17 minute read
EXAMINE
by TBI Times

The latest in traumatic brain injury research and treatment.
Advertisement
‘BRAIN GLUE’ HELPS REPAIR CIRCUITRY IN TBI
BY GREY NOLAN
In a new study at the University of Georgia, researchers have demonstrated the long-term benefits of a hydogel, which they call ‘brain glue,’ for the treatment of traumatic brain injury (TBI). The gel protects against loss of brain tissue after a severe injury and might aid in functional neural repair. The study shows the long-term benefits of brain glue for th treatment of TBI. The new study provides evidence that not only does the gel protect against loss of brain tissue after a severe injury, but it also might aid in functional neural repair. Brain damage following significant TBI commonly esults in extensive tissue loss and long-term disability. There currently are no clinical treatments to prevent the resulting cognitive impairments or tissue loss. As reported in Sciences Advances, the new finding i the first to povide visual and functional evidence of the repair of brain neural circuits involved in the reach-to-grasp movement in brain glue-implanted animals following severe TBI. “Our work provides a holistic view of what’s going on in the recovery of the damaged region while the animal is accomplishing a specific each-and-grasp task,” said lead investigator Lohitash Karumbaiah, an associate professor in the University of Georgia’s College of Agricultural and Environmental Sciences. Brain glue was designed to mimic the structure and function of the meshwork of sugars that support brain cells. The gel contains key structures that bind to basic fiboblast growth factors and brainderived neurotrophic factors, two protective protein factors that can enhance the survival and regrowth of brain cells after severe TBI. In a prior short-term study, Karumbaiah and his team showed that brain glue significantly potected brain tissue from severe TBI damage. In this new research, to harness the neuroprotective capacity of the original, they further engineered the delivery surface of protective factors to help accelerate the regeneration and functional activity of brain cells. After 10 weeks, the results were apparent. “Animal subjects that were implanted with the brain glue showed repair of severely damaged tissue of the brain,” said Karumbaiah. “The animals also elicited a quicker recovery time compared to subjects without these materials.” To measure the glue’s effectiveness, the team used a tissue clearing method to make brain tissue optically transparent, which allowed them to visually capture the immediate response of cells in the reach-to-grasp circuit using a 3D imaging technique.

HYPERBARIC OXYGEN THERAPY FOR TBI
BY NAOMI KHAN
CLINICAL REPORT
VA Evidence-based Synthesis Program
(ESP) investigators found that HBOT did not provide a clinically relevant improvement in post-concussive symptoms after 8 to 10 weeks of treatment, nor did it cause any serious adverse effects. That being said, ESP states in their conclusions that many limitations were encountered when conducting their study, making their findings inconclusive.

Hyperbaric oxygen therapy (HBOT) is defined as th use of oxygen at higher than atmospheric pressure for the treatment of underlying disease processes and the diseases they produce. Modern HBOT in which 100% O2 is breathed in a pressurized chamber dates back to the 1930s when it was first used for the teatment of decompression illness in divers. There are currently 13 FDA-approved uses for HBOT. Though traumatic brain injury (TBI) treatment is not an FDA-approved use for HBOT, many physicians have used it as an “off-label” teatment with notable results. Though not yet scientifically poven, it has been said that HBOT can dramatically and permanently improve symptoms of chronic TBI months or even many years after trauma. This assertion is generally met with skepticism within the medical establishment because it is widely accepted that any post-concussion symptoms persisting more than 6 months after a head injury are due to permanent brain damage that cannot be repaired. Therefore, treatment has been limited to symptom management and rehabilitative services, and any claim suggesting that fundamental healing is possible is not considered mainstream. Researchers started investigating HBOT as a TBI treatment in the 1960s because of its ability to slow cell death, suppress inflammation, and boost cell and blood vessel growth. Most of the research was conducted on animals until recently because of the ethical issues involved in experimenting on humans with severe brain injury. One of the biggest issues complicating research of HBOT in brain injury is the ability to conduct randomized, double-blind, placebo-controlled studies. Brain injury varies widely from person to person, making it difficult findTBI patients to study who have similar injury severity and affected egions. Finding an objective way to measure the effects of HBOT is also an obstacle with several published studies failing to use a placebo. However, recently researchers have devised and used a placebo for HBOT in their studies, usually by increasing the air pressure without changing the oxygen content of the air being delivered. It’s imperfect (since air pressure increases while oxygen stays the same), but it does improve the reliability of results and possibly paves the way for HBOT as an acknowledged treatment for TBI.
THE CRANIOCERVICAL JUNCTION AND MILD TRAUMATIC BRAIN INJURY
BY GREY NOLAN
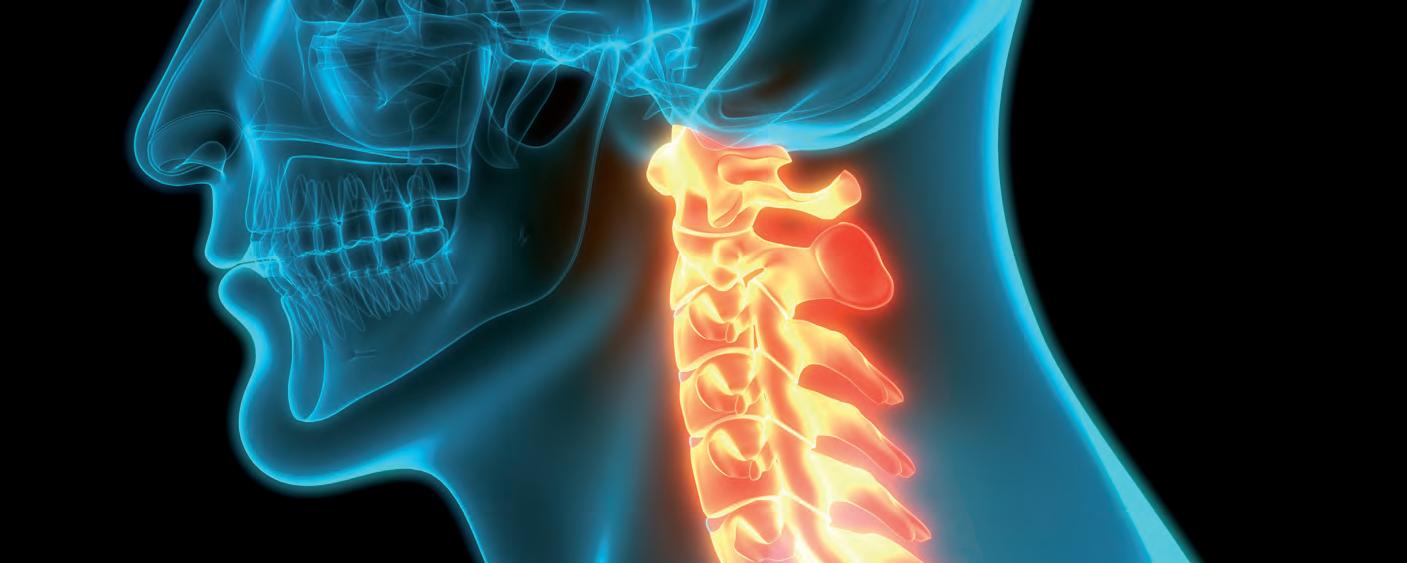
The craniocervical junction (CCJ) is a complex transitional region between the base of the skull and the upper cervical spine. It is comprised of the occiput, atlas, and axis and plays a vital role in craniospinal hydrodynamics, the relationship between blood and cerebrospinal fluid volume, pessure, and flow in the compartments of the cranial vault and spinal canal. The CCJ also encloses the encephalic vasculature of the central nervous system. Housing such important system components, it isn’t surprising that any damage to this area of the spine can lead to numerous neurologic symptoms, many of which mimic the symptoms of brain injury. In recent years studies have shown that injury to the CCJ may cause or contribute to symptoms of mild traumatic brain injury (mTBI), including headache, dizziness, balance and coordination problems, cognitive deficits, fatigue, insomnia, and emotional changes such as irritability, depression, and anxiety. In 2015, Dr. John Leddy and his team at the University of Buffalo published an article suggesting just that and other articles have followed adding credibility to Dr. Leddy’s findings. For example, the Journal of Sports Medicine wrote about the topic in an article titled Cervical Spine Involvement in Mild Traumatic Brain Injury: A Review. In this article, the author wrote “following a trauma, structures such as the cervical spine, the vestibular ocular system, and the temporomandibular joint can be injured.” The article also notes that “neck pain, headaches, dizziness, and balance dysfunction are common symptoms associated with both mTBI and cervical spine injury.” Addressing neck injuries, the article suggests, may lead to better mTBI recovery. A leading researcher in the chiropractic field, D. Scott Rosa, has also written about how injury to the CCJ may cause or contribute to mTBI symptoms. He refers to this as “Craniocervical Junction Syndrome” and has treated many high-profile patients, including Jim McMahon, former Chicago Bears quarterback. While randomized controlled trial testing on this hypothesis is currently in progress, the notion raises the question of how MRIs should be performed when diagnosing mTBI. Doctors typically order an MRI of the skull in a patient showing symptoms of brain injury. However, it is possible, based on the articles aforementioned, that an MRI of the cervical spine would help in developing an effective teatment plan for mTBI patients.

AN ANTI-INFLAMMATORY DIET CAN REPAIR THE BRAIN
BY APRIL DANIELS
5 ANTI-INFLAMMATORY FOOD SWAPS
1. Replace processed sugar with natural sweeteners 2. Replace canola oil with extra-virgin olive oil 3. Replace cow-derived dairy with products made from goat or sheep milk 4. Replace traditional bread with a gluten-free option 5. Replace alcoholic beverages with naturally flavored sparkling water
Traumatic brain injury (TBI) rapidly induces inflammation. This inflammation is poduced both by endogenous brain cells and circulating inflammatory cells. ogether they drive they inflammatory esponse when damaged cells release chemicals, including histamine, bradykinin, and prostaglandins. These chemicals cause blood vessels to leak fluid into the tissues, causing swelling Even after the initial injury, a prolonged state of brain inflammationmay linger for years. Eating an anti-inflammator diet can counteract long and short-term inflammation The basics of an anti-inflammatory diet include eatin more plants, as whole plant foods have the antiinflammatory nutrients that your body needs. So eating rainbow of fruits, veggies, whole grains, and legumes is the best place to start. These are some specific examples
Incorporating Antioxidants
This helps prevent, delay, or repair some types of cell and tissue damage. They’re found in colorful fruits and veggies like berries, leafy greens, beets, and avocados, as well as beans and lentils, whole grains, ginger, turmeric and, green tea.
Eating Omega-3s
Omega-3 fatty acids play a role in regulating your body’s inflammatory pocess and could help regulate pain related to inflammation. Find these healthy fats in fish like salmon tuna, and mackerel, as well as smaller amounts in walnuts, pecans, ground flaxseed, and so.
Eating Less Red Meat
Red meat can be pro-inflammator . Substituting your lunchtime beef with fish, nuts, or soy-based potein a few times a week can be very beneficial
Eliminating Processed Foods
Sugary cereals and drinks, deep-fried food, and pastries are all pro-inflammatory offenders. They can conta plenty of unhealthy fats that are linked to inflammation
But eating whole fruits, veggies, grains, and beans can be quick if you prep ahead for multiple meals. In addition to healing damage caused to the brain immediately following TBI, an anti-inflammatory diet als minimizes the potential for post-TBI conditions such as fatigue, depression, anxiety, migraine, and seizures.
STUDIES LOOK AT CBD AS A TREATMENT FOR TBI
BY LAURA TRESCOT
CBD products are extracted from hemp or marijuana, which are essentially the same cannabis plant but are cultivated diffeently, hemp plants being grown to contain less than 0.3% THC. Numerous clinical trials in which traumatic brain injury (TBI) patients are being treated with CBD oil from hemp, which has virtually no THC, are showing positive results. In the United States, the first big study on cannabinoid treatment for concussion is being done by the University of Miami which received a $16 million grant. The research is a five-yea, three-stage study that will assess the effectiveness of a new cannabinoid-based pill to treat concussion injuries. This partnership aims to propel this research and potential treatment forward by using two classes of drugs in a combination that scientists believe will reduce brain inflammation and the immune esponse. The study will also test the cannabinoid-based pill on a small pilot group of acute and chronic TBI patients. Another new study being conducted at the University of Miami is investigating if using a pill form of cannabidiol (CBD) and the psychedelic drug psilocybin effectivel treat and possibly prevent symptoms of two conditions that commonly occur together: mild traumatic brain injury (mTBI) and post-traumatic stress disorder (PTSD). Up to 40% of people impacted by TBI also suffer fom PTSD, according to a University of Miami press release. A preclinical trial on animals is in progress. The university expects this phase to last around 9 to 12 months. Researchers hope to transition to human clinical trials and file th treatment with the FDA in 2021.
A study published in Brain Injury in October 2019 found that even though cannabis use didn’t affect concussion recovery time, it was associated with a lower symptom burden in the third and fourth weeks after injury. A December 2018 study in the journal Neurology indicates that medical cannabis (marijuana) helps concussion patients with concussion symptoms, especially pain, mood, sleep, and quality of life. The study also specifies the optimal forms of medical cannabis for the patients in the study in terms of ratios of CBD to THC and methods of intake, such as a tincture (oral) or a vapor pen (inhaling).

CLINICAL REPORT
In a study published in The Journal of Neurotrauma Vol. 38, No. 14, pre-clinical traumatic brain injury (TBI) research suggests that cannabinoids have neuroprotective and psychotherapeutic properties. Studies demonstrate that TBI patients are using medical and recreational cannabis to treat their symptoms, highlighting inconsistencies between public policy, perception of potential efficacy, and the dearth of empirical evidence. We conclude that randomized controlled trials and prospective studies with appropriate control groups are necessary to fully understand the efficacy and potential adverse effects of medical cannabis for TBI.
BIOMARKERS CAN DIAGNOSE MILD TBI
BY NAOMI KHAN

Certain plasma microRNAs could serve as diagnostic biomarkers in mild traumatic brain injury (mTBI), a new study shows. The biomarkers were discovered in an animal model and successfully used to diagnose mTBI in a subgroup of patients.
mTBI is difficult to detect by contemporary convention imaging methods. Most patients do not exhibit visible structural damage to the brain. Even without visible structural damage, it is extremely important to diagnose mTBI since patients’ ability to work and their overall quality of life might deteriorate. There is a major unmet medical need to identify accurate, affodable, and widely accessible diagnostic biomarkers that could be used to better diagnose patients with mTBI and to guide them to symptomatic, timely, and rehabilitative treatment.
Blood-based biomarkers enable minimally invasive and costeffective diagnostics. Earlier studies have shown that many biomarkers hold promise for characterizing the severity of traumatic brain injury, and they can provide molecularlevel information about the ongoing pathological changes. In the newly published study, researchers set out to find microRNAs that could serve as biomarkers to diagnose traumatic brain injury (TBI). MicroRNAs, or miRNAs, are small RNA molecules that regulate the expression of proteincoding genes. Blood plasma samples were sequenced from an animal model both after mild and severe TBI. The miRNAs showing the greatest potential based on the sequencing data were selected for further analysis. “We have been developing a suitable analysis and measurement method especially for miRNAs that can be found in small amounts in plasma, and this method is based on digital droplet PCR,” Dr. Noora Puhakka from the A. I. Virtanen Institute for Molecular Sciences at the University of Eastern Finland says. “Humans and animals share many identical miRNAs, and this makes them excellent candidates for translational studies, where results achieved in animal models are sought to be applied in humans. However, it has proven challenging to reproduce results from diffeent studies and diffeent sets of data. This is why assessing the quality of measurement methods and reproducibility is an extremely important part of biomarker research.”
The objective of the newly published study was to identify plasma miRNA biomarkers that are sensitive and specific to mTBI in an animal model and to explore whether they could also be used to diagnose mTBI in humans.
ACUPUNCTURE OFFERS MANY BENEFITS AFTER TBI
BY GEORGE PLATT
CLINICAL REPORT
Researchers from South Medical University conclude that acupuncture provides relief of limb paralysis due to traumatic brain injury (TBI). In a study combining acupuncture with drug therapy, patients had superior outcomes compared with patients receiving only drug injections. The researchers conclude that the addition of acupuncture to the standard drug treatment regimen improves limb motor function and daily life activity capabilities.

Acupuncture is a traditional Chinese practice that is primarily used to treat chronic pain. However, it can also relieve the anxiety, depression, and insomnia that often affect patient after a traumatic brain injury (TBI). This makes acupuncture a possibly beneficial practice for brain injury survivors Acupuncture originated in China over 2,000 years ago. It involves placing thin needles into the skin at certain points in the body. These points, called meridians, are thought to trigger the body’s natural healing responses. According to traditional Chinese medicine, the body has a natural flow of enegy called qi. When qi gets congested, a person can become susceptible to pain, anxiety, and disease. By puncturing the body in the correct spots, acupuncture can clear away the congestion and restore the body’s natural balance. A more modern way of explaining how this works is that acupuncture gently stimulates the nerves and causes an inflammatory esponse. These responses activate the body’s natural healing process. Perhaps the most exciting benefit that acupunctue can offer brain injury patients is the ability to egenerate brain cells. One study in 2017 found that acupuncture increased the production of BDNF. BDNF stands for brain-derived neurotrophic factor, a growth factor that acts as a fertilizer for your brain. BDNF triggers your brain to initiate a process known as neurogenesis. Neurogenesis is similar to neuroplasticity, except where neuroplasticity refers to the brain’s ability to rewire itself, neurogenesis involves the creation of new brain cells.
This has huge implications for TBI patients since this would enable them to recover more fully from any brain damage that may have occurred. Studies have also found that acupuncture increases blood flow to the brain, which lets the brain ge more of the critical nutrients it needs to heal. It does this by releasing vasodilators into the bloodstream, which causes your blood vessels to relax and expand. Acupuncture also triggers the release of endorphins in the brain. Endorphins are hormones that activate your body’s opiate receptors, which means they act as natural painkillers. This effect makes acupunctue an alternative treatment for conventional pain management after traumatic brain injury.
TBI TREATMENT DIFFERS FOR MEN AND WOMEN
BY APRIL DANIELS

New research has determined that the window of opportunity to provide possible treatments for patients suffering fom traumatic brain injuries (TBIs) differs depending on whether the patient is male or female. Building on this, scientists from The University of Texas Health Science Center at Houston (UTHealth) and Arizona State University have teamed up on the first study looking at sex-targeted drug delivery for TBI in a five-yea, $2.5 million project funded by the National Institutes of Health (NIH). The study will be used to help design nanoparticle delivery systems targeting both sexes for treatment of TBI. “Under normal circumstances, most drugs, even when encapsulated within nanoparticles, do not reach the brain at an effective concentration due to the pesence of the blood-brain barrier. However, after a TBI this barrier is compromised, allowing us a window of opportunity to deliver those drugs to the brain where they can have a better chance of exerting a therapeutic effect,” said D. Rachael Sirianni, Ph.D., associate professor of neurosurgery at McGovern Medical School at UTHealth. Sirianni’s collaborator and co-lead investigator on this grant, Dr. Sarah Stabenfeldt, PhD, was the first to demonstrate that the window of opportunity created in the blood-brain barrier diffeed between men and women, and it was this key finding that led to them applying for the NIH grant A TBI is an acute force trauma that occurs to the head as a result of a fall or an object hitting the head with any amount of force. The body responds with an acute response to the injury, followed by a chronic phase as it tries to heal. Under normal circumstances the blood vessels in the brain are very selective about what they allow to enter the brain, helping to protect it from substances that might hurt neuron cells and to create a very carefully controlled blood-brain barrier. However, during this second phase of healing following a TBI, those blood vessels are compromised and substances might be allowed to seep in. “With these nanoparticle systems, we’re looking at how we can revisit a drug that showed promise in preclinical studies or clinical trials but then failed,” Stabenfeldt said.
SURGICAL CENTERS

UNLOCK THE MOST CUTTING EDGE IMAGING AND SURGICAL FACILITIES IN CALIFORNIA.
By becoming a member of PacificCrest Healthcare IPA, you instantly unlock access to an extensive network of imaging and surgery centers. Our imaging partners offer state-of-the-art equipment and access to some of the best neurological and musculoskeletal radiologists in California, ensuring high-quality reads and optimal outcomes. Our surgical partners take outpatient surgery to a new level, with strong track records of quality care and positive results. www.pchipa.com 1-833-PCH-4111

EXCEPTIONAL SPEAKERS. WARRIORS UNITE. FUN WITH THE VOLUME TURNED UP.