7 minute read
TBI TREATMENT: A MULTIDISCIPLINARY APPROACH
by TBI Times
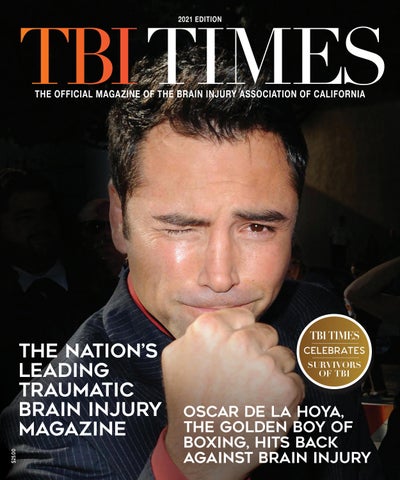
Neurosurgeon Dr. Fardad Mobin, M.D. and neuropsychiatrist Dr. Rod Amiri, M.D. shed light on two key roles in the treatment of TBI.
Advertisement
BY MICHELLE ST. HILAIRE
Traumatic brain injury (TBI) is a common and often serious condition that occurs in accidents involving an impact to the head. In many cases, the victim does not realize the full extent of their injury until months or even years after the trauma has occurred and symptoms surface. This can result in great personal suffering and even monetary epercussions for example a personal injury case being settled before it is clear that the victim has a brain injury. Although fragile bones can mend, TBI can leave a person’s life irrevocably changed, permanently damaging their relationships, work, mental capacity, and quality of life. For these reasons, it is important for those who have experienced head trauma to be acutely aware of the potential of TBI so that they may seek out treatment as soon as possible. TBIs can range from mild (concussions) to severe, with causes ranging from simple slip and fall injuries or major motor vehicle collisions to full-contact sports injuries. From a physiological perspective, TBI trauma occurs as a consequence of a sudden acceleration or deceleration or by a complex combination of both movement and sudden impact. Depending on the severity of the injury, the required treatment may be minimal or multidimensional and can include various types of intervention. This is called team-based treatment and is defined as pofessionals from a range of disciplines working together to deliver comprehensive care that addresses as many of the patient’s needs as possible. In this treatment model, care can be provided by a range of professionals functioning as a team under one organizational umbrella or by professionals from a range of organizations brought together as a unique team. As a patient’s condition changes over time, the composition of the team may change to reflect the changing clinical and psychosocia needs of the patient. There are many options available to doctors when taking a multifaceted approach to diagnosing and treating TBI. Symptom triggers can be successfully identified though cognitive therapy, surgical intervention is also appropriate in some cases, and medication can play an important role in managing symptoms. Thrive talked to two authorities in their fields, D. Fardad Mobin, M.D. (a neurosurgeon), and Dr. Rod Amiri, M.D. (a neuropsychiatrist) to learn how these two specialties contribute to the successful treatment of TBI.
In more severe cases of TBI, neurosurgery may be a necessary part of treatment. A neurosurgeon is a medical doctor who specializes in evaluating, diagnosing, and treating conditions of the brain, spine, and nervous system. Neurosurgeons have extensive training, knowledge, and experience performing some of the most complex surgical procedures the human body can undergo and can also diagnose and treat conditions affecting the stuctures that support the nervous system including the skull, spinal vertebrae, spinal discs, and blood vessels. Dr. Fardad Mobin, M.D. is a highly-skilled, board-certified neurosurgeon. He has performed over 2,000 surgeries and is recognized for his exceptional operative skills as well as his excellent patient care. Dr. Mobin is a graduate of the Rensselaer Polytechnic Institute in Troy, New York, holds a medical degree from the University of California Davis School of Medicine, and has completed a fellowship at the University of California, Los Angeles.
THRIVE MAGAZINE: How would you describe a neurosurgical approach to the treatment of TBI?
DR. Mobin: Neurosurgeons are at the frontline when it comes to caring for TBI patients. We are routinely consulted by emergency room physicians and trauma surgeons to take an active role in the management of individuals with acute traumatic brain injury, from mild uncomplicated head injuries to severe life-threatening intracranial injuries. The first goal o neurosurgical intervention is to relieve the build-up of pressure within the enclosed cranium and prevent brain herniation. The

next course of action is to rescue the brain tissue at risk of irreversible damage. Neurosurgical intervention consistently involves control of intracranial pressure by performing craniotomies to control and evacuate intracranial bleeds and restore normal pressure within the cranium. The neurosurgeon is an active player in postoperative critical care, working hand in hand with the ICU team to manage the multitude of parameters that are critical to the recovery of TBI patients.
Dr. Fardad Mobin, M.D.
NEUROSURGERY
TM: Specificall, how do neurosurgeons neuropsychiatrists work together to treat TBI?
DM: Individuals with TBI can suffer fom an array of brain functionality issues, often manifesting as personality change, short-term or long-term memory loss, cognitive decline, and difficulty with focus and information ocessing. Neuropsychiatrists can perform detailed cognitive testing to link the observed deficits to any underlying stuctural injuries. This information will then help guide the patient’s rehabilitation program.
TM: Can neurosurgery alone ever successfully treat TBI?
DM: No. Both acute and chronic phases of TBI require a multidisciplinary treatment team. Neurosurgeons play a very important role in the treatment of both the acute and chronic phases of TBI, however, the coordinated care of several disciplines including neurosurgeons, trauma surgeons, physiatrists, physical therapists, neuroradiologists, neurocognitive psychiatrists, and speech therapists, to name a few, are necessary for the successful treatment of TBI.
TM: Is neurosurgery used in the treatment of mild, moderate, and severe TBI?
DM: Yes. The discipline of neurosurgery places a great deal of concentration on the treatment of acute brain injury, and neurosurgical training concentrates on both surgical and medical care of TBI. Neurosurgeons are uniquely positioned to conduct life-saving procedures to relieve intracranial pressure and employ the critical care necessary to prevent secondary brain damage. For more information on Dr. Mobin: (310) 829-5888 or spinesurgeonla.com.
Neuropsychiatrists also play an essential role when treating patients who have experienced TBI and are trained in the diagnosis and treatment of a wide range of conditions. The main focus of neuropsychiatry is understanding the psychological and psychiatric symptoms that arise from brain injury and disease and how to go about treating them. Dr. Rod Amiri, M.D. is a board-certified psychiatris and diplomate of the American Board of Psychiatry and Neurology as well as the American Board of Addiction Medicine. Based in Los Angeles, California, Dr. Amiri is also an injury specialist (CBIS) certified by the Brai Injury Association of America. Committed to the everevolving and growing understanding of the psychological and psychiatric impacts of TBI, his concentration on the psychological symptoms of brain injury and disease gives him a unique perspective when it comes to treating the mental health side effects of TBI
THRIVE MAGAZINE: In your opinion, how important is a multidisciplinary approach to the treatment of TBI?
DR. AMIRI: When we take a multifaceted approach to treating the symptoms of TBI we have many tools at our disposal, increasing the odds of a patient making a successful recovery. Cognitive therapy is important to identify symptom triggers, in many cases, surgical intervention is warranted, and at times medication plays a role in managing symptoms. This is why it is so important to approach treatment from many angles.

Dr. Rod Amiri, M.D.
NEUROPSYCHIATRY
TM: What is the connection between the specific nature of a TB and the psychological symptoms a patient may experience?
DA: There is no question that physical damage to the brain can cause cognitive, emotional, and behavioral issues. Research has shown that the specificarea of the brain affectedby TBI translates directly to the potential side effects a patient may experience. Fr example, injuries on the right side of the head are more likely to cause manic symptoms, injuries to the left side of the head are more likely to cause depressive symptoms, and frontal-cortex injuries can lead to personality-disrupting symptoms such as impulsivity and disinhibition.
TM: If patients experience psychological symptoms associated with TBI, what might they expect?
DA: The short- and long-term psychological effects depend o the severity and location of the injury as well as the age of the patient and their overall mental state before the TBI, especially if there were pre-existing psychological or functionality issues. The ideal treatment approach depends on multiple factors. This is why a team approach is advantageous so that we can cover as many bases as possible to benefit the patient
TM: What role does psychiatric medication play in TBI recovery?
DA: Medication is just one component of TBI treatment. A simple analogy would be that therapy is akin to an elite athlete’s training while finding the ideal medication for a patient is akn to finding the ideal diet for that athlete. ake Michael Phelps, for instance. He would not have been successful at the Olympics if he was eating unhealthy foods. He needed a certain diet to achieve success. Although the medications we use in TBI patients are often the same as those used to address primary psychological disorders, it is important to start a TBI patient on a very low dosage. This is because TBI-induced psychological symptoms are inherently diffeent from typical psychiatric issues. For more information on Dr. Amiri: (424) 360-0155 or connectwellnesscenter.com.