap

facilitate mass screenings and generate reports for public health authorities. Data analytics enable administrators to identify trends, allocate resources strategically and implement preventive measures efficiently. Digital education campaigns, delivered via in-house television or tablets, help promote hygiene and awareness among inmates — critical during events such as influenza outbreaks or education on the Prison Rape Elimination Act.
Barriers, Limitations and Ethical Considerations
While technology promises significant efficiency gains,
its deployment in correctional healthcare is not without challenges. Data security and privacy are paramount, given the sensitive nature of health information. Robust cybersecurity measures are essential to protect against breaches and misuse.
Additionally, budget constraints may limit the acquisition of cutting-edge tools, especially in underresourced facilities. Staff training and acceptance can also pose hurdles — technology must be user-friendly and integrated seamlessly into existing workflows. The current facilities’ aged infrastructure may pose challenges for implementation or creating the efficiency expected.
Ethical considerations abound, particularly concerning autonomy and consent. People incarcerated may face barriers to accessing technology-based care due to literacy, disability or language. Efforts must be made to ensure that innovation does not inadvertently exacerbate disparities or infringe upon patient rights.
The Future of Technology in Correctional Healthcare
Looking ahead, emerging technologies such as artificial intelligence (AI), predictive analytics and wearable devices hold immense promise for correctional healthcare. AI-powered triage could prioritize at-risk patients, while predictive models might help facilities anticipate outbreaks or mental health crises. Wearable health monitors could facilitate continuous tracking of chronic conditions like diabetes or heart disease.
Partnerships between correctional healthcare providers, academic institutions and technology firms are crucial for piloting and scaling these innovations. Policymakers must ensure that legal and regulatory frameworks keep pace, safeguarding patient rights while maximizing the benefits of technological advancement and differences in correctional settings.
Technology Can Improve Wellness and Safety
Technology has become an indispensable tool for delivering efficient, high-quality healthcare within correctional facilities. From telemedicine and electronic health records to mobile health and digital mental health platforms, innovation is helping to surmount longstanding barriers of distance, resource scarcity and complexity.
By embracing technology thoughtfully — balancing efficiency with privacy, accessibility, and ethical care — correctional systems can transform health outcomes for one of society’s most vulnerable populations. Ultimately, the pursuit of technological efficiency in correctional healthcare is not just about cost savings or convenience; it is a matter of dignity, wellness, rehabilitation and safer communities.
Helen Hanks joined the New Hampshire Department of Corrections in 2003 and was confirmed as Commissioner in 2017 before leaving her role in 2025. Under her leadership, the department implemented innovative therapeutic communities, such as Wellness and Residential Treatment Units, focusing on mental health and substance use disorder treatment. She successfully aligned healthcare payment models during incarceration with Medicaid and Medicare, securing legislative changes to improve care continuity.
The implementation of electronic health records and note-taking is another cornerstone of technological efficiency in correctional healthcare.
Photo Credit: NoteActive