9 minute read
Commentary
Home made
Brain organoids are not real brains; they cannot be used as replacement organs in case of brain damage. But these artificially grown, living mini-brains made of human cells do offer a unique opportunity to unravel the dynamics of brain cells.
Advertisement
By Marieke Buijs Images: Bram Belloni
Neuroscientist Paul Ormel puts on a white lab coat and squeezes his hands into purple latex gloves. Just to be sure, he spritzes them with alcohol. Now he is ready to fish out container ‘#2 22/11/18 ProLabb’ from a swinging rack in the incubator. The clear plastic dish looks deceptively ordinary as the casing of a creation that is everything but ordinary. There they are, floating in a thin layer of clear pink fluid. Four mini-brains. Dull, pale pink lumps, roughly half a centimeter in diameter, with random dents and bulges. These are brain organoids. Tiny brain structures made of human cells. Thought of and created by humans. Developed thanks to ingenious molecular tricks in the high-tech equivalent of a human uterus: nutrient-rich fluid that is carefully kept at body temperature. These are the creations that should help scientists figure out how the brain develops and what goes wrong in conditions like Alzheimer’s, ALS, and schizophrenia.
From the lab In the summer of 2013, a shudder went through the world of brain research. Bioengineer Madeline Lancaster and her colleagues described how they managed to grow mini-brains in the prestigious scientific journal Nature. To Professor of Translational Neurosciences Jeroen Pasterkamp of UMC Utrecht it was instantly clear that this was a breakthrough. He began setting up a lab to create and, in particular, to study brain organoids. After the start-up and development stages, the first experiments in schizophrenia and ALS are now under way, and soon an organoid study of Alzheimer’s will begin.
The human brain is a collection of some 90 billion nerve cells that each have an estimated 7,000 communication links to other cells. This inconceivably complex information network plays a role in everything we do; from walking to having a discussion in a café, and from falling asleep to daydreaming. A vital organ. And, therefore, well hidden, floating in shock-absorbing brain fluid and packaged in a thick layer of bone – the scull.
Both this complexity and thorough packaging put scientists in an awkward position. How do you discover where things are going wrong when someone develops amnesia or when speech becomes distorted? Taking a peek, touching the tissue or put
ting it under a microscope is not something that is easily done.
Over the course of centuries, brain researchers have built up a repertory of work-around tactics to gain insight into this complex organ. For example, the brains of deceased people are put under the microscope, scientists use fMRI scanners to visualize the living brain in action, and the genetic makeup of mice and rats is altered to create and study rodents with Alzheimer-like symptoms.
All these methods offer valuable insights, but they also have shortcomings. The resolution of the brain scanner is not high enough to see what is happening at a cellular level, and a disease model for ALS in mice is actually not the same as for ALS in humans. Medication that may seem promising in mice-models of ALS often doesn’t seem to work in human patients.
Smaller than the real thing PhD student Ormel is now holding a promising extension kit of the scientific toolbox between his fingers. ‘For the first time, we have a three-dimensional structure of living human brain tissue in a Petri dish, with which we can simulate the brain of a living patient and study it at a microscopic level,’ says the neuroscientist. Another bonus: the organoids were created using the building plan that the cells carry in their own DNA. So, to a certain extent, they are taking their natural shape.
Let there be no misunderstanding here: brain organoids are not real brains. They cannot be used as a replacement organ in case of brain damage – something that can be done with, for example, lab-cultured bladder tissue. Think of them like this. Imagine you give a hundred toddlers each a Lego Duplo set of a castle and let the children get to work. The resulting structures relate to the intended castle in approximately the same way as the brain organoids relate to the human brain. One looks a bit more like the original than the other, but most structures contain the most important elements. The brain organoids, for example, display the structures of the hippocampus, an area of the brain involved in learning and navigation, and the cerebral cortex is also visible, the outer section of the brain that is responsible for, among other things, impulse control and planning. But the areas of the brain are not consistently in the same place and some parts are missing. Furthermore, the organoids are many times smaller than the real brain. There are no blood vessels running through them, and so the laborious circulation of fluids is a limiting factor for growth and preservation. Without the supply of nutrients to the inner cells of the organoid, the brains remain relatively small – even though they do contain millions of cells within a few millimeters. With daily care, they will survive approximately two hundred days in the lab.
A valuable window Despite their limited size, the mini-brains offer a unique opportunity to unravel the dynamics of brain cells. For example, in the case of ALS, which Pasterkamp is researching. This motor disorder causes the death of brain cells that are responsible for muscle control. The result: patients slowly lose the ability to walk, the power of speech, and the ability to breath, until they die a few years later. There are a number of genetic anomalies that mean that people have an increased chance of ALS. But the big question is: how does such a mutation lead to the death of control cells? And how can this process be stopped? Comparing brain organoids made of cells from ALS patients with organoids on the basis of healthy cells offers Pasterkamp a valuable window into the disease mechanism.

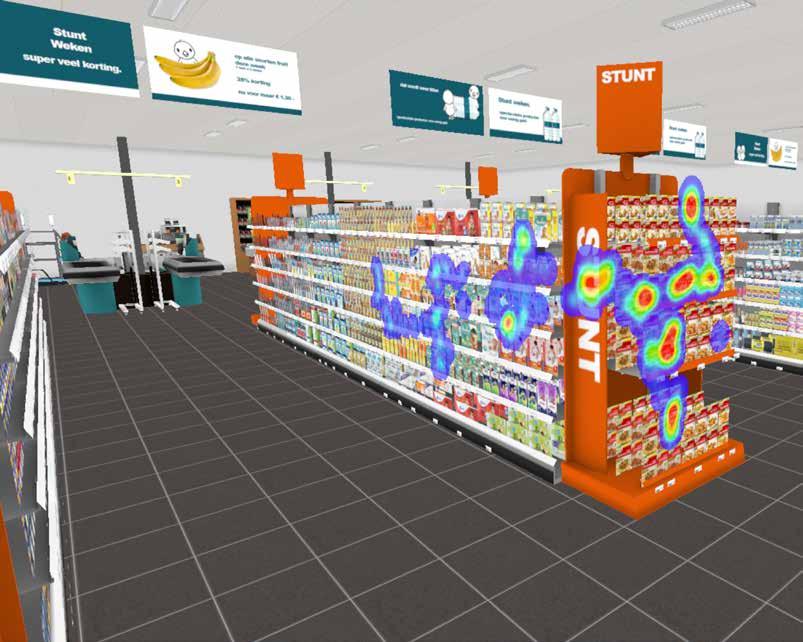
Part of this comparison takes place in a darkened room, a few doors down from the lab with the organoid incubators. In the semidarkness, there are two large microscopes connected to impressive-looking computer screens. Pasterkamp and his colleagues examine the mini-brains at various stages in the development of the ALS and control organoids. Step one in this process is decolorizing. By extracting the fats from the tissue, the dull pink matter changes into a transparent, gelatinous substance. Within this transparent tissue, the researchers color only those cells that they are interested in, e.g. all microglia, the brain’s cleaning cells. Then they place the organoids under a microscope, which scans the tissue layer by layer, over the course of many hours. All these layers are then digitally reassembled to form an extremely high-resolution 3D image of the organoid. The researchers zoom in on these images: what happens to this tissue at a cellular level? What do, for example, the synapses, the contact points between brain cells, look like? Are they still intact or are they attacked by the cleaning cells in the brain, as seems to be the case in ALS? In parallel, the scientists analyze what happens within the brain cells. Are specific genes allocated for the production of protein when things go wrong in the ALS organoid? Genes that are not active in the healthy organoids? Pasterkamp: ‘If, on the
one hand, we see irregularities in the 3D imaging of the ALS organoids and, on the other hand, anomalies in protein production in those organoids, we are given an idea of the molecular mechanisms that underlie the disruption at the cellular level.’
Getting to work You have to have a bit of luck with the anomalous proteins that Pasterkamp identifies in this way, he says. ‘Sometimes these are proteins of which the function is known. And occasionally, it is a function that you already know how to manipulate. If the anomalous proteins play a role in, say, controlling ion channels that determine whether a nerve is activated, you can manipulate this with anti-epileptic drugs.’ This brings the professor to the next miracle of the organoids. Instead of setting up expensive and risky medical studies with real patients, you could potentially test a new drug on the organoids in the Petri dish first. Do they behave more ‘normally’ when you put a few drops of an anti-epileptic drug in their bath? Pasterkamp: ‘You can see the effects of medication immediately. That could show which drugs are worth further study on human subjects.’
Organoids also offer a solution for research into psychological disorders. Professor of Glia Biology Elly Hol focusses on a neglected part of the brain: the glial cells. These cells are just as numerous as nerve cells but were originally less appealing to researchers because their activity is more difficult to measure. Their name alone is ominous: glia is ancient Greek for ‘glue’; they were long seen as the glue that supported the brain cells. We now know that they do play an active role. They participate in the chemical communication between cells, help to speed up signal transmission, and are responsible for cleaning up waste. Hol suspects that the cells play a crucial role in Alzheimer’s, to which she has devoted the majority of her research, and in schizophrenia, to which she is taking a research excursion as the PhD supervisor of, among others, Paul Ormel.
When it comes to the complex developmental disorder schizophrenia, glial cells are under suspicion. Schizophrenia patients have episodes of severely disrupted perception and thought; for example, they hear voices that comment on their actions. This could be connected to a disruption of one of the curious developmental processes in the brain. During learning and development in childhood, countless connections are created between brain cells. These connections are like experiments of the brain. Some prove useful – for example, they assist in the newly acquired skill of solving differential equations – are used more often, and take root. Other prove not very useful, fall into disuse, and are ultimately ‘pruned’ by the tidying microglia. In schizophrenia patients, many connections are missing. It is thought that this might be caused by overzealous cleaning cells that – perhaps as a result of miscommunication – prune too many connections and cause something similar to a short circuit. Analogous to unravelling the differences between brain organoids of ALS patients and healthy people, Hol and Ormel are exploring the differences between organoids of patients with schizophrenia and those of healthy people at the cellular, genetic, and protein levels.