RADICAL PREVENTION
Their Ideas for Stopping Suicide Are the New Frontier—and Rolling Out Worldwide
Alumnus Makes History but Remembers Her Roots


When the Doctor Became the Patient
Women in Medicine Group Guides and Inspires
UNIVERSITY OF ROCHESTER MEDICAL CENTER | SCHOOL OF MEDICINE AND DENTISTRY | 2023 VOLUME 1
On the cover
Peter A. Wyman (Flw ’88, PhD ’87, MA ’84) and Arielle Sheftall, PhD, are two of the many researchers doing groundbreaking work aimed at preventing suicide “upstream,” before a person ever gets so despondent.

“Being embedded within a cohesive, healthy social network can be the difference between life-saving hope and despair,” Wyman says.
POINT OF VIEW
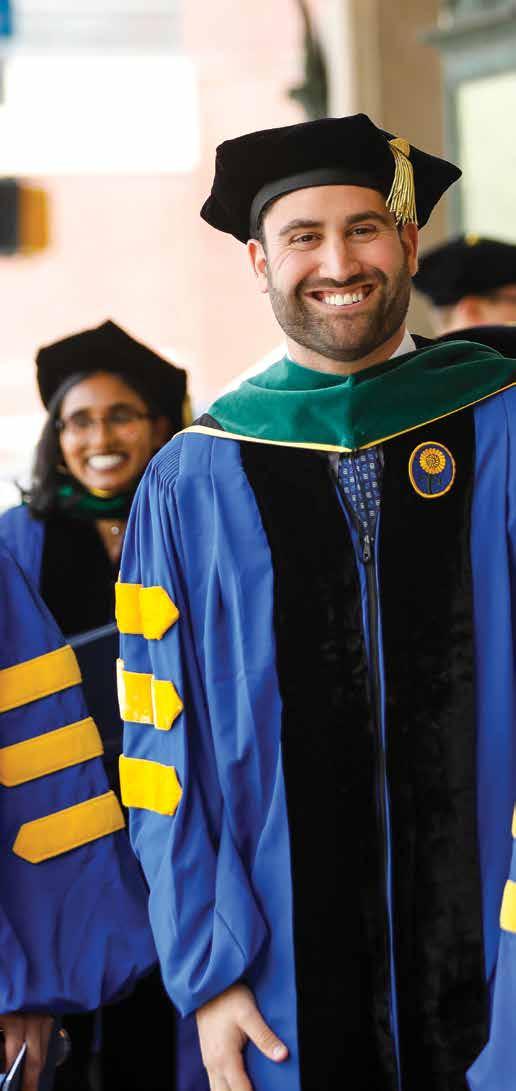
Students from the School of Medicine & Dentistry walked the stage May 12. See more snapshots from the celebration on page 6.
2 ROCHESTER MEDICINE | 2023 – V1
Photo by Matt Wittmeyer

3 ROCHESTER MEDICINE | 2023 – V1
Mark B. Taubman, MD CEO, University of Rochester Medical Center Dean, School of Medicine and Dentistry Senior Vice President for Health Sciences

TSuicide is a public health crisis. It has touched all of us and our communities directly or indirectly, just like cancer or COVID. The isolation fostered by the pandemic, by our technology-heavy lifestyles, and by our increasingly complicated world has only made the crisis worse. Most disturbing is that the problem is reaching younger and younger populations.
As you’ll see from the stories in this issue, the University of Rochester is leading the way in responding to this public health crisis. For those who know our institution well, this should not come as a surprise. The School of Medicine & Dentistry’s biopsychosocial model demands that we take a holistic view of our patients, rather than focusing solely on their illness.
In particular, the biopsychosocial model requires that we address not only our patients’ diseases but also the psychological and social issues that affect their well-being and may interfere with a successful outcome. The suicide prevention work of our faculty that you will read about in these pages springs directly from that legacy.

The results, including efforts reaching into local communities and around the world, speak for themselves. That’s where the hope comes in. We are using new approaches and taking advantage of the latest technologies to better identify and reach out to those at risk for suicide and to provide them with treatment options that truly take into consideration their socioeconomic conditions.
I hope as you read this issue, you will share my deep sense of pride in our faculty’s endeavors, which exemplify the spirit of the University of Rochester and its School of Medicine & Dentistry and which demonstrate our reach as a national leader.
I am grateful for your continued support and partnership as our journey continues. Meliora!
his issue of Rochester Medicine is about suicide. But it is also about hope. Read more Rochester Medicine RochesterMedicine.urmc.edu Submit Class Notes RochesterMedicineMagazine@urmc.rochester.edu Write to Us Rochester Medicine magazine University of Rochester Medical Center 601 Elmwood Avenue Box 643 Rochester, New York 14642 What do you think? Rochester Medicine welcomes letters from readers. The editor reserves the right to select letters for publication and to edit for style and space. Brief letters are encouraged. RochesterMedicineMagazine@urmc.rochester.edu
4 ROCHESTER MEDICINE | 2023 – V1




6 6 Crossing the Finish Line 13 Medical Center Rounds 20 No One Left Behind 30 The Power of Prevention 36 Faculty News 44 Philanthropy 48 Class Notes 50 In Memoriam 20 Cover Story Find us on facebook at: www.facebook.com/urochestermed Rochester Medicine is published by: The University of Rochester Medical Center, Department of Communications, in conjunction with the Department of Alumni Relations and Advancement for the School of Medicine and Dentistry Editors Lori Barrette Mark Liu Art Direction & Design Karen Ver Steeg Staff Writers Bethany Bushen Jim Miller Production Manager Bethany Bushen Feature Photography Matt Wittmeyer Contributors Barbara Ficarra Scott Hesel Jeff Koslofsky Mark Michaud Leslie Orr Susanne Pallo Sally Parker Sandra Parker Kelsie Smith-Hayduk Kristine Kappel Thompson Leslie White Assistant Vice President B. Chip Partner of Communications, URMC For questions or comments, contact: Dept. of Alumni Relations and Advancement for the School of Medicine and Dentistry 300 East River Road, Rochester, NY 14627 Phone 800.333.4428 585.273.5954 Fax 585.461.2081 Comments on this issue, e-mail: RochesterMedicineMagazine@urmc.rochester.edu 5 ROCHESTER MEDICINE | 2023 – V1 44 Cover Story



6 ROCHESTER MEDICINE | 2023 – V1
Crossing the Finish Line
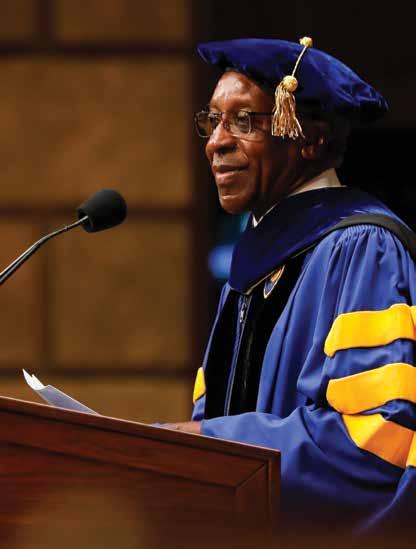
Commencement celebrations were held for students from the School of Medicine & Dentistry’s graduate and master’s programs on May 12 and 13 at Kodak Hall at Eastman Theatre and Kilbourn Hall at the Eastman School of Music campus, respectively.


Alumnus Michelle Albert (MD ’94), associate dean of admissions and professor of medicine at University of California San Francisco, gave the keynote address at SMD’s ceremony, where speakers also included University President Manglesdorf, SMD Dean Mark Taubman, MD, and others.


7 ROCHESTER MEDICINE | 2023 – V1


8 ROCHESTER MEDICINE | 2023 – V1



9 ROCHESTER MEDICINE | 2023 – V1
Alumnus Michelle Albert’s Remarkable Firsts
Commencement Keynote Speaker Reflects on Challenges Along the Way
By Bethany Bushen
Physician-scientist Michelle A. Albert (MD ’94) is the first person in history to serve concurrently as president of the American Heart Association, the Association of University Cardiologists, and the Association of Black Cardiologists. She’s also the first woman of color and Black woman to be president of the AHA and AUC. (where she is now past president).

10
–
ROCHESTER MEDICINE | 2023
V1
To be the “first” is noteworthy, but as Albert has found, it can also mean you must find ways to thrive when you feel alone.

While humbled and grateful to be asked to deliver the commencement keynote at her alma mater, Albert’s time in medical school was no picnic. She recalls being one of only three Black students in her class of 90 students. Cardiology is also a field historically dominated by males, mostly white.
Luckily, she says that good mentors don’t need to be exactly like you. They just need to be able to help you visualize a future that you can’t see for yourself.
But at first, she had to visualize on her own. Albert was born and raised in Guyana, where she and her younger sister, Maxine, lived with their grandparents in a working-class community. Her father, Michael Albert, had received a government scholarship to study in England, where he and her mother, Carmen Albert, studied and worked to help support the family.
When Albert was 14, her grandfather collapsed from cardiac arrest. Where they lived, people didn’t know CPR or have access to a portable defibrillator. Her grandfather died that day. It was a painful way for Albert to experience the impact of socioeconomics on historically under-resourced communities. But it lit the spark that set her career into motion.
Developing True Selves
Now, as a practicing clinician, researcher, and epidemiologist at the University of California at San Francisco (UCSF), she is in the position to mentor directly. She also serves as the dean of admissions for the UCSF School of Medicine and director of its NURTURE Center (CeNter for the StUdy of AdveRsiTy and CardiovascUlaR DiseasE).
Both roles have brought her full circle in many ways. She has chosen to recruit and retain a workforce that can address the unmet needs in health care. Part of her commitment is drawing more people of color into the field of cardiology. In 2022, Forbes magazine named her to its “50 Over 50” list for the impact she has made.
“Mentorship is a priority for me because I absolutely know that we all need mentors and sponsors to develop our true selves and have successful careers with authenticity,” said Albert. “I know the sense of isolation that I felt early on, and I don’t want to see the same thing perpetuated for others like me. Mentors allow us to stretch ourselves—because oftentimes we want to sit in the comfort zone. They help us see a different version of ourselves.”
“She Just Opens Doors”
Those who have had Albert as a mentor point to the example she sets and the remarkable level of care she offers people.
“The cardiovascular workforce lacks representation of Black physicians, especially Black women, and can be very isolating,” said Jonathan Butler, PhD, a social epidemiologist and minister at the NURTURE Center. He says watching Albert overcome many obstacles has inspired him. “I’ve never seen somebody so focused on work, no matter how many obstacles come her way.”
Butler first met Albert when he was a postdoctoral fellow. He applied to the position after a mutual colleague suggested she would be a good fit with his research interests (social determinants of health and cardiovascular disease, to name just two). Albert, he said, embraced him with open arms.
She is more than a professional mentor; she is a trusted friend. Every major holiday or birthday, he receives a personalized gift from her, and he still has one of the first—a set of customized gold pencils.
“Frequently, we would celebrate a NURTURE team member’s birthday,” said Butler. “Michelle planned every detail, down to the seating chart; menu; and personalized, hand-wrapped gifts for each person who came.” As he put it, “That’s the caring and detail-oriented person Michelle is.”
Melissa Burroughs, MD, credits Albert with guiding her on a long and winding road. They met when Burroughs was a medical student at Harvard and on track to become a cardiologist. For big career decisions, from choosing a residency program to getting her first job at UCSF, Burroughs, who left academics five years ago to become a noninvasive cardiologist in private practice, says Albert has been a constant source of support.
11 ROCHESTER MEDICINE | 2023 – V1
Burroughs was a resident at UCSF and returned to join the cardiology faculty in 2015. At the time, she and Albert had been only the first and second Black cardiologists on faculty.
“She’s the only reason I took that job,” Burroughs said, noting that the diversity of faculty and fellows has improved since then. She credits this to Albert’s leadership and example. “She just opens doors. We all have obstacles we need to face, especially in medicine, but it’s so much better when you have a more senior person opening doors for you.”
Burroughs said she has learned from Albert how to combine rigor with creativity. The field of cardiology is based on exciting data, but the work doesn’t stop there. “I learned from her that it’s not always about the content; it’s the approach,” Burroughs said. “I think she brings all the best qualities we want in a physician and teaches them so well. All the skills she has, you can apply to whatever you do.”
One of these skills includes compassion—both for your patients and the people you work alongside. Most important, for yourself. Burroughs says the rigor of medical training has a way of beating the compassion out of you, making it easy to fall into a trap of abandoning self-care in the process. Albert provided a voice of clarity when it was needed most.
“I called her when my father died,” said Burroughs. Her advice was simple: Work is secondary. Send an email to work and book a flight home the next day. In those moments when you know what’s most important, Burroughs reflects, “sometimes you just need someone to give you permission.”
Why Rochester?
It’s no surprise that Albert, whose interest in social determinants of health inspired her to go into medicine, was drawn to the University’s School of Medicine and Dentistry and its biopsychosocial model, which takes a holistic approach to health and looks beyond scientific presentation. Today, her research as a physician-scientist-epidemiologist explores those very questions.
“The medical school that you attend does have a significant influence on where you go in the future—through its perspectives that help shape you as a person,” said Albert. “Rochester helped crystallize that for me over time. I’ve come to realize the impact that it has had on me. It’s a process of being divinely drawn to certain things over time, resulting in my building a career around those building blocks, and Rochester was the place where the chips started falling into place.”

Albert, who lives in the San Francisco Bay Area with her husband, Edward Brown, hadn’t been back in more than two decades, despite spending years in the Northeast: She was chief medical resident at Columbia University and went on to complete a master’s degree in public health at Harvard School of Public Health as well as fellowships at Harvard Medical School and Brigham and Women’s Hospital, where she became a rising star.
She has won numerous awards and serves on national boards and committees through her affiliation with the AHA and American College of Cardiology (ACC). Her research has been featured on international media outlets, and she is an often-quoted expert on cardiovascular health, maternal health, and health equity. She is also an elected member of the National Academy of Medicine, one of the highest honors in medicine.
But she never set out to land leadership positions in the nation’s most prestigious cardiology associations. Albert says she simply followed her interests and worked hard to seize opportunities that aligned with her desire to make a difference—on a large scale.
“I think, honestly, you’re defeating yourself to start with a goal of being the president of an organization,” she said. “Your goal should be about having an impact in things that are important to developing people, including the health of the population.” RM

12 ROCHESTER MEDICINE | 2023 – V1
Dr. Albert’s School of Medicine and Dentistry class photo in 1994.
Dr. Albert in 2022, when she was named to the Forbes “50 Over 50” list.
People with Autism May Process Illusory Shapes Differently
There is this picture—you may have seen it. It is black-and-white and has two silhouettes facing one another. Or maybe you see the black vase with a white background. But now, you likely see both.
URMC researchers are finding the process in our brains that allows us to understand that these visual distinctions may not happen the same way in the brains of children with autism spectrum disorder.
“How our brain puts together pieces of an object or visual scene is important in helping us interact with our environments,” said Emily Knight, MD, PhD (Flw ’22), assistant professor of Neuroscience and Pediatrics and first author on a study published in the Journal of Neuroscience. “When we view an object or picture, our brains use processes that consider our experience and contextual information to help anticipate sensory inputs, address ambiguity, and fill in the missing information.”
Knight and fellow neuroscience researchers in the Frederick J. and Marion A. Schindler Cognitive Neurophysiology Laboratory at the Del Monte Institute for Neuroscience used visual illusions—groups of Pac-Man-shaped images that create the illusion of a shape in the empty space. Using electroencephalography (EEG), researchers revealed that children with autism did not automatically process the illusory shapes as well as children without autism.
“This tells us that these children may not be able to do the same predicting and filling in of missing visual information as their peers,” Knight said. “We now need to understand how this may relate to the atypical visual sensory behaviors we see in some children on the autism spectrum.”
Knight’s past research study, published in Molecular Autism, found that children with autism may not be able to see or process body language as their peers do, especially when distracted by something else.

The University of Rochester is one of about a dozen Intellectual and Developmental Disabilities Research Centers (IDDRC) designated by the National Institute of Child Health and Human Development (NICHD) as a national leader in research for conditions such as autism, Batten disease, and Rett syndrome. Knight and fellow researchers in both studies collaborated with fellow IDD researchers at the Rose F. Kennedy Intellectual and Developmental Disabilities Research Center (RFK-IDDRC) at Albert Einstein College of Medicine.
Other URMC authors of the Journal for Neuroscience paper include Ed Freedman, PhD, associate professor of Neuroscience; Evan Myers, PhD (Flw ’19); and Leona Oakes, PhD
MEDICAL CENTER ROUNDS NEUROSCIENCE
13 ROCHESTER MEDICINE | 2023 – V1
Frequent COVID Testing of Nursing Home Staff Protected Residents, Saved Lives

A study by URMC researchers published in the New England Journal of Medicine shows that nursing homes that conducted staff surveillance testing more regularly experienced significantly lower rates of COVID infections and deaths among residents.
“Testing is a key part of any infectious disease response, surveillance testing in particular,” said Brian McGarry (PhD ’16), an assistant professor of Medicine and Public Health Sciences and lead author of the study. “This study found that greater surveillance testing of nursing home staff was associated with clinically meaningful reductions in resident COVID cases and deaths, particularly before the availability of vaccines.”
McGarry and his co-authors tracked more than 90 million COVID test results for staff in 13,433 skilled-nursing facilities from 2020 to 2022.
The researchers found that:
• During outbreaks, high testing frequency (1.7 COVID tests per week per staff) was associated with fewer resident cases and deaths
compared to low testing frequency (0.6 per week). This difference was particularly pronounced during the pre-vaccine period—when high testing facilities had almost 25 percent fewer deaths.
• Based on the estimated relationship between test frequency and COVID cases and deaths, the study authors projected that had all facilities performed an additional test per staff member per week during the pre-vaccine phase of the pandemic, 30 percent of resident cases and 26 percent of resident COVID deaths could have been prevented.
• For nursing homes that predominantly used lab-processed COVID testing—as opposed to rapid, point-of-care tests—faster test turnaround time was associated with fewer resident deaths. The difference between receiving results in two days or fewer vs. three or more days during the pre-vaccine period was associated with 13 percent and 28 percent fewer cases and deaths, respectively.
Breastfeeding and Lactation Division Is World’s First
A first-of-its-kind breastfeeding and lactation division at URMC is leveraging the expertise of breastfeeding-medicine providers, dentists, toxicologists for medication consulting, family-medicine physicians, and researchers to promote and advance breastfeeding.
Led by Casey Rosen-Carole, MD, MPH, MSEd, FABM (Flw ’16), the division is the culmination of long-standing efforts by the departments of Pediatrics and Obstetrics and Gynecology to promote and advance the cause of breastfeeding and lactating families.
“The formation of this division confirms breastfeeding and human lactation belong in the medical field,” said Rosen-Carole.
She credits URMC Professor Emerita Ruth Lawrence (MD ’49, Res ’58) for establishing the modern foundation of breastfeeding as medical practice.
As a fully independent, multi-disciplinary group, the Division of Breastfeeding and Lactation Medicine provides a variety of services for patients. The division additionally will work to make breastfeeding accessible for families who may face obstacles due to socio-economic barriers or lack of institutional support.
• Surveillance testing was not strongly associated with cases or deaths during the post-vaccine/pre-omicron phase.
• Frequent surveillance testing was associated with fewer resident cases but no difference in deaths during the omicron wave, a finding consistent with the reduction in vaccine efficacy for preventing COVID infections, but not in preventing hospitalizations and deaths.
“The best evidence recommends that children are breastfed for at least two years, but the world is not set up for lactating families,” said Rosen-Carole. “There remains inadequate paid parental leave, poor coverage for lactation support, and inadequate access to donor milk for most families in this country.”
The division will navigate these obstacles by meeting patients where they are and setting realistic, sustainable goals.
Since 2016, Rosen-Carole has been the director of Lactation Services and has overseen the growth of the program. In 2019, the group established its own clinical site, and in 2020, added third-year fellow Michele Burtner, CNM, MS, IBCLC (Flw ’21, MPH ’21), as assistant director of the program.
In addition to providing clinical services, the division will advance research in human milk and feeding science, best-practice implementation, and breastfeeding education. Bridget Young, PhD, assistant research professor of Pediatrics and Public Health Sciences, is research director of the division.
14 ROCHESTER MEDICINE | 2023 – V1
NEW PARTNERSHIP
Public Health
MEDICAL CENTER ROUNDS
Team Discovers Previously Unknown Brain Component and Why It’s There
URMC researchers have discovered a previously unknown component of brain anatomy that acts as both a protective barrier and a platform from which immune cells monitor the brain for infection and inflammation.
Conditions as diverse as multiple sclerosis, central nervous system infections, and Alzheimer’s might be triggered or worsened by abnormalities in how this newly discovered component functions.
The work, described in the journal Science, comes from the labs of Maiken Nedergaard, MD, DMSc, co-director of the Center for Translational Neuromedicine at University of Rochester and the University of Copenhagen, and Kjeld Møllgård, MD, a professor of neuroanatomy at the University of Copenhagen.
“The discovery of a new anatomic structure that segregates and helps control the flow of cerebrospinal fluid (CSF) in and around the brain now provides us much greater appreciation of the sophisticated role that CSF plays not only in transporting and removing waste from the brain but also in supporting its immune defenses,” said Nedergaard.
Traditional understanding of the brain’s meningeal layer identifies the three individual layers: dura, arachnoid, and pia

matter. URMC’s researchers further divided the space between the arachnoid and pia layers—the subarachnoid space— into two compartments separated by the newly described layer, which the researchers named SLYM (Subarachnoidal LYmphatic-like Membrane).
This membrane is thin, delicate, and only a few cells thick. Yet SLYM is a tight barrier, and it also seems to separate “clean” from “dirty” CSF. This hints at the likely role played by SLYM in the glymphatic system, which requires a controlled flow and exchange of CSF—allowing the influx of fresh CSF while flushing away the toxic proteins associated with Alzheimer’s and other neurological diseases.
The SLYM also appears important to the brain’s defenses. The central nervous system maintains its own native population of immune cells, and the membrane’s integrity prevents outside immune cells from entering. In addition, the membrane appears to host its own population of central nervous system immune cells that use SLYM as an observation point, close to the surface of the brain, from which to scan passing CSF for signs of infection or inflammation.
CLINICAL INNOVATION
Skin Cancer Detection: New Device Seeks to Shorten Wait Time for Biopsy Results
A 3D imaging device invented by a young investigator at the Wilmot Cancer Institute can accurately detect two types of non-melanoma skin cancer and report results within minutes, according to a pilot study published in JAMA Dermatology

Michael Giacomelli, PhD, assistant professor of Biomedical Engineering, started working on the device when he was a doctoral student at the Massachusetts Institute of Technology. Since then, he’s been conducting research
to test its efficiency. Of the 15 biopsies reported in JAMA, diagnosis of basal cell carcinoma displayed perfect accuracy, and diagnosis of squamous cell skin cancer displayed 89 percent sensitivity and 100 percent specificity.
The imaging system was designed to be rolled on a small cart into an operating room or other clinical space and provide real-time results to physicians who have taken biopsies of lesions suspected to be cancerous.

NEUROSCIENCE
15 ROCHESTER MEDICINE | 2023 – V1
Harnessing Power, Precision of RNA to Make Mutations Invisible
University of Rochester Medical Center scientists have discovered a new way to suppress mutations that lead to a wide range of genetic disorders. A study published in the journal Molecular Cell describes a strategy that co-opts a normal RNA modification process within cells to transform disease genes into normal genes that produce healthy proteins.
Around 15 percent of mutations that lead to genetic diseases are called nonsense mutations, which occur when an mRNA molecule contains an early “stop” signal. When the mRNA takes genetic instructions from DNA to create a protein, this early stop sign orders the cell to stop reading the instructions partway through the process. This results in the creation of an incomplete protein that can lead to disease.
Led by Yi-Tao Yu, PhD, Dean’s Professor of Biochemistry and Biophysics, a team of researchers from University of Rochester’s Center for RNA Biology designed an artificial guide RNA to target mRNA molecules that contain premature-termination codons.

Like DNA, RNA is made up of molecular building blocks that are
represented by the letters A (adenine), G (guanine), U (uracil), and C (cytosine). Premature-termination codons always have the building block U in the first position. The team’s artificial guide RNA was designed to modify the U in the first position, changing the molecular makeup of the targeted mRNA so that the stop signal is no longer—or is less well— recognized by the cell.
The team—including Paul Boutz, PhD, assistant professor of Biochemistry and Biophysics; graduate students Yi Pan and Xueyang He; postdoctoral fellow Jonathan Chen; staff scientist Hironori Adachi; and researchers from ProQR Therapeutics—tested the artificial guide RNA in yeast cells and in human disease cells (derived from cystic fibrosis and neurofibromatosis patients). In both cases, they found that the action of the artificial guide RNA rendered the prematuretermination codon (stop sign) invisible, allowing cells to read the genetic instructions all the way through and create full-length, functional proteins.
They also discovered that the guide RNA suppressed another mechanism, known as nonsense-mediated mRNA
decay or NMD, in the cell. Curbing NMD is another way the artificial guide RNA ensured that a significant amount of mRNA was present in the cell and that the genetic instructions carried by the targeted mRNAs were read all the way through and translated into complete proteins.
Yu believes his team’s strategy to suppress nonsense mutations in disease genes has great potential to help patients with CF and many other inherited genetic diseases.
“Our technique is promising because we didn’t observe any negative, off-target effects. Using a single guide RNA in disease cells—and nothing else—we can specifically suppress nonsense mutations without disturbing other parts of the cell,” said Yu.
“Dr. Yu’s research is at the forefront of the most promising treatment modalities for cystic fibrosis and, potentially, other genetic diseases,” said Jeffrey J. Hayes, PhD, chair and Shohei Koide Professor of Biochemistry and Biophysics at URMC’s School of Medicine and Dentistry.
GENETICS
MEDICAL CENTER ROUNDS 16 ROCHESTER MEDICINE | 2023 – V1
Members of Yi-Tao Yu’s lab in the Center for RNA Biology.
Studies Show Telemedicine is Effective, Doesn’t Reduce Access to Care

Common concerns about telemedicine don’t hold up to scrutiny, a first-ofits-kind study highlighting telemedicine’s remarkable effectiveness concludes.
The paper is one of two studies on telemedicine by URMC researchers that appeared simultaneously in NEJM Catalyst. The second study demonstrates the success of URMC’s effort to provide mental-health services to nursing homes via a hybrid model that includes telemedicine.
“For patients, the message is clear and reassuring: Telemedicine is an effective and efficient way of receiving many kinds of health care,” said Kathleen Fear, PhD, lead author of the first paper, “Busting Myths about the Impact of Telemedicine Parity,” and director of data and analytics at the UR Health Lab. “Especially for those with transportation challenges, it is a service that really fills a gap—and, vitally, it does not compromise the quality of the care that patients receive.”
Fear and her co-authors used data generated in part by the COVID pandemic to examine three specific concerns about telemedicine:
• That it will reduce access to care for the most vulnerable patients who may be unable to access digital services.
• That reimbursing providers for telemedicine services at the same rate as traditional services will encourage telemedicine overuse.
• That telemedicine is not an effective way to provide care.
“We really dug into the data, and it disproved all three concerns, which is really quite exciting,” Fear said. “Not only did our most vulnerable patients not get left behind—they were among those engaging the most with, and benefitting the most from, telemedicine services. We did not see worse outcomes or increased costs or patients needing an increased amount of in-person follow up. Nor did we find evidence of overuse. This is good care, and it is equitable care for vulnerable populations.”
Michael Hasselberg, RN (MS ’07, PhD ’13), URMC’s chief digital-health officer and the study’s senior author, said the paper marks the first time anyone has published comprehensive data refuting
the three myths. URMC researchers were in a unique position to undertake the study because of the work of more than 3,000 providers across the health system who engage in telemedicine and of the UR Health Lab’s ability to analyze the data generated by their work.
The second NEJM Catalyst study looked at a program URMC physicians developed to bring psychiatric and psychotherapeutic resources to nursing home patients through a combination of telehealth, on-site visits, and staff education. The researchers concluded that the program improved access to care and reduced the number of residents requiring anti-psychotic medication.
“With a small team that we assembled here at URMC, we’ve been able to have a huge reach, extending care to patients in parts of the state where high-quality mental-health services are scarce at best,” said Adam Simning (PhD ’11, MD ’13, Res ’17, Flw ’18), assistant professor of Psychiatry and the study’s lead author.
PATIENT CARE
17 ROCHESTER MEDICINE | 2023 – V1
ORTHOPAEDIC RESEARCH

CMSR Sustains National Leadership Standing for 20+ Years
In the intense competition for ever-scarcer NIH funding, leading musculoskeletal research centers across the nation jockey for top positions year after year. The Center for Musculoskeletal Research has been in the top 10 NIH-funded orthopaedic research centers since 2000 and placed fourth in national funding in orthopaedics for 2022, according to rankings compiled by the Blue Ridge Institute for Medical Research.
It’s no secret why CMSR has been at the top so consistently and for so long, said Edward M. Schwarz, PhD, the Richard and Margaret Burton Distinguished Professor of Orthopaedics and Director of CMSR. “You have to make the commitment to sustain and grow the next generation of researchers to have results like this for more than two decades.”
CMSR’s formula for developing young researchers into fierce grant competitors includes:
• Researcher-physician dyads: CMSR pairs each new PhD recruit with an orthopaedic surgeon to give the researcher real-world understanding of the clinical challenges their investigations can impact—because high-value investigations win the competition for NIH support.
• Mentoring: All new investigators are assigned more experienced CMSR researchers to mentor them on research planning, grant applications, and more
• Weekly focus sessions: Every Friday morning, new researchers meet as a group with Schwarz to review every challenge they’re facing, from setting up and staffing their labs to grant writing to work-life balance.
The center’s focus on career development and its longstanding funding success attract talent from outside as well as from within URMC, Schwarz added.
CMSR’s project outcomes are getting national attention. A research team led by Chao Xie, MD, MSBA (Flw ’07), recently achieved a world-first, microscopic look—captured on video— at a joint implant infection overtaking the joint space in real time and presented their findings at the Orthopaedic Research Society meeting.
“The attendees were awestruck,” Schwarz said. “The scientific finding about infection of an implant is not the remarkable part—it’s that you can actually see it taking place and see how quickly an untreated infection can overwhelm an implant. Industry reps and FDA officials at the meeting were very interested in this as a way to more quickly evaluate potential new drugs and antimicrobial implants and bring them to market.”
MEDICAL CENTER ROUNDS
18 ROCHESTER MEDICINE | 2023 – V1
Black Patients Less Likely to Undergo Minimally Invasive Heart Surgery, More Likely to Die
A URMC study suggests that Black patients do not have the same level of access to minimally invasive heart procedures as white patients.

“We’ve known for 35 years that historically marginalized racial and ethnic groups tend to have less access to cardiovascular procedures,” said lead study author Laurent G. Glance, MD, professor of Anesthesiology and Perioperative Medicine. “This study highlights the fact that, even in 2022, if you’re not white, you don’t get the same therapies that white people do.”
Published in JAMA Network Open, the study found that compared to non-Hispanic white patients, non-Hispanic Black patients had 35 percent lower odds of undergoing minimally invasive mitral-valve surgery and 62 percent higher odds of having serious complications or dying. Hispanic patients, on the other hand, had 26 percent higher odds of major complications or death compared to white patients, but they were not less likely to receive minimally invasive surgery.
“Minimally invasive surgeries set patients up for the best outcomes,” said
study co-author Peter Knight, MD (Flw ’87), Department of Surgery chief and Dr. Jude S. Sauer Family Distinguished Professor in Cardiac Surgery, who has spearheaded the adoption of minimally invasive procedures at URMC. “That is why the inequities we found in this study are so troubling.”
The authors note several patterns in the data that may point to factors contributing to this inequity: Black patients were more likely to have Medicaid insurance, seek treatment at under-resourced hospitals, and be treated by less experienced surgeons. Where patients sought care mattered. This study found that Black patients had 31-fold higher odds of being treated at hospitals that serve a very high proportion of Black patients than they were to be treated at a hospital that serves a low proportion.
Unfortunately, hospitals that primarily serve historically marginalized racial and ethnic groups tend to be under-resourced. To improve equity, Glance recommends that the Centers for Medicare and Medicaid Services create
better financial incentives for care for historically marginalized patients.
Black patients were also more likely than white patients to be treated by doctors who perform a low volume of mitral-valve surgeries. These less-experienced surgeons were 20 times less likely to perform minimally invasive procedures.
Study authors believe that regionalizing care may help increase Black patients’ access to highly experienced surgeons.
Other study co-authors at URMC include Michael P. Eaton, MD, chair of Anesthesiology and Perioperative Medicine; Denham S. Ward, MD, PhD, professor of Anesthesiology and Perioperative Services; Isaac Y. Wu, MD, associate professor of Anesthesiology and Perioperative Services; Julie A. Wyrobek, MD, assistant professor of Anesthesiology and Perioperative Services; and Changyong Feng (PhD ’02), professor of Biostatistics and Computational Biology, Anesthesiology and Perioperative Services, and Dentistry.
EQUITABLE CARE
19 ROCHESTER MEDICINE | 2023 – V1

20
Peter A. Wyman
No One Left Behind
By Sandra Parker
In recent decades, military suicide rates have increased substantially. Suicides now account for 25 percent of all active-duty military deaths, and rates in the Air Force have risen even faster than other military branches. Since 2015, the Air Force has lost more members to suicide than to combat.
That same year, a University of Rochester Medical Center program of the Center for the Study and Prevention of Suicide (CSPS) launched at an Air Force base in Wichita Falls, Texas. That in itself was noteworthy—research trials between universities and the military are rare. But this intervention also took a decidedly different approach.
Peter A. Wyman (Flw ’88, PhD ’87, MA ’84), co-director of the CSPS, founded and directed the Wingman-Connect program as proactive, “upstream” prevention aimed at the source. It would work to harness the power of groups and social networks to prevent thoughts of suicide before they ever occurred.
After nearly a decade of deployment, the program’s results have been impressive—impressive enough for the Air Force to expand the program to all 68 bases around the world. The Air Force’s $5 million contract will allow Wyman and core members Anthony R. Pisani, PhD (Flw ’03) and Bryan Yates (BA ’13) to update the curriculum and develop resources for a large-scale rollout that is projected to reach more than half a million airmen (the Air Force term for all of its members) by 2035.
Their success is especially significant because the problem has proven stubbornly resistant to change, despite unprecedented increases in funding to support military suicide prevention.
“If you think of suicide as the tip of the iceberg, something isn’t working well,” says Eric D. Caine, MD, a long-time member of the research team measuring results. “Suicide is the uppermost weathervane for how a service is doing.”
Most other programs present information about suicide warning signs and adopt a reactive approach by identifying and treating people at risk. But one chilling statistic explained the need for something more: Most suicides occur in people not identified as high risk. So it was absolutely necessary to go back to the drawing board and “build a better aircraft.”

In doing so, Wyman’s group made an important discovery. Suicide-preventive coping skills are most often learned from close-knit peers who are readily accessible and share values.
In a radical departure from the standard suicide prevention paradigm, Wingman-Connect builds suicide protection directly into military social networks. By strengthening all members and connections within a small peer network, vulnerable members can “borrow strength” from the others during times of need.
A Rochester program took a radical new approach to suicide prevention. Now the Air Force is rolling it out to every base in the world.
Members of one Air Force cohort in the program learned the importance of keeping fellow airmen from isolating too much.

22 ROCHESTER MEDICINE | 2023 – V1
“For a suicidal individual, being embedded within a cohesive, healthy social network can be the difference between life-saving hope and despair,” Wyman says.

23 ROCHESTER MEDICINE | 2023 – V1
“For a suicidal individual, being embedded within a cohesive, healthy social network can be the difference between life-saving hope and despair,” Wyman says.

The promise of this approach is that it can apply to other settings. In recently funded work, Wyman’s team is adapting the program to other groups that are high priorities in suicide prevention. As testament to the versatility of the “Connect” model, new projects have begun in predominantly Black churches and also first-responder groups.
So far, these efforts have gone well. Versatility could prove to be the model’s biggest breakthrough.
Career Goals = Health Goals
Wyman’s gold-standard, randomizedcontrolled trial at Sheppard Air Force Base in Wichita Falls assessed the program for first-term airmen.

“Typically, military suicide prevention programs have been rolled out with minimal testing,” says Wyman, “and that’s part of why this problem has been so hard to resolve. And so conducting a rigorous randomized trial of this program is both important and rarely done.”
Wyman obtained a $4 million grant in 2014 from the Department of Defense to create Wingman-Connect for the Air Force and roll it out over a five-year period. He selected four core principles—kinship, purpose, guidance, and balance—based on research showing that they’re key to health, mental health, and career success. And he made the strategic decision to promote the training primarily as a means to improve overall health and career success.
“Our initial work showed that airmen are highly motivated to achieve their career
goals, and this was the key incentive to getting them engaged” says Wyman. “And so we don’t say, ‘Hey, come to anti-suicide training.’ That’s not a strong motivator. We say, ‘Come to careerenhancement training.’ ”
To test the program, Wyman conducted a special cluster randomized trial, which randomly assigns whole groups rather than individuals. Participants were 1,485 airmen in 215 training classes. Half were enrolled in Wingman-Connect (three blocks of two hours each), using interactive, group-facilitated sessions and sharing of personal examples to build cohesion.
The other half, the control group, received training designed to mimic standard military mental health resilience training. This included a two-hour stress management program using passive learning through slide shows, videos, and discussions. Afterward, both groups received a one-hour refresher session and follow-up text messages.
The study, published in JAMA Network Open in 2020, found that WingmanConnect, in comparison to the stress management program, significantly reduced the severity of suicide-risk scores, depression symptoms, and work-related issues. And the effects were still apparent in follow-up contact six months later.
It’s not just about stemming individual negative behaviors, but also about building positive group connections and practices that serve as a strong foundation of healthy norms. The study reported gains on multiple suicideprotective factors: “cohesion, morale, bonds to classmates, and perceptions that members support healthy behaviors.”
In follow-ups, airmen in the WingmanConnect program were 20 percent less likely to report elevated depression symptoms than those who participated in the stress management program.
And they were 50 percent less likely to report significant incidents of occupational problems such as corrective job training.
Borrowed Strength
Wingman-Connect was not designed specifically for airmen at elevated suicide risk, but analysis showed that those who entered the program already at risk for suicide experienced the greatest benefit.
“For airmen who were at elevated risk for suicide, their isolation tends to worsen over time, and this is a known risk factor for suicide,” according to Ian Cero (Flw ’21), a member of the research team. “Wingman-Connect, in contrast, counteracted this expected drift, increasing the number of new connections that vulnerable airmen made to members of their unit.”
Ian Cero
Cero and Wyman published these findings in 2022 in Social Science and Medicine. Cero says the most surprising thing about these findings is that Wingman-Connect increased the number of healthy airmen who said they were connected to vulnerable members, even though the training provides no specific direction to connect with at-risk peers.
In the control group, however, 10 percent of vulnerable airmen remained isolated, reporting no connections to classmates at the end of the training.
Wyman says suicides are commonly preceded by “disrupted relationships,” a common issue in the military as members often move far from home. Yet the standard paradigm for preventing suicides doesn’t address disconnection from others, which is a known risk.

“In more connected, healthier units, vulnerable members can borrow strength from adaptive members,” Wyman found.
Participants in Wingman-Connect were significantly more likely to name two classmates as “valued connections,” which was the benchmark for successful unit integration set by the military.
The study validated Wyman’s “network health model”—the idea of strengthening the network so it can strengthen the individual.
How that’s done might come as a surprise to people who have preconceived notions about what the military is like.
A Six-Hour Tour— Yarn Provided
A startling aspect of WingmanConnect’s success is that the program consists of only six hours of actual training: Three two-hour blocks take place over three days, followed by weekly text messages for six months.
It’s also active, as opposed to the traditional—and passive—approach of sitting through slide presentations. Airmen take part in experiential group activities, with a facilitator playing a nuanced role in encouraging the trainees to discover positive strategies from each other.
“The learning happens through personally meaningful sharing,” says Pisani.
Sometimes it involves an empty chair and a ball of blue yarn.

In a departure from the boring icebreaker of going around the room and stating your name, WingmanConnect opens with a version of the musical chairs game. The group of about 40 airmen sit on chairs arranged in a circle. Seven of them volunteer to turn their chairs around and gather in the middle to share their names, hometowns, and reasons for enlisting.
“Airmen sharing their reasons for enlisting increases the personal meaningfulness of the training, and others learn of their values, critical for building strong bonds,” Wyman says.
Then the facilitator asks questions, such as who has ever caught a fish. As the airmen-fishermen rise and come to the middle, others race to fill their empty seats. The game ends when everyone who is willing to share has done so. By the end of the game, almost everyone has shared (no one is forced to share), and the bonds of kinship begin to grow.
In the yarn knot game, pairs are tied together with yarn and need to figure out how to untether themselves without simply pulling off the yarn. There’s a trick to it, which involves working with your partner.
Another game shows that small cracks, not just major ones, can lead to hardship. One person stands on a wooden platform while 12
others grab attached ropes and hoist the platform. They march around the room, supporting the person on the wobbly platform. Then the number of people holding the ropes is gradually reduced, representing the loss of relationships supporting those four principles that are at the core of the program. Things get wobblier as core support diminishes.
After a discussion about stressors, airmen make posters to illustrate what has gotten them through the tough times at Basic Military Training and what helps them manage the stress and challenges in technical school. Some simply write a list, others draw their answers (stick figures abound, and labeling is critical to tell a cat from a rat, but that’s fine—it’s a lesson in bonding, not artistry). The posters explore the program’s core principles: kinship, purpose, guidance, and balance. Airmen begin to see the person behind the uniform, says core member Yates, who serves as one of the facilitators.
The culmination arrives when airmen do a self-assessment of the four core principles. In one session, Yates asks them to share their strategies for managing anger, sadness, and anxiety, focusing on the positive coping mechanisms rather than the challenging emotion itself. Then Yates introduces the idea of sustaining oneself through personal initiative and group support. Rather than offer a list of solutions, Yates asks trainees to share their own
 Bryan Yates
Bryan Yates
strategies and ways they’ve found success in their military careers.

On day two, the seed previously planted has typically germinated. The chair game is repeated, but this time airmen share their favorite healthy activities. The discussion session that follows is about purpose, so they’re asked to share how to turn their initial reasons for enlisting into commitment. After acknowledging difficult issues that arise, such as thoughts of quitting, Yates shifts the focus to the positive by encouraging airmen to share strategies for staying connected to and building their core of purpose.
At this point, a group identity has emerged and, after the day’s training, breakout groups are tasked with devising a plan to build on one of the core strengths. Some build kinship by dining together or working out in the gym. Yates recalls that one participant, Airman Juel Eason, persuaded his group to buy 1980s-style basketball shorts and ride through the base on bicycles. It was a spectacle and great fun.
On the last day, groups fill out a poster listing everyone’s name and strength under at least one of the four principles. Many airmen are surprised at how others in the group view them.
“We often see a real transformation that unifies them in ways we haven’t seen before,” Wyman says.
One airman who had continually voiced her opposition to being at the training announced that she wasn’t strong in any category because she was falling short of her goals. The group strongly disagreed, pointing out that she was motivated and accomplished.
“People in her group weren’t going to let her talk down about herself,” Yates says. “That’s the secret sauce. This training is not just about mindset but behavior. The connections that carry forward from the room are the new protection.”
In an audio recording of one group, a collegial and relaxed dynamic is obvious as airmen enthusiastically call out each other’s names.

“Beamer goes in ‘Guidance’,” one airman says. “He mentors us.” Another chimes in: “He tells us not to stress out.”
Then Mace Beamer himself weighs in cheerfully. “I bring a lot of life experience,” he says.
Other airmen are praised for strengths such as being the voice of reason, or staying focused on values and goals. There is typically a class comedian, the one who “lightens the mood.” Someone else gets a nod in the kinship column for being “the fist-bump god.”
The program showed Airmen Isaiah Rush (left) and Tarzis Lobos that they could count on each other as friends who have each other’s back.
Getting the Nod from the Generals
Universities and the military operate with very different needs and norms, so partnerships between them are complicated. But they’re essential, and this one took substantial commitment from Air Force leaders to make it work, says Peter Wyman, PhD, co-director of the Center for the Study and Prevention of Suicide.

Steven E. Pflanz (MD ’94), then USAF colonel and director of Psychological Health, was one of these critical leaders. Air Force generals had to buy into the program, says Pflanz, now the deputy chief of staff at Syracuse VA Medical Center.

The common perception of the military might be tough guys with philosophies of “Suck it up” and “Drop and give me 20 pushups, maggot,” but the generals were active advocates of the idea of protecting mental health.
“The military is much more enlightened than [the film] Private Benjamin,” Pflanz says. “The military has imperfections, but it’s committed to evolving. There are dinosaurs, but most are moving forward.”
Key to the success of suicide prevention programs is eliminating the shame often associated with mental health struggles and promoting understanding of the need for prevention and treatment.
“Wingman-Connect reduces suicide risk but also builds cohesion and makes the group healthier, which is important for a fighting unit,” Pflanz says. “So much of leaving no one behind is simple but so powerful. Morale is essential.”
“The service is dedicated to meeting the needs of our airmen, guardians, and families,” says Christopher Goode, PhD, the acting division chief for the Integrated Resilience Directorate of the Air Force. “Wingman-Connect has shown extraordinary results during its pilot and implementation phases.”
In the Department of Defense’s 2021 annual report on suicides, Secretary Lloyd J. Austin III succinctly stated his opinion on the stigma problem: “Mental health is health, period.”
With Wingman-Connect, says Pflanz, “it was always about how to fit it in, not whether we should do this.”

“Wingman-Connect reduces suicide risk but also builds cohesion and makes the group healthier, which is important for a fighting unit.”
27 ROCHESTER MEDICINE | 2023 – V1
Steven E. Pflanz
One goal of the training is to ensure that everyone leaves with at least two valued colleagues. Trainees discover that they have a wingman. And, typically, more than one.
In videotaped comments, Airman Tyler Wilkey says: “I learned that you have to have a balance in life. If you don’t get that balance, then everything just falls apart. And it did fall apart once or twice since I’ve been in, but I had my friend to back me up whenever I needed him.”
Airman Tarzis Lobos said the interactivity made the training more effective. “In other trainings, I just watch it and I’m supposed to get something out of that, but in the end I take away nothing.”
Wingman-Connect prompted him to open up and share with the other trainees.
“At certain times you feel very alone,” he says. “You need those bonds, people who can pull you out of your room so you’re not just sitting and stewing in your sadness but can get you out there so you can see brightness again.”
Airman Isaiah Rush gleefully points to himself when Lobos mentions people who pull him out of isolation.
“After the Wingman-Connect interaction, it really made us come together because we started hanging out together,” Rush says. “It started a lot of friendships for me.” At one point in the discussion of friendship, Rush elbows Lobos, who smiles.
Lobos speaks gratefully of the airmen who “forced me to leave my room and really want to go places.”
And the training has given him the insight and skills to identify that behavior in others: “Whenever there are people that separate a little too much and it feels that maybe they are struggling, you understand to pull them back into the group.”
Using Contagious Attitudes for Good

The success of Wingman-Connect has led the team to further adapt the program to reach other groups in need.
“Schools, workplaces, faith and other community organizations provide most people with some opportunity to become part of a social network,” Wyman says. “What inspires my research team is learning how we can enrich and build those natural social networks to increase suicide protection and health.”
It is well established that peers wield tremendous power over each other, so Wyman decided to make use of that as a force for change.
“Rather than bemoaning this fact, it actually offers immense opportunity to capture and leverage peer group influence for prevention and health,” Wyman says. “Just as suicide can be contagious, so too can be the attitudes and behaviors that counter suicide and help people thrive.”
“The core concepts are widely applicable,” Pisani says. “People live, change, and grow in relationships, and those relationships form a network. Strengthening that network is key. There’s a great deal of promise that it can be applied across a wide range of environments.”
So Wyman’s team collaborated with Sherry Molock, PhD (George Washington University), and Sidney Hankerson, MD (Mt Sinai), to adapt the Connect strategies to address the increasing suicide rate of Black adolescents. The Haven-Connect program is now being tested in a dozen predominantly Black churches in Rochester and Harlem.
Pastor Fredrick Johnson of the First Genesis Baptist Church in the city of Rochester says he hopes the training will help heal the damage that lingers since the darkest days of the pandemic. Depression and anxiety are well-known effects of the forced isolation, which was especially devastating for teens.
So far, Johnson has heard only positive comments from the teens and adult church members who have gone through the training. They appreciate the engaging, group-bonding activities that replace the standard method of dispensing advice via slide shows. Some teens who were introverted or disruptive began to alter their behavior after the training.
“I think there’s a hunger of many young folks looking for healthy, engaging relationships,” Johnson says. “This program creates an environment of healthy, supportive interaction. And it’s not just for those in crisis mode but for those who are ready to shift paths. It gives them tools.”
Another new expansion is the Connect program for New York State police officers, which so far has been implemented in Albany, Mamaroneck, and Port Chester, with support from the New York State Office of Mental Health. The training is adapted for the variety of ages and experience levels. Wyman says it has been well received by the officers.
Positivity is one component that sets Wingman-Connect and its offshoots apart from other prevention programs.
“Other trainings focus on the negative effects that come from stressors, whereas Wingman-Connect, I believe, is focused on—it’s in the name—building that connection with our wingmen,” says Airman Destiny Garner.
“I think Wingman-Connect reminds us at the end of the day that, although we put on this uniform, we are still people.” RM


29 ROCHESTER MEDICINE | 2023 – V1
“This program creates an environment of healthy, supportive interaction. And it’s not just for those in crisis mode but for those who are ready to shift paths. It gives them tools.”
Pastor Fredrick Johnson
The Power Prevention of

30 ROCHESTER MEDICINE | 2023 – V1
Arielle Sheftall
Center
By Sally Parker
When Arielle Sheftall, PhD, was 14, she lost her mother to cancer. Depression and anxiety took hold, and she started to experience thoughts of suicide.
In the end, her family got her the treatment she needed. Now, as an associate professor of Psychiatry in the School of Medicine and Dentistry, Sheftall understands there are many people facing similar moments in life, and she’s determined to change that, using her experience as a guide.
Sheftall is co-leading a five-year, $4.5 million research project funded by the National Institutes of Health to see if nerve-stimulating earbuds and a newly created peer support app can help reduce risk factors (such as depression) in teens to prevent suicidal thoughts from occurring.

The use of earbuds and a phone app is recognition that for hard-to-reach populations like teens, help must find those in need, not the other way around.
It’s just the latest example of innovative approaches that have kept Rochester at the forefront of suicide prevention and research for more than two decades. Sheftall works in the Center for the Study and Prevention of Suicide (CSPS), where faculty and postdoctoral fellows team up across disciplines to study the issue of suicide from all angles—psychiatric, psychological, social, cultural, and medical.
The work began in the late 1980s, when Eric Caine, MD, professor emeritus of Psychiatry in the School of Medicine and Dentistry, along with Yeates Conwell, MD, professor of Psychiatry in the School of Medicine and Dentistry, collaborated with the Monroe County Medical Examiner’s Office to study deaths of undetermined cause. At a time of growing interest in suicide research, they were among the first in the world to systematize
what became known as the psychological autopsy. (See It Started with a Simple Call on page 32 )
Conwell, who is also vice chair of the Department of Psychiatry, soon founded the Laboratory for Suicide Studies. As colleagues in various disciplines joined, the research effort took shape as the CSPS in 1998. Kimberly Van Orden, PhD, associate professor of Psychiatry, and Peter Wyman, PhD, professor of Psychiatry, are current co-directors.
The center’s focus from the start has been the public health aspect of suicide, and it has earned an international reputation as a leader in the field. The CSPS has a long history of collaboration with suicide prevention researchers around the world.
All this has helped the CSPS lead research and interventions that cover the entire lifespan and reach more and more into diverse populations. The work is leveraging the latest tools such
as digital health platforms and social networking, with real-world effects. Recently, a CSPS program to help stem a rise in the rate of suicide in the armed forces has begun rolling out to every U.S. Air Force base in the world. (See No One Left Behind on page 21.)
All told, the Center promises to make a difference in a tragic problem that remains near its peak, even as society only slowly changes to acknowledge it.
Addressing All Stages in Many Places
Roughly 132 people in the U.S. die by suicide each day—a rate of 13.42 per 100,000, according to the Centers for Disease Control and Prevention. The rate hit a 20-year high in 2018, dipped for two years, but then spiked in 2021.
Traditional approaches focus on helping people who show warning signs. But as Caine points out, many people who attempt suicide are not
31 ROCHESTER MEDICINE | 2023 – V1
The
for the Study and Prevention of Suicide has led the way for decades. Now comes the next frontier.
It Started with a Simple Call
in contact with the health system. So investigators have had to get creative. They’ve teamed up with community systems outside the Medical Center—schools, courts and criminal justice programs, social services, and aging-support agencies—to understand the societal and individual causes of suicide and to find ways to prevent it.
The Center has received continuous funding from the National Institutes of Health, the Centers for Disease Control, and several foundations since the early 1990s.
In 2000, it launched the nation’s first NIH-funded T32 postdoctoral training fellowship in suicide prevention. Fellows are core team members and some, like co-director Van Orden, have stayed on as URMC faculty members.


According to Conwell, their work is based on a longstanding belief “that we can make the most progress and best contribution to suicide prevention by recognizing it as a multi-determined phenomenon that requires lots of different perspectives to be brought together.”
The key, says Caine, is to ask, “What can we do for people who are suicidal now—what are the acute treatments? And then, what are the interventions that we can do upstream that prevent them from ever becoming suicidal?”
In the 1980s, Eric Caine, MD, picked up the phone and called Nick Forbes, the Monroe County medical examiner, to ask if he’d like “a couple of free psychiatric consultants.” As a psychiatrist, Caine, a self-described optimist, wanted to understand what causes people to take their own lives.

He and Yeates Conwell, MD, looked at hundreds of files of adult deaths—autopsies, toxicology reports, narratives—for whom manner of death was uncertain.
Their work helped pioneer the psychological autopsy, a review of information culled from interviews with friends and family in order to understand how things unfolded in the final weeks of life.
Conwell started the Laboratory of Suicide Studies in 1989 to study late-life depression. Soon he and Caine, fueled by funding from the National Institutes of Health, expanded the team to include psychologists, sociologists, and others through hiring and fellowship programs. By the mid-1990s, the CSPS had taken shape.
The center’s influence widened in the 2000s. It began a robust research collaboration and exchange with scientists in Hong Kong and China that continues today. From 2001 to 2005, CSPS conferences in Washington, D.C., cemented its reputation as a leader in its publichealth approach.
In 2021, CSPS faculty developed a plan to answer these questions. It established three focus areas: innovative methodologies, the full lifespan, and diverse populations. These priorities—achieved through everything from texting to companionship programs—will guide the Center’s direction for the next several years, carrying their work to new frontiers.
Can a Text Save Lives?
The use of smartphones and digital health platforms in suicide prevention science is exploding. “Many of our early career scientists are eager to study these innovative methodologies,” co-director Van Orden says.
Rochester investigators are using technology to find new avenues for their work in assessment and intervention on suicide risk factors. New technology also makes it easier to deliver mental health services to underserved populations.
In a study with Spanish speakers, assistant professor of psychiatry Caroline Silva, PhD, connects with participants through their smartphones to assess social engagement and suicide risk. Van Orden and Silva are using this method with older adults as well.
ROCHESTER MEDICINE | 2023 – V1 32
Kimberly Van Orden, PhD
Yeates Conwell, MD
Eric Caine, MD
Text4Strength, developed by Anthony Pisani, PhD, an associate professor in Psychiatry and Pediatrics, sends automated text messages to students enrolled in Sources of Strength, a high school suicide prevention program. The goal is for students to build help-seeking skills, emotion self-regulation, and stronger connections. Pisani has developed texting and social media components for a similar program, led by Wyman, for young enlisted airmen in the U.S. Air Force.

Center investigators are also working on a crisis text suicide prevention program for young people. They’re collaborating with the nation’s largest crisis text provider to test the potential. Others are working with computer scientists on the University’s River Campus to develop an online social skills coach for older adults that mimics human interaction.

Part of the idea behind these new methodologies is reaching people where they live. But there’s also a need to address the growing age span of suicide.
Addressing the Troubling Age Range
Understanding what drives suicide and finding ways to prevent it along the entire lifespan is another key focus area for the Center.
Suicide rates among children and teens are rising at an alarming pace. From 1990 to 2020, the youngest age at suicide fell from nine to just five years old. In that same timespan, the number of deaths by suicide among five- to twelve-year-olds shot up 195 percent.
At the University’s Mt. Hope Family Center, director of research Elizabeth Handley, PhD, studies the ways childhood maltreatment increases risk for suicide among youth. For children who live in high-risk environments, family depression and substance-use disorders can increase vulnerability. Handley, a research associate professor in Psychiatry, is among a cadre of CSPS investigators who are deeply involved in Mt. Hope, a national leader in research and clinical

33 ROCHESTER MEDICINE | 2023 – V1
Anthony Pisani, PhD
Caroline Silva, PhD
(From left) Rachel Missell-Gray, Jenson Rowan, Arielle Sheftall, and Dakota Daniels work on the peer-support app for teens.
care in developmental psychopathology.
Sheftall is studying emotion regulation and neurocognitive functioning in nine- to elevenyear-olds who have a parental history of suicide attempts. The study, funded by a grant from the National Institute of Mental Health, will follow 300 youth in Rochester over four years.
“I really believe at the adolescent stage, we’re coming to the party late already,” says Sheftall, who also focuses on racial disparities in suicidal behavior among children and teens. “If we attack emotion dysregulation early on in a child’s life, we might have a fighting chance at saving that child and making sure they get the help they need.”
But she knows the need is there for older children as well. The NIH-funded research project she’s co-leading with colleagues from the University of Notre Dame will enroll 212 teen participants in Rochester and Indiana.

Some will use an FDA-approved device, which looks like ear buds, to stimulate the transcutaneous vagus nerve. This has been shown to decrease anxiety and depression in adults. Another group will use a peer-support phone app with a journaling component for expressing their feelings in words, “in a space instead of in their heads,” Sheftall says. It also will
Serving Those Who Served
have a gaming feature with a chat component that breaks the ice for conversations with other teens who share what they’re going through.
A third group will use both approaches. Sheftall says she hopes nontraditional methods for a tech-savvy generation will open new doors.
“We know rates of suicide among adolescents and even younger [children] have been increasing drastically over the last decade. That’s why I keep doing the work I do,” she says.
Center faculty also research suicide risk in midlife, focusing on addiction struggles, sleep problems, and language and cultural isolation. Wilfred Pigeon, PhD, a professor of Psychiatry and former executive director of the VISN2 Center of Excellence for Suicide Prevention at the Canandaigua VA Medical Center, looks at suicide risk and prevention through the lens of sleep disturbance.
Kenneth Conner, PsyD, MPH, professor of Emergency Medicine, led a team studying a brief intervention for use with individuals with alcohol or drug use problems who have been hospitalized following a suicide attempt. He is also developing projects to prevent unintentional drug overdose. (See story below.)

The Veterans Administration calls veteran suicide prevention its highest clinical priority. In 2020, the suicide rate for veterans was 57 percent higher than for non-veteran U.S. adults, adjusting for population, age, and gender differences. Nearly 6,200 veterans took their own lives that year.

Since 2007, when Eric Caine, MD, helped shape the VISN2 Center of Excellence for Suicide Prevention at the Canandaigua VA Medical Center, CSPS investigators have been deeply involved in studying the issue. Today their work is a national resource.
Most of the VA faculty have URMC appointments; the junior investigator training programs of both centers work closely together. Several former executive directors of the VISN2 Center have roots at URMC, including current Executive Director Stephanie Gamble, a former postdoc fellow, and Professor Wilfred Pigeon, PhD.
Again, the work is ambitious in scope. Studies and interventions seek to reduce suicide risk through a veterans’ crisis line, pain management, violence prevention, and help with depression, sleep disorders, PTSD, and injuries.
Elizabeth Handley, PhD
34 ROCHESTER MEDICINE | 2023 – V1
Kenneth Conner, PsyD
Greater social connection is a crucial factor in healthy aging, and many studies show disconnection is a public health concern. As a mortality risk, it’s as big as obesity, physical inactivity, alcohol misuse, and smoking.
Van Orden studies interventions that will foster connection among older adults. She and Conwell have tested community-based social services designed to encourage more social connection in later life, including a peer companionship program called The Senior Connection and volunteering with AmeriCorps Seniors. The team has also developed a brief psychotherapy intervention that Silva is adapting for Spanish speakers at risk for suicide.
A key benefit of how the Medical Center functions is the interplay between research and clinical work.
“URMC is a world leader in the collection of patient-reported outcomes, including depression, as part of routine clinical care,” Van Orden says. It’s a matter of capitalizing on URMC’s “infrastructure and expertise—as both a laboratory for studying suicide prevention efforts as well as a means to optimize the quality of care for patients in UR Medicine.”
Diverse in Many Ways
The Center’s reach into diverse populations includes Black and Hispanic youth and adults and the Deaf community.
Deaf and Hard of Hearing people are at greater risk of suicide than the general population. They have higher rates of severe mental health issues and, at the same time, are more likely to mistrust the health care system and so are less likely to receive treatment.
Aileen Aldalur, PhD senior instructor of Psychiatry, is working on ways to more easily connect Deaf and Hard of Hearing people to mental health services. The CBT intervention she is adapting uses videophone or Zoom technologies that are more accessible.

Sheftall is particularly interested in a concerning rise in suicide rates among Black teens and children. Her research has shown that five- to twelve-year-olds who are Black are twice as likely to take their own lives than are their white counterparts. And in 2020, suicide was tied for the No. 1 cause of death among Black girls ages 12 to 14.
“I think this information is something people are not aware of,” she says. “It’s just not out there.”
And it’s difficult for society to solve a problem that isn’t even known. So Sheftall’s research has been raising awareness. She has made
HOPE in Later Life
The HOPE (Helping Older People Engage) Lab engages in upstream suicide prevention by helping older adults build healthy social connections.

Kim Van Orden, PhD, runs the lab, which teams with Lifespan and other community agencies on studies and interventions for loneliness and suicide risk. One study is testing the benefits of volunteering for lonely older adults—making phone calls to isolated individuals or helping out at an animal shelter. Other studies have tested the value of peer companionship programs and behavioral psychotherapy.
Van Orden says older people prioritize emotional well-being, and it increases with age—“a strength we can capitalize on.” She says her mother, despite physical health and cognition problems, was her happiest after moving into a senior living community, where she made new friends and fell in love at age 72.
“To me,” says Van Orden, “suicide prevention in later life is about course correcting—getting older adults back onto the healthy aging trajectory and helping them address risk factors for suicide by growing their own protective factors.”
it a point to discuss her findings in public statements, op-ed articles in the media, and interviews to get the research in front of more people.
This is the kind of exploration that is leading the CSPS into the future, Van Orden says. “We want to extend that work,” she says, in new directions “that capitalize on the expertise of our investigators and emerging, innovative methodologies.” RM
35 ROCHESTER MEDICINE | 2023 – V1
Aileen Aldalur, PhD
Vertino Takes the Reins as Leader of Basic Science at SMD
Paula Vertino, PhD, an accomplished cancer research scientist and Wilmot Cancer Institute Distinguished Professor in Cancer Genomics, has been appointed senior associate dean for Basic Research.


Vertino was recruited to Wilmot in 2018 to promote collaboration and team science. She enjoys bringing people together using a “grass roots” approach.
In her new role, she wants to work with institutional leadership to create an environment that fosters faculty and trainee success. She also plans to further integrate the basic and clinical research enterprise.
“I feel strongly that as a leader, one needs to be as invested in what others are doing as in one’s own research program,” noted Vertino.
“Paula’s role in bridging the gap from very basic science to more applied cancerclinical work, along with the enrichment she’s already brought to our educational programs, makes her a perfect fit for this position,” said Mark B. Taubman, MD, dean of the School of Medicine and Dentistry and CEO of URMC. “We can’t wait to see her new ideas come to fruition and help
continue to foster a vibrant research community here at SMD.”
Steven Dewhurst, PhD, vice dean for research, noted the impact Vertino has made on the University since moving to Rochester four years ago: “One of Paula’s many gifts is her ability to build connections between people and to make members of our scientific community feel valued and included. She’s a brilliant scientist, but she’s also warm and kind.”
Vertino, who is also professor of Biomedical Genetics and Pathology and Laboratory Medicine, pioneered a new elective concentration in cancer biology, which saw its first graduate last May. And she continues to work closely with researchers at the UR Aging Institute to develop ways for older cancer patients to use digital technology for behavioral and supportive-care interventions.
Vertino, along with Kah Poh Loh, MBBCh (Flw ’18, Flw ’19), a hematologist, oncologist, and geriatrician, and Michelle Janelsins-Benton, PhD (MS ’05, PhD ’08, MPH ’13), associate professor of Surgery, Radiation Oncology, and Neuroscience, were
Maquat Awarded 2023 Gruber Genetics Prize
Lynne E. Maquat, PhD, founding director of the Center for RNA Biology, received the 2023 Gruber Genetics Prize for her discovery of nonsense-mediated mRNA decay, or NMD, in humans. The Gruber International Prize Program, administered by Yale University, honors scientists from around the world whose groundbreaking work leads to fundamental shifts in knowledge and benefits mankind.
Maquat has spent her career deciphering the many roles that RNA plays in health and is best known for elucidating the complexities of NMD in mammalian cells and human disease. One of the major surveillance systems in the body, NMD protects against mistakes in gene expression by targeting and eliminating deleterious mRNAs that could lead to incomplete and potentially toxic proteins.
Maquat’s lab also revealed that NMD helps our cells adjust to changes in development and in their environment as well as more rapidly respond to certain stimuli.
“Lynne’s scientific prowess and steadfast commitment to her research is exemplary and has helped catapult the field of RNA biology to the forefront of medicine over the past decade,” said Mark B. Taubman, MD, CEO of URMC and dean of the School of Medicine and Dentistry. “This is an exciting time, as Lynne and other scientists are putting her mechanistic findings related to NMD to use to design treatments. She is incredibly deserving of this honor.”
Maquat shared the award with Allan Jacobson, PhD, of the University of Massachusetts Chan Medical School, who was honored for his contributions in describing the mechanism of NMD in yeast.
Maquat’s lab is using its knowledge of NMD to inform the development of therapeutics for fragile X syndrome, a neurological disorder that leads to intellectual disability and severe learning problems.
Maquat, the J. Lowell Orbison Endowed Chair and Professor in the Department of Biochemistry and Biophysics in SMD, is the recipient of several other significant honors,
awarded the inaugural UR Aging Institute pilot grant last year—a perfect example of the type of cross-center collaboration Vertino hopes to inspire.
Vertino takes over for Dirk Bohmann, PhD, who stepped down in late 2022.
including the Wolf Prize in Medicine (2021), Warren Alpert Foundation Prize (2021), Wiley Prize in Biomedical Sciences (2018), Vanderbilt Prize in Biomedical Science (2017), Canada Gairdner International Award (2015), and RNA Society’s Lifetime Achievement Awards in Service (2010) and in Science (2017).
36 ROCHESTER MEDICINE | 2023 – V1
FACULTY NEWS
Paula Vertino, PhD
Lynne E. Maquat, PhD
Friedman Ross Named Inaugural Chair of the New Department of Health Humanities and Bioethics
“This new department will embody the core principles of the biopsychosocial model, focusing attention on the moral aspects of research and patient care programs,” said Mark Taubman, MD, CEO of the Medical Center and SMD dean. “As a distinguished expert in clinical medical ethics, Dr. Ross will help us further strengthen a well-respected program and build a vibrant department to address today’s ever-expanding ethical and societal questions related to health care.”
URMC was among the first academic medical centers in the country to have a humanities division and, now, is just one of eight with a dedicated humanities and bioethics department.
to working with the many wonderful colleagues I have met, who understand and value the fundamental role that ethics, the arts, and the humanities play in promoting health.”
Ethical and policy issues in pediatrics, organ transplantation, genetics/genomics, clinical research ethics, and human-subject protections are the focuses of Ross’s expertise. She has published five books and more than 225 peer-reviewed journal articles and is writing a sixth book, examining ethical issues related to siblings in health care.
Lainie Friedman Ross, MD, PhD, a pediatrician and internationally renowned bioethicist recruited from the University of Chicago, has been tapped as the inaugural chair of URMC’s new Department of Health Humanities and Bioethics and director of the Paul M. Schyve, MD, Center for Bioethics.

Ross has nearly three decades of experience influencing discussion and policy around pediatric care, organ transplantation, genetics/genomics, clinical research ethics, and human-subject protections.
“I am excited to join an institution where the biopsychosocial model was developed and is rooted in every aspect of care, education, and research,” she said. I look forward
A frequent lecturer both nationally and internationally, Ross has been awarded prestigious honors and academic appointments, including the Kellogg National Leadership Fellowship, Class of XVI (1997–2000); a 2009 Hastings Fellowship; the Patricia Price Browne Prize in Biomedical Ethics in 2009; and a 2014 John Simon Guggenheim Memorial Foundation Fellowship. In 2015, she received the American Academy of Pediatrics William G. Bartholome Award for Ethical Excellence.
Baumhauer to Serve as Senior Associate Dean for Academic Affairs
Judith Baumhauer, MD, MPH, a long-time faculty leader, has been named senior associate dean for Academic Affairs.

“Judy’s deep commitment to her colleagues, to URMC, and to those we serve has long been evident, whether through her groundbreaking work with patient-reported outcomes, her leadership in clinical trials or, most recently, her service as associate dean for Academic Affairs,” said SMD Dean and URMC CEO Mark Taubman, MD. “Her experience, institutional knowledge, and track record of success make her an ideal person to fill this vital position and to ensure Academic Affairs thrives in the years ahead.”
Baumhauer, tenured professor of Orthopaedics, succeeds Jeffrey Lyness (BA ’82, MD ’86), who accepted a position as president and CEO of the Chicago-based American Board of Psychiatry and Neurology.
As senior associate dean, Baumhauer will oversee faculty appointments and reappointments, along with the promotion and tenure processes. She’ll spearhead professional development initiatives as well as the recruitment and onboarding of faculty leaders.
“I’m grateful to accept this role and excited by the opportunity to have a meaningful and positive impact on the growth and advancement of our outstanding faculty and staff within SMD,” said Baumhauer.
“I look forward to both building on Dr. Lyness’s positive legacy and to bringing fresh ideas forward for faculty development and processes.
“As faculty, we are here to provide the best possible care to patients, to lead and mentor others, to teach the physicians of the future, and to undertake transformative research. Academic Affairs plays a key
role in fostering the vitality that makes this possible, and it is a privilege to be chosen to lead it.”
37 ROCHESTER MEDICINE | 2023 – V1
Lainie Friedman Ross, MD, PhD
Judith Baumhauer, MD, MPH
Hartmann to Retire after 20 Years of Dedication to GME Programs
Diane Hartmann (MD ’87), whose two-decade tenure as senior associate dean for graduate medical education saw dramatic growth in our residency programs, is stepping down.

“Diane was never content just to meet the standard—she wanted to set the standard, and she did,” said SMD Dean Mark Taubman, MD “She brought increasing structure and visibility to our programs. Her national profile and credibility was never more evident than when she led the effort that resulted in URMC being one of only a handful of institutions nationwide chosen to participate in the ACGME’s Pursuing Excellence initiative, which will help ensure the prestige of our programs for years to come.”
Under Hartmann, the number of accredited training positions for residents and fellows rose from 598 to 930. The number of ACGME-accredited residencies and fellowships rose from 49 to 93. Collaboration deepened between her office and our hospitals, as did an emphasis on wellness, quality, and safety.
“Our program has evolved with the times to remain a national leader,” Hartmann said. “We’ve worked quickly to adapt to changing technologies and incorporate them into our programs, to make wellness an essential part of our residency and fellowship experiences, and to remain on the cutting edge as education has shifted from time-based requirements to a greater—and very welcome—emphasis on competency and work quality.”
Hartmann considers the Pursuing Excellence grant, which was awarded in 2018, one of her biggest contributions to URMC. The resulting initiative, which operates under the aegis of the Quality Institute, focuses on building better teams, integrating residents and fellows directly into performance-improvement and qualityimprovement teams.
“Pursuing Excellence is transforming medical education through an increased emphasis on experiential, team-based learning and
patient care—with an increased emphasis on quality, safety, and continuous improvement,” said CMO Michael Apostolakos, MD (Res ’90, Flw ’93), who, with Hartmann, serves on the Pursuing Excellence executive team. “Diane has led the way on both fronts and has been a key part of our successes, which include both decreased length of stay and readmissions.”
A national search will be conducted for her successor.
“One day in GME is never like the next,” she said. Things are always changing, and they have to for medical education to grow and to allow the physicians of the future to gain the skills they will need in practice.”
Ania Majewska Named Co-Director of UR-IDDRC
Ania Majewska, PhD, professor of Neuroscience, has joined John Foxe, PhD, as co-director of the University of Rochester Intellectual and Developmental Disabilities Research Center (UR-IDDRC). Majewska is also the director of the Cell and Molecular Imaging core of the Center.

Her research, focused on developmental neuroscience, recently showed that the toxin the consumption of meat, dairy products, and fish, can cause the brain’s immune system to go awry later in life, potentially damaging important brain circuits and potentially contributing to disorders such as autism and ADHD.
“We are absolutely thrilled to have Dr. Majewska in this role,” said Foxe. “She is a leader in IDD research at the Medical
Center. Her research is transforming what we understand about the developing brain. Coupled with her storied history of being an outstanding mentor, she will help continue to support and leverage the IDD research underway across the University and Medical Center.”
The University of Rochester is one of 16 institutions to receive IDDRC designation.
Majewska received the National Institute of Neurological Disorders and Stroke (NINDS) 2022 Landis Award for Outstanding Mentorship. In 2021, she received the Peter Shrager Award for her successful leadership of the Neuroscience Graduate Program, dedication to science, and compassion.
FACULTY NEWS 38 ROCHESTER MEDICINE | 2023 – V1
Diane Hartmann, MD
Ania Majewska, PhD
M. Patricia Rivera Used Great Resolve on Her Way to Presidency of the American Thoracic Society
M. Patricia Rivera, MD, who grew up hearing that “people like you” don’t go to college, is the new president of the American Thoracic Society (ATS).
A noted lung cancer specialist who serves in many leadership roles at the University of Rochester Medical Center and Wilmot Cancer Institute, Rivera is the first Latino woman to lead the large, international organization. She is also the first faculty member from the University of Rochester to do so.

When Rivera took the helm on May 23, 2023, she shared some personal aspects of her life story at an installation ceremony in front of a large audience. She spoke of hardships—she is the daughter of Cuban-Columbian immigrants who fled Cuba during the revolution, and as a young professional she faced the devastating loss of a child. But she said her journey has provided valuable lessons along the way.
“I learned about dedication, hard work, and resilience,” Rivera said. “It’s what many immigrants need to do to survive.”
Rivera, the Jane Davis & C. Robert Davis Distinguished Professor in Pulmonary Medicine at URMC, joined URMC in April of 2022. She serves as chief of the Division of Pulmonary and Critical Care Medicine and also filled a newly created position at Wilmot Cancer Institute as associate director for Diversity, Equity and Inclusion (DEI).
In her various roles, she emphasizes that “climbing the ladder” takes courage and help from others.
“You have to always extend a hand,” she said. “There’s a misconception that people who are successful in academic life have had a linear path. But there are a lot of setbacks along the way. Nelson Mandela said: ‘Do not judge me by my successes; judge me by how many times I fell down and got back up.’ ”
From Can’t to Can Do
Rivera lived in Cuba and Colombia before emigrating to the United States, spending her early years in Brooklyn. Although she often heard, “people like you can’t or don’t go to University,” her grandmother and mother encouraged her to pursue her ambitions.
She was awarded a full undergraduate scholarship to Pace University, working two jobs while completing studies and graduating summa cum laude with a bachelor of science degree in Biology.
She then attended Stony Brook School of Medicine in New York and proceeded as an intern and resident at North Shore University Hospital. Her fellowship training and the start to her career in pulmonary medicine began at Memorial Sloan-Kettering Cancer Center in New York City.
Years earlier, Rivera said, her grandmother in Cuba was denied those same opportunities for medical school because she was a woman. So, her grandmother chose pharmacy instead—and became one of the first women to graduate from the University of Havana’s School of Pharmacy. She worked hard while raising five children.
One of those children was Rivera’s mother, who studied dentistry. Eventually, Rivera’s parents fled Cuba for South America and several years later landed in downstate New York to build a new life. But tragedy struck when Rivera’s father died unexpectedly of a massive stroke.
“My mother became a widow at age 36 with four children,” Rivera said. “I watched my mother overcome many obstacles and work so hard until age 72 to raise us and provide us with an education. From her, I learned how to push through.”
Heartbreak and Heart
She would need those lessons in resilience during a painful time in her own adult life, as Rivera and her husband were establishing themselves, newly married in 1993, in Chapel Hill, North Carolina. While her husband, Ben, a surgeon, was starting his career at the University of North Carolina, Rivera was the “trailing spouse” and put aside her academic aspirations for a time. In 1994, she was also pregnant with twin boys, and sadly, one passed away immediately after birth.
At that time, popular opinion among female professionals said it was not wise to “let them see your grief,” she said. There were no grief support groups on campus, but Rivera sought help in the broader
community. She ended up getting involved in counseling others as she made her own peace with grief. She also said she discovered that being transparent with colleagues and academic leaders, male and female, was the best course of action.
A year later, she was recruited to UNC. “Experience taught me that I could start again and achieve success,” she said.
While at UNC, Rivera co-founded the first Multidisciplinary Thoracic Oncology Program (MTOP) in the country, a premier program that became the model for multidisciplinary care and defined the vital role pulmonologists play in patients with thoracic malignancies.
At the American Thoracic Society, the largest respiratory society in the world with 16,000 members, Rivera will lead a five-member executive committee.
Jim White, MD, PhD, professor of Medicine and leader of the URMC pulmonary hypertension program, was in the audience at ATS and came away energized.
“I was so proud to call myself a U of R faculty member after this address,” he said in an email to Department of Medicine colleagues. “I’m sure there were many in the audience motivated and inspired to be better humans and citizens of a global community after listening to her.”
39 ROCHESTER MEDICINE | 2023 – V1
M. Patricia Rivera, MD
Dr. David Linehan Associate Director of Clinical Research Wilmot Cancer Institute Chair, Department of Surgery University of Rochester Medical Center
September 30, 2023 Inaugural Breakaway Ride
October 1, 2023 Warrior Walk and 5K

WILMOT WARRIOR WEEKEND leaving cancer in the dust
40 ROCHESTER MEDICINE | 2023 – V1
Giving 100% to conquer cancer. Register | Form a team | Sponsor warriorweekend.urmc.edu

"
"
I walk to honor my friends and family, and the Wilmot Cancer Institute doctors, nurses, and researchers–they’re making a real difference and saving lives. They’re all part of my team.
Emily Robbins, T-Cell Acute Lymphoblastic Leukemia survivor
#WilmotWarrior WARRIOR WEEKEND 41 ROCHESTER MEDICINE | 2023 – V1
PATRICK BROPHY
Says Fond Farewells to a Community that Rallied Around Him

 By Jim Miller
By Jim Miller
42 ROCHESTER MEDICINE | 2023 – V1
Patrick Brophy, MD, outgoing William H. Eilinger Chair of Pediatrics, learned early in his tenure just how special the University of Rochester Medical Center and the Rochester communities are.
While still new in town, Brophy discovered he had a recurrence of lymphoma. He was far from his extended family and existing support networks, yet he found himself among friends. Rochester rallied around him. So did his colleagues, from fellow pediatricians to School of Medicine and Dentistry Dean Mark Taubman, MD
Brophy, who was also physician-in-chief at Golisano Children’s Hospital (GCH), became a patient at the Medical Center, taking part in a clinical trial of CAR T-cell therapy that put him in a coma for two weeks.
“The first person I really remember seeing when I woke up was Dean Taubman, and I was told he’d come quite often to check on me,” Brophy said. “He’d never ask to be acknowledged for that, but when you hear that and see that from a leader, it means a heck of a lot. I’d just arrived in Rochester, and here was this amazing support—from him and from the entire community.”
In the years since, Brophy has amply repaid that debt. Presiding over a period of sustained growth, he emphasized equity and diversity while launching a bold strategic plan that will guide GCH for years to come. He also spearheaded community outreach efforts and embraced new technologies.
And he did it all while leading GCH and the department through the COVID-19 pandemic.
Now, Brophy is stepping down to become provincial head of Child Health and Pediatrics for the Canadian province of Saskatchewan—a move that will both bring him closer to family and allow him to effect change on a regional scale.
Brophy joined URMC in 2018 after a decade at the University of Iowa. He quickly began work on the new strategic plan, which launched in January of 2020 with emphases on patient care, research, education, culture, digital health, population health, and community outreach.

He and his team ultimately worked with more than 70 community partners, organizing collaborative efforts to secure more than $25 million in public funding for various programs.
“I’ve always believed in reaching out to the people we serve—not just waiting for them to come to the hospital,” Brophy said. “We’ve worked to improve bus routes so kids can get to clinics; reached out to ensure high-risk kids were getting vaccinated, maintaining local rates as they declined nationwide; established an initiative that uses long-active reversible contraception to reduce unwanted pregnancies; and launched partnerships to send nurses out to mothers with newborns. We focus on health—not just health care.”
Those who have worked with Brophy say they’ll remember his extraordinary kindness, creativity, and energy.
Tim Stevens, MD, professor of Pediatrics and chief clinical officer for GCH, said Brophy was known for responding to problems with an understated “I have an idea about that.” He’d then follow up with a novel and effective approach.
Elizabeth McAnarney, MD, former GCH physician-in-chief and Pediatrics chair, called him a change leader and a big thinker.
“He’s really a person for all seasons with regard to the mission of academic pediatrics, with achievements in research and education—as well as in clinical care—that have built on our department’s long-standing legacy of community pediatric excellence,” she said. “He has also made great strides toward equity and inclusivity, appointing a number of women to leadership positions and creating scholarship programs named for Susan B. Anthony and Frederick Douglass.”
For faculty, Brophy became a person to rely on and a source of strength during the difficult pandemic years. When large in-person meetings became inadvisable, he instituted weekly Zoom rounds to keep everyone connected. He led successful fundraising efforts and emphasized growth and recruitment—key factors in the success of a relatively young children’s hospital like GCH.
“The second you meet Pat, it’s clear he’s very personable,” said Kurt Ingalls, CFO for the Department of Pediatrics. “You see, hear, and experience it. He has a fantastic sense of humor, and one of his gifts is that he can really connect with anyone—faculty, staff, donors, the community.”
The results are clear. During his tenure, GCH recruited more than 70 new faculty members and saw significant increases in patient numbers. Efforts to address the pediatric behavioral health crisis were launched, including a new Behavioral Health & Wellness Center, expanded Mobile Crisis Team and school partnerships, and the region’s first pediatric walk-in behavioral health center.
Federal funding for faculty research grew. A first-of-its-kind Division of Breastfeeding and Lactation was established, along with a new residency track in digital health.
“Dr. Brophy is an inspiring leader who always puts children first,” said Jill Halterman, MD, MPH, interim chair of Pediatrics. “It has been exciting to see the department and the Children’s Hospital grow under his leadership to meet the needs of children and families throughout the region. I am personally extremely grateful for his ongoing partnership and support as we aim for a seamless transition to keep all of the good work moving forward.”
Brophy, says Taubman, “has been an exemplary and visionary leader. It speaks volumes about Dr. Brophy’s talent that his work here at the Medical Center led to this extraordinary opportunity. We wish him well.”
A national search is underway for Brophy’s successor. Whoever it is, Brophy sees great potential in the role.
“The soul of a community is reflected in how it cares for its children, and Rochester cares deeply about its kids,” Brophy said. “Whoever takes on my roles is a very lucky person. We’re starting to make headway on the national stage even as we become Upstate’s primary child-health center and research powerhouse. We’re doing that while maintaining our focus on providing access and care for all the children we serve. If we keep that as our North Star, the future is limitlessly bright.”
43 ROCHESTER MEDICINE | 2023 – V1
P. Christopher Cook, MD, and the Secret to Training Orthopaedic Surgical Residents
An orthopaedic rotation during medical school changed the life of P. Christopher Cook, MD, the Dr. C. McCollister Evarts Professor in Orthopaedics.

“That rotation set my career path,” says Cook, who is also chief of the Division of Pediatric Orthopaedics and head of resident training for orthopaedic surgery.
“Combining my interest in both pediatrics and orthopaedic surgery has allowed me to help children in a hands-on way, both of which were, and remain, important to me.”
But he also chose to help surgical residents, because he knows the difference that excellent training can make.
One thing that has made the resident program he oversees so coveted and effective is an emphasis on innovation— specialty labs and equipment, for example, made possible by funding from generous donors such as William P. Thorpe, MD (Res ’81), and his wife, Judy. In the Kenneth DeHaven Skills (KEDS) Laboratory at UR Medicine’s Sawgrass Surgical Center, the Thorpes’ funding has allowed residents to
learn techniques such as drilling a pin into bone and practicing arthroscopy using simulation software. Arthroscopy is the minimally invasive surgical procedure that DeHaven himself, the first chief of sports medicine in the Orthopaedics Department, helped pioneer. It is now practiced worldwide for joint repair and ACL reconstruction.
Cook explains that training like this helps students “gain the essential surgical skills they need before entering the operating room to work on real patients. It’s a
Orthopaedics & Physical Performance Center Nears Completion
The new UR Medicine Orthopaedics & Physical Performance Center at Marketplace Mall in Rochester, slated to fully open in late 2023, will offer easy access, the latest and best approaches to care, and a full range of musculoskeletal services for patients of all ages and abilities. This includes all the expertise, facilities, and equipment needed to diagnose and treat bone, muscle, spine, and joint conditions. It also includes an array of medical imaging, physical therapy, sports medicine, athletic training, injury prevention, and nutrition and mind-body wellness services. Everything will be available under one roof, creating an orthopaedics campus unlike any other in the Northeast. Philanthropy like the Thorpes’ has provided vital support for the center and the education and training that will happen there.

ROCHESTER MEDICINE | 2023 – V1 44 PHILANTHROPY
distinguishing aspect of what the orthopaedics department offers, and it draws the most qualified residents.”
In fact, every year, up to 800 medical students apply for the eight available resident spots. Cook and department leadership interview about 120 applicants, then pare those down to fill the coveted positions. His goal is to make sure that residents become competent, well-rounded surgeons who excel in patient care and surgical skills.
The resident training program offers learning opportunities across all orthopaedic specialties. In his supervisory role, Cook is responsible for overseeing resident education, curriculum, and well-being, as well as the application process. This is on top of his work helping children with bone issues, including infections, birth defects, spinal deformities, and trauma to bones and joints (including sports injuries).
The Thorpes’ gift will also be felt in the new Orthopaedics & Physical Performance Center (see bottom of page 44). The KEDS Lab will move to a space four times larger at the new location.
“In the new KEDS Lab, our orthopaedic residents will get to practice a variety of techniques, including using equipment such as sawbones; these are composite bone models designed to simulate real bones,” says Cook. And virtual reality programs “will allow them to practice and observe what they are doing as they are doing it and make corrections along the way.”
The Thorpes’ support also will further collaborative learning. Experts such as Cook will be able to link various classrooms digitally to UR Medicine’s 150-person auditorium and to operating rooms so people can work and learn together no matter where they are.
Adds Cook, “As with computers, which tend to double in speed and power every 18 months or so, there’s a constant need for us to bring in new equipment and techniques. The Thorpes’ generosity helps us do that and keeps us on the cutting edge of surgical technology and training.”
“Judy and I are and remain grateful to those institutions from whom we received our education and preparation for work life. I did not attend the University, even though I grew up in Rochester. But I did my orthopaedic residency there. I felt well trained and very respectful of all my instructors— Drs. Evarts, Burton, DeHaven, Jackman, and many others. Judy and I are fond of having included the University in our grateful giving. I know many others are likewise so grateful.” —William P. Thorpe, MD (Res ’81), and Judy Thorpe
$1.5 Million Gift Establishes the Serletti Family Cleft and Craniofacial Humanitarian Outreach Initiative and Future Professorship
In the fall of 2022, Joseph Serletti (MD ’82, Res ’88) and Bonnie Serletti (MD ’90, Res ’94), made a $1.5 million gift to endow the Serletti Family Cleft and Craniofacial Humanitarian Outreach Initiative at URMC.


The Serlettis’ generosity will initially support local and international outreach and advocacy efforts of the Pediatric Cleft and Craniofacial Center within URMC’s Division of Plastic Surgery at Golisano Children’s Hospital.
In the future, the endowment will fund the Serletti Family Professorship, which will help attract, retain, and honor exemplary faculty clinicians in the plastic surgery division.
“The University of Rochester Medical Center is my home,” says Joseph Serletti, the Henry Royster-William Maul Measey Professor of Surgery, chief of the Division of Plastic Surgery, and vice chair for finance in the Department of Surgery at the University of Pennsylvania. “It’s where Bonnie and I were educated and trained and where I practiced for many years. It was important for me and Bonnie to give back to a place that gave us both so much.”
45 ROCHESTER MEDICINE | 2023 – V1
Finding a Home in Her Hometown
Aekta Miglani (’04, MD ’10, Res ’13) didn’t expect to stay local. Now, she’s a leader in Strong’s Emergency Department as it embarks on record-breaking growth.
What kind of place could take someone who wanted to go far away—as far as the moon, say—and entice her to stay right where she was?
As a child, Aekta Miglani (’04, MD ’10, Res ’13) wanted to grow up to be an artist or architect, or maybe even an astronaut. She dreamed big, and her parents encouraged her through it all. But they also shared the future they saw for her: a career in medicine.

When it came time to apply to college, Miglani, who grew up in Pittsford, New York, wanted to prove her parents wrong. “My plan was to apply to the University of Rochester’s undergraduate-to-medical school program and show my parents that I could get in, after which it would be clear to everyone that medicine would not be the right path for me,” says Miglani.
Sure enough, she was accepted into the University’s Rochester Early Medical Scholars (REMS) program, which grants select students admission to both the undergraduate College and the School of Medicine and Dentistry (SMD). But when Miglani met with her advisor and head of REMS, Gregory Connors, MD, he told her something she didn’t expect.
“He said that as a college student at Rochester, I could still pursue my creative interests and that the best physicians use both sides of their brain,” she adds. “I was intrigued and quickly realized that medicine could very well be a good fit.” Her parents were right after all.
Because Miglani was already accepted into the medical school, she had proven her aptitude for the sciences. This meant she could take full advantage of the University’s flexible undergraduate curriculum, which she did. She took courses in art, religion, and philosophy—and she loved it all.
Would she ever leave?
At the end of her senior year of college, Miglani was a bit nervous about the pending demands of medical school. That’s when she met Flavia Nobay, MD, a recent transplant to Rochester and the new director of the REMS program, who inspired
and reassured her. Nobay—now a professor in the Department of Emergency Medicine and the associate dean for student affairs— and others like her reaffirmed Miglani’s decision to become a physician.
Miglani has never looked back. As she finished medical school, she was on track to pursue a surgical residency.
She did her final clinical rotation, in her fourth year of medical school, in emergency medicine. “After the second or third shift in Strong Memorial Hospital’s Emergency Department, I realized that this was the place for me,” she says. “I fell for the people who worked in the ED and their approach to medicine.”
When it came time to match for her residency, the University of Rochester’s medical school became Miglani’s first choice—again.
By the time her three-year residency ended, Miglani had become one of the ED’s chief residents. She thought it was finally time to leave Rochester.
But then her mother was diagnosed with cancer, so Miglani needed to stay nearby. She spoke with Michael Farhad Kamali, MD (Res ’01), a professor and the chair of the ED, about staying another year. “Dr. Kamali told me that I could stay, but that I might never want to leave. He was right.”
Since completing her residency in 2018, Miglani has served in several roles within the ED and is currently its vice chair of operations and medical director.
There have been many highlights. In the early days of COVID, Strong sent Miglani and a small team to New York City to treat patients. “We came back with tools that helped us manage our ED response when COVID hit Rochester hard,” she says.
Miglani has also been involved in community outreach programs, including programs with the Rochester City School District that encourage students to explore careers in medicine. In 2021, Miglani was nominated for a Greater Rochester Chamber of Commerce ATHENA Award, which recognizes women leaders in the community.
The largest capital project in University history
More than 110,000 patients visited the ED in 2021, in a space designed to serve less than half that number. Strong ED’s overcrowded waiting room and treatment areas are just some of the issues that the Strong Expansion Project will address in phases, with scheduled completion in 2027.
The project, the largest capital project in the University of Rochester’s history, will nearly quadruple the ED’s footprint. It will create a designated triage area, separate waiting rooms, and private treatment areas for adult and pediatric patients. It also will house the Comprehensive Psychiatry Emergency Program and the Kessler Trauma Center.
Plans also include a new nine-story inpatient-bed tower, which will add floors for cardiovascular care, short-term patient observation, and future operating rooms and treatment services, along with additional private inpatient rooms.
Until that happens, Miglani and the ED staff will continue to use every space possible to treat patients, from hallways to former staff areas to makeshift patient and family consultation areas.
“It’s challenging, but we do our best,” she says. “This is our community, and we are here to serve it.”
Support the Strong Expansion Project at www.urmc.rochester.edu/ emergency-medicine/ways-to-give.
46 ROCHESTER MEDICINE | 2023 – V1
PHILANTHROPY
Aekta Miglani, MD
Women in Medicine Group Offers Discussion and Solutions





Burnout, gender bias, pay gaps, career advancement, work-life balance—vital issues such as these are at the heart of the Women in Medicine group.
Formed in 2017, the group provides resources to and fosters community among students, residents, fellows, alumnae, clinicians, and faculty members affiliated with the University of Rochester Medical Center.







The group serves to inspire women to thrive and succeed in medicine, providing a platform for the discussion of common challenges and solutions around topics such as mentorship, leadership, and career pathways.
Heidi Schwarz (MD ’83, Res ’89) and Allison Ramsey (MD ’05, Res ’08)—the group’s founding co-chairs—meet quarterly with seven School of Medicine and Dentistry alumnae committee members to plan programming. Before the pandemic, the group offered in-person lectures and networking events several times each year. When COVID hit, the committee kept its momentum through virtual programming.
“During the pandemic, many women, including those of us in medicine, took on an overwhelming amount of responsibility,” says Schwarz, a professor of Clinical Neurology at URMC. “Our careers have always required us to be productive, work long hours, and provide exemplary patient care. With COVID, we found that we had to do all of that while doing more at home and in support of our families, including our aging parents and children.”
Ramsey, an allergy, immunology, and rheumatology clinical assistant professor within URMC’s Department of Medicine, says this has taken a toll on many women—regardless of whether they’re in medical school or work in education, industry, a clinical environment, or at a not-for-profit organization. “COVID has certainly reinforced how important it is to offer programs that focus on supporting women in medicine, expanding and diversifying perspectives, and informing and encouraging all who participate,” she says.
Career and work-wellness issues prompted the group to develop a four-part discussion series for 2022 and 2023 around the theme of self-advocacy. The first two virtual events featured URMC alumnae moderators plus panelists from industry, health care, and education. The third session, scheduled for July, will explore empowerment.
“Although we may come from different places, be in different stages of our careers, and serve in different roles, we are all in medicine,” says Ramsey. “We face a landscape of similar and relatable issues and benefit from drawing on each other’s wisdom and experiences.”
“We encourage all women to join our programs and community,” adds Schwartz. “There is a powerful, shared experience around which our group coalesces, and we know that the work we are doing helps so many women in our field.”
You can learn more and engage with the Women in Medicine group on The Meliora Collective (thecollective.rochester.edu), an online platform that fosters personal and professional exploration among University alumni, parents, faculty, staff, and undergraduate and graduate students.




ALUMNI LEADERS
47 ROCHESTER MEDICINE | 2023 – V1
Heidi Schwarz, MD
Allison Ramsey, MD
Share your news
Your classmates want to hear about you! Did you move to a new city, begin a new project, or make a career shift? Tell us about your recent travels, job developments, family updates, or anything else you want to share by submitting a class note.
Submit notes to your class agent or to uofr.us/smdclassnotes.
Or use this QR code:

MD Alumni
1960s
Carol Nadelson (MD ’61, Res ’62) was honored for her work as Distinguished Chair in Psychiatry at a celebration hosted by Robert S.D. Higgins, MD, MSHA, president of Brigham and Women’s Hospital and vice president at Mass General Brigham.
Gilbert Simon (MD ’62), a primary care physician for more than 50 years, has published Ripped Off! Overtested, Overtreated, and Overcharged, the American Healthcare Mess (published by Value-Based Health Care). Gilbert says, “I wrote my book to help the layperson understand why their health costs are going through the roof and what can be done about it.”
1970s
Note: Alumni are listed by decade, then chronologically by class year under their respective degree categories which include Resident & Fellows and PhD & Graduate Alumni.
Ruby Belton (MD ’72, Res ’74) was honored in May by the Rochester chapter of The Links, Inc., with the White Rose Friendship Award, which recognizes women of African descent or women of color within the greater Rochester community for their service, talent, friendship-oriented spirit, and overall persona.
1980s
Phillip Templeton (MD ’82), chief medical officer and co-founder of DocPanel Technologies, has released Cyberbolt (self-published), which he describes as “the result of years of work coming from a passion to ring loud an alert about medical cybersecurity—as well as to create an exciting thriller novel.”
Victoria Korth (MD ’84, Res ’03) has published her second poetry chapbook, Tacking Stitch (Finishing Line Press). She is a psychiatrist with Rochester Regional Health System and says she writes flash fiction and book reviews in addition to poetry. Korth holds an MFA from the Warren Wilson College Program for Writers and an MA in English and Creative Writing from SUNY Brockport.

Mark Eisenberg (MD ’85) a professor of medicine and director of the MD-PhD program at McGill University in Montreal, Quebec, has been named a James McGill Professor of Medicine. The distinction recognizes outstanding and original researchers who are international leaders in their fields.
Lawrence Marks (MD ’85) will become the assistant dean for Organizational Health and Quality at the University of North Carolina School of Medicine, effective July 1, 2023. Previously, Marks was chair of the UNC School of Medicine Department of Radiation Oncology, a position he held for 15 years.
School of Medicine and Dentistry
classmates Paul Strumph (MD ’86), Jeff Lyness (MD ‘82, Res ‘87), Thomas Perls (MD ’86), and James A. Schuster (MD ’86) have stayed close since graduating. Recently, they took a trip to The Hague in the Netherlands and reminisced on anatomy lessons at the medical school, this time with a Rembrandt twist featuring The Anatomy Lesson of Dr. Nicolaes Tulp, painted in 1632.

48 ROCHESTER MEDICINE | 2023 – V1
CLASS NOTES
2010s
Patrick Milord (MBA ’12, MD ’12) was part of the NYC Health + Hospitals 2022–23 fellowship class. Assigned to the Office of Managed Care and Patient Growth, he conducted his clinical practice at NYC Health + Hospitals/ Queens.

of Pediatrics at the Children’s Hospital of Richmond at VCU Health.
1980s
Jeff Lyness (MD ’82, Res ’87) see MD Alumni.
1990s
Steven D. Hanks (BS ‘84, MD ’89, Res ‘92) began his tenure as the newest president and chief executive officer at St. Peter’s Health Partners (SPHP) in Albany and St. Joseph’s Health in Syracuse on January 1, 2023.

2000s
Chirag P. Shah (BA ’99, MD ’04), an assistant professor at Tufts University School of Medicine, published Financial Freedom Rx, a financial planning guidebook for physicians, with co-author Jay Sridhar, MD. It is a resource that medical students and physicians can reference throughout their careers and various stages of financial growth. “The book educates physicians on the fundamentals of financial literacy, investing, and wealth management,” Shah writes. “It might be the most important (nonmedical!) book physicians will read.” Shah teaches a seminar of the same title at Harvard Medical School during the fall semester, which is broadcast virtually to more than 20 medical schools, including ours.
Sarah Ackroyd (BA ’11, BS ’11, MD ’16) and Miles Nowak (’17 MBA) were married in Chicago last July. They were joined by friends from undergraduate and medical school. From top left are Kayla Florian, Pat Abt (BA ’11), Kevin Rhie (MD ’16), Jason Kopec (MD ’16), Jill Kulla (BA ’12), Jason Birnbaum (BS ’12, MD ’16), Meredith Boyd (BS ’12), Sarah, Miles, Sunisa Mathews (BA ’14), David Oles (BS ’14), Daniel Charen (MD ’16), Kim Bui (MD ’16), Sthuthi David (BS ’12, MD ’17), and Hanna Algattas (MD ’16)
2020s
Colleen Schneider (MA ’18, MD ’22) wrote a poem titled “2020 touch” that was published in the Summer 2022 issue of The Pharos.
Resident & Fellow Alumni
1960s
Carol Nadelson (MD ’61, Res ’62) see MD Alumni.
1970s
Camelia Lawrence (MD ’05), on February 10, 2023, became the first Black woman elected president of the Fairfield County Medical Association’s board of directors. In addition to her work as the director of Breast Surgery with Hartford Healthcare at the Hospital of Central Connecticut and Midstate Medical Center and as an assistant professor of Surgery at UCONN School of Medicine, Lawrence now leads a 231-year-old organization with nearly 1,000 members.
Ruby Belton (MD ’72, Res ’74) see MD Alumni.

Harry L. Gewanter (Res ’79, Flw ’81) of Richmond, Virginia, was inaugurated as the 202nd president of the Medical Society of Virginia at its most recent annual meeting. Gewanter is the medical director of Medical Home Plus, Inc., a nonprofit he helped co-found with Colleen Kraft, MD, FAAP, MBA, and Francine Gallagher, MEd. Gewanter is a clinical associate professor
Steven D. Hanks (BS ‘84, MD ’89, Res ’92) see MD alumni.
Michael Tracy (Res ’99) received the 2022 Laureate Award from the Wyoming Chapter of the American College of Physicians. Tracy has practiced internal medicine and pediatrics in Powell, Wyoming, since 2002. He is a co-founder of 307Health, a multi-physician direct primary care practice in Wyoming.
2000s
Babur Lateef (Res ’00), a board-certified ophthalmologist and prominent physician in northern Virginia, has been appointed by Rector Whitt Clement as chair of the Health System Board of the University of Virginia Board of Visitors.
Victoria Korth (MD ’84, Res ’03) see MD Alumni.
PhD and Graduate Alumni
1990s
Tener G. Veenema (MS ’92, PMC ’93, MPH ’99, PhD ’01) is senior scholar at the Johns Hopkins Center for Health Security and a senior scientist at the Johns Hopkins Bloomberg School of Public Health. Veenema was elected to the National Academy of Medicine, where she is a member of the Forum on Medical and Public Health Preparedness, the Disaster Research Action Collaborative, and chair of the Standing Committee for Preparedness and Response.
2010s
Colleen Schneider (MA ’18, MD ’22) see MD alumni.
49 ROCHESTER MEDICINE | 2023 – V1
In Memoriam
The School of Medicine and Dentistry expresses its sympathy to the loved ones of alumni and friends who have passed. (October 2022 to April 2023)
1956
William A. Kern Jr. passed away on Jan. 20, 2023.
1958
Hereward Seagrieve Cattell passed away on Dec. 29, 2022.
1960
William A. Peck passed away on Feb. 22, 2023, in St. Louis County, Missouri.
1961
William Angell passed away on June 20, 2022, in Tampa, Florida.
1962
William R. Crawford passed away on July 31, 2022, in San Diego, California.
1967
William P. Arnold III passed away on Dec. 30, 2021, in Charlottesville, Virginia.
1968
Dennis O’Leary (Res ’68) passed away on Jan. 29, 2023, in Kansas City, Missouri.
1974
Frederick W. Engstrom passed away on Jan. 17, 2023, in Brattleboro, Vermont.

50 ROCHESTER MEDICINE | 2023 – V1 In Memoriam
Add some meliora spirit to your calendar.
SEPTEMBER 29–OCTOBER 1
Wilmot Warrior Weekend
OCTOBER 5–8
Meliora Weekend
CHECK uofr.us/events FOR DATES + SPEAKERS
Experience Rochester
Our signature online and regional event series exemplifies the University of Rochester’s commitment to lifelong learning and features topics and speakers unique to the University.
REAL Conversations
This virtual lecture series offers authentic discussions featuring brave and candid dialogues around equity, measurable action, and meaningful change.
uofr.us/events
@rochesteralumni
2023 UPCOMING EVENTS
Visit us online to view a complete virtual and in-person event listing— including those that may be happening where you live—or to watch recordings of past
events.
51 ROCHESTER MEDICINE | 2023 – V1
Stay informed.
Want to be sure you’re receiving the latest news and events? Update your information! Your response also helps the School of Medicine & Dentistry learn more about its alumni community so that we can create meaningful programs that best represent all interests.
Scan to update your info or visit rochester.edu/alumni/update

NONPROFIT ORG U.S. POSTAGE PAID UNIVERSITY OF ROCHESTER PERMIT 780
of
University
Rochester School of Medicine and Dentistry 601 Elmwood Avenue, Box 643 Rochester, NY 14642



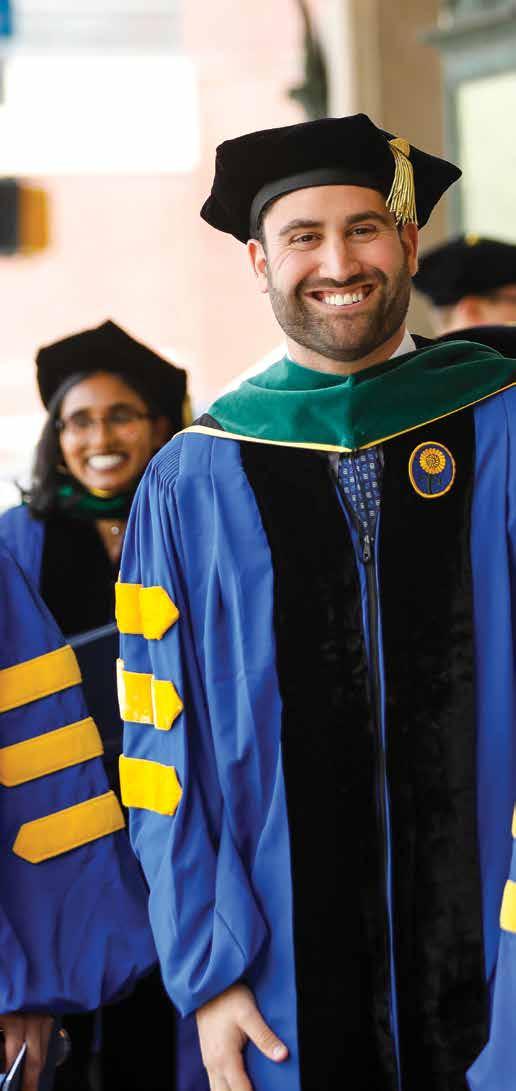

















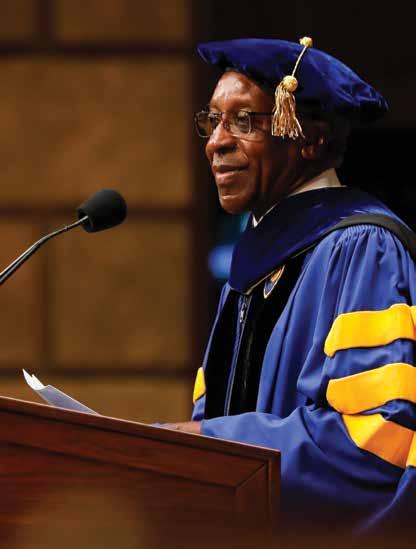







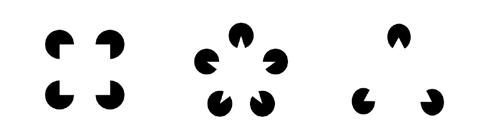

















 Bryan Yates
Bryan Yates



























 By Jim Miller
By Jim Miller