




Chief Executive Officer
Megan N. Schagrin, MBA, CAE, CFRE mschagrin@saem.org
Director, Finance & Operations
Doug Ray, MSA, dray@saem.org Manager, Accounting Edwina Zaccardo, ezaccardo@saem.org
Director, IT
Anthony "Tony" Macalindong, amacalindong@saem.org
IT AMS Database Specialist
Dometrise "Dom" Hairston, dhairston@saem.org
Specialist, IT Support Dawud Lawson, dlawson@saem.org
Director, Governance
Erin Campo, ecampo@saem.org
Manager, Governance Juana Vazquez, jvazquez@saem.org
Director, Communications & Publications
Laura Giblin, lgiblin@saem.org
Sr. Manager, Communications & Publications
Stacey Roseen, sroseen@saem.org
Manager, Digital Marketing & Communications, Alison “Ali” Mistretta amistretta@saem.org
Specialist, Web and Digital Content Alex Gorny, agorny@saem.org
Sr. Director, Foundation and Business Development
Melissa McMillian, CAE, CNP mmcmillian@saem.org
Sr. Manager, Development for the SAEM Foundation
Julie Wolfe, jwolfe@saem.org
Manager, Educational Course Development
Kayla Belec Roseen, kroseen@saem.org Manager, Exhibits and Sponsorships
David Perez, MSMC, dperez@saem.org
Director, Membership & Meetings
Holly Byrd-Duncan, MBA, hbyrdduncan@saem.org
Sr. Manager, Membership
George Greaves, ggreaves@saem.org
Sr. Manager, Education
Andrea Ray, aray@saem.org
Sr. Coordinator, Membership & Meetings
Monica Bell, CMP, mbell@saem.org
Specialist, Membership Recruitment
Krystle Ansay, kansay@saem.org
Meeting Planner
Kar Corlew, kcorlew@saem.org
AEM Editor in Chief
Jeffrey Kline, MD, AEMEditor@saem.org
AEM E&T Editor in Chief
Susan Promes, MD, AEMETeditor@saem.org
AEM/AEM E&T Peer Review Coordinator
Taylor Bowen, tbowen@saem.org aem@saem.org, aemet@saem.org
CONTACT US!
Monday - Thursday: 8 a.m. to 5 p.m. CT; Friday: 8 a.m. to 3 p.m. CT Phone: (847) 257-SAEM (7236) or email: saem@saem.org
Wendy C. Coates, MD President
UCLA Department of Emergency Medicine
David Geffen School of Medicine at UCLA
Ali S. Raja, MD, DBA, MPH President Elect Massachusetts General Hospital/Harvard
Members-at-Large
Pooja Agrawal, MD, MPH
Yale University School of Medicine
Jeffrey Druck, MD
The University of Utah School of Medicine
Julianna J. Jung, MD
Johns Hopkins University School of Medicine
Nicholas M. Mohr, MD, MS University of Iowa
Michelle D. Lall, MD, MHS Secretary Treasurer Emory University
Angela M. Mills, MD Immediate Past President Columbia University Vagelos
Ava E. Pierce, MD UT Southwestern Medical Center, Dallas
Jody A. Vogel, MD, MSc, MSW Stanford University
of Emergency Medicine
Resident Member Michael DeFilippo, DO, MICP
- Columbia & Cornell


“It has been my sincere pleasure to serve as your president this past year, and I eagerly anticipate future collaborations as we continue our efforts to advance academic emergency medicine.”

UCLA Department of Emergency Medicine
David Geffen School of Medicine at UCLA
2023-2024 President, SAEM
The 2024 NRMP Match demonstrated the tenacity of our specialty, as we welcomed over 3,000 new colleagues who will begin their residencies in July 2024. Through our collaboration with the "All EM Match Task Force," we adopted a specialty-wide approach to recruitment and the dissemination of a positive message about our field. Residency program leaders and clerkship directors nationwide worked diligently to create an unparalleled experience for residents and medical students that underscored the advantages of being an emergency medicine physician. Departmental leaders, faculty, and residents played pivotal roles in conveying this message. SAEM remains committed to supporting the advancement of academic EM and will continue to provide resources for both trainees and faculty. As the new academic year begins, I encourage you to extend a welcoming hand to those entering our specialty. Embrace the role of mentor, seek out mentorship opportunities, and build networks and connections that will shape the future of academic EM. Together, through mentorship and collaboration, we can realize our vision and mission.
I look forward to connecting with many of you at SAEM24 — the Society’s 35th SAEM Annual Meeting. Aligned with our mission to advance education, research, and professional development, this event offers something for everyone. Academies (complimentary with SAEM membership), committees, and interest groups will host in-person meetings, open to all attendees, providing an opportunity to gain insight into these groups and connect with their members. With over
1,000 educational presentations covering various aspects of EM academics, including nearly 800 research abstracts, attendees will find ample opportunities for professional development. For our SAEM families we will once again provide an on-site private family/lactation room equipped with everything to meet baby and parent needs.
On Wednesday, Robert Neumar, MD, PhD, will deliver the Dr. Peter Rosen Memorial Keynote titled “Emergency Medicine Research: Past, Present, and Future.” Following his presentation, four plenary abstracts will be featured. SAEM remains dedicated to expanding opportunities for emergency care researchers and has collaborated closely with the NIH this year to identify shared interests with individual Institutes, maintaining a strong relationship with the Office of Emergency Care Research. We are eagerly anticipating the launch of the new K12 initiative, the Emergency Medicine Research Career Development Program in Neurological Sciences. This program, spearheaded by the Office of Training and Workforce Development (OTWD) at the National Institute of Neurological Disorders and Stroke (NINDS), is designed to recruit, mentor, train, and support early-career emergency medicine faculty. Its primary goal is to enhance their ability to conduct NIH-funded research on neurological disorders in both pre-hospital and emergency department settings. Further details can be found on page 50 of this issue of Pulse. SAEM's proactive
on Page 4

PRESIDENT'S COMMENTS
continued from Page 3
approach and strategic partnerships in achieving this milestone mark a significant advancement in emergency medicine research, ensuring progress and innovation in the field.
On Thursday, Holly Caretta-Weyer, MD, MHPE, will present the Education Keynote, titled “Patient-Focused and Learner-Centered: The Promise of Competency-Based Medical Education,” likely to be of interest to
all EM practitioners. CompetencyBased Medical Education (CBME) is poised to become a standard learning and assessment strategy throughout medical education, from medical school to continuous certification. SAEM actively participates in a specialty-wide working group to determine the optimal implementation strategy. Dr. CarettaWeyer’s lecture will be followed by four additional plenary abstracts focusing on education research.
Find everything you need to “Know Before You Go” to SAEM24 on page 12 of this issue of SAEM Pulse!
Lastly, I extend my gratitude to each SAEM member for your dedication to emergency medicine. It has been my sincere pleasure to serve as your president this past year, and I eagerly anticipate future collaborations as we continue our efforts to advance academic emergency medicine.
ABOUT DR. COATES: Wendy Coates, MD, is professor of emergency medicine at David Geffen School of Medicine at UCLA and senior faculty/ education specialist at UCLA Department of Emergency Medicine
The annual SAEM Foundation (SAEMF) Challenge is underway! YOUR gift or pledge to SAEMF by August 31 will help your Academy, Committee, or Interest Group rise to the top.

saem.org/donate
Winning groups will receive:
Bragging rights for a year!
A special treat at your group meeting during SAEM25
Recognition as the 2024 Challenge champions in SAEM communications
Challenge donors will also be recognized as Annual Alliance Donors
Thanks to generous SAEM members, many of whom are Challenge donors, SAEMF invested close to $1 million in the research and career development of its 2024-25 research and education grantees. Let’s take the next step to transform emergency care together – become an SAEMF Challenge donor today at saem.org/donate.
“I am so grateful for the grant I received from SAEMF. It allowed me to help jumpstart my research looking at the clinician workforce. Since my initial pilot award from SAEMF, I’ve subsequently gone onto obtain two separate R01 grants from NIH related to clinician psychological and cardiovascular health. The funding allowed me to work with a number of mentees and other trainees passionate about this area.
I am grateful for the support from SAEMF and its supporters!”
Bernard P. Chang, MD, PhD Associate Dean of Faculty Health and Research Career Development Vice Chair of Research, Tushar Shah and Sara Zion Associate Professor of Emergency Medicine
Angela M. Mills, MD
Immediate Past President, 2023-2024 SAEM Board of Directors
J. E. Beaumont Professor and Chair of Emergency Medicine Services, Columbia University Irving Medical Center and Chief of Emergency Medicine Services, NewYorkPresbyterian.
Dr. Mills is SAEM Board Liaison for the following groups:
President: Kathleen “Kat” Ogle, MD Overview
The Academy for Women in Academic Emergency Medicine (AWAEM) was established to promote the recruitment, retention, advancement, and leadership of women in academic emergency medicine. The success of academic emergency medicine and the ability of the specialty to train future emergency physicians are intrinsically linked with the success of women faculty as they now represent half of the medical student body and almost half of physicians
Wellness Committee co-chairs: Mia Karamatsu, MD and Wendy Sun, MD
• A to Z Wellness Tips included in WhatsApp chats for AWAEM members
• Webinar on Chrononutrition
• Life Hacks Didactic
Awards Committee co-chairs: Amy Zosel, MD, MSCS and Nancy Jacobson, MD
• Current AWAEM Awards are: Administrator Award, Catalyst Award, Early Career Educator Award, Early Career Research Award, Grant Writing Workshop, Legacy Award (new last year), Mentor Award (new this year), Mid-Career Faculty Award, Outstanding Department Award, Resident Travel Award, SAEM Leadership Forum (SAEMLF) Scholarship, and Social Medicine Advocacy Award
Research Committee co-chairs: Jennifer Love, MD and Joe-Ann Moser, MD, MS
• AWAEM K Club
• Research Consult Service
• Pilot grants
• Multiple didactics
Letter Writers’ Bureau lead: Mary Tanski, MD, MBA
• Resource for AWAEM members going up for promotion
• Working with Faculty Development Committee on collaboration
• Streamlining the demographic updates to the list
Chair: Fiona Gallahue, MD Overview
SAEM Consultation Services provides emergency medicine (EM) departments and institutions the opportunity to improve their practices by leveraging the expertise of accomplished SAEM committee and academy members. Consultation Services currently offers consultations in residency consultations, academic departmental consultations, and faculty development consultations.
• The committee, in partnership with the SAEM ED administration and clinical operations committee, finalized the operations consultation service (featured in the Mar-Apr 2024 Pulse). Lead: Dr. Casey Clements.
• In partnership with AACEM the committee finalized two SAEM
research consultation services: federal funding and general. Lead: Dr. Aasim Padela.
• Two new initiatives are currently in process:
° Wellness consultation in partnership with the SAEM Wellness Committee, Lead: Dr. James O’Shea. A needs analysis from department chairs and residency program directors has been completed. Pilot of a wellness consultation with a volunteer residency program is underway. After this pilot and feedback, a formal rollout of the wellness consultations is anticipated in 2025.
° Ultrasound consultation in partnership with the SAEM Academy of Emergency Ultrasound, Lead: Dr. Joshua Guttman.
Chair: Nancy Kwon, MD, MPA
The Faculty Development Committee (FDC) is charged with achieving objectives set forth by the SAEM President and Board for the development of tools and techniques to assist academic faculty physicians throughout the course of their careers.
• Implementation of inaugural vice chairs (Drs. McCoin and Gupta) to sponsor objectives and for faculty development and succession planning
• Creation of the SAEM’s first Academic Job Toolkit (pending publication to the SAEM website)
• Update to the Academic Career Guide originally published in 2019 (pending publication to the SAEM website)
• A total of 7 SAEM didactics/ presentations Sponsored by FDC were accepted for SAEM24 on a diversity of faculty development topics
• SAEM Pulse articles published
° Faculty Focus on Dr. Sanjey Gupta (Jan-Feb 2024 issue)
° Challenges of a New Residency Program (Nov-Dec 2023 issue)
° Faculty Focus on Dr. Jeffrey Glassberg (Sept-Oct 2023 issue)
• In collaboration with the Membership Committee, the addition of faculty development related questions in the upcoming Membership survey
• Recruitment and engagement for the committee has been high with over 100 members at all academic levels.
• Collaboration with AWAEM on an academic promotion letter writers bureau and advisors to assist SAEM members seeking promotion to associate professor and professor
• Development of a career webinar series with a diversity of speakers geared toward residents on topics related to early leadership development
• Development of a continuing faulty development toolkit for junior and midcareer faculty
• Creation of an academic metric dashboard/framework for evaluating academic productivity that chairs can use as a foundation to build their own internal metrics and dashboards (in collaboration with AACEM)
Co-Chairs: Basmah Safdar, MD and Neha Raukar, MD, MS
In the past year, the Vice Chair Interest Group has undertaken several significant responsibilities, aligning its efforts with strategic goals to enhance community
building, membership engagement, content development, and partnership initiatives.
• Community Building and Networking: The group prioritized fostering connections among its members by organizing in-person networking meetings at prominent events such as ACEP/AACEM/SAEM, providing valuable opportunities for collaboration and relationship building. We also had zoom meetings monthly to build a community and a sense of “togetherness” where we discussed challenges and solutions.
• Membership Recruitment and Engagement: Through targeted content development tailored to the interests and expertise of vice chairs, the group successfully increased membership recruitment and engagement, ensuring relevance and value to its diverse membership base.
• Content and Resource Development: Collaborating closely with AACEM, the Vice Chairs Interest Group decided to create a comprehensive repository of role descriptions for vice chairs, serving as a valuable resource for members navigating leadership roles within their institutions.
• Fundraising Success: The group partnered with SAEM to secure funding, emerging victorious in the funding challenge, and reaffirming its commitment to supporting initiatives that benefit its members.
• Educational Initiatives: Regular bimonthly virtual meetings were organized, focusing on pertinent topics that were obtained after surveying the members such as “Managing up for Vice Chairs,” addressing health care unionization, fostering diversity, equity, and inclusion, and exploring alternative career trajectories for vice chairs beyond chair positions.
• Facilitated Communication: The establishment of a dedicated vice chair email server enabled seamless asynchronous communication, providing members with a platform to address queries and concerns regarding various operational aspects, including weekend coverage, residency applications, and the integration of community attendings into academic medical centers.
As the Vice Chair Interest Group moves forward, its focus remains on increasing visibility and further enhancing membership participation. The group is committed to exploring innovative approaches to engage members actively, amplify their voices, and provide meaningful support throughout their leadership journey. The Vice Chair Interest Group expresses gratitude for the ongoing support and participation of its members. Together, they will continue to drive positive change and empower members to excel in their roles.

Robert Neumar, MD, PhD, chair of emergency medicine at the University of Michigan, is well-regarded for his contributions to emergency care research. The primary focus of his research over the past 35 years has been cardiac arrest resuscitation. He has mentored medical students, doctoral candidates, residents, post-doctoral fellows, and NIH K-award recipients. A leading advocate for federally funded emergency care research, Dr. Neumar served as the inaugural co-chair of the ACEP/SAEM Task Force on Emergency Care Research, which played a pivotal role in facilitating the 2009 NIH Roundtables, establishing the first NIH K12 program dedicated to emergency care research in 2011, and founding the NIH Office of Emergency Care Research.
Dr. Neumar formerly led the ACEP Research Committee, ACEP Scientific Review Subcommittee, and ACEP Research Section. Currently, he cochairs the AACEM Research Workgroup, playing a key role in developing the Emergency Medicine Research: 2030 Strategic Goals. He also serves as the co-chair for the International Liaison Committee on Resuscitation (ILCOR).
Dr. Neumar's significant contributions to the field have earned him several accolades, including the ACEP Award for Outstanding Contribution in Research, the SAEM John Marx Leadership Award, the AACEM Distinguished Service Award and his election to the prestigious National Academy of Medicine.
Dr. Neumar will deliver the SAEM24 Dr. Peter Rosen Memorial Keynote, "Emergency Medicine Research: Past, Present, and Future," on Wednesday, May 15, 2024. In his keynote address, Dr. Neumar will explore the evolution of research in the specialty of emergency medicine. Focusing on the pivotal role of research in driving advancements to improve patient care, he will trace the specialty’s growth over the past few decades, assess the present condition of our research enterprise, and articulate a vision for the future.



What are some of the most significant changes, challenges, and advancements you've witnessed throughout your career, particularly in the realm of research?
The most significant change I have witnessed is the growth of the research workforce in the specialty of Emergency Medicine. When I started my emergency medicine residency in 1990, there was only one EM faculty member in the entire country who was PI on an NIH-R01 grant. In 2023, there were 147 NIH-funded EM PIs with 206 active projects in 45 different departments of emergency medicine. Second is the diversification of our research capabilities across the spectrum of translation with the greatest growth in clinical and health services research.
Looking ahead, what do you perceive as the most urgent issues facing emergency medicine (EM) research in the next decade?
The most urgent research questions in emergency medicine will change over time, and any topic focused set of research priorities will likely be outdated by the time consensus is achieved. Therefore, what is most urgent is to build a diverse and sustainable research workforce and infrastructure within our specialty capable of addressing the most important research questions that arise over time.
Your role in shaping emergency care research and nurturing new investigators is noteworthy. Why do you believe cultivating independent researchers is vital for the field of emergency medicine?
As a medical specialty, the 140 million patients who seek care in our EDs every year expect us to discover new and better ways to care for them. We cannot rely on other specialties to make
those discoveries. We are on the front line. We know what is working and what is not working. Therefore, we need to be fully equipped to create new knowledge needed to improve ED patent care and outcomes. Otherwise we are not fulfilling our mission as a specialty.
What guidance do you have for early career EM researchers who aspire to establish themselves in the field?
Invest in yourself early in your career. Seek out the research training needed to answer the kind of questions you believe are most important and be sure the mentorship and resources needed to be successful are available. While taking time to get additional training may feel like it is delaying your career, it will in fact accelerate your career and make it much more sustainable.
How crucial do you deem mentorship to be in fostering a successful and rewarding research career, and what strategies do you recommend for building effective mentormentee relationships?
Good mentorship will accelerate your development as an independent investigator and help guide you away from paths that are unlikely to get you to your destination. Multiple mentors are key, especially with different expertise, experience, and strengths. A successful mentorship relationship requires effort and commitment from the mentor and even more from the mentee. As a mentee it is critical to put in the effort needed to take maximal advantage of the resources, guidance, and advocacy that your mentor provides.
continued on Page 10
Ribbon cutting ceremony for the Joyce and Don Massey Family Foundation Emergency Critical Care Center (EC3). From left to right is Kyle Gunnerson, founding EC3 medical director; Robert Neumar, emergency medicine department chair; Brenda Massy, Massy Family Foundation president; Jim Wooliscroft, medical school dean; Bill Barsan, former emergency medicine department chair; and Tony Denton, chief operating officer, Michigan Medicine

continued from Page 9
What aspects of working with learners do you find most fulfilling?
Most rewarding for me is to see the people that I have mentored succeed and advance in their careers.
What counsel would you offer to residents preparing for their initial academic job search?
Carefully consider why you have chosen an academic career. Think about what you want to achieve, and seek out opportunities that provide the infrastructure, resources, and mentorship that will optimize your chances of success. Once those pieces are in place, the rest is up to you.
What advice would you give mid-career faculty who are contemplating a career as a chair?
Carefully consider why you are seeking the role. Envision what you hope to accomplish over a 5-, 10- or 15-year period and weigh that against the personal sacrifice needed to be successful.
Dr. Neumar and wife Kathy out to dinner with Bob’s mom Janet in Ann Arbor, Michigan.“Invest in yourself early in your career... it will in fact accelerate your career and make it much more sustainable.”
In your view, what are some of the primary challenges and opportunities that a newly appointed chair may encounter?
Most important is to ensure that your vision as the department chair is aligned with the vision of the faculty, the medical school dean and health system leadership. Second is to secure any resources needed to achieve that vision. If either are missing, it is difficult to be successful and find joy in the role.
Balancing responsibilities as a chair, conducting research, fulfilling clinical duties, and maintaining a personal life can be demanding. How do you effectively manage these various roles and commitments?
I don’t think you can ever expect to achieve a steady state of balance. I think to be successful, priorities will always need to be out of balance at any one moment in order to give adequate focus to each role or responsibility. You just need to make sure each gets enough turns and time being the top priority.
What advantages can individuals derive from active involvement in national organizations like the Society for Academic Emergency Medicine (SAEM) and the Association of Academic Chairs in Emergency Medicine (AACEM)?
One of the major advantages of engaging with national organizations such as SAEM and AACEM is the opportunity to network with thought leaders in the field and have an impact beyond what can be achieved at the individual or institutional level. We have certainly seen this come to fruition with our advocacy for federal funding of emergency care research. Your list of your achievements is extensive. If you had to identify your most significant achievement as chair, what would it be?
Our departmental vision has been to create the future of emergency care. My hope is that what have contributed to that future by creating an innovative model of delivery critical care in the ED setting, training a generation of innovators and and leaders in the field, and building a research infrastructure, including new centers and institutes, that will continue to support the growth of scientific discovery in our specialty and beyond.
As you transition to the next phase of your career, what legacy do you aspire to leave behind? What will be your primary focus in this new chapter?
The legacy question will take some time to answer, but I hope that some what we have done will have a sustained impact on the field. The primary focus of this next chapter will be to help further develop our emergency medicine research workforce and infrastructure at the national and international level. I truly believe that global collaboration is a powerful mechanism to accelerate the advancement of emergency medical care and can help us move toward a world where the quality of care you receive is not dependent on where your medical emergency occurs.

What is a song one might overhear you singing in the shower? I don’t sing in the shower, but I do a lot of thinking in the shower and that is where I often get my best ideas.
Do you have a favorite quote you try to live by? The Serenity Prayer: God, grant me the serenity to accept the things I cannot change, the courage to change the things I can, and the wisdom to know the difference
What is your guiltiest pleasure (book, movie, music, show, food, etc.)?
Jalapeño potato chips
You have a full day without obligations — how do you fill it? Golf
What tops your bucket list? My wife Kathy and I living to be great grandparents.
What's one thing few people know about you? Former pole vaulter in high school and college.
Dr. Neumar and wife Kathy with granddaughters Ziggy and Eloise.





We’re excited to welcome you in Phoenix, Arizona for what promises to be THE academic emergency medicine event of the year and an educational experience you won’t soon forget. Get ready to immerse yourself in insightful workshops and engaging forums, connect with colleagues and thought leaders, and even indulge in some friendly competition! Our online Program Planner has all the details you need to plan your agenda. Just don't forget to carve out time for fun because Phoenix offers an array of experiences for everyone. Whether you're into live music, savoring authentic Southwestern cuisine, or exploring the breathtaking desert landscape, Phoenix has something to offer. So pick your passion, dive in, and savor Phoenix like a local — unwind, relax, and embrace every moment! Safe travels to Phoenix, and we can't wait to see you there!

The Sheraton Phoenix Downtown, at 340 North 3rd Street, is the official host hotel for SAEM24 meetings, educational sessions, and most events. Enjoy well-appointed guestrooms, inviting communal areas, fine on-site dining, a sunlit terrace pool, and a top-notch fitness center. Conveniently located minutes from Sky Harbor Airport, the Sheraton is just steps away from Phoenix’s vibrant arts and culture scene and worldclass dining and nightlife options. Meeting spaces are on floors 2-3, accessible by escalator, with additional space on the fourth level, accessible by elevator.
The fastest way to get from Phoenix Airport (PHX) to the Sheraton Phoenix Downtown is to taxi or use a ride hailing service which takes about 10 minutes and costs $15- $20.
The Sheraton does not have an airport shuttle.
There are several ways to navigate the city once you arrive:
Public Transportation
• Valley Metro Rail
• Phoenix Dial-a-Ride
• Guided Tours
Transportation Services
• Pedicabs
• Ride-hailing services
• Taxis
• Phoenix Transit Bus
• E-Scooters
• Downtown Phoenix
• E-Scooters
• Waymo (autonomous vehicle)
• Vehicle rentals



You should have received a confirmation email with a barcode. Please save this to your mobile device or print it out. You can scan it at our convenient self-serve preregistration kiosks, which are located near the SAEM24 registration desk on the second level, outside of the exhibit hall/Valley DE Foyer.
If you forget your confirmation, don’t worry! Just select ‘User Lookup’ on the screen and search for your name. Then hit print and your badge, along with any applicable tickets, will be printed out for you. Badge holders and lanyards will also be available at the kiosks.
As always, our fully staffed registration desk will be available to assist you. The SAEM24 registration area can be found on the second level outside the exhibit hall/Valley DE foyer.
Registration hours are as follows:
• Monday, May 13: 3 p.m.–6 p.m. MT
• Tuesday, May 14: 7 a.m.–6 p.m. MT
• Wednesday, May 15: 7 a.m.–7:30 p.m. MT
• Thursday, May 16: 7 a.m.–6:30 p.m. MT
• Friday, May 17: 7 a.m.–1:30 p.m. MT
Please remember that all annual meeting participants, including members, nonmembers, partners, children, and guests, must register and wear badges for admission to sessions, the exhibit hall, and most events.
If you’re a presenter and wish to review your slides, please visit the Speaker Ready Room located in the Coronado Boardroom on Level Three.

In adherence to CME Guidelines, all presenter disclosures and bios were required by April 8, and presentation slides were due by April 28. Only presentations where no presenter has anything to disclose may make edits to slides onsite. The Speaker Ready Room will be open during the following hours:
• Monday, May 13: 3 p.m.–6 p.m. MT
• Tuesday, May 14: 7 a.m.–5:00 p.m. MT
• Wednesday, May 15: 7 a.m.–5:30 p.m. MT
• Thursday, May 16: 7 a.m.–5:30 p.m. MT
• Friday, May 17: 7 a.m.–1:00 p.m. MT
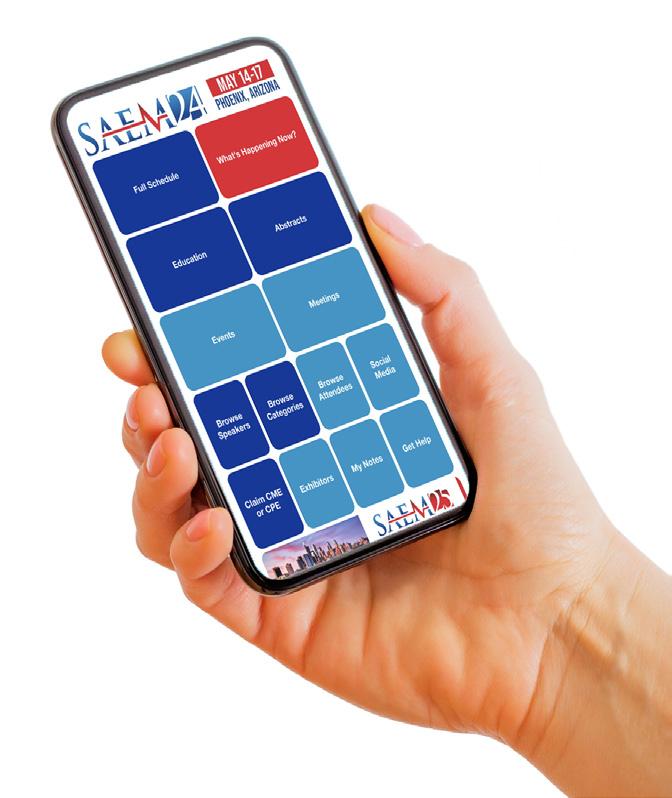
Navigate SAEM24 like a pro by downloading the SAEM Annual Meeting app. Download the app from the Apple App Store or Google Play, then log in using your SAEM username and password to get started. With the app, you can:
• Explore the full list of Advanced EM Workshops, educational sessions, meetings, and events.
• Access abstracts, learning objectives, and information about speakers for educational sessions.
• Navigate the exhibit hall using the online floor plan and create a personalized list of exhibitors you want to visit.

Need assistance with downloading or navigating the SAEM Annual Meeting app? Have questions about your SAEM membership? Visit the App Desk and Member Services at the Valley DE Foyer, located on the Second Level.
SAEM’s Medical Student Ambassadors (MSAs) will be stationed throughout the Sheraton Phoenix Downtown Host Hotel. They’ll be wearing blue, SAEM-branded jackets so they’ll be easy to spot. MSAs are ready to assist and answer any questions you may have.
Additionally, SAEM staff will be available at the registration desk during registration hours and at SAEM Booth #321 during exhibit hours to provide assistance.
Are you attending the SAEM Annual Meeting for the first time or have recently joined SAEM? Visit SAEM Booth #321 in the exhibit hall during exhibit hours to connect with us! Introduce yourself, get a professional headshot, pick up a tee shirt and some SAEM swag, and enter our drawing for a chance to win fun prizes. Our friendly staff is eager to meet you, share information about SAEM’s programs and services, and help you make the most of your experience at the annual meeting.
Tune in to SAEM’s Facebook and YouTube channels May 15-17 for live SAEM24 programming direct from Phoenix, Arizona.
Wed., May 15, 9:00 a.m.-5:20 p.m.
Awards Ceremony and Dr. Peter Rosen Memorial Keynote, select abstracts and didactics
Thurs., May 16, 9 a.m.-3:50 p.m.
Awards Ceremony, Education Keynote, education plenaries, select abstracts and didactics
Fri., May 17, 9 a.m.-12:50 p.m. Select didactics
To enhance your experience at the annual meeting, SAEM offers complimentary wireless Internet access. Enjoy Wi-Fi connectivity throughout the meeting space at the Sheraton Phoenix Downtown host hotel during SAEM24. Use the following credentials to connect:
• Username: SAEM24
• Password: AnnualMeeting
Our private family room, located in Room 444 on the Fourth Level, is fully
equipped to cater to the needs of parents and babies. Amenities include a refrigerator, wipes, sanitizer, burp cloths, a changing table, comfortable seating, water, and snacks. Feel free to visit the SAEM24 Family Room during the following hours:
• Tuesday, May 14: 7:30 a.m.–5:30 p.m. MT
• Wednesday, May 15: 7:30 a.m.–5:30 p.m. MT
• Thursday, May 16: 7:30 a.m.–5:30 p.m. MT
• Friday, May 17: 7:00 a.m.–1:00 p.m. MT
Stay connected with us throughout the annual meeting by following SAEM on Facebook,Twitter (@SAEMOnline and @SAEM_RAMS) and Instagram (using the hashtag #SAEM24). Get the latest meeting announcements and join the conversation with fellow attendees by sharing your insights.
Access SAEM24 educational content conveniently online at SOAR (SAEM Online Academic Resources) starting August 1. Explore over 120 hours of original content, including Advanced EM Workshops, didactics, and forums. Enjoy flexible viewing options on both desktop and mobile devices, with
downloadable PDFs and MP3 files for on-the-go learning. Dive deeper into presentations by viewing synchronized slides alongside audio. Simply log in with your SAEM username and password to access the content.
• Members have a professional and ethical obligation to act in a manner that upholds the purposes, values, and objectives of SAEM.
• Members shall conduct themselves in a professional manner while attending or participating in SAEM-sponsored events and all communications with SAEM staff.
• While alcohol is served at many SAEM events, members shall not use any substance to an excess that negatively impacts the member’s ability to act in a professional manner.
• Members shall be honest and fair, and act respectfully and with integrity.
• Members shall not discriminate against members or SAEM staff regarding religion, race, ethnicity, color, national origin, gender, gender identity, sex, sexual orientation, or disability.
Resident’s and medical students, at SAEM24, you can engage with expert faculty, experience excellence in innovation and research, and participate in tailored learning activities developed exclusively for you! It’s not just an event; it’s a platform for learning, reconnecting with peers, and fostering connections within the tight-knit emergency medicine community.

To help you build your personalized SAEM24 agenda, we’ve handpicked a selection of mustattend activities and events. While navigating the website, be sure to watch the informative video featuring insights and recommendations from RAMS Board Member-at-Large Zoë Fisher, offering valuable insider tips and her personal ‘don’t miss’ suggestions.
Still on the fence about attending? Here are the Top 10 Reasons Residents and Med Students Should Attend SAEM24, complete with a sneak peak at The Duce, the venue for this year’s RAMS Party!
Pro tip: When you see a Rams head icon next to an abstract, didactic, workshop, event or activity in the mobile app or program planner, it signifies sessions specifically designed to offer enhanced value for residents and medical students.
Conduct unbecoming of an SAEM member should be reported to the CEO. The SAEM Executive Committee may refer the case to the SAEM Ethics Committee, which will investigate any reported breaches of professional conduct. We reserve the right to enforce the SAEM Code of Professional Conduct up to and including removal of SAEM Membership.
The CME program offered by SAEM is targeted (but not limited to) emergency health care professionals such as medical students, allied health care providers (nurse practitioners, physician assistants), emergency medicine technicians, nurses, residents, fellows, researchers, faculty, and physicians.
Overall Program Objectives:
• To enhance participant knowledge of cutting-edge research being conducted in emergency medicine
• To provide physicians with the tools to address gaps in their knowledge competence, and experience
Joint Accreditation Statement: This activity has been planned and implemented in accordance with the accreditation requirements and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint providership of the University of Cincinnati and Society for Academic Emergency Medicine. The University of Cincinnati is accredited by the ACCME to provide continuing medical education for physicians. The University of Cincinnati designates this live activity for a maximum of 30 AMA PRA CME Category 1 Credits™ Physicians should claim only the credits commensurate with the extent of their participation in the activity.

The University of South Carolina College of Pharmacy is accredited by the Accreditation Council for Pharmacy Education as a provider of continuing pharmacy education. This activity is eligible for ACPE credit; see final CPE activity announcement for specific details.
From tranquil desert gardens to one-ofa-kind museums, award-winning dining to thrilling desert adventures, urban exploration to leisurely margaritas by the poolside, Phoenix offers an array of experiences waiting to be discovered. Here’s a starting point to ignite your exploration:
1. Roosevelt Row Arts District
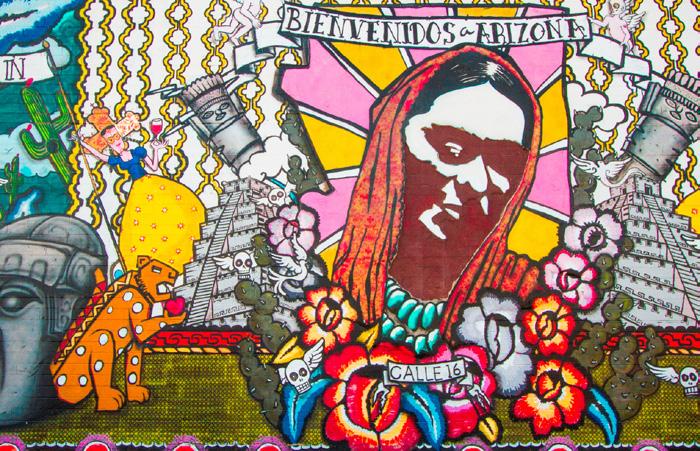
A vibrant, walkable arts district boasting art galleries, restaurants, bars, and boutique shops set against a backdrop of colorful street art.
Bonus: “Mural Alley” mapped out here
2. Papago Park

1,500 acres of picnic areas, lagoons, biking and hiking trails (including the famous “Hole in the Rock” hike ) in one of Arizona's most scenic desert areas
Bonus: Desert Botanical Garden and Phoenix Zoo
3. Phoenix Art Museum
The southwest’s largest art museum, this cultural gem in the heart of the city boasts a collection of 20,000 objects spanning the globe, from modern to contemporary art, photography to fashion.
Bonus: Barbie: A Cultural Icon exhibit
4. Camelback Mountain

Named for the distinctive silhouette it casts on the Valley skyline, experienced hikers can choose between two challenging trails that ascend 1,420 feet to the summit, where breathtaking 360-degree views await, showcasing the sprawling cityscape below.
Bonus: 8 restaurants with stunning views of Camelback
5. Heard Museum

Explore the rich tapestry of indigenous cultures through a diverse array of exhibits, including 12 galleries showcasing both contemporary and historic masterpieces.
Bonus: Extensive collection of Hopi Katsina dolls
6. Musical Instrument Museum
Explore the world’s largest collection of musical instruments and more than15,000 artifacts from over 200 countries.
Bonus: Acoustic America: Iconic Guitars, Mandolins, and Banjos
Discover the quintessential flavors of Phoenix with these must-try food and libation classics, along with the perfect spots to savor them.

Chicago has its celery salt and bright green relish (no ketchup). In New York it’s sauerkraut and brown mustard. In Phoenix, the bacon-wrapped, pintobean topped Sonoran reigns supreme. Here’s a selection of local joints in Phoenix that do the dog right:
• Caprichoso
• Moreno’s Mexican Grill
• La Pasadita
• Nogales Hot Dogs Stand
• El Sabroso Food Truck
Prickly Pear Margaritas

Phoenix is a tequila town and the pretty pink prickly pear margarita is its unofficial signature drink. You can order this fresh and fruity cocktail almost anywhere in Phoenix. This will get you started:
• Blanco Tacos + Tequilas
• Taco Chelo
• Chelsea’s Kitchen
• El Chorro
• Joyride Taco House
• Modern Margarita
• Rito’s Mexican
• Sandbar Mexican Grill
Bonus
• Cheese Crisps at Rosita’s Place
• Chimichanga at Macayo’s
• Fry Bread at Fry Bread House
Best Tacos
Tacos are everywhere in Phoenix. From succulent carne asada to tender pollo asado with a smoky twist, and even refried pinto beans served in fry bread, here are a few spots where you can indulge your craving:
• Taco Guild
• Blanco Tacos + Tequilas
• Chico Malo
• Barrio Queen
• La Santisima Taco Shop
• Tacos Chiwas
• Ta’Carbon
In May, Phoenix offers the perfect blend of warm days and cool nights, making outdoor dining an unforgettable experience. Here are a few options for enjoying the many flavors of the Valley under open skies:
Rooftop
• Théa
• Different Pointe of View
• Don Woods’ Say When
• From the Rooftop
• Floor 13
• Rustler’s Rooste
Patio
• Arizona Wilderness Brewing
• Chelsea’s Kitchen
• Cibo
• Ocotillo
• Palma
• Windsor


Since its inception in 2012, the annual Sonogames event has experienced remarkable growth, evolving into an interactive, gamified educational experience for resident learners. Organized annually by the SAEM Academy of Emergency Ultrasound (AEUS), the Sonogames Planning Committee, and the SAEM Executive Committee, this event not only involves participants in hands-on learning but also delivers passive education to a broader audience. It has become a highlight of the SAEM Annual Meeting, drawing avid “Sonophiles” from across the United States and around the globe. This year’s event takes place on Friday, May 17, in Phoenix, Ariz. during SAEM24.
Reflecting on my experience as a junior resident attending the inaugural games in 2012, I had the opportunity to witness my Boston Medical Center co-residents Joe Pare, Derek Wayman, and Neil Hadfield clinch the gold (this superstar team won again in 2013!). At that time, the event featured a simpler format, lacking the elaborate costumes and clever team names seen in recent years. Nonetheless, it was a resounding success, laying the groundwork for the immersive educational experience it has become.
While a select few in our community (you know who you are!) have played pivotal roles in shaping Sonogames over the past decade, it is the collective effort of many that brings this innovative educational experience to lif each year.
From crafting peer-reviewed questions to coordinating equipment and logistics, organizing Sonogames is a year-long endeavor requiring dedication and meticulous planning.
The impact of Sonogames extends beyond resident participants, fostering an inclusive experience for all to engage with point-of-care ultrasound (POCUS). Over the years, attendees have witnessed its evolution, with Di Conneybeare, emergency ultrasound fellowship director at Columbia University Irving Medical Center, noting, “Sonogames has transformed clinical ultrasound from something that only a geeky few would touch into rock star
continued on Page 18

SAEM24 SPECIAL FEATURE continued from Page 17
status as a highly coveted and essential skill.”
Romolo Gaspari, executive vice chair of the Department of Emergency Medicine at UMass, aptly described it in the 2018 Sonogames history video: “Over time it has evolved to being kind of like a carnival — there are examinations and competitions, but it is completely different from any other type of education.”
To trace the origins of this phenomenon, let us rewind to 2011 and the establishment of AEUS. Driven
by a need for innovative educational initiatives amidst the growing demand for POCUS training, Sonogames emerged under the leadership of AEUS President Dr. Resa Lewiss and AEUS Education Chair Dr. Andrew Liteplo, as a fun and interactive solution. All United States emergency residency programs were invited to send three of their residents to participate as a team. With POCUS as an Accreditation Council for Graduate Medical Education (ACGME) core competency at that time, the games served to assess both resident knowledge and performance Initially spanning three rounds over four hours, the event has since expanded dramatically, now boasting over 100 participating teams.
Originally, Round 1 consisted of a multiple-choice test with image review-style Type 1 questions. The correct and incorrect answers were then reviewed in real-time, providing education for volunteers, cheerleaders, and participants. That first year, the five top-scoring teams then proceeded to Round 2, an interactive and handson ultrasound activity. Finally, the top teams advanced to the final round, a game show event, to once again test ultrasound knowledge and determine a winner.
Since then, the format has evolved. Round 0, the most recent addition, occurs before the SAEM Annual Meeting and presents the teams with a competitive challenge ranging from making a POCUS-related video to creating a song. While Round One remains multiple choice, with 25 questions of varying point values related to difficulty, the questions have evolved from Type 1 to Type 2 questions. Additionally, after the multiple-choice questions, Round 1 now includes a hands-on scan portion, often scanning a phantom to identify buried objects, allowing all teams to participate in some hands-on fun. After the completion of Round 1a and Round 1b, the top 15 teams (rather than 5) will progress to Round 2, allowing continued participation for a larger number of teams.
Since as early as 2013, resident competitors have begun to devise creative POCUS-related team names (and corresponding costumes) such as “Fast Scans of Ridgemont High,” “If


You Like It Then You Should Have Put a Probe on It,” “Betty and the Ureteral Jets,” “Fifty Shades of Grayscale,” and “Scrotal Pearls of Wisdom.” Event themes, particularly for Round 2 stations, often relate to the host city. In New Orleans, there was a Mardi Gras theme including a crawfish boil at one of the stations; Indianapolis had a car racing theme; Las Vegas featured a casino theme, and there was a NASA theme at one of the Texas games.
Chris Fox, MD, chair of emergency medicine and director of ultrasound in medical education at the University
of California, Irvine, sums it up well: “Sonogames gamifies the process of learning; people get into the competitive spirit and they start ingesting the material in a real way.”
Megan Leo, MD, former ultrasound section chair now quality director, at Boston Medical Center, adds, “Learners do better and retain knowledge better when you make it into a game and make it fun.”
The effectiveness of Sonogames was described in a 2018 survey study, revealing significant increases in POCUS
knowledge, enthusiasm, and clinical utilization among participants. 81% of participants felt their POCUS knowledge increased, 87% felt their enthusiasm for POCUS increased, and 61% reported an increased use of POCUS clinically as a result of participating in Sonogames. Such findings underscore the profound impact of this gamified approach to education. As a POCUS division and fellowship director who stays up nights trying to figure out how to effect positive POCUS culture change, these statistics are particularly impressive.
In summary, Sonogames stands as a testament to the power of gamification in medical education, inspiring learners and driving positive change within the field of emergency ultrasound. As we eagerly anticipate this year’s event, let us celebrate the ingenuity and dedication of its creators and look forward to the insights and innovations that await us in 2024.
Recognizing everyone who has contributed to the planning and execution of the 2012-2023 Sonogames would be an immense task, and regrettably, we might inadvertently overlook some while acknowledging others. Therefore, we extend our heartfelt gratitude to the entire community for their invaluable contributions to this educational success over the past 12 years.

Dr. Dwyer is director of the Division of Emergency Ultrasound (EUS) and director of the EUS Fellowship, as well as associate professor of emergency medicine and teaching scholar in the Department of Emergency Medicine at The Warren Alpert School of Medicine at Brown University.

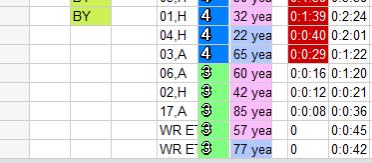
The problem of boarding in emergency departments (ED) in the United States has reached alarming proportions, reflecting systemic issues within the health care infrastructure. With increasing demands on emergency services, EDs often operate at or beyond capacity, leading to prolonged wait times. This impediment to the flow of incoming cases has led physicians to see fewer new patients in each shift, leaving emergency medicine (EM) physicians frustrated and dissatisfied as patients remain unseen in the waiting room. Additionally, it has led to a decline in the skills required to manage higher patient volumes and interfered with imparting those skills to trainees. While
“Acknowledging the challenge we face is the first step. Our patients are safer awaiting us in ED care spaces than in the waiting room.”
the solution is to reduce or eliminate boarding, a new challenge has emerged — the stress a physician feels when overwhelmed by an increasing number of patients bedded but awaiting a provider. On our electronic tracking board (see Figure 1), these patients are in all white, leading to our term “white space anxiety.”
The Adult Emergency Department (ED) at our institution is a beacon in trauma and acute care services, a level 1 trauma center, welcoming approximately 81,000 new adult arrivals annually. As the regional academic site, it plays a pivotal role in shaping medical education and practice in the region. Recent assessments, however,

shed light on a concerning trend: our emergency department ranked 4th in the total number of boarding hours in 2023, averaging a staggering 1,135 hours per day according to AAAEM Benchmark results.
In the face of this challenge, there's been a notable shift catalyzed by the swift implementation of effective hospital flow strategies. Over a remarkably short span of time, the ED witnessed a significant reduction in patient boarding, marking a 25% decrease from 1,159 hours per day in December 2023 to 896 hours per day in February 2024. Remarkably, this improvement was achieved while maintaining similar admission rates and even experiencing an uptick in the number of patients seen per day.
However, this reduction in boarding hours revealed a new bottleneck within the system — the providers themselves. Timely access to patients became hindered as physicians struggled to keep pace with the influx of cases.
Addressing this issue necessitates a multifaceted approach, starting with ensuring appropriate and aligned staffing levels. Once there is adequate staff and a reasonable flow of patients to their work areas, leadership must devise strategies to support physicians and trainees in adapting to the increased workload, fostering skills in multitasking and the development of coping mechanisms.
Acknowledging the challenge we face is the first step. Our patients are safer awaiting us in ED care spaces than in the waiting room. With renewed practice, we will be able to juggle our numerous patient care tasks in parallel. Through frequent communication with our nursing partners, we can still assure patient safety and improve patient experience.
This transition, while eagerly anticipated at our institution, does require an adjustment period. Adapting to these new conditions is challenging, particularly considering the upheavals caused by the onset of COVID-19. However, with
commitment, flexibility, and strategic support, our ED will continue its mission of delivering exemplary emergency care to the community it serves.

Dr. Gemme is associate professor and chair of the Department of Emergency Medicine at the University of Massachusetts Chan Medical School – Baystate. Prior to this role, he served as vice chair of clinical operations, overseeing the operations of five emergency departments in the system.

Dr. Lutfy-Clayton is an associate professor in emergency medicine, chief of service for the Baystate Medical Center Adult ED, and medical education fellowship director in emergency medicine at Baystate Medical Center, as well as head of professional development.


Dr. Kellogg is associate professor and residency program director in the Department of Emergency Medicine at the University of Massachusetts Chan Medical School – Baystate.
Dr. Kramer is currently a PGY-2 resident in the Department of Emergency Medicine at the University of Massachusetts Chan Medical School –Baystate.

Acute respiratory distress syndrome (ARDS) is a common diagnosis in ICUs with a high mortality rate. Despite decades of research, few treatments have shown a mortality benefit. Globally, ARDS accounted for 10% of all ICU admissions in the LUNGSAFE prevalence study, with continued under-recognition and undertreatment. In its severe form, the hospital mortality rate was 46%. For COVID-19 ARDS, reported mortality rates were as high as 80%. Given this high mortality despite treatment, there is increased focus on ARDS prevention. In a concise clinical review for the 50 Years of Research in ARDS series, the rationale, current
evidence, and future directions in ARDS prevention were summarized, posing the question: Is Acute Respiratory Distress Syndrome a Preventable Disease? Herein, we summarize the work thus far in the investigation, prediction, and prevention of ARDS in at-risk populations.
In 2008, a grand challenge for the United States Critical Illness and Injury Group (USCIITG) was a proposed shift in clinical investigation toward lung injury prevention. A year later, the Division of Lung Disease of the NHLBI convened a workshop of international experts who “the capability to perform ALI prevention trials should be developed.”
Around the same time, the USCIITG Lung Injury Prevention Study Group enrolled 5,584 emergency department (ED) and high-risk surgical patients over six months, developed, and validated the Lung Injury Prediction Score (LIPS). This score identified patients at high risk for acute lung injury (ALI) early in their illness course. LIPS discriminated patients who developed ALI from those who did not with an AUC of 0.80 (95% CI, 0.78-0.82). After adjusting for illness severity and predisposing conditions, ALI development increased in-hospital mortality odds by 4.1 (95% CI, 2.9-5.7).
LIPS, derived from a heterogeneous cohort, showed varied utility in specific
populations and settings. It performed well in a cohort of surgical critical care patients with an AUC of 0.79 (95% CI, 0.74-0.84). However, it underperformed in a cohort of 900 adult non-ED hospitalized patients with at least one ARDS risk factor, with an AUC of 0.70 (95% CI, 0.64–0.74).
Subsequent efforts were made to refine LIPS for specific populations. A LIPS ancillary study was performed for the subgroup of 1,233 high-risk surgical patients (22%) to derive a Surgical Lung Injury Prediction (SLIP) score, and the SLIP-2 score for predicting risk of early postoperative ARDS performed well with an AUC of 0.84 [95% CI, 0.81-0.88]. In addition, a subgroup analysis was performed on the 4,351 ED patients (78%) to derive and validate an EDLIPS model. The ED cohort incidence of ALI was 7.0%, and EDLIPS discriminated patients who developed ALI from those who did not with an AUC of 0.78 (95% CI 0.75, 0.82), similar to LIPS (p = 0.07). At an EDLIPS cutoff of 5, positive and negative likelihood ratios for ALI development were 2.74 (95%, 2.43-3.07) and 0.39 (95%, 0.30-0.49), respectively, with a sensitivity of 0.72 (95%, 0.64-0.78), specificity of 0.74 (95% CI, 0.72-0.76), and positive and negative predictive values of 0.18 (95% CI, 0.15-0.21) and 0.97 (95% CI, 0.960.98). Another ED-specific ALI prediction model developed was the early ALI (EALI) score, which had an AUC of 0.86 and performed similarly to LIPS. An EALI score ≥ 2 accurately identified patients who progressed to ALI requiring positive pressure ventilation with 89% sensitivity and 75% specificity.
Internationally, LIPS performed well in a Korean ICU cohort, with an AUC of 0.82 (95% CI, 0.75–0.88), where a LIPS > 6 predicted the development of ARDS with 84.8% sensitivity and 67.2% specificity. In contrast, LIPS performed with an AUC of 0.77 (95% CI, 0.72-0.81) in a Chinese ICU cohort; this study cohort was also used for the derivation (AUC 0.80; 95% CI, 0.75-0.85) and validation (AUC 0.79; 0.71-0.86) of a modified ARDS prediction score (MAPS).
With respect to specific conditions, LIPS for COVID-19 (c-LIPS) was developed and validated in COVID-19 patients who required organ support and discriminated COVID-19 patients who did and did not develop ARDS with an AUC of 0.79, comparable to LIPS, which
had an AUC of 0.74 (P < .001). A study of acute pancreatitis patients, simplified both LIPS (sLIPS) and EALI (sEALI) and derived and validated both models to predict persistent acute respiratory failure; the authors showed that sLIPS was significantly more accurate than sEALI in both derivation and validation cohorts.
The development and validation of these lung injury prediction scores has allowed ARDS prevention trials to use these scores as inclusion criteria. ED patients with a LIPS ³ 4 were considered for inclusion in the 2012-2014 NHLBIfunded phase 2, multicentered, randomized controlled trial (RCT): Lung Injury Prevention Study with Aspirin (LIPS-A). However, the use of aspirin compared with placebo among at-risk ED patients did not reduce the risk of ARDS at 7 days. In a 2013-2015 RCT of 61 patients, early treatment with inhaled budesonide/formoterol in patients at risk for ARDS was feasible and improved oxygenation as assessed by S/F (LIPS-B). In a 2017-2018 phase 3 RCT, LIPS was incorporated in the NHLBI Prevention and Early Treatment of Acute Lung Injury (PETAL) Network Vitamin D to Improve Outcomes by Leveraging Early Treatment (VIOLET) protocol, as part of the baseline assessment and as an a priori subgroup for analysis. With ARDS as a secondary endpoint, there was no significant difference in new ARDS to 7 days between the Vitamin D and placebo groups.
Low tidal volume ventilation (LTVV) is the standard of care for patients with established ARDS, and it has been studied as a treatment strategy to prevent ARDS in patients without ARDS but at-risk for ARDS development. A metaanalysis showed better clinical outcomes with a decrease in ALI development (risk ratio [RR] 0.33; 95% CI, 0.23-0.47; number needed to treat [NNT], 11), and mortality (RR, 0.64; 95% CI, 0.460.89; NNT, 23) in patients receiving LTVV. A prospective assessment on the feasibility of a pragmatic trial of LTVV for patients with acute respiratory failure found that the mean initial TV was 7.1 ml/kg predicted body weight (95% CI, 7.1–7.2), with 78% of patients receiving TV £ 8 ml/kg. The sample size, with 90% power and estimated mortality benefit of 0-2% would require an enrollment of over 100,000 patients, which, in 2016, was deemed infeasible. Furthermore, in a RCT of ICU patients without ARDS
with anticipated extubation more than 24 hours from randomization, treatment with a LTVV strategy did not result in a greater number of ventilator-free days than an intermediate TV strategy.
Although the NHLBI PETAL Network’s task to develop randomized controlled ARDS prevention trials ended on December 31, 2013, research in ARDS prediction and prevention continues Robust artificial intelligence and machine learning-assisted clinical prediction models are needed to identify atrisk patients. As the NHLBI-funded ARDS, Pneumonia, and Sepsis (APS) Consortium seeks to understand the phenotype of critical illness syndromes, including adults with ARDS, developing different clinical prediction models targeting various ARDS phenotypes is essential for ARDS prevention.


Dr. Char is a clinical fellow in emergency medicine/critical care medicine at Brigham and Women’s Hospital, Boston, Mass.
Dr. IIg is an emergency medicine instructor at Harvard Medical School. She practices as an emergency physician and intensivist in the emergency department, cardiac surgical ICU, thoracic surgical ICU, and medical-surgical ICU at Brigham and Women’s Hospital, Boston, Mass.

Dr. Seethala is an assistant professor of emergency medicine at Harvard Medical School. He is an emergency physician and intensivist who attends in the emergency department, cardiac surgical ICU, thoracic surgical ICU, and medical-surgical ICU at Brigham and Women’s Hospital, Boston, Mass.

Dr. Hou is an assistant professor of emergency medicine at Harvard Medical School. He is an emergency physician and intensivist who attends in the emergency department, surgical ICU, thoracic surgical ICU, and medical-surgical ICU at Brigham and Women’s Hospital and in the ICU at Brigham and Women’s Faulkner Hospital, Boston, Mass.

With an estimated 13% of the 2023 US population being affected by disability (excluding those with mental health problems), or 26% including mental health (CDC), and the prevalent culture of ableism in our society, health care providers and institutions must foster an environment of inclusion by enhancing accessibility. Ableism, defined as the notion that able-bodiedness is humanity’s default state, manifests in practices or policies treating people with disabilities as invisible, inferior,
and less than human. It encompasses any statement or behavior directed at a disabled person that denigrates or assumes a lesser status for the person because of their disability. It includes social habits, practices, regulations, laws, and institutions that operate under the assumption that disabled people are inherently less capable overall, less valuable in society, and/or should have less personal autonomy than is ordinarily granted to people of the same age” [Forbes]. Ableism promotes a narrow
view of “normalcy” affecting interactions with the disability community, including use and provision of technology.
The use of accommodating technology can promote inclusion and offer benefits to everyone, exemplified by the widespread use and universal benefits of closed captioning. However, there is evidence indicating lower rates of technology access among people with disabilities, such as lower cellphone usage compared to those without disabilities (77% vs 88%, respectively).

“Ableism promotes a narrow view of 'normalcy' affecting interactions with the disability community, including use and provision of technology.”
Nonetheless, reasons for this usage differential are not clearly delineated, underscoring the need for researchers and advocates to identify technology access/use disparities and promote the use of valuable technology to foster equity in health care.
Accommodation Need: Lack or Loss of Vision, Color Blindness
Available Technology/ Equipment/Modifications
Text to Speech or Screen Readers
Several text-to-speech readers are available, with some capable of
converting text to Braille. These readers enable users to capture text from photos or directly read from web pages, usable on both phones and computers. It’s worth noting that these tools may also benefit patients with dyslexia. Examples include KNFB reader and Speechify, which offers a free online service with extended features available for a fee. BRLTTY is specifically designed for computers, driving a Braille display and providing screen review alongside some speech capability, all at no cost.
Desktop Magnifier Applications
These applications, downloadable from Apple App Store and Google Play, scan and magnify items or convert them into
audible speech. Examples: Magnifying Glass + Flashlight, Big Magnify, NowYouSee.
Color Identification Applications
These applications identify colors for people with color blindness. Examples: NowYouSee.
Braille Keyboards
These beneficial tools are designed to enhance communication for individuals with vision loss. They serve as an additional means of communication, complementing interpretative services that hospitals may provide.

continued from Page 25
Artificial Intelligence (AI) Smart Glasses
These glasses function similarly to text-to-speech readers but in wearable form. Some incorporate Generative Pretrained Transformer (GPT) technology resembling Apple’s “Siri.”
Accommodation Need:
Autism Spectrum
Available Technology/ Equipment/Modifications
Autism Information Platform
Encouraging individuals with autism or their advocates/caregivers to complete applications such as ICE4Autism
facilitates access to detailed information regarding communication challenges, unique behaviors, sensitivities, allergies, medical history, and emergency contacts. This practice can significantly improve the outcome of emergency response interactions by ensuring responders have vital information to provide appropriate support.
Communications Applications
Individuals with autism exhibit a broad range of communication abilities. Some may experience challenges such as rigid or repetitive speech, uneven language development (i.e., they may speak well on certain topics but struggle with others), or difficulty conveying messages through gestures [NIH]. To address these challenges, various applications have been developed to aid communication. These
“The use of accommodating benefits to everyone, benefits of closed
applications typically feature symbols for constructing sentences, emotion charts, and graphical representations of the body. Examples of such applications include Proloquo2Go, GoTalk, italkdoc (which is free), and Emergency Chat (an app designed to display a message alerting others when the user is experiencing a meltdown, allowing communication through typing).
Accommodation Need:
Hearing Loss, Deaf/Hard of Hearing (DHH), American Sign Language (ASL) Users, Oral Deaf, and Deaf-Blind Individuals
The DHH community encompasses individuals with a wide range of hearing abilities

accommodating technology can promote inclusion and offer everyone, exemplified by the widespread use and universal
captioning.”
and communication preferences. For ASL users, in-person interpreters, ideally Certified Deaf Interpreters (native Deaf individuals whose primary language is ASL), are paramount in care provision.
Available Technology/ Equipment/Modifications
Proper Lighting and Room Spacing
Proper room spacing ensures that individuals who are speaking or signing can be fully seen. Additionally, bright lighting and the use of softer colors in the room help reduce eye strain for individuals who rely on visual communication.
These applications generate large print on your smartphone and transcribe speech. The adjustable font size is particularly beneficial for individuals with easy reading ability. Moreover, healthcare providers can engage in a back-and-forth exchange, akin to using a pen and pad, with patients who can read and write. It’s crucial to carefully match the literacy level of the patient during such interactions.
Transparent masks, such as ClearMask and The Communicator, are facial coverings that offer “see-through” panels, allowing the lips and

Services such as Cyracom can be accessed on smart devices. Many hospitals provide portable tablets for this purpose, with larger screens being preferable for American Sign Language (ASL) users. However, if a tablet is not available, health care providers can use their smartphones with permission, using the hospital’s login information.
In recent years, telehealth programs for individuals with IDD have shown benefits including reduced ED utilization, cost savings, overcoming transportation barriers, improved access to specialists, and increased patient satisfaction. This area of telehealth for individuals with IDD is still emerging, with ongoing research and the development of additional home-based care programs. People with intellectual and developmental disabilities constitute a diverse group with varying levels of communication ability and independence, requiring different levels of support.
For patients who are non-verbal or experience communication differences, there are several AAC applications available. Examples include MyFirstAAC, Twinkl Symbols, Leeloo, Card Talk, Proloquo2Go, and TD Snap - Core First (which is more expensive). For a more comprehensive list, please refer to this resource.
Health passports are a valuable tool that patients with Intellectual and Developmental Disabilities (IDD) can utilize to articulate their needs while in a health care setting. Studies have demonstrated their benefits for both
patients and providers. For instance, the HSE Healthpassport ID app, available on iOS, offers five sections: About Me, Communication, Medical History, Looking After Me, and Keeping Me Safe and Happy. This app enables the streamlined sharing of information with health care providers, especially in acute care settings.
A plethora of accommodating technology and software is available to aid patients in navigating daily life and the health care system. However, prevalent barriers to access, including cost, lack of integration, and ableist policies, hinder implementation. Utilizing existing or new technology with patients can positively impact long-term health care delivery by fostering a more accommodating and inclusive hospital environment.
No author has any financial incentive from or relationship with any product mentioned. The cited products are merely examples of available options.

Dr. Backster is an assistant professor at Emory University and the longtime co-chair of their department’s Equity, Diversity, and Inclusion Committee. She is one of the founding members of the SAEM ADIEM Accommodations Subcommittee.

Dr. Whitten Sapp is a thirdyear resident in the Harvard Affiliated Emergency Medicine Residency who is passionate about improving health care for individuals with disabilities through medical education and research on health care disparities. @SappMD


Dr. Johnson MD is a PGY-3 in emergency medicine at the University of Rochester. He is also a Child of Deaf Adults (CODA) and fluent in American Sign Language (ASL).
Dr. Rotoli is associate residency director, Department of Emergency Medicine and director, Deaf Health Pathways, at the University of Rochester Medical Center.

Why Is Understanding Economics in the ED Important?
When individuals enter a grocery store, visit a website, or engage in any other form of consumer activity, they usually have a general understanding of the cost of products or services, enabling them to manage their expenses effectively. However, this principle doesn't extend to healthcare, especially when seeking care in the emergency department. Ironically, neither the patient nor the physician is adequately aware of the potential costs associated with the visit, including specific prices for labs or imaging tests. This lack of information impedes informed decisionmaking on both sides. Patients struggle to gauge the urgency of their medical condition and explore alternative options like urgent care or primary care clinics. Emergency medicine providers also lack
sufficient information to make informed decisions about whether certain orders could help reduce expenses for the patient. For instance, would opting for a point-of-care testing (POCT) instead of a lab test for a troponin make a difference in the overall cost? If individual hospital systems provided a standardized "menu" of average service costs in the emergency department based on billing data, would this help patients make more informed decisions, or could it potentially discourage them from seeking necessary care?
It's reasonable to ask about the average cost of an emergency department visit. Unfortunately, these costs vary significantly across states, ranging from the $600 to thousands of dollars. According to the Health Care Cost Institute in 2021, the
average cost nationally for all services without insurance was $2,909. This comprehensive figure encompasses triage fees, facility fees, professional fees, and supplies. Why is health care pricing so complicated? The complexity arises from the absence of a standardized cost and multiple factors contributing to the overall cost. Prices fluctuate based on set rates by Medicare, negotiated rates by insurance companies, individual deductibles, and copayments. Billing is also influenced by CPT (Current Procedural Terminology) codes, which originate from symptoms, treatments, and interventions. While these codes offer a means to compare prices across hospitals, they require an itemized bill, which is not automatically provided and takes additional time to obtain. Furthermore, the itemized bill is typically not sent until after the visit and offers limited assistance in determining the upfront cost. Disparities exist for
“Neither the patient nor the physician is adequately aware of the potential costs associated with the visit, including specific prices for labs or imaging tests.”
uninsured patients, who accrue additional costs charged at a premium due to lack of coverage.
As with other aspects of medical care, visits to the emergency department are not covered by a single payer. In recent years, the largest payer has been Medicaid, a federally-funded, state-administered insurance program designed for low-income and disabled individuals and families. Following closely are various private insurance companies, which individuals may obtain through their workplace or the Health Insurance Marketplace, established by the Affordable Care Act. The third largest category comprises visits covered by Medicare, federally funded and administered health insurance for individuals aged 65 and above. Lastly, the fourth largest group includes uninsured individuals who either pay what they can out of pocket or experience uncompensated visits. Additionally, several smaller groups have their care covered through a combination of these options or other programs.
For insured individuals, the amount they pay for a visit is determined by the specifics of their insurance plan and can be categorized into direct and indirect costs. The largest indirect cost for patients is their premiums, paid irrespective of their medical care utilization. Insurance plans may also implement cost-sharing measures, requiring insured individuals to contribute out-of-pocket for certain care costs. Examples of such measures include copayments, deductibles, or coinsurance.
Apart from the costs individuals are expected to cover as part of their insurance plan, there are cases where insured individuals are billed directly for services not covered by their insurance. This practice, commonly known as "balance billing," has received recent media attention and prompted federal legislation, namely the No Surprises Act, which aims to provide protections against it. This legislation holds particular
relevance to emergency medicine, as one common scenario where balance billing occurs is when individuals receive emergency care at an out-of-network facility or receive some out-of-network services at an in-network facility. The No Surprises Act eliminates patients' involvement in these disputes and compels physicians and insurance plans to directly settle disputes over charges owed. ACEP and other organizations are currently advocating for the fair implementation of this legislation, ensuring that emergency physicians and providers are treated equitably.
Although complex, the advocacy surrounding the No Surprises Act underscores the importance of physicians comprehending the economics and public policy dynamics related to their compensation. This understanding is important because it profoundly influences patient care and our professional livelihood. The high cost of accessing health care places a heavy financial burden on many Americans, leading patients to forego necessary care due to financial worries. This impact is felt daily in the emergency department, where individuals often present with complications of medical conditions that could have been addressed earlier. Understanding how patients cover the costs of medical care can facilitate the development of various solutions at the level of care provided or within the broader policy framework. Additionally, it's essential to recognize that the care patients pay for encompasses the services provided by emergency physicians. While patients should not face excessive charges or undue financial strain, it is critical for physicians to be fairly compensated for their expertise and service, rather than allowing insurance companies to disproportionately benefit and enrich themselves.
Given the importance of understanding the payment dynamics of emergency care, medical school and resident education should include instruction on health policy and economics. While
most medical schools incorporate some aspect of health economics into their curriculum, assessing its standardization across schools and the quality of content provided proves challenging. Therefore, it's imperative for medical schools to standardize the education offered on health economics and public policy to ensure every student gains a consistent understanding of how the medical system interacts with society. Moreover, emergency medicine residencies should integrate similar education into their didactic plans for residents. While the ACGME currently mandates “considerations of value, equity, cost awareness, delivery, and payment” to be incorporated into emergency medicine resident education, further refinement is necessary to ensure all residents receive uniform education and develop a shared understanding of how patients pay for care and how they, as providers, will be compensated.
Understanding how health care is financed in the United States is a challenging task given the numerous responsible organizations and overlapping systems involved. Nonetheless, it's essential to grasp these complexities so that emergency medicine residents and physicians can advocate for a health care system that effectively serves patients and supports those delivering emergency care.


Dr. Blum is a third-year emergency medicine resident at Boston Medical Center. He graduated from Icahn School of Medicine and Harvard Kennedy School. Prior to medical school, he worked on Capitol Hill.
Dr. Pecheny is a clinical assistant professor at the University of South Carolina School of Medicine. She graduated from the University of Rochester after completing residency as well as a fellowship in medical education while obtaining a master's in education.

In life-threatening conditions such as trauma and sepsis, minimizing delays to the initiation of treatment is paramount. Emergency medical services (EMS) agencies now equip personnel with antibiotics to start treatment in the field for suspected sepsis as well as prophylaxis in suspected open fractures.
A 2022 meta-analysis of more than 3,500 patients demonstrated a 28-day mortality reduction among patients receiving prehospital antibiotics. This effect could be magnified in EMS systems with prolonged transport times or transport to receiving hospitals with prolonged patient off-load times. The choice of antibiotic is crucial as the ideal drug should be affordable, broadspectrum, easy to administer, shelf-
“Prehospital antibiotics show a significant 28-day mortality reduction, especially in systems with prolonged transport times.”
stable, and have a favorable dosing schedule. Ceftriaxone has become the go-to antibiotic for many agencies based on these criteria.
Some potential concerns regarding prehospital antibiotic administration include antibiotic administration prior to blood cultures, sanctions for nonadherence to Centers for Medicare & Medicaid Services (CMS) standards,
poor antibiotic stewardship, and variability among prehospital sepsis screenings used. CMS provides a provision allowing for the collection of blood cultures following prehospital antibiotic administration. Blood cultures should still be collected upon emergency department arrival following prehospital antibiotics, as any positive growth could direct future antibiotic

choices. However, even in cases of cultures collected prior to antibiotic administration, most cases of sepsis are culture-negative. Additionally, choosing a sepsis screening tool can be challenging without access to labs. A validation study identified CIP, NEWS, and qSOFA tools, all relying on signs and symptoms, as having good predictive ability for sepsis diagnosis in the field. Some agencies use a combination of a sepsis screening tool and end-tidal carbon dioxide, a surrogate for lactate, to further improve sepsis recognition.
In the setting of trauma, prophylactic antibiotics are administered for open fractures and grossly contaminated or penetrating wounds. The U.S. military has been applying these practices in the prehospital setting as part of Tactical Combat Casualty Care. Broad-spectrum antibiotics are indicated for all open combat wounds and can be administered by combat medics or those with a higher level of training. Casualties who can tolerate oral intake receive 400 milligrams of moxifloxacin daily, while all others receive one gram of ertapenem daily by intravenous (IV), intramuscular (IM), or intraosseous (IO) routes. These antibiotics are well-suited for this application due to their environmental stability, ease of administration, infrequent dosing schedule, and broad spectrum of activity
against both gram-negative and grampositive pathogens frequently implicated in major combat wounds.
Outside of the austerity of combat, IV cefazolin is a common choice for prehospital prophylaxis of traumatic wounds. Per Advanced Trauma Life Support guidelines, cefazolin can be administered at one gram for patients weighing less than 50 kilograms, two grams for patients weighing 50-100 kilograms, and three grams for patients weighing more than 100 kilograms. Due to its narrower spectrum of coverage, additional antibiotics may be warranted at emergency department (ED) provider discretion in certain instances such as hollow viscous injury or wounds with significant contamination. Administration of antibiotics en route to the ED is once again even more important during prolonged transports and can offload the task burden of the ED team conducting the trauma resuscitation.
Ultimately, the administration of prehospital antibiotics for the treatment of sepsis or traumatic injury may facilitate improved patient outcomes provided protocols are in place to ensure appropriate patient selection and communication of interventions to the ED team. Larger studies are warranted to further elucidate the magnitude of benefit
and most appropriate protocols for the administration of prehospital antibiotics. The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Defense Health Agency, the Department of Defense, nor any agencies under the U.S. Government.



Dr. O'Conor is a third-year emergency medicine resident at Brooke Army Medical Center in San Antonio, Texas. He is interested in wilderness and operational medicine.
Dr. Meyer is a third-year emergency medicine resident at Emory University in Atlanta, Georgia. She is interested in EMS and event medicine.
Dr. Husain is an assistant professor of emergency medicine at Emory University School of Medicine. He also serves as the associate medical director for Sandy Springs Fire Department and MetroAtlanta Ambulance Service.

The current state of interpreter usage for patients with Limited English Proficiency (LEP) in emergency departments (EDs) is not well known, likely due in part, to inadequate documentation of patients’ language preferences and interpreter use in the electronic health record (EHR). High-quality data is key for ensuring equitable delivery of emergency care. With recent updates to coding and billing requirements for ED documentation, it’s an opportune time to develop new strategies addressing this need. These strategies can subsequently be applied in various contexts. This concepts
piece reinforces the importance of documenting language preference and interpreter use and proposes strategies for improvement. Improving the quality of EHR data related to language preference and interpreter usage will set the stage for future efforts to address health inequities for LEP patients.
According to the 2019 Census Bureau, over 67 million people in the United States speak a primary language other than English, with more than 25 million people classified as having LEP. Effective, patient-centered communication is fundamental to the delivery of emergency care, regardless
of language preference. Unfortunately, for LEP patients, language barriers make these interactions more difficult and hinder the effective transmission of medical information, increasing the risk for adverse outcomes in the health care system. The United States Civil Rights Act of 1964 mandates hospitals receiving funding from the Department of Health and Human Services (DHHS) to provide adequate language and interpreter assistance. Nonetheless, studies show that LEP patients experience care delays, lower clnical trial enrollment, and more care interruptions, as outlined by Karliner et al

“The current state of interpreter usage for patients with Limited English Proficiency in emergency departments is not well known, likely due in part, to inadequate documentation of patients’ language preferences and interpreter use in the electronic health record.”
Although improving clinician use of interpreters is crucial, it’s not sufficient on its own. Without clear documentation of interpreter use, emergency physicians (EPs) face higher medicolegal risk, hampering their ability to evaluate care delivery support future implementation and research. On the other hand, proper documentation of interpreter use can facilitate patient care decisions, reduce treatment errors, and inform future resource allocation for health systems.
EPs have expressed concerns about perceiving language interpreters as inefficient, which has likely contributed to their underuse. The challenge
of incorporating and documenting interpreter use in a busy ED is significant, especially amidst competing demands such as identifying and treating timecritical diagnoses, managing full waiting rooms, and addressing increasing wait times.
Despite the challenges in both usage and documentation, the updates to billing and coding guidelines for EDs in 2023 present a key opportunity for improvement. The shift in focus toward medical decision making (MDM)-based documentation can be leveraged to introduce other necessary updates
in documentation practices related
to interpreter use. Health systems and physicians are developing and incorporating new documentation templates, along with establishing new documentation routines and practice patterns. Therefore, it’s crucial to involve physicians in EHR changes during this time to maximize efficiency and raise the potential for adoption by other physicians.
The importance of this issue became apparent to us during a chart review study, where the use of medical interpreters was a key variable. During
“The importance of interpreter care delivery for patients by civil rights acts, government standards established organizations.”
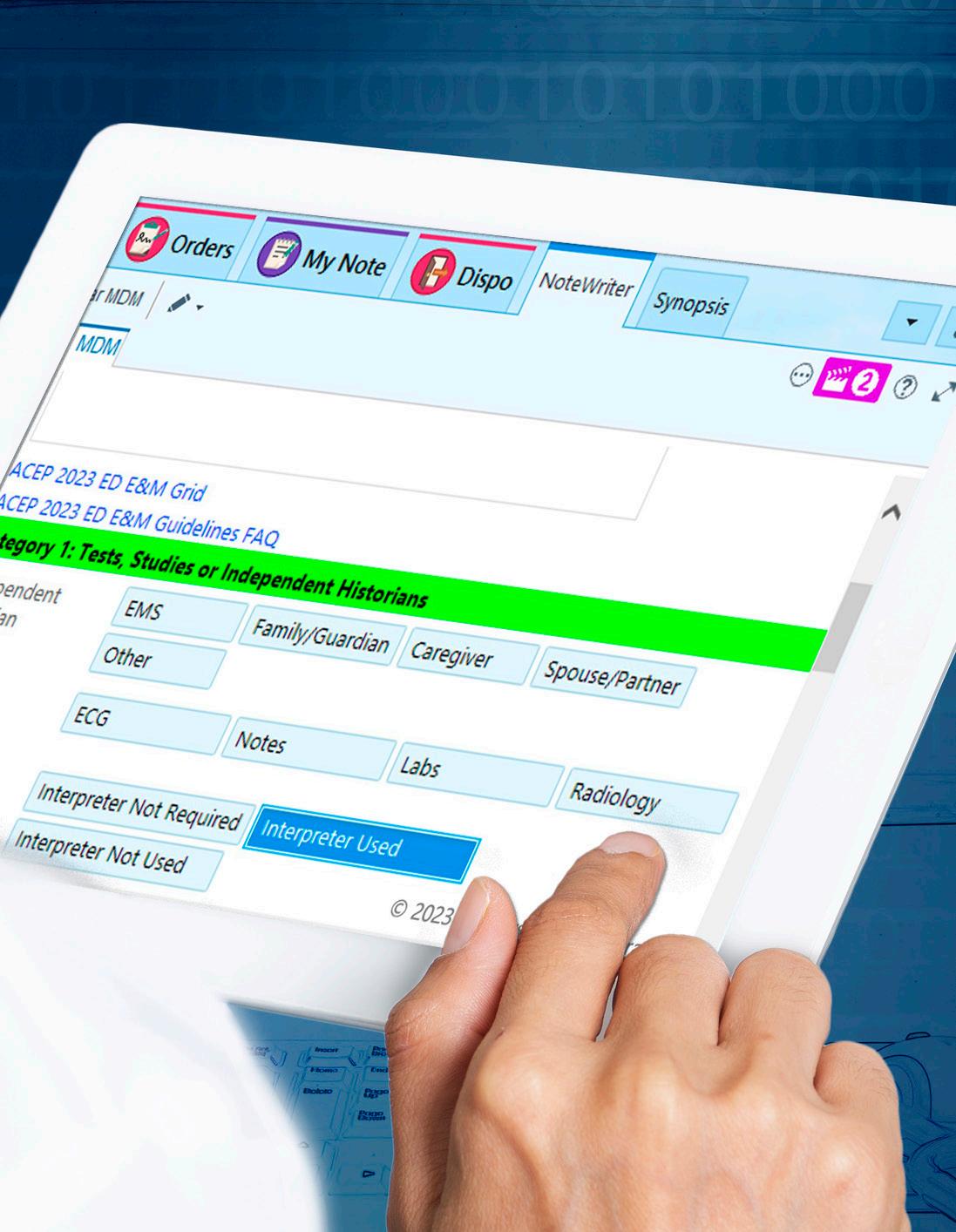
from Page 33
our review, it became evident that the necessary content to study our hypothesis was not readily available due to inadequate documentation of interpreter use. Among the 668 patients in this study who expressed language preferences other than English, only 27% had documented interpreter use during their encounter. Possible explanations include under-documented use of interpreters or suboptimal utilization. Regardless, the discovery of this deficiency in our ED notes catalyzed efforts to improve emergency medicine note templates in our health system’s EHR to ensure improved documentation moving forward.
In conjunction with updates to the MDM section of emergency medicine notes related to the 2023 changes in billing and coding requirements in the U.S., we updated our EHR documentation template to facilitate the capture of interpreter use. If a patient’s primary language is documented as any language other than English, the attending physician note template will include a button giving options for “Interpreter not used,” “Interpreter used”, and “Interpreter not required” (Figure 1). Selecting the “Interpreter not used” option prompts the text to auto-populate with the phrase “A medical interpreter was not required during this visit.” Conversely, choosing the “Interpreter used” option inserts “A medical interpreter was used during this visit” into the text. Moreover, an “Interpreter not required” option has been introduced for individuals who may have indicated a second language in their charts but prefer English. In such cases, the field auto-populates with “A medical interpreter was not used during this visit because ***”. This solution offers several advantages: it serves as a visual
interpreter use and equitable patients with LEP is underscored government policies, and by prominent medical
prompt in a crucial documentation area, it’s user-friendly, requiring only one or two clicks, and it coincides with other documentation requirement changes from the past year. Additionally, because this field is part of the MDM tab, which is a mandatory section of the physician note, we anticipate this change will improve documentation of interpreter use. Alongside improving documentation of interpreter use, our department has simultaneously worked to increase accessibility to interpreters.
iPads, directly connected to interpreter services, have been installed in every evaluation room. Additionally, faculty received an educational intervention regarding a phone application that grants easy access to interpreter services. These solutions aim to address perceived inefficiencies related to language interpreter use in the ED.
The ongoing changes in EHR updates and EP documentation practices provide a key opportunity to improve documentation of interpreter use as a critically important component in delivering equitable emergency care in our EDs. Ideally, physicians, health systems, and EHR vendors, will recognize the importance of these changes and adopt them voluntarily. Alternatively, certifying bodies and payers may also play a role in driving these improvements.
The Joint Commission, responsible for hospital accreditation in the United States, has health equity standards. Standard RC.02.01.01 mandates that “The [medical] record contains information that reflects the [patient’s] care, treatment, and services,” emphasizing the inclusion of language interpretation services in documentation. A future version of these standards might enhance hospitals’ accountability for advancing equity for patients with LEP by explicitly emphasizing the significance of both interpreter use and documentation.
Another potential solution is to link reimbursement from payers such as Medicare and Medicaid to the documentation of interpreter use. The Department of Health and Human Services (DHHS) and Medicaid policies have outlined various modes of reimbursement for language interpreter services. In the updated 2023 Inpatient Prospective Payment System (IPPS) Final Rule, the Centers for Medicaid and Medicare Services (CMS) introduced two new reporting measures, SDOH-1 and
SDOH-2, pertaining to Social Drivers of Health. Further refinement of these measures could explicitly target patients’ language and communication needs.
The importance of interpreter use and equitable care delivery for patients with LEP is underscored by civil rights acts, government policies, and standards established by prominent medical organizations. By implementing straightforward, practical changes in our EHR and care delivery system, we can move toward addressing this issue and improving equity in our delivery of emergency care.
This work was supported by the National Foundation of Emergency Medicine.


Alessandra Karam is a fourthyear medical student at Central Michigan University College of Medicine. She will be joining the University of Michigan for her emergency medicine residency this summer. @KaramAlessandra Dr. Samuels-Kalow is an associate professor of Emergency Medicine and Pediatrics at Harvard Medical School and an attending physician in both emergency medicine and pediatric emergency medicine at Massachusetts General Hospital. @m_e_s_k


Dr. Carreras Tartak is an instructor in emergency medicine at Harvard Medical School and an attending emergency medicine physician at Beth Israel Deaconess Medical Center.
Dr. Dutta is an emergency physician at Massachusetts General Hospital and served as the physician lead for Emergency Medicine and Clinical Decision Support at Partners eCare, which maintains the Epic Electronic Health Record for the enterprise.

Dr. Zachrison is an associate professor of Emergency Medicine at Harvard Medical School and Chief of the Division of Health Services Research for Mass General Brigham Emergency Medicine. @k_sauser

You receive the medical record of a 53-year-old woman sent from urgent care due to high blood sugar. She visited the urgent care center suspecting a possible urinary tract infection (UTI). Tests show she has a high level of glucose in her urine (greater than 1,000), indicating glucosuria, and her fingerstick blood sugar level measures above 500 milligrams per deciliter. She informs you that she has Type II diabetes and has been managing it well with an A1C level consistently below 7% for the past three years, using the medication semaglutide.
However, she has been unable to refill her prescription for the past month because several pharmacies in the area are out of stock due to increased demand from non-diabetic individuals seeking the medication for weight loss. She expresses frustration about the unavailability of her medication. A colleague suggests that there are alternative medications for diabetes, and that making semaglutide available for weight loss in non-diabetic individuals could prevent new cases of diabetes and other weight-related chronic medical conditions. Does the potential benefit to a larger population, particularly overweight individuals, justify the decision to prioritize access
to semaglutide for weight control over its availability to a smaller group, specifically diabetics who rely on it for management?
The Discussion
We acknowledge that in serving the greater public good — helping as many people as possible — it may be acceptable to make decisions that do not benefit, or in extreme cases, harm a smaller group. This was evident during the recent COVID-19 pandemic, where various decisions aimed at protecting the majority from infection (such as masking, economic closures, and vaccines) adversely affected smaller groups in different ways, from business
“The ethical premise underlying these decisions, and many in public health ethics, is utilitarianism, which posits that the ethically correct choice is that which maximizes good for the most people.”

closures to rare but severe side effects like cardiomyopathy from vaccines. The ethical premise underlying these decisions, and many in public health ethics, is utilitarianism, which posits that the ethically correct choice is that which maximizes good for the most people.
The utilitarian philosophy and deontology stand in almost direct opposition to each other. Deontology asserts that the morality of an action is inherent to the action itself, meaning that whether an action is morally and ethically correct is independent of factors such as who benefits more from it. In other words, if an action is deemed unethical, it remains so regardless of any potential benefits it might bring. Sometimes, these two philosophies align on certain issues, but other times they do not.
A classic example in medical ethics is the use of torture in interrogating terror suspects during the War on Terror. A deontologist would argue that regardless of whether the information obtained through torture might save many lives, torture itself is always wrong. On the other hand, a utilitarian might disagree, believing that if the suffering of one individual could potentially save the lives of many, then the action might be justified.
In our case, the patient suffers from poorly controlled diabetes due to the
unavailability of her medication that previously helped maintain her blood sugar levels. This situation arises because the medication manufacturer has shifted its distribution focus towards nondiabetic individuals seeking it for weight loss, leaving diabetic patients unable to access their prescriptions. Our patient is not alone in facing this issue; other diabetic patients also struggle to obtain semaglutide. While some pharmacies prioritize dispensing semaglutide to diabetics, not all follow this practice. Should diabetics, especially those reliant on semaglutide, receive priority for the medication?
There are valid arguments on both sides of the issue. Diabetes is widespread, with thousands of individuals relying on semaglutide to manage their condition effectively. The unavailability of this medication has had a deleterious effect on many of these patients, potentially leading to short and long-term consequences of poor glycemic control.
On the other hand, obesity is even more prevalent than diabetes, and its complications extend beyond just diabetes itself, including cardiovascular disease, sleep apnea, and more. Achieving sustained weight loss poses a significant challenge, with few proven non-surgical options available. Additionally, many bariatric surgeries carry both short-term and long-term risks.
Given these considerations, if a medication could help a much larger group address one of the most significant public health issues in our country today — obesity — but at the expense of harming a smaller group — diabetic patients reliant on semaglutide — the ethical dilemma arises: Is it still justifiable to prioritize the broader benefit over the well-being of a smaller group?
There are additional arguments to consider from both perspectives. For instance, there are various treatment options available for diabetes, such as medications, dietary changes, weight loss, and exercise. It's uncommon for
diabetic patients to rely solely on one medication for glucose control, as there are typically multiple strategies employed. Consequently, from a utilitarian standpoint, prioritizing access to semaglutide for obese patients, who have fewer effective options available, may seem ethically justified, even if it means some diabetic patients have limited access to the medication.
However, similar arguments can be made from the opposite standpoint. Effective treatments for weight loss do exist, including surgery, dietary adjustments, and exercise. If a medical treatment proves effective, it could potentially reduce the emphasis on adopting healthy diet and lifestyle changes for weight loss. This might result in overweight patients relying solely on the medication and neglecting other important lifestyle modifications. Additionally, some individuals may desire the medication despite having lesser needs for weight loss, which could lead to unnecessary usage.
Making health care decisions based on utilitarian principles often involves moral complexities, as compelling arguments can arise from both sides regarding what constitutes the most ethical choice. It's common for there to be no definitive "right" answer, and what may appear to be the best decision initially could eventually be deemed ethically incorrect. While drugs like semaglutide hold promise in benefiting numerous individuals, determining who should receive priority access to it is not a straightforward task.

Dr. Maloney is an associate professor of medicine, Case Western Reserve University, Cleveland, Ohio and medical director, emergency department, Louis Stokes Cleveland VA Medical Center.

In the dynamic landscape of health care, cultivating a passion for emergency medicine amongst the next generation of medical professionals is paramount. In the heart of Uganda, the Mbarara University of Science and Technology Emergency Medicine Interest Group (MUST-EMIG) stands as a beacon of inspiration and excellence. Founded in 2019 by five forward-thinking fourthyear medical students, MUST-EMIG has rapidly evolved into a pioneering force, igniting enthusiasm for emergency medicine and shaping the future of health care in east, central, and north Africa.
Mission and Vision: At the core of MUSTEMIG's mission lies a dedication to fostering interest, knowledge, and skill development in emergency medicine among undergraduate medical students. With a commitment to excellence and collaboration, MUSTEMIG aspires to become a model for university organizations, enriching the educational experience and advancing health care practices at Mbarara University and beyond.
Empowering Activities: MUST-EMIG's journey is marked by a variety of engaging activities designed to equip students with practical skills and academic insights in emergency
medicine. From hands-on training sessions and virtual lectures to inperson workshops and community outreach initiatives, MUST-EMIG offers a multifaceted approach to learning and engagement. Through strategic collaborations with the Department of Emergency Medicine, MUST-EMIG ensures access to invaluable resources and opportunities, nurturing a generation of competent and compassionate health care professionals.
International Collaboration: One of the key milestones in MUST-EMIG's journey has been its collaboration with international emergency medicine faculty. Through
“MUST-EMIG has been instrumental in my development as a future health care professional. Not only has it provided me with the practical skills and knowledge needed to handle emergencies, but it has also given me the platform to engage in leadership roles.”

collaboration with faculty from renowned institutions such as Washington University in St. Louis, Yale University, and the University of Southern California, MUSTEMIG has had the privilege of hosting virtual guest lectures and engaging with experts in the field. These collaborations have greatly enriched our understanding of emergency medicine both locally and internationally, broadening our perspectives and enhancing our learning experiences.
Research and Academic Achievements: MUST-EMIG has actively engaged in research activities, with members presenting abstracts at the African Conference on Emergency Medicine in Ghana in 2022 and the 2nd Emergency Care Conference Uganda. These opportunities have not only allowed us to showcase our academic contributions but have also inspired a culture of research excellence within our group.
Challenges and Triumphs: Despite facing challenges such as limited financial resources, MUST-EMIG remains committed to its mission. Securing funding would enable us to support research interests amongst our members and further enhance our impact in the field of emergency medicine. Nevertheless, through resilience and innovation, MUST-EMIG continues to thrive, driving positive change and progress in emergency medicine education.
Impact and Sustainability: The impact of MUST-EMIG extends far beyond the confines of academia, reaching local communities and inspiring future generations of health care professionals. Through initiatives such as community health fairs, mentorship programs, and research collaborations, MUST-EMIG serves as a catalyst for positive change, promoting awareness, preparedness, and excellence in emergency medical care.
With a vision for long-term sustainability, MUST-EMIG is poised to continue its transformative journey, leaving an indelible mark on the landscape of emergency medicine in Uganda and beyond.
Future Plans: Looking ahead, MUSTEMIG aims to expand its reach and impact by hosting mini conferences that bring together EMIGs from various universities. This initiative not only fosters collaboration but also provides a unique opportunity for undergraduate students to showcase their work and contributions to the field of emergency medicine. Through these endeavours, MUST-EMIG seeks to inspire future generations of health care professionals and contribute to the advancement of emergency medical care in Uganda and beyond.
As MUST-EMIG charts its course towards a future of endless possibilities, one thing remains abundantly clear: the journey of excellence in emergency medicine is a collective endeavour fueled by passion, perseverance, and collaboration. With a steadfast commitment to its mission and a vision for a brighter tomorrow, MUST-EMIG stands as a testament to the power of education, innovation, and community in shaping the future of health care. Together, let us continue to embrace the spirit of excellence, as we journey towards a world where every life is valued, and every emergency is met with skill, compassion, and unwavering dedication.

Reagan Kakande is a fourthyear medical student at Mbarara University of Science and Technology, Uganda and president of the Mbarara University of Science and Technology Emergency Medicine Interest Group (MUST-EMIG). @reagankakande4, @MUST_EMIG, emig.must@gmail.com

In the bustling streets of Kampala, Dr. Moses Kitakule found himself grappling with a pressing inquiry: "What are the odds of surviving a heart attack?" This question weighed heavily on his mind, spurred by the tragic loss of a cherished friend and esteemed professor due to insufficient medical attention during a myocardial infarction. Referencing the Uganda Country Report 2020, statistics unveiled a distressing reality — a 10% prevalence of premature cardiovascularrelated deaths among individuals aged 30 to 70.
As globalization and urbanization sweep across Uganda, the prevalence of cardiovascular risk factors such as
alcohol and tobacco consumption, obesity, hypertension, and diabetes mellitus has surged. Dr. Moses Kitakule, the visionary founder and medical director of Samaritan Health Systems, resolved to be a pivotal force in remedying this dire situation. His vision encompassed the establishment of home health care services, ensuring that individuals with chronic conditions received regular wellness checks, support for medication adherence, and education on lifestyle modifications — all within the sanctuary of their homes.
Moreover, Dr. Kitakule identified the imperative need for comprehensive life support training encompassing
basic, advanced, and pediatric cardiac care. Through collaborative efforts with Babcock Health Education Services and the American Heart Association, Samaritan Health Systems pioneered Uganda's first training site. Over the span of a year, 50 pilot training sessions were conducted across various disciplines to tailor the curriculum to the unique needs of the Ugandan context, spanning both prehospital and in-facility settings.
Amid Uganda's classification as a low-income country, the scarcity of resources within medical facilities poses a ubiquitous challenge for patients and health care professionals alike. The pilot trainings conducted by Samaritan
Health Systems underscored deficiencies in basic assessments and practical application among students, highlighting a stark imbalance between theoretical knowledge and its real-world application.
In response to these identified gaps, Dr. Kitakule and his team integrated patient medical assessment training into the Basic Life Support (BLS) Course. They introduced hybrid and manikin simulations across all courses and instituted a three-day electrocardiogram course as a prerequisite for the Advanced Cardiac Life Support (ACLS) and Pediatric Advanced Life Support (PALS) courses. Their observations underscored the paramount significance of early recognition and prompt referrals, particularly given the limited availability of cardiac catheterization labs — only four in the entire country, all concentrated within the capital city region.
Since its inception, Samaritan Health Systems has provided Heartsaver training to 11 civilians. To date, BLS students have totaled 76 participants, comprising 53% nurses/midwives, 33% prehospital personnel, and 10% medical officers/ physicians. Additionally, Samaritan Health Systems has trained 18 health care professionals in ACLS and PALS, with nurses constituting 67% and medical officers/physicians representing 33% of the participants.
Several participants have offered glowing feedback regarding the training sessions conducted by Samaritan Health Systems. One participant remarked, "The content was well laid out, providing us with a systematic approach for assessment and EKGs."
Another expressed appreciation for the simulation exercises, stating, "I enjoy the simulations, which offer a mix of real and mannequin patients."
All participants who have provided feedback have expressed confidence in the skills acquired through these

trainings, particularly in their ability to respond effectively to emergencies.
Samaritan Health Systems endeavors to sustain this positive momentum by continuing to offer these life support courses and virtual continuing medical education opportunities to health care professionals across the continuum of care. Specifically, the organization aims to enhance the skills of medical first responders, emergency medical technicians, and paramedics, as the nation endeavors to fortify and establish a dependable emergency response system. Additionally, Samaritan Health Systems plans to collaborate with the Uganda Heart Association to develop a mandatory cardiovascular certification curriculum for all health care practitioners, further fortifying the skills and knowledge of health care professionals in addressing cardiovascular emergencies.
“Participants lauded Samaritan Health Systems' training sessions, expressing confidence in their ability to respond effectively to emergencies with acquired skills.”

Bethel Mwenzeis the training site coordinator at Samaritan Health Systems, an American Heart Association training site in Uganda. With prior experience as a licensed paramedic in the U.S., she aims to enhance emergency response skills among pre-hospital and hospital personnel and standardize ambulance safety and equipment standards.

Dr. Kitakule is currently a consultant Pulmonologist in Louisiana. He is Director of Pulmonary and Critical Care at Iberia Medical Center. He is a consulting Pulmonologist and Intensivist at Our Lady of Lourdes Regional Medical Center and Ochsner Lafayette General Medical Center in Lafayette, Louisiana.
Dr. Kitakule is founder and medical director of Samaritan Health Systems an organization with a vision to improve health care delivery in Uganda.

Dr. Pelletier currently serves as the African Medical Coordinator for Techies Without Borders, a global non-profit organization dedicated to increasing access to continuing medical education to resource-constrained regions. Her interests include graduate medical education, the use of osteopathic manipulative therapy in the emergency department, and global emergency medicine expansion.

Publishing plays a crucial role in career progression and academic promotion within academic emergency medicine. However, it comes with challenges, including costly publication fees ranging from $1500 to $5000. These fees, known as Article Processing Charges (APC) for Open Access journals, may or may not be covered by the faculty's department, posing a significant hurdle, especially for education research studies that may not be funded by large grants.
So, what can be done with a groundbreaking manuscript that has the potential to reshape the emergency
medicine field but lacks the financial means to cover publication fees? Fortunately, there are several options available. This article organizes peer-reviewed journals into four main groups, with many of them not requiring fees for publication. These categories include:
1. Academic Emergency Medicine Education and Training (AEM E&T): A quarterly, peer-reviewed journal specifically dedicated to disseminating information relevant to education and
training within emergency medicine. It encompasses a range of article types, including original contributions, brief contributions, innovative approaches to bedside teaching, educational case conferences, and commentary/ perspectives.
2. Western Journal of Emergency Medicine (West JEM): This journal, which Integrating emergency care with population health, this journal focuses on education among other categories. It publishes original research, brief research reports, reviews, educational advances, and brief educational advances.

General Medical Education/ International Medical Education Journals
1. Academic Medicine: Journal of the Association of American Medical Colleges (AAMC): An international forum dedicated to addressing challenges in academic medicine, with articles ranging from innovations and scholarly perspectives
to research reports and literature reviews.
2. Medical Education: A leading international journal covering a wide array of article types, including original research, review articles, cross-cutting edge papers, and "Really Good Stuff,” which focuses on lessons learned through innovation in medical education.
3. Advances in Health Science Education: Focused on linking theory to practice, this journal includes research (quantitative/qualitative/mixed methods), reviews, evaluations, and reflections.
continued on Page 45
“When considering where to submit your manuscript, it's essential to first identify your target audience and align your research with journals that match your criteria.”
continued from Page 43
4. Medical Teacher: An International Journal of Education in the Health Sciences: Recognized as the leading international journal on research into medical education, this journal seeks to address the needs of teachers involved in health professions training. It publishes original research, short communications, “Twelve Tips,” and “New Wave,” which focuses on innovations in health professions education.
5. BMC Medical Education: This journal focuses on the training of health care professionals, including those at the undergraduate, postgraduate, and continuing education levels. It emphasizes curriculum development, performance evaluations, training needs assessments, and evidence-based medicine. Articles submitted may include original research, analyses of biomedical databases, or reviews.
1. Advances in Simulation: This journal provides a platform for scholarly endeavors aimed at advancing the use of simulation in health and social care. It encompasses research, reviews, innovations, and advancing simulation practice.
2. Simulation in Healthcare: This journal publishes research on all aspects of simulation technology applications, including empirical investigations,
technical reports, concepts, reviews, and case reports.
1. MedEdPORTAL: The Journal of Teaching and Learning Resources: This openaccess journal is designed for educators to submit innovative educational materials, featuring educational summary reports.
2. Medical Education Online: This openaccess journal publishes original research, reviews, and short/rapid communications in health care education.
When considering where to submit your manuscript, it's essential to first identify your target audience and align your research with journals that match your criteria. Utilizing free online bibliographic journal comparison or selection tools, such as the Journal/ Author Name Estimator (JANE) database, can help identify potential target journals to start this process.
Once you have potential journals in mind, review their table of contents and compare your work with similar articles already published in those journals to ensure that your manuscript complies with the formatting and article type requirements specified by the journal.
After aligning your manuscript with a suitable journal, proceed with drafting your cover letter and initiating your submission.
Remember, there is no one-size-fitsall approach to publishing educational research. Persistence, along with
“There is no one-size-fits-all approach to publishing educational research. Persistence, along with exploring various options, is key to success in this process.”
exploring various options, is key to success in this process. Don’t be discouraged; with time and effort, your work can find its place in the academic landscape.
It's important to remember that there is no one-size-fits-all approach to publishing educational research. Persistence and exploring various options are key to success in this process. Don't be discouraged; with time and effort, your work can find its place in the academic landscape. The opinions and assertions expressed herein are those of the authors and do not reflect the official policy or position of the Uniformed Services University of the Health Sciences, the United States Navy, or the Department of Defense.

Dr. Carmelli is an assistant professor of emergency medicine at the University of Massachusetts Chan Medical School. His interests are in resident education, curricular design, medical education research, and innovative digital design.

Dr. Rudinsky is an associate professor of emergency medicine and chair of the Department of Military and Emergency Medicine at Uniformed Services University, Bethesda, Maryland. She is board certified in emergency medicine and pediatric emergency medicine.

Dr. Cole is a research associate professor and director of research in the Department of Military and Emergency Medicine at the Uniformed Services University, Bethesda, Maryland. She currently chairs the SAEM Education Research Committee.

This month, we’ll discuss the T32 grant, which isn’t accessible to individual researchers; instead, it’s awarded to an institution and led by a principal investigator. But before diving into the specifics, let’s provide some context.
In 2011, the National Heart and Blood Institute (NHLBI) awarded a K12 training grant to several universities. Like the T32, this grant was awarded to institutions rather than to an individual investigator. The NHLBI supported the Icahn School of Medicine at Mount Sinai, Oregon Health & Science University, the University of California,
Davis School of Medicine, the University of Pennsylvania, the University of Pittsburgh, and Vanderbilt University Medical Center. The aim of the K12 at each site was to train researchers in emergency medicine to become independent R01 (or equivalent) researchers.
In 2016, the National Institute of Mental Health (NIMH) and the National Institute of Nursing Research (NINR) expanded the program to encompass emergency mental health research and nursing science. Among the recipients were Indiana University, the University of Oregon, Vanderbilt University, and the University of Michigan.
In a review of the program’s outcomes published in 2022 in Academic Emergency Medicine, the authors noted that the initial K12 in emergency care research yielded a newly funded cohort of successful interdisciplinary clinician-scientists in this field. Threequarters of them secured a funded career development award or research project grant principal investigator (PI) during the seven-year follow-up period. However, the NHLBI did not renew the K12 program. So where do institutions now turn to train the next cohort of emergency care researchers? Enter the T32 program. These institutional awards are geared toward

“The T32 grant isn't accessible to individual researchers; instead, it's awarded to an institution and led by a principal investigator.”
supporting predoctoral and postdoctoral research training, aiming to “meet the needs of the nation’s biomedical, behavioral, and clinical research agenda.” These training programs comprise a blend of didactic, research, and career development components. Additionally, they may support senior residents and early-career attending physicians across various disciplines.
For those interested in applying for T32 support, the first question is: “To which NIH institution should we apply?” There isn’t a universal T32 for emergency care. Instead, each institute supports T32 programs aligned with its own research portfolio.
You can find further details about the T32 program and which institutes might back an application from emergency care researchers here. To illustrate the scope of these programs, the National Institute of Arthritis and Musculoskeletal and Skin Disorders (NIAMS) supports over over 60 T32 training programs, yet none (so far) are from the emergency care research community. On the other
hand, the National Institute of Mental Health (NIMH) supports numerous T32 programs focusing on many different aspects of mental health care research, including comparative effectiveness for suicide prevention, childhood neuropsychiatry, and schizophrenia. Why not a T32 in mental health emergency care?
There have already been several successful applications from the emergency care community. For instance, the Icahn School of Medicine at Mount Sinai in New York has a T32 in Emergency Care Research ,as did the University of Pittsburgh. But there’s plenty of room for new applications. Last year, the National Institute for Neurological Disorders and Stroke (NINDS) received 34 applications for T32 support, with 16 of them being successful. Similarly, the National Institute of Allergy and Infectious Disease received nearly 60 applications, awarding grants to a third of them.
To explore further opportunities available for an emergency care T32
program, check out the webinar hosted by the Society for Academic Emergency Medicine. Emergency care research deserves more focused researchers, and this begins with their training. So, what are you waiting for?

Dr. Brown is the director of the Office of Emergency Care Research (OECR) where he leads efforts to coordinate emergency care research funding opportunities across NIH. Additionally, Jeremy is the primary contact for the NINDS Exploratory and Efficacy FOAs and serves as NIH's representative in government-wide efforts to improve emergency care throughout the country. He is also the medical officer for the SIREN emergency care research network which is supported by both NINDS and NHLBI. Jeremy.brown@nih.gov

In residency, individuals often find themselves torn between spending their limited daily free time either eating or sleeping. This dilemma can make it difficult to envision how to integrate meaningful scholarly activities into their schedules. Reflecting on our collective years of research experience during residency, we offer the advice we wish we had received from the beginning.
1. Go after the problem that gets you worked up. Research can be grueling, and without genuine passion for the topic you’re studying, you're unlikely to be invested enough to dedicate the necessary effort to it, especially before or after long shifts. Consider the clinical problems that genuinely intrigue you and pursue the questions that excite you, even in your limited free time.
There’s a better chance you’ll make progress if you genuinely care about finding answers that matter to you.
2. Measure twice, and cut once. Set yourself up for success by planning meticulously. Start by developing a clear research question, utilizing the FINER criteria (Feasible, Interesting, Novel, Ethical, Relevant) to refine and evolve iteratively. To inform your question development, conduct a thorough literature search. Once you have your question, finalize your approach, i.e. your methods and analysis plan. This proactive step will save you time down the road by preventing the need to revisit data due to unforeseen variables, such as additional factors that might require analyzing hundreds of charts again. While frustrating, investing
time in developing a comprehensive background review and thoughtful methods early on pays off in that those key sections of future scholarly publications are essentially completed in advance. Additionally, most institutional review boards require these components for their review before data collection. Consider publishing this work as a scoping review if it is not already present in the literature or incorporating it into a residency lecture.
3. Teamwork makes the dream work. Don't tackle research projects alone. Working with others not only ensures accountability but also helps round out your weaknesses by bringing different strengths to the table. For instance, if you're not a whiz with R programming, a fellow resident might excel in it. Use
“Teamwork not only ensures accountability but also helps round out your weaknesses by bringing different strengths to the table.”
your resources creatively and build a strong team. With the convenience of platforms like Zoom, your team members don't have to be at your institution. Take advantage of this opportunity to collaborate with individuals from other institutions who share similar interests or possess complementary expertise. Another plus: collaborating with multiple institutions means the work is multicenter! Additionally, consider including medical students on your team. Like residents, medical students vary in their research experience but are often eager to prove themselves to residency selection committees and may have more flexible schedules.
4. Be transparent about authorship. Moving a first-author paper across the finish line requires hard work that yields a high reward for your CV. However, it is a rare paper that gets published without a team behind it. Therefore, it's essential to have upfront discussions about authorship with all team members to avoid surprises down the line.
5. Strategically position your roadblocks. Research is full of rate-limiting steps. Whenever possible, minimize the involvement of residents during these critical stages. Ideally, schedule these tasks during lighter rotations. If research is a priority, schedule your electives for times when you're most productive. When working with a team, ensure everyone shares their schedules. The goal is to designate the team member with the most flexibility to handle responsibilities until passing the baton on to the next team member.
6. Deadlines are everything. Establish clear deadlines using various techniques such as shared calendars, regular meetings, setting mini-deadlines, and breaking down tasks into manageable parts. Creating a calendar involves working backward from the due date and allowing for unforeseen events. When collaborating with a team, factor in the time required for each member to weigh in on each step. Have a clear discussion
about expectations regarding turnaround times, whether it's responding to emails within 24 hours, 48 hours, or any other agreed-upon timeframe.
7. Money begets money. Grant committees appreciate seeing that you've received funding from other sources, no matter how small the grant. Numerous grants are specifically designated for residents. Applying for these grants allows you to develop your grantsmanship skills and can lead to future awards. Explore grant opportunities such as SAEMF/RAMS or EMF/EMRA grants. Additionally, your local state medical association and many hospitals offer resident-specific grant opportunities. Don't overlook local institutions, as they often provide grants for new investigators or funds for travel expenses for presentations.
8. You don’t need to do it all at once. It's okay for a resident research project to set the stage for your future career or to help you learn a new method or acquire new skills. You don't need to solve every problem you encounter. Regardless of whether you have four weeks, four months, or four years, you can embark on a research project; however, the type of project you undertake will vary depending on the amount of time available to you. If there's insufficient time for data collection, consider options such as conducting a review, meta-analysis, or writing an opinion piece. If your schedule allows only sporadic time, a chart review might be more feasible. If writing papers doesn't fit into your schedule, explore alternative scholarly pursuits like serving as a reviewer, participating in quality improvement projects, or developing a curriculum. Whatever you choose, seek guidance from an experienced researcher to obtain a realistic time estimate as you plan your approach.
9. Aim high. Strive for a journal that you think may be beyond your reach. The worst thing that can happen is they say no, but even then, you'll gain valuable feedback through the peer review process. Choosing backup journals with similar
formatting will save time if your top pick rejects your submission. Keep in mind that most journals rely on a few reviewers to make decisions, and you never know when you might have your submission accepted. Deciding early on your target journal for your initial submission allows you to align your writing style with that journal’s specific instructions for authors right from the start.
10. Don’t give up. Research, much like mastering ultrasound-guided IV placement, requires practice and repetition. Failure is a natural part of the learning process for everyone involved in research. At the end of the day, residency offers an opportunity to decide whether research will play a role in your career. While you may have preconceived notions about your research interest, trying it firsthand may lead to surprises. Consider taking this advice to heart and diving in!

Dr. Mayes currently serves as chief resident at the Harvard Affiliated Emergency Medicine Residency at Mass General Brigham. She will be on faculty at Virginia Tech Carilion School of Medicine starting this summer. Her research interests include the social determinants of health and traumatic brain injury. Dr. Cloessner is a PGY-3 and incoming chief resident at Washington University in Saint Louis. She is also a memberat-large on the SAEM RAMS board and liaison to the SAEM Research Committee.


Dr. Kane is the associate program director (research) at Lehigh Valley Health Network, where he also serves as president of the Medical Staff. He is a professor of medicine with the Morsani College of Medicine, University of South Florida.

Dr. Samuels-Kalow is an associate professor at Harvard Medical School, an attending physician in emergency medicine and pediatric emergency medicine at Massachusetts General Hospital, and the vice-chair for research in the Department of Emergency Medicine at Mass General Brigham.

In conjunction with the NIH Office of Emergency Care Research (OECR), SAEM's leadership has been working tirelessly to advocate for increased funding for emergency care research. The result of their efforts is the creation of the new K12 program by the Office of Training and Workforce Development (OTWD) at the National Institute of Neurological Disorders and Stroke (NINDS) called the Emergency Medicine Research Career Development Program in Neurological Sciences (EMRCDP-NS). EMRCDP-NS is an innovative initiative that aims to recruit, mentor, train, and support early-career emergency medicine faculty, enhancing their ability to conduct NIH-funded research on neurological disorders in pre-hospital
and emergency department settings.
In addition to funding scholars through the K12 portion of the program, the EMRCDP-NS will support a Pipeline Program for early career investigators who are not yet eligible or ready to apply for the K12 program. A primary goal of the Pipeline Program is to promote the diversity of emergency medicine research and the pool of successful emergency medicine physician-scientists by enhancing the participation of individuals from backgrounds and with perspectives that are underrepresented in medicine.
SAEM's proactive approach and strategic alliances in achieving this milestone marks a pivotal moment in
emergency medicine research, ensuring progress and innovation in the field.
K12 Program
Who should apply?
• Clinically practicing emergency medicine physicians within their first two years of a faculty position after residency or fellowship training.
Funding Availability
• The EMRCDP-NS funds 3 new scholars each year and provides up to 3 years of support for each scholar.
Award Requirements
• Dedication of 75% effort to research and career development during the first 3 years of the program.

• Commitment from the awardee’s department chair to provide 2 additional years of at least 50% protected time for research after the funding period.
• Submission of an individual NIH K application (or R01-equivalent) by halfway through the third year of the program.
• Attendance at the EMRCDP-NS Annual Retreat during the 3 years of K12 funding, plus the 2 years immediately following K12 funding.
Accepted Research Types
• Basic, clinical, translational, health services, etc.
• Research must align with the missions of National Institute of Neurological Disorders and Stroke (NINDS), National Institute on Drug Abuse (NIDA), or National Institute on Aging (NIA).
Award Deliverables
• Salary support of $115,000 (plus fringe benefits) per year for up to 3 years.
• $40,000 for research and career development costs per year for up to 3 years.
• Travel/lodging expenses to attend the required EMRCDP-NS Annual Retreat for up to 3 years.
Application Timeline
• First round applications due: October 1, 2024.
• Interviews conducted: December 4-7, 2024, at the EMRCDP-NS Annual Retreat.
• Awardees notified: January 2025.
• Anticipate start of scholar funding: July 2025
How to Apply
• The EMRCDP-NS application is similar to an NIH individual K award application.
• Interviews conducted by National Advisory Board members at the EMRCDP-NS Annual Retreat.
• Further details forthcoming.
Learn More
• Visit the EMRCDP-NS program website for additional details and to subscribe to program updates.
Pipeline Program
Ideal Candidate
• Emergency medicine senior residents, fellows, and first-year faculty interested in neurological sciences research who could be future K12 program applicants.
• Nominations encouraged for individuals from backgrounds and with perspectives that are underrepresented in medicine.
Program Capacity
• The program will support up to 10 pipeline investigators to attend the EMRCDP-NS Annual Retreat.
Program Deliverables
• Travel/lodging expenses covered for attending the EMRCDP-NS Annual Retreat on December 4-7, 2024.
• Grant writing training and support for 1-2 years preceding application for the EMRCDP-NS K12.
• Candidates must be nominated by a chair, division chief, or program director.
• Details and the official nomination form will be provided soon.
Nomination Timeline
• Nominations due: October 1, 2024.
• Program attendees notified: November 1, 2024
Learn More
• Visit the EMRCDP-NS program website for additional details and to subscribe to program updates.

Residency is a highly demanding period marked by numerous stressors that can detrimentally affect the mental and physical well-being of residents. Acknowledging personal achievements during this time can prove challenging and may be overlooked. Hence, the motivation behind the gRatitude initiative at our department of emergency medicine was to address this issue by fostering mindfulness and appreciation among emergency medicine residents. This initiative received funding support from the Rutgers New Jersey Medical School wellness grant.
The gRatitude project aimed to nurture a culture of appreciation and wellness among residents by encouraging them
“Residency is a highly demanding period marked by numerous stressors that can detrimentally affect the mental and physical well-being of residents.”
to celebrate each other. Residents were invited to submit shoutouts for their peers, which were then displayed on a gRatitude board in the conference room. These shoutouts encompassed a wide range of expressions, from recognizing acts of kindness by peers to acknowledging exceptional clinical performances by colleagues who had made a significant impact during shifts in the emergency department (ED). Each
month, one resident was chosen by their peers as the "gRatitude" recipient and received a gift card as a token of appreciation. Additionally, a monthly gRatitude breakfast gathering was organized during residency didactics, providing residents with an opportunity to decompress and strengthen bonds. Residents felt that this time allowed them to come together, expressing that it was like "coming home from being off-

service, and we cherish these moments with our co-residents so much."
The rationale behind the gRatitude project stemmed from the significant strain that emergency medicine has experienced in recent years. Physicians on the frontlines frequently feel undervalued and underappreciated. However, despite these challenges, emergency medicine physicians consistently exhibit acts of kindness, grace, and empathy toward both patients and colleagues. The gRatitude project aimed to recognize and celebrate these positive and impactful actions among residents. By doing so, the project sought to foster a culture of kindness within the residency program while also addressing compassion fatigue.
Moreover, the project aimed to provide residents with ongoing opportunities for self-reflection and to appreciate their colleagues' achievements. By regularly highlighting examples of excellence in teaching, camaraderie, and clinical care, the project aimed to reinforce the importance of these contributions to the residency community. Additionally, by drawing attention to the positive impact of residents' actions, the project sought to instill a sense of pride and fulfillment, reminding residents that even small gestures can have a significant impact on someone's life.
Throughout the year, a brief survey was conducted to gauge residents' perceptions of and gather feedback for the gRatitude project. Results revealed that a significant majority, 94.8% of residents, strongly agreed that the project had a positive impact on their well-being. Residents expressed appreciation for various aspects of the project, such as the opportunity to offer positive recognition to their colleagues, the satisfaction of hearing others being acknowledged, and the enjoyment of social interactions during the gRatitude breakfasts. Furthermore, many residents expressed excitement for the project's continuation in the future. One resident aptly articulated, "Resident wellness would benefit from the continuation of the gRatitude project."
In summary, the gRatitude project effectively served as a catalyst for nurturing a supportive and appreciative environment within the Rutgers NJMS Emergency Medicine residency program. By offering opportunities for recognition, fostering social connections, and improving overall well-being, the project contributed to increased resilience, camaraderie, and satisfaction among residents.




Dr. Lieu is a second-year resident at Rutgers New Jersey Medical School. Dr. Attaalla is the medical education fellow at Rutgers New Jersey Medical School. Dr. Eager is a third-year resident and future chief resident at Rutgers New Jersey Medical School.
Dr. Kei U. Wong is an assistant professor of emergency medicine in the division of pediatric emergency medicine (PEM) at Rutgers New Jersey Medical School (NJMS). she is the clinical director of PEM education for the residency program. she also serves as the director for PEM elective, and preclerkship course director for NJMS students.

Physicians across all specialties are well-acquainted with the potentially fatal consequences of alcohol withdrawal. Withdrawal is so prevalent that hospital systems have developed extensive protocols to mitigate these dangerous symptoms. When we think of alcohol use in acute health care settings, we often envision a tremulous and anxious patient with a long history of known alcohol use; however, the impact of alcohol on both our patients and our health care system extends far beyond acute withdrawal, with complications varying widely between sexes.
In every global region outlined by the World Health Organization, males exhibit a higher prevalence of harmful
alcohol use and dependence compared to females. Furthermore, males have a higher overall mortality rate from alcohol-related deaths, including those stemming from accidental injuries related to alcohol use. Nevertheless, females who drink in excess (>2 drinks per day or episodic binge drinking) have been shown to develop earlier onset and more severe medical complications associated with alcohol use. For instance, females are susceptible than males to die from cardiovascular disease related to alcohol use (41.6% vs. 13.4%). Additionally, females are more sensitive to certain neurologic complications of alcohol. One study demonstrated poorer performance
on cognitive skills testing for memory, spatial planning, and problem solving in females with harmful alcohol use. Moreover, some of the adverse effects commonly associated with alcohol use differ between the sexes. Females with alcohol use disorder (AUD) tend to develop more severe alcoholic liver injury and cirrhosis compared to males, even with lower intake volumes and fewer years of alcohol use. These sex differences observed in alcohol-related disease burden can be partly explained by the way alcohol is metabolized in the body. Alcohol dehydrogenase (ADH), the enzyme responsible for alcohol breakdown, exhibits lower activity in the livers of females, while greater

“Withdrawal is so prevalent that hospital systems have developed extensive protocols to mitigate these dangerous symptoms.”
ADH is found in the stomachs of males. Consequently, males possess a greater capacity to metabolize alcohol as it is consumed.
Given the more severe complications resulting from harmful alcohol among females, more aggressive screening and prevention measures are warranted in all health care settings, particularly in the emergency department (ED). It is wellestablished that women tend to utilize health care services more frequently than men. According to the National Center for Health Statistics, women consistently had higher primary care and emergency department visit rates between 2000 and 2018. Although the primary care setting is traditionally regarded as the primary venue for screening and intervention,
the ED has evolved into a de facto primary care clinic in many parts of the United States. A 2019 survey found that 33% of Americans had sought nonurgent medical care in the emergency department, with14% considering it their primary mode of receiving health care. Consequently, the ED is emerging as a crucial site for disease screening.
However, the screening tools we employ also serve as barriers to AUD prevention. Two of the most used screening tools for AUD are the AUDIT (Alcohol Use Disorders Identification Test) and the CAGE questionnaire. Nonetheless, these questionnaires, along with many other screening options, fail to consider sex or gender when determining AUD criteria. As we continue
to work toward more widely available and inclusive screening and prevention of harmful alcohol use in emergency and acute care settings, it is imperative to recognize the impact of sex on alcoholrelated disease burden and seize the opportunities available to address this disparity.

Madison Stanley is a third-year medical student at the University of South Carolina School of Medicine Greenville. Madison is applying to obstetrics and gynecology and has an interest in sex- and gender-based medicine research.

Simulation has become integral to medical training, reshaping skill development for health care professionals. It provides handson learning in a safe and controlled environment, reducing risks to real patients while enhancing training for infrequent, yet high-stakes, scenarios. However, the use of simulation training can pose financial challenges, especially in acquiring necessary equipment. For instance, a cricothyrotomy task trainer costs approximately $250 initially and includes materials for only three uses, posing challenges when multiple types of task trainers are needed.
3D printing offers a solution to the financial barriers associated with purchasing commercial task trainers. Despite moderate initial costs, 3D printing has the potential to change simulation programs, making medical training models more accessible and cost-efficient.
Dr. Bertalan Mesko, a physician and medical futurist, expands on this concept, illustrating how technology can reshape health care and health education. He provides examples of 3D printers creating models for surgical
planning and education, reducing reliance on cadavers, and even aiding in patient care. For example, one model produced finger splints using only two cents worth of plastic material.
Using 3D printing, educators can create detailed models replicating human anatomy based on CT scans, offering trainees a highly realistic experience. These models can simulate various procedures such as cricothyroidotomies, lumbar punctures, IV-guided injections, and thoracotomies.
Although the upfront investment in a printer ranges from $200 to $500, it
can be used repeatedly, and instructions for inexpensive models can be shared among multiple learners. Filament, the primary material used, is available on platforms like Amazon, priced between $15 to $30 per spool, and can be used for multiple models. For instance, one research study demonstrated that 3D printed cricothyrotomy models can be produced for as little as $5/ model, with an additional cost of $3-5 for the replaceable portion. The study additionally compared their model to other options, highlighting its advantages Given that some task trainers, like those for procedures such as a thoracotomy, can carry price tags ranging from $15,000 and $20,000, employing 3D printing technology can lead to significant cost savings.
Learning to operate a 3D printer is less daunting than one might think. Numerous online resources provide tutorials on material management (“Guide to 3D Printing Materials: Types, Applications, and Properties” and the “Ultimate 3D Printing Materials Guide”) and how to create models (“Thinker Cad”) Furthermore, there are freely accessible
“Using 3D printing, educators can create detailed models replicating human anatomy based on CT scans, offering trainees a highly realistic experience.”
instructions and models online for Chest Tube Simulator, IO Access Simulator and, Tracheostomy/Cricothyrotomy Trainer These predesigned models simply require downloading the file and uploading it to the printer, streamlining the process of creating cost-effective task trainer models at home.
In summary, integrating 3D printing into medical simulation programs offers a cost-effective and versatile solution, enhancing training opportunities while minimizing financial constraints. Producing task trainers using 3D printing can be easily achieved at a fraction of the cost of traditional options, making it a viable solution for programs with limited funding access.


Dr. Attaalla is a medical education fellow in the Department of Emergency Medicine at RutgersNew Jersey Medical School.
Dr. Dunn is an assistant professor and clerkship director in the Department of Emergency Medicine at Rutgers New Jersey Medical School.

Emergency medicine providers interact with upwards of 50 individuals during each shift, including patients, family members, consultants, nurses, paramedics, and laboratory and radiology technicians. Effective communication in clinical settings is integral to being an emergency medicine physician. Despite its importance, communication skills are not consistently emphasized in medical school or residency education. However, there is a growing recognition within the medical community that these skills are crucial for the success of emergency physicians. The American Board of Emergency Medicine (ABEM) recently introduced a new certifying examination specifically designed to assess these competencies,
covering areas such as high-stakes communications, difficult conversations, patient communications beyond diagnosis, and team management. Simulation provides an ideal platform to prepare emergency medicine residents for this new examination format and their future careers.
Incorporating communication-based simulation necessitates attention to available simulation time and resources, as well as fostering flexibility in didactic curricula. Frallicciardi et al. published an example curriculum in Academic Emergency Medicine Education & Training. Their emergency medicine interns participated in six simulation cases centered on “service failures,” covering scenarios like patients
leaving against medical advice, missed radiologic findings, and inadequate pain management. Following three cases, they underwent a debriefing session before participating in the remaining three cases. Evaluation of their communication skills before and after the debrief showed improved scores, as rated by faculty instructors.
Given the newfound recognition of the importance of clinical communication and interpersonal skills, it's anticipated that there will be an increased demand for communication-based simulation curricula for residents. Leveraging our collective simulation experience, we propose recommendations for developing curricular elements that integrate communication objectives.
Beginning the day with an introduction to the objectives, or prebrief, and integrating communication stations into established simulation-based educational days can enhance resident engagement. It's advisable to select critical yet less frequently encountered topics for simulated discussions, such as patient satisfaction, care challenges, pediatric-parent dyad interactions, or interdisciplinary team challenges. To make efficient use of available time, residents can focus solely on critical communication aspects, such as disclosing bad news or managing challenging staff interactions, by receiving clinical case information tailored to these elements. In situations where budget or time constraints prohibit the use of simulated patients (SP), faculty members can assume the dual role of patient and discussant in communication scenarios. Each case should present clinical information from the perspective of the faculty member or SP participant, along with prompts for resident responses.
Programs with SP resources may also consider occasional experiences with SP evaluators to acquaint residents with evaluative settings. These initial recommendations aim to assist programs in developing communication-based simulation scenarios, while simulation experts at various institutions may be open to sharing their content for broader utilization.
While residents regularly utilize critical communication skills during their shifts, they often lack formalized feedback on these interactions from their supervisors. To enhance patient safety and satisfaction among both staff and patients, it's crucial for residents to hone these skills in a controlled and evaluative environment. Simulation, being flexible and accessible as an educational modality, presents an ideal opportunity to focus on and develop these competencies.

Dr. Pauw is an emergency medicine physician at Vanderbilt University Medical Center where she is currently completing a one-year simulation fellowship. Her interests in emergency medicine include medical education, task trainer development, and in-situ simulation.
“Effective communication in clinical settings is integral to being an emergency medicine physician.”



Introduction
Generation Z learners have reshaped the educational landscape in undergraduate medical education and are now entering emergency medicine (EM) residency training. Defined by the Pew Research Center as individuals born from 1997 onwards, Generation Z learners grew up in an era of rapid technological advancements and widespread information accessibility, alongside the economic upheavals of the Great Recession of 2008 and the COVID-19 pandemic. These influences have uniquely shaped their expectations and preferences regarding their learning environment. To construct simulationbased education that effectively engages and motivates Generation
Z learners, educators may benefit from gaining deeper insights into their perspectives.
While generational categories are broad and should not be used for stereotyping, shared social and cultural influences can significantly influence a generation’s beliefs, attitudes, and behaviors, including those in educational settings. Generation Z exhibits distinct educational preferences compared to previous generations, such as Generation X and Millennials, some of which are outlined below.
Generation Z learners, being the first generation immersed in instantly
accessible digital information from birth, including platforms like Wikipedia, YouTube, and social media. As a result, they may perceive the “how, when, and where” of education differently from earlier generations. In addition to traditional classrooms, they embrace learning in virtual, remote, or asynchronous environments. Accustomed to instant answers via handheld devices, they value educational content tailored to their individual needs, especially when addressing specific questions in real-time.
Generation Z learners favor visual modalities, particularly video, and expect technological integration in
Individualized and Self Paced Learning
Engaging and Visual Learning Environments
Immediate and Actionable Feedback
Combined Personal and Academic Support
• Thrive equally learning in virtual, remote, or asynchronous environments.
• Appreciate educational content tailored to their individualized needs as they are accustomed to use of tech for near instantaneous answers.
• Affinity for visual modalities, particularly video.
• Expect technological engagement in learning format.
• Favor instructional strategies centered around application of previously learned content.
• Desire instantaneous and frequent feedback that is applicable to their immediate goals.
• Satisfaction with learning improves when they understand what is expected of them, and what they can do to meet competency standards.
• Expect their education to promote their overall development on both a personal and academic level.
• Educators must anticipate that these learners may require additional mental health support throughout their medical education.
Learner-Centered Debriefing
Rapid Cycle Deliberate Practice
Virtual Simulation
• A type of debrief that personalizes the simulation experience by prioritizing learner concerns (instead of instructor set objectives) and adapts the debrief to the learners’ context.
• A technique where learners progress through multiple cycles in which they perform a task, receive targeted micro-feedback, then rewind to perform the task again until competency is achieved.
• Provides customized, stepwise skill development and immediate, applicable feedback.
• Employs digital technologies to mimic high-stakes clinical scenarios in online or classroom environments.
• Provides unique opportunities for distance education
Table 1. Highlights of characteristic Generation Z learning profiles across educational modalities and settings
“Generation Z learners grew up amidst rapid technological advancements and economic upheavals, shaping their unique expectations for education.”
classrooms. Continuing a trend from Millennials, they prefer instructional strategies centered around applying previously learned content to solve reallife problems in relevant settings.
Immediate and Actionable Feedback
Feedback is integral to medical education. Generation Z learners desire prompt and frequent feedback applicable to their immediate goals. This emphasis on practical, actionable feedback may stem from a heightened awareness of the economic consequences of failure. Given their experience growing up amidst the uncertainties of the Great Recession and COVID-19 pandemic., Generation Z learners tend to be highly attuned to
the cost of their increasingly expensive education. Satisfaction with learning increases when Generation Z learners understand expectations and how to meet competency standards.
Combined Personal and Academic Support
Generation Z learners hope that their education will promote their overall development on both a personal and academic level. It’s noteworthy that Generation Z exhibits elevated rates of depression, anxiety, and mental health utilization compared to preceding generations. Educators should anticipate the need for additional mental health support during their medical education.
Simulation for Generation Z
Simulation holds promise as an educational modality for Generation Z learners due to its interactivity, individualization, and immediate applicability to real clinical scenarios. Effective debriefing provides actionable resolutions in a supportive and nonjudgmental environment; however, there are opportunities to improve and innovate simulation to better align with Generation Z preferences, as suggested below.


“Accustomed to instant answers via handheld devices, Generation Z values tailored educational content that addresses specific questions in real-time.”
continued from Page 61
Debriefing impactful learning experiences, enabling reflection and synthesis of new understandings. Learner-centered debriefing, in contrast to instructorcentered debriefing, is a distinct group of debriefing behaviors that move the focus away from the facilitator and towards the learner. In instructor-centered debriefing, priorities are often determined by the facilitator’s expertise, perceived significance of topics, and preset objectives. In contrast, learner-centered debriefing prioritizes the concerns of the learners, adapting the discussion to their specific context. This heightened personalization of the debriefing process may be particularly well-suited to Generation Z learners.
Since its inception in 2014, Rapid Cycle Deliberate Practice (RCDP) has garnered attention and sparked discussions among simulation educators. Unlike conventional simulation methods, where a scenario is completed followed by an extensive debriefing session, RCDP involves learners going through multiple cycles. During these cycles, they execute a task, receive targeted micro-feedback, and then repeat the task until competency is achieved. This iterative approach allows for customized, incremental skill development and immediate, relevant feedback, which Generation Z learners may find particularly appealing.
While virtual or remote simulation has been technologically feasible for a while, it catapulted into mainstream EM residency training during the COVID-19 pandemic. Unlike traditional methods reliant on costly manikins in specialized simulation centers, virtual simulation utilizes digital tools to replicate high-stakes clinical scenarios in online or classroom settings. Given their technological fluency,
members of Generation Z are well-suited to adapt to this electronic learning format, offering distinct opportunities for distance education.
Generation Z learners bring unique, characteristic learning preferences to EM residency, which will shape their educational approach. Understanding these preferences can assist medical educators in developing engaging and high-yield content for this learner group. This article highlights emerging Generation Z learning preferences and simulation educational strategies that may prove particularly impactful for these learners.
Effective teaching entails recognizing and adapting to the needs of learners. EM educators must be prepared to acknowledge, embrace, and realign their instructional strategies with Generation Z learning preferences to create education that authentically engages and motivates our future generation of residents



Dr. Chen is an associate professor of emergency medicine and the associate dean of simulation and clinical skills at Saint Louis University School of Medicine.
Dr. Bentley is a professor of emergency medicine and medical education, chief wellness officer, and the director of simulation innovation and research at New York City Health + Hospitals/Elmhurst.
Dr. Cohen is an assistant professor of emergency medicine, director of simulation, and simulation fellowship director at the University of Central Florida.

When a patient presents to the emergency department with concerns about toxic alcohol exposure, one laboratory parameter to consider is the osmolar gap. This test holds more nuance than many providers realize.
To start, what is the equation for the osmolar gap?
Formula 1: Osmolar Gap (OG) = Osmolality measured - Osmolarity calculated
Formula 2: Osmolarity calculated = 2(Na) + BUN/2.8 + glucose/18 + ethanol/4.6
(It is important to obtain the chemistry, Osmolality measured, and serum
ethanol concentration simultaneously when performing this calculation.)
Most providers are taught Forumula 2 for the calculating Osmolarity; however, even this equation is debatable. In a 2018 paper, Boru et. al. looked at six variations of this equation. Others debate using 4.6 as the denominator for ethanol, with some using 3.7, 4.0, or 4.2.
Many providers will use mobile apps to calculate the OG. A popular choice is MDCalc®. On this app, Formula 2 is applied for Na, BUN, and glucose, but the app offers a range for calculated osmolarity, using both 3.7 and 4.6 for the ethanol denominator. Ultimately the
OG value uses the denominator of 3.7. Note that a larger denominator (4.6) is more conservative, minimizing ethanol's contribution to calculated osmolarity (dividing by a larger number reduces ethanol's impact).
Formula 2 suffices for clinical use, and the accepted normal OG range is -14 to 10, based on a 1993 paper from Hoffman et. al. But how do we interpret these values? Does an elevated OG always suggest a toxic alcohol exposure, and does a normal OG rule it out? Likely not. We must explore this in three scenarios.
Firstly, toxic alcohols are metabolized by alcohol dehydrogenase into
“An elevated osmolar gap doesn't always imply toxic alcohol exposure, as various factors can influence its interpretation, requiring a thorough clinical assessment.”

intermediates, then by aldehyde dehydrogenase into main toxic metabolites (except for isopropyl alcohol, which stops at acetone after alcohol dehydrogenase, resulting in ketosis without acidosis). The parent toxic alcohol is osmotically active, and toxic metabolites cause high anion gap metabolic acidosis and end-organ damage. As the parent toxic alcohol metabolizes, OG decreases, and high anion gap metabolic acidosis develops (Figure 1). Thus, if a patient presents late after the initial exposure, OG may be minimally elevated or normal. However, if suspicion for a toxic alcohol exposure is high, treatment (alcohol dehydrogenase blockade with fomepizole, appropriate cofactors, hemodialysis, etc.), is still warranted, as even a normal OG may portend significant toxic alcohol concentration (more below).
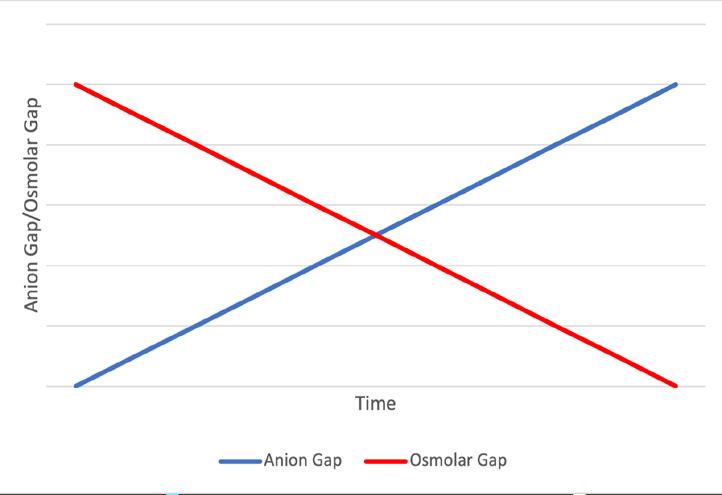
Secondly, a normal OG doesn’t rule out significant toxic alcohol concentration. Consider a case: a 5-year-old boy presents to the emergency department after reportedly drinking several sips of ethylene glycol from a bottle. (The parents are sure that he drank some, and the boy admits it as well.) However, when you obtain laboratory studies, the serum pH, bicarbonate, and anion gap are all normal, and the OG is 9. Could he have not ingested any? The OG falls within the -14 to 10 reference range. However, some calculation shows it could still align with a significant ethylene glycol concentration.
Suppose we knew the patient’s OG at this moment should ideally be -5 (a hypothetical scenario). Even with an OG from the previous day, variations occur throughout the day and between days. However, for the sake of this thought experiment, let’s pretend we know today’s OG should be -5. We can then determine the “delta gap” (a theoretical value, unattainable in clinical), which is 14 (Calculation 1).
Calculation 1:
Delta gap = osmolar gap – baseline gap
Delta gap = 9 – (-5)
Delta gap = 14
This hypothetical “delta gap” helps estimate the patient’s ethylene glycol concentration with a “normal” OG (calculation 2, using a denominator of 6.2 for ethylene glycol based on the molecular weight of the molecule.
Calculation 2:
Estimated Concentration:
Delta gap = [EG]/6.2
14 = [EG]/6.2
[EG] = 86.8 mg/dL
As evident, the potential ethylene glycol concentration in this patient, with normal laboratory results and and OG, could reach as high as 86.8 mg/dL! This is well above the usual treatment threshold of 25 mg/dL or greater.
Finally, does an elevated OG always suggest a toxic alcohol exposure? In the initial workup for elevated anion
gap acidosis, providers typically check lactate, a beta-hydroxybutyrate, etc. and may include OG in the evaluation. Patients with elevated lactate (perhaps from sepsis) or beta-hydroxybutyrate (perhaps from diabetic ketoacidosis or alcoholic ketoacidosis), may also exhibit an elevated OG. Conditions like sepsis, diabetic ketoacidosis, alcoholic ketoacidosis, and others can release osmotically active substances affecting OG. Therefore, an elevated OG alone does not necessarily indicate toxic alcohol exposure. However, a notably high OG likely indicates toxic alcohol ingestion and should be treated as such. The exact threshold for a “notably high” OG is unclear, but likely exceeds 40-50 mOsm/L.
In summary, history and overall clinical context are crucial in interpreting OG. Figure 2 summarizes it best.
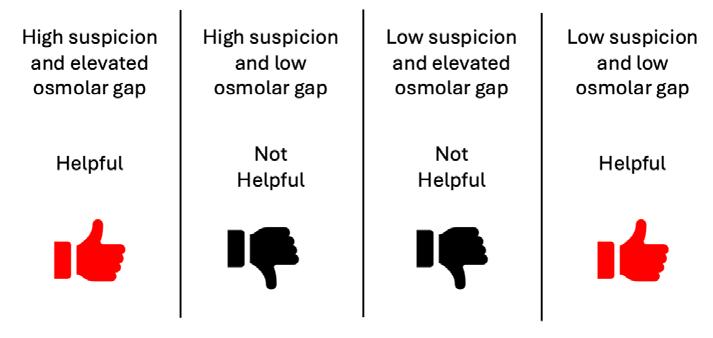
The OG is a useful yet nuanced tool. Understanding its limitations ensures accurate interpretation. For any questions or concerns, contact your local poison center for further assistance at 1-800222-1222. As toxicologists, we eager to assist in any case!

Dr. Keenan is an assistant professor of emergency medicine at Upstate Medical University and the assistant medical director of the Upstate New York Poison Center. He completed an emergency medicine residency at the University at Buffalo in 2020 and a fellowship in medical toxicology at Upstate in 2023.
Figure 1: Graphic representation of the change in the osmolar gap and anion gap over time Figure 2: Summary of interpretation of the osmolar gap
Pericardial tamponade, one cause of obstructive shock, represents a time-sensitive condition that can be challenging to diagnose rapidly. Historically, emergency physicians relied solely on clinical features of tamponade (classically: jugular venous distension, hypotension, and muffled heart tones); however, these findings have proven inconsistent and unreliable over time. Enter, point-of-care ultrasound (POCUS).
Point-of-care echocardiography is commonly utilized in the emergency department and can rapidly diagnose and guide management of various conditions. This modality can be particularly useful when evaluating distinct features of tamponade at
the bedside, potentially leading to immediate, lifesaving interventions.
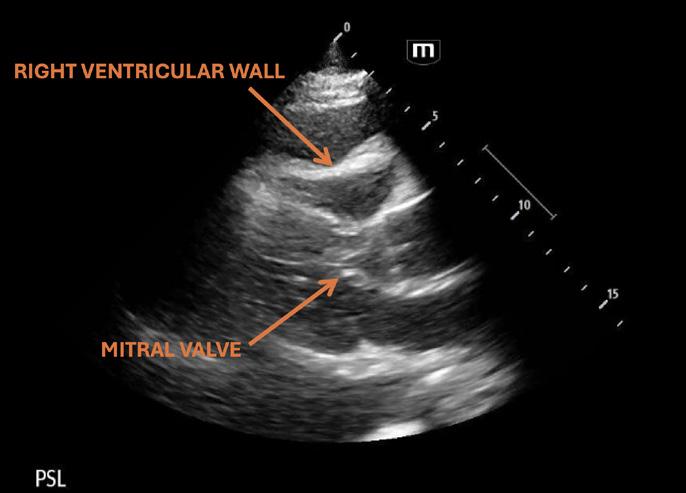
The sonographic definition of pericardial tamponade is right ventricular end-diastolic collapse (see Figure 1). This is the most specific, but least sensitive finding for tamponade. Right atrial collapse also occurs and given
that the right atrium has the lowest filling pressure, it is the earliest affected and the most sensitive finding. Right atrial collapse can be observed in multiple views, including the inferior vena cava (IVC) view (see Figure 2). Additionally, the adjacent IVC can appear plethoric due to the obstructive nature of tamponade.
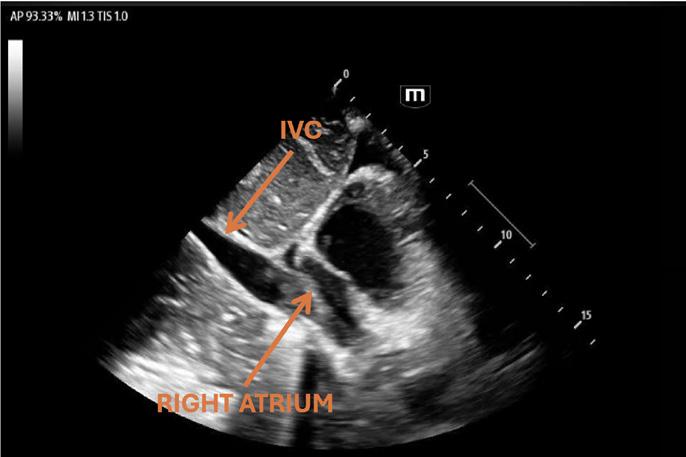 Figure 1 - Click to expand image
Figure 1 - Click to expand image
“Mitral and tricuspid valve inflow velocity variation is another useful tool when assessing for pericardial tamponade.”
Diagnosing tamponade with POCUS can be more difficult than it seems. Multiple factors can contribute to difficult image acquisition and interpretation. Thankfully, a few advanced yet easy-tolearn ultrasound tips can prove useful at the bedside.
Views often reveal a hyperdynamic heart, sometimes swinging in fluid, with chamber walls that are difficult to evaluate in real-time. I’ve often found myself staring too long at the right ventricular wall to determine if it is collapsing during the right phase of the cardiac cycle. To address this, first obtain the parasternal long view of the heart and use M-mode ultrasonography to capture a snapshot of the right ventricular (RV) free wall and mitral valve over time to determine if collapse occurs in diastole. Note of the depth of each visualized structure (right ventricular free wall, septum, and mitral valve) and correlate it with the M-mode tracing. Mitral valve opening (the peak of the wave approaching the septum) occurs in diastole, and if the motion of the RV free wall appears to collapse (appearing as a “trough”) during this event, tamponade is likely (see Figure 3).
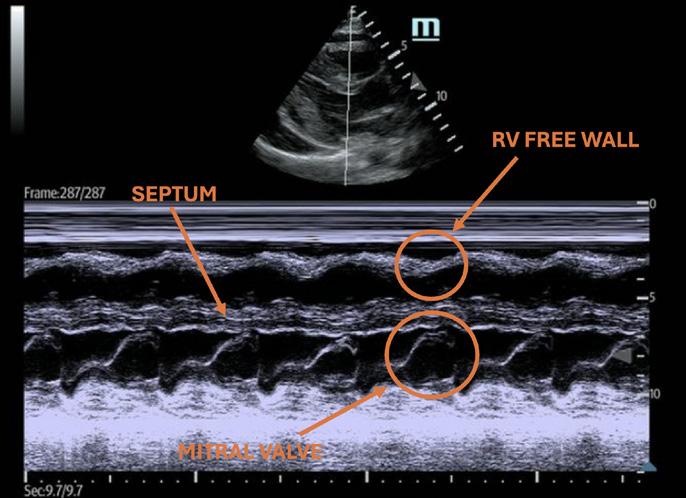
Mitral and tricuspid valve inflow velocity variation is another useful tool when assessing for pericardial tamponade. This is essentially the sonographic equivalent of pulsus paradoxus (fall of systolic blood pressure during the inspiratory phase).
Obtain the apical 4 chamber view and place the pulse wave (PW) Doppler gate just above the tip of the mitral or tricuspid valve leaflets (on the ventricular side).
This will create a wave flow pattern that corresponds to the velocity of blood flow over time. As the direction of blood approaches the probe, the corresponding waves will appear positive on the baseline. These waves represent an "E" wave (early wave) and a smaller "A" wave (atrial wave) corresponding to early diastolic filling and the atrial “kick,” respectively (see Figure 4).
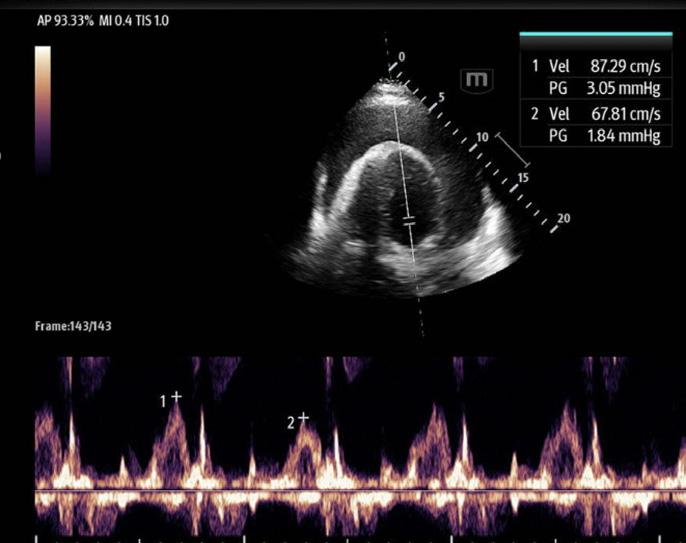
Measure both the largest and the smallest "E" waves. These waves correspond to inspiratory variation during spontaneous respiration.
A variation of more than 25% in the mitral inflow velocity or more than 40% in the tricuspid inflow velocity supports a diagnosis of tamponade physiology (Otto, Textbook of Clinical Echocardiography, 2013).
Several common misconceptions exist surrounding pericardial effusion and tamponade, outlined well in Dr. Edgar Argulian and Dr. Franz Messerli’s article titled “Misconceptions and Facts about Pericardial Effusion and Tamponade” in the American Journal of Medicine, 2013.
A few notable highlights include:
All patients with pericardial tamponade are hypotensive.
• Hypotension is rather uncommon in subacute (medical tamponade); contrarily, hypertensive tamponade can be seen in 27-43% of patients.
Pericardial tamponade is a clinical diagnosis.
• Tachycardia, jugular venous distention, pulsus paradoxus, and diminished heart sounds (Beck’s triad) lack both sensitivity and specificity.
• In one systematic review, jugular venous distention had a pooled sensitivity of 76% (Roy CL, et al. JAMA 2007)
• The incidence of pulsus paradoxus has a wide range, from 12% to 75%, reducing the reliability of this finding.
All patients with pericardial tamponade should be stabilized initially with IV fluids.
• Cardiac index can be increased with 500 cc bolus (>10%) in those with a systolic blood pressure of less than 100.
• Decreased cardiac output and pulmonary edema can occur with pressure increases from excessive IV fluids.
In summary, incorporating point-of-care ultrasound at the bedside, along with the application of these tips, can instill much needed confidence when determining whether a pericardial effusion represents tamponade physiology.

Dr. Filler is an assistant clinical professor in the department of Emergency Medicine at Creighton University and the University of Arizona, Phoenix. He is the Emergency Ultrasound fellowship director at Valleywise Health in Phoenix, Arizona.
Figure 3 - Click to expand image Figure 4 - Click to expand image
Point-of-Care Ultrasound (POCUS) has revolutionized emergency medicine (EM). At the bedside, we can now instantaneously diagnose the etiologies of shock, perform diagnostic imaging, and guide our procedures in real-time, all enhancing patient care. While the benefits of POCUS are numerous, many providers remain hesitant to adopt it due to concerns about increased litigation risks. With over 75% of EM physicians facing medical malpractice cases in their lifetime, the question arises: does performing POCUS increase one’s risk of being sued?
What is the medicolegal risk of POCUS?
Medicolegal risk is the potential legal liabilities and consequences associated with providing medical care and services. It encompasses situations where medical decisions or actions
result in harm to patients and lead to litigation. Regarding POCUS, these risks include inadequate image acquisition, misinterpretation of findings, failure to perform indicated scans, and scope of practice issues.
Much of what we know about the risk of using POCUS comes from retrospective analyses of medical malpractice cases. Through legal databases, several studies have analyzed the available public cases involving emergency medicine physicians and POCUS. An initial study performed by Blaivas et al., searched Westlaw, a legal database, for cases in the United States involving emergency medicine physicians and ultrasound between 1987-2007. While 659 medical malpractice cases met their initial search criteria, there were zero cases involving EM physicians incorrectly performing or interpreting an ultrasound.
A subsequent study performed between 2008-2012 by Stolz et al. utilized the same database and identified 120 potential medical malpractice cases between 2008-2012, with five cases where the physician was accused of misconduct in the emergency department (ED), and the interpretation or failure to perform an ultrasound that was within the ACEP (American College of Emergency Physicians) core applications was discussed. Of these five cases, three involved the ED physician not performing an ultrasound study, while the other two involved radiologyperformed ultrasounds. There were no cases involving misinterpretation or missed diagnosis by an emergency physician performing POCUS. A more recent analysis by Russ et al. between 2012 and 2021 similarly revealed no lawsuits involving misinterpretation or
“The greatest medicolegal risk for POCUS appears to be the failure to perform POCUS scans that are clinically indicated and within the ACEP ultrasound compendium.”
performance of POCUS scans; rather, most lawsuits stemmed from a failure to perform indicated scans.
It is important to note that these studies have limitations; they only include cases brought before the court and exclude settled cases, dismissed cases, or cases that are not publicly accessible. There may indeed be cases where emergency physicians faced litigation related to their performance or interpretation of POCUS scans.
What does this mean?
The greatest medicolegal risk for POCUS appears to be the failure to perform POCUS scans that are clinically indicated and within the ACEP ultrasound compendium. While there are medical malpractice cases involving emergency medicine physicians and a misdiagnosis, these cases were caused by findings missed by a specialist (i.e., radiology, cardiology, OB-GYN) and not misdiagnosed by an EM-performed POCUS. Therefore, emergency physicians should feel comfortable performing any scans that are clinically indicated and within their scope of practice.
Which studies should I be comfortable performing as an EM Physician?
ACEP has developed an Emergency Ultrasound Imaging Criteria
Compendium, which reveals both primary and extended uses of ultrasound that emergency physicians should be able to perform. Some of these primary indications include:
Aorta: Evaluating the abdominal aorta for aneurysm
Cardiac: Evaluating for pericardial effusion/ tamponade, gross cardiac activity during CPR, global left ventricular systolic dysfunction, and evidence of right heart strain
Female Pelvis: Evaluating for intrauterine pregnancy (IUP) and gestational age, fetal cardiac activity, and free fluid exceeding physiological fluid
Gastrointestinal: Evaluating for small bowel obstruction (SBO) and acute appendicitis
Kidney: Evaluating for sonographic evidence of obstructive uropathy and urinary retention
Lungs: Evaluating for acute pneumothorax, abnormal pleural fluid collections, and interstitial lung fluid
Ocular: Evaluating for retinal detachment, vitreous detachment/hemorrhage, and indirect evaluation of intracranial hypertension via optic nerve sheath diameter (ONSD) and optic disk visualization
Right Upper Quadrant: Evaluating for symptomatic cholelithiasis and cholecystitis
Soft Tissue: Evaluating for cellulitis, abscess, bursitis, foreign bodies, and joint effusions
TEE (Transesophageal Echocardiography): Assessing myocardial activity during standstill, cardiac arrest etiologies, guiding mechanical compression, and ECMO procedures.
Trauma: Evaluating for free fluid in the peritoneal, pericardial, and pleural cavities
Venous Thromboembolism: Evaluating for acute proximal deep vein thrombosis (DVT)
Now that I am performing POCUS scans, what can I do to mitigate my risk?
As with all medical cases, our defense lies within our records and documentation. It is important to present a logical thought process explaining a patient's workup, including rationale behind obtaining imaging. If it is ultimately decided not to perform a scan, it is important to document why it is not being pursued. Furthermore, if a scan that is in the repertoire of an emergency physician is deferred to radiology to perform, it is important to document that the patient is stable enough to wait for said exam.
Once you decide to pursue bedside POCUS scans, it is important to ensure that all scans are performed, saved, and documented correctly. It is recommended that all exams must have adequate views, including in 2 dimensions for every structure of interest, and proper
labeling (including both the area being scanned and the probe orientation). All exams performed must be saved and stored. Finally, all exams must have documentation accessible in the patient's chart of the findings seen. There must also be a quality assurance process, ensuring that there is a process for reviewing cases by ultrasound trained physicians and informing patients of any potential misses.
As POCUS technology expands and becomes more deeply integrated into everyday practice, questions regarding physician accountability surface. Will EM physicians be held accountable for incorrectly performed scans or interpretations? Will EM physicians be held accountable for not performing any scan under the compendium? Can EM physicians be held accountable for scans performed or interpreted incorrectly by radiology that are within EM physicians’ scope of practice? While these questions remain, prioritizing patient care by incorporating POCUS into clinical practice continues to be paramount.

Dr. Gomberg is a clinical instructor in the Ronald O. Perelman Department of Emergency Medicine at NYU Grossman School of Medicine and an Emergency Ultrasound Fellow at NYU Langone Health/ Bellevue. Her interests include ultrasound and medical education.
For information on which scans you should be familiar with:
Emergency Ultrasound Imaging Criteria Compendium
For information on Scope of Practice and Quality Assurance: Ultrasound Guidelines: Emergency, Point-of-care, and Clinical Ultrasound Guidelines in Medicine

Shoulder dislocations are a common pathology familiar to emergency department (ED) physicians, with about 70,000 ED visits seen annually throughout the United States [1]. Traditionally shoulder dislocations are identified using x-rays but there has been increasing use and efficacy of point-of-care ultrasound (POCUS) in the diagnosis and management of shoulder dislocations. [2, 3] The most common POCUS approach to identify a shoulder dislocation is posterior, utilizing a curvilinear or linear probe transversely just inferior to the spine of the scapula at the glenoid fossa. However, in patients
who require spinal precautions or who have difficulty in sitting up due to pain, it is challenging to obtain sonographic windows for this approach. Although there have been previous reports of an anterior and lateral approach to identifying shoulder dislocations, we discuss a novel axillary approach with an endocavitary probe which can enable assessment of normal and dislocated shoulder anatomy, without the need for additional imaging.
The shoulder joint is formed by the articulation of the humeral head with the glenoid cavity of the scapula. The
endocavitary probe has the advantage of a relatively small footprint combined with a long transducer handle, making it ideal to visualize this articulation from an axillary view. The probe is positioned in the axilla and sonoanatomy can be visualized in both a coronal axis, with the probe marker facing towards the patient’s right, and a sagittal axis, with the probe marker facing anteriorly. Normal articulation of the humeral head in the glenoid fossa can be visualized with the endocavitary probe in sagittal orientation with lateral to medial tilting of the probe coronally. This articulation is lost in a shoulder dislocation and


Figure 2: Here is a sonographic endocavitary axillary view in the coronal plane visualizing the right shoulder. Here we see the humeral head (A) articulating with the glenoid process (B) without a noticeable gap in articulation. Click to expand image
a clear gap is seen sonographically. In addition, shoulder dislocations yielded discrepant anterior-posterior distances when comparing the position of the humeral head and glenoid sagittally. Once the shoulder is reduced, the same approach demonstrates clear articulation between the humeral head and glenoid with positioning in the sagittal plane.

Figure 3: Here is another sonographic endocavitary axillary view in the coronal plane visualizing the left shoulder. The humeral head (A) is displaced with a clear gap noted between the humerus and glenoid fossa (B). Click to expand image
Detection of shoulder dislocations using endocavitary ultrasound may have clinical utility in patients with limited access to a posterior approach, however additional research is needed to assess this modality in patients with shoulder dislocations and to potentially guide real-time visualization of a successful reduction.





Lisa Chan is the current ultrasound fellow, Emergency Ultrasound Division, Department of Emergency Medicine, Hartford Hospital, Hartford, CT. She completed her emergency medicine residency at St. John’s Riverside in Yonkers, NY.
Felix Pacheco is an ultrasound faculty member, Emergency Ultrasound Division, Department of Emergency Medicine, Hartford Hospital, Hartford, CT.
Adam Wise is an ultrasound faculty member, Emergency Ultrasound Division, Department of Emergency Medicine, Hartford Hospital, Hartford, CT.
Seth Lotterman is an ultrasound faculty member, Emergency Ultrasound Division, Department of Emergency Medicine, Hartford Hospital, Hartford, CT. He is also the assistant program director for the University of Connecticut Emergency Medicine Residency. Trent She is the ultrasound director and ultrasound fellowship director, Emergency Ultrasound Division, Department of Emergency Medicine, Hartford Hospital, Hartford, CT.
1. Ultrasound for the diagnosis of shoulder dislocation and reduction: A systematic review and meta-analysis
2. Epidemiology of shoulder dislocations presenting to United States emergency departments: An updated tenyear study
3. Musculoskeletal Ultrasonography to Diagnose Dislocated Shoulders: A Prospective Cohort
4. Bedside ultrasonography for verification of shoulder reduction: A long way to go
Figure 1: An example of endocavitary probe placement into the axilla of a patient. In this case, the probe marker is oriented to the patient’s right which will allow for the coronal plane.
In January 2023, Dr. Ahmad spent nearly three weeks as a member of MedGlobal’s WHO Emergency Medical Team delegation, deployed to Gaza and working in the now defunct and catastrophically damaged Nasser Hospital, which was the second largest hospital in Gaza. Here is an account of his experiences…
In the resuscitation bay of Al Nasser Hospital's emergency department in Gaza, a 14-year-old boy lies on the floor, brought in by his family after sustaining shrapnel injuries from a missile strike near their tent. He has multiple wounds to his chest, abdomen, and lower extremities, is having trouble breathing, and exhibits diminished breath sounds on the left side with no lung sliding detected by a
butterfly probe. The resuscitation bay, much like every day during the three weeks I was there in January, is full of patients, many of whom are relegated to the floor like this patient. With a sporadically functioning portable pulse oximeter that intermittently works and only four monitors in the resuscitation bay, all in use, we lack portable X-ray capability and oxygen saturation readings. Consequently, as the patient's respiratory effort becomes increasingly labored, we decide to place a chest tube.
The skilled and knowledgeable Palestinian physicians in Gaza are all too familiar with trauma cases and mass casualty incidents, yet they face the daunting challenges of multiple events, scarce supplies, and overworked and under-resourced staff. Since the October 7 attacks, which claimed nearly
1,200 Israeli lives and left 5,400 injured, an intense military campaign involving airstrikes, tank shelling, drone strikes, and ground offensives has resulted in over 32,000 Palestinian fatalities and 75,000 injuries. The resulting devastation and damage to civilian infrastructure and health care facilities have severely restricted access to relief agencies and hindered health care provision. Humanitarian aid, averaging around 500 trucks daily before the conflict, now struggles to surpass 250 trucks, exacerbating an already dire situation. Moreover, delivering aid, especially to vulnerable areas like North Gaza, poses significant risks, deepening the crisis.
The health care system's collapse compromises the standard of care. After administering iodine, we give my 14-year-old patient a bolus of 25
“Over the past six months, practicing medicine in Gaza has presented unfathomable challenges on several levels. The physical, mental, and spiritual toll it takes on both providers and patients is undeniably tragic from any perspective.”
milligrams of Ketamine and place a 24inch chest tube into his left thorax using a blade with no handle. My team of three and I lift him off the floor so the chest tube can drain. We do this three times every hour until we can confirm tube placement via X-ray and transfer him to a bed next to another patient.
Al-Nasser, Gaza's second-largest hospital after Al-Shifa, which became inoperable in November, has a capacity of around 300 patients, six operating rooms, a 12-bed adult ICU, a six-bed neonatal ICU, and a pediatric ICU. In January, the hospital housed over 1,000 recovering patients, with thousands more seeking refuge in and around the hospital complex. You could not walk anywhere in the hospital without seeing displaced families sleeping in the hallways, many of the health care staff among them.
These mass casualty events necessitate resource mobilization, often involving improvisation due to equipment shortages. Imagine intubating a patient while delegating tasks to relatives, such as bagging or holding blood products due to a lack of ventilators and rapid infusers.
As one might anticipate, these mass casualty events often demand a significant mobilization of resources. Picture this scenario: you're intubating a 26-year-old man, knowing you must rapidly assess five other patients. So, you assign his brother to assist with bagging him and his cousin to hold up and squeeze the packed red blood cells (pRBCs) because there's no rapid infuser or ventilator available. Blood products are stored in a drink cooler in the corner of the resuscitation bay. Although the CT scanner at Al Nasser functions well, many days pass without contrast due to critical medical supplies likely stuck at border crossings, hindering the functioning of partially operational hospitals. The inconsistent availability of medicines and equipment extends beyond contrast media to include intravenous antibiotics,
anesthetics, beta-blockers, calcium channel blockers, amiodarone, nebulized albuterol, and more. Suffice it to say, essential resources for a trauma center to serve its patients were never reliably accessible, severely impeding our ability to provide consistent and predictable management.
Providing health care during wartime is never easy, but certain rules and laws enable health care workers to practice in a relatively safe and secure manner. Unfortunately, in Gaza, I witnessed how the health care system was dismantled and health care workers, along with infrastructure, were devastated. As of the time of writing, only 12 out of 36 hospitals are partially functioning, and the two largest hospitals with multiple specialties are no longer operational. During my time at Al Nasser Hospital, it was surrounded by tanks, and I vividly recall being in the call room and the constant fear of being struck by shrapnel or that the building would be hit by a missile. Every explosion shook the hospital, damaging the ceiling and terrifying those seeking shelter. Fortunately, I was evacuated to safety, but I left behind my colleagues and patients. Eventually, the hospital was raided, leading to the arrest of 70 staff members.
During my final days in Gaza, I worked at Al Aqsa Hospital in Deer El Balah (Central Gaza). This hospital was overwhelmed, handling a large volume of trauma patients with only one CT scanner that could produce axial images of the brain due to outdated software and broken parts. During this time, I assessed a 50-year-old male who was on the third day of his hospital stay, recovering from a shrapnel injury that required a left-sided chest tube and serial abdominal exams. Upon examination, he appeared confused and febrile, with a distended abdomen. Due to our imaging limitations, we utilized a portable ultrasound and observed dilated small bowel loops. Consequently, we placed a nasogastric tube and drained 3 liters of dark black liquid from
his stomach. We sought consultation from a surgeon, who expressed concerns about the patient's development of anuric renal failure and hemodynamic instability secondary to sepsis, making the likelihood of survival from an exploratory laparotomy unlikely. Additionally, the surgeon questioned the necessity and potential outcomes of such a procedure. Sadly, later that night, the patient coded and died. The following day, I returned to the hospital and witnessed his family performing the traditional funeral prayer over his body before burying him in the hospital cemetery.
Over the past six months, practicing medicine in Gaza has presented unfathomable challenges on several levels. The physical, mental, and spiritual toll it takes on both providers and patients is undeniably tragic from any perspective. However, a key advantage of being in medicine is the ability to transcend political and partisan divides. We advocate tirelessly for all our patients, regardless of their race, ethnicity, background, or creed. The Palestinians of Gaza are in desperate need of necessities such as food, water, medicine, shelter, and safety. I can confidently say those are the doctor’s orders.
The views and opinions expressed in this article are those of the author and do not necessarily reflect the official policies, positions, opinions, or views of the Society for Academic Emergency Medicine or its members.

Dr. Thaer Ahmad is the emergency department director of global health and medical ethics and an emergency medicine physician at Advocate Christ Medical Center in Oak Lawn where he is also assistant residency program director.
Pride Month is a moment of celebration and joy, showcasing the vast diversity of the LGBTQ+ community and their journey toward acceptance and freedom to love. Beyond parades and parties, Pride Month commemorates the Stonewall Riots of June 1969 in New York City, a pivotal moment in the fight for LGBTQ+ equality in the United States. Despite gradual progress toward equal rights in recent decades, societal prejudice and discrimination persist, resulting in significant disparities
for this community. LGBTQ+ youth are disproportionately affected by bullying, suicidal thoughts, substance use disorders, and homelessness For transgender women of color the situation is even more dire, with lower life expectancies and higher murder rates than their cisgender counterparts. Additionally, public queer spaces are frequently targeted for mass shootings and violent protests.
Challenges to LGBTQ+ equality have intensified in recent years. Notable
setbacks include a transgender military service ban, restrictions Pride flag displays at U.S. embassies, limitations on LGBTQ+ educational content in schools, curtailments of health care access, and the elimination of diversity programs. In 2023, over 350 antitransgender bills were introduced in state legislatures. Several states prohibit transgender youth from participating in sports according to their gender identity, restrict access to gender-affirming treatment and public restrooms, and
impose trans-targeted restrictions on gender changes to government documents.
Emergency medicine (EM), with its focus on social health determinants, inadvertently contributes to LGBTQ+ disparities. Even as allies or members of the LGBTQ+ community, all providers may play a role in perpetuating health inequities, often due to ignorance or inaction. Negative patient experiences, such as misgendering, care refusal, discriminatory remarks, and provider ignorance, heighten reluctance to seek medical care. Research by Moll et al. underscores the scarcity or absence of LGBTQ+ health care education in residency programs, as well as microaggressions and discrimination against LGBTQ+ trainees.
As emergency physicians, we have the opportunity to employ various strategies to enhance support for LGBTQ+ individuals. Your engagement with this content demonstrates a commitment to learning and improvement. We encourage you to use Pride Month in June as an opportunity for reflection and to consider actionable steps to address these issues and effectively support the LGBTQ+ community.
Take the initiative to learn about LGBTQ+ history and health issues by reading works by queer authors and seeking insights from colleagues. If you’re involved in emergency medicine education, evaluate and enrich your curriculum to ensure comprehensive coverage of LGBTQ+ health care topics. Here’s a resource.
Acknowledge the national assault on LGBTQ+ rights and the barriers to advocating for diversity, equity, and inclusion. Speaking up against these challenges demonstrates compassion and advocacy for positive change.
Deepen Your Understanding
Get to know us. Make an effort to understand the lived experiences of LGBTQ+ patients, learners, and colleagues. Deep, engaged conversations can help break down barriers and foster connections.
Value Individuals Beyond
Recognize each person as an individual

first, not just by their LGBTQ+ identity. Avoid tokenism by treating everyone as valued members of the health care team with diverse identities.
Actively stand against bias, microaggressions, and discrimination in health care settings. Small actions can significantly impact creating an inclusive environment. For some simple tips, check out this resource
Show Your Support Visibly
Simple gestures, including pronouns in virtual meetings or wearing pride symbols, signal allyship and create a welcoming atmosphere.
Celebrate and Advocate
Pride is a time of celebration, solidarity, and hope for queer people across the country. Participate in Pride and support LGBTQ+ rights year-round. Advocacy and celebration are crucial to fostering progress and unity, especially in challenging times.
By implementing these strategies, we can better support our LGBTQ+ friends, colleagues, and patients, creating a more inclusive and understanding health care environment.
The views in this article are the authors’ own and not necessarily those of their institutions. It reflects personal insights on LGBTQ+ equity and inclusion in emergency medicine.



Dr. McFarland is assistant residency program director, University Hospitals. Dr. Alvarez, MD, is director of well-being at Stanford Emergency Medicine and the 2023-2024 chair of the SAEM Wellness Committee. @alvarezzzy
Dr. Weygandt is an assistant professor and associate residency program director at Johns Hopkins Emergency Medicine.

Key learning points for the following article were adapted from the SAEM webinar "Chrono-nutrition: Timing and Frequency of Meals for Optimal Health.”
Navigating a shift schedule, especially within the demanding environment of the emergency department (ED), involves juggling fluctuating working hours and heavy workloads. The additional responsibilities of an academic physician further compound these challenges. Amidst the hustle and bustle of the ED, personal needs, such as maintaining proper meal timing and nutrition, often get overlooked,
particularly during busy shifts. However, with strategic planning and mindful adjustments, emergency physicians can prioritize their well-being, even during the busiest shifts.
• Establish a consistent meal schedule regardless of your shift schedule.
• Aim to eat your main meals (breakfast, lunch, and dinner) at regular intervals.
• Consume your first meal about an hour after waking up to kickstart your metabolism. Ensure adequate protein
intake (about 0.3 grams per kilogram of body weight) in your first meal.
• Aim for higher-calorie meals earlier in the day and lighter meals in the evening to align with your body's natural rhythms. (Our bodies digest food, particularly carbohydrates, better in the morning than in the evening.)
• Finish your last meal at least four hours before bedtime to aid digestion and promote better sleep.
• Optimize fasting periods in the evening and while sleeping, aiming
“Navigating a shift schedule, particularly within the demanding environment of the Emergency Department (ED), involves managing fluctuating working hours and heavy workloads.”
for 12-14 hours starting one to two hours after waking to maintain glucose tolerance and potentially leaner body composition.
• Avoid late eating windows (e.g. 12 noon to 8 p.m.)
• Choose nutrient-dense foods such as nonstarchy vegetables, fruits, lean or plant-based sources of protein, whole grains, and small amounts of nuts and seeds to sustain energy and mental alertness. Consider using the Diabetes Plate Method
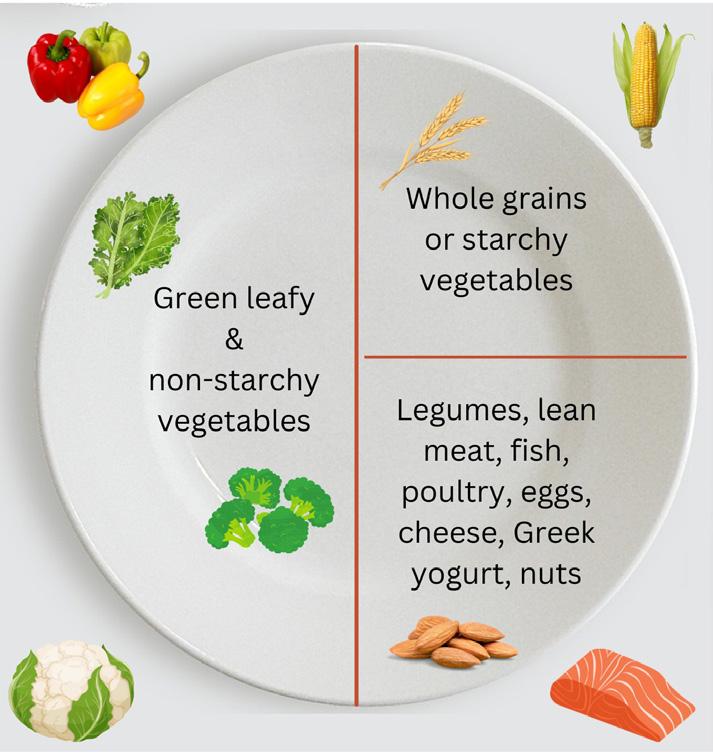
• Prepare meals and snacks in advance for readily available healthy options during shifts. Portable choices like high-protein sandwiches, fresh fruits, unsweetened yogurt, low-fat cheese, hummus, and homemade trail mix (unsweetened dried fruits and nuts) are convenient.
• Include snacks with 5-10 grams of protein to keep you feeling satisfied and stabilize blood sugar levels.
• Stay hydrated throughout your shift by keeping a large water bottle at your workstation and drinking regularly. Dehydration can lead to mental and physical fatigue, agitation, and decreased cognitive function, impacting performance.
• Aim for euhydration and optimal total body water content using a urine color chart
• Consume caffeinated beverages strategically to minimize the effects of sleep deprivation, particularly during long shifts.
• Opt for small, frequent (as needed) doses of caffeine (40-60 grams) to maintain alertness and minimize its effect on recovery sleep.
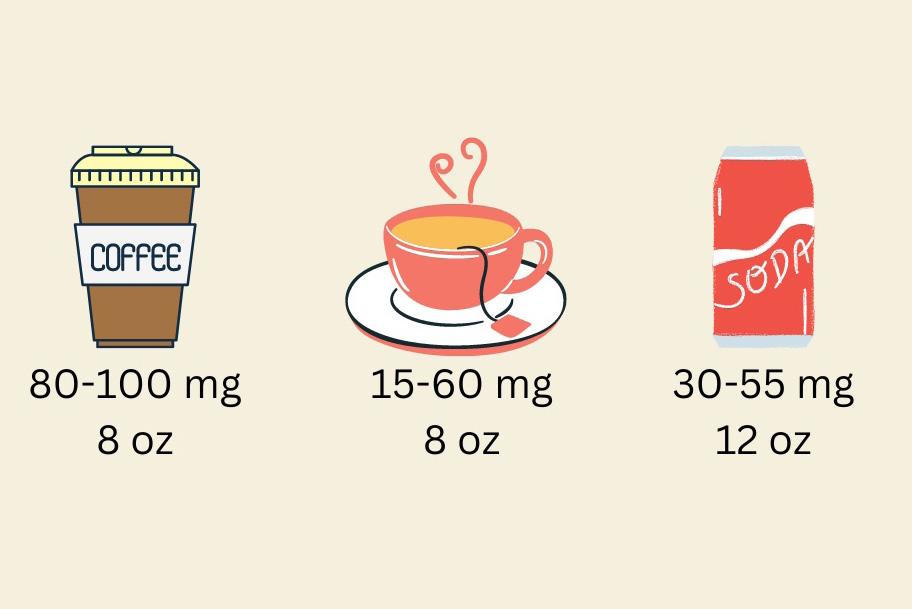
• Green tea and matcha are more effective than coffee or other caffeinated beverages in increasing focus.
• Be aware of caffeine’s half-life (approximately six hours) and avoid consumption too close to bedtime to prevent sleep disturbances.
• Maintain consistency in your daytime eating schedule to regulate your body's internal clock.

• Avoid eating during typical sleep hours to minimize disruption to your circadian rhythm.
• Consume a high protein dinner before midnight and avoid eating during periods of low alertness, such as between 2-6 a.m., to support cognitive function, minimize errors, and maintain peak performance. Focus on hydration instead.
• Limit caffeine intake after midnight if planning to sleep soon after your shift ends and consider alternatives such as herbal teas or gum for alertness.
• Communicate with supervisors, colleagues, trainees, and ED staff about your plan to take a break to eat. Setting this expectation can help prioritize wellbeing during busy shifts.
Implementing these strategies can optimize meal timing and nutrition even amidst the challenges of working on a shift schedule. Prioritizing self-care ultimately supports overall health, wellbeing, and performance in the demanding environment of the ED.


Dr. Karamatsu is a pediatric emergency medicine wellness champion and an assistant professor of emergency medicine and pediatrics at Stanford University School of Medicine.
Dr. Makowski is a clinical associate professor, nutrition professional, and physician wellbeing coach in the department of psychiatry and behavioral sciences. She is also the associate director of scholarship and health promotion at Stanford Medicine WellMD and WellPhD.

I check each cord one more time. Ethernet to ensure flawless connection? Plugged in. Charging cable to prevent unexpected power loss? Check. Ring light to look as professional as possible? On and working. Adjusting my camera angle once more, I ensure everything is set just right. Three books under the computer? No, four would offer a better view. I add the book, adjust the camera angle, check the image, and... perfect. Not only do I look presentable, but the secret I am trying to hide from the interviewer on the other end of this virtual residency interview is completely out of sight. My secret? No, I’m not wearing sweatpants, though they would be more comfortable than the slacks I wear, unbuttoned and unzipped to accommodate my real secret: my pregnant belly.
I understood then, as I do now, that my pregnancy should not affect how the interviewer perceives me, yet I worried it might. I feared programs would rank me lower because of my clear intention to have children. I realize now, since choosing a residency can be so challenging, that I should have used my pregnancy as a tool to filter out programs that would not be family friendly. Ultimately, and ironically, after all my anxiety during interviews, the program I matched at was the only program that knew I would be a mother when I started training.
Thankfully, I have been well-supported as a mother throughout my training, though I’m aware not all parents have had the same experience. Before I officially started, I brought my infant son to a residency social event and felt
immediate care and support. When I disclosed my desire for more children, leadership assured me it would not be an issue, and indeed, it wasn’t. Upon disclosing my pregnancy during second year, night shifts vanished off my schedule to support my and my developing daughter’s health. I was encouraged to take as much maternity leave as I needed or wanted, even extending my residency if I desired. My rotation schedule was adjusted to ease my return to full-time residency training. When I chose to breastfeed my second born, co-residents and attendings reminded me to pump on shift, and a breastmilk fridge was placed in the resident workroom. Even when my children accompanied me to a journal club due to my husband’s last minute work emergency, my co-residents
“Not only do I look presentable, but the secret I am trying to hide from the interviewer on the other end of this virtual residency interview is completely out of sight.”
warmly welcomed them, helping to entertain them, and acknowledging their good behavior.
Overall, I have been loved and supported and encouraged to be my best as both a mother and a physician.
Despite all this support, challenges exist. Countless bath times, mealtimes, and bedtimes are missed. There are full days during which I see neither of my children. Favorite songs, books, and routines change without me. The house remains a mess with old food on the table and toys on the floor as neither my husband nor I have the time or the energy to clean between our jobs and parenting. “I want my Daddy!” rings through the house during a tantrum, breaking my heart for the bonds cleaved by the essentials of modern residency. On many days, my husband functions as a single parent, taking the kids to and from daycare, feeding them, putting them to bed, and finally going to bed alone, all while I care for the children and spouses of strangers in the emergency department.
I do my best across the board, yet I feel myself grazing the bar of bare minimum. As most of us who have pushed through medical training, bare minimum has never been acceptable. There is mom guilt, there is work guilt, both of which are unrelenting and can be crushing. I cannot fathom what could have been my struggle had I ended up at a residency program that supported growing my career and education without supporting my growing family as well. I know I am a lucky one, and I worry for the unlucky ones as I hear the quiet mutterings of struggle from other mothers dedicating their professional lives to the practice of medicine.
How parents are treated in their medical training will change the landscape of medicine. Recent surveys have found that one-sixth to one-third of trainees feel their program is not supportive of their decision to start a family. Forty percent of graduate medical trainee parents
report that having children changed their plans for subspecialty training or practice environment. Residency applicants are recognizing the need for support and seeking it out as well, with over half of respondents reporting that their rank lists were affected by the perceived support of the families of trainees.
Parental leave policies are one means by which programs can support their residents. Forty-four percent of women who had a child during medical training described inadequate leave. ABEM requires 46 weeks of training per level, with an allowance for two additional weeks of leave at the program director’s discretion. This equates to a maximum of 6-8 weeks per training level, including vacation time. Beyond this, residents must extend their training. Per Accreditation Council for Graduate Medical Education (ACGME) rules, the first six weeks of approved parental leave must be paid. The American Academy of Pediatrics recommends a guaranteed 6-8 weeks for new parents of all familial structures and specifically states that it is preferable to protect vacation, sick leave, and electives. Despite this, a recent survey found that 58% of parent trainees needed to use all their vacation/sick/ leave time, with 100% of respondents expressing a desire for more maternity leave.
There also exists room for improvement in the way lactation is addressed in medical training. Only 53% of female trainees felt supported in lactation and pumping endeavors. ACGME also has a policy requiring space for lactation, but notably does not define any protected time for lactation. Though not mentioned in the ACGME policies, the PUMP Act 2023 delineates the worker’s right to reasonable break time in addition to a place for mothers to express breast milk while at work. To help mitigate the many challenges of lactation during residency, since 2019 the Office of Graduate Medical Education at the University of Kansas School of Medicine has been providing resident physicians with free,
wearable breast pumps for up to one year to support their lactation endeavors. Anecdotally, I can say that I purchased my own wearable breast pump and that its use revolutionized my ability to function simultaneously as mom and doctor.
The challenges of parenthood are innumerable, and compounded by the demands of residency, at times seem insurmountable. While tangible changes are being made regarding parental leave and lactation support, the need for support extends beyond childbirth and breastfeeding. And while I have primarily spoken of motherhood, many fathers experience similar struggles. I have received estimable advice from several attendings, both mothers and fathers, who are also navigating parenthood and physicianhood. Though I’ve yet to need it, my list of co-residents and attendings willing to provide last-minute babysit in an emergency is extensive. The ability to bring my children to residency events and have them welcomed with smiles and hugs is invaluable.
Reports suggest that about onethird of respondents, regardless of gender, and nearly one-half of mothers, considered leaving medical training after having children due to familial stressors. Residency is hard enough. Parenthood is hard enough. It is crucial that we take steps to protect and support our residents as parents, through both written policies and unwritten cultural changes.
The author would like to acknowledge Drs. Michelle Lall and Christine Stehman for their assistance in the completion of this article.

Dr Beetler is a third-year emergency medicine resident at the University of Illinois College of Medicine, Peoria, where she also obtained her medical degree. She is a mother of two: Teddy, 3, and Bridget,1.

As we enter yet another recordsetting Everest tourism season, some circumspection is warranted surrounding our interaction with guiding companies and high-altitude porters. Tourism volumes have skyrocketed on the Everest base camp trek and multiple budget guide companies have sprung up to meet the growing demand, offsetting that cost and displacing the medical risk onto a vulnerable population: the high-altitude porter. This history is shared with consent of the patient, a high-altitude porter (lowlander by birth) operating in the Himalayas during the 2023 summiting season.
Kaji’s Story
Around eight in the morning, Kaji was carried into our aid clinic lying limp in a
basket suspended only by a rope slung high on the forehead of a fellow porter. He had been found during a morning check of the rooms at a local teahouse. When no response came to knocks at the door, a local sherpa broke the door down to find Kaji’s unresponsive body slumped in the bed. He was rushed to our clinic where a quick once-over revealed a profoundly tachypneic young man, tachycardic to the 160s, pressure 60s over palp, completely unresponsive, with an SpO2 in the high 40s. Kaji (though we didn’t know his name at the time) was as close to death’s door as anyone we’d seen that summiting season.
Porters are a common site on most highaltitude treks. Many popular summits like Kilimanjaro mandate their use
as a means of providing jobs and stimulating the local economy. These industries are largely unregulated by local governments. In the Khumbu, the region of Nepal encompassing most of the Everest base camp trek, porters are often hired on site at the start of the trek with nothing more than a handshake and a verbal agreement with the lead guide of a basecamp trek. Because they are compensated based on the weight (in kilograms) they carry to camp, porters often shoulder tremendous loads to basecamp in a matter of just a few days.
Kaji was a mystery to us when he first arrived. No one in the tea house knew his name or recognized him. Our only clue was a note found in his wallet, presumably from a trekker he had

“Tourism volumes have skyrocketed on the Everest base camp trek and multiple budget guide companies have sprung up to meet the growing demand, offsetting that cost and displacing the medical risk onto a vulnerable population: the high-altitude porter.”
worked with, dated from 2013. This note provided his name, or rather, his nickname. Kaji, as I came to learn, roughly translates “captain,” and is a name given to many Nepali with a family military background. It often serves as a nickname, adopted by multiple members of those same families. Therefore, it was as nondescript as finding a note addressed “to Mr. Smith” in the United States.
Medically, Kaji was no less enigmatic. The undifferentiated obtunded patient is a common presentation in the emergency department, but in an aid station equipped only with point-of-care tests
and a bedside ultrasound, diagnostic certainty is often a helicopter evacuation and a day’s travel away. A bedside ultrasound revealing florid b lines strongly favored our suspicion of profound high altitude pulmonary edema (HAPE), but whether his mental status was due to high altitude cerebral edema (HACE), intracerebral hemorrhage (ICH), profound acidosis, or a host of other causes was still anyone’s guess.
The Nepali Board of Tourism has recently imposed weight restrictions on the loads porters carry at altitude. In the mid 2010s, those loads were set at 35 kilograms, or around 75 pounds. Suggested
maximum loads have since been revised to 25 kilograms, or about 55 pounds. Because no enforcement mechanism exists for these restrictions, loads carried often tremendously exceed this. A 2017 study of 113 porters trekking to Namche found that the average load carried was 90% of body mass. For a 160-pound human, that would equate to carrying a staggering 140 pounds of load. Because they are paid by the trip to basecamp, many altitude porters make this trip, typically nine-day ascent, in a mere three

WILDERNESS MEDICINE continued from Page 81
to four days. This dual threat of extreme exertion and rapid ascent is the classic setup for severe altitude illness.
Kaji remained under our care for nearly 24 hours until we could secure him a helicopter evacuation for him down the mountain. I stayed in the clinic with him overnight, huddled into a sleeping bag on a small wooden slat not far from his bed, administering serial doses of empiric glucocorticoids to treat presumptive HACE, continuous facemask oxygen, and performing regular neurologic exams. His obtundation gradually improved over the first six hours. By hour 12, around the middle of the night, he said his first word since I’d met him: “toilet.” As we removed his restraints — placed around the sixth hour as he began to move,
“The Nepali Board of Tourism has recently imposed weight restrictions on the loads porters carry at altitude.”
agitated and flailing, and ripped out his IV — he attempted to get up to pee but displayed marked ataxia. We quickly arrested his desperate stumble to the door and supported his weight enough to use a bedside urinal. By morning he was able to string together a few broken sentences and provide us with his name and the name of the guiding company with whom he had made a verbal agreement at basecamp.
Our paramedic and jack-of-all trade Thaneshwar called the guiding company who flatly denied any knowledge of Kaji. This practice is not unusual for
unscrupulous companies in the region. The cost of evacuating a porter by helicopter and paying for their stay at a local hospital is considered a significant expense, typically ranging from $100-$200. Fortunately our medic Thaneshwar was adept in the political and social maneuverings of the Everest region. After an unambiguous threat to report the guiding company to the head of the board of tourism, a payment was suddenly secured for Kaji’s helicopter down to Kathmandu. Following nearly a full day of continuous treatment and close monitoring, Kaji managed to walk,
Kaji shortly after arrival being seen by our medic Thaneshwar (left) and Nepali doctor Nishant Joshi (right)
albeit a bit shakily, to the helicopter that transported him to a hospital located at a lower elevation.
The perverse incentives of cheaper altitude tourism and higher volumes have led to an unmistakable trend in the epidemiology of altitude disease in the Khumbu. Himalayan Rescue Association records of clinic visits indicate that annually, local porters and guides represent between 70 and 80% of severe altitude illness cases. This distribution of disease provides a clear thesis: porters not only shoulder the physical burdens of trekkers and climbers, they absorb real medical risk on behalf of tourists in the region.
Nonprofits seeking to safeguard porter welfare have sprung up on some popular mountain routes. For instance,
the Kilimanjaro Porter Assistance Project seeks to ensure fair wages and safe carrying loads for porters. In the Everest region, these initiatives have largely been confined to individual guide companies who report load limits and wages for their own porters but do not safeguard the broader vulnerable population.
Efforts to establish a nonprofit monitoring group to oversee porter welfare in the Khumbu have encountered with challenges owing to the corruption present across most levels of the Nepali government. Nevertheless, the Himalayan Rescue Association serves as a de facto monitor, reporting violations to the Nepali Board of Tourism. There is still much hard regulatory work to be done in securing safeguards for this vulnerable population. However, for those of us embarking on
high-altitude expeditions, there is another crucial step to take: ensuring that your guiding company prioritizes the welfare, wages, and loads of its porters. Despite potentially higher costs, whether you realize it or not, you are contributing to saving lives.
Dr. Apisa is the assistant fellowship director of the Massachusetts General Hospital (MGH) Wilderness Medicine Fellowship, the inaugural fellow of MGH's Space Medicine Fellowship, and a clinical instructor of emergency medicine at Harvard Medical School.
The SAEM Foundation (SAEMF) is the philanthropic arm of SAEM which works to bridge the research funding gap in emergency medicine (EM), advance the science and innovation at the heart of the specialty, and build the pathway of talented EM research and education leaders for the future. Please join the SAEMF



Evangelia Murray, MD
Denver Health
Board of Trustees and all of our generous donors in celebrating our 2024 SAEMF grant recipients! Thanks to our Annual Alliance donors, $970,261 was awarded to these 30 promising researchers and educators to fund their work in academic emergency medicine.
SAEMF Research Training Grant - $300,000
Comprehensive Emergency Department-based Social Needs Screening
Lauren K. Stewart, MD, MS
Trustees of Indiana University
SAEMF Research Large Project Grant - $150,000
Targeting Metabolic Syndrome from the Emergency Department through Mixed-Methods
Vytas P. Karalius, MD, MPH, MA
Stanford University
SAEMF Education Research Training Grant - $100,000
The Resident Unionization Study: A Qualitative Analysis of Drivers and Outcomes
Torben K. Becker, MD, PhD, MBA
University of Florida Board of Trustees
SAEMF Emerging Infectious Disease and Preparedness Grant - $100,000
MotoMeds: Preventing Child Morbidity and Mortality from Infectious Diseases in Ghana







Ravi V. Chacko, MD, PhD; Ryan McKillip, MD
Advocate Health Care Network
SAEMF Emerging Infectious Disease and Preparedness Grant - $99,106
Improving Antibiotic Stewardship for Urinary Tract Infections Using Machine Learning
Samita M. Heslin, MD, MBA, MPH, MA, MS
Stony Brook University
SAEMF/ED Benchmarking Alliance Clinical Operations Research Grant$50,000
Artificial Intelligence Augmented Emergency Department Triage
Rachel M. Skains, MD, MSPH
University of Alabama at Birmingham
GEMSSTAR for Emergency Medicine Supplemental Funding Program$25,000
Risk Factors and Time Course of Incident Delirium Among Older Adults in the Emergency Department (ED)
Leland Perice, MD
Rhode Island Hospital
SAEMF ARMED Pilot Grant - $25,000
Ultrasound-guided Serratus Anterior Plane Block in ED Patients with Rib Fractures
Elizabeth J. Yetter, MD, MHPE
Icahn School of Medicine at Mount Sinai
SAEMF ARMED MedEd Pilot Grant - $25,000
Barriers and Motivators for High- vs. Low-utilizers of POCUS: A Mixed Methods Study
Emily Chien, MD, MPH, MBA
Weill Cornell Medicine
SAEMF Education Project Grant - $20,000
Evaluation of the Emergency Medicine Training Program at Aga Khan
University Hospital
Joan Chen, MD
Mount Sinai Emergency Medicine
SAEMF NIDA Mentor-Facilitated Training Award - $12,000
Community Paramedicine Interventions for People Who Use Drugs







Kira Gressman, MD
University of Washington
SAEMF NIDA Mentor-Facilitated Training Award - $12,000
Establishing a Quality Framework for Post Overdose Care and Harm Reduction in the Prehospital to Emergency Department Care Continuum in Seattle, King County, Washington
Simon J. Ostrowski, MD
University of Pittsburgh
SAEMF/MTF Toxicology Research Grant - $13,610
Feasibility of Assessing Alcohol Withdrawal Syndrome with a Wearable Biosensor
Denise N. Fraga, MD
Atrium Health - Carolinas Medical Center - Wake Forest Baptist
SAEMF/AEUS Research Grant - $10,000
Pediatric Cranial Ultrasound for Point-of-Care Intracranial Pathology Detection
Lynn P. Roppolo, MD
Integrative Emergency Services at Tarrant County Hospital District, JPS Health Network
SAEMF/AEUS Research Grant - $10,000
A Multi-center Trial to Determine eFAST Longitudinal Curves Using CUSUM Analysis
Megan Rybarczyk, MD, MPH
University of Pennsylvania, Department of Emergency Medicine
SAEMF/GEMA Research Pilot Grant - $10,000
Acute Coronary Syndrome in a Pakistan ED: Risk Factors and Clinical Pathway
Ryan E. Tsuchida, MD
University of Wisconsin, Department of Emergency Medicine
SAEMF/ADIEM Research Grant - $6,000
A Qualitative Case Study Analysis of Diversity, Equity, and Inclusion Leaders in Emergency Medicine
Joe-Ann Moser, MD, MS
The Board of Regents of the University of Wisconsin System
SAEMF/AWAEM Research Grant - $5,000
Non-Promotable Task Completion by Emergency Medicine Chief Residents





Kei U. Wong, MD
Rutgers New Jersey Medical School
SAEMF/Simulation Academy Novice Research Grant - $5,000
High-risk, Low-frequency Pediatric Procedural Training: Simulationbased Pediatric Emergent Airway Curriculum for EM Residents
Ashley P. Cohen, MD
University of Michigan
SAEMF/RAMS Resident Research Grant - $5,000
Law Enforcement As a Bridge between Bystanders and EMS in Cardiac Arrest
Marina Gaeta Gazzola, MD
New York University Grossman School of Medicine
SAEMF/RAMS Resident Research Grant - $5,000
Enhancing Emergency Department Distribution of Drug Checking Tools
Thomas K. Hagerman, MD
Henry Ford Health System
SAEMF/RAMS Resident Research Grant - $5,000
Improving the Emergency Department Discharge Process for Older Adults: The GET HOME Safe Discharge Intervention
Jane M. Hayes, MD, MPH
Mass General Brigham
SAEMF/RAMS Resident Research Grant - $5,000
Policies and Practice for Prehospital Blood Transfusion in the United States
Rebecca A. Leff, MD
College of Medicine Mayo Clinic (Rochester)
SAEMF/RAMS Resident Research Grant - $5,000
Implementation of a Multi-Tier Trauma Activation Protocol in Kumasi, Ghana
Carly Whittaker, DO, MPH
Memorial Healthcare System
SAEMF/RAMS Resident Research Grant - $5,000
Sequential and Simultaneous Video Laryngoscopy-assisted Flexible Endoscopic Intubation




Pauline Wiltz, DO
University Hospital Cleveland Medical Center
SAEMF/RAMS Resident Research Grant - $4,045
From Margins to Mainstream: Mapping Health Disparities in Obstetric Care in the Emergency Department
Elizabeth A. Abrams, MSPH
The Ohio State University
SAEMF/RAMS Medical Student Research Grant - $2,500
Comparing Health Records and Self-Report Data to Target ED HIV Screening
Arthi Kozhumam, MScGH
Ann & Robert H. Lurie Children’s Hospital of Chicago
SAEMF/RAMS Medical Student Research Grant - $2,500
Child Passenger Safety and Associations with the Child Opportunity Index
Michael Makutonin
The George Washington University
SAEMF/RAMS Medical Student Research Grant - $2,500
Effects of Prolonged ED Length of Stay in Pediatric Psychiatric Crisis Patients
Over $160,000 raised…80 Chairs are now 2024 donors… 21 states and the District of Columbia have gone green!
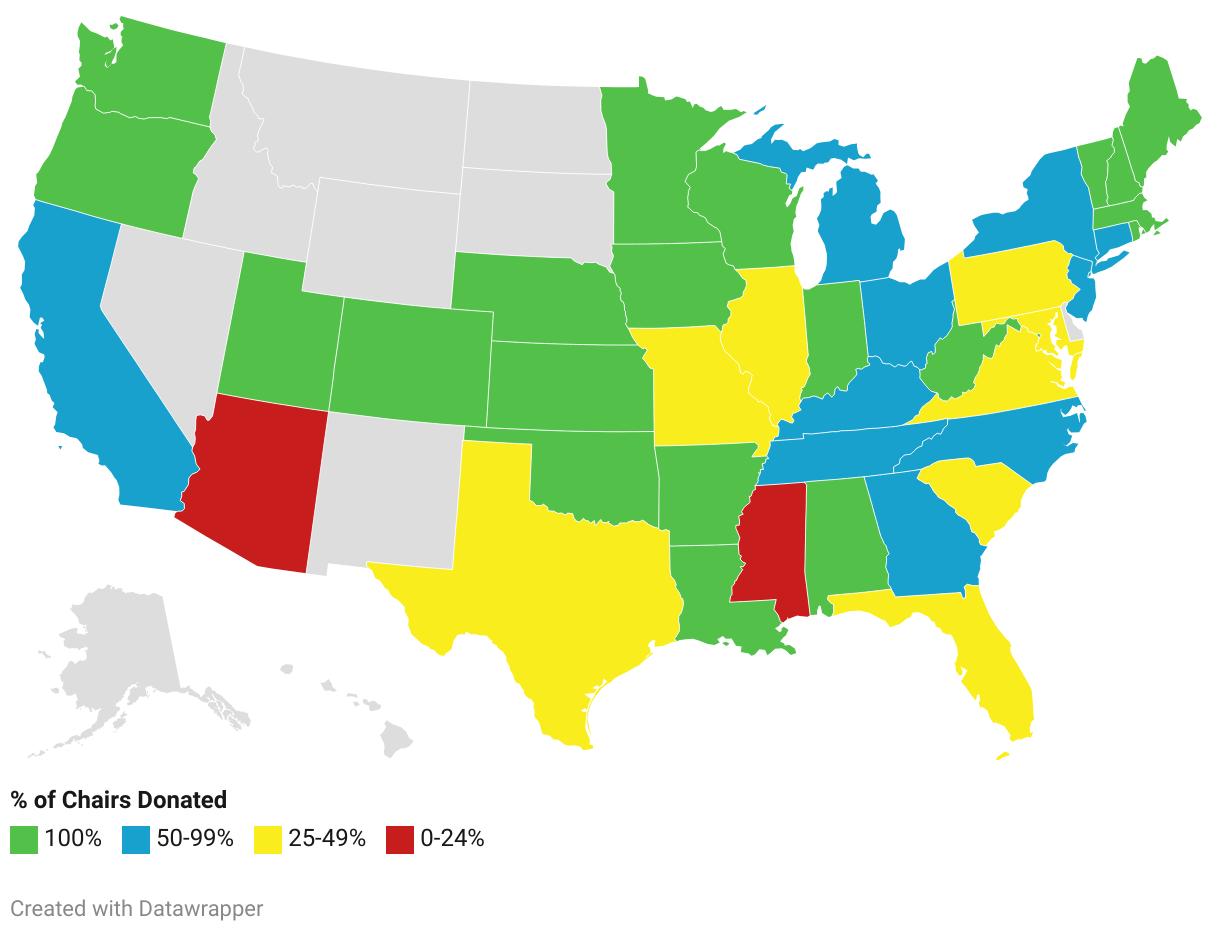
$160,090
Since 2019, AACEM members have donated over $560,000 to support and train emergency medicine researchers and educators via SAEMF’s grants initiative. Thanks to our generous Chairs’ Challenge donors, SAEMF invested nearly $1 million to support its 2024-25 SAEMF grantees! SAEMF President, Manish N. Shah, MD, MPH asked AACEM Chairs to once again show leadership and to facilitate even more research by making a personal gift of $1,000 to SAEMF during the recent AACEM Chairs Retreat. They responded to that request by donating and pledging over $160,900! States turn from red to green based on the donation participation rates of AACEM member Chairs in the state. Congratulations and thank you AACEM – the 2024 Challenge map is a sea of green!
Email Julie Wolfe to pledge support as an Advocate Donor of the SAEMF Annual Alliance with a commitment to donate $1,000/year for 2024-26. As a special “thank you” for your gift, we invite you to be our guest in the SAEM24 VIP Lounge during our annual meeting. Here, you’ll find a quiet environment to work and recharge, complimentary snacks and beverages, and the opportunity to network with other VIPs. Become an Annual Alliance donor today and take your place on our digital donor wall alongside other generous academic emergency medicine leaders! Check out all the Annual Alliance donor benefits and consider donating or pledging your support today!
SAEMF’s Vice Chairs’ Challenge showcases the generous giving that comes from our vice chairs each year and serves as a rallying call to unite vice chairs in support of more funding for future EM researchers and educators.
Become a Vice Chairs’ Challenge donor www.saem.org/donate or email Julie at jwolfe@saem.org to pledge support
Donate or pledge a gift of $250 or more by August 31, 2024 and be recognized:
As an Annual Alliance Mentor or Young Professional
With your name on the big screen during the AACEM/AAAEM Annual Retreat
With the opportunity to network with grantees and leaders at the SAEMF’s Coffee & Networking session at SAEM24
With your name in lights on the electronic donor wall at SAEM24 Visit saem.org/vicechairschallenge for details
Thanks for considering a donation today !
You can Name a grant in honor of someone who has made a difference in your career or in the field. Email Julie Wolfe for details.
Your gift of any amount counts toward participation in the Chairs Challenge (if made before March 22nd), Vice Chairs' Challenge (if made before the end of the AACEM Retreat), and the Academy, Committee, Interest Group Challenge (if made before August 31st). Give once and you are done!
It’s easy to become a Mentor level donor with an annual monthly gift of just $100 (March - December 31, 2024). Pledge that same monthly gift for three years and you’ll be our newest Advocate donor. Join now to take advantage of 2024 recognition benefits. Your gift will help fund future researchers, educators, and leaders.
SAEM Issues Formal Opposition to the EDUCATE Act
In a statement issued April 3, 2024, the SAEM Board of Directors announced the Society’s opposition to the Embracing Anti-Discrimination, Unbiased Curriculum, and Advancing Truth in Education (EDUCATE) Act (H.R. 7725), citing the bill’s failure to acknowledge the importance of DEI initiatives in fostering innovation, advancing health equity, and improving health outcomes for patients. SAEM criticized the bill’s constraints on federal funding for DEI-based educational programs for hindering efforts to address systemic inequities and perpetuate health care disparities. Emphasizing the necessity of integrating DEI principles into medical education, SAEM urges policymakers to reject the EDUCATE Act to ensure equitable access to quality care for all Read the full statement here
Call for Topic Proposals: 2026 Consensus Conference
SAEM is now accepting proposals for topic ideas for the 2026 Consensus Conference, to be held April 14, 2026, at SAEM26 in Atlanta, GA. The consensus conference gathers researchers, thought leaders, and other stakeholders in emergency medicine to generate research agendas for the important, unanswered questions facing emergency care, leading to high-quality, funded research projects of varying scopes from a variety of funding sources. Topics must be submitted by 5 pm (Central Time) on May 24, 2024. If your topic is selected for consideration, you will be invited to submit a full proposal to host the 2026 consensus conference.
Every year the SAEM Foundation (SAEMF) aims to award close to $970,000 to SAEM members to enhance their career development and study the most critical challenges in emergency medicine (EM). To date, the SAEMF,
together with SAEM, has awarded more than $13.5 million to over 570 academicians. Check out this year’s grant funding opportunities and apply by 5 p.m. CT August 1, 2024!
Grant Funding Opportunities
• Research Training Grant (RTG)$300,000
• Research Large Project Grant (LPG)$150,000
• Education Research Training Grant (ERG) - $100,000
• SAEMF Emerging Infectious Disease and Preparedness Grant - Up to $100,000
• SAEMF/ED Benchmarking Alliance Clinical Operations Research Grant$50,000
• SAEMF ARMED Pilot Grant - $25,000
• SAEMF ARMED MedEd Pilot Grant$25,000
• Education Project Grant (EPG)$20,000
• Geriatric Emergency Medicine Research Catalyst Grant, Supported by Michelle Blanda, MD - $10,000
• SAEMF/Clerkship Directors in Emergency Medicine (CDEM) Innovations in Undergraduate Emergency Medicine Education Grant - $5,000
• MTF/SAEMF Toxicology Research Grant - $20,000
• SAEMF/Academy of Emergency Ultrasound (AEUS) Research Grant$10,000
• SAEMF/Global Emergency Medicine Academy (GEMA) Research Pilot Grant - $10,000
• SAEMF/Academy for Women in Academic Emergency Medicine (AWAEM) Research Grant - $5,000
• SAEMF/Simulation Academy Novice Research Grant - $5,000
• SAEMF/Academy for Diversity and Inclusion in Emergency Medicine (ADIEM) Research Grant - $6,000
• SAEMF/Resident and Medical Students (RAMS) Research Grant - $2,500$5,000
Thanks to the visionary philanthropy of several of our longtime donors, RAMS now have two new opportunities that
will support their research and career development, and enhance the funding they receive from SAEMF:
• The Ali and Danielle Raja RAMS Medical Student Research Grant encourages more medical students from diverse backgrounds to pursue careers in academic emergency medicine research. See the RAMS Medical Student Research Grant Request for Applications for details.
• The David E. Wilcox, MD, FACEP Scholarship elevates funding for RAMS Resident and RAMS Medical Student Research Grants and recognizes excellence. Scholarships will be awarded to the highest scoring RAMS Resident Research Grant and RAMS Medical Student Research Grant recipients. See "What We Fund" for details.
Questions? Contact us at grants@saem.org or visit saemfoundation.org for detailed information.
SAEM Journals Announce the Appointment of Resident and Fellow




Corey Hazekamp, MD, Lincoln Emergency Medicine and Mehrnoosh Samaei, MD, Emory University School of Medicine, were selected to fill the resident editor positions on the editorial board of Academic Emergency Medicine (AEM).
continued on Page 92
Dr. Corey Hazekamp Dr. Mehrnoosh Samaeicontinued from Page 91
Neelou Tabatabai, DO, UNC Health Southeastern and Ivan Zvonar, MD, University of Washington, were selected to fill the fellow editor positions on the editorial board of Academic Emergency Medicine Education and Training (AEM E&T). Selected from competitive pools of applicants, these appointments will provide the chosen editors the opportunity to sit on an editorial board of a peer reviewed journal, while gaining valuable mentorship and hands-on experience in peer reviewing, editing, and journal publishing.
New Podcaster Opportunity Available Academic Emergency Medicine Education & Training (AEM E&T) has a new opportunity for an SAEM member who is interested in leading the journal’s podcasting program. AEM E&T podcasts feature informative interviews with academic emergency medicine’s leading medical education researchers. As the journal’s designated podcaster, you’ll be at the forefront of managing this program, including coordinating interviews and conducting insightful discussions. AEM E&T publishes six issues annually, with one article from each issue selected for a podcast interview. If you’re eager to contribute to the advancement of emergency medicine education through dynamic audio content, contact lgiblin@saem.org by Wednesday, May 8, 2024.
Check Out Our 2024 Lineup of RAMS Ask a Chair Podcasts!
These insightful interviews, hosted by Hamza Ijaz, MD, MPH, explores the career trajectories of several prominent EM chairs. Discover what steered them toward emergency medicine, explore the pivotal factors that helped them carve their career niche, and much more! To date, our 2024 podcasts feature the following individuals:
• Christopher McDowell, MD, MBA, MEd, Southern Illinois University School of Medicine
• Vicki Noble, MD, University Hospitals Cleveland Medical Center
• J. Jeremy Thomas, MD, MBA, University of Louisville
• Leigh A. Patterson, MD, MAEd, East Carolina University
• Sudave Mendiratta, MD, University of Tennessee Health Sciences Center College of Medicine
For a front-row seat to this enriching conversation and to stay connected with the ongoing discourse, simply navigate to the RAMS Ask a Chair webpage!
Free Live and Recorded Webinars for Your “Must Watch” List
SAEM offers live and recorded webinars covering a variety of emergency medicine topics, providing an excellent opportunity to stay current and learn from your colleagues. All webinars, both live and recorded, are free for SAEM members. Navigate to our SAEM Webinars page and select a few to add to your “must watch” list.
Research Learning Series: An Invaluable Resource for Novice and Mid-Career Researchers
The SAEM Research Learning Series (RLS) provides a wealth of educational resources tailored for budding and midcareer researchers. Through recorded lectures, panel discussions, and podcasts leading experts in the field of emergency research present invaluable insights to elevate your research skills. Explore our RLS website to access past recordings. Nurturing Diversity, Equity, and Inclusion in EM: The SAEM DEI Resource Library
Explore the SAEM DEI Resource Library, a free online repository fostering diversity, equity, and inclusion (DEI) in emergency medicine. Open to all SAEM members, this resource covers eight vital DEI topics, including discrimination history, patient care disparities, and faculty diversity. Members can access articles, books, videos, and more. All are encouraged to participate in the ongoing growth of this dynamic repository by contributing valuable resources. Whether planning a
journal club or seeking DEI insights, the library offers a wealth of information. Read all about this valuable member benefit in the Mar-Apr issue of SAEM Pulse!
the
The Academy for Women in Academic Emergency Medicine (AWAEM) Toolkit is a digital guide designed to empower women navigating the complexities of academic emergency medicine. This essential resource spans professional development, mentoring, promotion, recruitment/support, grant writing, scholarship development, wellness, and gender-specific needs. Beyond a mere guide, it serves as a compass, providing insights and strategies to overcome challenges and seize opportunities. Whether addressing gender-specific needs or fostering wellness, the AWAEM Toolkit is a roadmap for success in academic emergency medicine.
Our four speakers bureaus offer highquality presentations on timely topics relevant to the practice of academic emergency medicine. Top-tier speakers cover important subjects and provide cutting-edge information and insights on a wide variety of important subjects. Book your speaker today!
• ADIEM Advisory Council on Equity, Diversity and Inclusion Team
• AACEM Faculty Lectures Speakers Bureau
• AWAEM Speakers Bureau
• Palliative Medicine Speakers Bureau
SAEM’s Global Emergency Medicine Academy (GEMA) focuses on improving the global delivery of emergency care through research, education, and mentorship. GEMA provides resources for students, residents, fellows, and others interested in global health careers, including:
• Trainee Info • Short Courses
• Resource Library • Research
• Books • Travel Tips
• And More!

On March 7 and 8, the University of Southern California Keck School of Medicine (KSOM) Department of Emergency Medicine hosted the 2024 SAEM Western Regional Meeting in Long Beach, California. For more than 20 years, this conference has alternated its location among universities in the western region. However, due to the pandemic’s impact on emergency medicine, hosting the conference lost its priority status for many departments.
The KSOM Department of Emergency Medicine took on the initiative to revitalize the conference, drawing over 230 registered attendees from across the Western Region. The two-day conference featured a wide range of sessions, including moderated research abstract presentations, breakout sessions focusing on five subspecialty areas, a new speakers competition, and an audienceinteractive case presentation competition known as EM Elucidation. Additionally, networking opportunities were abundant, allowing attendees from participating institutions to connect and collaborate.
The event kicked off with a compelling keynote address by Dr. Garen Wintemute of UC Davis, highlighting the impactful work of the Violence Prevention Research Program and the California Firearm Violence Research Center. This was followed by a presentation from the LA County Hospital Based Violence Intervention Program, featuring community-engaged researchers Dr. Todd Schneberk (USC) and Dr. Shamsher Samra (Harbor UCLA Medical Center), along with representatives from Soledad Enrichment Action, a key partner in the project.
In the New Speakers Forum, Dr. Robert Ray, Jr., Toxicology Fellow at UC Davis, captured the audience with his presentation titled “Good Kids Maad Honey.” The EM Elucidation case competition saw the team from UCLA-Harbor, led by Dr. Jonathan Warren, MD, clinching the award for Best Case Elucidation, while Dr. Steven Johnson of the University of Southern California secured the title for Best Case Presentation.
Nearly 100 studies were presented across a plenary abstract session and ten moderated abstract sessions. Among these, Zachary Reichert, MD, an incoming research fellow at the University of Southern California Department of Emergency Medicine, stood out, winning Best Plenary Abstract for his study on EMTALA Violations Related to On-Call Responsibilities, a comprehensive review spanning from 2011 to 2023.
The event also featured five breakout sessions offering deep dives into academic emergency medicine topics such as operational research, educational scholarship, social determinants of health in the emergency department, the interface of critical care and emergency medicine, and emergency medical services and pediatrics.
With the highest attendance record to date, this Western Regional Conference marked a significant milestone. Looking ahead, UC Irvine has enthusiastically taken up the baton and will host the conference in 2025, ensuring the continuation of this valuable tradition.
Submitted by Elizabeth Burner, MD, MPH, PhD, on behalf of the SAEM Western Regional Meeting Committee










SAEM leaders, L to R, top row: Michelle D. Lall, MD, MHS; Jody A. Vogel, MD, MSc, MSW; Wendy C. Coates, MD; Pooja Agrawal, MD, MPH; Jeffrey P. Druck, MD; Julianna J. Jung, MD; L to R, bottom row: Ryan LaFollette, MD; Nicholas M. Mohr, MD, MS; Ava E. Pierce, MD; Lewis S. Nelson, MD, MBA; Daniel N. Jourdan, MD, NRP
SAEM Board of Directors
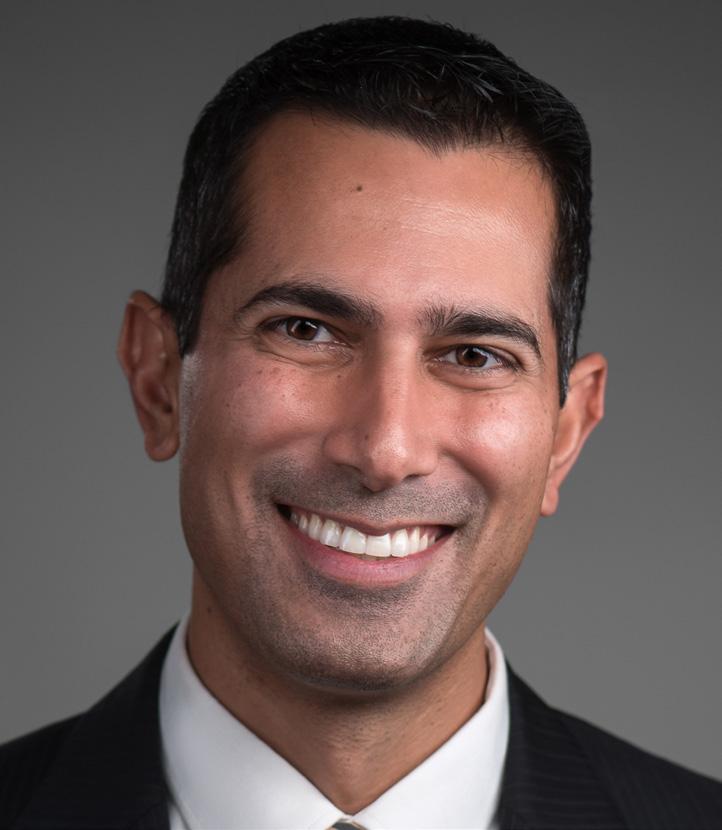
President
Ali S. Raja, MD, DBA, MPH
Massachusetts General Hospital/Harvard
President-Elect
Michelle D. Lall, MD, MHS Emory University
Secretary-Treasurer
Jody A. Vogel, MD, MSc, MSW
Stanford University Department of Emergency Medicine
Immediate Past President
Wendy C. Coates, MD
Los Angeles County Harbor-UCLA Medical Center
Members-at-Large
Pooja Agrawal, MD, MPH
Yale University School of Medicine
Jeffrey Druck, MD
University of Utah School of Medicine
Julianna J. Jung, MD
Johns Hopkins University School of Medicine
Ryan LaFollette, MD
University of Cincinnati Medical Center/ College of Medicine
Nicholas M. Mohr, MD, MS University of Iowa
Ava E. Pierce, MD
UT Southwestern Medical Center, Dallas
Chair Member
Lewis S. Nelson, MD, MBA
Rutgers New Jersey Medical School
Resident Member
Daniel N. Jourdan, MD, NRP
Henry Ford Hospital
SAEM Nominating Committee
Michelle D. Lall, MD, MHS
(Chair, SAEM President-Elect)
Emory University
Wendy C. Coates, MD
(SAEM Immediate Past President)
Los Angeles County Harbor-UCLA Medical Center
Al'ai Alvarez, MD
Stanford Emergency Medicine
Angela Jarman, MD, MPH
University of California, Davis
SAEM Bylaws Committee
Ronny Otero, MD, MSHA (Chair) Medical College of Wisconsin
Peter Hou, MD
Brigham and Women's Hospital
Michael Gottlieb, MD
Rush University Medical Center
AACEM Executive Committee

Jane H. Brice, MD, MPH
President
Jane H. Brice, MD, MPH
University of North Carolina at Chapel Hill School of Medicine
Ali S. Raja, MD, DBA, MPHPresident-Elect
Ian B.K. Martin, MD, MBA
Medical College of Wisconsin
Secretary-Treasurer
Mary E. Tanski, MD, MBA
Oregon Health & Science University
Immediate Past President
Lewis S. Nelson, MD, MBA
Rutgers New Jersey Medical School
Members-at-Large:
Susan B. Promes, MD, MBA
Penn State
Andra L. Blomkalns, MD, MBA
Stanford Department of Emergency Medicine

Emily (Ly) Cloessner, MD, MSPH
President
Emily (Ly) Cloessner, MD, MSPH
Washington University in St Louis
Secretary-Treasurer
Daniel Jose Artiga, MD
University of Cincinnati College of Medicine
Immediate Past President
Daniel N. Jourdan, MD, NRP
Henry Ford Hospital
Members-at-Large
Alison Bonner, MD
New York Presbyterian- Cornell/Columbia
Aaron D'Amore, MD
Harvard Affiliated Emergency Medicine
Residency - Mass General Brigham
John Dickens, MD, MBA
Northwestern Memorial Hospital/McGaw Medical Center
Lauren Diercks
UT Southwestern Medical Center, Dallas
Hart L. Edmonson, MD
Northwestern University
Juliet Jacobson, MD
New York Presbyterian- Cornell/ Columbia
Mit Patel, MD
Henry Ford Hospital
Genevieve Pentecost, MD (she/her/hers) Washington University in St. Louis/ Barnes-Jewish Hospital
Medical Student Representatives
Stephanie Balint Quinnipiac University
Sara Schulwolf
University of Connecticut
SAEM Foundation Board of Trustees

J. Scott VanEpps, MD, PhD
President
J. Scott VanEpps, MD, PhD University of Michigan
President-Elect
Zachary F. Meisel, MD, MPH, MSHP University of Pennsylvania
Secretary-Treasurer
Jamie J. McCarthy, MD, MHA
Memorial Hermann Health System
Immediate Past President
Manish N. Shah, MD, MPH
University of Wisconsin School of Medicine and Public Health
Members-at-Large
Michelle Blanda, MD
Northeast Ohio Medical University/ Western Reserve Hospital
Charles B. Cairns, MD
Drexel University College of Medicine
Christopher R. Carpenter, MD, MSc
Mayo Clinic & Mayo Clinic Health System
Cherri D. Hobgood, MD University of North Carolina Hospitals
Paul I. Musey, Jr., MD, MS Indiana University
Robert W. Neumar, MD, PhD University of Michigan
Susan B. Promes, MD, MBA Penn State
Niels K. Rathlev, MD University of Massachusetts Chan Medical School - Baystate
Neha Raukar, MD, MS
Mayo Clinic & Mayo Clinic Health System
SAEM Grants Committee Chair
Elizabeth Burner, MD, MPH
University of Southern California/LA General Hospital Medical Center
SAEM Finance Committee Chair
Marquita S. Norman, MD, MBA
UT Southwestern Medical Center, Dallas
SAEM President
Ali S. Raja, MD, DBA, MPH
Massachusetts General Hospital/Harvard
SAEM President-Elect
Michelle D. Lall, MD, MHS
Emory University
SAEM Secretary-Treasurer
Jody A. Vogel, MD, MSc, MSW
Stanford University Department of Emergency Medicine
SAEM Immediate Past President
Wendy C. Coates, MD
Los Angeles County Harbor-UCLA Medical Center
Turn to these pages in the next issue of SAEM Pulse for the full slate of 2024-2025 leadership for SAEM’s Academies!
Academy of Women in Academic Emergency Medicine
Girls Just Want to Have Fun(ding): A Mentored Writing Initiative for Early Career Women
Researchers
Over the last two decades, National Institutes of Health (NIH) funding for emergency medicine (EM) research has shown growth and launched impressive resources, such as the Office of Emergency Care Research. However, EM researchers are still only awarded 1.5% of total NIH spending. The percentage of NIH-funded female EM researchers is even more limited, with only 23% of NIH-funded EM researchers identifying as female. Career development awards are a competitive funding mechanism to support junior researchers to gain research skills, mentorship, and preliminary data in preparation for an R01. These mentored career development awards are referred to as “K-awards” (e.g., K08, K23) while R-awards (e.g., R01) are independent research awards. In December 2023, the Academy for Women in Academic Emergency Medicine (AWAEM) research committee launched “K Club,” a research mentorship small group to assist AWAEM junior researchers with their career development award applications.
NIH Funding in Emergency Medicine
A recent assessment of NIH funding from 2010-2017 showed only 1.7% of total NIH funded grants were directed by an EM primary investigator, and only 1.5% of total NIH dollars support EM research studies Career development awards sponsored by the NIH or other emergency medicine foundations, including SAEM, offer junior researchers the opportunity to gain research training, dedicated mentorship, and preliminary data in preparation for an R01 independent award. K-series submissions are not common in EM: only 16% of total EM NIHfunded awards were K23 awards, while 29% were R01 awards2
A recent study of career development award applicants in EM cited lack of mentorship, time management and lack of administrative support as the three biggest barriers to K award submission
Female investigators remain underrepresented in NIH EM research. While data shows increasing representation of females in career development awards, female EM researchers are still globally underrepresented in NIH funding. Past analyses of gender differences among NIH-funded researchers in EM have called for improved attention and support towards female EM researchers, especially in transitioning from mentored to independently funded NIH awards.
The AWAEM research committee supports research focused on assessing and improving gender equity in emergency medicine, and the career development of researchers within AWAEM. The research committee offers AWAEM members research consultative services, monthly works-in-progress meetings, cross-institutional collaborative research partners, and small grant funding support. Discussions within the research
committee during monthly meetings and SAEM’s annual meeting revealed a gap in mentoring support to AWAEM junior investigators intending to submit career development award applications.
What is AWAEM K Club?
AWAEM K Club is a mentorship meeting to support AWAEM members preparing career development awards for NIH or foundation funding. Mentees and mentors are self-identified through AWAEM email list-serve and submit data on their award type and planned submission date using a Google form. Meetings are held three times per year, approximately two months prior to NIH K08/K23 application submission dates.
Mentors and mentees are divided into small groups for each session; groups contain 2-3 mentees and 2-3 mentors. Meetings allow AWAEM mentees to present a written component of their career development award, including Specific Aims or Career Development Plan, for feedback from peers and mentors. AWAEM members who are also in the precontemplative stages of a research career or career development award are also invited to attend sessions to listen and learn about EM research careers. Mentors and co-mentees may offer writing critiques, suggestions for research or training strategy, apparent training gaps, or connections to new mentors or consultants. Mentors may also offer to provide feedback and editing on documents outside of the formal meeting time or meet for additional sessions to help support an applicant. To date, AWAEM K Club has supported 10 AWAEM mentees during two meetings sessions with the support of six AWAEM research mentors.
The primary goal of AWAEM K Club is to foster mentored writing groups for career development applicants and address one of the primary barriers to K award submission for early career researchers in EM. Additionally, we are excited for other potential outcomes that may arise in relation to AWAEM K Club, including new research collaborations and a sustained pipeline of junior investigators and senior research mentors within AWAEM. We plan to obtain formative feedback from applicants and mentors to meet varying participant needs throughout the year. Future initiatives may include expansion to support midcareer AWAEM researchers transitioning from K to R awards and integrated instructional sessions on writing different grant components.
For more information about the AWAEM research committee and AWAEM K-Club, email us at awaemres@saem.org
• NIH Grants & Funding: How to Apply-Application Guide
• Writing An Effective “K” Application: A Video Guide
• Examples of Successful Grants
• SAEM Research Learning Series
Submitted by Jennifer S. Love, MD, MSCR; Michelle P. Lin, MD, MPH, MS; Danielle M. McCarthy, MD, MS; Elizabeth Schoenfeld, MD, MS; Catherine A. Staton, MD, MScGH; and Maggie Samuels-Kalow, MD, MPhil, MHSP, on behalf of the Academy for Women in Academic Emergency Medicine
Association of Academic Chairs of Emergency Medicine/Academy of Administrators in Academic Emergency Medicine
The 16th Annual AACEM/AAAEM Retreat, held in sunny Puerto Rico in March 2024 was hosted by the Association of Academic Chairs of Emergency Medicine (AACEM) and SAEM’s Academy of Administrators in Academic Emergency Medicine (AAAEM). This event stands as a pivotal event in academic emergency medicine (EM) leadership and administration. Attended by chairs, vice chairs, and administrators of academic departments of emergency medicine, this retreat gathered over 200 distinguished leaders dedicated to advancing the field of academic EM.
Leading Across Generations
The conference led off with an energetic keynote by Megan W. Gerhardt, Ph.D., professor of management and leadership at the Farmer School of Business at Miami University. Her work focuses on understanding and cultivating the concept of generational intelligence (aka “Gentelligence”). Dr. Gerhardt offered practical insights and strategies for individuals and organizations to develop intergenerational teams and leverage generational diversity in the workplace with self-awareness, empathy, and effective communication.
Fostering Connections
Central to the success of the retreat was the opportunity it provided for attendees to cultivate meaningful connections and establish collaborative partnerships. From departmental leaders to administrators, participants engaged in vibrant discussions, exchanged ideas, and forged valuable relationships. The networking opportunities were instrumental in fostering a sense of community and collaboration among attendees.
Enriching Professional Development
The program schedule offered an array of educational sessions, workshops, and interactive discussions tailored to the needs of academic EM leaders. With a focus on strategic leadership, financial management, operational efficiency, and faculty development, the retreat provided attendees with practical insights and strategies to navigate the complexities of academic EM. Renowned experts and thought leaders shared their perspectives, stimulating thought-provoking conversations and equipping participants with the tools needed to excel in their roles.
The retreat served as a forum for candid conversations about the challenges and opportunities facing academic EM departments. Topics such as workforce development, optimizing residency training programs, fostering diversity and inclusion, and adapting to evolving health care delivery models were explored. Through collaborative problem-solving and knowledge sharing, attendees gained valuable insights into addressing these complex issues and driving positive change within their institutions.
Amidst the enriching atmosphere of the AACEM/AAAEM Retreat, notable leaders were celebrated and honored for
their exemplary contributions to the field of academic EM administration. These awards serve as a testament to their dedication, innovation, and outstanding leadership.

The AACEM Distinguished Service Award was bestowed upon David P. Sklar, MD, an esteemed emergency physician and professor at Arizona State University. Dr. Sklar also serves as the director of the Office of Interprofessional Continuing Health Education. His unwavering commitment to advancing EM education and his profound impact on interprofessional collaboration have earned him this prestigious AACEM accolade.

The AACEM Lifetime Service Award was presented to Gregory A. Volturo, MD, chair of the Department of Emergency Medicine at the UMass Chan Medical School. Dr. Volturo also serves as the service line chief for emergency medicine for the Umass Memorial Health Care System. Throughout his distinguished career, Dr. Volturo has demonstrated exemplary leadership and dedication to advancing EM practice and administration, including as a past president of AACEM.

The AAAEM James J. Scheulen Lifetime Achievement Award in Academic Emergency Medicine Administration was conferred upon Travis W. Schmitz, PhD, MBA. Dr. Schmitz serves as the department administrator for emergency medicine at Northwestern Memorial HealthCare and Northwestern University’s Feinberg School of Medicine. Additionally, he holds the position of director of operations for the Office of the Chief Medical Officer for the 11-hospital health care system. Dr. Schmitz’s outstanding contributions to health care administration and his commitment to excellence have left an indelible mark on the field of academic EM.
These distinguished individuals exemplify the highest standards of leadership, innovation, and service in academic emergency medicine. Their dedication and contributions inspire others to strive for excellence and drive positive change within the field. We applaud their achievements and express our gratitude for their continued commitment to advancing the mission of academic EM.
As the AACEM Executive Committee contemplates the success of this year’s retreat, we are reminded of the profound impact of collaborative efforts in shaping the future of academic EM administration. We are committed to further advancing academic EM through innovation and supporting departmental leaders and administrators nationwide.
Submitted by Ian B. K. Martin, MD, MBA, Jane H. Brice MD, MPH, Richard J Hamilton, MD, MBA, Mary E. Tanski, MD, MBA, Lewis S. Nelson, MD, MBA, and Susan B. Promes, MD, MBA on behalf of AACEM.
SAEM Reports continued on Page 98
Dr. Gregory A. Volturo Dr. Travis W. Schmitzcontinued from Page 97
Bridging Passions:
As a Brazilian medical student who dreams about pursuing emergency medicine in the United States, I am no stranger to sitting alone by airport gates. However, as I waited for my flight home after completing my geriatric emergency medicine rotation at the University of North Carolina, the experience felt entirely different.
Emergency medicine has always been my specialty of choice and the reason behind my pursuit of medical education. At my medical school, geriatrics is a core rotation in our curriculum, and it was during this rotation that I fell in love with the distinct aspects of caring for older adults. Imagine my delight when I discovered I could combine my passion for emergency medicine with my interest in geriatrics!
Seeking to gain further hands-on experience in this area, I applied for the Academy of Geriatric Emergency Medicine's Geriatric Away Rotation Scholarship in June, unaware of how it would shape my trajectory.
From the outset, I was awestruck. Chapel Hill proved to be an incredible, lively town, teeming with collegiate energy, sporting events, and excellent restaurants. Moreover, the faculty and residents extended warm hospitality, ensuring that I learned as much as possible during shifts and conferences and actively involving me as a team member.
Over the course of four weeks, I had the opportunity to complete ED shifts at two campuses: the UNC Main and Hillsborough. Additionally, three days a week were dedicated to accompanying Dr. Lindsay Wilson to various senior care settings, including geriatric clinics, independent living, and assisted living facilities. This exposure allowed me to experience a diverse patient profile with a mix of complexities, provided access to a range of resources, and allowed me to tailor my approach to patient care based on the specific needs of each individual.
With plenty of space to dive deeply into geriatric emergency medicine, I had the opportunity to manage my own patients and formulate treatment plans, under the watchful guidance
of my preceptors, who steered me according to my level of training. This experiential learning was significantly different from the medical education model in Brazil, providing an invaluable opportunity to exercise my geriatric clinical thinking. Furthermore, close patient interaction allowed me to experience first-hand how thankful and appreciation older patients can be, even for seemingly small gestures like providing instructions and reassurance. Some of these stories I will treasure for the rest of my career.
Without question, this rotation presented an invaluable learning experience and the chance of a lifetime to network within the field of geriatric emergency medicine. Through classes, shifts, and mentorships with several members of the UNC faculty, I not only deepened my understanding but also became involved in additional projects, fostering enduring professional relationships.
In summary, this rotation stood out as the highlight of my medical school experience, and I am immensely grateful to AGEM for the opportunity. It allowed me to explore geriatric emergency medicine, nurturing my passion, meeting remarkable individuals, and planting seeds for future projects.
Submitted by Carolina Diniz Hooper a medical student in her final year at Faculdade Ciências Médicas de Minas Gerais, Brazil interested in applying for emergency medicine training in the United States. She was 2023 recipient of the AGEM Geriatric EM Away Rotation Scholarship.


The Society for Academic Emergency Medicine (SAEM) and the American College of Emergency Physicians (ACEP) are members of The Medical Society Consortium on Climate and Health (MSCCH), which collaborates with over 100 medical societies and allied health groups nationwide in pursuit of a healthy, safe, and just world. Liaisons from SAEM, along with members of the SAEM Climate Change and Health Interest Group, participated in the Consortium’s 2024 Annual Meeting held in February in Washington, DC. Emergency physicians and trainees from across the country gathered to share research and educational innovations aimed at driving high-quality patient care.
To kick off the conference, the American Lung Association presented of its annual “State of the Air” report, providing attendees with insights into air quality rankings across various cities. (See where your city ranks.) Additionally, experts also shared strategies for communicating with patients regarding climate change and provided specialty-specific guidance on addressing heat-related issues, with a particular emphasis on vulnerable populations. Emphasis was placed on engaging youth in climate action and promoting mental well-being. Julia Olson, executive director and chief legal counsel of Our Children’s Trust, highlighted the scientific basis and data behind the recent Held v. Montana lawsuit, while indigenous health and climate change leaders shared their efforts to protect and honor their communities’ lands, values, and people. Environmental justice discussions encompassed the integration of individuals with disabilities into emergency preparedness efforts. Additionally, a research “hot topics” session highlighted emerging evidence and health solutions across specialties focusing on mitigation, adaptation, and resilience. A complete list of topics and other resources from the annual meeting can be found here
As part of the traditional conference format, a voluntary Hill Day provided health care professionals with the opportunity to engage with legislators and staffers interested in climate change and health. Dr. Gayle Kouklis, an SAEM member, reflected on her experience, emphasizing the importance of advocating for patients affected by fossil fuel pollution and climate-related disasters:
“I attended the recent MSCCH Annual Meeting for the first time. In partnership with the American Lung Association and
George Mason University, we reviewed best practices for talking to Congressional staffers and legislators. Armed with the briefings and my scribbled notes, we approached the Hill on a rainy Tuesday to meet with, educate, and build relationships with state senators and representatives. Our focus was simple: to improve health and advance equity using science and our clinical experiences. We were able to share stories of how our communities have been harmed by climate-related exposures and why reducing air pollution and heat stress is important to protecting the health of their constituents. We discussed the new soot standard, which uses science to reduce the acceptable standard of pollution, saving thousands of lives annually and keeping patients out of busy hospitals. It was clear to me why physicians belong at the bedside, on the Hill, and in the climate change space.

“I encountered individuals who questioned the relevance of a physician’s involvement. They wondered, “What does a physician have to say about air quality standards?” However, throughout history, physicians have consistently found themselves in unexpected advocacy roles, whether it be in the realms of tobacco control or gun regulation. In these instances, physicians bring objective experiences with patients supported by research, which are pivotal in shaping policies. Climate change and environmental exposures are no exception to this rule. The lived experiences of individuals affected by these issues represent direct, unbiased effects of policy decisions. Research repeatedly shows that physicians are trusted voices, especially when addressing climate change, and this trust transcends all aspects of the political spectrum. Just as we care deeply about the impact of different decisions on our patients’ health, legislators are equally invested in the well-being of their
Reports continued on Page 100
continued from Page 99
constituents. As physicians, we advocate with the best interests of both our patients and constituents at heart. Consequently, our voices are valued by many policymakers on Capitol Hill.
“During these meetings, staffers demonstrated genuine interest by asking thoughtful questions about how the proposed standards were relevant to health. They quickly grasped the significance of the concepts discussed, with one even involving a transportation staffer in the conversation, facilitating interdisciplinary discussion on the health implications of vehicle emissions. As a physician, I felt seen as an expert in health matters, and as an emergency medicine EM physician, I felt right at home learning the language of staffers from various subspecialties. One health staffer, in particular, had expertise in emergency department boarding and asked about my experiences in my workplace. This exchange led to further conversations about disaster preparedness, especially in light of the increasing wildfires and extreme heat events in the Northwest.
“I started the week feeling intimidated by a new and unfamiliar environment. However, I left with a sense of fulfillment, knowing that I had engaged in meaningful discussions with policymakers on the Hill whose decisions will impact my patients directly and indirectly. I felt welcomed, and after returning home, continued to build relationships with health staffers, offering additional data and insights on climate and health-related issues. While nothing can replace the connection formed at the bedside, stepping outside my comfort zone to advocate for my patients makes each patient encounter that much more powerful.”
Submitted by Gayle Kouklis, MD, co-lead of the SAEM Climate Change and Health Interest Group; Tara Benesch, MD, MS; and Caitlin Rublee, MD, MPH, liaison to The Medical Society Consortium on Climate and Health for SAEM, serving as vice chair of the steering committee.
Read
• RAMS Climate Change and Health Roadmap
• National Academy of Medicine Carbon Accounting 101
• Sustainable Healthcare Certification through the Joint Commission
• CDC: Climate Effects on Health
• Climate Change and EM: A 10-day Intensive, Open Access Curriculum
• U.S. Dept. of HHS: Catalytic Program on Utilizing the Inflation Reduction Act Funds
• AMA Medical Legislation Advocacy
• American College of Physicians Advocacy Resources
Academic Emergency Medicine Pharmacists
Introducing AEMP: Shaping the Future of the Academic EM Pharmacy Community
AEMP, the Association of Emergency Medicine Pharmacists, emerged as an integral interest group within SAEM following a successful collaboration between SAEM and a cohort of EM pharmacists who orchestrated an EM pharmacy-centric, one-day
conference during SAEM23 in Austin, Texas. Rooted in a shared desire to advance EM pharmacy practice, AEMP aims to foster leadership, research, and multidisciplinary collaboration in the field. Prior to AEMP’s formation, EM pharmacists primarily found professional homes within pharmacy organizations, with limited opportunities for national-level collaboration. Recognizing the pivotal role of pharmacists as integral members of the bedside team, AEMP leaders hope to expand collaboration opportunities on a broader scale, facilitating networking, research endeavors, and knowledge exchange among pharmacists and healthcare providers alike.
AEMP has formed a steering committee along with four additional inaugural committees that are responsible for the following:
Steering Committee: This committee is responsible for providing guidance, direction, and decision-making oversight for AEMP. Its principal responsibilities include crafting a strategic plan and objectives, allocating resources effectively, and maintaining alignment with the member-focused goals of AEMP.
Career Development Committee: This committee is responsible for creating and curating resources to support EM pharmacists throughout their professional careers. For instance, this committee is currently developing materials that can be used locally to justify the introduction or expansion of EM pharmacy services.
Communications Committee: This committee focuses on generating online content, maintaining social media presence, and developing an AEMP Newsletter. Additionally, they facilitate future contributions to PULSE, an avenue for sharing insights and updates within the field.
Membership Committee: This committee ensures that the evolving needs of AEMP members are met through analyses of membership statistics, administering surveys, and tracking trends. Moreover, they identify potential new members and develop strategies for recruitment and retention to sustain and grow the AEMP community.
Programming Committee: This committee is responsible for designing the AEMP Conference for SAEM24 and for contributing to the development of EM pharmacy-related sessions and activities at the SAEM annual meeting.
Looking ahead, AEMP aspires to transition from an interest group into an SAEM academy, in hopes of deepening collaboration across EM disciplines and integrating pharmacists into a national multidisciplinary framework reflective of clinical practice. Keep updated on AEMP’s journey and growth through our X/Twitter account @SAEM_AEMP.
Finally, AEMP is extremely grateful to its inaugural leaders for their unwavering dedication to our collective success. Join us in shaping the future of EM pharmacy practice — share your ideas and get involved!
Submitted by Lisa Hayes, PharmD, AEMP communications chair, on behalf of the AEMP Interest Group.

Saadia Akhtar, MD, has been promoted to senior associate dean for trainee well-being in graduate medical education (GME) at the Icahn School of Medicine at Mount Sinai, within the Office of Well-being and Resilience and the Office of Graduate Medical Education. In this role, Dr. Akhtar oversees initiatives to advance the well-being of approximately 2,500 residents and clinical fellows. Dr. Akhtar previously served as the director of the Emergency Medicine Residency Program at Mount Sinai Beth Israel. Dr. Akhtar is a former president of the Council of Residency Directors in Emergency Medicine (CORD) and an oral board examiner for the American Board of Emergency Medicine. She is the recipient of numerous awards, including the prestigious ACGME Parker J. Palmer Courage to Teach Award for Program Director Excellence.

Rebecca Cunningham, MD, was unanimously selected by the University of Minnesota Board of Regents as the university's 18th president. Her inauguration will take place on July 1, 2024.
Dr. Cunningham currently serves as the vice president for research and innovation at the University of Michigan (U-M) and holds the William G. Barsan Collegiate Professorship in Emergency Medicine. She is also a professor of emergency medicine in the U-M Medical School as well professor of health behavior and health education in the U-M School of Public Health.
Dr. Cunningham was a featured keynote speaker at SAEM19 in Las Vegas and is the recipient of both the 2019 SAEM Excellence in Research Award and the 2019 American College of Emergency Physicians (ACEP) Outstanding Contribution in Research Award.

Erick A. Eiting, MD, MPH, has been promoted to professor of emergency medicine at the Icahn School of Medicine at Mount Sinai. Additionally, he holds the role of vice chair of operations for emergency medicine at Mount Sinai Downtown, overseeing operations at the Emergency Department at Mount Sinai Beth Israel and the Urgent Care Center at Mount Sinai Union Square in New York City. Additionally, Dr. Eiting serves as director of the LGBTQ+ Medicine Fellowship Program.

Charles (Chuck) J. Gerardo, MD, has been named the chair of the Department of Emergency Medicine at Duke University School of Medicine. Dr. Gerardo has served as interim chair since July 2022, when the former Division of Emergency Medicine in the Department of Surgery was elevated to department status. He previously served as chief of the division. Gerardo joined Duke’s faculty in 2000. During his time at Duke, he has served in multiple leadership roles including director of undergraduate medical education, director of the Emergency Medicine Global Health Program, and vice chief of clinical operations.

Christopher McDowell, MD, MBA, MEd, is the new executive associate dean of the Southern Illiniois University (SIU) School of Medicine. He also serves as associate professor and department chair of emergency medicine and the medical director for the Memorial Learning Center. In addition, Dr. McDowell has oversight of the Office of Correctional Medicine, the educational function of the Office of Telehealth, the Office of Rural Health and Social Service Development, the Office of Community Care, and the development of the SIU System’s Institute for Rural Health.
The University of South Florida (USF) Morsani College of Medicine is pleased to announce a significant development: the transition of its Division of Emergency Medicine into a Department of Emergency Medicine, effective immediately. Previously, USF's emergency medicine operations were part of Tampa General Hospital's department and were also housed within the USF Health Department of Internal Medicine as a division. This transition grants USF Emergency Medicine independent status, bringing it in line with the organizational structure and faculty standards of other respected academic medical centers.
The role played by SAEM’s Consultation Services was crucial in facilitating this transition. Their assistance and support to the proposal team were instrumental in navigating the complexities of this process.
“This serves as an excellent example of SAEM/AACEM resources working to support the growth of academic emergency medicine,” remarked Jason W. Wilson, MD, PhD, who, with this announcement, transitions from the role of chief to chair of the department.
Dr. Saadia Akhtar Dr. Christopher McDowell Dr. Erick A. Eiting Dr. Charles J. GerardoAccepting ads for our “Now Hiring” section!
Deadline for the next issue of SAEM Pulse is June 1.
For specs and pricing, visit the SAEM Pulse advertising webpage.



The University of California San Francisco, Department of Emergency Medicine is recruiting for a full-time faculty member at the Associate Professor or Professor level to serve as the Director of Quality Improvement at our UCSF Hellen Diller Medical Center at Parnassus Heights campus. We seek individuals who meet the following criteria: emergency medicine faculty with a track record of successfully developing and maintaining rigorous, data-driven quality and safety programs, establishing a culture of safety, improving the identification and review of cases, and ultimately, optimizing the quality of patient care. Rank, step and series will be commensurate with qualifications.
The Department of Emergency Medicine provides comprehensive emergency services to a large local and referral population at multiple academic hospitals across the San Francisco Bay Area, including UCSF Hellen Diller Medical Center, Zuckerberg San Francisco General Hospital and Trauma Center, and the UCSF Benioff Children’s Hospitals in San Francsico and Oakland. The Department of Emergency Medicine hosts a fully accredited 4-year Emergency Medicine residency program and multiple fellowship programs. There are opportunities for leadership and growth within the Department and UCSF School of Medicine.
Board certification in Emergency Medicine is required. All applicants should excel in bedside teaching and have a strong ethic of service to their patients and profession.
The University of California, San Francisco (UCSF) is one of the nation’s top five medical schools and demonstrates excellence in basic science and clinical research, global health sciences, policy, advocacy, and medical education scholarship. The San Francisco Bay Area is well-known for its great food, mild climate, beautiful scenery, vibrant cultural environment, and its outdoor recreational activities.
PLEASE APPLY ONLINE AT: https://aprecruit.ucsf.edu/apply/JPF05030
Applicants’ materials must list current and/or pending qualifications upon submission. The posted UC salary scales set the minimum pay determined by rank and step at appointment. See [Table 5] (https://www.ucop.edu/academic-personnel-programs/_files/2023-24/oct-2023-acad-salary-scales/t5-summary.pdf). The minimum base salary range for this position is $177,100-$377,200. This position includes membership in the [health sciences compensation plan] (https://ucop.edu/academic-personnelprograms/_files/apm/apm-670.pdf) which provides for eligibility for additional compensation.
UCSF seeks candidates whose experience, teaching, research, and community service has prepared them to contribute to our commitment to diversity and excellence. UCSF is an Equal Opportunity/Affirmative Action Employer. The University undertakes affirmative action to assure equal employment opportunity for underrepresented minorities and women, for persons with disabilities, and for covered veterans. All qualified applicants are encouraged to apply, including minorities and women. For additional information, please visit our website at http://emergency.ucsf.edu/










Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pa.




The Department of Emergency Medicine at the Boston University Chobanian & Avedisian School of Medicine and Boston Medical Center (BMC) is recruiting fellowship candidates in: Addiction Medicine Emergency Department Administration Emergency Medical Services (EMS) Emergency Ultrasound (EUS)
Global Health Equity Local Health Equity Neurocritical Care (NCC)
We offer 1- and 2-year fellowship training opportunities for graduates of accredited Emergency Medicine Residency Programs. We train up to 6-8 fellows per year in a collaborative and nurturing community of practice, with support from orientation to graduation through the Fellowship Academy.
BMC Emergency Medicine provides exceptional training in the care of critically ill/injured patients, point-of-care ultrasound, prehospital & EMS, public health, social EM, and research. BMC is the safety-net hospital for the city of Boston, serving a diverse, multicultural population in a county-type practice environment, within a world-renowned tertiary hospital system.
Applications are being accepted now, please send your letter of interest to BMCFellowships@bmc.org for further instruction. EUS applicants, please visit eusfellowships.com for complete program description and to submit your application materials.
At BMC we welcome and support those who have faced barriers to practicing medicine, specifically those who identify as underrepresented In medicine, whether defined on the basis of race, ethnicity, socioeconomic status, gender, sexual orientation, physical ability, religion, first generation in higher education, or otherwise. In 2023, the Lown Institute ranked Boston Medical Center 1st in the nation for racial inclusivity.
BMC EMERGENCY DEPARTMENT
• Largest and busiest provider of Level 1 trauma and emergency services in the New England
• 130,000 annual patient visits
• 4-year EM Residency Program
• Provides medical control and oversight for Boston EMS
• Interpreter services for more than 150 languages
• 22% of residents are URM (national average is 11%)

BMC ED PATIENT DEMOGRAPHICS
• 70% Black or Hispanic
• 32% do NOT speak English as their primary language
• >50% have annual household income <$20,400
• Black or African American: 24.4%
• Hispanic or Latino of any race: 17.5%
• Native American: 0.4%
• Asian: 8.9%
EM clinicians work closely with the Departments of Surgery, Pediatrics, Neurology, and Geriatrics, the Boston University School of Public Health, the Massachusetts Department of Public Health, and other regional and national injury research centers.
Successful candidates must be a graduate of an ACGME-accredited Emergency Medicine residency and can apply for a 1-year or 2-year program (if pursuing an advanced degree). Fellows are expected to work alongside and train EM residents and medical and PA students. The position comes with an excellent benefits package and a faculty appointment. BMC/Chobanian &Avedisian School of Medicine are equal opportunity/affirmative action employers. Email us for more information @ BMCFellowships@bmc.org


• Explore new career opportunities for FREE!
• Click on any websites, emails, and videos to learn more.
• Download the guide to look back on organizations and positions that appeal to you.



Wednesday, May 15, Noon
AstraZeneca
Title: Management of FXa Inhibitor-Related Life-Threatening or Uncontrolled Bleeding
Speaker: Lionel Picot-Vierra, PharmD, Medical Science Liaison
AstraZeneca Pharmaceuticals LP
Inflammatix
Title: Revolutionizing the Diagnosis of Acute Infection and Sepsis with Cutting-Edge Host Response Diagnostics
Speaker: TBD
Physicians Choose Envision for Academic Emergency Medicine Opportunities Because…
Our strong partnerships with academic medical centers and teaching hospitals enable you to choose the environment in which you practice and the place you want to live.
We are a physician-led medical group. With Envision, you are fully supported in your pursuit of leadership, academic, clinical practice or research opportunities in emergency medicine.
Stop by Booth 203 to talk with our clinical leaders and enter our drawing for a chance to win a $100 Amazon gift card
ASSISTANT PROGRAM DIRECTOR
HCA Florida Lawnwood Hospital Fort Pierce, FL
PEDIATRIC EM MEDICAL DIRECTOR
HCA Houston Healthcare Kingwood Houston, TX
CORE FACULTY OPPORTUNITY FOR EM PHYSICIAN
HCA Florida Oak Hill Hospital Brooksville, FL
EM PHYSICIAN, FELLOWSHIP TRAINED IN CRITICAL CARE, SPORTS MEDICINE OR RESEARCH Morristown Medical Director Morristown, NJ
CORE FACULTY OPPORTUNITY FOR ULTRASOUND DIRECTOR
HCA Florida Ocala Hospital Ocala, FL
Contact our experienced recruiters for details about these opportunities.
Climate Change is a Health Emergency
Climate Change is a Health Emergency
Step up to be part of the solution.
Step up to be part of the solution.
Climate and Human Health Fellowship
Climate and Human Health Fellowship
Department of Emergency Medicine | BIDMC
Department of Emergency Medicine | BIDMC
2 Years | Master’s Degree | Funded Research
2 Years | Master’s Degree | Funded Research
Mentored by faculty a liated with:
Mentored by faculty a liated with:
• Harvard C-CHANGE
• Harvard C-CHANGE
• Harvard FXB Center
• Harvard FXB Center
• Harvard University Center for the Environment
• Harvard University Center for the Environment








To learn more, visit climateandhumanhealth.org and https://bit.ly/2YELgi4.
To learn more, visit climateandhumanhealth.org and https://bit.ly/2YELgi4.






Various locations across Pennsylvania
Come visit us at booth 119 at SAEM24 in Phoenix!
At Geisinger, you don’t have to put your life on hold to move healthcare forward. Living in Pennsylvania and working at a nationally recognized system, you’ll have opportunities to deliver innovative patient care, while enjoying a work-life balance that gives you time to explore everything the outdoors has to offer. This is a place where you can get more out of life and make a difference in the lives of your neighbors – at home and across the country.
We’re proud to offer our Emergency Medicine providers the support they need to succeed professionally and personally:
• Competitive compensation package & benefits including three robust retirement plans, CME, relocation and more
• Academic opportunities with Geisinger Commonwealth School of Medicine
• Better quality of life – Enjoy fresh air, short commutes, and tight-knit communities in our respective regions across Pennsylvania
• Satisfaction of working for a nationally recognized, physician-led healthcare organization committed to leading healthcare change
Interested candidates, please contact Miranda Grace, CPRP, Senior Provider Recruiter, at 717-899-0131 or mlgrace@geisinger.edu
Visit jobs.geisinger.org/physicians
EOE/AA: Disability/vet.
Only at Geisinger. Top 8 Most Innovative Healthcare Systems Becker’s Hospital Review Nationally recognized by Forbes, Fortune and TIMECreating a Diverse & Sustainable Emergency Medicine Investigator Pathway
Tuesday, May 14 8:00 AM - 5:00 PM

Supported



Check companies advertising jobs on SAEM’s EM Job Link against your LinkedIn contacts. Leverage professional connections for more information about the company or request a referral.

