2 minute read
Rectal Cancer
suggested that intensive chemotherapy should be used with caution in patients ≥75 years with low autonomy and cognitive impairment, and support the importance of the evaluation of risk factors for toxicity in older cancer patients being considered for chemotherapy (eg comprehensive geriatric assessment).
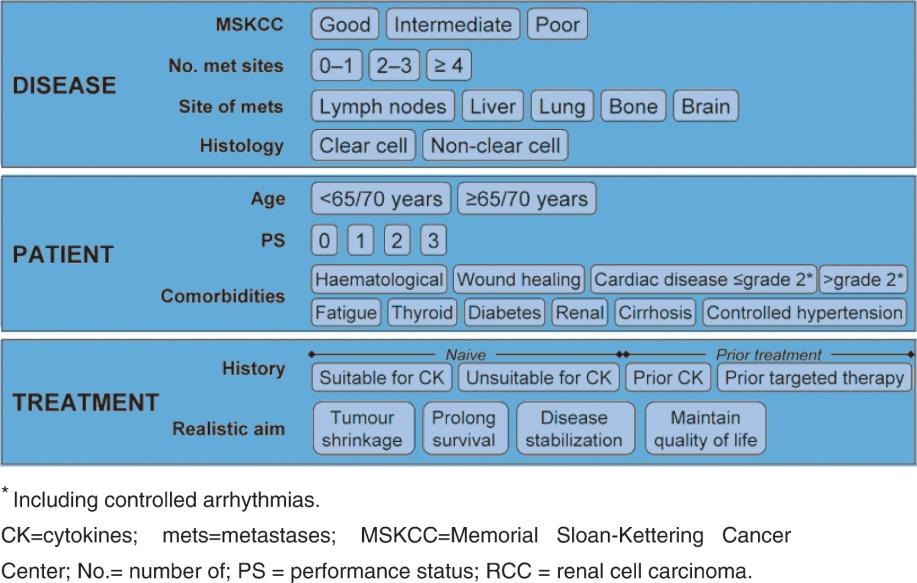
Increasingly, combination chemotherapy plus a targeted agent (bevacizumab, cetuximab, and panitumumab) is being used to treat mCRC patients. Fit older patients selected for inclusion in clinical trials appear to derive a similar benefit to younger patients in terms of RR and PFS from the use of bevacizumab plus full-dose combination chemotherapy. However, the data are lacking as to whether this leads to significant patient-relevant gains such as improved survival with an acceptable QoL. Bevacizumab has a side-effect profile that needs careful consideration when treating older patients, with a modest increase in the risk of arterial thrombotic events in addition to side-effects seen also in younger patients such as hypertension. The addition of Bevacizumab to single agent capecitabine in patients over 70 (“AVEX” trial) achieved encouraging results with a significant PFS improvement over single agent capecitabine. For those older patients for whom intensive combination therapy would be inappropriate, such a lower dose capecitabine plus bevacizumab regimen can therefore be considered. Evidence for the use of epidermal growth factor receptor (EGFR) inhibitors is less abundant. Based on limited data from pooled analyses, it seems that the use of Cetuximab in combination with FOLFIRI or FOLFOX, according to K-ras status, may provide a PFS and OS benefit in patients over 70 as well. The commonest toxicity observed is skin rash. Although the prevalence of this side effect is similar between all age groups, older patients may appear with higher grades and duration of skin toxicity. Data for the use of panitumumab and newer agents like regorafenib and aflibercept in older patients are still limited.
Advertisement
Overall, older patients with mCRC may gain survival benefit and symptomatic relief from 5U/LV or capecitabine monotherapy. Cytotoxic combination treatment with irinotecan, oxaliplatin or targeted agents may benefit more fit older patients. Compromising doses with combination chemotherapy in less fit patients on the other hand may not have a clear impact on symptoms, QOL improvement or survival extension. For such patients, less intensive regimens may be used such as the “stop and go” approach, where treatment is given intermittently according to the patient’s condition and wishes.
Total mesorectal excision and rectal surgery in general are technically demanding, especially in older patients. Postoperative mortality and severe complications are higher than in younger patients. Aggressive surgical treatment or permanent stoma can come at the expense of reduced functional status for older patients, and therefore the risk of local recurrence with regards to life expectancy must be considered before any therapeutic decision is taken.