Celebrating student diversity



FALL 2022
Nurse-midwifery at 50 How the program has grown up LGBTQ+ health Trends nurses should know The afterglow of IGNITE Nursing helps UIC’s capital campaign make history
With the launch of IGNITE: The Campaign for UIC, we embarked on a journey to do no less than shape the future. Eight years and $37.5 million later, our donors—alumni, faculty, staff, students, patients, friends and partners—have done it. Thank you for creating opportunities for hungry minds, empowering faculty educators and scientists, and connecting us to communities near and far.









Read more on p. 28. And please remember that your gifts are always appreciated investments, even in the quiet period between campaigns. Give today at go.uic.edu/GiveToNursing.

UIC Nursing debuts its 3D printer (p. 11)
12 Accomplished Alumni
Meet the 2022 recipients of UIC Nursing’s top alumni awards.


14 Beyond a Buzzword
Students of color made up more than half of UIC Nursing’s student body this fall. Why it matters.
18 Dean’s Dream Team
Representing a diversity of backgrounds and experiences, meet the team that’s prepared to lead the college forward.
20 50 Years of Nurse-Midwifery Born of necessity, the first-ofits-kind program has grown up to meet the needs of the times.
DEPARTMENTS

2 Dean’s Message

3 Notepad College of Nursing news
24 Student Spotlight
Sabrina Jamal-Eddine brings disability justice to nursing.


26 Focus on Education Study abroad spans from the Caribbean to Africa.
28 IGNITE Impact
The campaign ends with all expectations exceeded.
31 Research Round-up Highlights from UIC nurse scientists

34 Expert Viewpoint
Two faculty discuss trends in LGBTQ+ health.
36 Around the State
Updates from Peoria, Quad Cities, Rockford, Springfield and Urbana
40
Looking Back

The early years of academic computing
DEAN
Eileen G.
On the cover:
Jessica Dudley, DNP ’20, MS ’17, RN, stands in front of her childhood home in South Chicago. Dudley, working on her post-DNP midwifery certificate, is part of an increasingly diverse UIC Nursing student population. (see p. 14)
GRAPHIC DESIGNER
Joanne Chappell CONTRIBUTING PHOTOGRAPHERS
Mark Mershon, Joshua Clark, Diane Smutney
UIC COLLEGE OF NURSING OFFICE OF MARKETING AND PUBLIC AFFAIRS
Lauren Diegel-Vacek, DNP, FNP-BC, CNE, FAANP, Executive Associate Dean (Interim)
Liz Miller, Director, Marketing and Public Affairs
Joanne Chappell, Graphic Designer

Jennifer Samples, Digital Content Strategist
Deborah Ziff Soriano, Editorial Writer
Vital Signs is published for the alumni, faculty, students and friends of the University of Illinois Chicago College of Nursing. © 2022
Your comments are welcomed: University of Illinois Chicago College of Nursing (MC 802) 845 S. Damen Ave. Chicago, IL 60612
Phone: 312.413.2337 Email: lhmiller@uic.edu Web: nursing.uic.edu Facebook: @uic.con Twitter: @uicnursing Instagram: @uicnursing LinkedIn: @UIC-College-of-Nursing
20
Volume 37
Collins, PhD, RN, FAAN, ATSF CHIEF EDITOR Liz Miller MANAGING EDITOR & WRITER Deborah Ziff Soriano CONTRIBUTING WRITERS
Lori Botterman, Liz Miller, Laura Fletcher
FEATURES 14
Snapshots from REUNION 2022 (inside back cover)
FALL 2022
This fall, while hosting more than 100 UIC pre-nursing students for an open house at our building in Chicago, I reflected on how much has changed for the better since spring 2020.
Those were days of relatively empty hallways, classrooms and labs, and now our campuses are buzzing once again, filled with the energy and enthusiasm of future and current nurse leaders (still using sensible precautions).
I completed my first full year as dean in September. Since the start, I’ve been putting in place my “dream team” (see p. 18) of associate and assistant deans to help guide the research, practice and educational missions of the college. They bring a remarkable breadth and depth of experiences, passions and ideas to their respective jobs. I don’t think it would be an overstatement to say that, together, they are the most diverse team ever to lead UIC Nursing, a fact that aligns with our vision of transforming health and health care by creating a pipeline of future nurse leaders with diverse backgrounds. For so many of our students who come from minority backgrounds (as you’ll read about on p. 14), my hope is that they will see themselves reflected in this team.
Another enormous highlight of the past year was the conclusion of IGNITE: The Campaign for UIC. Thanks to the participation of hundreds of generous donors, we surpassed our $33 million goal (see p. 28). I want to thank Dean Emerita Terri Weaver and Steven George, our former assistant dean for advancement who has since been promoted to university-level leadership as assistant vice chancellor for advancement. Terri and Steve steered us through seven of the campaign’s eight years, and our strong finish owes an enormous debt to their vision and leadership.
All in all, it’s been a fabulous year for the UIC Nursing community, and I am excited to tell you about much of it in the pages of this issue of Vital Signs.
On that note, it’s worth mentioning that, with this issue, we celebrate 30 years of Vital Signs magazine. It debuted in fall 1992, and collectively, the issues make up a sort of journal kept by the college, chronicling many of the people, initiatives and events that gave shape to all that we are today. Though much has changed over 30 years, including an evolving sense of what it means to bring more health equity to our communities, our commitment to driving discovery through research and preparing the best nurses, nurse scientists and nursing educators, has been essential to UIC Nursing all along.
 Eileen Collins, PhD, RN, FAAN, ATSF Professor and Dean
Eileen Collins, PhD, RN, FAAN, ATSF Professor and Dean


UIC
College of Nursing
2 | College of Nursing DEAN’S MESSAGE
Diving in!



For the first time in three years, UIC College of Nursing bachelor’s degree students revived the decades-old tradition of celebrating graduation by jumping into a pool in their scrubs.


The annual rite of passage was sidelined during the COVID-19 pandemic. But students at all three of the college’s bachelor’s degree-granting campuses— Chicago, Urbana and Springfield—brought back the literal plunge this year, which is symbolic of their plunge into the nursing profession. (See p. 36 for more on Springfield and Urbana jumps.)
The tradition began on the Chicago campus sometime in the early 1980s and took root by word of mouth, each class of undergraduate students passing it on to the next.
Across the three campuses, around 100 students took part in the event, which was covered by CBS 2 Chicago, the Chicago Tribune and the State Journal-Register.
Overall, 344 bachelor’s, master’s, DNP and PhD students graduated in spring 2022.
VITAL SIGNS FALL 2022 | 3 NOTEPAD
U.S. NEWS & WORLD REPORT RANKINGS FOR 2023 RN to BSN completion program #11 DNP program #13 MS program # 9 BSN program #3
UIC Nursing clinical assistant professor Karen Cotler, left, is the lead provider at the Center on Halsted clinic, Cotler is assisted by students, pictured here with Lauren Koenig, DNP ’22.












STUDYING PrEP IN A DIFFERENT POPULATION
UIC Nursing clinical assistant professor Randi Singer received a grant to study whether “Centering”—a community empowered group health care model—is feasible and acceptable for PrEP education, navigation and adherence among sex workers. Singer and her team, in collaboration with sex workers and a community advisory board, will conduct a pilot study with a federally qualified health center.








Getting to zero
A UIC College of Nursing and UI Health clinic based at Center on Halsted is finishing up its second year of bringing HIV prevention and STI treatment services to the center’s LGBTQ+ community members.

UIC Nursing clinical assistant professor Karen Cotler, DNP, FNP-BC, FAANP, is lead provider for the weekly clinic, which offers HIV pre-exposure prophylaxis (PrEP), a medication-based strategy to prevent HIV infection, and universal STI screening. The clinic opened in January 2021.
APPLAUSE!

Wiphawadee Potisopha, PhD ’21, won an American Heart Association 2022 Paul Dudley White International Scholar Award.
Ariel Smith, PhD, RN, assistant professor, was selected to join the 2022 Sinai Urban Health Institute Equity Research Fellows program.
“It’s been a success,” Cotler says. “We’re getting a lot of people on PrEP who might not have been on it otherwise, and we’re treating a lot of STIs. I’m proud of a service that really does make an impact on infectious disease in the community.”

The clinic is aligned with the state of Illinois’ Getting to Zero initiative, which aims to end the HIV epidemic in the state by 2030.
“A PrEP clinic is what we see as the next evolution in HIV/AIDS care that we can be part of to get Illinois to zero new infections by 2030,” says Kim Fountain, chief administrative officer at Center on Halsted. “UIC Nursing has always been a trusted partner and is the perfect match for what we want this clinic to be.”
Center on Halsted, located in Chicago’s Lakeview neighborhood, is a comprehensive LGBTQ+ community center that offers cooking classes, yoga, group therapy and more—and is visited by more than 1,000 community members each day.
The center has long offered walk-in HIV testing, but previously referred community members to other sites for further treatment. Now, individuals who test negative—a prerequisite for PrEP treatment—are referred to the in-house clinic to be evaluated as candidates for PrEP.
Clinical assistant professor Denise Bockwoldt, PhD, FNP-BC, CDE, was chosen for the 2021 Marie Lindsey Spirit of Advanced Practice Nursing Award on behalf of the Illinois Society of Advanced Practice Nursing (ISAPN) Awards Committee and the ISAPN Board of Directors.
4 | College of Nursing
NOTEPAD
“I’m proud of a service that really does make an impact on infectious disease in the community.”
—Karen Cotler
[L-R] Dean Emerita Terri Weaver, then-associate dean of equity and inclusion Phoenix Matthews, Dean Eileen Collins, UHP assistant director Charese Smith, and then-student Adam Saleh, BSN ’22, cut the ribbon on the new center in May.



Centering student success
The new Center for Academic Excellence and Cultural Engagement in the Chicago campus building is a “second home” for students, says Adam Saleh, BSN ’22.
The center, initiated by requests from students, will serve as a place for students to study, receive academic support and take part in programming, such as wellness sessions, lunch-and-learn sessions, cultural exhibits and inclusive dialogue circles.
“I am happy for the future generations of nursing students that will get the opportunity to engage in this center where transformational dialogue will take place and feelings of belonging for students of all backgrounds will be guaranteed,” says Saleh, who spoke at the center’s unveiling in May 2022.





The space and its programming will be managed by staff at the Clinical Learning Resource Center and Charese Smith, assistant director for the Urban Health Program.



The center is largely funded with internal college funds, in addition to a philanthropic gift from Terri Weaver, PhD, RN, FAAN, ATSF, FAASM, dean emerita of UIC Nursing, and her husband, Bruce Fiedler.








Five faculty from the UIC College of Nursing were named to the 2022 class of fellows of the American College of Nurse-Midwives, including: instructor Erin Farah, PhD ’16, MS ’05, BSN ’00, CNM; associate professor Mary Dawn Koenig, PhD, CNM; instructor Elizabeth Muñoz, DNP, CNM; clinical assistant professor Pamela Pearson, DNP ’18,
CNM;
instructor Ellen Solis, DNP, CNM
Associate professor Judith Schlaeger, PhD, MS ’88, BSN ’80, CNM, LAc, FACNM, FAAN, was selected for the 2022 Mid-Career Award by the Midwest Nursing Research Society’s Symptom Science Research Interest and Implementation Group.

VITAL SIGNS FALL 2022 | 5 NOTEPAD #UICPROUD
NOTEPAD
Mary Dawn Koenig
UIC




Prof’s efforts improve umbilical cord care in Haiti

From the time she began leading medical teams to a clinic in Haiti in 2006, UIC Nursing clinical associate professor and pediatric nurse practitioner Susan Walsh, DNP ’14, MS ’00, BSN ’80, CPNP-PC, noticed that newborns were developing infections—sometimes fatal—from traditional umbilical cord practices in the region.


These practices—which involve covering the cord stub with cloth bindings and substances, such as herbs, ash or even animal excrement—were thought to protect the baby, but instead introduce germs and cause infection.

Walsh set about studying the issue in partnership with Global Health Action, a nonprofit organization that has worked in Haiti since 1982. Together, they conducted a community campaign among pregnant women and lobbied the Haitian Ministry of Health for approval to bring potentially life-saving medicine into Haiti.


This years-long effort paid off in late 2021 when the Haitian government officially added 7.1% chlorhexidine digluconate—a topical antiseptic that has been shown to reduce local infection to the cord stump—to the list of approved National List of Essential Medications on its website. Only medicine on that list can legally be brought into the country.
“It was really amazing that after all these years, it finally got accepted,” Walsh says. “Now [chlorhexidine] can be brought in and aid organizations can begin to save babies by implementing an information campaign and distribution process.
READ MORE visit go.uic.edu/WalshHelpsHaiti
APPLAUSE!

Rebecca Singer, DNP ’18, RN, was awarded a Fulbright fellowship to teach and conduct community service work in Sofia, Bulgaria, in spring 2022. Also, Singer has been elected President-Elect of the Global Alliance for Behavioral Health & Social Justice, formerly the American Othopsychiatric Association.
On Sept. 14, UIC cut the ribbon on the $194 million UI Health Specialty Care Building at the corner of Taylor and Wood Streets. The building includes six floors of patient care space and is projected to serve up to 800 patients per day.
College of Nursing
NOTEPAD
Nursing associate professor Susan Walsh sees an infant in a rural Haitian clinic.
FIRST RESPONSE















Monkeypox, or MPV, vaccinations were given to nearly 1,200 people at a mass vaccination event held at the UIC College of Nursing on Sunday, Aug. 14. The event was coordinated by the Outbreak Response Team, co-led by UIC Nursing assistant professor Rebecca Singer, DNP ’18, RN. The team included some 90 people from Rush University Medical Center and UIC, many of whom were volunteering their time.
Alum wins UIC’s highest honor
The UIC Alumni Association Board chose Sheila Dinotshe Tlou, PhD ’90, to receive the UICAA 2022 Alumni Achievement Award. This is the highest honor bestowed on UIC alumni by the university.






“Dr. Tlou’s life and work illustrate the profound influence nurses can have on both small and large scales,” says Dean Eileen Collins
Early in her career, Tlou was director of the nursing program at the University of Botswana, developing her nation’s nursing workforce and influencing care available to individuals and families. Her desire to have broader impact in her home country led her to serve as a member of Parliament in Botswana, then eventually as minister of health from 2004 to 2009.

From 2010 to 2017, she served as regional director of the joint United Nations Program on HIV/AIDS (UNAIDS), where her policies helped stem the spread of HIV.
Today, Tlou is co-chair of the UNAIDS-initiated Global HIV Prevention Coalition and co-chair of the Nursing Now Global Campaign, a project of the World Health Organization and the International Council of Nurses. She is also chancellor of Botswana Open University, appointed by the nation’s president in May 2021.
Among her many accolades, Tlou was named one of the “100 Most Influential African Women” in 2019.
In the UIC Nursing faculty awards program for 2022: Karen Cotler, DNP, FNP-BC, FAANP, received the Judith Lloyd Storfjell Distinguished Practice Award; Alana Steffen received the Distinguished Researcher Award; Phoenix Matthews, PhD, received the Julie & Mark Zerwic Diversity Award; and Crystal Patil, PhD, was named Distinguished Mentor of Faculty.
UIC Nursing adjunct professor Pamela Meharry, PhD, CNM, helped launch the first Master of Science in midwifery program at the University of Rwanda. The inaugural class began the program in April 2022.
Current DNP student Sheila Harmon, MSN, APRN, CDCES, was named the Illinois Diabetes Education Specialist of the Year for 2022 by the Illinois Coordinating Body of the Association of Diabetes Care & Education Specialists.
FALL 2022 |
NOTEPAD
SIGNS 7
A GOOD DAY FOR GIVING

























In what’s become a favorite annual tradition, Giving Tuesday 2022 gave students, staff, faculty and friends an opportunity to flaunt college pride and support mission-critical funds for scholarships, student emergency assistance, flexible spending, and equity and inclusion initiatives.







Dean Eileen Collins boosted the effort with a generous “challenge” gift, unlocked by the 100th donor.
“I was proud to take part and was even more proud that so many chose to join me,” Collins says.


Nursing profs can be comic book heroes
In a piece published in The Journalist’s Resource, comics journalist Josh Neufeld immortalized the work of UIC College of Nursing faculty members Randi Singer, PhD, Natasha Crooks, PhD, RN, and Singer, DNP ’18, RN.


In partnership with Noel Green at the Chicago Center for HIV Elimination and Jahari Stamps, a Chicago House Ball “father” with the House of Ferré, faculty worked to increase COVID-19 vaccination rates of Black and Latino LGBTQ individuals.
The comic, “Vaccinated at the Ball: A True Story about Trusted Messengers,” focuses on the use of community representatives to promote vaccinations at Chicago House Balls, which are events that celebrate Black and Latino LGBTQ+ culture.
The full comic ran in the Chicago Sun-Times on Sunday, June 26, the day of the 51st annual Chicago Pride Parade.
The team, including Crystal Patil, PhD, and Phoenix Matthews, PhD, published a paper in the American Journal of Public Health in January 2022 about their use of “ballroom icons”—leaders who represent the community—to overcome mistrust and misinformation.
The comic also illustrates Stamps getting vaccinated at a ball, and later getting his booster at #JamOutSaveLives, a vaccination clinic and jam session held in Chicago’s Jackson Park, where UIC Nursing students administered the vaccines. A video made from the event has been viewed more than 1 million times on Instagram.
SEE MORE See the full comic at journalistsresource.org.
8 | College of Nursing NOTEPAD
Rebecca
Quinn named to Hall of Fame Philanthropy at work Irwin Chair
Geraldine Gorman, PhD, RN, has been named the inaugural Kathleen M. Irwin Endowed Clinical Chair in Outstanding Nursing Practice. The appointment took effect August 16.
The chair was established last year with a gift from G. Steven Irwin, MD, in accordance with the wishes of his late wife, Kathleen, a nurse, to support an outstanding clinical faculty member who is active in nursing practice.
Gorman has taught at the College of Nursing since 2002 and maintained a clinical practice in hospice and palliative care throughout that time.
Werley Chair


Ardith Z. Doorenbos, PhD, RN, FAAN, has been selected as the Harriet H. Werley Endowed Chair for Nursing Research, the college’s top honor for research faculty.
The Sigma International Nurse Researcher Hall of Fame member is internationally recognized for her contributions to palliative care, oncology and pain and symptom management.

Kim Scholar
Shannon Halloway, PhD, RN, FAHA, FAAN, has been selected as the inaugural Heung Soo & Mi Ja Kim Endowed Faculty Scholar. The honor, made possible by a generous gift from Dean Emerita Mi Ja Kim and her husband, is designated to support an outstanding faculty member who demonstrates excellence in research.
Halloway, a 2022 American Academy of Nursing Fellow who studies the benefits of physical activity on cardiovascular and brain health, comes to UIC Nursing from Rush University College of Nursing.
Minnich Professorship
Lauretta Quinn, PhD ’96, RN, FAAN, FAHA, CDE, was named the second holder of the Katherine M. Minnich Endowed Professorship.


Katherine Minnich, who had narcolepsy, made her gift to promote sleep research. Quinn’s internationally-recognized work (see next column) on metabolism, diabetes and sleep positions her well to lead the college’s Center for Sleep and Health Research.
Quinn poses with two campers at the American Diabetes Association camp, where she volunteers almost every summer.



Lauretta Quinn, PhD ’96, RN, FAAN, FAHA, CDE, Katherine M. Minnich Endowed Professor and director of the Center for Sleep and Health Research at the UIC College of Nursing, has been inducted into the International Nurse Researcher Hall of Fame, one of 32 nurse researchers from around the world selected for the honor in 2022.
“These inspiring, world-renowned nurse researchers represent the staggering, collective impact of nursing and nursing research on global health care,” said Sigma President Kenneth Dion, PhD, MBA, RN, FAAN.
Sigma inducted the new honorees at its 33rd International Research Congress in Edinburgh, Scotland, in July. In her research, Quinn has tackled questions of how physical activity and stress affect metabolic processes and diabetes management, including cutting-edge work to develop an “artificial pancreas.”
Quinn became the 11th faculty member or alumna from the UIC College of Nursing to be inducted.

VITAL SIGNS FALL 2022 | 9 NOTEPAD
A team of Black midwives, doulas and nurse navigators has been hired to carry out the Melanated Group Midwifery Care model in an effort to improve pregnancy outcomes for Black people.

The model is funded with a $7.1 million grant from the Patient Centered Outcomes Research Institute in which Karie Stewart, MS ’17, CNM, MPH, a UI Health midwife, Kylea Liese, PhD, CNM, a UIC Nursing assistant professor, and Stacie Geller, PhD, are principal investigators.
The Melanated Group Midwifery Care model is a multipronged strategy to improve Black people’s experiences in pregnancy and postpartum: Black pregnant people are matched with Black midwives; a Black nurse coordinates care; and a Black doula provides in-home support for the patients for up to a year after delivery. The model also calls for prenatal care to be provided in a group setting for peer support.
The study will enroll 435 patients over the course of five years, comparing experiences and outcomes of patients receiving traditional care with those receiving care using the new model.
The site of the study shifted from University of Chicago Medicine to UI Health, and researchers are now recruiting pregnant people who identify as Black.
“We were really trying to be intentional about diversifying the midwifery practice, making the practice reflect the population we serve,” says Stewart, who is also a PhD student at UIC Nursing. “If we’re really serious about addressing Black maternal health in Chicago, we have to lay the groundwork for a new model of care, and that means having the providers and facilities for this relatively radical shift in health care delivery.”
10 | College of Nursing NOTEPAD
Melanated Group Midwifery Care team [L-R]: Chelsia Love, CNM, APRN; Hannah Howell, RN, nurse navigator; Amber Rideout, CNM; Tayo Mbande, lead doula (co-founder of Chicago Birthworks Collective); Pamela Pearson, DNP, CNM, (also director of the UIC Nursing DNP program in nurse-midwifery); Cynthia Jacinthe, CNM; Jessica Ogwumike, MPH, research coordinator; Karie Stewart, CNM, MPH, co-principal investigator; Crystal Stamps, CNM
In Chicago, Black women are six times as likely to die of a pregnancyrelated condition as non-Hispanic white women, according to the Illinois Department of Public Health.
Melanated midwives find home at UI Health
NURSING EDUCATION

The UIC College of Nursing received its first 3D printer thanks to funding from the Consortium of Academic and Research Libraries of Illinois.

Clinical associate professor Karen Vuckovic, PhD ’13, ACNS-BC, FAHA, is principal investigator on the grant, which will also allow her to create an open educational text in pharmacology for advanced practice nursing students.
Vuckovic says the 3D printer will help students visualize certain complex components of pharmacology, such as how drugs interact with G-protein receptors. She also sees future use in patient education and hopes it may lead to collaborations with other UIC health science colleges. Upon completion of the grant, the 3D printer will be housed at UIC’s Library of the Health Sciences.



Mobilizing to help teens
The College of Nursing secured a $3.1 million grant from the federal Health Resources and Services Administration, an agency of the Department of Health and Human Services, to run a mobile health unit for underserved teens in Illinois.

The unit will operate for four years in disadvantaged rural and urban areas of the state, providing services to improve teen health and well-being, including reproductive health services such as well visits, contraceptive management and screening for sexually transmitted diseases. The unit will also provide point-of-care tests for pregnancy and reproductive health.
Kelly Rosenberger, DNP ’12, CNM, WHNP-BC, FAANP, associate professor and director of the UIC College of Nursing’s campus in Rockford, will serve as principal investigator for ENRICH, which stands for Enhancing Nursing Education and Retention by Initiation of Care Delivered by Mobile Health Units. Rosenberger was inspired to launch the program after seeing the critical need among vulnerable high school students in rural Illinois for access to reproductive health services and STI prevention and treatment.
In addition to providing needed services to teens, the mobile unit program will also provide clinical training to Doctor of Nursing Practice students, as well as other students at UIC Nursing’s six urban and rural campuses.
Within days of its arrival, the Josef Prusa printer passed its first test: printing a pre-loaded model of a small dog. The printer’s academic purpose is to help students visualize complex components of pharmacology.
VITAL SIGNS FALL 2022 | 11 NOTEPAD
Accomplished alumni
In 2022, the UIC College of Nursing conferred the 44th annual Distinguished Alumni Award and honored the fifth class of Outstanding Alumni Achievement Award winners
Distinguished Alumni Award Sue Penckofer
PhD ’93, MS ’82, BSN ’79, RN, FAAN • Emeritus professor, Marcella Niehoff School of Nursing at Loyola University Chicago
Sue Penckofer wanted to be a nurse as far back as she can remember. Her father, a Chicago firefighter, encouraged her to go to a diploma program—a specialized program that resulted in nursing licensure, but not a college degree.
Penckofer objected.
“[It was a different time, and] in his mind, women never got a college education,” she recalls. “I said, ‘no, I have to go to a university. I have to get a college education.’”
Penckofer went on to earn not one, but three degrees from the UIC College of Nursing, and made her career in academia at Loyola University Chicago, rising to associate dean for the Graduate School.

Over the course of her career, Penckofer made important strides in understanding cardiovascular disease risk among women. She also worked on influential therapies to treat depression in women with diabetes, long before the topic of mental health was mainstream.
READ MORE


Visit go.uic.edu/MeetNursingAlumni to read full profiles of our award winners.
The college is accepting nominations for the 2023 Alumni Awards Program through February 15. Nominate a colleague at go.uic.edu/NursingAlumAwards.
Through a large scale, NIH-funded study on the use of vitamin D to relieve depression in women with type 2 diabetes, Penckofer demonstrated that even a low dose of vitamin D was effective at improving mood, making it a cost effective option for patients.
“[Sue] is a stellar alumna, who has improved the daily lives and health of women with diabetes by providing relief of depressive symptoms,” says UIC Nursing professor emerita Carol Ferrans, PhD ’85, MS ’82, RN, FAAN, and Penckofer’s former classmate.
12 | College of Nursing
Penckofer describes her experience at UIC as “wonderful” and credits her exacting advisors with helping her to become a scholar.
“To this day, I think the University of Illinois Chicago has the best education in the state of Illinois,” she says.
Over the course of her career, Penckofer has published more than 60 papers and has served as the chair of more than 30 dissertation committees. She’s proud of her students who have gone on to obtain NIH funding and assume prestigious positions across the country, among them UIC College of Nursing Dean Eileen Collins, PhD, RN, FAAN, ATSF.
“It brings me pleasure to see [my students] become even more successful than I’ve been,” she says. “It feels good that my students have gone on to carry on nursing science.”
Outstanding Alumni Achievement Awards
Lilian Ferrer
PhD, MS ’01, FAAN



Professor and vice president for international affairs at Pontificia Universidad Católica de Chile
Lilian Ferrer is a risk-taker. At the age of 25, Ferrer moved from Santiago, Chile, to Chicago with her husband and young son to pursue her master’s degree in public health nursing at the UIC College of Nursing.
She says she knew by observing nursing abroad that she could learn “how to better improve or do things here in Chile.”


Now, Ferrer has made globalism a hallmark of her approach to her work.
Over the course of her career, Ferrer has conducted cutting-edge work on HIV/AIDS prevention in Chile, worked to establish a culture of internationalism at her university, and promoted the training of advanced practice nurses.
“Being a nurse means I’m part of a group of people who care about others, who care about human beings,” Ferrer says.

In addition to nursing, Ferrer says she’s most proud of her family: her husband and eight children, who range in age from 6 to 27 years old.



Sarah Ailey
PhD ’02, MS ’98, BSN ’96 Professor at Rush University College of Nursing

Sarah Ailey’s son is her muse. Now 46, he was born with an intellectual disability. It was Ailey’s experiences navigating the health care system that led her to her life’s work—improving the lives of those with intellectual disabilities.

“I’ve been through the health care system with him, and have seen its better and worse sides,” says Ailey.


Ailey’s research found that individuals with intellectual disabilities are more vulnerable to depression, aggression and challenging behavior as they get older.
She developed an intervention delivered in Chicago-area group homes to enhance social problem-solving skills for residents and staff; co-hosted a national conference to address issues and standards of care for individuals with intellectual disabilities; and is addressing the lack of content about individuals with intellectual and developmental disabilities in interprofessional health care curriculum.
VITAL SIGNS FALL 2022 | 13
BEYOND A BUZZWORD



At the UIC College of Nursing, diversity is a reality that students are immersed in every day. In fall 2022, for the first time ever, more than half of the college’s students were racial or ethnic minorities, infusing critical experience and perspectives into the future nursing workforce.
Jasmine Medina, BSN ’22, chose UIC for its diversity.
From a Puerto Rican family living in a predominantly Latino neighborhood of Chicago, Medina didn’t want to go to a college where her racial and ethnic identity would stand out. She wanted to be around students who looked like her, while also getting exposure to people with a wide variety of backgrounds.
“Going to school at the UIC College of Nursing, you just look at all of the students in class with you, and it’s diverse,” Medina says. “They come from a bunch of different backgrounds, and I’ve learned a lot from them – their struggles and their barriers.”
So, when she applied to give the UIC College of Nursing student commencement address, she knew she wanted to make diversity the hallmark of her speech.

On stage in May, she asked her fellow graduating students to stand if they fit into one of four categories: a racial or ethnic minority group; a first-generation college student; a DREAMer (brought to the U.S. as a child) or bilingual.
“ GOING TO SCHOOL AT THE UIC COLLEGE OF NURSING, YOU JUST LOOK AT ALL OF THE STUDENTS IN CLASS WITH YOU, AND ITʼS DIVERSE.” —Jasmine Medina
By the time she finished, she estimates at least two-thirds of the graduates were standing, and the audience was roaring with applause.
“I really wanted to do a speech for the students,” she says. “Seeing that [much diversity] is not something you see all the time, and those students worked super, super hard.”

14 | College of Nursing
UIC is one of the nation’s most diverse public research institutions, ranked among the 25 most diverse schools in the nation in U.S. News & World Report’s ethnic diversity index.
Within UIC Nursing, the diversity of the student body has been growing each year. In fall 2022, for the first time, more than half of the students identified as racial and ethnic minorities. That compares to 2014-2015, when just 35% of students were in that category, which includes Asians, African Americans, Hispanics, international students, and those who identify as multi-race.
And while UIC cultivates diversity broadly (including veterans, students with disabilities, sexual and gender minorities, and more), there has been a deliberate effort in the College of Nursing to recruit and support students of color, who have historically been underrepresented in the nursing profession.
IN FALL 2022, FOR THE FIRST TIME, MORE THAN HALF OF UIC NURSING STUDENTS IDENTIFIED AS RACIAL AND ETHNIC MINORITIES.
“It’s important because Hispanics, African Americans and Native Americans—they make up a large portion of the U.S. population,” says Rose Hernandez, PhD, UIC Nursing associate dean for equity and inclusion. “But there have been barriers, sometimes through systemic or structural violence, that have kept some of these students out of academia.”
Hernandez says it was in large part her own story that drew her to UIC Nursing. The daughter of Mexican immigrants, her father never had any formal schooling, only learning enough to sign his name. Hernandez grew up in Chicago and was introduced to higher education—and UIC specifically— through the Urban Health Program, which recruited at her high school. Hernandez got three degrees from UIC, with a PhD in public health.
“That’s the story of many of our students,” Hernandez says. “Their parents are coming from different parts of the world, coming to the U.S. for the first time, and often not knowing how to navigate the university environment. How do we build the system at UIC Nursing that allows students that share that type of background to succeed?”
The program was established 43 years ago to address “the injustices that underrepresented minorities faced in gaining admission to some of our health science programs,” says Charese Smith, who has led the UIC Nursing division of the program since 2009. Now the program involves 538 nursing students, about a third of the college’s student body.
ABOUT 1/3 OF NURSING STUDENTS ARE PART OF THE URBAN HEALTH PROGRAM.
But Smith says it’s not enough to just bring students into the program. They also need to feel like they’re in a safe space. She wants students to know: “We support you; we want you to do your best; and we want you to excel while you’re here.”
Hernandez credits the Urban Health Program with allowing her to meet mentors and friends who shared similar backgrounds, championing her academic ambitions. “To see someone from my own background, doing this type of work [in higher ed], was encouraging to me,” she says.
The program’s signature series is the Seminars for Excellence in Nursing Sciences Program, which helps prepare incoming Urban Health Program students for the rigors of nursing coursework. A peer-mentoring program launched in 2021 focuses on the psychological and emotional well-being of students, featuring sessions on topics like coping with microaggressions and adversity.
The Chicago campus also opened the Center for Academic Excellence and Cultural Engagement in spring 2022—a brick-and-mortar space intended to promote academic success and build a sense of inclusion and respect for diversity among all students, not only those from minority backgrounds. [See p. 5 for more on the new center.]
VITAL SIGNS FALL 2022 | 15
0%10%20%30%40%50% 2022 2021 2020 2019 2018 BLACK/ AFRICAN AMERICAN ASIAN
DIVERSITY
MULTI-RACE INTERNATIONAL HISPANIC
The population of students of color at UIC Nursing has increased steadily over the past 5 years.
GOAL
37% OF 2022 GRADUATES INTEND TO WORK WITH RURAL OR MEDICALLY UNDERSERVED POPULATIONS

When a student graduates from UIC Nursing’s bachelor’s, master’s or DNP program, the college asks if they intend to work with a largely rural or medically underserved population. In 2021-22, about 37% of respondents said yes.
Jessica Dudley, DNP ’20, MS ’17, RN, is one of those graduates. She loves Chicago and says she never wants to leave. She’s from the working-class neighborhood of South Chicago on the Southeast side of the city, one of six children raised by a single mom.
“I’m very grateful to [my mom] because she gave me so many unique experiences, like sleepovers at the Field Museum,” Dudley says. “I never felt like the poor little girl from the South Side.”
Although Dudley’s family lived below the poverty line, she spent her childhood playing outside, biking, going to the park and museums. She always had food, clothes and supplies for school. Her experiences were far from the stereotypical images of the South Side depicted in media, but she still noticed qualities about her neighborhood that she questioned.

DUDLEY
“I’m not [criticizing] my neighborhood,” she says. “I love where I came from. But we had candy stores on every corner in my neighborhood. There was a liquor store down the block from my church. I didn’t understand why my neighborhood had so many liquor stores, especially with the number of folks you would see who were alcohol dependent.”
16 | College of Nursing
IS NOW DETERMINED TO EFFECT CHANGE AND IMPROVE HEALTH OUTCOMES— SPECIFICALLY BIRTH OUTCOMES AMONG PEOPLE OF COLOR.
Dudley connected some of these neighborhood qualities to the general health of her community. As a student in UIC’s Advanced Generalist Master of Science/graduate-entry program, Dudley was able to name what she had observed: social determinants of health.
Dudley is now determined to effect change and improve health outcomes—specifically birth outcomes among people of color. She is currently a labor and delivery nurse at UI Health. As she’s progressed through her UIC Nursing education—from the master’s program, to a DNP in advanced population health, and currently to a post-DNP certificate in midwifery—one goal has remained constant: “I knew for sure I wanted to advocate for and work with people like the ones I grew up with in Chicago,” she says.

The trend toward increasingly diverse classes at UIC Nursing stems in part from a change to holistic admissions in 2014. Then, the college began incorporating an applicant’s experiences and attributes into admission decisions, in addition to using traditional academic metrics.
Concerns about potential negative outcomes—such as declining graduation or NCLEX pass rates—were unfounded, according to a 2018 study of the program. College leaders believe strongly that admitting students with a diversity of backgrounds means all UIC Nursing students become better equipped for patients they will encounter in practice.
“One of the goals behind increasing student diversity is to expose all students to different views and perspectives,” says Dean Eileen Collins. “We want students, in partnership with faculty, to be in dialogue and to share lived experiences that might help each other connect with their patients. Regardless of their background, all students benefit from a diverse student body and can bring what they learn into their practice.”
Increasing student diversity also serves to “infuse the health professions workforce with practitioners that can serve their community,” says Smith.
NURSES WHO CAN SPEAK A PATIENTʼS NATIVE LANGUAGE—IF ITʼS NOT ENGLISH—CAN BE CRITICAL TO ENSURING PATIENTS GET APPROPRIATE CARE AND CONTINUE TO SEEK IT.
The nursing profession remains predominantly female and white. The National Nursing Workforce Study in 2020 found about 19% of RN respondents self-reported as minority, while about 42% of Americans are non-white, as of 2020.
Nurses who can speak a patient’s native language—if it’s not English—can be critical to ensuring patients get appropriate care and continue to seek it. Medina says she noticed this among her community in Humboldt Park.
“I’ve seen it with my own eyes,” she says. “A lot of patients don’t go to the doctor because they fear they won’t be understood. [They wonder:] ‘Why can’t I have someone I can speak to?’ It makes the visit unfair and less meaningful.”
In her commencement speech, Medina imagined a different reality for her community and others like it.
“Now imagine looking into your patient’s eyes and saying, ‘It’s ok. Yo hablo Español. I speak Spanish.’ Think about the happiness that they will feel. Diversity in health care fields is essential. UIC will be sending out future nurses that are diverse and well-rounded.”
VITAL SIGNS FALL 2022 | 17
Jessica Dudley, DNP ’20, MS ’17, RN, has fond memories of running track as a high school student in South Chicago at Eckersall Stadium, a spot that she frequented with her friends.
Dean’s Dream Team
Since her appointment in September 2021, Dean Eileen Collins has assembled a diverse cadre of experienced leaders to help her accomplish her goals across all aspects of the college’s mission-driven work. Meet the dean’s energetic, innovative and collaborative leadership team.

Assoc. Dean for Research
Previous role: Assoc. Dept. Head, UIC College of Pharmacy
Lauren Diegel-Vacek, DNP ’10, MS ’02, FNP, CNE, FAANP
Int. Executive Associate Dean
Previous role: DNP Program Director, UIC Nursing
Jon Morelos, JD Assoc. Dean for Administration
Morelos has been in this role since 2011
READ MORE Read bios of all these leaders at go.uic.edu/NursingDreamTeam.
Previous role: Development Officer, Chicago Botanic Garden
18 | College of Nursing
Lisa Sharp, PhD
Jill Corr Asst. Dean for Advancement
Carolyn Dickens, PhD ’17, ACNP, FAANP
Int. Assoc. Dean for Faculty Practice and Community Partnerships
Continuing roles: NP and Asst. Director of Advanced Practice Providers, UI Health
Rohan Jeremiah, PhD, MPH Assoc. Dean for Global Health
Previous role: Assoc. Professor, UIC School of Public Health


Elizabeth Aquino, PhD ’13, RN Assoc. Dean for Academic Affairs
Previous role: Assoc. Professor, School of Nursing, DePaul University
Rosalba Hernandez, PhD, MPH Assoc. Dean for Equity and Inclusion
Previous role: Assoc. Professor, School of Social Work, University of Illinois at Urbana-Champaign
VITAL SIGNS FALL 2022 | 19
When the UIC College of Nursing opened its nurse-midwifery degree program in 1972, it was the first of its kind in Illinois.

Fifty years later, it’s still the only brick-and-mortar program in the state, and boasts more than 500 alums, including nurse-midwifery leaders scattered across the country and world.





The beginning
The nurse-midwifery program at UIC Nursing was born of a mutual need, says Carrie Klima, PhD, MS ’86, CNM, FACNM, who was the director of the nurse-midwifery program from 2012 to 2022.
Augusta Webster, then head of obstetrics at Cook County Hospital, was keen on starting a midwifery service to help handle some 15,000 deliveries a year. Meanwhile, Lillian Runnerstrom, who had been recruited to establish the UIC nurse-midwifery program, needed a site for her students to train. Thus, began a symbiotic relationship.
There were just five students in that first class at UIC. Students did their clinical training in prenatal, intrapartum and postpartum care at Cook County under faculty midwives who served as preceptors, including Patricia Urbanus,Jean Downie and the late Joyce Roberts, PhD ’79. Because of the scarcity of midwives with master’s degrees at the time, it was not uncommon
20 | College of Nursing
Celebrate!
More than 100 alumni gathered together on May 23, 2022, to celebrate the 50th anniversary of the UIC College of Nursing nurse-midwifery program during the American College of Nurse Midwives annual conference in Chicago.

for new graduates to turn around and become faculty while also practicing at Cook County Hospital.
Classes grew—they routinely have about 25 students now—and so did the acceptance of midwifery practice. When it started, Cook County was the only hospital in the state with a midwifery service, says Sabina Dambrauskas, MS ’76, BSN ’68, FACNM, a member of the inaugural class, and early nurse-midwives faced misconceptions and stereotypes.
“The old granny midwives were not nurses but were called midwives,” Dambrauskas says. “There was always skepticism with that name. People would ask: ‘What’s your actual training? Are you just apprentice-trained or do you have some formalized education?’ That’s why it was important in those early days to stress we were nurse-midwives: that we had nursing degrees, experience and medical training.”








From left, standing: Jean Downie, one of the first clinical faculty members and the first director of Cook County Hospital’s midwifery services; Katherine Camacho Carr, MS ’74, a member of the first class and former ACNM president; Sabina Dambrauskas, MS ’76, BSN ’68, a member of the first class and former faculty member. Seated: Ruth E. Alteneder, MS ’74, a student in the first class.

It’s really wonderful to have this big community, which feels like a big family, There are so many stellar graduates: former presidents of the American College of Nurse Midwives, a high-ranking offi cial in the World Health Organization, researchers and heads of programs.
—Sabina Dambrauskas
VITAL SIGNS FALL 2022 | 21
From left, standing: Crystal Patil, PhD, head of the Department of Human Development Nursing Science; Diane Boyer, MS ’79, BSN ’76; Naeema Al-Gasseer, PhD ’90, MS ’87; Carrie Klima, MS ’86. Seated: Patricia Urbanus, one of the first clinical faculty.
1971 1971 1972
Cook County Hospital begins midwifery service under its first director, Jean Downie.







UIC launches first nursemidwifery program in Illinois.
Lillian Runnerstrom is the first program director.
Integral to women’s health care

Through the decades, more clinics began adding midwifery services, and in 1992, midwives were first allowed to care for patients during labor and birth at UI Hospital, facilitated by Roberts, who was then incoming head of the UIC Nursing Department of Women and Children’s Health. (Roberts was also program director from ’81 to ’84 and again from ’97 to ’98.)


“It really did change obstetrics at UI Health, and now our midwives see patients in clinics all over the city, mostly with our Mile Square network, and deliver about 40% of the babies at the hospital,” Klima says. “They are integral to the functioning of women’s health care at UIC.”
Betty Schlatter, PhD ’90, who was program director from ’89 to ’95, and Janet Engstrom, PhD ’85, MS ’81, program director from ’98 to ’05, were instrumental in expanding the nurse-midwifery program beyond Chicago to all UIC Nursing campuses and creating more distance-learning options. These efforts “pushed midwifery into other parts of the state,” says Klima.
Globally, alumni like Naeema Al-Gasseer, PhD ’90, MS ’87, have long been influencing women’s health issues. Al-Gasseer is currently the World Health Organization representative in Egypt, and before that, Sudan.
Chicago Mayor Eugene Sawyer proclaims Oct. 2-8 Nurse-Midwifery Week in Chicago.
1992 1989-1995
Midwifery program expands to UIC Nursing campuses outside of Chicago under Betty Schlatter’s leadership.
22 | College of Nursing
Midwifery given full scope of practice at UI Health. 1972 1988 1989-1995 1992
The program changed from a master’s degree to a Doctor of Nursing Practice degree program in 2014. Klima says students today graduate with a broader skill set, including primary care training, and are prepared to see more complex cases.
“A big trend is the expansion of midwives caring for women and families in a variety of settings and conditions,” Klima says. “Midwives are more integrated into health systems now and are seen as integral partners in taking care of women, whereas when I went to school, we were still fighting our way into every place that we wanted to be.”
Tradition lives on
Still, some things about the program haven’t changed.
Beginning with the program’s inception, Runnerstrom welcomed new students with a lasagna dinner at her apartment each year. Each fall— with a recent exception due to the COVID-19 pandemic—the college still hosts the Lillian Runnerstrom Lasagna Dinner, although as the program has expanded, it’s now held at a restaurant instead of at the director’s home. Runnerstrom’s lasagna recipe was even passed out as a party favor at the anniversary celebration.
1998-2005
1998 1998-2005 2001 2014


Gov. Jim Edgar signs the Illinois Advanced Practice Nursing Act.

Program director Jan Engstrom facilitates distance-learning options for students across the state, outside the walls of a brick-and-mortar campus.
The table is set for the “blessing of the hands,” the ceremonial moment when midwives reflect on the care that their hands bring.
Program changes from master’s degree to DNP degree.
Directors


Lillian Runnerstrom, PhD 1972-1976
Connie Adams 1976-1981
Joyce Roberts, PhD ’79 1981-1984
Diane Boyer: MS ’79, BSN ’76, PhD 1984-1989
Betty Schlatter, PhD ’90 1989-1995




Deborah Woolley, PhD ’88 1995-1997
Joyce Roberts, PhD ’79 1997-1998
Janet Engstrom, PhD ’85, MS ’81 1998-2005
Barbara Camune, DrPH 2006-2012
Carrie Klima, PhD, MS ’86 2012-2022

Pamela Pearson, DNP ’18, CNM, FACNM 2022-present
Pamela Pearson becomes the first African American director of UIC’s nursemidwifery DNP program.
VITAL SIGNS FALL 2022 | 23
1998
2001 2022 2022

STUDENT SPOTLIGHT
Disability justice for nurses

Sabrina Jamal-Eddine, BSN, RN, was a sophomore in high school when she underwent posterior spinal fusion surgery to correct a spinal curvature. But the surgery was a failure, and rather than repairing the problem, it created a host of new ones.
“The minute I got out of surgery, it started to hurt to breathe,” Jamal-Eddine recalls. “Every time I inhaled, it felt like someone was cutting me with a knife. That pain didn’t go away.”
Two years later, she had a revision surgery, which successfully corrected the mistakes of the first with the insertion of new, properly-contoured hardware. But two major back surgeries left her with trauma to her spine and a permanent, non-apparent physical disability, entailing lifting limitations, protruding screws, and pain with certain types of movement.
Her experiences with nurses during and after those two surgeries solidified her desire to be a nurse. She recalls nurses who showed empathy, positivity and caring—as well as those who didn’t. She was determined to be like the former.
“I’ve always been a caretaker and knew that taking care of people and alleviating pain was something that would bring me joy,” she says.
Breaking down barriers for disabled students


To Jamal-Eddine’s surprise, she faced barriers when she entered her undergraduate nursing program as a disabled student.
Her course syllabus posted a “disability statement,” asking students to come forward if they have a disability. She later learned through research that nearly all nursing programs have “technical standards,” referring to physical requirements to complete the program.
Jamal-Eddine knew she would struggle with one of those requirements—lifting a patient in bed—but felt that shouldn’t sideline her entire nursing career.

Nursing is inherently a flexible profession, she says, offering opportunities for nurses with a wide range of abilities and disabilities, including careers in telehealth, administration, informatics and advanced practice nursing.
“I could do everything that was required in my nursing program besides lifting a patient up in bed,” she says. “I never had any intentions of doing bedside nursing. It was
silly that this generic program requirement was posing barriers for future nurses who might never need that skill.”
Despite the deterrent, Jamal-Eddine stayed in the program. She faced resistance from some clinical instructors, who questioned her ability to complete the program, while others showed empathy and support. An instructor on a progressive care unit—which required heavy lifting—was particularly understanding.
Jamal-Eddine recalls the instructor saying: “‘Nursing is a team profession. Nurses are always relying on each other. Any time you need to lift a patient up in bed, we have seven other people in this clinical rotation who can help you.’”
Jamal-Eddine is now taking those experiences into her PhD program at UIC to study how she can educate nursing students, instructors and practitioners about ableism—discrimination against disabled people— and disability justice.
For Jamal-Eddine, one of the most powerful ways to do this is through spoken word poetry. She used the format in a 2019 TedX Talk about her experiences with Islamophobia and xenophobia.
She sees an important intersection between humanities and nursing and explored this as the first nursing student ever chosen for a prestigious Humanities Without Walls Predoctoral Career Diversity Summer Workshop, hosted by the University of Michigan’s Institute for Humanities.
“Even though I have the inherent experiences as a marginalized person, the humanities provide me with the language I need to articulate these inequities, and they help me advocate to progress beyond those,” she says.
“We talk about nursing as art and science, but art isn’t given the space it deserves in nursing curricula. I believe humanities help us humanize people and often work toward belongingness.”
“We talk about nursing as art and science, but art isn’t given the space it deserves in nursing curricula. I believe humanities help us humanize people and often work toward belongingness.”
Nursing without borders

UIC College of Nursing faculty are expanding study abroad options for students, with courses offered last summer in Rwanda and the twin island Caribbean nation of St. Kitts and Nevis, with more opportunities in the works.
“This concerted effort to give our nursing students more formal study abroad experiences aligns with our vision as a college, which calls for preparing nurses who can lead change globally,” says Rohan Jeremiah, PhD, associate dean for global health. “While we had to take a pause from international learning experiences for the last two years due to the COVID-19 pandemic, we are thrilled to be offering even more courses this summer.”


In 2019, clinical assistant professor Gwyneth Milbrath, PhD, RN, MPH, worked with the UIC Study Abroad Office to establish the college’s first faculty-led study abroad course. The course, Disaster Preparedness and Global Health in the Caribbean, a three-credit class in St. Kitts and Nevis, opened the possibility for more formal study abroad experiences for nursing students.
“Carving out study abroad opportunities, particularly for pre-licensure nursing students, has historically been difficult because of the structure of the nursing program, which is jam-packed and doesn’t require electives,” says Milbrath, who is also associate director of the college’s Global Health Leadership Office. “But with careful scheduling and deliberate content development, we’ve been able to develop courses that fit within the curriculum’s scope and timing.”

26 | College of Nursing FOCUS ON EDUCATION
For Sayuri Fujita, MPH, a student in the MS/graduateentry program who participated in the St. Kitts and Nevis experience, global health has always been a “calling.” She adds that emergency preparedness is one of her interests, particularly because natural disasters affect the lives of people across the globe.
“I lived in the Philippines when I was younger, and having a global perspective has always been a part of me,” says Fujita, whose father is Japanese and mother is Filipino. “I can’t just think about the U.S., even though I am an American citizen. I still have people all over the world that I care about.”


The experiences offered in summer 2022 included:
• St. Kitts and Nevis: In late May, Milbrath returned to St. Kitts and Nevis with 14 interdisciplinary students from UIC. Students worked with the country’s National Emergency Management Agency on a project to survey residents about needs related to COVID-19 and food security. Co-leading the course was Audrey Snyder of the University of North Carolina Greensboro, who brought six students.
• Rwanda: Adjunct professor Pamela Meharry, PhD, CNM, is faculty director for Global Maternal and Child Health at the University of Rwanda. The six-credit, month-long course is the first-ever maternal and child health course offered by the UIC Study Abroad Office. A mix of midwifery, graduate-entry master’s and public health students spent the month of July there.
(Above) Pictured here are students and faculty who took part in the Global Maternal and Child Health in Rwanda course: (back, from left to right) Donatilla Mukamana, professor; Celeste Jimenez, student; Angelique Muhammad, student; Marya Elliot, student; Angela O’Bryant, student; Philomene Uwimana, deputy dean; Paolina Guerrier, student; Pamela Meharry, UIC Nursing visiting professor; Rohan Jeremiah, interim associate dean for global health. (Front row, left to right) Students Dhriti Patel and Aubrey Meunier.

Prior to 2019, graduate and professional students had opportunities to earn clinical practicum hours in international settings—such as with the Department of Midwifery at Karolinska Institute in Sweden or with associate professor Susan Walsh, DNP ’14, MS ’00, BSN ’80, CPNP-PC, in Haiti—but those were not for-credit courses through the university’s official study abroad office.
Milbrath says study abroad experiences allow nursing students to experience the strengths of health care models that are different than the U.S. system. They also get to see how the scope of practice for nurses can be broader or more limited in other parts of the world.



“I think it’s really good to see other cultures and see other ways of doing things, especially because students are in learning mode and have an open mind,” Milbrath says. “That can help us to think of more creative ways to address some of the challenges we have here.”
Study abroad experiences in development for 2023 and 2024 include:
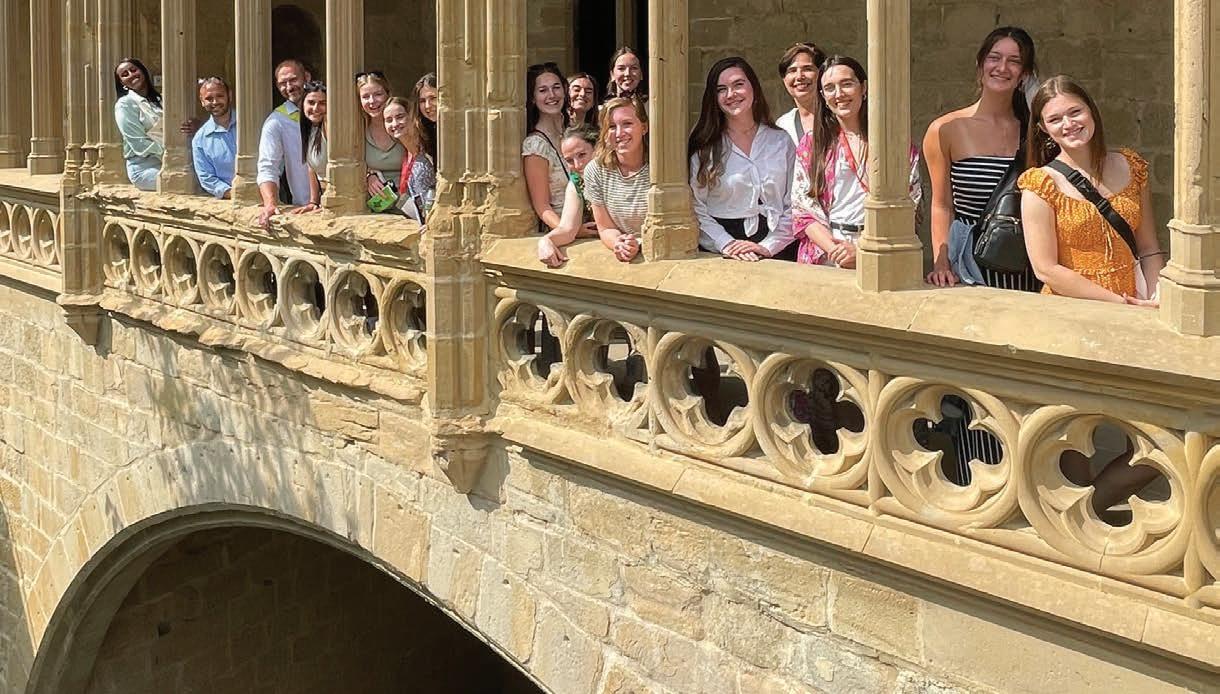
• Spain: Assistant professor Susan Kilroy, PhD ’20, RN, CHSE, and Milbrath are developing a summer 2023 study abroad course for pre-health and health sciences students in Pamplona, Spain. They both served as visiting instructors for a weeklong workshop on cross-cultural perspectives on health care at the University of Navarra this summer, which was attended by two UIC Nursing students from the Urbana campus.
• Ireland: Urbana campus director Krista Jones DNP ’11, MS ’07, PHNA-BC, received funding to create a proposal for a study abroad program in Dublin, Ireland. She will travel there in February to develop the full proposal, with a tentative start date of summer 2024. The proposed course will be open to health sciences students and will provide a comparative focus on health care systems, with an emphasis on community-based care.
(Left) Sayuri Fujita, MPH, a student in the MS/ graduate-entry program who went to St. Kitts and Nevis, is pictured here with 5-year-old twins she met at the farmer’s market while conducting a food security survey.
(Far Left) UIC Nursing Urbana students Carrie Wolter (farthest right) and Maggie Moore (second from right) were in the town of Olite, touring palaces and learning about the history and culture of Spain, during a weeklong workshop at the University of Navarra.

VITAL SIGNS FALL 2022 | 27
‘I can’t just think about the U.S.’
3×
Tripled the useable space on our college lower level (from 5,000 to 15,000 sq ft)
The most ambitious fundraising effort in UIC’s history concluded with a record level of giving to promote student success, empower faculty, drive discovery and connect to communities.
On June 30, 2022, the University of Illinois Chicago ended IGNITE: The Campaign for UIC. The seven-year effort to raise $750 million universitywide was a resounding success, closing at $803.4 million, more than $125 million more than in the campaign that preceded IGNITE.
Of that UIC total, $37,529,703 is attributable to the generous donors who supported the College of Nursing, helping us end the campaign having raised two and half times more than the college raised during the university’s most recent campaign preceding IGNITE.


Throughout, UIC Nursing focused its fundraising efforts on three mission-critical aspects of our college: enhancing key brick-and-mortar spaces, building scholarship assistance for students, and supporting faculty and research.


$8.2M
Total gifts directed toward space enhancements
Enhancing Space
More than $8 million given to the College of Nursing during IGNITE was aimed directly at enhancing physical spaces dedicated to learning and researching. Alumna Christine Schwartz, BSN ’70, gave $5 million, the largest gift in college history, to create the M. Christine Schwartz Experiential Learning & Simulation Laboratory. The Schwartz Lab—which includes the Francis Family Birthing Suite, named by a $1 million gift from Nita and Phil Francis—has been transformative for the college. Not only does it provide multiple, true-to-life simulated environments where faculty can immerse students in high-stakes scenarios with low-stakes consequences, but it was also instrumental in enabling the college to conduct necessary, in-person education during the height of the COVID-19 pandemic.
28 | College of Nursing
6,814 Total donors to UIC Nursing: individuals, businesses and foundations $35M NURSING ACTUAL $33M NURSING GOAL $803M UIC ACTUAL $750M UIC GOAL THE AFTERGLOW OF
$8.8M
Supporting Students
Students are the lifeblood of any college, and it is a principal aspiration of UIC Nursing leaders, faculty and staff to support all students’ success, from Day One through graduation. That support takes many forms, and during IGNITE, donors contributed nearly $9 million to the effort. About 65% of that has been directed to scholarships that help students with financial need and academic merit afford to stay enrolled and on track. Because of those gifts, the college has been able to quadruple the number of students receiving scholarship assistance each year. (The goal was to triple the number.) Additional gifts are funding instructional tools and supplementary programming, including, for example, the Center for Academic Excellence and Cultural Engagement.
$17.6M
Supporting Faculty
UIC is one of the world’s most productive hubs of nursing research. Currently ranked No. 7 for NIH funding to U.S. nursing schools, UIC Nursing has long been a reliable investment for individuals, foundations and corporations wanting to help drive discovery. Similarly, with BSN, MS and DNP programs ranked in the top 15 nationally by U.S. News & World Report, UIC boasts some of nursing education’s most effective classroom and clinical instructors. Recruiting and retaining top-tier nurse scientists and educators is highly competitive, which is why the college was proud to receive $17.6 million during IGNITE to support faculty. These investments yielded nine new endowed chairs, professorships, faculty scholars, faculty awards and research funds; that was four times the number of philanthropically supported faculty positions in the college at the beginning of IGNITE.

$2.9M



Flexible Funding
During IGNITE, unrestricted gifts totaling nearly $3 million provided nimble support, directly and indirectly, to students and faculty alike. These gifts, each typically under $1,000, come from hundreds of donors and collectively provide a powerful source of funding that the dean can direct where it’s needed, when it’s needed. This type of funding has become especially important as state support for public higher education has declined roughly 25% over the past 10 years.
For more about gifts to the college during IGNITE and the many people who benefited from them, visit our Faces of Philanthropy gallery at go.uic.edu/GiveToNursing.

240
55
of students receiving scholarship
12
Current number
Original number Quadrupled number
support
Current number 3 Original number Quadrupuled number of philanthropically supported faculty positions
VITAL SIGNS FALL 2022 | 29
In her DNA

Victoria Venable Fletcher, MS ’78, CNM, FACNM, remembers being the only African American student in her Master of Science in nurse-midwifery program at the UIC College of Nursing in the mid-1970s.
As a pioneering student in the young program, she recalls facing bias from faculty and staff, but also benefited from the encouragement of champions who wanted her to succeed.
“That’s why I know it’s important to have someone that demonstrates an interest and shows that they care—that they’re invested in your success,” she says.
Her experiences and “a desire to change the narrative” prompted Fletcher to make a gift to the UIC College of Nursing to create a scholarship for underrepresented students in the nurse-midwifery and nurse-midwifery/ women’s health nurse practitioner programs.
“I want to be there to offer a hand and help uplift these students,” Fletcher says.
Fletcher was inspired to go into a health-related field by her uncle, Howard Phillip Venable, MD, a renowned ophthalmologist and civil rights advocate who championed equitable care and mentored dozens of Black physicians at Homer G. Phillips Hospital and Washington University School of Medicine in St. Louis.
Paying it forward
Patricia Lewis, PhD ’93, who served as director of the UIC College of Nursing’s Rockford campus for 13 years, and her husband, Stephen, recently endowed the first named scholarship for Rockford students.
The creation of the Patricia Ryan Lewis Scholarship Fund means that each of UIC Nursing’s five campuses beyond Chicago now has a dedicated scholarship for its students. Lewis is a former president of the UIC College of Nursing Alumni Board and is still a board member.
“Over the 30-plus years that I worked with students, there were so many barriers for them to overcome,” says Lewis. “It isn’t always about tuition and books. It’s also, can you
“It’s in my DNA to be an advocate and a disruptor,” Fletcher says.

Fletcher’s wide-ranging career reflects this commitment, bringing her from California to South Carolina to Washington state, including working for more than 20 years with Planned Parenthood.
“You don’t have to be wealthy to do this,” she says. “I would encourage other alumni and interested people to give what they can, at whatever level they can, to help deserving students achieve their goals. It is important and will make a difference in moving the needle, increasing diversity in nursing and midwifery, and in turn in decreasing health disparities in communities of color.”
READ MORE about Fletcher’s life, work and gift at go.uic.edu/FletcherImpact

afford to live and eat? People are pretty close to the edge a lot of times.”
Lewis notes that her career in nursing education didn’t make her extravagantly wealthy, but after retiring, she and her husband realized they could afford to fund the scholarship if they broke up the payments over several years.


Lewis says her own path through higher education inspired her to make the gift, including an ethos of “paying it forward.” Growing up as one of three children in a single-earner household in Milwaukee, Lewis’ parents couldn’t afford to pay for her bachelor’s degree in nursing from the University of Wisconsin-Madison. When an administrator helped her put together a financial aid package to carry her through school, she remembers the advice that came with it.
“When I thanked her, she said, ‘Don’t stop there. When you’re done with school, you need to help someone else get through school—and don’t forget that,’” Lewis recalls. “I never did.”
30 | College of Nursing IGNITE IMPACT
Victoria Venable Fletcher holds her grandson, who she helped deliver in 2012.
COVID’s effect on Black girls

The physical, psychological and sexual development of Black adolescent girls has been “heavily impacted” by the COVID-19 pandemic, says UIC College of Nursing assistant professor Natasha Crooks, PhD, RN.
Crooks published a recent paper, titled, “The Impact of COVID-19 Among Black Girls: A Social-Ecological Perspective,” in the Journal of Pediatric Psychology. The paper reports on the findings of a qualitative study that featured interviews with 25 Black girls—ages 9 to 18—from December 2020 to April 2021. Most participants reported significant psychological and physical consequences, including depression and anxiety, disrupted eating, distorted body image, and changes in self-esteem.



“Black girls are a very vulnerable and unprotected population, especially within the context of COVID,” Crooks says.




Black girls enter puberty and develop secondary sex characteristics earlier than their non-Black peers, according to the paper, causing them to suffer from
“adultification” and “sexualization by society.” This can lead to elevated sexual and mental health risks.
Crooks found that only two of the girls in the study received any formal sexual education during the pandemic, as schools opted to delay teaching sex education during online learning due to the sensitive nature of the topic, according to the study.
The pandemic also intersected with the Black Lives Matters movement. The participants saw mistreatment of Black people by police, including the murders of Breonna Taylor and George Floyd, nationally broadcasted. These messages led to mixed feelings among the participants.
“A lot of what the girls talked about was feeling empowered to be Black and having a sense of pride within their identities,” Crooks says. “On the other hand, there was fear that came with color of their skin—fear of being harmed themselves, or their fathers, brothers or other family members being hurt. There was this constant fear and threat to Black families.”
VITAL SIGNS FALL 2022 | 31
RESEARCH ROUND-UP
Deterrent to dementia?
Could an exercise program help slow the effects of dementia in older adults with chronic kidney disease?

Ulf Bronas, PhD, ATC, FSVM, FAHA, UIC Nursing associate professor, suspects that it could, and will test his hypothesis with a $2.68 million grant from the NIH.
It matters, Bronas says, because older adults with chronic kidney disease show signs of Alzheimer’s disease and related dementias about 10 years earlier than patients without kidney disease.
combining comprehensive assessments of cognition with brain imaging, we’ll be able to evaluate the relationship between behavior change, brain neural networks, and cognitive function at a level previously not completed in this understudied population.”
Bronas will enroll 140 older adults with mild cognitive impairment and chronic kidney disease in the five-year study, which will examine whether a six-month, home-based walking program improves executive function, cognition, brain matter integrity and neural network connectivity.
Studying acupuncture for breast cancer pain
Assistant professor Hongjin Li, PhD, was awarded a grant through the National Center for Complementary and Integrative Health to study whether acupuncture could alleviate breast cancer symptoms for patients at a federally qualified health center.
Nearly 94% of breast cancer patients experience symptoms—such as joint pain, hot flashes, sleep disturbance, fatigue, depression and anxiety—during or after endocrine therapy, also known as hormone therapy.
Although past studies have shown acupuncture can holistically address multiple symptoms in patients with other conditions, it has not been investigated among breast cancer patients receiving endocrine therapy.
Significantly, Li’s research will focus on patients at a federally qualified health center (FQHC), which provides
Bronas and his colleagues will use exercise testing, cognitive testing and MRI to measure and test outcomes of the exercise intervention.
“This study will allow us to address a critical gap in how exercise might be used to prevent and treat age-related cognitive decline,” he says. “By combining comprehensive assessments of cognition with brain imaging, we’ll be able to evaluate the relationship between behavior change, brain neural networks, and cognitive function at a level previously not completed in this understudied population.”
care to an underserved population who may experience barriers to health care. Other studies of acupuncture have focused on privately insured clinic settings.
“There is an urgent need to remove barriers and ensure equal access to this evidence-based treatment among breast cancer survivors with limited access to acupuncture,” she wrote in her abstract.
The results will potentially provide the foundation for a larger, multisite study of acupuncture at FQHCs for breast cancer survivors, and could ultimately promote broader insurance coverage for acupuncture, Li says.
Li’s team includes fellow UIC Nursing faculty Ardith Doorenbos, Harriet H. Werley Endowed Chair for Nursing Research, Judith Schlaeger, associate professor and Crystal Patil, professor. It also includes Oana Danciu, associate professor at the UIC College of Medicine, and Zhengjia Chen, associate professor at the UIC School of Public Health.
32 | College of Nursing
RESEARCH ROUND-UP
“By
Words that hurt

Two recent papers by UIC College of Nursing faculty found that microaggressions—common, subtle indignities—can be just as harmful as a major discriminatory event, contributing to negative mental and physical health outcomes in bisexual women.
Associate professor Wendy Bostwick, PhD, MPH, and assistant professor Ariel U. Smith, PhD, RN, were co-authors on both papers, one published in the Journal of Bisexuality and the other in Psychology of Sexual Orientation Gender Diversity, a publication of the American Psychological Association. Both relied on findings from the Women’s Daily Experience Study of 112 ethnically and racially-diverse bisexual women.
survey, followed by 28 days of e-diaries to capture microaggressions that they may have experienced during the previous 24 hours.
“The old saying goes, ‘sticks and stones may break your bones, but words can never hurt you,’” Smith says. “But you look at the data and realize that’s simply not true. Microaggressions that someone has experienced over a lifetime are correlated with mental and physical ailments they experience even today.”
The researchers looked at microaggressions related to sexual orientation, race and gender. Microaggressions could include denying a person’s bisexuality—such as suggesting it’s “just a phase”—or a rude or insulting comment about lesbian or gay individuals. A comment minimizing or denying the existence of racial discrimination is an example of a racial microaggression.
Participants reported an average of eight microaggressions of any type in the previous month, with almost all women—97%—reporting at least one microaggression throughout the duration of the study.
Bostwick is principal investigator on a National Institute on Minority Health and Health Disparities grant which funded the Women’s Daily Experience Study, one of the first ever to focus on bi-identified women and mental health. Participants completed a baseline

Transparency with research participants
For participants enrolled in research studies, receiving results – both individual health results and broad findings from the study—can be inconsistent.
UIC Nursing clinical assistant professor Denise Kent, PhD, APRN, calls this is an “unregulated part of doing research.”

She received a grant to create a tool to improve the return of results to study participants, allowing patients to take a survey to indicate preferences for receiving results, which she hopes can then be used in other large-scale research studies.


Her pilot study, called MIRROR, is part of a four-year study of long COVID-19, which will enroll around 1,200 patients.
The studies found that microaggressions were associated with poor mental health and binge drinking, smoking and marijuana use. The most consistent finding was an association between microaggressions and anxiety.
“It’s two sides,” Kent says. “We can’t do research without participants. They need to be recognized as a valuable part of the project. If we want to ask people to keep coming, to let us keep poking them so we can get more information, we have to ask, what are we doing for them?”
Kent says that while the participants will receive compensation for their involvement in the study—with cash or gift cards for each visit—she also wants to be sure that participants are receiving valid, usable health information in a personalized format.
This is an evolving study, and scientists don’t know what they’ll learn in the next four years about long COVID, she says.
“Maybe it will be something that will be pertinent to the participants and their families, that they’ll want to know,” she says. “We need to have a mindset of transparency, recognizing that the research participants are a valuable part of the team.”

VITAL SIGNS FALL 2022 | 33 RESEARCH ROUND-UP
“Microaggressions that someone has experienced over a lifetime are correlated with mental and physical ailments they experience even today.”
LGBTQ+ Acronym used to describe the community of people who identify as: Lesbian, Gay, Transgender, Bisexual and Queer. The plus is for those not represented in the acronym, such as intersex or asexual.








(See p. 33 for more on a recent study.)
Research + Practice + LGBTQ+























The UIC College of Nursing is home to some of the country’s foremost experts on sexual and gender minority health. We brought two together to discuss how research and practice meet to inform care for this population.





Wendy Bostwick (W.B.): We know that sexual and gender minorities do experience discrimination, mostly in the form of microaggressions. We know that trans and gender-nonconforming or non-binary people are especially likely to experience discrimination in health care settings.

Paige Ricca (P.R.): I hear these types of stories working with youth. I’ve been on the wellness team for the Illinois Safe Schools Alliance–Action Camp [a five-day camp that brings together LGBTQ+ youth leaders and allies] four times. Youth come from all over Illinois. They tell me they drive two hours or more from the middle of Illinois to go to Howard Brown Health in Chicago [a federally qualified health center serving the LGBTQ+ community], because that’s where they feel the safest. They’re not going to seek care elsewhere because they don’t want to be traumatized by a discriminatory experience.
W.B. We tend to think of “health care” as a solution to disparities. That’s not always the case. Sometimes health care creates, promotes and exacerbates disparities. Research shows that discriminatory experiences in a health care setting will cause people not to go back, or to delay seeking care, which can worsen problems to such an extent that people only show up in the ER. It’s a bad cycle; that’s not what we want to be happening, especially if we’re trying to think preventatively.
In a city like Chicago, yes, we do have plenty of places that are LGBTQ-focused. There can still be quite a dearth of either allied or actual queer providers in rural areas.
P.R. When I worked with 360 Youth Services out of DuPage County [which offers housing, counseling and prevention services], there was only one provider that the director felt she could recommend to her LGBTQ+ or
34 | College of Nursing
EXPERT VIEWPOINT
Clinical assistant professor Paige Ricca, DNP ’17, RN, is an LGBTQ+ community advocate who has worked as a wellness nurse for sexual- and gender-minority youth.
Associate professor Wendy Bostwick, PhD, MPH, has been conducting research on health inequities among sexual- and gender-minority populations for 20 years.
non-binary youth. In DuPage County, a pretty populated county, that’s kind of scary.
W.B. Welcoming and affirming health care settings are not just about the nurses and the physicians. It’s also about the literal environment. What are the posters on the wall? What sort of signage is on your bathrooms? Do they say “all genders,” or do they say men and women? What do your forms say? How does your front desk staff treat people?
We have many alums who are in higher-level positions that can advocate for ensuring these policies are in place. There are administrative-level things that even non-practicing nurses can be engaged in. Advocacy is a huge part of what we’re talking about here. It’s not just practice. There’s a whole host of things that happen before someone even gets into the examination room.
P.R. This was exactly the focus of my DNP project, which involved creating a quality-improvement tool to enhance LGBTQ+ sensitivity in a clinic setting. That included having a leader who champions the continuation of trainings and other policies.
W.B. I think there’s room to grow within colleges of nursing, in terms of to how and when we train our nurses on LGBTQ+ health issues. We need to ensure that principles of equity—whether that’s racial, gender or queer equity—are integrated into our curriculum starting the minute our students walk in the door.
P.R. We need to infuse it early in the process, and we are getting better. I can speak to one example. I coordinate and teach in the pediatrics/OB course for prelicensure master’s students. When I first got here in 2018, I talked to the coordinators about making one of the simulations involve a transgender child—in the middle of transitioning—presenting in the ER with signs of dehydration. We also included LGBTQ+ cultural sensitivity training prior to simulation day.
In our community health courses, we’re introducing students to more gender-nonconforming patients so that we can use a more affirming approach, an approach that enhances cultural safety. We’ve also gotten better about hiring authentic actors who are gender-nonconforming and trans for standardized patient simulations.
W.B. I want to point out that while there’s absolutely a need for trans- and gender-focused trainings, it’s also the case that the needs of all sexual minority people [including those in the ‘L,’ ‘G’ and ‘B’ categories] need to be considered, affirmed, recognized and acknowledged. There is variation within the [LGBTQ+] population, and
good training will make the space to identify those distinctions for students so that they’re not treating LGBTQ+ patients as a monolithic population.
For practitioners, I go back to my number one rule, which is basically, don’t be a jerk [laughs]: Make no judgment about sexual partners or behaviors, mirror people’s language, don’t make assumptions.
P.R. I’m still growing as an expert, so I rely on other experts who have given me a lot of guidance about translating knowledge into clinical practice. The National LGBTQIA+ Health Education Center [Bostwick is adjunct faculty with The Fenway Institute, which runs the center] has fabulous mini seminars for training. “The Clinician’s Guide to LGBTQIA+ Care” is a gold mine. [Clinical assistant professor] Randi Singer is a co-editor.
—Wendy Bostwick
W.B. So much has changed in 20 years. I work in this area, and I am the first to admit that language is changing very quickly, but staying abreast of language is important, because how we address people is a fundamental sign of respect.
P.R. It’s dynamic. It always has been and always will be.
W.B. I think there’s a lot of opportunity within our own College of Nursing when it comes to sexual- and gender-minority health. I certainly see more and more students open—and having a desire—to focus on these sorts of issues in all areas of practice.
P.R. It’s important to recognize faculty from the college who were earlier leaders, like [professor emerita] Tonda Hughes, Charlie Yingling and Carrol Smith.
W.B. We have a lot of people in the college who are interested, willing and already working on this. And it’s just a matter of fostering and supporting those collaborative endeavors.
READ MORE Go to go.uic.edu/BostwickRicca for a longer version of this conversation.
VITAL SIGNS FALL 2022 | 35 EXPERT VIEWPOINT
“It’s important to have a conversation about both research and practice, because they’re meant to inform one another. In terms of changing norms and health inequities, my research can point it out, but the research on its own doesn’t solve the problem.”
UIC Nursing AROUND THE STATE SPRINGFIELD
Fueling student success
The Springfield campus has implemented a multipronged strategy to boost student success, including an introductory bootcamp for incoming juniors, a robust tutoring program, cutting-edge NCLEX exam review and assessment tools, and the addition of a student success coordinator and retention specialist. That role was filled by Susan Hovey, PhD, RN, associate director of the Springfield campus.
Much of this programming was made possible by funding from Memorial Health System.
“This is so important—especially now, with students reorienting and playing catch-up after spending a year doing much of their learning remotely [due to the COVID-19 pandemic],” says Sara McPherson, PhD, RN, CNE, Springfield campus director. “We are so grateful to Memorial for giving us the tools to help students not just survive, but succeed, under even the most challenging circumstances.”
An enriched tutoring program, overseen by instructor Katherine Breen, PhD ’20, meant that in-person tutoring was offered four nights a week. During academic year 2021, juniors received 520 hours of tutoring.
In addition, incoming juniors spent two days on campus before the semester started at a bootcamp, going over study skills, like notetaking; meeting faculty; and
familiarizing themselves with the UIC Nursing facilities and the UIS campus.
McPherson says it was also Memorial’s support that enabled the campus to purchase an ATI testing package, which includes NCLEX test prep, critical thinking case studies and study tools. At the time of writing, 100% of Springfield BSN grads who used the ATI package and took the NCLEX after graduating in May passed the exam on first attempt.
“A lot of students used to take independent review courses that cost anywhere from $500 to $700,” McPherson says. “It’s such a gift to our students.”
As part of the Transition to Nursing boot camp, incoming juniors participated in a scavenger hunt of Springfield’s campus. Here, they found the simulation lab and documented it by taking a selfie.

Jump of joy!
Graduating BSN students at the Springfield and Urbana campuses were as ready as their Chicago counterparts to revive the pool jump tradition in 2022 after a two-year hiatus. As in prior years, students in Urbana proved their mettle by taking the plunge in the chilly outdoor pool at the Activities and Recreation Center (ARC) on the Urbana-Champaign campus on May 3. A local fitness club hosted Springfield students on Apr. 26. Their jump was shared with the Springfield area via a large photo, left, published in the State Journal-Register the following day.

36 | College of Nursing
– USA TODAY
SPRINGFIELD | URBANA © THOMAS J. TURNEY
UIC Nursing AROUND THE STATE
URBANA
Buoying evidence-based practice

Krista Jones, DNP ’11, MS ’07, PHNA-BC, clinical associate professor and director of the UIC College of Nursing’s Urbana campus, along with a team of nurses and librarians, received a new phase of funding for Nursing Experts: Translating the Evidence. The award, from the National Library of Medicine Region 6, began in 2014 and is now in phase five, with a total of $100,000 in funding awarded since its inception.
To date, more than 900 public health and school nurses and 550 acute and ambulatory care nurses have benefited from the project, Jones says. Evidence-based practice is a process used to review the latest scientific evidence and incorporate it into clinical practice.
“Nurses and public health professionals need to document and demonstrate that they engage in research and implement [evidence-based practice] to enhance health care quality, improve patient outcomes, and reduce costs,” says Jones. “However, despite the explosion of scientific evidence, evidence-based care is not standard of care.”
In phase four, Jones and her team surveyed past participants to learn about challenges in underserved communities. They also expanded their promotion of evidence-based practice to underserved community hospitals, health departments and clinical agencies.
In the fifth phase, they will continue that outreach, while also expanding online modules to include content applicable to all public health professionals and providing continuing education units for librarians, nurses and public health professionals.
QUAD CITIES
Celebrate!
After forgoing its traditional spring dinner in 2020, 2021 and 2022, the Quad Cities campus community was elated to gather in September to honor graduates of all three classes. While not all graduates were able to attend, those who did celebrated with family, friends, faculty and staff.

During the program, Jennifer Junis, MS ’12, BSN ’01, was recognized in absentia for receiving the Quad Cities campus’s 2022 Distinguished Alumnus Award. Junis is senior vice president of OSF Saint Gabriel Digital Health, an initiative of OSF HealthCare to expand access to care via technology.
Other highlights included presenting the Quad Cities campus’s 2022 Community Partner Award to Ashlee Misiag, APRN, in absentia, and Magdy Mostafa, MD, both from Genesis Health System. And Dean Eileen Collins recognized the service of Kathleen Sparbel, PhD, MS ’96, FNP-BC, who in 2022 marks 10 years as director of the UIC Nursing–Quad Cities Campus.

(above) Recent graduates in attendance (L-R):
Erin Gholson, DNP ’22
Haylea Dorathy, DNP ’21
Kristen Hawk, DNP ’21

Kimberly Hurley, DNP ’22
Meredith Parizek, DNP ’22
Hayley Mills, DNP ’21
KoDee Plambeck, DNP ’22
Gina Zelle, DNP ’22
Kelli Bartels, DNP ’21
VITAL SIGNS FALL 2022 | 37
(left) Eileen Collins and Kathleen Sparbel
UIC Nursing AROUND THE STATE PEORIA | CHICAGO


Three recognized as Schweitzer fellows
Three UIC College of Nursing DNP students, including one from the Peoria campus, were selected for the distinguished Schweitzer Fellowship, a year-long, service-learning program intended to address the unmet health needs of underserved communities.
The three students were among 28 selected for the fellowship from more than 100 applicants. In collaboration with existing community organizations, each Schweitzer Fellow launches a community-based project, providing 200 hours of service.
The fellows from UIC Nursing are: Jenn Cunningham, RN: Cunningham’s project will be carried out in Peoria’s most disadvantaged area. A student in the Pediatric Nurse Practitioner–Primary Care program, she is partnering with a local, grassroots, nonprofit organization called Southside Community Center to work on building resilience in families and children.
ALL CAMPUSES
Immersion into interprofessionalism
Cindy Cruz, BSN ’12, RN: Cruz, whose focus area is Advanced Population Health Nursing, will develop a series of short and supplemental mental health presentations called Un Minuto Conciente (Mindful Minute) at Alivio Medical Center in Chicago.




Jean Gavina, RN: A Health Systems Leadership student, Gavina’s project will concentrate on preventative health, wellness and self-care sessions, in collaboration with L.E.S. Live Every Second and other community organizations in the Chicago area, to advocate for healthier communities among Filipino Americans and other minority groups.
The Peoria Immersion Day program for interprofessional education was awarded the Office of the Vice Chancellor for Health Affairs’s 2022 I-TEAM award, an annual award given to faculty and staff who have demonstrated excellence in interprofessional practice and education.
From UIC Nursing, the team included representatives from four campuses, including: Quad Cities campus director Kathleen Sparbel, PhD, FNP-BC; Quad Cities office manager Claire DeConte; Peoria DNP student Angela O’Bryant, MSN, RN; Springfield campus director Sara McPherson, PhD, CNE; and Urbana campus director Krista Jones, DNP ’11, MS ’07, PHNA-BC.
The team, which also includes faculty and staff representing pharmacy, social work, medicine and dentistry, will receive $2,500.
THE WORK THAT WON
Peoria Immersion Day has traditionally been held each spring in Peoria’s Jump Simulation Center, bringing together students from health disciplines at UIC, the University of Illinois Urbana-Champaign and Bradley University, to work on interprofessional case-based scenarios.
In March 2020, just weeks into the COVID-19 pandemic, the program’s planners quickly transitioned to a virtual format. That continued in 2021 and 2022. Sparbel says this new virtual format allowed the program to grow from a maximum of 270 participants in person to 470 participants this year, including students from all six UIC Nursing campuses.
The program has also evolved to build upon a Foundations of Interprofessional Collaborative Practice course now offered for all UIC health profession programs. Sparbel says the immersion day offers scenario-based “next-steps application and practice, with the assumption that students already know the foundational IPE content.”
38 | College of Nursing
Jean Gavina
Cindy Cruz
Jenn Cunningham will conduct her Schweitzer fellowship project in Peoria.
URBANA
Retooling STD education

UIC College of Nursing faculty members in Urbana received a grant to create the STD Toolkit for Schools – a community-based educational initiative to provide adolescents in Vermilion County, Illinois, with information about STDs, sexual health and free testing resources.
Amanda Sperry, MS, BSN ’97, PEL-CSN, a visiting teaching associate, is principal investigator on the grant from the Robert Wood Johnson Foundation, Illinois Healthcare Action Coalition and the Illinois Nurses Foundation. Urbana campus director Krista Jones, DNP ’11, MS ’07, PHNA-BC, clinical associate professor, is co-investigator.
Sperry says the intervention is important because chlamydia and gonorrhea rates in Vermilion County remain higher than overall state rates. Vermilion County is on the eastern edge of Illinois, between the Indiana state border and Champaign County. (Champaign County is home to UIC Nursing’s Urbana campus.) About 25% of the county’s population lives below the poverty line, far higher than the national average.
“There are limited sexual-health resources available to adolescents because many clinics have closed due to economic constraints,” Sperry says. “While providing core infectious disease services and STD/HIV surveillance, the health department no longer offers STD and family planning services.”
In fall 2022, UIC Nursing bachelor’s and master’s degree students began developing toolkits—composed of sexual health education pamphlets and resources—for the Vermilion County Health Department. The health department will then be able to loan the toolkits to eight area high schools, where school nurses and teachers can use them in required health classes.
Sperry adds that the adolescent population is at greater risk for contracting an STD. They are less likely to get recommended STD tests, lack insurance and transportation to access STD testing, may have multiple sexual partners, and are hesitant to discuss sexual health with medical providers.
“Research has shown that providing comprehensive sex education positively contributes to decreased rates of STDs,” Sperry says.
UIC Nursing AROUND THE STATE
VITAL SIGNS FALL 2022 | 39
“Research has shown that providing comprehensive sex education positively contributes to decreased rates of STDs”
LookingBack
Booting up digital education
In the 1960s and ’70s, the University of Illinois was at the forefront of computer-assisted instruction with PLATO (Programmed Logic for Automatic Teaching Operations), which was designed and built at the Urbana-Champaign campus. In this photo from the mid-1970s, two midwifery students—Sarah Naber, PhD ’87, MS ’75, BSN ’71 (standing) and Laurie J. Stortz Driscoll, MS ’76—work on an early computer in the fourth floor library of the Chicago campus. Nursing students could use the system to practice analyzing case histories, but the practicality was limited, recalls Sabina Dambrauskas, MS ’76, BSN ’68, a former faculty member.

“The algorithms were good, but the machine was bulky and slow and there were only a few of them, so mostly students used it to practice test-taking skills,” Dambrauskas says.
THANK YOU, SARA!

The UIC College of Nursing Office of Advancement has bid a fond farewell to Sara Almassian, who worked to foster alumni engagement and participation for the last 10 years.
Sara’s many accomplishments included establishing the college’s now-annual REUNION event and leading our Giving Tuesday efforts each year. (She twice led UIC Nursing to win the friendly Giving Tuesday competition among UIC colleges for most dollars raised and/or most donors participating.)
Luckily, Sara isn’t going far; she remains at the college working in the human resources department, where she will put her superior project-management skills to work.
Send Sara your well-wishes at salmas1@uic.edu.
40 | College of Nursing 40 of Nursing
2022 Alumni REUNION























As in past years, the first session of the day was the Alumni Nurse Leaders Panel. This year’s topic, “Innovative Nursing Education and Emerging from the Pandemic,” was presented by panelists: 1—Terri Burch, PhD ’89, Professor Emerita, California State University, San Bernardino; 2—Beena Peters, DNP ’17, MS ’94, System Chief Nurse Executive, Cook County Health; and 3—Susan Kilroy, PhD ’20, Clinical Assistant Professor, UIC College of Nursing.




REUNION
 REUNION includes our annual celebration of those who have received the year’s UIC College of Nursing Alumni Awards. (L-R) Distinguished Alumni Award recipient Sue Penckofer, PhD ’93, MS ’82, BSN ’79, FAAN, Marcella Niehoff School of Nursing at Loyola University Chicago; Outstanding Alumni Achievement Award recipients Sarah Ailey, PhD ’02, MS ’98, BSN ’96, FAAN, College of Nursing at Rush University and Lilian Ferrer, PhD, MS ’00, FAAN, Pontificia Universidad Católica de Chile; UIC Nursing Dean Eileen Collins.
2022 saw the continuance of a tradition started several years ago at the event: presenting gold medallions to commemorate 50 years or more since graduating. (L-R) Three “Golden” alumnae attended this year: (L-R) MaryAnn Lilich, BSN ‘72; Paulette Zachman, BSN ‘72, Nancy Schuller, BSN ‘72.
Dozens of alumni and friends gathered on the Chicago campus for the 2022 All-Alumni REUNION on Saturday, Oct. 8. Traveling from as far as Chile and as near as Chicago, they represented UIC College of Nursing graduating classes spanning more than 50 years. Alumni had a chance to reconnect, network, visit old haunts, see our current facilities, learn from an expert panel and celebrate fellow alums.
REUNION includes our annual celebration of those who have received the year’s UIC College of Nursing Alumni Awards. (L-R) Distinguished Alumni Award recipient Sue Penckofer, PhD ’93, MS ’82, BSN ’79, FAAN, Marcella Niehoff School of Nursing at Loyola University Chicago; Outstanding Alumni Achievement Award recipients Sarah Ailey, PhD ’02, MS ’98, BSN ’96, FAAN, College of Nursing at Rush University and Lilian Ferrer, PhD, MS ’00, FAAN, Pontificia Universidad Católica de Chile; UIC Nursing Dean Eileen Collins.
2022 saw the continuance of a tradition started several years ago at the event: presenting gold medallions to commemorate 50 years or more since graduating. (L-R) Three “Golden” alumnae attended this year: (L-R) MaryAnn Lilich, BSN ‘72; Paulette Zachman, BSN ‘72, Nancy Schuller, BSN ‘72.
Dozens of alumni and friends gathered on the Chicago campus for the 2022 All-Alumni REUNION on Saturday, Oct. 8. Traveling from as far as Chile and as near as Chicago, they represented UIC College of Nursing graduating classes spanning more than 50 years. Alumni had a chance to reconnect, network, visit old haunts, see our current facilities, learn from an expert panel and celebrate fellow alums.
1 2 3 4 1 2 3 READ MORE AND SEE MORE: visit go.uic.edu/NursingREUNION
1—Outstanding Alumni Achievement Award recipient Lilian Ferrer and her husband, Manuel, chat with Nikita Mehotra, MS ‘18 (far left) and TK Le, MS ‘18. 2—2020 Outstanding Alumni Achievement Award recipient Phyllis Pelt, MS ‘95, BSN ‘67, shares a hug with Marlene Sefton, PhD ’99. 3—Assoc. dean for academic affairs, Elizabeth Aquino, PhD ’13 (left), and Danielle Humes, BSN ’07, connect over lunch. 4—Maureen Reilly McCormick, BSN ‘78, MS ‘02, celebrating 20 years since getting her master’s, enjoys remarks by a luncheon speaker.

845 S Damen Ave, MC 802 Chicago, IL 60612 30 | 8 | 6 30 AAN FELLOWS, 8 ACNM FELLOWS & 6 AANP FELLOWS ON FACULTY Ready for the next step? Make it your best step. Get your advanced practice degree from one of the nation’s top programs at the UIC College of Nursing. #1 TOP PUBLIC DNP PROGRAM IN ILLINOIS 12 EDUCATING APRNs IN 12 FOCUS AREAS, PLUS POST-MS OPTION UNIVERSITY OF ILLINOIS CHICAGO | NURSING.UIC.EDU | CONGRADAPPLY@UIC.EDU | (312) 996-7800
CNM,
UIC
of Nursing
Pamela Pearson, DNP ’18,
FACNM Nurse-Midwife, UI Health Director, Nurse-Midwifery/ Women’s Health NP Programs,
College






















 Eileen Collins, PhD, RN, FAAN, ATSF Professor and Dean
Eileen Collins, PhD, RN, FAAN, ATSF Professor and Dean





























































































































































































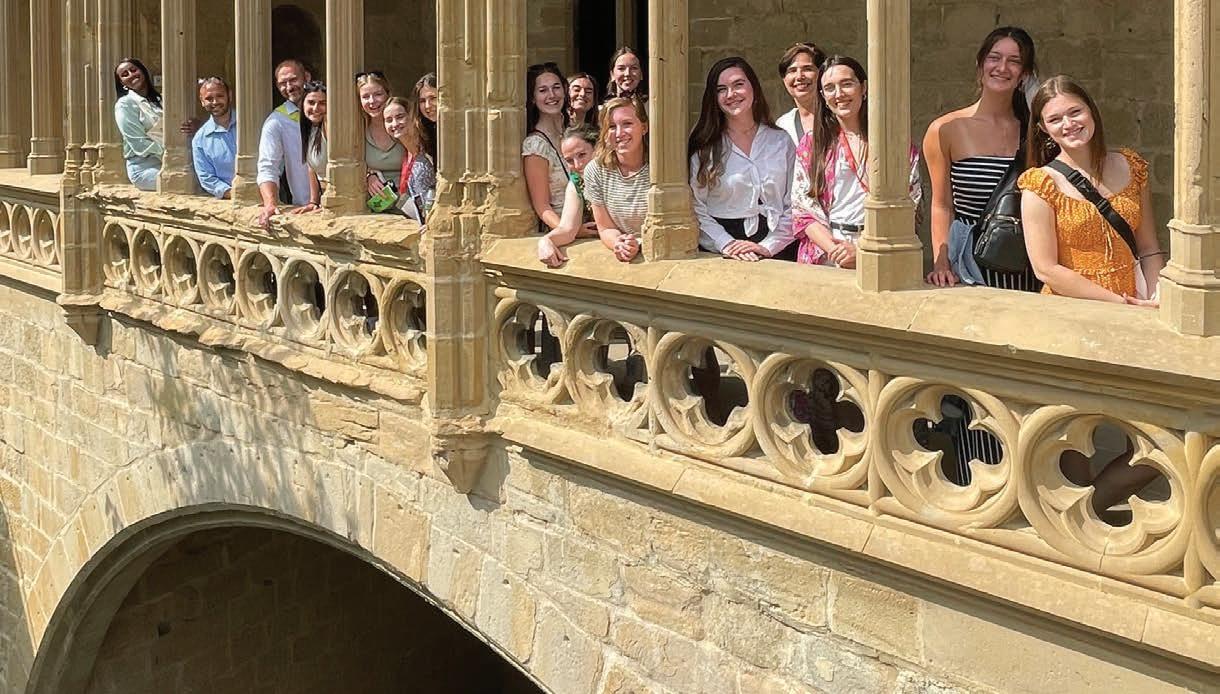














































































































 REUNION includes our annual celebration of those who have received the year’s UIC College of Nursing Alumni Awards. (L-R) Distinguished Alumni Award recipient Sue Penckofer, PhD ’93, MS ’82, BSN ’79, FAAN, Marcella Niehoff School of Nursing at Loyola University Chicago; Outstanding Alumni Achievement Award recipients Sarah Ailey, PhD ’02, MS ’98, BSN ’96, FAAN, College of Nursing at Rush University and Lilian Ferrer, PhD, MS ’00, FAAN, Pontificia Universidad Católica de Chile; UIC Nursing Dean Eileen Collins.
2022 saw the continuance of a tradition started several years ago at the event: presenting gold medallions to commemorate 50 years or more since graduating. (L-R) Three “Golden” alumnae attended this year: (L-R) MaryAnn Lilich, BSN ‘72; Paulette Zachman, BSN ‘72, Nancy Schuller, BSN ‘72.
Dozens of alumni and friends gathered on the Chicago campus for the 2022 All-Alumni REUNION on Saturday, Oct. 8. Traveling from as far as Chile and as near as Chicago, they represented UIC College of Nursing graduating classes spanning more than 50 years. Alumni had a chance to reconnect, network, visit old haunts, see our current facilities, learn from an expert panel and celebrate fellow alums.
REUNION includes our annual celebration of those who have received the year’s UIC College of Nursing Alumni Awards. (L-R) Distinguished Alumni Award recipient Sue Penckofer, PhD ’93, MS ’82, BSN ’79, FAAN, Marcella Niehoff School of Nursing at Loyola University Chicago; Outstanding Alumni Achievement Award recipients Sarah Ailey, PhD ’02, MS ’98, BSN ’96, FAAN, College of Nursing at Rush University and Lilian Ferrer, PhD, MS ’00, FAAN, Pontificia Universidad Católica de Chile; UIC Nursing Dean Eileen Collins.
2022 saw the continuance of a tradition started several years ago at the event: presenting gold medallions to commemorate 50 years or more since graduating. (L-R) Three “Golden” alumnae attended this year: (L-R) MaryAnn Lilich, BSN ‘72; Paulette Zachman, BSN ‘72, Nancy Schuller, BSN ‘72.
Dozens of alumni and friends gathered on the Chicago campus for the 2022 All-Alumni REUNION on Saturday, Oct. 8. Traveling from as far as Chile and as near as Chicago, they represented UIC College of Nursing graduating classes spanning more than 50 years. Alumni had a chance to reconnect, network, visit old haunts, see our current facilities, learn from an expert panel and celebrate fellow alums.
