




Chief Executive Officer
Megan N. Schagrin, MBA, CAE, CFRE Ext. 212, mschagrin@saem.org
Director, Finance & Operations
Doug Ray, MSA Ext. 208, dray@saem.org
Manager, Accounting
Edwina Zaccardo Ext. 216, ezaccardo@saem.org
Director, IT
Anthony "Tony" Macalindong Ext. 217, amacalindong@saem.org
IT AMS Database Specialist

Dometrise "Dom" Hairston Ext. 205, dhairston@saem.org
Specialist, IT Support
Dawud Lawson Ext. 225, dlawson@saem.org
Director, Governance
Erin Campo Ext. 201, ecampo@saem.org
Manager, Governance
Juana Vazquez Ext. 228, jvazquez@saem.org
Director, Communications & Publications
Laura Giblin Ext. 219, lgiblin@saem.org
Sr. Manager, Communications & Publications
Stacey Roseen Ext. 207, sroseen@saem.org
Manager, Digital Marketing & Communications
Alison “Ali” Mistretta Ext. 244, amistretta@saem.org
Sr. Director, Foundation and Business Development
Melissa McMillian, CAE, CNP Ext. 203, mmcmillian@saem.org
Sr. Manager, Development for the SAEM Foundation
Julie Wolfe Ext. 230, jwolfe@saem.org
Manager, Educational Course Development
Kayla Belec Roseen Ext. 206, kroseen@saem.org
Manager, Exhibits and Sponsorships
Bill Schmitt Ext. 204, wschmitt@saem.org
Director, Membership & Meetings
Holly Byrd-Duncan, MBA Ext. 210, hbyrdduncan@saem.org
Sr. Manager, Membership
George Greaves Ext. 211, ggreaves@saem.org
Sr. Manager, Education
Andrea Ray Ext. 214, aray@saem.org
Sr. Coordinator, Membership & Meetings
Monica Bell, CMP Ext. 202, mbell@saem.org
Specialist, Membership Recruitment
Krystle Ansay Ext. 239, kansay@saem.org
Meeting Planner
Kar Corlew Ext. 218, kcorlew@saem.org
AEM Editor in Chief
Jeffrey Kline, MD AEMEditor@saem.org
AEM E&T Editor in Chief
Susan Promes, MD AEMETeditor@saem.org
AEM/AEM E&T Peer Review Coordinator
Taylor Bowen tbowen@saem.org aem@saem.org aemet@saem.org
Wendy C. Coates, MD President
UCLA Department of Emergency Medicine
David Geffen School of Medicine at UCLA
Ali S. Raja, MD, DBA, MPH President Elect
Massachusetts General Hospital/Harvard
Members-at-Large
Pooja Agrawal, MD, MPH
Yale University School of Medicine
Jeffrey Druck, MD
The University of Utah School of Medicine
Julianna J. Jung, MD
Johns Hopkins University School of Medicine
Nicholas M. Mohr, MD, MS University of Iowa
Michelle D. Lall, MD, MHS Secretary Treasurer Emory University
Angela M. Mills, MD Immediate Past President
Columbia University Vagelos
Ava E. Pierce, MD UT Southwestern Medical Center, Dallas
Jody A. Vogel, MD, MSc, MSW Stanford University
Department of Emergency Medicine
Resident Member
Michael DeFilippo, DO, MICP NewYork-Presbyterian - Columbia & Cornell
3 President’s Comments
The ERAS Season: An Opportunity to Foster Partnerships, Mentorships in Academic EM
4 SAEM Board Corner
SAEM board liaisons provide a roundup of what's happening in the Society's many active groups.
6 Spotlight
Shaping the Future of the Academic EM Specialty – An Interview With Daniel N. Jourdan, MD, NRP 2023-2024 RAMS President
10 Career Pathways
Crafting a Compelling Cover Letter: A Guide to Standing Out in the EM Job Market
12 Clerkship Column
The Winds of Change Are Howling This EM Residency Application Cycle
14 Critical Care
5 Lessons in Creating a Resuscitation Fellowship
18 Educational Techniques Using Affordable, Reusable Simulation for Pericardiocentesis Training: A High Acuity, Low Opportunity Procedure
20 Ethics in Action
Treating an Undocumented Survivor of Assault and the Involved Assailant in the Emergency Department
22 Faculty Focus
Dr. Jeffrey Glassberg: A Leader in Research and the Care of the Sick Cell Disease Patient
26 Geriatric EM
Enhancing Older Adult Care in the ED: The Impact of a Geriatric Comfort Cart
28
Pediatric EM
THC-8 Toxicity in Pediatric Patients: Understanding the Risks and Ensuring Safety
30 Research Addressing Diversity in the EM Research Workforce
34 Toxicology
Snake Envenomation Follow-Up Clinic Expands Frontiers of Emergency Medical Care
38
Ultrasound
Contrast Enhanced Ultrasound: The Missing Puzzle Piece in the Care of the Acutely Ill Child
40 Viewpoint
Supreme Court of the United States Affirmative Action Rulings
44 Wellness Perspective
#StopTheStigmaEM Month: From Awareness to Embracing and Elevating Daily Well-Being
46 Wilderness Medicine
Altitude Illness, Migraines and Concussions: Are They Related?
48 Nutrition in the Endurance Athlete
50 Workforce Update: Fall 2023
The Past, Present, and Future of the EM Workforce
52 The Legacy Society: Donors Sustaining EM Research Well Into the Future
54 Briefs & Bullet Points
Important news, information, and upoming deadlines from SAEM.
58 SAEM Reports
News from SAEM's committees, academies, and interest groups.
60 Academic Announcements Appointments, promotions, awards, and other good news about your EM peers and colleagues!
62 Now Hiring

UCLA Department of Emergency Medicine
David Geffen School of Medicine at UCLA 2023-2024 President, SAEM
“Each of us can contribute by engaging with the eager medical student rotators to help them feel welcome in our departments, sharing our enthusiasm and the reasons we chose emergency medicine, and exposing them to the depth of scholarly opportunities of a career in academic EM.”

As we transition from a busy summer that boasts excitement in launching our graduates to the workforce, welcoming new faces, and engaging in activities with our families, to the more structured “school year,” we can now focus on how to create new opportunities for career advancement and professional fulfillment for ourselves and our colleagues.
The “ERAS* season” is upon us, and the program leadership team at each institution is hard at work identifying potential residents who will be a "great fit" to interview. Each of us can contribute by engaging with the eager medical student rotators to help them feel welcome in our departments, sharing our enthusiasm and the reasons we chose emergency medicine (EM), and exposing them to the depth of scholarly opportunities of a career in academic EM. Our residents are settling into the rhythm of their new responsibilities. What an excellent time to identify someone to approach for collaboration on a project, to seek as a mentor, or to take on as a mentee!
Whether you aspire to improve your skills as a researcher, educator, or administrative leader, SAEM offers professional development opportunities for you! I urge you to consider joining one
of our cohort courses that will provide you with organized and critical knowledge, while also connecting you to a rich network of like-minded academicians across the career spectrum. The deadlines for applying to these courses vary, and some are rapidly approaching.
Establishing these professional connections is not only a good way to ensure career advancement but also a means to belong to a caring community. Every October, SAEM leads the #StopTheStigmaEM month-long campaign to raise awareness about the mental health strain that affects EM physicians. Our hope is to lower the barriers to mental health care and normalize conversations about mental health. I encourage you to take some time to focus on your own personal and professional satisfaction and growth and be open to lending a hand to others in our EM community.
*Electronic Residency Application Service®ABOUT DR. COATES: Wendy Coates, MD, is professor of emergency medicine at David Geffen School of Medicine at UCLA and senior faculty/ education specialist at UCLA Department of Emergency Medicine
The SAEM Bylaws Committee is one of two standing committees elected by the entire SAEM membership. Each Bylaws Committee member serves a three-year term, with the addition of a new member annually. SAEM is governed by officially ratified bylaws, sanctioned by the voting members. The Bylaws Committee is responsible for attaining a thorough understanding of these bylaws and reviews them annually to ensure their current and accurate status.

Professor of emergency medicine, David Geffen School of Medicine at UCLA Senior faculty/education specialist, UCLA Department of Emergency Medicine @CoatesMedEd
Dr. Coates is the SAEM Board liaison for the following SAEM groups:
Chair: Richard Rothman, MD, PhD
Overview
The main purpose of this collaborative group is to monitor National Institutes of Health (NIH) activities that are relevant to SAEM’s mission, build relationships with key NIH personnel, respond to NIH requests for information (RFI) on behalf of SAEM, and communicate opportunities to SAEM members.
During the current academic year, the group is focusing on increasing the number of EM departments applying for T32 awards. The goal is to double the number from 5 to 10 and increase the number of individuals funded through the T32 mechanism.
Collaborating with the NIH Office of Emergency Care Research (OECR), the group co-hosted a webinar, presented by Drs. Jeremy Brown and Cliff Calloway and featuring valuable insights for T32 applications.
Moreover, the group functions as a reservoir of resources for SAEM members seeking to understand how to navigate the NIH funding process. It also seeks to cultivate sustained relationships with each NIH Institute.
Chair: James Paxton, MD, MBA

Overview
In the event of a proposed modification or amendment, the Bylaws Committee studies the potential merits, possible drawbacks, and legal implications. Subsequently, they furnish their findings and recommendations to the SAEM Board for preliminary assessment before presenting them for formal consideration by the membership. If you see proposed Bylaws changes on any upcoming ballots, you can rest assured that this dedicated cohort has invested substantial effort into reviewing them prior to submitting them to the Board and subsequently, to you, for your vote! The commitee may also propose bylaws amendments directly to the SAEM Board. This close-knit and supportive small group provides a unique vantage point to understand the inner workings of the organization.
The SAEM Industry Advisory Council (IAC) collaborates with the SAEM leadership, SAEM Foundation, and Association of Academic Chairs of Emergency Medicine (AACEM) to fulfill the organization’s mission of fostering scientific discovery, advancing education, and upholding the highest professional and ethical benchmarks for clinicians, educators, and researchers.
Functioning as an advisory entity, the IAC provides input and insight from an industry perspective. Its purpose is to amplify the relationship between SAEM members operating within both industry and academia, while simultaneously advancing the Society’s presence within the corporate realm.
All IAC members are required to submit to and uphold a standard Code of Interaction with Companies, ensuring ethical and professional conduct in their engagements.
Chairs: Nicholas Stark, MD, Zaid Altawil, MD, Jonathan
Oskvarek, MD, MBAInterest groups hold a unique position within the organization, as they bring together members who share similar interests to set their own agendas and receive support from SAEM staff to accomplish their objectives.
The Innovation Interest Group has developed a Mission Statement: “To inspire and foster collaboration among innovation-minded emergency physicians to improve health through novel ideas and technology.”
Their objectives are to foster a network of individuals and institutions to share ideas and collaborate on applying innovation principles to the health care setting; inspire innovation-minded EM physicians to incorporate the best of design thinking and technology to improve the clinical practice and processes of medicine; support academic and community EDs in the design and operation of innovationfocused laboratories and centers; develop educational opportunities that further an understanding of innovation in emergency medicine; and cultivate collaboration between the technology industry, makerspaces, and EM physicians.
At their meeting during SAEM23, the interest group drew a standing room only audience of dozens of interested attendees. As this dynamic group moves forward, stay tuned for updates on how their innovative ideas are taking tangible shape and making a substantial impact.
Nicholas Mohr, MD, MS Member-at-large, SAEM BOD Professor, University of Iowa Carver College of Medicine @nicholas_mohrDr. Mohr is SAEM Board liaison for the following SAEM Groups:
Director: Stefanie Sebok-Syer, PhD
The ARMED MedEd course builds upon foundational research skills and teaches core concepts and principles of medical education, with a specific focus on increasing emergency medicine educational research funding. Offered annually, this competitive cohort-based year-long course comprises online lectures and in-person workshops.
• Preparing for the in-person ARMED MedEd workshop (for the 2023-24 cohort) this September at SAEM Headquarters in Chicago
• Accepting applications for the 2024-25 ARMED MedEd course, with a deadline of November 30, 2023.
• Celebrating five ARMED MedEd graduates or mentors (Jennifer Carey, MD; Petra Duran Gehring, MD; Hillary Moss, MD; Terena Chan, MD, MHPE; Di Coneybeare, MD, MHPH) who received educational research grants or distinctions in the past year
Chair: Keme Carter, MD
The Education Committee focuses on undergraduate, graduate, and continuing medical education in emergency medicine, and seeks to advance projects that improve emergency medicine education at all levels.
• Developing a formal RAMS Roadmap template outlining pathways in emergency medicine education, with recent offerings in palliative care, toxicology, resuscitation and critical care, and community medicine
• Hosting live webinars on medical education implementation science, featuring leading authors and journal editors
• Releasing many educational products (didactics, concept papers, podcasts, and webinars) covering topics such as effective learner supervision, entrustment to learners, bedside teaching, procedural instruction, and medical education trends
• Refining a diversity, equity, and inclusion (DEI) framework to serve as a foundation for educational products
Chair: D. Mark Courtney, MD, MSc
The Workforce Committee is committed to understanding the evolving landscape and workforce needs in emergency medicine by identifying opportunities to expand scope of practice, evaluating the evidence-based value proposition of emergency physicians, ensuring a robust training pipeline, and increasing understanding of emergency medicine workforce needs.
• Conducting qualitative study of EMinterested recent medical school graduates who chose non-EM residencies to understand attitudes, beliefs, and sources of guidance influencing final specialty selection (David Lu, MD, MSCI)
• Measuring and analyzing national trends in the emergency medicine workforce using publicly available billing and workforce datasets (Cameron Gettel, MD, MHS and Christopher Bennett, MD, MSc)
• Partnering with the American Board of Emergency Medicine (ABEM) to collect data on emergency medicine resident beliefs, attitudes, and anticipated future work arrangements through questions posed in conjunction with the Intraining Examination
Chair: Bernard Chang, MD, PhD
The Behavioral and Psychological Interest Group provides a platform for SAEM members interested in behavioral and psychological-themed topics to collaborate, share ideas, and disseminate ongoing and planned work.
Updates/Status
• Authoring several SAEM Pulse publications on provider education about opioid use and clinician health
• Leading buprenorphine training initiative in collaboration with faculty (Dana Sacco, MD) and residents (Corey Hazekamp, MD, MS)
• Collaborating with peer groups within the American Psychological Association and the Association for
Psychological Science to discuss future EM/mental health-focused projects
Chair: Robert Turer, MD, MS
The Informatics and Data Science Interest Group concentrates on recruitment, outreach, education, and collaboration for members interested in the intersection of emergency medicine and data science.
• Hosting an educational series on data science and machine learning concepts and applications, in partnership with the Innovation Interest Group, Telehealth Interest Group, and Residents and Medical Students (RAMS)
• Conducting a needs assessment to gauge the current landscape of education, training, and leadership in EM/data science
• Collaborating on a multicenter research project centered on patients’ use of personal health portals which has collated over 1 million patient ED encounters
Chairs: Laura Janneck, MD, MPH and Henny Hong, MD, MS
The Social Emergency Medicine and Population Health Interest Group provides a forum for the exchange of ideas and a platform for curriculum development related to the interplay between the emergency care system and social factors such as housing, food, violence, and other determinants.
Updates/Status
• Developing a residency curriculum of modules on core social emergency medicine topics in collaboration with ACEP (planned release 2023-24)
• Establishing a network of social emergency medicine fellowship program directors for a collaborative forum to share resources, content, innovations, and fellowship curricula
• Presenting cutting-edge research at the Social Emergency Medicine Journal Club, which meets the third Thursday of every month at 3 p.m. CT
Daniel N. Jourdan, MD, NRP, is a fourth-year resident in the combined emergency medicine/internal medicine program at Henry Ford. He attained a Bachelor of Science degree from the University of North Carolina Chapel Hill and a Doctor of Medicine from the Brody School of Medicine at East Carolina University, where he was also honored as a Gold Humanism Fellow. Prior to his medical schooling, Dr. Jourdan dedicated four years to serving as an enlisted special operations soldier, completing two tours in Afghanistan. Throughout his undergraduate and medical studies, he concurrently worked as a paramedic for various emergency medical services (EMS) operations in North Carolina.
Dr. Jourdan currently holds the position of SAEM-RAMS President for the term 2023-2024. His involvement with RAMS commenced during his time as a medical student, during which he participated as a member of the RAMS Education Committee and was a developer of one of the first RAMS RoadMaps. He was subsequently elected as a RAMS Board member-at-large and served in that capacity for three consecutive terms. Dr. Jourdan has also fulfilled the role of RAMS Board Liaison to several SAEM committees, including the education, faculty development, membership, nominating, and program committees. Most recently, he chaired the RAMS Nominating Committee. Dr. Jourdan's contributions to SAEM-RAMS have yielded numerous nationally published articles, podcasts, and educational materials available on SAEM.org, as well as presentations at the SAEM Annual Meeting. In addition to his commitment to SAEM-RAMS, Dr. Jourdan has been an integral part of various national task forces, including the SAEM Workforce Task Force, SAEM Advanced Practice Provider (APP) Task Force, and SAEM Onboarding Task Force.
As the new president of SAEM RAMS, what issues do you feel are most germane to current and future emergency medicine trainees? What steps do you hope to take toward addressing these issues during your tenure as RAMS president?
While the future of emergency medicine remains bright, our rapidly evolving specialty has encountered a multitude of challenges for our members in training that the RAMS Board is actively working to address — most importantly, the recent workforce study denoting findings concerning the availability of future employment. This is certainly one of the largest drivers of the recent decrease in emergency medicine residency applicants. We continue to focus on potential errors within the studies and work to educate applicants on the benefits of the specialty while readdressing workforce projections given the changes experienced during the pandemic. Additionally, our Workforce Task Force continues to focus on promoting better conditions for residents throughout the country. As well, we continue to focus efforts on addressing prolonged emergency department boarding times, diminishing emergency psychiatric resources and midlevel encroachment on training environments.
When, why, and how did you first become involved with RAMS?
I was initially pointed toward RAMS by one of my mentors, Dr. Laun Lawson, an assistant dean at my medical school. I joined and immediately became heavily involved in the SAEM Education Committee producing one of the first RAMS RoadMaps focused on a career in EM medical education. I ran for, and lost, an election for RAMS Board member-at-large but persisted and won the following year.
Why should EM residents and medical students become involved with RAMS? What needs does the group meet or concerns does it address?
For those who care about and want to help shape the future direction of our specialty, RAMS provides excellent opportunities to get involved in doing so. Our specialty remains young and rapidly evolving in the face of changing health care in the United States. We need early training participants to provide insight and recommendations to help focus RAMS’ and SAEM’s efforts
to address the challenges of workforce growth, mental health stigma, work conditions for residents, and advanced practice provider encroachment. Opportunities exist from limited, shortrun projects to multiple-year projects, so residents and medical students can be involved as their time permits.
Who or what influenced your decision to choose the academic/EM specialty and if you were not doing what you do, what would you be doing instead?

My time in the U.S. Army directly resulted in my interest in medicine, so I knew from the beginning I wanted to be on the front lines. When you close your eyes and imagine what a doctor is, often the tasks that come to mind are exactly those that occur in the emergency department: responding to medical emergencies and providing immediate stabilization and treatments. If I was not doing emergency medicine, I would likely pursue critical care, as it is largely an extension of the same —responding and treating the broad spectrum of medical emergencies.

Where do you see yourself in five years? Twenty-five years?
In five years, I hope to occupy an academic teaching role and continue to work in a quaternary academic center serving an underserved population. The challenge of dealing with the most complex patients and fostering the next generation of physicians is a reward in and of itself.
Given my nontraditional status, I would likely be approaching the twilight of my career in 25 years. I aspire to hold an administrative role in an academic institute continuing to focus my efforts on shaping the future of emergency medicine and its next leaders.
October is #StopTheStigmaEM month. Stigma is a leading barrier to mental health care for emergency physicians. Many fear that treatment for mental illness could jeopardize their careers or their licenses to practice. What would you say are the key challenges to addressing this stigma?
At this point, the challenges are well elucidated: the stigma that surrounds mental health and addiction within society has
continued on Page 8
Dr. Jourdan and his best friend, Zachary VanWyhe, in Afghanistan in 2010.continued from Page 7
ironically crept into the medical field. Instead of considering these issues as medical conditions similar to heart disease, they're often stigmatized. One significant challenge is that licensing boards inquire about past mental health treatments, and there's a prevailing attitude that mental health problems are personal failures rather than legitimate medical concerns. In the broader context, there's a longstanding belief in medicine that individuals with mental illness lack the personal fortitude required to be successful physicians. To overcome this, we need to actively confront and challenge this stigma. By doing so, we can create an environment where those struggling with these issues feel comfortable seeking the care and support they need. It's crucial that we stand by both ourselves and our colleagues, as we are only able to provide the best care to our patients when we are at our best.
What can be done to create a sense of safety for EM physicians and medical trainees that would encourage them to ask for help or self-report when they’re struggling with their mental health.
As above, we must continue to challenge the stigma and change the culture regarding mental health care for medical providers. Part of this will require leaders to be more transparent regarding their own mental health struggles and seeking help. This can help trainees who are also dealing with these challenges see that seeking assistance doesn't equate to failure. Furthermore, we must continue to ensure that resources for mental health are readily available and easy to access. Additionally, we must continuously check in on our colleagues and provide a safe space and open environment where they can freely talk about their emotions and thoughts.
What do you think the EM specialty and/or SAEM can do to address stress and improve physician well-being?
To destigmatize mental health care, it’s important to keep reaching out and talking about mental health concerns. Culture change takes time, it doesn't happen overnight. As new generations of providers emerge, hopefully they'll be
more comfortable conveying their concerns and seeking care when they need it.
I would like to see SAEM commit to addressing the current back-up systems for trainees. Right now, the systems in place can make trainees feel punished if they need time off. This makes people sometimes not take the time they need for their health and wellness because they don't want to burden their colleagues. Instead, we should make systems where it's expected that people will need sick days — which is true for everyone — and it's seen as okay, not a negative thing.
Any tips on surviving, perhaps even thriving, during residency? Similarly, how have you managed stress and attended to your mental health, especially during these unprecedented times?
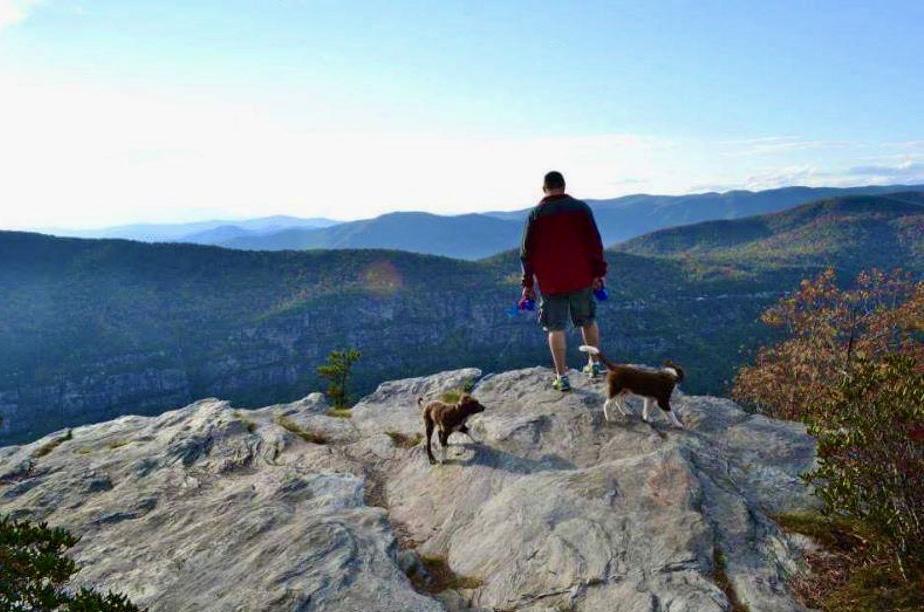
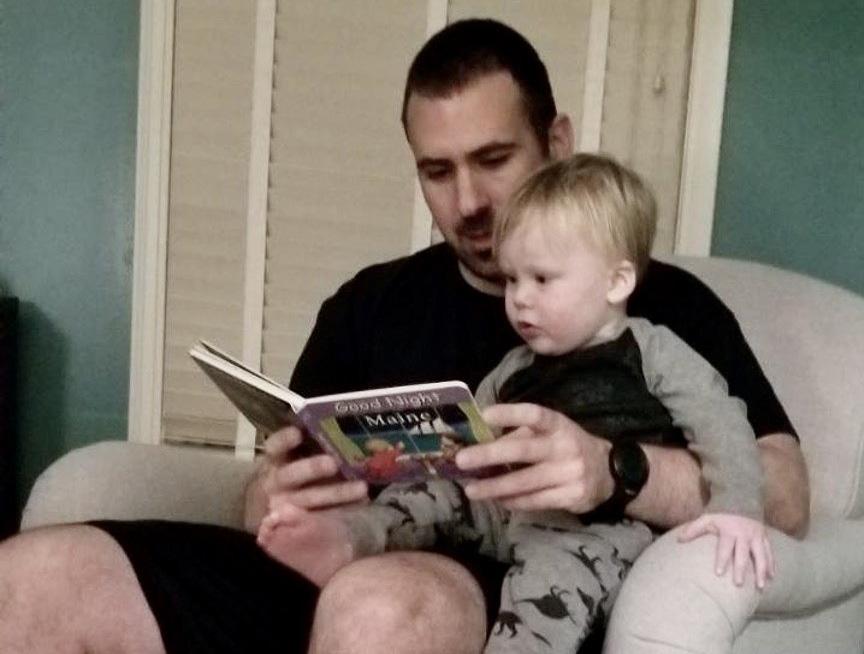
In the military, it is often preached that it is the quality not the quantity of time spent outside of work that improves one’s well-being. One must actively ensure that time away from work is filled with activities one enjoys. We can continue to advocate for less working hours, but at the end of day, physician training is a huge time commitment. We all must ensure we use our time away “filling our cups” by doing what brings us joy, be that spending time outside or with loved ones.

What advice would you give to an individual who is struggling to manage stress and a maintain work/life balance?
First and foremost, assess how you spend your free time. You may not have much control over your work schedule, but you can control how you spend your time away from work. Don’t feel pressured to fill your every waking moment bolstering your CV by completing research or serving on committees. Often these projects are unfulfilling and uninteresting. Step back and ask yourself which tasks during the day you need to accomplish and then focus only on those. As time allows, add extracurriculars that you find interesting. This will be less draining and overall more impactful than ensuring you check all the boxes on your CV. Physician training is a marathon, not a sprint.
When you spend time on boats, it means you spend time working on boats. Dr. Jourdan on “The Rooster” exchanging a fuel pump in the middle of the Chesapeake Bay.What one thing can you not do without while on shift?
Coffee. Not a shift goes by without coffee. When I’m short on time or unable to procure a quality cup, I will sometimes even resort to the rancid breakroom coffee in the emergency department.
What is your “go to” work/on-shift hack?
Just go see the patient. Early in my career I spent way too much time reviewing the chart (including notes and prior labs) when if I had just talked to the patient first I would have narrowed down what I needed to review and spent much less time overall.
What is a favorite FOAMed resource?
Wikem.org for sure. When you are in a pinch it’s the best resource for concise differential, evaluation, and treatment plan for any condition.
What would most people be surprised to learn about you?
I enjoy floor medicine! Yes, I said it. The challenge of pinpointing a diagnosis, developing, implementing, and adjusting a treatment plan, and ensuring patient buy-in and adherence is a marked difference from the challenge of stabilization, triage, and emergency treatment in the emergency department.
Who would play you in the film of your life and what would that film be called?
Oh wow. That would be terribly boring. John Krazinski with a beard maybe? “Doctor Dan.” Geez. Not even my mom would want to watch that!
What is your guilty pleasure?
Rewatching movies, especially terrible action movies. My favorite is Armageddon. A simple plot, good action, and the good guys win.
What is at the top of your bucket list?

Visiting all the National Parks. At last count, I am about three-fifths of the way through the list of current parks; however, the remaining parks are some of the more austere and difficult to access, including Alaska’s impressive eight national parks.
Who would you invite to your dream dinner party?
I am a history buff. I even minored in history as an undergrad. I would love to sit down with some of my favorite historians, including Doris Kearns Goodwin, Anne Applebaum and Jon Meachem and discuss contemporary history. I find politicians who shape history are too focused on furthering a narrative, but historians provide insight into the fallacies of their thought and the events that enable them.
“Please provide a cover letter in addition to your CV when applying.”
This sentence strikes fear in many job applicants. In fact, merely asking for a cover letter is enough to dissuade a substantial number of job seekers.
Barbara Katz, an experienced physician recruiter, estimates that only 10% of the CVs she receives are accompanied by a supplementary cover letter. The cover letter, at first glance, might seem like an extraneous task or a vestige of the corporate past. Nonetheless, it remains an important tool for all physicians pursuing job opportunities in emergency medicine.
A cover letter is an opportunity to express oneself and convey personal strengths and goals. As Will Rogers
famously said, “You never get a second chance at a first impression.” The cover letter is that initial impression when applying for employment, so it is important that it conveys one’s intended message. The letter provides a pre-interview opportunity to explain any gaps in one’s CV and highlight key experiences that might otherwise be overlooked. In a fiercely competitive job market, a well-crafted cover letter may stand out among other applicants and might be the reason an application gets a thorough review.
Drafting a cover letter can evoke anxiety. Using an outline to structure the cover letter and avoiding a few key pitfalls can streamline the writing process and amplify the application’s impact.
1. Salutation/Greeting
Determine to whom the letter should be addressed. The default is usually the department chair; however, liaising with administrative staff to discern the responsible individual for the hiring process is advisable. Avoid using the phrase “To Whom It May Concern.”

2. Introduction
The introduction comprises two essential elements: 1) one’s qualifications and 2) the sought-after job that is being applied for. Highlight one or two key experiences that relate to the required qualifications of the position. This could include residency, fellowship training, or years of accumulated
experience. It is imperative to specify the position being applied for or the desired job category.
This is the motivation behind one's interest in the job or institution and should be expounded upon. Researching and addressing what sets the institution apart can contribute to addressing this aspect. This is also an opportunity to underscore any geographic connections or institutional affiliations.
This is the rationale that outlines why one is suitable for the job. Moderate self-promotion and modest bragging about one’s accomplishments are okay. If relevant, work or residency experience within a department analogous to the one being applied for can be cited.
5.
The cover letter's conclusion is an opportune moment for boldness. Offer to follow up in-person or online. Leave a strong final impression that conveys the reasons one is the right choice for the position.

• Reiterating the contents of the CV. The letter should complement your CV but also be able to stand alone.
• Formulating a generic letter. Write a distinct, tailored letter for each job prospect. It pays to do one’s homework. Tailoring the letter increases the chances of landing an interview.
• Poor grammar and spelling. The application review and hiring process is challenging, and a letter marred by spelling and grammar errors signals indifference about the job.
• Don’t be long-winded. The cover letter should not exceed one page; in fact, just a few paragraphs is okay.
A well-composed cover letter can serve as the hook needed to secure one’s dream job. Using the above-outlined tips and techniques can reduce the anxiety of starting the writing process. When composing a cover letter, remember that it represents one's first impression with the prospective organization, so make sure it’s a good one!
Dr. Kilpatrick serves as the Clinical Skills Course Director, EM Clerkship Director, and Student Advisor for Western Michigan University Homer Stryker School of Medicine. He is a recent graduate of Thomas Jefferson University Hospital’s Medical Education Fellowship program. @je_kilpatrick

Dr. Raps is an Assistant Residency Program Director at the University of Utah. After graduation from the University of Utah in 2019, she spent two years as a core faculty member and Co-director of Emergency Ultrasound at St. Joseph’s Medical Center in Stockton, Calif.

“In a fiercely competitive job market, a wellcrafted cover letter may stand out among other applicants and might be the reason an application gets a thorough review.”
 By Sharon Bord, MD and Bradley S. Hernandez, MD on behalf of the SAEM Clerkship Directors in Emergency Medicine Academy
By Sharon Bord, MD and Bradley S. Hernandez, MD on behalf of the SAEM Clerkship Directors in Emergency Medicine Academy
A gust of transformation is sweeping through the 2022-2023 emergency medicine residency applications cycle, reshaping a process that had long remained relatively unchanged. In the last ten years, the tradition among EM-bound medical students involved completing their applications through ERAS (Electronic Residency Application Service), carefully refining their personal statements, and anguishing over which programs to choose. Except for a short-lived (2 year), unsuccessful operational pilot of the AAMC standardized video interview for professionalism assessment, the process had remained remarkably unaltered since the inception of the standard letter of evaluation (SLOE). Yet, this year marks a substantial departure,
encompassing adjustments to the ERAS application format, the USMLE Step 1 scoring system, and interview protocol recommendations.
The most significant change in this year’s application cycle is the AAMC's myERAS application. The traditional format of listing the entirety of the applicant’s work and research experience has been eliminated. Students now are asked to list their 10 most impactful experiences and highlight three which were most meaningful to them and why. Hobbies and interests have been integrated with these experiences. An additional opportunity has been introduced for applicants to recount any adversities they navigated which subsequently influenced their journey to a residency.
Listing geographic and clinical preferences are now also part of the application process. The United States has been partitioned into nine geographical regions and students may select three regions that most entice them, accompanied by explanations for their choices. Alternatively, an option for no geographic preference is also available and underscores the applicant’s willingness to train anywhere across the country.
Last year emergency medicine followed the lead of a few other specialties by adopting a practice called "program signaling." Applicants were given five tokens to “signal” their interest in particular programs. This year, the number of signaling tokens has risen to seven. Differing from last
year's advice that applicants refrain from signaling programs where they completed EM clerkships, this year's counsel encourages applicants to signal such programs and then allocate the remaining tokens at other EM residency programs.
As of January 2023, USMLE Step 1 has transitioned to a pass/fail system. In the previous application cycle, there was a mix of students who received either a pass/fail result or a numerical score for Step 1. In the current cycle, all traditional allopathic medical students will receive a pass/fail outcome for USMLE Step 1. Consequently, EM residency programs will now only have access to numerical scores from USMLE Step 2, the timing of which depends on when applicants take the exam and release their scores. Although most applicants will likely have their Step 2 scores by the match, there's a possibility that many won't have them available when applications open on September 29, 2023. This change means that residency programs may no longer be able to rely on USMLE filters as an initial screening tool for ERAS applications.
Beginning last year, the SLOE, considered by program directors as a valuable component of a student’s file, underwent a restructuring. Evaluation categories were aligned with Core Entrustable Professional Activities (EPA) standards and residency readiness. The conventional tripartite student division for global assessment was overhauled, acknowledging that a standard degree of guidance is typical during residency. The new letters more accurately reflect student performance and predictions of success in residency.
The final change for the 2023-24 application cycle is from the Coalition of Physician Accountability (COPA), an ACGME member that provides guidance on the structure and format of residency interviews. Since 2020, virtual interviews have been the recommended format. This year, the official stance endorses EM programs to primarily adopt virtual



interviews, reserving in-person visits for later in the interview season. Yet, they concede that “the decision on interview format is an individual one that may be determined by program and institutional factors,” allowing room for programs to pursue the format they feel best supports their individual circumstances. Recognizing that this statement opens the door for in-person interviews, they strongly recommend a virtual interview option and that interview opportunities are equitable and unbiased for all applicants, with no penalty based on the format of interview chosen.
Amidst these winds of change, the hope is that these measures will guide students toward a successful match by providing a fair and equitable application procedure for all applicants. These changes should also help programs perform a more holistic application review. In the ongoing navigation of the everchanging EM application climate, these exciting transformations hold the promise of positive change in the application process, creating the potential for clear skies on the horizon.
Dr. Bord is an assistant professor in the department of emergency medicine at the Johns Hopkins University School of Medicine. She has a focus on both undergraduate and graduate medical education and is the director for the required medical student clerkship and subinternship in emergency medicine. She also directs the capstone course, TRIPLE, for graduating fourth year medical students teaching critical skills to aid with the transition to internship and beyond.
Dr. Hernandez is a senior staff physician at Regions Hospital in St. Paul, Minnesota and is an assistant professor in the department of emergency medicine at the University of Minnesota Medical School. He attended medical school at the University of Iowa College of Medicine and residency training at Regions Hospital. He is an assistant residency director, clerkship director and gameday physician for the Minnesota Vikings.
Clerkship Directors in Emergency Medicine (CDEM) represents the interests of undergraduate medical educators in emergency medicine. It serves as a unified voice for EM clerkship directors and medical student educators and provides a forum for them to communicate, share ideas, and generate solutions to common problems. For more information, visit the CDEM webpage Membership in SAEM's academies and interest groups is free. To participate in one more groups: 1.) log into SAEM.org; 2.) click “My Participation” in the upper navigation bar; and 3) click “Update (+/-) Academies or Interest Groups.”
 By Gregory P Wu, MD; Alexander Bracey, MD; Cameron Waldman, MD; Megan Lieb, DO; Sean Geary, MD; and Luke Duncan, MD on behalf of the SAEM Critical Care Interest Group
By Gregory P Wu, MD; Alexander Bracey, MD; Cameron Waldman, MD; Megan Lieb, DO; Sean Geary, MD; and Luke Duncan, MD on behalf of the SAEM Critical Care Interest Group
Resuscitation and emergency critical care (RECC) (commonly referred to as “resuscitation” or just “resus”) is one of the fastest growing fellowships in emergency medicine (EM). RECC fellowships give EM graduates the skills to care for critically ill patients in emergency departments (EDs), from the hyperacute initial minutes of arrival through their disposition or at any point throughout prolonged ED visits, which are commonplace currently due to the growing boarding crisis. Albany Medical Center (AMC) graduated its first RECC class July 2023.
The AMC RECC fellowship is based in the Department of EM. The AMC ED serves about 3 million people in western New England and upstate New York. The Emergency Critical Care division is composed of 7 physicians, with a mixture of training in surgical critical care, critical care medicine, and resuscitation graduates. The EM Critical Care division has operated an ED Critical Care Consult (EDC3) service since 2020, which provides consultation and management support to primary ED teams caring for critically ill adults and children during the busiest hours. This article highlights lessons learned from program leadership, with perspectives from first-year fellows.
Lesson 1: Resuscitation exists on a spectrum of critical care.
Unlike other areas of the hospital, patients presenting to the ED are often poorly differentiated with nebulous disease features or even mixed diseases that defy easy siloing. As such, we decided early that the RECC fellows would be trained by a diverse team. This approach requires multiple teachers, settings, and perspectives. To this end, we purposefully built in clinical experiences beyond the EDC3, including the medical, surgical, neuroscience, and cardiac surgery intensive care units. We were fortunate to have program leadership made up
of a resuscitation trained emergency physician as well as an EM medical intensivist and an EM surgical intensivist. We found that this was highly beneficial to our fellows’ experience because they were able to learn from a wide array of training and incorporate the strongest elements of each approach into their practice. In sum, we found they were able to parlay these broad experiences to create an approach to critical care well-suited to the ED.
Time spent on the EDC3 service was the primary focus during design of the RECC fellowship. Fellows spent over 800 hours resuscitating and overseeing the ongoing care of critically ill patients in our ED. We felt strongly that a high-volume of patient encounters with the sickest patients in the ED was integral to further refinement and mastery over the often complex and high-stakes care of this group.
However, we also felt it was important to spend time developing theory. The fellows had a weekly twohour conference with a schedule designed to cover critical care topics (Figure 1). These were built on core physiologic principles, such as hemodynamics and respiratory mechanics. These were then applied to clinical presentations and management to solidify both theory and practice. Critical care often requires caring for patients where there are no evidence-based practice or guidelines, therefore physiology becomes the guiding principle. We found that fellows were able to apply advanced physiologic principles to the patients in the ED and adjust management.

In the original design of the didactic schedule, we had left time open for lecture topics to be determined by fellow interests. Our fellows indicated that they were frequently encountering pediatric resuscitations of medically complex children, in which our group lacked expertise. To rectify this, we invited pediatric intensivists to our didactic sessions who offered their expertise, perspective, and
continued on Page 16
“Critical care often requires caring for patients where there are no evidencebased practice or guidelines, therefore physiology becomes the guiding principle.”Figure 1
CRITICAL CARE
continued from Page 15
clinical teaching. The RECC fellows proved to be instrumental in managing critically ill children during the surge in pediatric ED visits seen in the winter of 2022-2023.

Our fellows also showed interest in extubating low-risk patients in our ED. We created a quality improvement project for the fellows to work on guidelines on how to safely liberate ED patients from the ventilator. One of our fellows expressed significant interest in the function of a Critical Care Receiving Unit (CCRU), a concept pioneered by the R Adams Cowley Shock Trauma Center. We arranged for the fellow to spend an elective month in the CCRU, learning about the similarities and differences in practice setting.
Tantamount to the diversity of thought within program leadership is strong support from departmental leadership. We benefit from a department chair who shares the goal of high-quality critical care for our region and recognized the value of having fellows within the department solely dedicated to management of the sickest patients through their ED course. This also
benefits the patients being managed by the general EM faculty, as it allows the mental offloading of highest-acuity patients. Moreover, in contrast to the RECC programs at Stony Brook University and Hartford Hospital, our ED does not assign patients location based on acuity. Therefore, our model had to ensure that the RECC fellows were able to go to the highest-acuity patients.
There was initially concern among EM residency leadership that this might interfere with resident education;
“Tantamount to the diversity of thought within program leadership is strong support from departmental leadership.”
however, the presence of RECC fellows did not take away from the EM residents from either medical theory or practical experiences. Contrariwise, fellows heightened the discussion surrounding the nuances of management of highacuity patients, provided closer real-time supervision and feedback during critical procedures, and often led EM residency didactics. The result was a robust experience for all learners and a safer patient environment that would not have been possible without strong buy-in and foresight from all levels of ED leadership. Lesson
As we graduate our first class of resuscitationists, we welcome our newest fellow who is already board-certified in emergency medical services (EMS).
EMS lends itself well to RECC, given the highly diverse and undifferentiated patient population. The physiology approach of RECC synergizes with EMS, given the unpredictable and often austere environments and ever-expanding volume of interfacility transports. We plan to further develop pathways that combine EMS and RECC for those who are interested in this new type of hybrid practice.
RECC also synergizes well with ultrasound. Critical care and EM have both readily adopted point of care ultrasound as a diagnostic tool during acute resuscitation. Echocardiography particularly has implications for managing shock. Ultrasound and RECC have the shared goals of care of undifferentiated patients, and future endeavors to combine RECC with ultrasound focused practice designation are expected to be readily achievable. Our program requires RECC fellows to take the Critical Care Echocardiography Exam, which both successfully passed, offering further proof of the synergy of these two related disciplines.
Training in RECC meant a deep dive into critical care management and principles, but also learning the opposite: skills of de-escalating care. Good critical care management also means weaning therapies and downgrading when appropriate. As fellows, much of our focus this year has been in this realm of de-escalation and using these lessons to help improve patient care in our department. We created blueprints for extubation protocols, identified criteria for de-escalation after intravascular thrombectomy for massive pulmonary emboli, and received additional training on palliative care in emergency medicine.

The history of critical care and EM is one of parallel maturation through the mid-20th Century. Both specialties have similar goals of caring for patients based on where they need help, and not limited to one organ system, demographic, or type of disease. RECC marries these two histories into a new discipline, one that will continue to grow for the decades to come. We hope by sharing the lessons learned in the development of a young program, we can further foster growth of new RECC programs coming into existence.
Dr. Wu, an assistant professor of emergency medicine and internal medicine at Albany Medical College, is a medical intensivist and emergency physician. He serves as the clerkship director for critical care and associate director for Resuscitation and Emergency Critical Care Fellowship.
Dr. Bracey, an emergency physician at Albany Medical College, directs the resuscitation and emergency critical care program and assists with the EM residency. His interests encompass managing critically ill ED patients, advanced ECG interpretation, airway management, and advanced vascular access techniques.
Dr. Waldman, an emergency physician and resuscitationist at Albany Medical Center, completed her emergency medicine residency in 2022 and subsequently the Resuscitation and Emergency Critical Care Fellowship in 2023.

Dr. Lieb, an emergency physician and resuscitationist within the Albany Med Health System, concluded her emergency medicine residency in 2022 and the Resuscitation and Emergency Critical Care Fellowship in 2023.
Dr. Geary, an associate professor of emergency medicine and surgical critical care at Albany Medical College, holds certifications in emergency medicine, surgical critical care, and neurocritical care. As a practicing emergency physician and program director of the emergency medicine residency, Sean's interests encompass medical education, extracorporeal membrane oxygenation, trauma, and traumatic brain injury management.
Dr. Duncan, dual-boarded in EM/surgical critical care, completed his fellowship at Albany Medical Center. Serving as chief of the division of emergency critical care and assistant director for the Resuscitation and Emergency Critical Care Fellowship, he plays a pivotal role in the program's leadership.




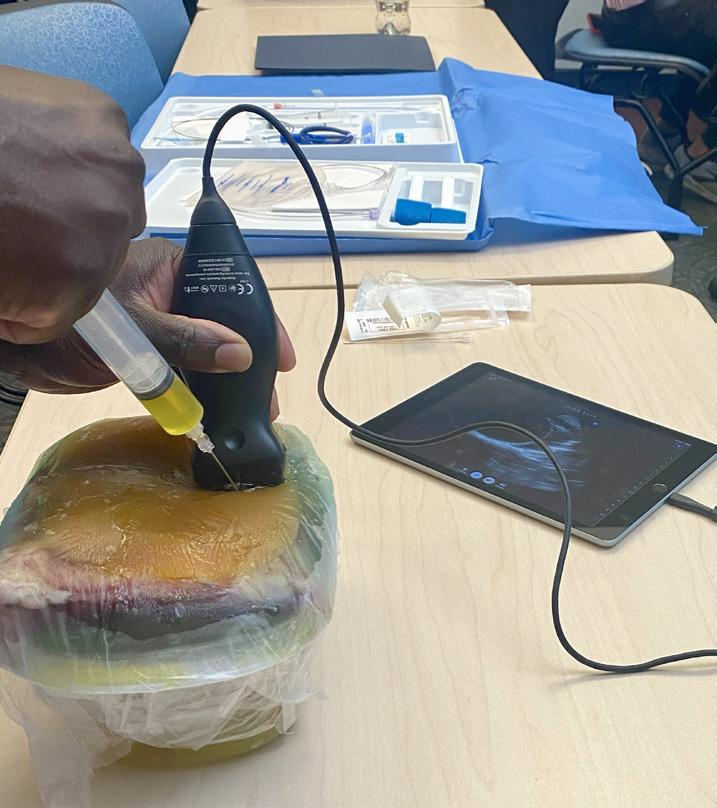
Pericardiocentesis is one of the high-acuity, low-opportunity (HALO) procedures encountered in emergency medicine. Due to its infrequent occurrence, resident physicians may lack the necessary hands-on experience to confidently perform this life-saving intervention when necessary.
Although pericardiocentesis is considered a key index procedure mandated by the Accreditation Council for Graduate Medical Education (ACGME), it is a rare procedure that
many emergency medicine residency programs practice solely in simulated sessions. To enhance our simulated scenarios, our team was able to create low-cost, reusable simulation models specifically for pericardiocentesis training.
To address the need for hands-on training, we utilized online sources to develop low-cost, reusable simulation models. Drawing inspiration from readily available demonstrations, we successfully constructed three models
for pericardiocentesis. The materials needed were Tupperware containers, Ziploc bags, water-filled balloons, red and yellow food coloring, ultrasound gel, beef or pork ribs, press and seal-type wrap, and, in some models, a gelatin

“The cost-effectiveness and resource for various training
mixture. Using the containers as the base for the model, we filled Ziploc bags with water mixed with yellow food coloring. A water-filled balloon with red food coloring was placed inside the Ziploc bag, which was then filled with enough water to completely cover the balloon. Air was removed from the bag and placed into the container. Ultrasound gel filled in gaps between the container, the Ziploc bag, and the ribs, with the press and seal-type wrap covering the top.
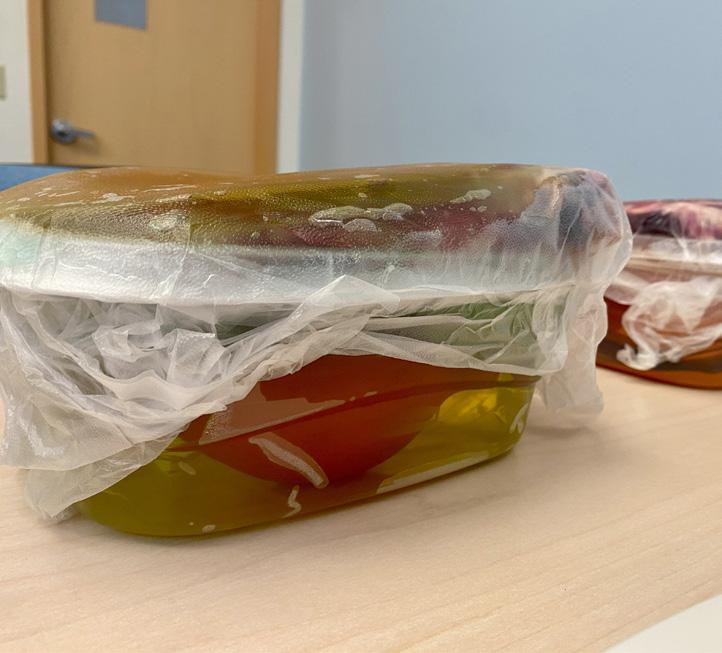
Our simulation models incorporated two ultrasound-guided approaches (apical and parasternal techniques) and an additional model for a blind subxiphoid approach. The ultrasound-guided models allowed residents to familiarize themselves with the relevant anatomy and practice positioning required to perform a successful pericardiocentesis. The blind subxiphoid model provided an opportunity to refine tactile skills and improve procedural dexterity. To further enhance the realism of the model, we introduced a gelatin mixture to simulate soft tissue. This gelatin-based skin layer closely resembled the density of human tissue, offering a more realistic training experience. If an ultrasound is not readily available it is also possible to make multiple gelatin layers to further replicate varying body habitus and add to the challenge of identifying landmarks. By incorporating this element, residents gained a better understanding of the tactile sensations they would encounter during the actual procedure, thereby bridging the gap between simulation and real-world scenarios.
To supplement our hands-on demonstration and create a more comprehensive understanding of the pericardiocentesis procedure,
our team created a presentation, reviewing essential knowledge regarding indications, contraindications, and various approaches to the procedure. This multifaceted approach was crucial to ensuring a well-rounded understanding of the procedure, combining basic knowledge with practical application.
The cost-effectiveness and reusability of these models ensure an accessible resource for various training programs. By reducing financial barriers, more institutions can implement this simulationbased training, allowing all residents to experience this essential handson simulation and gain confidence and proficiency in performing pericardiocentesis.
It is crucial for emergency medicine residency programs to recognize the value of incorporating simulation-based training into their curricula. By embracing these educational techniques, residents are prepared to handle rare, high-acuity procedures.

Dr. Nidal Choujaa is an emergency medicine resident (PGY-3) at Aultman Hospital in Canton, Ohio.

Dr. Alison Southern is the program director for Aultman Emergency Medicine, Canton, Ohio, and an associate professor of emergency medicine at Northeast Ohio Medical University.

and reusability of these models ensure an accessible training programs.”
“Our simulation models incorporated two ultrasound-guided approaches (apical and parasternal techniques) and an additional model for a blind subxiphoid approach.”
A 47-year-old man has arrived at your emergency department in New York City via emergency medical services (EMS). He is exhibiting facial bleeding. He has arrived from the location of a low-speed car accident during which he collided with the car in front of him at a speed of approximately 5 mph. EMS has indicated that there is no observable damage to his vehicle, and the patient himself has conveyed that there is minimal to no apparent damage to the other involved vehicle. However, subsequent to the collision, the driver of the vehicle that was rear-ended proceeded to exit his car, approach the patient, and deliver repeated punches to the patient's face and neck. Following
the assault, the assailant then returned to his vehicle and left the scene. EMS asks the patient if he wishes to file a police report, but he adamantly declines.
The patient is not in acute distress but is visibly shaken by the incident. On examination, the patient displays swelling on the left side of his face, including the eyelid, which is beginning to swell shut. A 2x3 cm abrasion is noted on his left cheek; it is not actively bleeding. He reports pain on the left side of his neck and shoulder, where he was assaulted. Pain control is administered, his Tdap vaccine is updated, and a CT scan is ordered to rule out additional injuries.

During the wait for the CT scan, the next patient, a 26-year-old male,
presents himself. He arrives from the front triage, complaining of "whiplash" following a car accident. He recounts being rear-ended at a traffic light and acknowledges assaulting the driver responsible and that he “made sure that guy won’t do it again.” It becomes evident that this patient is the perpetrator in the earlier assault. He appears visibly intoxicated and complains of diffuse neck pain, including midline neck discomfort. Otherwise, his physical examination is unremarkable. He asserts that he believes his neck is broken due to the accident. Considering his intoxication and midline neck pain, pain medication and a CT scan are prescribed.
Upon returning to the initial patient, the CT scan indicates a questionable left-sided retrobulbar hematoma
and a left zygoma fracture. Apart from the swelling of his left eye, preventing self-opening, the patient remains clinically unchanged. Ophthalmology is consulted, recommending observation and monitoring of intra-ocular pressures. His wife, present during the assault, has now joined him. After communicating the results, they both express anxiety and distress. The wife confides that her husband is undocumented and, given this, they are uncertain about the next steps they should take. Financial concerns and fear of deportation loom as they contemplate reporting the incident to the police. Seeking guidance, they ask your opinion as to what they should do.
What is your obligation with regard to reporting the assailant? He admits to the assault but denies any ongoing intent to harm others or himself. He is not an immediate danger to anyone and displays signs of intoxication but exhibits no signs of a mental health emergency. No threats are made. The assaulted individual is neither a minor nor elderly. Legal obligation to file a police report does not apply in this case, and out of respect for patient confidentiality, the physician's duty is to the patient's privacy, provided there is no risk to anyone's safety.
Principle IV of the American Medical Association's Code of Medical Ethics directs that "a physician shall respect the rights of patients, colleagues, and other health professionals, and shall safeguard patient confidences and privacy within the constraints of the law." Patient privacy is upheld unless legal requirements, patient consent, or ongoing threats are involved. Ethically, since the assailant poses no lasting threat, privacy is paramount.
The "within the constraints of the law" clause permits disclosure as mandated by law, with exceptions for patient consent or threats. There are legal guidelines in most states requiring the report of injuries due to firearms, knives, and other weapons, assaults that are considered life threatening, as well as child abuse or ongoing threats to society. Most states do not have reporting laws for simple assaults, however. Although the assailant confessed to a crime, his ongoing threat is absent, warranting privacy protection. There is no ethical or legal basis to report him to law enforcement.
Turning to the assault victim, it is vital to address concerns about ED visit costs
and protections if a police report is filed. For financial concerns, undocumented patients lack public insurance entitlement but can receive emergency medical assistance. This program assists uninsured individuals facing health risks and having conditions that can jeopardize health or bodily function. This is often the only way for undocumented patients to get health care coverage if they do not buy their own private health insurance. Social work involvement is feasible if available.
Regarding reporting incidents while undocumented, sanctuary states offer protection and undocumented patients are free to report to the police without fear of immigration repercussions. In nonsanctuary regions, sharing databases with immigration enforcement is possible, risking deportation for reporting a crime. Variations exist based on location. The emergency physician must understand local laws for undocumented patients' guidance. New York City, where this case occurred, is a sanctuary city.
Ultimately, after discussing New York City's sanctuary status, the assault victim and his wife decide to report to the police. During the police report filing, the wife goes to the bathroom and subsequently identifies the assailant as another patient in the emergency department. Law enforcement identifies the assailant and documents the report for future follow-up. The outcome remains unknown.
Dr. Molyneux is an attending physician and fellow in Global Emergency Medicine at Columbia University. He focuses on health at the U.S.-Mexico border, working in health promotion in Ciudad Juárez in addition to being an asylum clinician in New York City.


“For financial concerns, undocumented patients lack public insurance entitlement but can receive emergency medical assistance during emergencies.”
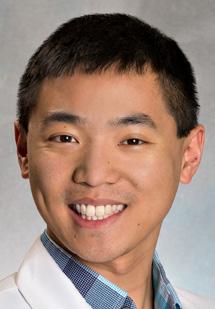
 By Nancy Kwon, MD, MPA; Tabia Santos, MD; and Yves Duroseau, MD on behalf of the SAEM Faculty Development Committee, SAEM Equity and Inclusion Committee, and SAEM Research Committee
By Nancy Kwon, MD, MPA; Tabia Santos, MD; and Yves Duroseau, MD on behalf of the SAEM Faculty Development Committee, SAEM Equity and Inclusion Committee, and SAEM Research Committee
Sickle Cell Disease (SCD) is a vaso-occlusive hemoglobinopathy that distorts the shape of hemoglobin causing ischemia with severe, life-threatening consequences. According to data from The Centers for Disease Control (CDC), SCD affects approximately 100,000 Americans and is predominantly observed in underrepresented populations. SCD occurs in approximately 1 out of every 365 Black or African American births, and in 1 out of every 16,300 Hispanic-American
births. The life expectancy of adults with SCD is decades shorter than that of the general population due to the ischemic nature of the disease and its debilitating long-term complications. While some improvements in the management of SCD pain have been made with the addition of hydroxyurea and other more recent therapies to treatment protocols, patients often require emergency care for pain crises and other complications. SCD is the genetic condition most detected in newborn screenings, yet it remains one of the most neglected in terms of advancements, interventions, and research. This disparity can be attributed in part to significant underfunding of SCD research. For
example, funding from the National Institutes of Health (NIH) and private foundations for cystic fibrosis (CF), which affects one-third as many people as SCD, was 3.5 times and 440 times higher, respectively, than funding for SCD
Dr. Jeffrey Glassberg is a physician who is actively addressing the disparities in SCD. He holds positions as a professor of emergency medicine and a professor in hematology and medical oncology. He also serves as the director of the Mount Sinai Comprehensive Sickle Cell Program at the Icahn School of Medicine at Mount Sinai. His passion for research and addressing care gaps for SCD began
prior to his medical career. While pursuing a doctorate in medicine and a master’s degree in clinical research at Washington University in St. Louis’ School of Medicine, he found an early mentor in research, Dr. Michael R. DeBaun. Dr. DeBaun, a renowned pediatrician, is nationally and internationally recognized for his clinical and translational research focusing on the etiology and management of cerebrovascular injury in children with SCD. Dr. DeBaun was part of team of collaborators that received funding for the first National Institutes of Health (NIH)-sponsored international clinical trial in sickle cell disease known as the Silent Cerebral Infarct Multi-Center Trial. Dr. Glassberg's experience with Dr. DeBaun and other advocates for SCD patients ignited his own drive to pioneer translational and clinical research and improve clinical care to impact health equity and outcomes for those afflicted by the disease. He has since become a researcher, health care advocate,
mentor, and educator. Dr. Glassberg's collaboration with Dr. DeBaun has continued, including additional studies stemming from the Silent Cerebral Infarct Transfusion trial
Dr. Glassberg pursued his emergency medicine residency in 2006 at New York University Hospital/Bellevue Hospital Center, completing it in 2010. He began his career as an emergency medicine faculty member and researcher at Mount Sinai Hospital and the Icahn School of Medicine at Mount Sinai. Throughout his residency, he gained direct clinical exposure to SCD patients, mainly at Bellevue Hospital, which served as a safety net for individuals with SCD complications. Emergency care was often the only option for many patients at the time, given limited outpatient management and access to care. Dr. Lewis Goldfrank, the chair of the department during Dr. Glassberg's residency, became another mentor,
engaging in discussions about challenges faced by SCD patients and supporting Dr. Glassberg's path to expertise in SCD.
In 2010, Dr. Glassberg affiliated with Mount Sinai Hospital once again, this time to undertake a research fellowship focused on SCD. He remained as faculty to establish a distinctive approach to address the disease through both clinical practice and research. Dr. Paul Frenette, a leader in SCD research and a mentor, was a faculty member during that period. Dr. Frenette's recruitment to the Albert Einstein College of Medicine in 2010 led to his role as the founding director and chair of the Ruth L. and David S. Gottesman Institute for Stem Cell Biology and Regenerative Medicine Research. While Dr. Glassberg was able to maintain remote mentorships with Drs. DeBaun and Frenette, initiating research and
continued on Page 25

“SCD is the genetic condition most detected in newborn screenings, yet it remains one of the most neglected in terms of advancements, interventions, and research.”

continued from Page 23
navigating his career as a young scientist in a new institution presented challenges. However, Dr. Glassberg’s unwavering determination led him to forge his own unique path, even though he acknowledges that at times, the process was arduous.
Early on, he recognized the necessity of securing substantial grant funding to establish the research foundation for SCD. He continued collaborating with his previous mentors and sought new guidance from Dr. Lynne Richardson at Mount Sinai, a seasoned researcher and faculty member.

In 2013, Dr. Glassberg secured an NIH K23 grant titled “Inhaled Mometasone to Promote Reduction in Vaso-occlusive Events," known as the “IMPROVE” trial. One of the primary risk factors for vaso-occlusion and death in adolescents and adults with SCD is the presence of respiratory symptoms like cough or wheeze. Dr. Glassberg's K23 grant was built on preliminary data suggesting that respiratory symptoms, such as recurrent cough or wheeze—present in half of individuals with SCD who lack a physician's asthma diagnosis—constitute a risk factor for vaso-occlusion and death. His research tested the hypothesis that inhaled corticosteroids would prevent painful vaso-occlusive episodes in SCD adults with wheezing, but who did not meet the criteria for an asthma diagnosis. Dr. Glassberg's initial findings demonstrated promising outcomes, revealing a reduction in pain scores and SCD biomarkers with the use of inhaled steroids.
Dr. Glassberg's K23 award and his innovative approach were just the beginning of a fast trajectory toward receiving numerous research awards from NIH, foundations, and industry for SCD. His K23 award paved the way for NIH R01 funding to continue his research in SCD and vaso-occlusive complications with the “IMPROVE 2” trial and the “SCD REVIVE” trial. In the latter, or “Retina to Evaluate Vaso-occlusion in the Vasculature of the Eye,” Dr. Glassberg and his research team are investigating advanced retinal imaging to predict the severity of SCD disease.
Dr. Glassberg is renowned for his innovative research approach and

stands as a pioneer in constructing the foundational infrastructure to address the immediate needs of patients grappling with SCD. Leveraging his determination, grant funding, and the cultivation of trust among colleagues and patients, he successfully crafted both outpatient and inpatient frameworks alongside a team of clinicians and researchers. Through these efforts, he has provided comprehensive care for individuals affected by SCD. Recently, he instituted a fellowship program specializing in SCD. Open to emergency medicine physicians, the fellowship aims to shape the next generation of clinical and research experts. His leadership extends to the advancement of evidence-based strategies for SCD. His engagement spans both regional and national realms, evident in his participation as a member of the Queens Sickle Cell Advocacy Network, the New York Sickle Cell Advisory Council, and the Sickle Cell Disease Association of America
Dr. Duroseau is the chair of emergency medicine at Lenox Hill Hospital and the vice president for Northwell Health’s Emergency Medicine Service Line for the Western Region. He also serves as the president of the medical board for Lenox Hill Hospital and is an assistant clinical professor of emergency medicine at the Zucker School of Medicine at Hofstra/Northwell.
Dr. Santos is a PGY-3 resident physician at Northwell Northshore-LIJ in NYC, NY and one of the leaders of the Diversity, Equity, and Inclusion Resident Subgroup Committee. A New York native, Dr. Santos completed her undergraduate career at Barnard and her doctorate at the Hofstra-Northwell Zucker School of Medicine.

Dr. Kwon is the vice chair of emergency medicine at Long Island Jewish Medical Center, which is part of Northwell Health. She has been an active member of SAEM as part of the Faculty Development, Research, and Equity and Inclusion committees and is presently a member of the SAEM Nominating Committee.

A hectic and unfamiliar environment, the uncertainty surrounding one’s health, the windowless confines of patient's room that can extend for hours, the constant flow of physicians, nurses, and staff... Countless sources of stress confront all patients in the emergency department (ED). For older adults in particular, these ED conditions and accompanying feelings of discomfort can often exacerbate comorbidities and symptoms including visual and auditory impairments, cognitive decline due to delirium and dementia, and compromised communication.
Geriatric patients account for 45% of ED visits, underscoring the imperative

on behalf of the SAEM Academy of
to address the unique needs of this population to enhance emergency care. Improving the comfort of older adults in the ED, however, can be difficult due to the fast-paced nature of emergency medicine (EM).
One intervention that can improve the geriatric patient experience is a comfort cart designed for older adults. In one study a comfort cart led to improved comfort levels and communication for older adults. Of the surveyed respondents, 98.0% affirmed the cart's positive impact on their comfort, while 95.1% reported an improved overall experience during their ED stay, highlighting the cart's
Geriatric Emergency Medicinepotential advantages in reducing stress and anxiety associated with emergency health care settings.
The cart also demonstrated its efficacy in promoting independence, with 67.5% of patients expressing a stronger sense of self-reliance. Clinicians similarly recognized the value of the geriatric comfort cart, with 97.0% acknowledging its positive impact on patient comfort, which, in turn, contributed to improved patient satisfaction.
The cart facilitated a more compassionate care delivery approach, with 87.0% of providers reporting an increased capacity for empathetic and
patient-centered care. Importantly, 83% of clinicians observed that the comfort cart improved patient orientation — a pivotal factor in delirium prevention and boosting patient engagement in their care.
The cart comprises various nonpharmacological therapies designed to increase comfort, improve communication, and reduce stress and boredom for older patients in the ED. The components of the cart include communication-enhancing tools such as hearing amplifiers, headphones, magnifying glasses, pens, notepads, reading glasses, and chargers. To bolster comfort, the cart stocks hats, mittens, blankets, and aromatherapy options featuring scents such as lavender, lemon, and eucalyptus to help mitigate stress and nausea. Distraction tools like snacks, magazines, word puzzles, playing cards, and coloring books are also available. Personal care items including toothbrushes, toothpaste, sleep masks, combs, hand lotion, and deodorant cater to the specific needs of older adults.

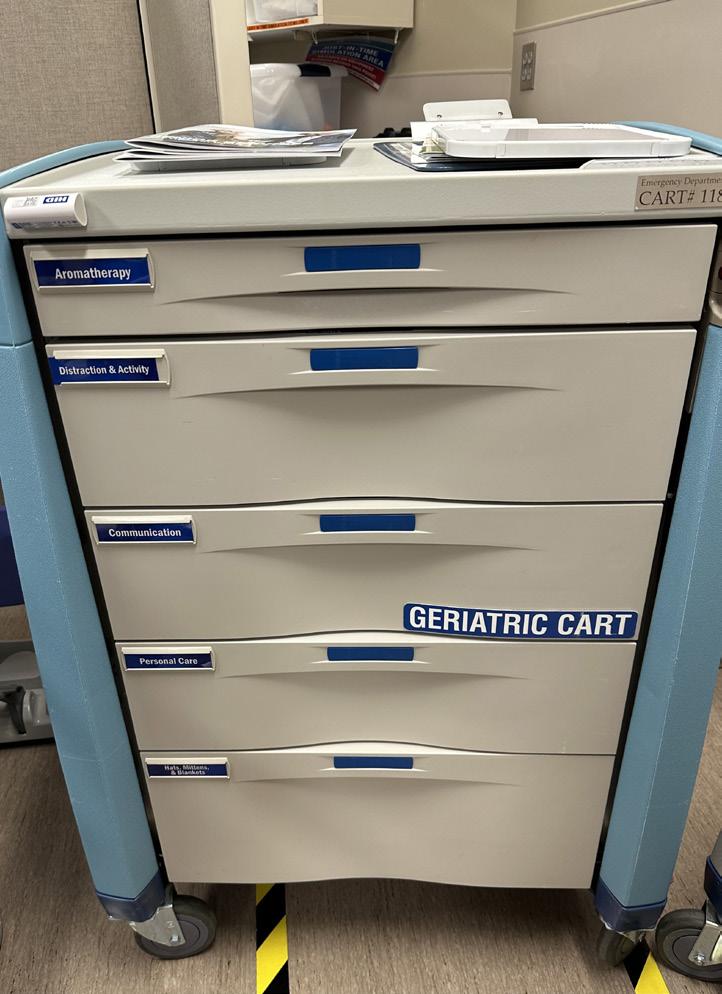
Along with increasing comfort, facilitating communication, and reducing stress, these interventions help older adults feel seen, acknowledged, and
cared for as individuals and patients. By improving comfort and orientation, they may also play a role in deferring, if not preventing, delirium in geriatric patients. In addition to improving the comfort and ED experience for older adults, the cart is low cost and causes minimal disruptions for ED staff. It requires no structural changes to the ED environment, enabling providers to implement the cart and confer benefits to patients in mere minutes.
Simple interventions such as hearing amplifiers, magazines, and coloring books may seem insignificant, but can prove pivotal in the unfamiliar environment of the ED by meeting the unique needs of older adult patients and fostering a culture of patient-centeredness and compassion among health care providers, thereby elevating the overall quality of care.
The geriatric comfort cart is an affordable and feasible intervention that addresses the unique needs of older adults in the ED. As health care systems strive to create age-friendly environments and improve patient-centered care, initiatives like the comfort cart offer a promising avenue to enhance the wellbeing and experience of older adults during their time of need.
Kayla Carpenter is a senior at Hope College in Holland, Mich. studying biochemistry, molecular biology, and Spanish. Kayla is from St. Louis, Missouri and is pursuing a career as a physician and clinical investigator. She recently completed a Summer Undergraduate Research Fellowship in the Department of Emergency Medicine at Mayo Clinic and is a member of SAEM’s Academy for Geriatric Emergency Medicine.

Dr. Bellolio is a professor of emergency medicine with a joint appointment in Health Sciences Research, Division of Health Care Policy and Research, and Department of Medicine, Division of CIM, Palliative Care, and Geriatric Medicine at Mayo Clinic. She is a member-at-large of SAEM’s Academy for Geriatric Emergency Medicine and a methodologist for SAEM’s Guidelines for reasonable and appropriate care in the Emergency Department (GRACE).
The Academy of Geriatric Emergency Medicine (AGEM) works to improve the clinical care of older patients, prepare trainees to care for older patients, and advance the geriatric EM research agenda. Joining AGEM is free! Just log into your member profile. Click “My Account” in the upper right navigation bar. Click the “Update (+/-) Academies and Interest Groups” button on the left side. Select the box next to the academy you wish to join. Click “save.”

Introduction
Concerns have been raised about pediatric cannabis exposure in light of the increasing legalization of cannabis for medical and recreational purposes in numerous states. Accessible cannabis products, including those containing delta-8 tetrahydrocannabinol (THC-8) have resulted in an increase in unintended exposures among children. This article aims to present a comprehensive overview of the emerging issue of pediatric THC-8 toxicity, covering adverse effects, diagnostic approaches, and
management strategies. Furthermore, it highlights the importance of extensive education and stringent regulation to prevent pediatric exposure to THC-8.
Legalization of cannabis has evolved swiftly over the past few years. At the beginning of 2017, 30 states and the District of Columbia permitted the use of cannabis for medical purposes, while eight states and the District of Columbia permitted recreational use. By the end of 2023, 37 states will have legalized
medical marijuana, while 20 states and the District of Columbia will permit adults to use marijuana for recreational purposes. This pervasive legalization has significantly contributed to the increase in pediatric cannabis exposure.
The incidence of pediatric THC- 8 toxicity and poison center calls associated with edible cannabis exposure has risen sharply in recent years. In 2016, 187 cases were reported for children ages 0–12; by

2022, that number had increased to 6,379 cases. Sadly, approximately 56% of all poisoning cases reported in 2021 involved pediatric patients, with 41% of these cases involving children aged 5 or younger. Most of these unintentional exposures can be attributed to edible cannabis products, including those containing THC-8.
THC-8 is a cannabinoid compound found in the cannabis sativa plant. While not naturally abundant, it can be synthetically produced in concentrated quantities. Distinct from delta-9tetrahydrocannabinol (THC-9), which primarily induces cannabis-like effects, THC-8 acts as a partial agonist at the cannabinoid receptor type 1 (CB1) receptor, displaying lower psychotropic potency. The pharmacokinetics and pharmacodynamics of THC-8 closely resemble those of THC-9.
Pediatric THC-8 toxicity can result in various symptoms, including tachycardia, agitation, drowsiness, nausea/ vomiting, hallucinations, hypertension, hyperglycemia, hypokalemia, chest pain, seizures, myoclonia, acute psychosis, sedation, respiratory failure and, ultimately, death. Prompt medical attention is crucial in cases of pediatric THC-8 ingestion. Recognizing the potential risks and symptoms associated with THC-8 toxicity is paramount in providing appropriate care.
THC-8 in the body can be detected using a variety of diagnostic techniques. The standard urine drug test, which can detect THC metabolites in a range of 20 to 100ng/ml, is commonly used. After prolonged and intensive daily use, these metabolites are detectable in the urine for up to 30 days. This indicates that employing this method can effectively confirm the presence of THC in urine samples.
Alternative methods for THC testing encompass hair, oral fluid, and blood analysis. THC can be detected in hair for up to 3 months after use, in oral fluid within 24 hours, and in blood approximately 14 to 21 days after use. Breathalyzer testing has not gained acceptance due to inconsistent results caused by the release of small amounts of THC-8 from fat into the blood.
The management of pediatric THC8 toxicity involves supportive and symptomatic measures. Immediate medical attention is crucial if a child or adolescent has ingested THC-8. Ensuring patient safety and monitoring for lifethreatening symptoms are the first steps in treatment. In some cases, hospitalization may be necessary for close observation and symptom management. As there is currently no specific antidote for THC-8 toxicity, the primary focus of treatment is on symptom management. This may involve the use of benzodiazepines, most commonly lorazepam, to control seizures, and antipsychotics, such as haloperidol, olanzapine, and quetiapine to alleviate anxiety and agitation and to regulate heart rate and blood pressure. Additionally, diagnostic tests, such as 12-lead ECG and cardiac marker evaluations, are conducted to rule out the possibility of myocardial infarction (MI) or ischemia in cases of chest pain. If the ECG shows changes like QRS or QT prolongation, potential toxic ingestion and electrolyte abnormalities should be investigated. Treatment with magnesium may be necessary in such cases. Severe cases of THC-8 toxicity may require ventilatory support. Monitoring vital signs, fluid replacement to prevent dehydration and rhabdomyolysis, and assessing the severity of symptoms and the overall health of the patient are important factors in determining the treatment strategy.
Given the escalating incidence of pediatric THC-8 toxicity, it is imperative to educate parents about the risks and symptoms associated with exposure. Clear and concise information should be provided, explaining what THC-8 is, how it can be harmful, and what the symptoms of toxicity are. It is crucial to emphasize the importance of keeping THC-8 products away from children, storing them out of reach in a secure location, and discussing the dangers of accidental ingestion. Furthermore, regulations should be considered to ensure child-resistant packaging for THC-8 products, as they are not currently required. Packaging targeted towards young children and teenagers, including brightly colored containers with cartoon characters, sweet or fruity flavors, and images of candies, may lead to increased ingestions. The minimal regulation of
THC-8 products has also led to concerns regarding purity and standardization. Contamination by other drugs or substances and discrepancies between actual product contents and package labeling are significant issues that need to be addressed through rigorous regulation and quality control measures.
The increasing accessibility of cannabis products, particularly those containing THC-8, has resulted in a worrisome surge in pediatric THC-8 toxicity cases. While THC-8 holds promise for various medical applications, it is crucial to weigh its potential benefits against its negative effects and addiction potential. Extensive education, comprehensive regulation, and prompt medical attention are necessary to address this emerging public health concern and protect pediatric patients from the risks associated with THC-8 exposure. By providing clear information to parents, moving towards childresistant packaging, and ensuring accurate labeling and product quality, we can mitigate the risks and promote the safe use of cannabis products in the context of pediatric health.
Dr. Lathiya is a research fellow in the Department of Emergency Medicine at Mayo Clinic Health System, Eau Claire, WI. He is an international graduate medical student, a U.S. emergency medicine residency applicant, and a member of the SAEM Program Committee and Wellness Committee. Lathiya.Maulik@mayo.edu

Dr. Cullinan is an assistant professor in the Mayo Clinic College of Medicine and Science, serving as the chair in emergency medicine for Mayo Clinic Health System, a member of International Quality, and the Mayo Clinic Ambulance Board. She is a diplomat of the American Board of Emergency Medicine.

Dr. Horvath is an instructor in the Mayo Clinic College of Medicine and an emergency physician in the Department of Emergency Medicine at Mayo Clinic Health System, Eau Claire, WI. He is the physician site lead for Menomonie in Mayo Clinic Health System.

 By Joshua Davis, MD, Cole Ettingoff, MPH, Adrienne Malik, MD, and Melissa Thomas, MD on behalf of the SAEM Research Committee
By Joshua Davis, MD, Cole Ettingoff, MPH, Adrienne Malik, MD, and Melissa Thomas, MD on behalf of the SAEM Research Committee
Racism and bias in medicine have perpetuated inequities for underrepresented minority groups (URMs) for centuries. URMs have long experienced multifaceted prejudice and injustice within the field of medicine, including receiving poor care as patients due to implicit and explicit biases of caregivers, a shortage of representation in the physician workforce, and particularly a broad lack of inclusion across multiple domains of medical research. This problem is pervasive across all medical specialties, including emergency medicine (EM). While the entire medical community increasingly acknowledges these disparities and
their harmful effects on health care, it is especially critical to identify, comprehend, and tackle these issues within the context of EM research.
A significant lack of URM representation in the EM research workforce is well-established. The roots of this underrepresentation are deep and multifactorial, originating at a societal level, compounding through secondary education, medical school, residency recruitment, and perpetuating in medical specialty selection and academia. These issues are deeply rooted in societal and medical systemic policies and beliefs and perpetuated across generations. This leads to a
system of entrenched marginalization. A reflection of this can be observed in the AAMC 2022 match data which shows that the majority of newly recruited EM residents continue to be predominantly white and male.
Examples of representation disparities are abundant in medicine as a whole and in EM. Historically, Black adults have historically been underrepresented across STEM fields, and this lack of diversity extends to the workforce in emergency medicine. Although Black adults constitute 11% of the U.S. workforce and have roughly equal representation in the health care workforce, they make up only 7% of
STEM bachelor’s degree recipients and 5.4% of physicians Moreover, not only are Black physicians underrepresented, but a racial pay gap is also evident in the medical field. AAMC’s report on active EM residents for the year 2021-2022 highlights representation disparities at the residency level, with the majority identifying as White (69.4%), followed by Asian (15.4%), Hispanic/ Latino (9%), Black (6.7%), Other (3.5%), Native American (0.9%), and Pacific Islander/Hawaiian (0.3%). This disparity persists in the 2018 AAMC data on the demographics of full-time U.S. medical school faculty, with only 3.6% identifying

as Black, 3.2% as Hispanic, 0.2% as Native American, and 0.1% as Pacific Islander/Hawaiian. A 2022 paper by paper by Manchanda et al. examining demographic trends in EM faculty revealed persistent underrepresentation of Black and Latinx physicians in these roles over three decades. Similar challenges are faced by many other marginalized groups. Despite the increasing number of individuals nationwide identifying as gender non-binary or transgender, less than 1% of medical students and physicians share share these identities. These recruitment inequities contribute to the substantial underrepresentation
of URMs in the EM research workforce today. For instance, in 2011, white applicants for National Institutes of Health (NIH) grants were more likely to receive funding than Asian and Black applicants. Similarly, a disproportionate majority of Emergency Medicine Foundation grant recipients were white, cis-gendered, heterosexual males, with only 2% identifying as Black and less than 2% identifying as LGBTQ+.
Greater involvement of URMidentifying researchers may increase the
continued on Page 33
“Greater involvement of URM-identifying researchers may increase the confidence of potential minority research participants and improve diversity and representativeness in emerging EM research.”

RESEARCH
continued from Page 31
confidence of potential minority research participants and improve diversity and representativeness in emerging EM research. More inclusive trial outcomes will directly lead to improvements in EM care for URM groups. Additionally, prioritizing URM physician researchers may facilitate engagement with URM community leaders and stakeholders, who play a crucial role in broader study participation. Elevating URM individuals as key members or leaders of study teams can help researchers identify and study potential barriers to the involvement of marginalized groups, contextualize research questions, and appropriately describe the benefits of study participation. Furthermore, research demonstrates that diverse teams consistently outperform homogenous ones across various domains.
Establishing a diverse and inclusive EM research workforce is an important and achievable objective for our specialty, but it will require substantial systemic reforms and proactive engagement across multiple systems. While policies addressing systemic inequities in areas like housing, education, and income inequality are crucial, their implementation is complex, time-consuming, and difficult. Meanwhile, a multi-pronged approach should be undertaken to effect change at every level of physician employment mentioned earlier, ensuring URM representation throughout EM. This includes actively recruiting URMidentifying students into EM residencies, creating mentorship pipelines for URM residents and faculty interested in research, actively recruiting URM physician researchers as grant applicants on both local and national levels, and intensifying focus on promoting and retaining URM faculty in academic institutions.
Key interventions that can be immediately implemented include openly
acknowledging the importance of a diverse research workforce; showcasing successful URM researchers; designing curricula that addresses biases, diversity, and inclusivity; establishing programs for recruitment, career development, mentorship, and retention of diverse researchers; and striving to diversify opportunities for funding, promotion, presentations, publications, and leadership opportunities.
Recruitment is the initial process to scrutinize through a diversity lens. For instance, admissions staff should receive training on implicit biases and inclusive language and ideally should come from diverse backgrounds themselves. Interviewers should be given sufficient time for each interview, as implicit biases are more likely to manifest under time constraints. Anonymous review of applications and standardized interview questions can mitigate the risk of racial and gender biases. Recruitment materials should emphasize the diversity of the workforce and the institutional culture. A successful diversity initiative, such as an open house centered on URM representation, offers a useful model.
After hiring, programs directed at retention are imperative, as trainees or faculty might otherwise perceive that diversity is not genuinely prioritized by the institution. Standardizing compensation and evaluation processes and continually analyzing them for inequities is essential. Leaders must recognize and acknowledge inequities and seek input from employees and students regarding barriers to promotion or perceived bias in promotions, evaluations, and compensation. Grants tailored specifically for URM researchers can improve funding opportunities.
Lack of mentorship is frequently cited as a major barrier to a successful academic career, and this is equally true among URMs in academic EM. Formal institutional mentorship programs have been shown to bolster career success, promotion, and research funding for
faculty. Developing and executing a successful mentorship program for URMs may be challenging, but with dedicated effort, it is attainable. Leaders should identify future URM clinician-scientists early and actively foster mentorship connections for them.
While recent progress has been made in advancing EM research workforce diversity as a specialty, substantial work remains to be done. The historical (and current) lack of diversity in the research workforce erodes confidence in institutions engaged in biomedical research. As physicians, our commitment to promoting equity in health outcomes is best realized by actively cultivating a diverse research workforce.
Dr. Davis is assistant medical director at Vituity in Wichita, Kan. and clinical instructor at University of Kansas School of Medicine


Cole Ettingoff is a medical student at Trinity School of Medicine,


Dr. Malik is an assistant professor of emergency medicine and core faculty of the emergency medicine residency at the University of Kansas Medical Center in Kansas City, Kansas.
Dr. Thomas is an associate professor of emergency medicine and the vice chair of diversity, equity and inclusion at the University of Kansas Medical Center in Kansas City, Kansas.
“Establishing a diverse and inclusive EM research workforce is an important and achievable objective for our specialty, but it will require substantial systemic reforms and proactive engagement across multiple systems.”
In North America, about 45,000 snakebites occur annually, leading to over 9,000 emergency department visits. The crotalinae subfamily of pit vipers, including copperheads, cottonmouths, and rattlesnakes, account for the majority of envenomations. While most clinical research to date has focused on inpatient resuscitation and acute management, less attention has been given to post-discharge care.

Since early 2021, all snake envenomation cases reported to our statewide poison center, serving around 5 million people, are offered follow-up appointments at our snake envenomation clinic. This outpatient clinic, affiliated with the University of Alabama Birmingham and Children’s of Alabama, is staffed by emergency physicians with advanced training in medical toxicology and wound care.
Patient referrals are initiated through the Alabama Poison Information Center or by direct consultation with medical toxicology during a patient’s hospitalization, with follow-up within one week of discharge. The clinic cares for patients aged 5 and older. During visits, patients are evaluated for persistent limb edema, wound complications, functional deficits, and delayed coagulopathy. Interventions, such as debridement, or physical therapy referrals are provided as needed, and further follow-up is scheduled as necessary.
This commentary aims to:
a) Examine the therapeutic utility of a dedicated snakebite follow-up clinic, focusing on post-envenomation care, including range of motion exercises, wound assessment and debridement of hemorrhagic bullae, treatment of ongoing lymphedema, and screening for rebound coagulopathy.
b) Advocate for seeking out emergency physicians with specialized training in medical toxicology, wound care, and/ or wilderness medicine as crotalinae envenomation specialists due to their advanced experience and expertise.
Following a snake envenomation, patients with residual edema, pain, or reduced limb function practice range of motion (ROM) exercises with the clinic provider. Follow-up continues every 2-4 weeks until symptoms resolve. Patients with ongoing joint pain, stiffness, edema, and decreased range of motion undergo light limb compression along with ROM exercises. Elevation of affected limbs is encouraged. Those with prolonged pain, stiffness, or reduced ROM are referred to occupational or physical therapy, depending on the bite location.
Snakebite Pathway 1: Patients are assessed for signs of persistent wounds which can be bullae, skin break down, and very rarely secondary infection.
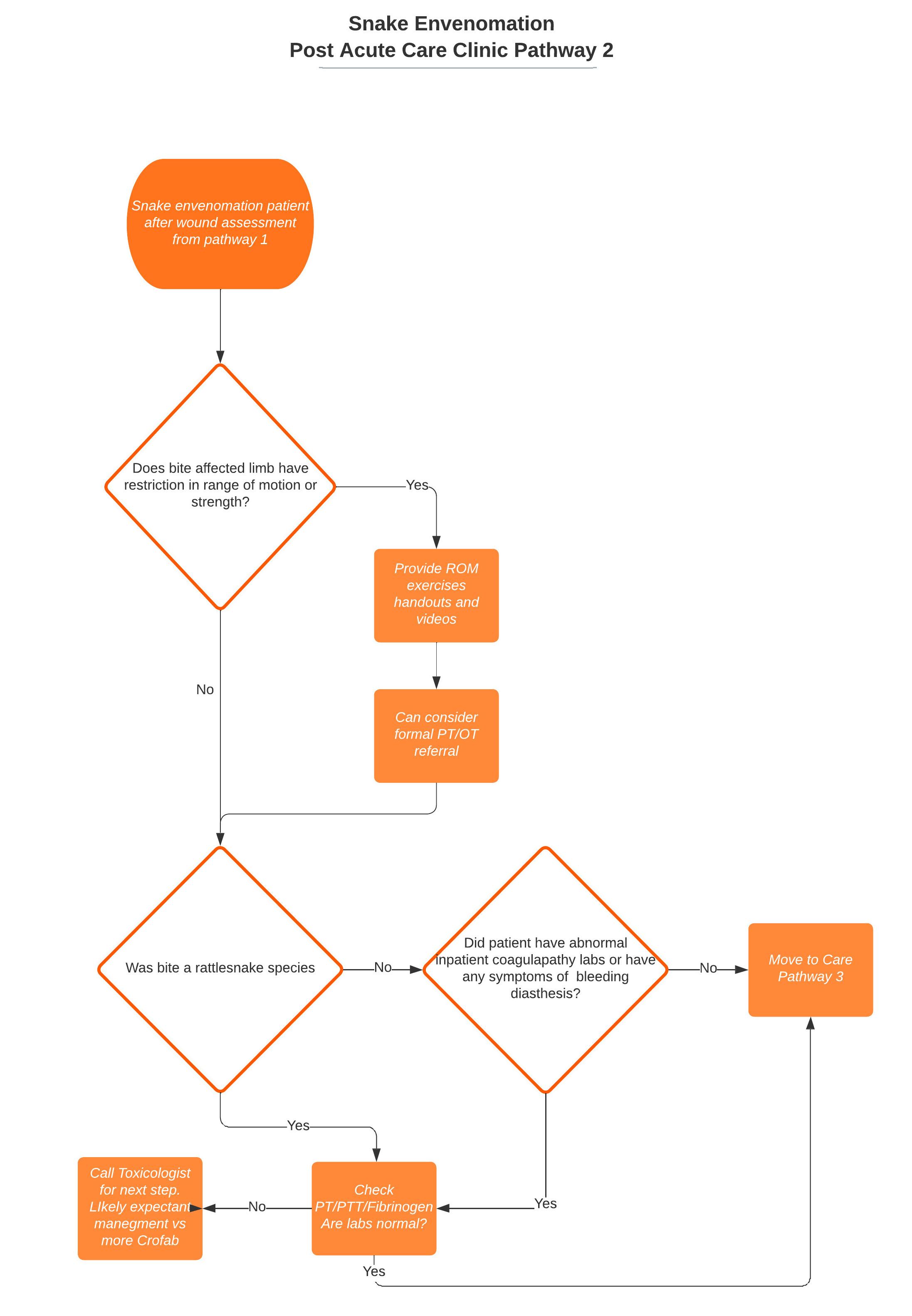

All snakebite patients are evaluated for wounds, blisters/bullae, infection, or other issues. Wounds are treated with aggressive cleansing, debridement, moist wound healing, light compression, and off-loading. Secondary wound treatments such as collagens or skin substitutes are considered at the discretion of the treating wound care specialist. Patients with open wounds are followed until fully healed. (See snakebite pathway 1 and 2).
Snakebite Pathway 2: Patient are next assessed for range of motion of affected limbs and joints. ROM exercises are taught. For severe immobility, referrals to PT and OT are made. In case of rattlesnake envenomation or coagulopathy seen on inpatient labs, repeat coagulation factors are checked.
Hematologic irregularities are a common consequence of snake envenoming worldwide. Venom-induced thrombocytopenia (VIT) and venominduced consumption coagulopathy (VICC) remain the typical manifestations of crotalinae coagulopathy. VICC, produced by venom components like thrombin-like enzymes, results in significantly elevated international normalized ratios (INR) and undetectable
fibrinogen concentrations. While coagulopathy may initially respond to antivenom therapy, it frequently persists and can resurface up to two weeks post envenomation. Mechanisms behind coagulopathy recurrence could involve venom factors accumulating at the bite site, slowly releasing venom over time, or antivenom disassociation from longer-
continued on Page 36
acting venom proteins, permitting rebound symptoms. While delayed coagulopathy can be managed safely if identified, rare cases of morbidity and mortality have been documented in the United States. A rapid and reliable follow-up within a dedicated snake clinic facilitates close monitoring of laboratory parameters such as fibrinogen, PT/INR, and platelet count to screen for delayed coagulopathy. Our clinic mandates repeat lab tests for patients with abnormal hospital results or those at risk of delayed hematological complications, like rattlesnake envenomation. (See snakebite pathway 2)
Addressing Lymphedema
During initial clinic visits, ongoing active envenomation signs are carefully considered. When patients no longer exhibit progressing swelling, emerging bullae, or rebound coagulopathy, the focus shifts from acute venom effect management to continuous care for the affected limb(s). A frequent post-snake envenomation finding is lymphedema. While data surrounding the true incidence of crotalinae-induced lymphedema and subsequent long-term effects is limited, venom-induced injury to lymphatic vessels may explain this complication.
The North American Snakebite Registry (NASBR) reported that out of 450 crotalinae envenomated patients, 96.2% presented with limb edema and 62% exhibited ecchymoses. Unfortunately, there remains a paucity of literature characterizing persistent limb dysfunction post acute crotalinae envenomation.
While venom directly injures lymphatic vessels causing lymphedema, persistent lymphedema could worsen soft tissue damage through a cascade of pathological changes. Untreated chronic lymphedema results in thickening of lymphatic vessel basement membranes, accompanied by fragmentation and degeneration of the elastic fibers. This inhibits coherence between epidermal cells due to intercellular bridge breakdown. Hyperproliferation of keratinocytes and fibroblasts, along with macrophage invasion, culminate in chronic soft tissue inflammation. Clinically, this presents as
lipodermatosclerosis, skin thickening, edema, reduced limb mobility, pain, and discoloration. Untreated lymphedema following snake envenomation could likely lead to a progression of these pathophysiological changes.
The mainstay of lymphedema treatment involves compression and lymph massage. Adequate compression is administered through a variety of techniques. Particularly, compression hose is used to manage lymphedema and offers several benefits, including easy application and availability without a prescription. Additional methods include elastic compression, inelastic neoprene garments, and adjustable Velcro compression. High-compression stockings (30–40 mm Hg) and multilayer compression devices prove effective in treating edema and aiding the healing of active leg wounds when more intensive compression is necessary. However,
milder compression (10-30 mm Hg) can be applied for cases of mild lymphedema or general leg edema. (See snakebite pathway 3)

Expert consensus guidelines concede a scarcity of data regarding the necessity, frequency, and timing of post-hospital envenomation follow-up. The unified treatment algorithm for the management of crotaline snakebite in the United States suggests that followup might not be beneficial for patients not requiring antivenom, those with mild envenomations, and copperhead (Agkistrodon contortrix) envenomations. When follow-up is recommended, focus is placed on 2-7 day post-discharge screening for rebound coagulopathy and self-monitoring for signs of type III serum sickness. However, following these guidelines, the North American Snake Bite Registry (NASBR)

reported residual limb deficits in 30 of 280 (10.7%) of patients who had follow-up data after crotalinae envenomation. Conversely, the incidence of serious late rebound coagulopathy was relatively low, with <5% readmitted for hematological effects. This updated data underscores the need for post-hospital evaluation, not solely for coagulation marker screening, but also for specialized wound care for tissue damage associated with snake envenomation.
The long-term morbidity and complication rates associated with crotalinae envenomation are insufficiently studied. Patients with manageable envenomationrelated complications, including lymphedema, soft tissue injury, and

musculoskeletal injuries, are likely under-detected and untreated. Current guidelines discourage pressure immobilization in the acute envenomation phase prior to hospital evaluation, but do not address compression therapies in the post-acute phase. However, previous literature indicates untreated lymphedema can delay soft tissue healing while increasing the risk of bullae, pain, reduced mobility, and skin ulcers. Without compression dressings, limb pain may be prolonged, limiting range of motion and recovery of limb function.
Connecting a statewide poison center, wilderness medicine specialists, and wound care centers to provide post-snake envenomation follow-up expedites patient care, closely monitors high-risk bites on an outpatient basis, and attends to the wound care needs of affected patients. Our collaboration among different emergency medicine subspecialists has created a regional referral resource for outpatient primary care providers who have less experience in managing snake envenomation, thereby reducing potential associated morbidity. The components of a successful snake envenomation clinic inherently align with the skills of emergency medicine physicians and can be further expanded through subspecialty training and interdisciplinary collaboration.
Dr. Rushton is an associate professor who specializes in emergency medicine and medical toxicology. He holds the position of medical director at the Alabama Poison Information Center and serves as the director of the Office of Medical Toxicology at the University of Alabama Birmingham and Children’s of Alabama. He can be found on Twitter at @rushtonation
Dr. Rivera is an assistant professor and clinical pharmacist in emergency medicine at the University of Alabama at Birmingham. She holds board certification in clinical and provides consultation services for patients through the Office of Medical Toxicology and the Alabama Poison Information Center. She can be reached on Twitter at @jess_rivera11
Dr. Marshall serves as an assistant professor in the Department of Emergency Medicine at the University of Alabama Birmingham (UAB). She is a practicing medical toxicologist and addiction medicine specialist at the Alabama Poison Information Center and UAB.



Dr. Kelly holds the position of associate professor in the Department of Emergency Medicine at the University of Alabama Birmingham (UAB). He also serves as the co-medical director for the Wound Care and Hyperbaric Medicine Program at UAB.


Dr. Schrading is a professor of emergency medicine at the University of Alabama at Birmingham (UAB). In his role as Director of the Office of Wilderness Medicine, he oversees the wilderness medicine track in the UAB emergency medicine residency program. He has extensive experience in teaching wilderness medicine to students, residents, and other health professionals. He can be followed on Twitter at @WalterSchrading
Dr. Atti practices emergency medicine and medical toxicology and holds the position of assistant professor at the University of Alabama at Birmingham (UAB). Currently, she serves as the associate medical director of the Alabama Poison Information Center and takes on the role of course director for medical toxicology at UAB. Connect with her on Twitter at @SukhiAtti
Dr. Shapshak is an associate professor of emergency medicine at the University of Alabama, Birmingham. His additional expertise extends to wound care and hyperbaric medicine, where he practices at the Russell Clinic where he fulfills the role of co-medical director.

“Connecting a statewide poison center, wilderness medicine specialists, and wound care centers to provide post-snake envenomation follow-up expedites patient care, closely monitors high-risk bites on an outpatient basis, and attends to the wound care needs of affected patients.”

Andrea Mancinelli, DO on behalf of the SAEM Academy of Emergency Ultrasound
Emergency physicians have enthusiastically adopted point-ofcare ultrasound (POCUS). In the late 1990s, the Focused Assessment with Sonography for Trauma (FAST) exam was incorporated into Advanced Trauma Life Support® (ATLS®), followed by mandatory training in POCUS for emergency medicine residents in 2001. While the use of POCUS in pediatrics has been slower to evolve, the incorporation of ultrasound into pediatric emergency medicine fellowship training in 2015 marked a recognition of its value in pediatric patient care within the emergency department. Moreover, concerted efforts to reduce radiation exposure among pediatric patients have encouraged the uptake of ultrasound, particularly point-of-care ultrasound (POCUS).
However, conventional B-mode sonography presents numerous challenges. In trauma cases, ultrasound has a poor positive predictive value, necessitating cross-sectional imaging to identify or exclude the presence of significant pathology. Enter contrastenhanced ultrasound (CEUS), a potential game-changer in defining and delineating injuries in the acute setting and for follow up of lesions.
Understanding CEUS
CEUS involves administering intravascular microbubbles while performing a bedside ultrasound. Intravascular microspheres with ultrasound can allow us to delineate vascular structures and localize lesions. These microspheres, composed of a gas core surrounded by various
shell compositions—typically lipid or albumin— are small enough to pass through pulmonary capillary beds yet large enough to reflect diagnostic ultrasound signals. Low mechanical index sonographic waves elicit microbubble oscillation through rarefaction and compression, enhancing ultrasound imaging. In the context of trauma, this accentuates solid organ lacerations, contusions, or even detects active bleeding that presents as contrast material extravasation. These microbubbles are destroyed through increased mechanical index during sonography, while the shell is metabolized by the liver and the gas is exhaled intact through the lungs, eliminating risks of nephrotoxicity, and minimizing side effects.
Several FDA-approved ultrasound contrast agents (UCAs) are available for pediatric use. While CEUS finds primary application in pediatric echocardiography, focal liver lesion identification, and vesicoureteral reflux diagnosis—largely outside the emergency department— their presence in the pediatric domain offers a unique opportunity to expand the diagnostic information available in the hyperacute phase of critically ill pediatric patient care. From trauma cases to refining the diagnosis of abdominal pathologies such as appendicitis, contrast may increase ultrasound’s diagnostic yield. The use of the FAST exam in pediatrics is often controversial due to low specificity and sensitivity; however recent studies indicate that incorporating ultrasound contrast agents can increase organ injury identification sensitivity from 45.2% to 85.7% compared to conventional ultrasound.
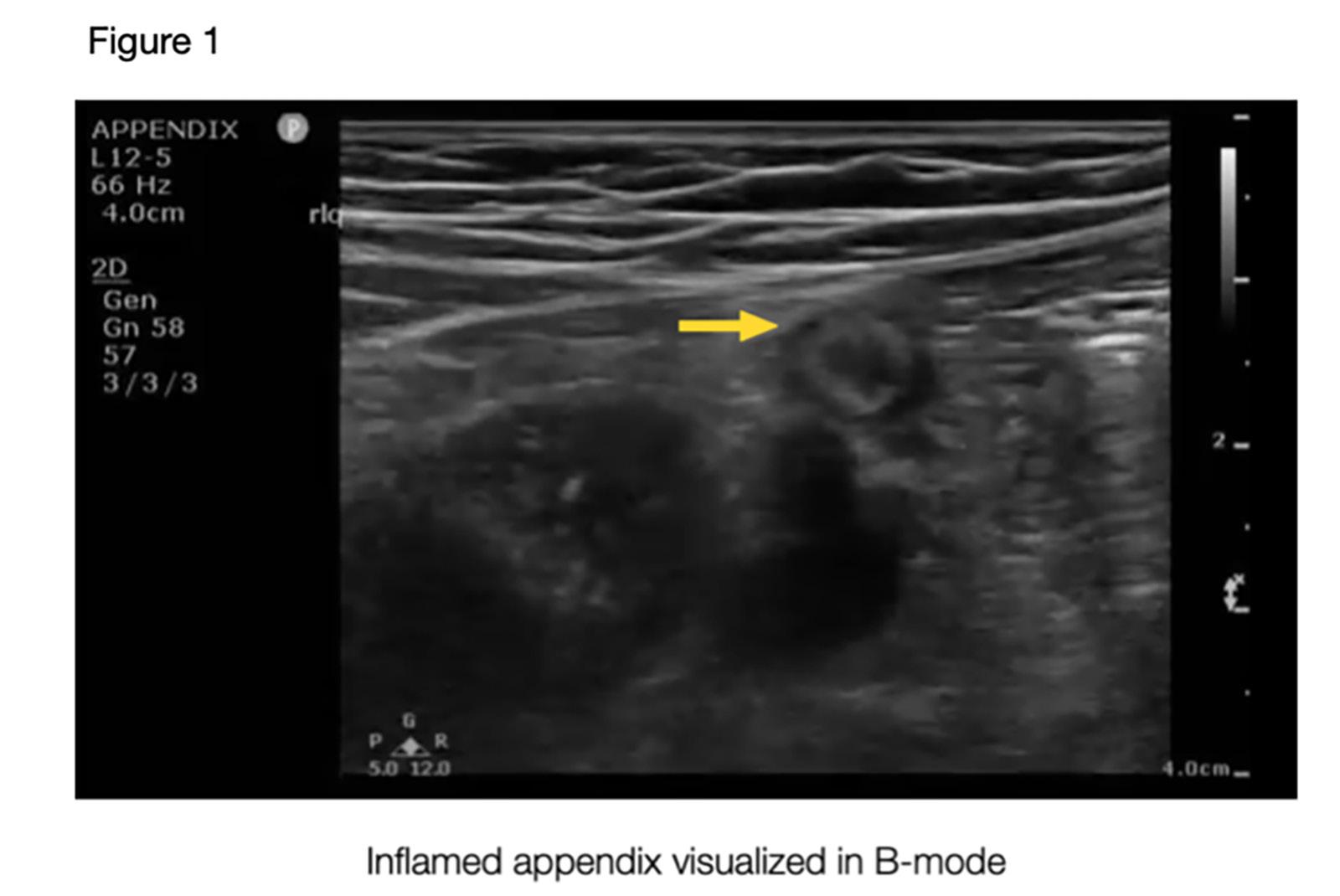
Using intravascular microbubbles with point-of-care ultrasound has the potential to expand diagnostic capabilities, revolutionizing approaches to pediatric patients in scenarios where crosssectional imaging such as CT or MRI are currently needed. For stable patients with traumatic injuries, CEUS could expand the existing binary detection system for free fluid in conventional ultrasound, enabling real-time lesion visualization. Liver and spleen lacerations or fractures would appear as hypoechoic linear or branched patterns within the parenchymal or subcapsular areas. CEUS is rapid, reproducible, and adds
valuable information without extending diagnosis time, taking merely 4-6 minutes to perform. European protocols for CEUS in the FAST exam enable real-time detection of solid organ injuries in in the order of uptake of the UCA: right kidney, left kidney, liver, and spleen. Bedside exams create a child friendly experience by eliminating large, noisy, scary, isolating machines, and reducing reliance on sedation. Notably, CEUS avoids ionizing radiation and nephrotoxic contrast agents, ensuring a safe, non-invasive imaging modality for young patients. Even in the cases where MRI is used with contrast, emerging evidence indicates potential long-term risks associated with gadolinium deposition in developing brains.
CEUS has a more favorable safety profile compared to CT or contrast-enhanced MRI. Allergic reactions are very rare, with anaphylaxis affecting a mere 0.22% of children. Side effects such as headache, nausea, vomiting, and metallic taste appear in only 1.2% of cases. Ultrasound contrast agents (UCAs) have a very short half-life and are readily excreted through expiration via the lungs.
Despite its advantages, barriers to CEUS implementation in the ED remain, including the need for specialized equipment, training in contrast agent utilization, and fostering interdepartmental collaborations. Ultrasound machines need to be optimized for CEUS application, entailing specialized software packages to maintain a low mechanical index for microbubble preservation.
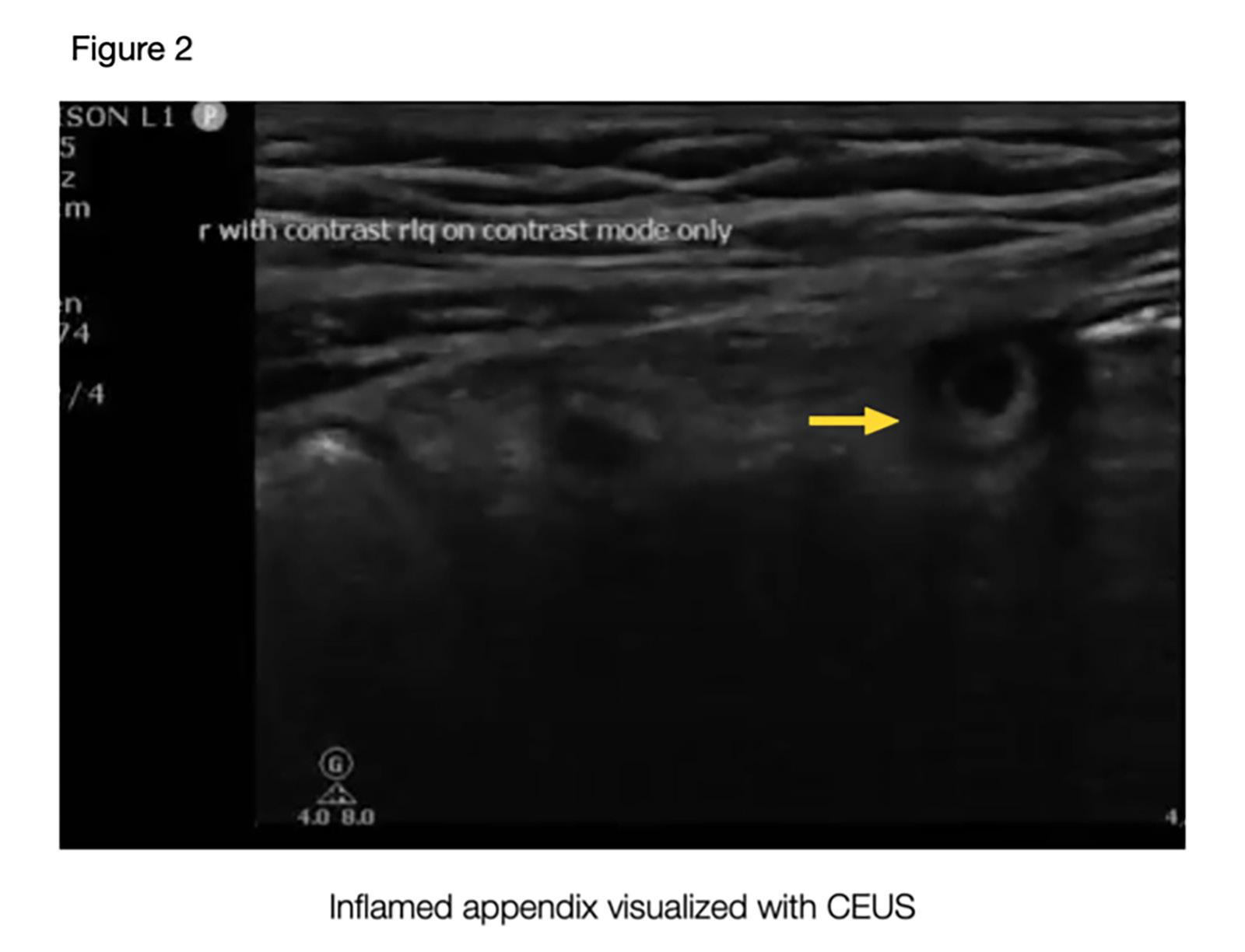
While initial institutional setup costs might require an investment to obtain the UCAs, the long-term costs of CEUS remain lower than those of CT or MRI
The time has come. We owe it to the children to find better approaches to care for them while upholding our oath of “do no harm.” The missing puzzle piece in the care of the acutely ill child, CEUS holds the potential to expand diagnostic horizons and enhance patient outcomes. We must continue researching and validating the utility of CEUS, extending its applications beyond trauma. This would elevate the diagnostic accuracy of common pediatric pathologies while providing the best patient care.
Dr. Mancinelli completed a pediatric residency at the University of Miami/Jackson Memorial Hospital, followed by a fellowship in pediatric emergency medicine at NewYork-Presbyterian Brooklyn Methodist Hospital. Driven by her passion for point-ofcare ultrasound, Dr. Mancinelli pursued further training, completing a second fellowship in emergency ultrasound at NewYork-Presbyterian Brooklyn Methodist Hospital. Currently, she serves as a pediatric emergency attending and ultrasound faculty for the emergency department at Jackson Memorial Hospital in Miami, Florida.


John Riggins Jr, MD is an emergency medicine physician in the Columbia University Irving Medical Center (CUIMC) Department of Emergency Medicine. He serves as the assistant medical director for NYP-Allen ED and the DEI committee chair for the department. He received his training at SUNY Downstate/Kings County and attended the Albert Einstein College of Medicine.

On June 29, 2023, the Supreme Court of the United States (SCOTUS) reversed the rights of universities and colleges to use affirmative action to impact their
incoming class demographics. This was said to be done to make the college admissions process more equitable for “everyone.” I received this shocking news on my phone as I had just finished taking care of one of my patients in the emergency department. I thought about what this would mean for the makeup of colleges, medical schools, and the diversity of our healthcare workforce. I thought about this extensively as a Black male physician who knew what it felt like to be one of only a handful in the room in many places. The Supreme Court justified their majority decision by focusing on what they thought would make the college admissions process more equitable. What the Supreme Court did not consider was the impact that this could have
on our underrepresented minority (URM) pipeline and the diversity of our healthcare workforce. According to the Association of American Medical Colleges (AAMC), Black men account for only 3% of American physicians. The enrollment of Black men in medical school hovers around 3%. There were more Black men enrolling in medical school in the 1970s when compared to the 2010s.
In 2021, the AAMC described how medical school applications and enrollments were finally moving in the right direction among underrepresented populations in the U.S. Could it have been galvanized by the murder of George Floyd and other social justice movements? The devastating Covid-19
“The Supreme Court reversed affirmative Action. The future of diversity within our physician workforce is in trouble.”
pandemic? There was no clear answer, but the fact remained that the numbers were higher than what we had previously seen. How quickly will the Supreme Court’s decision stop this progress that we had just started to make? Not too long ago, many people from Black, Indigenous, and People of Color (BIPOC) and certain religious backgrounds were hindered from entering the medical field which contributed the current makeup of our physician workforce today. The road to becoming a physician is long, taking at least 20 years of schooling for one to be able to call themselves a physician. This country already suffers from healthcare disparities like the high morbidity and mortality rates of pregnant Black Women and the relatively low lifespans of American Indian/Alaska Native (AI/ AN) populations when compared to other groups within the United States. Affirmative action gave opportunities to those who were historically socially disadvantaged from birth, not for any flaw an individual possessed, but due to the societal flaw of building an unjust hierarchy based on categories like phenotype, bank accounts, sexual orientation, and religious beliefs. Although the numbers were still subpar, affirmative action helped to build and promote a pipeline of young, intelligent, ambitious, passionate BIPOC students who would join their white colleagues in the pursuit of their dreams to become a physician in a system that was built to exclude them. The American Medical Association (AMA) recognized and committed to advancing the diversification of the physician workforce through strategic focuses on racial justice and equity, understanding the importance of a diverse workforce in ensuring the highest quality and equitable care for all patients within this country.
As I read through the Supreme Court Decision, I had flashbacks to conversations that I had with some patients in underserved communities who felt unseen and unheard. Some of them felt that they were finally able to
connect to a physician in this puzzling system when I took care of them. They felt that they were finally able to be equitably served and validated within a healthcare system that too often ignored them. The pride that I saw in their faces as I introduced myself as their doctor for the visit is something that continues to encourage and motivate me. As an emergency medicine physician, I always prided myself on being able to take care of any patient from all backgrounds and walks of life. What is society saying to and about our patients when they see a physician workforce that doesn’t reflect our society’s impressive diversity in this country?
I’ve also had to deal with the negative consequences of being one of the few Black male physicians in this country: the result of a leaky pipeline from secondary schools and colleges/universities to medical school that made it hard to recruit and retain BIPOC students throughout the decades on the difficult road to becoming a physician. “Sir, when will I be seeing the doctor?” “Are you here to take me to the CAT scan?” “You don’t look like a doctor.” “Sir, you haven’t taken out my trash yet.” These are just some of the questions and statements that I’ve received from patients of all backgrounds throughout my training and career. Despite my frustrations in these circumstances, I know that there is a dominant image of what a physician looks like in society, and it is not typically assumed to be someone from a BIPOC background. Media’s portrayal of who can be a physician has changed over time, but there is still a lot of work to do. Medical schools look to colleges and universities for their pipeline of students from all backgrounds to evaluate who can withstand the rigorous curriculum of undergraduate medical education. Who will they turn to now if these undergraduate institutions don’t find a way to keep their classes as diverse as our society is becoming?
With the reversal of affirmative action, many colleges and universities are now struggling to figure out how they can ensure that their incoming classes remain diverse. A diverse and inclusive environment has been shown, both in the corporate and healthcare spaces, to improve outcomes, customer/ patient satisfaction, productivity, and organizational culture in many of these institutions. I’ve invested many hours of my life in mentoring and advising students from all age groups. I’ve heard the desperation, frustration, and sadness in some of their voices as they spoke about the lack of opportunities and adequate support given to them as they pursued their dream of becoming a physician. I wonder how many of these students could potentially have been or will be blocked from opportunities if they had not been given the historical opportunities that were taken away from them through legislation and societal practices. Affirmative action did not help to create a pipeline of unworthy, underachieving students who would later become mediocre physicians. Instead, it removed the historical roadblocks that prevented these talented students from achieving their goals, while also strengthening the diversity of our physician workforce, which would benefit all patients and society.
I have hope knowing that there are pipeline programs and individuals who are passionate about ensuring that a diverse pipeline to medical schools continue, but I fear that the legal ramifications of reversing affirmative action might outweigh the positive impact of these individuals’ programs in the long run. Only time will tell.
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policies, positions, opinions, or views of the Society for Academic Emergency Medicine or its members.
“affirmative action helped to build and promote a pipeline of young, intelligent, ambitious, passionate BIPOC students who would join their white colleagues in the pursuit of their dreams to become a physician in a system that was built to exclude them.”with The Op Ed Project.
A wave of anti-diversity, equity, and inclusion (DEI) initiatives are sweeping the nation. The latest attack against DEI, and its positive impact on decreasing health inequities, came in the form of another groundbreaking Supreme Court of the United States (SCOTUS) decision. In June, by a vote of 6-3, justices ruled that the University of North Carolina and Harvard College’s admissions processes violate the
Constitution’s equal protection clause, which makes it illegal for government entities to discriminate based on race. To some, this may seem like an isolated ruling pertaining only to those whose eyes are set on the prize of an elite college education. To those of who have been paying attention, it is about far more. It is about the move towards a color-blind and culturally blind society that ignores the impact of systemic racism. It is about stripping away the tools that mend the inequitable health outcomes experienced by society’s most vulnerable populations.

EM
Centuries of legalized racial discrimination in this country led to inequitable access to education, a social driver of health. Even with the use of race conscious admissions, Black and Latinx students are more
underrepresented at top universities today than they were 35 years ago. With the recent SCOTUS decision, we will see a decrease in the racial diversity of college students. This decreases the diversity of the pipeline for medical school and emergency medicine residencies. As a result, the quality of all learners’ education will suffer, and health disparities will persist. For example, the American Medical Association (AMA) and Association of American Medical Colleges (AAMC) filed a brief arguing that when colleagues’ diverse racial and ethnic backgrounds reflect our diverse patients’ backgrounds, health disparities are minimized. This impediment to diversity at the undergraduate and graduate medical education level leads to a less diverse healthcare workforce.
As academicians, we pride ourselves in practicing evidence-based medicine to best serve our patients. We utilize research-proven algorithms to decide when to scan patients’ heads after

“While the burden of combatting the fallout of the SCOTUS decision is daunting, it is not insurmountable. Academic emergency medicine is responsible for creating and maintaining safe and brave spaces for our patients, trainees, and faculty.”
Katrina Gipson, MD, MPH is an assistant professor of emergency medicine at Emory University School of Medicine and practices at Grady Memorial Hospital. She is a thought leader in health advocacy and an avid writer as a Public Voices Fellow of Academy Health in partnership
@DrKatrinaGipson
traumatic injuries. We incorporate HEART scores into our clinical decisionmaking when caring for patients with chest pain. Similarly, we must use the countless research showing that diverse healthcare teams deliver better care and increase morale amongst faculty and staff. For instance, as a Black woman in medicine, my demographic represents 2.8% of the physician workforce. As a result of my marginalized identity, I experience countless microaggressions in the workplace from faculty, residents, and support staff. Despite all clues to the contrary, where I’m sitting in the ED, strategically placed “DOCTOR” badge under my hospital credentials, I’m rarely considered a physician. Even rarer than this consideration is a colleague stepping in on my behalf as an ally. The hesitancy to be an upstander or anti-racist isn’t always rooted in a lack of care and interest. It often stems from a fear of making the recipient of the microaggression even more uncomfortable or from receiving systemic backlash. My personal experiences with microaggressions are by no means isolated. Studies show that Black residents are dismissed from their training programs at far higher rates than their white counterparts. According to the Accreditation Council for Graduate Medical Education (ACGME) in 2015, Blacks represent 5% of all residents and 20% of those who are dismissed. These residents often report racially hostile work environments, biased feedback, and inadequate appeal processes. Affirmative action cultivates a workplace environment where diversity, equity, and inclusion (DEI) and implicit bias training are valued and supported. Without specific training to increase cultural awareness and humility, Black residents and faculty will continue to suffer. The recent SCOTUS decision will not only decrease the diversity of the pipeline but complicate retention of diverse faculty and staff.
It is clear how the SCOTUS decision impacts the diversity of the medical trainee pipeline and, as a result, the diversity of the medical workforce. However, improved patient outcomes serve as our North Star for research and education endeavors. Decreased racial diversity in medical education and the healthcare workforce will lead to worse patient outcomes. For instance, the Association of American Medical Colleges (AAMC) recently showed that racial concordance (when
patients and physicians share racial and ethnic commonalities) improves communication, trust, and adherence to medical advice. Fewer racial minorities in higher learning institutions mean fewer Black physicians. This results in fewer opportunities for racial concordance for Black patients, which may lead to worse healthcare outcomes. Additionally, racial biases in pain perception lead to the undertreatment of Black patients’ pain. College-educated Black women are 5 times more likely to die than their white counterparts from pregnancyrelated complications. A racially diverse workforce and focused training in recognizing implicit biases address these inequities. Affirmative action practices in education and hiring play an integral role in decreasing the biases that fuel inequitable health outcomes.
While the burden of combatting the fallout of the SCOTUS decision is daunting, it is not insurmountable. Academic emergency medicine is responsible for creating and maintaining safe and brave spaces for our patients, trainees, and faculty. This requires a specific call to action for leadership:
• Program directors (PD) must ensure a holistic review of resident applications. Emergency medicine training programs are academically rigorous; however,
Medical College Admission Test (MCAT) scores and Grade Point Average (GPA) are not the only indicators of academic grit and dedication to the field. Use qualitative analyses that incorporate each applicants’ lived experiences, hardships, and dedication to medically underserved populations as indicators for success.
• Department chairs and PDs must create and maintain a fair and inclusive environment. Department chairs must reward DEI work in the same way that all other academic productivity is awarded in order to avoid the minority tax. Equitable promotion and financial support for DEI work is essential for retention of minority faculty. DEI and implicit bias training for faculty and staff who interact with and evaluate learners are essential. Departments must develop tools to identify potential biases in learner feedback and dismissal rates. Additionally, learners and faculty should know that concerns about discrimination in the workplace aren’t met with unfair criticism of their professionalism.
• A successful emergency medicine residency application isn’t made overnight. The preparation begins long before an applicant prepares for The Match. As such, emergency medicine departments should pair with their associated medical schools in developing pipeline programs for underrepresented minorities in medicine. Provide high school students with the academic and professional mentorship needed for medical school and residency before they even apply to college.

The recent SCOTUS decision striking down affirmative action is a formidable weapon against DEI in healthcare and addressing health inequities. It is part of a strategic plan to reverse the strides made in establishing social justice. However, it is by no means the nail in the coffin. Emergency medicine leadership must be proactive in cultivating safe working and learning environments for students, residents, and faculty. The nation’s health depends on the equitable care of our most vulnerable populations
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policies, positions, opinions, or views of the Society for Academic Emergency Medicine or its members.
 By Amanda Deutsch, MD, and Al’ai Alvarez, MD, on behalf of the SAEM Wellness Committee
By Amanda Deutsch, MD, and Al’ai Alvarez, MD, on behalf of the SAEM Wellness Committee
October 2023 marks the second #StopTheStigmaEM month, a period devoted to recognizing and addressing the mental health challenges in emergency medicine (EM). The selection of October for this awareness campaign is strategically aligned with National Physician Suicide Awareness Day, ensuring that the conversations remain relevant and prominent. Furthermore, our objective is to commemorate the life and legacy of Dr. Lorna Breen, a respected EM physician who sadly took her own life during the peak of the COVID-19 pandemic. It is significant to note that October holds special significance as it marks her birthday, making it a poignant time to pay tribute to her.
Considering that a majority of resident deaths by suicide occur during July-September and JanuaryMarch it is crucial that this dialogue be maintained. By openly and honestly addressing these issues, we can strive for a healthier and more supportive environment for EM professionals. Our goal is to reduce the stigma associated with seeking mental health support and foster a culture that promotes mental well-being for all those working in EM.
This year's #StopTheStigmaEM month seeks to extend beyond raising awareness of the campaign and normalizing conversations surrounding mental health. Our goal is to acknowledge that prioritizing
mental well-being is a daily necessity. As a specialty, the focus should be on proactive, preventative mental health care, rather than solely reacting to crisis moments. Even a single patient death or instance of violence, which EM increasingly encounters, is one too many. Fluctuations in our mental health are normal. Some days are great and we can handle any challenges thrown our way; other days our mental state may be less than optimal, and each additional stressor leaves an imprint that we carry into the next patient encounter, our homes, and the following shift.
It is imperative to disconnect our mental health care from any suggestion
of diminished capacity to provide patient care. Mental illness should not infer impairment. It is essential to actively address our mental health to ensure a healthier and more resilient workforce, better equipped to provide excellent care while maintaining professional fulfillment.
Our focus should be on improving our mental health and seeking care for mental illness. Just as we encourage patients to practice preventative measures, we can lead by example and do the same for ourselves, our families, friends, and patients. Prioritizing mental well-being benefits us all. Let's champion mental health awareness and cultivate a supportive environment for seeking care.
Discover more about #StopTheStigmaEM month this October. Participate in this second-ever campaign by following us online for upcoming events. If you've never consulted with a therapist, consider reaching out to one within the next month. Additionally, unite with the Dr. Lorna Breen Heroes'
Week 1: October 1-7
Sponsored by the Society for Academic Emergency Medicine (SAEM), American Board of Emergency Medicine (ABEM), Association of Academic Chairs of Emergency Medicine (AACEM), American Association for Emergency Psychiatry/Coalition on Psychiatric Emergencies (CPE)
Week 2: October 8-14
Sponsored by the American College of Emergency Physicians (ACEP)
Week 3: October 15-21
Sponsored by the American Academy of Emergency Medicine (AAEM), Canadian Association of Emergency Physicians (CAEP), American College of Osteopathic Emergency Physicians (ACOEP)
Foundation to advocate for changes regarding excessively broad and intrusive mental health inquiries posed by state licensing boards and your hospital. Let's work together to make a positive impact on mental health support and awareness in the EM community.
Dr. Deutsch is director of well-being at Thomas Jefferson Emergency Medicine and subcommittee chair of the SAEM Wellness Committee’s #StopTheStigmaEM initiative. @amandajdeutsch

Dr. Alvarez is director of wellbeing at Stanford Emergency Medicine and chair of the SAEM Wellness Committee.

@alvarezzzy
Week 4: October 22-28
Sponsored by the Council of Residency Directors (CORD) SAEM Residents and Medical Students (RAMS), Emergency Medicine Residents' Association (EMRA), AAEM Resident and Student Association (RSA)
Week 5: October 29-31
Sponsored by the Society for Academic Emergency Medicine (SAEM),
#StopTheStigmaEM month is supported by the Dr. Lorna Breen Heroes’ Foundation, The Physicians Foundation, the National Alliance on Mental Illness, Art of Emergency Medicine, and The Whole Physician
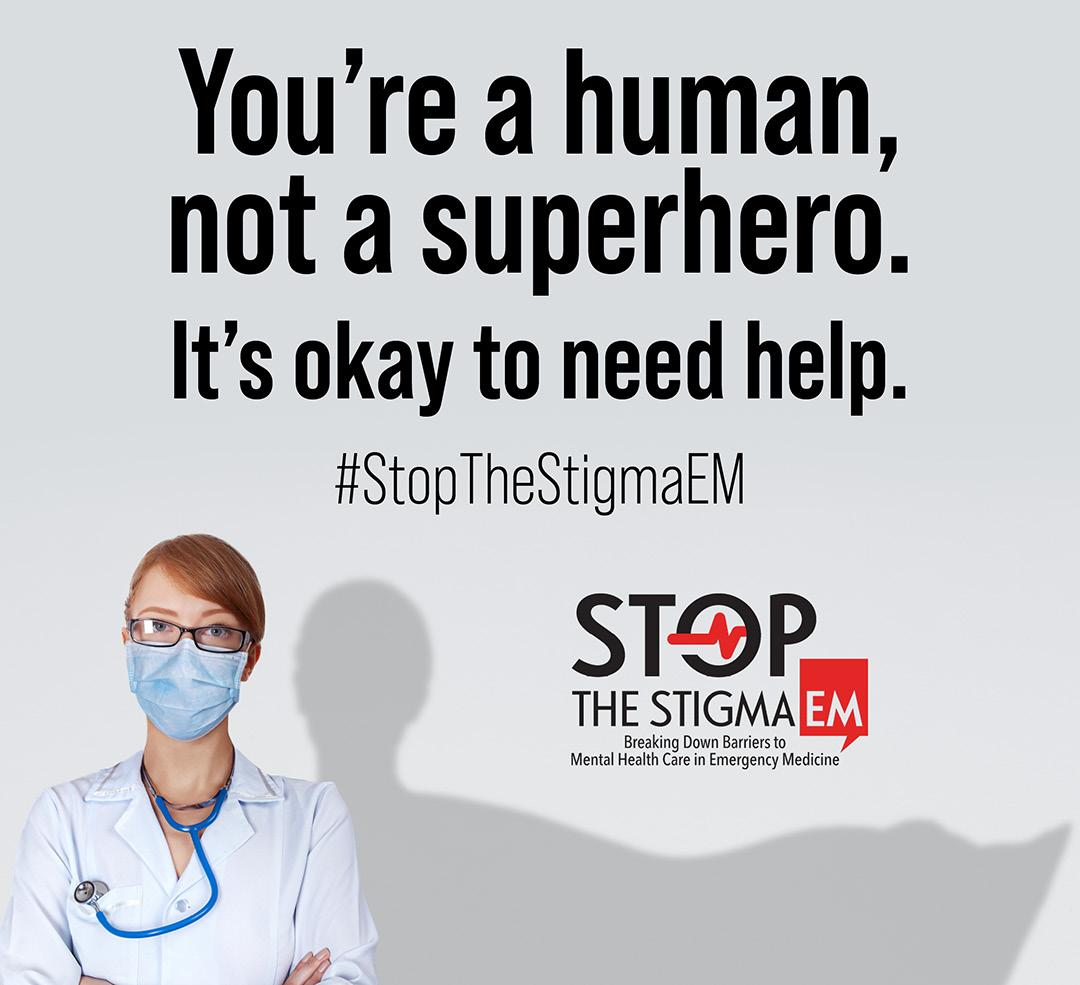
“Our goal is to reduce the stigma associated with seeking mental health support and foster a culture that promotes mental well-being for all those working in EM.”
 By Lara Phillips, MD; Austin Klein, MD, MBA; and William Brincheiro
By Lara Phillips, MD; Austin Klein, MD, MBA; and William Brincheiro
As wilderness medicine enthusiasts, we understand the importance of prevention. Yet, despite extensive research into acute mountain sickness (AMS), there is still no verified objective test for its diagnosis. Why is this the case? Among all the organs in the human body, we know the least about the brain. Many conditions afflict the brain, prompting curiosity about the potential common underlying pathophysiology of seemingly unrelated conditions. Could conditions such as AMS, migraines, and concussions, share a similar physiological basis? If so, could evidence from one condition be applied to broaden our comprehension of the brain?
For example, many patients present with headaches to the emergency department during storms. For migraine sufferers, low-pressure systems can be a trigger. Both AMS and migraines are characterized by headache and associated symptoms like nausea, fatigue, and dizziness. The physiology of AMS is thought to be attributed to hypoxia leading to changes in the cerebral vasculature. At altitude, there is also lower pressure. Could low pressure contribute to AMS? Although uncertain, this is an interesting confounder that warrants attention, especially considering physiological distinctions noted in studies comparing hypobaric hypoxia and normobaric hypoxia.
Those with a history of migraines are also at risk for high altitude headaches, with headache as an isolated symptom rather than part of a syndrome as seen in AMS. Interestingly, one study demonstrated that a history of migraines only minimally predicted development of AMS (Schneider and Bartsch, 2018). Regarding individuals with recent concussions, there is a theoretical risk that exposure to high altitude will lead to worsening post-concussive symptoms. Unfortunately, there is little research to substantiate this theory, and, like AMS, cerebral vascular dysfunction is thought to be the underlying physiology.
The significance of considering AMS, migraines, and concussions
as either separate entities, or as part of a spectrum of pathologies linked by common physiological changes, lies in its potential for valuable research pursued by aspiring wilderness physicians. In addition, conceptualizing a continuum of brain pathology could help us better understand the mechanisms behind altitude-related illness, leading to the development of more effective screening regimes and treatments. For example, detecting early signs of the physiologic response to cerebral vascular dysfunction could enable intervention before the development of severe altitude-related
conditions like high-altitude cerebral edema.
Currently, the most widely used screening tool for AMS is the Lake Louise Score, a questionnaire reliant on a communicative, literate, and insightful patient, rendering it subjective. A suggestion is to adopt a more objective tool, such as the Vestibular Ocular Motor Screening (VOMS) test. Designed to detect signs and symptoms of a concussion by testing eye movement reflexes, this test is 90% accurate, takes only 5-10 minutes to administer, requires


no specialized, equipment, and is feasible to perform in the field.
Could the VOMS test emerge as the next useful objective screening tool for altitude illness? Taking a broader perspective with a larger spectrum of pathology and applying insights from migraine and concussion data to AMS might pave the way for advancements in diagnosis and treatment of these conditions. We encourage those interested in this field to keep working to improve our understanding and treatment of altitude-related illnesses, so that we can help people safely explore and enjoy all that the wilderness has to offer. Your research contributions could catalyze the development of these essential tools.
Until next time, stay safe up there!
Dr. Phillips serves as an emergency medicine physician on the faculty of Thomas Jefferson University Hospital. Additionally, she is the faculty advisor of the Sidney Kimmel Medical College's Wilderness and Disaster Medicine Interest Group and is the co-director of the BreckWild Breckenridge Wilderness and Environmental Medicine Elective. Dr. Phillips underwent a fellowship in Wilderness Medicine at Massachusetts General Hospital where she researched cognitive changes at high altitude.
Dr. Klein will be starting as an anesthesiology resident at University of Massachusetts Chan. He recently completed an MD/MBA program through Thomas Jefferson University and Widener University. He has published research in public health and medical genetics and was inspired by his experience in the BreckWild Breckenridge Wilderness and Environmental Medicine Elective to pursue further experience with wilderness medicine.
William Brincheiro is an MD candidate at Sidney Kimmel Medical College with a passion for high-altitude exploration. His research interests include the utility of screening measures at the emergency department level for both wilderness medicine and addiction medicine. He plans to pursue the BreckWild Breckenridge Wilderness and Environmental Medicine Elective in his fourth year.


“The significance of considering AMS, migraines, and concussions as either separate entities or a spectrum of pathologies linked by common physiological changes lies in its potential for valuable research pursued by aspiring wilderness physicians.”
Endurance races have surged in popularity in recent years. What was once a sport dominated primarily by young, healthy males now attracts individuals of all ages, genders, and physiological backgrounds, all seeking to test the boundaries of physical fitness, as well as mental and emotional perseverance. As interest and diversity grows, more research is focused on addressing a crucial question: "Do endurance athletes have specific nutritional and hydration requirements?"
Before answering this question, it is worth noting several differences in endurance athlete physiology compared to the average, healthy, untrained adult. First, endurance athletes exhibit an elevated VO2max compared to the general population, with elite endurance

athletes demonstrating notably higher VO2max values. VO2max, a numeric measurement given in mL/ kg/min, serves as the gold standard for assessing cardiorespiratory fitness. It describes an individual’s maximum aerobic capacity or the uppermost limit of oxygen consumption and utilization within a given timeframe. Among average, healthy, untrained adults, VO2max ranges from 27 to 40 mL/kg/ min, with females tending to fall at the lower end and males at the higher end of this spectrum. In elite endurance athletes, average VO2max values range from 60 to 85 mL/kg/min.
Unfortunately, an individual's VO2max is largely predetermined by genetics. However, studies indicate that rigorous training can increase an
individual’s VO2max by 10 to 15%. Secondly, endurance athletes also possess a higher lactate threshold. This threshold is another variable that sets the physiology of the endurance athlete apart from that of untrained adults. Through consistent daily training, skeletal muscles upregulate mitochondrial protein synthesis and synthesis of enzymes involved in glycogen, fatty-acid, and protein catabolism and metabolism. The result is increased capacity for lactate production, disposal, and skeletal muscle clearance, resulting in less physiological disruption at the same absolute exercise intensity.
Given this information, one might wonder how these aforementioned factors influence the nutritional
and hydration requirements of these borderline superhuman individuals. The answer, it appears, is "it depends." After many years of research, many scientists have concluded that while overarching principles exist, individuals performing in endurance and ultra-endurance events (lasting more than 6 hours) should collaborate with a multidisciplinary team to establish specific nutrition and hydration goals and to ensure these are being met both in training and on race day. From here, we will delve into some universally recommended guidelines with the understanding that these are not personalized and should therefore be considered as guidance rather than law. Let’s begin with carbohydrates, the primary fuel source during aerobic exercise.
For those engaging in one to two hours of aerobic exercise daily, a recommended carbohydrate intake of 5 to 8 g/kg is advised. Individuals involved in more
than three hours of daily aerobic exercise should increase carbohydrate intake to 7 to 10 g/kg/day. Athletes should aim to consume between 1 and 4 g/kg approximately one to four hours prior to training. Preworkout food should also be low in fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAP) to minimize gastrointestinal distress during exercise. Post-workout, athletes should target a carbohydrate intake of 1 to 1.2 g/kg to aid muscle glycogen resynthesis. In total, carbohydrates should constitute around 60% of an athlete's daily caloric intake, with adjustments based on weight and body fat percentage. Fat is another crucial macronutrient for endurance athletes as it is the favorable substrate for catabolism during prolonged moderate-intensity exercise, or when glycogen stores are depleted. In this context, consumption of 1.1 to 1.5 g/ kg/day, roughly 25% of daily caloric intake, is recommended. Lastly, protein consumption, vital for tissue recovery, is recommended at 1.5 and 2.0 g/kg/day, or approximately 15% of daily caloric intake.
Compared to nutrition, hydration recommendations are simpler, yet equally crucial. During exercise, endurance athletes can lose between 600-2000 mL of fluids per hour. Although it may seem intuitive to match fluid replacement with fluid loss, repeated studies have shown that the best way to maintain proper hydration is to practice “drinking to thirst,” which is as simple as it sounds. This strategy has proven most successful in avoiding both dehydration and overhydration. Overhydration increases risk of gastrointestinal discomfort, unnecessary fluid-carrying, and most significantly, exercise-induced hyponatremia (EIH).

EIH is the most common complication of nutrition and hydration shortcomings in endurance athletes. It is characterized by serum sodium concentrations below 135 mmol/L during or within 24 hours of exercise. Studies suggest that up to 50% of endurance athletes experience EIH during prolonged periods of aerobic exercise. Symptoms can range from mild lightheadedness to altered mental status, coma, and death. Females, overall, are more susceptible to EIH, perhaps due to lower body mass, reduced metabolic rate, diminished sweat production, and insufficient vasopressin secretion.
Another common complication arising from nutrition and hydration deficiencies is Energy Deficiency Syndrome. This syndrome can manifest in various ways, including underperformance, exerciseinduced gastrointestinal syndrome, hormonal imbalance such as the female athlete triad, soft tissue injuries such as stress fractures, and an elevated risk of illness or infection.
Whether striving to complete a marathon or conquer the Four Pass Loop in a single day, it is important to be well-informed, prepared, and most importantly, empowered by the body's remarkable capabilities.
Dr. Bozsi is an emergency medicine resident physician at Cleveland Clinic Akron General with a special interest in wilderness medicine. Outside of work, she enjoys running, hiking, and caring for her rescue cats, Toxoplasma and Henselae.

“After many years of research, many scientists have concluded that while overarching principles exist, individuals performing in endurance and ultra-endurance events (lasting >6 hours) should collaborate with a multidisciplinary team to establish specific nutrition and hydration goals and to ensure these are being met both in training and on race day”
 By Wendy W. Sun, MD; Christopher Bennett, MD, MSc, MA; Stephanie Balint; Carleigh Hebbard, MD, PHD; D. Mark Courtney, MD; and Cameron J. Gettel, MD, MHS, on behalf of the SAEM Workforce Committee
By Wendy W. Sun, MD; Christopher Bennett, MD, MSc, MA; Stephanie Balint; Carleigh Hebbard, MD, PHD; D. Mark Courtney, MD; and Cameron J. Gettel, MD, MHS, on behalf of the SAEM Workforce Committee
Garnering a considerable amount of attention, a publication from 2021 addressing the emergency medicine (EM) workforce projected a surplus of EM physicians (EPs) by 2030. The forecasting model primarily considered four variables: the supply of new EPs (estimated through EM graduate medical education growth), EP attrition, the percentage of patients cared for by non-physician practitioners (physician assistants and advanced practice registered nurses), and the projected demand for emergency care. The model incorporated three different estimates for each variable, resulting in a range of possible scenarios, from a potential shortage of 2,855 EPs to a surplus of 14,937 EPs.
Based on what was deemed by the authors to be the “most likely” scenario at that time — including a 2% GME growth, 3% EP attrition rate, 20%
of visits handled by non-physician practitioners, and an 11% increase in ED visits — the model predicted a surplus of 7,845 EPs in 2030. This
“Since the publication of the 2021 workforce article, new studies examining the EM workforce have demonstrated its fluidity on both the supply and demand sides, the potential pitfalls of forecasting projections, and the need for continuous measurement.”
article, coupled with sharp decline in ED visit volumes and a hiring pause during the initial stages of the COVID-19 pandemic, served as a wake-up call for the specialty, as it highlighted what 2030 might feel like. Since the publication of the 2021 workforce article, new studies examining the EM workforce have demonstrated its fluidity on both the supply and demand sides, the potential pitfalls of forecasting projections, and the need for continuous measurement.
Anecdotally, EPs have seen an increasing number of colleagues pursuing roles in medicine beyond traditional hospital- or facility-based emergency practice. With annual attrition rates among EPs ranging from 3.8% to 4.9% during pre-COVID years and rising to about 8.2% in the early stages of the pandemic, questions have arisen as to a potential overestimation of the projected EP surplus. Furthermore, non-EM board-certified and ruralpracticing EPs face a greater attrition risk compared to board-certified and urbanpracticing EPs. Additionally, female EPs seem to leave the workforce at a younger age compared to their male counterparts. An AMA masterfile data study yielded similar findings when examining attrition trends and how the trends differ by region, residency training, and board certification status.
With a precipitous increase in the number of unmatched EM residency positions — from 14 in 2021 to 219 in 2022 and 554 in 2023 — only 81.6% of positions were initially filled (pre-SOAP) in the 2023 Match. This represents the lowest Match rate since the National Resident Matching Program (NRMP) began presenting EM data in 1983. Several factors likely contribute: the aforementioned projection
of an EP surplus, ED-specific challenges such as crowding and boarding, high burnout rates, and the rapid expansion of EM residency programs. Table 1 displays data from the NRMP Advanced Data Tables spanning 2019 to 2023.
There is a clear and unmet need for further investigation into the variables influencing the stability of the EM workforce, including the inflow (medical student applicants and non-physician practitioner roles) and outflow (attrition) of emergency clinicians. Granular postpandemic prospective survey data, qualitative research at the medical student level, quantitative analysis of existing EM resident attitudes as reported on the in-service exam and needs assessments of EM department chairs will be essential for future descriptions and evaluations of the EM workforce. Over the past year, the SAEM Workforce Committee has collaboratively worked to identify the contextual implications of these recent findings and events, ensuring that the best minds are drawn to the EM specialty and can enjoy enduring careers.
Dr. Sun is an administration fellow at Yale-New Haven Health and past president of SAEM RAMS.

Dr. Bennett is a physician scientist and assistant professor of emergency medicine at Stanford University.



Stephanie Balint is a third-year medical student at Quinnipiac University. She is the RAMS Medical Student Representative, and RAMS liaison to the SAEM Workforce Committee.
Dr. Hebbard is a toxicology fellow at Washington University in Saint Louis and an outgoing SAEM RAMS Board Memberat-Large.
Dr. Courtney is the vice chair and professor of emergency medicine at UT Southwestern in Dallas Texas, and chair of the SAEM Workforce Committee.
Dr. Gettel is an assistant professor in the Department of Emergency Medicine at the Yale University School of Medicine.

“There is a clear and unmet need for further investigation into the variables influencing the stability of the EM workforce, including the inflow (medical student applicants and non-physician practitioner roles) and outflow (attrition) of emergency clinicians.”










Your contributions and dedication have helped shape today's emergency medicine (EM) care, leaving a lasting impact on the field. Through your involvement in SAEM and SAEMF committees and generous giving, you have supported education, research, and training that benefit SAEM members and enhance patient care.



Today, we invite you to consider becoming a part of the Legacy Society by making a planned gift to the SAEMF. By including SAEMF in your estate plans or planned giving, you ensure that future generations of SAEM members can continue to enjoy the same opportunities and support that have been vital to your career.

Take some time to browse SAEMF’s legacy giving resources. We just added several new legacy giving video resources that you may find helpful as you consider opportunities:
• Bequests
• Retirement Plans
• Donor Advised Funds
We recommend consulting with your financial advisor to identify a planned gift that aligns with your intentions. If you would like to hear about the experiences of other Legacy Gifts Committee members and their SAEMF planned gift journeys, we are happy to connect you with them.
Your legacy gift will ensure that the SAEMF continues to be a driving force in advancing emergency medicine education and research, benefiting countless future generations of SAEM members and their patients. Together, let's shape the future of emergency medicine and leave a lasting impact on the field we hold dear.
The Legacy Society is our way of expressing gratitude to visionary donors like you who commit to supporting the SAEMF beyond their lifetime. Your thoughtful contribution solidifies the future of this organization that has been instrumental in your professional journey. We will be honored to recognize your status as a Legacy Society donor in our communications and at events.
“I literally grew up with SAEM, first as a resident presenting at my first national meeting, then as a junior faculty member serving on committees, and then in leadership roles. With this strong, almost visceral connection to the organization, it seemed natural to include SAEM in my legacy planning with the hope that those funds will help the next generation of academic emergency physicians advance in their careers, with the help of SAEMF.”
Brian J. Zink, MD Legacy Society Donor
Experts recommend reviewing your estate plan and will throughout your lifetime, especially during significant life events. When you update your will, it is an ideal time to consider including SAEMF as a beneficiary.
If you are ready to make a legacy gift decision now, a simple bequest is often the easiest, and the language to include in your bequest and/or trust is as follows:
"I give, devise, and bequeath to The SAEMF, a 501(c)(3) charitable organization having its principal offices in Des Plaines, Illinois: the sum of $_____ or _____ percent of my estate. [or all (or _____ percentage of) the rest, residue, and remainder of my estate.] This gift is to be used to further the charitable purposes of The SAEMF, the philanthropic arm of the Society for Academic Emergency Medicine, at the discretion of the foundation's board of trustees. (The SAEMF Taxpayer Identification Number is 262371803.)"
Let us know using the SAEMF Legacy Society Letter of Declaration. Contact Julie Wolfe, Senior Manager of Development, SAEMF for more information.
Join a Committee: Develop Leadership Skills, Build Connections, and More! Committee signups are now open and this year, each SAEM member will apply for SAEM via their own individual link to the committee application form. Your unique link was sent to your SAEM membership email on August 30, 2023. Didn’t receive it? Got questions? Reach out to us at governance@saem.org
Committee involvement nurtures leadership and teamwork skills, provides opportunities to collaborate with diverse individuals; connects you with likeminded professionals; and expands your network. Through committee participation, you’ll enrich your knowledge and expertise while gaining insights into the latest innovations and best practices. Moreover, committee membership serves as a platform to drive positive change within the association and the academic EM specialty, allowing you to leave a lasting impact. Signups close October 13, 2023. Visit our SAEM Committees page to learn more!
Step Up for Leadership in
Nominations Open September 27
Play a pivotal role in shaping the direction of SAEM, RAMS, AACEM, SAEMF, and the SAEM academies by nominating yourself or someone you know for a leadership position. We’re in search of individuals who are not only committed but driven by a passion to foster growth and innovation within our SAEM community. If you bring a diverse range of perspectives to the table and possess the invaluable skills and experience needed to lead effectively, we encourage you to take the leap. Do you know someone who embodies these qualities? Is it you? This is your opportunity to make your mark. Visit our nominations webpage for details on the nomination process. Deadline for submission is November 10, 2022.
Celebrate Excellence: Submit Your Award Nominations
SAEM awards season opens October 1, and we invite you to join us in recognizing excellence in emergency medicine by nominating a colleague, mentor, or yourself for an SAEM or RAMS award.
Developed by SAEM’s Equity and Inclusion Committee, the new and comprehensive Diversity, Equity, & Inclusion (DEI) Curriculum empowers emergency physicians to catalyze positive change in the emergency department by nurturing a culturally competent and inclusive environment that enhances patient outcomes and eradicates disparities.
The curriculum equips you with the essential concepts, tools, and resources to lead your department toward a brighter, more inclusive future. Topics are organized into eight categories, each presenting a collection of resources that can be flexibly applied to meet various needs. These resources vary both in the target audience and in the time available for presentation. Users can choose the resources that best fit their application and adapt and refine them as needed.
• Flexibly Scalable: Adjust content to different learners and contexts.
• Customizable: Tailor for specific departmental needs.
• Regular Reflection: Cultivate ongoing DEI awareness and dialogue.
• Inclusive Language: Decode DEI terms for universal participation.
• Personalization: Integrate pertinent case studies and discussion points.
• Local Solutions: Stimulate conversation about regional issues and support community-driven answers.
• Broad Engagement: Extend DEI involvement to all department members, including those not primarily focused on DEI.
If you are an emergency physician who is committed to cultivating an inclusive emergency medicine workforce and providing the best possible care to all patients, then this curriculum is your definitive guide!
These awards celebrate excellence, honor achievements, and acknowledge the very best in academic emergency medicine research, education, and leadership. Take a look at the awards details and the nomination process and plan to submit your nomination by December 9! Your involvement is the key to making this season of recognition truly special.
Join the SAEM staff and your EM colleagues for the EMRA-sponsored EM Day of Service. Pick any day in September that suits your schedule (or even multiple days!) and lend your volunteering spirit to your local community. For this year’s EM Day of Service, your SAEM staff will once again volunteer at Feed My Starving Children. We’ll be packing bags with a blend of
rice, soy, dried vegetables, and essential vitamins, destined for developing nations across the globe to nourish underprivileged children. What will you be doing? SAEM is a proud sponsor of EM Day of Service. For more information visit: EM Day of Service.
September 17 Marks National Physician Suicide Awareness Day Physicians stand strong as healers, yet they face a stark challenge – one of the highest suicide rates across professions. Over half of physicians have encountered a colleague who has grappled with thoughts of suicide, attempted it, or tragically lost their battle. A somber truth emerges: each year, a million Americans lose a physician to suicide. National Physician Suicide Awareness Day (NPSAday.org) is a rallying cry and a
beacon of hope. Together, we can work to combat burnout, uplift job satisfaction, stop the stigma around seeking mental health support, reshape the narrative around mental wellness, and intercept physicians’ struggles before they escalate into mental health crises. It’s up to all of us to be vigilant, initiate conversations, and disseminate the tools and resources that can guide those in need toward mental health care. Let’s do more to extend a lifeline to those in dire need. Prevention starts with us – let’s stand united to prevent physician suicide.
Join Us in October for
#StopTheStigmaEM Month!
In the demanding and high-pressure nature of emergency medicine, the physicians who stand at the forefront often grapple with unseen battles— stress, anxiety, and burnout. However, unwarranted stigma tied to seeking mental health care hinders them from seeking the help they need. The fear of appearing weak hampers open conversations around mental well-being. This silence perpetuates untreated issues, harming doctors and affecting patient care. To combat this challenge, SAEM, as part of an all-EM Mental Health Collaborative, designates October as #StopTheStigmaEM Month. This international initiative unites EM organizations and their members in a collective effort to dismantle obstacles to mental health care in emergency medicine.
Visit our Stop the Stigma EM webpage beginning October 1 for updated resources and a #StopTheStigmaEM Month calendar of events. Then, stay tuned to SAEM’s social media channels throughout the month as we spotlight initiatives that foster education, raise awareness, and instigate policy reforms — all aimed at bolstering mental health support within emergency medicine and catalyzing a shift from a culture of silence and stigma to one of resilience and empowerment.
SAEM24
Circle These SAEM24 Submission Dates!
The SAEM Annual Meeting’s emphasis on groundbreaking education and research, coupled with a commitment to knowledge sharing and career development, makes it an exceptional platform for showcasing your work and
gaining the professional recognition that can propel your career forward. Submit your work to SAEM24!
• Accepting workshop proposals
• Accepting didactic submissions
• Accepting applications for Dr. Peter Rosen Memorial Keynote
• Abstracts platform opens Nov. 1
• IGNITE platform opens Nov. 1
• Innovations platform opens Nov. 1
SAEM23
Announcing SAEM23 Abstract Awards
Congratulations to the following SAEM23 individuals who were selected as recipients for this year’s abstract awards which recognizes excellence in academic research and presentation.
Basic Science
A Novel Rat Model of Microvascular Blood Flow Derangement After Polytrauma Faculty Breaking Through the Glass Ceiling: Networking Best Practices for Women in Emergency Medicine
Fellow
Utility of End-Tidal Carbon Dioxide to Guide Resuscitation in Prolonged Out-ofHospital Cardiac Arrest
Medical Student
Prevalence of DrugDrug Interactions
That Elevate Bleeding Risk in Older Adults

Presenting with Falls
Medical Student
Gender Differences in Automated External Defibrillator Use and Time-to-Shock in Outof-Hospital Cardiac Arrest
Resident Smartphone App for Estimating Hemoglobin Non-Invasively from Conjunctiva Images
Young Investigator Impact of Receiving Hospital on Out-ofhospital Cardiac Arrest Disparities


Just for SAEM Members: Free and Unlimited SAEM23 Content
SAEM Online Academic Resources (SOAR) has been updated with SAEM23 content available exclusively to SAEM members. With just a few clicks, you can access over 150 cutting-edge SAEM23 educational sessions, presented by experts in academic emergency medicine. SOAR lets you engage with top-notch content anytime, anywhere, giving you the flexibility to expand your expertise at your convenience. Don’t miss out on this golden opportunity to explore the latest insights and advancements in the field. SOAR access is free and unlimited for SAEM members.
Add These Webinars to Your Calendar! SAEM offers live and recorded webinars on a variety of EM topics and are a great way to stay current and learn from your colleagues. SAEM webinars are free for SAEM members and webinar recordings are available after each event. New webinars are constantly being added so check back soon and often for the most up-to-date lineup.
• GEMA HTF’s Humanitarian Research Series: Documenting Conflict with the Yale Humanitarian Research Lab, Sept. 26

• Meet the RAMS Board, Sept. 27

• It’s OK to not be OK: What to Consider When Facing Unexpected Challenges in Your Academic Career, Sept. 28

• Bylaws Committee Webinar, Oct. 3
• GEMA HTF’s Humanitarian Research Series: Research in Action at the World Health Organization, Oct. 10
continued on Page 56
Dr. Alexander St. John Dr. Kathryn Thompson Dr. Courtney Bearnot Dr. Ryan Huebinger Dr. Melissa Parsons Dr. Connor Hambelton Dr. Lindsay Klicksteincontinued from Page 55
There's Still Time to Register for the Midwest Regional Meeting
You’re invited to attend the 2023 SAEM Midwest Regional Meeting, to be held September 14, 2023. The meeting, to be hosted by the Michigan State University Department of Emergency Medicine, will be held at the L.V. Eberhard Center in Grand Rapids, Mich. Program highlights will include research posters, lightning presentations, and a plenary oral session. Register today!
Accepting Applications to the 20242025 ARMED MedEd Class
The Advanced Research Methodology Evaluation and Design: Medical Education (ARMED MedEd) course builds upon the fundamental knowledge and skills of health professions education researchers and equips them to design a high-quality medical education research project and grant proposal. This course is recommended for those who have an
interest and basic level of understanding or experience in medical education research. Scholarships are available! Apply by November 30, 2023.
Accepting Applications: AACEM Chair Development Program
Enhance your effectiveness as a new or aspiring department chair and pave the way for your success as a leader in emergency medicine with SAEM’s Chair Development Program (CDP)! Presented by SAEM’s Association of Academic Chairs of Emergency Medicine (AACEM), the CDP is a leadership training initiative designed to enhance the capabilities and effectiveness of new and aspiring academic emergency medicine department chairs through skill development, advising, and mentorship. Apply by October 1, 2023!
AEM Education & Training
Accepting Submissions for 2023 Annual Meeting Proceedings Issue
AEM Education and Training (AEM E&T) invites submissions from SAEM academies, committees, and interest groups, for a special issue of AEM E&T which will highlight the proceedings from
SAEMF Extends a Warm Thanks to the 2023 SAEMF Annual Alliance Donors

the 2023 SAEM Annual Meeting relevant to education and training. In addition to the standard manuscript types, conceptually based white papers that share cuttingedge ideas and concepts unique to their areas of expertise will be accepted. The issue will publish in early 2024. Submit your paper by September 15, 2023.
AEM E&T Achieves Publishing Milestone! Academic Emergency Medicine
Education and Training (AEM E&T) has received its first Impact Factor™ of 1.8 from Clarivate’s 2023 edition of the Web of Science Journal Citation Reports™. This ranks the journal 25 out of 54 in the emergency medicine subject category. Obtaining an initial Impact Factor marks a major milestone for the journal and signifies its growing influence within the scientific community, as well as its dedication to publishing valuable and relevant research. This metric, in combination with AEM E&T’s first Journal Citation Indicator of 0.75 and CiteScore of 2.2, is an acknowledgement of the exceptional research, high standards, and innovative scholarship demonstrated by the many contributors to the journal. Congratulations to AEM E&T editor-inchief, Dr. Susan Promes and AEM E&T’s editors, reviewers, authors, and all who have added to the journal.
A special issue of AEM Education and Training (AEM E&T) highlighting proceedings from SAEM22 in New Orleans, is now available. The issue includes conceptually based white papers from SAEM academy, committee, and interest group members that share cutting-edge ideas and concepts relevant to education and training. (Note that SAEM member login is required to access journal content.)
SAEM Consultation Services offers EM departments and institutions the chance to improve their practices by leveraging the expertise of our accomplished SAEM committee and academy members. Tailored to your needs, our services provide actionable recommendations across various areas. We ensure a collaborative and productive consulting experience by closely partnering with your department and institution. Learn more.
Are you ready to take the next step in your career or broaden your professional network? Look no further than SAEM’s EM Job Link, your ultimate resource for employment opportunities within the academic emergency medicine community. You’ll discover a curated selection of featured jobs and gain access to insightful tidbits that can help shape your career path. Elevate your career aspirations with SAEM’s EM Job Link!
The new CDEM M3 curriculum provides a framework for a consistent experience for students rotating through emergency medicine during their third year. The focus of this curriculum is the exposure of the student to core emergency medicine concepts and is meant to both supplement and be independent of the M4 curriculum, with certain topics geared towards the M3 student. The background for the curriculum, the full set of objectives divided into the MUSTSHOULD-CAN framework, and the guide for implementation of a third-year EM medical student curriculum can be found on the M3 curriculum webpage.

SAEM announces an exciting opportunity for emergency medicine pharmacists: the Academic Emergency Medicine Pharmacists (AEMP) Interest Group. The short-term goal is for the AEMP is to transition into the SAEM Academy of Emergency Medicine Pharmacists. The purpose of the AEMP is to advance the practice of EM pharmacy by:
• Creating an academic home for EM pharmacists.
• Cultivating multidisciplinary collaboration.
• Facilitating networking opportunities.
• Establishing nationally recognized leadership positions, policies, and platforms.

• Engaging in groundbreaking research in collaboration with EM professionals.
• Providing growth opportunities for our EM pharmacy residents.
• Hosting a prestigious EM pharmacy conference held within the SAEM annual meeting.
Together, we have the unique opportunity to contribute, grow, and enhance the resources and connections within the EM pharmacy community and forge stronger bonds between the EM pharmacist community and SAEM's extensive network of over 8,500 EM physicians.
To join AEMP email governance@ saem.org with your name, designations, institution, and contact information.
In addition, new AEMP committees are now being formed. To sign up as an inaugural leader of AEMP, please complete the online committee interest form by October 2, 2023.
Interested pharmacists can access this new community for FREE until May 17, 2024. For all the exciting details, visit the new AEMP webpage!
Free print and digital materials are available for SAEM members to use to help education patients about
• Who is at increased risk for severe illness from COVID
• The availability of COVID treatments
• The importance of getting treated early
Join the Bylaws Committee and Impact Positive Change Through Your Leadership!
Bylaws Committee member, Ronny Otero, MD, MSHA, interviews the other two members of the committee: James H. Paxton, MD, MBA (committee chair), and Angela Lumba-Brown, MD, about what it’s like to serve as members of the SAEM Bylaws Committee.
Dr. Lumba-Brown: Depending on the Bylaws Committee membership, these discussions may drill down to things as mundane as grammar or take a birds-eye view of whether the document represents SAEM’s commitments to equity as written. As you may imagine, perceptive, diverse, and thoughtful leaders on this committee can make all the difference to policy/ procedure interpretation and suggestions for revision.
Dr. Paxton: The frequency of Bylaws Committee meetings is highly variable and largely depends on how much work needs to be done. On average, we meet for 1-2 hours per month. Because members are elected to a three-year term, we typically think of our workload in terms of three-year cycles. At least once per cycle, the committee will review the entire bylaws document and all significant SAEM policies to assess whether any part of these documents may need to be updated or clarified.
Dr. Otero: What are some other aspects of Bylaws Committee involvement that you enjoy? I enjoy our committee's “limited” scope, which allows us to focus on one topic at a time and keep our discussions focused.

Dr. Otero: What drew you to this position, and why did you choose to run for election to the SAEM Bylaws committee?
Dr. Lumba-Brown: I am a physician-leader with experience in other academic and national committees focusing on policy and organizational improvement. I wanted to advocate for equity, diversity, inclusion and accessibility through policy review with the Bylaws Committee.
Dr. Paxton: I was drawn to the Bylaws Committee for multiple reasons. I learned much from my involvement in various nonprofit organizations and wanted to use what I learned to benefit SAEM and its members. I also wanted to learn more about how the Society is run and connect with others interested in advancing SAEM through their leadership.
Dr. Otero: What are SAEM Bylaws and why are they needed?


Dr. Lumba-Brown: The SAEM Bylaws are a varied collection of policies, rules/regulations, and operating procedures that, like with any governing documents, are nuanced. The Bylaws Committee brings a lens to these documents with the hope of clarifying these nuances and continually updating them to reflect the values of SAEM as they translate into the present.
Dr. Paxton: The SAEM Bylaws provide the rules by which SAEM is governed. They have been approved by a formal vote of the SAEM membership and can only be amended or changed by a majority vote of SAEM members. They provide clear guidance on essential topics such as who qualifies for SAEM membership, member rights and privileges, the SAEM Board of Directors structure, executive officer responsibilities, how meetings and elections are conducted, and the fundamental ethical principles by which our Society operates. We must be cautious and deliberate when considering changes to the Bylaws because even seemingly minor changes can substantially alter how our organization is governed now and far into the future.
Dr. Otero: Please explain what happens during a typical Bylaws Committee meeting and how much work is involved for members?
Dr. Lumba-Brown: I have been a committee member for a little over a year at this point. I have enjoyed learning about the organization and the care that goes into its governance. I have also enjoyed taking a stance when I feel that something requires change.
Dr. Paxton: I have enjoyed working with the SAEM Board of Directors. These are some of our most dedicated SAEM members, and many have been with the organization for a lot longer than I have. Being on the Bylaws Committee is a great chance to get to know SAEM’s leadership team and appreciate the complexity of the decisions they are asked to make every day. The “bonus” is that you help them make tough decisions by lending your bylaws expertise to the discussion.
Dr. Otero: What are some things you have learned from participating in the Bylaws Committee?
Dr. Lumba-Brown: I have learned that there is a robust system of checks and balances in place at SAEM. I have also learned that there is always room for improvement and the need for different perspectives at leadership levels.
Dr. Paxton: The biggest lesson I have learned from my time with the SAEM Bylaws Committee is the importance of considering multiple perspectives when making decisions that influence our entire Society. Although only three members are on the Bylaws Committee, we are still expected to represent the best interests of SAEM’s broader membership. That can be challenging, given the diversity that exists within SAEM.
Dr. Otero: I am only a few months into my term, but my experiences with the SAEM Bylaws committee have given me a greater appreciation for SAEM. I have learned that SAEM is inclusive by design because our bylaws specifically recognize the contributions of military members, senior emergency physicians, and residents. Serving on a committee that advises our board and general membership is an honor that those of us on the Bylaws Committee take seriously.
Dr. Lumba-Brown: SAEM is inclusive by design and yet, we can do more. There are many more groups not listed above that require recognition for their contributions. Please consider nominating or self-nominating to join the Bylaws Committee and continue to impact positive change through your leadership.
Interested in serving on the SAEM Bylaws Committee or any SAEM Committee? Your unique signup link was sent to your SAEM membership email on August 30, 2023. Didn’t receive it? Reach out to us at governance@saem.org. Signup deadline: October 13, 2023. Visit the “Join a Committee” page to learn more.
The Sex and Gender Interest Group (SGIG), established with the aim of integrating and promoting sex and gender concepts into emergency medicine education and research, has made significant strides since its inception. Founded in 2015, the SGIG's initial membership of 25 has steadily grown to 285 dedicated individuals. Annually, this active interest group delivers multiple didactic sessions, workshops, and abstracts/manuscripts encompassing a spectrum of sex and gender subjects.
This year, the SGIG showcased four didactic presentations at SAEM, covering diverse topics ranging from research methodologies to post-Dobbs America's abortion care. Notably, SGIG members featured prominently among the awardees. Dr. Tracy Madsen was honored with the prestigious Advancement of Women in Academic EM award, while Dr. Angela Jarman received the AWAEM Young Investigator Award. Additionally, SGIG members spearheaded a working group at this year’s
Consensus Conference, focusing on the pivotal role of Sex & Gender in Precision Medicine. The group’s goal was not only to formulate a comprehensive 10-year research agenda but also to provide a definitive framework for precision sex and gender research. The outcomes of this group’s work is anticipated to be published later this year.
Under the stewardship of Dr. Jeannette Wolfe, the SGIG, in collaboration with AWAEM, ADIEM, and RAMS, sponsored an innovative and interactive treasure hunt at SAEM 2023. This initiative aimed to educate residents about sex- and genderspecific medicine and foster informal social networking.
Beyond their contributions at the annual SAEM conference, SGIG members remain proactive contributors to research and scholarship in the field of sex and gender. This year, several members published an editorial in Annals of Emergency Medicine which addressed workforce challenges pertaining to gender disparities in academic EM. Furthermore, the group authored two additional manuscripts based on previous didactic sessions: "Incorporating Sex- and Gender-based Medicine into Journal Club" and "Achieving Equity in Emergency Medicine Quality Measures Requires a Sex and Gender Lens." Additionally, SGIG members authored a chapter in the forthcoming textbook, "A Physician’s Path: Emergency Medicine," focusing on sex and gender fellowship opportunities.
With an expanding membership, the Sex & Gender Interest Group continues to flourish as a hub of collaboration, scholarship, and mentorship. We extend an invitation to those interested to join our active and productive community.
SAEM interest groups offer a platform for like-minded members to convene, exchange ideas, and network in a casual and organic manner. Joining these groups is completely free! Interested? Visit the webpage for all the details!
Chuck Shufflebarger, MD, associate professor emeritus of clinical emergency medicine at Indiana University Health Methodist Hospital, officially retired in June after serving on the emergency medicine faculty since 1990. Throughout his tenure, Dr. Shufflebarger's contributions have made a lasting impact on the field. His dedication to providing exceptional patient care in a composed and professional manner has set a standard for excellence in medical practice. He has served as a physician role model and a source of inspiration for his colleagues. As Dr. Shufflebarger embarks on this new chapter, his colleagues, students, and the medical community at large celebrate his achievements and wish him a fulfilling retirement.

Sara Manning, MD, has been appointed as an assistant program director for the Department of Emergency Medicine residency team at Indiana University School of Medicine. Dr. Manning, an assistant professor of clinical emergency medicine, will officially join the team in October.
In this new role, Dr. Manning will contribute to leading the residency program, furthering Indiana University's commitment to innovation and clinical excellence. Her extensive experience with the IUEM clerkship team will serve as a strong foundation as she focuses on advancing graduate medical education.
Ryan E. Tsuchida, MD, has been announced as the interim assistant dean of the Office of Multicultural Affairs for Health Professions Learners at the University of Wisconsin School of Medicine and Public Health, effective August 1, 2023. In this role, Dr. Tsuchida, assistant professor of emergency medicine and chair of the Equity, Diversity, and Inclusion Committee in the BerbeeWalsh Department of Emergency Medicine at UW, will provide leadership, vision, and oversight to enhance diversity, equity, and inclusion efforts for the school’s five health professions degree programs and accredited residency and
fellowship programs administered by UW Health and the school. Dr. Tsuchida also serves as the current Membership Committee Chair for SAEM’s Academy for Diversity and Inclusion in Emergency Medicine (ADIEM).


Cameron J. Gettel, MD, MHS, has been designated as the 2023-2025 fellow for the American Board of Emergency Medicine (ABEM) National Academy of Medicine (NAM). Dr. Gettel holds the position of assistant professor within the Department of Emergency Medicine at the Yale School of Medicine and serves as a clinical investigator at the Yale Center for Outcomes Research and Evaluation (CORE). The ABEM NAM Fellowship aims to offer promising early-career health science scholars in emergency medicine the chance to engage in evidence-based healthcare studies that enhance patient care outcomes both within domestic and global healthcare systems.


Jim McClay, MD, MS, has been designated as the chief research informatics officer for the School of Medicine and appointed chair of the newly established Department of Biomedical Informatics, Biostatistics, and Medical Epidemiology at the University of Missouri in Columbia. He maintains a concurrent appointment with the emergency department. Formerly, Dr. McClay served as an adjunct professor in the Department of Emergency Medicine at the University of Nebraska Medical Center in Omaha. He has a longstanding affiliation with the Society for Academic Emergency Medicine (SAEM) and was actively engaged with SAEM's Academic Informatics and Data Science Interest Group.
Julian Hertz, MD, has been elevated to the position of associate professor of emergency medicine at Duke University. Dr. Hertz has directed his research efforts towards utilizing implementation science techniques to formulate innovative interventions aimed at improving the care provided for acute myocardial infarction and hypertension in Tanzania. Dr. Hertz has been honored with several awards that span the domains of clinical expertise,
 Dr. Chuck Shufflebarger
Dr. Sara Manning
Dr. Ryan E. Tsuchida
Dr. Julian Hertz
Dr. Jim McClay
Dr. Chuck Shufflebarger
Dr. Sara Manning
Dr. Ryan E. Tsuchida
Dr. Julian Hertz
Dr. Jim McClay
educational leadership, and research excellence. Notably, he received the coveted Duke Master Clinician/Teacher Award, a testament to his exceptional skills in imparting knowledge and guidance to the next generation of medical professionals. In addition, Dr. Hertz's dedication to advancing medical scholarship on an international scale has been recognized with the Global Academic Achievement Award from the Society for Academic Emergency Medicine (SAEM).
Brian Patterson, MD, MPH, has achieved the rank of associate professor with tenure at the BerbeeWalsh Department of Emergency Medicine within the University of Wisconsin (UW) School of Medicine and Public Health. Dr. Patterson serves as the inaugural Medical Informatics Director for Predictive Analytics and Clinical Decision

Support for UW Health, the health system affiliated with UW. He leads a federally funded research program aimed at studying and implementing routine use of clinical data and information systems to improve healthcare quality, with a
particular focus on using these data and systems to improve emergency care for older adults.

Michael Pulia, MD, PhD, has been elevated to the position of associate professor with tenure within the BerbeeWalsh Department of Emergency Medicine at the University of Wisconsin (UW) School of Medicine and Public Health. Dr. Pulia is Director of the Emergency Care for Infectious Diseases (EC-ID) research program at UW. He leads a federally funded health services research program focused on improving the diagnosis and management of infectious diseases in the ED and downstream care settings, with an emphasis on systems engineering guided interventions. Dr. Pulia is a nationally recognized expert in antimicrobial stewardship and COVID-19, serving on numerous national and international panels and working groups.
 Dr. Brian Patterson
Dr. Brian Patterson

Accepting ads for our “Now Hiring” section!
Deadline for the next issue of SAEM Pulse is October 1.

For specs and pricing, visit the SAEM Pulse advertising webpage.






Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital, and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Penn State Health Lancaster Pediatric Center in Lancaster, Pa.; Penn State Health Lancaster Medical Center (opening fall 2022); and more than 3,000 physicians and direct care providers at more than 126 outpatient practices in 94 locations. Additionally, the system jointly operates various health care providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center, Hershey Endoscopy Center, Horizon Home Healthcare and the Pennsylvania Psychiatric Institute.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.






Benefit highlights include:
• Competitive salary with sign-on bonus

• Comprehensive benefits and retirement package

• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic Central Pennsylvania
Penn State Health is fundamentally committed to the diversity of our faculty and staff. We believe diversity is unapologetically expressing itself through every person’s perspectives and lived experiences. We are an equal opportunity and affirmative action employer. All qualified applicants will receive consideration for employment without regard to age, color, disability, gender identity or expression, marital status, national or ethnic origin, political affiliation, race, religion, sex (including pregnancy), sexual orientation, veteran status, and family medical or genetic information.

We have academic leadership and staff positions at leading client partner sites across the nation. Let us help you find the academic position that fits your needs, goals and schedule!
RESIDENCY PROGRAM DIRECTOR
Centerpoint Medical Center
Kansas City, MO
RESIDENCY PROGRAM DIRECTOR
HCA Florida Lawnwood Hospital
Fort Pierce, FL
ULTRASOUND PHYSICIAN
St. Joseph Mercy Health System
Ann Arbor, MI
PEDIATRIC SITE MEDICAL DIRECTOR
Medical City Dallas
Dallas, TX
CORE FACULTY OPPORTUNITIES
HCA Florida Lawnwood Hospital
Fort Pierce, FL
RESEARCH DIRECTOR
Morristown Medical Center
Morristown, NJ
Emergency Medicine



Emergency Medicine
is currently accepting applications for July 2024 from individuals who wish to pursue fellowship training in emergency care research. Clinical and health services research tracks are available. This NHLBI-funded T32 program will provide qualified candidates with:
Outstanding Mentorship
Multidisciplinary Research Training
Career and Leadership Development

Masters of Science in Clinical Research
2-3 years of salary support
Lynne D. Richardson, MD, FACEP, Program Director
Alex Manini, MD, MS , Associate Program Director
Roland Merchant, MD, MPH, ScD, Associate Program Director
Ethan Cowan MD, MSc, Assistant Director
Cindy Clesca, MA, Program Administrator
Department of Emergency Medicine of the Icahn School of Medicine at Mount Sinai
For more information, please contact us at ERTP@mountsinai.org or 212-824-8057, or to apply online click here
The Icahn School of Medicine at Mount Sinai is located in New York City. Our top-ranked Emergency Medicine Research Division is comprised of talented investigators conducting high quality research in a supportive, collegial atmosphere that promotes scholarly inquiry and mutual respect. We value diversity of all kinds.
