In this issue



Dear ACCE Community,
As Fall begins, with children back in school, football games starting, pumpkin-spice everything, and cooler weather (or at least less hot if you’re in South Texas like me!), it is also time for a new year for ACCE!
First, thank you for electing me as your President; I am incredibly honored and filled with gratitude to step into this role for the upcoming year. I extend my deepest thanks to the outgoing Board members, Qusai Shikari and Arif Subhan for their leadership and contributions. I also want to thank Kim Greenwood, Ilir Kullolli, and Arif Subhan for mentoring and guiding me to this position and whose dedication and direction have brought ACCE to this point. Your efforts have laid a strong foundation upon which we will continue to build!
Welcome, 2025 - 2026 ACCE Board members and Committee Chairs! Your energy, expertise, and commitment are vital to ACCE’s success, and I appreciate your willingness to volunteer your time. Continuing on the Executive Board are Suly Chi (Secretariat), Michele Manzoli (Secretary), while taking on new roles are Kim Greenwood (Immediate Past President), Bhaskar Iduri (President-Elect), Juuso Leinonen (Vice-President), and Jennifer Nichols Treasurer). Our Board members, Jim Panella, Kevin Kreitzman, Erin Sparnon and Ashley O’Mara are continuing their service as Members at Large. Also continuing in their Committee Chair roles are, Francisco Rodriguez-Campos (Advocacy) and Amy Klemm (Membership). Mike Powers is joined by Elizabeth Sayles to co-chair the Education Committee. Also stepping up to Committee Chair positions are Christopher Riha (Body of Knowledge/CE Certification Promo), Kim Greenwood (Nomination), and Arif Subhan (CE-HOF Nominations Review). I am pleased that Ted Cohen continues as Managing Editor for the ACCE News. I look forward to collaborating closely with each of you as we champion the future of ACCE and clinical engineering!
In addition to continuing to provide robust and timely educational resources this year, I would love to see us expand our membership by welcoming even more talented professionals from across the world into the ACCE family. Our members are vital to our organization as our strength lies in our collective knowledge and diverse experiences, and together, we can elevate the impact of clinical engineering across the healthcare landscape.
Announced in this newsletter is the latest edition of the CCE Certification Study Guide to help those who wish to pursue CCE certification. Additionally, the HTCC has been working hard to draft a new Candidate Handbook for CCE Certification, which introduces some major, beneficial changes to the program. The enhancements, expected later this year, reaffirm our
This column provides example questions and information regarding preparation for the CCE exam. The questions are based on topics from the ACCE Body of Knowledge survey and the CCE Study Guide, Version 13. Note that the instructors for the ACCE CCE Prep courses, and the writers for this column, do NOT have any affiliation with the CCE Board of Examiners and have no access to the actual exam questions. If you have specific topics you would like us to cover please contact editor@accenet.org
1. True or False: The number of different SSIDs should be limited in any one wireless environment?
2. Which of the following are most likely to use DICOM?
a. MRI
b. CT
c. Ultrasound
d. Patient monitors
e. All of the above
f. A, B and C

ACCE News
ACCE News is the official newsletter of the American College of Clinical Engineering (ACCE).
Managing Editor
Ted Cohen tedcohen@pacbell.net
Co-Editors
Sonja Markez
Jason Launders editor@accenet.org
Circulation & Address Corrections
Suly Chi, ACCE Secretariat secretariat@accenet.org
Advertising
Dave Smith advertising@accenet.org
3. As more and more employees and vendors work from home, what is the role of a VPN in providing additional IT network security:
a. VPN is a Very Private Network that improves performance for remote users.
b. A VPN is a service that creates a secure connection between a device and a remote server, allowing users to access that server privately and securely.
c. VPNs give encrypted access to the internet so that all of your outgoing and incoming traffic is secure and anonymous.
d. All of the above
e. B and C
4. (Cybersecurity): True or False: Whenever Microsoft issues an OS patch, it should be applied as soon as possible to every applicable medical device.
(Answers on page 16)
ACCE News is a benefit of ACCE membership; non-members may subscribe for $100 per year.
subscribe e-mail: secretariat@accenet.org
Copyright © 2025 by ACCE

This guest Insights into Innovation author is Rajani Kumar Sindavalam, B.Tech, PGCBM, PMP, a systems engineering leader with 18+ years in medical device development. He has led global programs at HCLTech involving infusion pumps, peritoneal dialysis cyclers, bedside monitors, novel medical devices, and regulatory remediation across Class II/III platforms. The insights and opinions of the author are his own.
In the complex world of medical devices, much attention is devoted to hardware reliability, software validation, and regulatory compliance. However, one of the most persistent threats to patient safety doesn’t come from a component failure or software bug it comes from human interaction. Use errors, often silent and difficult to detect, can result in patient harm, delayed treatments, or even fatalities. Despite their significance, these errors are often underrepresented in risk management activities and postmarket surveillance until they culminate in adverse events or regulatory findings.
Use errors occur when a user’s actions or decisions during interaction with a device lead to unintended results. Unlike device malfunctions, use errors often stem from poor interface design, misaligned workflows, or inadequate consideration of user context. These errors are not necessarily the result of user negligence but rather of design oversights that fail to anticipate how devices will be used in real clinical settings.
Common examples include:
• Misinterpreting graphical data or alarm signals
• Incorrect device programming due to ambiguous instructions
• Failure to notice or correctly interpret critical feedback from the device interface
These issues can result in medication delivery errors, missed diagnoses, or surgical complications. In many cases, root cause analysis reveals that user interface design, labeling, or training materials did not align with real-world use scenarios.
Use errors are often a symptom of broader system design deficiencies. Key contributing factors include:
• Lack of contextual understanding: Devices are often designed without firsthand observation of clinical environments.
• Complex or cluttered interfaces: Overloading users with too much information or poorly grouped functions.
• Inadequate user training: Relying on assumptions about user expertise without providing adaptive instruction.
• Cognitive overload: Stressful environments such as ICUs can diminish a user’s ability to follow multi-step processes or retain instructions.
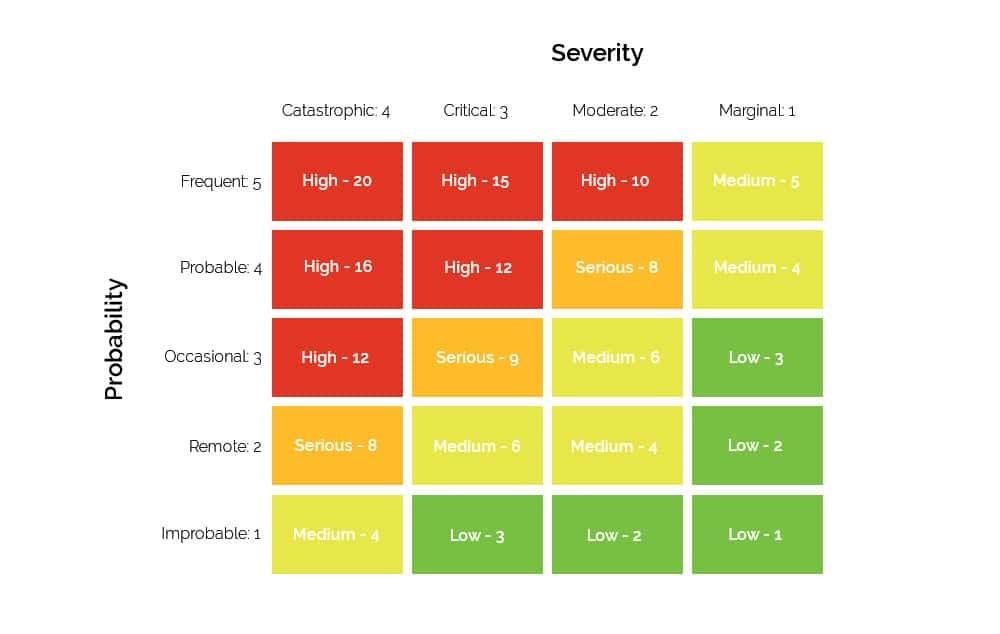
Regulatory bodies like the FDA have increasingly focused on the role of human factors in medical device safety. FDA guidance, along with IEC 62366-1 and ISO 14971, emphasizes integrating usability engineering into the design and development lifecycle. These standards call for:
• Identification of critical tasks
• Systematic usability risk assessment
(Continued
• Formative evaluations during development
• Summative validation before release
Manufacturers who fail to address usability-related risks have been subject to 483 observations and product recalls. As the FDA continues to scrutinize the connection between design and user behavior, usability engineering is no longer optional it’s a regulatory and business imperative.
To effectively reduce use errors, medical device companies must shift from reactive correction to proactive prevention. Key strategies include:
• Early user involvement, Engage representative users through contextual inquiry and observational studies.
• Iterative usability testing, Validate interfaces and workflows using formative studies before finalizing designs.
• Clear, unambiguous labeling, Ensure instructions and on-device labels are intuitive, language-appropriate, and scenario-tested.
• Risk-based training programs, Tailor training content to high-risk tasks and environments.
Advancements in digital health and simulation technologies now offer new ways to anticipate and mitigate use errors:
• Simulation-based testing can replicate high-stress environments for testing device usability
• AI-driven analysis of usage logs can highlight patterns that signal emerging risks
• Augmented reality interfaces can be tested for procedural clarity before launch
These tools complement traditional usability engineering by providing deeper insights into user behavior and performance.
Conclusion
Use errors are a silent but significant threat in the field of medical devices. They represent the gap between technical performance and human reality. By treating usability as a core pillar of product design not an afterthought manufacturers can improve patient outcomes, reduce regulatory risk, and accelerate adoption. The future of safe, effective medical technology depends on designing not just for performance, but for people.
Contact: Daniel Visnovsky (AAMI) Manager, Media Relations AAMI dvisnovsky@aami.org (Continued
Healthcare systems around the world must provide high-quality patient care while also reducing their environmental impact. Clinical engineers play a crucial role in enhancing sustainability by implementing responsible design, managing equipment lifecycles, and reducing waste. These initiatives are crucial for building a healthcare system that is more sustainable and resilient.
Clinical engineers are vital when it comes to checking out medical technologies before they’re bought and figuring out how these technologies affect the environment. By supporting green design principles, they can zero in on technology that doesn’t guzzle energy, uses materials that can be recycled, and cuts back on nasty chemicals. Plus, clinical engineers can really push for buying from brands that are eco-conscious and have those green certifications, like ISO 14001. These early choices affect hospital operations and encourage the broader medical technology sector to embrace sustainability.
Another area where clinical engineers can drive change is in equipment lifecycle management. Hospitals typically oversee thousands of devices, from infusion pumps to MRI machines. The traditional “buy-use-dispose” model leads to increased waste and costs. Clinical engineers can adopt circular economy strategies to extend the life of medical equipment through preventive maintenance, refurbishment, and redeployment. Regular evaluations and data-driven maintenance schedules ensure devices remain reliable. When equipment reaches the end of its initial use, refurbishment can redirect it to other departments or facilities. Partnerships with manufacturers or vendors enable reuse and donations, reducing landfill waste. By managing the entire equipment lifecycle, clinical engineers promote efficient resource use.
Healthcare facilities and resources produce a lot of waste, and most of it is related to technology. The single-use instruments, the outdated electronics, and the improper disposal of batteries or circuit components are creating ongoing challenges. Automated alerts for preventive maintenance help avoid early breakdowns and unnecessary disposals. Working with infection control teams can identify situations where using reusable devices is both safe and practical. This strategy balances patient safety with environmental goals. Additionally, effective management of electronic waste is essential. Implementing organized programs for the collection, recycling, and safe disposal of electronic equipment will ensure compliance with regulations and safeguard staff and communities from hazardous materials.
Clinical engineers have an opportunity chance to take the lead on eco-friendly projects in their hospitals, doing more than just the usual tech fixes. By jumping into interdisciplinary committees, they can really blend sustainability into the hospital’s overall strategy, making sure everything lines up with keeping patients safe and hitting clinical targets. Plus, they’ve got a big part to play as teachers showing biomedical teams, doctors, and hospital leadership how to go green and pointing out the long-term perks of managing tech in a sustainable way. Collecting and analyzing data on reduced energy costs, longer equipment life, and lower disposal expenses strengthens the case for sustainability, reinforcing hospital leaders’ commitment to environmentally friendly healthcare.
The connection between clinical engineering and sustainability offers a chance to change healthcare. This change can help heal patients and protect the planet. With a focus on responsible design, the management of the lifecycle of products, and waste reduction, clinical engineers can make significant contributions to greener hospitals and healthier communities. As the need for sustainable practices increases, Clinical Engineering responsibilities will go beyond just solving technical problems. They will also advocate for medical technology that benefits current patients and future generations.
Fabiola M. Martinez-Licona BME, MEng, PhD. Board Chair
ced.chair22@gmail.com

ACCE thanks our outgoing Education committee Co-Chair Juuso Leinonen for his leadership and dedicated support March 2023 - August 2025. And we welcome our incoming co-Chair, Elizabeth Sayles MBA, MSIT, BSN, CHTM.
Elizabeth Sayles currently serves as the Manager of Quality, Safety &, Education for Mass General Brigham Biomedical Engineering in Boston. She is also a part-time Associate Professor with the College of Biomedical Equipment Technology. She began her career as a BMET and has had various roles throughout her 20-year HTM career. Elizabeth has Masters Degrees in Information Technology and Business Administration, as well as Bachelors of Science Degrees in Electrical Engineering and Nursing.
Elizabeth has been an active member with the Education Committee since August 2024.


ACCE thanks our outgoing CE-BOK committee co-Chair Jennifer Nichols, MSE, CCE, CHTM for her leadership and dedicated support September 2021 - August 2025. Welcome our incoming co-Chair, Chris Riha CCE, CSEP, PMP.
Christopher D. Riha is currently self-employed as a consultant working with several companies in healthcare, as well as a guest lecturer at Virginia Tech University in the Biomedical Engineering Department.
Prior to his current consulting work, Chris was the Senior Cybersecurity Analyst at a Fortune 500 medical device manufacturer, worked as the Lead Health System Engineer at MITRE, and as an independent consultant for 4 years, providing Clinical Engineering, Cybersecurity, and Project/Program Management expertise to a wide variety of clients.
Mr. Riha also had a 14-year tenure at Carilion Clinic. He was responsible for managing up to 70 FTEs in a dynamic
(Continued on page 7)
(Continued from page 6)
and mission critical environment, reporting to the C-suite and clinical leaders of the organization. His responsibilities at Carilion included management of the Clinical Engineering Department, as well as application support for all clinical, and business applications, for a $1.2B healthcare delivery organization.
Chris has been an active member with the CE/BOK Committee since August 2021.


If you are interested in volunteering with ACCE’s committees, please complete this ACCE volunteer form.
(Continued from page 1)
commitment to excellence in this certification program and provide multiple paths for our members to demonstrate their expertise, while maintaining value to the field.
At the end of September, Kim Greenwood traveled to Adelaide, Australia to present a session titled “A Review: Standardization of Neonatal Patient Transport Equipment in Ontario” at the IUPESM World Congress on Medical Physics and Biomedical Engineering. Also, in October, Suly will be representing ACCE at the 2nd Brazilian Congress of Clinical Engineering in Sao Paulo, Brazil and will be presenting the 2023 ACCE/HTF International Organization Award to the Brazilian Association of Clinical Engineering (ABEClin). We will provide more information on these exciting events in future newsletters and emails!
I am genuinely excited for the year ahead and for the opportunity to serve ACCE. I believe that by working together, we can achieve great things, strengthening our community and advancing the vital role of clinical engineers in patient care. Thank you for your dedication to ACCE, and I look forward to connecting with many of you in the months ahead!
Sincerely,
Katherine Navarro, CCE ACCE President katherine.breffeilh@va.gov

ECRI White paper shares best practices and reflections from leaders on how prioritizing patient safety strengthens organizational resilience.
As pressures mount for health system leaders nationwide, ECRI convened four virtual roundtables with 17 C-suite healthcare leaders from across the country, representing integrated health systems, children’s hospitals, rural providers, and national associations. The goal was to capture unfiltered insights into what truly drives and sustains patient safety and continuous improvement.
The white paper – published on World Patient Safety Day, Sept. 17 – is the first in a series of articles born from the ECRI C-Suite Roundtables featuring candid insights from healthcare leaders.
ECRI President and CEO Marcus Schabacker, MD, PhD, and ECRI Chief Medical Officer Dheerendra Kommala, MD moderated the discussions.
“This is a tumultuous time for healthcare leaders and frontline providers in our nation,” said Schabacker. “We launched this roundtable series to dive deeper into the issues they’re facing, and how they elevate patient safety despite these challenges – from shrinking resources to medical misinformation to persistent causes of preventable harm. Together we share what’s truly moving the needle. Only by learning from one another and sharing best practices can we break the cycles that have long held our industry back.”
Participants included (in alphabetical order):
• Rick Bassett, MSN, RN, APRN, ACNS-BC, CCRN, FCNS, LSSGB, President of the National Association of Clinical Nurse Specialists, and Adult Critical Care Clinical Nurse Specialist at St. Luke’s Health System
• Richard Bates, MD, Chief Executive Officer, Thunder Bay Community Health Service
• Dana Bledsoe, DHA, MBA, MS, RN, NEA-BC, FACHE, Chief Executive Officer, Ochsner Children’s Health
• Matthew Davis, MD, MAPP, Executive Vice President, Enterprise Physician-in-Chief, and Chief Scientific Officer, Nemours Children’s Health

• Mindy Dunkerley, MBA, MSN, RN, Chief Quality Officer, Independence Health System
• Michael Fiorina, DO, FAAFP, Chief Medical Officer, Independence Health System
• Jonathan Gleason, MD, EVP and Chief Clinical Officer, Prisma Health
• Djana Harp, MD, MS, MBA, Chief Medical Officer, Norwalk Community Health Center
• Omar Hasan, MD, MS, MPH, Chief Quality Officer, MaineHealth
• Mark Leahey, President & CEO, Medical Device Manufacturers Association
• Kristie Lenze, CEO/CFO, Keystone Rural Health Consortia
• Tara Jo Manal, PT, DPT, FAPTA, Vice President of Scientific Affairs, American Physical Therapy Association
• William G. Morice II, MD, PhD, CEO, Mayo Clinic Laboratories
• Michael Seim, MD, Chief Quality Officer, WellSpan
• Anne Marie Watkins, DNP, MSHCA, RN, CENP, Chief Nursing Executive, UCI Health
• Jacqueline Webb, CPNP, Quality, Risk, and Lab Director, Tri-Area Community Health
• James Werth, Jr., PhD, ABPP, Chief Executive Officer, Tri-Area Community Health
Key findings from the roundtables include: Proactive systems prevent harm. Leaders are shifting from reactive models to proactive approaches by hardwiring learning into daily operations and embedding human factors into workflows.
(Continued on page 13)
In this issue, we will highlight the journey of two extraordinary Clinical Engineers who have been contributing members to the profession:

Carolyn Mahoney, MEBE, CCE, CHTM Consultant
Sigma Health Consulting, LLC
While I was attending Worcester Polytechnic Institute earning my Bachelor’s degree in electrical engineering and my Master of Engineering I was first introduced to the field of clinical engineering. Most importantly as a student I understood the direct connection between healthcare, engineering and the patient.
Before graduating, a friend of mine who had also just finished school told me about the VA’s Technical Career Field (TCF) program. They had nothing but positive things to say about it, especially how it helped them grow and gave them a real chance to make a difference for veterans. That really inspired me, so I decided to apply. I ended up joining the TCF program at the Seattle VA Medical Center. Since then, I’ve worked in different roles across several VA Medical Centers and picked up a ton of valuable experience along the way.
I really enjoyed my 30 years working in clinical engi-
neering in the VA it’s incredibly rewarding to support healthcare providers as they care for veterans and their families.
Since retiring from the VA two years ago, I’ve been with Sigma Health Consulting, LLC. I still get to work closely with my VA colleagues, helping them ensure the medical equipment used in patient care is safe and effective.
I was honored to receive the Professional Achievement in Management and Managerial Excellence Award from ACCE in 2024.

Allison White, BS, MS, MBA Executive Director Clinical Equipment Life Cycle Management
Growing up, I was taught to make practical and intentional choices. My parents emphasized the importance of finding a career that was both fulfilling and financial-
(Continued on page 10)
ly sustainable. Their guidance shaped my college decision: choose a major that leads directly to a job ideally one that could help fund graduate school. I would eventually do just this. I did not declare a major until my sophomore year at SUNY Binghamton, when I discovered Bioengineering, a field that beautifully blended biology and engineering. It felt like the right fit since I enjoyed biology, math, and problemsolving. After graduation, I hadn’t yet heard of clinical engineering. That changed when the Chair of the Bioengineering department shared an opportunity with the VA Healthcare System in Buffalo: a Biomedical Engineering internship through the Technical Career Field (TCF) program. I wanted to work in a field aligned with my engineering background, so I applied. At the time, I had already accepted a position at a major investment and wealth management firm, but when the VA offer came through, I followed my instincts and accepted it. That decision launched my career in clinical engineering. I’ve enjoyed the journey so far. It’s an engineering field where I get to interact with customers and still apply my engineering skills. Fast-forward to today, and I’ve mentored over 15 HTM professionals, from student interns to managers. It is a rewarding field. I didn’t always know what I wanted to do whether in college or professionally but my Bioengineering foundation opened doors I hadn’t imagined. I’m glad it led me to the clinical engineering world. My journey has been shaped by curiosity, family influence, and a commitment to purposeful work.
How long have you been involved with ACCE?
Carolyn: I have been involved off and on over the past several years.
Allison: I’ve been a member for over 15 years.
What do you think of being female in engineering?
Carolyn: I think it is important for women to be in engineering and bring their unique perspectives and experiences to the field.
Allison: I’m proud to be a woman in the engineering field and encouraged by the growing presence
of women in this profession. My recent clinical engineer hire is a woman, and both of my current HTM interns are women as well. They’re bright, quick learners, and bring fresh energy to the team. It’s inspiring to see greater representation in engineering especially in clinical engineering and I’m excited to be part of that progress.
for choosing clinical engineering?
Carolyn: My greatest influence was my parents. They encouraged me to do well in math and science. I was encouraged to look into professions that utilized those skills
Allison: I wasn’t aware of the clinical engineering field until after I graduated college, but I’m grateful I trusted my instincts and accepted a Biomedical Engineer Intern position at the VA. My first supervisor and preceptor, Kimberly Brayley, played a pivotal role in shaping my early experience. Her mentorship was instrumental in helping me build confidence and gain the skills I needed to thrive in the industry. She encouraged me to attend training sessions and conferences, which became invaluable opportunities to learn and network. That support made all the difference in my decision to stay in the field.
Carolyn: I am surprised at how the clinical engineering profession keeps growing and changing. It is adapting to the changing needs of the medical field, by providing classes and training on new technologies.
Name Class
Marcus Coleman Inst/Associate Manager. HTM
Steve Irish Inst/Associate Manager, HTM
Robert Fraser Inst/Associate Biomedical Engineer
Farheen Shaikh Student Grad Student University of Ottawa ON/ Canada

https://www.islandhealth.ca/
Amy.s.klemm@gmail.com

In ACCE’s 2025-2026 Educational inaugural webinar session, Patient Monitoring System Integration, speaker Nick Everson shared Mayo Clinic’s journey in standardizing and integrating patient monitoring systems across the enterprise, highlighting the organization’s efforts to standardize their patient monitoring systems spanning a period from 2014 to 2022. He discussed the range of interfaces that enable this integration, including inbound ADT and Auto-ADT for patient data, outbound wave strip exports and highfidelity data export. Multi- and single-patient viewers, mobile patient viewers, and Epic EHR waveform viewer integrations were also discussed. Nick emphasized that the features once considered “nice to have”, such as mobile patient viewers and EHR waveform integration, have now become essential tools in clinical practice. A key theme throughout the session was the importance of proactive planning, cross-team collaboration between HTM, IT, informatics, clinical, and EHR teams to ensure effective and seamless system integration.
In case you missed the live session, you may review the presentation material on ACCE’s website by login to your member’s account.
Priyanka Shah, session Moderator, and Education Committee member pshah@ECRI.org
To celebrate the Cybersecurity Awareness Month, the ACCE Education Committee is presenting a session on October 09 covering the topic: Healthcare Technology Management –Benefits of Networking and Cybersecurity Certifications.
Register today and join our speakers Eddie Myers and Douglas Cesconetto to learn how certifications in IT, networking, and cybersecurity not only can elevate your career in Clinical Engineering (CE) and Healthcare Technology Management (HTM) but also enhance your ability to tackle everyday technical and operational challenges in healthcare environments.
Suly Chi, Webinar Coordinator secretariat@accenet.org

We’re pleased to announce that ACCE Members will have exclusive access to Collaborator Rates (equivalent to HIMSS member pricing) for registration to HIMSS26 – an outstanding opportunity to participate in one of healthcare technology’s premier events.
Save the Date: March 9, 2026 We’re thrilled to share that the 2026 ACCE CE-IT Symposium will take place on Monday, March 9, 2026. This premier educational event promises to deliver cutting-edge insights and invaluable networking opportunities for clinical engineering and IT professionals.
We look forward to sharing comprehensive details about the symposium programming and registration process in the coming weeks. This will be an exceptional opportunity to advance your professional development while connecting with industry leaders and peers.
More information coming soon – we can’t wait to see you there!
Click here for the agenda at-a-glance.
Book your HIMSS26 hotel today at authorized hotels
Travel discounts
(Continued from page 8)
System design and standardization saves lives. Safety issues can cause longer stays and liability. Well-designed, standardized systems make the safe choice the easy choice and ensure consistent outcomes across sites. Safety is a sound business strategy. Health systems that embed safety and create reliable systems can reduce extended stays, boost staff engagement, strengthen payer negotiations, increase patient satisfaction, and improve margins.
There was broad consensus among C-Suite Roundtable participants on the challenges and the path forward. The groups also discussed these challenges, slated for forthcoming publications in the series:
• How organizational culture shapes safety reporting and outcomes
• Navigating care delivery without trusted federal agencies as beacons of truth
• Role of boards and executive leaders in safety and quality
Please keep in touch. We would love to hear about your thoughts on these challenges.
Ismael
Cordero,
Senior Project Engineer, Device Safety, ECRI
icordero@ecri.org
The Associate Clinical Engineering and Clinical Engineering Certification Study Guide was prepared by the Body of Knowledge committee as part of the American College of Clinical Engineering. It reflects the collective knowledge of a group of senior clinical engineers about the current body of clinical engineering knowledge. As such, this Guide should help gauge the depth and breadth of your working knowledge in the clinical engineering field and point you in the right direction as you study for the ACE/CCE exam.
ACCE thanks the contributions of all our volunteers who have contributed over the past 29 years (1996-2025) to updating the CCE Study Guide.
You may order your copy here.
The following volunteers have shared their expertise over the years:
• V14.0 (August 2025): Kim Greenwood, Board Member; Jenn Nichols, BOK Committee Chair; Chris Riha, Daisha King, Ishtar Al-Tahir, Kajal Madhusudan, Kindall Drucker, Michele Manzoli.
• V13.0 (June 2024): Kim Greenwood, Board Member; Jenn Nichols, BOK Committee Chair; Chris Riha, Daisha King, Ishtar Al-Tahir, Kajal Madhusudan.
• V12.0 (June 2023): Kim Greenwood, Board Member; Katherine Navarro, Board Member; Jenn Nichols, BOK Committee Chair; Alan Lipschultz, Chris Riha, Daisha King, Ishtar Al-Tahir, Kajal Madhusudan.
• V11.0 (June 2022): Kim Greenwood, Board Member; Katherine Navarro, Board Member; Jenn Nichols, BOK Committee Chair; Alan Lipschultz, Chris Riha, Jason Howard, Parisa Bahrami.
• V10.0 (July 2021): Kim Greenwood, Board Member; Bhaskar Iduri, BOK Committee Chair; Katherine Navarro, Alan Lipschultz, Jenn Nichols.
• V9.0 (May 2020): Kim Greenwood, Bhaskar Iduri, Steph Liddle, Alan Lipschultz, Chris Riha.
• V8.0 (Jul 2019): Katherine Navarro, Lucio Brito, Sarah Brockway, Mark Bruley, Jennifer DeFrancesco, Murat Firat, Dave Gretzinger, Renee Huval, Bhaskar Iduri, Scott Kopp, Nicholas Muhlenbruch, Bhavesh Patel,
Sara Salari, Rehman Syed, Binseng Wang, Rachel Zhang.
• V7.0 (May 2018): Katherine Navarro, Sarah Brockway, Renee Huval, Bhaskar Iduri, Jeanine Maier, Meet Patel, Rehman Syed, Arleen Thukral, Tony Tai.
• V6.0 (August 2016): Matthew Baretich, Tobey Clark.
• V5.0 (May 2016): Christopher Falkner, Jennifer DeFrancesco, Austin Hampton.
• V4.0 (July 2014): Jacob Johnson, Jennifer DeFrancesco.
• V3.0 (August 2012): Ilir Kullolli, Kindall Druker, Frank Painter.
• V2.0 (July 2007): Arif Subhan, Ismael Cordero, Evelyn Fan, Robyn Frick, Jennifer Jackson, Jeff May, Frank Painter, Bokang Rapoo.
• V1.0 (1996): Jerry Anderson, Salil Balar, Ted Cohen, Vinnie DeFrancesco, Izabella Gieras, Stephen L. Grimes, Frank Painter, Christine Ruther, Marv Shepherd.
Jenn Nichols, CE-BOK Chair jennie_nichols@yahoo.com
Allison: I love that CE is constantly evolving. Years ago, the discussion was about CE-IT collaboration. We’re now living the CE-IT life, working on medical device integrations and cybersecurity initiatives, and looking ahead to AI applications in HTM.
What would you tell other female when considering engineering?
Carolyn: Engineering is a great field to be involved in. It is always changing and there is often something new to learn.
Allison: Engineering is a deeply rewarding field,
even if you’re not sure exactly where you’ll end up. I didn’t know my career path right away, and that’s okay. I always encourage students to explore internship programs that offer hands-on exposure to engineering. At SUNY Upstate, we offer one-year paid internships for incoming seniors enrolled in a biomedical engineering undergraduate program. These internships include comprehensive training and rotations that introduce students to all aspects of Clinical Engineering and Healthcare Technology Management (HTM). Successful interns are considered for one of two career tracks within our department: Biomedical Equipment Technician (BMET) or Clinical Engineer.
The ACCE Secretariat is a critical position that serves as the backbone of the organization’s daily operations. You will wear many hats, providing comprehensive administrative and logistical support across various departments. This role offers a dynamic and fast-paced environment where you can contribute significantly to the success of ACCE.
Responsibilities:
• Membership management
• Support board and committees
• Coordinate educational webinars and ACCE News
• Manage collaborations & social media
• Support webmaster with website content, ensuring accuracy and functionality
Qualifications:
• Bachelor’s degree in relevant field (e.g., Business Administration, Communications) or equivalent experience preferred
• Proficiency in MS Office Suite, Intuit, Acrobat, Zoom
• Working knowledge of accounting software (QuickBooks preferred)

• Ability to work independently with minimal supervision, demonstrating initiative and problem-solving skills
• If you are interested, or know someone that would be willing to help the ACCE, please contact Bhaskar Iduri at: contact@accenet.org
Correct answer: True
Explanation:
Explanation: It is recommended that the number of Service Set Identifiers (SSIDs) be limited in order to reduce overhead and provide optimum available bandwidth. Often HDOs need several different SSIDs in one environment, for example, to separate clinical, non-clinical, and guest wireless traffic. However, for best performance it is a best practice to limit the overall number of SSIDs for the following reasons:
• Performance Degradation: With increased airtime taken up by beacon frames and other SSID-specific management traffic, for multiple SSIDs there’s less bandwidth available for actual data transfer leading to a potential slowdown in network performance.
• Complexity: Managing multiple SSIDs means managing multiple security keys, policies, and configurations, thus increasing administrative overhead.
Correct answer: F (A,B, and C)
Explanation:
DICOM, or Digital Imaging and Communications in Medicine, is the international standard for handling, storing, printing, and transmitting medical imaging information and related data. It defines a standardized file format that includes both the medical image data and a header containing patient demographics, study parameters, and other essential information. DICOM ensures interoperability between different medical imaging devices and systems, allowing for seamless sharing and management of medical images across a healthcare organization. Patient monitoring systems generally do not use DICOM.
Correct answer: E (B and C)
Explanation: VPNs (Virtual Private Networks) create a secure, encrypted tunnel between your device and the internet. This process helps protect your data from interception by encrypting it, making it unreadable to anyone who might try to access it while it is in transit. VPNs also mask your IP address providing some anonymity.
Correct answer: False
Explanation: Most medical device manufacturers require that THEY test the patch first. The FDA also recommends,
but does not require, that the HDO receive manufacturer approval prior to the HDO installing a patch on a medical device.
Questions written by the ACCE CCE Written Exam Study Group Instructors.
Ted Cohen Editor, ACCE News tedcohen@pacbell.net

The Journal of Clinical Engineering is a compilation of articles, papers, and extensive manuscripts relevant to clinical/biomedical engineering or biomedical technology. Subject matter directly relates to the engineering or technology involved in patient care and treatment or technology in the broad field of health care delivery.
ACCE members receive a discounted subscription to the Journal of Clinical Engineering for only $99! (Originally $378). You must login to the ACCE website to view the code. Then visit LWW.com to enter code.