38 minute read
Division Highlights
Cardiovascular Medicine
Cllinical At the onset of the COVID-19 pandemic, our clinical program transitioned to provide Telehealth care and urgent procedures for those in need. This facilitated an expanded program for international consultation, as well. We quickly built protocols for the safe and efficient provision of care for those in need and addressed many of the misconceptions regarding treatments, such as ACE inhibitors for hypertension, with community programs. Our cardiologists participated in setting national standards for these activities, such as the treatment of patients with ST elevation myocardial infarction. The Division assembled a Dream Team that designed and oversaw the MIAMI Protocol for evaluation of student and professional athletes who had had COVID-19 to determine if it was safe to return to practice/competition given the risk of post-COVID myocarditis. The team included sports medicine, sports cardiology, cardiac electrophysiologists, and experts in cardiac imaging and myocarditis. The vast majority of athletes evaluated were able to be cleared and returned to their sport with no adverse consequences. A vascular medicine program has been started via a collaboration between our division and vascular surgery. In collaboration with radiology, our preventive cardiology team identified an important quality improvement initiative – underreporting of coronary calcium on non-coronary chest CT scans. Addressing this will improve treatment for prevention of coronary events.
Advertisement
Research Division faculty has continued to maintain a robust clinical and translational research program. Key UM initiated clinical trials that are in
Cardiology fellows with Cardiology Program Director Carlos Alfonso, M.D.; Interventional Cardiology Program Director Michael Dyal, M.D.; and Division Chief Jeffrey Goldberger, M.D., M.B.A.


process are: 1) the NIH sponsored LEAF trial has been enrolling patients undergoing ablation for atrial fibrillation to assess whether liraglutide pre-treatment can help stabilize the atrial substrate underlying the development of atrial fibrillation; 2) the NIH sponsored ACESO trial testing the effects of stem cells on endothelial function in diabetic patients undergoing percutaneous coronary intervention; and 3) the Department of Defense sponsored stem cell trial in patients with nonischemic cardiomyopathy evaluating the role of underlying genetic causes of cardiomyopathy. In addition, there was a new NIH R01 award evaluating the proteomic, genomic, and metabolomic associations between epicardial adipose tissue and atrial fibrillation. We were key participants in the multicenter randomized controlled REPLACECOVID trial evaluating whether to continue or discontinue reninangiotensin system inhibitors in patients admitted to the hospital with COVID-19, published in the Lancet.
Education A virtual clinical observership was established enabling learners from throughout the world to participate in CCU rounds and conferences. Heart month was highlighted by four state-of-the art lectures for cardiology grand rounds. The annual Miami Valves conference was transitioned to a virtual format with attendees from 45 countries. Scholarly work by our educators includes several publications and a $100,000 grant from the Mitchell Wolfson Sr. Foundation. We have also opened up a new subspecialty fellowship in Sports Cardiology. Our faculty initiated a case-based program for all interventional cardiology programs in Florida to promote interaction and exchange across Florida.
Other Highlights Administration transitioned to provide strong support for all divisional activities including supporting frequent faculty meetings to provide updates on the rapidly evolving events in the medical center and community. This was critical to maintain a sense of connectedness and focus on our tripartite mission. The annual Heart Month campaign was successfully launched with a revamped and updated version of the HeartAware program – expanding from a focus only on coronary artery disease prevention to diabetes, sudden cardiac death, and COVID-19. This required extensive cooperation and collaboration with multiple groups in the health center. A focused effort to streamline clinical operations that are managed/comanaged by multiple departments within the medical center was initiated and has dramatically improved communication and collaboration. Our faculty have been involved in the writing of high-profile documents, including the Cardiac Intensive Care of older adults, the revascularization guidelines, and the Braunwald’s Heart Disease chapter on Sudden Cardiac Death. Innovative efforts include the development of an emergency AV sequential pacing system and ongoing work developing a novel mapping approach for atrial fibrillation. Our CCU faculty were phenomenal in adapting to the expanded role of supervising medical intensive care patients during the periods of overload due to COVID-19 hospitalizations.

Division Highlights
Clinical Pharmacology
Clinical Trials and Research The greatest challenge of 20202021 was restarting our clinical phase I operation following several months of suspended study enrollment due to the COVID-19 pandemic. With the patience, support, and encouragement of Department of Medicine leadership, we renewed our research participant database, retrained staff, obtained necessary approvals, and renewed our relationships with both clients and sponsors. Despite the closure, we have successfully completed enrollment for 12 phase Ib trials and have acquired new contracts/awards worth approximately $3,264,000.
The restart of phase I studies required the division to devise and implement a comprehensive COVID-19 mitigation strategy to protect staff and research participants. Our 18-page plan is considered by several large pharmaceuticals and contract research organizations to set the highest standard for COVID-19 prevention in phase I units.
During this time period, we collected four-year longitudinal data for a cohort investigation of 1,597 patients presenting with hypertensive urgency over a three-year enrollment period. This is the largest and most comprehensive investigation to date in patients with hypertensive urgency. The division has also been awarded the phase Ib trial: A Phase 1, Non-Randomized, OpenLabel, 2-Part Study to Assess the Pharmacokinetics, Safety and Tolerability of Effect XX Boosted with Ritonavir in Adult Participants with Renal Impairment and in Healthy Participants with Normal Renal Function. The research team will test the pharmacokinetics/ safety of a novel inhibitor of the SARS-CoV-2 3CL protease under development as a specific oral treatment for COVID-19. This pivotal investigation will provide crucial data that is required for the design of the upcoming phase III trial.

Left to right: (Top) Miriam Gonzalez Sosa, M.D.; Nadine Francois, M.A. and Rolando Rodco M.D.; (Center) Evelyn V. Caizapanta, M.D.; (Bottom) Eileen Alonso, A.R.N.P. and Richard A Preston, M.D., M.S.P.H., M.B.A.

Digestive Health and Liver Diseases
Clinical During the early months of the pandemic when most clinical activities were shutting down, the Division of Digestive Health and Liver Diseases expanded patient access through several initiatives. Providers and staff began screening patients early for COVID-19, allowing for a safer patient experience. Procedures were expanded to include Saturdays as an appointment option for patients and additional faculty and APRN sessions were made available for telehealth visits, including on evenings and weekends. This allowed the division to rebound rapidly. Telehealth visits were key to our mission to provide high-quality, continuing care to our patients over this past year. Our clinics remained open for essential in-person encounters throughout the pandemic, and telehealth has become a staple for our practice through a hybrid model for some providers and full-time telehealth for others. Pre-procedure COVID testing allowed our endoscopists to stay ahead of the curve and safely provide high volumes of both therapeutic and elective procedures in a safe environment. Our therapeutic endoscopists offer innovative methods, including Per Oral Endoscopic Myotomy (POEM) and endoscopic submucosal dissection (ESD). Expanded industry clinical trials provides the South Florida


Division Highlights
community with increased access to therapies for inflammatory bowel diseases, cancer predisposing syndromes, and liver diseases.
Research Our division kept essential clinical studies open for patients who rely on innovative therapies to manage complex diseases. Early in the
pandemic, research staff worked in staggered shifts to keep patients safe while still providing essential care.
The division remained highly productive this past year with the funding of a U01 and R01 (David Goldberg) and an industry grant (Pfizer, Oriana Damas).
Though not grantfunded, members of our division (Amin, Deshpande) participated in an alliance, comprised of medical centers across North America, identifying the Digestive Manifestations in Patients Hospitalized with Coronavirus Disease 2019.
Division members also published our experience with pre-procedure COVID screening and testing in a high impact journals.
Education The pandemic did not slow our progress in training the future of gastroenterology and hepatology at UHealth. Through online conferences, the Fellowship Program pivoted toward enhanced interdisciplinary collaboration with colleagues from surgery, radiology, and pathology. The division brought together international leaders in the field for an Academic Day of Learning through the American College of Gastroenterology’s Visiting Professor Program. Dr. Mohammad Othman from Baylor College of Medicine, a pioneer in advanced endoscopy techniques, spent a virtual day lecturing, moderating case-based interactive sessions with fellows, and meeting with fellows, faculty, and staff to share his wealth of experience. Dr. Justin Forde, one of two chief administrative fellows, published the UHT Endoscopy Center’s experience in screening patients for COVID ahead of GI procedures in Gastroenterology. Dr. Sunil Amin, Director of Endoscopy at JMH and Lennar, created the division’s first Advanced Endoscopy Fellowship that will begin in July 2022 with our other Chief Administrative Fellow, Dr Jordan Goldstein as the inaugural Advanced Fellow. The training program is now thriving due to our ability to expand educational opportunities during the pandemic.
When learning opportunities were limited for students during the pandemic, UHealth service lines expanded and accommodated learners of all levels. First-year students received their first patient exposures in clinic through SCOPE, the students interest group for GI. Third-year medical students were consistently staffed on the inpatient consult services in both GI and hepatology, as well as in the outpatient setting rotating through varied outpatient clinics at the main hospital and at our satellites for the

Amar Deshpande, M.D. working with a GI fellow using innovative technology he is co-developing to improve patient care.


core internal medicine clerkship. Fourth-year students successfully completed electives throughout the year. Virtual video conference calls allowed more attendees to join our morning educational conferences, with medical students and residents routinely in attendance. Learners (medical students, residents, and fellows) also gained their first exposures to telehealth in the GI and hepatology clinics.
Other Highlights Division faculty, fellows, and APRNs remained connected through bi-weekly and monthly virtual divisional meetings throughout the year. This allowed for participants to communicate critical information and assess the needs for patient care, fellow education, and research projects and successes. These meetings were critical in obtaining feedback from providers on how to best implement telehealth services and to identify areas for improvement. In addition, division members conducted weekly virtual meetings with the clinic and procedure area leadership to respond to the ever-changing needs of our patients. Didactic sessions combining the experience of attending physicians and the educational needs of fellows and residents transitioned to a virtual format. This novel approach allowed us to include clinical staff from UHealth Tower in these learning experiences.
Endocrinology, Diabetes & Metabolism
Clinical Faced with the challenges brought on by the COVID-19 pandemic, clinical faculty of the Division of Endocrinology, Diabetes and Metabolism displayed unwavering commitment in providing uninterrupted patient care. With the implementation of telemedicine, continuity of care was maintained while minimizing virus exposure to faculty, staff, and patients. The pandemic minimally affected the number of outpatient visits with a 5% decrease in outpatient encounters.
Diabetes management in the hospital setting is an important component of the diabetes program. This year, a dedicated inpatient diabetes program at Jackson Memorial Hospital (JMH) and UHealth Tower (UHT) was developed. With an addition of an APRN to the team, the division is able to care for a higher volume of patients, which has been instrumental in helping develop postdischarge care to decrease hospital readmissions. This program also includes educational modules for nursing staff and physicians as well as hospital policies with updated order-sets consistent with latest guidelines. EMR (Electronic Health Record) solutions to alert providers to request diabetes consults when indicated were implemented. These efforts have led to a 22% increase

Division Highlights
of inpatient diabetes consults, improved inpatient glucose control, and decreased length of stay and improved outcomes.
Research Supporting our faculty with their innovative research is essential to our research mission. Dr. Joao Werneck De Castro, Research Assistant Professor, has developed a novel platform to study tumor growth potential, thyroid tumor biology, and test the responses to different chemotherapeutic and immune modulator agents. In addition, he is studying in vivo effects of physical exercise on human islet structure and function. This research will use the human islet transplantation into the mouse eye model to allow studies on human islet transcriptome, structure and function which is impossible in human beings. His studies will serve as the basis of exercise prescription for human subjects aiming to improve pancreatic islet function of diabetic people and to optimize islet transplantation in type 1 diabetes patients. Dr. Werneck’s research is funded by two grants from the NIHNIDDK.
The division also collaborated with the Division of Pulmonary, Critical Care and Sleep Medicine to study the effects of sleep apnea in regulation of glucose homeostasis and diabetes. This effort has recruited a graduate student and will evolve into a translational research program to study the metabolic effects of sleep apnea. Additionally, Dr. Bernal-Mizrachi established a collaboration with Dr. Schally to investigate the effects of GHRH agonists in beta cell function. These studies will serve to develop these agents for the treatment of diabetes.
Notable developments from prior years included a group QI project that resulted in the first formal thyroid ultrasound and FNA simulation-based course conducted at the JHS Center for Patient Safety using a Blue Phantom thyroid ultrasound and FNA training model under the leadership of Dr. Zeina Hannoush. The project continues during weekly FNA clinics at JHS where fellows and attendings collaborate with cytopathology to assess the effects of training on adequacy of FNA specimens. As part of this initiative, cytopathology fellows participate in the FNA clinic and provide reads for adequacy in real time.
Education A significant change in the training program was the expansion inpatient diabetes management training with a more structured program for consultations and the addition of a nurse practitioner to collaborate with fellows on patient care, which has provided a valuable opportunity for training in interdisciplinary teamwork.
Additionally, the Lawrence M. Fishman, M.D. Endocrine Fellow Fund was developed, which will allow the division to undertake a number of activities such as providing key financial support to those in the Endocrine Fellowship Program who wish to travel and present research at meetings as well as provide the necessary seed money to support new research. The fund will also provide the needed infrastructure to allow current and recent endocrine fellows to connect with already established endocrinologists across the country (previous program graduates) for mentorship and networking. Other activities are planned to enrich fellows’ training and community connections while in the program.

Other Highlights Other notable announcements include: Dr. Rene Barro-Soria’s appointment to the Biophysics of Neural Systems Study Section at the Center for Scientific Review, National Institutes of Health; Dr. Caicedo NIH Cell Signaling and Molecular Endocrinology Study Section; Dr. Ernesto Bernal- Mizrachi is a permanent member of the Veterans Administration Study section in Endocrinology (ENDA); Dr. Mark Jara completed an Oncologic Endocrinology Fellowship at the University of Texas MD Anderson Cancer Center.
General Internal Medicine
Clinical Throughout the pandemic, our providers remained focused on providing world-class primary care services to patients. We rapidly transitioned to telehealth and then back to hybrid care models to ensure patients received the necessary preventive, acute, and chronic care services. This included managing a large number of COVID cases in the outpatient setting. We also piloted the UHealth Televigilance Program, allowing providers to remotely monitor and care for COVID-19 patients who might otherwise need to continue care in inpatient settings. US Precision Medicine Project where have enrolled more than 10,000 participants, 75% of which are African American or Hispanic.


Research The Division of General Internal Medicine participated in several large COVID observation and interventional studies, including recruitment of nearly 400 patients for the Johnson & Johnson COVID vaccine trial. We also are leading the NIH-funded Florida Community Engaged Alliance Against COVID Disparities (CEAL). This statewide coalition addresses the unequal burden of COVID disparities among racial and ethnic minorities and the promotion of vaccine update. We also continued our work on other important projects such as the All of Education Our division faculty, which includes institutional educational leaders, led a seamless transition from in-person to virtual learning to ensure our graduate and undergraduate students continued to receive top-notch instruction in the safest (Top) Olveen Carrasquillo, M.D., M.P.H. (left) and Ana Riccio learning environments (right); (Bottom) Elizabeth Greig, M.D. (left) and Sabrina possible. The division Taldone, M.D., M.B.A. (right). also continued to enhance efforts to further diversify and voluntarism by our faculty, our student body and develop was critical to the division’ success curricular innovations as part of during a very dynamic and fluid the NextGen Curriculum, including environment this past year. The training in cultural division also formally took over humility and promotion operations of the UHealth Fischer of health equity. Island practice, providing conciergetype care to all Fischer Island Other Highlights residents and providing acute During these turbulent care for employees. With a gift times, the division from the Ocean Reef Foundation, took a multipronged we also are involved in COVID approach aimed community outreach and vaccine at supporting each education to low-income residents other and sharing and immigrants in the southern tip information (such as of Florida and Upper Keys. Our meetings, frequent work with HIV community outreach communication, and other engagement among low-income opportunities for open dialogue). African Americans in Overtown This, in combination with an and Liberty City also continued unprecedented level of altruism throughout the pandemic.

Division Highlights
Geriatrics and Palliative Medicine
Clinical In response to the COVID pandemic, all outpatient services of the division have been transitioned to the telehealth model. This has allowed the division to further increase the number of patients with access to palliative medicine services. The division continued to cover the critical needs of the residents of the Miami Jewish Home and Hospital, a senior healthcare facility.
Research Dr. Perez-Stable received an R03 award from the National Institute of Health to study strategies for increasing Proteotoxic Cell Death in Hepatocellular Carcinoma. Dr. Dang participated in a study published in the Journal of the American Medical Directors Association looking into the “Factors Associated With Hospitalization by Veterans in HomeBased Primary Care.”
Education The innovative combined Geriatrics and Palliative Medicine Fellowship has graduated its first fellowship class. Meanwhile, our palliative medicine fellowship continues to grow with recent approval for a new position. The Palliative Care Interest Group was established at the UM Miller School of Medicine in 2020, which has allowed for earlier exposure to palliative care and hospice. The group has a liaison to set up early shadowing experiences. The group also works to connect medical students with faculty mentors in the field for education and research. Several division members entered posters and submissions to the American Academy of Hospice and Palliative Medicine (AAHPM)
Other Highlights The End-of-Life Taskforce, led by Dr. Julia Sanchez, continues to work on improving awareness of advance care planning and the roll out of the advance care planning tab on Epic as well as ACP bookends.


(Left to right) Allison Leff, L.C.S.W.; Kirsten Luft, A.P.R.N.; Yvette Gomez, M.B.A.; Jenny Drice, M.D.; Julia Sanchez, M.D.; Marcio Soares, M.D.; Grisel Fed-Vega Martinez, A.P.R.N.; David Barquero, Mariana KhawandAzoulai, M.D.; Maria Rose van Zuilen, Ph.D.
Hematology
Clinical The Division of Hematology has undergone a remarkable period of growth and change this past year. Under the new leadership of Mikkael Sekeres, M.D., M.S., our division was organized into four sections to better reflect the worldclass, sub-specialized hematology faculty now in place. We also have standardized operations and care across the network, in both inpatient and outpatient settings. This includes sections for leukemia, lymphoma, myeloma, and general hematology.
We added 10 new faculty members to our team, with the largest expansion in the myeloma section, under the leadership of Ola Landgren, M.D. We have also expanded geographically. Our latest site in Fort Lauderdale has four staff physicians who are committed to high quality of service and specialization for our patients in Broward County. In total, the division now has 61 faculty, staff physicians, and advanced practice providers.
The pandemic has forced us to adapt how we administer patient care and to implement innovative approaches to treatments so we can continue to provide outstanding care for patients with blood conditions. We were one of the first divisions to switch to telehealth in April 2020 and, as a result, telemedicine accounted for more than half of all patient visits last year. Many of our physicians volunteered at the hospital during COVID staff shortages and our APRNs handled the hotline and provided critical information to the public
Research With the goal of conducting innovative research to improve patients’ lives, faculty and medical students have been actively conducting research and clinical

Hematology-Oncology Program members, 2021-2022



Division Highlights
trials, garnering 14 grants this fiscal year valued at close to $15 million. Even with the challenges of the pandemic, division researchers were able to conduct 268 accruals to intervention clinical trials. Twentyfour of our faculty published in 223 research publications of which 119 had an impact factor greater than 10, further demonstrating the depth and breadth of our research programs.
Teaching As a teaching institution, many of our faculty are course directors in the NextGen curriculum and are heavily involved with the recruitment and education of medical students, residents, and fellows. This year, we’ve had over 500 applicants to our Hematology-Oncology Fellowship Program, resulting in the matching of six fellows. It’s exciting to note that most of the fellows we matched in hematology are females, and the majority of our fellows are racially and culturally diverse, which reflects the department’s emphasis on diversity and inclusion.
Other Highlights Our division conducts weekly hematology-oncology conferences and tumor boards, and despite the pandemic, our faculty has participated in or has led international education meetings attracting thousands of participants. In addition to these educational meetings, the division holds monthly meetings for faculty, APRNs, and staff.




Hematology-Oncology fellows enjoying the Romero Britto Installation at Holtz Childrens Hospital

Hospital Medicine
Clinical Hospitalists function as primary care physicians when a patient is first admitted at UHealth Tower, Sylvester Comprehensive Cancer Center, Bascom Palmer Eye Institute, and Jackson Memorial Hospital. The division continues to expand and finetune its infrastructure with a focus on quality patient care. We modified our Nurse Care Model to improve patient to provider ratio. Most teams are now comprised of a physician along with a collaborating APRN.
During COVID, we restructured our teams in order to keep COVID patients separated from the rest. In theory, we built a hospital within a hospital and by doing so, we significantly helped reduce the spread of COVID. Our faculty have gone above and beyond to fill crucial scheduling gaps in order to care for our most vulnerable patients.
Education In the past year, the Division of Hospital Medicine has expanded to include 64 faculty and staff dedicated to teaching, research activities, and academic missions, all focused on quality inpatient care. Our average hospital census is 250 patients per day. We have two teaching teams composed of senior faculty mentoring internal medicine residents sponsored through our affiliated JMH Health System.
Other Highlights Dr. Maria Delgado recently placed UHealth in the spotlight for being recognized as a designated Comprehensive Hypertension Center by the American Heart Association. Dr. Efren Manjarrez is a respected speaker and on the Board of Editors for the Society of Hospital Medicine (May 2021-2024). Dr. Manjarrez also was awarded the 2020 Society of Hospital Medicine Award of Excellence for Outstanding Service. Other noteworthy faculty with a focus on teaching is Dr. Matthew Imm, who holds a clerkship director role during a time of great change/ adaptation due to COVID. (He currently oversees and mentor’s third- and fourth-year residents). Dr. Armen Henderson’s participation in diversity efforts awarded him a U-link grant earlier last year. Vital to the division’s success was the formal appointment of Medical Directors Dr. Olga Tarasova, Dr. Vijay Mehta, Dr. Pamela Trotter (nocturnist director) and APRN Laura Traini-Mongelli.
Division Highlights
Infectious Diseases
Clinical Although challenging at the beginning, telemedicine was a very useful resource during the peak of the COVID pandemic by enabling us to follow patients closely through a virtual platform. The division has been a nationwide leader regarding the management of the pandemic and testing COVID variants. Jackson Health System, our affiliated system, led South Florida in vaccinations and the dissemination of multilingual, multicultural education to the community.
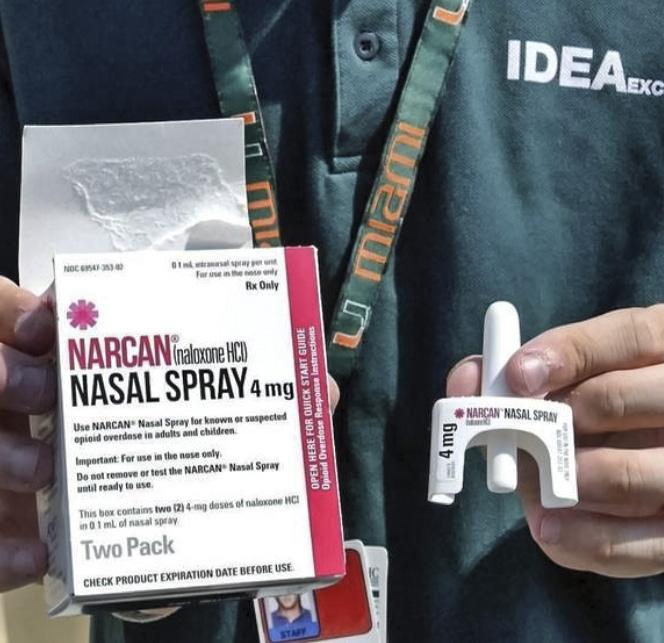
The quality of outpatient care improved during the last fiscal year. The advent of telemedicine has increased access to division services as well as reducing the number of appointment no-shows. Through both medical student efforts and grant funding from the Florida Department of Children and Families, we have drastically increased our capacity to provide addiction treatment services through our division at the IDEA Syringe Services Program. Research The role of division faculty during COVID has been invaluable. Dr. Doblecki-Lewis worked on CoVPN Moderna COVID vaccine and Compass trials, Dr. Jayaweera was involved with the Janssen vaccine trial, Dr. Stevenson secured an AIDS Healthcare Foundation grant to conduct COVID surveillance. Dr. Tookes received the NIH DP2 Director’s New Innovator Award to implement a tele-harm reduction intervention at the IDEA SSP. Additionally, both Dr. Doblecki-

The Rapid Access Wellness team: (Left to right) Marco Torrealba, Stefani Butts, Inza Patton, Liz Rivera, Jakisha Blackmon, Katherine King, Susanne Doblecki-Lewis, M.D., Katie Klose, Blonsky Batalien, Brahian Erazo, Gilianne Narcisse, Cristobal Becerril, Brian Baez, and Junlin Long.

(Left to right) Marilyn Fernandez, Lunnaire Acosta, Adhar Mohamed, Maria Alcaide, M.D., Patricia Raccamarich, Emily Montgomerie, E’lexus Ryan, and Jesus Senabre in front of Converge Miami.
Lewis and Dr. Tookes were awarded funding from the NIH CFAR Ending the HIV Epidemic (EHE) Supplements.
Education Although this was an atypical year, the division continued to make education of our learners a high priority. The constraints placed on in-person teaching made the division more resourceful. Dr. Powell and Dr. Serota both completed one year as longitudinal clinical educators for the NextGenMD curriculum.

Other Highlights Dr. Bhavarth Shukla, Medical Director for Infection Control and Employee Health, played a crucial role during the pandemic. He was involved in numerous aspects of pandemic response including creation of COVID-19 wards, institutional guidelines for care of patients and employees, prediction modeling, a comprehensive testing and tracing program, and most recently vaccination efforts. The division took strategic steps to encourage the development of the division and the best outcomes for its clinical, research, and educational missions. Meetings (COVID update meetings, virtual international conferences, clinical update meetings) were very helpful, not only at the administration level, but to ensure division staff were consistently engaged and focused on the demands of a difficult year.
Division Highlights
Medical Oncology
Clinical The Division of Medical Oncology expanded its sarcoma services to Broward patients during FY20. Dr. Emily Jonczak joined the division in August 2020 and has been providing sarcoma services in our Plantation and Miami satellite oncology clinics.
The division provided telemedicine services, which enabled us to reach patients who live in remote areas and follow up with patients who were unable to or feared coming into the facility due to COVID-19. The division also restarted our Oncology Care Clinic, to serve as a walk-in, urgent care option for patients and physicians. The goal of this service is to decrease the number of ER visits and UHealth Tower admissions over time.
Research Dr. Gilberto Lopes continued to lead the COVID-19 and Cancer Consortium (CCC19), which has led to more than six high-impact journal entries, including publications as senior author in Nature Cancer, Annals of Oncology, The Oncologist, JCO Global Oncology, and coauthored publications in the Lancet and JAMA Oncology. Dr. Erin Kobetz had leadership roles in several COVID-19-related projects, including publications on SARS-Cov2 testing programs published in academic journals such as Academic Pathology, Science of the Total Environment, and the Journal of Occupational and Environmental Medicine.
Dr. Jaime Merchán published his work on the development of several different compounds in cancer with publications in Nature

Gilberto Lopes, M.D., M.B.A., F.A.M.S., with fellows Thomas Platé, M.D., Nina Nguyen, M.D., and Asaad Trabols, M.D., at Jackson Memorial Hospital’s Ambulatory Care Center East Oncology Clinic.





Jonathan Trent, M.D., P.h.D., Stephen Nimer, M.D., Alejandra Perez, M.D., Carmen Calfa, M.D., and Gina D’Amato, M.D. Gina D’Amato, M.D. with nephew Joseph (Joey) D’Amato Kass at the American Society of Clinical Oncology Annual Meeting.

Medicine, The New England Journal of Medicine, and Investigational New Drugs. Dr. Gilberto Lopes published the results of two papers in Lancet Oncology and Lancet Diabetes and Endocrinology on the RET inhibitor pralsetinib, leading to its approval in lung and thyroid cancers that harbor RET gene fusions. Drs. D’Amato and Trent also published several articles in Lancet Oncology, JAMA Oncology, and Annals of Oncology on new drugs for the treatment of various sarcomas. Dr. Carmen Calfa published results of immunotherapy in breast cancer form the TAPUR study in the Journal of Clinical Oncology.
Other awarded grants include: Zinzi Bailey. NIMHD U01 Supplement (PI): The Development of Sexual Orientation and Gender Identity Measures (in a CHW-led multimodality intervention). Drs. Carmen Calfa and Gilberto Lopes as co-PIs 15. NIH UG3/UH3. Avanzando Caminos (Leading Pathways): The Hispanic/Latino Cancer Survivorship Cohort Study. Total grant value: US$ 999,612.
Education All activities transitioned to a virtual format due to the pandemic, including lectures, discussions, tumor boards, and journal clubs, which were recorded so trainees could access the videos at any time. Virtual meetings also provided the opportunity to bring in national and international experts to discuss their specific topics of interest with our fellows. These experts also served as an inspiration for fellows when considering their research careers.
Other Highlights The division continued to coordinate monthly meetings with faculty and staff, weekly grand round teaching conferences, and ad hoc meetings to discuss specific topics. We also reached out to national and international organizations to increase the national recognition of our faculty. Dr. Carmen Calfa was selected as Chair for the ASCO Tapur study steering committee and Dr. Jaime Merchán was invited to lead an educational session at the annual genitourinary (GU) cancers conference by ASCO.



Division Highlights
Katz Family Division of Nephrology and Hypertension
Clinical Telehealth visits were critically important over the last year to provide high-quality and safe continuity of care especially for patients at high risk for severe COVID infection. These virtual visits also helped to increase the division’s outpatient volume by 25%.
Our APRNs added an educational telehealth clinic for those patients starting on dialysis. Additionally, the division developed a Hypertension Nephrology Clinic Cardiovascular Center at UHealth Tower. Dr. Efren Chavez and Dr. Yelena Drexler – both certified hypertensions specialists – joined the UHealth Hypertension Center to lead an expansion of services in collaboration with Hospitalist, Dr. Maria Delgado. The center also earned an AHA Comprehensive Hypertension Center designation by the American Heart Association, one of only 18 centers in the U.S. and the first in Florida.
Despite the challenges wrought by COVID, the division continued to witness clinical growth on both inpatient and outpatient service sides over the past year.
Research The division remained highly productive, receiving funding from several grants. Dr. Alessia Fornoni received an NIH new training grant. The goal of this initiative is to engage first-year medical students across the state in a summer program designed to foster interest in nephrology by exposing students to basic, clinical, and translational science research



opportunities. Dr. Tali Elfassy received an NIN/NIA related supplement to better understand the drivers of incident hypertension disparities among U.S. Hispanics. Dr. Yelena Drexler received the Miami CTSI Mentored Translational Research Scholars Program Award (KL2) for a research study titled Apolipoprotein M and S1P as Novel Biomarkers of Glomerular Lipotoxicity in Nephrotic Syndrome. Dr. Alla Mitrofanova received the Carl W. Gottschalk Research Scholar Grant, a very prestigious ASN grant— the first time a UM faculty member has been awarded such a grant as well as a Chernowitz grant. Jin Ju Kim received an NIH K01 Research Scientist Development Award (pending official NOA).
The division also received a large industry grant from Kyowa Kirin for Mechanistic and PK study of Apolipoprotein M-Fc (APOM-Fc). The PIs are Drs. Fornoni, Merscher, and Al-Ali. An internal grant for High Risk/ High Reward pilot (Hassan Al-Ali) was also received. The division was also involved in 12+ industry or NIHsponsored clinical trials (ContrerasFornoni-Drexler-Munoz Mendoza, Chavez, Mattiazzi, Sosa) and more than 12 COVID -related publications (JAMA, Annals of IM, Critical Care Med, JASN and more). Division faculty published 56 peer-reviewed publications in 2021 and 58 between June and December 2020, 12 of which are COVIDrelated.
Education The fellowship training program continues to attract a highly diverse and competitive group of fellows. In collaboration with the Division of Hospital Medicine and the Gordon Center for Research in Medical Education, the program has strengthened its focus on simulation training to enhance patient safety, starting off the academic year with simulation training for central line placements. Dr. Maria Antonietta Mosetti was instrumental in providing a hands-on renal ultrasound course and supports the kidney biopsy simulation training. Dr. Ross Scalese (Division of General Internal Medicine) has provided unwavering support to ensure the successful annual Objective Structured Clinical Examination (OSCE). The COVID-19 pandemic has resulted in a significantly higher patient load, but thanks to the combined effort of all faculty members who took on additional patients this has not had a negative impact on the training program. Instead, fellows learned how to adapt to changing demands, such as increased dialysis needs and the inability to conduct in-person clinic visits. The expansion of telemedicine has allowed the fellows to become familiar with this modality and learn its advantages and limitations.
Other Highlights Division faculty, fellows, and APRNs, remained connected through monthly virtual division meetings throughout the year. This allowed us to communicate critical information and assess our needs for patient care, fellow education, and communicate on research projects and successes.
Alessia Fornoni, M.D., P.h.D., Gabriel Contreras, M.D., M.P.H. and the Katz lab members with retired Miami Heat basketball player Alonzo Mourning.


Division Highlights
Pulmonary, Critical Care, and Sleep Medicine


Clinical Several services were launched and/ or expanded this year to better serve our patients. The Pulmonary Clinic opened at UMH West to promote improved provider collaboration and access for patients. The JMH Progressive Care Unit (PCU) and vent (ventilator) management was expanded. Intuitive Ion Robotic Bronchoscopy technology was implemented at UHT. Future phase 2 expansion of the UHT CCU was approved but CCU has not opened due to the surge in COVID-19. Future expansion of the interventional pulmonology procedure service line has been approved and will facilitate the expansion of our procedure team by adding more support staff to better meet the needs of our growing patient population. Plans are also underway to expand the PFT/Bronchoscopy service.
Telemedicine has had a positive impact on clinical operations and patient care, especially for immunocompromised patients and those who live far from the medical campus. Telemedicine visits have become a safe, viable option for care. Telemedicine also allowed providers the flexibility to swap clinic days with minimal notice or prior clinical manager approvals.
Research The Division is in collaboration with other divisions (Endocrinology, Diabetes & Metabolism) as well as other departments (Public Health) to conduct research and is also focusing on some PI initiated studies. Our faculty were highly productive this past year and this is evidenced by the multiple R01s (Wanner, Gershengorn) received as well as a grant from the CDC (Mallow) and an I-SPY grant (Kett). We currently have 9 COVIDrelated active trials and we completed 7.
Education To ensure the best learning environment for medical students, residents, fellows, and other learners, the Division implemented changes in its academic interactions with fellows. The Division has streamlined all academic activities and standardized the time, place, and purpose of many educational series. The Fellows Bootcamp was modified by incorporating input from division faculty and fellows, which has allowed for additional guided training and resources for fellows. A quarterly discussion with the chief and fellows was also launched with the goal of listening to fellows’ input and comments to help guide future academic medicine efforts.
Our new structured academic/ scholarly activities have sparked renewed interest in research. We now have more engaged junior faculty with interest in academics/ scholarly events. This effort has also reinvigorated interest from some fellows who are requesting more involvement in research focused training. We hope this will lead to more academic/scholarly active physicians in the future.
Other Highlights Many strategic steps were implemented this year to encourage the development of the division and the best outcomes for our clinical, research and educational missions. The division has focused on additional cross training on


Division of Pulmonary, Critical Care and Sleep Medicine faculty.
the clinical and research support side, which has proven helpful with flexibility and cross coverage capabilities.
Weekly PCCSM leadership meetings to plan and coordinate weekly events and strategize/ operationalize tasks have been organized, including bi-weekly team huddles to discuss relevant topics for clinical and research support groups and monthly faculty divisional meetings to provide up-to-date information on current developments and updates that impact operations.
Teamwork has been essential in our day-to-day operations. Faculty, APPs, Clinical and Research Staff provided substantial support to the COVID mission. Faculty/APPs came together to support one another, provide support with coverage, communicate challenges and needs.
PCCSM Leadership came together to listen to faculty and staff to better gauge the needs of the division and modify as needed. During these challenging times, the division has focused on finding solutions to problems to make it through the last few difficult months. This has led to creative coverage models and matrices to use available resources and to provide quality cardiovascular care.



Division Highlights
Rheumatology and Immunology
Clinical The Division of Rheumatology quickly adapted to the challenges of the pandemic. A strong telemedicine component was developed, which complemented our in-person clinical services, and served as a vehicle for providing care not only to those concerned about in-person visits but also to expand the reach of the division’s consultative services throughout Florida, particularly Central Florida and the Keys.
Research Dr. Eric Greidinger obtained a new research grant from Eli Lilly and Company. This one-year grant will study the efficacy of Baricitinib in animal models to treat mixed connective tissue disease ($87,190 direct costs per year). Dr. Ozlem Pala continues active participation in the national CORRONA registry of inflammatory arthritis, recently renamed CorEvitas. Dr. Maria Carpintero and Dr. Greidinger are actively participating in over 13 clinical trials in the management of systemic lupus erythematosus and other autoimmune diseases. Division Chief Dr. Carlos Lozada is part of a leadership group developing the new Panamerican guidelines for the management of spondyloarthropathies.
Education Numbers of applicants to our renowned Rheumatology Fellowship Program continued to increase on a yearly basis, surpassing 200 this year. Dr. Lozada, Division Chief and Program Director, was honored with the 2020 Distinguished Program Director Award from the American College of Rheumatology. His career trajectory as program director was recognized as was his leadership role in originating the use of the ERAS system and the medical subspecialties match in rheumatology. Dr. Lozada is currently developing a program within the Panamerican League of Associations for Rheumatology (PANLAR) that will lead to an increased number of training positions in rheumatology throughout the Americas.
Other Highlights Dr. Carlos Lozada, Division Chief, is serving as President of the PanAmerican League of Associations for Rheumatology (PANLAR) 20202022 and served as Chair of the Executive Committee of the International League of Associations for Rheumatology (ILAR) in 2020. Senior Rheumatology fellow Dr. Amanda Worme was honored with an invitation to present her research at the American College of Rheumatology’s Rheumatology Research Workshop in May. Her presentation was entitled “Adherence to Bone Health Guidelines in Patients on Long Term Steroids for Rheumatic Disorders at the Miami Veterans Affairs Medical Center.” Nurse Navigator Denise Perez joined the Division of Rheumatology. She will play a critical role in facilitating care in chronically acute patients.

Maria Carpintero, M.D. and fellows in clinic.

Transplantation and Cellular Therapy
Clinical The Division of Transplantation and Cellular Therapy continued to expand its national footprint as a leader in clinical care in hematopoietic stem cell transplantation (both autologous and allogeneic) and at the cutting edge of T cell immunotherapies. Division faculty adapted to the COVID19 pandemic by creating a hybrid system to evaluate new patient consultations and follow-up visits by using telemedicine whenever possible, while continuing the intensive inpatient care required in cellular therapy.
Research Researchers within the division are conducting research across multiple areas, spanning the spectrum from basic to translational research and novel investigator-initiated and multicenter trials, including those funded by the NIH sponsored BMT Clinical Trials Network. Some particularly exciting areas include: the expansion of the use of mismatched unrelated donor transplantation, a key option for the diverse population we serve in South Florida, who often lack matched registry donors; expansion of an already strong program in adoptive cellular immunotherapy, including “off the shelf” CAR-T therapies derived from donors and CAR-T therapies targeting multiple antigens to reduce relapse; a continued expansion in translational research to improve complications of donor stem cell transplantation, including graft-versus-host disease and viral infections; leadership in clinical research in infectious complications of transplantation and cellular therapy, including studies of COVID-19 infection in our patients. Multiple grants were received this past year, including one from the Applebaum Foundation as well as collaborative grants from the NIH to the Komanduri laboratory and multiple investigator-initiated clinical trial awards from industry partners to division faculty.
Education Faculty members were actively involved in medical school and postgraduate medical education, both in the classroom and clinical settings. In addition, faculty and staff hosted a major national educational conference targeted at advanced practice professionals and hematology/oncology and cellular therapy fellows.
Other Highlights Faculty meetings were held on a weekly basis to discuss clinical and research issues and then monthly to focus on special concerns. Dr. Denise Pereira continued in her role as President of the Medical Staff. The division adapted quickly to the challenges posed by the COVID-19 pandemic, which were magnified for our highly immunocompromised patient population. This was done by adapting all clinical care approaches to deal with the high susceptibility of our patient population and publishing multiple papers related to COVID-19 incidence, diagnosis, and outcomes in cellular therapy recipients. Despite the challenges of the past year, we have an extraordinary and cohesive group of physicians, staff, and administrators who continue to support the broad range of clinical and emotional needs of our unique and deserving patient population.

(Top) Michelle Emokpae, A.P.R.N.; Juan Ramirez, A.P.R.N.; Lazaro Lekakis, M.D. and Laura Baquero, A.P.R.N. (Bottom) Yvette Morlote, A.P.R.N.; Sila Shalhoub, Pharm.D.; Selgrys Cisneros, A.P.R.N. and Katrina Piedra, Pharm.D. at the Dolphins Cancer Challenge.