2 minute read
Age-Adjusted Models and Assessment in Elderly MDS Patients
Prognostic Scoring System (IPSS) published in 1997 has become the most widely used risk assessment tool for MDS (Table 1). A revised IPSS (IPSS-R) was developed in 2012 (Table 2). Improvements include a refined classification of cytogenetic abnormalities. More detailed cut-offs for bone marrow blast counts and cytopenias, weighted for their severity, are integrated. Age has been included resulting in the IPSS-RA (Table 3). The IPSS-R has been validated in several studies and represents the gold-standard for clinical risk assessment in patients with primary MDS. Based on the IPSS patients are divided into lower-risk (Low to intermediate-1 IPSS; very low, low to intermediate IPSS-R) and higher-risk (Intermediate-2 to high IPSS; high to very-high IPSS-R) MDS. These prognostic subgroups differ significantly in survival and rates of leukemic transformation and maintain their prognostic significance even in MDS patients aged 70+. Both, IPSS and IPSS-R have improved risk stratification in clinical trials and are widely used for decision-making in clinical practise. However, IPSS and IPSS-R were established in primary MDS at initial diagnosis. Thus, limitations of both scores are the lack of data on dynamic aspects and therapy-related MDS. Moreover, molecular abnormalities, which are emerging as one of the most relevant clinical prognosticators, have not yet been integrated in IPSS/IPSS-R at all.
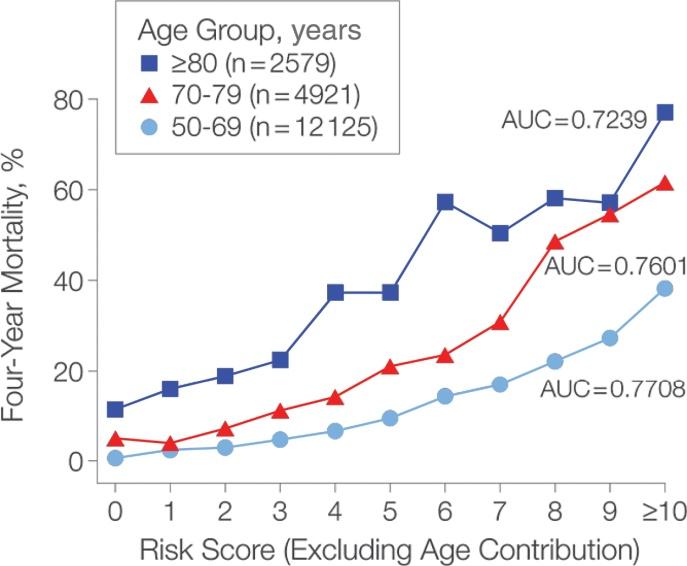
Age has a significant negative impact on overall survival in most analyses performed in MDS. In general, the relevance of age in prognostication is more pronounced in low-risk MDS than in high-risk disease. As shorter overall survival in older persons is logical, prognostication in the elderly should include age-adjusted parameters like the standardised mortality rate (SMR) or age-adjusted survival based on local survival statistics. Thus the survival in a given MDS patient is compared with an age- and sexmatched population. Analyses in representative cohorts of MDS patients achieved a SMR of around 5, implying a 5-fold increased risk of death for MDS. Addressing various age groups, younger patients revealed an SMR of 10 and elderly an SMR of 3.4. Even in elderly persons, MDS represent a relevant disease with a greater than threefold risk of disease-related death, resulting in a significant loss of life years in the majority of prognostic subgroups. However, in the prognostically excellent subgroup of elderly patients (70+ years of age), life expectancy was not different from the general population, pointing out the relevance of age-matched prognostic scoring systems for designing age and risk-adapted treatment strategies.
Advertisement
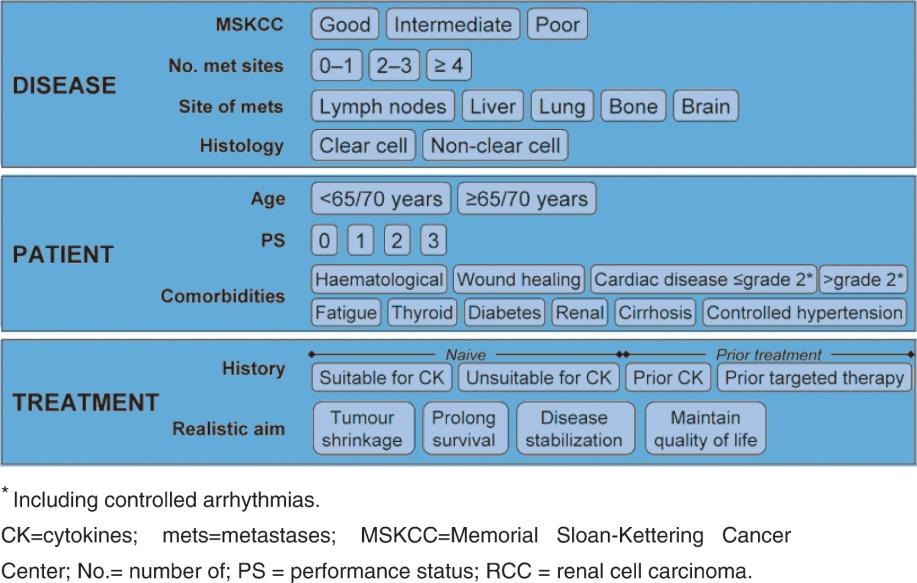
Whereas the scoring systems established so far are based on disease-specific prognostic factors like bone marrow blasts, karyotype or cytopenias, patient-related factors namely functional capacities or co-morbidities including cardiac insufficiency or tolerance to chemotherapy are less well defined. The integration of structured co-morbidity scores to classify and quantify co-morbid conditions has revealed a relevant prognostic impact of comorbidities in several studies. The haematopoietic stem-cell transplantation-specific co-morbidity index (HCT-CI), was found to be a significant prognostic factor for overall