2 minute read
Future Perspectives
overall survival in higher-risk MDS in comparison with a conventional care regimen. Effectiveness of AZA in response and survival prolongation was demonstrated in a subgroup analysis even in elderly MDS patients ( 75 years). As patients respond often after several courses, at least six cycles of AZA are recommended. In the absence of unacceptable toxicity or disease progression, continued AZA treatment might further improve responses in MDS. Besides induction of a complete remission (CR) or a partial remission (PR), hematologic improvement of anaemia or thrombocytopenia including stable disease, might be clinically relevant as they have shown to be associated with prolonged survival. Actually studies are ongoing to improve the effectiveness of AZA by addition of lenalidomide or histone deacetylase inhibitors.
• Decitabine and azacitidine show similar response rates and toxicities, azacitidine significantly improved overall survival and time to acute myeloid leukaemia transformation. These benefits were not found with decitabine (Xie M et al. 2014).
Advertisement
Therefore, azacitidine is recommended as the first-line hypomethylating agent for
MDS, especially in elderly patients or those with high risk. • Valproic acid (VPA) was used as an anticonvulsant for decades and might be effective in myeloid neoplasms by the inhibition of histone deacetylase. As VPA causes an erythroid response in about 50% of patients in low-risk MDS, treatment with valproic acid might represent a useful alternative in low-risk MDS patients with a low probability of erythropoiesis-stimulating factors (ESF) response (Figure 1). In senior patients monitoring of VPA serum concentrations is essential.
Intensive Therapies in elderly MDS: Current Standards
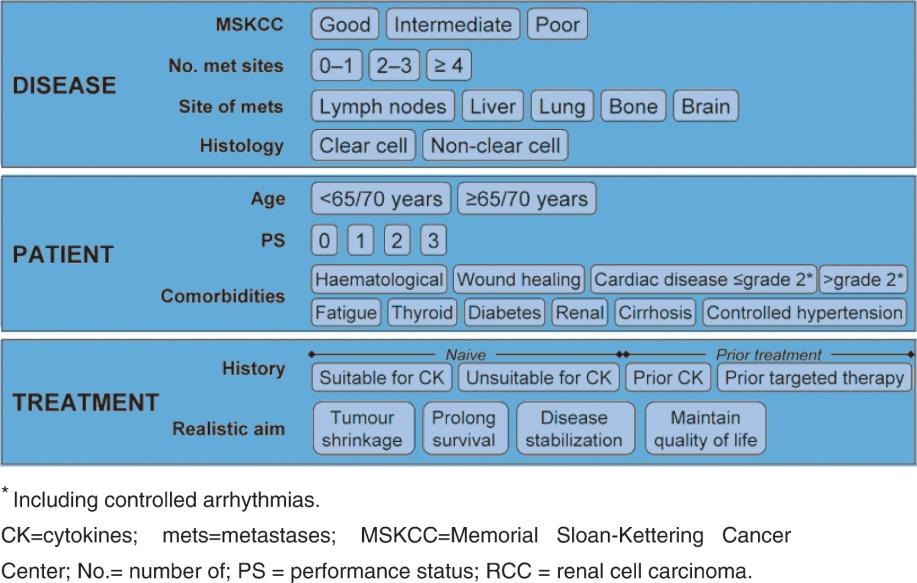
Allogeneic HSCT represents so far the only curative treatment approach in MDS. As this therapy is associated with a relatively high risk of transplant-related morbidity and mortality, a HSCT with reduced intensity conditioning (RIC-HSCT) can only be offered to a small cohort of elderly patients, who are characterised by an excellent performance status and the lack of relevant co-morbidities. Similarly to HSCT, intensive AML-like polychemotherapy can restore normal polyclonal haematopoiesis in subgroups of patients, but induces long-term disease-free survival only in a minority of patients. In a given elderly patient, the final decision to apply intensive therapies must be based on multiple parameters including karyotype, functional capacities, co-morbidities and patient preference (Figure 2).
As a result of the development of innovative therapeutic options in MDS including epigenetically active drugs, immune modulating agents, thrombopoietic agents and effective iron chelators, the treatment of elderly MDS patients has become more successful, but also more complex. The results of relevant clinical phase III studies, which might change daily practise, are expected in the near future. To choose the appropriate treatment for an elderly MDS patient, not only chronological age but also aspects of age-