5 minute read
PROTECTING PATIENTS
From reducing unexpected costs to improving patient outcomes
Reducing Opioid Overdose Risk
Advertisement
While public awareness and efforts to stop addiction and overdoses have intensified, some communities reported higher-thanever rates of opioid-related deaths in 2020. Recent research led by Dima M. Qato reveals that although high-risk prescription opioid use has declined, nearly 1 in 10 adults takes opioids that put them at increased risk of an overdose. “These findings underscore the importance of strengthening the implementation of overdose prevention, particularly naloxone access laws, and harm-reduction strategies,” Qato says.
Qato and colleagues examined a representative 5% sample of anonymized data drawn from individual prescription claims from
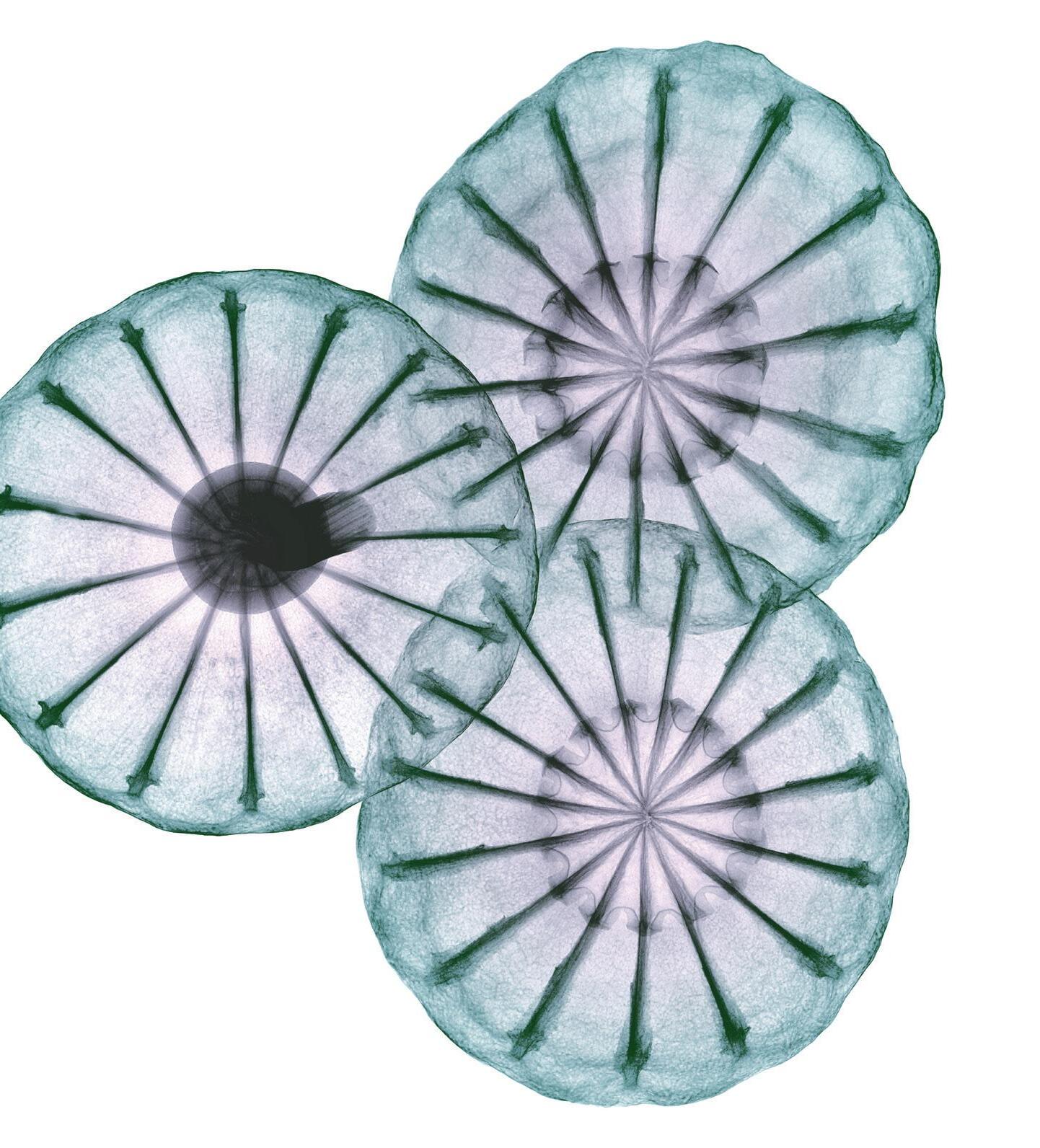
Color-enhanced X-ray of the seedpod of an opium poppy (Papaver somniferum). Opioid drugs are obtained from these unripe seedpods. In the body, the drugs bind to opioid receptors on neurons (nerve cells) and block the pathways of pain signals. USC Mann School faculty are working to address the opioid epidemic on multiple levels.
2011 through 2016. The study analyzed use among U.S. adults age 18 and older who filled prescriptions at retail pharmacies.
The research team factored in dangerous co-prescriptions of benzodiazepines, a class of sedatives commonly prescribed for anxiety, seizures or insomnia. Combining opioids with benzodiazepines further increases the risk of overdose and death, the investigators found. More than half of high-risk prescription opioid users received their prescriptions from a single provider. The study detected higher rates of risk among older consumers, who tended to use Medicare for payment. They were also more likely than their younger counterparts to have multiple prescribers and purchase from multiple pharmacies.
Improving Medication Use
Suboptimal medication adherence puts patients at risk and costs our nation’s healthcare system hundreds of billions of dollars annually. Steven Chen—associate dean for Clinical Affairs and the William A. Heeres and Josephine A. Heeres Chair in Community Pharmacy—works to optimize medication use to save lives and eliminate avoidable medical expenses.
His research earned a landmark $12 million grant from the Centers for Medicare & Medicaid Innovation to test the effectiveness of having pharmacists deliver comprehensive medication management as a way to improve adherence, especially in underserved communities. That work led Chen to establish and lead the influential California Right Meds Collaborative, which engages health plans, pharmacists, health systems and pharmacy schools in advancing sustainable comprehensive medication management services. The results turn patients into partners with pharmacists and physicians to ensure that vital medications are chosen, prescribed and taken for the best results and fewest side effects possible.
Saving Money but Increasing Risk
Although warfarin is the standard treatment for lowering the risk of stroke from atrial fibrillation, non–vitamin K antagonist oral anticoagulants (NOACs) have emerged as a more effective alternative with fewer side effects. NOACs also tend to be more expensive. Research led by Geoffrey Joyce and Seth Seabury finds that the formulary restrictions used by insurers and pharmacy benefit managers to save money result in fewer patients using NOACs or warfarin— which likely leads to poor health outcomes.

The study finds that beneficiaries in Medicare Part D plans with restricted access to NOACs have a lower probability of using the drugs, and those with reduced access show worse medication adherence. In addition, patients in the sample faced longer delays in filling their initial prescription after an atrial fibrillation diagnosis. This all adds up to a higher aggregate risk of death, stroke, transient ischemic attacks or systemic embolism for patients with restricted coverage.
The researchers note that, while formulary restrictions can be appropriate, such policies should be continuously reviewed to ensure that patients have timely access to effective medications.
Improving Safety for Cannabis Users
While many believe that using cannabis, particularly CBD, is perfectly safe, new research by Kari Franson demonstrates that some people are at real risk. She focuses on increasing the understanding of how cannabis affects health and how policy can enhance safety. Her work has revealed that the effects of cannabis on the endocannabinoid system— which regulates numerous bodily functions but produces molecules structurally similar to those of marijuana—increase the risk of mood disorders in certain users.

Easing Anxiety Disorders
Jing Liang recently revealed a connection between Alzheimer’s and stress-induced neuroinflammation of the kind heightened by social isolation during the COVID-19 pandemic. This work suggests that interventions may be able to stave off the disease in its earliest stages. Homing in on astrocytes—cells that regulate brain function—as a probable mechanism in social isolation-induced anxiety, Liang and colleagues, including Daryl Davies, are examining the potential of a compound she developed from the herbal supplement dihydromyricetin (DHM) in restoring the function of astrocytes damaged by stress. They previously demonstrated that

DHM counteracts the effects of alcohol intoxication and has liver-protective properties. Liang and Davies are refining DHM to enhance its uptake in the bloodstream and improve its clinical effectiveness. Their work also has the potential to help military veterans affected by post-traumatic stress disorder, who face a heightened risk of Alzheimer’s.
Promoting Youth Mental Health
Despite increased public funding and awareness, access to mental healthcare remains limited for many vulnerable groups—especially young people. On average, only one specialized psychiatrist is available for every 10,000 children needing mental health services nationwide. Even when treatments are available, medication safety in children and adolescents remains a public health challenge. Julie Dopheide and Steven Chen contributed to a review paper offering a solution to this shortfall: Add pharmacists to mental health teams. Their piece for the journal Child and Adolescent Psychiatric Clinics of North America explained the importance of interdisciplinary collaboration between pharmacists and child psychiatrists to achieve better outcomes for patients.
Recognizing the critical need for comprehensive medication management in psychiatric care, Chen adds that numerous states and counties are expanding pharmacists’ roles in the specialty. Policymakers in California, Indiana, Texas and other states have partnered with pharmacists to issue pediatric psychotropic guidelines or practice parameters. The authors bolstered their findings with three case studies illustrating the difference that psychiatric pharmacists and comprehensive medication management made in the lives of patients between ages 10 and 16 with conditions such as schizophrenia, severe depression, attention deficit hyperactivity disorder and autism spectrum disorder.

Taking the Sting out of Surprise Billing
Patients have long suffered financial strain from exorbitant, surprise medical bills stemming from out-of-network care. Collaborative work at the Schaeffer Center and its Schaeffer Initiative for Health Policy—a partnership with Brookings Institution—has informed numerous pieces of legislation at the state and federal levels to protect consumers from this practice, also known as balance billing.
The most sweeping of these is the federal No Surprises Act, which went into effect January 1, 2022. In addition to making it illegal to bill patients for more than innetwork cost-sharing for certain services, the legislation establishes an arbitration process to resolve disputes between providers and insurers. Following the bill’s passage, Schaeffer Center researchers have continued to conduct analyses, examine the best ways to maximize its effectiveness and write recommendations for implementing the new law, many of which were adopted in the administration’s rulemaking.
“The law is a big win for patients, employers and consumers,” Schaeffer Center CoDirector Erin Trish notes.
Other recent research by Trish showed that, in just one year, Medicare paid $2.6 billion more for generic medications than the amount spent by cash-paying Costco members for the same drugs. “Policymakers should do what they can to interject transparency and competition to improve incentives,” she says.

MEDIA MENTIONS QUOTING SCHAEFFER INITIATIVE ABOUT THE NO SURPRISES ACT
$ 2.6 BILLION EXCESS AMOUNT MEDICARE PAID FOR GENERIC DRUGS OVER COSTCO’S PRICE









