2 minute read
Comprehensive Geriatric Assessment
instruments in six comparisons, whereas results were mixed for the VES-13 in seven comparisons.
None of these tools are very specific and, therefore, if positive, they need to be supplemented by a more complete GA. However, they can help to focus geriatric resources towards those patients who need them most.
Advertisement
Practical Tips
Review a few of the tested tools and choose the one best adapted to your clinical setting. For example, a short tool filled out by patients, such as the G8, is probably best if you want many clinics to test all older patients for referral to a multidisciplinary clinic. On the other hand, if you have a multidisciplinary clinic where team members can assess the patients at first visit, a slightly more extensive tool, such as the SAOP2, can help you identify more precisely which team members to involve. Most screenings can be patientanswered or included in the initial nursing assessment.
Further assessment is needed if a patient screens positive using the short screening tools described above. The format for further assessment is highly dependent on the local resources: some institutions have an embedded geriatric oncology team; others have a geriatric consultation service; other centres have combined outpatient visits by a geriatrician and an oncologist; in other settings, the only option might be for the medical team to add geriatric instruments to its oncologic evaluation.
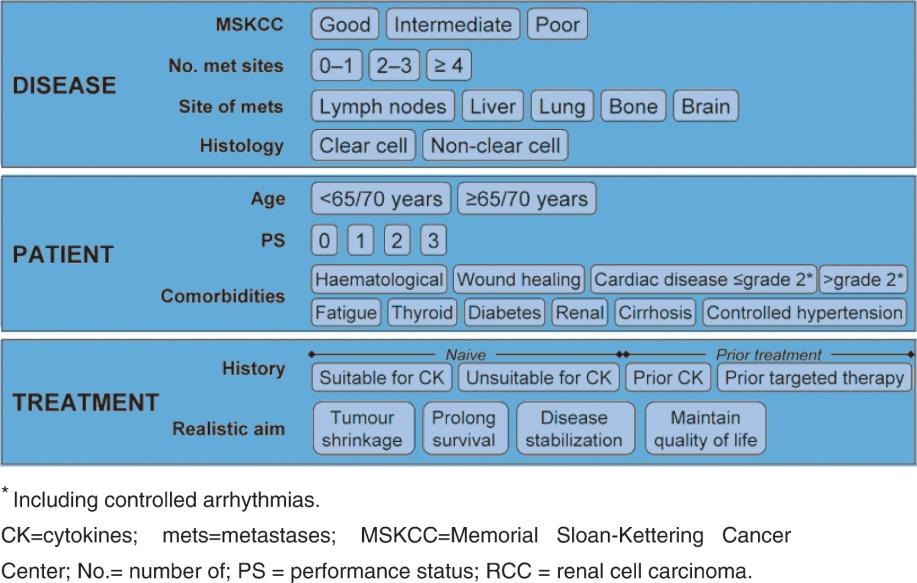
Important domains in a GA are functional status, comorbidity, cognition, mental health status, nutrition, social status and support, fatigue, and assessment for polypharmacy and presence of geriatric syndromes. Various tools are available for assessing these domains.
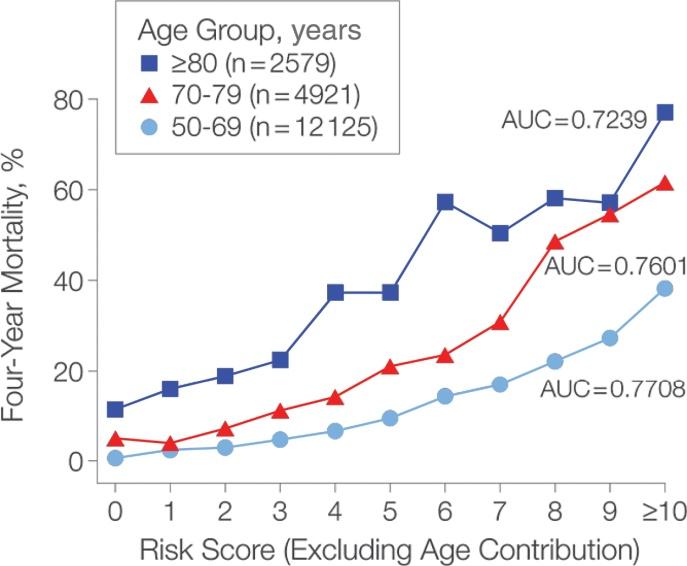
There are strong general data on the effectiveness of geriatric interventions. What are the data specific to cancer patients? Here again, SIOG has published a recent update of its 2005 guidelines. Besides the ability of CGA to detect unidentified problems, there is now solid evidence that these problems affect prognosis independently from classic oncology predictors. CGA items can predict survival or treatment complications. More research still needs to be done on its ability to predict functional and QOL outcomes in cancer patients. There are now several studies demonstrating that a CGA/geriatric consultation modifies the management of cancer patients (Table 2).
Table 2. Treatment modifications by CGA. Studies reporting changes from a baseline oncology treatment plan.
Study # Patients Intervention Treatment changes Comments
Aliamus 49 GA
Aparicio 21 Mini GA 44.9%
0%
72% adaptation of non-oncological treatment
Caillet 375 Referral to geriatrician, extensive CGA, multidisciplinary meeting 20.8% intensification
of cancer treatment (n= 8, 10.2%), delayed cancer treatment to allow geriatric management (n= 7, 9.0%), and decrease in cancer treatment intensity (n= 63, 80.8%;
Chaibi 161 Full geriatric consultation 79 pts (49%)
Delayed therapy in 5 patients, less intensive therapy in 29 patients and more intensive therapy in 45.
76% of patients had a geriatric therapeutic intervention
Decoster 902 GA by trained nurse, filed in chart.
42.2% oncologists modified treatment based on age (44.2% in the subgroup where they consulted the GA)
Based on GA, 6.1% did extra modification. The judgment as to whether the treatment was modified due to age or the GA was rated by the oncologists a posteriori.