TINNITUSTODAY
To Promote Relief, Help Prevent, and Find Cures for Tinnitus

To Promote Relief, Help Prevent, and Find Cures for Tinnitus
Nurturing Healthy Digital Habits Among Today’s Youth Understanding Pediatric Sound Sensitivities
Are Migraines Linked to Sound Disorders?
AirPods Pro 2 Authorized as OTC Hearing Aid Device





SPECIAL FEATURES 8| The Stars in My Eyes: A Perspective on Pediatric Tinnitus
22| Tiny Ears, Big Sounds: Understanding Sound Tolerance Issues in Children
24| Beyond the Noise: How a Teen Overcame Misophonia 34| Sounding the Alarm: Protecting Young People From Noise-Induced Hearing Loss 48| Mild to Moderate Hearing Loss? Amplify Your Hearing World With Apple’s Latest Innovation

TINNITUS TOOLS & RESOURCES
12| A New Tool for Young Ears: The Children’s Tinnitus Questionnaire

18| How 504 Plans Support Individuals at Every Age

51| Navigating the Complexities of Migraine, Ménière’s Disease, Tinnitus, and Hyperacusis PERSONAL STORIES
19| Steps to Take When Tinnitus Turns Work and Concentration Into a Mental Maze 30| Building Balanced Screen Time for Today’s Tech-Savvy Youth 45| Progressive Tinnitus Management: Take It One Step at a Time! 56| Tinnitus Support Groups 58| Spotlight on Patient Providers


4| Finding Purpose in the Pursuit of Silence: A Journey to Lead ATA

16| Hearing the Unheard: Why Children With Tinnitus Need Recognition
38| Turning Away From the Brink: Embracing a Life Transformed

40| Hitting the Right Note at the Kentucky State Fair
43| The Transformative Power of Community, Music, and Fishing



Chair, Board of Directors
One group that hasn’t received much attention from researchers is children, which is why I’m pleased that this issue of Tinnitus Today considers the needs of children and teens living with tinnitus and other auditory disorders. But it’s also important to understand why researchers tend to shy away from investigations with minors, despite knowing that tinnitus occurs in this age group.
First and foremost, conducting studies with minors requires extra protections to ensure their well-being. Parental consent and, often, child assent are necessary, making recruitment more complex and limiting the types of investigations that can be conducted. Additionally, children’s cognitive and emotional development varies widely with age, which can impact their ability to understand procedures, accurately report symptoms like tinnitus, and engage in certain testing protocols, particularly those that require sustained focus or detailed feedback. Nonetheless, we need to understand and hear their voices and experiences.
In fields like auditory health, where age and development can play a major role in how a condition manifests and progresses, omitting the pediatric population leaves gaps in our knowledge. For instance, understanding how tinnitus affects children could provide insights into developmental differences in auditory processing, brain plasticity, and how the condition impacts learning and social interactions. There may also be unknown factors, biological processes, or genetic markers in children that influence the development and progression of tinnitus. By investigating these aspects, researchers could uncover new pathways to treatment and prevention.
Research that includes children with tinnitus can also foster a better understanding of how tinnitus affects quality of life at different ages. As you’ll note in this issue, for children, tinnitus can impact concentration, sleep, and social interactions, which are often misinterpreted as behavioral or learning issues. Addressing these challenges can improve children’s mental and emotional well-being, supporting their academic and social development.
In the years ahead, I hope to see a comprehensive approach to tinnitus research, encompassing all ages, which could transform our understanding of this condition. Such research not only holds promise for those currently affected by tinnitus but also for future generations
MANAGING EDITOR AND PUBLISHER
Joy Onozuka, MA
American Tinnitus Association
COPY EDITOR
Christina Palaia
Emerald Editorial Services
EDITOR-AT-LARGE
James A. Henry, PhD
Ears Gone Wrong®, LLC
Portland, OR
EDITORIAL ADVISORY PANEL
Marc Fagelson, PhD
East Tennessee State University
Johnson City, TN USA
Gail M. Whitelaw, PhD
Department of Speech and Hearing Science
The Ohio State University
DIGITAL DESIGN & PRODUCTION TEAM
JML Design, LLC
ATA BOARD OF DIRECTORS
Jinsheng Zhang, PhD, Detroit, MI—Chair
Stelios Dokianakis, AuD, CH−TM, Holland, MI—Vice Chair
Gordon Mountford, South Pasadena, CA—Treasurer
John Minnebo, MBA, Philadelphia, PA—Assistant Treasurer
Sara Downs, AuD, Duluth, MN—Secretary
Jeff Bingham, San Diego, CA
Shahrzad Cohen, AuD, CH−TM, Oaks, CA
Marc Fagelson, PhD, Johnson City, TN
Jennifer Gans, PsyD, San Francisco, CA
David Hadley, MBA, San Francisco, CA
Emily McMahan, AuD, CH−TM, Anchorage, AK
Samantha Morehouse, AuD, CH−TM, Cincinnati, OH
Julie Prutsman, AuD, Highlands Ranch, CO
Robert Travis Scott, Abingdon, VA
Joseph Trevisani, New York, NY
Dan Torpey, CPA, Irving, TX
Erin Walborn-Sterantino, AuD, Rensselaer, NY
HONORARY DIRECTOR
William Shatner, Los Angeles, CA
ATA HEADQUARTERS
American Tinnitus Association
8300 Boone Blvd., Suite 500
Vienna, VA 22182 USA
T: 800.634.8978 (Toll Free) www.ata.org
The American Tinnitus Association is a non-profit corporation, tax exempt under 501(c)(3) of the Internal Revenue Code, engaged in educational, charitable, and scientific activities.
Tinnitus Today magazine is © copyrighted by the American Tinnitus Association.
ATA™ is a registered trademark of the American Tinnitus Association.
Marc Fagelson, PhD—Chair
East Tennessee State University, Johnson City, TN
Carey D. Balaban, PhD University of Pittsburgh, PA
Jianxin Bao, PhD
Duke University, Durham, NC
Shaowen Bao, PhD
University of Arizona Tucson, AZ
Julia Campbell, AuD, PhD University of Texas at Austin, TX
Donald Caspary, PhD
Southern Illinois University School of Medicine, Springfield, IL
Christopher R. Cederroth, PhD University of Tübingen, Tübingen, Germany
Richard Gault, PhD
Queen’s University Belfast, Northern Ireland
Karah Gottschalk, AuD, PhD
Mountain Home VA, Johnson City, TN
Sylvie Hébert, PhD
Université de Montréal, Canada
James Henry, PhD
Ears Gone Wrong®, LLC Portland, OR
Bruce Hubbard, PhD
CBT for Tinnitus, Morristown, NJ
Maria Kleinstaeuber, PhD
Utah State University, Logan, UT
Jose Antonio Lopez Escamez, MD, PhD University of Sydney, Australia
Don McFerran, MD, MA FRCS (Retired) Colchester Hospital, UK
Kenneth Morse, AuD, PhD
West Virginia University, Morgantown, WV
Arnaud Norena, AuD, PhD
National Center for Scientific Research (CNRS)
Aix-Marseille University, France
Jay Picciillo, MD
Washington University School of Medicine, Saint Louis, MO
Daniel Polley, PhD
Massachusetts Eye and Ear, Boston, MA
Josef Rauschecker, PhD
Georgetown University, Washington, DC
Tricia Scaglione, AuD
Holistic Hearing & Wellness, LLC, Fort Lauderdale, FL
William Sedley, PhD
Newcastle University Billingham, UK
LaGuinn Sherlock, AuD, CH–TM
Walter Reed National Military Medical Center Bethesda, MD
Paul Smith, PhD, DSc
University of Otago School of Biomedical Sciences University of Otago, Dunedin, New Zealand
Sarah Theodoroff, PhD
VA Portland Health Care System, Portland, OR
Pim van Dijk, PhD
University Medical Center Groningen, Netherlands
Sven Vanneste, PhD
Trinity College Dublin, Ireland
Florian Vogt, PhD, PsyD
University College London, UK
Nathan Weisz, PhD
University of Salzburg, Austria

As we approach the end of the year, I want to take a moment to reflect on the difference you’ve made and the impact you can continue to have on the lives of those affected by tinnitus. Your support as a donor and friend of the American Tinnitus Association has been transformative, allowing us in 2024 to fund over $400,000 in research; to enhance awareness of tinnitus, patient care, and ATA support at more than a dozen venues; and to provide critical resources through our helpline to more than 2,000 individuals living with tinnitus.
Tinnitus can be an invisible yet overwhelming condition, touching millions worldwide. At ATA, we’re committed to improving the lives of people with tinnitus through education, advocacy, and research. However, the reality is that none of this can happen without the support of generous individuals who believe in our mission. With no consistent public funding dedicated exclusively to tinnitus research, ATA relies on the backing of our community to drive meaningful change. This is why your end-of-year contribution matters so profoundly. You are a part of the mission.
When you give to ATA, you’re doing more than donating. You’re actively investing in hope, in scientific advancements, and in the well-being of individuals who struggle daily with tinnitus. This support enables us to fund groundbreaking research and expand our educational initiatives, bringing us closer to finding effective treatments—and someday, a cure.
End-of-year giving holds special significance. For many, it is a time to reflect on the past year and make purposeful decisions about supporting causes they deeply care about. Contributions made now can have a double impact, helping ATA plan our initiatives for the year ahead while potentially providing you with tax benefits for the current year.
This holiday season, I invite you to partner with us in our mission. Together, we can bring the tinnitus community hope and relief. With your help, we’re paving the way for a future where no one has to live with tinnitus. Thank you for standing with us.

Patrick A. Lynch, Esq., MBA Chief Executive Officer
The opinions expressed by contributors to Tinnitus Today are not necessarily those of the publisher or the American Tinnitus Association. This publication provides a variety of topics related to tinnitus for informational purposes only.
ATA’s publication of any advertisement in any kind of media does not, in any way or manner, constitute or imply ATA’s approval or endorsement of any advertised product or service. ATA does not favor or endorse any commercial product or service.

By Patrick A. Lynch, Esq., MBA
To truly understand a journey, the traveler oftentimes cannot make sense of its purpose or direction until well after it has begun. This certainly has held true in both my personal and professional lives. Today, I serve as the newest CEO of the American Tinnitus Association, yet this role is not something I could have ever anticipated or planned for earlier in my life.
It is an incredible honor to lead ATA in its mission to help others seek relief from the relentless, invisible hum of tinnitus. My path to this role was anything but straightforward; however, with the benefit of hindsight, I now recognize the pattern: a journey where struggle met purpose, and purpose met passion. The irony is that my work today stems from a seemingly unrelated battle with adolescent
cancer that left me with tinnitus, with the practice of law and politics sprinkled in along the way.
At 15 years old and during my sophomore year of high school, my entire way of life was upended when I was diagnosed with a blood cancer known as acute lymphocytic leukemia. Suddenly, my world was dominated by chemotherapy treatments, spinal taps, blood work, and hospital visits that became the background rhythm of my young life. After a three-yearlong protocol concluded, the cancer relapsed, and I discovered that I needed a bone marrow transplant, including total body irradiation, to have a 50 percent chance at survival.
The story ends well: I am still here to share it and have gained invaluable life lessons as a result. I had to learn

how to dig deep, find strength, and hold on to hope. It was a trial by fire in the truest sense, one that would eventually show me how fleeting life and health can be, and how to prioritize the things that matter most in one’s life.
The irony wasn’t lost during my treatments when I started to hear a subtle, persistent ringing in my
“Today, I serve ATA with a profound sense of gratitude and purpose, finding that all the twists and turns of my life, including the struggles with cancer and tinnitus, ultimately shaped my journey here.”
ears—a constant companion that emerged from the very treatments that saved my life. Initially, I shrugged it off as a minor inconvenience, something that would disappear on its own. But over time, it became clear that this sound wasn’t going anywhere. I had developed tinnitus, potentially a side effect of the aggressive cancer treatments I endured. At the time, over 25 years ago, I was told by an audiologist there was “nothing that can be done” and to “learn to live with it.” And so, I did.
Once my battle with adolescent cancer concluded, I attended college, then business and law school, eager to make my mark on the world. I dove headfirst into corporate law, driven to succeed and to prove that nothing— not even cancer—could hold me back. My colleagues and mentors were talented, my work was challenging, and I was making strides in my career. But there was an undeniable void, a lingering question of purpose.
As I navigated corporate law’s demanding world, there was a persistent feeling deep in my gut that I had survived cancer to eventually make a dent in the universe—a subtle but unrelenting nudge reminding me
of a time when life was less about prestige and more about the fragility of health and the value of time. The longer I spent in law, the louder that call became.
Eventually, it was time to make a professional change and to dedicate myself to work that could make a difference. It was that pull toward purpose that led me to the public charity sector, where I could use my background in advocacy and fundraising to help others.
My transition from corporate law to charity work was like stepping into a world I’d long been destined to join. The most rewarding part was connecting with people, hearing their stories, and being able to make a tangible difference in their lives through the mission of the organizations I was part of. This shift also allowed me to use my experience and perspective in ways that felt authentically “me.”
As I delved deeper into public service, I discovered charities’ ability to impact issues that often go unrecognized in the broader public discourse. The most important way to make the most effective impact, it was clear, was via fundraising and fund
development. Funding was the number one factor that determined whether an organization had the resources it needed to pursue its mission. Little did I know, my initial journey into this world would soon bring me face-toface with an organization whose cause hit very close to home: the American Tinnitus Association.
My career in public service brought me to cancer organizations, healthcare systems, and social service programs; I had never expected to find an opportunity at an organization with a mission like that of ATA. Tinnitus had been my silent partner since my teenage years, a constant reminder of what I’d been through and what I’d overcome. Yet, I never considered that my personal history with cancer and the subsequent tinnitus could ever serve as a part of my professional life as well. The opportunity to serve as a new leader for ATA presented a chance to do for others what I’d longed for back when my tinnitus first began: to provide answers, hope, and support. I have been shocked to learn that today, tinnitus patients are still being told the same thing I was told over 25 years ago: “Learn to live with it.” We can change this.
Today, I serve ATA with a profound sense of gratitude and purpose, finding that all the twists and turns of my life, including the struggles with cancer and tinnitus, ultimately shaped my journey here. Since joining ATA, I’ve met countless people whose lives are disrupted by tinnitus, who often feel as though they’ve lost a piece of themselves to this invisible affliction.
And every day, I’m inspired by the work we do to alleviate this burden.
The role and purpose of ATA are clear: to pursue easing the burden of living with tinnitus through providing reliable information, patient and provider education, and the funding of research to silence this unwanted sound. Each pillar of this mission resonates with my own journey with tinnitus and healthcare, especially as I recall my own early days of confusion, frustration, and the need for reliable answers.
ATA offers resources that I wish had been available to me—information that is both clear and trustworthy— acting as a beacon of hope in the often-overwhelming world of tinnitus. The education of providers is also of paramount importance, ensuring that every community has a professional who can help navigate the myriad various strategies, interventions, and treatments available for a tinnitus patient. Finally, the funding of groundbreaking research is also helping us to better understand and, ultimately, find treatments for tinnitus. The research we support is bringing us closer to new therapies and hopefully a cure.
I’m continually inspired by the scientists and researchers who dedicate themselves to unraveling the mysteries of tinnitus. They are driven by the same resolve and hope that carried me through my own journey. Supporting their work, advocating for more funding, and bringing awareness to the public are just some of the ways ATA makes a difference every day.
A major focus for us at ATA is building a supportive, informed tinnitus community. Tinnitus, an invisible struggle that others can’t see or hear, can be isolating. Through ATA’s outreach, we are bridging that gap by connecting individuals with one another and with experts in the field.
As someone who knows firsthand the toll that tinnitus can take, I want to ensure that everyone who reaches out to us feels heard, validated, and supported. Whether they are newly diagnosed or have been living with tinnitus for years, we strive to make ATA a place where they can find resources, relief, and perhaps most importantly, community.
ATA has done a great deal in its more than 53-year history. We can— and will—do more. But we cannot give what we do not have, and it is part of my leadership role to ensure that we have plenty. A rising tide lifts all boats, and funding and revenue will directly address many of our existing and future needs and goals.
Reflecting on my path to ATA, I can’t help but marvel at the providential way life has woven my experiences into a cohesive journey. From cancer to corporate law and now to public service, every chapter has added depth and meaning to my story. Now, I have the unique privilege of using my experiences to guide an organization dedicated to helping others find relief from the very condition that became a part of my daily life in my teenage years.
The hum of tinnitus, once a symbol of hardship, has transformed into a call to action—an opportunity to drive change and offer hope. By facilitating ATA’s work, I am honored to lead an organization that not only helps others pursue silence but also reminds us all of the strength that can emerge from adversity. Together, through research, support, and education, we are making strides toward a future where tinnitus no longer holds power over our lives.
For me, leading the American Tinnitus Association isn’t just a job; it’s a profound confluence of events that turned struggle into purpose. In the silence we pursue, we find meaning, connection, and hope. Just wait till you see where the journey takes us next.

“As someone who knows firsthand the toll that tinnitus can take, I want to ensure that everyone who reaches out to us feels heard, validated, and supported.”


By Gail M. Whitelaw, PhD
A group with tinnitus that is often overlooked are children and adolescents, even though it is estimated that as many children as adults experience tinnitus and that, just as in the adult population, the tinnitus can be disturbing. Although most children and adolescents do not spontaneously report tinnitus, it is not an uncommon issue in the pediatric population. This article is designed to introduce the topic of tinnitus in children and to address its significance to children and their families.
It is assumed that children are generally unaware of their tinnitus or that they cannot describe it. The truth is that children are typically not asked about tinnitus; therefore, little is known about their experiences or what they
know about their tinnitus.
Many parents and professionals assume that children cannot describe or discuss it, but my experience with this population suggests that children have insight into their tinnitus. Children seen in our clinic often provide a positive response to the question “Do you have sounds in your ears?” but add that they did not know that “it” had a name or that other people also had this.
The title of this article refers to the response from a 4-year-old child we saw for a tinnitus consultation at our clinic. His parents noted that at age 2, he started to say that he had “stars” in his ears when he lay down to sleep at night. His reporting escalated as he got older, and his “stars” seemed more disturbing to him. His astute parents mentioned it to their pediatrician, who referred for an audiologic evaluation, which resulted in a referral to our clinic for a
tinnitus assessment. A combination of education, counseling, and sound therapy significantly reduced this boy’s tinnitus perception, and he indicated he was no longer bothered by his tinnitus.
Research and clinical protocols for addressing tinnitus in children are sparse; however, clinical interest and research have been growing in the past decade. One of the reasons that information is lacking is that children are not asked about their tinnitus in the clinical setting or when they participate in research projects that address hearing or listening. The belief that tinnitus impacts older adults with hearing loss and/or noise exposure has dominated both epidemiology and clinical perspectives in tinnitus. Recent interest in pediatric tinnitus challenges this stereotype and expands our information about this population. Estimates of tinnitus in children vary widely, partially because of
differences in terminology used and partially because children are generally not asked for their input regarding tinnitus.1,2 It is estimated that between 10 percent and 15 percent of children experience chronic tinnitus.3,4 Bothersome tinnitus has been reported in children as young as 3 years.1
Evidence of comorbidity with hearing loss is variable and inconclusive. A strong association between tinnitus and hearing loss in children is noted, with the hearing loss thought to be the cause of the tinnitus.5,6 Some research indicates that tinnitus is more often reported in children with mild to moderate hearing loss than in children with more severe to profound degrees of hearing loss. Savastano and her colleagues found that 25 percent of children with hearing loss reported bothersome tinnitus.7
Children often report tinnitus when they have a conductive hearing loss, such as during a period of prolonged middle ear infections. Also, children with normal peripheral hearing and tinnitus report the tinnitus to be more disturbing than do children with hearing loss and tinnitus.8 An interesting aspect of pediatric tinnitus is that sound tolerance disorders, which may also be referred to as hyperacusis, are five times more prevalent in children who demonstrate spontaneous tinnitus.9
Additional research is needed to understand the relationships between hearing and tinnitus in children. To clarify this, it is important that children and adolescents are asked about tinnitus as part of the case history during their hearing evaluation. Since most public-school children and adolescents have school-based hearing screenings over their years in school, this is an ideal time to obtain information on children’s experience with tinnitus.10
As noted previously, children generally do not spontaneously report tinnitus unless it’s a new experience for them. For many children, the tinnitus has been present for their entire life and they do not identify it as unusual or unique. When questioned, they often think their ear noise is “normal” because they don’t know “quiet.” Additionally, children with tinnitus may not correlate their sound to a “medical issue” and thus don’t see it as problematic. Children may have difficulty identifying tinnitus and generally do not report it to parents.11
The mechanisms of tinnitus in children are poorly understood. Tinnitus in children is more common in girls than in boys.9,10 A genetic component for tinnitus has been suspected based on years of anecdotal reports, and evidence to support this claim is beginning to emerge.12 As noted previously, hearing loss is thought to be a risk
“The truth is that children are generally not asked about tinnitus; therefore, little is known about their experiences or what they know about their tinnitus.”
factor for tinnitus. Recreational noise exposure, history of ear infections, gaming, alcohol use, and cigarette smoking have all been identified as risk factors for tinnitus in children and teens.10 Tinnitus is often reported after concussion or traumatic brain injury. Children who have been given treatment with ototoxic medications, such as some cancer medications, often have tinnitus.
As with adults, the current focus of tinnitus assessment and management in children with chronic tinnitus is on those who experience bothersome tinnitus. Tinnitus in children has been noted to impact their quality of life and emotional well-being. Although this applies to children of all ages, the impact of bothersome tinnitus on school-aged children can be significant in the learning environment. As is the case with adults, children who experience hearing loss—even subclinical changes in sensitivity or auditory processing disorder— may attribute classroom listening difficulties to tinnitus. As a result, the child’s negative evaluation of tinnitus’s importance may be amplified, thereby exacerbating difficulties the child experiences when focusing on teachers or other students.
Children with tinnitus may be misidentified as having attention deficit disorder; however, the underlying attention issues are related to ability to hear auditory information over the tinnitus. Children with reactive tinnitus, which is triggered by sound or noise in the classroom, have described fight-orflight responses.
Tinnitus has been demonstrated to interfere with cognitive processing and executive functioning, which impact attention and speech comprehension in the classroom.13–15 Many children describe anxiety and depression in
response to their tinnitus. Tinnitus is the source of distress, anxiety, and worry for some children and their families and may include sleep disturbances and difficulties with attention and concentration.8 It is clear that if children raise tinnitus as a concern, often after being asked about it, it should be acknowledged and an opportunity for further discussion should be created.
Smith and colleagues suggest that even though significant evidence of children experiencing troublesome tinnitus exists, services for children are far less established than those for adults.16 A way to start remedying this discrepancy is by creating a child-friendly environment where audiologists can listen to the child and their family. Children can often describe their tinnitus by imitating the sound in their ears or drawing a picture that represents their tinnitus.
A child in our clinic brought me a picture he had drawn after our first appointment: cicadas, which was his “ear sound.” He also drew a picture of himself feeling sad, which described how his “ear sound” affected him.
Visual-analog scales, used most commonly to help a person describe the impact of an issue like pain, can be used in helping children identify the loudness, annoyance, and how they are coping with their tinnitus. The Ida Institute’s Tinnitus Thermometer is one example. For older children and teens, asking how often they are aware of their tinnitus and what percentage of
(iTICQ) was recently validated for use with children 8–16 years of age.16 Items in the questionnaire range across the subscales of (1) sleep and feeling tired, (2) learning, (3) emotional health, (4) hearing and listening, (5) participation, and (6) relationships, all domains thought to be most relevant in children’s lives. Even more recently, the Children’s Tinnitus Questionnaire has been introduced for use with 11to 14-year-old children.17 The Vanderbilt Fatigue Scale for Children, although not designed specifically for tinnitus, can provide insight into the impact that listening with tinnitus has on a child’s daily listening in a classroom.
Case history and assessment need to be modified from the tinnitus evaluation used for adults and can be done by audiologists and otolaryngologists who work with children. Evaluation of tinnitus establishes the foundation for management of children. As noted, there is a scarcity of literature for evidence-based management in children.18 Although there are currently no guidelines specific to management of tinnitus in children, the impact of tinnitus on the quality of their life, their listening, and their learning in the classroom make developing a treatment program imperative. This may start with providing the child and family with information about tinnitus.
that time it is bothersome can provide insight into their tinnitus perception. The My World tool in Ida Institute’s online materials can provide a foundation for talking with younger children about tinnitus and guide the discussion. Most tinnitus questionnaires have been validated on adults, which limits the use of standardized case history materials. The Impact on Tinnitus in Children Questionnaire

Many children often feel relief when they realize that other people also experience tinnitus. This is not to minimize the impact it may have on their life but to create an open environment for them to ask questions and for practitioners to provide additional information. Another aspect of educating children and families is addressing the importance of using appropriate hearing protection to protect hearing and prevent tinnitus.
This is essential for students who may be involved in noisy activities, such as music and farming.
Anecdotal reports suggest that counseling to address a child’s anxiety and emotional issues surrounding tinnitus is useful, although no current research specifically supports counseling approaches in this population.
Educating school personnel is a critical component of supporting school-aged children, and in some cases, developing an educational plan, such as a 504 plan, is also necessary. Sound therapies, including the use of low-gain hearing aids (LGHAs) and consideration of sound treatment, including Lenire, based on its success with adults, are options. It should be noted that use of a remote microphone with hearing aids or digitally moderated (DM) receivers can be beneficial so that children can “hear over” their tinnitus in the classroom. An excellent resource for addressing school-based management for children with tinnitus is the 2014 UK Guidelines for Management of Tinnitus in Children published by the British Society of Audiology.19
Addressing the sleep issues of children with tinnitus is critical to providing a foundation for tinnitus management and ensuring the child receives appropriate rest to be effective at school. Use of a sound pillow with a tinnitus management app, such as Widex Zen or ReSound
Relief, may provide support for both falling asleep and staying asleep.
A team management approach for children and teens with tinnitus is often necessary and results in the best outcomes. The team may include school personnel, a sleep specialist, a psychologist/cognitive behavioral therapist, pediatrician, otolaryngologist, physiatrist, and oncologist, among others. This also provides an opportunity for team members to expand their knowledge of the impact of tinnitus on the patients they serve.
In our practice, pediatricians are generally excited to learn about tinnitus and to learn that many things can help minimize the impact of tinnitus on their patient’s life. The goal is to help physicians realize the breadth and importance of options for addressing tinnitus so that the message “there’s nothing that can be done for tinnitus” is discarded and replaced by a narrative of hope for children, teens, and their families.
Working with children and teens with tinnitus is fun and fulfilling and can be life-changing for the child. A middle school student was referred to our clinic for an auditory processing evaluation. She was described by her teachers and her parents as inattentive and a poor listener. She was on medication for her attention, which she noted “did nothing” to help her. She had several hearing tests, and all were normal. As a routine part of our case history, she
“It is clear that if children raise tinnitus as a concern, often after being asked about it, it should be acknowledged and an opportunity for further discussion should be created.”
was asked about any sounds in her ears, and that’s when she lit up and started describing her tinnitus.
Her parents seemed surprised and asked why she never said anything about it, and she noted that no one had ever asked her. She hadn’t thought to say anything. The more she opened up, the clearer it became that the student attributed listening challenges to her tinnitus. As a result, tinnitus affected her performance in school and caused anxiety.
A combination of counseling and sound therapy was initiated. She noticed that listening was easier, she wasn’t as fatigued in school, and she was less anxious once she understood her tinnitus. Both her teachers and parents echoed these observations. She went from being a C student to being on the honor roll every semester. She attributed it to acknowledging and managing her tinnitus. This is an example of understanding how addressing “the stars” in children’s ears creates a positive journey for children with tinnitus.

Gail M. Whitelaw, PhD, is a clinical associate professor and the Director of the SpeechLanguage-Hearing Clinic at The Ohio State University in Columbus.
Dr. Whitelaw is a clinical preceptor in the Doctor of Audiology (AuD) program and also provides direct clinical care. Her clinical interests are in tinnitus and related sound tolerance disorders, auditory processing disorders, traumatic brain injury, and professional leadership development. She is a Certificate Holder in Tinnitus Management (CH–TM) from the American Board of Audiology. Dr. Whitelaw is a frequently invited presenter on the topic of tinnitus management, particularly as it relates to children and teens.
Complete references can be found here.

By Danuta Raj-Koziak, MD, El˙zbieta Gos, PhD, Piotr H. Skar˙zyn´ski, MD, and Henryk Skar˙zyn´ski, MD
Tinnitus affects both adults and children. A systematic review shows that the prevalence of tinnitus in children ranges from 4.7 percent to 46 percent among children with normal hearing and from 3.2 percent to 62.2 percent in children with impaired hearing.1 A large study that
included 43,064 children shows that tinnitus affects 3.1 percent of children with normal hearing and tinnitus is significantly more frequent in children with hearing loss, at 9 percent.2 Only 1.4 percent of parents of the 3.1 percent of children with tinnitus were aware of the presence of tinnitus in their children.
Interviewing a child about their tinnitus is often a tricky process because children respond to questions
in different ways from how adults do. If a child does not understand the question, they may still want to please the questioner and so will answer all questions positively. Conversely, they may be confused by the questioning and respond negatively.3
It is well known that children rarely report tinnitus spontaneously, but when asked about the condition in the right way, they can thoroughly explain what they are hearing. One reason why children fail to report tinnitus spontaneously is that children who have permanent tinnitus may consider it a normal phenomenon. Similarly, if a family member, for instance, a parent, experiences tinnitus and tells the child about the condition, the child may consider tinnitus to be normal. Unlike many adults, children can more easily divert their attention to other things,
because they are typically actively engaged with external stimuli in their environment.3,4
We maintain that because the child is the only source of information, they need to be directly involved in any tinnitus assessment. Note that consistent answers concerning tinnitus cannot be obtained from children younger than 5 years.5 However, assessment can be supported through the use of a childspecific measurement tool that is appropriate to the child’s cognitive and linguistic abilities, and that poses no risk of harm to the child. Information must be obtained from both child and parent. It is important to appreciate that the parent may also be anxious or distressed by the child’s symptoms. Because little research has been done on how tinnitus manifests in children and how it affects their wellbeing, there is limited understanding of the problems children with tinnitus face, although the available data show
“Interviewing a child about their tinnitus is often a tricky process because children respond to questions in different ways from how adults do.”
that tinnitus can have a significant negative impact on their quality of life. The most frequently identified problems children with tinnitus experience are sleep difficulties, emotional burdens, concentration and
1 Conceptualization of tinnitus: physical, emotional, and social spheres
2 Generation of an initial pool of 33 possible question items
3 Assessment of content validity by four subject matter experts that led to reduction of question items to 21
4 Pilot study among 14 children that led to reduction of question items to 15 (experimental version)
5 Main study among 192 children with tinnitus
6 Psychometric and statistical analyses
7 Formulation of the final version of the Children’s Tinnitus Questionnaire, which includes 11 assessment items
attention difficulties, and difficulties hearing and listening.
Many clinicians and researchers have highlighted the need for improved understanding of tinnitus in children and for a standardized child-specific questionnaire.6–8 To meet that need, we developed and validated a child-specific questionnaire to assess the impact of tinnitus on children’s lives.
The stages of creating the questionnaire are presented in Figure 1 and the Children’s Tinnitus Questionnaire is presented in Figure 2.
We propose this tool be used for diagnostic purposes to assess how tinnitus affects children’s daily functioning.9
The questionnaire should be used with children for whom tinnitus is a problem, who have the full support of their parents and a qualified clinician. The tool has the potential to evaluate the effects of treatment, but before this can be done with confidence, the tool needs to have documented responsiveness; that is, it should be able to measure change over time, and this is an aspect that requires separate research.
The Children’s Tinnitus Questionnaire is more than just a clinical tool; it represents a significant step forward in addressing a condition that can profoundly affect young lives. By prioritizing the unique challenges children with tinnitus face, we not only improve individual patient care but also contribute to a broader understanding of this condition. As research progresses, this questionnaire can provide essential insights and foster better strategies for prevention, treatment, and, ultimately, improved outcomes for children with tinnitus.
First name and family name
Sex Age
Some children have tinnitus. It can resemble humming, buzzing, ringing, clicking, or other sounds. If you have it, YOU are the only person who can hear it, and only YOU know if it bothers you. Some children are bothered a little, some are bothered a lot, and some are not bothered at all. How is it with you? Please read the sentences below carefully and think about how it has been for you over the past month. Choose the answer that best fits. Remember, that there are no correct or wrong answers here. We just want to know what you really think and feel.
1. Tinnitus disturbs me when I want to rest.
2. Tinnitus distracts me when I am doing tests at school.
3. I am upset because of my tinnitus.
4. Tinnitus makes it harder for me to hear what somebody is saying to me.
5. Tinnitus makes it difficult for me to fall asleep.
6. Because of tinnitus it is difficult for me to concentrate during school lessons.
7. Tinnitus bothers me when I am spending time with my friends.
8. I feel tired because of tinnitus.
9. Tinnitus makes it hard to understand what the teacher and other children are saying in class.
10. I sleep badly because of tinnitus.
11. Tinnitus interferes with my ability to do homework.

Danuta Raj-Koziak, MD, PhD, is head of the Tinnitus Department and a research scientist at the World Hearing Center of the Institute of Physiology and Pathology of Hearing. She is the author of 79 publications and 3 monographs, and her chief areas of interest are tinnitus and hyperacusis.

Henryk Skar˙zyn´ski, MD is a professor and doctor of medicine, doctor honoris causa of four Polish universities, and honorary professor of three foreign universities. He is a member of the Polish Academy of Sciences and European Academy of Science and Art. He is globally renowned for performing the world’s first partial deafness surgery in adults and children. He is also the author of more
than five thousand publications and conference presentations. He was awarded an ECCE HOMO order for the exceptional dedication of his life and talents in service to people.

Piotr H. Skar˙zyn´ski, MD, PhD, MSc, is the director for science and development in the Institute of Sensory Organs, deputy head of the Department of Teleaudiology and Screening at the Institute of Physiology and Pathology of Hearing, and professor at the Medical University of Warsaw. His scientific activity is reflected in the implementation of national and international research projects, active membership in national and international scientific societies, and active participation in numerous conferences and workshops. He is the author of nearly a thousand scientific papers. He is also a reviewer for several foreign and domestic journals.

El˙zbieta Gos, PhD, is a psychologist specializing in psychometircs. She works in the Teleaudiology and Screening Department of the Institute of Physiology and Pathology of Hearing. She develops and validates measurement tools and research methodology and performs statistical analyses. Her scientific interests involve the subjective aspects of hearing disorders, especially in tinnitus, hyperacusis, and misophonia.
Complete references can be found here.

The FDA-cleared Levo System was developed by an international team of world-class neuroscientists, clinicians, business professionals, and patients. The patented technology and sound therapy system are scientifically proven to diminish the effect of tinnitus over time.
• Reduces the intensity of a patient’s tinnitus by 80%1
• Improves the quality of a patient’s sleep by 81%1
• Works with patients who have normal hearing and/or tinnitus frequency components outside the range of amplification
• No-risk 3-month return policy2
Neuroscience Based Therapy
Leveraging the cognitive abilities of the brain, the Levo System relieves the symptoms of tinnitus through the process of neural habituation.
Personalized Sound Print Assessment
Just as no two fingerprints are the same, no two people have the same tinnitus sound. Use the Levo System to identify, map, and create the therapy to match the patient’s unique sound print.
Therapy During Sleep
At night, sensory systems remain active with fewer competing sensory inputs, making this 8-hour therapeutic window extremely effective.
(1) https://levomedical.com/wp-content/uploads/2023/10/international_journal_of_audiology_study.pdf
(2) Terms & conditions apply
By Joy Onozuka
In September 2023, Nataleigh sat on the bleachers with her parents, watching her older sister play volleyball. The game was part of an awareness night called “Hitting to Hear,” featuring a speaker who shared the story of Kenna, diagnosed with bilateral sensorineural hearing loss at just eight weeks old. The speaker went on to describe other pediatric hearing disorders, and when she explained tinnitus, Nataleigh turned to her parents and shared that she experienced it too. This revelation was a pivotal moment, providing her parents with a diagnosis that had previously eluded them and setting a new direction for their 7-year-old’s care and support.
Because tinnitus is often thought of as an adult hearing disorder, children are often left to deal with it on their own, as happened with Justin Shwetzer, a 25-year-old chef and parttime musician living in St. Petersburg,

Fla. “I’ve had tinnitus for as long as I can remember… I thought everyone had ringing in their ears.” He finally realized it wasn’t a shared experience when he made an off-hand remark to a friend about it in middle school and received a blank stare in response. For adolescents, discovering that tinnitus is not a shared or typical experience can be surprisingly isolating and emotionally challenging.
Moreover, the issues that adults with tinnitus encounter, such as anxiety and difficulties concentrating and sleeping, mirror those faced by young children and teens with tinnitus.
For Justin, tinnitus was primarily a problem at night. “I had to keep a fan or some sort of white noise going or it would be difficult to sleep,” he said.
For Nataleigh, the struggle with tinnitus was most pronounced at school, where she had trouble focusing.
“Sometimes when I’m at school, it distracts me when my teacher is teaching us things. It’s also hard to read sometimes because of the

Nataleigh is thriving in school now that she’s learned to manage her tinnitus.
sound,” she said. Her grades suffered as a result, which points to the importance of diagnosing hearing issues early. Children with undiagnosed tinnitus, hearing loss, hyperacusis, or misophonia may struggle to keep up in the classroom, appear withdrawn, or act out—all symptoms that can lead to mistaken labels of behavioral or learning problems.
For both Nataleigh and Justin, the cause of their tinnitus remains unknown.
Nataleigh’s mom, Ashley, said, “We wonder[ed] if there was a connection to her rheumatological and neurological symptoms she had been suffering from.” Both parents had noticed that she would turn up the volume on the TV and her tablet, which can be an indicator of hearing loss.
They had her hearing checked, and as often happens with younger patients, the results from the testing fell in the normal range, and failed to capture Nataleigh’s reported difficulties. They would later come to understand that Nataleigh used loud sound to drown out the sound of her tinnitus, which adults with tinnitus understand as “masking.” Fortunately, Nataleigh’s physicians agreed that she should be referred to a tinnitus specialist.
By the time Nataleigh and her father Andrew arrived at Dr. Gail Whitelaw’s clinic at the Ohio State University Department of Speech and Hearing Science, both had a good understanding of tinnitus and its management. In fact, Nataleigh’s first question was, “Do I get hearing aids today?” For Nataleigh, it was an exciting appointment. “[Dr. Whitelaw] took time to explain things to me too, not just to my mom and dad. She let me see cool stuff on her computer on how she can see how my hearing is and showed me some really cool ears toys [models] to teach me about my hearing.” After Nataleigh completed a hearing test and tinnitus screening, Dr. Whitelaw agreed that trialing hearing aids would be an appropriate next step.
With hearing aids programmed with the sound of ocean waves, the change for Nataleigh was immediate, according to her mom, who said there was then a major improvement in Nataleigh’s grades and overall behavior. Nataleigh, who described her tinnitus as “brr, brr, brr,” shared that Dr. Whitelaw’s management tips helped her navigate school better. “She told me that sometimes it’s better for me to be in a louder area when doing tests and school stuff,” she said. “The use of my hearing aids with the ocean sounds helps with the
sound, but nothing makes it just go away.… If I can’t use my hearing aids, like when I am at recess, I just get over it and ignore it so I can play and have fun with my friends.”
Nataleigh’s parents met with her teachers to educate them about tinnitus, which led to the development of a 504 plan to address Nataleigh’s learning and support needs. After four months of trialing hearing aids, Nataleigh got her own pair last April.
Understandably, looking back at it, Ashley and Andrew wish they’d understood earlier that tinnitus was behind Nataleigh’s difficulties focusing at school. Yet, neither of them has it, so, like countless others, they couldn’t identify something they knew nothing about, which highlights the importance of awareness events like “Hit to Hear,” which gave Nataleigh the vocabulary and opportunity to share what she was experiencing.
Justin, who never received counseling or accommodations for tinnitus, said, “For a long time I did nothing to manage my tinnitus. I just accepted it as a relatively annoying part of life.” It was through YouTube that he discovered ways to manage it. He was also diagnosed with insomnia in his late teens, which put him on the right track to better sleep, which can help reduce the intrusiveness of
tinnitus. Reflecting on how he’s gotten by, he said, “I haven’t let tinnitus have much of an effect on my life essentially by virtue of sheer stubbornness.”
Although healthcare from his youth didn’t offer much input on tinnitus, Justin knows that protecting his hearing is key to ensuring that his tinnitus doesn’t get worse, which is why he wears hearing protection while playing music.
Ashley and Andrew are emphatic in encouraging parents and educators to be proactive on anything they notice that seems amiss with a child. “Look for clues, like how loudly they listen to television, their electronics, and how noises around them affect them. These were the indicators we noticed,” Ashley said, adding, “If you feel something is off or wrong, advocate for them to get the testing and help that they need; your child needs you to be there for them.”
By shining a light on how prevalent pediatric hearing issues like tinnitus can be in young children and teens, healthcare providers, educators, and parents can work toward earlier identification and support, helping them thrive academically and socially with a renewed sense of confidence, appropriate care and support, and better understanding of their auditory world.
“Children with undiagnosed tinnitus, hearing loss, hyperacusis, or misophonia may struggle to keep up in the classroom, appear withdrawn, or act out—all symptoms that can lead to mistaken labels of behavioral or learning problems.”
Section 504 of the Rehabilitation Act of 1973 requires public and private schools that receive federal funding to provide children with disabilities, including auditory dysfunctions, accommodations and modifications that support their learning needs. Section 504 covers a wide range of conditions, such as attention-deficit/ hyperactivity disorder (ADHD), diabetes, mobility impairments, vision impairment, and mental health conditions, and a “504 plan” is created for each child who needs one.
For children with auditory dysfunctions, audiologists may initiate or provide input into the 504 plan, which should involve the school’s educational audiologist when possible.
Schools typically review 504 plans annually to ensure that they meet students’ needs and that accommodations are working as intended and are still needed. Parents can also request a review of their child’s 504 plan if they believe further modifications would help.
For students struggling with tinnitus, hyperacusis, and/or misophonia, a 504 plan might include any of the following accommodations:
• Environmental modifications: For tinnitus, that might mean modified seating that allows a student to sit near an airconditioning vent, which serves as masking. For students with sound sensitivities, an environmental modification might mean they have access to quiet areas during breaks.
• Flexible scheduling: Students with tinnitus, hyperacusis, or misophonia may be allowed flexible testing-taking times or breaks during the school day to help manage symptoms.
• Use of assistive technology: Students with tinnitus, hyperacusis, or misophonia may be allowed to wear noisecanceling headphones or sound generators to help manage difficult sounds.
• Teacher awareness training: Teachers who understand tinnitus, hyperacusis, and misophonia can better support students, thereby avoiding unnecessary disciplinary actions or misunderstandings. Training can also help teachers identify situations when the student may need support or accommodation.
• Modified participation in noisy activities: Students with sound sensitivities, reactive tinnitus, or misophonia may be allowed to eat in quieter areas instead of the cafeteria or use hearing protection during loud events, such as school assemblies or gym class.
• Counseling and support services: Students with hearing disorders may receive access to school counseling to help cope with the emotional and social impacts of their condition, such as anxiety, depression, frustration, or social isolation.

For students in private schools without 504 plan obligations, parents may need to work with the school to establish a similar plan or consider other educational accommodations.
Section 504 protections extend into higher education and the workplace, although the process and support structures differ from those in K–12 schools. Colleges and universities that receive federal funding, which includes most institutions, are required by Section 504 and the Americans with Disabilities Act (ADA) to provide reasonable accommodations to students with disabilities. Students must register with the university’s disability services office and provide documentation of their hearing disorder. Colleges are not required to develop a 504 plan, but they must provide accommodations tailored to the student’s needs, such as extended time on exams, priority seating, and reduced-distraction testing environments.
For work, section 504 and the ADA require employers with 15 or more employees to provide reasonable accommodations to qualified employees with disabilities. Examples of workplace accommodations include flexible work hours, modified equipment, accessible workspaces, and assistive technology. In the workplace, individuals are responsible for disclosing their disability and requesting accommodations; employers are required to engage in an interactive process to find reasonable adjustments that don’t impose an undue hardship on the organization.

By Bruce Hubbard, PhD
Many people are afraid to reveal their struggles with tinnitus for fear that it will place them at a disadvantage at work. Others, including medical professionals, engineers, mechanics, accountants, and drivers, quit their jobs, which they love, or retire early for fear they’ll make a mistake that could negatively impact others.
As a cognitive behavioral therapist who also has tinnitus, I’ve successfully treated many people with tinnitus and concentration concerns, including surgeons, lawyers, pilots, and CEOs, who have effectively navigated this challenge and, often after a period of reduced responsibility, went on to resume their full duties at work.
In this article, I’ll address the questions: When should you consider stepping back from work responsibilities? How should you report your concerns to an employer? And what steps can you take to improve concentration with tinnitus and resume your prior level of functioning?
Many people assume that to have tinnitus is to suffer. However, the fact is most people with tinnitus aren’t bothered, and surprisingly, it has little or nothing to do with the sound of their tinnitus.1,2,3 To address the problem of concentration then, it helps to first understand the distinction between tinnitus and tinnitus distress Tinnitus refers to the internal sounds we hear. Tinnitus distress is how we feel about these sounds and how the sounds and negative thoughts and feelings affect our ability to sleep, concentrate, and feel like ourselves. Although tinnitus may not go away, the associated distress and its impact on concentration can ease significantly over time. There are clear steps one can take to promote this recovery and resume full functioning.
When tinnitus first starts, it can stand out like a beacon in the night.
This can absorb much, if not all, of our attention. Trying to concentrate on anything other than tinnitus can seem impossible. Negative thoughts and feelings about tinnitus create additional distractions that further impair our ability to focus. Concentration is most affected by tinnitus early in the process of recovery, before your brain has begun to adapt to the sounds through habituation and when your distress is at its highest level. As this distress subsides, concentration will gradually return to normal. The solution to concentrating with tinnitus, then, is to stop trying to control the volume of your tinnitus and instead address the distress reaction to tinnitus.
This is an important decision you will make in consultation with your physicians. If your physician does not grasp the impact of tinnitus distress on your ability to work, it can be helpful to involve your audiologist or therapist in this discussion. Here are some

considerations to help you decide when to be concerned:
1. Are you in a job where there is a high negative consequence for making mistakes?
2. Since tinnitus started, have you been having trouble keeping your mind on your work?
3. Since tinnitus started, have you made any uncharacteristic mistakes?
4. Have you tried some of the strategies listed below but are still struggling with concentration at work?
If you’ve answered yes to any of these questions, you may consider asking your physician’s advice on whether you should discuss options with your employer.
Tinnitus is an invisible injury, and often one we are ashamed to report. Many believe they will be judged negatively, that others will believe they’ve lost their edge. Rather than quit your job in desperation, I recommend first raising your concerns with your employer. You may choose to first discuss the problem with a trusted coworker or with your Human Resources department before approaching your direct supervisor. Often, temporary accommodations can be made, such as reducing the level of responsibility, working parttime to allow longer periods to restore, or working from home, where there
“If your tinnitus distress is severe and your attention is hijacked around the clock, you may seek a temporary disability leave.”
may be fewer distractions. If your tinnitus distress is severe and your attention is hijacked around the clock, you may seek a temporary disability leave. That period would be used to focus on getting the right intervention to resolve the distress and prepare for your return to work.
We can’t treat tinnitus, but we can manage the distress. The following recommendations are directed at reducing tinnitus distress and improving concentration while tinnitus sounds are present: Learn to apply mindfulness skills during periods of concentration
A commitment to regular mindfulness practice is my first recommendation for improving concentration with tinnitus. Mindfulness is used widely in the health sciences to help us accept and adapt to those aspects of life that we desperately don’t want but can’t get rid of, like tinnitus.
In part, mindfulness is a form of attention-control training, where
you practice paying attention to a chosen target—your breath, body sensations, ambient sound—without getting distracted by spontaneous negative thoughts, feelings, and sensations like tinnitus. A free guide to general mindfulness training is available through the UCLA Mindful Awareness Research Center.4 A guided mindfulness exercise for tinnitus is available as a free resource on my website.5
Try sound enrichment for concentration
Tinnitus tends to be most distracting during quiet, less active times, as when concentrating. Even if you choose not to use sound enrichment for tinnitus 24/7, it may be helpful to experiment with this strategy during activities that require concentration. Sound enrichment (or sound therapy) can be audiologist-guided, using hearing aids or audiology-based “maskers,” or self-guided, through use of Bluetooth devices, speakers, and over-the-counter hearing aids. The ReSound Relief app is a free sound enrichment app designed for tinnitus, which can be found at www.resound.com 6

Get a hearing test and, if appropriate, try hearing aids
Tinnitus clinical guidelines all recommend use of hearing aids for people who have noticeable hearing loss.7 Hearing aids will improve your ability to hear, which will raise the level of natural background sound so that tinnitus may be less intrusive. Hearing aids can also help with speech-related concentration tasks, such as meetings, presentations, and taking direction. Take additional steps to reduce the burden of tinnitus and tinnitus distress
• Discover hope by learning about tinnitus habituation and recovery. This can often lead to an immediate reduction in tinnitus distress and improvement in concentration.8
• Learn reassuring facts about tinnitus and a future with tinnitus. Keeping this more encouraging thinking top of mind can reduce tinnitus distress and help with concentration.8
• Learn to “unhook” from recurrent doubts and worries about tinnitus through an Acceptance and Commitment Therapy (ACT) strategy called cognitive defusion. ACT is a clinically proven treatment for tinnitus distress.9
• Feel like yourself again. A core theme of both cognitive behavior therapy (CBT) and ACT is Feelings Follow Behavior. It’s okay to push yourself a little at a time to get back into life. Behaving like yourself again helps you gradually feel like yourself again, including your ability to concentrate on your work.
• Manage anxiety and depression. Anxiety and depression, common correlates of tinnitus distress, are in themselves known to impair concentration. Addressing these concerns with therapy and/or medication can help improve concentration when tinnitus is present.
It’s common at the onset of tinnitus to experience challenges with concentration at work. To address this problem, find the right help to reduce your distress and to adapt and habituate to tinnitus. CBT or ACT delivered by a behavioral health professional with knowledge and experience treating tinnitus is your best bet. Tinnitus Retraining Therapy (TRT) can also help.
Concerns about effective work performance can be discussed with
your physician. You may choose to seek temporary accommodations or short-term disability leave to reduce concerns about making errors and to provide space to heal. And take heart in the fact that the majority of people with tinnitus aren’t bothered. With the right steps, you can eventually join our ranks!

Upon developing tinnitus distress in 2005, Bruce Hubbard, an experienced clinical psychologist, turned for help to the only evidence-based treatment, cognitive behavioral therapy (CBT). Following his recovery, Dr. Hubbard founded CBT for Tinnitus, LLC, to provide global access to online training and coaching to people struggling with tinnitus distress and tinnitus education for professionals. He has published numerous articles and podcasts on CBT, mindfulness, and tinnitus. His webinar, Cognitive Behavior Therapy for Tinnitus, sponsored by the Anxiety & Depression Association of America (ADAA), has received close to 400,000 views.
Dr. Hubbard is a visiting scholar at Columbia University, Teachers College, and past president of the New York City Cognitive Behavior Therapy Association (2016–2018). Additionally, he is certified in cognitive and behavioral psychology through the American Board of Professional Psychology (ABPP). He completed his doctorate in clinical psychology at Binghamton University and his clinical internship at New York University Medical Center.
Complete references can be found here.
By Karen L. Wilber, AuD
Sound sensitivities, also known as Decreased Sound Tolerance (DST) problems, are not unusual in young children. They may cover their ears when entering public bathrooms with loud hand dryers and self-flushing toilets, or in noisy crowds. Parents can help their child by talking about the sounds before their child enters the situation, distracting their attention from the sounds, or giving other support that reduces their anxiety and improves their tolerance. Most children outgrow these behaviors. However, when sound sensitivities persist into kindergarten and/or disrupt daily life, parents may need to consult a healthcare professional to figure out what is going on and to come up with a management plan.
Sound sensitivity issues are definitely a family affair when a child is affected. They may cause a child to melt down at a parade, refuse to go to birthday parties, or avoid mealtime with family. A child’s vigilance about protecting themselves from problem sounds can cause anticipatory anxiety and difficult behaviors such as fleeing from the classroom or going to the nurse’s office instead of attending gym class.

DST issues have a variety of presentations as a result of these conditions or a combination of them: hyperacusis, phonophobia, or misophonia. DST issues are common in autistic children and have a higher incidence among children with other neurodevelopmental disorders including attention-deficit/hyperactivity disorder (ADHD).
Hyperacusis causes a child to perceive moderate or even quiet everyday sounds, which do not bother others, as much too loud. The problem sounds may be any sound that reaches a certain decibel level or has certain pitch characteristics. A child with hyperacusis can exhibit great distress when confronted with these sounds. They may become anxious, cover their ears and cry, or exhibit tantrum-like behavior. Hyperacusis can be severe and cause avoidance of activities, including refusal to go to school. Sometimes children complain of pain in or around their ears from sound.
Phonophobia occurs when a child develops a fear of certain sounds. It is not about loudness, but about an association of that sound with a time or place when they were greatly startled or frightened by sound. After that exposure, a child who develops phonophobia will do whatever they can to avoid hearing that sound again
and their behavior may be out of sync with their developmental level. The child may have such anxiety about encountering the sound that they flee a situation in which that sound might occur, or refuse to attend certain events. In general, these children are not affected by all loud or moderately loud sounds but only sounds that are in a certain category or are related to specific environments or activities.
Phonophobia can develop because of hyperacusis, when a child becomes fearful of situations in which the sounds that cause discomfort and/ or pain may occur and actively avoids them. Alternatively, being startled and frightened by a sudden loud sound can be a starting point of phonophobia with hyperacusis piling on right behind it.
Misophonia causes the individual to experience physiological arousal or the fight-or-flight response followed by negative emotions such irritation and anger, when they hear certain common, repetitive sounds. Typically, the trigger sounds are made by others and are associated with the acts of breathing, eating, or talking. Triggers can also be repetitive environmental sounds like tapping on a keyboard or the ticking of a clock. An individual’s

triggers can be specific to certain people or places. For example, a sniffing sound from siblings and parents may induce an aversive response, but being around a friend who is sniffing can be completely innocuous. The number of triggers and the context in which they occur vary from individual to individual. Children with more severe misophonia symptoms may experience trigger sounds at school, at home, and with their friends, and the reaction may be so intense that it is extremely disruptive to their daily lives. Misophonia on the milder end may involve less intense reactions to and fewer numbers of trigger sounds. It is not unusual for hyperacusis to accompany misophonia.
To introduce the appropriate treatment or management plan, the DST disorder or combination of disorders should be diagnosed. A pediatric audiologist can make these
The content in Tinnitus Today magazine is intended to provide helpful health information for the general public. It is made available with the understanding that the American Tinnitus Association (ATA) is not engaged in rendering medical, health, psychological, or any other kind of personal or professional services. The magazine content should not be considered complete and, therefore, does not cover all physical conditions or their treatment as it relates to tinnitus and tinnitus management.
ATA always recommends that you consult and work with a medical,
diagnoses or refer you to an audiologist who specializes in these issues.
Hyperacusis symptoms can improve with educational counseling and sound therapy provided by an audiologist, or behavioral health therapy, or occupational therapy. A combination of these disciplines may be the best approach, depending on the magnitude of the problem.
Phonophobia is best handled by a behavioral health provider who can help the child develop skills to reduce anxiety and introduce gradual, supported exposure to the feared sounds and situations.
Currently, although there is no standardized treatment to resolve misophonia, there are interventions that can help with management of this disorder. Development of coping skills can be assisted by behavioral health therapy or occupational therapy. Each of these disciplines can provide tools for down-regulation of the child’s nervous system so that reactions may be less intense and they can regulate more quickly. An audiologist can fit
sound generators, which are hearing aid-sized devices that do not amplify external sounds, but are programmed to emit constant white noise or a similar type of broadband sound. These devices can reduce perception of triggers and increase the child’s comfort, depending on the severity of their symptoms.
If we pay attention when small children behave in ways that demonstrate decreased sound tolerance issues, we can find ways to help them cope.

Karen Lincoln Wilber, AuD, has over 30 years of experience in pediatric audiology. At Boston Children’s Hospital, she holds the position of Specialty Audiologist in Tinnitus and Decreased Sound Tolerance. Dr. Wilber initiated the program for diagnosis and treatment of these disorders at Boston Children’s in 2020. She has written and presented on the topic extensively, including for the American SpeechLanguage Hearing Association and the Canadian Audiology Association.
healthcare, or other competent professional when considering the best course of tinnitus management. This begins with a medical examination to rule out possible underlying medical causes for tinnitus. If you’re interested in adopting guidance/suggestions made in the magazine, you should discuss this first with your medical provider before doing so.
Any information about drugs and supplements contained in the magazine is general in nature, and does not cover all possible uses, actions, precautions, side effects, or interactions of the medicines

mentioned. The content of the magazine is not intended as medical advice for individual problems or for making an evaluation for pursuing a particular course of action.
ATA and authors of articles in the magazine specifically disclaim all responsibility for any liability, loss, or risk, personal or otherwise, which is incurred as a consequence, directly or indirectly, of the use and application of any of the content in the magazine.

By Brittany Grayless, AuD
Misophonia is a condition in which individuals experience an emotional response to specific sounds in their environment. These sounds can include breathing, swallowing, and chewing.1 Individuals with misophonia are typically bothered by these sounds emitted by others, not when they make the sound themselves. Although there is currently no cure for this condition, some treatment strategies have been shown to reduce the intrusiveness of symptoms, including sound therapy.2
Although misophonia is not specific to the pediatric population, at our clinic it typically presents in pediatric patients, which is consistent with research suggesting the average onset of misophonia symptoms begins
around 13 years of age.3 It is important not to ignore misophonic symptoms in children because the condition can lead to social withdrawal and isolation, and negatively affect familial and peer relationships.4 Emerging research shows the prevalence of misophonic symptoms among adult students (18 to 54 years) ranges from 6 percent to almost 20 percent.5,6 Here, I’m sharing a case study of a female adolescent who came to our clinic for help managing misophonia.
At age 14, Amber came to our clinic for an evaluation of misophonia. When she sat down to begin the case history, she immediately began crying. I asked her if she was nervous about the appointment, and she replied yes. I assured her that she was in control
of the appointment, and we would not do anything that would make her feel uncomfortable.
During the case history, she revealed that she was bothered by the sounds of others eating and chewing, tapping (repetitive sounds), breathing, and others eating crunchy foods, and it had begun between the fifth and seventh grades. Her mother, who accompanied her to the appointment, shared that Amber had been sensitive to sounds and smells since a young age. Her mom also noted that Amber had a difficult time transitioning to high school at the start of the school year. Amber already had a 504 plan in place for these symptoms, which allowed her to leave the classroom when she became overwhelmed by trigger sounds. However, Amber said she seldom used the accommodation,
often pushing through her emotions to avoid attracting attention to herself. When asked about stressful situations that she had experienced, Amber said the COVID-19 pandemic period was especially stressful, with her trigger sounds becoming even less tolerable. Her emotional reaction to trigger sounds was anger, while her physical reaction included nausea and fist clenching. Because correlations between misophonia and obsessivecompulsive disorder have been found in research,7 Amber was also asked about related symptoms. Amber said she liked to keep her things very organized and would get upset when people touched her things. At this time, Amber was still eating dinner at the dinner table with her parents; however, she often felt the need to leave the table to escape the sound of chewing.
Because misophonia is subjective, it is important to gain as much information as possible from the person to assist in diagnosis. To facilitate this, patients being seen for a misophonia diagnostic appointment at the University of Tennessee Health Science Center
(UTHSC) Audiology Clinic are mailed several questionnaires. We use these questionnaires to gain insight into the intrusiveness of misophonic symptoms, as well as other factors that may contribute to overall mental health, including anxiety and depression.
Misophonia Assessment
Questionnaire (MAQ): The MAQ assesses severity of misophonic symptoms, and the total sum score is used to indicate severity level. A total score of 1–21 indicates mild, 22–42 indicates moderate, and 43–63 indicates severe.8 Amber scored 46, putting her in the severe category.
Amsterdam Misophonia Scale (A-MISO-S): The A-MISO-S assesses misophonic symptoms in the following areas: time, interference, distress, resistance, control, and avoidance.9 It is a six-item scale, with scores ranging from 0 to 24. Amber’s sum score of 17 suggested severe misophonic symptoms.
Misophonia Impact Survey (MIS): The MIS helps providers gain insight into how misophonia is impacting different areas of the patient’s life.10 It is composed of five questions that explore interpersonal relationships, family life, social life/
“It is important not to ignore misophonic symptoms in children because the condition can lead to social withdrawal and isolation, and negatively affect familial and peer relationships.”
leisure activities, school and work, and personal activities on a scale of 0 to 10. The questionnaire helps the provider understand what areas to focus on when seeking to improve the patient’s quality of life. Amber reported that her misophonia had impacted her family life (7—severely), social life (8—severely), and schoolwork (9—severely). Amber also reported that her misophonia impacted her individual/alone time (4—moderately).
Misophonia Activation Scale (MAS-1): The MAS-1 is a two-item survey designed to focus on the emotional and physical reactions to a specific trigger sound that a patient may experience.11 Severity levels range from 0 (no discomfort) to 10 (reacts with violence toward a person, animal, or self). Amber’s emotional response to her trigger sounds was an 8: “I experience psychic discomfort and some violence thoughts.” Amber’s physical response to her trigger sounds was a 3: “I feel some physical sensation but have difficulty or cannot ignore it.”
Detailed Trigger Inventory (DTI): The DTI form provides a way for the patient to document their trigger sounds, where the sound comes from (e.g., parent, friend, sibling), and the emotional and physical responses to the trigger sound, referencing the MAS-1 severity levels. At this point in the intake packet, Amber became

emotionally distressed from having to think about her trigger sounds. Because of this, she did not complete the rest of the intake packet to avoid further distress. During the case history portion of the appointment, I asked Amber if she felt comfortable simply stating what her trigger sounds were without giving them a severity rating. Her trigger sounds included eating and chewing by family members at home, breathing by individuals at home and in the classroom, and tapping sounds in the classroom.
Child Anxiety and Depression Scale (RCADS): The RCADS is a scale developed to assess anxiety and depression in children in third to twelfth grade.12 It also provides an assessment of subscales, including social phobia, panic disorder, major depressive disorder, separation anxiety disorder, generalized anxiety, and obsessive-compulsive disorder.13 The scale has parent and child forms so that health practitioners can gain insights into both perspectives, and the forms can highlight some of the underlying characteristics of misophonia sufferers, such as obsessive-compulsive disorder and anxiety.14 Amber reported considerable distress that prevented her from completing this form. When completed, I find this questionnaire useful in screening for depression and
anxiety in the misophonia pediatric population.
Although there is no objective test to diagnose misophonia, it is important to rule out hearing loss. Therefore, an audiological assessment including pure-tone thresholds should be completed. Additionally, misophonia may present in patients with normal to reduced loudness discomfort levels (LDLs),15 so an assessment of LDLs should also be included. Amber presented with normal hearing for both ears at all frequencies tested (250–8,000 Hz). Her LDLs ranged from 60 dB to 85 dB in the right ear and 40 dB to 75 dB in the left ear, indicating the presence of hyperacusis bilaterally.
Based on the severity of the reported misophonic symptoms and their impact on Amber’s quality of life, as well as the presence of bilateral hyperacusis, it was recommended that Amber use ear-level maskers to incorporate sound therapy. Additionally, Amber was recommended to pursue cognitive behavioral therapy to aid coping. Lastly, consideration of where she sat in classrooms was recommended, such as sitting near the air conditioner, so that she could
utilize environmental masking in her learning environments.
Amber was fit with bilateral earlevel maskers (Oticon Zircon 2). She was asked to rate her mood on a scale of 1 to 10 (1 being the worst she has ever felt, 10 being the best she has ever felt). Amber rated her mood at a 3. Because sound therapy is used differently for misophonia and hyperacusis, Amber was asked to choose which she wanted to prioritize; she chose misophonia.
Amber selected the following masking sounds as her ear-level maskers: (1) red noise, (2) pink noise, (3) modulated pink noise, and (4) no maskers on. For each masking program, the mics were turned off to ensure that no amplification was provided to her trigger sounds. Amber was instructed to close her eyes to remove visual triggers while her mom chewed gum. The masking level was increased until Amber’s facial reaction was visibly reduced. This process was repeated for each of the masking programs. Because of the severity of her emotional distress and to prevent further trigger sounds from developing, it was recommended that Amber wear her maskers during all waking hours.

“Amber recently reached out to me expressing interest in pursuing audiology as a career, reminding me that compassion, dedication, and individualized patient care can lead to life-affirming changes.”
To understand the effectiveness of the maskers, Amber was asked to rate her mood again on a scale of 1 to 10 at her one-week follow-up. She reported a 7, which was a significant improvement from the week before, when she’d reported her mood at a 3.
She had tried all her masking programs, and the red noise program became her preferred one. She mentioned wanting to raise the masker volume in some environments, specifically when taking exams, where the quiet setting made trigger sounds more noticeable, and in auditoriums, when noise was overwhelming. In both scenarios, she found herself having to leave the room.
She also noted wanting to turn down the masker volume when she got home from school. Amber explained that wearing the maskers at the dinner table seemed to help her tolerate chewing sounds. At this appointment, the masker volume control was activated, and Amber was introduced to the ReSound Tinnitus Relief smartphone app to give her more customized masking options to stream to her hearing aids.
At Amber’s one-month follow-up, she said the maskers had been very helpful. She often raised the volume
in school settings and lowered it in quieter environments like her home. She said that, although she no longer felt compelled to leave the room to escape trigger sounds, she still was having difficulty with trigger sounds in high-concentration environments such as test-taking and writing. She also reported feeling overwhelmed when she couldn’t identify the source of a trigger sound.
Amber was counseled on concentration strategies and deep breathing to draw on in such situations. She was also encouraged to utilize the preferential seating outlined in her 504 plan, which would allow her to sit in the back corner of the class during tests so she could view where sounds were coming from as a way to reduce her anxiety. It was also advised that she explore use of fidget toys or other methods of distraction like progressive muscle relaxation when she felt triggered by sounds. Amber had yet to explore the smartphone app for additional masking, so she was advised to experiment with the different masking options.
Amber reported wearing her hearing aids all waking hours and was pleased overall with the masking programs. An additional program of
white noise was added to the hearing aids to use for when noisy situations felt overwhelming. She reported also seeing a psychologist to help manage anxiety stemming from her misophonia. We revisited the idea of using fidget toys, coloring books, and crossword puzzles as distractions in noisy situations.
Amber had begun a new school year and reported that it was going well. She said her wellness class was the only one in which she struggled because of the volume of noise. She continued to wear her maskers all waking hours and to meet weekly with her psychologist. It was recommended that she increase the volume of the masker before going into noisy situations to preemptively shield her from a triggering environment.
Fitting misophonia patients with ear-level maskers has become my most rewarding type of appointment. To see the distress evoked from trigger sounds dissipate from the patient, to be replaced with relief and hope, is a fulfilling experience. Pediatric misophonia affects not only the patient’s quality of life but also the family members’, who are searching for anything that can help their child. Amber’s case is not unique among misophonia patients I’ve worked with. A thorough case history provides insight into different areas that are affected by the condition. When the assessment is complete, an individualized treatment plan is developed. Sound therapy is utilized to make trigger sounds tolerable. It is

important to set realistic expectations in that the goal is not to make the trigger sound a likeable sound but rather a tolerable sound. Stress and anxiety seem to play a role in the reaction to trigger sounds, so discussion of coping strategies and a referral to a behavioral health specialist are important.
Amber began her journey at our clinic experiencing significant distress and anxiety from her misophonic symptoms. She is still being seen annually and now comes in with a smile on her face. She feels more in control of her environment by using the masking sounds in her hearing aids. Her mom has expressed how thankful she is for the services we’ve provided to help her daughter.
Although there currently isn’t a cure for misophonia, in this and other case studies,16 sound therapy provides a way for sufferers of misophonia to improve quality of life and engagement with others in settings that would otherwise be difficult to endure.
Amber recently reached out to me expressing interest in pursuing audiology as a career, reminding me that compassion, dedication, and individualized patient care can lead to life-affirming changes.

Brittany Grayless, AuD, is an associate professor at the University of Tennessee Health Science Center in Knoxville, Tenn. She completed her training at the University of Tennessee Health Science Center with a residency at Duke Medical Center. She has been with UT since 2014 and provides services to adults and adolescents with tinnitus, hyperacusis, and misophonia. She is currently pursuing her doctorate in hearing sciences, and her research efforts are primarily focused on the psychological aspects of these clinical populations. She is eager to contribute to tinnitus research by providing clinically applicable information that can be utilized by clinicians to provide individualized patient-centered care.
References
1. L. R. Rappoldt, M. M. van der Pol, C. de Wit et al. (2023). Effectiveness of an innovative treatment protocol for misophonia in children and adolescents: Design of a randomized controlled trial. Contemporary Clinical Trials Communications, 33, 101105. https://doi.org/10.1016/j. conctc.2023.101105
2. D. Palumbo, O. Alsalman, D. Ridder, J. Song, & S. Vanneste. (2018). Misophonia and potential underlying mechanisms: A perspective. Frontiers in Psychology, 9, 953. https://doi.org/10.3389/ fpsyg.2018.00953
3. I. J. Jager, N. C. C. Vulink, I. O. Bergfeld, A. J. J. M. van Loon, & D. A. J. P. Denys. (2020). Cognitive behavioral therapy for misophonia: A randomized clinical trial. Depression and Anxiety, 38(7), 708–718. https://doi.org/10.1002/da.23127
4. A. G. Guzick, M. Cervin, E. E. A. Smith et al. (2023). Clinical characteristics, impairment, and psychiatric morbidity in 102 youth with misophonia. Journal of Affective Disorders, 324, 395–402. https://doi. org/10.1016/j.jad.2022.12.083
5. M. S. Wu, A. B. Lewin, T. K. Murphy, & E. A. Storch. (2014). Misophonia: Incidence, phenomenology, and clinical correlates in an undergraduate student sample. Journal of Clinical Psychology, 70(10), 994–1007.
6. X. L. Zhou, M. S. Wu, & E. A. Storch. (2017). Misophonia symptoms among Chinese university students: Incidence, associated impairment, and clinical correlates. Journal of ObsessiveCompulsive and Related Disorders, 14, 7–12.
7. T. Webber, P. Johnson, & E. Storch. (2014). Pediatric misophonia with comorbid obsessive-compulsive spectrum disorders. General Hospital Psychiatry, 36(2), 231.e1–231.e2. https://doi.org/10.1016/j. genhosppsych.2013.10.018
8. T. H. Dozier. (2015). Understanding and overcoming misophonia: A conditioned aversive reflex disorder. Misophonia Treatment Institute.
9. A. Schröder, N. Vulink, & D. Denys. (2013). Misophonia: Diagnostic criteria for a new psychiatric disorder. PLOS ONE, 8(1), art. e54706. https://doi.org/10.1371/journal.pone.0054706
10. T. H. Dozier. (2016). Misophonia forms. Misophonia Institute. Retrieved from https:// misophoniainstitute.org/forms/
11. G. Fitzmaurice. (2010). The Misophonia Activation Scale. Misophonia UK. Retrieved from http://www. misophonia-uk.org/the-misophonia-activation-scale. html
12. B. F. Chorpita, C. Ebesutani, & S. Spence. (2015). Revised Children’s Anxiety and Depression Scale: User’s guide. https://www.childfirst.ucla. edu/wp-content/uploads/sites/163/2018/03/ RCADSUsersGuide20150701.pdf
13. B. F. Chorpita, L. Yim, C. Moffitt, L. A. Umemoto, & S. E. Francis. (2000). Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behaviour Research and Therapy, 38(8), 835–855. https://doi.org/10.1016/S0005-7967(99)00130-8
14. S. E. Cusack, T. V. Cash, & S. R. Vrana. (2018). An examination of the relationship between misophonia, anxiety sensitivity, and obsessivecompulsive symptoms. Journal of ObsessiveCompulsive and Related Disorders, 18, 67–72. https://doi.org/10.1016/j.jocrd.2018.06.004
15. P. J. Jastreboff & M. M. Jastreboff. (2013). Using TRT to treat hyperacusis, misophonia, and phonophobia. ENT & Audiology News, 21, 88–90.
16. B. Grayless. (2021). Assessment and management of misophonia in a female adolescent: A case study. Perspectives of the ASHA Special Interest Groups







By Jan L. Mayes, MSc (Audiologist, Retired)
In today’s world, children wearing headphones and earbuds linked to laptops, TV screens, tablets, smartphones, and gaming consoles has become almost as common as seeing children wearing backpacks, and it raises concerns about how this constant auditory and visual exposure may be shaping young ears and minds. A recently published New Zealand study reviewed negative impacts of recreational and educational screen time on the health and well-being of children and adolescents.1 This review became the starting point for developing recommendations for the use of digital technologies in educational settings to maximize youths’ learning benefits while mitigating risks. Lead author Julie Cullen and contributing
authors, including me, developed specific age-based recommendations on safer screen use for students in preschool or early childhood education up to high school.
Our study explored eight health areas to allow for a holistic overview. We found that some use of technology could support youths’ health and well-being, but frequent and extended screen time presents risk of harm to young people, with negative impacts occurring with two to six hours of daily usage. The American Academy of Child and Adolescent Psychiatry estimates that average screen time in the United States is about four to six hours for children ages 8 to 12, and up to nine hours for teens.2 This excessive screen time likely puts many young people at risk of negative health consequences.
The consequences of unsafe screen habits are widespread, including
higher risk of impaired vision (dry eye disease and myopia), loss of physical fitness and obesity, headaches and pain, disturbed sleep, attention problems and impaired cognition, anxiety and depression, and impacts on emotional and social well-being. Digital devices are now commonly used with headphones and earbuds as personal listening systems for music, videos, gaming, and educational content. Noise-induced hearing loss is a significant risk if earbuds or headphones are used at loud volumes during screen time. Risk of developing tinnitus and hyperacusis or decreased sound tolerance are also linked to use of earbuds or headphones at unsafe listening volumes.3
These findings are troubling, and screen time is only increasing as devices are used more commonly at school and at home. Our editorial
in the New Zealand Medical Journal states, “Digital technologies are changing the way we live in society, and ensuring that they provide opportunities to our young people, contribute to equity and do not cause harm will require a multi-pronged approach for caregivers, educators and policy makers.”4
The Pediatric Society of New Zealand has endorsed our recommendations for the use of digital technologies in schools and early childhood education.5 (See the accompanying table.) These evidencebased recommendations to lower risks across different ages and stages of development include interventions such as screen time limits and balancing screen and nonscreen learning tasks, taking eye breaks, safer use of headphones and earbuds, ergonomic use of screens and lighting adjustments, and regular vision and hearing testing.
The less time spent using headphones or earbuds during screen time and the lower the personal listening volume used, the lower the risk of noise-induced hearing health damage. If using headphones or earbuds during screen time, early warning signs of noise damage include tinnitus and/or hyperacusis, difficulty hearing or understanding in background noise, and speech difficulties. Prevention includes limiting headphone and earbud
use to purposeful and time-limited tasks as well as choosing well-fitting headphones and earbuds with noise cancellation or sound-isolating features and built-in volume output limits if possible. Limiting use of headphones and earbuds with smartphones or mobile phones could also help protect hearing health of children and teens.
Loose or poorly fitting headphones and earbuds are even less safe because users tend to turn the volume up to hear or understand audio content over background noise. Headphones and earbuds with noisecanceling technology also help users listen at lower, safer volumes in the presence of background noise or in busy or crowded spaces. Headphones are preferred for younger children (age 12 and under). Earbud styles are less safe for children because of looser fit since sizing is generally for mature or adult ears, and there is higher risk of ear infections. Some headphones and earbuds offer volume output limits that might help improve personal listening safety. Unfortunately, independent testing has found too many fail to limit sound levels as advertised, and manufacturers typically fail to limit output below the 70 dB (Leq,24-hour) public health daily average exposure limit recommended to prevent noiseinduced hearing loss.3,6
Risk of hearing health damage also depends on the type of device used. Most devices can be made
safer by using built-in output limits and safer-listening features, typically found under settings for audio and/or headphones. Together with the child or teen, turn down any output limits and safer-listening features to the softest or lowest decibels possible. These settings can usually be locked under parental controls. It’s important to teach young people that even at the lowest device settings, if they listen at too loud a volume setting, they could still be exposed to harmful sound energy without getting any unsafe listening alerts. Even at lower volume settings, mobile phones or smartphones have the highest audio output compared to other devices. Children and teens have the highest risk of noise-induced hearing health damage when they use headphones or earbuds with cell phones during screen time.
“Headphones and earbuds with noise-canceling technology also help users listen at lower, safer volumes in the presence of background noise or in busy or crowded spaces.”
For personal listening with headphones or earbuds, it is very important to encourage children and teens to use the lowest functional listening volume possible. This means starting at zero and slowly turning the loudness up to the lowest volume they can hear clearly and understand, without it sounding loud. The functional listening volume might vary a bit depending on the source content. Louder or less safe volumes are often used for music and gaming compared to other audio or audiovisual sources such as speech, videos, and audiobooks. Functional listening volume can also vary depending on the individual, such as a child with hearing loss who may appropriately need a higher or louder functional listening volume.
Generally, children and teens using headphones or earbuds should be encouraged to use a loudness setting as low as possible below 50 percent
volume, meaning below 50 percent on a device’s visual analog volume scale. Personal listening volumes of 50 percent and higher may be linked to increased risk of noise-induced tinnitus and hyperacusis, with volumes of 60 percent and higher linked to noiseinduced hearing loss.3 If not using headphones or earbuds, children and
teens should mute the volume during screen time to avoid disturbing others. Digital technologies can provide opportunities for learning, but calls have been made to balance benefits with harms. Some education authorities are already taking steps to protect students from digital technology risks. For example, various school districts in Canada and the
United States have banned cell phones in classrooms. A school counselor in Canada reported remarkably positive outcomes six months after a ban was introduced, including improved mental health, decreased bullying, more engagement in class, more social interaction, increased academic success, and children playing together instead of being on their phones.7
Restrict
Limit
• No screen use under 2 years old.
• No screen use in early childhood education without teacher approval.
• For 3- to 6-year-olds, maximum 10-to 15-minute sessions if using screens.
• Limit headphone use; avoid earbuds.
• No smartphone/smartwatch access during class, unless exempt.
• No screen use in class without teacher approval.
• Maximum session length 20 minutes.
• At most, up to one-third of school day learning on screens (2 hours max), unless required for special learning needs.
• Limit headphone use; avoid earbuds.
• No smartphone/smartwatch access during class, unless exempt.
• Eye breaks every 20 minutes of screen time, or change tasks.
• Limit headphone/earbud use.
Encourage
• Purposeful and intentional use, coviewing advised.
• Correct ergonomics and lighting.
• Lowest functional personal listening volume if using headphones.
• Outdoor exercise and free play.
• Reward prosocial and positive learning behaviors with social or physical activities instead of screen-based.
• Purposeful and intentional use of devices in schools only.
• Correct ergonomics and lighting.
• Lowest functional personal listening volume if using headphones.
• Outdoor exercise/activities.
• Protect play in break periods (screen-free, outdoors if possible).
• Reward prosocial and positive learning behaviors with social or physical activities instead of screen-based.
• Paper homework option preferred.
• Education on healthy screen behaviors, digital citizenship, and cyber security.
• Purposeful and intentional use of devices in schools only.
• Correct ergonomics and lighting.
• Lowest functional personal listening volume if using headphones/earbuds.
• Balance of screen and nonscreen learning tasks.
• Outdoor exercise/activities.
• Reward prosocial and positive learning behaviors with social or physical activities instead of screen-based.
• Paper homework option if tasks allow.
• Education on healthy screen behaviors, digital citizenship, and cyber security.
*Adapted from “Recommendations for the Use of Digital Technologies: Schools, Kura, and Early Childhood Education,” from the Pediatric Society of New Zealand. Note: In New Zealand, kura is a word in te reo Mˉaori, which is the language of Mˉaori (the indigenous people of New Zealand), meaning a state school where the teaching is based on Mˉaori culture, values, and language.
In the U.S., the National Center for Educational Statistics found 76 percent of U.S. public schools prohibit nonacademic use of cell phones or smartphones during school hours.8 For example, in Kansas, a pilot program banning cell phones found phone-free ninth-grade students had the highest grade point averages across their school, and a Utah school bought pouches so students could keep cell phones on them while restricting use to help protect them academically, mentally, and emotionally.9
Unfortunately, most countries currently don’t provide any national guidance to prevent health and safety problems associated with use of digital technologies in classrooms. In an interview with the New Zealand Herald, Julie Cullen said, “The United Nations General Assembly recently highlighted the digitization of education and called for urgent discussion and regulation of the impacts of using these technologies within schooling.”10,11
The bottom line is that there needs to be a balanced approach for children and teens to access technologies in an increasingly digital world while mitigating their health and safety risks at school and at home. Negative consequences to vision and hearing, physical health, sleep, neurology, and cognition and the social and emotional impacts need to be considered to best protect child and adolescent wellbeing, health, and development.
Early onset of impaired health has lifelong consequences to quality of life at school, home, and play. Hopefully, more education authorities will implement evidence-based recommendations to minimize health and safety risks linked to use of digital technologies at school. The goal is
“Unfortunately, most countries currently don’t provide any national guidance to prevent health and safety problems associated with use of digital technologies in classrooms.”
to promote safe and healthy screen habits while maximizing learning benefits that screen-based digital tools can offer in educational settings.

Jan L. Mayes, MSc, has had tinnitus for more than 40 years. She is an awardwinning author of nonfiction hearing health books. As a retired audiologist, Mayes continues to write about tinnitus, hyperacusis, and community noise impact on disability access, communication, and hearing wellness. In her spare time, Mayes enjoys writing dystopian fiction. To learn more, visit her website: https:// janlmayes.wordpress.com/
References
1. J. Cullen, A. Müntz, S. Marsh, L. Simmonds, J. Mayes, K. O’Neill, & S. Duncan. (2024). Impact of digital technologies on health and wellbeing of children and adolescents: A narrative review. New Zealand Journal of Physiotherapy, 52(1), 62–77. https://doi.org/10.15619/nzjp.v52i1.364
2. American Academy of Child and Adolescent Psychiatry. (2024). Screen time and children. Facts for Families, no. 54. https://www.aacap.org/ AACAP/Families_and_Youth/Facts_for_Families/ FFF-Guide/Children-And-Watching-TV-054.aspx
3. D. Fink & J. L. Mayes. (2021). Unsafe at any sound: Hearing loss and tinnitus in personal audio system users. Proceedings of Meetings on Acoustics, 43, 040003. https://doi.org/10.1121/2.0001452
4. J. Cullen, A. Muntz, S. Marsh, L. Simmonds, J. Mayes, K. O’Neill, & S. Duncan. (2024). Impacts of digital technologies on child and adolescent health: Recommendations for safer screen use in educational settings. New Zealand Medical Journal, 137(1958), 9–13. https://doi. org/10.26635/6965.6565
5. Pediatric Society of New Zealand. (2024). Recommendations for the use of digital technologies: Schools, kura, and early childhood education. https://www.paediatrics.org.nz/ knowledge-hub/view-resource?id=59
6. Environmental Protection Agency Office of Noise Abatement and Control. (1974). Information on levels of environmental noise requisite to protect public health and welfare with an adequate margin of safety. EPA/ONAC No. 550/9-74-004. U.S. Environmental Protection Agency. https://www.nrc. gov/docs/ML1101/ML110110692.pdf
7. J. Benchetrit. (2023, June 13). Canadian schools are experimenting with cell phone bans, but some parents say the devices are a lifeline. CBC News. https://www.cbc.ca/news/canada/canadianschools-cell-phone-bans-1.6869993
8. National Center for Educational Statistics. (2024, January 17). New schools data examine violent incidents, bullying, drug possession, “restorative” practices, security staff, and more [Press release]. National Center for Educational Statistics. https://nces.ed.gov/whatsnew/press_ releases/1_17_2024.asp
9. C. Tabachnick. (2024, September 2). Schools across the U.S. restrict cellphones amid growing behavior, mental health, academic concerns. CBS News. Retrieved from https://www.cbsnews.com/news/ cellphone-bans-in-schools
10. I. Davison. (2024, July 4). Screen time: New limits needed in New Zealand schools, experts say. New Zealand Herald https://www. nzherald.co.nz/nz/screen-time-new-limitsneeded-in-new-zealand-schools-experts-say/ CLU4QMG3WNHPLEN4XI6IZNTUPU/
11. United Nations General Assembly. (2022). Impact of the digitalization of education on the right to education: Report of the Special Rapporteur on the right to education, Koumbou Boly Barry (Fifteenth session, Agenda item 3). United Nations. https://www.right-to-education.org/sites/right-toeducation.org/files/resource-attachments/UNSR_ Impact%20of%20the%20digitalization%20of%20 education%20on%20the%20right%20to%20 education_A.HRC_.50.32_April2022_EN.pdf
By Becca Kane, AuD, ATA Tinnitus Program Advisor
According to the U.S. Centers for Disease Control and Prevention (CDC), an estimated 12.5 percent of children and adolescents have been diagnosed with noise-induced hearing loss.1 This is significant because even mild hearing loss in children can have a profound impact on their speech and language development, classroom performance, and overall social and emotional development. Noiseinduced hearing loss can result from frequent exposure to loud sound or even an isolated one-time loud event.
According to the World Health Organization (WHO), besides the known auditory side effects of noiseinduced hearing loss and subsequent
tinnitus, the nonauditory side effects of loud noise found among frequently exposed individuals are also cause for concern. They include sleep disturbance, cognitive difficulties, and increased hypertension and cardiovascular disease. Basner et al. suggest that children may experience psychological stress, among other symptoms, because they lack coping strategies to deal with the annoyance and physical impact of ongoing noise exposure.2
In addition, WHO and recent research have highlighted that an estimated 1 billion young people are at risk of hearing loss resulting from unsafe listening practices, primarily from prolonged exposure to high volumes on personal audio devices and loud environments such as
concerts and clubs.3 This risk affects people in the age range of 12 to 35, with factors such as volume intensity and listening duration contributing significantly to potential hearing damage. For the purposes of this article, we’re focused on children’s and teens’ typical noise exposure and ways to prevent noise-induced hearing loss because once hearing is lost, it cannot be restored.
Fireworks, gunfire, and concerts are examples of commonly understood loud events. And some recreational events, such as professional football games, where crowds can pump up the noise to root for their team, are even louder than we’d expect. Would you believe, during a 2014

“Would you believe, during a 2014 home game for the Kansas City Chiefs vs. New England Patriots, a Guinness World Record was set with crowd noise recorded at an astonishing 142.2 dBA?”
home game for the Kansas City Chiefs vs. New England Patriots, a Guinness World Record was set with crowd noise recorded at an astonishing 142.2 dBA? That’s the same volume as a jet engine, which can cause immediate and irreversible hearing damage depending on one’s distance from the sound source. Less obvious loud environments include restaurants, grocery stores, and public transportation. Loud environments specific to children include recreational sports games, birthday parties, pep rallies, and cafeterias.
But how loud is too loud? The Occupational Safety and Health Administration (OSHA) established criteria to safeguard against noise hazards in the workplace for adults. Noise exposure is driven by a time intensity formula: For every 5 dB (decibels) the sound increases, the recommended time in that environment is reduced by half. So, for example, if someone is operating work-related equipment with noise averaging 90 dB, the Permissible Exposure Level (PEL) should be no greater than 8 hours TWA (time weighted average) without appropriate hearing protection.
In contrast, it’s worth considering that other organizations, including the
National Institute for Occupational Safety and WHO, use the 3 dB rule, reflecting a doubling of sound energy with every 3 dB increase, which is considered more protective.
As evidence of the negative impacts of unsafe listening levels grew, WHO created a Safe Listening initiative to encourage children and adults to limit their daily noise exposure from personal listening devices. The formula utilizes decibels (loudness), time (how long), and frequency (how often) to establish guidelines to lower the risk of noise-induced hearing loss. WHO determined that safe listening is defined as follows:
• Adult safe listening: Total of 40 hours per week at no greater than 80 dB
• Pediatric safe listening: Total of 40 hours per week at no greater than 75 dB
A sound-level meter is the gold standard for measuring sound in a particular environment. OSHA first considered measuring sound to keep individuals safe from hearing damage in the work environment. Now, with easily accessible technology, we
can measure sound in any given environment.
Apple iPhone (with iOS 15 or later) and Apple Watch (Apple Watch Series 4 or later) allow users to quickly analyze the ambient noise level in an environment with the push of a button, and users can set automatic warnings for when the sound level is dangerously loud.
Apple’s Noise app is denoted by a yellow ear. The app automatically alerts the user when the environmental sound is higher than 90 dB for a duration of three minutes. At this concerning level of ambient noise, a notification pops up saying “Loud: Repeated, long-term exposure to sounds above 80 dB can lead to permanent damage. Consider using hearing protection or moving to a quieter area.” Users can set the alert threshold to loudness levels between 80 dB and 100 dB.
Sound Level Meter (SLM) apps are available for Android and older Apple devices that help determine a safe listening environment:

• Decibel X (Apple and Android devices)
• Decibel Pro (Apple and Android devices)
• NIOSH Sound Level Meter (SLM) (Apple devices)
• SPL Meter (Apple devices)
• Sound Meter and Dose Detector (Android devices)
• Too Noisy (Apple and Android devices; web version available)
These apps measure the sound of a particular environment in real time, and although these smartphone
technologies do have some limitations, they give the user a general estimation of whether the environment warrants wearing hearing protection or other modifications to protect hearing.
The Apple Noise app and other SLM apps can also calculate the user’s weekly noise exposure to determine whether they are at risk for hearing loss. The Too Noisy app was designed to measure classroom noise. With visual interfaces, this technology gives students feedback on the sound level so they can create safe listening and learning environments.
The concern lies not only in repetitive loud noise exposures but also with single-impulse noise exposures. Depending on where you live, your child may be exposed to certain daily environmental loud sounds. For example, if you live in a city with public transportation, your child may be exposed to the city’s sources of high-volume sound, whereas children who live in rural settings may be exposed to loud farm equipment.
Events with crowd noise, for example, concerts and sporting
events, and even places of worship should raise flags and be where you monitor environmental sound. Closely monitor the volume levels your child or teen experiences on their personal listening devices with headphones when they use them for school and recreation. Indoor and outdoor household noise such as vacuums, hand dryers, blenders, blow dryers, and lawn equipment should also prompt you to move your children away from the sound source. Toys, especially toys for babies, also produce louder-than-desired noise exposures.
Although we can’t remove all sources of daily noise pollution from our children’s lives, using SLM technologies, reducing overall volume, and using hearing protection in noisy environments can help mitigate the cumulative impact of noise exposure on younger people. Increasing children’s and adolescents’—as well as their parents’ and caregivers’— awareness about the impacts of noise can help create safe listening habits and prevent noise-induced hearing loss and tinnitus in children and teens.

Rebecca Kane received her AuD from James Madison University, Va., in 2007. She was the lead in establishing the Duke Tinnitus Clinic, connected with the Duke Medical Center in Durham, N.C., where she worked for 13 years. She has presented on electrophysiology, tinnitus, and hyperacusis at various local and national conferences. Her publications have focused on utilization of an integrative medicine approach for tinnitus management. She currently provides remote support for tinnitus patients in her role as a Tinnitus Advisor for the American Tinnitus Association.
References
1. Centers for Disease Control and Prevention. (n.d.). Preventing noise-induced hearing loss. Retrieved from https://www.cdc.gov/hearing-loss-children/ about/preventing-noise-induced-hearing-loss.html
2. M. Basner, W. Babisch, A. Davis, M. Brink, C. Clark, S. Janssen, & S. Stansfeld. (2014). Auditory and non-auditory effects of noise on health. Lancet, 383(9925), 1325–1332. https://doi.org/10.1016/ S0140-6736(13)61613-X
3. L. K. Dillard , M. O. Arunda , L. Lopez-Perez, et al. (2022). Prevalence and global estimates of unsafe listening practices in adolescents and young adults: A systematic review and meta-analysis. BMJ Global Health, 7, e010501.
4. World Health Organization. (n.d.). Make listening safe. Retrieved from https://www.who.int/ activities/making-listening-safe
5. National Institutes of Health. (n.d.). It’s a noisy planet: Protect their hearing. Retrieved from https://www.noisyplanet.nidcd.nih.gov/


WHO’s “Make Listening Safe” and the National Institutes of Health “It’s a Noisy Planet: Protect Their Hearing” are public awareness campaigns that provide guidance on preventing noise-induced hearing loss and creating safe listening habits in children and adolescents.4,5 They offer these recommendations that you can teach your children:



Target a volume of 75 dB or lower or approximately 60 percent of the maximum volume on personal audio devices.
Avoid standing directly next to speakers.
The highest level of attenuation (reduction) or the highest noise reduction rating (NRR) of hearing protection is 33 dB with earplugs (in the ear) and 31 dB with earmuffs (over the ear), meaning these forms of hearing protection can reduce environmental noise by these levels. Combining earplugs with earmuffs provides a maximum attenuation of 36 dB. Hearing protection products advertise the NRR on the outside of the packaging. Typically, the higher the noise reduction rating, the more expensive the hearing protection.
Proper fit of hearing protection is the most important factor when choosing which style may be best for your child. Difficulty arises with earplugs in children because their smaller ear canals make a proper fit challenging. A child using earplugs will almost always require an adult present to help with proper insertion, whereas a child can quickly and easily put on earmuffs. Another factor to consider is that a

child’s ear canal is still growing, so an earplug that may fit one day can be quickly outgrown. Earplugs are not recommended for children younger than 12.
If your child is a musician with frequent noise exposure, custom hearing protection with musicians earplugs may be appropriate. To fit musicians earplugs, an appointment with an audiologist is required to take custom earmolds of your child’s ear canal. A variety of attenuation filters are available depending on your child’s musical needs.
Noise-canceling headphones reduce external sound so that the user is less likely to turn up the volume to hear over outside noises.
Volume-limiting headphones max out at 85 dB, which removes the user’s ability to turn up the volume to concerning loudness levels. This additional layer of protection can give parents peace of mind even when children are tempted to play with volume controls.

Noise exposure is cumulative, and taking breaks from loud environments gives sensory receptors time to recover.
5 in 10
young people (like you) listen to their music or other audio too loudly
https://www.nidcd.nih.gov/news/multimedia/listen-up-protect-your-hearing
4 in 10
young people (like you) are around dangerously loud noises during events like concerts and sports game
48 million people in the U.S. have trouble hearing with one (or both) of their ears

By Dustin Godwin, LMSW
Approximately 17 years ago, I was hit in the head by a softball. Because of the errant throw of an overeager beer league softball player, I have not known silence ever since. For 13 of those years, my tinnitus was manageable. At best, I didn’t know it was there. At worst, it was like the night after a concert. When everything was absolutely quiet, and I concentrated really hard, I could hear a dull, high-pitched ringing. If anything, it was amusing (shame on me for ever having that thought).
In November 2020, my mild case of tinnitus was exacerbated by COVID-19. It became a loud siren 24/7 for approximately four months. Since then, my tinnitus has quieted;
however, it never fully came down to the level it was before that.
I’ve put a lot of hard work into getting better, and truthfully, I’m a much better person now. Tinnitus forced me to change my way of life. I had to get healthier: mind, body, and soul. I began to eat and drink healthier. I limited my alcohol, caffeine, and sugar intake. I started working out, meditating, and praying regularly. I utilized cognitive behavioral therapy. (If you’re struggling, find a therapist and learn coping skills, which may include cognitive behavioral therapy, Acceptance and Commitment Therapy, and mindfulness.) To put it in the simplest of terms: I incorporated more positive things and separated myself from more negative things.
When I first became aware that my tinnitus was going to be a problem,
I took to the internet. (Most of you already know where this is going and this was a bad idea.) All I saw was “no cure” and something along the lines of “welcome to hell” from many tinnitus support groups.
When I saw my ENT, he said, “You just gotta relax.” Keep in mind, I was going through the worst time of my life, and the specialist that I was begging for help said, “Take a bath with some lavender or something.” It was all I could do not to lash out.
I had tests done on me by a neurologist. I’ll never forget the expression on her face when I told her how upset I was that she didn’t find a tumor (or some other ailment). She couldn’t understand why I’d ever hope for something like that. I had to explain that I needed to find something
tangible, something real, to explain why I was living in hell.
The details are different, but the story remains the same for all the other specialists I saw (audiologists, a psychiatrist, priests, etc.). I never truly stepped down from the ledge (figuratively, but nearly literally) until I heard, “I know what you’re going through. It’s hard. I know it doesn’t seem like it right now, but you’re going to be okay, and I’m going to help you.”
The problem with tinnitus, among many things, is that we hear (pun intended) too many horror stories and not enough success stories. Well, here’s mine: tinnitus nearly ripped my life apart. Every day was a fight for survival. I feared the nighttime, because it meant struggling and begging for just a few hours of sleep. Depression, anxiety, insomnia, stress, and paranoia were constant for me. I started thanking God for the life that I had but knowing that I couldn’t go on like this.
One morning, you might wake up and find that your tinnitus is completely gone; unfortunately, that’s not what happens most commonly. What happens is it consumes you, with no end in sight. Then, you slowly learn to live with it. Then, you slowly learn to let it motivate you. Finally, you slowly forget that it’s there (which is what we call habituation). For me, it didn’t happen overnight, but my tinnitus did improve.
If you take anything from this, let it be that I know what you’re going through is hard. I know it doesn’t seem like it right now, but you’re going to be okay.
“In my darkest times, ATA staff and their tinnitus advisors helped me understand that there’s light at the end of the tunnel and life wasn’t always going to be like this. I want to be that person for someone who is in the same situation that I was in four years ago.”
I look back on the darkest time of my life—I barely made it out, and that was with the love and support of my family and friends, savings to allow me to quit my job (and inevitably, make a career change), insurance to help with medical bills, and access to technological resources (including but not limited to sound machines, earbuds, and internet-capable devices to help with research). I can’t imagine trying to make it through without those tools at my disposal. I pray for others struggling with tinnitus, particularly those without the funds, resources, and support that I had.
Because of my personal experience with tinnitus, I made a career change from working in finance to working as a mental health therapist. I want to devote my life to being happy and helping others find happiness. Everyone experiences trauma in one form or another, and it’s important for them to know that they’re not alone, and people are there to help.
This is why I volunteer for the American Tinnitus Association. In my darkest times, ATA staff and their tinnitus advisors helped me
understand that there’s light at the end of the tunnel and life wasn’t always going to be like this. I want to be that person for someone who is in the same situation that I was in four years ago.
So, if you’re struggling, reach out. People are here to help. If you’ve overcome the negative side effects of tinnitus, share your story—you may save a life.

Before becoming a licensed master social worker, Dustin Godwin spent more than 10 years in the banking industry building client relationships. In 2024, after completing his master’s degree in social work at the University of North Carolina at Charlotte, he returned to Missouri with his wife, newborn baby girl, and dog. Today, he’s a therapist at Sandhill Counseling & Consultation, where he specializes in therapy with adults, adolescents, and couples, helping them reach their goals by utilizing a strengths-based approach and cognitive behavioral therapy skills.
Outside of work, he enjoys time with his family and friends, volunteering for the American Tinnitus Association’s peer support network, being outdoors, reading, attending concerts, visiting local breweries, and watching sports.

By Juan Vasquez, AuD, and Marc Fagelson, PhD
The American Tinnitus Association and Texas Roadhouse teamed up in August at the Kentucky State Fair to advance a mission that strives to make a profound and lasting impact on hearing conservation and tinnitus prevention among music industry professionals. For Texas Roadhouse, this mission reflects its commitment to community and the legacy of their founder, Kent Taylor, an avid
music fan and licensed songwriter who struggled with severe tinnitus. For ATA, it provided a valuable opportunity to connect with music industry professionals who often face challenges accessing healthcare in general, and hearing healthcare in particular. By gaining insights into their specific needs, the ATA team offered targeted hearing conservation advice, including resources on sound level awareness, hearing health status, and access to custom ear protection, all
essential for preserving and protecting the hearing of music industry professionals.
Just outside downtown Louisville, Ky., ATA staff and the audiology team, consisting of Juan Vasquez, AuD, Marc Fagelson, PhD, and audiology student Brynne Stevens, met at the fairgrounds, where they worked behind the scenes for three days at the Texas Roadhouse Stage of the Kentucky State Fair. There, music industry workers were invited to have
a conversation with the team to get more insight on their ears and hearing.
Conversations considered practical solutions and centered on the risk of acoustic overexposure, specific listening needs, tinnitus and hearing loss prevention strategies, and hearing protection device options. Because custom hearing protection and in-ear monitors are valuable tools for these professionals, the clinicians also made earmold impressions on location.
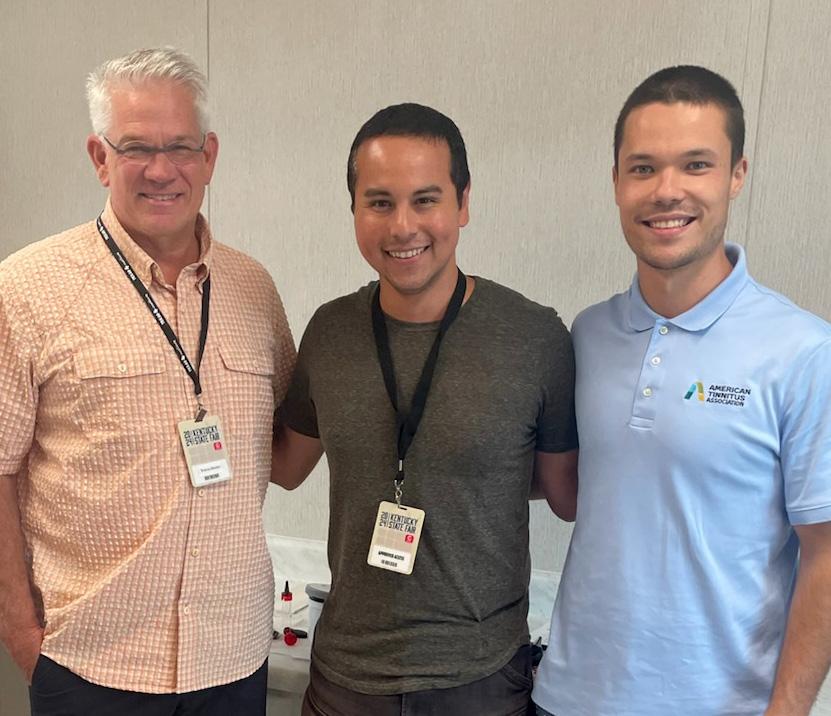
Music audiologists are niche hearing healthcare providers. They recognize that the music industry population hear and use their ears differently from other people. Generally, this population, which includes stage performers, musicians, sound engineers, backstage crew, audiovisual personnel, security, and service workers, requires substantial listening effort for extended periods of time in loud environments. The amount of sound exposure can pose a hazard to their health and well-being in both the short and long term.
Music industry professionals are in a line of work that is not regulated with safety standards like other occupational industries are, despite spending much of their work time in loud environments. Recognizing
the population’s risk of hearing injury and the difficulty they might have accessing a traditional clinical setting because of their work schedules, musician audiologists typically are committed to bridging this gap.
Although music audiology might seem glamorous at first glance, it takes a certain type of personality to work in the field, which is why having a student intern involved was a priority. Brynne Stevens, a third-year audiology student at Washington University in the St. Louis School of Medicine, joined the event to further her skills in musician hearing healthcare, hearing conservation, and tinnitus management.
“It was extremely rewarding to receive hands-on experience,” said
Stevens, adding that the event highlighted how local outreach empowers individuals to advocate for the health of their ears and overall well-being. “I’m grateful for the opportunity to learn from such experienced professionals and excited to see how this mission will expand in the coming years,” she said, noting that events like this are crucial for normalizing hearing healthcare for musicians.
Traditional hearing loss prevention or hearing conservation approaches are not always implemented or accepted by this population for a variety of reasons, including their specific and demanding listening or communication needs. Generic hearing protection, for instance, alters the sound quality of music, which changes the way music professionals use their ears for work. In-person directed conversations, on the other hand, enable music audiologists to provide options and strategies that are appropriate and useful for these professionals.
Another challenge of providing audiological services to this population is that on-site services are often limited, as they are provided in loud or uncontrolled spaces. This was certainly the case for the team
at the Kentucky State Fair, who primarily worked in a dressing room backstage. Nevertheless, counseling opportunities allowed the team to emphasize the importance of understanding one’s hearing profile and the benefits of annual hearing checks.
The team addressed the audiology testing component by providing another resource for this population, TunedCare, which is a tele-audiology platform that offers personalized consultations and services including a hearing screener and access to a music audiologist. These services are funded by the charitable arm of the Recording Academy known as MusiCares. Music industry professionals interested in checking their eligibility for MusiCares benefits can use the following link: https:// www.tunedcare.com/musicares
At the Kentucky State Fair, the team shared the idea that when a music industry professional takes steps to prevent potential hearing injuries, they have the opportunity to not only reduce the possibility of their own future suffering and hopelessness, but they may also extend their career in the music industry, and as a result, continue sharing, or supporting those who share their art with the rest of us. Their self-care is part of a pathway that enriches the lives of their audiences.
Although not all music industry professionals will acquire musicinduced hearing disorders (MIHDs), such hearing disorders have the potential to shorten careers and affect mental and physical well-being. The music audiologist introduced the idea that industry professionals should better understand the importance of hearing loss prevention because those exposed to hazardous sound levels associated with music have been, and always will be, prone to developing MIHDs.
As we look to the future, ATA, Texas Roadhouse, and this team of audiologists hope to expand our voice by providing more extensive services to music industry professionals. Plans are underway to offer more comprehensive audiometric evaluations on-site at venues and events throughout the U.S.. We will also continue to prioritize education and counseling for individuals dealing with tinnitus and other music-induced hearing disorders.
But our work doesn’t stop there— each new event offers an opportunity to advocate for and normalize the awareness of hearing health in the music industry. By building on the momentum of this year’s efforts, we aim to ensure that musicians can protect their most vital instruments— their ears—so they can continue inspiring us with their music for years to come.

Juan Vasquez is an audiologist based in Chicago, Ill. Before pursuing a career in audiology he taught, recorded, and performed music with various ensembles and as a solo artist. In 2019, he earned a Doctor of Audiology degree from Pacific University and has had various experiences in ENT, Veterans Affairs, Department of Defense, private practice, research, and hospital settings. Currently, his clinical focus is centered around hearing loss prevention, particularly for musicians. Utilizing the telehealth services, Juan provides virtual consultations for hearing wellness. He also coproduces the show Talking Ears, a podcast that focuses on music creators and their experiences with what is perhaps their most important instrument - their sense of hearing.

Marc Fagelson, PhD, is a professor of audiology at East Tennessee State University. He received a BA in English and MS in audiology from Columbia University, and his PhD in hearing science from the University of Texas at Austin.
In 2001, he opened the James H. Quillen Veterans’ Affairs Medical Center (VAMC) Tinnitus Clinic that now enrolls more than 1,300 patients.
Dr. Fagelson co-edited with Dr. David Baguley two texts published by Plural that center on tinnitus and disorders of sound tolerance. He also collaborated with Dr. Suzanne Kimball on the Tinnitus and Hyperacusis Casebook, published by Thieme in November 2021. He has more than 50 publications and has given more than 100 conference and workshop presentations. In July 2023, Dr. Fagelson was voted to chair the American Tinnitus Association’s Scientific Advisory Committee.


By Joy Onozuka
Pro bass angler Mike Delvisco looked out at Douglas Lake, Tenn., following the 2nd Annual CelebrityPro Am Fishing Tournament, and pondered, “How can we have greater impact?” It was a question posed after a breathtaking acoustic tinnitus awareness concert, successful raffle, and an exciting half-day fishing competition, which raised almost $16,000 for the American Tinnitus Association.
“That’s Texas Roadhouse culture,” said Mike, who has been sponsored for more than 20 years by Texas Roadhouse, the nationwide (and international) steakhouse, which was founded by Kent Taylor in 1993. “Let’s think about how to grow this, make it better, and have fun while doing it,” Mike said smiling. The two-day tinnitus awareness and fundraising event benefiting ATA and honoring Kent, who struggled with severe tinnitus, was launched in 2023 by Mike and his
wife, Brandie. “When you start talking about tinnitus, it’s amazing how many people say they have it,” Mike noted. “What they often don’t know is that ATA is a resource where you can get help.”

For this year’s tournament, there were 19 boats—up from 13 last year—captained by a professional angler, and a celebrity paired with an amateur who had placed the winning bid to join a particular boat. Country music celebrities who performed and fished in the tournament included Wade Hayes, Michael Ray, Scott Smith of Smith & Wesley, Tony Justice, and rising star Connor Hicks, among others. All of them—through years of playing music—grasp the significance of tinnitus and its ability to change the trajectory of someone’s life.
Ray credited older musicians who shared their experiences with tinnitus and a sound engineer who introduced him to in-ear monitors for enabling him to limit hearing damage and prevent tinnitus. But that awareness and shift in playing happened years after performing and practicing with no hearing protection. “[As a younger musician,] I thought ringing in the ears
at the end of the show meant you had a good show, not realizing how this can affect you.” He noted that, although music industry awareness about tinnitus is better today, not everyone understands the wideranging impact tinnitus can have or where to get help.
This year’s event also had the support of Matt and Hanah from Knoxville radio station Wolf 100.3 Matt, who has a brother living with tinnitus, emceed the concert, and Hannah served as the announcer for
each of the teams as they brought up their catch to be weighed before releasing the fish back into the lake. They, like many other participants, have already signed on for next year’s concert and tournament, which is scheduled for August 27 and 28.
“Mike and Brandie—like everyone else who came together the last two days—symbolize the power of community and our ability to effect change,” said Patrick A. Lynch, ATA CEO, who joined a boat and spoke to help deliver the message that

tinnitus must be silenced. “Every individual matters and ATA is here to serve, to offer meaningful hope through education and support, and to, ultimately, cure tinnitus. It’s a mission that can only be achieved through ongoing engagement, fundraising, research, and events that resonate across a wide audience. I look forward to being here next year,” said Patrick, echoing the sentiments of many other participants. Stay tuned for upcoming events.




Title: The Progressive Tinnitus Management Book: Step-by-Step Through the Five Levels of PTM
Author: James A. Henry, PhD
Publisher: Ears Gone Wrong, LLC
Number of pages: 298
Paperback ISBN: 978-1962629072
By Cheri R. Ribbe, AuD
For the millions of people with tinnitus, from slightly bothersome to highly distressing and anywhere in between, it can feel scary and overwhelming when searching for reliable information. Most often, people turn to the internet and find themselves down a rabbit hole of unending misinformation that can lead to unnecessary expense for devices or supplements that claim to “cure” tinnitus. Or they talk to their primary healthcare provider, who may not know what to say or how to help, which leads to discouragement and additional anguish.
But if you are like me, when something feels overwhelming and I need practical answers, I look to the experts, and to my bookshelves. One expert in the area of tinnitus research and patient care is James Henry, PhD, a research career scientist and a pioneer in the management of tinnitus.
When I heard Dr. Henry was retiring from his distinguished career with the U.S. Department of Veterans Affairs at the National Center for Rehabilitative Auditory Research in Portland, Ore., where he’d amassed hundreds of publications, research studies, and
awards for his work on understanding tinnitus, its effects, and its treatment, I was concerned that his crucial voice in the field would be lost.
Therefore, I was quite happy to see that his quest to keep educating as many people as possible has continued with his latest publication, The Progressive Tinnitus Management Book. This is the third book in Dr. Henry’s series published by Ears Gone Wrong®, LLC.
Dr. Henry’s book explains in simple terms what Progressive Tinnitus Management (PTM) is and is chock full of user-friendly figures, test-your-knowledge quizzes, tables, questionnaires, website links, and references for the clinician and the lay person.
He dives into the PTM protocol that is based on decades of research, much of it led by Dr. Henry himself. Randomized controlled trials have provided the outcomes necessary to build the foundation for treatment plans that help people improve the quality of their life while living with tinnitus. Dr. Henry provides the reader with clinical tools, materials, and guidance in an effective and efficient manner, saving you time, money, and confusion.
As in his previous two books, Dr. Henry introduces the case studies of relatable people, which in this book are Allessia and Dimitri, and how they are guided through individualized PTM plans for self-care and management of their tinnitus. These are two people with varying tinnitus needs. Dr. Henry takes the reader on the step-by-step journey to managing their tinnitus.
The five levels of PTM—Referral, Audiology Evaluation, Skills Education, Interdisciplinary Evaluation, and Individualized Support—are described in an easily understood format. A patient only progresses to the level of PTM that is needed to feel that selfmanagement has been achieved.
Level 1, Referral, is when a healthcare provider, who may be the first person a tinnitus patient encounters, refers the patient to specialized help. Healthcare providers are instructed on how to effectively assess and refer patients with tinnitus. No longer should healthcare providers tell patients, “You need to learn to live with it” and stop there. In the book, Table 5-1 provides an easy guide for providers on what to do and how to refer appropriately.
Level 2, Audiology Evaluation, encompasses the audiological
assessment. Ninety percent of those with tinnitus also have some degree of hearing loss or auditory dysfunction. In addition to a comprehensive hearing test, an educated provider can administer tinnitus questionnaires, answer frequently asked questions, and counsel on basic tinnitus education and strategies to allay the patient’s fears.
As a clinician myself, I highly recommend the Tinnitus and Hearing Survey (THS), shown in Figure 6-1 of the book. The survey quickly shows how much of the patient’s problem is due to tinnitus versus hearing loss versus sound hypersensitivity. The THS then guides the conversation and the counseling toward whether the person may need or want Level 3 Skills Education services specific for tinnitus management. This can be done concurrently with recommendations of hearing aids and assistive devices if needed.
Unfortunately, many healthcare providers think of tinnitus as only an audiology concern or an ear condition. Yet, I commonly hear from patients, “When I’m stressed, anxious, or tired, my tinnitus feels worse and sounds louder, and when my tinnitus is worse,
“…if you are a person with tinnitus, this book is a guide for you to achieve selfmanagement to the level you require for relief, taking it one step at a time. ”
I feel more stressed and anxious.” And so the vicious cycle begins.
Dr. Henry and his colleagues realized that to address this cycle, PTM needed to include audiologistled services in the form of sound therapy and cognitive behavioral therapy (CBT) services led by a behavioral health provider. CBT is one of the most researched methods for tinnitus management, and for efficiency’s sake, PTM focuses on three areas of CBT: stress reduction, distraction techniques, and cognitive restructuring.
I recommend reading this book from the start to understand the foundation of PTM at Levels 1 and 2, particularly for clinicians. However, if you are a reader who would like to thumb to the heart of the Level 3, Skills Education, Part 3 provides details on decision-making for the step to Level 3, Skills Education, and guides readers through developing a personalized Sound Plan and tracking progress on the Changing Thoughts and Feelings worksheet. The Sound Plan is developed by teaching the uses of sound in three ways: soothing sounds to induce relaxation and therefore reduce reactions to tinnitus; interesting sounds to distract and shift focus away from tinnitus; and background sounds for the goal of habituation to the tinnitus, or helping the brain better ignore the tinnitus.
Table 9-1 provides a nicely formatted graph of the sound therapy goals. The Changing Thoughts and Feelings worksheet develops a plan for using relaxation techniques and planning pleasant activities while tracking your changing thoughts associated with tinnitus.
The next step, Level 4, if needed, is Interdisciplinary Evaluation. The audiologist and the therapist, along with the patient, can consider the following questions:
1. Does the person need to focus more on the audiology skills of sound therapy?
2. Do they need to focus on CBT skills and perhaps add third-wave CBT in the form of mindfulness or Acceptance and Commitment Therapy?
3. Do they need both?
The answers to these questions lead to the next and final step in PTM, Level 5, Individualized Support, which is a unique plan to meet an individual’s needs.
Dr. Henry’s books provide the clinician and the person affected by tinnitus an opportunity for a successful outcome. Dr. Henry states that he cannot claim PTM is more effective than other methods, but I can
personally and professionally attest to the countless people I have been able to guide through the five levels of PTM and the overwhelming positive impact it has had on them.
This book never feels too wordy, never goes too far off in the weeds with research and terminology. It is simple and straightforward and is filled with information based on research and clinical implementation. Clinicians and readers with tinnitus will learn that tinnitus needs to be managed differently for each person. What works for one does not necessarily work for another.
If you are a clinician, the beauty of PTM is that it provides a manageable framework and valuable clinical tools that you can apply in any setting to begin helping your patients today. And if you are a person with tinnitus, this book is a guide for you to achieve selfmanagement to the level you require for relief, taking it one step at a time.


Cheri R. Ribbe, AuD, has been a clinical audiologist for 29 years, including 23 with the Veterans Health Administration, where she is currently the assistant chief of Audiology & Speech Pathology Service at VA Central Western Massachusetts (CWM). She ran the Progressive Tinnitus Management (PTM) program at VA Boston from 2009 to 2016 and continues the program at VA CWM. She served as a member and author for the 2015 Adult Tinnitus Management Clinical Practice Recommendations for VA providers.
She has been a guest presenter at national conferences as part of a panel of PTM subject matter experts, and in 2017 she coauthored the study “Progressive Tinnitus Management Level 3 Skills Education: A 5-Year Clinical Retrospective.” Serving our nation’s veterans in their healthcare journey continues to be her greatest honor.
Every day, people struggling with tinnitus turn to personal stories to understand what the future might hold. The stories are honest and don’t sugarcoat the challenges and time it often takes to learn how to manage and live with tinnitus.
If you have tinnitus and/or other sound tolerance disorders, we’d like to hear from you. Please send your story to editor@ata.org by January 30. Suggested word length is between 600 and 1,000 words.

By Joy Onozuka
If you’ve ever seen a physician about tinnitus, you were likely referred to an audiologist for a hearing exam because 90 percent of individuals with tinnitus have some degree of hearing loss, and use of hearing aids to address that loss can reduce tinnitus perception. For individuals with tinnitus and mild hearing loss, the suggestion to wear hearing aids can be jarring.

as hearing conversations in noisy environments, hearing soft sounds, or hearing streaming video or phone calls, but why invest thousands of dollars in a technology associated with old age?
Yes, hearing aids may reduce tinnitus perception and help with certain communication issues, such
That thinking is shared by countless people with hearing loss, who often delay trying hearing aids for many
years. Apple hopes to change that through its second-generation AirPods Pro 2, which received FDA authorization as the first over-the-counter hearing aid software device this fall.
Already in the hands and ears of millions of people in the United States, second-generation AirPods Pro 2, priced at about $250, enable users to explore their auditory health beginning with a validated airconduction hearing test. Shortly after Apple received FDA authorization, ATA attended a briefing to learn more about the company’s growing suite of
hearing-focused product features and research collaborations.
The overview outlined how products, evolving technology, and the company’s focus on inclusion, which is informed by its accessibility team, shaped Apple’s foray into the hearing health space. The spokesperson also stressed that Apple adheres to three core principles for all of its products’ health features:
• Features must be science based.
• Information must be actionable and paired with education so users are informed, not scared, by notifications and links to additional information.
• Features must protect privacy, meaning users have control over their data.
It was the development of the H2 silicon chip that brought Apple to the intersection of listening and hearing health. That technology made it possible for Apple to optimize users’ listening experience across a wide spectrum. Apple’s health, acoustic, and accessibility teams came together to focus on next steps in the hearing health space.
The group landed on prevention, which would home in on protection tools; awareness, which would involve hearing tests; and assistance, which would provide aid in hearing. These initiatives prompted the teams to question whether first-generation AirPods, released in 2016, could be used as a personal sound amplification product (PSAP). PSAPs are consumer electronic products capable of amplifying sound.
“A significant portion of participants [in the Apple Hearing Study] with hearing loss did not use hearing aids, and nearly 40 percent had not had a professional hearing test in over a decade.”
With the congressional passage of the Over-the-Counter Hearing Aid Act of 2017, which directed the FDA to establish a category for OTC hearing aids to make it easier for adults with mild to moderate hearing loss to purchase hearing aids without a prescription, Apple was further thrust into the hearing health space. As an emerging health company, it had to learn to conform products to federal regulations and consider software as a medical device on top of commercial hardware.
Drawing on Apple Watch technology, Apple implemented a feature that could tabulate a rolling dose of noise exposure, from hour to day to week to month to year. The rollout of the first-generation AirPods Pro included a transparency mode feature, which enabled users to hear sounds from their environment while still using the earbuds to listen to music, podcasts, or talk on the phone. The external microphones capture ambient sounds and play them back through the earbuds along with whatever sounds the user is streaming. This feature
enables users to remain aware of their surroundings, which is especially valuable in situations like biking on a street, running on a trail, walking in busy areas, hearing announcements, or engaging in conversation without removing the AirPods Pro. The pro version of the devices also included Conversation Boost, which provides users who have mild hearing loss slight amplification in noisy environments. By leveraging the H2 chip and transparency mode, the AirPods Pro could also be used as hearing protection. Because of the negative impact of hearing loss, the feature is automatically turned on and provides active attenuation up to 110 dB. The silicone ear tips come in four sizes to accommodate different ear shapes, ensuring they fit properly. A correct fit is essential for the ear tips to provide adequate hearing protection.
In November 2019, Apple, in collaboration with the University of Michigan’s School of Public Health, embarked on the Apple Hearing Study, which has become the world’s largest longitudinal hearing study. Utilizing
the Apple Research app, investigators recruited 160,000 participants, who voluntarily provided deidentified data from various health-related metrics, such as headphone usage and feedback on hearing-related issues, including tinnitus. The study, which is scheduled to last 10 years, was expanded to include an additional 140,000 participants, with recruitment taking place now.
Initial findings reveal that about 77.6 percent of study participants reported experiencing tinnitus at least once, with 15 percent experiencing it daily. Tinnitus prevalence increases with age, and for those 55 years and older, daily tinnitus becomes three times more common. Additionally, about 10 percent of participants reported that their tinnitus interfered with their ability to hear clearly.
The study also categorized tinnitus experiences, with many participants describing their tinnitus sound as a
A self-administered hearing test is a quick and convenient first step in assessing your hearing, but it’s only part of the picture. The screening provides an initial indication, not a full diagnosis. Also, earbuds used to address mild to moderate hearing loss block the ear canal, which may feel unnatural or awkward for some users. For a complete understanding of your hearing and listening needs, it’s essential to follow up with a licensed audiologist who can provide a thorough evaluation and personalized care.
pure tone or as white noise. The study aims to characterize these experiences to inform potential future management techniques. By collecting comprehensive lifestyle and environmental data, researchers are working to understand which demographics are most affected.
Additionally, the research findings emphasize the gap in hearing support: A significant portion of participants with hearing loss did not use hearing aids, and nearly 40 percent had not had a professional hearing test in over a decade. These statistics underscored the need for broader awareness around hearing health and preventive measures, such as regular hearing screenings and early adoption of hearing support devices.
To access Apple’s Hearing Aid Feature in the second-generation AirPods Pro 2, users, who must be 18 years or older, take a clinical-grade air-conduction hearing test, which takes about five minutes to generate an audiogram. If you have mild to moderate hearing loss, the hearing aid features can be activated or turned off. The Apple spokesperson acknowledged that the pure-tone
test is only one component of a comprehensive hearing assessment. Nonetheless, it is easy to understand, repeatable, and provides next steps, which Apple hopes will result in people seeing a licensed audiologist for a more comprehensive exam.
As with other Apple health initiatives, the company hopes that its hearing tools will break down barriers so that people have conversations with family, friends, and their healthcare providers using the correct vocabulary for what are very common problems—hearing loss and tinnitus. For this reason, the spokesperson said Apple isn’t dodging the use of the term hearing aids to describe this product feature.
With increased accessibility to over-the-counter hearing aids for moderate to mild hearing loss and the first round of results from the Apple Hearing Study and its tinnitus report, Apple could be the catalyst that enables hearing healthcare providers, associations like ATA, and policymakers to promote preventive strategies that resonate with a public newly attuned to its auditory world— and this would be a joy to hear.

By James A. Henry, PhD, and Hamid Djalilian, MD
A classic migraine headache is experienced as severe throbbing pain, usually in one side of the head (unilateral). There is typically a preheadache (prodrome) phase lasting a day or two and a post-headache (postdrome) phase lasting for up to a day. The migraine attack can last from hours to days. Migraine episodes are experienced by about 15 percent of the global population.1
Importantly, migraine does not necessarily refer to a headache. “A headache can be a symptom of a migraine, but not all patients with a migraine have headaches.”2 For example, patients with two variants of migraine, known as ocular migraine
and abdominal migraine, do not necessarily experience a headache.
The symptoms of migraine are generally associated with abnormal perception of the senses—sight, hearing, smell, and touch. The symptoms can also include neck stiffness, sinus pain or pressure, dizziness, vertigo, ear fullness, and fluctuating hearing loss. Many publications are available that describe these symptoms.3-6 Here, we are focused on symptoms of tinnitus and hyperacusis (hypersensitivity to the loudness of sound).1,2,7,8 When people experience any of these symptoms without experiencing severe headaches, the symptoms are considered atypical symptoms of migraine 9
Migraine is genetic and thus a lifelong problem. “It may start in childhood and disappear and
reappear in new forms throughout an individual’s life. In general, there is a decrease in headache intensity and an increase in the incidence of atypical symptoms of migraine… as patients mature. Migraine tends to run in families, so having a relative with migraine makes it more likely that you will have migraine as well.”9
During a migraine attack, abnormal electrical activity may occur in and around the brain.9 The electrical activity results in changes in blood flow. Nerve cells have ion channels that are like little gates that allow sodium, potassium, and other elements into and out of the cells. People with migraine are thought to inherit abnormal forms of these ion channels, which “primes” them to have migraine attacks triggered by stress, hormonal changes, certain foods, dehydration

and hunger, disrupted sleep, weather changes, and intense stimulations such as loud sound. Centers in the brain that process sensory input can become “hypersensitized,” resulting in exaggerated responses to sensory stimuli.
Another causative factor of migraine is the trigeminal (fifth cranial) nerve, which transmits sensations from many areas of the head and neck, including the face, scalp, and ears.9 This nerve becomes overactive and very sensitive in migraine and releases inflammatory chemicals that can leak through blood vessels into surrounding tissues, causing them to swell and become painful. Classic migraine headache can be caused by this form of inflammation occurring in the brain, which has been referred to as neuroinflammation.
Although there is controversy (as discussed below), Ménière’s disease is usually considered to be a disease of the inner ear.10 It is also referred to as endolymphatic hydrops (endolymph is the inner compartment of fluid in the inner ear; hydrops refers to swelling of the fluid). The swelling (expansion) of endolymph can disrupt the neural signals sent into the brainstem from the inner ear, altering both auditory and balance functions.
Symptoms of Ménière’s Disease. The symptoms of Ménière’s are vertigo (spinning sensation), ear pressure or fullness (the ear feels blocked, clogged, or stuffed), tinnitus (usually a whooshing or roaring sound—like the sound of a large seashell held against the ear, or an engine), and hearing loss. These symptoms occur suddenly as
“Along with vertigo, tinnitus can be one of the most disabling symptoms of Ménière’s disease.”
episodes and without warning. Each episode lasts for about 20 minutes up to about 12 hours.4 It has been noted that the duration of these symptoms falls within the approximate time frame for migraine attacks.11
The precise cause of Ménière’s symptoms is not yet known. “It appears that although sufferers of Ménière’s disease will in all cases have at least one ear with hydrops, not every individual with endolymphatic hydrops experiences symptoms of Ménière’s disease. This finding has led to the conclusion that there must be another factor at play”4 that induces those with Ménière’s disease to develop symptoms. Endolymphatic hydrops may be the result of gradual damage to the inner ear that causes a disruption in the fluid regulation in the inner ear. This causes the accumulation of more endolymph, which is what is seen after damage to the ear.
A current theory is that Ménière’s disease may be related to restricted blood supply (ischemia) or other vascular conditions (dilation of blood vessels) that affect the delivery of blood (perfusion) to the inner ear during episodes.4 One such condition is migraine headaches (or atypical migraine attacks targeting the inner ear), “which appear to have a partly vascular component to their
manifestation and have been found in close association with Ménière’s disease.”4
Between 51 percent and 60 percent of people with Ménière’s experience migraine headaches,12 and up to 45 percent experience migraine symptoms during an episode.4 “In our practice, we have found that the vast majority of the patients with Ménière’s disease also have histories that are consistent with the presence of migraine”6 even in the absence of a history of headaches.
Ménière’s disease was named after Prosper Ménière, who was the first to describe its characteristic symptoms in 1861.3 An additional symptom he described in all his patients was migraine headaches because they occurred so frequently along with the other symptoms. He theorized that all of these symptoms had a common cause within the inner ear. This theory was studied for approximately the following 10 years, but not again until the 1960s.
It is clear that migraine can be associated with inner ear disorders that are related to the vestibular (balance) system and/or the cochlea.4,12 People may have purely vestibular symptoms, such as vertigo, motion sensitivity, and imbalance. Or they

may have purely cochlear symptoms, including tinnitus, loudness hyperacusis, and hearing loss (even sudden sensorineural hearing loss).
Migraine with primarily vestibular symptoms is considered vestibular migraine. Migraine with primarily cochlear symptoms is considered cochlear migraine. Migraine with a combination of both vestibular and cochlear symptoms is referred to as cochleovestibular (or vestibulocochlear) migraine, which may be considered the equivalent of Ménière’s disease.11 The term otologic migraine has been used as an all-encompassing term for all ear-related symptoms, including cochlear, vestibular, and ear (aural) pressure and pain.
Ménière’s Disease and Tinnitus. The association between Ménière’s disease and tinnitus is well known.13 Along with vertigo, tinnitus can be one of the most disabling symptoms of Ménière’s disease. Often, tinnitus is the first symptom experienced— preceding the other classical symptoms of vertigo, hearing loss, and aural fullness. Over time, the vertigo may be replaced with feelings of imbalance while the hearing loss progresses along with persistent tinnitus.
Early in the disease, the tinnitus is often experienced only during the vertigo attacks.13 But the tinnitus can become permanent and is commonly described as a “roaring or machinelike sound.” During the course of the disease, the characteristics of the tinnitus sound (its pitch and loudness) may change, which patients often report is a warning of an impending vertigo attack. In the last stages of the disease, the vertigo may resolve,
leaving tinnitus as the predominant symptom and main cause of disability.
Ménière’s Disease and Hyperacusis. Less well known are studies that have shown an association between Ménière’s disease and hyperacusis.14-16 Cochlear migraine and cochleovestibular migraine may both be associated with hyperacusis along with other auditory symptoms.5 Hyperacusis is not a vestibular symptom, and it would seem that vestibular migraine would not be associated with hyperacusis. However, in a study of 131 patients who met the criteria for vestibular migraine, hyperacusis was present in 90 percent of the patients during episodes and in 2.3 percent of patients between episodes.17
How can people with vestibular migraine also experience hyperacusis? Migraine is a hypersensitivity in the brain that causes peripheral symptoms based on which area of the brain is involved. Although vestibular migraine symptoms are primarily vestibular, hyperacusis can be experienced, as well, due to the brain hypersensitivity, termed central sensitivity. This would be similar to a classic migraine headache patient who experiences hyperacusis (called phonophobia by neurologists) during a headache episode.
In vestibular migraine, the peripheral (vertigo) symptoms are likely to occur as a result of a change in blood flow at the vestibular level or due to trigeminal nerve-induced inflammation in the inner ear, but the brain hypersensitivity that amplifies sound and light, and other sensory input, is still a factor. Because hyperacusis, as well as tinnitus,
ear fullness, and hearing loss, can accompany vestibular migraine, it has raised the question of whether “vestibular migraine should be termed vestibulocochlear migraine.”11
Recent systematic reviews have concluded that most studies show a strong association between migraine and tinnitus.18,19 “Although not all migraine patients experience tinnitus, many migraine patients both clinically and in our literature review report auditory (hearing related) symptoms in association with migraine, with tinnitus being one of the most common auditory symptoms.”7
A large-scale study reported that “patients with a history of migraine had a tendency to develop cochlear disorders, especially tinnitus.”2 People with migraine headache history are three times more likely to develop tinnitus during their lifetime than those without migraine.2
“An association of hyperacusis has been made with chronic migraine headaches.”5 It has also been reported that sound hypersensitivity is experienced between migraine episodes (when no headache is present) and that it worsens during the episodes.20
The migraine literature generally refers to the hypersensitivity to sound as phonophobia, which would imply a fear response. Such a label, however, is inaccurate for what has been described as feelings of “discomfort or pain.”15 Sound hypersensitivity associated with migraine could

“Avoiding triggers and making lifestyle changes to reduce stress, improve sleep, and get sufficient exercise can often be successful in reducing or even eliminating migraine attacks.”
be loudness hyperacusis, pain hyperacusis, or noise sensitivity.8
Completing a full assessment should clarify which of these disorders would be the appropriate diagnosis. Of course, phonophobia (defined as irrational fear of sound) could also be present.
Answering this question thoroughly would require a deep dive into the scientific literature. Very briefly, hearing cells (hair cells) in the inner ear (cochlea) detect sound vibrations, convert them to electrical (nerve) signals, and send those signals into the brainstem via the hearing (auditory) nerve. The first processing center (nucleus) in the brainstem is the cochlear nucleus
One theory about what causes tinnitus and/or hyperacusis is that damage to the hearing cells reduces the nerve signals being sent to the brainstem center (dorsal cochlear nucleus; DCN), thereby provoking a compensatory adjustment that can be recorded in the DCN—indeed, the DCN may overcompensate for the reduced input from the inner
ear.7 The resulting hyperactivity can create or increase the perception of tinnitus and make the auditory system hypersensitive to the loudness of sound (hyperacusis).
The DCN also receives indirect input from the trigeminal (fifth cranial) nerve.5 It is hypothesized that the hypersensitivity caused by migraine can be transmitted via the trigeminal nerve to modulate activity in the DCN.7 Further, the trigeminal nerve innervates the blood supply in the inner ear, which can cause inflammation and a change in the blood flow to the inner ear.9 Finally, there is an increase in the sensitivity of the brain after the migraine process has become active in the brain, which can amplify external sounds and lead to hyperacusis.
These connections of the trigeminal nerve to the auditory system and the increased brain sensitivity could explain why some migraine patients experience louder tinnitus and more sensitivity to outside sound. More specifically, this hypothesis could explain why tinnitus and hyperacusis can get worse around migraine attacks. This trigeminal nerve-related sensitization
may be the common factor between migraine and auditory symptoms.
The best way to treat migraine headache and atypical migraine symptoms (e.g., fluctuating tinnitus and hyperacusis) is trigger identification and avoidance 9 Patients are advised to use a migraine diary to record likely triggers that cause attacks. Avoiding triggers and making lifestyle changes to reduce stress, improve sleep, and get sufficient exercise can often be successful in reducing or even eliminating migraine attacks. Keep in mind that in some individuals, the “migraine” can manifest only as increased loudness of the tinnitus or hyperacusis. A headache is not necessary for the diagnosis of migraine.
If Ménière’s is indeed a manifestation of migraine, then people with Ménière’s can be effectively treated with therapies that are helpful for migraine.4,5 One group treated hyperacusis with a “multi-modal migraine prophylactic regimen.”16 Patients were counseled on making lifestyle modifications, including dietary changes (avoiding certain foods and dehydration), dietary supplementation (prescribed doses of magnesium and riboflavin/ vitamin B2), eating three meals, and sleeping on a regular schedule. Patients were also prescribed medications using a stepwise approach to adjust medication types and dosages based on outcomes and side effects. This treatment regimen was effective for both hyperacusis

and tinnitus, which may be explained by the many parallels that exist between the two conditions.
A recent article noted that treatment is challenging “because of the lack of evidence-based treatment and randomized controlled trials. As a result, the current treatment options for vestibular migraine rely on those used for migraine headaches.”11
In that article, the authors review abortive therapy (“to halt or lessen the severity of an acute vestibular attack”), pharmacological prophylaxis (“to reduce attack frequency and severity”), nonpharmacological prophylaxis (to manage migraine triggers), vestibular rehabilitation, and “new and emerging therapies.” They also review “treatment of other migraine-related otologic symptoms,” including tinnitus, dizziness, and sudden sensorineural hearing loss. For tinnitus, they recommend a multimodal approach including “cognitive behavioral therapy (CBT) with a potential consideration of sound therapy.”11 Internet-based CBT (iCBT) that provides education on migraine and tinnitus has been found to benefit in reducing Tinnitus Handicap Inventory
scores significantly when combined with customized sound therapy.21
Brooks and colleagues (2023) note, “In our clinical practice, we have found improvement in the fluctuation of tinnitus and reduction of loud tinnitus in patients treated with a migraine regimen and control of migraine triggers. Other keys to tinnitus management include dietary modifications such as having regular eating habits and avoiding migraine food triggers, maintaining a regular sleep schedule, gaining control over stress, and use of supplements such as magnesium and vitamin B2.”11
The cause of Ménière’s continues to be debated, as indicated by the following two quotes:
“The symptoms of Ménière’s disease are likely a manifestation of migraine rather than an independent inner ear condition.”12
“Although there is conflicting evidence regarding the cause and treatment of Ménière’s disease, current evidence favors it as a disorder of the inner ear,”10 which may be due to a central (brain-related) phenomenon.
“…It appears that for some patients, their tinnitus and/or hyperacusis may share a pathophysiologic basis with migraine disorder and may be successfully treated using migraine therapy.”
Regardless of this controversy, it appears that for some patients, their tinnitus and/or hyperacusis may share a pathophysiologic basis with migraine disorder and may be successfully treated using migraine therapy. There is still much to be learned and research is urgently needed to answer remaining questions.

James A. Henry, PhD, is an audiologist with a doctorate in behavioral neuroscience. He recently retired as a Senior Research Career Scientist at the Veterans Affairs (VA) Rehabilitation, Research & Development (RR&D) National Center for Rehabilitative Auditory Research (NCRAR) located at the VA Portland Health Care System in Portland, Ore. For most of his 35-year career, his focus was researching clinical methods of tinnitus management. In addition to providing consultation services, he is currently writing a series of books on tinnitus, hearing loss, and sound tolerance disorders, under the heading Ears Gone Wrong®, LLC.

Hamid Djalilian, MD, is a professor of otolaryngology, neurosurgery, and biomedical engineering and director of otology and neurotology at University of California Irvine (https://ent.uci.edu). He has published over 300 articles and lectured more than 200 times at national and international meetings. In addition to a busy clinical practice, Dr. Djalilian conducts research in several areas related to device and software development for treating tinnitus, hearing loss, dizziness, ear infections, among others. He is the chief medical advisor to the NeuroMedCare telemedicine clinic (https://www.neuromedcare.com) to medically treat tinnitus using the new understanding of migraine as the cause of loud tinnitus.
Complete references can be found here.

People with tinnitus at every stage in their journey, from the first few days to many years later, can benefit from membership in a support group. Every tinnitus support group operates differently; but they all share a passion for providing meaningful discussion and a caring
environment where one can be understood through shared experience. Below is a list of groups and meeting dates, current at time of print. Each support group referenced here is independently operated and led by volunteers who wish to provide education and support to the tinnitus community.
The American Tinnitus Association (ATA) does not sponsor or endorse these activities and expressly disclaims any responsibility for the conduct of any independent support group or the information it may provide. ATA is not a healthcare provider and you should consult with a primary care physician or hearing healthcare professional for qualified medical advice on tinnitus and related disorders.
*To allow for flexibility in planning, some groups do not schedule meetings far in advance. When we receive updates from support group leaders, we update meeting information on our online Events Calendar at www.ata.org . The information was provided to ATA staff at the time the magazine went to print; therefore, please confirm meeting details with the contact person prior to a meeting or reference our website at: https://www.ata.org/news/events
This is a partial listing of support groups and scheduled meetings. A complete list can be found at https://www.ata.org/ your-support-network/find-a-supportgroup/. New groups continue to be added, so please check the website for updates periodically.
If you’re interested in forming a group, please contact Joy Onozuka at tinnitus@ata.org
If there isn’t a group in your area, ATA has an extensive network of volunteers who provide email and telephone support and educational information. To connect with a volunteer in your time zone, see: https://www.ata.org/your-support-network/ telephone-support/
Support group information in the magazine and on the ATA website is provided by group leaders and is subject to change. Please contact the support group leader directly to confirm meeting information.
California
The Palo Alto Tinnitus Support Group at Avenidas Blue Room of the Avenidas Senior Center
450 Bryant St. Palo Alto, CA 94301
Contact: Ken Adler
T: 650–839–1770
E: karmtac@aol.com
3rd Thursday of the month, 5:30–7:30 pm
Colorado
Mesa County Tinnitus Support Group Community Hospital, Legacy Room 1 2351 G Rd.
Grand Junction, CO 81505
Contact: Elaine Conlon
T: 970–589–0305
E: conlonelaine@aol.com
3rd Wednesday of the month, 6:00 pm
North Denver Tinnitus Support Group
Broomfield Community Center
Overland Room
Contact: Melissa Golden
T: 303–506–9389
E: mbaycon@hotmail.com
Florida
Clermont Tinnitus Support Group
Citrus Hearing Clinic, LLC
835 Seventh Street, Ste. 2 Clermont, FL 34711
Contact: Laura Pratesi
T: 352–989–5123
E: office@citrushearing.com
2nd Monday of the month, 1:00 pm
RSVP required
Michigan
Marketplace Tinnitus Group
2020 Raybrook SE Grand Rapids, MI 49505
Contact: Robert Ellis
T: 616–949–4911
E: robe7350@gmail.com
Holland Tinnitus Support Group
Holland Doctors of Audiology
399 E 32nd St.
Holland, MI 49423
Contact: Stelios Dokianakis
Website: https://holaud.com/contact/
T: 616–392–2222
E: info@holaud.com
Meeting date and time TBD
Please email/call the point-of-contact person listed for information on upcoming meetings.
Arizona
Tucson Tinnitus Support Group
Contact: Trudy Jacobson
E: trudyj@cox.net
4th Saturday of the month, 1:00 pm Arizona residents only
California
Los Angeles/Orange County Tinnitus Support Group
Contact: Barry Goldberg
E: bargold06@yahoo.com
3rd Saturday/Sunday of the month, 10:00 am
Sacramento Area Tinnitus Support
Contact: Pat Clark
E: sactinnitus@gmail.com
2nd Wednesday of the month 6:30–8:00 pm
San Diego Tinnitus & Hyperacusis Support Group
Contacts: Michael J. Fischer, Loretta Marsh, David Phaneuf, Tom Sutton
E: michaeljohnfischer@hotmail.com
E: lorettamarsh@hotmail.com
E: djphaneuf@yahoo.com
E: tomsutton63@gmail.com
1st Tuesday of the month, 6:00–7:30 pm
Colorado
Denver Tinnitus Support Group
Contact: Rich Marr
T: 303–875–5762
E: rmarr5275@gmail.com
2nd Monday of the month, 7:00–8:30 pm
Iowa
The University of Iowa Tinnitus Education and Support Group
Contact: Julie Jeon, AuD, PhD
E: csd-audiologyclinic@uiowa.edu
2nd Wednesday of the month, 9:00–10:00 am
UMD Tinnitus & Hyperacusis
Support Group
Contact: Christina Shields, AuD
T: 301–405–5562
E: shields3@umd.edu
Meets quarterly, date and time TBD
St. Louis Tinnitus Support Group
Contact: Tim Busche
T: 636–734–4936
E: tbusche@stltinnitus.org
1st Wednesday of even months
South Jersey Tinnitus Support Group
Contact: Beth Savitch, Erin Lustik
E: tsg@advancedent.com
2nd Thursday of the month
Jan., Mar., May, July, 7:00–8:30 pm
New York
Bronx Tinnitus Support Group
Contact: Dr. S. Karie Nabinet
T: 917–797–9065
E: kkwn12u@aol.com
1st Thursday of the month, 6:30 pm
Pennsylvania
Lehigh Valley Tinnitus Support Group
Contact: Luke Ciaccio, PhD
T: 610–776–3117
E: lciaccio@gsrh.org
2nd Tuesday of month, 5:30–6:30 pm
Texas
South & Central Texas
Tinnitus Support Group
Contact: Matthew Randal
T: 512–660–7276
E: atasg.satx@gmail.com
1st Saturday of the month, 10:00 am
Dallas-Ft. Worth Tinnitus Support Group
Contact: John Ogrizovich
E: dfwtsg@yahoo.com
Saturday, every six weeks, 10:00 am
Virginia
National Capital Region
Tinnitus Support Group
Contacts: Elaine Wolfson, David Treworgy
E: erwolfson@comcast.net
E: david_treworgy@yahoo.com
Meets monthly, date and time TBD
Madison WI Tinnitus Support Group
Contact: Deb Holmen
T: 608–219–0277
E: dholmenihearu@gmail.com
Website: TinnitusWISupport.com
4th Wednesday of the month, 6:30–7:30 pm
The Palo Alto Tinnitus Support Group at Avenidas
Contact: Ken Adler
E: karmtac@aol.com
T: 650–839–1770
3rd Thursday of the month, 5:30–7:30 pm
“Tinnitus Together” Support Group
Crossings Community Church, Life Care Center
Contact: Pam Timmons
E: ptimmons@houghear.org
1st and 3rd Monday of the month, 6:30–7:30 pm
First-time attendees must register using the following link: https://crossings.church/ groups?groupId=487170

Listing current as Oct. 29, 2024
When making an appointment, please mention that you learned of the provider from the ATA, thereby ensuring that providers understand the importance of being a part of the ATA’s tinnitus patient provider network.
Purple: Audiology
Green: Medical practitioner
Blue: Hearing aid dispenser
Orange: Therapist
Pink: Complementary/ Alternative Medicine practitioner
Navy: Other
Alabama
Lynette Bardolf, AuD Audiology Solutions, LLC Enterprise, AL
Monica Boudreaux, AuD South Alabama Hearing and Tinnitus Center, LLC Foley, AL
Susan Sheehy, AuD Alabama Hearing Associates Madison, AL
Emily McMahan, AuD, CH–TM Alaska Hearing & Tinnitus Center Anchorage, AK
Lynn Callaway, BC–HIS Affordable Hearing Solutions Green Valley, AZ
Evan Davies, AuD, CH–TM Arizona Hearing Specialists Tucson, AZ
Mehdi Foroogozar, HIS Enticare
Casa Grande, AZ
Judy Huch, AuD Oro Valley Audiology, Inc. Oro Valley, AZ
Bomina Kang, AuD Sound Relief Hearing Center Peoria, AZ
Steven Lopez, CCHT Awaking Healing, LLC Glendale, AZ
Sarah Pitrone, AuD, CH–TM Sound Relief Hearing Center Mesa, AZ
Meg Safko, MA, CH–TM AOC Physicians Phoenix, AZ
Adriana Sanchez AuD, CH–TM Arizona Hearing Specialists Tucson, AZ
Greg Swingle, AuD Arizona Hearing Associates Tucson, AZ
Peter Vernezze, LCSW, PhD Tucson, AZ
Kelley Linton, AuD, CH–TM Center for Hearing, Ltd. Fort Smith, AR
Kasra Abolhosseini, AuD Tustin Hearing Center Tustin, CA
John Barrett, Lac The Acupuncture Wellness Center, Inc. Los Angeles, CA
Randall Bartlett, MA Tinnitus & Audiology Center of Southern California, Inc. Santa Clarita, CA
Maryellen Brisson, AuD Parker Hearing Hermosa Beach, CA
Shahrzad Cohen, AuD, CH–TM Hearing Loss Solutions Sherman Oaks, CA
David DeKriek, AuD Fidelity Hearing Center Cerritos, CA
Gregory Frazer, AuD Pacific Hearing & Balance Center, Inc. Los Angeles, CA
Jennifer Gans, PsyD Mindful Tinnitus Relief San Francisco, CA
Amit Gosalia, AuD West Valley Hearing Center Woodland Hills, CA
Alyse Gulack, AuD VA Palo Alto Healthcare System Menlo Park, CA
Danielle Hall, AuD California Hearing Center San Mateo, CA
Tracy Peck Holcomb, AuD Treble Health San Francisco, CA
Kim Hoppin, AuD Marin Hearing Center Corte Madera, CA
Beverly Lew, AuD Sound Advice Burbank, CA
Peter Marincovich, PhD Audiology Associates Santa Rosa, CA
Sara Mattson, AuD Rancho Santa Fe Audiology Rancho Santa Fe, CA
Suzanne May, AuD, CH–TM Treble Health Sacramento, CA
Kirsten McWilliams, AuD, CH–TM The Hearing Solution Sacramento, CA
Marni Novick, AuD, CH–TM Silicon Valley Hearing, Inc. Los Gatos, CA
Angela O’Boyle, AuD Hearing Associates Inc. Northridge, CA
Cathie Pechnick, LCSW Los Angeles, CA
Tina Penman, AuD US Department of Veterans Affairs Citrus Heights, CA
Ramsay Poindexter, AuD, CH–TM Treble Health San Jose, CA
Brook Raguskus, AuD, CH–TM Pacific Hearing Service Los Altos, CA
Samantha Ramirez, AuD Kaiser Permanente Redwood City, CA
Ashley Richards, AuD Veterans Administration San Francisco, CA
Rixon Rouse, AuD Kaiser Permanente San Francisco, CA
Mimi Salamat, PhD Dr. Mimi’s Audiology Clinic Walnut Creek, CA
Cheri Taylor, AuD Emerald Hill Audiology Monterey, CA
Ben Thompson, AuD Treble Health Berkeley, CA
Margaret Wallhagen, PhD (Prof.) University of California, San Francisco San Francisco, CA
Brian Worden, MD Kaiser Permanente Woodland Hills, CA
Colorado
Paige Andrade, AuD, CH–TM Sound Relief Hearing Center Lakewood, CO
Julie Eschenbrenner, AuD Flatirons Audiology, Inc. Lafayette, CO
Kaela Fasman, AuD, CH–TM Sound Relief Hearing Center Golden, CO
Brandi Greenhouse, AuD, CH–TM Sound Relief Hearing Center Highlands Ranch, CO
Emily Hensarling, AuD, CH–TM Kaiser Permanente Lone Tree, CO
Tony Kovacs, AuD, CH–TM Sound Relief Hearing Center Fort Collins, CO
Alison Labrec Gomez, AuD, CH–TM Treble Health Denver, CO
Sarah Mathews, AuD Treble Health Denver, CO
Abigail McMahon, AuD, CH–TM Sound Relief Hearing Center Fort Collins, CO
Elizabeth McNichols, AuD, CH–TM Sound Relief Hearing Center Highlands Ranch, CO
Leah Mitchell, AuD, CH–TM Sound Relief Hearing Center Westminster, CO
Natalie Phillips, AuD Audiology Center of Northern Colorado Fort Collins, CO
Drew Price, AuD, CH–TM Sound Relief Hearing Center Denver, CO
Julie Prutsman, AuD, CH–TM Sound Relief Hearing Center Highlands Ranch, CO
Megan Read, AuD, CH–TM Sound Relief Hearing Center Highlands Ranch, CO
Mackenzie Reichert, AuD, CH–TM Hear-Lab Centennial, CO
James Richwine, HIS Conifer Hearing and Tinnitus Conifer, CO
Senia Romero, AuD, CH–TM Sound Relief Hearing Center Centennial, CO
Jackie Smith, AuD, CH–TM Sound Relief Hearing Center Highlands Ranch, CO
Mandi Solat, AuD, CH–TM Audiology Services & Hearing Aid Center Lakewood, CO
Robert Traynor, EdD, CH–TM Fort Collins, CO
Kelli Whitley, AuD Sound Relief Hearing Center Highlands Ranch, CO
Jenny Crews, AuD ENT Medical and Surgical Group New Haven, CT
Laura Kruger, AuD VA Medical Center West Haven, CT
Ashley Helthall, AuD HearingLife Dover, DE
Katlynn Roldan, AuD Hearing Life Dover, DE
Sherrie Alpert, AuD Hear Again America Stuart, FL
Indira Alvarez, AuD Palm Coast Hearing Center Palm Coast, FL
Hyo Chang Arnold, AuD, CH–TM Advanced Audiology & Hearing Aids Port St. Lucie, FL
Kelly Breese, AuD, CH–TM Murphy Hearing Aids of Sarasota Sarasota, FL
Anne Carter, PhD, CH–TM Pasadena Hearing Care South Pasadena, FL
Maura Chippendale, AuD, CH–TM Chippendale Audiology Cape Coral, FL
Melissa Kipp Clark, AuD Suncoast Hearing Services Plus Bradenton, FL
Noel Crosby, AuD Advanced Hearing Solutions Englewood, FL
Ali Danesh, PhD Labyrinth Audiology Boca Raton, FL
Edvaldo de Oliveira Leme, BS Medika Jacksonville, FL
Kristin DesErmia, AuD Coastal Hearing Care Bradenton, FL
Kelly Dyson, AuD Suncoast Audiology, LLC Largo, FL
Kimberly Lamb, AuD Lake Medical Center Eustis, FL
Mark Rahman, HIS Gulf Gate Hearing Aid Center Sarasota, FL
Breanne Schwartz AuD, CH–TM Treble Health Miami, FL
Melisa Sharpe, AuD First Coast Mobile Audiology Ponte Vedra Beach, FL
Cindy Ann Simon, AuD South Miami Audiology Consultants South Miami, FL
Mindy Stejskal, MCD The Hearing Center Pensacola, FL
Susan Terry, AuD Broadwater Hearing Care St. Petersburg, FL
Liz White, AuD Harbor City Hearing Solutions Melbourne, FL
Kayla Wilkins, AuD Aspire Hearing and Balance Lakeland, FL
Stephanie Zang, HIS Digital Hearing Lab Clermont, FL
Alicia Bernstein, MS, CH–TM ENT of Georgia/Advanced Hearing LLC Alpharetta, GA
Elisa Bobbitt, AuD Newtown Hearing Center Alpharetta, GA
Christopher Campellone, HIS GoToHearing Gainesville, GA
Will Dennison, HIS Dennison Hearing Solutions Dacula, GA
Sonia Hamidi, AuD, CH–TM Ear Nose & Throat Institute Alpharetta, GA
Avni Patankar, AuD Maple Hearing Clinic Cumming, GA
Liz Ramos, AuD, CH–TM ENT of Georgia/Advanced Hearing Atlanta, GA
Nikki Weaver, AuD Fayette Hearing Clinic and Coweta Hearing Clinic Peachtree City, GA
Melissa Wikoff, AuD, CH–TM Peachtree Hearing Marietta, GA
Bailey Neuhaus, AuD, CH-TM Boise VA Medical Center Boise, ID
Kalob Parsons, AuD Better Hearing and Audiology LLC Idaho Falls, ID
Christine Pickup, AuD Mt. Harrison Audiology & Hearing Aids, LLC Rupert, ID
Tosha Strickland, AuD Strickland Ear Clinic Meridian, ID
Courtney Baker, AuD Hearing Brain Audiology, PLLC Chicago, IL
Steve Bonzak, MS Health Traditions Chicago, IL
Megan Bradshaw, AuD, CH–TM Revolution Hearing Napervville, IL
Nancy Congdon, AuD, CH–TM The Hearing Care Clinic Downers Grove, IL
Phillip Elbaum, LCSW Stritch School of Medicine Loyola University, Chicago Deerfield, IL
Victoria Frank, AuD Sertoma Speech & Hearing Association Palos Hills, IL
Ryland Gallagher, AuD Northwest Speech & Hearing Arlington Heights, IL
Lori Halvorson, AuD, CH–TM Lake Forest Hearing Professionals Lake Forest, IL
Dawn Heiman, AuD Advanced Audiology Consultants Woodridge, IL
Jaclyn Jansen, AuD
Sarah Bush Lincoln Effingham, IL
Julie Lendzion, AuD Naperville Hearing Services Naperville, IL
Anne Miller, AuD Sonova / RUSH Univ Montgomery, IL
Maria Morrison, AuD, CH–TM Geneva Hearing Services Geneva, IL
Rebecca Murphy, AuD Kerr Hearing Aid Center Inc. Springfield, IL
Mark Partain, AuD, CH–TM Treble Health Chicago, IL
James Peck, HIS Life Hearing Health Centers Rockford, IL
Jeanne Perkins, AuD Audiologic Services Glen Ellyn, IL
Ann Perreau, PhD Augustana College Center for Speech, Language, and Hearing Rock Island, IL
Daria Popowych, AuD North Side Audiology Group, Inc. Chicago, IL
Alyssa Seeman, AuD Illinois State University Normal, IL
Maria Vetter, AuD Chicago Hearing Services Chicago, IL
Curt Esterline, HIS Concierge Hearing Healthcare New Haven, IN
Laura Fragomeni, AuD, CH–TM Audiology Solutions, PC Indianapolis, IN
Sharon Hirstein, MA Elkhart Audiology Rehab Elkhart, IN
Lindsey Koble, AuD, CH–TM Audiology Always Auburn, IN
Allison Morris, AuD Treble Health Indianapolis, IN
Erica Person, AuD Flex Audiology Lawrenceburg, IN
Iowa
Julie Jeon, PhD (Prof.) The University of Iowa Iowa City, IA
Diana Kain, AuD Heartland Hearing Center Hiawatha, IA
Jill Nesham, AuD Professional Hearing Solutions by Dr. Jill Cedar Rapids, IA
Jonathan Stirn, AuD Hope Hearing & Tinnitus Center Hiawatha, IA
Heather Thatcher, HIS Hope Hearing & Tinnitus Center Hiawatha, IA
Kansas
Paige Arbanas, AuD Veterans Administration Kansas City, KS
Matthew Brown, AuD Kaw Valley Hearing Lawrence, KS
Marli Gathright, AuD Hearing & Balance Specialists of Kansas City Overland Park, KS
Bryne Gonzales, AuD NuSound Hearing & Tinnitus Center Topeka, KS
Darcie Hartwick, HIS Hartland Hearing Care Centers Manhattan, KS
James Mangimelli, AuD Mosaic Life Care Atchison, KS
Lauren Mann, AuD University of Kansas Medical Center Kansas City, KS
Kentucky
Nachiketa Bhatt, RN Healthy Living Primary Care Louisville, KY
Stacy Garrard, AuD Kentucky Audiology & Tinnitus Services Lexington, KY
Ann Rhoten, AuD Kentucky Audiology & Tinnitus Services Lexington, KY
Kari Wickstrom, AuD Bluegrass Hearing Clinic Nicholasville, KY
Louisiana
Catherine Lo, AuD The Hearing Clinic Thibodaux, LA
Mary Miller, PhD Premier Hearing and Balance Hammond, LA
Elena Treadway, AuD Noel ENT Hearing Center Abbeville, LA
Maine
Lindsay Allison, AuD, CH–TM Capital Hearing Wellness Center, LLC Augusta, ME
Kelly Lynch, MA
Mercy Ear Nose And Throat Associates Portland, ME
Kassander Thompson, AuD MaineHealth Norway, ME
Ashlee Vandiver, AuD Red Maple Audiology, LLC Turner, ME
Maryland
Chelsea Carter, AuD University of Maryland Medical Center Baltimore, MD
Ross Cushing, AuD Live Better Hearing & Balance Montgomery Village, MD
Katelyn Leitner, AuD, CH–TM Hearing Assessment Center Nottingham, MD
Candice Ortiz–Hawkins, AuD Capital Institute of Hearing & Balance Silver Spring, MD
Tricia Pastore-Bard, AuD, CH–TM Frederick Health Medical Group New Market, MD
Sofia Roller, AuD The Hearing Wellness Center, LLC Lutherville-Timonium, MD
Yael Schonfeld, AuD Chesapeake Ear, Nose & Throat Owings Mills, MD
Christina Shields, AuD University of Maryland College Park College Park, MD
LaGuinn Sherlock, AuD, CH–TM Walter Reed National Military Medical Center Bethesda, MD
Massachusetts
Dierdre Anderson, AuD Audiology Network Services Salisbury, MA
Judith Bergeron, HIS Beauport Hearing Care Gloucester, MA
Collin Campbell, Lac
Campbell Acupuncture and Herbal Medicine Clinic South Dennis, MA
Theresa Cullen, AuD, CH–TM Cape Cod Hearing Center Hyannis, MA
Peter Harakas, PhD CBT Associates, LLC Lexington, MA
Stephane Maison, AuD, PhD, CH–TM Massachusetts Eye & Ear Tinnitus Clinic Boston, MA
Dana Mario, AuD Mario Hearing & Tinnitus Clinics Mansfield, MA
Karen Wilber, AuD, CH–TM Boston Children’s Hospital Lexington Lexington, MA
Michigan
Stelios Dokianakis, AuD, CH–TM Holland Doctors of Audiology Holland, MI
Allie Heckman, AuD, CH–TM Michigan Medicine–University of Michigan Ann Arbor, MI
MaryRose Hecksel, AuD Audiology & Hearing Aid Center Lansing, MI
Tiffany Inman, AuD Inman Audiology Troy, MI
Angela McNabb, MS Hear Now Audiology & Tinnitus Center Clinton Township, MI
Jacklyn Miller, AuD Advanced Audiology DeWitt, MI
Shannon Radgens, DO
Red Cedar Ear Nose & Throat & Audiology Owosso, MI
Virginia Ramachandran, AuD Oticon, Inc. Plymouth, MI
Michelle Rankin, AuD
Rankin Audiology and Hearing, LLC Chelsea, MI
Michelle Schuiling, AuD, CH-TM
Holland Doctors of Audiology Holland, MI
Karrie Slominski, AuD
Henry Ford Health System West Bloomfield, MI
Rachel Allgor, AuD Journey Audiology & Hearing Care Hastings, MN
Jennifer Anfinson, AuD Treble Health Plymouth, MN
John Coverstone, AuD, CH–TM Audiology Ear Care
New Brighton, MN
Sara Downs, AuD
Hearing Wellness Center Duluth, MN
John Ehlen Hear Central Victoria, MN
Jessica Fredine, HIS Hearing Life Anoka, MN
Jason Leyendecker, AuD Audiology Concepts Edina, MN
Katie McManus, LPC CBT Minneapolis-St. Paul Minneapolis, MI
Ann Miller, AuD Park Nicollet St. Louis Park, MN
Laura Morrison, AuD, CH–TM Hearing Life Edna, MN
Jerry Zhou, PhD Hearing of America, LLC Oakdale, MN
Mississippi
Kasi Saucier, AuD, CH–TM Renew Audiology–Hearing Aid and Tinnitus Center Madison, MS
Missouri
Laura Flowers, AuD Hearing and Balance Specialists of Kansas City Lee’s Summit, MO
Montana
Tana Whicker, MA Hearing & Speech Connection Miles City, MT
Nevada
Robyn Lofton, HIS Hearing Associates of Las Vegas Las Vegas, NV
Allison Treseder, AuD, CH–TM Neosensory, Inc Reno, NV
New Hampshire
Nataliya Ayzenberg, AuD, CH–TM Alliance Hearing Center Concord, NH
New Jersey
Yasmin Battat, AuD Oracle Hearing Center Lawrenceville, NJ
Granville Brady Jr., AuD East Brunswick, NJ
Jennifer Elfert, AuD, CH–TM Alliance Speech & Hearing Center Howell, NJ
Jade Igbokwe, AuD, CH–TM NTI Audiology Jersey City, NJ
Michelle Neidleman Kennedy, AuD Treble Health Newark, NJ
Tatyana Kennedy, AuD Treble Health Jersey City, NJ
William J. McDonnell, VSO Dept. of Veterans Affairs Mount Laurel, NJ
Nicole Piasentini, AuD, CH–TM New Jersey Hearing Health Center Brick, NJ
Marion Rollings, PhD Holistic Health Counseling Center LLC Hillsborough, NJ
New Mexico
Dorothy McCurley, AuD McCurley Hearing Design Albuquerque, NM
Allison Moneypenny, AuD Advanced Hearing Care Alamogordo, MN
Catherine Worth, MS Capital Hearing Care Albuquerque, NM
New York
Nicole Ball, AuD Hearing Evaluation Services of Buffalo, Inc. Tonawanda, NY
Dawn Bowerman, MS dB Hearing Center Williamsville, NY
Julia Bramley, AuD Slocum Dickson Medical Group New Hartford, NY
Lois Cohen, LCSW, ACSW, BCD Tinnitus Distress & Relief Counseling Northport, NY
Natalie Crossland, AuD, CH–TM Audiology Island Staten Island, NY
Nancy Datino, AuD Audiology and Speech Solutions Rye, NY
Elliot Davis, BS DDS
Elliot R. Davis, DDS New York, NY
Stefan Fosco, AuD Audiologic Solutions Rensselaer, NY
MaryMargaret Griffin, AuD The Hearing Connection Massapequa, NY
Bruce Hubbard, PhD CBT for Tinnitus, LLC New York, NY
Craig Kasper, AuD
New York Institute for Hearing & Balance New York, NY
Tracey Lynch, AuD
Island Better Hearing Inc. Melville, NY
Jeffrey Shannon, AuD
Hudson Valley Audiology Center Pamona, NY
Randall Solomon, MD
Long Island Mental Health Port Jeff Station, NY
Garrett Thompson, AuD Treble Health New York, NY
Lori Trentacoste, AuD Island Better Hearing Inc. Melville, NY
Diana Vetere, AuD Treble Health Huntington, NY
Erin Walborn–Sterantino, AuD Audiologic Solutions Rensselaer, NY
Carolyn Yates, AuD, CH–TM Hearing Evaluation Services of Buffalo, Inc.
Amherst, NY
Caitlyn Adams, AuD East Coast Hearing & Balance Durham, NC
Jennifer Auer, AuD Audiology Attention & Tinnitus Care, PLLC Concord, NC
Susan Bergquist, MS Heritage Audiology Wake Forest, NC
Kendall Carroll, AuD
Atrium Health Wake Forest Baptist Winston-Salem, NC
Shelly Cristobal, AuD Hearing Health Care Services Durham, NC
Lisa Fox–Thomas, PhD UNCG Speech and Hearing Center Greensboro, NC
Goutham Gosu, AuD Hearing Solution Center Charlotte, NC
Julia Hess, MHDL, RN WG Bill Hefner VA Medical CenterKernersville Clinic Greensboro, NC
Danielle Jenkins, AuD Raleigh Hearing and Tinnitus Center Raleigh, NC
Patricia Johnson, AuD, CH–TM
UNC School of Medicine
Chapel Hill, NC
Carroll Kendall, AuD, CH–TM
Atrium Health Wake Forest Baptist Clemmens, NC
Allison King, AuD
Palmetto Family Hearing Center Waxhaw, NC
Kelly Knolhoff, AuD
Birkdale Audiology Huntersville, NC
Saranne Lentz-Barker, AuD, CH–TM
Spectrum Hearing Clinic Henderson, NC
Nancy McKenna, AuD, PhD University of North Carolina at Chapel Hill Chapel Hill, NC
Sheri Mello, AuD
Raleigh Hearing and Tinnitus Center Raleigh, NC
Melissa Palmer, AuD Clayton Audiology, PLLC Clayton, NC
Stan Phillips, MD
South Lake Hearing and Tinnitus Center Huntersville, NC
Ivy Saul, AuD
Audiology & Hearing Services of Charlotte Charlotte, NC
Michael Slater, AuD
South Lake Hearing and Tinnitus Center Huntersville, NC
Emilee Tucker, AuD, CH–TM
Carolina Ear, Nose & Throat— Sinus and Allergy Center, PA Hickory, NC
Mackensie Brandt, AuD Altru Professional Center Grand Forks, ND
Ohio
Joe Baker, MA Hearing Science Westlake, OH
Sarah E. Curtis, AuD
Sounds of Life Hearing Center, LLC Concord Township, OH
Ellen Foltz, AuD, CH–TM Modern Hearing Solutions Canton, OH
Ryan Hill, AuD
The Hill Hear Better Clinic Cincinnati, OH
Cathy Kooser, MSW, LISW Hillcrest Hearing & Balance Center Centerville, OH
Thomas Lolan, AuD
South Dayton Hearing Aids & Audiology Kettering, OH
Heather Malyuk, AuD Soundcheck Audiology Cuyahoga Falls, OH
Heather Maze-Smith, AuD Maze Hearing, LLC Bellefontaine, OH
Samantha Morehouse, AuD, CH–TM
Mercy Health ENT & Audiology Cincinnati, OH
Samantha Morgan, AuD Mary Rutan Audiology Bellefontaine, OH
Richard Reikowski, AuD Family Hearing & Balance Center Akron, OH
Eryn Staats, AuD Memorial ENT Marysville, OH
Taylor Verba, AuD, CH–TM Echo Hearing Systems & Audiology Powell, OH
Babette Verbsky, PhD, CH–TM Hearing Connections Audiology Lebanon, OH
Gail Whitelaw, PhD, CH–TM The OSU Speech–Language–Hearing Clinic Columbus, OH
Suzanne Kimball, AuD University of Oklahoma Health Sciences Center Oklahoma City, OK
Sidney Lawler, MD Tulsa, OK
Caitlyn Matthews, AuD Hearts for Hearing Oklahoma City, OK
Mark Robertson, MD Ascension Bartlesville, OK
Anna Forsline, AuD VA Portland Healthcare System Portland, OR
Kristen Furseth, AuD, CH–TM Willamette ENT Salem, OR
Bryan J. Greenaway, AuD, CH–TM Pacific University Hillsboro, OR
James Henry, PhD Ears Gone Wrong®, LLC Portland, OR
Erika Shakespeare, AuD Audiology & Hearing Aid Services La Grande, OR
Sarah M. Theodoroff, PhD VA Portland Healthcare System Portland, OR
Colette Vossler-Welch, AuD Hearing Associates Eugene, OR
Sandi L.B. Ybarra, AuD Hearing Associates Eugene, OR
Krista Blasetti, AuD WellSpan ENT and Hearing Center York, PA
Gail Brenner, AuD Tinnitus & Sound Sensitivity Treatment Center of Philadelphia, PC Bala Cynwyd, PA
Mindy Brudereck, AuD, CH–TM Berks Hearing Professionals Birdsboro, PA
Lucy Tence Corbin, AuD PA Hearing & Tinnitus Center Selinsgrove, PA
Linda Dallas, MEd Allentown Ear, Nose and Throat Allentown, PA
Amy Greer, AuD, CH–TM Lemme Audiology Associates Ebensburg, PA
Jacob Hulswit, AuD Jefferson Balance and Hearing Center Philadelphia, PA
Jennifer Isayev, AuD Audiometrics, Inc. Bryn Mawr, PA
Jeannie Karlovitz, AuD Advanced Hearing Solutions Exton, PA
Debbie Lombardi, AuD, CH–TM Premiere Speech and Hearing Brownstown, PA
Anthony Napoletano, HIS Lansdowne Hearing Lansdowne, PA
Alexandra Taylor, AuD Aberdeen Audiology Wayne, PA
Holly Puleo, AuD Gateway Hearing Solutions Warwick, RI
Alexandra Tarvin, AuD Elevate Audiology Hearing and Tinnitus Center Easley, SC
Jason Wigand, AuD Beach Audiology Hearing & Balance Center Myrtle Beach, SC
Tiffany Ahlberg, AuD Ahlberg Audiology & Hearing Aid Services Cleveland, TN
Marc Fagelson, PhD East Tennessee State University Johnson City, TN
Brittany Grayless, AuD University of Tennessee Health Science Center Knoxville, TN
Jennifer Hausladen, AuD University of Tennessee Health Science Center Knoxville, TN
Andrea Plotkowski, AuD Ear, Nose and Throat Consultants of East Tennessee Knoxville, TN
Paul Shea, MD Shea Ear Clinic Memphis, TN
Elizabeth Welch, AuD Hear Tennessee Franklin, TN
S. Diane Allen, PhD
The Grove Counseling & Wellness Center Dallas, TX
Katherine Alsop, AuD University of North Texas Speech and Hearing Center Denton, TX
Theodore Benke, MD Benke Ear, Nose, & Throat Clinic Cleburne, TX
Arica Black, AuD
The Hearing Doctor Lubbock, TX
Bethany Brum, AuD, CH–TM UT Southwestern Medical Center Dallas, TX
E. Suzanne Carter, LPC Private Practice San Antonio, TX
Tracey Castillo AuD, CH–TM Houston Ear, Nose and Throat Houston, TX
Christina Corrales AuD, CH–TM Cornerstone Audiology Lubbock, TX
Heather Dean, AuD Burleson Audiology Clinic Burleson, TX
Shannon Frugia, AuD, CH–TM
Southeast Texas Ear Nose & Throat Beaumont, TX
Mary Sue Harrison, AuD Today’s Hearing Katy, TX
Jamie Hawkins, AuD Clarity Hearing The Woodlands, TX
Rachel Higginbotham, AuD Estes Audiology Hearing Centers Boerne, TX
Carla Hoffman, HIS Hoffman Hearing Solutions Corpus Christi, TX
Margaret Hutchison, PhD, CH–TM Austin Hearing Services Austin, TX
Danielle Jenkins, AuD IlluminEar Tinnitus & Audiology Austin, TX
Candace Johnson, AuD Cook Hearing & Balance Cedar Park, TX
Kristen Keener, AuD IlluminEar Tinnitus & Audiology Center
Austin, TX
Beki Kellogg, AuD Hope Hearing & Tinnitus Center Southlake, TX
Christina Lobarinas, AuD UT Southwestern Medical Center Dallas, TX
Cynthia Lockhart, HIS Avalon Hearing Aids Carrollton, TX
Tony Milesi, AuD RK Audiology Austin, TX
Celia Miranda, AuD, CH–TM Hear In Texas New Braunfels, TX
Elly Pourasef, AuD Memorial Hearing Houston, TX
Christie Spencer, AuD, CH–TM Fort Bend Hearing
Sugar Land, TX
Beth Rasmussen, AuD Texas State University Round Rock, TX
Victoria Villareal, AuD RK Audiology
Austin, TX
Crystal Wiggins, AuD, CH–TM Memorial Hearing Houston, TX
Erika Wilcox, AuD, CH–TM Memorial Hearing Houston, TX
Seth Austin, HIS Timpanogos Hearing American Fork, UT
Layne Garrett, AuD Timpanogos Hearing American Fork, UT
Jessica Lui Nelson, BC–HIS Timpanogos Hearing Spanish Fork, UT
Stephanie Hollop, AuD, CH–TM Univ. of Vermont–E.M. Luse Center
Burlington, VT
Ana Anzola, AuD
Ascent Hearing
McLean, VA
Please note that the American Tinnitus Association does not verify providers’ certifications and expertise in tinnitus treatment. The list is meant expressly for informational purposes and should not be construed as the ATA’s endorsement of the providers listed. The ATA strongly advises anyone using the list to check practitioners’ websites and tinnitus services before scheduling appointments. Please note that the list includes hearing aid dispensers because hearing aids can be helpful to some people in the management of their tinnitus.
Ann DePaolo, AuD
The Audiology Offices, LLC Kilmarnock, VA
Julie Farrar–Hersch, PhD Augusta Audiology Associates, PC Fishersville, VA
Kristin Koch, AuD Evolution Hearing Charlottesville, VA
Fred Lindsay, DO Hampton Roads ENT and Allergy Hampton, VA
Thomas Armstrong, PhD, PLLC Walla Walla, WA
Tyler Ellis, AuD, CH–TM Northwest Hearing + Tinnitus Seattle, WA
Melanie Hecker, AuD, CH–TM Northwest Hearing + Tinnitus Seattle, WA
Erika Kay, AuD Highline Audiology & Hearing Aids Burien, WA
Thomas Littman, PhD, CH–TM Factoria Hearing Center Bellevue, WA
Laura Moran, AuD, CH–TM Northwest Hearing + Tinnitus Olympia, WA
Janice Powis, AuD, CH–TM Mind Over Tinnitus Bainbridge Island, WA
Dustin Spillman, AuD, CH–TM Audiologists Northwest Bremerton, WA
Kindra Veith, AuD, CH–TM Northwest Hearing + Tinnitus Seattle, WA
Natalie White, AuD, CH–TM Eastside Audiology Snohomish, WA
Wisconsin
Hugo Guerrero, AuD, CH–TM Mayo Clinic Health System Onalaska, WI
Veronica Heide, AuD, CH–TM Audible Difference, LLC Madison, WI
Dan Malcore The Hyperacusis Network Green Bay, WI
Christina Milos, AuD, CH–TM Audiologic Wellness, LLC Pleasant Prairie, WI
Samantha Sikorski, HIS Sikorski Hearing Aid Center, Inc. Spooner, WI
Puerto Rico
Isamar Gonzalez–Feliciano, AuD Centro Audiológico e Interdisciplinario, Isamar González, Inc. Arecibo, PR
Edvaldo Leme, PhD Médika Curitiba, PR
Neysa Orraca, AuD
Centro Neymar Bayamon, PR
Soami Santiago de Snyder, PhD Universidad de Puerto Rico Medical Sciences Campus Gurabo, PR
Alejandro Torres Torres, AuD The Hearing Center San Juan, PR
Argentina
Susana A. Dominguez Conacu.com.ar Buenos Aires
Australia
Fabrice Bardy, MClinAud, PhD MindEar Surry Hills, NSW
Lynne Blackford, MClinAuD MQ Health Speech and Hearing Clinic
Macquarie University
Minakshi Gupta, MA All Ears Hearing Mount Waverley, VIC
Jennifer Yeowart, AuD
Tinnitus Relief Australia Maroochydore, QLD
Belgium
Haike Bruneel, MD
HB Consulting Borgerhout
Canada
Nashlea Brogan, AuD Bluewater Hearing Sarnia, ON
Ronald Choquette, AuD, CH–TM Montreal University Audiology Clinic Montreal, QC
Sabrina DeToma, AuD
Salus Hearing and Tinnitus Centre Vaughan, ON
Patrick DeWarle, AuD, CH–TM Winnipeg Hearing Centres Winnipeg, MB
Kimberly Eskritt, AuD Lambton Audiology Associates Sarnia, ON
Deborah R. Lain, MSc
Hope For Tinnitus Calgary, AB
Carol Lau, HIS Sound idEARS Inc. Vancouver, BC
Suzanne MacLaren, AuD Calgary Ear Centre Calgary, AB
Margaret Jane Steinberg, AuD Total Hearing Centre Ancaster, ON
Cayman Islands
Annette Stephenson, AuD Cayman Hearing Center George Town
Costa Rica
Silvia Bonilla, AuD
Conservacion Auditiva Ocupacional y Comunitaria CAOC
San Rafael
Juan Olmo, AuD
Conservacion Auditiva Ocupacional y Comunitaria CAOC
San Jose
Czecklsolvakia
Lenka Povová, MD
Myrinx SRC, Ear Nose & Throat Specialist Nový Bor
Ghana
Neal Boafo, AuD NeuroAudiology Ltd Haatso
Hong Kong
David Ho, MD
Shangzhi Medical Group
Hong Kong
Italy
Andrea Beghi, MD Centro di Medicina Ferrara Ferrara
Mattia Peirano, AuD Freelance Vallecorsia, IM
Malaysia
Wan Syafira Ishak, PhD, CH–TM Universiti Kebangsaan Malaysia Malaysia, Kuala Lumpur
Mexico
Monica Palacios Orozco, AuD
Monica del Carmen Palacios Orozco
Guanajuato, Mexico
Peru
Oxana Panduro, MHSc Centro de Diagnóstico y Rehabilitación
Auditiva Vestibular
San Isidro, Lima
Singapore
Sharad Govil, AuD
Amazing Hearing Group
Singapore
United Kingdom
Lisa Caldwell
The Hearing Coach Glossop
Alan Hopkirk
The Invisible Hearing Clinic Paisley
Tinnitus Today magazine is a print and electronic media magazine published in April, August, and December, and circulated to 25,000+ ATA contributors, donors, patients, supporters, researchers, and healthcare professionals.
The magazine editorial team empowers readers with information, including up-to-date medical and research news, feature articles on urgent tinnitus issues, questions and answers, self-help suggestions, and letters to the editor from others with tinnitus. Strong service journalism, compelling storytelling, first-person narrative, and profiles are presented in an inviting format to encourage readers to reflect, engage, and better understand a chronic condition that affects millions.
Editorial Calendar is subject to change.
To advertise, contact: tinnitus@ata.org
The mission and core purpose of ATA are to promote relief, help prevent, and find cures for tinnitus evidenced by its core values of compassion, credibility, and responsibility.
Compassion: Evidenced in a spirit of hope reflected in the commitment to finding a cure, preventing the condition, and supporting those affected by the condition.
Credibility: Evidenced in accurate information from reliable sources, transparency in decisionmaking, and an earned reputation for trustworthiness.
Responsibility: Evidenced in patient-centered advocacy by a collaborative community of forward thinking leaders accountable to its mission and members.
www.ATA.org







“The Stars In My Ears”: A Perspective
1. S. N. Rosing, J. H. Schmidt, N. Wedderkopp, & D. M. Baguley. (2016). Prevalence of tinnitus and hyperacusis in children and adolescents: A systematic review. BMJ Open, 6, e010596. https:// doi.org/10.1136/bmjopen-2015-010596
2. R. Humphriss, A. Hall, & D. Baguley. (2016). Prevalence and characteristics of spontaneous tinnitus in 11-year-old children. International Journal of Audiology, 5(3), 142–148.
3. Tinnitus, Boston Children’s Hospital. (2024). https://www.childrenshospital.org/conditions/ tinnitus#:~:text=If%20you%20are%20 seeking%20help,%40childrens.harvard.edu
4. C.M. Jarach, A. Lugo, M. Scala, P.A. Van den Brandt , C.R. Cederroth, A. Odone, & S. Gallus. (2022). Global prevalence and incidence of tinnitus: A systematic review and meta-analysis. JAMA Neurology, 79(9):888.
5. S. K. Swain & P. Baliarsingh. (2022). Self-reported tinnitus in pediatric age group: Our experiences at a tertiary care teaching hospital in Eastern India. International Journal of Contemporary Pediatrics, 9, 884.
6. D. Raj-Koziak, E. Gos, W. Swierniak, H. Skarzynski, & P. H. Skarzynski. (2021). Prevalence of tinnitus in a sample of 43,064 children in Warsaw, Poland. International Journal of Audiology, 60(8), 614–620.
7. M. Savastano, G. Marioni & C. de Fillippi. (2009). Tinnitus in children without hearing impairment.
on Pediatric Tinnitus footnotes continued from page 11 A New Tool for Young Ears: The Children’s Tinnitus Questionnaire footnotes continued from page 14
1. S. N. Rosing, J. H. Schmidt, N. Wedderkopp, & D. M. Baguley. (2016). Prevalence of tinnitus and hyperacusis in children and adolescents: A systematic review. BMJ Open, 6, e010596. https:// doi.org/10.1136/bmjopen-2015-010596
2. D. Raj-Koziak, E. Gos, W. Swierniak, H. Skarzynski, P. H. Skarzynski. (2021). Prevalence of tinnitus in a sample of 43,064 children in Warsaw, Poland. International Journal of Audiology, 60, 614–620. https://doi.org/10.1080/14992027.2020.1849829
3. D. M. Baguley & D. J. McFerran. (1999). Tinnitus in childhood. International Journal of Pediatric Otorhinolaryngology, 49, 99–105. https://doi. org/10.1016/S0165-5876(99)00111-1
4. M. Savastano. (2007). Characteristics of tinnitus in childhood. European Journal of Pediatrics, 166,
International Journal of Pediatric Otolaryngology. 79 (Supp1), S13-15.
8. R. Kentish. (2016). Managing tinnitus in childhood. In D. M. Baguley & M. Fagelson (Eds.), Tinnitus: Clinical and research perspectives (pp. 63–73). Plural Publishing.
9. S. Nemholt, J. H. Schmidt, N. Wedderkopp, & D. M. Baguley. (2020). A cross-sectional study of the prevalence and factors associated with tinnitus and/or hyperacusis in children. Ear and Hearing, 41(2), 344–355.
10. J. Rhee, D. Lee, M. W. Suh, J. H. Lee, Y.-C. Hong, S. H. Oh, M. K. Park. (2020, July 31). Prevalence, associated factors, and comorbidities of tinnitus in adolescents. PLOS ONE https://doi.org/10.1371/ journal.pone.0236723
11. S. Kedzirawska, A. Niedzielski, A. Al-Jazani, & G. Mielnik-Niedzietska. (2017). A sense of disability in children with tinnitus. Journal of Hearing Science, 7(2), 106–107.
12. P. Perez-Carpena, J. A. Lopez-Escamez, & Á Gallego-Martinez. (2024). A systematic review on the genetic contribution to tinnitus. Journal of the Association for Research in Otolaryngology, 25, 13–33. https://doi.org/10.1007/s10162-024-00925-6
13. R.S. Hallum, L. McKenna, L. Sherlock. (2004); Tinnitus impairs cognitive efficiency. International Journal of Audiology. 43(4), 218-226.
14. P. Neff, J. Simões, S. Psatha, et al. (2021). The impact of tinnitus distress on cognition. Scientific
Reports, 11, 2243. https://doi.org/10.1038/s41598021-81728-0
15. N. Sommerhalder, P. Neff, Z. Bureš, O. Profant, T. Kleinjung, & M. Meyer. (2023) Deficient central mechanisms in tinnitus: Exploring the impact on speech comprehension and executive functions. Hearing Research, 440, 108914. https://doi. org/10.1016/j.heares.2023.108914
16. H. Smith, K. Fackrell, V. Kennedy, J. G. Barry, C. Benton, L. Partridge, & D. J. Hoare. (2023). Development of the Impact of Tinnitus in Children Questionnaire (iTICQ). Frontiers in Audiology and Otology, 1, 1323864. https://doi.org/10.3389/ fauot.2023.1323864
17. World Hearing Center. (2024). Children’s Tinnitus Questionnaire. Retrieved from https://ars.els-cdn. com/content/image/1-s2.0-S0165587624001782mmc2.pdf
18. R. Deutsch. (2023). Evidence-based practice in the management of tinnitus in children and adolescents: A systematic review of the literature [Capstone project, City University of New York]. CUNY Academic Works. https://academicworks. cuny.edu/gc_etds/5320
19. C. Benton, C. Munro, J. Phillips, & V. Kennedy. (2015). British Society of Audiology Good Practice Guidance for the management of children with tinnitus. British Society of Audiology.
797–801. https://doi.org/10.1007/s00431-0060320-z
5. R. P. Mills & J. R. Cherry. (1984). Subjective tinnitus in children with otological disorders. International Journal of Pediatric Otorhinolaryngology, 7, 21–27. https://doi.org/10.1016/s0165-5876(84)80050-6
6. H. Smith, K. Fackrell, V. Kennedy, J. Barry, L. Partridge, & D. J. Hoare. (2019). A scoping review to catalogue tinnitus problems in children, International Journal of Pediatric Otorhinolaryngology, 122, 141–151. https://doi. org/10.1016/j.ijporl.2019.04.006
7. British Society of Audiology. (2017). Tinnitus in children: Practice guidance.
8. S. Tegg-Quinn, R. H. Eikelboom, D. M. Baguley, C. G. Brennan-Jones, W. H. A. M. Mulders, & R. J. Bennett. (2023). The use of patient-report
measures and intervention strategies for children and adolescents with chronic tinnitus: A scoping review. International Journal of Audiology, 62 1109–1117. https://doi.org/10.1080/14992027.2022.2 111371
9. D. Raj-Koziak, E. Gos, M. Porowski, P. H. Skarzynski, & H. Skarzynski. (2024). Children’s Tinnitus Questionnaire—a novel tool for assessing the impact of tinnitus on a child’s everyday life. International Journal of Pediatric Otorhinolaryngology, 182, 112024. https://doi. org/10.1016/j.ijporl.2024.112024
1. D. M. Baguley, G. Andersson, D. McFerran, & L. McKenna. (2013). Tinnitus: A multidisciplinary approach, chap. 2. 2nd ed. Wiley-Blackwell.
2. M. B. Meikle, J. Vernon, & R. M. Johnson. (1984). The perceived severity of tinnitus. Otolaryngology—Head & Neck Surgery, 92, 689.
3. C. Manning, E. J. Thielman, L. Grush, & J. A. Henry. (2019). Perception versus reaction: Comparison of tinnitus psychoacoustic measures and Tinnitus Functional Index scores. American Journal of Audiology, 28, 174–180.
4. UCLA Mindfulness App, at https://www.uclahealth. org/ulcamindful/ucla-mindful-app
5. Dr. Bruce Hubbard CBT for Tinnitus, at https:// www.cbtfortinnitus.com/guided-mindfulness-fortinnitus
6. ReSound Relief app, at https://www.resound.com/ en-us/hearing-aids/apps/relief
7. AAO-HNSF Clinical Practice Guideline: Tinnitus— press release & fact sheet. (2014). American Academy of Otolaryngology—Head and Neck Surgery Foundation. https://www.entnet.org/
resource/aao-hnsf-cpg-tinnitus-press-release-factsheet/
8. ADAA Anxiety. (2014). Cognitive behavior therapy (CBT) for tinnitus distress, with N. Sideman and Bruce Hubbard [Podcast]. Retrieved from https:// youtu.be/fVaac8TNoAs?si=QtiuiRTdnGXWATJb
9. Cognitive defusion (deliteralization). (n.d.). Association for Behavioral Science. Retrieved from https://contextualscience.org/cognitive_defusion_ deliteralization
Navigating the Complexities of Migraine, Ménière’s Disease, Tinnitus, and Hyperacusis footnotes continued from page 55
1. L. Qi, Z. Jilei, Y. Lisheng, & J. Yuanyuan. (2024). Hyperacusis questionnaire and event-related potential correlation in migraine patients. Scientific Reports, 14(1), 14117. https://doi.org/10.1038/ s41598-024-65014-3
2. J. H. Hwang, S. J. Tsai, T. C. Liu, Y. C. Chen, & J. T. Lai. (2018). Association of tinnitus and other cochlear disorders with a history of migraines. JAMA Otolaryngology Head & Neck Surgery, 144(8), 712–717. https://doi.org/10.1001/ jamaoto.2018.0939
3. O. Moshtaghi, R. Sahyouni, H. W. Lin, Y. Ghavami, & H. R. Djalilian. (2016). A historical recount: Discovering Meniere’s disease and its association with migraine headaches. Otology and Neurotology, 37(8), 1199–1203. https://doi. org/10.1097/MAO.0000000000001122
4. B. Sarna, M. Abouzari, H. W. Lin, & H. R. Djalilian. (2020). A hypothetical proposal for association between migraine and Meniere’s disease. Medical Hypotheses, 134, 109430. https://doi.org/10.1016/j. mehy.2019.109430
5. K. K. Umemoto, K. Tawk, N. Mazhari, M. Abouzari, & H. R. Djalilian. (2023). Management of migraineassociated vestibulocochlear disorders. Audiology Research, 13(4), 528–545. https://doi.org/10.3390/ audiolres13040047
6. Y. Ghavami, H. Mahboubi, A. Y. Yau, M. Maducdoc, & H. R. Djalilian. (2015). Migraine features in patients with Meniere’s disease. Laryngoscope, 126(1), 163–168. https://doi.org/10.1002/lary.25344
7. A. Lee, M. Abouzari, M. Akbarpour, A. Risbud, H. W. Lin, & H. R. Djalilian. (2023). A proposed association between subjective nonpulsatile tinnitus and migraine. World Journal of Otorhinolaryngology Head and Neck Surgery, 9(2), 107–114. https://doi.org/10.1002/wjo2.81
8. J. A. Henry, S. M. Theodoroff, C. Edmonds, et al. (2022). Sound tolerance conditions (hyperacusis, misophonia, noise sensitivity, and phonophobia): Definitions and clinical management. American Journal of Audiology, 31(3), 513–527. https://doi. org/10.1044/2022_AJA-22-00035
9. H. R. Djalilian. (2024). Migraine—more than a headache. UC Irvine Otology, Neurotology, and Skull Base Surgery.
10. J. G. Ahmad & K. F. Lin. (2023). Meniere’s disease is a disorder of the inner ear. Current Opinion in Otolaryngology & Head and Neck Surgery, 31(5), 320–324. https://doi.org/10.1097/ MOO.0000000000000921
11. K. A. Brooks, K. Tawk, H. R. Djalilian, & C. E. Hobson. (2023). Migraine management for the otolaryngologist. Laryngoscope Investigative Otolaryngology, 8(4), 1080–1093. https://doi. org/.1002/lio2.1109
12. M. Frank, M. Abouzari, & H. R. Djalilian. (2023). Meniere’s disease is a manifestation of migraine. Current Opinion in Otolaryngology & Head and Neck Surgery, 31(5), 313–319. https://doi. org/10.1097/MOO.0000000000000908
13. P. Perez-Carpena, L. Frejo, & J. A. Lopez-Escamez. (2024). Meniere’s disease, a set of rare disorders with tinnitus. In W. Schlee, B. Langguth, D. DeRidder, S. Vanneste, T. Kleinjung, & A. R. Moller AR (Eds.), Textbook of tinnitus (pp. 399–411). 2nd ed. Springer.
14. O. Zagolski, P. Papiez, B. Kruk, & D. Kruk. (2023). Tinnitus characteristics in patients with hyperacusis and vertigo (including Meniere’s disease) vs. hyperacusis alone. Acta Otorrinolaringologica (English Edition), 74(1), 8–14. https://doi. org/10.1016/j.otoeng.2021.09.004
15. D. McFerran. (2018). Hyperacusis: Medical diagnoses and associated syndromes. In M. Fagelson & D. M. Baguley (Eds.), Hyperacusis and disorders of sound intolerance: Clinical and research perspectives, (pp. 107–131). Plural Publishing.
16. M. Abouzari, D. Tan, B. Sarna, et al. (2020). Efficacy of multi-modal migraine prophylaxis therapy on hyperacusis patients. Annals of Otology Rhinology and Laryngology, 129(5), 421–427. https://doi. org/10.1177/0003489419892997
17. S. C. Beh, S. Masrour, S. V. Smith, & D. I. Friedman. (2019). The spectrum of vestibular migraine: Clinical features, triggers, and examination findings. Headache, 59(5), 727–740. https://doi.org/10.1111/ head.13484
18. C. P. Campello, C. A. A. Lemos, W. T. L. Andrade, L. P. F. Melo, G. R. S. Nunes, & H. G. Cavalcanti. (2024). Migraine associated with tinnitus and hearing loss in adults: A systematic review. International Journal of Audiology, 63(1), 1–7. https://doi.org/10.1080/14992027.2022.2151943
19. T. Benjamin, D. Gillard, M. Abouzari, H. R. Djalilian, & J. D. Sharon. (2022). Vestibular and auditory manifestations of migraine. Current Opinion in Neurology, 35(1), 84–89. https://doi.org/10.1097/ WCO.0000000000001024
20. J. V. Vingen, T. Sand, & L. J. Stovner. (1999). Sensitivity to various stimuli in primary headaches: A questionnaire study. Headache, 39(8), 552– 558. https://doi.org/10.1046/j.1526-4610.1999.3908552.x
21. M. Abouzari, K. Goshtasbi, B. Sarna, et al. (2021). Adapting personal therapies using a mobile application for tinnitus rehabilitation: A preliminary study. Annals of Otology Rhinology and Laryngology, 130(6), 571–577.