Leading With Purpose and Heart
A
Conversation With Cassandra Bradby, MD
2025 –2026 SAEM BOARD OF DIRECTORS
EXECUTIVE COMMITTEE

Michelle D. Lall, MD, MHS
SAEM President
Emory University School of Medicine
Board Liaison to:
• Bylaws Committee
• Governance Committee
• Ethics Committee

Jody A. Vogel, MD, MSc, MSW
SAEM President-Elect
Stanford University
Board Liaison to:
• RAMS Board
• Committee of Academy Leaders
• SAEM Federal Funding Committee
• Nominating Committee
• Sex and Gender in Emergency Medicine Interest Group

Pooja Agrawal, MD, MPH
Member at Large Yale Department of Emergency Medicine
Board Liaison to:
• Clerkship Directors in Emergency Medicine
• ED Administration and Clinical Operations Committee
• Grants Committee
• Behavioral and Psychological Interest Group
• Pediatric Emergency Medicine Interest Group

Bryn Mumma, MD, MAS
Member at Large
University of California, Davis
Board Liaison to:
• Academy for Women in Academic Emergency Medicine
• Research Committee
• Disaster Medicine Interest Group
• Palliative Medicine Interest Group
• Research Directors Interest Group
• Trauma Interest Group

Cassandra Bradby, MD Member at Large East Carolina University
Board Liaison to:
• Academy of Emergency Ultrasound
• Awards Committee
• Critical Care Interest Group
• Oncologic Emergencies Interest Group
• Toxicology/Addiction Medicine Interest Group

Jane H. Brice, MD, MPH Chair Member University of North Carolina at Chapel Hill School of Medicine
Board Liaison to:
• Faculty Development Committee
• Vice Chairs Interest Group

Ava E. Pierce, MD
SAEM Secretary-Treasurer
UT Southwestern Medical Center
Board Liaison to:
• Global Emergency Medicine Academy
• Finance Committee
• Program Committee
• Clinical Researchers United Exchange Interest Group
• Wilderness Medicine Interest Group

Jeffrey P. Druck, MD
Member at Large
The University of Utah
Board Liaison to:
• Academy for Diversity & Inclusion in Emergency Medicine
• Fellowship Approval Committee
• Climate Change and Health Interest Group
• Evidence-Based Healthcare & Implementation Interest Group
• Tactical and Law Enforcement Interest Group

Patricia Hernandez, MD Resident Member
Massachusetts General Hospital
Board Liaison to:
• Wellness Committee
• Innovation Interest Group
• Neurologic Emergency Medicine Interest Group,
• Telehealth Interest Group
Ryan LaFollette, MD Member at Large University of Cincinnati
Board Liaison to:
• Simulation Academy
• Education Committee
• Airway Interest Group
• Operations Interest Group
• Transmissible Infectious Diseases Interest Group

Ali S. Raja, MD, DBA, MPH
SAEM Immediate Past President
Massachusetts General Hospital/ Harvard Medical School
Board Liaison to:
• Academy of Administrators in Academic Emergency Medicine
• Workforce Committee
• Educational Research Interest Group
• Informatics, Data Science, and Artificial Intelligence Interest Group
• Quality and Patient Safety Interest Group

Nicholas M. Mohr, MD, MS Member at Large University of Iowa Carver College of Medicine
Board Liaison to:
• Academy of Emergency Medicine Pharmacists
• Academy of Geriatric Emergency Medicine
• SAEM Federal Funding Committee
• Membership Committee
• Emergency Medical Services Interest Group

Megan Schagrin, MBA, CAE, CFRE
SAEM Chief Executive Officer
Liaison to:
• SAEM Executive Committee
• Association of Academic Chairs of Emergency Medicine (AACEM)
• RAMS Board
• SAEM Foundation

Loperamide Toxicity in the Era of Opioid Misuse
Hidden Dangers of Nitrous Oxide Abuse: What to KN2OW
Clerkship Myths: What You Need to Know, Part 2 — The Truth About Interviews
Your Focus: Deciding Whether Fellowship
for
in
Family Planning Meets Residency: Infertility and Parenthood in Emergency Medicine
in Avalanche

A Season of Momentum and Connection at SAEM PRESIDENT’S COMMENTS

Michelle D. Lall, MD, MHS
Emory University 2025-2026 President, SAEM
As the seasons change, so too does the momentum of our work at SAEM. This fall, your board of directors gathered for an intensive two-day meeting to chart important priorities for the coming year. I’m excited to share highlights of our work and ways you can get involved.
Collaboration Across Emergency Medicine
In October, SAEM sent representatives to the All EM AI Summit, ensuring that our voice is part of national conversations on the role of artificial intelligence in emergency care. I also attended ACEP on behalf of SAEM, participating in the Council Meeting and in meetings with leaders from across emergency medicine organizations. These collaborations are vital as we strengthen our collective influence on the future of emergency medicine.
Building Connection and Engagement
One of our priorities is enhancing the ways you connect with each other and with SAEM. We are exploring multiple new avenues to improve your communication experience with the organization and other members, including updates to our website and community platforms designed to
make it easier to share ideas, resources, and opportunities.
Spotlight on SAEM Courses
Our educational programs remain one of the society’s crown jewels. If you haven’t yet participated in a course, now is the perfect time to explore how they can become part of your professional journey.
• Advanced Research Methodology Evaluation and Design (ARMED): Since 2017, 214 participants have advanced their careers through this ninemonth curriculum, which includes webinars, workshops, and mentoring.
• Emerging Leader Development Program (eLEAD): A yearlong leadership development program fostering foundational skills and networks for midcareer faculty. Now entering its fifth year, eLEAD has already supported 68 participants.
• Certificate in Academic Emergency Medicine Administration (CAEMA): Our certificate program for academic emergency medicine administrators, now training its fifth cohort, continues to grow in impact.
“As we look ahead, I encourage you to explore a course, engage in group, or academy, and connect with other members.”
• Advanced Research Methodology Evaluation and Design: Medical Education (ARMED MedEd): Focused on medical education scholarship, this program connects participants with mentors and provides training in grant writing, with 74 participants to date.
• Chair Development Program (CDP): Entering its thirteenth year with the largest cohort to date, the CDP prepares new, interim, and aspiring academic EM Chairs through a series of in-person and virtual lectures and networking opportunities.
Strategic Visioning
At our board meeting, we also devoted time to strategic planning in medical education, research, and professional development. With input from thought leaders across SAEM, we brainstormed new strategies to achieve our objectives.
Our Greatest Strength
Finally, a heartfelt thank-you to the SAEM staff. Their tireless dedication and behind-the-scenes work make our society’s progress possible.
As we look ahead, I encourage you to explore a course, engage in a committee, interest group, or academy, and connect with other members. Together, we are building a stronger, more connected, and more impactful SAEM.
ABOUT DR. LALL: Michelle D. Lall, MD, MHS, is professor and vice chair of diversity, equity, and inclusion in the Department of Emergency Medicine at Emory University School of Medicine.
in a committee, interest members.”

SAEM Educational Courses: Which One is Right for You?
SPOTLIGHT

Leading With Purpose and Heart
A Conversation With Cassandra Bradby, MD
Cassandra Bradby, MD, is an associate professor and residency program director in the department of emergency medicine at the Brody School of Medicine at East Carolina University and ECU Health Medical Center. In September 2025, she also became assistant dean of graduate medical education, expanding her leadership in medical education and training.
She earned her undergraduate degree in biology from the College of William & Mary and her medical degree from Meharry Medical College. She completed her emergency medicine residency at SUNY Downstate Health Sciences University and Kings County Hospital, where she served as education chief resident during her final year.
Dr. Bradby’s academic interests center on medical education, with a focus on recruitment, retention, and the impact of diversity, equity, and inclusion. She was a contributing participant in the 2022 Consensus Conference on Developing a Research Agenda for Addressing Racism in Emergency Medicine.
An active member of the Society for Academic Emergency Medicine since 2014, Dr. Bradby has held several leadership roles, particularly within the Academy for Diversity and Inclusion in Emergency Medicine. She has served on the academy’s executive board since 2019 in multiple positions, including member-at-large, secretarytreasurer, president-elect, president, and immediate past president. She currently serves as a member-at-large on the SAEM Board of Directors.
Dr. Bradby speaking at the ECU SNMA Andrew A Best Banquet.


From biology at William & Mary to medical school at Meharry—what inspired you early on to pursue emergency medicine, and how have those experiences shaped your approach to leading a residency?
My journey toward emergency medicine started long before medical school. In high school, I was fortunate to have mentors in academic family medicine who encouraged me to explore opportunities and even took me on a college tour at William & Mary, which inspired me to pursue my undergraduate education there. One of those opportunities led me to serve as a scribe in the emergency department — my first real exposure to emergency medicine — and I was instantly captivated.
Their guidance also instilled in me a desire to give back, which I carried into medical school as a tutor in the basic sciences and as president of the Emergency Medicine Interest Group. By the time I graduated, I knew academic medicine was my path. Now, as a residency director, I try to honor that early mentorship by supporting and encouraging junior learners, remembering how meaningful it can be to have someone believe in you.
Your emergency medicine training at SUNY Downstate and Kings County concluded with you as Education Chief Resident. In what ways did that leadership role influence your career ambitions and leadership style?
My first SAEM Annual Meeting was during my time as chief resident, when we attended the Chief Resident Forum to network and learn best practices for the role.
That experience not only introduced me to SAEM but also opened my eyes to the wealth of opportunities within the organization.
Serving as chief resident was my first real lesson in leadership — and in middle management. It taught me how to negotiate, advocate for my peers, and, most importantly, communicate effectively. I learned that people often just want to feel heard and valued, and that communication is the foundation of good leadership. The role also gave me a preview of what it means to be an assistant program director — coordinating lecture schedules, working with speakers, and developing curriculum — so when I stepped into formal residency leadership, I was able to hit the ground running.
You’ve focused considerably on medical education— particularly recruitment, retention, and the impact of diversity, equity, and inclusion (DEI). Can you share a story or project that illustrates your biggest challenge or proudest success in this area?
Over the past 10 years in residency education, I’ve had the privilege of mentoring students and residents from across the country and around the world. My proudest successes are seeing them grow into the emergency physicians they aspired to be.
For example, mentees like Daniel Jourdan went on to become SAEM Residents and Medical Students (RAMS)
continued on Page 8
Dr. Bradby traveling to Munich with her family.
Dr. Bradby and her fiance, Terrance Hale, taking a walk in the Outer Banks

president, and Italo Brown is now the chief impact officer of T.R.A.P. Medicine. I know they would have achieved great things regardless, but it warms my heart to know I may have helped a little along the way.
The 2022 Consensus Conference on Addressing Racism in Emergency Medicine marked a key milestone. What lasting lessons and strategies emerged from that meeting, and how are you putting them into practice?
The 2022 Consensus Conference on Addressing Racism in Emergency Medicine highlighted how much of what we “know” is anecdotal, underscoring the urgent need for rigorous, evidence-based strategies. Key recommendations included prioritizing research on structural interventions, tracking equity metrics, and ensuring accountability in patient outcomes and institutional practices.
In my work, I aim to support multicenter collaborations, mentorship pathways for underrepresented scholars, and funding for research that tests interventions to reduce disparities. The goal is to move beyond best-practice assumptions toward strategies that are reproducible, scalable, and truly improve equity in emergency care.
As Residency Program Director at Brody School of Medicine, what innovations in curriculum or training have you introduced—especially around DEI, rare high-stakes procedures, or addressing imposter syndrome?
Recognizing that many of these challenges stem from soft skills, we took our curriculum “back to the basics” this year. During intern orientation, residents completed an observed history and physical with direct feedback from both a standardized patient and an attending,
including communication of the plan of care. We also added skills stations on breaking bad news and performing sensitive exams such as pelvic exams — essential skills often overshadowed by the focus on rare procedures.
Beyond clinical skills, we expanded our didactic series to include sessions on health equity, imposter syndrome, second victim syndrome, and the impact of soft skills on both patient and provider satisfaction. By reinforcing these fundamentals and fostering self-awareness early, we’re building residents who are not only technically strong but also empathetic, confident, and resilient.
You’ve been deeply involved with SAEM since 2014 and have served in every ADIEM leadership role. What has been the most transformative initiative you’ve championed, and why does it still resonate with you today?
One of the most transformative initiatives I’ve had the privilege to help develop was ADIEM’s first pathway program — the Leadership, Engagement, and Academic Pathway (LEAP) Program. Our goal was to create a structured mentorship experience that introduces medical students, starting as early as their third year, to academic emergency medicine and provides them with the tools to become successful faculty members early in their careers.
The program is designed to guide students through each stage of their professional journey — from preparing for the Match, to thriving in residency, to ultimately transitioning into their first faculty role. We welcomed our first two students into the program last year, and it’s been incredibly rewarding to watch them grow — presenting at the SAEM Annual Meeting, engaging confidently on calls, and now beginning their residency interview
continued from Page 7
Dr. Bradby visiting a Richmond tea parlor with her family.
“I try to honor that early mentorship by supporting and encouraging junior learners, remembering how meaningful it can be to have someone believe in you.”
process. Seeing their progress reminds me why intentional mentorship and early exposure to academic medicine matter so much.
As a new member-at-large on the SAEM Board, what are your top priorities moving forward, and how do you hope to influence the organization’s direction in the coming years?
As a new member-at-large on the SAEM Board, my top priority is to deepen my understanding of the organization — how each component, from the SAEM Foundation to our bylaws and governance, works together to advance our mission. It’s been fascinating to see the incredible amount of collaboration and thought that goes into shaping the direction of the organization.
Looking ahead, I hope to help SAEM continue to grow and evolve with the times. Our political, social, and technological landscapes are changing rapidly, and we need to ensure our members — especially our learners and educators — are prepared to adapt and thrive in this new environment.
One area I’m particularly interested in is the responsible integration of artificial intelligence in medicine and medical education. We’re entering a new era of innovation, and as educators, we’re already seeing AI influence applications, evaluations, and letters of recommendation. My goal is to help SAEM lead this conversation thoughtfully — promoting the use of AI as a tool for advancement while remaining vigilant about issues of bias, accuracy, and ethical implementation.
Mentorship is central to academic medicine. How do you mentor residents and students, especially those from underrepresented backgrounds, and what advice do you have for early-career faculty who want to be effective mentors?
Mentorship can easily shift to being about the mentor rather than the mentee, but it should never be that way. The goal is to help your mentee become who they want to be — not a replica of you. I focus on asking thoughtful questions about their goals, values, and what success looks like for them, and then I try to meet them where they are.
For residents and students, especially those from underrepresented backgrounds, intentional mentorship and visibility are critical. I make it a point to create opportunities for them to shine — sending along invitations
to speak, write, or serve on panels that can help build their curriculum vitae and confidence. For junior faculty, this often evolves into true sponsorship — using your platform and connections to help open doors.
For learners, the focus is more on guidance and navigation — helping them understand what’s realistic and what’s possible. That might mean talking through how many residency programs to apply to, how to tailor their application, or how to choose the right environment for their growth. I also remind mentors that today’s trainees are navigating a very different landscape than we did, so our advice has to evolve with the times.
My best advice for new mentors is to set clear goals and expectations at the start of the relationship. Define what both of you hope to gain from the experience. That shared understanding helps frame every conversation and ensures that your guidance stays focused on helping the mentee move confidently toward their own vision of success.
Emergency medicine can be intense and emotionally demanding. How do you recharge and protect against vicarious trauma or burnout, and what do you encourage your trainees to do?
I try not to carry the weight of the emergency department home with me — what happens there, I do my best to leave there. That kind of compartmentalization helps keep the emotional load manageable. Shifting between my clinical and administrative roles also helps prevent burnout; the variety keeps me engaged and focused on new challenges.
I truly love emergency medicine and can’t imagine doing anything else, but my academic roles help sustain that passion and keep me connected to my “why.” Outside of work, I love to travel and spend time at the beach. When I really need to recharge, I escape to the Outer Banks during the off-season — it’s quiet, peaceful, and the perfect place to let my mind settle and just enjoy the rhythm of the waves.
I encourage my trainees to do the same — to always remember why they chose this specialty and this profession in the first place. Take time for yourself, step away when you need to, and find your peace. It’s the only way to sustain the joy and purpose that brought you here.

Dr. Bradby hand knit a blanket at a local art class!
How do you envision the role of emergency medicine evolving in terms of community health, equity, or national health crises—and what role might SAEM and ADIEM play in that vision?
With the constantly shifting political and healthcare landscape, I believe emergency medicine will become more vital than ever as the nation’s healthcare safety net. Our role continues to expand — we’re boarding patients longer, managing increasingly complex care, and often providing what amounts to primary care for those who have nowhere else to turn. The emergency department remains the only place where patients can receive care 24 hours a day, seven days a week, 365 days a year — regardless of their ability to pay.
As private practices close and rural hospitals disappear, more communities are relying on the emergency department as their only point of access to the healthcare system. This places emergency physicians at the intersection of clinical care, public health, and social justice. We are not only treating medical emergencies but also confronting the consequences of health inequities, limited access, and policy failures.
Organizations like SAEM play a critical role in this evolving space. They help prepare and empower academic and clinical leaders to advocate for equity, strengthen community partnerships, and ensure that our specialty continues to adapt to the changing needs of our patients. Through mentorship, research, and education, SAEM and ADIEM can help guide emergency medicine toward a future that is more inclusive, more responsive, and more resilient.
Up Close and Personal
What’s one thing you always keep in the pocket of your scrubs—and one thing you probably should take out?
As a resident, I probably had more pockets than should be legally allowed — my cargo pants had pockets within pockets. I carried everything from intravenous start kits to bags of gloves to lidocaine and guaiac developer. As an attending, I’ve pared it down to just a pen and a piece of paper.
That said, I probably should remember to take the pen out before tossing my scrubs in the wash — I’ve lost more than a few pieces of clothing to ink splotches this year.
If you had a soundtrack playing behind you during a busy ED shift, what song would be on repeat?
“All I Do Is Win” by DJ Khaled featuring Ludacris, Rick Ross, T-Pain, and Snoop Dogg. It’s upbeat, full of energy, and features an all-star lineup — just like my team in the emergency department. Plus, it always puts me in a positive, winning mindset, which is exactly what you need on a busy shift.
What’s your secret superpower outside of medicine?
I’m a self-proclaimed “find-out-ologist.” If something piques my curiosity, I will find the answer — no matter how deep the internet rabbit hole goes. From the latest celebrity gossip to cutting-edge medical innovations, I’ll track it down, learn it, and probably share it with a few people along the way.
If you’re ever in need of some completely unnecessary but highly entertaining information, I’m your girl.
Who was your childhood hero—and how close is that to what you do now?
My mom. She has always been my superhero. An immigrant from Malaysia, she joined the U.S. military just months after arriving in the country and later served in the National Health Service Corps as a nurse. Her dedication to service and caring for others inspired me to pursue a career in medicine. While nursing wasn’t quite the right fit for me, I found my perfect place in medicine itself.
What’s your favorite way to unwind after a high-stress day?
You can usually find me with some yarn in hand — either working on a new project or hunting for the next pattern to try. Nothing helps me unwind quite like crocheting or knitting (though I’ll admit, I’m much faster with a crochet hook).
Over the years, I’ve made blankets, hats, scarves, and wraps — though sweaters are still on my “someday” list. My mom taught me to crochet when I was a kid, and I’ve been hooked ever since. One of my favorite personal traditions is making a baby blanket for every new baby born in our residency program. What advice do you give to mentees that you secretly still need to remind yourself of, too?
Time doesn’t stop — it’s always moving forward. I often remind my mentees (and myself) to pause and truly enjoy the wins, celebrate with family, and take in the peace and beauty around us.
There’s never a perfect time to start something new — just do it, and the rest will work itself out. Each day is unique, and once it’s gone, you don’t get it back.
ACADEMIC CAREER DEVELOPMENT
Building a Career in Academic Emergency Medicine: A Roadmap for Every Stage
By Bret Nicks, MD, MHA; Justin Myers, DO, MPH; Tim Palmieri, MD; Douglas M. Char, MD, MA; Jennifer Kanapicki Comer, MD; and Christine Ju, MD, on behalf of the SAEM Faculty Development Committee
Emergency medicine is where curiosity meets crisis and where teaching and research are anchored in real-time impact. For those pursuing a career in academic EM, the routes are varied. Success comes from building skills, scholarship, leadership, and service. This roadmap offers practical guidance for building a meaningful career and highlights SAEM resources to support you along the way.
Start Early: Academic Engagement During Residency Residency is the time to develop academic habits that last. Find mentors who match your interests and commit to one or two longitudinal scholarly projects. Say yes to roles that build durable
skills. Teaching small groups, designing simulation cases, writing clinical questions, leading a quality improvement project, or supporting a resident-as-teacher curriculum all help build a teaching portfolio.
SAEM offers structured, high-yield resources for residents that can help you choose scholarly lanes and find collaborators beyond your program. Fellowship curiosity often begins in residency—use SAEM’s searchable directories to explore programs and compare expectations.
Early Career (Years 0–5): Choose a Lane, Build Reputable Work Your first faculty years are the time to identify your niche and engage meaningfully. Turn opportunities into visible, peer-recognized
contributions. Many offers will come your way, but balance departmental needs with your expertise. Take time to reflect—waiting even 24 hours before accepting a new role helps ensure it aligns with your priorities.
SAEM’s Academic Promotion Toolkit provides next steps. Aim for three early-career mileposts:
1. A coherent academic identity (“I study decision tools in PE,” “I build ultrasound education for rural ED physicians”).
2. Tangible artifacts such as curricula, protocols, datasets, manuscripts, or FOAMed outputs.
3. Regional or national presence through speaking, committees, or multicenter collaborations.

“Residency is the time to develop academic habits that last, and finding mentors who match your interests is the most important first step.”
SAEM’s toolkits, guidebooks, and online academic resource (SOAR) library offer step-by-step guidance and topic-specific curricula to smooth the transition from residency to faculty.
Midcareer (Years 6–19): Deepen Expertise, Lead Programs, Advance Rank Midcareer is about scale and stewardship. Translate your niche into leadership—direct ultrasound, didactics, a research program, EMS medical direction, or a global health partnership. Build teams, mentor
junior colleagues, and shift from individual projects to programs with measurable outcomes such as publications, grants, or operational benchmarks.
This is also the time to formalize your promotion dossier, aligning outputs with your track (clinical educator, clinical scholar, research-intensive). Service opportunities broaden your impact and network—journal editorial roles, academy leadership, or committee chairs all expand visibility while advancing the field. The SAEM
Career Roadmap for faculty highlights leadership pathways and points to networks that can foster multicenter work and national reputation.
Late Career (Years 20+): Legacy, Sponsorship, and Field-Shaping Work
Late-career academic physicians shape strategy for departments, health systems, and the specialty. Many serve as vice chairs or chairs, senior editors, or leaders in SAEM
continued on Page 15
“Midcareer is about mentoring junior projects to

continued from Page 13
academies and foundations. The emphasis tilts toward sponsorship while continuing to publish synthesis work, write position statements, secure large grants, or direct crossinstitutional initiatives. This is the time to steward culture, standards, and equity, ensuring excellent emergency care for all.
2. Rebuild mentorship deliberately Identify new mentors and sponsors; join SAEM academies and interest groups to find collaborators.
3. Use structured development. Attend skills courses, seek external consultations, and benchmark with peers. SAEM’s faculty development consultation services can help design growth plans and assess success.
academic promotion toolkit to shape your dossier and align with institutional criteria.
Emergency medicine is more than a specialty; it is a platform for teaching, discovery, leadership, and service. With a clear roadmap and the right SAEM resources, you can craft a career that is meaningful and field-shaping. EM remains the best specialty in the house of medicine, and your academic journey in it is worth every mile. ACADEMIC CAREER
Fellowships: When and Why Fellowships are not required for success but can compress learning curves and expand networks. Consider one if:
• You want a career in academic medicine and need protected time to master methodology (research), pedagogy (education scholarship, simulation), or technical skills (ultrasound, EMS, wilderness).
• You aim for credentials that support division or national leadership roles.
• You need structured mentorship to position for grants or multiinstitutional projects.
SAEM’s fellowship directories help compare curricula, expectations, and alumni outcomes.
Navigating Transitions: When Interests Change (They Will)
Academic careers evolve. You might pivot from operations to education, from global EM to research, or from bench science to policy. Healthy transitions follow three principles:
1. Reframe your narrative, don’t erase it. Connect prior wins to your new lane (“Operational QI experience informs my education scholarship on implementation science”).
Continuous Professional Development: Keep Your Edge
Academic EM rewards lifelong learning. Protect time each quarter to keep your scholarly engine running:
• Skill up: Use SAEM’s SOAR library and career development content to stay current on teaching, research design, equity, and leadership.
• Network with purpose: Present annually, volunteer for abstract review, or join a multicenter consortium.
• Document impact: Maintain a living CV and teaching/service portfolio. Align your outputs with promotion criteria. SAEM’s guides and AEM Education & Training literature can help you translate work into promotable artifacts.
Your Next Step (Wherever You Are)
• Resident: Find two mentors, start one project you can finish, and present nationally. Explore SAEM’s approved fellowships if you want structured mentorship and depth.
• Early faculty: Define your niche in one sentence. Produce visible work such as presentations, publications, or curricula.
• Mid/late career: Scale programs and sponsor others. Use SAEM’s
about scale and stewardship—building teams, junior colleagues, and shifting from individual to programs with measurable outcomes.”
ABOUT THE AUTHORS





Dr. Nicks is a professor and executive vice chair of emergency medicine at Wake Forest University School of Medicine and Atrium Health Wake Forest Baptist Medical Center.
Dr. Myers is an associate professor of emergency medicine at the University of North Carolina in Chapel Hill. He is director of faculty education and the global emergency medicine fellowship.
Dr. Palmieri is an associate professor of emergency medicine at Albany Medical College, associate program director for the residency program, and associate course director for the college’s course in evidence-based healthcare.
Dr. Char is a professor and vice chair of academic and faculty affairs at Washington University School of Medicine.
Dr. Kanapicki Comer is an associate professor of emergency medicine at Stanford University and co-director of the medical education scholarship fellowship and director of faculty development.
Dr. Ju is an assistant professor in the department of emergency medicine at UTHealth Houston McGovern Medical School. She is director of undergraduate medical education, emergency medicine specialty advisor, and co-director of the acute care career focus track.
ASK THE PHARMACIST
High-Dose Insulin Therapy: A Life-Saving Strategy for Cardiovascular Drug Overdose
By Reem Alsultan, PharmD; Dawn R. Sollee, PharmD; Reeves Simmons, PharmD; and Charles Foster, PharmD, on behalf of the SAEM Academy of Emergency Medicine Pharmacists
Cardiovascular drugs are among the most frequently reported ingestions to poison centers, ranking fifth overall behind analgesics, antidepressants, antihistamines and alcohols in 2023. Calcium channel blockers and beta blockers are ranked sixth and seventh, respectively, for being associated with the largest number of fatalities, behind acetaminophen, sedatives/ hypnotics/antipsychotics, alcohols, opioids and stimulants/street drugs.
Hyperinsulinemic-euglycemic therapy (HIET), also known as high-dose insulin euglycemia, is a valuable treatment option in the management of calcium channel
blocker and beta blocker toxicity. Several mechanisms of action have been proposed to describe the therapeutic benefits of HIET in this setting.
Proposed Mechanisms of HIET in CCB/BB Toxicity
• Provides glucose to the heart for energy utilization
• Increases cardiac output by enhancing nitric oxide synthase
• Impairs Na+/Ca2+ exchange to retain intracellular calcium
• Improves endocrine dysfunction (hyperglycemia) found in severe calcium channel blocker overdose
Place of HIET in Therapy
Toxicity from calcium channel blocker and beta blocker ingestion classically presents with hypotension and bradycardia. Initial treatment includes intravenous (IV) fluids to support blood pressure, in addition to adjunctive therapies such as atropine and calcium (for calcium channel blocker toxicity) or glucagon (for beta blocker toxicity) to address bradycardia. If hypotension is refractory to IV fluids, the next step is to start a vasopressor such as norepinephrine, with a key decision point being whether to also initiate treatment with HIET. Insulin, especially at high
doses, produces potent inotropic and vasodilatory effects, improving cardiac contractility, increasing myocardial glucose uptake, and enhancing perfusion to the heart.
Special Considerations With Calcium Channel Blocker Toxicity
Non-dihydropyridine (non-DHP) calcium channel blockers such as verapamil and diltiazem exert their primary effects on the myocardium. In the setting of overdose, this can result in marked myocardial depression, making HIET particularly effective because of its inotropic effect.
In contrast, dihydropyridine (DHP) calcium channel blockers such as amlodipine act mainly on vascular smooth muscle with minimal effects on the myocardium at usual dosages. In overdose, however, most notably with amlodipine, synthesis of nitric oxide is increased in a dosedependent manner, which produces profound vasoplegia rather than the myocardial depression commonly associated with non-DHPs. Because HIET can also produce peripheral vasodilatory effects, it does not address this vasoplegic physiology and may even exacerbate distributive shock.
For this reason, HIET may not be prioritized as highly in the management algorithm for DHP calcium channel blocker toxicity compared with treatment of nonDHP toxicity. When a DHP calcium channel blocker is the predominant ingestant, vasopressors play the main role in addressing vasoplegia, with HIET often reserved for cases where
Subclass Examples
Dihydropyridines
Nondihydropyridines
myocardial depression is evident. It should be mentioned, however, that pharmacological selectivity between DHP and non-DHP calcium channel blockers can become blurred in the midst of excessively high levels in systemic circulation, such as in overdose.
Patient’s Clinical Status
Clinical status ultimately guides therapy decisions regardless of the ingested agent (beta blocker, DHP calcium channel blocker or non-DHP calcium channel blocker), and HIET is likely appropriate for initiation when there is evidence of reduced cardiac contractility. If a bedside echocardiogram or ultrasound reveals a reduced ejection fraction, initiating HIET for inotropic support may be beneficial, even with DHP calcium channel blocker toxicity, to improve contractility and perfusion. Other therapies that have been tried in cases of refractory vasoplegia include nitric oxide scavengers such as methylene blue and hydroxocobalamin.
HIET Dosing and Titration
Reported dosing strategies for HIET vary in the literature, but the usual dose is approximately 10 times higher than what is needed for managing diabetic ketoacidosis. This can understandably lead to practitioner hesitation when considering HIET; however, with frequent lab monitoring and judicious supplementation of glucose and electrolytes, this resource-intensive therapy can be implemented safely as a potentially life-saving treatment for cardiac drug poisonings.
Primary Sites of Action Main Therapeutic Effects
Before starting the insulin infusion, obtain baseline blood glucose and serum potassium. If blood glucose is less than 200 milligrams per deciliter, administer 25 to 50 grams of IV dextrose. A continuous IV infusion of 10 percent dextrose (peripheral line) or 20 percent dextrose (central line) should also be initiated and titrated during HIET to maintain glucose between 100 and 200 milligrams per deciliter. If potassium is less than 3 milliequivalents per liter at baseline, provide supplementation before starting HIET.
When ready to begin, administer an IV bolus of 1 unit per kilogram of regular insulin using actual body weight (no consensus on a maximum weight), followed by a continuous IV infusion of 1 unit per kilogram per hour.
HIET should be titrated every 15 to 30 minutes as needed, based on cardiac output parameters (contractility and perfusion) and blood pressure:
• Contractility: Assess by bedside ultrasound in the emergency department. Increase HIET rate if ejection fraction is less than 50 percent.
• Perfusion: Target urine output greater than 0.5 milliliters per kilogram per hour, warm skin with normal color, palpable peripheral pulses and improving serum markers (basic metabolic panel, lactate, venous blood gas).
• Blood pressure: Goal is systolic blood pressure 90 millimeters of mercury or higher, or mean arterial pressure 60 millimeters of mercury or higher.
Amlodipine, Nifedipine, Nicardipine, Clevidipine
Verapamil
Diltiazem
Vascular smooth muscle
Myocardium & AV node
Intermediate (AV node + some vascular)
Potent arterial vasodilation
↓SVR, ↓BP (minimal cardiac conduction effect)
↓HR (negative chronotropy), ↓contractility (negative inotropy), ↓AV conduction
Slows AV conduction, modest ↓HR, moderate vasodilation
SVR, systemic vascular resistance; BP, blood pressure; HR, heart rate; AV, atrioventricular
Clinicians should not rely solely on blood pressure goals to guide therapy. HIET can lower vascular tone, while vasopressors may raise mean arterial pressure without improving tissue perfusion. HIET should instead be titrated based on contractility, perfusion and blood pressure goals, up to 10 units per kilogram per hour
continued on Page 18
CCB or BB overdose with hypotension
refractory to IV fluids, calcium, and atropine
It can be cardiogenic shock:
Start HIET with 1 unit/kg bolus followed by infusion of 1 units/kg/h + D10W infusion.
Titrate up by 1-2 units/kg/hour every 15-30 mins up to a MAX of 10 unit/kg/h based on cardiac output goal parameters
Consider adding: Epinephrine infusion, other inotropes, and pacemaker placement.
ConsiderconsultECMOteam
It can be distributive shock:
Increase norepinephrine infusion
Consider vasopressin
Consider methylene blue or hydroxocobalamin if refractory
ASK THE PHARMACIST
continued from Page 17
Risk of Volume Overload
Administering high amounts of insulin using a standard concentration (1 unit per milliliter) for IV infusion can lead to potential volume overload, especially in patients who may already be in distributive shock. Using concentrated preparations of insulin (for example, 16 units per milliliter) can reduce total fluid volume administered. Institutions should ensure safety measures are in place and provide education to nurses, pharmacists and providers to prevent confusion between concentrated and standard insulin drips.
“Insulin, especially at high vasodilatory effects, improving glucose uptake, and
Atropine
Glucagon
Epinephrine infusion
Inotropes
Pacemaker placement (if refractory bradycardia)
minimize volume and decrease the risk of hypoglycemia. Blood glucose should be monitored every 20 to 30 minutes for the first four hours following insulin initiation. If blood glucose is 100 to 200 milligrams per deciliter at hour four and the insulin drip rate is stable (no further titration needed to maintain hemodynamic stability and perfusion), monitoring may be reduced to every hour while HIET is running.
Blood sugar checks should continue for at least four hours after HIET is stopped to monitor for hypoglycemia, as it may take time for accumulated insulin to clear. When serum glucose levels begin to stabilize, it may indicate resolution of calcium channel blocker overdose. This observation does not apply to beta blocker overdoses.
HIET Monitoring
Frequent lab draws and attentive patient monitoring are imperative. While insulin greatly improves glucose uptake by myocardial cells, hypoglycemic events and significant electrolyte derangements can occur fairly quickly due to the amount of insulin being administered. Some have reported a hypoglycemia incidence of 31 percent—a common risk during HIET, albeit one that can be avoided with appropriate monitoring and supplementation of glucose.
The optimal glucose level during HIET is not defined but is typically targeted at 100 to 200 milligrams per deciliter using dextrose infusions. In patients with central venous access, concentrated dextrose solutions (20 percent or greater) are preferred to
For potassium, the target concentration during HIET is not well defined, but maintaining a mild hypokalemic range (2.7-3.2 milliequivalents per liter) is common, with monitoring every one to two hours during initial stabilization and with any titration of insulin. Aggressive potassium repletion is not recommended, and a lower potassium goal is appropriate to avoid rebound hyperkalemia once the insulin infusion is stopped and extracellular potassium shifts occur.
HIET Duration and Discontinuation
Duration of HIET varies based on clinical response. In the available literature, infusion durations range from a single insulin bolus to infusions lasting hours to days. On average, insulin duration is reported as 24 to 31 hours.
When considering discontinuation, vasopressors and other inotropes
should be tapered off before HIET is discontinued, as HIET is vasopressorsparing and abrupt discontinuation may precipitate cardiogenic shock. There is no consensus on how to discontinue HIET. One method is to decrease the rate by half every one to four hours; another is to decrease the infusion by 1 unit per kilogram per hour. Insulin levels can remain elevated even after discontinuation, so blood glucose, symptoms of hypoglycemia and potassium concentrations should be monitored for at least 24 hours afterward.
Standardizing for Safety and Effectiveness
Using HIET as a potential life-saving treatment in cases of beta blocker and calcium channel blocker overdose should be available in all emergency departments. Standardized protocols outlining dosing, monitoring and titration parameters are essential for safe and effective use. When designing a protocol, a multidisciplinary approach is best, and clinicians are encouraged to consult their local poison center at 1-800-222-1222
ABOUT THE AUTHORS




Dr. Alsultan is a clinical pharmacy specialist in emergency medicine at Brigham and Women’s Hospital in Boston, Massachusetts.
Dr. Sollee is a professor at the University of Florida College of Medicine, Department of Emergency Medicine, a clinical toxicologist, and the director of the Florida/USVI Poison Information Center –Jacksonville.
Dr. Simmons is the assistant director of the Florida/USVI Poison Information Center – Jacksonville, a clinical toxicologist, and an emergency medicine pharmacist at UF Health Jacksonville.
Dr. Foster is a clinical content specialist with Merative, Micromedex, and an emergency medicine pharmacist at Poudre Valley Hospital in Fort Collins, Colorado, and the Medical Center of the Rockies in Loveland, Colorado.

Improving Patient and Staff Safety in the ED Through Standardized Behavioral Health Intake
By Mary-Kate Gorlick, MD; Catherine Reynolds, MD; and Kunal Sharma, MD, MBA
Background
Behavioral health patients presenting to the emergency department (ED) require timely and coordinated care, yet triage, intake and assessment processes are often fragmented and inconsistent. At Lyndon B. Johnson Hospital in Houston (LBJ Hospital), behavioral health triage and intake historically occurred in the main ED triage area, a crowded and overstimulating environment not designed for patients in psychiatric crisis. There was no standardized nursing involvement, variable provider participation and inconsistent safety protocols, all of which contributed to delays
in evaluation, safety events such as elopement and ingestion, and inefficiencies in documentation. These challenges were not only frustrating but unsafe and often left staff feeling that they had little control over their own well-being at work.
Intervention
In May 2025, we implemented a new standardized behavioral health intake (BHI) process designed to improve safety, efficiency and coordination of care. Intake was relocated from ED triage to a quieter, dedicated pod, better suited for psychiatric evaluation. A multidisciplinary team
was established, integrating intake nurses, technicians, providers and security into a unified process. All participants in the intake process were assigned defined roles to reduce duplication of effort and improve accountability. Security presence was streamlined to ensure continual coverage, supported by weapons detectors and managed belongings to reduce risk of violence.
A structured risk stratification system was introduced. Patients were classified as low, medium or high risk in consensus with the intake team. Low-risk patients returned to the general ED for
“Median arrival-to-provider times decreased by nearly 50 percent, arrival-to-psychiatry consult times decreased by more than 60 percent, and overall emergency department length of stay for this patient group decreased by one-third.”
standard evaluation and disposition. Medium- and high-risk patients received expedited psychiatric consultation when appropriate, safety sitters and psychotropic medications if clinically indicated. This approach allowed for consistency and timeliness in patient care and important safety interventions for higher-risk patients. It also minimized unnecessary delays for those who did not require extended psychiatric evaluation and treatment.
Standardized documentation tools were developed and embedded in the electronic health record. Smart phrases, checklists and a risk assessment tool helped ensure that critical safety information was captured reliably and consistently.
Results
The new BHI process produced measurable and meaningful improvements. Median arrival-toprovider times decreased by nearly 50 percent, arrival-to-psychiatry consult times decreased by more than 60 percent, and overall ED length of stay for this patient group decreased by one-third. Importantly, there have been no patient elopements since the standardized intake process was launched. Safety risks such as ingestion were more reliably identified, with appropriate precautions implemented earlier in the patient’s ED course. The process also had added benefits in identification and safe disposition of other patients who lacked decision-making capacity, including those with undifferentiated encephalopathy and unaccompanied minors.
Staff reported greater efficiency, clarity of responsibilities and a stronger sense of both psychological and physical safety. Many noted that the dedicated space and team-based model reduced stress, improved communication and allowed them to focus more fully on patient care rather than environmental and workflow challenges.
Challenges and Next Steps
While the new workflow addressed many critical gaps, challenges remain. The administration of nonemergent psychotropic medications in the ED requires formal patient consent under state regulation, which can delay initiation of treatment. Work is ongoing to refine the consent process and ensure that patients receive timely access to appropriate medications. Further, the new BHI process required the dedication of nine ED care spaces to support the intake process and subsequent bedding of each patient, which has the potential to worsen crowding and boarding in other care areas. Additional efforts are focused on sustaining standardized practices, optimizing the patient flow for medium-risk cases and expanding staff education to reinforce safety and efficiency.
Conclusions
The implementation of a standardized BHI process in the LBJ ED has improved timeliness of evaluation, reduced length of stay, enhanced patient and staff safety and strengthened staff experience. By relocating intake to a dedicated pod, coordinating clinical and security teams and applying structured risk
stratification, the ED has created a more reliable and patient-centered process for behavioral health care.
This initiative underscores three major wins: standardization brought clarity to roles, responsibilities and actions; operational metrics such as length of stay and elopements improved; and patient and staff safety—including staff psychological safety—was strengthened. Relatively straightforward operational changes can have a profound impact not only on patient outcomes but also on staff well-being, retention and performance. We believe this model can be adapted by other institutions and hope to spark dialogue and collaboration as we continue refining the process and preparing for formal publication.
ABOUT THE AUTHORS



Dr. Gorlick is an assistant medical director of emergency medicine at Lyndon B. Johnson Hospital in the department of emergency medicine at UTHealth Houston.
Dr. Sharma is a vice chief of staff for quality at Lyndon B. Johnson Hospital and a vice chair of clinical affairs in the department of emergency medicine at UTHealth Houston.
Dr. Reynolds is a chief of service of emergency medicine at Lyndon B. Johnson Hospital in the department of emergency medicine at UTHealth Houston.
CAREER PATHWAYS

From Bench to Bedside: Careers in Emergency Medicine Innovation and Translational Research
By Sara Schulwolf, MD, on behalf of SAEM Residents and Medical Students (RAMS)
Innovation and translational research are reshaping the future of emergency medicine, bringing new ways to move discoveries from the laboratory to the bedside. To explore how these advances are opening career opportunities for trainees, Sara Schulwolf, MD, spoke with two leaders in the field. Dr. Christopher Kabrhel and Dr. Drew Birrenkott share their paths into research, insights on innovation, and advice for residents and medical students interested in charting their own careers in this rapidly evolving area of emergency medicine.

Christopher Kabrhel, MD, MPH, is an emergency physician and director of the Center for Vascular Emergencies at Massachusetts
General Hospital. His research focuses on the epidemiology, diagnosis, risk stratification, and treatment of venous thromboembolism. He leads a multidisciplinary team developing innovative approaches to diagnosis, risk stratification, and care delivery.

Dr. Drew Birrenkott
Drew Birrenkott, MD, DPhil, is an emergency physician and the inaugural fellow in clinical innovation and research translation in vascular emergencies at Mass General Brigham. He earned his doctorate in biomedical engineering with a focus on signal processing and machine learning and now uses proteomics to identify novel biomarkers for pulmonary embolism diagnosis.
Drs. Kabrhel and Birrenkott, please provide a brief primer on translational research and the integration of omics, big data, and artificial intelligence. How will this shape the future of emergency medicine practice?
Translational research moves scientific innovations from “bench to bedside.” The goal is to use basic
“Now my research omics and artificial of venous thromboembolism tests and treatments.”
research to design tests, devices, and drugs that improve clinical care. To be successful, researchers must consider the validity of the science, the clinical usefulness and usability of the test or treatment, and how it can be implemented into existing workflows, regulatory frameworks, and economic systems.
Innovations in omics, big data, and AI offer many opportunities for emergency physicians to participate in translational research. Historically, translational research meant moving a molecule or technology from the lab to the hospital. Now, we can
create predictive models using large data sets with complex omics and patient-level descriptors. This builds on decades of emergency medicine research in clinical decision rules. The growth of these fields will accelerate the process, and when models are implemented into workflows, they will improve patient outcomes.
Dr. Kabrhel, you’re best known for your work on VTE and creating decision tools to guide risk stratification of patients with potential PE. How did you become interested in this area?
During my ICU rotation in medical school, I learned why PE causes
research is coming full circle, as we use modern intelligence to explore the molecular basis thromboembolism and develop new diagnostic treatments.” — Dr. Christopher Kabrhel
hypoxia—which intuitively it shouldn’t, since it’s primarily a dead-space phenomenon. This sparked my interest in the molecular basis of PE, so as a resident I proposed a project to Dr. Sam Goldhaber, a renowned PE expert. My idea was comically ambitious, but Sam agreed to mentor me anyway—on a more realistic project.
We prospectively enrolled patients in the ED to validate the Wells score, which was new at the time. Shortly after, I was introduced to Jeff Kline, who had the idea for what would become the PERC rule. We combined our data, and my research career took off. Since then, I’ve worked on VTE epidemiology, diagnosis, risk stratification, and programs like PERT. Now my research is coming full circle, as we use modern omics and AI to explore the molecular basis of VTE and develop new diagnostic tests and treatments.
Dr. Birrenkott, how did you become interested in pursuing this career path? I became interested in translational
continued on Page 25

“My advice is that it is never too early to get involved. Everyone’s path is different, but as a student or resident you have the chance to try different opportunities.” — Dr. Drew Birrenkott
CAREER PATHWAYS
continued from Page 23
research during my biomedical engineering courses as an undergraduate. Many design classes assigned real-world problems and required a deliverable product or prototype by the end of the course. That meant collecting and analyzing data to compare the product to existing technology. I now think about how we can apply this model to challenges in emergency medicine.
As a specialty, we are still relatively young, but we have the unique ability to collect large amounts of high-quality clinical data at the time undifferentiated patients present with acute illness. Leveraging this data, along with the electronic health record, omics, and AI, I believe emergency physicians can become leaders in developing new acute diagnostics.
Dr. Birrenkott, as a student and resident, what steps did you take to pursue this field? What advice do you have for trainees?
To set myself up for success, I did three things. First, I sought opportunities to get involved at my institutions and within the emergency medicine community. I highly recommend engaging with SAEM. For example, as a resident, I participated in the 2024 omics consensus
conference, which allowed me to meet clinicians working in translational research.
Second, I sought out mentorship during medical school and residency. That network has been invaluable. Finally, I always looked ahead. Once I knew this was the work I wanted to do, I began talking with mentors about what my next steps should be after residency.
My advice is that it’s never too early to get involved. Everyone’s path is different, but as a student or resident you have the chance to try different opportunities. Talk to people doing innovative work at your institution and beyond. Find mentors and get involved. One of the reasons we wrote this article is to reach medical students and residents. If you’re not sure where to start, this is your invitation to reach out to us.
Dr. Birrenkott, you recently began a fellowship in clinical innovation and research translation. What does this fellowship offer trainees, and what expertise will graduates gain?
As the inaugural fellow, I can say this program offers opportunities beyond a traditional research fellowship. Typical research fellowships provide projects, grant writing education, a didactic curriculum, and often a degree program. Our fellowship includes those but adds skills for translating research into practice.
That includes collaborations with engineers, computer scientists, and computational biologists, plus access to innovation officers, intellectual property experts, industry partners, investors, and clinicians who have successfully translated their work.
The fellowship gives a survey of the innovation landscape and connects trainees with people who can guide the process of moving research from bench to bedside.
Drs. Kabrhel and Birrenkott, tell us about your current projects. What are you most excited about?
We’re especially excited about two projects. The first is the Automated Registry of Cardiovascular Emergencies (ARCVE), a collaborative registry with colleagues at Vanderbilt and other centers. ARCVE includes data on about 400,000 ED patients evaluated for possible PE, and it’s growing rapidly. We are using this registry to build predictive AI models for PE diagnosis and treatment.
The second area is high-throughput proteomics and metabolomics to improve PE diagnostics. These two data sources integrate well. For example, we can harmonize ARCVE’s clinical data with our proteomic data to enhance analysis.
Drs. Kabrhel and Birrenkott, your work relies heavily on interdisciplinary partnerships. What unique skills do EM physicians bring to the table?
Collaborating with experts from other fields is fun and energizing, but emergency physicians bring unique strengths. We care for patients with acute, undifferentiated illness. We have access to patients and samples, and we know firsthand how they present and what’s needed for rapid, accurate diagnosis. That’s why emergency physicians need to be at the forefront of this science.
ABOUT THE INTERVIEWER

Dr. Schulwolf is a resident physician at the Harvard Affiliated Emergency Medicine Residency at Mass General Brigham and a member-at-large on the SAEM RAMS Board.
CAREER PATHWAYS
From Residency to Leadership in Academic Emergency Medicine
By Mel Ebeling, MD, on behalf of the SAEM Membership Committee
The path to academic emergency medicine is rarely straightforward. For many physicians-in-training, it is shaped by moments of inspiration, strong mentorship, and opportunities to step into leadership roles. To explore how today’s residents are charting their careers — and how they are already shaping the field — Dr. Mel Ebeling spoke with three members of the SAEM Residents and Medical Students (RAMS) Board.

Lauren Diercks, MD, is a resident physician at Stanford University and secretarytreasurer on the SAEM-RAMS Board.

Juliet Jacobson, MD, is a resident physician at NewYorkPresbyterian/ Weill Cornell and Columbia University and a member-atlarge on the SAEM-RAMS Board.

Indrani Guzmán Das, MD, MPH, is a resident physician at Stanford University and a member-atlarge on the SAEMRAMS Board.
In the following conversation, they share their journeys into
emergency medicine, the mentors who shaped them, the challenges and opportunities of serving on the RAMS Board, and their advice for students and residents eager to grow in academic EM. Their stories highlight the importance of career development — building skills, seeking mentorship, and finding ways to contribute meaningfully to the profession while still in training. Why did you choose emergency medicine?
Dr. Diercks: “I grew up with my family serving on ski patrol. A pivotal moment came when a cardiac arrest happened on the slopes. My aunt, an accountant, performed CPR while I
Dr. Lauren Diercks
Dr. Juliet Jacobson
Dr. Indrani Guzmán Das
“Meeting people who do EM in different settings gave me perspective and made me more receptive to diverse viewpoints—all in the best interest of the patient.”
— Dr. Juliet Jacobson
kept the patient’s daughter away. He survived after being transported in a toboggan, receiving CPR and bagging en route, and being flown out. That inspired experience shaped my desire become a physician. Now, in full circle, I’m about to be a certified ski patroller at the same place my family served.”
Dr. Guzmán Das: “I chose emergency medicine because during medical school it was the one rotation where people were genuinely excited to teach and eager to involve me. My background in health economics and passion for health equity also drew me in, since the emergency department is often the access point for patients when cost or medical debt prevents them from seeing a primary care physician. Finally, I value the camaraderie—the team dynamic among physicians, nurses, techs, and clerks is unique and motivating.”
Dr. Jacobson: “I didn’t have an ‘aha’ moment. As a child, I considered careers from cleaning to being a chef before realizing I loved science. In a pre-med program, while others were terrified of the emergency department, I loved it. Hearing a code made me want to run toward it. In medical school, I struggled to choose a specialty, but emergency medicine combined everything I loved—I didn’t have to choose.”
Who has influenced your path in academic emergency medicine, and how did they shape your goals or leadership journey?
Dr. Diercks: “Although my aunt inspired me initially, my mother is an emergency medicine physician and
both an academic leader and strong clinician. My younger sister, who is applying to emergency medicine this year, also pushed me forward. She’s followed my path—from our sorority and major to medical school, and now EM. Knowing she looks to me pushes me to a thoughtful doctor and make good choices.”
Dr. Guzmán Das: “Dr. Giovanni Rodriguez, a former RAMS Board member, encouraged me to attend conferences, apply for opportunities, and not be discouraged by rejections. Her advice—to keep showing up— opened doors I hadn’t expected, and I pursued leadership in part by following her example.”
Dr. Jacobson: “My mentor, Dr. Mike DeFilippo, was on the RAMS Board when I was an intern. He encouraged me to apply for leadership positions. His support gave me the confidence to pursue these roles.”
How did you first get involved in SAEM or RAMS, and what drew you to it?
Dr. Diercks: “In my first year of medical school, I submitted an abstract to the virtual SAEM annual meeting during COVID-19. I later joined the SAEM Medical Student Ambassador program and discovered the RAMS Board. Even earlier, I knew I wanted to be a leader in EM, and SAEM aligned with my academic interests and my desire to be part of the broader EM community.”
Dr. Guzmán Das: “At Cornell, part of the New York Presbyterian network, I was surrounded by EM leaders, so academic EM was on my radar early. With encouragement from
mentors like Dr. Rodriguez, SAEM and RAMS became natural next steps for opportunities and leadership development.”
Dr. Jacobson: “There was no EM residency at my third-year rotation site, so I had to find my own mentors. I wish I had known about SAEM sooner. Once I discovered RAMS in residency, I loved it and wanted to strengthen its resources—especially the website’s accessibility for students.”
What has been the most meaningful RAMS project or initiative you’ve worked on, and what impact has it had on you and others?
Dr. Diercks: “One of our biggest challenges and most meaningful efforts as a Board was identifying our brand. At first, we weren’t sure how to connect with medical students across the country or what message to convey. Over time, we defined RAMS as the premier academic EM organization for students and residents—and our work now centers on delivering resources that reflect that identity.”
Dr. Guzmán Das: “Many of my projects focus on mentorship and career growth. I’ve worked on a podcast featuring advice from department chairs, developed jobsearch resources, and helped launch a mentorship program to connect RAMs with faculty at the SAEM annual meeting. These projects build stronger networks and support systems for our community.”
continued on Page 29
“There’s true camaraderie in the emergency department. Everyone— physicians, nurses, techs, clerks—plays this team sport.” — Dr. Guzmán Das

CAREER PATHWAYS
continued from Page 27
Dr. Jacobson: “Developing an EMIG curriculum and supporting students in tailoring it to their schools demonstrated to me how small contributions can have national impact and reinforced the value of sharing resources across programs.” What challenges have you faced during your time on the RAMS Board, and how have you worked through them while balancing other responsibilities?
Dr. Diercks: “When I first joined the Board, the challenge was clarifying our brand and learning how to communicate with medical students nationwide. Over time, we built a clear identity and developed strategies to connect meaningfully with students and residents.”
Dr. Jacobson: “Becoming chief resident and joining the RAMS Board at the same time was overwhelming, especially with a fellowship added during my fourth year. I learned to say ‘no,’ stay organized, and lean on my support system.”
Looking ahead, what excites you about the future of academic emergency medicine and RAMS, and what role do you see residents playing in shaping that future?
Dr. Diercks: “I hope RAMS strengthens its message to medical students and expands opportunities —publications, projects, or committee roles — that boost their resumes while advancing the specialty.”
Dr. Guzmán Das: “As digital natives, residents are uniquely positioned to harness new technologies in the ED. Artificial intelligence, for example, could help screen patients, simplify discharge instructions, and reduce jargon, freeing time for patient interaction and to address systemic challenges.”
What lessons, passions, or personal interests have helped ground you, and how do they influence the way you show up as a physician?
Dr. Diercks: “My mother and sister
remind me that my actions and decisions ripple beyond myself. Being a role model to my sister grounds me to stay thoughtful.”
Dr. Guzmán Das: “I joined a ceramics studio when I started residency, and it has taught me to accept failure gracefully. Hiking, time outdoors recharge me. Adopting a dog and that unconditional companionship, helps me separate work from personal life. These passions help me bring my best self to patients.”
Dr. Jacobson: “My biggest takeaway from RAMS has been learning from colleagues who are practicing in very different environments. It’s helped me appreciate the resources at my own institution and stay open to diverse perspectives. That mindset has grounded me in both clinical practice and collaboration.”
What advice would you give to residents or students interested in academic emergency medicine or RAMS?
Dr. Diercks: “Build connections with colleagues during your off-service rotations. You’ll be working with many of them later as consultants, and it’s much easier when you already recognize familiar faces across the hospital.”
Dr. Guzmán Das: “My advice is simple: apply and get involved. Even if you don’t see leaders who remind you of yourself, your perspective is valuable and welcome. Don’t underestimate what you bring to the table.”
Dr. Jacobson: “Be open to anything. In EM, you must be comfortable with everything, but you can still carve out your niche. SAEM academies and interest groups are great places to meet people with similar interests and find projects to join.”
ABOUT THE AUTHOR

Dr. Ebeling is an emergency medicine resident physician at the University of Cincinnati and RAMS Board Member-At-Large
EDUCATION & TRAINING

Shaping the Future of Emergency Medicine Training: Inside the ACGME’s Proposed Revisions
By Daniel Artiga, MD; Mel Ebeling MD; Carlisle Topping; Lauren Querin, MD, MEd; and Adebisi Adeyeye, MBBS, MSc, on behalf of SAEM Residents and Medical Students (RAMS)
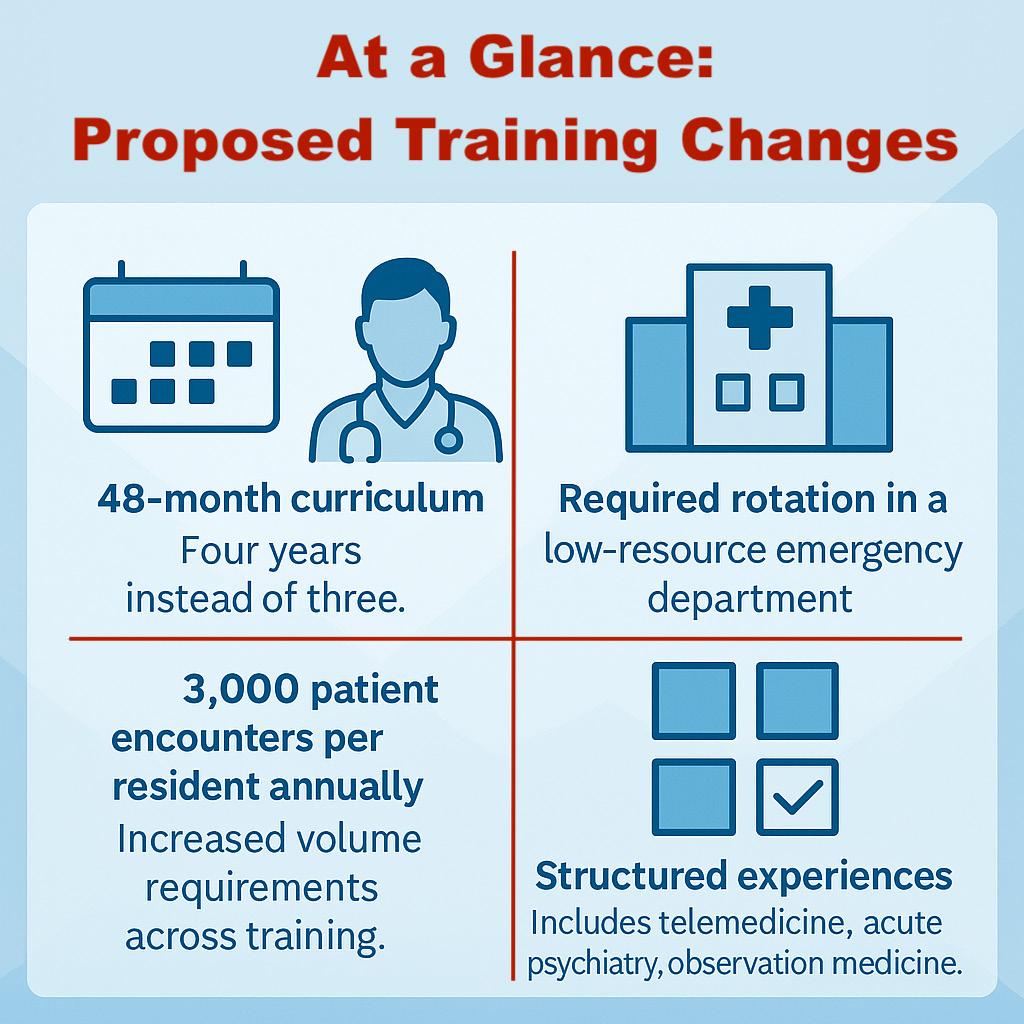
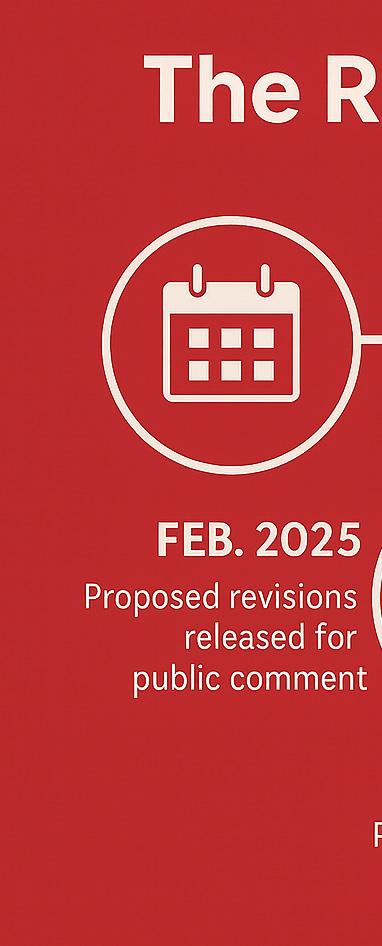
In February 2025, the Accreditation Council for Graduate Medical Education (ACGME) proposed major revisions to the emergency medicine (EM) residency program requirements, sparking dialogue and debate within the specialty. The proposed revisions include a new 48-month curriculum, an aggregate annual volume per resident of 3,000 patient encounters, and the addition of a required rotation in a lowresource emergency department,
among other changes. If approved, the revisions would take effect no earlier than July 1, 2027.
To appreciate the significance of the proposal, it is important to understand the ACGME’s process for revising specialty-specific program requirements. This article outlines that process, the key stakeholders, how the proposed revisions were developed, and what to expect in the coming months.
Why Now?
The ACGME reviews specialtyspecific program requirements at the least every 10 years, following a standardized process that engages multiple stakeholders. These periodic reviews aim to advance medical education and prepare physicians to meet evolving patient and system needs.
The proposed EM program requirement revisions are not
“The proposed revisions include a new 48-month curriculum, an aggregate annual volume per resident of 3,000 patient encounters, and the addition of a required rotation in a lowresource emergency department, among other changes.”
intended as a critique of existing programs, a means of influencing workforce distribution, or a strategy to diminish smaller programs or contract management groups. Rather, they are part of the ACGME’s routine review cycle and were shaped by feedback and insights from within the EM community.
Who Makes the Changes?
Four ACGME entities are involved in the development and approval of EM program requirements:
Emergency Medicine Program
Requirements Writing Group (PRWG)
Includes eight EM attending physicians, one EM resident physician, two public members, and nine ACGME staff, including three from the Review Committee (RC). The PRWG led the multi-stage process of drafting the proposed revisions.
Emergency Medicine Review Committee (RC)
Composed of 13 members: 11 nominated by the American Board of Emergency Medicine (ABEM), American College of Emergency Physicians (ACEP), American Medical Association (AMA), and American Osteopathic Association (AOA); one resident member; and one public member. Members include past EM society presidents, national conference leaders, and nearly all are current or former program directors or designated institutional officials. The RC reviews the proposed revisions before they are sent forward. Current members of the RC can be viewed here. Selection criteria can be found here
Committee on Requirements (CoR)
A committee appointed by the ACGME Board of Directors The CoR reviews proposals from the RC and ensures revisions align with the ACGME mission before forwarding recommendations.
ACGME Board of Directors
Composed of 24 members nominated by seven member organizations, along with resident physicians, public directors, at-large directors, and other
appointed representatives. The Board is the final approving body for all program requirements. The current ACGME Board can be viewed here
Revision Timeline
Since 2023, the Program
Requirements Writing Group (PRWG) has gathered input through a strategic planning session, stakeholder summit, and program director survey. The
continued on Page 32
continued from Page 31
proposal was posted for public comment in February 2025, with final approval by the ACGME Board expected in February 2026 and implementation no earlier than July 2027.
How the Proposed Revisions Were Developed
The ACGME piloted its forwardlooking revision model in internal medicine (2018) and general surgery (2022) Emergency medicine adopted a similar process, beginning with the PRWG.
Strategic Planning
The PRWG held a four-day strategic planning session with an external facilitator. The group reviewed evidence, procedural competencies, resident workload, and the evolving scope of EM practice. They also conducted interviews with EM leaders, program directors, and recent graduates in both community and academic settings to ensure perspectives were broad.
Stakeholder Summit
A stakeholder summit followed, bringing together representatives from societies including SAEM, Association of Academic Chairs of Emergency Medicine (AACEM), Council of Emergency Medicine Residency Directors (CORD), ACEP, American College of Osteopathic Emergency Physicians (ACOEP), American Academy of Emergency Medicine (AAEM), Emergency Medicine Residents’ Association (EMRA), Residents and Students Association of the American Academy of Emergency Medicine (RSA), ABEM, and the American Osteopathic Board of Emergency Medicine (AOBEM), along with the RC past chair and two recent graduates. Participants were asked: “What training will emergency physicians need to practice effectively in 2050?”
Key Insights
Themes included inefficiencies in patient care (low patient volume
per hour), limited understanding of administration (billing and coding, quality assurance), and declining competency with common loweracuity procedures (e.g., suturing, incision and drainage, fracture reduction). The need for stronger training in pediatrics was identified, along with an expanded focus in addiction medicine, EMS, obstetrics/ gynecology, toxicology, point-of-care ultrasound, telemedicine, observation medicine, and transitions of care.
Taken together, these insights highlighted the need to prepare emergency medicine residents not only as skilled clinicians but also as leaders capable of working within complex, multidisciplinary health systems. This perspective shaped a new vision of the future emergency physician and guided the development of the core competencies and curriculum elements. The result was a de novo curriculum designed not on existing structures, but on consensus around the competencies required for future EM physicians.
Curriculum Highlights
The new curriculum includes traditional rotations, structured experiences, and procedural competency expectations. The PRWG also emphasized the need for diverse clinical exposure across varying acuity levels and resource environments, while accounting for the number of patient encounters in the ED and the ICU
“Structured experiences” are distinct educational activities that may not require a minimum block rotation but provide essential exposure. Nine were identified, including acute psychiatry, airway management, non-laboratory diagnostics, observation medicine, ophthalmology, sensitive examinations, primary decisionmaking within multidisciplinary teams, telemedicine, and transfers/ transitions of care.
Surveying Program Directors
To ensure the curriculum revisions reflected the broader EM community, the PRWG surveyed
289 emergency medicine program directors, achieving a 60% response. Results closely aligned with the curriculum the PRWG had developed independently, confirming similar priorities and elements.
At CORD 2025, some directors raised concerns about how survey results would be used. The survey introduction explained that responses were intended to inform the development of new program requirements, not to affect program accreditation decisions. That language was meant to reassure directors but instead caused confusion, with some questioning whether their input would actually
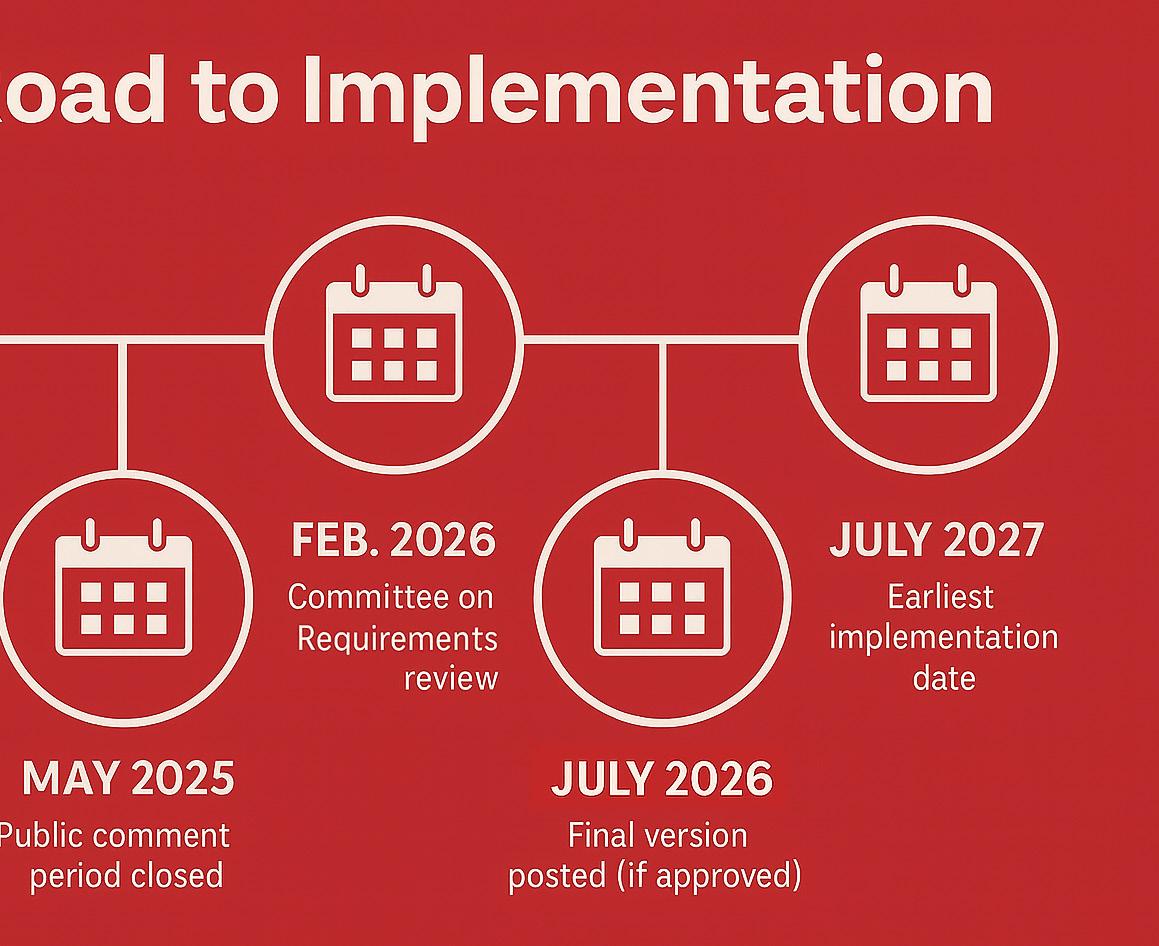
influence the revisions to the program requirements. In fact, the survey was explicitly designed to guide the revision process.
Drawing together findings from the strategic planning session, stakeholder summit, and program director survey, the PRWG finalized its draft of the proposed revisions to the EM program requirements. The ACGME program requirement revision process are described here and EMspecific changes here ACGME has also discussed the process at the 2025 ACGME Annual Educational Conference, ACGME webinar, CORD Academic Assembly 2025, and AACEM Annual Retreat 2025.
Three vs. Four Years
The most debated aspect of the proposed curriculum is its four-year structure. Importantly, this should not be viewed as criticism of existing three-year programs. Members of both the PRWG and RC have acknowledged the literature showing that current three-year and four-year EM residencies produce similar clinical outcomes and performance measures. Within the RC itself, members are evenly split between leaders from three-year and four-year programs.
Historically, both formats have followed the same curricular requirements, with four-year programs
required to provide an additional rationale for the extended time. Regardless of length, the goal has always been the same: to graduate competent, practice-ready emergency physicians. The new curriculum, however, is a comprehensive redesign that will require modifications for all programs.
To avoid bias, the EM program director survey did not ask directly about ideal program length. Prior research shows respondents often favor the format in which they trained. Instead, directors were asked to design the curriculum
on Page 34
“With
advocacy from the American College of Emergency
Centers for Medicare and Medicaid Services agreed to recognize
Initial Residency Period for emergency medicine beginning
EDUCATION & TRAINING continued from Page 33
element by element. Of the 179 respondents, 80% represented threeyear programs and 20% four-year programs. Results supported the PRWG’s proposed elements and indicated that the ideal program length exceeded 41.5 months. At ACEP 2025, the RC noted that it explored the possibility of a 42-month curriculum, but the ACGME requires residency training to be structured in 12-month increments.
Another concern was patient volume. Internal ACGME analysis suggested that many three-year programs would fall short of the proposed threshold of 3,000 patient encounters per resident. Data showed that all but seven threeyear programs would be above that benchmark.
After reviewing these issues and finalizing the new curriculum design, the PRWG concluded that a four-year structure was necessary to achieve the training objectives. Both the PRWG and RC, however, have acknowledged at CORD 2025, SAEM 2025, and ACEP 2025 that there is no direct evidence supporting this entirely new model, since it represents a forward-looking redesign rather than a refinement of existing structures
Financing Four-Year Programs
Another major question is how four-year emergency medicine programs will be financed. The issue
is complex, as funding depends on Medicare’s Graduate Medical Education (GME) payment structure. GME funding rests on three key mechanisms: the Initial Residency Period (IRP), full-time equivalent (FTE) calculations, and two funding streams—Direct Graduate Medical Education (DGME) and Indirect Medical Education (IME). The IRP sets the number of years Medicare pays 100% DGME support for each resident. IME payments are provided across all years of training and are meant to offset indirect costs of clinical education, such as treating more complex patients and maintaining additional hospital resources.
Historically, emergency medicine’s IRP has been three years. As a result, four-year programs received full IME funding for all four years, full DGME for the first three years, and only 50% DGME in the fourth. Because IME makes up about two-thirds of total funding, this structure provided roughly 96% of full financial support. With advocacy from ACEP, the Centers for Medicare and Medicaid Services (CMS) agreed to recognize a four-year IRP for emergency medicine beginning July 1, 2027. This means programs will receive 100% DGME and 100% IME funding for residents in all four years. Combined programs (such as EM–Internal Medicine) may require further discussion to align funding across specialties.
A program’s ability to realize this funding still depends on its
institutional cap, which limits the number of residents eligible for full reimbursement. Caps are institutionspecific, set by the Balanced Budget Act of 1997, and generally cannot be increased unless a new teaching hospital is created. Institutions under cap will be able to expand resident classes and receive full funding for the additional fourth year. Institutions already at or above cap, however, cannot receive full reimbursement for added residents, regardless of program length. This makes the transition from threeto four-year format financially challenging for some three-year programs that wish to expand while maintaining class sizes. Program leaders will need to assess their institution’s cap status and residentto-bed ratios before deciding on expansion.
For more details, see the GME Financing session presented by RC members at CORD 2025.
SAEM and RAMS Perspectives
SAEM and RAMS quickly reviewed the ACGME’s proposed program requirement revisions. During the public comment period ending in May, SAEM, RAMS, AACEM, and the SAEM Clerkship Directors in Emergency Medicine academy submitted a joint statement to the ACGME outlining their position and highlighting areas of concern. In addition, SAEM’s Academy of Emergency Ultrasound co-signed a multi-society statement addressing revisions related to point-of-care ultrasound.
Emergency Physicians, the
recognize a four-year beginning July 1, 2027.”
At the SAEM annual meeting, the ACGME Review Committee participated in an open forum to answer questions and clarify the review timeline for public comments. Much of the information in this article was shared during that session.
In August, SAEM, RAMS, and partner emergency medicine societies issued a Joint Response on ACGME Program Requirements, reaffirming their shared values and commitment to advancing the academic mission of emergency medicine.
Current Status in the Approval Process
At SAEM 2025, the RC reported that more than 2,000 comments were submitted during the public comment period in response to the PRWG’s proposed program requirement revisions. These comments will not be made public.
The RC will review each comment, looking for key issues and recurring themes to guide potential changes. If the proposed revisions are substantial, the proposal must return for another round of public comment.
After completing its review, the RC will forward the revised proposal to the Committee on Requirements (CoR), along with all comments received and the RC’s responses. For each comment, the RC must indicate whether the suggestion was incorporated and provide a rationale if it was not.
The CoR will then conduct its own independent review of the revisions, comments, and responses. Only after
the CoR endorses the proposal will it be sent to the ACGME Board of Directors for final approval.
The ACGME Board is expected to consider the proposal in February 2026. If approved, the new Common Program Requirements will be shared with the EM community via the ACGME website and an electronic communication and posted publicly in July 2026.
Implementation Plan
If approved, the ACGME Board will set the date when the revised program requirements take effect. Historically, the Board has allowed programs and institutions enough lead time to adapt, and it will consider the RC’s recommendation on timing.
The earliest possible implementation date is July 2027. This would affect today’s second-year medical students, who would enter residency under the new four-year structure. Residents beginning in July 2026 or earlier would be allowed to graduate from existing three-year programs. It is still unclear whether current residents would need to meet some of the additional new requirements.
At ACEP 2025, the RC emphasized that adoption of the new requirements indicates movement toward compliance but does not mean immediate full enforcement. A phased rollout is planned, similar to the gradual transition used when AOA-accredited programs joined the ACGME single accreditation system. Details of this implementation plan will be finalized and released after the Board approves the revisions.
Concerns remain about how strictly the new rules will be enforced and how long programs might extend the transition period. Another issue is the potential for a temporary graduation gap, since some programs may transition later than others. However, a phased rollout should help reduce disruption by preventing all programs from shifting formats at the same time.
Looking Ahead
Whether you are an experienced
attending physician or a new medical student just beginning your path, SAEM and RAMS are prepared to support you. The landscape of medical education and practice continues to evolve, and our community must navigate these changes together.
SAEM and RAMS are committed to providing resources, guidance, and opportunities for discussion to ensure a smooth transition and to maintain excellence in training academic emergency medicine physicians. The ACGME has also indicated that it will release additional support for programs during the transition, including guidance on class sizes, funding mechanisms, structural adjustments, and best practices for curriculum design, structured experiences, and procedural training.
ABOUT THE AUTHORS





Dr. Artiga is a resident physician at the University of Cincinnati and president of SAEM Residents and Medical Students (RAMS).
Dr. Ebeling is a resident physician at the University of Cincinnati and board member-at-large for SAEM RAMS. Carlisle Topping is a fourthyear medical student at Yale University and a medical student representative for RAMS.
Dr. Querin is an assistant professor of emergency medicine and residency advising director for emergency medicine at Mayo Clinic Arizona.
Dr. Adeyeye is a first-year emergency medicine resident at Mayo Clinic in Rochester and serves as the medical student and resident representative for the SAEM Global Emergency Medicine Academy.
EDUCATION & TRAINING

Level Up Your Feedback Game: Practical Tips for On-Shift Feedback in the ED
By Kathryn Ritter, MD, MEHP, and Sean McCormick, MD, on behalf of the SAEM Education Committee
In an academic emergency department, we may work with a variety of learners on every shift. It is crucial to provide feedback in order to support their continued growth. However, there is often a disconnect: residents and students hope to receive more feedback than they actually do when working clinical shifts. As educators, how can we successfully fulfill our responsibility to provide high-quality feedback within the constraints of a busy clinical setting?
Characteristics of High-Quality Feedback
We must strive to maximize these characteristics of high-quality feedback:
1. Timely: Feedback should be given in real time whenever possible. This allows learners to immediately apply what they have learned to their next patient or shift. When feedback is delayed, it can be difficult for both learners and educators to remember the details.
2. Specific: Effective feedback must be precise enough for trainees to understand exactly what is being communicated. Vague generalities do not foster meaningful growth. Instead, we should discuss specific examples of observed behaviors. To reduce implicit bias, focus on directly observed behaviors rather than personality traits.
3. Balanced: Feedback should include both reinforcement and constructive points. Focusing only on reinforcing feedback may fail to push learners toward advancing their practice. Conversely, solely offering constructive feedback may make learners less receptive. Striking a balance is key.
4. Actionable: Learners should be able to incorporate feedback into their individualized learning plans. Reflect with the learner on observations and collaborate to map out specific steps for progress.
When to Give Feedback
Feedback is most effective when the learner is ready to receive it.
“Feedback should be given in real time whenever possible. This allows learners to immediately apply what they have learned to their next patient or shift.”
However, the emergency department requires vigilance and multitasking, making timing tricky. Waiting until the end of a shift may mean the learner is mentally exhausted and unable to fully absorb the discussion. Consider preset times, such as midshift or before stopping to pick up new patients. Positive feedback is often best delivered in the moment, while constructive feedback may be more effective in a protected, private space Night shifts may also offer opportunities for more in-depth discussions.
Where to Give Feedback
The Council of Residency Directors in Emergency Medicine recommends a non-threatening, supportive environment. While finding privacy in a busy emergency department can be difficult, even small efforts matter. A hallway, empty patient room, or resuscitation bay can provide partial seclusion when an office is unavailable.
Help Residents Be FeedbackSeeking
Research shows residents sometimes seek or avoid feedback. They are more likely to seek feedback from attending physicians they respect, who are in a good mood, or who share similar practice styles. They may avoid asking for feedback after difficult shifts or from attendings they perceive differently. As educators, we should recognize these dynamics and take the initiative to start the conversation. Consider Learners’ Feedback Receptivity
As clinical educators, we must acknowledge how our learners’ receptivity to feedback can impact the effectiveness of our feedback
discussions. We must be aware that they may not want feedback in the same way as previous generations. Current students and residents are more comfortable with technology than ever before, and they may prefer electronic feedback. In addition, it is important to consider how certain feedback triggers may cause a learner to tune out of the remainder of a feedback conversation if you unintentionally strike a chord with one of these.
As clinical educators, we must recognize that learners’ receptivity to feedback directly affects its impact. Today’s students and residents may not want feedback delivered in the same way as previous generations. Many are more comfortable with technology and may prefer electronic feedback.
It is also important to consider how certain “feedback triggers” can cause a learner to disengage. For instance, feedback may unintentionally threaten a core element of a learner’s self-identity—known as an identity trigger—even when this is not the intent. A learner who sees themselves as a compassionate communicator, for example, may feel threatened if a supervisor offers constructive feedback on how they delivered bad news to a patient and family.
This underscores the importance of providing behavior-based feedback rather than comments about personality traits or characteristics.
Finding Your Feedback Flow
Incorporating feedback strategies into clinical practice may feel challenging at first, given the many competing demands of an emergency department. With practice, however,

you will develop a feedback flow. The feedback you provide is key to your learners’ growth, and the time invested is a worthwhile contribution to the future of our specialty
ABOUT THE AUTHORS


Dr. Ritter is an associate program director for the emergency medicine residency and assistant director for the medical education fellowship at the Johns Hopkins University School of Medicine.
Dr. McCormick is an assistant program director for the emergency medicine residency at Wayne State University School of Medicine Detroit Receiving Hospital.
EDUCATION & TRAINING

From Training to Triage: Preparing EDs to Care for Pregnant and Postpartum Patients
By Pavitra Kotini-Shah, MD; Nazra Zafar; Stacie Geller, PhD; Lauren Sayah, MPH; Emilie Glass, MA; and Katherine Craemer, MPH
Introduction
Inside a busy Illinois hospital emergency department (ED) without in-house obstetric services, a clinician evaluates a patient who presents three days postpartum with heavy vaginal bleeding and dizziness. Recognizing the symptoms as postpartum hemorrhage — often life-threatening — the clinician must rely on their own expertise to stabilize the patient and coordinate a safe transfer to an obstetric facility.
This scenario is increasingly common in EDs across the United States. Each year, more than 2.7 million pregnant patients visit an ED, and one in four postpartum
patients seek care there within six months of giving birth. As birthing and non-birthing hospitals close and access to obstetric care dwindles, the ED often becomes the only place pregnant and postpartum patients can receive care
Although obstetric care is not the primary role of the ED, providing training and resources offers an opportunity to improve maternal health outcomes. More than 60,000 women in the U.S. experience severe maternal morbidity (SMM) annually, resulting in more than 700 pregnancy-related deaths
In Massachusetts, high ED use during pregnancy was linked to an increased risk of SMM, with many
patients visiting multiple EDs. According to the Illinois Maternal Mortality Review Committees’ (MMRCs), 66% of Illinois residents who died from pregnancy-related causes had at least one ED visit before death, most with three or more. In rural Illinois, that number rose to 90%.
These findings highlight an urgent reality: EDs are increasingly providing obstetric care, and their role will only grow. In 2023, more than 5.5 million women lived in U.S. counties with limited or no maternity care For many, the ED serves as the primary access point for perinatal care, despite not being designed or staffed for that purpose.
“Each year, more than 2.7 million pregnant patients visit an emergency department, and 1 in 4 postpartum patients seek care there within six months of giving birth.”
Inside the Toolkit: FrontlineDelivered Training
The Maternal Health Emergency Department Toolkit was created to prepare ED providers for pregnant and postpartum patients. Developed by the Center for Research on Women and Gender at the University of Illinois Chicago College of Medicine, this free
training arose in response to Illinois MMRC findings.
A multidisciplinary task force of nurses, physicians, researchers, and experts in maternal health, mental health, emergency medicine, hospital policy, and social work designed the training with the realities of ED practice in mind.
The self-paced toolkit accommodates hospitals regardless of geographic location or obstetric resources. It also aligns with quality improvement objectives and national clinical competencies set by the Illinois Department of Public Health, the Centers
continued on Page 41
Figure 1. Pregnant and Postpartum Patient Care in the Emergency Department, Aggregate Pre- and Post-Pilot Study.
Obstetrics Care

continued from Page 39
for Disease Control and Prevention, American College of Obstetricians and Gynecologists, and Center for Medicare and Medicaid Services.
The five educational modules combine didactic content, casebased learning, and implementation resources. They focus on data from the Illinois MMRCs, triage and management of emergencies in perinatal patients, screening and treatment of mental health and substance use disorders, addressing trauma, resuscitation during pregnancy, and coordinated discharge of perinatal patients from the ED. The modules include:
• Module A: Introduction to Maternal Mortality: How Emergency Departments Can Help
• Module B: Acuity Assessment and Management of Perinatal Emergencies —Includes interactive case studies on sepsis, hemorrhage, pulmonary embolism, hypertensive disorders, and ectopic pregnancy
• Module C: Screening and Treatment for Perinatal Mental Health and Substance Use Disorders in the ED
• Module D: Trauma and Resuscitation in Pregnancy
• Module E: Best Practices for Discharge of Pregnant and Postpartum Patients from the ED
Outcomes of the Pilot Study:
Implementing Change Through Practice
Between 2023 and 2024, six Illinois hospitals piloted the toolkit. Using
electronic medical record data before and after implementation, these hospitals showed measurable improvements in practice:
• Documentation of pregnancy or postpartum status among female patients of reproductive age increased from 56.4% to 83.4%.
• Screening for mental health conditions or substance use disorders increased from 52.2% to 69.6%.
• Communication between ED and obstetric providers rose from 30.1% to 56.4%.
• Referrals to obstetric providers increased from 43.2% to 56.8%.
These changes occurred across hospitals regardless of geography or availability of obstetric care, underscoring the toolkit’s versatility and effectiveness.
Real-World Impact and The Road Ahead
As more pregnant and postpartum patients rely on EDs, the Maternal Health Emergency Department Toolkit provides critical, evidence-based resources to improve triage, manage complications, address behavioral health and substance use disorders, perform trauma resuscitation, and support safe discharge.
While the toolkit cannot close systemic gaps in maternity care, it equips emergency clinicians with the knowledge and tools to strengthen maternal care when patients engage with the ED.
The toolkit is now available at all 188 Illinois EDs, is being adapted
in Massachusetts, and has been shared with more than a dozen states. Results from these broader implementations are forthcoming, and the learning modules remain available by request.
For more information, visit the UIC College of Medicine Center for Research on Women and Gender
This work was supported by the Illinois Department of Public Health Maternal and Child Health Title V Block Grant, work order #36300007K.
ABOUT THE AUTHORS

Dr. Kotini-Shah is an associate professor of emergency medicine, director of research strategy and innovation in the department of emergency medicine, and director of emergency ultrasound research in the division of emergency ultrasound at the University of Illinois Chicago. Nazra Zafar is an undergraduate student at the University of Illinois Chicago College of Liberal Arts and Sciences Honors College majoring in integrated health studies and biological sciences.



Dr. Geller is the G. William Arends professor of obstetrics and gynecology and director of the Center for Research on Women and Gender at the University of Illinois Chicago College of Medicine.
Lauren Sayah is a senior research specialist at the Center for Research on Women and Gender at the University of Illinois Chicago College of Medicine.
“More than 60,000 women in the United States experience severe maternal morbidity annually, resulting in more than 700 pregnancy-related deaths.”


Emilie Glass is a senior research specialist at the Center for Research on Women and Gender at the University of Illinois Chicago College of Medicine.
Katherine Craemer is a senior research specialist at the Center for Research on Women and Gender at the University of Illinois Chicago College of Medicine.
EDUCATION & TRAINING

Why Oncologic Emergency Medicine Education Matters—and How to Integrate It Throughout Medical Training
By Caleigh Donnelly; Greg Chang, MD; Kelsey Harper, MD; and Monica K. Wattana, MD, on behalf of the SAEM Oncologic Emergencies Interest Group
The Urgency of Oncologic Emergencies in the ED
Case 1: A 49-year-old man with diabetes presents to the emergency department with low-grade fever, fatigue, and blood-streaked sputum. His vital signs show tachycardia. Laboratory testing reveals a white blood cell count of 56,000, and a chest X-ray shows diffuse bilateral opacities. He is admitted with a working diagnosis of sepsis secondary to pneumonia and treated with antibiotics. Two days later, he dies of diffuse alveolar hemorrhage caused by disseminated intravascular coagulation secondary to newly diagnosed acute myeloid leukemia.
Case 2: A 60-year-old woman with lung cancer undergoing treatment
with pembrolizumab presents to the emergency department with diarrhea and low-grade fever. A CT scan of the abdomen and pelvis demonstrates mild colitis, thought to be either inflammatory or infectious in origin. She is treated symptomatically with loperamide and discharged home. One week later, she dies from bowel perforation.
These cases illustrate the critical need for rapid recognition and treatment of oncologic emergencies in the emergency department. While emergency physicians may not provide longitudinal cancer care, they are often the first clinicians to evaluate patients experiencing oncologic crises. Emergency physicians must recognize these life-threatening
conditions, initiate time-sensitive interventions, and engage oncologists and other specialists quickly.
The Growing Burden of Cancer in Emergency Care
Cancer incidence continues to rise, with more than 2 million new cases projected in the United States in 2025. As cancer treatments expand and more patients live longer with cancer, oncologic emergencies— such as neutropenic fever, spinal cord compression, tumor lysis syndrome, blast crisis, and adverse effects of immunotherapy—are becoming increasingly common in emergency medicine practice.
Despite this growing need, oncologic emergency medicine
“Emergency physicians must recognize these life-threatening conditions, initiate time-sensitive interventions, and engage oncologists and other specialists quickly.”
remains underrepresented in medical education. Addressing this educational gap requires integration of oncologic emergency medicine into both medical school and residency curricula.
Building Awareness in Medical School
Preclinical medical school curricula should introduce the recognition and management of oncologic emergencies. This can be achieved by incorporating lectures within hematology/oncology courses dedicated to emergent pathologies and how they differ in patients with and without cancer.
At a national level, licensing exams such as the United States Medical Licensing Examination (USMLE) should include oncologic emergencies as a core competency—similar to how neurologic and cardiac emergencies are emphasized.
During the clinical years, opportunities for medical students to participate in hematology/oncology rotations are essential. Regardless of specialty choice, all physicians must understand the fundamentals of oncologic care and emergencies as the population of patients with cancer continues to grow. Core rotations in hematology/oncology should be required in all medical schools.
With the USMLE Step 1 now pass/ fail and many schools shortening preclinical education, students often
have additional time during clinical years to explore specialties. This flexibility offers an opportunity for more robust hematology/oncology rotations and hands-on experience with oncologic pathology and emergencies.
Exposure to oncologic care can also be expanded during internal medicine and emergency medicine rotations. For example, students may benefit from attending interdisciplinary grand rounds, tumor boards, and other multidisciplinary discussions. Early exposure builds awareness of common oncologic conditions and enhances understanding of complex clinical decision-making in cancer care.
Advancing Competency in Residency
Oncologic emergency medicine education should continue throughout residency training. Many emergency medicine programs hold weekly educational conferences that include lectures, case discussions, and simulation sessions. These can serve as platforms to integrate oncologic emergency medicine content across all training years.
Emergency medicine residents should master recognition and management of common oncologic emergencies such as tumor lysis syndrome and febrile neutropenia, as well as adverse effects of modern therapies, including immune
checkpoint inhibitors and chimeric antigen receptor (CAR) T-cell therapy.
As oncologic emergencies become more frequent, the development of an oncology–emergency medicine subspecialty or fellowship could help train physicians with a focused interest in this area. This would allow emergency physicians to better meet the complex needs of an expanding oncologic patient population.
The Path Forward
Innovation and adaptation are hallmarks of emergency medicine. Just as ultrasound has become an essential skill through deliberate integration into training, so too should the recognition and management of oncologic emergencies.
Integrating oncologic emergency medicine education at every level— medical school, residency, and beyond—will ensure that future emergency physicians are equipped to care for the growing number of patients with cancer who depend on the emergency department for timely, life-saving care.
ABOUT THE AUTHORS



Caleigh Donnelly is a medical student at the California University of Science and Medicine, Class of 2028.
Dr. Chang is an assistant attending in emergency care services at Memorial Sloan Kettering Cancer Center.
Dr. Harper is a fourth-year emergency medicine resident at the Warren Alpert Medical School of Brown University.
Dr. Wattana is an associate professor and director of education in the department of emergency medicine at MD Anderson Cancer Center.

When Patients Cannot Decide: Navigating Surrogate Decision-Making in the ED
By Justine McGiboney, MD, on behalf of the SAEM Ethics Committee
Case Presentation
A 73-year-old man with a history of severe COPD requiring four ICU stays this calendar year presents to the emergency department (ED) with acute on chronic hypercapnic respiratory failure. His respiratory status declines despite BiPAP, and his ED physician worries that he may require intubation. The patient’s mental status currently precludes his ability to consent for intubation or share his wishes for his medical care.
His girlfriend of 20 years and his daughter arrive at bedside; he has no other children. His girlfriend requests
that the team do everything possible to save his life, while his daughter shares that he has been through “a lot” in the past year and wouldn’t want to continue living like this. Who is the legally appropriate person to help the ED physician guide the next steps in this patient’s care?
Autonomy, Competence, and Capacity
The ethical principle of autonomy underpins the process of medical decision-making. Autonomy reflects the value that all persons have intrinsic worth and should therefore be allowed to make their own choices concerning their body
and medical care. Autonomy does not extend to persons unable to act autonomously—obvious examples being infants and small children. But what about adult patients with mental or physical disorders limiting their ability to make decisions for themselves?
Here, it is helpful to briefly distinguish between the legal term competence and the medical term capacity. Competence is a legal determination; namely, all patients are considered competent to make their own medical decisions unless a court has declared otherwise. Capacity, on the other hand, is
assessed clinically on a decision-bydecision basis.
A patient is assessed to lack decisional capacity if he or she cannot understand the nature, alternatives, and risks and benefits of a proposed intervention. Importantly, capacity is assessed at a particular point in time and is decision-specific. For example, a patient may not have capacity to weigh the risks and benefits of an operation, but he may retain capacity to choose among lunch options from the hospital cafeteria. Even when a surrogate decision-maker is ultimately required, physicians should engage patients whose capacity is impaired in decisions involving their own care to the greatest extent possible.
The Legal Surrogate Hierarchy
In cases where a patient is clinically assessed to lack decisional capacity, the medical team must engage a surrogate for decision-making. The legal hierarchy for determining the appropriate medical decision-maker varies by state. However, there is a general common order to the hierarchy, as follows:
1. Designated health care power of attorney
2. Spouse (unless divorced or legally separated)
3. Adult children
4. Parents
5. Adult siblings
6. Adult grandchildren
A growing number of states additionally allow for close friends to
serve as surrogates when relatives are unable to do so. Although usually at the bottom of the hierarchy list, the growing inclusion of distant relatives and close friends helps accommodate nontraditional family structures.
Consensus, Judgment, and Best Interests
State-by-state differences primarily arise in the nuances. For example, if a patient’s adult children are approached for surrogate decisionmaking, state laws vary if the children must all agree (consensus decision) or if a majority decision is acceptable.
Regardless of who ultimately makes the legal decision, it is generally best practice to update and engage all present family, especially in cases of disagreement, to show respect and support during an emotionally trying time.
Appropriate surrogates should make decisions for the patient based not on what they themselves would select, but on what the patient would select if able (substituted judgment standard). In cases where the patient’s interests are not known, surrogates should weigh risks and benefits to determine which choice would likely best serve the patient’s interests (best interests standard).
A glance around a typical Thanksgiving table demonstrates that families are complex, and in some cases, identification of the legally appropriate surrogate decisionmaker is not always possible—or
Key Takeaways
• Autonomy is central to ethical decision-making but does not apply when a patient lacks capacity.
• Competence is a legal concept; capacity is a clinical assessment made per decision and per moment.
• Health care power of attorney and state hierarchy laws determine who can act as a surrogate.
• Surrogates should use substituted judgment or, when unknown, the best interests standard.
• Consult the ethics committee when surrogate identity or decisionmaking is unclear.
always enough. In cases where an appropriate surrogate cannot be identified or where the legally appropriate surrogate is unable to make decisions using substituted judgment or the best interest standard, it is reasonable to consult the hospital ethics committee for assistance and clarity.
Application to the Case
Applying these general principles to our case at hand, the ED physician correctly assesses that the patient does not currently have capacity to engage in medical decisionmaking. The patient does not have a documented health care power of attorney, making it necessary to engage a surrogate decision-maker.
Although the patient is in a longterm committed relationship, he is legally unmarried and his girlfriend is thus considered a close friend on the surrogate hierarchy scale. In the state where this case takes place, his adult daughter is the legally appropriate surrogate decision-maker.
The physician updates all family present but ultimately engages the patient’s adult daughter as the legal surrogate decision-maker. In weighing the decision of whether to intubate, the patient’s daughter uses substituted judgment to consider the decision from her father’s perspective.
With the prognosis shared by the physician—that her father’s respiratory condition is ultimately incurable and likely to recur—she determined that intubation would not lead to an improvement in his quality of life and made the decision to transition to a comfort-focused trajectory of care. The patient ultimately died peacefully on the palliative care unit, surrounded by family.
ABOUT THE AUTHOR

Dr. McGiboney is an assistant professor at the University of Alabama at Birmingham with dual faculty appointments in the departments of emergency medicine and palliative medicine. She serves on the SAEM ethics committee.

When Consent Ends: Ethical Questions in Donation After Cardiac Death
By Jeremy R. Simon, MD, PhD
A previously healthy 72-year-old widower presents unaccompanied to the emergency department unresponsive after a fall on the street. Shortly after returning from a CT scan of his head and cervical spine, he has a witnessed respiratory arrest. He is intubated immediately, and after two rounds of compressions, he regains a pulse. The CT results show a moderatesized subdural hemorrhage with a small amount of midline shift and a C2 fracture. The subdural hemorrhage likely explains his altered mental status, and the
C2 fracture likely explains the respiratory arrest.
Soon thereafter, the patient’s two adult children arrive in the emergency department. When the situation and prognosis are explained, they state that they are certain their father would not have wanted to be intubated in this situation and request that life support be removed. As the patient’s next of kin and with no evidence of a separate health care agent having been appointed, they are legally authorized to make this decision. Before proceeding, however, the attending physician contacts the local organ procurement
organization (OPO), as required by law for every impending death. The OPO responds that representatives will arrive within 30 minutes and instructs the physician not to extubate the patient.
When the OPO representative arrives, they determine that the patient is a candidate for donation after cardiac (or circulatory) death (DCD)*. They also report that the patient was on the state’s organ donor registry. In light of this, they inform the children that they will be preparing their father for DCD and that he will be extubated in the operating room at the appropriate time. When told the details of DCD,
however, the children strenuously object, saying that their father would not have wanted that. The OPO replies that, because their father was on the donor registry, his prior consent overrides the family’s objection. The children become extremely upset.
There have been many changes in organ donation procedures over the years, but from an ethics perspective, perhaps the two most significant are the reintroduction of DCD and the decreased deference given to family objections. Before the acceptance of neurological criteria for death, all donations were DCD. Once brain death became accepted, the practice largely stopped. Over the last 25 to 30 years, however, DCD has been reintroduced to increase the supply of donor organs. Similarly, until almost 20 years ago, great weight was given to family objections. In 2006, the Uniform Anatomical Gift Act—adopted in some form by all 50 states and the District of Columbia—was revised to explicitly reduce the influence of families on donation decisions for individuals without capacity who were listed on organ donor registries.
The trend of disempowering families accelerated during the first Trump administration, when OPOs were threatened by the Department of Health and Human Services with contract termination if their organ retrieval rates were deemed inadequate. Needless to say, this led OPOs to become more aggressive in their retrieval practices.
While there is great value in respecting patients’ wishes regarding transplantation and in increasing the organ supply, greatly sidelining the family raises several significant ethical concerns.
Primarily, these issues relate to consent. No one has obtained explicit consent for donation generally, let alone for DCD. As anyone who has filled out a driver’s license application or joined an organ donor registry knows, there is no information of clinical relevance provided. One is only asked to check a box indicating willingness to be an organ donor. This may be adequate for donations
“It is also crucial to recognize that organ procurement organizations not only remove these matters from the family’s hands but also from those of the medical team.”
after brain death, where the entire procedure occurs postmortem and is treated as a legal gift rather than a medical procedure—much like instructions for one’s burial.
In the case of DCD, however, the process by definition begins before death, and therefore cannot be interpreted merely as honoring the donor’s wishes regarding the disposition of their remains. Furthermore, very few people who register as organ donors understand what is involved in DCD or even that it is an option. To the extent that signing up for a donor registry could be interpreted as consent, it would not apply to DCD.
Another issue is the sidelining of the family. In every state, unless a health care agent has been designated, the closest immediate family member serves as the surrogate decisionmaker. As noted, interventions must be performed antemortem in DCD cases, and these require consent— even if only implicit. If the decisionmaker objects, they cannot ethically proceed. The surrogate must act in the patient’s best interests, but that was not the basis of the OPO’s objection; rather, the OPO objected to any interference with the donation.
In addition to being the authorized decision-makers, next of kin are often best placed to interpret the patient’s true intentions. Did the patient change his mind? Would he have wanted to participate in DCD if he had understood it? For any other advance directive, surrogates are accepted as reliable interpreters of the patient’s wishes. Yet in a DCD case I am directly familiar with, the OPO
required an “uninterested” witness to verify that the patient had changed her mind about donation, even though the family was unanimous in reporting this. Even in the face of objections that are ethically significant in all other areas of medical decision-making, the OPO proceeded.
These concerns are important to understand, particularly as recent reporting in The New York Times has brought the issue of DCD back to the forefront of health care policymaking. It is also crucial to recognize that OPOs not only remove these matters from the family’s hands but also from those of the medical team. Hospitals that block the retrieval of organs claimed by an OPO face significant sanctions, up to and including removal from Medicare and Medicaid participation—a virtual death sentence for any hospital. This is not a burden that individual physicians should be expected to bear under any circumstance.
*Technically, cases such as this one, where the patient is still alive when the decision to pursue DCD is made is called controlled DCD (cDCD), since the timing of the death is controlled. There are also cases of DCD donation where the process begins after the loss of cardiac function. This is known as uncontrolled DCD (uDCD). However, these case are quite uncommon and raise somewhat different issues. In this piece we are discussing only cDCD.
ABOUT THE AUTHOR

Dr. Simon is a professor of emergency medicine at Columbia University and a faculty associate at the Columbia Center for Clinical Medical Ethics.
FACULTY DEVELOPMENT

From Pen to Prompt: Reimagining Letters of Recommendation in the Age of AI
By Robert Cooney, MD, MS; David Barnes, MD; Deborah Diercks, MD, MSc; David Leon, MD; Julie McCausland, MD, MS; Jim Miner, MD; and Kabir Yadav, MD, MS, MSHS, on behalf of the SAEM Faculty Development Committee
It’s application season, and your inbox is swelling:
“I’m up for promotion. Would you be willing to write me a letter of recommendation?”
“I’d be honored to have your support on my residency application.”
“My ERAS deadline is soon. Thanks again!”
If you’re an emergency medicine (EM) faculty member, you know this drill. Between regular letters of recommendation (LORs) for
colleagues and the more formalized standardized letters of evaluation (SLOEs) for students, writing season can quickly become a second full-time job. The stakes feel high, the deadlines tighter, and the writing process — well, sometimes repetitive.
We’ve all been there: copying last year’s letter, digging through evaluations, trying to capture what makes each student unique while juggling shifts and academic responsibilities. And if you’ve reviewed applications, you’ve likely
seen the fallout. Once upon a time, I read two letters from the same faculty member — identical down to the punctuation — submitted for different applicants. A generic, recycled letter is useless to both faculty and applicants, but when you’re asked to write 10 in two weeks, something’s got to give.
That’s where artificial intelligence, especially large language models (LLMs) like ChatGPT, Claude, and others, are starting to enter the scene. Quietly, many faculty are already experimenting with AI tools
“Large language models can be valuable tools for writing strong letters of recommendation in academic medicine by improving efficiency, equity, and consistency.”
to help them draft, revise, or polish letters. Some are doing it out of curiosity, others out of desperation. But as with any emerging technology, the question isn’t just “Can we use AI?” It’s “Should we?” And if the answer is “yes,” then, “How should we?” to reap the benefits and best support ourselves and our learners.
The Role and Weight of the Letter of Recommendation
Letters of recommendation are important in academic medicine because they provide a trusted, detailed perspective on an applicant’s clinical skills, academic potential, and
professional qualities that grades or test scores cannot fully capture.
They serve as evidence of how an individual performs in real-world medical and research settings, highlighting strengths such as clinical judgment, teamwork, leadership, and dedication to patient care. Strong letters also reflect how well an applicant is regarded by mentors and faculty, which can signal future success as both a physician and a scholar.
In a competitive field where many candidates have similar academic achievements, LORs help distinguish applicants by offering authentic insight
into their character, growth, and potential contributions to the medical community.
As one of the few narrative components in a holistic review, these letters are often reviewed early and can carry outsized influence. This is complicated by the fact that they can also be a strong source of bias, and variability in interpretation can lead to inequity. In the face of time constraints and a desire to be fair and productive, letter writing can become stressful and emotionally draining.
“By embracing artificial an author, emergency stress, and ensure promise and

continued from Page 49
Enter the LLM: Potential Benefits
Large language models can be valuable tools for writing strong letters of recommendation in academic medicine by improving efficiency, equity, and consistency.
Given the heavy workloads during peak application seasons, LLMs can help streamline the drafting process by quickly generating structured, polished drafts that reduce cognitive load and save time.
LLMs can also support bias reduction by being prompted to avoid gendered, stereotypical, or doubtraising language, helping to ensure that all candidates are described with fairness and professionalism — an important step toward promoting equity in letters of recommendation.
Additionally, LLMs can assist with standardization by maintaining a consistent tone, structure, and level of detail across multiple letters, minimizing unintentional discrepancies that might disadvantage certain applicants.
By serving as a drafting aid, LLMs allow recommenders to focus more on personalizing content and less on mechanics, ultimately producing letters that are both equitable and efficient.
Looking Ahead
As AI tools continue to evolve, their role in academic medicine will expand beyond letters and into teaching, feedback, and research support. The key is to approach these technologies thoughtfully — using them not to replace human insight but to enhance fairness, efficiency, and balance in our academic responsibilities.
Read More, Learn More
• Implications of Large Language Models for Clinical Practice: Ethical Analysis Through the Principlism Framework
• Using Generative Artificial Intelligence When Writing Letters of Recommendation
• A Scoping Review of Artificial Intelligence in Medical Education: BEME Guide No. 84
• Comparing Letters Written by Humans and ChatGPT: A Preliminary Study
By embracing AI as an assistant rather than an author, EM faculty can reclaim time, reduce stress, and ensure that each letter they write truly reflects the promise and individuality of the learners they support.
To be continued in Part 2, SAEM Pulse January-February 2026.
ABOUT THE AUTHORS





Dr. Cooney is associate professor of emergency medicine and associate dean, faculty development, at Geisinger College of Health Sciences.
Dr. Barnes is health sciences clinical professor of emergency medicine at UC Davis Health and serves as physician advisor, emergency department operations team member, and director of emergency medicine faculty development, alumni relations, and sustainability.
Dr. Diercks is professor and chair of the Department of Emergency Medicine at UT Southwestern Medical Center and holds the Audre and Bernard Rapoport Distinguished Chair in Clinical Care and Research.
Dr. Leon is health sciences assistant clinical professor with dual appointments in emergency medicine and anesthesiology at UC Davis.
Dr. McCausland is associate professor of emergency medicine and medicine at the University of Pittsburgh School of Medicine and attends in the Emergency Department at UPMC.
artificial intelligence as an assistant rather than emergency medicine faculty can reclaim time, reduce ensure that each letter they write truly reflects the individuality of the learners they support.”


Dr. Miner is professor of emergency medicine at the University of Minnesota Medical School and chief of emergency medicine at Hennepin Healthcare.
Dr. Yadav is vice chair for research and academic affairs and professor of emergency medicine at Harbor-UCLA Medical Center and is also on faculty at UCLA.
FACULTY DEVELOPMENT
From Prompts to Practice: Preparing Faculty for the Era of Artificial Intelligence in Medicine
By Hannah Mishkin, MD, MS; Wan-Tsu Wendy Chang, MD; Lindsay MacConaghy, MD; Neha P. Raukar, MD, MS; Moira E. Smith, MD, MPH; Wendy W. Sun, MD, MBA; and Laura Walker, MD, MBA
Artificial intelligence (AI), specifically large language models (LLMs) such as OpenAI’s ChatGPT, Google’s Gemini, Microsoft’s Copilot, and OpenEvidence, are now part of our learners’ lived educational experience. Students and trainees use these tools daily to draft patient notes, summarize complex readings and create flashcards, generate differential diagnoses, and practice clinical reasoning in simulated patient cases. Just ask them — they will tell you.
Modern learners are digital natives, and they are using LLMs in education. Some are experimenting responsibly, while others may be overly reliant or unaware of the limitations inherent to these tools. Many are uncertain about when and how to use them appropriately.
For faculty, educating our digital natives in the context of this new technology presents a challenge: How do we bridge the gap in digital literacy between educators and learners? That gap must be closed
not only for the sake of educational integrity, but also to uphold our role as mentors and models of lifelong learning.
This is where faculty development in prompt engineering becomes essential.
How Prompt Engineering Skills Enhance Evidence-Based Teaching
“Prompt engineering” refers to the practice of crafting precise and effective inputs in an LLM to
“Prompt engineering is a process of asking the right questions to generate the desired output — and if faculty understand the limitations of large language models and the nature of the contextual information needed, they will be in the best position to help learners use these tools to augment their learning.”
shape the quality and relevance of its outputs. It is emerging as a foundational literacy for the AI era. It is a form of cognitive structuring that helps educators and learners think clearly, ask better questions, iterate thoughtfully, and engage with technology in ways that support and enhance learning.
For faculty, prompt engineering is a natural extension of what we already do. We teach learners how to frame clinical questions, explore differentials, synthesize information, and refine reasoning when presenting patients. The logic used in prompt engineering parallels the logic used in medical decision-making.
Let’s look at a specific example of this parallel logic. A medical student wants to know the risk of death for a patient who presents with chest pain. They could ask their senior resident, “What is the risk of death for a patient with chest pain?” Alternatively, they could provide more context and ask, “What is the risk of a major adverse cardiac event in the next 30 days in a 50-year-old hypertensive, diabetic male smoker who presents with substernal chest pain and nonspecific EKG changes?”
The second question has contextual information that will elicit a more specific and clinically useful response from the senior resident. The same logic applies to prompt engineering. The more context provided to the LLM,
the more specific and relevant the output will be.
In this way, prompt engineering is a process of asking the right questions to generate the desired output. If faculty understand the limitations of LLMs and the nature of the contextual information needed, they will be in the best position to help learners use LLMs to augment their learning.
Much like evidence-based medicine, AI use requires us to ask the right question, frame it effectively, analyze the response, and apply it with clinical judgment. Faculty must help learners understand the difference between using AI as a brainstorming tool versus a trusted source of information.
Integrating Prompt Engineering Into Medical Education and Faculty Development
Educators can introduce structured approaches to evaluating the accuracy and completeness of LLM outputs, recognizing hallucinations and bias, cross-checking references and sources, and understanding the risks of overreliance. These steps parallel how we teach learners to read research articles or appraise clinical trials. Prompt engineering and AI literacy fit naturally within existing competencies.
Without clear guidance, learners may default to convenience over accuracy. For instance, they may use an LLM to draft a patient
handoff without verifying medication lists, or generate SOAP notes with incorrect assumptions or inadvertent HIPAA violations. Some may ask vague prompts that return generic, nonactionable content.
Faculty should be ready to ask questions such as, “What was your prompt?” “What did you expect?” and “How did you verify the response was accurate?” These are teachable moments — if we are equipped to identify and use them.
Prompt engineering is not a trendy or niche topic. It is a skill that intersects with clinical reasoning, communication, and professionalism. We must integrate it into faculty development now. If not, our learners will outpace our ability to guide them.
Practical Approaches for Faculty Development
Faculty development must go beyond basic introductions to these AI tools. It should empower educators with frameworks and fluency. These sessions might include foundational knowledge about how generative AI works, including its limitations and risks.
Hands-on workshops allow participants to experiment with prompt iteration, specificity, and problem framing. Sessions should offer guidance on mentoring trainees
on Page 55


FACULTY DEVELOPMENT
continued from Page 53
to integrate AI into their learning without undermining independent thought and should present use cases for how LLMs can be used in teaching materials, assignments, and reflection exercises.
Educators can join AI-focused interest groups or interdepartmental collaborations to stay current. Scholarly work in AI education and advocacy for institutional recognition of AI literacy as a core faculty skill are also important.
Resources to Support Educator Fluency
Several excellent resources already exist to support these efforts. SAEM Online Academic Resources (SOAR): AI in Medical Education is a good starting point. OpenAI’s Prompt Engineering Guide and Google’s Gemini Guidebook provide accessible tutorials, examples, and best practices that are immediately applicable.
Learning platforms such as Coursera offer a variety of structured tracks in AI and machine learning, many of which include modules on prompt engineering, digital literacy, and ethical considerations. Educators can also explore the growing body of literature on AI in medical education, AI literacy, and prompt engineering pedagogy.
As medical educators, we are responsible for preparing learners for
“Much like evidence-based medicine, artificial intelligence use requires us to ask the right question, frame it effectively, analyze the response, and apply it with clinical judgment.”
the future of AI-enhanced health care. That future is already here — and it requires fluency in new languages, including the language of prompts.
Disclosure: The authors utilized AI-based tools to help refine the language and structure of this article. We have no financial interests or affiliations with any of these services.
ABOUT THE AUTHORS







Dr. Mishkin is assistant professor of emergency medicine at Drexel University College of Medicine and emergency medicine residency program director at Reading Hospital, Tower Health.
Dr. Chang is associate professor of emergency medicine at the University of Maryland.
Dr. MacConaghy is assistant professor of emergency medicine at Geisinger Commonwealth School of Medicine and assistant residency program director at Guthrie Robert Packer Hospital.
Dr. Raukar is associate professor and vice chair for academic advancement and faculty development at Mayo Clinic Rochester.
Dr. Smith is assistant professor of emergency medicine and clinical informatics at the University of Virginia and medical information officer for emergency medicine. She chairs SAEM’s Informatics, Data Science, and Artificial Intelligence Interest Group.
Dr. Sun is assistant professor of emergency medicine at Columbia University and assistant medical director at New York-Presbyterian Allen Hospital.
Dr. Walker is assistant professor of emergency medicine at Mayo Clinic.
FEDERAL FUNDING FOCUS

Steadying the Course: How SAEM Is Guiding Members Through a Changing Federal Funding Landscape
By Manish N. Shah, MD, MPH on behalf of the SAEM Federal Funding Committee
Shifts at the National Institutes of Health (NIH) are reshaping how emergency care investigators plan their research and position themselves for success. Grants are frozen, then unfrozen; notices of award are delayed; priorities are shifting; and new funding opportunity announcements are trickling in—all of which puts investigators under
pressure to adapt quickly to an evolving and uncertain research environment.
Our specialty has always thrived amid uncertainty. Emergency care researchers excel at adapting to change, and we are well positioned to do so again. Now more than ever, pooling our knowledge, sharing
successes, and helping each other forge a new path forward will be key to positioning emergency medicine to take advantage of this new funding environment.
A New SAEM Approach and Resource for Members
The SAEM Federal Funding Committee has been newly
Changes We Know About Change What It Does Implications for EM Researchers
FY 2026 Federal Budget Impasse
FY 2026 Continuing Resolution
NIH Salary Limitation
Changes in Funding Announcements
No-Cost Extensions
No budget or continuing resolution has been passed yet, putting the government at risk of a shutdown.
If a continuing resolution passes, it will hold the NIH budget at fiscal 2025 levels, at best. Under similar resolutions in the past, the NIH has applied costmanagement guidelines, including conservative paylines and cuts to existing grants.
Salary cap at Executive Level II (about $225,700) for NIH-supported salary components on grants awarded on or after Jan. 1, 2025 (NHLBI).
All notices of funding opportunities (NOFOs) are being posted to Grants.gov rather than the weekly NIH Guide as of Oct. 1.
The first no-cost extension, previously managed by universities through eRA Commons, was removed earlier in 2025 but has now been reactivated.
established to ensure emergency medicine remains visible and valued at the federal level and to provide SAEM members with the tools and insights they need to navigate ongoing federal changes.’
We are starting by focusing on seven key NIH institutes: NIA, NIDA, NHLBI, NIAAA, NICHD, NIGMS, NIMH, NIMHD, and NINDS. We plan to work directly with program officers and agency leadership to make the case for including emergency care research in each institute’s portfolio, as well as to share information, funding opportunities, and policy updates with SAEM members.
During this first year, we will work hard to establish the committee, build its infrastructure, and organize our efforts. In the future, we will broaden our scope, expand participation, and seek more members to get involved.
We also want to showcase your successes. By collecting and reporting members’ experiences, we can present a fuller picture of emergency care research and its impact.
continued on Page 59
The NIH is likely to close, delaying study section meetings, funding decisions, and release of notices of award. Plan for these delays and work with department leadership to mitigate their impact.
Grant award timelines or amounts may be delayed or reduced. Plan spending carefully and coordinate with department leadership to address potential funding gaps.
Review budgets for necessary adjustments. Plan ahead for a similar change in 2026.
Visit Grants.gov and set up searches to stay current on new NOFOs.
The process for obtaining a no-cost extension has been streamlined and the administrative burden reduced.


Changes Being Mentioned or Discussed
Proposed Change Status and Uncertainty
Cuts to NIH Budget
Changes to Indirect Costs (F&A)
Shifts in funding priorities (DEI programs, vaccine hesitancy, foreign collaborations)
Proposed by the president in early 2025 budget drafts. Congress is working on a bill to maintain current funding levels. The larger concern is whether NIH will fully spend its allocated budget.
Changes were made but are on hold due to court injunctions. The federal government is pursuing similar goals through other channels.
Implications for EM Researchers and What to Do
A reduction would sharply limit available grant dollars. Continue monitoring NIH announcements and news reports.
This uncertainty is putting researchers in difficult positions. Check with your institution for guidance, especially regarding requests to take lower rates. If the indirect rate is reduced—as many anticipate— institutional resources will be strained, creating major budget challenges.
Some changes have been implemented, including new NIH requirements affecting grant language and policy compliance. This remains an evolving area.
Track funding priorities, new restrictions, and collaboration policies to ensure proposals remain compliant and competitive.
“Through the Federal Funding Committee, the Society for Academic Emergency Medicine is building a bridge between our members and federal funders, offering clearer insight, timely intelligence, and a stronger collective voice.”
FEDERAL FUNDING FOCUS
continued from Page 57
A Changing Landscape at NIH NIH policies are in flux. If enacted and sustained, they will have a profound effect on emergency care researchers. Below are some of the changes already in effect, as well as others under discussion—and how you can prepare.
What You Can Do Right Now
As the federal funding environment changes, there are several steps you can take to stay competitive in the new era of NIH funding:
• Stay informed. Sign up for newsletters from the NIH, Grants. gov, and the institutes most relevant to your work.
• Keep applying. You can’t get a grant if you don’t apply. Continue submitting strong proposals despite uncertainty—history shows that well-prepared applications still get funded.
• Be strategic. Frame your aims to match each institute’s stated priorities, and monitor NOFOs for relevant keywords and themes.
• Diversify your funders. Consider other funding sources, such as PCORI or private foundations.
• Share your wins. Let SAEM know about your awards and publications so we can highlight emergency medicine successes in communications with NIH and within SAEM Pulse.
The Bottom Line
The federal and NIH environments
are changing—but so is our ability to navigate them together. Through the Federal Funding Committee, SAEM is building a bridge between our members and federal funders, offering clearer insight, timely intelligence, and a stronger collective voice. With your input and participation, we can ensure our research not only adapts but thrives in the years ahead.
ABOUT THE AUTHOR

Dr. Shah is chair of the BerbeeWalsh Department of Emergency Medicine at the University of Wisconsin School of Medicine and Public Health, where he is also a professor of emergency medicine, population health sciences, and geriatrics. He chairs the SAEM Federal Funding Committee.
GERIATRIC EM

Rethinking Antithrombotic Use After Falls in Older Adults: An Emergency Department Opportunity
By Lindsay C. Klickstein, MD, and Martin F. Casey, MD, MPH
Falls, Antithrombotics, and the Emergency Department Falls among older adults remain a pressing concern. One in four Americans over age 65 reports a fall each year, and the one-year mortality after a fall exceeds 20 percent. For the many older adults who take antiplatelet or anticoagulant medications (collectively “antithrombotics”), these events carry even greater risk.
While these medications prevent devastating conditions such as stroke and myocardial infarction, they also increase bleeding risk — including the potential for intracranial hemorrhage after ground-level falls.
The emergency department (ED) is often the first point of contact for these patients. Beyond managing acute injuries, emergency physicians are uniquely positioned to reassess the appropriateness of antithrombotic therapy after a sentinel health event such as a fall.
The Study: Measuring Appropriateness
Our team conducted a secondary analysis of a prospective cohort study at a large southeastern academic emergency department. We evaluated 171 older adults (mean age 81, two-thirds female) who presented after a fall and were taking an antithrombotic.
We assessed the appropriateness of each patient’s medication using a modified Medication Appropriateness Index (MAI), focusing on four domains:
1. Clear indication
2. Appropriate dose
3. Absence of significant drug-drug interactions
4. Absence of significant drugdisease interactions
Scores categorized medications as appropriate, potentially inappropriate, or likely inappropriate.
Key Findings
• High prevalence of inappropriateness: More than 80 percent of patients were taking an
antithrombotic deemed potentially or likely inappropriate.
• Aspirin stood out: Nearly 60 percent of aspirin users had likely inappropriate use, often due to drug-drug interactions or lack of a clear indication.
• Other agents were not immune: Inappropriateness was also observed among patients on direct oral anticoagulants (29 percent), P2Y12 inhibitors (53 percent), and warfarin (30 percent).
• Interactions were common: The most frequent issues included aspirin–SSRI and aspirin–DOAC combinations, both of which elevate bleeding risk.
• Polypharmacy was the norm: Nearly 75 percent of patients were taking 10 or more medications, compounding the challenge.
Why This Matters for Emergency Medicine
This study represents the first structured assessment of antithrombotic appropriateness in a fall cohort seen in the emergency department. The findings highlight both the scope of potentially and likely inappropriate prescribing and the unique opportunity the ED provides to intervene.
Despite guideline changes discouraging aspirin for primary prevention in older adults, many patients continue to use it — sometimes purchased over the counter, without clinician oversight. These patterns create preventable risks, yet emergency visits after falls often focus narrowly on acute injury management, leaving medication appropriateness unaddressed.
Practical Takeaways for Emergency Physicians
1. Screen for antithrombotic use during medication reconciliation.
• Don’t overlook over-the-counter aspirin.
• Ask about recent falls, bleeding history, and other high-risk medications that increase bleeding risk (for example, SSRIs, NSAIDs, corticosteroids).
2. Identify red flags for inappropriate use.
• No clear indication for ongoing therapy (for example, aspirin for primary prevention).
• Excess dosing (for example, supratherapeutic anticoagulation in chronic kidney disease).
• Significant drug-drug or drugdisease interactions.
3. Engage in shared decision-making.
• Discuss risks and benefits with patients and caregivers.
• Recognize that some may prioritize stroke prevention over bleeding risk — but ensure this is an informed choice.
4. Communicate with outpatient providers.
• The emergency department visit is a critical moment to initiate a “therapeutic pause,” or temporary stoppage of the medication until reevaluation by an outpatient prescriber.
• A brief note or phone call can trigger deprescribing or adjustment by the primary care clinician or specialist.
5. Leverage available resources.
• Clinical pharmacists, when available, can provide essential expertise.
• Consider simple interventions such as patient education materials, clinical decision support, or electronic health record alerts.
Moving Forward: The Role of Deprescribing Deprescribing — systematically discontinuing medications when risks outweigh benefits — is a growing area of geriatric care. For emergency physicians, a realistic first step may be recommending a therapeutic pause with close outpatient follow-up. Even raising the question of appropriateness can open the door to safer prescribing.
Not every inappropriate score should trigger antithrombotic discontinuation; sometimes addressing another medication (such as an SSRI) can reduce bleeding risk without compromising cardiovascular protection. In some cases, prescribers may have additional information about patients that justifies continued use. Future research should clarify which emergency department–based strategies are most effective and acceptable to patients.
Conclusion
Older adults presenting to the emergency department after a fall often take antithrombotics that may no longer be appropriate, especially aspirin. For emergency physicians, this represents a vital opportunity: beyond treating immediate injuries, we can initiate conversations that improve long-term safety and quality of life.
By incorporating medication appropriateness into fall care, emergency department teams can help prevent future harm and promote thoughtful, patient-centered prescribing.

ABOUT THE AUTHORS


Dr. Klickstein is a first-year emergency medicine resident at Boston Medical Center.
Dr. Casey is an emergency department physician and assistant professor at the University of North Carolina. He has received SAEM Foundation and National Institutes of Health grants to advance geriatric emergency medicine and health services research.
GERIATRIC EM

Closing the Loop: Improving Transitions of Care for Socially Vulnerable Older Adults
By Jaiya Bolden; Beata Huang; and Tehreem Rehman, MD, MPH, MBA
Introduction
Older adults who visit the emergency department (ED) are a vulnerable population. They are more likely than younger people to visit the ED and to be admitted, but they also face elevated risks even when discharged back to the community. After discharge, older adults are more likely to experience loss of independence and mobility, which makes them more susceptible to incomplete follow-up care and adverse health events. They are up to three times as likely to return to the ED after discharge Nearly 30 percent of older adults lacked ambulatory follow-up within 30
days, which was associated with a higher risk of hospitalization. Preventing these outcomes depends on high-quality care coordination and communication, yet discharge management remains fragmented and often fails to address the unique barriers faced by this population.
Barriers to Successful Post-ED Transition
Older patients, as well as those with limited English proficiency or living in socially vulnerable areas, face heightened risks in emergency care. The Social Vulnerability Index (SVI), which captures socioeconomic, household, minority, and housing/ transportation factors, has emerged
as a valuable tool for identifying at-risk communities. In a study of patients 65 years and older admitted through the ED over a 10year period and referred to internal medicine or geriatrics at a Canadian tertiary care hospital, higher SVI scores were associated with longer hospital stays and a greater likelihood of discharge to long-term care. Beyond geriatric populations, Wilder et al. demonstrated that higher community-level SVI scores significantly increased rates of primary care-treatable ED visits, with housing and transportation vulnerabilities showing the strongest effect. These findings suggest social
“Older adults are more likely than younger patients to visit the emergency department and to be admitted, but they also face elevated risks even when discharged back to the community.”
vulnerability as a critical driver of ED utilization and the need to address community-level barriers to improve outcomes, particularly for older adults.
Barriers to Successful Post-ED transition
Older adults often spend longer times in the emergency department, in part because they undergo more laboratory and imaging tests than younger adults. Extended ED length of stay can lead to additional complications, including, new-onset delirium. Those with delirium superimposed on dementia are less likely to understand their discharge diagnosis or postdischarge instructions. A lack of understanding of diagnosis and recommended follow-up may lessen the sense of urgency and delay necessary action. Additionally, some adults do not have a reliable support system to aid them in this transition. Feelings of isolation and being a burden to others are common among older adults, who may then be less likely to follow up on care. Older adults also cite poor communication and difficulties scheduling appointments with family physicians Poor communication makes new diagnoses, medications, and timesensitive follow-up appointments difficult for patients to manage. Without reliable coordination of health services, these barriers remain a challenge in the discharge process.
Current Interventions
Effective interventions vary in both type and intensity. One study found that nurse discharge coordinators— who assisted with patient education, appointment coordination, and telephone follow-up for patients
75 and older—led to a 27 percent reduction in unscheduled emergency department return visits. Personalizing discharge management may improve health outcomes for patients. The DEED study highlighted the value of collecting patient-reported information through questionnaires to identify individuals at highest risk for adverse outcomes and guide the development of more effective follow-up plans. As a post-discharge intervention, home visits by community paramedics led to a significant reduction in 30-day ED visits for older adults with cognitive impairments and improved adherence to care plans and awareness of red flag symptoms.
Callbacks have been widely implemented, but their effectiveness is dependent on program location, delivery method (automated vs. live), and the maximum number of call attempts. These factors contribute to varying call success rates and patient outcomes. In one study, older adults who received callbacks attended follow-up appointments sooner than those who did not, though there was no reduction in emergency department revisits.
Early follow-up attendance can be vital for patients with care plans requiring timely action. Expanding metrics to include patient-centered outcomes may highlight valuable impacts of callbacks that would not be captured by healthcare systemcentered metrics such as revisits.
Conclusion
Recent research demonstrates the importance of geriatricspecific services such as focused
assessments and multidisciplinary approaches. However, these interventions often remain limited to the time spent within the emergency department. Expanding patient connections to outpatient resources has the potential to improve health outcomes. Integrating approaches such as the Geriatric Emergency Department model and callback programs with targeted strategies for socially vulnerable populations identified through tools like the Social Vulnerability Index could strengthen follow-up care and reduce preventable emergency department use by older adults.
ABOUT THE AUTHORS

Jaiya Bolden is a biology major with minors in French and chemistry at Howard University. She participated in the iCORE program at the Icahn School of Medicine at Mount Sinai, conducting geriatric emergency medicine research on missed callbacks in patients with limited English proficiency.


Beata Huang is a nursing and public health major at New York University. She participated in the iCORE program at the Icahn School of Medicine at Mount Sinai, assisting with research on geriatric callback success and emergency department transitions of care.
Dr. Rehman is associate medical director and director of geriatric service for the emergency department at The Mount Sinai Hospital and a board-certified clinical informaticist and physician advisor for utilization review at Mount Sinai Health System.
GLOBAL HEALTH
From Connectivity to Care: The Digital Transformation of Emergency Medicine in The Gambia
By Jessica Pelletier, DO, MHPE; John George Johnson; Sheikh Omar Bittaye, MD; Buba Barrow; Frederick Barton, MSN; Sabel Bass, MD, MPH; Abdoulie Njai, MD, MPH; and Manoj A Thomas
Imagine you’re a trainee physician in a busy tertiary hospital. Your patient is in septic shock, and you need to quickly confirm the dosing for norepinephrine. But the hospital Wi-Fi is down, your phone battery is dead, and the power is out. You may use mobile data—knowing it will cost you—to search for answers. You find a promising peer-reviewed article, only to discover it’s locked behind a
paywall your hospital can’t afford. The next best option becomes unverified Google links.
This is not a hypothetical. It’s the daily reality for many clinicians in The Gambia and other low- and middle-income countries (LMICs), where access to reliable, up-todate medical information is often limited by infrastructure, cost, and connectivity.
But a quiet revolution is underway. Techies Without Borders (TWB), a 501(c)(3) international nonprofit organization, has developed the Continuing Medical Education Solutions (CMES) program—a low-cost, high-impact initiative that brings emergency care education directly to the bedside, even in settings with unreliable internet and electricity.
“Techies Without Borders has developed the Continuing Medical Education Solutions program—a low-cost, high-impact initiative that brings emergency care education directly to the bedside, even in settings with unreliable internet and electricity.”
The CMES system uses a compact computer installed in hospital wards that emits its own intranet Wi-Fi signal. Clinicians connect via a custom CMES mobile app to access a rich offline library of emergency care resources, including procedure videos, podcasts, and PDFs. When the device detects an internet signal, it automatically updates its content from a cloud-based server. The library evolves based on user feedback, ensuring relevance and responsiveness to local needs. The CMES program is currently available in 19 LMICs, serving more than 13,000 doctors who care for over 20 million patients.
The Gambia: A Case Study in Innovation
The CMES program launched in The Gambia in fall 2023, with the first device installed at Edward Francis Small Teaching Hospital (EFSTH), the country’s largest tertiary referral center located in Banjul. Despite being the smallest country in continental Africa with an average annual income of just $900—the nation’s clinicians are deeply committed to improving patient care.
Emergency medicine is not yet a recognized specialty, and the national referral hospital has only two ambulances. There is no formal emergency medical services system or national triage program. Yet the hunger for knowledge is palpable.


“What sets the Continuing Medical Education Solutions program apart is its commitment to co-creating knowledge; Gambian clinicians are not just users—they’re collaborators.”
GLOBAL HEALTH
continued from Page 65
By summer 2024, a second device was placed at Ocean Medical Clinic in Brikama, with the Ministry of Health endorsing a nationwide rollout. As of August 2025, CMES devices are active in four departments at EFSTH, one in Brikama, and one in Bansang—a rural referral hospital five hours east of the capital. More than 100 clinicians from The Gambia have joined the CMES Global Community on WhatsApp, receiving monthly emergency care updates and resources.
Knowledge Co-Creation and Cultural Relevance
What sets CMES apart is its commitment to co-creating knowledge. Gambian clinicians are not just users—they’re collaborators. During the initial rollout, users requested more content on tropical medicine. In response, CMES participants from The Gambia, Nigeria, and Uganda began co-authoring peer-reviewed blog posts for emDocs. net, which were then uploaded to the CMES library.
TWB also launched the ID4U podcast, focused on infectious diseases in LMICs. Today, clinicians from 19 nations work together as colleagues to provide evidence-based care across the globe.
Voices from the Frontlines
The impact is tangible. Chief Matron Horeja Saine, head of nursing at EFSTH, said:
“We really appreciate this, and I hope staff will utilize this platform for better patient outcomes.”
A physician at EFSTH reflected:
“CMES has widened my scope, especially in tropical medicine. It may have even triggered my interest in pursuing a diploma in tropical medicine. These may seem like small things, but they have a big impact.”
Sarra Baldeh, marketing manager at Ocean Clinic, added:
“Your successful CMES installation is truly transformative. By delivering up-to-date medical education even in offline settings, you’ve empowered not only our clinicians but neighboring facilities as well.”
Looking Ahead
The CMES program is more than a tech solution—it’s a catalyst for building a sustainable learning culture in healthcare facilities across LMICs. By offering reliable information and supporting initiatives such as interprofessional journal clubs and hands-on simulations, CMES helps prevent skill decay and promotes collaboration. The program also recommends strategies such as continuing professional development incentives and dedicated Wi-Fi access to strengthen educational infrastructure.
In this way, CMES is not only democratizing access to emergency care education—it is helping clinicians in The Gambia and beyond deliver better care, foster continuous learning, and build the foundation for emergency medicine, a discipline still emerging in many LMICs.
ABOUT THE AUTHORS









Dr. Pelletier is medical director for Techies Without Borders and an emergency medicine residency associate program director at the University of Missouri–Columbia.
John George Johnson is a final-year medical student at the University of The Gambia. He is coordinator and liaison officer for Techies Without Borders at Edward Francis Small Teaching Hospital in Banjul, The Gambia.
Dr. Bittaye is deputy head of the Department of Internal Medicine at Edward Francis Small Teaching Hospital. He is also a lecturer in internal medicine at the University of The Gambia.
Buba Barrow is founder and CEO of Ocean Clinic in Brikama, The Gambia, with a special interest in trauma care.
Frederick Barton is a nurse practitioner dual boarded in family and emergency medicine. He is faculty at Seattle University and has a special interest in rural medicine.
Bethel Mwenze is a licensed paramedic in the United States and serves as African medical coordinator for Techies Without Borders.
Dr. Bass is a PhD student in health outcomes research at Saint Louis University.
Dr. Njai is a third-year orthopedic surgery resident at the University of Missouri–Columbia.
Manoj Thomas is deputy head of discipline (research) and associate professor of business information systems at the University of Sydney in Australia.
Reassessing “Excited Delirium”: Aligning Emergency Medicine With Evidence and Equity
By Emmanuel Scaife on behalf of the SAEM Social EM & Population Health Interest Group
High-Profile Cases With Restraint Use
Between August 2019 and May 2020, the deaths of George Floyd and Elijah McClain—both African American men who were restrained by law enforcement—sparked national attention and widespread discussion about law enforcement practices and medical involvement. In both cases, restraint played a central role. Beyond the political and legal debates, a controversial medicalized label repeatedly appeared at the intersection of medicine, law enforcement, and the courts: excited delirium
The continued use of the term excited delirium in clinical and legal
settings has raised significant clinical and ethical concerns. The label has been associated with inappropriate restraint use and increased risk of patient injury and death. Moreover, its application has disproportionately affected Black and Hispanic patients, reflecting systemic inequities in both prehospital care and emergency department settings.
“Excited Delirium”
In Historical Context
The concept originated in the late 19th century as “delirious mania,” describing patients with hyperactivity, psychosis, and sudden collapse. Reframed in the 1980s as excited delirium, it became
associated with agitation, paranoia, hyperthermia, and stimulant use. Later, some physicians described it as severe agitation followed by sudden death—often in prehospital settings and frequently in law enforcement custody.
In medicine, it has been used as a psychiatric descriptor to explain agitation requiring restraint in the emergency department or prehospital setting. In the legal system, it has been cited to explain deaths in police use-of-force cases.
The Harvard Law Review has described excited delirium as a “psychiatric issue characterized by the acute onset of extreme agitation
“The continued use of the term excited delirium in clinical and legal settings has raised significant clinical and ethical concerns.”
that can become so severe that someone might die spontaneously, on their own, without anyone to blame except the person’s own mental condition … some deaths in police custody occur … because the mysterious onset of a psychiatric illness led them to die suddenly.”
The American Medical Association, American College of Emergency Physicians, American Psychiatric Association (DSM-5), and the World Health Organization (ICD-10 and ICD11) have all concluded that excited delirium lacks recognized scientific or medical validity. Despite this consensus, the term still appears in clinical documentation, law enforcement records, and medical examiner reports as a cause of death.
Risks Associated With Restraint Use
When appropriately indicated, physical and chemical restraints can protect patient and staff safety, but they should remain a last resort after verbal and environmental de-escalation strategies have been attempted. Restraints carry serious risks, including apnea, hypoxia, trauma, cardiac arrest, or death Agitation can further amplify these risks.
A 2021 review linked prone physical restraint to reduced ventilation and subsequent cardiac arrest due to inadequate ventilation and circulatory compromise. While agitation contributes to risk, it is not the sole
factor associated with adverse outcomes.
Black and Hispanic patients are disproportionately subjected to both restraints and the label excited delirium. Studies show that patients restrained by law enforcement are more likely to remain restrained during their emergency department course, and Black patients are more than five times as likely to remain restrained even when de-escalation is possible. Prolonged inpatient restraint (more than four hours) has been associated with an increased risk of complications
continued on Page 71
“Black and Hispanic to remain restrained
from Page 69
Because many Black and Hispanic patients arrive restrained after law enforcement encounters, the cumulative effects of restraint use and diagnostic labeling warrant close examination. Together, these factors demonstrate the importance of equitable, evidence-based approaches to managing agitation.
Historical Legal Precedent
The use of excited delirium in clinical and legal contexts has helped establish its perceived legitimacy despite limited scientific support. Although the term was coined in the mid-1980s, its use became entrenched in the 1990s and early 2000s, even as concerns grew about its disproportionate application to Black Americans.
By 2012, the St. Louis Law Review noted that the National Association for the Advancement of Colored People had raised concerns that excited delirium was being used to justify excessive force against minority populations. By the 2000s, several court cases had cited excited delirium as precedent, effectively granting legal weight to a diagnosis not supported by medical evidence.
Continued use by medical examiners and clinicians reinforced the term’s perceived legitimacy, allowing it to persist within legal frameworks despite the lack of recognition in standard diagnostic systems. This cycle of clinical and legal reinforcement enabled excited delirium to remain in use as an explanatory label for in-custody deaths.
During George Floyd’s trial, Minneapolis police training materials
referencing excited delirium drew public scrutiny, as did its mention in the case of Elijah McClain. These examples illustrate the challenges that arise when evolving medical evidence and legal precedent are misaligned.
Policy Progress: California Assembly Bill 360
To address inconsistencies in the use of excited delirium, the California Assembly passed Assembly Bill 360 in 2023, which. The legislation:
• Prohibits the use of excited delirium as a valid medical diagnosis or cause of death
• Prevents state or government officials from documenting the term in any capacity
• Bars coroners, medical examiners, and physicians from listing excited delirium on reports or death certificates
• Forbids law enforcement agencies from using the term in incident reports
Following California’s example, Minnesota and Colorado—the states where George Floyd and Elijah McClain died—passed similar legislation. These measures aim to promote consistency and accuracy across medical, legal, and law enforcement documentation.
Policy Recommendations
Although state-level reforms have begun, the use of excited delirium persists in federal courts through historical precedent, and only a few states have enacted related policies. This inconsistency underscores the need for ongoing evaluation of terminology and training practices.
Osagie K. Obasogie, a law and bioethics scholar at the University of California, Berkeley, in his 2021 Virginia Law Review and 2025 Harvard
Hispanic patients are more than five times as likely restrained even when de-escalation is possible.”
Law Review, outlined six policy recommendations to address these gaps:
1. Eliminate excited delirium as a legal term at the national level.
2. Prohibit medical examiners and coroners from attributing cause of death to unvalidated diagnoses such as excited delirium.
3. Amend federal and state evidence rules to exclude invalid medical terminology from expert testimony.
4. Discontinue law enforcement training that references unsubstantiated diagnoses.
5. Allow judges to independently evaluate expert testimony on a case-by-case basis rather than relying on historical precedent.
6. Ensure that legal and medical systems promote clarity and accountability in describing causes of death.
Pursuing reforms simultaneously at local, state, and national levels may help ensure consistent, evidencebased approaches across disciplines.
Conclusion
Emergency physicians routinely encounter patients who are agitated or restrained on arrival to the emergency department, often after law enforcement involvement. Recognizing the clinical, ethical, and policy implications of such encounters is essential for safe and equitable care.
Improving patient safety depends on aligning medical and legal frameworks with current scientific consensus. Emergency physicians can play an important role by applying evidencebased de-escalation strategies and ensuring that documentation reflects accurate, validated terminology.
ABOUT THE AUTHOR

Emmanuel Scaife is a secondyear medical student at the University of California, Riverside School of
Medicine.
HEALTH POLICY
Federal Focus: How New Artificial Intelligence and Telehealth Bills Could Shape Emergency Medicine
Prepared for SAEM Members by the SAEM Leadership, Bylaws, and Governance Committee
The Society for Academic Emergency Medicine (SAEM) leadership is committed to keeping members informed about federal policy developments that may affect the practice of emergency medicine. Two recent U.S. House resolutions introduced during the 119th Congress highlight key issues for clinicians: the role of artificial intelligence in health care and the future of telehealth access.
HR 5045 – The HEALTH AI Act
Introduced in August 2025 by Rep. Ted Lieu, D-Calif., and co-sponsored
by Rep. Ami Bera, D-Calif., HR 5045 seeks to advance the responsible use of generative artificial intelligence in health care.
Key Provisions
• Administrative burden reduction: Supports research to study how AI can reduce documentation and paperwork required of health care professionals.
• Improved patient care: Promotes projects that evaluate AI tools to assist with note-taking and generating medically relevant questions during patient visits.
• Claims processing: Encourages research into AI systems that may streamline and expedite health insurance claims.
• Grant prioritization: Gives preference to initiatives that expand AI adoption, train clinicians, address workforce burnout, and improve access to care for underserved populations.
Why It Matters to Emergency Medicine
Emergency physicians face heavy documentation demands and high patient volumes. The HEALTH AI Act
“Emergency physicians face heavy documentation demands and high patient volumes. The HEALTH Artificial Intelligence Act emphasizes tools that could reduce administrative burden and improve efficiency while addressing equity and clinician well-being.”
emphasizes tools that could reduce administrative burden and improve efficiency while addressing equity and clinician well-being.
HR 4206 – The CONNECT for Health Act of 2025
Introduced by a bipartisan group of lawmakers—including Reps. Mike Thompson, D-Calif.; Don Bacon, R-Neb.; Troy Balderson, R-Ohio; and Nanette Diaz Barragán, D-Calif.—HR 4206 focuses on making telehealth a permanent feature of the U.S. health care system.
Key Provisions
• Elimination of geographic restrictions: Allows patients to receive telehealth care regardless of location.
• Expansion of originating sites: Broadens the range of settings where telehealth services may be provided.
• Support for rural and Native American health centers: Expands telehealth options for federally qualified health centers (FQHCs) and Native American health facilities.
• Quality measurement and reporting: Directs the Department of Health and Human Services (HHS) to establish telehealth quality measures and publish quarterly data on utilization, expenditures, and outcomes.
• Engagement study: Requires HHS to examine strategies to enhance beneficiary participation in telehealth, with emphasis on underserved populations.
Why It Matters to Emergency Medicine
Telehealth has become an essential
tool for follow-up care and for patients in rural or underserved areas. This bill seeks to ensure access continues beyond the temporary flexibilities granted during the COVID-19 pandemic.
Context: Telehealth Flexibilities
The Centers for Medicare and Medicaid Services (CMS) telehealth exceptions are scheduled to expire Sept. 30, 2025. Exceptions for FQHCs and rural health clinics extend until December 2025. Without congressional action, reimbursement
for telehealth visits to Medicare beneficiaries in their homes will revert to pre-pandemic restrictions.
SAEM members are encouraged to remain informed about these legislative developments. HR 5045 and HR 4206 could affect patient care, clinician workload, and access to services within emergency medicine. Portions of the CONNECT for Health Act may also provide opportunities for academic inquiry into populations served by emergency telehealth.
INFORMATICS, DATA SCIENCE & AI

From Notes to Knowledge: How Generative AI Is Reshaping the Emergency Department
By Mona Moukaddem MD, MS; Will Freeman, MD; and Greg Han, MD, on behalf of the SAEM Informatics, Data Science, and
Artificial Intelligence Interest Group and the SAEM
Introduction
Emergency department (ED) documentation is rich in clinical information but is primarily stored in unstructured narrative documents such as triage assessments and provider notes. This information must be broken down into pieces a machine can “read” before largescale data analytics or artificial intelligence (AI) tools can be applied. Natural language processing (NLP) tools do just that—they transform unstructured language into structured formats by breaking text into smaller pieces, or “tokens,” which can then be analyzed further.
As AI becomes more prevalent in medicine, clinicians must understand how it works in order to use it effectively and avoid its pitfalls. These tools will inevitably change
Administration and Clinical Operations Committee
how we work—for the better if we know how to leverage them.
Core Natural Language Processing Tasks
Different AI tools have different tokenizers, as they serve different purposes. Even conceptually simple tasks such as data extraction use various approaches:
• Named entity recognition (NER): Identifies clinical concepts in text. For example, in “The patient was given 5 mg of morphine for chest pain,” NER would detect “morphine” as a medication and “chest pain” as a symptom.
• Clinical concept normalization: Maps varied terms such as “MI,” “myocardial infarction,” and “heart attack” to standardized codes such as ICD-10 or SNOMED CT.
• Relation extraction: Links entities such as “elevated troponin” to “NSTE-ACS” to reconstruct and infer clinical logic.
• De-identification: Removes protected health information (PHI) to enable privacy-preserving data reuse. Transformer-based models are being studied for this task, but they still face important limitations and require safeguards and human oversight.
From Rule-Based NLP to Large Language Models
Early NLP tools were rule-based, allowing them to function with relatively small training datasets. However, these tools were inflexible and required significant upfront work to develop their rules. Deep learning models improved upon this

“Generative artificial intelligence can ease the documentation burden by drafting discharge instructions and synthesizing clinical information for provider notes and patient handoffs.”
by learning context and relationships between tokens, allowing for greater flexibility.
Tokenized text is also often “embedded” or “vectorized” to support downstream tasks. The term vectorized refers to the representation of words as lists of numbers—socalled vectors—where similar words have similar vectors. For example, “1st-gen” plus “cephalosporin” might equal “cephalexin.”
In the clinical context, embedding models capture meaning at multiple levels:
• Concept embeddings (for example, BioWordVec) reflect semantic proximity between terms.
• Visit embeddings summarize patterns across diagnoses, medications, and labs to support episode-level analysis.
• Patient embeddings represent longitudinal trajectories across multiple visits.
These deep learning models build representations that support downstream tasks such as risk prediction and patient similarity analysis.
Ongoing Challenges in Emergency Department NLP
Despite these advances, NLP still faces notable challenges. Emergency department notes vary widely in format, abbreviations, and syntax,
which complicates analysis. Temporal reasoning—understanding time references such as “before arrival”— remains underdeveloped. Annotated datasets for ED-specific text, especially triage notes, are limited and often inconsistently labeled.
Even purpose-built models like ClinicalBERT, trained on MIMIC-III (a large database of deidentified intensive care unit patient cases), continue to struggle with generalizability.
How Large Language Models Work
Newer AI tools such as transformers
continued on Page 77

“Overreliance on artificial intelligence–generated content could erode clinician skills and diminish the personalized communication central to quality emergency care.”
INFORMATICS
continued from Page 75
and large language models (LLMs) address these challenges differently. These tools consider tokens relative to one another, assigning higher “attention weights” to pairs of words with stronger relationships.
For example, in the phrase “Troponins were elevated in the setting of type 2 NSTE-ACS,” the word “troponin” attends most closely to “elevated.” This framework enables LLMs to generalize across tasks rather than adhering to predetermined rules—but at the cost of requiring vast quantities of training data and computing power.
Generative AI at the Bedside
The way LLMs process text mirrors how clinicians synthesize information at the point of discharge. They condense multiple sources into a patient-friendly summary, often with added considerations such as reading level, language preference, and incidental findings that require follow-up.
Generative AI can ease this burden by drafting discharge instructions and synthesizing clinical information for provider notes and patient handoffs. When guided by appropriate prompts and clinician oversight, these tools can meaningfully reduce cognitive load while maintaining accuracy.
Implementation Risks and Safeguards
Although AI can enhance every phase
of the ED workflow, it introduces significant risks. “Hallucinations”— factually incorrect but convincingly written statements—could mislead clinicians or patients if left unchecked. Overreliance on AI-generated content could also erode clinician skills and diminish the personalized communication central to quality emergency care.
The emerging physician-in-the-loop model offers a potential safeguard. In this workflow, AI-generated drafts require clinician review and explicit approval before entering the medical record. Interfaces designed to highlight frequently edited sections, track changes, and prompt verification of key details such as medications and follow-up timing can balance efficiency with accuracy and safety.
AI tools may also link to cited sources within a patient’s chart, helping to ensure transparency and accuracy. Institutions adopting these tools must establish clear governance for how they are trained, validated, and monitored to ensure equitable performance across diverse patient populations.
The Path Forward for AI in ED Documentation
Natural language processing tools have significant potential to revolutionize ED documentation. Rule-based NLP can structure disparate information, while modern, attention-based LLMs can summarize and synthesize text in clinically useful ways. These technologies could transform both data analytics and clinical workflows—but only
if implemented with appropriate oversight.
Key Takeaways for the ED
• ED text poses unique challenges: Variability in structure, abbreviations, and limited annotated datasets hinder reliable NLP performance.
• Traditional NLP is narrow in scope: Rule-based and early machinelearning methods can extract entities and normalize concepts but lack adaptability.
• LLMs shift the paradigm: Attentionbased models capture context and enable generalization across tasks but require substantial training data.
• Generative AI has clinical relevance: Drafting discharge instructions, provider notes, and handoffs can reduce documentation burden.
• Risks must be managed: Hallucinations, inequitable model performance, and clinician deskilling pose safety concerns.
• Physician-in-the-loop is essential: Oversight, edit tracking, and sourcelinked verification ensure accuracy and accountability.
• Equity and governance are critical: Ongoing monitoring across diverse populations prevents bias and maintains trust in emergency care.
ABOUT THE AUTHORS


Dr. Moukaddem is a postdoctoral fellow at the University of Chicago.
Dr. Freeman is an emergency medicine resident physician at the Washington University School of Medicine. Dr. Han is an emergency medicine resident physician at NewYork-Presbyterian Hospital (Cornell/Columbia)
ONCOLOGIC EMERGENCIES

When Minutes Matter: Reducing Boarding Risks for Cancer Patients in the ED
By Allison M. Savon; Angela Bray Lindsay, DO; and Monica K. Wattana, MD on behalf of the SAEM Oncologic Emergencies Interest Group
The Challenge of Boarding Inpatient boarding within the emergency department poses a significant challenge to timely and effective care, particularly for vulnerable patient populations. Patients with cancer carry unique risks for life-threatening conditions such as neutropenic fever, malignant spinal cord compression, sepsis, and tumor lysis syndrome, making rapid assessment and intervention essential. Increased boarding often contributes to delays in workup, diagnosis, and therapeutic interventions, including the administration of antibiotics.
Additionally, boarding may result in patients waiting for extended periods in overcrowded, closequartered spaces, increasing their risk of hospital-acquired infection. While there is not yet a universal solution to the problem of boarding, thoughtful models developed for specific patient populations have
shown promise in mitigating this systemwide issue.
Evidence Linking Boarding and Outcomes
A recent large scale retrospective study by Brock et al. evaluated the relationship between mortality and boarding times at a comprehensive cancer center. The authors found that boarding for 5.1 or more hours was associated with a 19% greater likelihood of in-hospital mortality compared with boarding times of less than 1.5 hours, even after adjusting for comorbidities and acuity.
Delays in definitive care can worsen electrolyte derangements such as those seen in tumor lysis syndrome or hypercalcemia. Timesensitive antibiotics may be delayed for patients with febrile neutropenia, leading to higher mortality rates. Patients with malignant spinal cord compression may not be rapidly identified, delaying treatment such
as steroids, radiation, or operative decompression, and potentially resulting in lifelong neurologic deficits. Surgical intervention can also be affected. For instance, a bowel obstruction secondary to a cancerous mass may worsen if consultation or nasogastric decompression is delayed, leading to increased morbidity.
The High-Risk Environment of the ED
Emergency departments are inherently high-risk environments for oncology patients. Prolonged exposure to sick contacts, limited isolation options, and crowded waiting areas increase the risk of hospital-acquired infections — a serious concern for immunocompromised patients receiving chemotherapy or other intensive treatments.
These patients should not be left waiting in spaces not designed for

“Patients with cancer carry unique risks for life-threatening conditions such as neutropenic fever, malignant spinal cord compression, sepsis, and tumor lysis syndrome, making rapid assessment and intervention essential.”
their vulnerability. As emergency physicians, we must advocate for system-level improvements that prioritize this population’s safety and expedite their care.
Toward Specialized Oncology Pathways
While solving inpatient boarding is a complex challenge, implementing specialized protocols for oncology patients offers a tangible step forward. In Cancer Patients in the Emergency Department: A “Nightmare” that Might Become a Virtuous Clinical Pathway, Legremante et al. describe the creation of a dedicated cancer pathway in the emergency department. The process, supervised by a dedicated oncology resident, improved key outcomes, including emergency department (ED) mortality,
mean length of stay, inpatient admission rate, and inpatient length of stay.
A Call to Action
Patients with cancer face increased risks of acute decompensation, and even short delays in care can be dangerous. Collaboration between emergency medicine and oncology services to create specialized emergency department protocols can facilitate more rapid assessment, enhance interdisciplinary care, and promote safer, more efficient treatment for these high-risk patients.
As emergency physicians, we must continue to advocate for systemlevel solutions that protect our most vulnerable patients and ensure that timely, equitable care remains at the center of our mission
ABOUT THE AUTHORS

Allison Savon is a third-year emergency medicine resident at Virginia Commonwealth University.

Dr. Lindsay is an associate professor of emergency medicine, core faculty for Virginia Commonwealth University Health’s emergency medicine residency, and medical director of the emergency center at New Kent.

Dr. Wattana is an associate professor, director of education, and program director for the oncologic emergency fellowship in the department of emergency medicine at the University of Texas MD Anderson Cancer Center.
PEDIATRIC EM

Closing the Treatment Gap: Emergency Department Strategies for Youth With Opioid Use Disorder
By Stephen Sandelich, MD, and Christopher Buresh, MD, MPH, on behalf of the SAEM Pediatric EM Interest Group
Opioid use disorder (OUD) continues to be a major driver of morbidity and mortality in the United States, and adolescents are not immune to its impact. In 2024, only about 30% of adolescents ages 12 to 17 with OUD received any treatment in the previous year, despite increasing rates of overdose deaths. Buprenorphine dispensing among individuals ages 10 to 18 has nearly doubled since 2020, an encouraging acknowledgment that buprenorphine is both safe and effective for youth.
The emergency department (ED) is uniquely positioned to close the treatment gap. Many adolescents who die of an opioid overdose have an ED visit in the weeks before their
death, many in the first 48 hours after discharge. ED clinicians can initiate evidence-based treatment, prevent withdrawal, and link patients to care, thereby increasing recovery rates.
Despite this opportunity, a 2024 national survey found that few pediatric EDs have formal protocols for starting buprenorphine in adolescents, citing barriers such as limited training, concerns about precipitated withdrawal, and lack of clear follow-up pathways.
Buprenorphine is the most practical and scalable medication for OUD in adolescents. It is FDAapproved for individuals 16 and
older but is safely used in younger patients. It is a partial μ-opioid receptor agonist with high receptor affinity. By displacing full agonists like fentanyl from the receptor while only partially activating it, buprenorphine controls cravings and withdrawal. Importantly, buprenorphine carries a very low risk of respiratory depression. These pharmacologic properties make it particularly valuable in the fentanyl era, when consistent receptor blockade can prevent death from overdose.
While buprenorphine is safe, it is still not clear if it is best initiated in the inpatient or outpatient setting. Traditionally, buprenorphine initiation
in the ED is done once the patient has objective signs of withdrawal. Most protocols recommend waiting until the Clinical Opioid Withdrawal Scale (COWS) score is at least eight before starting therapy, with a minimum period of abstinence from fentanyl of 12 to 24 hours. A typical and safe regimen involves a 4- to 8-mg sublingual dose, followed by reassessment every 30 to 60 minutes, with repeat doses as needed, up to a total of 16 mg on the first day.
Some adolescents, especially those with heavy fentanyl exposure or concurrent pain, may struggle to tolerate the withdrawal required for standard induction. Microinduction is an alternative that allows buprenorphine to be started in small doses while the patient continues to use or receive full-agonist opioids, thereby avoiding withdrawal. Doses can start around 0.5 mg every few hours and gradually increase over one to three days until reaching a therapeutic range. This method can be challenging in the outpatient setting, but it can be accomplished in an inpatient setting.
Some states have interpreted the American Society for Addiction Medicine (ASAM) criteria for complicated withdrawal to include adolescents, and therefore will reimburse for medical admission in these cases. Providers should check with their inpatient services to see if this is a possibility.
Long-acting injectable (LAI) buprenorphine is an emerging option for adolescents. Monthly subcutaneous formulations provide steady receptor occupancy, reduce the adherence burden, and lower the risk of diversion. One case series reported successful transition from sublingual to injectable buprenorphine in adolescents, with early remission and improved engagement. From an ED perspective, LAI buprenorphine may be especially valuable for youth with unstable housing or those unlikely to attend follow-up appointments. Some centers now offer same-day initiation after a single sublingual dose or high-dose induction, allowing patients to leave
the ED stabilized for an extended period.
It is critical to provide adjunctive medications to keep patients comfortable while waiting for a high enough COWS score (eight or higher) to initiate buprenorphine. Medications such as ondansetron, clonidine, and hydroxyzine can help mitigate symptoms during that interval. Some centers have done unobserved standard inductions with adolescents at home with designated support people. This practice is beneficial for patients who are not yet in withdrawal in the ED and are motivated with an outpatient follow-up plan in place.
Scaling ED buprenorphine initiation for a larger adolescent population requires programmatic development. Successful programs incorporate clinician education, electronic order sets, and clear linkage agreements with outpatient providers willing to treat youth. Educational materials for patients and families are critical. Embedding peer recovery specialists or social workers into a program facilitates bedside engagement and subsequent connection to community care.
Beyond MOUD initiation, ED visits should offer harm reduction strategies that reduce morbidity and mortality; these should be provided universally, regardless of readiness to start treatment. Naloxone distribution should be routine for all at-risk youth and their families, accompanied by brief education on recognizing overdose and administering intranasal naloxone.
Counseling on safer use practices, such as avoiding use alone, testdosing new batches, and using fentanyl test strips, can empower adolescents to make safer choices until they are ready for treatment. Contingency management, which uses small rewards to reinforce treatment adherence or negative drug screens, is emerging as a promising strategy, especially via smartphone platforms, and may improve adolescent engagement when introduced during the ED visit. Providing information about syringe service programs, when
available locally, may help prevent infections, and HIV or hepatitis C transmission, among youth who inject drugs.
By combining buprenorphine initiation with harm reduction and behavioral supports like contingency management, ED clinicians can offer a more comprehensive, patient-centered approach that meets adolescents where they are and increases the likelihood of long-term recovery.
Because consent requirements for adolescent substance use treatment vary by state, ED teams should work closely with local legal and ethics experts to create policies around consent and confidentiality. Providing naloxone at discharge and developing a network of outpatient prescribers who accept adolescents can help maintain continuity of care.
Adolescents with OUD represent a high-risk population with tremendous opportunity to improve treatment engagement. The ED encounter offers an important chance to initiate buprenorphine—whether with standard induction, high-dose protocols, or micro-induction—and potentially transition to long-acting injectable formulations. Developing youth-focused ED medicationassisted treatment programs, with standardized workflows and linkage to outpatient care, is an essential step toward closing the treatment gap. For many adolescents with OUD, the ED visit may be the last chance to intervene. That intervention saves lives
ABOUT THE AUTHORS


Dr. Sandelich is an assistant professor of emergency medicine and pediatrics at Penn State Medical Center.
Dr. Buresh is an associate professor of emergency medicine and pediatrics.
continued on Page 25
QUALITY IMPROVEMENT

Optimizing Emergency Airway Carts: A Systems Approach to Safer Airway Management
By Anita Goel, MD; Andrew J. Adan, MD; Courtney Kein, MD; and Anthony Martella, MD
Airway management is among the most time-critical and cognitively demanding tasks in the emergency department. In 2021, the University of Cincinnati faced a persistent challenge: essential airway supplies were haphazardly organized on a small table, leading to variability in availability, efficiency, and preparedness during critical encounters. The system relied on second-year residents to check and restock multiple tables after each use and at shift change. This disorganization led to wasted time and unnecessary cognitive burden without assurance of completeness.
Recognizing the need for a more systematic approach, our team began researching organizational methods aligned with the most common airway needs encountered in any emergency department.
Literature Review: Bridging Best Practices
While airway carts are nearly ubiquitous across emergency departments, literature guiding their design is surprisingly sparse and often borrowed from the operative setting. Much of what exists centers on operating room workflows, lean methodology, and human factors
engineering, with limited direct application to the dynamic, highacuity emergency department environment.
Still, several themes emerge across disciplines:
• Cognitive load matters: Studies in anesthesia emphasize the role of cognitive aids—like standardized layouts and color coding—in reducing errors and decision fatigue. One emergency department-based QI initiative showed that a colorcoded airway cart significantly reduced time to equipment retrieval in simulations. These principles
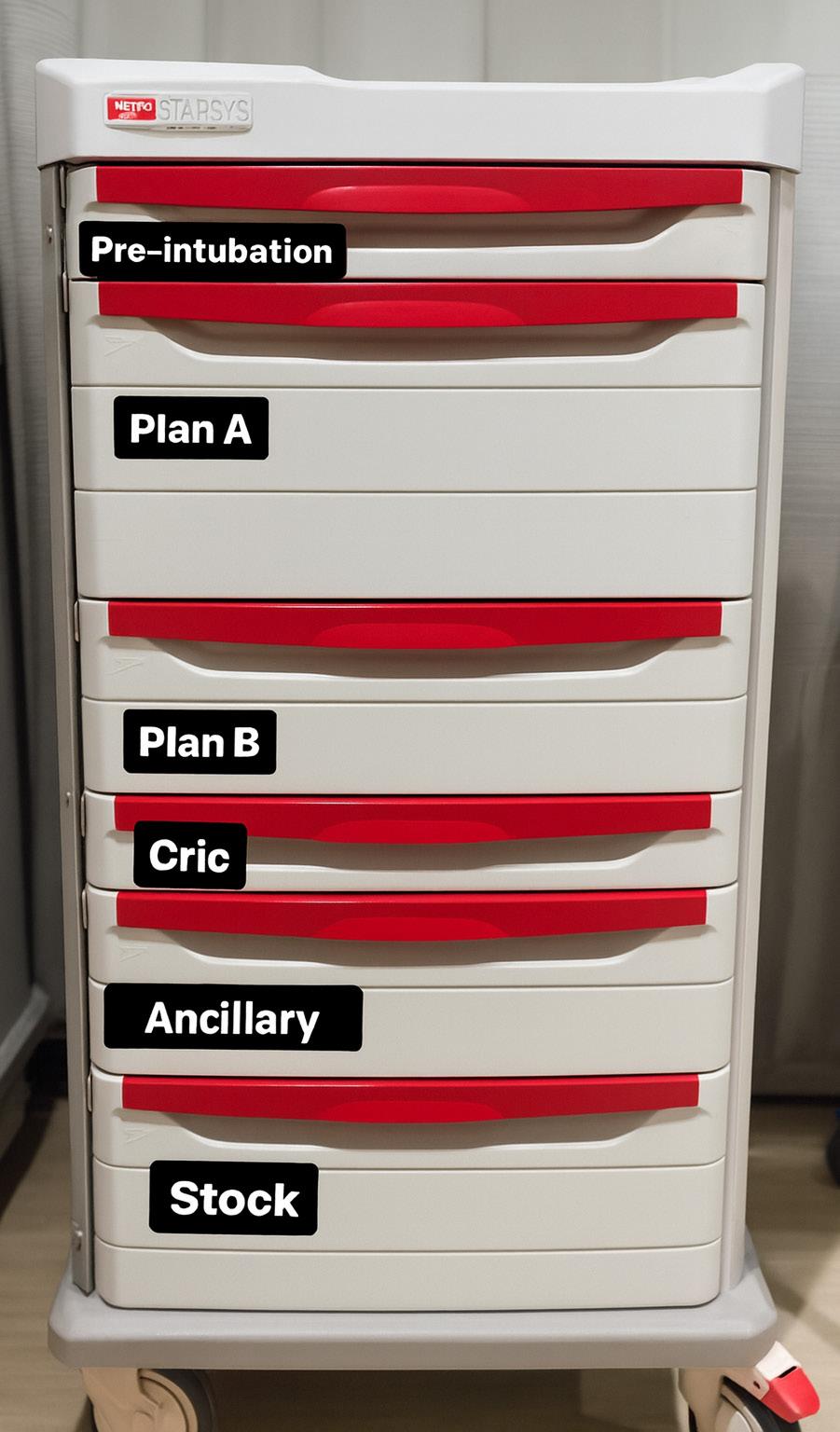

“Thoughtful cart design can reduce delays, improve team performance and support safer airway management.”
could help mitigate the chaos of time-sensitive intubations and enable other personnel, such as nurses or students, to retrieve equipment efficiently.
• Clutter is the enemy: In many anesthesia departments, airway carts include pre-packaged kits for specific procedures—cricothyrotomy or endoscopic intubation—allowing clinicians to grab a single bundle rather than hunt for individual components. This minimizes delays and ensures critical equipment isn’t missed. Emergency departments, by contrast, often rely on open-access
carts with loosely grouped supplies, leading to clutter and confusion.
• Two roads to organization: Airway cart design tends to follow one of two philosophies. Some prioritize frequency of use—placing commonly needed items in top drawers. Others adopt an escalation-based approach, organizing drawers to mirror airway progression: oxygenation tools up top, followed by standard intubation equipment, supraglottic devices, and finally cricothyrotomy.
Though the evidence base is patchy, the message is consistent: thoughtful cart design can reduce delays,
improve team performance, and support safer airway management. Our redesign aimed to bring these principles to life - tailored to the realities of emergency care.
Back to Our Department: What Did We Do?
Our initial innovation divided supplies into two streamlined boxes - “emergent” and “urgent” - based on anticipated frequency of use and space limitations. After one year, this framework evolved
continued on Page 84
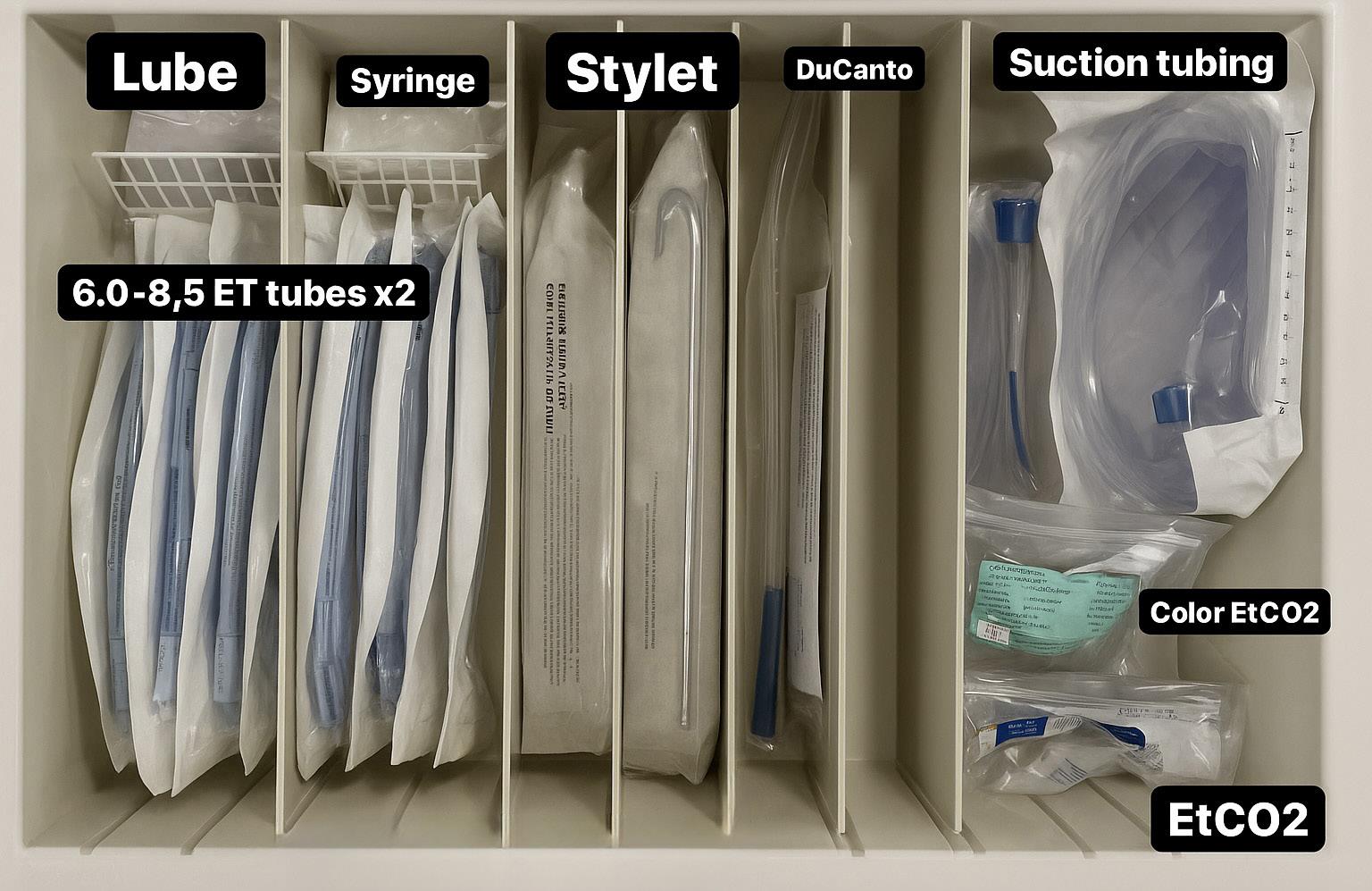
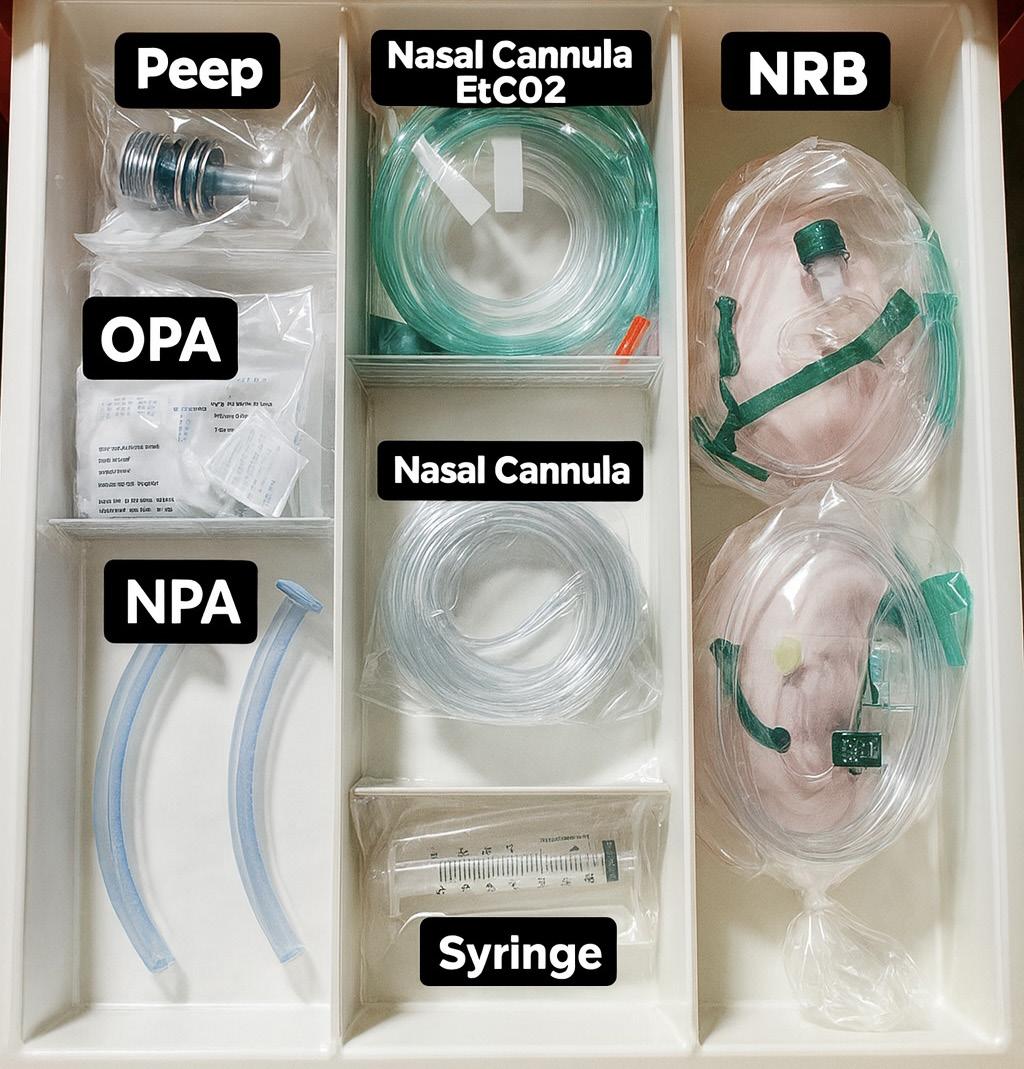
QUALITY IMPROVEMENT
continued from Page 83
into a comprehensive airway cart organized in a stepwise manner.
Guided by available literature, we adopted the escalation-based approach.
Drawers progressed from preoxygenation to primary and secondary airway strategies, airway adjuncts, and a large bottom drawer for restocking commonly used items. We incorporated kit architecture
“This progression—from evidence-based airway problem catalyzed an and safety in
“Our initial innovation divided supplies into two streamlined boxes—‘emergent’ and ‘urgent’—based on anticipated frequency of use and space limitations.”
into each drawer, particularly for cricothyrotomy. For this rare but critical procedure, we crafted a dedicated, minimalist drawer with only the necessary items. Importantly, the system was structured to minimize recency bias, ensuring that rare or complicated encounters didn’t distort stocking priorities.
Implementation
Though our design was intentional and evidence-informed, we knew the real test would be implementation. We were given a convenient opportunity with the opening of a new emergency department space in July 2023. Provided with an empty modular cart as a blank canvas, we chose optimal locations for each item to be easily found in high-stress moments. Large items were hung on the cart’s side rather than folded or placed in distant locations.
Duplicate airway carts were stocked and placed in each large resuscitation bay, with two additional carts at other key junctions in the department. The new physical space brought new logistics and workflows, easing some of the burden of change. Implementation coincided with the start of a new academic year, allowing
a new cohort of second-year residents to learn the new setup from the outset, rather than retraining those accustomed to the previous system.
We iterated based on user feedback. Inventory lists were added to each airway cart to reduce the cognitive load of restocking and assist those who interact with the carts less frequently. However, intermittent stocking issues did arise—particularly in the surgical airway drawer, which we most wanted to protect. To address this, we added a breakaway security tag to that drawer as a safeguard.
With departmental buy-in and consistent messaging, implementation was well-received and relatively smooth.
Conclusion
This airway cart system has now been in place for over two years with relative stability. The escalation-based drawer system has been praised for mirroring the airway algorithms we use, aligning with the conditioned cognitive processes relied upon during emergency airways. It creates a logical workflow and prompts the team to consider each step in the airway management process.
progression—from ad hoc supply management to deliberate, airway cart design—illustrates how a local systems innovation to improve consistency, efficiency in emergency airway management.”
The carts and bottom supply drawer have improved stocking ease and reduced the mental load for junior learners and other staff. This progression—from ad hoc supply management to deliberate, evidenceinformed airway cart design— illustrates how a local systems problem catalyzed an innovation to improve consistency, efficiency, and safety in emergency airway management.
ABOUT THE AUTHORS


Dr. Goel is an associate professor of emergency medicine at the University of Cincinnati. She directs longitudinal programs for medical students interested in emergency medicine and leads a section of the transitions to residency course.
Dr. Adan is an assistant professor at the University of Cincinnati and associate medical director at the Jewish Hospital. He directs emergency airway management operations and education, with research focused on emergency department operations, airway training and angioedema.


Dr. Kein is a critical care fellow and chief fellow at Henry Ford Health. She contributes to institutional education programs and airway training, with research focused on faculty teaching assessment.
Dr. Martella is an operations and administrative fellow and assistant medical director at University Hospitals Cleveland Medical Center. He contributes to emergency department quality initiatives and leads research on the emergency department–run observation unit.
QUALITY IMPROVEMENT

Asymptomatic Hypertension in the ED: A Critical Opportunity to Initiate Care
By Dina Gozman, MD and Yosef Berlyand, MD, on behalf of the SAEM Quality Improvement & Safety Interest Group
Hypertension is the most prevalent modifiable risk factor for developing cardiovascular disease, which is the leading cause of death in the United States. Recent data show a hypertension prevalence of 47.7 percent, yet only 20.7 percent of adults have their blood pressure controlled to the target of less than 130/80 mm Hg. Although most treatment guidelines are designed for the primary care setting, access to regular medical care remains a significant barrier in the U.S. healthcare system. About 8 percent of the population is uninsured, and an estimated 27 percent of adults report no usual access to medical
care outside of the emergency department (ED).
It is well established that rapid reduction of blood pressure in asymptomatic patients in the ED is not recommended due to the risk of hypoperfusion of vital organs. However, less guidance exists on how to manage patients who present with elevated blood pressure, no symptoms, and no reliable access to follow-up care.
In our experience, ED physicians are often hesitant to initiate antihypertensive therapy, either due to concerns that elevated readings may be attributable to acute stressors or that initiating treatment
could lead to adverse effects. While the ED is not the ideal setting for chronic disease management, it may represent the only interaction many patients have with the healthcare system. In these cases, starting treatment provides a valuable opportunity to offer education and begin addressing a major risk factor for cardiovascular disease.
This potential gap in care was recently addressed in the 2025 ACEP Clinical Policy on elevated blood pressure in the ED, which reviewed evidence supporting the safety and efficacy of initiating outpatient antihypertensive therapy in the appropriate patient population.
“While the emergency department is not the ideal setting for chronic disease management, it may represent the only interaction many patients have with the healthcare system.”
Practical Management
• All patients with elevated blood pressure should be encouraged to monitor their levels at home using a reliable cuff. Primary care guidelines recommend checking blood pressure twice in the morning before breakfast and twice in the evening before bed.
• For patients with stage 1 (≥130/80 mm Hg) or stage 2 (≥140/90 mm Hg) hypertension, lifestyle modifications should be recommended along with resources for establishing primary care followup. In some states, pharmacists are authorized under collaborative practice agreements to initiate and manage antihypertensive therapy, which may serve as a temporary bridge to care.
• For patients with severe hypertension (≥180/120 mm Hg), initiating medication in the ED should be considered to begin lowering blood pressure while awaiting follow-up. The four main classes of first-line antihypertensive agents are:
• Thiazide-type diuretics (for example, hydrochlorothiazide, chlorthalidone)
• Long-acting dihydropyridine calcium channel blockers (for example, amlodipine, nicardipine)
• Angiotensin-converting enzyme (ACE) inhibitors
• Angiotensin receptor blockers (ARBs)
Because blood pressure is regulated by multiple pathways, most patients with severe hypertension will ultimately require two or more medications. The American Heart
Association recommends initiating therapy with a single-pill combination of two agents to improve efficacy and adherence. Evidence suggests that using lower doses of multiple medications reduces blood pressure more effectively and improves compliance without increasing the risk of adverse effects.
Common fixed-dose combinations include an ACE inhibitor or ARB with either a thiazide diuretic or amlodipine. ACE inhibitors and ARBs should not be co-prescribed due to the risk of adverse effects. Typical firstline choices include:
• benazepril-hydrochlorothiazide (10 mg/12.5 mg)
• losartan-hydrochlorothiazide (50 mg/12.5 mg)
• amlodipine-benazepril (2.5 mg/10 mg)
• amlodipine-valsartan (5 mg/160 mg)
Addressing Safety Concerns
While side effects from antihypertensives are relatively common, they are typically mild and well tolerated. Severe adverse effects, such as hyperkalemia, are uncommon. Although routine screening for target organ damage is not recommended in asymptomatic hypertension, it is reasonable to check a basic metabolic panel when initiating therapy in the ED to assess potassium levels. Ideally, electrolytes should be rechecked within four weeks of initiation.
Elderly and frail patients are also at higher risk for orthostatic hypotension, though this is more often associated with higher drug dosages than those typically started in the ED.
Why the ED matters
For many, the ED remains their only
consistent access point to healthcare. Barriers such as lack of insurance, limited transportation, long waits for primary care appointments, and absence of a regular physician often leave vulnerable populations reliant on emergency services for both acute and chronic care.
Although emergency physicians are not positioned to provide comprehensive primary care, they play a crucial role in health education and initiating essential treatments. For the right patient, starting antihypertensive therapy in the ED represents a critical opportunity to address uncontrolled blood pressure, potentially preventing future visits for hypertensive emergencies and reducing long-term cardiovascular risk.
The next time you see a patient with asymptomatic hypertension and limited access to care, pause to consider whether initiating treatment could be the first step toward lasting cardiovascular protection.
ABOUT THE AUTHORS


Dr. Gozman is associate medical director at the Miriam Hospital emergency department in Providence, Rhode Island, and assistant professor in the Department of Emergency Medicine at Brown University.
Dr. Berlyand is associate director of quality and patient safety, associate director of the Division of Emergency Department Operations and Quality Improvement, and assistant professor in the Department of Emergency Medicine at Brown University. He serves as chair of the SAEM Quality and Patient Safety Interest Group.
RESEARCH

Mapping the Funding Landscape: Using NIH RePORTER to Find and Shape EM Research Proposals
By Arthi Kozhumam; Dalia Owda, MD; and Joseph Miller, MD, on behalf of the SAEM Research Committee
The National Institutes of Health Research Portfolio Online Reporting Tools Expenditures and Results (NIH RePORTER) is a publicly available database that provides access to key information about NIH-funded research projects, investigators, publications, and patents.
This guide highlights practical strategies for using NIH RePORTER to frame grant applications and offers tips to help emergency medicine (EM) researchers maximize efficiency across all stages of grant and career development. A case example at the end illustrates how
these strategies can be integrated into a cohesive grant application.
Finding Institutes, Mechanisms, and Funding
Pathways
The Quick Search function is a useful starting point for an initial overview. Common entry points include principal investigator names, project numbers, or keywords— topics such as resuscitation, trauma, or prehospital care can help EM researchers design their research questions.
For greater specificity, the Advanced Search option provides
filters for activity code (for example, R01, R21, K-series), institute or center, fiscal year, organization, state, and human subjects or clinical trial flags.
Tip: Use the Export feature to download results for further analysis, or create saved searches with automated email alerts to stay updated on new EM-related projects and potential collaborators.
Applying activity code filters helps determine how often particular topics are funded under different mechanisms—R01 versus R21/R03,
NIH RePORTER for Emergency Medicine Grant Development
STEP 1
Initial Search (Quick Search)
Keywords: trauma, resuscitation, etc.
STEP 2
Refine Search (Advanced Search)
Filter by activity codes, institutes, fiscal year
STEP 3
Analyze Gaps & Find Collaborators
Review abstracts, identity research hubs
STEP 4
Use Matchmaker
Paste draft aims to find similar projects
for example—and whether multi-PI structures, career awards, training awards, or center grants are most common for your domain of interest.
R01s often fund multi-site or emergency department implementation science studies, while R21s and R03s typically support pilot studies on novel diagnostic tools or interventions. K awards are common among EM clinician-scientists pursuing protected research time.
Example: If you are developing a multicenter trial on a machine learning algorithm for early sepsis detection in the emergency department, you might search “sepsis emergency department machine learning.” By filtering for R01 and R21 activity codes and NIGMS and NHLBI institutes, you might learn that NIGMS consistently funds emergency department sepsis research, and R21s are often used for early-stage algorithm development.
Identifying Gaps, Collaborators, and Review Pathways
NIH RePORTER - Quick Search
Funding Landscape
• R01 vs R21 patterns
• Institute preferences
• Funding trends
Advanced Search Filters
Research Strategy
• Mechanism selection
• Study populations
• Outcome measures
Project Results - Gap Analysis
R01HL123456 - John Hopkins
Sepsis protocols in urban ED Gap: Rural EDs excluded
Matchmaker Tool
Paste your Specific Aims text here... Analyse
Collaboration Network
• Regional EM hubs
• Co-Investigators
• Implementation experts
Submission Strategy
• Target IC/study section
• Program officer contacts
• Review pathways NIMH (85%) ↓Dr. Jones PO
Within Advanced Search, use the Title, Abstract, and Terms fields to narrow to emergency care–specific areas such as emergency department–based screening, prehospital stroke triage, or disaster response.
Tip: When skimming funded project abstracts, ask three questions:
• What clinical outcomes were assessed (for example, 30-day mortality or revisit rate)?
• What interventions or workflows were tested (for example, pointof-care ultrasound or protocolized sepsis care)?
• What populations were excluded or underrepresented (for example, pediatrics or rural emergency departments)?
Filtering by organization or state/ city helps identify regional EM research hubs—academic medical centers or trauma systems with multiple funded projects. Reviewing publications tied to these projects often reveals statisticians, EMS
collaborators, or implementation scientists who could serve as coinvestigators for multisite or systemsbased work.
To extend this analysis, use the Matchmaker tool. Paste a section of text (such as Specific Aims), and Matchmaker identifies similar projects and the review sections that evaluated them. This is especially helpful for identifying the best NIH home for EM topics, which often span multiple institutes.
Tip: After running Matchmaker, record the top two relevant institutes or centers and associated program officers. Draft a concise outreach email that includes:
• Your EM research problem (for example, delayed tissue plasminogen activator administration in community emergency departments)

Case Example: ED Asthma Treatment Bundle (60
Landscape & Gaps (20 min)
• Search “emergency department asthma”
Map existing interventions
Minutes Total)
Home & Mechanism (10 min)
• Filter by NHLBI, compare R01 vs. R21 density
Result: Targeted Proposal
Review Pathways (10 min)
• Matchmaker with draft aims
Identify program officers
PNHLBI R21 mechanism identified. PDr. Martinez (NHLBI PO) contacted. PThree co-I collaborators recruited.
PGap in pediatric discharge bundles confirmed. P$275k budget validated against peer institutions.
RESEARCH
continued from Page 89
• The target population and setting (for example, rural stroke patients or EMS systems)
• The key innovation (for example, an artificial intelligence triage tool)
• A question about institute or study section relevance
Example: Suppose you are designing an intervention to improve follow-up care after suicidal ideation is identified in the emergency department. Your Advanced Search may reveal gaps in addressing linkage to care beyond the emergency visit. By pasting your specific aims, focused on intervention and follow-up, Matchmaker may identify the National Institute of Mental Health and the Eunice Kennedy Shriver National Institute of Child Health and Human Development as relevant homes, along with several recurring program officer names for outreach.
Using RePORTER and ExPORTER for Portfolio Analysis
For deeper analysis, you can export data from NIH RePORTER or use the ExPORTER platform to download datasets of NIH-funded projects. These can help you analyze funding trends in emergency care—such as which institutes consistently support emergency department–based interventions, trauma care, opioid response, or acute mental health care.
Exported data can be quickly summarized in pivot tables or spreadsheets for inclusion in grant sections.
Case Example: Using RePORTER to Develop an ED Asthma Treatment Proposal
Suppose you propose an emergency department–initiated discharge bundle for acute asthma treatment, including inhaler coaching, a single dose of dexamethasone, and text-based follow-up instructions, hypothesizing that it will reduce sevenday relapses and repeat visits.
In under an hour, NIH RePORTER can help shape every major element of your application:
• Landscape and Gaps (20 minutes): Search “emergency department asthma” and “acute asthma exacerbation,” with filters for R01/ R21, human subjects research, and the past 10 fiscal years. Skim abstracts to map outcomes, interventions, exclusions, and implementation strategies.
• Home and Mechanism (10 minutes): Refine by institute or center, such as the National Heart, Lung, and Blood Institute or the National Center for Advancing Translational Sciences. Compare the density of R01 versus R21 mechanisms to gauge readiness for each.
• Review Pathways (10 minutes): Paste draft aims into Matchmaker to see top institutes, program officers, and study sections. Focus on recurring names as outreach targets.
• Collaborators (10 minutes): Filter by organization to identify centers with pediatric and adult asthma volumes. Use publication networks to identify statisticians, implementation scientists, and pharmacists who could serve as co-investigators.
• Budget Framing (10 minutes): After finding similar projects, copy the Funding Opportunity Announcement numbers and review scope and allowable costs. Export a short list to calculate median per-year costs for comparable funded studies.
This structured approach enables you to create a targeted, competitive proposal aligned with NIH priorities.
Conclusion
NIH RePORTER is a powerful but underused resource for EM investigators. Strategic use of its search functions allows you to assess funding landscapes, collaboration opportunities, study sections, and realistic budget planning. Even brief exploration of this tool can help you approach grant development with clearer direction and better alignment with NIH funding priorities.
ABOUT THE AUTHORS



Arthi Kozhumam is a fourthyear MD-PhD candidate at Northwestern University Feinberg School of Medicine.
Dr. Owda is an emergency physician at Henry Ford Hospital and a clinical assistant professor at Henry Ford Health + Michigan State University Health Sciences.
Dr. Miller is a clinical associate professor of emergency medicine and director of research at Henry Ford Health.
RESEARCH

The Research Wheel: Connecting the Components of a Strong Study
By Susan M. Wojcik, PhD, on behalf of the SAEM Research Directors Interest Group
The Research Wheel: Ensuring Study Cohesion
Conducting research can often seem daunting—a complex puzzle. Developing a research study is less like following a recipe or step-bystep process and more like building a wheel, with each component interconnected to create a cohesive study. A well-structured study is essential for generating reliable and impactful findings.
Visualize the interdependence of the research process as a wheel. At the center—the indispensable hub—lies the research question. A well-defined, focused, feasible, and answerable research question within available resources is the single most important factor for success. A poorly defined or irrelevant research question results in a wobbly, ineffective wheel.
The Research Question
The research question defines what you aim to discover or understand. Every decision, choice, and action in the research process is grounded in this question. It shapes the trajectory of the study, guiding critical decisions and ensuring methodological integrity.
The Importance of Connection: A Wheel in Motion
Just as a real wheel’s spokes are connected by a rim, research components are interconnected. For the wheel to function efficiently, there must be strong connections between the hub and the outer rim, along with a cohesive surface around the entire wheel. The literature search informs the study design; design dictates subject and variable selection; good planning enables effective implementation; data
collection supports robust analysis; and results flow into dissemination. For the research study to keep rolling and yield meaningful, publishable results, all components must be firmly connected to the central research question. A disconnect in any one component weakens the Research Wheel.
The Literature Search
A thorough literature review refines your question, identifies gaps, avoids redundancy, and informs study design, subject selection, variable identification, data analysis, and dissemination plans.
Study Design
The study design serves as the roadmap. It must align with the research question while minimizing bias and maximizing validity. A poorly chosen design can render
“A well-defined, focused, feasible, and answerable research question within available resources is the single most important factor for success.”
even the most meticulous data collection efforts meaningless.
Subject Selection
Define the target population with clear inclusion and exclusion criteria that match your research question and study design to avoid validity bias. Practical considerations during study implementation may require adjustments to data collection or even re-evaluation of selection criteria.
Variable Selection
Identify and define the variables to be measured. Operational definitions for all variables are essential to ensure consistent data collection and meaningful analysis that directly answers the research question.
Study Implementation
This is where theory transitions into practice. It involves obtaining ethical approvals (such as IRB), developing protocols, training personnel, and establishing a timeline.
Data Collection
Data collection informed by the research question ensures accuracy, consistency, and completeness. The nature of the data will dictate the appropriate analysis techniques.
Data Analysis
Data should be systematically organized, cleaned, and analyzed to derive meaningful insights. Appropriate statistical methods depend on study design, variable types, and the research question. The implications of data analysis inform effective dissemination.
Dissemination
Planning dissemination during study development helps set deadlines. Identifying the target audience informs the research question, data

collection, and analysis. Preparing an abstract, presentation, or manuscript alongside the study can result in faster dissemination.
A Seasoned Researcher’s Mindset: Seeing the Whole Picture
The Research Wheel is not just a guide—it represents how seasoned researchers think. They approach a research idea holistically, not as isolated steps but as an interconnected system. This perspective allows them to anticipate pitfalls, optimize study design for rigor, and produce high-quality, impactful research. The experienced researcher understands that the strength of a study lies not in the isolated execution of each component but in the harmonious interplay among them, all anchored by a clear and compelling research question.
Mentoring with the Research Wheel
The Research Wheel offers a powerful visual tool for mentoring young investigators, including medical students, residents, fellows, and new faculty.
• It provides an accessible framework for understanding how all research components interrelate and originate from the research question.
• As learners develop projects, the wheel offers a “big picture” view, ensuring that components are logically linked and contribute to answering the primary research question.
• For more complex studies or grant writing, the wheel reinforces the need


“For the research study to keep rolling and yield meaningful, publishable results, all components must be firmly connected to the central research question.”
RESEARCH continued from Page 93
for a cohesive, well-justified research plan where every element supports the overarching aims.
By using the Research Wheel as a guide, mentors can effectively convey the importance of a cohesive and interconnected research process. It underscores that a well-designed study is not a collection of steps but
an integrated whole—each component essential and directly contributing to answering the central research question.
Summary
The Research Wheel emphasizes not the individual components of research, but the dynamic interconnections that make a study successful, with the research question at its core. Utilizing this conceptual framework, both new and experienced researchers can navigate the complexities of scientific
inquiry more effectively and contribute meaningfully to the advancement of emergency medicine
ABOUT THE AUTHOR

Dr. Wojcik is research director and associate professor at SUNY Upstate Medical University. She provides oversight, leadership, and mentorship in all aspects of research and scholarly activities for the department, and directs the fellow research seminar series, the residency research requirement, and a medical student research elective.

SIMposium: Dr. Lon Setnik’s “Name, Claim, and Aim” Approach to Teaming Through Crisis
By Sarah Rabinowitz, MD; Katherine Stewart, MD, MEHP; Tiffany Moadel MD; Janice Shin-Kim, MD; and Suzanne (Suzi) Bentley, MD MPH,
on behalf of the SAEM Simulation Academy
SIMposium is a bimonthly national presentation series hosted by the SAEM Simulation Academy, showcasing simulation careers and achievements while offering practical insights and reflections from experienced simulation educators. In this installment, an emergency medicine leader outlines a simple, high-reliability framework for building effective teams in crisis.
Introduction

Lon Setnik, MD, MHPE, is an emergency physician and simulationist with more than two decades of
experience in clinical practice, education, and systems improvement. He currently practices at Littleton Regional Hospital, a rural critical access hospital in the mountains of New Hampshire. He is the director of clinical programs at the Center for Medical Simulation and is known for his innovative approaches to faculty development, team training, and critical event management. He is passionate about empowering teams to deliver exceptional patient care by fostering psychological safety, relational excellence, and mastery through experiential learning.
Dr. Setnik presented his work on Name, Claim, Aim at the SAEM
Simulation Academy’s SIMposium Grand Rounds this September.
A Crisis With Strangers
Imagine starting your first shift at a small rural hospital. Just as you settle in, you get an urgent notification: A 12-year-old girl with a dusky appearance is being sent down from the pediatric floor with a suspected tension pleural effusion.
Your pulse quickens. This is an uncommon critical problem. You’re new here. You’re unfamiliar with the workflows, and the limited available consultants are people you’ve never worked with before.
You quickly ask your secretary to page everyone who might
Dr. Lon Setnik
“It’s like batting practice — you take a swing, get instant coaching, and try again.”
help — anesthesia, general surgery, pediatrics, and respiratory therapy.
As the patient arrives, so do the consultants.
Suddenly, you’re standing at the head of a crowded room full of capable strangers. The challenge is clear: “I have to turn this group of people who’ve never worked together into a cohesive team. And I need to do it right now.”
Teaming as a Procedure
Emergency physicians are comfortable with procedures. We break them down into steps, practice them repeatedly, and routinely execute them under pressure. But what about teaming — the process of transforming a group into a unified team during a crisis?
The Center for Medical Simulation in Boston has been working for more than 30 years to advance crisis resource management and team training. Its research shows that during high-stakes situations, creativity is limited and cognitive bandwidth is scarce.
The solution? A simple, repeatable framework — just like the ABCs for resuscitation.
That framework is “Name, Claim, Aim.”
1. Name: Establish a Shared Mental Model
The first step is to actively name what’s happening. This builds a shared mental model, ensuring everyone understands the problem:
“I think this is sepsis.”
“This looks like a tension pneumothorax.”
When a leader verbalizes their thinking, the room comes into

alignment. Without this step, individuals may operate with different assumptions, leading to delays or errors.
2. Claim: Identify Leadership and Assign Roles
Once the crisis is named, someone must claim leadership. That means clearly identifying yourself and your role: “I’m Dr. Lee, and I’ll run this resuscitation.”
The leader then assigns roles explicitly. Even highly skilled clinicians need clarity to prevent duplication or missed tasks:
“Anesthesia, please manage the airway.”
“General surgery, set up for a chest tube.”
“Pediatrics, help with weight-based medications.”
This structure provides stability and allows the team to function efficiently under stress.
3. Aim: Set Priorities and Invite Input
Finally, name the team’s aims — identifying and prioritizing next steps: “Our priorities right now are decompression and stabilization. What am I missing?”
That last phrase — “What am I missing?” — is crucial. It promotes psychological safety, empowering team members to speak up and share critical observations.
At the conclusion of the event, leaders should again seek input: “Anything we could have done better?”
This not only improves outcomes but also fosters team cohesion for future cases.
Practicing Teaming: From Skills to Mastery
The steps of Name, Claim, Aim sound simple, but like any skill, they
continued on Page 99

“The difference between chaos and coordinated care can be as simple as three steps: Name, Claim, Aim.”
SIMULATION
continued from Page 97
require practice. Research on mastery learning indicates that deliberate practice with feedback is the most effective way to develop expertise.
Dr. Setnik advocates a two-step training model:
Step 1: Rapid Cycle Deliberate Practice
Short, focused sessions that emphasize repetition and immediate coaching.
• Practice naming crises.
• Practice claiming leadership.
• Practice aiming priorities and inviting team input.
These exercises don’t require high-tech simulation labs. Even lowtechnology setups can be effective with a dedicated faculty educator to coach, debrief, and provide pointed feedback.
“It’s like batting practice — you take a swing, get instant coaching, and try again.” — Dr. Setnik
Step 2: Immersive Simulation and Debriefing
Once learners are proficient in the basics, they transition to immersive scenarios that incorporate real-world complexity. Adding a deliberate pause early in the scenario allows teams to reflect on their organization before the case becomes chaotic. This reinforces the leadership skill of stopping a disorganized team to reset and reorient.
Coaching vs. Debriefing: A Subtle but Key Difference
It’s important to keep in mind that coaching during rapid-cycle practice
differs from debriefing. Coaching provides real-time, specific feedback on communication and leadership behaviors. Debriefing often happens after the event, allowing participants to reflect on broader themes and dynamics.
Both are essential, but coaching builds skills step by step, while debriefing deepens understanding.
Practical Tips for Implementation
• Start Small: Run 10–15-minute drills focused only on Name, Claim, Aim steps.
• Keep It Simple: Use whiteboards, role cards, or verbal prompts instead of high-fidelity manikins. Provide a critical scenario, ask the learners to name the problem, claim the roles, and identify the aims.
• Build Psychological Safety: Leaders must model openness by soliciting team input — for example, by asking, “What am I missing?”
• Reflect and Debrief: After immersive sessions, debrief and discuss specifics of how leadership emerged and evolved, team dynamics, and how Name, Claim, Aim steps were conducted.
This approach supports learners at all levels.
Conclusion: From Chaos to Coordination
In a crowded ED bay filled with strangers, the difference between chaos and coordinated care can be as simple as three steps: Name, Claim, Aim.
By integrating this framework into everyday practice and simulation training, we can prepare clinicians to rapidly form teams, communicate
clearly, and lead effectively, regardless of the dynamic and potentially chaotic setting.
The next time you face a critically ill patient, remember: Name the problem. Claim the roles. Aim the team. Just like ABCs, these steps aren’t just a framework — they’re a lifeline
ABOUT THE AUTHORS



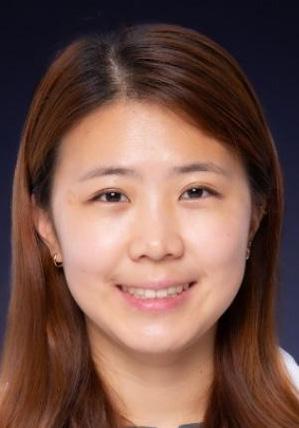

Dr. Rabinowitz is a medical simulation fellow at Northwell Health and with the SAEM Simulation Academy. She serves as an attending emergency physician at Long Island Jewish Medical Center.
Dr. Stewart is a simulation fellow with the SAEM Simulation Academy and an assistant professor of emergency medicine at Tufts University School of Medicine. She works clinically at Maine Medical Center.
Dr. Moadel is president of the SAEM Simulation Academy and director of the medical simulation fellowship within Northwell Health. She is an assistant professor of emergency medicine at the Zucker School of Medicine at Hofstra/Northwell.
Dr. Shin-Kim is director of emergency medicine simulation and an assistant professor in the Department of Emergency Medicine at Columbia University Medical Center.
Dr. Bentley is chief wellness officer at Elmhurst Hospital, immediate past president of the SAEM Simulation Academy, and a professor at the Icahn School of Medicine.
SIMULATION

Beyond the Screen: How Telesimulation Is Transforming Emergency Medicine Education
By Katherine Stewart, MD, MEHP; Sarah Rabinowitz, MD; and Suzanne Bentley, MD, MPH, on behalf of the SAEM Simulation Academy, Early Career Subcommittee
Introduction
As telemedicine cements its place in health care delivery, educators are turning to an equally transformative partner: telesimulation. Telesimulation uses communication technology, such as video conferencing, to provide simulation-based medical education when participants and facilitators are geographically separated. Learners interact with each other, embedded participants, simulated patients and other stimuli displayed via computer screen.
Telesimulation facilitates simulation-based education in locations far from a traditional simulation center (for example, global health applications) or when barriers limit in-person education
(such as during the COVID-19 pandemic). Blending simulationbased learning with virtual platforms, telesimulation is reshaping how clinical skills are taught, practiced and evaluated.
At the September SAEM Simulation Academy Mentor Hour, content experts Neel Naik, MD; Janice Shin Kim, MD; and Debayan Guha, MD, explored the promises and pitfalls of this evolving educational modality.
Panelist Bios
Dr. Lon Setnik
Dr. Janice Shin Kim is director of emergency medicine simulation and an assistant professor in the department of emergency medicine
at Columbia University Medical Center. Her interests include medical simulation, virtual reality and faculty development.

Dr. Debayan Guha
Dr. Debayan Guha is an assistant professor of emergency medicine at Albert Einstein College of Medicine and emergency medicine faculty at Jacobi Medical Center and North Central Bronx Hospital. His academic interests include global health simulation, curriculum design, interdisciplinary team training and using simulation as a driver for quality improvement.
“Blending simulation-based learning with virtual platforms, telesimulation is reshaping how clinical skills are taught, practiced and evaluated.”

Dr. Neel Naik is director of emergency medicine simulation education at Weill Cornell Medicine and faculty and lead educator at the Weill Cornell Medicine Center of Virtual Care, focusing on telemedicine simulation. He also serves as associate medical director of the WCM NYP Simulation Center and the simulation fellowship director.
Defining Telesimulation in Emergency Medicine
Telesimulation is the use of telecommunication and simulation resources to provide education, training, or assessment to learners at an off-site location. It involves physical simulators, task trainers or standardized patients, but is facilitated remotely. Telesimulation also includes simulation-based education delivered through virtual or telehealth platforms to simulate patient interactions and prepare providers for telemedicine practice.
In contrast, virtual simulation refers to a computer-based experience in which the physical world is replaced or simulated with a digital one (for example, virtual or augmented reality), and learners interact with a digital environment rather than physical tools. Remote simulation is a broader term describing any simulation in which participants, facilitators or both are separate. It includes telesimulation, virtual simulation and hybrid models.
Once a niche approach, telesimulation became a staple after the COVID-19 pandemic, enabling high-stakes training in trauma team
coordination, specialist consultations and mass casualty communication. The global shift to remote work didn’t just normalize telehealth — it propelled telesimulation from a backup plan to the front lines of medical education. The objective of this article is to describe telesimulation in emergency medicine, based on expert panel discussion and identified good practices, tips and pitfalls.
Setting the Stage: The Role of Prebriefing
In traditional simulation centers, learners benefit from physical cues, structured environments and face-toface interaction. Virtual simulations require different preparation with targeted prebriefing. Establishing clear ground rules around camera and audio use, creating psychological safety, acknowledging technological limitations and managing expectations all contribute to a session’s success.
When learners feel secure in the virtual space, they’re more likely to fully engage with the clinical content and their team.
Communication in a Virtual World
Without physical presence, instructors and learners lose access to nonverbal cues that aid in high-pressure settings, such as eye contact, posture and tone. In this context, word choice, facial expression and screen setup take on heightened importance. Facilitators must teach both clinical reasoning and how to navigate emotional conversations, such as breaking bad news, over video.
The technical limitations of videoconferencing software must also be considered, including the inability to have more than one person speak
at a time. Small learner groups and breakout rooms for side conversations with consultants or a patient’s family may be helpful. Educators should plan an effective communication strategy for facilitators—such as a separate chat box, text messaging, or a shared document—to track critical actions, provide feedback and modify the scenario in real time if needed.
Despite these challenges, the virtual format offers unique tools: sessions can be recorded and replayed for debriefing, allowing learners to reflect on language, tone and unconscious behaviors, and enabling delivery of simulation content to large audiences.
Keeping Learners Engaged From Afar
Engagement is a perpetual challenge in virtual learning, and telesimulation is no exception. Simulationists have responded with a variety of strategies, including using dual monitors to track reactions, assigning observer roles and building in structured chat prompts.
Facilitators should dedicate time to debrief the technological aspects in addition to the learning objectives, emotional debrief and take-home points. If you choose to call out participants, ensure this is noted in your prebrief and match questions to learner roles (team leader, observer, etc.). Again, small group size is ideal to maintain participant engagement, reduce barriers to speaking up, and ensure psychological safety.
Advancing Technology: Today and Tomorrow
While Zoom remains the default for most telesimulations, educators are
continued on Page 103
Dr. Neel Naik

SIMULATION
continued from Page 101
incorporating enhanced elements like displaying vital signs, diagnostic images or simulated injuries directly on screen. This represents a lowtech, high-fidelity virtual environment, differing from traditional VR by offering immersive cues without costly headsets or proprietary systems.
Looking ahead, AI-powered cofacilitators may soon deliver adaptive feedback in real time. Together, these innovations could expand access to world-class medical training, especially for providers in resourcelimited or remote areas.
Conclusion
As health care becomes increasingly digital, so too must the way we train clinicians. Telesimulation isn’t a temporary workaround; it has
“Telesimulation isn’t a temporary workaround; it has grown into a strategic evolution in medical education.”
Takeaways
grown into a strategic evolution in medical education. It enables scale, encourages reflective practice and prepares providers for modern clinical communication.
With continued innovation in technology and pedagogy, telesimulation will play an increasingly central role in how we deliver and expand access to high-quality clinical training
ABOUT THE AUTHORS

Dr. Stewart is a simulation fellow with the SAEM Simulation Academy and an assistant professor of emergency medicine at Tufts University School of Medicine. She works clinically at Maine Medical Center and has special interest in resident education and enhancing care in behavioral health emergencies.

Dr. Rabinowitz is a medical simulation fellow at Northwell Health and a simulation fellow with the SAEM Simulation Academy. She serves as an attending emergency physician at Long Island Jewish Medical Center. Her interests include quality improvement, improving health care systems and resident education.

Dr. Bentley is chief wellness officer at Elmhurst Hospital, immediate past president of the SAEM Simulation Academy and a professor at the Icahn School of Medicine. Her expertise includes interprofessional education, medical education research, novel simulation initiatives, curriculum design, assessment and global health.
• Prioritize thoughtful prebriefing: Orient learners to the technology, set clear expectations and create psychological safety.
• Utilize structured communication: Limit sessions to four or five participants, consider side channels (such as text, chat or shared documents) and encourage verbal clarity and screen presence.
• Design for active engagement: Use tools such as observer roles, chat prompts and breakout rooms to maintain participation.
• Debrief both content and technology: Keep cameras on to reinforce presence and discuss the emotional impact, clinical objectives and technology used.
• Telesimulation is here to stay: It delivers simulation-based education to remote and resourcelimited settings while expanding the use of augmented reality (AR), virtual reality (VR) and artificial intelligence (AI).

Advancing Health Equity Through Emergency Medicine in Indigenous Communities
By Emma Cortes, DO, and Joseph Ciano, DO, MPH, MS, on behalf of the SAEM Global Emergency Medicine Academy
Life expectancy for American Indian and Alaska Native (AI/ AN) people is lower than for any other racial and ethnic group in the United States. Compared with the general population, AI/AN children experience some of the highest rates of chronic diseases, including diabetes, cardiovascular disease, and depression and anxiety, as well as the highest rates of suicide. There are 574 tribal nations recognized by the U.S. government, not including state-recognized tribes. These
Indigenous communities represent innumerable unique and distinct cultures, all exemplifying resiliency and fortitude in the face of a long history of adversity.
The majority of AI/AN communities live in rural and smalltown areas. Rural populations already face health disparities and reduced access to healthcare With the physician shortage in these areas, emergency physicians can play a crucial role in improving AI/
AN health by expanding access and enhancing quality of care. There are multiple ways physicians can practice medicine in Indigenous communities, with full-time and parttime options that can fit within nearly any career path.
The Indian Health Service (IHS), an agency within the Department of Health and Human Services, was established in 1955 to deliver healthcare to AI/AN populations in the United States. It provides
“A key benefit of the Intergovernmental Personnel Act is that it fosters academic partnerships between universities and hospital sites, creating opportunities for educational collaboration while improving healthcare in one of the most underserved populations in the country.”
ambulatory, inpatient, and emergency care services for those enrolled in federally recognized tribes.
A subset of hospitals that operate under the Self-Determination and Education Assistance Act are sometimes referred to as “638 tribal health systems” or “tribal-operated 638 programs.” These hospitals have the flexibility to contract with the IHS to deliver health services using preexisting IHS resources, third-party reimbursements, grants, and other funding sources.
Both tribal-operated 638 health sites and IHS hospitals offer fulltime employment opportunities for physicians. Within IHS, careers can be pursued through several pathways, including direct tribal hire, civil service, the U.S. Public Health Service (USPHS) Commissioned Corps, and military transition programs. Directly hired tribal physicians receive salary and full benefits as federal employees. Physicians may pursue career growth within IHS and benefit from programs such as loan repayment or credit toward military service.
There are also opportunities for full-time employment within tribaloperated hospital systems. Salary and benefits vary by tribe. Full-time employment postings for both IHS and tribal-operated hospital systems can be found on the official IHS website.
Another option for emergency physicians is part-time or per diem work through locum tenens agencies. These agencies contract with both IHS and tribal-operated
hospitals. Physicians are employed as independent contractors, meaning they are self-employed and responsible for their own benefits and tax obligations. A key advantage of locum tenens work is scheduling flexibility, allowing physicians to design work schedules that best fit their lifestyle. Travel and lodging may be reimbursed depending on the agency. This option suits physicians balancing another career, frequent travel, or semi-retirement while maintaining clinical activity. It also allows physicians to work in a variety of clinical settings.
Federal employees, tribal employees, and independent contractors are protected from personal liability and malpractice under the Federal Tort Claims Act This federal legislation allows parties to file malpractice claims against the federal government and authorizes the government to defend such claims.
Another way for emergency physicians to work in Indigenous communities is through an Intergovernmental Personnel Act (IPA) assignment between an academic institution and an IHS site or a tribal-operated hospital. The act allows a physician to work in an emergency department and cover a predetermined number of shifts within a specific period. Compensation is negotiated through the physician’s academic institution. The Federal Tort Claims Act does not cover physicians working under an IPA, so malpractice coverage must be obtained separately. A key benefit
of the IPA is that it fosters academic partnerships between universities and hospital sites, creating opportunities for educational collaboration for both trainees and faculty while improving healthcare in one of the most underserved populations in the country.
AI/AN populations face distressing health disparities driven by social inequities compounded by the challenges of rural communities. Emergency physicians who bring determination, skill, and cultural humility can make a lasting impact in addressing these inequities. Working to advance health equity within Indigenous communities exemplifies the most meaningful elements of a career in emergency medicine.
ABOUT THE AUTHORS

Dr. Cortes is an emergency and family medicine physician and a global emergency medicine fellow at Brown University. She practices medicine in Indigenous communities in Arizona and South Dakota. She serves as co-chair of the American Indian and Alaska Native Health Committee and on the executive committee for the Global Emergency Medicine Academy.

Dr. Ciano is an emergency medicine physician at Penn Medicine and a global health practitioner. He also practices at Crow/Northern Cheyenne Hospital in rural Montana through the Indian Health Service. He cochairs the American Indian and Alaska Native Health Committee within the Global Emergency Medicine Academy.

Training for the Front Lines: Advancing Tactical Emergency Medicine Education
By Charles Ryan, MD; Daniel Micheller, MD; Florian Schmitzberger, MD, MS; and Jeremy Ackerman, MD, on behalf of the SAEM Tactical and Law Enforcement Interest Group
From Battlefield to Civilian Frontlines
Injuries once confined to military battlefields now occur with alarming regularity in civilian environments, including schools, concerts, places of worship, and other densely populated public spaces. Research examining wounding patterns from U.S. civilian mass shootings between 1999 and 2017 reveals a high rate of potentially preventable deaths.
This evolving pattern has fundamentally reshaped the landscape of trauma care, underscoring the need for rapid, effective intervention in the prehospital setting. Although recent
advancements have improved prehospital trauma management, ongoing research, training, and curriculum development remain essential to further reduce preventable mortality.
Lessons from Tactical Combat Casualty Care
Given these new realities, civilian emergency medicine can benefit from adopting military best practices. Tactical Combat Casualty Care (TCCC) provides an evidencebased framework that addresses the leading causes of preventable death, including extremity hemorrhage, airway compromise, and tension pneumothorax.
Maintained by the Department of Defense through the Joint Trauma System, the TCCC Clinical Practice Guidelines have helped standardize battlefield trauma care. These principles—such as tourniquet use, airway adjuncts, and needle decompression—have clear applications in the civilian prehospital environment and can inform medical education at all levels.
Translating Military Lessons to Civilian Response
Developments in the civilian sector, such as the Stop the Bleed campaign and the Tactical Emergency Casualty Care curriculum, have provided
pathways to bring this knowledge into civilian practice. These programs train community members and prehospital providers to respond effectively in high-risk situations.
TECC modifies the TCCC principles to fit civilian scenarios, accounting for differences in patient populations, responder scope of practice, and available resources. Today, TECC is deployed by a wide range of first responders, including law enforcement, EMS, and fire departments, when they operate in high-risk environments such as mass casualty incidents, law enforcement activities, forest fires, and other hazardous situations.
The core of TECC is a phased approach to care based on the immediate threat level, balancing provider safety with patient needs.
Building Tactical Emergency Medicine Within EM
Tactical Emergency Medicine (TEM) presents a compelling opportunity for the field of emergency medicine to adapt and evolve in response to emerging challenges. In addition to their roles in prehospital care, TEM practitioners can offer unique training opportunities to law enforcement agencies.
This collaboration not only enhances emergency response capabilities but also creates avenues for advocacy regarding use of force and detainee health. TEM providers can further partner with law enforcement on joint projects aimed at advancing public health objectives. Through TEM, healthcare professionals engage in advanced
trauma care, interdisciplinary research, interagency collaboration, and ethical decision-making. Reflecting this increasing relevance, the number of residency and fellowship programs offering dedicated TEM rotations has grown significantly over the past decade.
A Call for Standardized Training
To meet the educational demands of this evolving field, prior efforts have attempted to define competencybased guidelines for various audiences, including law enforcement personnel, medical providers, team leaders, and medical directors.
However, for TEM to mature within emergency medicine, the next critical step is the development of consensusbased, best-practice educational guidelines. These would serve as the foundation for a standardized national curriculum, ensuring that residents and fellows participate in TEM training with clearly defined competencies, ethical boundaries, and measurable learning objectives.
We propose convening a multidisciplinary group of educators and TEM experts to:
1. Compile a national inventory of existing TEM rotations.
2. Abstract and analyze their associated learning objectives and training models.
3. Use Delphi methodology to develop a consensus curriculum and competency framework.
Shaping the Future of Tactical Emergency Medicine
Tactical Emergency Medicine represents an important and growing subspecialty with the potential to
“Tactical Emergency Medicine presents a compelling opportunity for the field of emergency medicine to adapt and evolve in response to emerging challenges.”
significantly improve public safety and prehospital trauma outcomes.
As medical educators, we have a unique opportunity—and responsibility—to shape the future of this discipline by establishing robust, standardized, and ethically grounded training pathways. Doing so will ensure that the next generation of emergency medicine physicians is equipped to meet the evolving threats and care needs of the communities we serve.
To learn more about this project or to join in developing a TEM curriculum, please join the SAEM Tactical and Law Enforcement (TaLEM) Interest Group
ABOUT THE AUTHORS



Dr. Ryan is a second-year emergency medicine resident at the University of Michigan and a former EMT-B and sworn police officer.
Dr. Burke is a second-year resident at the University of Michigan. Lt. Burke currently serves in the United States Navy Medical Corps.
Dr. Micheller is assistant residency program director and adjunct clinical assistant professor in the Department of Emergency Medicine at the University of Michigan, practicing at Trinity Health Ann Arbor.
Dr. Schmitzberger is clinical assistant professor at the University of Michigan. He previously served as a medic in the Austrian military and is currently the medical director for the Genesee County Sheriff’s Department paramedic division and the medical director for the Special Operations Combat Medicine Course at Hurley Medical Center.

Dr. Ackerman is assistant professor in the Department of Emergency Medicine at Emory University School of Medicine. He also serves as a tactical and SWAT physician in Atlanta and is a sworn police officer.
Induce With Caution: The Clinical Relevance of Enzyme Induction in Poisoned Patients
By Andrew Posen, PharmD, and Jennifer Lee, PharmD, on behalf of the SAEM Academy of Emergency Medicine Pharmacists Toxicology Writing Group
The Role of Enzyme Activity in Detoxification
The body’s ability to detoxify and eliminate drugs relies heavily on enzyme activity. In most cases, drugs undergo biotransformation into more hydrophilic compounds by the hepatic cytochrome P450 (CYP) enzyme family and conjugating enzymes such as glucuronosyltransferases. The level of enzyme activity varies according to genetics and clinical conditions, and can be modified by diet, environmental pollutants, and drug therapy.
Both enhanced and depressed enzyme functionality can have toxic ramifications, with drug–
drug interactions being a notable example. Conversely, harnessing this knowledge may inform therapeutic options for poisoned patients.
Understanding Enzymatic Induction
Enzymatic induction refers to amplified enzyme activity occurring as an adaptive response to xenobiotic exposure—the inducer. The specific inductive mechanism is most influential to the clinical effect. Classically, ligand binding and nuclear receptor–mediated transcriptional activation upregulate expression of the target enzyme, with an average onset of one to two weeks.
Some processes occur more rapidly, and the magnitude of induction ultimately depends on the inducer’s potency, dose, halflife, and the affected drug’s halflife. In the context of drug–drug interactions, inducers may enhance the conversion of prodrugs to active metabolites or diminish the effect of active parent drugs.
Common pharmacologic inducers include rifampin, phenytoin, and St. John’s wort. A thorough medication history is essential for identifying these agents and their associated risks. For instance, a patient who initiates the herbal supplement St. John’s wort may experience decreased effectiveness of an
“Both enhanced and depressed enzyme functionality can have toxic ramifications, with drug–drug interactions being a notable example.”
antidepressant regimen. Each inducer functions differently, and the timing and extent of metabolic alterations can have significant clinical implications.
Applications in Poisoned Patients
The application of enzymatic induction to expedite toxin elimination in poisoned patients is uncommon, but not unheard of. In the 2010s, an outbreak of life-threatening bleeding events occurred after recreational use of synthetic cannabis contaminated with brodifacoum, a long-acting anticoagulant rodenticide (half-life greater than 14 days).
Facing potentially months of vitamin K supplementation to manage coagulopathy, daily phenobarbital was proposed as an adjunctive therapy to expedite brodifacoum clearance Phenobarbital is known to upregulate gene expression for numerous CYP enzymes, decrease enzyme catabolism, and increase hepatic blood flow, ultimately enhancing elimination of target substrates as early as three days after initiation after initiation. Results were mixed regarding whether phenobarbital was beneficial for brodifacoum-poisoned patients
A more recent example involves therapies developed for patients affected by SARS-CoV-2 (COVID-19). Organ transplant recipients were identified to be at greater risk for COVID-related morbidity and mortality, yet the popular antiviral therapy posed a significant drug–drug interaction with the immunosuppressant medication tacrolimus. Coadministration yielded profoundly supratherapeutic serum
concentrations, conferring risk for nephrotoxicity and neurotoxicity.
To enhance CYP3A4’s oxidative metabolism of tacrolimus, phenytoin was given. Phenytoin’s mechanism for induction is nuclear receptormediated, suggesting that clinically relevant induction would be delayed at least one week after initiation. Nevertheless, authors of one report concluded there was probable benefit of phenytoin within days.
Limitations and Risks
There are meaningful limitations to the previously mentioned treatments.
Although inducing metabolism with phenobarbital appears to be a practical strategy for reducing the duration and associated costs of brodifacoum-associated coagulopathy, phenobarbital is a sedative that increases emotional lability and risks somnolence
Increasing the risk of falls in patients already at heightened risk for life-threatening bleeds is not ideal, in addition to off-target drug interactions, such as with antiseizure medications
on Page 111

“In order for enzymatic induction to be a feasible intervention in poisoned patients, a rapid onset with minimal adverse effects is ideal.”
TOXICOLOGY
continued from Page 109
or hormonal contraceptives. Phenytoin also has significant adverse effects, including serious drug rashes and neurotoxicity such as nystagmus and ataxia.
Furthermore, it remains controversial whether phenytoin facilitated recovery from tacrolimus toxicity. Tacrolimus normally has an elimination half-life between 10 and 40 hours, with some pharmacogenomic variation. In reported success stories, concurrent administration of phenytoin for two to four days was associated with a decline in tacrolimus serum concentrations at a half-life of 10 to 30 hours. Therefore, it is difficult to ascribe clear benefit.
In order for enzymatic induction to be a feasible intervention in poisoned patients, a rapid onset with minimal adverse effects is ideal. While upregulation of gene expression takes weeks, there are other inductive mechanisms that produce effects more quickly, such as stabilization of mRNA and stabilization of the enzyme against degradation Rifampin is a potent enzyme inducer with a short half-life and widespread effects on metabolism. Clear evidence of induction is observed as early as 2 days after initiation, but its application in poisoned patients is minimal and the risks likely outweigh the benefits. A notable example of rapid-onset induction embraced by the toxicology community is the antidote fomepizole -- used for toxic alcohol exposure or as adjunctive support in acetaminophen toxicity. Similar to ethanol and isoniazid, fomepizole stabilizes CYP2E1 mRNA and protects
against enzyme degradation, which increases the amount of active CYP2E1 and results in enhanced elimination within 36 to 48 hours This is reflected in fomepizole’s standard regimen, whereby the dose is increased at 48 hours to maintain serum concentrations. Induction via post-transcription regulation offers prompt onset of clinical effects, but realistically appears to be limited to naturally unstable enzymes, such as CYP2E1, CYP2A5, and CYP2A6.
Mechanistic Considerations
For enzymatic induction to be a feasible intervention in poisoned patients, a rapid onset with minimal adverse effects is ideal. While upregulation of gene expression takes weeks, other inductive mechanisms may produce effects more quickly, such as stabilization of messenger RNA (mRNA) and stabilization of the enzyme against degradation
Rifampin is a potent enzyme inducer with a short half-life and widespread effects on metabolism Clear evidence of induction is observed as early as two days after initiation, but its application in poisoned patients is minimal and the risks likely outweigh the benefits
A notable example of rapid-onset induction embraced by the toxicology community is the antidote fomepizole, used for toxic alcohol exposure or as adjunctive support in acetaminophen toxicity. Similar to ethanol and isoniazid, fomepizole stabilizes CYP2E1 mRNA and protects against enzyme degradation. This increases the amount of active CYP2E1 and enhances elimination within 36 to 48 hours.
This is reflected in fomepizole’s standard regimen, in which the dose is increased at 48 hours to maintain
serum concentrations. Induction via post-transcription regulation offers prompt onset of clinical effects but appears to be limited to naturally unstable enzymes, such as CYP2E1, CYP2A5, and CYP2A6.
Conclusion
Should inducers be used to expedite toxin elimination in poisoned patients? To date, there is insufficient published evidence to demonstrate clear benefit. In fact, primum non nocere has been quoted in opposition to this strategy in the setting of drug-drug interactions.
Overall, the list of potent and rapidonset inducers is underwhelming due to their off-target activities and side effect profiles. Nevertheless, enzymatic induction remains a theoretically supportive maneuver to expedite toxin clearance. The decision to use enzyme-inducing agents in the management of toxicity should be guided by consultation with a medical toxicologist or poison control center.
Discovery of more specific, safe, and rapid-acting inducers could offer future advancements in the care of poisoned patients
ABOUT THE AUTHORS


Dr. Posen is a clinical pharmacist in emergency medicine at UI Health in Chicago, Illinois, where he completed his Doctor of Pharmacy degree and postgraduate training.
Dr. Lee is the critical care and emergency department pharmacy manager at Inova Fairfax Hospital in Virginia.

When Safe Becomes Deadly: Loperamide Toxicity in the Era of Opioid Misuse
By Liz Uttaro, PharmD and Renee Petzel Gimbar, PharmD
Background
Loperamide is a phenylpiperidine opioid commonly used as an overthe-counter antidiarrheal medication. It stimulates mu-opioid receptors in the gut and blocks intestinal calcium channels, slowing intestinal transit time. It also has antisecretory properties that reduce diarrhea. When taken at higher doses, loperamide can penetrate the central nervous system (CNS) and cause serious adverse effects including respiratory depression,
CNS depression, and cardiac dysrhythmias, which can be fatal.
After oral ingestion, loperamide undergoes extensive first-pass metabolism, resulting in extremely poor bioavailability and limited systemic circulation. Its metabolism primarily involves the CYP3A4 and CYP2C8 enzymes, which convert it to inactive metabolites. Additionally, P-glycoprotein (P-gp) efflux pumps (Figure 1) push loperamide back into the intestinal lumen and bile, preventing accumulation in the CNS and gastrointestinal tract.
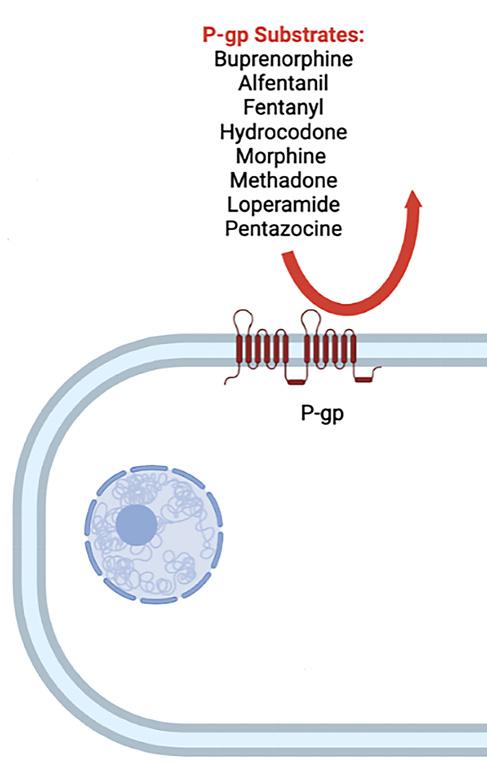
Figure 1: P-gp pump efflux
“When taken at higher doses, loperamide can penetrate the central nervous system and cause serious adverse effects including respiratory depression, central nervous system depression, and cardiac dysrhythmias, which can be fatal.”
Loperamide was originally classified as a Schedule II controlled substance due to its opioid properties and potential for abuse. It was reclassified as Schedule V in 1977 and finally became non-scheduled in 1982 after studies showed a low risk of physical dependence and abuse.
At therapeutic doses (2 to 16 mg per day), loperamide is generally safe. However, in higher doses, it may cross the blood-brain barrier and cause euphoria or respiratory depression. Against the backdrop of the opioid epidemic and restricted access to prescription opioids, a 2025 study analyzed online forums discussing illicit loperamide use. Of 258 posts reviewed, about 70% described using high doses to treat opioid withdrawal, and roughly 25% reported use for euphoria.
Data from the U.S. National Poison Data System (NPDS) showed a 91% increase in loperamide exposure calls between 2010 and 2015. From 2012 to 2017, intentional exposures rose from 92 to 272 cases, most often to self-treat withdrawal symptoms. Reported average daily doses ranged from 160 mg to 400 mg
Mechanism of Toxicity
Toxicity is not expected at therapeutic doses. However, in supratherapeutic doses (more than 16 mg per day), loperamide can overcome P-gp efflux pumps, allowing CNS penetration and serious toxicity.
From 2010 to 2016, the American College of Medical Toxicology (ACMT) Toxicology Investigators Consortium Registry reported 26 cases of

loperamide toxicity. The average daily intake among these cases ranged from 150 to 400 mg.
In addition to taking large doses to relieve withdrawal or achieve euphoria, some individuals intentionally alter loperamide’s metabolism. Substances that inhibit CYP3A4, such as grapefruit juice and cimetidine, can reduce metabolism, while inhibitors of P-gp, such as quinidine and black pepper, increase systemic absorption. Both actions raise CNS concentrations and heighten opioid-like effects.
When systemic absorption is increased, two primary toxicities can occur: opioid toxicity and cardiac toxicity.
Opioid toxicity results from mureceptor agonism in the CNS. Clinical findings include CNS depression,
miosis, and respiratory depression, which can be fatal. Online reports describe near-fatal respiratory depression after high-dose ingestion. In one case, a patient reported taking 72 mg of loperamide with black pepper and experiencing euphoria equivalent to 90 mg of oxycodone.
Cardiac toxicity stems from blockade of cardiac potassium and sodium channels. Potassium channel inhibition can prolong the QT interval, and sodium channel inhibition can prolong the QRS interval, both of which predispose to life-threatening ventricular arrhythmias.
Between 1976 and 2015, the U.S. Food and Drug Administration (FDA) MedWatch database documented
• Clinical Review: Loperamide
• Loperamide Toxicity:
• “I Just Wanted to Tell of Loperamide
• Surveillance of Loperamide
• Loperamide-Related
• Proarrhythmic Mechanisms from the Opioid Abuse
• Potent Inhibition of hERG
• Loperamide-Induced Over-the-Counter Drug
• ACMT Position Statement:
continued from Page 113
48 cases of serious cardiac adverse effects and 10 deaths related to loperamide. Median daily doses in these cases were 250 mg (range 70–1,600 mg). Four cases involved concurrent use of P-gp and CYP3A4 inhibitors.
In 2016, the North Carolina Medical Examiner’s Office reported 19 fatalities associated with loperamide. It was unclear whether deaths resulted from cardiac toxicity or respiratory depression. Other reports describe both monomorphic and polymorphic ventricular tachycardia (torsades de pointes).
Extremely high serum concentrations are required for cardiotoxicity. Potassium channel blockade occurs around 20 mcg/L, sodium channel blockade around 120 mcg/L, compared with a peak concentration of approximately 1 mcg/L after an 8 mg oral dose.
Treatment Overview
Treatment depends on the clinical presentation and may include naloxone or supportive therapy. Initial assessment should follow the ABCs: airway, breathing, and circulation.
If respiratory depression is present, administer naloxone starting at 0.4 mg intravenously and titrate as needed to reverse symptoms. In cases of large
More, Learn More
Loperamide Toxicity
or sustained ingestions—particularly when co-ingested with metabolic inhibitors—a continuous naloxone infusion may be required for recurrent or prolonged respiratory depression.
Gastrointestinal decontamination typically plays a limited role but may be reasonable with early presentation following acute ingestion. Activated charcoal can be considered. Because loperamide is highly lipophilic and protein bound, it is not removed by renal replacement therapy.
Management of cardiac toxicity targets sodium and potassium channel blockade:
• For QRS prolongation, administer 1 to 2 mEq/kg of sodium bicarbonate.
• For QTc prolongation, correct electrolyte abnormalities, including calcium, magnesium, and potassium.
• For ventricular arrhythmias, perform defibrillation or cardioversion depending on pulse presence.
• Torsades de pointes should be treated with 2,000 mg of intravenous magnesium sulfate.
• Persistent bradycardia may require transcutaneous or transvenous pacing, with or without a pure beta agonist such as isoproterenol.
Two salvage therapies —intravenous lipid emulsion (ILE) and extracorporeal membrane oxygenation (ECMO)—have limited supporting evidence but may
Toxicity: Recommendations for Patient Monitoring and Management Tell You That Loperamide WILL WORK”: A Web-Based Study of Extra-Medical Use
Loperamide Ingestions: An Analysis of 216 Poison Center Reports Deaths in North Carolina Mechanisms of the Common Anti-Diarrheal Medication Loperamide: Revelations Abuse Epidemic hERG Channels by the Over-the-Counter Antidiarrheal Agent Loperamide Loperamide-Induced Cardiogenic Syncope: A Case Report of a Life-Threatening Presentation of an Drug Statement: Guidance for the Use of Intravenous Lipid Emulsion
be considered in select cases.
ILE therapy, which theoretically binds lipophilic drugs like loperamide, has shown occasional benefit in case reports, though dosing remains controversial. ILE should be reserved for peri-arrest or cardiac arrest situations.
ECMO may serve as a last-resort intervention for severe cardiotoxicity unresponsive to other measures. However, evidence of survival benefit is lacking, and routine use is not recommended.
Conclusion
Loperamide is a readily available over-the-counter drug that is safe at therapeutic doses but can cause lifethreatening toxicity in large quantities. High doses used for euphoria or self-treatment of opioid withdrawal can lead to both opioid and cardiac toxicities.
Clinicians should consider loperamide toxicity in patients presenting with unexplained ventricular arrhythmias, particularly when there is a history of substance use disorder or electrocardiographic evidence of QRS or QT prolongation. Management is largely supportive and includes naloxone for respiratory depression and targeted therapy for cardiac dysrhythmias. Salvage therapies such as lipid emulsion or ECMO may be considered in refractory cases but should not be used routinely due to limited evidence.
ABOUT THE AUTHORS


Dr. Uttaro is an emergency medicine clinical pharmacy specialist at the University of Rochester Medical Center, Strong Memorial Hospital.
Dr. Gimbar is a clinical professor in the department of pharmacy practice at the University of Illinois Chicago College of Pharmacy and an emergency medicine and medical toxicology clinical pharmacist at UI Health. She directs the postgraduate year two emergency medicine pharmacy residency and was named a fellow of the American Academy of Clinical Toxicology in 2019.

The Hidden Dangers of Nitrous Oxide Abuse: What to KN2OW
By Peyton Matt Johnson, PharmD; Tiana Patriarca, PharmD; and Jessica Rivera Pescatore, PharmD
Background and Emerging Trends
Nitrous oxide is a colorless, nonflammable gas commonly used as an inhalational anesthetic in medical and dental settings. Since its discovery in 1772, it has also been misused for its euphoric and dissociative effects. Historically dubbed “laughing gas,” nitrous oxide gained popularity in the 19th century during so-called “laughing gas parties” among the British elite Today, recreational use has resurged across the globe.
The 2023 Annual Report of the National Poison Data System from America’s Poison Centers® highlighted nitrous oxide as an emerging trend after exposure rates
in the United States nearly doubled from 2014 to 2023. Conventionally available in small canisters known as “bulbs” or “whippets,” nitrous oxide is now increasingly marketed in brightly colored, fruit-flavored branded packaging.
Recent trends show a shift toward large-volume cylinders— some containing the equivalent of 300 standard-sized bulbs—further facilitating heavy recreational use. The perceived safety of nitrous oxide has contributed to rising use among unsuspecting individuals, many of whom are unaware of the gas’s potential for serious neurologic sequelae and systemic harm.
In response to growing public health concerns, numerous countries
and jurisdictions have introduced legislation to restrict access to nitrous oxide; however, enforcement remains variable. Moreover, widespread availability through unregulated sources—particularly online marketplaces and social networks—continues to undermine these regulatory efforts.
Pharmacologic and Toxicologic Mechanisms
The pharmacologic effects of nitrous oxide are mediated through several central nervous system pathways, including its primary mechanism as a competitive antagonist of N-methyl-D-aspartate (NMDA) receptors. While acute nitrous oxide intoxication is infrequently encountered in emergency
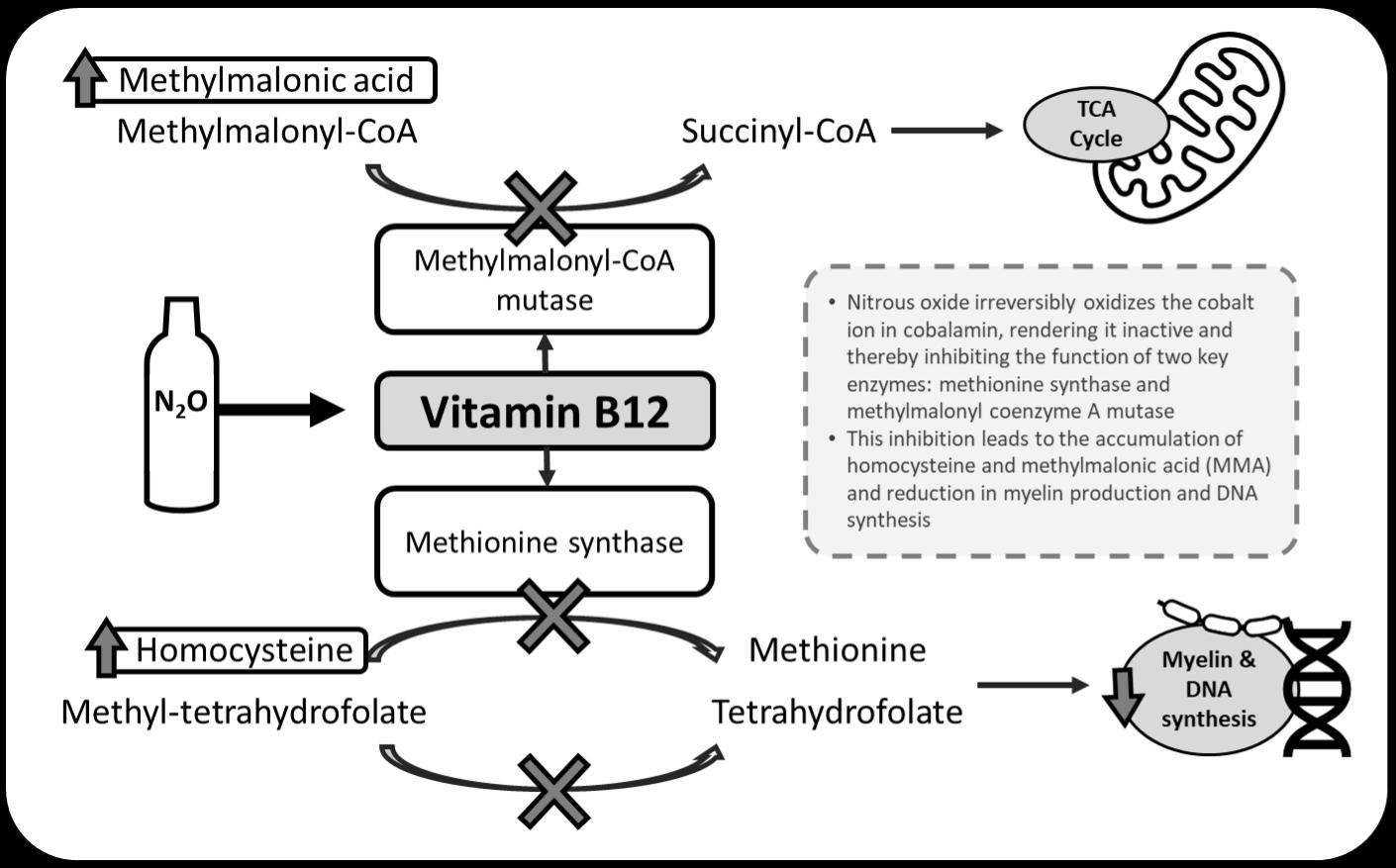
Figure 1 adapted from: Temple C, Horowitz Z. Nitrous oxide abuse induced subacute combined degeneration despite patient initiated B12 supplementation. Clinical Toxicology 2022;60(7):872-875.
“The perceived safety of nitrous oxide has contributed to rising use among unsuspecting individuals, many of whom are unaware of the gas’s potential for serious neurologic complications and systemic harm.”
departments, high-risk inhalation practices—such as inhalation of large volumes in enclosed spaces or direct inhalation from compressed tanks or via a plastic bag or mask method—can result in hypoxia, cold-related injuries, or fatal asphyxiation.
The toxic effects of nitrous oxide are predominantly neurologic and hematologic and result from a functional deficiency of vitamin
B12 (cobalamin). Nitrous oxide irreversibly oxidizes the cobalt ion in cobalamin, rendering it inactive and thereby inhibiting the function of two key enzymes: methionine synthase and methylmalonyl coenzyme A mutase. This disruption impairs the production of myelin and synthesis of DNA, contributing to demyelinating neuropathies and bone marrow suppression, respectively.
Functional B12 deficiency also leads to the accumulation of homocysteine and methylmalonic acid (MMA), which are often elevated in heavy use and can serve as biochemical markers of toxicity.
Clinical Manifestations
Clinically, nitrous oxide toxicity often manifests as subacute combined
continued on Page 119
“Long-term recovery sustained cessation of intervention offering

from Page 117
degeneration (SCD) of the spinal cord. Patients typically present with ascending weakness, gait ataxia, paresthesias, and loss of vibration and proprioception. The lower extremities are often affected first, with distal weakness greater than proximal, and a stocking-glove distribution of motor and sensory deficits. A positive Romberg sign is commonly revealed on physical examination and patients may report frequent falls or need for assistance when ambulating.
Additional findings, such as megaloblastic anemia is frequently encountered. Psychiatric symptoms, including hallucinations and neurocognitive changes, as well as thrombotic complications, such as venous thromboembolism, have been reported
Diagnosis and Evaluation
Diagnosis requires a high index of suspicion, supported by a thorough history and physical examination that considers alternative etiologies affecting the dorsal and lateral spinal cord. Laboratory evaluation should include a complete blood count with mean corpuscular volume (MCV), serum vitamin B12, serum folate, homocysteine, and methylmalonic acid (MMA).
It is important to note that serum vitamin B12 assays measure total cobalamin and cannot distinguish between active and inactive forms; thus, levels may appear normal in some patients, particularly those who self-supplement based on information obtained through online forums or other nonmedical sources.
Hospital admission should be considered for patients presenting with significant motor and sensory deficits, rapid progression of symptoms, or inability to safely ambulate. Inpatient management allows for prompt initiation of parenteral vitamin B12 therapy, advanced imaging, and multidisciplinary care.
Vitamin B12, 1,000 micrograms intramuscularly daily, should be initiated and continued for a minimum of seven to 14 days. Magnetic resonance imaging (MRI) of the spinal cord is recommended to assess for characteristic findings of SCD, including symmetric high intensity signal in the dorsal column seen in T2-weighted axial images, known as an inverted V-sign. Imaging also helps exclude alternative or coexisting pathologies.
Long-term recovery is possible but depends primarily on sustained cessation of nitrous oxide use. Vitamin B12 therapy is essential, though assessing treatment response can be challenging due to the functional nature of the deficiency. Homocysteine serves as a more sensitive biomarker, while MMA is more specific; both should normalize with adequate B12 supplementation and cessation of nitrous oxide use. Neurologic recovery may be gradual and, in some cases, incomplete—but with early recognition and sustained intervention, meaningful improvement is achievable.
The Role of Emergency Clinicians
Emergency clinicians are uniquely positioned to recognize the complications of chronic nitrous oxide abuse early and to collaborate with regional poison information centers
recovery is possible but depends primarily on of nitrous oxide use, with early recognition and the best chance for meaningful improvement.”
and medical and clinical toxicologists to initiate a comprehensive workup that facilitates seamless inpatient management.
By ordering critical diagnostic tests—such as serum homocysteine, methylmalonic acid, and spinal MRI—starting parenteral vitamin B12 therapy, and consulting physical therapy and addiction medicine when appropriate, emergency clinicians can provide inpatient teams with a well-coordinated and diagnostically informed foundation for continued care.
Similarly, emergency clinicians play a key role in initiating an adequate outpatient regimen and ensuring structured follow-up is in place for patients with milder symptoms who do not meet criteria for hospital admission. Emergency clinicians, including pharmacists, can work with their institutions to institute ambulatory pathways in collaboration with regional poison information centers and medical and clinical toxicologists.
This proactive approach not only accelerates treatment but also enhances diagnostic clarity, reduces unnecessary delays, and ensures continuity of care across disciplines
ABOUT THE AUTHORS



Dr. Johnson is a pharmacy resident at Jackson Hospital and Clinic in Montgomery, Alabama. He is a seasoned medic with extensive military and emergency medical services.
Dr. Patriarca is a clinical toxicology fellow at the Alabama Poison Information Center in Birmingham, Alabama.
Dr. Rivera Pescatore is the clinical director of the Alabama Poison Information Center and an assistant professor in the Department of Emergency Medicine through the Office of Medical Toxicology at the University of Alabama at Birmingham.
TRAINEE TOOLKIT

EM Clerkship Myths: What You Need to Know, Part 2 — The Truth About Interviews
By Moises Gallegos, MD; Corlin Jewell, MD; and Bradley Hernandez, MD, on behalf of the SAEM Clerkship Directors in Emergency Medicine
Myth: The more interviews, the better.
Truth: When it comes to interviews, this is not necessarily correct. Most students should aim to complete 10 to 12 interviews at the programs where they are most interested. After that, the likelihood of finding a “diamond in the rough” program to rank in the top three—the range where students are statistically most likely to match—is fairly low.
Remember that interviews are hard work. They take preparation,
dedicated time, and cognitive energy. Tackling too many interviews may cause you to reach your limit, and it will show in your performance. It also could take an interview opportunity away from another applicant who may be more interested in that program.
Applicants with academic difficulties, potential red flags, or who are couples matching may require extra interviews. Those applicants should discuss their interview schedule with their emergency medicine advisor.
Myth: You will learn everything you need to know on interview day.
Truth: A good interview comes from advance preparation. Review a program’s website and any provided resources. From these sources, create questions that help you understand how you might fit within the program and how it could satisfy your interests.
You cannot have too many questions. You will be asked, “Do you have any questions?” frequently during your interview days. Having
“You will be asked, ‘Do you have any questions?’ frequently during your interview days. Having questions prepared, even if you need to reference your notes, will be noticed and appreciated by interviewers.”
questions prepared, even if you need to reference your notes, will be noticed and appreciated by interviewers. Conversely, a lack of questions may be seen as unprepared or disinterested. Avoid asking about information that is clearly available on the website—such as salary or benefits—as it can convey a lack of preparation.
Myth: Interview socials are optional.
Truth: While interview socials are not technically mandatory, you should not dismiss them as optional. Programs spend considerable time and effort planning these events. While some programs have returned to in-person events, most remain online.
Virtual socials may not be everyone’s favorite activity, but residents take time from their busy schedules to attend. Your absence will be noticed. Legitimate reasons such as being on call or working an evening shift are understandable, but we don’t recommend skipping a great opportunity to gauge the resident culture and ask about their experiences in the program.
This is the time to ask about work-life balance, challenges in the program, and social life—topics you wouldn’t raise on your interview day. Remember, residents are also evaluating you and have input into the rank list, so show up with interest and enthusiasm.
Myth: Wild and crazy questions are common.
Truth: It is uncommon for interviewers to ask bizarre questions or present
rare medical scenarios. Don’t worry about being psychoanalyzed by questions like, “What is your spirit animal?” or “Who would play you in a movie?”
In general, emergency physicians are a laid-back group. They want to get to know you as a person, learn about your path to residency, and understand what makes you unique. Provide honest and professional answers and avoid anything controversial. Cursing, stereotyping, and overly casual remarks should be avoided.
Myth: Interview aesthetics don’t matter.
Truth: You want to appear professional during your interview. Make sure you have a quiet environment, strong internet connection, and a neutral background. It’s fine to use a plain white wall or a tidy, professional space such as a cubicle at your medical school.
If you are interviewing from home, putting effort into a clean background will be noticed and appreciated. Avoid cluttered or distracting surroundings and remember that anything visible behind you is fair game for discussion. Your attire should be clean and professional. Interviewing in your bedroom with an unmade bed or clothes on the floor will be seen as sloppy.
Myth: Canceling interviews can happen whenever.
Truth: The sooner you cancel, the better. Interviews are valuable and limited. Canceling early allows the
program to offer your slot to another applicant and gives others a chance to fill their schedules.
It’s important not to cancel with less than seven to 10 days’ notice. At that point, programs often cannot reschedule another applicant, which reflects poorly on you. Mishandling a cancellation can affect your reputation elsewhere—program directors talk to each other more than you might think.
Finally, it’s good etiquette to email the program director if you cancel to thank them for the opportunity.
ABOUT THE AUTHORS

Dr. Gallegos is a clinical associate professor with the Stanford Department of Emergency Medicine. He serves as core residency faculty and clerkship director for the required emergency medicine rotation. He is a member-atlarge for SAEM Clerkship Directors in Emergency Medicine and the SAEM Academy for Diversity and Inclusion in Emergency Medicine executive committee.


Dr. Jewell is director of medical student education and assistant professor of emergency medicine at the University of Wisconsin School of Medicine and Public Health. He is currently working toward a master’s degree in health professions education at the University of Illinois Chicago.
Dr. Hernandez is senior staff physician at Regions Hospital in St. Paul, Minnesota, and assistant professor in the Department of Emergency Medicine at the University of Minnesota Medical School. He is an assistant residency director, clerkship director, and gameday physician for the Minnesota Vikings.
TRAINEE TOOLKIT

Finding Your Focus: Deciding Whether Fellowship Training Fits Your Emergency Medicine Career
By Meta Carroll, MD, on behalf of the SAEM Pediatric EM Interest Group
Introduction: Training to Master Three Core Areas
As emergency medicine residents, you are being trained to master three areas: resuscitation, unscheduled care, and problem-solving. This is no small undertaking. EM residency places mental, psychological, and physical demands on each trainee while building substantial clinical and communication skills.
As you progress in residency— with your intern year of exhilarating and sometimes frightening firsts behind you—it’s time to put a new “metafocus” on your clinical and academic learning.
Defining “Metafocus”
We all understand focus in the emergency department—the fully “in it” moments of performing a new procedure, listening closely to a patient’s story, or learning nuanced decision-making from your attending.
Metafocus means you are not only attentive to your learning, but also aware of its impact on you—and, potentially, on your future—as a physician.
A Case Study in Metafocus
While I was on a toxicology rotation as a third-year resident, our team
was consulted on a 2-year-old who drank from a half-full glass of alcohol left within reach at a family gathering. Somnolent on presentation, the child’s alcohol level was 220 mg/dL, requiring an overnight ICU stay.
He woke the next day irritable, prompting jokes about the “hungover” toddler—but my metafocus sparked a realization. I had learned countless toxicology facts, but the poisoned patients I most enjoyed treating were children. And the adults I most wanted to teach were motivated parents and caretakers—people who might ignore advice about their own health but would move mountains for their kids.
“Begin your fellowship consideration by focusing on the patient population or intellectual pursuit that interests you most.”
That awareness led me from toxicology to a pediatric ED elective, a pediatric emergency medicine fellowship, and ultimately, a career in PEM.
Is Fellowship Training Right for You?
The answer begins with a foundational question: Which cases, clinical conditions, people, or intellectual pursuits get you excited to show up and learn more?
Your discovery may come slowly—or in a single “aha” moment like mine— but when that excitement hits, pay attention.
Fellowship Options for EM Physicians
Fellowships offering subspecialty certification by the American Board of Emergency Medicine (ABEM) include:
• Critical care medicine
• Emergency medical services
• Health care administration
• Hospice and palliative medicine
• Medical toxicology
• Neurocritical care
• Pain medicine
• Pediatric emergency medicine
• Sports medicine
• Undersea and hyperbaric medicine
You can also earn a Focused Practice Designation in advanced emergency medicine ultrasonography.
Additional subspecialty certifications for EM graduates are available through other American Board of Medical Specialties (ABMS) boards and accredited universities. These include addiction medicine, translational research, global health, implementation science, brain injury
medicine, health equity, narrative medicine, clinical informatics, and surgical critical care. Some require only 12 months of additional training.
Start With What Inspires You
You’ll receive plenty of advice to plan your career based on lifestyle, income, or location. These are important, but don’t fall into the trap of seeking a “perfect” combination.
Begin your fellowship consideration by focusing on the patient population or intellectual pursuit that interests you most. That approach leads to a specialization that keeps you curious and challenged—and supports longterm satisfaction.
Fellowship as a Buffer Against Burnout
Long before the COVID-19 pandemic, burnout in emergency medicine was identified at rates more than three times higher than in other specialties. The risks are well documented: infectious disease exposure, interpersonal violence, malpractice claims, unpredictable volumes and acuity, circadian disruption, and cognitive overload under the “pressure for perfection.”
Developing a career niche or area of expertise can help offset these stressors by restoring a sense of control and meaning in your professional life.
Do Your Research and Seek Mentorship
When exploring fellowship programs:
• Review details on the ABEM website and individual program sites.
• Seek mentorship within your residency, hospital, or university—and at regional or national conferences.
• Attend webinars and info sessions.
• Consult your program directors, faculty, and current fellows for guidance.
The Accreditation Council for Graduate Medical Education (ACGME) also provides essential information on emergency medicine subspecialties, including program requirements, application details, and survey data from faculty and trainees.
Clinical fellowship programs are designed to expand your skill set, provide graduated responsibility, offer research and elective time, and prepare you for successful board certification and career transition.
Lifelong Learning Beyond Residency
Not all career-defining decisions need to happen during residency. Many physicians pursue further education in epidemiology, public health, medical education, clinical bioethics, or quality improvement—sometimes mid-career or later.
Conclusion: Focus on a Fulfilling Future
Congratulations on your EM residency path. Your teachers are helping you build mastery in resuscitation, in the provision of unscheduled but compassionate care, and in complex medical and psychosocial problemsolving—often for patients who feel unseen elsewhere.
The demands of this specialty are real, but an EM career offers immense value and meaning. Fellowship training can deepen that fulfillment by helping you find your niche, sustain your growth, and ensure a long, rewarding professional journey.
Ready for some metafocus on yourself and your training? It’s worth it—for an EM career that inspires your best work.
ABOUT THE AUTHOR

Dr. Carroll is a clinical assistant professor at Northwestern University Feinberg School of Medicine and a distinguished clinician in the department of pediatrics at Ann & Robert H. Lurie Children’s Hospital of Chicago.
TRAINEE TOOLKIT

FOAM in Emergency Medicine: Power, Potential, and Pitfalls
By Loraine Ochoa
In recent years, emergency medicine has led a quiet revolution in how knowledge is accessed, shared, and applied—driven by Free Open Access Medical Education, or FOAMed. Born from the idea that medical education should be available to anyone, anywhere, FOAM encompasses a growing ecosystem of blogs, podcasts, videos, and social media threads that are freely accessible online. For trainees and seasoned clinicians alike, FOAM is transforming medical learning from static texts to dynamic, communitydriven platforms.
Why Emergency Medicine and FOAM Work Hand in Hand
Emergency medicine is uniquely suited to FOAM’s model. In a specialty defined by its fast pace and evolving evidence base, clinicians increasingly rely on these resources for up-to-date information. Many emergency medicine residents report using FOAM more frequently than traditional textbooks, drawn to its conciseness, accessibility, and relevance to clinical practice.
Platforms such as X (formerly Twitter), Reddit, and podcast apps have become informal classrooms for learners seeking
practical insights on everything from resuscitation techniques to toxicologic emergencies.
What FOAM Covers—and What It Misses
Notably, some topics receive disproportionate attention in FOAM. A review of nearly 900 online educational posts revealed a heavy emphasis on procedures, especially airway management, ECG interpretation, point-of-care ultrasound, and critical care. Subtopics such as acute coronary syndrome, sepsis, and diabetic ketoacidosis were among the most frequently discussed.
In contrast, areas such as obstetrics and gynecology, psychiatry, and ear, nose and throat topics were significantly underrepresented— raising concerns about potential knowledge gaps when learners rely solely on FOAM.
The Strengths of FOAM
While textbooks remain foundational for their comprehensive and peerreviewed content, FOAM resources offer a key advantage in timeliness— able to incorporate practice-changing evidence within days of publication. This makes FOAM particularly valuable for staying current on new research and evolving best practices.
FOAM also fosters a global, interdisciplinary community of educators and learners, encouraging collaboration and flattening traditional academic hierarchies.
Addressing Quality and Credibility
Despite these benefits, FOAM is not without limitations. One of the most persistent critiques is variability in quality and the lack of standardized peer review. Because many FOAM resources are self-published, content accuracy and depth can vary widely. This variability presents a risk when learners rely on FOAM as a primary source of education, potentially missing essential material covered in more structured curricula.
“Free Open Access Medical Education is transforming medical learning from static texts to dynamic, community-driven platforms.”
Several tools have emerged to help address these challenges. The Social Media Index, or SMI, was an early attempt to quantify the reach and influence of FOAM content creators. More recently, the METRIQ collaboration has developed structured quality assessment criteria through expert consensus. The METRIQ tool offers a framework to evaluate online educational resources based on clarity, transparency, and evidence-based content. These tools can help learners and educators identify high-quality materials and promote more intentional use of FOAM.
Integrating FOAM into Formal Education
Ultimately, FOAM is best viewed as a powerful adjunct to formal medical education. It thrives in areas where rapid updates and niche content are valuable, but it may lack the breadth needed for board preparation or
Leading FOAM Resources
A variety of widely used resources exemplify the breadth and utility of FOAM:
• Life in the Fast Lane (LITFL): One of the earliest and most comprehensive FOAM blogs, known for clinical pearls, ECG tutorials, and case-based learning.
• Academic Life in Emergency Medicine (ALiEM): Integrates digital scholarship with mentorship and curated educational content.
• EMCrit: Focuses on high-yield content in critical care and resuscitation, often geared toward experienced clinicians.
• Rebel EM: Offers concise, evidence-based reviews of emerging literature, useful for staying current.
• EM Cases: Delivers case-based podcast episodes and written summaries covering a wide range of emergency medicine topics.
• The Skeptics’ Guide to Emergency Medicine (The SGEM): Focuses on critical appraisal and translating cutting-edge research into clinical practice.
full-spectrum clinical competency. Awareness of its limitations is key. Learners should be encouraged to engage critically with FOAM, supplement it with comprehensive resources, and reflect on topic areas that may be underrepresented.
Looking ahead, FOAM’s influence in emergency medicine shows no signs of slowing. The next frontier may involve greater integration with formal curricula, blending the flexibility of FOAM with the structure of traditional education. Residency programs are increasingly recognizing FOAM content as legitimate asynchronous learning material, and academic journals have begun to cite blog posts and podcasts as scholarly contributions.
There’s also potential for emerging technologies—such as artificial intelligence, mixed reality, and interactive simulation platforms—to intersect with FOAM, ushering in a new era of immersive, learnercentered education.
The Bottom Line
FOAM continues to shape how emergency clinicians engage with knowledge. Its value lies in accessibility and agility—but its optimal use requires critical appraisal, awareness of content gaps, and thoughtful integration into a broader educational foundation.
ABOUT THE AUTHOR

is a fourth-year medical student at Robert Wood Johnson Medical School pursuing a career in emergency medicine. She served as a medical student ambassador at this year's SAEM annual conference.
Loraine Ochoa
TRAINEE TOOLKIT

Making the Most of Your Clinical Global Health Elective
By Youssef El Rahimy, MD; Ann Pearson, MD; and Nita Avrith, MD, MPH
Global health electives are popular among medical students and residents. Here are some tips to get the most out of your next clinical global health elective.
Know
What You Have and What You Can Do
Before your trip, familiarize yourself with the local burden of disease and standards of care. A good starting point is the Centers for Disease Control and Prevention’s (CDC) country-specific travel health information, but you should also review regionally relevant guidelines, such as those from the World Health Organization or local ministries of
health. These resources will help you anticipate common clinical presentations and prepare for diseases that may be less familiar from your U.S. training, including tropical infections, late-stage chronic diseases, or malnutrition.
In anticipation of limited internet access, download or bring print versions of any clinical references you rely on. Apps like UpToDate or CorePendium often offer offline functionality with preparation. Once you arrive on site, take time to assess the available infrastructure: What medications are regularly stocked? What diagnostic tools are
accessible? Are there specialists or referral centers nearby? Getting clarity on these questions will help you calibrate your diagnostic and therapeutic decisions to the setting.
“Cultural humility is key to building trust with patients and local colleagues.”
Understanding limitations is not about lowering your standards; it’s about delivering thoughtful, contextappropriate care. That might mean managing conditions empirically, modifying medication choices based on supply, or identifying what problems can safely be deferred or referred. Knowing in advance how and where escalation of care can happen— whether that’s a local pharmacy, a secondary clinic, or a regional hospital—can make the difference in navigating complex cases effectively.
Know How Your Care Fits Into the Patient’s Larger Healthcare Journey
Delivering meaningful care in a global health setting requires more than clinical competence—it also demands an awareness of how your role fits into the broader healthcare ecosystem. In some cases, you may be one link in a well-functioning chain; in others, you may be the patient’s first and only contact with the healthcare system. The context in which you practice should shape both your clinical decisions and your communication.
For instance, starting a patient on long-term treatment—such as antihypertensives, insulin, or antiepileptics—may be harmful if the patient cannot reliably refill medications or return for follow-up. In such cases, consider whether a nonpharmacologic approach or a referral to local care might be more appropriate. Talk with local staff to understand how patients typically access chronic disease care, and factor this into your decisions.
Before you arrive, try to learn about the structure of the local health system. Is there universal coverage? Are services free at the point of care? What types of facilities exist, and how do patients navigate between them? Having even a rough understanding of these elements will help you make more informed and sustainable choices.
Finally, remember that your documentation may be one of the few lasting clinical records for this patient. Write clearly and avoid using
abbreviations or specialty-specific terminology. Assume the next provider may not share your language, training, or assumptions but may still rely on your notes to understand what has been done and why. In this way, you can contribute to a continuum of care, even if your presence is short term.
Familiarize Yourself With the Local Community
Before departure, take time to read about the country’s history, people, and culture. Within healthcare systems, differences in how communities perceive illness, the role of traditional healers, and expectations around patient autonomy and provider authority can be significant. Speak with people who have worked within the local community to gain insight into cultural nuances and the clinical experience. Be prepared for different daily workflows, sometimes based on local or cultural norms.
On the ground, cultural humility is key to building trust with patients and local colleagues. Approach each interaction with respect, curiosity, and a willingness to learn. Making the effort to learn a few key words or phrases in the local language will also be extremely helpful. Ensure you will be working alongside either a professional medical interpreter or a local provider to help bridge language gaps and ensure respectful, effective, patient-centered care.
Build Real Relationships
The most meaningful global health electives are built on relationships with the community you’re working with. Before committing, ask if the program has genuine local buyin. Are community members and organizations involved in planning, and does the work continue after you leave?
Partnerships should be grounded in exchange. As a trainee, recognize that you will learn just as much from local colleagues as you are able to teach. Reciprocity comes from consistently showing up, listening to what the community values, and supporting efforts that last. Look for programs that have written memorandums
of understanding (MOUs). MOUs formalize these commitments and clarify the responsibilities of both parties.
When you return home, stay connected with the community, share your experiences in ways that highlight your hosts, and think about how you can contribute again. That is how short-term rotations can have a long-term impact.
Ethical Considerations
Every elective brings ethical questions, starting with your own motivation. Are you going primarily for personal experience, or does the community benefit as well? Global health settings can be resource-limited, and your presence may add to the workload. It is important to respect local practitioners and stay within your scope of training. Practicing procedures you would not be allowed to do at home, or offering help without considering sustainability, can cause more harm than good.
An ethical elective emphasizes mutual benefit and strengthening local systems, not creating dependency. Approach each situation with humility, be willing to step back when needed, and look for ways to contribute that will continue to support the community after you leave.
ABOUT THE AUTHORS



Dr. El Rahimy is an instructor of emergency medicine and a global health fellow at Mount Sinai Morningside/West.
Dr. Pearson is an assistant professor of emergency medicine and a global health fellow at Mount Sinai Morningside/West.
Dr. Avrith is an assistant professor of emergency medicine and the program director for the global health fellowship at Mount Sinai Morningside/West.
GUARD: A Simple Gastric Ultrasound Protocol for Aspiration Risk in the GLP-1 Era
By Allyson Hansen, DO, and Charlotte Derr, MD
The Question at the Bedside
As more patients arrive at the emergency department on GLP1 receptor agonists (GLP-1 RAs) such as semaglutide, one question keeps surfacing: What’s really in the stomach when it’s time to sedate?
Traditional fasting rules don’t always tell the full story. Gastric point-of-care ultrasound—quick, bedside, and reproducible—offers a practical way to directly assess aspiration risk, particularly in patients who may present a difficult airway.
Why It Matters
GLP-1 RAs slow gastric emptying. Even when patients stop these drugs
and report fasting, residual gastric contents may persist, raising the risk for aspiration during procedural (moderate) sedation.
This matters for clinicians who can’t delay care and need a rapid, patient-specific answer: empty or full stomach?
Policies from professional organizations vary because limited high-quality evidence surrounds GLP1 RAs and aspiration risk.
The American College of Emergency Physicians (ACEP) Clinical Policy, last updated in 2018, states not to delay emergency department procedural sedation based on fasting time alone, as pre-
procedural fasting times have not shown a reduction in aspiration risk.
The American Society of Anesthesiologists (ASA) Clinical Practice Guidance, updated in 2024, takes a slightly different stance: those at increased risk of delayed gastric emptying—such as patients just starting GLP-1 RAs or in the escalation phase—should consider gastric ultrasound to evaluate stomach contents or delay elective procedures.
Several small studies have shown residual gastric content in fasting individuals on GLP-1 RAs compared with those not taking them. This suggests a risk-stratified approach, which gastric ultrasound can help guide.
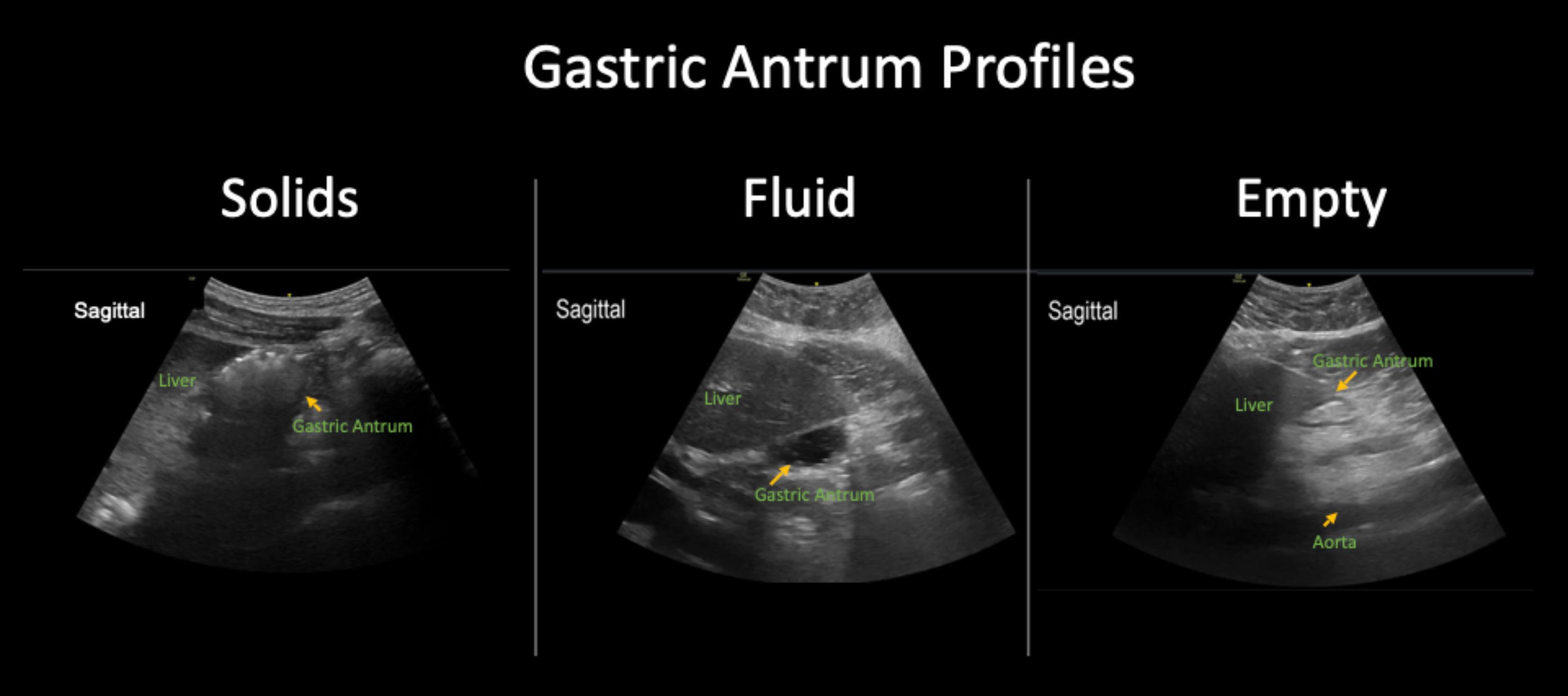

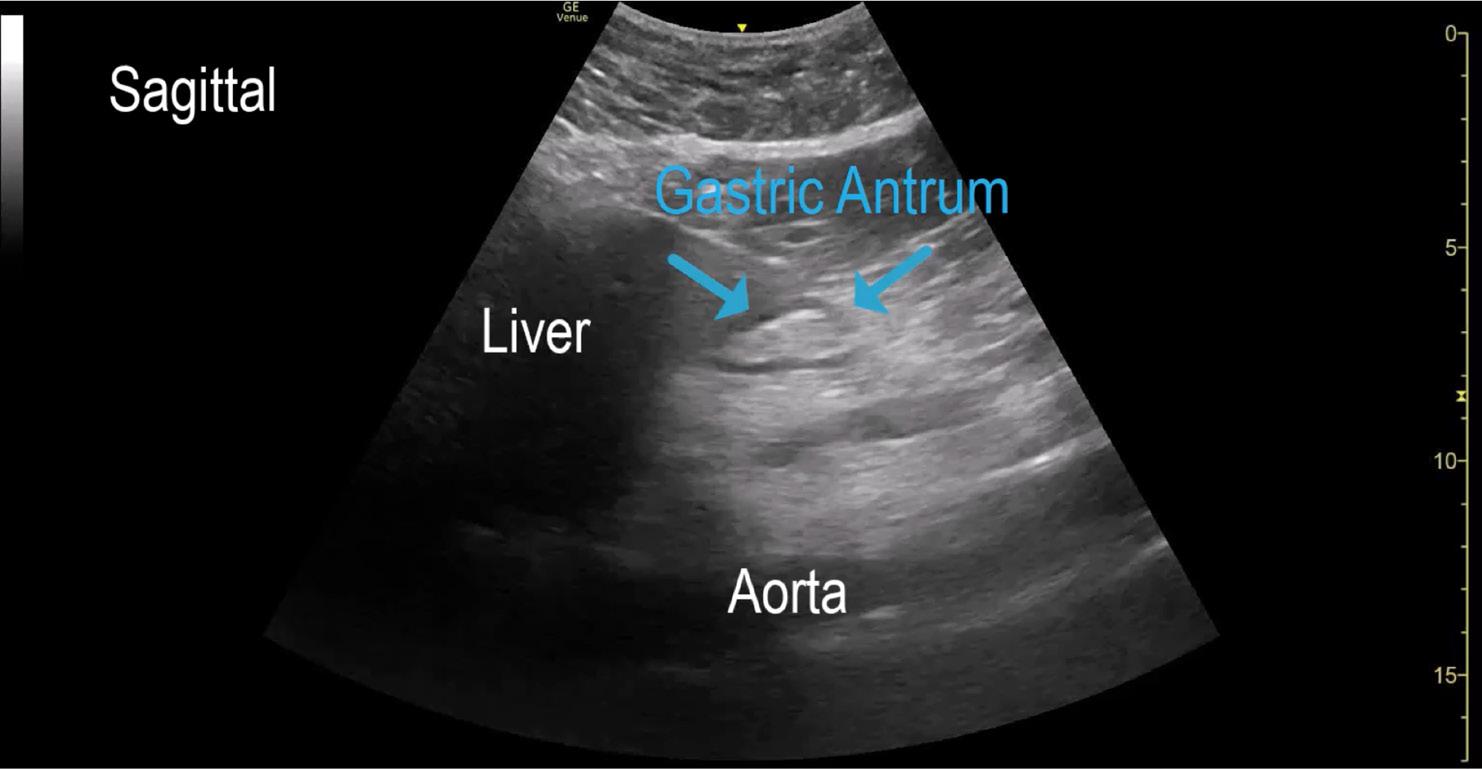
antrum! We see the medial liver to the left of the image, subcutaneous fat in the near field and long axis of the aorta in the far field. In the center is the gastric antrum. Note the hypoechoic outer wall - a classic finding when it comes to identifying the gastrointestinal system on ultrasound. This is an empty gastric antrum as you can see the hyperechoic inner mucosal walls juxtaposed.
A Practical, Fast, Bedside Tool
Gastric ultrasound has been extensively studied in adults and children and used as a valuable tool for assessing aspiration risk before anesthesia and endoscopy procedures—often performed without a secured airway.
Studies in anesthesia have shown that it can reliably predict gastric content and volume, helping identify patients at risk of aspiration. The technique demonstrates strong correlation with endoscopically
measured gastric volumes and can be applied to various patient populations, including those with obesity.
Many ultrasound examinations require significant practice to master, and bedside performance may not always be as fast as hoped in a busy emergency department. However, gastric ultrasound is surprisingly easy to learn, works well across body types, and can be completed in minutes.
Performing the Scan
Use a low-frequency curvilinear transducer to penetrate deeply into the
abdomen with the patient in a supine position.
1. Probe placement: Position the probe in the sagittal plane at the epigastrium or upper abdomen.
2. Landmarks: Identify the long-axis aorta in the far field and the medial edge of the liver in the near field to locate the gastric antrum between them (see Images 1–2).
Image 2. This is in the sagittal plane at the epigastrium with a curvilinear ultrasound probe placed just under the xiphoid. Here we can identify the key structures needed to ensure you are insonating the gastric
Image 1. The position is in the sagittal plane just below the xiphoid. Use the curvilinear probe. Here is where the key structures can be found to identify the gastric antrum.
“In the glucagon-like peptide-1 receptor agonist era, relying solely on fasting times is increasingly risky.”
ULTRASOUND
continued from Page 129
3. Second position: After assessing gastric contents, roll the patient to the right lateral decubitus (RLD) position, which often accentuates dependent fluid and improves sensitivity (Images 3–4).
While in the RLD position, find the antrum again as in the supine view. If there is anechoic fluid, measure its cross-sectional area (CSA) in the sagittal plane, including all layers of the gastric mucosa, using this equation: CSA = (AP × CC) × π/4, where AP is anteroposterior diameter and CC is craniocaudal diameter.
Your ultrasound machine may have this measurement tool built in (Images 5–6).
Interpreting Findings
There are three main gastric antrum profiles:
1. Complex fluid or solids –Echogenic, particulate, or layered material. Treat as a full stomach (high risk). No need to measure CSA.
2. Clear/simple fluid – Anechoic content. Quantify using CSA-based estimates to infer gastric volume with the validated adult chart by Perlas et al Chart the patient’s age and CSA to estimate gastric volume. Anything outside the green area represents a “full stomach.”
3. Empty/contracted antrum –Collapsed “bull’s-eye” appearance with hyperechoic juxtaposed inner mucosa, generally low risk.
Pediatric Considerations
Gastric ultrasound has been extensively studied in pediatric patients, and the principles are
Image 3. The patient positioned right lateral decubitus (RLD) to identify any gastric contents that may have not been noted while supine. This brings any residual gastric content to a more dependent position for optimal visualization, characterization and measurement.

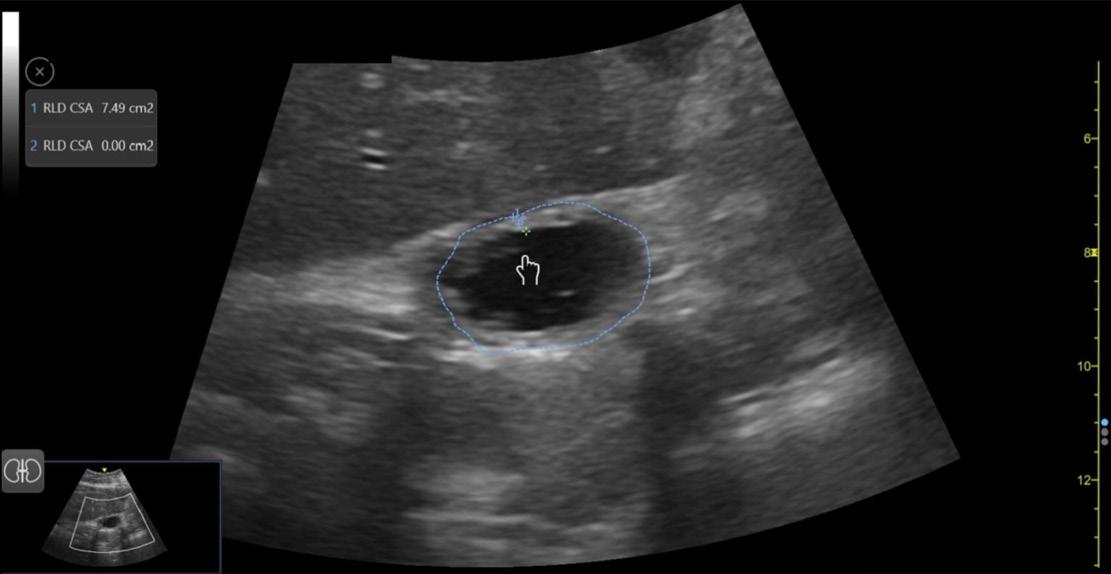
4,5. These images are in the right lateral decubitus position revealing residual gastric content not visible supine. Anechoic fluid fills the once empty antrum. Now, we are tasked to calculate if this anechoic fluid volume is more than normal gastric secretions. If your ultrasound machine has the function, you can choose “CSA” to be calculated. This requires you to trace the circumference of the gastric antrum including all layers of the gastric wall.
similar. However, size-based norms and clinical context matter even more.
For small children, maintain a high index of caution: any complex content warrants treating the stomach as full. A pediatric reference chart similar to the adult version is available from Spencer et al.
The GUARD Protocol
This exam can be distilled into a simple, emergency department–ready protocol for patients on GLP-1 RAs who require moderate sedation and may have a challenging airway.
GUARD (Gastric Ultrasound for Aspiration Risk Determination) includes three steps:
1. Scan the antrum in supine and RLD positions.
2. Measure CSA in RLD if clear fluid is present and record the value.
3. Escalate precautions if complex fluid or solids are seen—treat as a full stomach and adjust the sedation plan.
What the Data Show
In the authors’ GUARD quality initiative among 80 fasted, preoperative bariatric patients undergoing elective endoscopy, 33 of 80 were on GLP-1 RAs with variable timing of their last dose.
Ultrasound identified two “full stomachs,” which were confirmed by direct visualization during endoscopy. Only five of 80 scans were nondiagnostic due to limited windows in this bariatric population.
While preliminary, these results illustrate three practical points:
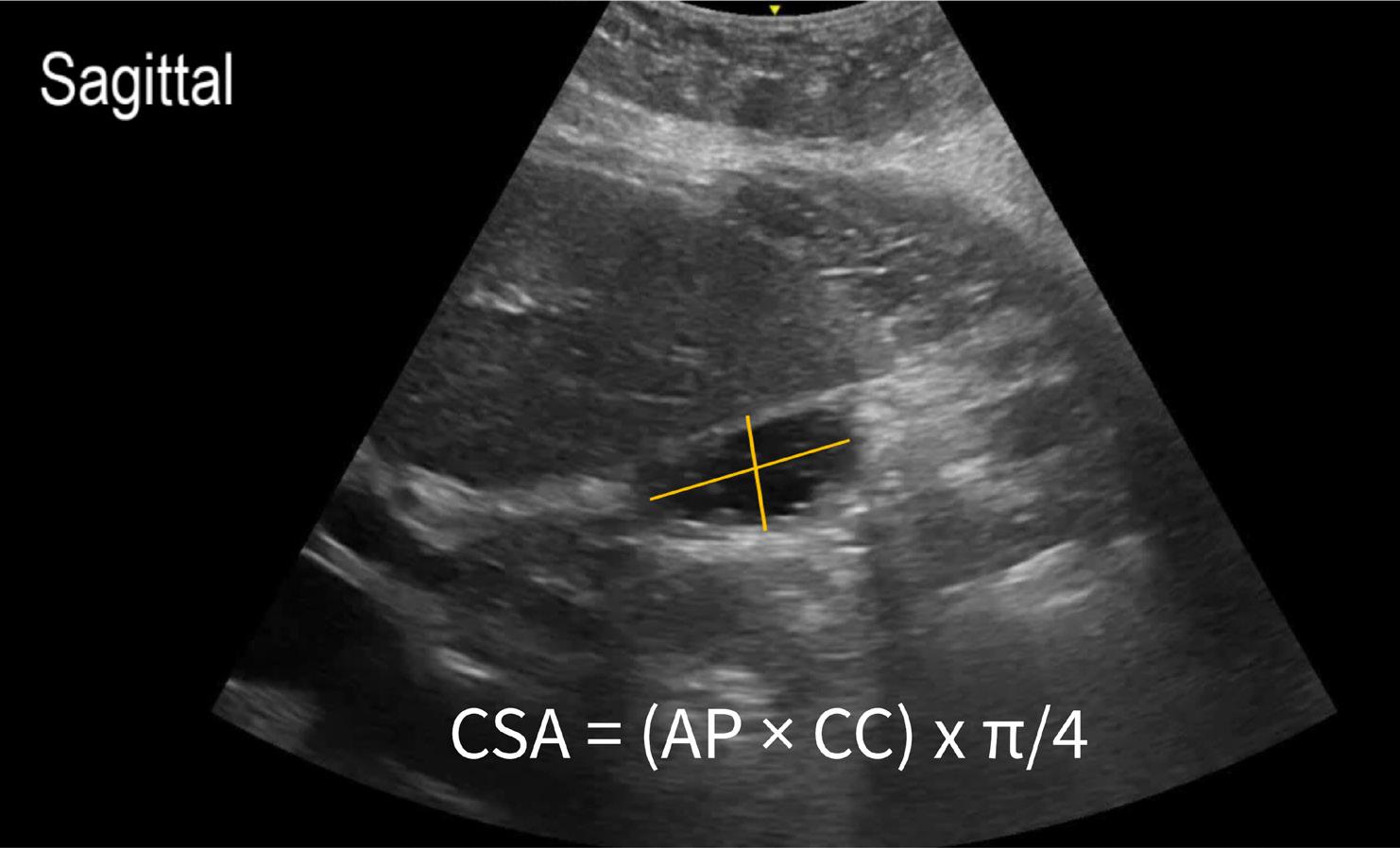
Image 6. Calculating the cross-sectional area manually requires anteroposterior (AP) and cranial-caudal (CC) measurements added to the equation.
1. Even “fasted” patients—especially those on GLP-1 RAs—can retain significant gastric contents. Timing of the last GLP-1 RA dose appears to matter.
2. GUARD can change management and enhance safety before sedation.
3. The scan is feasible across all body types.
The Bottom Line
In the GLP-1 RA era, relying solely on fasting times is increasingly risky. Until more high-quality evidence emerges, gastric ultrasound provides a rapid, bedside, patient-specific answer that can recalibrate your sedation and airway plan in real time. With a curvilinear probe, two positions, and a straightforward
interpretive framework, GUARD helps clinicians turn uncertainty into action— and gives teams the confidence to proceed safely
ABOUT THE AUTHORS


Dr. Hansen is the ultrasound director and an assistant professor of emergency medicine at the University of South Florida Morsani College of Medicine.
Dr. Derr is a professor of emergency medicine at the University of South Florida Morsani College of Medicine and directs the Advanced Emergency Medicine Ultrasound Fellowship.
Image

From HALO to HOLA: Redefining Ultrasound-Guided IV Training
By Andrew J Park, MD, and Christopher Clark, MD
Ultrasound-guided intravenous (USGIV) access represents a fundamental yet underemphasized procedure in emergency medicine training. Depending on protocol and credentialing, some emergency departments allow certified emergency department registered nurses to complete this procedure. While this is helpful for departmental flow and patient care, urgency for IV access is often fulfilled by nurses before it becomes a priority for residents, diverting training opportunities.
Residents are often guided carefully through central and arterial lines, yet USGIV lines receive little emphasis. Limited studies have
shown increased learner confidence with other procedures after gaining proficiency in USGIVs. Given its low risk, high utility and transferable skill set, USGIV warrants deliberate incorporation into emergency medicine didactics and merits its own classification as an HOLA procedure—high opportunity, lateral applicability—an acronym previously unestablished in the lexicon of medical education.
Micromastery and HOLA
The concept of “micromastery,” as described by Twigger, frames certain skills as discrete, selfcontained units that connect to broader domains of expertise. USGIV placement exemplifies this
framework: it provides residents with a manageable, repeatable skill that is both rewarding in the short term and foundational to procedural competence across multiple domains.
Developing proficiency in USGIV placement constitutes a micromastery with significant lateral transferability, enhancing competence across a wide range of procedures commonly performed in the emergency department. Unlike HALO procedures—high acuity, low opportunity—such as lateral canthotomies or surgical airways, the USGIV as an HOLA epitomizes the converse. The skill set developed through USGIV placement transfers
broadly to numerous procedures in emergency medicine, with the added benefit of frequent opportunities for deliberate practice.
From vessel cannulation that mirrors central venous or arterial access to needle visualization in nerve blocks; from optimizing angle of approach in lumbar punctures to holding the probe delicately for ocular scans, this keystone procedure underpins much of procedural practice in emergency medicine.
Patient Benefits
The clinical importance of USGIV placement extends beyond resident education. Multiple studies have shown that patients at high risk of difficult IV access (DIVA) benefit significantly from early ultrasound use. Implementing “ultrasoundfirst” protocols can reduce failed attempts, increase patient satisfaction and expedite vascular access in resuscitations.
In academic settings, structured training in USGIV can simultaneously improve patient care and provide residents with repeated, meaningful opportunities to refine procedural competence in a low-stakes environment.
Educational Strategies for Deliberate Training
Integrating USGIV as an HOLA procedure into resident didactics requires more than occasional exposure—it calls for structured educational design:
• Early exposure with deliberate practice: Introducing USGIV training during intern orientation or simulation boot camps helps establish procedural fluency before higher-stakes encounters. Anecdotally, USGIVs are deceptively tricky procedures in emergency medicine. The number of attempts required for proficiency ranges from 10 to 30 This variability underscores the need for structured practice opportunities. A curriculum emphasizing deliberate practice and mastery-based learning —with image capture and post-procedural feedback at its core—can flatten the learning curve.
• Microskill breakdown:
Deconstructing USGIV into discrete components—vessel scouting, probe handling, needle alignment, needle visualization—allows learners to master fundamentals before progressing to advanced procedures such as long-axis approaches, cannula troubleshooting or USGIV placement during resuscitations.
• Gamification: Gamified approaches can further encourage repetition and promote engagement and retention. Achievement pins can motivate learners, trigger social comparisons and encourage higher performance expectations. Our institution is piloting an achievement badge system that tracks successful USGIV placements and awards residents ranked pins for successive quotas to maximize engagement and peer recognition (Figure 1).

System and Institutional Considerations
Beyond educational value, USGIV carries practical and financial benefits. As a billable procedure, its cumulative value is significant when applied systematically in highvolume emergency departments. Physician-placed USGIVs can be billed as CPT codes 76937 (ultrasound guidance for vascular access) and 36410 (physician/QHP-performed venipuncture for diagnostic or therapeutic purposes).
Roll et al. reported increased revenue capture in a single emergency department after implementation of a dedicated USGIV difficult IV access

team and a specialized order set, with a jump from $140,000 to $2.4 million in three years. In true HOLA form, the USGIV can also improve resident charting: how physicians save their studies, store clips and document need in the electronic health record can pave the way to higher reimbursement for the department.
Conclusion
USGIV placement is more than a technical skill—it is a procedural micromastery with broad clinical and educational relevance. Its deliberate inclusion in emergency medicine curricula supports resident skill acquisition, enhances patient care and aligns with institutional priorities. By reframing USGIV as an HOLA procedure and investing in structured training methods, academic clinicians can transform a deceptively simple task into a cornerstone of resident development and patient-centered emergency care
ABOUT THE AUTHORS


Dr. Park is a faculty physician at Henry Ford Hospital in Detroit, where he completed his advanced emergency ultrasound fellowship. His clinical interests include gamification, masterybased learning and ultrasoundguided vascular access.
Dr. Clark is an emergency medicine physician and the advanced emergency ultrasound fellowship director at Henry Ford Hospital in Detroit.

When Family Planning Meets Residency: Infertility and Parenthood in Emergency Medicine
By Cristina Sanchez-Benitez, MD; Amanda J. Deutsch, MD; Pamela Dyne, MD; Andrew Wong, MD; Mia Karamatsu, MD; and Maia Winkel, MD, on behalf of the SAEM Wellness Committee
It’s 5 a.m., and the emergency medicine resident sees her last patient of the night — a 22-year-old woman with abdominal discomfort and vomiting. The resident obtains a history, performs an exam, and orders the usual lab tests and a urine pregnancy test. The test comes back positive, and an ultrasound confirms an intrauterine pregnancy. The patient is surprised — she wasn’t trying to get pregnant.
After discussing the discharge plan, the resident starts charting back at her desk, quietly fighting back tears. She and her husband have been trying to conceive for years without success, including multiple rounds of in vitro fertilization (IVF).
Her experience is not unique. Because medical training often overlaps with childbearing years, physician infertility is a significant
issue affecting trainees and practicing physicians. As we work to improve physician well-being and address individual and collective burnout, we must create space for conversations around infertility, parenthood, and reproductive choice — topics rarely discussed openly in emergency medicine training.
The Timing Dilemma
The typical emergency medicine training timeline overlaps with peak
“Because medical training often overlaps with childbearing years, physician infertility is a significant issue affecting trainees and practicing physicians.”
reproductive years — the late 20s to mid-30s — significantly affecting fertility and family planning. A 2021 study found that physicians delayed childbearing by an average of five years compared with nonphysicians, largely due to training.
Delaying childbearing contributes to physician infertility, compounded by demanding schedules and stress. One study found that nearly one in four female physicians are diagnosed with infertility, compared with 11 percent in the general population. Another showed that female emergency physicians had nearly twice the rate of impaired fertility — 25 percent compared with 12 percent in the general population. Those with impaired fertility reported working more hours and more night shifts, underscoring the strain of balancing infertility treatment with residency.
The residency training model, with its rigid timeline, does not easily allow for flexibility in scheduling. Despite the challenges imposed by this structure, few emergency medicine programs offer clear policies or support for residents pursuing fertility care. While some institutions are improving resident access to fertility services, a more standardized approach is needed — one that does not rely on the initiative of individual programs.
The Invisible Burden: Infertility
Fertility treatments are emotionally and physically demanding, requiring frequent appointments, hormone injections, and procedures such as egg retrievals and embryo transfers. These rarely align with the rigid and unpredictable residency schedule.
Residents must navigate the stress of training while managing infertility, and institutional support varies widely — in many cases, it may be minimal. A 2019 survey of nearly 300 program directors found that most were unaware of their program’s fertility coverage or whether trainees faced issues related to infertility. While many support improving resources, the lack of formal structures often leaves residents to carry this burden alone.
The Financial Burden of Infertility Treatment
The financial toll of infertility treatment is significant, especially for residents managing educational debt on limited salaries. A single IVF cycle can cost $12,000 to $25,000, and a successful pregnancy may require three to four cycles. Depending on insurance coverage, residents may need to use substantial personal funds to cover these costs. Some insurance plans cover up to 50 percent of expenses, while others offer a lifetime maximum benefit. The financial strain adds yet another layer of stress during an already demanding period.
Pregnancy and Parenting in Residency
While some residents struggle with infertility, others become pregnant or have children during residency — experiences that carry their own challenges, including issues with leave, scheduling, and bias.
Bias may take the form of “benevolent bias,” which involves making decisions or taking actions that seem kind or supportive but ultimately reinforce stereotypes, limit opportunities, or undermine autonomy. These challenges to work-life integration and autonomy contribute to burnout.
One review emphasized the need for national collaboration to create consistent leave policies. Even when policies exist, residents may feel uninformed or unsupported. A
study surveying program directors and medical students found that while most students wanted parental leave information during interviews, many did not receive it and felt uncomfortable asking. This lack of clarity affects both future parents and those experiencing infertility.
Program directors should ensure their program websites and materials clearly describe parental leave policies. Establishing clear and supportive policies is fundamental to promoting resident well-being — and may also enhance student recruitment.
The Choice Not to Have Children
Residents who choose not to have children or delay childbearing until after training also face challenges. Some delay strategically; others feel they have no real choice due to lack of support. In a commentary, obstetrician Dr. Duong emphasized that medical training remains a barrier to starting a family and called for better leave, childcare, and leadership support.
What Emergency Medicine Residency Programs Can Do
First, acknowledge and raise awareness around infertility, parenthood, and reproductive autonomy. These topics should be included in wellness programming from the perspective of autonomy and work-life integration.
Second, formalize accommodations for fertility treatments, advocate for insurance that includes fertility coverage, and be transparent about leave and fertility benefits — starting during the interview process, and at a minimum by ensuring such policies are visible on program websites.
Finally, leadership should normalize reproductive health discussions and foster a culture where all paths — parenthood, infertility, or voluntary childlessness — are respected and supported through both policy and action. Programs should ensure advocacy, maintain open dialogue about the challenges physicians face when they are ready to share, and keep the conversation going.
Conclusion
Family planning, infertility, and reproductive health are personal and often invisible struggles. Whether a resident is undergoing IVF, nursing a newborn, in the third trimester, or choosing to remain child-free, their experience matters. Emergency medicine programs must create environments that recognize and support all reproductive experiences — and, in doing so, build a more compassionate training culture
ABOUT THE AUTHORS


Dr. Sanchez-Benitez is a firstyear resident in the emergency medicine residency program at Orlando Health.
Dr. Deutsch is a clinical assistant professor and director of well-being in the Department of Emergency Medicine at Thomas Jefferson University’s Sidney Kimmel Medical College. She also serves as central region well-being co-lead for Jefferson Health and chair of the SAEM Wellness Committee.

Dr. Dyne is a professor of clinical emergency medicine at the UCLA David Geffen School of Medicine. She serves as director of academic affairs in the Department of Emergency Medicine and as chief physician well-being officer at Olive View–UCLA Medical Center.


Dr. Wong is a professor of clinical emergency medicine and medical director of managed care at UC Davis Health. Dr. Karamatsu is an assistant professor of emergency medicine and pediatrics and director of well-being in the Division of Pediatric Emergency Medicine at Stanford University School of Medicine.
Dr. Winkel is a clinical instructor and physician wellness fellow in the Department of Emergency Medicine at Stanford University.
WILDERNESS MEDICINE

From Burial to Survival: Key Updates in Avalanche Emergency Care
By Kailee Pollock, PharmD and Zachary Robinson, MD, on behalf of the Wilderness Medicine Interest Group
Introduction
Avalanche accidents are among the most feared scenarios in wilderness and mountain medicine, with an estimated 300 to 500 annual global avalanche deaths. Despite significant advances in forecasting, education, and rescue technology, mortality rates remain frustratingly high.
In 2024, the Wilderness Medical Society (WMS) released an updated set of clinical practice guidelines on avalanche and non-avalanche snow burial (NASB). These replace the 2017 document and reflect a stronger evidence base, greater alignment with international organizations such as the International Commission for Alpine
Rescue (ICAR) and the European Resuscitation Council (ERC), and consideration of new technology that has entered the field.
Prevention and Preparation
Most avalanche deaths occur within the first few minutes after burial, usually as a result of asphyxia or trauma. Because of this, education, preparation, and sound decisionmaking are likely to have the greatest impact on avalanche mortality.
Individuals entering terrain where avalanches are possible should attend accredited training courses and follow basic techniques to avoid triggering avalanches. These include avoiding slopes steeper than 30 degrees and traveling on ridges or
through thickly forested terrain when possible.
When entering a high-risk avalanche path for rescue or control work, use of a belay line securely anchored outside the path can prevent an individual from being swept downslope. Travelers should cross dangerous slopes one at a time, while being watched by a partner, and move between safer areas such as rock outcroppings, tree clusters, or adjacent low-risk slopes.
If caught in an avalanche despite these precautions, the priority is to escape the moving snow and avoid burial. Every attempt should be made to stay near the surface. Skis, snowboards, and snowshoes should
be jettisoned immediately, as they increase burial depth. Ski poles and ice axes may be used to self-arrest by anchoring into the base surface.
Safety Equipment
The classic beacon–shovel–probe triad remains the mainstay of avalanche preparation. However, the WMS guidelines highlight several additional devices that may improve outcomes.
The society recommends that anyone traveling in avalanche terrain wear a helmet designed for skiing or climbing. While helmets are unlikely to help in cases of deep burial, evidence suggests that traumatic brain injury can contribute to death by asphyxiation in small to medium avalanches.
Avalanche airbags are the only avalanche safety devices shown to prevent burial. These backpacks or vests contain balloons that can be inflated on demand from attached compressed gas cylinders. The inflated airbags increase the effective volume of the victim, keeping them closer to the surface. Some models include head and neck protection, though no data yet show reduced head or neck injury with their use. The WMS strongly recommends that travelers entering avalanche terrain use airbags and be familiar with their deployment.
Air diverters are another emerging device intended to help critically buried victims channel exhaled carbon dioxide away from the airway. The system separates exhaled, carbondioxide-rich air from oxygen-rich inhaled air, delaying asphyxia and the formation of ice in an air pocket. These devices include a mouthpiece connected to tubing with one-way inspiratory and expiratory valves. Evidence suggests air diverters may significantly increase survival time when buried. They are commercially available in Europe but not yet in North America. The WMS recommends travelers in avalanche terrain consider carrying an air diverter device.
Rescue and Team Coordination
When conducting a rescue, it is critical to immediately establish a team
“Most avalanche deaths occur within the first few minutes after burial, usually as a result of asphyxia or trauma.”
leader. These individual coordinates rescue efforts and resources while ensuring ongoing scene safety.
Initial search efforts should focus on a visual scan for surface clues and a transceiver search for buried avalanche beacons. Once highlikelihood areas are identified, pinpoint searches can be carried out using probes and shovels. Local emergency services should be notified, but notification should not delay the immediate rescue response.
Clinical Considerations and Resuscitation
Survival after avalanche burial depends on multiple factors, including severity of injury, duration of burial, airway patency, core temperature, and initial serum potassium (if available in the field). The Hypothermia Outcome Prediction after Extracorporeal Life Support (HOPE) score may also aid decision-making.
In general, patients retrieved in cardiac arrest have poor outcomes; however, those found in ventricular fibrillation or pulseless electrical activity (PEA) have greater odds of survival than those found in asystole.
The WMS recommends that if there are no vital signs and no indications for withholding resuscitation, rescuers should start cardiopulmonary resuscitation (CPR) and advanced life support (ALS) while performing further assessment.
If burial time is more than 60 minutes, core temperature is below 30 C, and the airway is patent, cardiac arrest was likely caused by hypothermia, so CPR should be continued and the patient transported to a hospital with extracorporeal life support (ECLS) capability.
In contrast, if burial duration is 60 minutes or less, core temperature is 30 C or higher, and the airway is not patent, resuscitation attempts should be stopped if return of spontaneous circulation (ROSC) is not achieved within 30 minutes. Resuscitation should be withheld in patients clearly in cardiac arrest due to trauma. Rescuers should also consider terminating efforts in patients who are pulseless and apneic with more than 60 minutes of burial and evidence of airway obstruction.
These recommendations align the WMS guidelines with those of ICAR and the ERC.
Conclusion
The 2024 WMS avalanche guidelines represent an important step toward aligning international best practices, clarifying decision-making, and addressing new challenges and evidence in avalanche care.
These and other wilderness-focused clinical practice guidelines are available at www.WMS.org under the “Learn” tab.
ABOUT THE AUTHORS


Dr. Pollock is a fourth-year medical student at Ohio Heritage College of Osteopathic Medicine and a clinical pharmacist at Cleveland Clinic Akron General. She involved with the research committee for the Wilderness Medical Society and serves as a WLS-MP instructor.
Dr. Robinson is faculty in the department of emergency medicine at Cleveland Clinic Akron General and an assistant professor of clinical emergency medicine at Northeast Ohio Medical University.
The Transformative Power of A Gift to SAEM Foundation
As this year comes to a close, we’re filled with gratitude for the generosity of our SAEM Foundation (SAEMF) donors. Because of hundreds of SAEM member donors, researchers and educators are innovating emergency care and are inspiring the next generation of academic emergency medicine physicians, just like Dr. Katie Buck who shares the impact of the SAEMF early career grant she received.
Each year, more deserving investigators come to SAEMF with bold ideas ready to transform emergency care—and we want to say “yes” to every one of them. Your gift before December 31, 2025, will bring us closer to the goal of annually funding over $1 million in research and education grants that will be truly transformational.
Here’s how you can help:
• Make a one-time or recurring online gift at www.saem.org/donate.
• Check with your/your partner’s company to see if they match gifts. If so, double your impact when you ask them to match your gift.
• Direct honoraria or grand rounds to support SAEMF.
• Consider a pledge, stock gift, or legacy commitment to sustain our mission for years to come.
• Contact Julie Wolfe, SAEMF’s Senior Manager of Development, for details about making any of these gifts, or, to pledge, before December 31st.
Every gift tells an SAEM member researcher, educator, or future leader that their work matters—that you believe in them. Thank you for considering a year-end gift to SAEMF.
A Special Thanks to SAEMF's 2025 Annual Alliance Donors
SAEMF extends its gratitude to the hundreds of SAEM members who have helped to build the pipeline of future EM researchers through an Annual Alliance donation to support SAEMF this year.

“I will forever be thankful to the SAEMF for the funding that provided a springboard to my career. As a researcher, my resident grant supported the project that gave me my first experience as the “PI” on my own mentored research project, and this provided the preliminary data for my NIA R03 GEMSSTAR. The EMF/SAEMF GEMSSTAR Supplement Grant supported critical career development during that R03. This led to my successful NIA K76 Beeson application. It also developed my leadership skills, which has led to leadership opportunities within AGEM and SAEMF. These roles have provided a way for me to be involved in guiding these two organizations that have meant so much to me over the years so that I can help pay it forward for future SAEM members.”
- Katie Buck, MD, MPH, EMF/SAEMF GEMSSTAR Grantee, SAEMF Board of Trustees Member, SAEMF Donor, and AGEM Past President EVERY $1 =
14 PUBLICATIONS 61% OF RESEARCH TRAINING GRANT RECIPIENTS Average number of publications per Research Training Grant recipient received subsequent funding from federal sources1
Now Could be the Time to Explore A Donor Advised Fund (DAF) to Enhance Your Charitable Giving
A Simpler Way to Support SAEM Foundation ’s (SAEMF) Mission
For many donors, generosity comes with paperwork, timing questions, and the challenge of keeping track of multiple gifts. A Donor Advised Fund (DAF) can simplify the process while maximizing your impact on SAEMF ’s mission.
Donors Use DAFs for A Variety of Reasons
• Convenience: One contribution, one receipt, countless grants.
• Flexibility: Recommend grants on your own schedule, across multiple charities.
• Impact: Assets in your DAF can grow tax-free, meaning more charitable dollars to deploy.
• Legacy: You can create recurring grants to ensure ongoing support for causes you value most. You can also include the SAEMF as a beneficiary of your DAF, should you wish to continue impact beyond your lifetime.
When donors recommend a grant to SAEMF, it directly strengthens the SAEMF’s funding available to award more research and education grants, leading to innovation in research and education, thereby transforming emergency care.
What is a DAF?
A DAF is like a charitable investment account for the sole purpose of supporting nonprofits you care about. You contribute cash, stocks, or other assets into your DAF, receive a tax deduction, and then recommend grants to the nonprofits of your choice from the DAF at times that make sense for you.

“I set up a Donor Advised Fund (DAF) last year through one of the bigger well known investment advisors. It was super easy. I got an immediate tax deduction, too. Then came the fun part: choosing how to make grants from the DAF. SAEMF was my first pick. It was so easy—there it was on the drop down menu on the DAF website. I made my SAEMF donation with a click of a button and, even better, got to watch the account grow again (tax free) for future donations. This is a no brainer—all my future SAEMF giving is going to come from this DAF.”
- Zachary F. Meisel, MD, MPH, MSHP, SAEMF President (2025-26) and Sustaining Donor of the Annual Alliance
How to Make a DAF Gift
If you already have a DAF, making a gift to SAEMF is simple:
1. Log in to your DAF provider’s portal. Search for SAEMF or SAEM Research Foundation, EIN #EIN: 26-2371803
2. Recommend your grant to support SAEMF ’s mission.
If you’re new to DAFs and want to learn more, we recommend consulting with your financial advisor to identify gift options that align with your intentions and to see if a DAF could be for you. Let us know if you’d like to visit to learn more about SAEMF and how our donors are transforming emergency care through their giving!
BRIEFS & BULLET POINTS
FEATURED NEWS
SAEM Awards Honor EM
Leaders, Mentors, Innovators
SAEM awards season is here! Join us in celebrating excellence in academic emergency medicine by nominating a colleague, mentor, or even yourself for an SAEM or RAMS award. These awards highlight outstanding contributions in research, education, leadership, and service — honoring the individuals who are shaping the future of our field. Explore the award categories, review the nomination process, and submit your nomination by December 9. Your participation helps ensure the achievements of our community are recognized and celebrated. Learn more 2026-2027 Leadership Nominations Are Open!
Nominations are open for leadership positions on the 2026–2027 SAEM Board of Directors, RAMS Board, Nominating and Bylaws committees, AACEM and SAEM academy executive committees, and the SAEM Foundation Board of Trustees. We’re seeking passionate, forward-thinking leaders committed to innovation and growth. If you or someone you know brings diverse perspectives, strong leadership, and a dedication to advancing academic emergency medicine, now is your opportunity to serve. Your personalized nomination link was emailed to your SAEM member email address. Questions? Contact governance@saem.org. Nominations close on Nov. 7, 2025. Visit the nominations webpage for more information.
SAEM Launches New Coaching Interest Group
SAEM is excited to introduce the new, Coaching Interest Group. This group aims to raise awareness of the value of coaching, provide opportunities to cultivate and practice coaching skills, and foster career development pathways related to coaching. By
connecting members with shared interests, the Coaching Interest Group will support professional growth, enhance leadership capacity, and expand resources across SAEM’s 10,000+ members. Join today!
SAEM FOUNDATION
2025 SAEMF Challenge: Record-Breaking Support for EM Education and Research!
The 2025 SAEMF Academy, Committee, and Interest Group Challenge was an incredible success! Together, our generous donors raised a record $99,400 and unlocked SAEM’s $10,000 matching gift and a special $5,000 matching gift for the Vice Chairs — bringing this year’s grand total to $109,400. This unprecedented support will expand SAEMF grant opportunities and empower grantees to advance innovations that will shape the future of emergency care. Thank you to everyone who contributed!
Congratulations to the 2025 SAEMF Challenge Winners!
Highest Participation Competition
• Academy of Geriatric Emergency Medicine
• Finance Committee & Bylaws Committee
Research Directors Interest Group & Vice Chairs’ Interest Group
Most Funds Raised Competition
• Academy for Diversity & Inclusion in Emergency Medicine
• Grants Committee
• Operations Interest Group & Vice Chairs’ Interest Group
Celebrating YOUR Impact
Winning groups get ready to be celebrated throughout the upcoming year and during SAEM26!
Support More EM Research
This Giving Tuesday!
This Giving Tuesday, December 2, support emergency medicine research through a contribution to the SAEM Foundation (SAEMF). Applications
for SAEMF grants have surged over the last two years, reflecting an unprecedented demand for funding innovative research that improves patient care. Your donation on #GivingTuesday will empower the next generation of emergency medicine leaders to drive groundbreaking advancements. Together, we can ensure a brighter future for emergency care and make a transformative difference in patients’ lives.
Don’t Miss These Deadlines! SAEMF Funding Opportunities!
• EMF/SAEM Medical Student Research Grants in Memory of Dr. Amy H. Kaji – Up to $5,000; up to four awards This grant offers medical students’ early exposure to emergency medicine (EM) research, along with skill-building and networking opportunities through the EMF-SAEMF Grantee Workshop. Apply by 5 p.m. CT, December 12, 2025. Visit saemfoundation.org to learn about the 2025 recipients of this grant.
• SAEMF Emergency Medicine Interest Group Grant (EMIG) – $1,000 Supports emergency medicine interest groups (EMIGs) in advancing medical student education, fostering innovative educational methodologies in undergraduate education, and enhance EMIG-led activities. Apply by 5 pm CT, January 31, 2026. Visit saemfoundation.org to learn about the 2025 recipients of this grant.
SAEMF is grateful to Dr. David Wilcox for his visionary endowment established to support emergency medicine education at the medical student level through support for the emergency medicine interest group grants program. Through his generosity, one grantee will be distinguished as recipient of The David E. Wilcox, MD, FACEP Emergency Medicine Interest Group Endowed Grant each year, in perpetuity.
SAEM MEMBER RESOURCES
Essential SAEM Resources for Building
Your Academic Emergency Medicine Career
Advance your academic emergency medicine career with SAEM’s expert-developed resources. Whether you’re a student, resident, fellow, or faculty member, these guides provide practical tools and insights to help you succeed in education, research, and leadership.
Academic Career Guide
A comprehensive roadmap for building a successful academic EM career, with guidance for aspiring leaders such as department chairs, program directors, and deans.
Competency-Based Medical Education Primer
A clear, practical guide to understanding and implementing CBME in emergency medicine. Includes key principles, program essentials, and real-world examples for educators at any institution.
The Reason for Research
An essential toolkit for medical students, residents, and junior faculty interested in EM research. Offers career planning advice, mentorship insights, and strategies for impactful academic work.
Securing Your First Faculty Position: A Guide for Residents and Fellows
A step-by-step guide to navigating the EM job search—from crafting your CV and acing interviews to setting the stage for long-term career success.
AEUS Narrated Lecture Series
An online ultrasound curriculum for EM trainees. AEUS faculty can manage learners, exams, and results through the portal, while non-members can access lectures on YouTube and Vimeo or join AEUS for full access.

26 ANNUAL MEETING UPDATES
ACCEPTING SUBMISSIONS!
The SAEM Annual Meeting is the premier destination for showcasing groundbreaking research in academic emergency medicine. By submitting your work, you’ll gain valuable exposure and connect with an engaged community eager to exchange innovative ideas.
SAEM26 highlights original research, educational excellence, and professional growth — the ideal venue to share your work, gain recognition, and advance your career. Don’t miss your chance to be part of this influential event. Submit your work today!

Abstracts
The SAEM Annual Meeting welcomes abstracts that reflect the real-world
SAVE THE DATES!
challenges and critical issues facing emergency medicine today. Submissions should advance knowledge, improve practice, and enhance patient outcomes — grounded in rigorous research or innovative educational practices.
Accepted abstracts will be published in a special supplement of Academic Emergency Medicine (AEM), giving contributors global visibility. Select abstracts will also receive special recognition and be featured in SAEM26 plenary sessions.
Deadline: January 5, 2026
Learn more and submit your abstract.

Innovations
Innovations offers a platform to present novel ideas in undergraduate and graduate medical education, as
SAEM26 Registration Opens December 1
The SAEM Annual Meeting offers something for everyone — from seasoned faculty to students beginning their academic journeys. Join us May 18–21, 2026, in Atlanta, Georgia, for this can’t-miss event and enjoy:
• Cutting-edge research presentations
• Expert-led educational sessions
• Hands-on workshops and experiential learning
• Networking and career development opportunities
SAEM26 Registration opens December 1
Early Bird Deadline: March 10, 2026
Visit the SAEM26 website for updates.
well as in nonclinical areas such as faculty development and operations. In addition to welcoming submissions from all areas, SAEM26 encourages authors to consider the following highlighted themes:
• Machine Learning / Artificial Intelligence in Medical Education
• Sustainability and Waste Reduction in Health Care
• Reproductive Health and Education
• Rural Health
Deadline: January 12, 2026
Learn more and submit your innovation.
IGNITE!
IGNITE! is a fun, fast-paced speaking competition that challenges presenters to deliver their message in just five minutes — accompanied by 20 automatically advancing slides.
These high-energy sessions feature captivating talks on diverse topics ranging from disaster relief to machine learning. A panel of judges selects a “Best of IGNITE!” winner for each session, and attendees vote for an Audience Choice Award.
Deadline: January 12, 2026
Learn more and submit your IGNITE!
Residency & Fellowship Fair Program Sign Up Starts December 1
The SAEM Residency & Fellowship Fair offers a streamlined, cost-effective recruitment opportunity to connect your program with hundreds of motivated candidates — all in one place. Engage in meaningful conversations, showcase your program, and meet the next generation of emergency medicine professionals. Program registration opens December 1! Learn more about program sign-up.

Clinical Images
The SAEM Clinical Images Exhibit showcases high-definition, educational, image-based case submissions that highlight key aspects of emergency medicine practice.
Accepted images are selected based on educational value, image quality, and relevance. Approved submissions with patient consent will also be featured in the Academic Life in Emergency Medicine (ALIEM) blog series, SAEM Clinical Images.
Deadline: January 12, 2026
Learn more and submit your clinical image.
A ONE-OF-A-KIND OPPORTUNITY FOR MEDICAL STUDENTS!
SAEM is recruiting 50 energetic, selfstarting, responsible, and enthusiastic medical students for the SAEM26 Medical Student Ambassador (MSA) program. Selected MSAs will work directly with the SAEM Program Committee to assist in the planning, coordination, and execution of SAEM26, May 18 - 21, 2026 at the Atlanta Marriott Marquis in Atlanta, Georgia.
7 Benefits of Being a Medical Student Ambassador
• Waiver of your SAEM26 registration fee
• Free registration to the Medical Student Symposium
• Exposure to current education and research in EM through participation in didactics, poster sessions, lectures, and other educational activities
• Pairing and scheduled one-on-one meetings with an academic EM
mentor (a faculty advisor from the SAEM26 Program Committee)
• Opportunities to form relationships with faculty members, residents, and medical students from EM programs around the country
• A personal letter from the program committee chair, sent to your dean of student affairs, acknowledging your contributions
• Your very own SAEM-branded athletic jacket! (All the cool kids are wearing them!)
How to Apply
Medical students who are interested in serving as a Medical Student Ambassador for SAEM26 can find more information and application details by visiting the MSA webpage Additional questions can be addressed to Holly Byrd-Duncan at hbyrdduncan@ saem.org or education@saem.org
Deadline: January 12, 2026

SAEM REPORTS
COMMITTEES Education
The Education Committee guides SAEM and RAMS on undergraduate, graduate and continuing medical education. In collaboration with partners such as Clerkship Directors in Emergency Medicine, it advances emergency medicine education for students, residents, and fellows and organizes educational tracks for the annual meeting.
Highlights
• Explore the committee’s education offerings, including webinars, journal clubs, and social media content. Topics range from medical students exploring EM to career clinician educators— something for everyone.
For more information, contact Sara Krzyzaniak at skrzyz@stanford.edu
ACADEMIES
Academy of Emergency Medicine Pharmacists (AEMP)
AEMP champions excellence, innovation, and advancement in emergency medicine pharmacy practice through advocacy, education, research, and collaboration. Its purpose is to foster a community of dedicated professionals, drive research, enhance training programs, and disseminate best practices to improve patient care.
Upcoming
• AEMP Town Hall: Nov. 4, 2025, 1–2 p.m. CT.
• JeopaRxdy: EM Pharmacist Takeover! Round Two: Nov. 19, 2025, 1 p.m. CT. Test and improve your pharmacotherapy knowledge and be eligible for prizes.
Calls for Submissions (SAEM26)
• Research abstracts: Due Monday, Jan. 5, 2026.
• Innovations and resident IGNITE! pearls: Due Monday, Jan. 12, 2026.
For more information, contact Megan Rech at megan.a.rech@gmail.com
Academy of Emergency Ultrasound (AEUS)
AEUS unites clinician sonologists to advance patient care and safety through bedside ultrasound. AEUS
develops training curricula and research resources for medical students, residents, and fellows to enhance education and innovation.
Funding
Opportunities
• AEUS Sound Start Award: $1,000 scholarship for medical students with a passion for point-of-care ultrasound (POCUS). Awardees will be recognized at the AEUS meeting during SAEM26 in Atlanta in May 2026. Applications must include a curriculum vitae, a 250-word personal statement, and a faculty support letter. Deadline: Nov. 3, 2025, at 9 p.m. CT
• AEUS Sono Innovation Award: Grants of $200–$2,000 support innovative ideas in emergency ultrasound, including POCUS educational resources, teaching materials, and assessment tools. Applicants must submit a three-minute video describing the idea, funding request, and success measures. Winners will provide a spring progress update and will be recognized during the AEUS annual meeting at SAEM26 in Atlanta in May 2026. Deadline: Nov. 3, 2025, at 9 p.m. CT.
Education
• Webinar — “State of Resuscitative Transesophageal Echocardiography”: Jan. 28, 2026, 2 p.m. CT. Panelists from established and new programs will share implementation strategies, practical tips, and future directions. Registration details will be announced. Join AEUS to stay informed about webinars, journal clubs, and other activities.
For more information, contact Meera Muruganandan at Meera.muruganandan@gmail.com.
Academy for Women in Academic Emergency Medicine (AWAEM)
AWAEM promotes the recruitment, retention, and advancement of women in academic emergency medicine. AWAEM emphasizes the essential role of women faculty in the specialty’s success and in training future emergency physicians.
Grand Rounds
• Inaugural AWAEM Grand Rounds — “Level Up: Women Faculty on the Rise + Lactation in the ED,” featuring Drs. Leenellett and Sabedra. Nov. 5, 2025, 2 p.m. CT (virtual). Register today! Interested in presenting? Submit here.
For more information, contact Margaret Samuels-Kalow at msamuels-kalow@mgb.org
INTEREST GROUPS
Operations
The Operations Interest Group brings SAEM members together to improve emergency department operations for patients and staff. It fosters community, shares best practices, and highlights innovative approaches for managing departments in today’s challenging health care environment.
Events and Updates
• Online workshop — “Best Practices in Teaching Our Learners ED Operational Leadership”: Oct. 20, 2025, 9:30 a.m. CT (30 minutes). For details, contact Nick Tsipis at netsipis@carilionclinic.org; updates will also be shared via the ED Operations Interest Group community site/listserv.
• Simulation-based clinical systems testing: One member institution’s ED identified critical safety threats in ST-segment–elevation myocardial infarction (STEMI), trauma, and stroke care, including communication barriers, inefficient layouts, and suboptimal equipment placement. Recommendations include standardized room designs, improved wayfinding, and stronger communication systems to enhance patient safety and operational efficiency before opening or expanding an ED. The group encourages further research and publication of these processes.
• We wish to celebrate a number of high-quality multi-institutional didactic submissions focused on emergency department operations for SAEM 2026. This impressive response underscores the dedication and collaboration within our community to advance emergency medicine. These submissions reflect a diverse range of innovative ideas and practical solutions aimed at enhancing ED efficiency and patient care. We extend our heartfelt appreciation to all contributors for their invaluable insights and commitment to excellence. As we look forward to abstract and other submissions for SAEM 2026, these contributions promise to inspire and drive meaningful discussions that will shape the future of emergency medicine.
• Community recognition: The Operations IG is proud to recognize the many high-quality, multi-institutional didactics on emergency department operations submitted for SAEM 2026. This strong response reflects our community’s dedication to advancing emergency medicine through collaboration and innovation. The submissions showcase creative, practical solutions to improve ED efficiency and patient care. We thank all contributors for their insight and excellence, which will continue to inspire dialogue and shape the future of our specialty.
For more information, contact Nick Tsipis at netsipis@ carilionclinic.org
Wilderness Medicine
The Wilderness Medicine Interest Group brings together emergency physicians interested in care in wilderness and austere environments. The group supports research, education, and collaboration on outdoor injuries and environmental emergencies to build skills for resource-limited settings.
Get Involved
• Social media quiz competition: Participate via SAEM’s social channels; a prize will be awarded to the winner.
• Call for authors: WMIG seeks contributors for SAEM Pulse article submissions.
• Conference programming: WMIG aims to increase wilderness medicine education at upcoming SAEM conferences, is collaborating with the Simulation Academy for SAEM26, and is considering the return of MedWars. Interested members are encouraged to reach out.
For more information, contact Kevin Watkins at watkink2@ccf.org.
RAMS
SAEM Residents and Medical Students serves as a forum for physicians-in-training to engage with the academic emergency medicine community. RAMS provides opportunities to participate in research, contribute to education, and develop leadership skills that advance the specialty. It also advocates for the perspectives and needs of trainees, ensuring their voices shape the field. All residents and medical students who join SAEM automatically become RAMS members.
Resources and Updates
• ResidencyCAS application support: Visit the RAMS ResidencyCAS page for resources to strengthen your application.
• RAMS President’s Reports: A new series highlighting key updates, ways to get involved, and leadership opportunities through projects, webinars, and more. Watch for emails; an online archive is available.
• Accreditation Council for Graduate Medical Education (ACGME) EM program requirements: Confused by the proposed changes? RAMS compiled a comprehensive, sources-based timeline and analysis. Read the article on page 30 in this issue of SAEM Pulse to get the facts.
For more information, contact Daniel Artiga at djartiga@gmail.com
ACADEMIC ANNOUNCEMENTS
Dr. Charlotte Goldfine Awarded K23 Career Development Award

Charlotte Goldfine, MD, has been awarded a K23 Career Development Award from the National Institute on Alcohol Abuse and Alcoholism to study the use of an ingestible electronic sensor to measure adherence to medications for alcohol use disorder in patients undergoing alcohol detoxification. Her work highlights the innovative nature of emergency medicine research within the emergency department and through collaboration with other specialties.
Dr. Stephanie Carreiro Receives NIH/ NIDA K24 Midcareer Investigator Award

Stephanie Carreiro, MD, PhD, has received a National Institutes of Health/National Institute on Drug Abuse K24 Midcareer Investigator Award in Patient-Oriented Research for her project, “Mentoring in PatientOriented Research for Digital Biomarker-Driven Solutions to Prevent and Treat Opioid Use Disorder.” This five-year award supports Dr. Carreiro’s mentorship of postdoctoral fellows and junior faculty, and advances precision medicine research using wearable sensors and digital biomarkers to personalize treatment and prevention of opioid use disorder.
Dr. Aaron D’Amore Appointed to ABEM Resident Ambassador Panel

Aaron D’Amore, MD, has been named to the American Board of Emergency Medicine (ABEM) Resident Ambassador Panel. Dr. D’Amore is an emergency medicine resident in the Mass General Brigham HarvardAffiliated Emergency Medicine Residency Program. He recently served on the Society for Academic Emergency Medicine (SAEM) Residents and Medical Students Board as a Member-at-Large and continues his involvement on the SAEM Administration and Operations Committee. He joins SAEM member Oladele Osisami, MD, an emergency medicine resident in the NewYorkPresbyterian – Columbia and Cornell residency program, who is entering his second year on the panel.
Dr. Tony Rosen Receives NIH/NIA K24 Midcareer Investigator Award
Tony Rosen, MD, MPH, has received a National Institutes of Health/ National Institute on Aging K24 Midcareer Investigator Award in Patient-Oriented Research. This award supports midcareer, clinically trained researchers in mentoring junior clinical investigators and conducting patientoriented research. Dr. Rosen is associate professor of emergency medicine and associate director of research in the Department of Emergency Medicine, Division of Geriatric Emergency Medicine, at NewYorkPresbyterian Hospital/Weill Cornell Medical Center. He also serves as program director of the Vulnerable Elder Protection Team (VEPT).
Dr. Peter Chai Awarded NIH/NIDA R34 Grant

Peter Chai, MD, MMS, associate professor of emergency medicine at Brigham and Women’s Hospital, has been awarded a National Institutes of Health/National Institute on Drug Abuse R34 grant for his project, “Harmonized Healing: Personalized Music Interventions to Address Chronic Pain in People Living with HIV.” This innovative study will develop and pilot a music-based digital intervention using personalized playlists to reduce chronic pain, improve mood, and enhance HIV care engagement, paving the way for a multisite clinical trial to advance whole-person, nonpharmacologic pain management.
Drs. Gelabert and Willis Promoted to Professor at UT San Antonio


Christopher Gelabert, MD, has been promoted to professor, clinical, of emergency medicine at the University of Texas at San Antonio Long School of Medicine. George Willis, MD, has been promoted to professor, clinical, of emergency medicine at the University of Texas at San Antonio Long School of Medicine. He also serves as vice chair of faculty development.
Dr. Charlotte Goldfine
Dr. Tony Rosen
Dr. Peter Chai
Dr. Christopher Gelabert
Dr. George Willis
Dr. Stephanie Carreiro
Dr. Aaron D’Amore
Dr. Frederick Korley Receives $13 Million in Awards for TBI Research

Frederick Korley, MD, PhD, professor and associate chair of research in the Department of Emergency Medicine at the University of Michigan, has received a total of $13 million in new awards to lead groundbreaking studies in traumatic brain injury (TBI). He is multiple principal investigator of a four-year, $6.1 million renewal grant from the National Institute of Neurological Disorders and Stroke to continue the Hyperbaric Oxygen in Brain Injury Treatment (HOBIT) trial, conducted through the Strategies to Innovate Emergency Care Clinical Trials (SIREN) Network. In addition, he is principal investigator of a $6.85 million Focused Program Award from the Department of Defense to launch the PIONEER Studies, a series of four innovative projects advancing biomarker-guided evaluation of TBI.
Dr. Christina Shenvi Promoted to
Professor of EM With Tenure at University of North Carolina

Christina L. Shenvi, MD, PhD, MBA, has been promoted to professor of emergency medicine with tenure at the University of North Carolina–Chapel Hill. She also serves as director of medical student case-based learning in the Office of Medical Student Education. Dr. Shenvi’s passion for the care of older adults inspired her to launch the Geriatric Emergency Medicine podcast, GEMCAST, and to serve on the board of governors for the American College of Emergency Physicians Geriatric Emergency Department Accreditation program. A dedicated educator, she has received multiple institutional and national teaching awards.
Elina Kurkurina Receives Cost of Care STARS Student Excellence Award

Elina Kurkurina has been named a recipient of the Cost of Care STARS (Students and Trainees Advocating for Resource Stewardship) Student Excellence Award, which recognizes outstanding contributions to advancing highvalue care in medical education. Kurkurina is a fourth-year medical student in the Healthcare Management and Organizational Leadership concentration at the Frank H. Netter MD School of Medicine at Quinnipiac University. She serves as director of data and quality for the Bobcat Student Clinic and president of the university’s chapter of the American College of Healthcare Executives. Her research focuses on improving care coordination for older veterans, emergency medical services operations, and screening initiatives. A two-time SAEM Medical Student Ambassador, Kurkurina plans to pursue a career in emergency medicine with a continued emphasis on high-value care.

Dr. Christina L. Shenvi
Elina Kurkurina
Dr. Frederick Korley
IN MEMORIAM
Remembering Robert Dailey, MD: Architect of Emergency Medicine Education
By Brian J. Zink, MD
Robert H. (Bob) Dailey, MD, passed away on August 10, 2025, a month shy of his 90th birthday. Dailey was a dynamic and influential leader in the development of emergency medicine as a specialty, a champion of residency education, and a builder of educational organizations.
I had the pleasure of interviewing Dr. Dailey for my book on the history of emergency medicine (1) in 2002 after we enjoyed a fly-fishing float trip down the Snake River in Wyoming with his good friend Dr. Peter Rosen. Bob was a tall, lanky man—high energy, fast-talking, with a ready laugh and a nonconformist approach to life. He was also immensely proud of what emergency medicine had become after his early efforts.
Dailey completed an internal medicine residency and then took a year off to travel the world with a friend. He began practicing in the Kaiser system in California in the mid-1960s. Just four months in, he had a “great realization that I was temperamentally unfit for internal medicine.” He started working in the emergency department (ED) at Highland Hospital in Oakland, California, and found the work stimulating and far more enjoyable than his previous practice. He loved teaching the rotating residents and medical students in the ED.
This interest led him to the University of Southern California, where a new EM residency and academic department had been established in 1971. Dailey became the residency director there and was deeply engaged in developing clinical teaching and didactics for the early residents. Faculty supervision and organized education of emergency medicine residents in those early years were often minimal, so Dailey’s approach was notable and soon emulated by others.
Dailey also felt the scorn of non-EM physicians and residents as he worked to establish a foothold for the specialty. He described this to me when I interviewed him, providing one of my favorite quotes for the book. Dailey noted that others saw the ED as “nothing but a problem. It was a wart on the ass of prosperity, no question about it.”
Determined to improve EM residency education, Dailey began organizing early educators to create standards and a review process for EM residency programs. At that time there was no EM board, no ACGME, and no Residency Review Committee. Dailey took the initiative, joining with other early leaders in the American College of Emergency Physicians (ACEP) to form a Residency Review Committee for emergency medicine in 1972–73. He was appointed as its leader.
At the time there were about 15 EM residencies established, so the committee had work to do—but no established criteria for approving programs. Dailey described how he sat in his apartment in Fresno, California, one afternoon and rapidly penned about 12 principles for EM residency approval. One of them required on-shift supervision of residents by a faculty member. Until then, residents often taught each other without faculty present.
Because no entity existed to conduct formal reviews of EM residencies, Dailey and others in ACEP reached out to the fledgling academic organization of the time, the University Association of Emergency Medical Services (UA/EMS), to find qualified reviewers. They formed the Liaison Residency Endorsement Committee (LREC), which reviewed 50 EM residency programs in its first three years, with Dailey participating in many of the reviews.
In 1975, Dailey was a key figure in developing an organization out of ACEP called the Society of Teachers of Emergency Medicine (STEM). This group aimed to balance the heavy surgeon
presence in UA/EMS by including practicing emergency physicians who were teaching early EM residents. Dailey served as STEM’s first president. The group eventually merged with UAEM (the later version of UA/EMS) to become SAEM in 1989.
Dailey was often at the table as early leaders pushed for EM to become an approved specialty board within the American Board of Medical Specialties (ABMS). He developed a lecture and article comparing the field of EM to a “new flower…in medicine’s garden of specialties,” complete with a diagram of a flower with 12 petals labeled with areas of education essential for EM training and their relationship to other areas of medicine. He wrote that the flower of EM “takes root in the most arid of soils where other flowers cannot and have not grown.” Familiar with California’s “flower children” of the 1960s, the analogy suited him perfectly.
Dailey, who was regarded as a leading figure in EM residency education, worked tirelessly with other early EM leaders to gain approval for the American Board of Emergency Medicine from the ABMS in 1979. He served as a member of the initial ABEM Board of Directors. Peter Rosen recruited Dailey as one of the original editors of what became the premier textbook in the field, Emergency Medicine: Concepts and Clinical Practice.
Although Dailey was never a researcher in EM, he expressed deep admiration and appreciation for how EM investigators had advanced the science of the field. When I interviewed him in 2002, he reflected: “I think that, probably more than anything, makes me very proud—that we have sought out our best practices and tried scientifically and objectively to determine what best practice is. It has benefited patient care immeasurably.”
All quotes from Robert H. Dailey in this essay come from interviews that were conducted in 2002 and published in the book: Zink, BJ. Anyone, anything, anytime – a history of emergency medicine. 2nd edition. ACEP Publishing 2018.
Dr. Robert H. Dailey
NOW HIRING
POST YOUR OPEN JOBS IN FRONT OF OUR QUALIFIED CANDIDATES!


Assistant Professor, Department of Emergency Medicine College of Medicine, University of Cincinnati
Founded in 1819, the University of Cincinnati ranks among the nation’s best urban public research universities. Home to over 50,000 students, 11,000 faculty and staff and 332,000 alumni, UC combines a Top 35 public research university with a physical setting The New York Times calls “the most ambitious campus design program in the country.”
With the launch of Next Lives Here, the Cincinnati Innovation District, a $100 million JobsOhio investment, nine straight years of record enrollment, global leadership in cooperative education, a dynamic academic health center and entry into the Big 12 Conference, UC’s momentum has never been stronger. UC’s annual budget tops $1.65 billion and its endowment totals $1.8 billion.
Job Overview
As one of the oldest medical schools in the country, the University of Cincinnati College of Medicine (COM) has a reputation for training bestin-class health care professionals and developing cutting-edge procedures and research that improves the health and clinical care of patients. In partnership with the UC Health academic healthcare system and Cincinnati Children’s Hospital Medical Center, College of Medicine’s faculty are transforming the world of medicine every day.
Essential Functions
• Collaborate with hospital operations teams to optimize throughput, capacity management, and ED flow.
• Mentor early-career faculty and trainees in academic scholarship, leadership development, and career advancement.
• Disseminate knowledge through peer-reviewed publications, grant activity, and national presentations.
• Participate in hospital committees, task forces, and systemwide initiatives that shape emergency and acute care delivery.
• Contribute to strategic planning, program development, and philanthropic efforts to advance the mission of the department and the College of Medicine.
Minimum Requirements
• MD/DO.
• Ohio Medical License.
• Completion of a four (4) year Emergency Medicine Residency -OrCompletion of a 3-year emergency medicine training program with at least one year of service in an academic setting or fellowship training.
Compensation and Benefits
UC offers a wide array of complementary and affordable benefit options, to meet the financial, educational, health, and wellness needs of you and your family. Eligibility varies by position and FTE. Competitive salary range dependent on the candidate’s experience.
For full description and to apply, please visit https://bit.ly/3IHHE6a
Interested candidates should also submit a cover letter, CV, and contact information for three references to:
Gregory J. Fermann, MD
Professor and Chair, Department of Emergency Medicine
Email: gregory.fermann@uc.edu
Applications will be reviewed on a rolling basis until positions are filled.
As a UC employee, and an employee of an Ohio public institution, if hired you will not contribute to the federal Social Security system, other than contributions to Medicare. Instead, UC employees have the option to contribute to a state retirement plan (OPERS, STRS) or an alternative retirement plan (ARP).
To learn more about why UC is a great place to work, please visit our careers page at https://www.uc.edu/careers.html
FOR ALL FACULTY HIRES OFFICIAL ACADEMIC TRANSCRIPTS WILL BE REQUIRED ATTHE TIME OF HIRE

EM Jobs Now on SAEM Facebook
Does your institution have an open position it’s looking to fill? Contact John Landry at 847-257-7224 or jlandry@saem.org to add your name to the career widget on our SAEM Facebook page. Job seekers: Click on “Careers” on the left-hand menu of SAEM’s Facebook page to view recently posted jobs in academic emergency medicine.
Free CV Critique
Did you know that EM Job Link offers a free CV critique service to job seekers? As a job seeker, you have the option to request a CV evaluation from a writing expert. You can participate in this feature through the CV Management section of your account. Within 48 hours of opt-in, you will receive an evaluation outlining your strengths, weaknesses and suggestions to ensure you have the best chance of landing an interview.
Job Alert!
Are you looking for a job in academic emergency medicine? Create a personal job alert on EM Job Link so that new jobs matching your search criteria will be emailed directly to you. Make sure the perfect opportunity doesn’t pass you by. Sign up for job alerts today on EM Job Link by clicking on Job Seekers and then selecting Job Alerts. You will be notified as soon as the job you’re looking for is posted.
UPDATE YOUR PROFILE






Penn State Health Emergency Medicine
About Us: Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pennsylvania



May 18-21, 2026 | Atlanta Marriott Marquis