

MODERNIZING HEALTH REGULATION IN BRITISH COLUMBIA

TRENDING
Artificial intelligence in licensing and professional regulation
GLOBAL INSIGHT
Ahpra regulates against racism in healthcare
Carin Plischke and Dianne Millette on the historic amalgamation and creation of two new colleges
Issue sponsor:
THE REGULATOR
The distinct attributes of regulating nurses in Canada's North





Issue 12 — Fall 2024
Journalists and Contributors
Damian Ali
Oluwatoyin Aguda
Dean Benard
Paul Byrne
Collette Deschenes
Jayde Fuller
M. Daniel Roukema
Graphic Designer & Production Manager
Allison Wedler
Editor in Chief
M. Daniel Roukema
Photo credits
Dean Benard
Jayde Fuller
Catherine MacIsaac Council for Licensure, Enforcement and Regulation (CLEAR)
MDR Strategy Group Ltd.
Adobe Stock
The Registrar magazine is produced and published by MDR Strategy Group Ltd.
800-1701 Hollis Street Halifax, Nova Scotia Canada B3J 2T9
editor@theregistrar.ca
www.theregistrar.ca
www.mdrstrategy.ca
© 2024. All rights reserved
From the Editor's Desk

Is it just me, or do we often get so swept up in the busy autumn months that we forget to pause and appreciate the beauty around us? The vibrant colours of the leaves, the refreshing crispness in the air, and that unmistakable pumpkin scent in nearly everything we consume. Meanwhile, our friends in the southern hemisphere are gearing up for summer—and let’s admit it, we’re a little envious!
We're thrilled to bring you the latest edition of The Registrar Magazine! This issue features insights from regulators around the world. We’re touched that Jayde Fuller in Australia collaborated with us, and thrilled to have had an insightful conversation with Paul Byrne from the Irish Medical Council. Beyond that, there’s advice from our trusted contributor and friend, Dean Benard, and we feature a deep dive into the unique challenges of regulating professionals across two jurisdictions in the North.
It’s conference season, and we tip our hats to the organizers of three incredible regulatory conferences: the Annual Education Conference of the Council on Licensure, Enforcement and Regulation (CLEAR) in Baltimore this past September, the International Association of Medical Regulation Authorities (IAMRA), also held in Baltimore, and the Canadian Network of Agencies of Regulation (CNAR) in Ottawa. Huge congratulations to everyone involved. Your hard work delivered meaningful discussions, learning, and collaboration, and we’re thankful to have been there.
On a personal note, I was touched to accept the Regulatory Excellence Team Award from CLEAR in Baltimore, alongside my amazing colleagues Collette Deschenes and Melissa Peneycad. I’m so proud of the passion and commitment our team brings to the table every day. The impact of their efforts is clearly reflected in the difference we’re making in the licensing and professional regulation sector.
Looking ahead, we’re gearing up for an exciting conference on artificial intelligence, set for Toronto in February 2025. I’d like to see you there! We’re expecting engaging presentations from esteemed speakers around the globe, including experts from the European Union, the Washington Medical Commission, and regulators from across Canada, who will focus on the profound impacts of AI on regulation and how we can protect the public interest in this new age of machine-driven decision-making and problem-solving. You can find more details on this groundbreaking event in this issue.
We hope you enjoy this edition, and as always, thank you.
M Daniel Roukema

IN THIS ISSUE
Assessing the rise of artificial intelligence (AI) in the regulatory sector.
A tale of four professions in two territories.
Meet the two regulatory leaders overseeing a new era of modern health regulation. 22 COMMUNICATIONS CORNER
Enhance your regulatory communications by building trust with stakeholders.

Highlighting the Australian Health Practitioner Regulation Agency’s commitment to eliminating racism from healthcare.

CLEAR’s AEC in Baltimore and MDR Strategy Group’s award for regulatory excellence.
Dean Benard, President and CEO of Benard + Associates, on investigating illegal practitioners.

Alycia Hunte on her professional journey in understanding human behaviour. 42
MDR Strategy Group's pre-CNAR conference sunset boat cruise.


Sam Lanctin, BPharm, MBA, ICD.D
DEI
in Regulation
FROM THE INDUSTRIAL TO THE IMAGINATIVE
Paul Byrne's deconstruction of AI and its impacts on licensing and professional regulation
The Registrar
Artificial intelligence (AI) has transformed numerous industries by enhancing operational efficiency, driving innovation, and enabling new business models.
In fact, AI was used to craft the introductory sentence above.
Including AI in workflows has sparked debate. The technology has slowly made its way forward in the regulatory sector, with regulators examining how to approach its use in operations. Paul Byrne, Executive Director of Regulatory Operations and Support Services at the Irish Medical Council, provides historical and contemporary insight on how AI could be applied in safe, legal, and ethical ways.
Distinct professional background
Byrne has helped advance regulatory developments for several years throughout his storied career. He was first introduced to regulatory environments and developed a fascination for using tech to optimize workflows, through his work at the Commission for Regulation of Utilities (CRU), where he worked multiple roles in customer complaints, regulatory policy, compliance and investigations.
Making a big career shift, Byrne decided to work in health. Before moving to his current role at the Irish Medical Council in 2023, he worked as head of registration for three years at CORU, Ireland’s regulator for health and social care professionals. It was an abnormal

start to his tenure at CORU, as the COVID-19 pandemic had just taken the world by storm.
“I came in just 10 days before COVID-19,” Byrne recalls. “Within the first week [at CORU] I had to very quickly reconstitute how we did registration in 18 days, which normally takes an unlimited budget and 18 months. Since then, I brought in new technologies such as SaaS to help automate registration processes, a first for a European country, and placed a renewed refocus on quality management and technology.”
Byrne attended University College Dublin in 2023, and earned his diploma, with distinction, in AI. He continues to study the impact of AI on the regulatory sector, having presented at numerous international conferences on the impact of technology on frameworks involving regulation.
Ethical impact of AI
Byrne asserts that the rise of AI in recent years is a powerful force and compares it to other key moments in history when technology significantly impacted society. “In the late 18th century, employers brought in cotton
milling technology, which eventually led to craftspeople revolting. The Industrial Revolution also demonstrated a shift in society’s response to integrating technology into [the consumer’s] life, but gradually allowed individuals to be reskilled.”
“The point of contention with AI is that this shift is happening in just 10 years, which will develop across every segment of society,” Byrne says. “How, then, do we rescale and retrain people to address this? I’m not sure there’s an immediate answer, and, with respect to regulation, our risk is that professionals will have to keep operating with updated skills and expertise in their practise.”
Byrne uses the example of COMPAS, or Correctional Offender Management Profiling for Alternative Sanctions, a decision support tool used by U.S. courts to determine the likelihood of a defendant reoffending, to highlight the need for careful training of AI platforms to ensure objectivity in assessments of individual profiles. “It was found, through bias-training data, that it disproportionately biased towards certain ethnicities. This impacts people’s lives, and we need to look at these historical examples so that the same mistakes aren’t repeated, especially where the stakes are huge.”
Recently elected President-elect of the Council on Licensure, Enforcement and Regulation (CLEAR), Byrne also Chairs the organization’s Technology and Innovation Task Force. Despite his passion for AI in licensing and regulation, he notes that the rapid pace of AI development has outpaced short-term, solution-focused efforts by those advocating for regulation.
“We need to come up with a higher-level governance principle here,” Byrne says. “In my role at the Task Force, our team will be putting together a high-level approach to using AI, closer to Q4, which is rooted in ethics rather than the technological side of things.”
Paul Byrne, Executive Director, Regulatory Operations & Support Services, Irish Medical Council
A future-friendly technology?
Byrne emphasizes that proper prompting is essential for effective AI use. The main area to address, he adds, is that feeding data to AI platforms must be assessed and applied with the right intentions, so that the platforms can mitigate harms and expedite solutions.
He affirms that it’s so much more about the philosophy than the speed, “this [application of AI in the future] needs to be done iteratively until there’s an actual regulator for AI on a national or global level.”
Knowing that AI will continue to change how regulators operate, Byrne stresses how important it is to understand how the systems are trained, how data is used, and how data will be audited. While certain standards and methodologies applied to assess data isn’t universal currently, he opines that it’s fundamental to create conversation spaces to discover applicable solutions.
“Sharing information and insights, and creating that sense of community among regulators internationally, will allow us to collect the right knowledge at the table so that informed decisions can be made from a fully dynamic and developed framework.”

“The point of contention with AI is that this shift is happening in just 10 years, which will develop across every segment of society.”
- Paul Byrne



Paul Byrne will be one of two in-person keynote speakers at the AI in Licensing and Regulation Conference in Toronto, Canada on February 11, 2025.
Paul Byrne will be one of two in-person keynote speakers at the AI in Licensing and Regulation Conference in Toronto, Canada on February 11, 2025.



















































































































































































































UPCOMING CONFERENCE

Global perspectives and local leadership
Industry leaders in AI, government, and the licensing and regulation sector from Canada and abroad will meet in February 2025 to discuss, discover, and determine the impacts and approaches to protecting the public interest in the new era of computer-generated reasoning, decisionmaking and problem-solving.
This critical meeting of Canadian regulatory bodies intends to provide a deeper understanding of AI’s use in regulation and its impact on professional standards, investigations, jurisprudence, communications, and complaints and discipline.

The Regulator
REGULATING NURSING IN THE NORTH
CANNN's vision for greater inclusion in public protection and nursing support
The Registrar
The Canadian North is a large, remote region, characterized by towering mountain ranges, vast boreal forests, icy coastlines along the Arctic Ocean, and the majestic Northern Lights painting the night sky with vibrant colours.
Communities are small and dispersed, with many residents in the region having deep, cultural ties to the land. Integral to the health care system in the Canadian north is the College and Association of Nurses of the Northwest Territories and Nunavut (CANNN), whose work is essential in maintaining the well-being of these communities across the landscape.
As the regulatory body for nursing in the territories, CANNN is responsible for ensuring that nursing professionals are competent, ethical, and able to meet the health care needs of the diverse and often isolated pop-
ulations in the north. A dual-mandate regulator, CANNN also serves as the voice of nurses in its jurisdictions.
The Registrar Magazine spoke with CANNN’s Executive Director and Registrar, Megan Wood. A Registered Nurse raised in Prince Edward Island and now longtime resident of NWT, she describes the organizational structure, transformation, and vision for the future.
A tale of four professions in two territories
CANNN has undergone several changes over the last four decades, with the organization originally established in 1975 as the Northwest Territories Registered Nurses Association (NWTRNA).

In 1999, the NWTRNA became the regulatory body and professional association for both the Northwest Territories and Nunavut, before becoming the Registered Nurses Association of Northwest Territories and Nunavut (RNANT/NU) in 2004.
New legislation in 2023 saw the creation of two new Nursing Profession Acts: The Nursing Profession Act of N.W.T. and the Nursing Professions Act of Nunavut and was renamed CANNN. The organization now regulates and speaks for Licensed Practical Nurses, Nurse Practitioners, Registered Nurses, and Registered Psychiatric Nurses.
Establishing a solid foundation
A name change was one of many new experiences for the organization in recent years, Wood says. After becoming executive director and registrar of CANNN in June 2024, she says that adjustments to leadership included updating Board structure and prioritizing Diversity, Equity and Inclusion (DEI).
“With the amalgamation of four designations, it also means that we want to bring them into the fold in the new board structure,” Wood says. “It’s a high priority for
“Not only are we looking at a person’s scope of practice in two jurisdictions, but there was also a requirement to consider what is included in both Acts for enforcement purposes, when it comes to professional conduct in those
jurisdictions.”
- Megan Wood

me to get LPNs and RPNs and have their voices heard. There is also the critical cultural aspect to the work we do, and if we don’t hear the voices of the public that we’re serving, then we’re not making informed decisions.”
The unique dual mandate structure of CANNN allows the organization to also expand team responsibilities. She says that a search is currently underway for a new director of quality practice, to enable CANNN to handle the volume of association-related responsibilities, while also engaging with the public to effectively protect the public interest.
Addressing unique complexities
Wood notes that the addition of two new nursing professions and two
distinct legislative acts being present was an initial challenge once CANNN was established.
“Not only are we looking at a member's scope of practice in two jurisdictions, but there was also a requirement to consider what is included in both Acts for enforcement purposes, when it comes to professional conduct in those jurisdictions,” she reveals.
Unlike most Canadian provinces, the North relies on nurses from other jurisdictions to fill their health care needs. Culture shock may take some from other provinces by surprise Wood emphasizes the need for those coming up north to be well-informed about the landscape, so that their practice can ultimately be successful. “When someone’s registered and they want to come up here to work, we want to ensure
Megan Wood, Executive Director and Registrar of CANNN
they are aware of the landscape they’re coming to and ensure they are in-the-know,” she adds.
The COVID-19 global pandemic required many regulatory authorities to institute new policies and practices for registrants to abide by to ensure public safety, and CANNN was no different. As a member of one of CANNN’s committees prior to assuming her existing role, Wood reflects that the pandemic disrupted their ability to find nurses due to travel restrictions.
Previously working in mental health and addictions recovery, and applying principles of public and cultural safety from past roles, she notes that creating opportunities for learning about the North was crucial. “In my personal experience
working on the frontline before this position, it [COVID-19] impacted my fitness to practice and ability to provide care,” Wood says. “Now that I’m at CANNN, it’s crucial to focus on member education, and how well they are being prepared before they walk into a community health centre with just one nurse responsible for the entire population.”
Traditional and new technologies to ommunicate
CANNN is committed to developing resources for members to stay engaged. This includes the quarterly CANNN newsletter which provides information on organizational activities, trends and issues in the North. Additionally, opportunities

"Now that I’m at CANNN, it’s crucial to focus on member education, and how well they are being prepared before they walk into a community health centre with just one nurse responsible for the entire population."
-Megan Wood
CANNN Staff (L-R) - Amelia Manuel, Director of Professional Conduct. Megan Wood, Executive Director and Registrar. Amelie Duval, Deputy Registrar
such as becoming National Council Licensure Examination (NCLEX) RN writers and reviewers, enable registrants to contribute to their profession beyond their clinical roles.
NCLEX tests the competency of nursing school graduates in the U.S. and Canada.
It's a key component of CANNN’s modernization efforts, and Wood says that it’s important to have those working in the North to have a better lens of both territories. Critical to the organization’s communication strategy is keeping members engaged with its media platforms. She adds that member education on areas like fees, for example, will demonstrate how certain standards contribute to a sustainable practise in both territories.
“Part of our communications-focused work will be to start getting more members engaged,” she explains. “It’s important for nurses to know what to expect in the north when working at CANNN, but also bring more members, volunteers and more eyes. This ultimately drives more public awareness, especially in nursing, where changes in healthcare, technology, and societal needs can significantly affect professional practice and standards.”
While CANNN is active on social media platforms like Facebook, LinkedIn, X, and Instagram, Wood points
out that radio is just as integral to communicate.
“One of the unique parts about being in the North is that a lot of small, underserved communities don’t have bandwidth, with a large amount of information being distributed by radio,” she reveals. “A big part of modernization at CANNN specifically, is making sure that if something noteworthy or important is going on, we air it on the public radio station while being creative and asking listeners for feedback or suggestions on what they want to hear.”
Ambitions of becoming a leader in nursing regulation
Despite having a small number of staff having to cover a large portfolio of work in four different nursing professions, Wood is positive that CANNN is equipped to stay on top of new developments and establish itself as a prominent regulatory leader in the field.
“I’m most excited about bringing us to the forefront of the sector, and ensuring that education for the public is just as engaging as education for our members,” Wood says. “CANNN is here as a resource to help nurses, and bringing awareness to who we are as an organization in this particular location will allow us to become a regulatory leader in this space.”


and professional regulation
CAREERS | VOLUNTEER POSITIONS | BOARDS/PUBLIC APPOINTMENTS | PROCUREMENT

PROTECTING THE PUBLIC THROUGH MODERNIZED HEALTH REGULATION
Through the lens of B.C.’s new regulatory college leaders
The Registrar
Modernizing licensing and professional regulation has been at the forefront of the health sector in recent years. Regulators are continually adopting new practices to update operations, streamline registration processes and enhance public safety, all to better fulfill their public protection mandate.
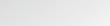
British Columbia has long led the modernization of regulation in Canada, with many regulatory colleges revising their practices. On June 28, 2024, two new colleges were es-
tablished by amalgamating several legacy regulatory colleges, with the goal of strengthening transparency and accountability within health profession regulation.
The Registrar Magazine spoke with the leaders of these two new colleges: Registrar & CEO of the College of Health and Care Professionals of B.C. (CHCPBC), Dianne Millette, and Registrar & CEO of the College of Complementary Health Professionals of B.C. (CCHPBC), Carin Plischke. Both respected leaders with decades of experi-
ence in the sector discussed how the new colleges were created, and what the public can expect in this new era of modern health regulation.
Years in the making
The idea of amalgamating multiple health regulators in B.C. into two separate colleges was part of an exhaustive process years in the making. In 2018, B.C.’s Ministry of Health (MOH) began a multi-year initiative to modernize regulatory frameworks ensuring health profes-


CCHPBC Ambassadors Group: Volunteers came together to welcome staff to the new office space and help them navigate it
CHCPBC Coast Salish blanketing ceremony

sions were regulated more consistently. In March 2019, an inquiry into the College of Dental Surgeons of British Columbia was spearheaded by the Ministry. Harry Cayton was directed to do the investigation by the minister, eventually leading to amalgamation being legislated.
“Voluntary amalgamations weren’t new, such as when the College of Registered Nurses of British Columbia amalgamated with two other nursing professions a year prior, before inevitably amalgamating with the midwifery profession,” Millette says. “Our colleges’ particular amalgamation, however, were mandatory.”
Plischke, the former registrar, CEO, and previous board member of the now-defunct College of Occupational Therapists of B.C., recalls that the pre-planning phase of amalgamation was meticulous. “Going to numerous events and hearing about the vision for modernizing health regulation, pre-COVID-19, was inspiring,” she says.
In August 2020, the MOH-led Steering
Committee on Modernization of Health
Professional Regulation issued recommendations to update the province’s health professions regulatory framework. Significant findings from the Cayton report and public consultations highlighted the need for health profession regulators to:
• Commit to cultural safety and humility
• Improve governance
• Improve efficiency by reducing the number of regulatory colleges from 20 to six
• Strengthen oversight
• Simplify complaints and discipline processes
• Share information to improve patient safety and public trust
As a result, in April 2023, the Deputy Minister sent a letter to the boards of each legacy regulatory bodies announcing that two colleges —one overseeing seven professions and the other four— were to be established in June 2024. Alan Seckel was appointed by the ministry as the amalgamation lead to support boards
In a priority setting session, the CCHPBC leadership team identified areas that will be the College’s main focus for the upcoming 6-8 months.
during the transition. In September 2023, Seckel appointed Joanie Bouchard, former registrar of the College of Dietitians of British Columbia, as chief transition officer. Bouchard worked with a project consultant team and some staff from the amalgamating colleges to develop project charters and assist with various aspects
of the transition.
In 2024, months of hard work came to fruition with the names of both colleges confirmed and Dianne and Carin appointed registrars and CEOs in February. Boards for both colleges were appointed in March, with consultations on required bylaws running from April until early


Timeline of the multi-year initiative to amalgamate multiple provincial health regulators
June before the CHCPBC and CCHPBC were legally amalgamated and formally opened on June 28.
Millette explains that her passion in the new position stems from a deep interest in licensing and professional regulation. With over 20 years of experience in regulatory roles in both Canada and the U.S., she saw leading the CHCPBC as a rare opportunity. “I really saw this as a once-in-a-lifetime opportunity” she says. “To lead an organization like this was an unprecedented opportunity, being committed to public service and safety as long as I have.”
Plischke echoes a similar sentiment, explaining that her enthusiasm for role stems from the opportunity to collaborate more directly with other health regulators. “We typically don’t work in isolation within this sector,” Plischke notes. “The delivery of safe health services from licensees presents a unique opportunity to show how team-based care can be done through consistent, enhanced collaboration.”
Prioritizing the public
When it comes to governance, both Millette and Plischke emphasize the importance of having a balanced split of members of the public and regulated professionals on the boards of both colleges.
“Our college’s board involves fifty per cent public members, with the other fifty per cent coming from legacy colleges,” Millette says. “Public service will be the main objective of our board and committees, instead of representation, as profession-specific expertise is embedded in our staff and committees.”
Plischke says that fifty per cent public representation on the board allows regulators to create new methods of fulfilling their public protection mandate. “As we continue building out our operations and outreach, our goal is to eventually have a governing board of directors, along with fulfilling our commitments to cultural
safety, humility and anti-racism,” Plischke says.
Measuring public impact
A key area of focus for Millette and Plischke is cultural safety, humility, and anti-racism, where each college prioritizes eliminating racism from policies, while actively working to create conditions that promote greater inclusion, equality and justice.
“We’ve established an office for social accountability, which embeds diversity, equity, inclusion (DEI), decolonization and justice principles into our work,” Millette says. “Our relationships with Indigenous Elders and Knowledge Keepers ensure board activities remain aligned with Truth and Reconciliation efforts already established by legacy regulators pre-amalgamation, such as territorial acknowledgements and approving guidelines for working with Indigenous Elders.”
Both Millette and Plischke sit on the Executive Committee of B.C. Health Regulators, which brings together B.C.’s health regulatory colleges to collaborate on improving regulation and regulatory practice across their organizations. Plischke highlights that this collaboration is crucial, so that mechanisms can be shared that will help to eliminate racism and discriminatory behaviours from the health care system to improve pa-

CCHPBC employees participated in a fun scavenger hunt activity to celebrate a successful amalgamation and to acquaint them with their new office and its location.

tient care and ultimately achieve public safety.
Millette explains that collecting registrant data will be crucial for CHCPBC moving forward. Drawing on her experience supporting the development of Ontario’s College Performance Measurement Framework (CPMF), she notes that CHCPBC is collaborating with the Canadian Institute for Health Information to identify what’s appropriate and ethical to collect, and how data will be integrated into regulatory standards and processes.
“We’re aiming to become more informed about our registrant population as a start, so that we can ensure that we’re both inclusive of those working across these various health professions and able to measure impact down the line,” she says. “Once we get through the initial phase of harmonizing our processes, the next step will be to really assess the measurements of those outcomes,” she adds.
The vision ahead
CHCPBC is an amalgamation of seven legacy colleges and regulates nine professions, with one legacy college regulating three distinct professions. Millette notes that this raises several important questions that CHCPBC is eager to address.
“First, how does the regulator hear from the various publics that are being served? It’s fine to have public representation on our board, but to hear from the broader public, it’s important to learn from our international colleagues who’ve overseen multi-disciplinary jurisdictions for a long time. The other important task ahead is to find a way of responding to compliments, instead of just concerns. We have a lot to learn from people who just want to share an experience, good or bad, as this is crucial for modernization efforts.”
Ultimately, Plischke’s vision as registrar & CEO is to have a multi-disciplinary, team-based health care regulator that supports a mandate of ensuring health professionals practise in a way that is safe for the public. “It’s really about decreasing confusion for the public and being efficient in the little, but important things,” she says. “For example, how do we get consent to provide services? As a modern regulator, I’m excited about CCHPBC demonstrating leadership in this area, which inevitably encourages public

safety.”
With new legislation - the Health Professions and Occupations Actset to come into force in 2025, both Millette and Plischke are thrilled to continue supporting licensees in transitioning to the requirements of this new Act. Plischke emphasizes the evolving importance of demonstrating how well multi-disciplinary regulators can work under one framework with measurable outcomes, a perspective Millette shares.
“There’s a lot of work to be done. However, the future is bright and, in time, we will demonstrate to the public what is possible with modern health regulation,” Millette concludes.
CHCPBC Registrar & CEO, Dianne Millette
CCHPBC Registrar & CEO, Carin Plischke
IS YOUR COMMUNICATION BUILDING TRUST OR CREATING BARRIERS?
Kindness in regulatory communications
Collette Deschenes

Imagine you’ve missed the deadline for your annual renewal with a regulatory body. You receive an email informing you and the tone of the communication
Now imagine the same scenario except you receive the notification written in plain language, with an understanding tone, clearly outlining the steps you need to take to remedy the situation.
The difference in your response was
likely significant. The first scenario, receiving a communication with a stern tone, may leave you anxious and defensive. The second scenario likely leaves you feeling more supported and compelled to address the situation.
This is one of many examples highlighting how regulatory communications can either build bridges or create barriers. The language, voice and tone we use can help cultivate a sense of support, openness, trust
Collette Deschenes, Director, Communications Strategy, MDR Strategy Group
and transparency. On the other hand, it can create evoke the opposite reaction and lead to negative perceptions of the regulator.
Know your stakeholders
As a communications professional, one of the first things that comes up when crafting messaging that helps to build bridges is the principle of “knowing your audience.” This has been ingrained in me since my days in public relations school where they consistently emphasized this critical part of PR practice.
Within the context of regulatory communications, and particularly when we talk about kindness in your organization’s communications, we often need to think beyond target audiences. We’re typically communicating with individuals and groups who have a vested interest in and varying levels of influence over the regulator’s decisions, changes and policies. In this case, we want to “know your stakeholders.”
This starts with identifying your stakeholders but it’s critical to go deeper. Recognize that each group and individual will have their own perceptions and relationships with your organization. Aim to understand what they care about and what challenges they may be facing. Our team frequently supports regulatory bodies by auditing the organization’s communication using our regulatory lens and expertise. We thoroughly examine all communications and engage comprehensively with stakeholders to understand their needs and identify any gaps or challenges.
The audit is a foundational step as it provides crucial insights into stakeholder perceptions. This understanding is typically the starting point for ensuring that the regulator’s communication is strategic, aligned with their mandate and reflects kindness.
But this isn’t a one-time engagement effort. We also provide recommendations that encourage ongoing dia-
logue with stakeholders – one that helps build trust and strengthens relationships over time.
Review your organization’s voice and tone
As we review communications, we closely examine the voice and tone of a regulatory body’s communication to identify any inconsistencies and ensure alignment with its mission, vision, and values. This review also helps to ensure the voice and tone is approachable, supportive and reflects kindness.
First, consider this: Does your organization have a cohesive voice? Your voice should be consistent across all communication and should align with your mission, vision, and values. For example, if your organization values transparency, your voice should always reflect this by being open and clear. This means that your communication will provide accessible information without jargon and aim to ensure that stakeholders understand your organization’s decisions, initiatives and policies.
Your tone adjusts based on the context of the communication. For example, the tone of a professional conduct communication will vary from a social media post highlighting your organization’s latest newsletter. Regardless of the context, the tone should convey a commitment to helping stakeholders, like registrants, navigate their responsibilities and challenges.
So how can you ensure your organization’s voice remains consistent, that the tone adapts appropriately, and that they both reflect kindness and empathy? After reviewing your organization’s communication and identifying gaps or inconsistencies, decide on the key characteristics of your voice. Use those characteristics to develop voice and tone guidelines to apply across all communications.
Remember that trust is built not only through what we say but also how we say it. How you communicate will
either reinforce trust and build relationships with stakeholders or create barriers that can lead to confusion, frustration or disengagement.
Identifying stakeholder communication needs and creating consistent voice and tone principles are just two actionable ways to shift to kind, connection-driven communication. As you know, this shift takes time. It requires alignment and agreement on a unified approach across the organization. It’s never a one-time effort but it’s an effort that reinforces your organization’s commitment to regulatory excellence, continuous improvement and most of all, kindness.
Are you ready to enhance your regulatory communications?
MDR’s regulatory communications expertise can support your organization in building trust, improving stakeholder relationships, and achieving your communication goals.
Join other regulators who choose the MDR solution to deliver their messages with meaning and purpose.
www.mdrstrategy.ca




Global Insight
AUSTRALIA IS REGULATING AGAINST RACISM IN HEALTHCARE
Jayde Fuller, National Director, Australian Health Practitioner Regulation Agency (Ahpra)

Globally, there’s been an escalation of white supremacy culture which seeks to silence dialogue and discredit thought leadership around racism, diversity, equity and inclusion.
This serves to maintain the status quo by upholding power within non-Indigenous structures, systems and stakeholders. White supremacy culture poses a threat to our regulatory remit of protecting the
public, by selecting which communities are worthy of protection and safety and ignoring or failing to take action to protect or redress harm to those who aren’t.
I work at the Australian Health Practitioner Regulation Agency (Ahpra) in partnership with the National Boards and accreditation authorities, and we’ve gone against the tide of white supremacy culture by remaining committed to eliminating racism from healthcare for
Jayde Fuller, National Director, Australian Health Practitioner Regulation Agency (Ahpra)
Aboriginal and Torres Strait Islander Peoples.
The Australian context
Australia has a total population of 25.69 million people, with the total Indigenous population accounting for 3.8%, just under 1 million people, drawn from 500 separate nations with different languages and histories.
There are two distinctly separate First Nations groups in Australia, Aboriginal people who inhabit the mainland and Torres Strait Islander people who are custodians of the chain of islands in the Torres Strait region which is positioned between the state of Queensland and Papua New Guinea.
We have occupied Australia for 65,000 years, and have one of the longest, continuing cultures in the world. The country was colonised by the English 254 years ago.
Colonisation in Australia was justified by the false legal status of ‘terra nullius’ meaning ‘nobody’s land’ in Latin justifying claims that territory may be acquired by a state's occupation. The history of colonisation included seizure of land, massacres, removal of children from their families, displacement from tribal lands onto reservations, unpaid labour known today as Stolen Wages of which many hospitals and health infrastructure was built from, assimilation, and more recently reconciliation.
Aboriginal men and women live on
average 10 years less than the non-Indigenous population, have higher suicide rates and are impacted by a higher burden of disease in relation to mental health, cardiac-related and chronic disease. The population is largely a younger one with a significant proportion being under 29 years old.
On October 14th 2023, we had a referendum in Australia seeking to establish an Indigenous voice to Parliament to be enshrined into our constitution, a mechanism that would allow Indigenous Peoples to advise the government on matters that affect us.
60% of Australians voted against this and the state I reside in of Queensland, had the highest ‘no’ vote of all the states and territories in the country.
Resulting in a resounding message to Aboriginal and Torres Strait Islander Peoples that we are not viewed by the majority of Australians as valuable citizens who should be able to have a say over decisions that impact our lives. Racism is inherently about power within society—wielded collectively by those who have it - against those who don’t.
Faced with these results, how could one not accept that Australia is indeed a racist country?
In 2020, we released the National Scheme’s Aboriginal and Torres Strait Islander Health and Cultural Safety Strategy 2020-2025 – which set the strategic and operational priorities to move us towards the elimination of racism.
"Although progressing cultural safety and anti-racism work is a challenging space to be in, you need to understand that this work is life-long and must be self-determined by us as Indigenous Peoples. " – Jayde Fuller

The most impactful actions in this strategy can be broadly categorised under the following verbs - define, legislate, educate, participate and govern.
Define: language matters
In 2019, we standardized the definition of ‘cultural safety’ through a six-week community consultation which was decided upon by the Aboriginal and Torres Strait Islander Health Strategy Group and peak Indigenous body the National Health Leadership Forum.
Having a common, cross-profession (we regulate 16 health professions), definition aligned with our core purpose as a regulator of patient safety and asserts that cultural safety is self-determined by Aboriginal and Torres Strait Islander Peoples, families and communities.
Working in partnership with our National Boards and accreditation authorities, it allowed us to change practitioner’s codes of conduct and accreditation standards at scale and pace, driving accountability around cultural safety to measure performance using a number of regulatory mechanisms.
Legislate: landmark decision
Leveraging off the definition, in October 2022, we passed the expectation of it into law in relation to service provision, access and workforce capability. This time explicitly mentioning through the guiding principle that the workforce needs to ‘contribute to the elimination of racism.’ It was the first time the word ‘racism’ has been featured in healthcare legislation in Australia. We’re now able to hold practitioner’s accountable at tribunal for the most serious misconduct relating to racism against Indigenous health consumers and practitioners. This includes practitioners experiencing racism from other practitioners.
Jayde Fuller, National Director, Australian Health Practitioner Regulation Agency (Ahpra)
Medical Board of Australia vs CDA –landmark decision
Last year, we had a landmark tribunal decision on anti-Indigenous racism made in the medical profession - resulting in a non-Indigenous doctor’s behaviour being constituted as professional misconduct. He was prohibited from providing any health service and cannot apply for registration for 12 months.
A racially offensive email was sent to Prof Rallah-Baker, former Australian Indigenous Doctors Association and highly respected, Yuggera, Warangoo and Wiradjuri ophthalmologist. The Tribunal found that he was treated less favourably than other persons because of his racial background and had the potential to bring the medical profession into disrepute.
The Chair of the National Medical Board, Dr Anne Tonkin said, ‘this ruling is a clear message that racist and culturally unsafe practice and behaviour is unlawful and carries substantive penalties, including disqualification from registration.’
Educate: how to practice cultural safety
Between 2021 and 2023, an Indigenous owned consultancy PricewaterhouseCoopers Indigenous Consulting delivered Moongmoong-gak cultural safety training to almost 1,800 Board, committee
and staff members. This education program was the first of its kind globally for health regulators and aimed to really plant the seeds of what culturally safe practice means for regulatory administrators – the start of a lifelong commitment.
It sets an important precedent that we’re willing and able of practicing what we preach in requiring ongoing learning in culturally safe practice for Aboriginal and Torres Strait Islander Peoples. In the near future, it’s very likely we will expect all practitioners to commit to learning on cultural safety throughout their learning and practice years.
Importantly, it also begins the unlearning process, challenging the lies and preconceptions of who we are as Indigenous Peoples – the ideologies developed and reinforced through the colonial project. This directly impacts how we’re treated.
Participate: representation matters
Having an Indigenous employment strategy has been critical for us and has increased the level of participation of Aboriginal and Torres Strait Islander Peoples in Ahpra. However, more work needs to done with the agency still needing to improve its understanding of what attracts us to work in regulation, the nuance of Indigenous recruitment, how to retain us and address unsafe con-
duct or racism in the workplace.
In 2021, we established the Aboriginal and Torres Strait Islander Health Strategy Unit (HSU) and it’s 100% Indigenous led and staffed.
We also established an Aboriginal & Torres Strait Islander Support and Engagement Team (Indigenous registrations) who assist Indigenous practitioners with registration and broader workforce issues. They’re a front door to Ahpra, often the first contact. They help to redirect practitioners to the right place in the agency in a responsive way.
Importantly, we've increased our representation on Boards and committees.
Govern: selfdetermination in action
Culturally safe regulatory decisionmaking
Changes to governance structures that places us at the centre, in a self-determining way is most evident in the larger reform project deliverables of the Culturally Safe Notifications Project and the Culturally Safe Accreditation and Continuing Professional Development Project. Both projects are informed by working groups comprised of Aboriginal and Torres Strait Islander health practitioners, leaders and community members.

We’ve successfully established a medical and nursing and midwifery regulatory decision-making committees comprised of Aboriginal and Torres Strait Islander Peoples who decide on whether to take regulatory action on all matters that involve an Indigenous person.
Another key project milestone has been the recruitment of the Aboriginal and Torres Strait Islander Peoples to support Indigenous complainants through the process and to provide cultural advice to investigators.
We know that collecting data is important for quality improvement and measuring cultural safety effectiveness – we engaged Yardhura Walani an Indigenous led and governed research centre at the Australian National University to undertake focus groups with Aboriginal and Torres Strait Islander Peoples who've gone through our complaints process.
Cultural Safety Accreditation and Continuing Professional Development Project
In regulation, ideally we’d like to prevent harm from occurring. In taking a preventative lens, we've committed to develop a sector-wide national cultural safety and
accreditation framework and strategy for all the practitioners we regulate.
We hired Weenthunga Health Network to deliver the project milestones, a Victorian based Aboriginal and Torres Strait Islander owned and run organisation, that supports the upholding of health sovereignty and progressing health justice.
It's a big paradigm shift for non-Indigenous allies to give up power in regulatory spaces, and accept that just because it's their way of doing business, it's not the only way of doing business, and to trust we are fully capable of achieving meaningful change if we're supported to lead.
Although progressing cultural safety and anti-racism work is a challenging space to be in, you need to understand that this work is life-long and must be self-determined by us as Indigenous Peoples. We’ve had enough of being told by non-Indigenous Peoples how we can be ‘fixed.’ I urge you to appreciate that trust and relationship building with Indigenous Peoples will take time and you’ll inevitably get it wrong, but if you respond with humility and you take the time to critically self-reflect on your discomfort, this will set you up for success as you embark on your anti-racism regulatory journey.
Click here to find out more about the National Scheme’s Aboriginal and Torres Strait Islander Health and Cultural Safety Strategy.
This article is a contribution from Jayde Fuller, National Director, Aboriginal and Torres Strait Islander Health Strategy Unit Strategy, Policy and Health Workforce from the Australian Health Practitioner Regulation Agency (Ahpra).
Jayde Fuller, Ahpra (left), Kym Ayscough, Ahpra (centre), Linda Renouf, Medical Board of Australia, (right)


CLEAR ANNUAL EDUCATION CONFERENCE
September 2024, Baltimore, MD







September 2024, Baltimore, MD



Investigator Insights
INVESTIGATING ILLEGAL PRACTITIONERS: STRATEGIES, CHALLENGES, AND INSIGHTS
Understanding the issue
Dean Benard, President and CEO Benard + Associates

Illegal practitioners are individuals who offer professional services without the necessary licenses or credentials, posing significant risks to public safety.
These unlicensed professionals operate across various fields, including a multitude of healthcare professions, law, engineering, social work, and the list goes on. They will employ a variety of deceptive tactics to avoid detection. Most will use occupational titles such as “doctor,” “lawyer,” or “psychologist,” which are interpreted by the public as a sign of special expertise or qualification.
The consequences of illegal practice can be severe, ranging from inad-
equate healthcare, physical harm, financial exploitation, and substandard construction that poses public risk. Illegal practitioners not only endanger public safety but also undermine trust in the professions they impersonate. They often prey on the most vulnerable segments of society, including new immigrants, economically disadvantaged groups, and those who may not have the knowledge or resources to verify the credentials of their providers.
Investigation challenges
These cases can pose many challenges and investigators need to think carefully about the approach
Dean Benard, President and CEO, Benard + Associates
they take, not only to get the evidence, but to avoid making the challenge greater by alerting the subject they are being watched.
Illegal practitioners often exploit community ties or create complicit networks that make it difficult to detect their activities. For example, some illegal practitioners operate exclusively within their ethnic communities or rely on personal referrals, which reduces their exposure to the authorities. In one case, an unlicensed dentist was able to operate for an extended period by only accepting clients through community referrals, thereby avoiding detection. These scenarios can lead to non-cooperation as witnesses, employers, or community members may be unwilling to cooperate, due to fear of repercussions or legal implications, or even because they want to protect the practitioner because, like it or not, it is all they (individual or community) have available.
Finding where an illegal practitioner is operating can be difficult, especially when they are mobile or working across multiple jurisdictions. In another instance, a woman with revoked nursing registration forged documents to gain registration / licensure in multiple jurisdictions, demonstrating the lengths to which some of these fraudsters will go, to bypass regulations. So now we are investigating a person who is practicing illegally but appears to be legal and hops for province to province and even other countries to keep going, trying to stay one step ahead of the investigator, who might not have the authority to investigate in all jurisdictions. This means regulators must work cooperatively and share information, as well as involve other agencies including immigration and the police.
Some illegal practitioners are hiding in plain sight, by making use of fabricated references, fake backgrounds, or identity theft. I once investigated an illegal practitioner who assumed the identity of her dead sister and openly practiced as a nurse in a hospital with no nursing education whatsoever. It was by pure luck, that a distant friend of the deceased sister discovered the is-
sue, but not until that illegal practitioner provided “care” to hundreds of people over two years, shockingly without being detected.
Investigative tactics and strategies
The investigation of illegal practitioners requires a creative and multifaceted approach. The goal is to obtain evidence that shows the individual is engaged in one or all the following behaviours:
• Holding themselves out as qualified to practice.
• Using a protected title or designation.
• Performing acts restricted to licensed professionals.
Evidence can be gathered from documentation such as advertising, client files, or human resources records. Interviews with coworkers, employers, and clients, as well as surveillance and undercover operations, are also a key component to the evidence gathering process.
Additional strategies involve:
• Following suspects and observing their activities.
• Engaging suspects by requesting their services.
• Infiltrating agencies where the suspect may be working.
• Other tactics we won’t share in this article, to keep what little tactical advantage we can.
The extent of undercover operations can be significant. In one case several years ago one of our investigators (the author) posed as a tourist to catch a healthcare provider practicing in a small tourist community in northern Ontario. This involved staging an accident so locals would bring the investigator to the practitioner for treatment. This allowed the investigator to obtain firsthand evidence, which was captured on hidden audio and video recorders. Had the investigator just showed up looking for treatment, it would have been highly suspicious.

To address the investigative challenges, investigators may need to exercise the powers available to them, such as obtaining search warrants (not always easy to do) or leveraging the influence of other agencies (e.g., insurance companies, or public health organizations). Appealing to employers’ sense of morality or reassuring them about their legal standing can also help gain cooperation.
To determine where an illegal practitioner might be working, investigators might use pretext calls, surveillance, social media searches, determining the geo-tagging of photographs can also help identify the location of suspects. It is a range of approaches that must be employed to complete these investigations successfully. This article is not meant to explore these strategies at length, as some level of discretion is important, so our tactics are not widely known.
Legal considerations and prevention
The options available to combat illegal practice include cease and desist orders, criminal or quasi-criminal prosecution, and injunctions (civil court orders). Cooperation agreements, like memorandums of understanding (MOUs), can facilitate information sharing and resource allocation across jurisdictions and between agencies, but this is also surprisingly challenging in many cases.
Prevention strategies focus on making it harder for illegal practitioners to operate. This includes moving away from physical licensure cards (forcing online verification instead), educating prospective employers, and publicizing the identities of known offenders through press releases following successful prosecutions or civil injunctions.
Many regulators are assertive in this regard and creating greater public awareness. However, despite these efforts the problem runs deep and rooting out these bad actors will take an extreme level of effort, which arguably most regulators are not resourced enough to undertake. So, prevention efforts and reactive investigations when illegal practitioners are identified through complaints, remains the primary approach to managing this problem.
Another consideration is the fact that despite prosecution or court orders, these illegal practitioners must be monitored to ensure they don’t start practicing again.
The need for vigilance and cooperation
Investigating illegal practitioners requires persistence, creativity, and strategic collaboration between regulatory bodies, communities, and law enforcement. Successful investigations depend on a combination of innovative tactics and the ability to adapt to evolving challenges. Public awareness and engagement are also
critical in safeguarding against these fraudulent activities, making it essential for everyone to stay informed and vigilant.
Case study
• A person (later identified as having some experience as a veterinary assistant) is reported to be advertising a mobile service where they can come to peoples’ homes and spay or neuter people’s cats and dogs
• This person advertises within a narrow community in in their native language
• When this is reported and the advertisement is examined, searches of public registers in several provinces is undertaken, and the person in question is not registered as a veterinarian
• A translator is engaged and given a script to engage the person by phone (call recorded). The script conveys that she operates a daycare in her home and can’t have him to her home to spay her cat… she asks if she can bring the cat to him
• The illegal practitioner agrees and offers the service and advises of his home address, the cost of the service, and a date and time to attend
• The investigator arrives at the home of the illegal practitioner and says his mother will arrive with the cat in five minutes
• A prearranged call is made to the investigator that he answers in the presence of the subject. The investigator reports to the illegal practitioner that his mother was in a minor car accident and won’t be able to attend
• The investigator asks if they can reschedule and offers to pay half the 200-dollar fee now and the rest when they return another day
• All of this is captured on an audio recording
• While at the home the investigator gathers photographic evidence of the coffee table which is set up as an operating table with scalpels, retractors etc.
• All this information is used to apply for
a search warrant, which is granted
• On the date scheduled to return with the cat*, the investigator brings the police to keep the peace and safety, and executes the warrant, gathering all the evidence needed to prosecute the illegal practitioner
• There was no sterilization equipment on site and some instruments had stains on them
• The illegal practitioner was charged under the Veterinary Act and was also brought to civil court, where an injunction (court order) was obtained ordering him to cease and desist
*No cats or any animals were involved or harmed in the investigation ☺

The Registrant
FROM RECE TO RP: THE INTERSECTION OF HUMAN BEHAVIOUR IN TWO DIFFERENT CAREERS
Meet one of the College of Registered Psychotherapists of Ontario’s newest registrants
The Registrar
Alycia Hunte's journey from early childhood educator to registered psychotherapist has been an evolving journey of a passion for understanding human behaviour.
Her career began unexpectedly when she took a temporary role in childcare while her then-husband transitioned to a new career. What started as a short-term
gig became a quarter-century-long professional metamorphosis.
A resident of the Ottawa region, Hunte was born in Montreal and spent her adolescent years in Toronto. Now, a mother of two, she worked worked at several childcare centres over the years, gaining experience with various age groups and refining her ability to sup-

port children’s emotional and developmental growth, in addition to teaching. Eventually, she transitioned to home childcare, taking on a supervisory role where she focused on policy compliance and provided guidance to other childcare providers.
Despite the rewards of her role, Hunte found that the growing administrative responsibilities began to overshadow the aspects of the job she enjoyed most: interacting with children and families. Her passion for
psychology and desire to work more closely with individuals on an emotional level led her to pursue a career in psychotherapy.
"The part I enjoyed most in my previous roles was interacting with people, learning about their lives, and helping them navigate their challenges,” Hunte reflects. Moving into therapy felt like a continuation of that journey.”
Alycia Hunte, former Registered Early Childhood Educator, now Registered Psychotherapist
"The
part I enjoyed most in my previous roles was interacting with people, learning about their lives, and helping them navigate their challenges,” Hunte reflects. Moving into therapy felt like a continuation of that journey."
– Alicia Hunte
Confronting challenges of stigma and demographic nuances
Registered with the College of Psychotherapists of Ontario (CRPO) since March 2022, Hunte completed her Counselling Psychology Masters from Yorkville University in November 2022, holding the title of (RP Qualifying). In April 2024, she became a fully licenced Registered Psychotherapist (RP) with the CRPO. In practice in downtown Ottawa, Hunte sees a range of clients, including children, adolescents, and adults. She explains that working with children, particularly those aged seven to ten, presents unique challenges as they navigate important developmental transitions. While she also works with adolescents, she notes that their engagement with therapy tends to be less consistent.
Hunte’s practice also includes a significant number of women in their thirties,

a stage that she describes has a tremendous impact. "This phase seems to be a turning point for many women,” she says. “It’s a pivotal time in their lives as they start coming to terms with what they want to do next. They’ve gone through their youth and now want to shift towards healthier choices."
She observes that it’s an interesting dynamic with men who are less frequent clients in her practice. "When men do seek therapy with me, it's often because they have a strong relationship with their mother, which makes them more comfortable talking to a woman, or they feel uneasy discussing their issues with a fellow man. There's often a hesitation to open up in therapy. Even male colleagues in the field say they don’t see many male clients. It seems to be rooted in the belief that men should be able to figure things out on their own, without needing help.”
Although the stigma surrounding therapy has lessened over the past decade, Hunte notes there's still a pervasive idea that seeking therapy means admitting an individual can't handle things by themselves. This mentality she admits, although prevalent among men, is also present in women. “Many people delay seeking therapy because they believe they should be able to solve their problems alone. For many men, expressing emotions, especially to someone outside their family, can be challenging. The notion of showing vulnerability in front of someone who isn't close can be particularly difficult for them."
As she transitioned into psychotherapy, Hunte embraced a client-centred ap -
Alycia Hunte, Registered Psychotherapist

I ask them what they’re looking for,” she says. “We work together to find an approach that resonates with them, because therapy isn’t one-size-fits-all.”
Title protection
As a CRPO registrant, Hunte explains that professionals in her field in Canada practice under protected titles. This ensures that professionals are trained to a high degree of competence, allowing clients to feel safe when their needs are addressed.
“You can’t just get someone to open up their trauma and then leave them [after a couple of sessions],” Hunte says. “There are certain procedures present to keep people safe, especially when you’re dealing with highly traumatized people who are, for example, homebound. Is the professional on the other end exposing their client to certain safety protocols and standards, as well as ensuring they are being kept safe? Sometimes, that doesn’t always happen which could unintentionally result in harm.”
As with most professions, registered psychotherapists
in the province of Ontario are required to take a set number of professional development training hours annually. Hunte looks forward ensuring she remains informed about the latest treatment methods and research. "Supervision is key,” she says about learning to manage complex cases and maintaining high standards in her practice. “We have guidelines to ensure continuous education and supervision, particularly for challenging cases. Therapists are naturally curious. We're constantly reading articles, exploring new modalities, and discussing approaches with peers.”
Hunte’s career shift from early childhood educator to psychotherapist is testament to her commitment to understanding and supporting others. Her experiences have shaped her client-centred approach, allowing her to provide meaningful guidance and support to individuals across various life stages.
“I love where my life has taken me,” says Hunte. “We all have a past we would like to change, but this journey has been right, and I’m thrilled.”

Alycia Hunte, former Registered Early Childhood Educator, now Registered Psychotherapist



MDR Strategy Group's pre-CNAR sunset boat ride for clients, colleagues, and friends








October 7, Rideau Canal, Ottawa








Our Communications on Retainer (CORe) program enables regulators with limited resources or temporary capacity constraints to retain MDR Strategy Group to support new and ongoing communication priorities.
