2 minute read
Palliative Setting: Toxicity and Efficacy Ratio
Response depends on sensitivity of tumour cells to radiation with adequate tissue oxygenation and ongoing cellular proliferation. Ongoing cellular proliferation varies according to the neoplasm site, its histology, and individual tumour biology. Two neoplasms at the same anatomic site, and with the same histology, may show a different response when exposed to the same radiation dose because of differences in proliferation.
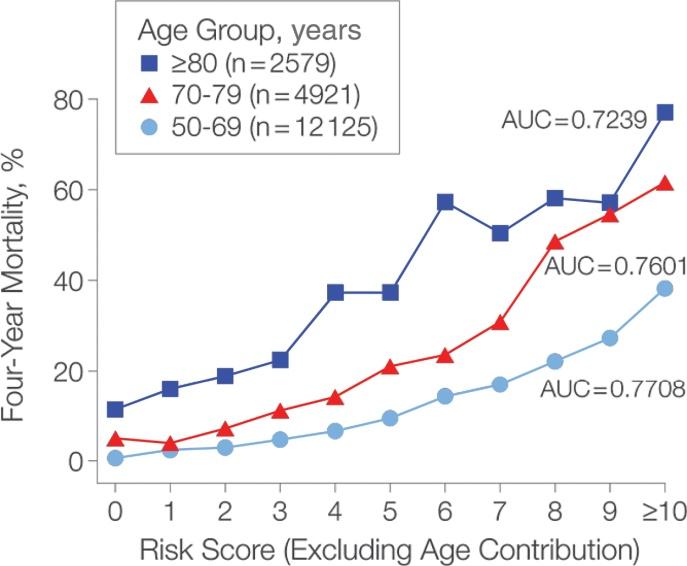
There is little information about the proliferative activity of tumours in the elderly, and there are no clinical data correlating tumour oxygenation with patient age. Experimental data in tumour-bearing mice have demonstrated that oxygenation of tumour cells decreased with age of the tumour-bearing animal. This correlation may be extrapolated to cancer patients, leading to a relevant age-related decrease in tissue perfusion. This, in return, may significantly affect sensitivity of some solid tumours to irradiation. But proliferative activity seems to be inversely correlated with age only for some neoplasms while in others, it remains independent. In several tumours, the H3-thymidine labelling index (TLI), a measure of cell proliferation, is decreased in elderly patients, suggesting that sensitivity of tumours to radiation may also be decreased compared with younger ones. Tissue hypoxia caused by age-related decrease in circulation and tissue perfusion might lead to reduced tumour sensitivity.
Advertisement
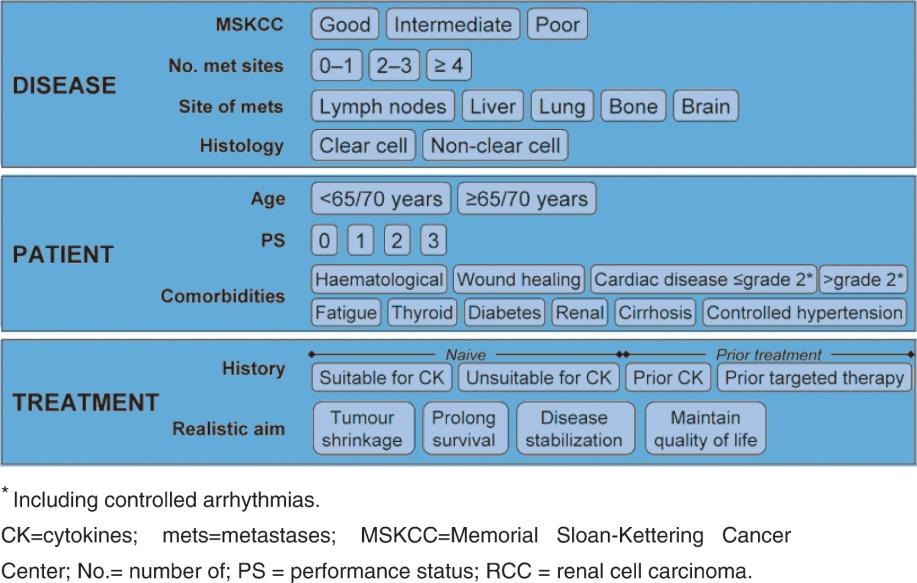
As for local control, there is currently no evidence that solid tumours show different outcomes between different age groups. In a retrospective analysis of nine European EORTC trials in patients with pelvic tumours and age over 70, it was concluded that there were no differences in local control and overall survival following radiotherapy based on patient age. In 1996, 1997, and 1998, three reviews have analysed the relationship between age at presentation and clinical outcome of patients treated within EORTC radiotherapy protocols. These reviews included 4,406 patients with different cancers [e.g. head and neck, thoracic (including breast and lung cancers), and pelvic cancers (including bladder and prostate)].
Age did not influence locoregional recurrences and overall survival for head and neck tumours after radical radiotherapy. In pelvic malignancies, analysis adjusted for T stage showed comparable local control and disease-free survival between different age groups for anal, prostate, and uterine cancers. In contrast, younger patients with rectal cancer survived significantly longer than older patients, possibly explained by increased treatment-related mortality in this setting. On the whole, patient age did not represent a limiting factor for radical radiotherapy in pelvic malignancies, excluding rectal cancer.
Once cure is no longer realistic because of large bulky tumours or advanced disease, palliative radiotherapy may still be administered with palliative intent. The predominant aims of radiation in this setting are symptom relief (e.g. bone pain in bone metastases, reduction of neurological symptoms in brain metastases, bleeding of mucosal tumours) and control as well as improvement of quality of life. Toxicity to normal tissues and