4 minute read
Treatment Options in Elderly MDS Patients
survival as well as for event-free survival in MDS patients in uni- and in multivariate analyses and predicts non-leukaemic deaths.
The systematic evaluation of the scores of the geriatric assessment in MDS has just started. The prognostic relevance of functional capacities, mood and cognition has been demonstrated in MDS recently and forms the basis for further analyses. The inclusion of patient-reported outcomes (PROs) including health-related quality of life (HR-QoL) by assessing and integrating the patient’s wishes and needs, will further improve individualised decision-making in MDS.
Advertisement
The performance and integration of scores of the geriatric assessment in MDS has just started but will considerably improve individualised therapy-planning in clinical studies and in medical practise.
Transfusion Therapy, Growth Factors and Iron Chelation
An essential goal in the treatment of senior MDS patients is to manage and to counteract the consequences of cytopenias and to maintain and increase the quality of life (QOL).
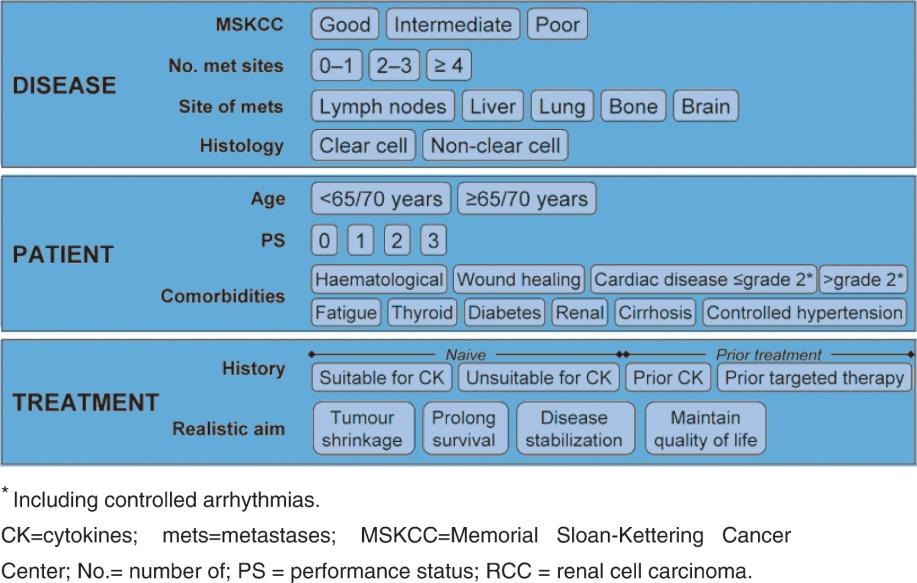
• Anaemia is present in the vast majority (80-90%) of MDS patients and results in an impaired HR-QoL. In addition, a high red blood cell (RBC) transfusion frequency represents an unfavourable risk factor for survival. Transfusion therapy using RBC aims to reach a range of 80-100 G/L in cardio-respiratory healthy persons and >100120 G/L in elderly and in persons displaying co-morbidities. RBC-transfusions should be kept to a minimum. Erythropoiesis-stimulating agents (ESAs) with or without granulocyte-colony stimulating factor (G-CSF) represent the standard of treatment for transfusion-dependent anaemia in lower-risk MDS (Figure 1). • ESAs represent an effective treatment of anaemia in MDS to improve haemoglobin levels, to reduce transfusion need and to increase QoL. As low endogenous erythropoietin (EPO) levels as well as a low transfusion need result in an increased response rate, predictive models for ESA treatment have been developed. The Nordic
Score identifies patients with low, intermediate and high probability of response (Table 5). Moreover, G-CSF is administered in combination with ESAs in low/intermediate risk patients to augment the erythroid response, which is particularly effective in patients with an increase of ring sideroblasts (RARS). ESAs have been used safely in larger numbers of MDS patients with no evidence for negative impact on survival or AML evolution. Moreover, ESAs even seem to improve survival in treated patients. Despite their widespread use in MDS, ESAs are so far not registered in this indication. Prospective, randomised clinical studies are ongoing. When applying ESAs the increased risk of thromboembolic complications should be considered. Whereas the majority of MDS-patients suffer from iron-overload, iron deficiency should be assessed at the start and during the course of an ESA-therapy
by analysing serum ferritin levels, transferrin saturation and corrected by iron supplementation orally or i.v. • In neutropenic infections in MDS the interventional use of G-CSF is recommended. • In thrombopenic patients platelet transfusions are given to prevent bleeding.
However, due to immunisation, frequent transfusions might cause a poor response.
Thrombopoietic agents like romiplostim or eltrombopag, which are approved for the treatment of immune thrombocytopenic purpura (ITP), have been introduced in MDS and are currently evaluated in clinical trials. First reports promising results show that romiplostim results in a decrease in the number of bleeding events and platelet transfusions. Although the study drug was discontinued because of an initial concern of AML risk, survival and AML rates were similar with romiplostim and placebo. • Frequent RBC transfusions result in iron overload and may cause transfusion-related hemochromatosis, which primarily affects the heart and the liver. As the risk of events becomes apparent when RBC transfusions exceed 20 and serum ferritin levels exceed 1500-2000 ng/mL, treatment with iron-chelating agents such as desferoxamine (applied either subcutaneously or intravenously) or deferasirox (orally), should be considered. In most guidelines a reasonable expected survival (at least more than one year) is anticipated. Renal function has to be monitored carefully in elderly patients treated with deferasirox.
Immunomodulating Agents
• Lenalidomide represents an immunomodulating drug (IMiD) which is highly active in
MDS with 5q-. Lenalidomide produces major clinical and even cytogenetic responses that formed the basis for EMA and FDA approval. Lenalidomide also reveals activity in non-del5q- lower risk MDS (phase III studies to evaluate the relevance of lenalidomide in non-del5q- lower-risk MDS are ongoing). Relevant side effects of
Lenalidomide are neutropenias and thrombocytopenias. • Immunosuppressive strategies using combinations of anti-thymocyte globulin (ATG) and Cyclosporin-A (CyA) are effective in subgroups of younger patients in hypoplastic
MDS and with a HLADR15 phenotype. As ATG is poorly tolerated in elderly patients, a CyA monotherapy is generally preferred. Due to nephrotoxicity renal function has to be monitored closely.
Epigenetic Therapies
The hypomethylating agents 5-azacitidine and decitabine have shown encouraging results in higher-risk MDS patients. 5-azacitidine (AZA) is already considered to be the standard of therapy in elderly higher-risk MDS, who are not eligible for intensive therapies such as AML-induction or hematopoietic stem cell transplantation (HSCT) (Figure 2). AZA has received EMA approval in MDS for this indication. In low risk patients, these drugs are analysed in clinical studies and might so far only be considered when signs of progression occur. AZA was demonstrated in a phase III study to significantly extend