2 minute read
Treatment Strategies of Polythemia Vera (PV) in the Senior Patient
to a higher co-morbidity burden. Thus, dasatinib is effective and safe also in older patients.
In the nilotinib clinical trials, approximately 30% of patients were older than 65 years of age. No major differences in safety were observed in patients >65 years of age compared to patients <65 years. Bosutinib, another second generation TKI, was tested in Phase 13 clinical trials. In those trials up to 20% were more than 65 years of age with 4% older than 75 years of age. No overall differences in safety or effectiveness could be observed between the younger and elderly patients. Other reported clinical experiences, have not identified any differences in responses between elderly and younger patients.
Advertisement
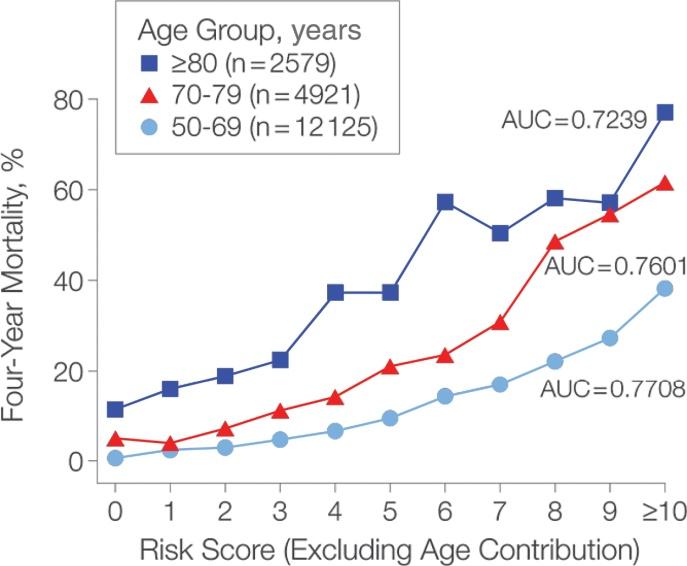
In PV the increased number of red blood cells or platelets can cause bleeding problems and induce clot formation in blood vessels. This can cause serious complications such as stroke or heart attack. In patients older than 65 years, the risk of stroke and heart attack is clearly higher, and PV is more likely to transform into acute leukaemia or PMF. Without treatment, patients with PV usually die from bleeding or blood clotting. In contrast, median survival is about 10 years in older patients when appropriately treated. Many patients can reach their normal life expectancy, if they do not develop marrow fibrosis or transform to leukaemia.
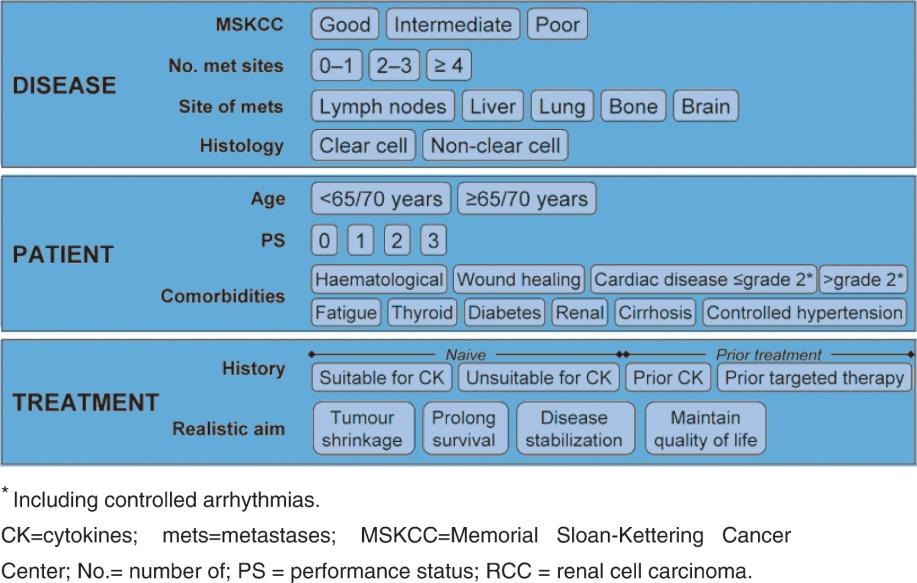
Currently, there are no studies available specifically addressing the question of how senior PV patients should be treated. However, the treatment options currently available for this disease are generally well tolerated and (after careful evaluation of relevant comorbidities of the individual patient) can be applied to elderly patients, for example:
• Periodically removing erythrocytes by phlebotomy represents a safe and very effective way to treat low-risk PV patients. The seminal CYTO-PV study provides clear evidence that haematocrit should be kept below 45% in both men and women. • Due to platelet activation, patients should also receive low dose aspirin (i.e. 100 mg per day), which can also be easily prescribed to elderly patients who have no contraindications against aspirin (major side effects are gastrointestinal intolerance and bleeding). • Patients with a higher risk of clotting (i.e. those who have risk factors such as leukocytosis, age >65 years and/or a previous thrombotic event) should receive additional cytoreductive therapy, such as hydroxyurea. This drug has relatively few side effects, and its beneficial effects in terms of prevention of vascular complications outweigh its potential harm (i.e. induction of leukaemia), which may not be as relevant in the elderly population when compared to younger patients. • In the case of insufficient response or intolerance to hydroxyurea or high symptom burden, the JAK1/2 inhibitor ruxolitinib is now also approved for PV therapy. Other