




Chief Executive Officer
Megan N. Schagrin, MBA, CAE, CFRE mschagrin@saem.org
Director, Finance & Operations
Doug Ray, MSA, dray@saem.org Manager, Accounting Edwina Zaccardo, ezaccardo@saem.org
Director, IT
Anthony "Tony" Macalindong, amacalindong@saem.org
IT AMS Database Specialist
Dometrise "Dom" Hairston, dhairston@saem.org
Specialist, IT Support Dawud Lawson, dlawson@saem.org
Director, Governance
Erin Campo, ecampo@saem.org Manager, Governance Juana Vazquez, jvazquez@saem.org
Director, Communications & Publications
Laura Giblin, lgiblin@saem.org
Sr. Manager, Communications & Publications
Stacey Roseen, sroseen@saem.org Manager, Digital Marketing & Communications, Alison “Ali” Mistretta amistretta@saem.org Specialist, Web and Digital Content Alex Gorny, agorny@saem.org
Sr. Director, Foundation and Business Development
Melissa McMillian, CAE, CNP mmcmillian@saem.org
Sr. Manager, Development for the SAEM Foundation
Julie Wolfe, jwolfe@saem.org Manager, Educational Course Development
Kayla Belec Roseen, kroseen@saem.org Manager, Exhibits and Sponsorships Bill Schmitt, wschmitt@saem.org
Director, Membership & Meetings Holly Byrd-Duncan, MBA, hbyrdduncan@saem.org
Sr. Manager, Membership George Greaves, ggreaves@saem.org Sr. Manager, Education Andrea Ray, aray@saem.org
Sr. Coordinator, Membership & Meetings
Monica Bell, CMP, mbell@saem.org
Specialist, Membership Recruitment
Krystle Ansay, kansay@saem.org
Meeting Planner
Kar Corlew, kcorlew@saem.org
AEM Editor in Chief Jeffrey Kline, MD, AEMEditor@saem.org
AEM E&T Editor in Chief Susan Promes, MD, AEMETeditor@saem.org
AEM/AEM E&T Peer Review Coordinator Taylor Bowen, tbowen@saem.org aem@saem.org, aemet@saem.org
WE HAVE A NEW PHONE SYSTEM! For the most up-to-date contact information, visit the “ Contact Us ” page.
Wendy C. Coates, MD President
UCLA Department of Emergency Medicine
David Geffen School of Medicine at UCLA
Ali S. Raja, MD, DBA, MPH President Elect Massachusetts General Hospital/Harvard
Members-at-Large
Pooja Agrawal, MD, MPH
Yale University School of Medicine
Jeffrey Druck, MD
The University of Utah School of Medicine
Julianna J. Jung, MD
Johns Hopkins University School of Medicine
Nicholas M. Mohr, MD, MS University of Iowa
Michelle D. Lall, MD, MHS Secretary Treasurer Emory University
Angela M. Mills, MD Immediate Past President Columbia University Vagelos
Ava E. Pierce, MD UT Southwestern Medical Center, Dallas
Jody A. Vogel, MD, MSc, MSW Stanford University
Resident


“We have taken steps to ensure that universally relevant themes, such as equity and inclusion, as well as the emergency medicine workforce, are integrated into the activities of all SAEM groups.”

David Geffen School of Medicine at UCLA
2023-2024 President, SAEM
Spring is a season of new beginnings, and SAEM is blooming across many areas! In January, your Board of Directors devoted three focused days to map out the Society’s new strategic plan, that will be in effect from 2025-2028. While remaining committed to our mission of “Leading the advancement of academic emergency medicine through education, research, and professional development,” we have updated goals and objectives within each of our three core pillars to align with member needs. Additionally, we have taken steps to ensure that universally relevant themes, such as equity and inclusion, as well as the emergency medicine workforce, are integrated into the activities of all SAEM groups.
In March 2024, we will welcome a new cohort of enthusiastic junior colleagues to our EM family on Match Day, which falls on Friday, March 15, 2024. I urge everyone to extend a warm welcome to these newly matched residents, offering mentorship and involving them in your scholarly work. Recognizing that this period may be stressful for some, we are well-positioned to provide support and guidance.
SAEM RAMS provides a wealth of resources for medical students and residents interested in careers in emergency medicine (EM), RAMS Roadmaps, the Academic Career Guide, and our Career Roadmaps for Residents and Medical Students I strongly recommend enrolling your new residents as SAEM RAMS members so they can
access the full spectrum of benefits offered to our members. Additionally, it’s noteworthy that SAEM, AACEM, CDEM, and RAMS are actively collaborating on the all-EM Match Taskforce, continuing our commitment to enhancing the match process in emergency medicine.
As we approach our upcoming Annual Meeting, set to take place in Phoenix, Ariz., May 14-17, the Program Committee, led by Dr. Ryan LaFollette, has planned an exceptional experience for attendees. We are thrilled to have received a record-breaking number of proposed presentations for this meeting. Your valuable contributions are sure to make this a truly exciting and enriching experience for everyone.
We are pleased to again offer free professional childcare during SAEM24 so that parents can enjoy and participate in the meeting worry-free. To take advantage of this service, please sign up by the early bird registration deadline on March 12, 2024.
On Wednesday, May 15, Dr. Robert Neumar, a distinguished researcher, will present the Dr. Peter Rosen Memorial Keynote. He will enlighten us about the current landscape of emergency care research and underscore the significance of federal funding for our specialty
Throughout the year, we have proactively fostered connections with the National Institutes of Health (NIH),

continued from Page 3
striving to strengthen ties with individual Institutes. This collaborative effort aims to identify areas of mutual interest. Notably, we are in regular collaboration with Dr. Jeremy Brown, from the NIH Office of Emergency Care Research (OECR). I encourage you to make the most of the upcoming Program Officer Event at SAEM24 and stay tuned to Dr. Brown’s insightful columns featured in each issue of Pulse.
On Thursday, May 16, Dr. Holly Caretta-Weyer, a prominent figure in competency-based medical education (CBME), will deliver the SAEM24 Education Keynote She will speak about CBME and its direct relevance to emergency medicine board certification and maintenance. This concept spans the entire spectrum of medical education, from medical school to Graduate Medical Education, with far-
reaching implications for maintaining certification and fostering lifelong learning.
The American Board of Medical Specialties (ABMS) supports the incorporation of CBME by its member boards. Both SAEM and AACEM are active participants in the recently convened multi-organizational task force, led by ABEM. This task force is dedicated to exploring the integration of CBME across the continuum of EM education and certification and is committed to minimizing any disruption in time-based educational traditions. I strongly encourage everyone to attend this session, as it promises invaluable insights into how CBME will shape the future landscape of EM education and certification, impacting both individuals and departments alike.
On Tuesday, May 14, we are delighted to host Academic Emergency Medicine Pharmacists (AEMP) during their Annual Conference Any SAEM member is
welcome to join the AEMP Interest Group, for enhanced collaboration within our community. We extend a warm welcome to the AEMP, embracing them as new members of SAEM. We encourage individuals at your institutions to become involved with this vibrant community for mutual benefit and growth.
I am grateful to every SAEM member, as each of you contributes to creating a welcoming and productive environment for collaboration, friendship, and the advancement of science and education within our Society. Together, we are poised to advance and further elevate the field of academic emergency medicine. I eagerly anticipate seeing you in Phoenix!
ABOUT DR. COATES: Wendy Coates, MD, is professor of emergency medicine at David Geffen School of Medicine at UCLA and senior faculty/ education specialist at UCLA Department of Emergency Medicine


There’s


Jeffrey Druck, MD
Member-at-Large, 2023-2024 SAEM Board of Directors
Vice Chair for Faculty Advancement, DEI and Wellbeing, and Professor, Department of Emergency Medicine, University of Utah School of Medicine
Dr. Druck is SAEM Board Liaison for the following SAEM groups:
President: Liz Goldberg, MD
Overview
The Academy for Geriatric Emergency Medicine (AGEM) is dedicated to enhancing the quality of emergency care for older patients. Its mission encompasses advancing research, education, and faculty development, while serving as a unified voice for professionals in geriatric emergency medicine. AGEM provides a platform for researchers, educators, trainees, and clinicians to address challenges related to geriatric emergency medicine.
Updates/Status
• Over the past year, AGEM has prioritized promoting diversity, equity, and inclusion (DEI). This includes a new scholarship program offering $1,000 to medical students and residents seeking financial support for away rotations. Recipients are paired with experienced mentors in geriatric emergency medicine at various U.S.
and international locations, facilitated by AGEM leadership.
• AGEM has also collaborated with a foundation to enhance DEI in geriatric emergency medicine research. A systematic review conducted by AGEM members identifies areas for improvement in the reporting of research findings, aiming for greater inclusivity and transparency. AGEM actively shares its insights with the academic community, including a dedicated dinner at the upcoming SAEM conference.
• AGEM Zoom Meetings: First Thursday of each month at noon, CT.
• Geriatric Emergency Department Collaborative Dinner (co-led by AGEM and ADIEM): May 14, 2024, 6-8 p.m. MT, focusing on “Including DEI Principles in Studies of Geriatric Patients.”
Chair: Megan A Rech, PharmD, MS
Overview
The Academic Emergency Medicine Pharmacists Interest Group (AEMP) is focused on creating an academic home for emergency medicine pharmacists and cultivating multidisciplinary collaboration.
• Formed 5 committees: Career Development (Chair: Elise Metts, PharmD); Communications (Chair: Lisa Hayes, PharmD); Membership (Chair: Tara Flack, PharmD); Program (Chair: Caitlin Brown, PharmD); Steering (16 members total)
• Created programming for PharmERgency: AEMP24 Conference, an annual, multidisciplinary event open to all SAEM attendees, dedicated to celebrating advancements in the research and practice of emergency medicine pharmacotherapy.
• Late-breaking EM pharmacy literature/Journal clubs
• New guideline reviews
• Pharmacy Pearls
• Online resources (www.SAEM.org)
• EM Pharmacists’ Favorite Drug References/Tools
Chair: Samuel E. Sondheim, MD, MBA
Mission
The Disaster Medicine Interest Group is committed to providing up-to-date, accurate, and useful information to emergency medicine professionals regarding their role in disaster research, preparedness, and response activities. The group is currently working on a position statement highlighting challenges related to Mass Casualty Incident (MCI) readiness and emergency departments’ ability to respond amid high boarding volumes and real estate constraints.
• Development of a disaster medicine just-in-time training handbook in collaboration with national organizations.
• Monthly Meetings: Fourth Thursday of each month at 12 p.m. CT
Chair: Leon D. Sanchez, MD, MPH
Mission
The ED Administration and Clinical Operations Committee focuses on implementing methods to enhance clinical operations within academic emergency departments. This committee actively monitors operational trends, disseminates best practices, and promotes original research opportunities through SAEM channels.
• Asynchronous Operations Curriculum: The committee offers an asynchronous operations curriculum available on YouTube, providing valuable insights into clinical operations.
• Boarding Resources: A comprehensive list of boarding resources, soon to be accessible on the SAEM website.
Chair: Bryn E. Mumma, MD, MAS
Mission
The Grants Committee actively supports the mission and goals of SAEM and the SAEM Foundation (SAEMF). Their primary focus is on developing and implementing grant programs that contribute to the advancement of the field of emergency medicine. Additionally, the committee is committed to conducting a thorough and methodologically rigorous peer review of all submitted proposals.
Updates/Status
• Welcomed 10 resident reviewers to the 2023-24 Grants Committee, offering personalized one-on-one mentoring during the grant review process.
• Successfully reviewed and scored all grant applications submitted to the SAEMF.
• Currently in the planning stages for formal evaluations of the SAEMF education research grants, including the Education Project Grant and Education Research Training Grant.
• The Grants Committee convenes regularly on the second Monday of each month at 3 p.m. CT. This consistent schedule ensures a dedicated forum for collaboration and decision-making within the committee.
Chair: Gregory Wu, MD
Mission
The Critical Care Interest Group (CCIG) is dedicated to creating a collaborative forum for academic physicians with specialized training or a keen interest in critical care. The mission is centered around fostering the sharing of expertise and interests, mentoring junior faculty members, advocating for the field, and advancing knowledge through education and research.
Updates/Status
• Sponsored three didactics at SAEM23 and two additional didactics for SAEM24, providing valuable learning opportunities for members.
• Contributed four SAEM Pulse articles in the last two years, showcasing the group’s commitment to disseminating critical care knowledge and insights.
• CCIG will meet at SAEM24 on Friday, May 17, 2024, 10-10:50 a.m. MT
Co-Chairs: Lauren Mamer, MD, Katherine Dickerson Mayes, MD, PhD
Mission
The Neurologic Emergency Medicine Interest Group is committed to enhancing research, education, and patient care in the domains of traumatic brain injury, stroke, epilepsy, and other acute neurological emergencies.
Updates/Status
• Contributions to the GRACE 3 guidelines on dizziness, demonstrating their commitment to advancing knowledge in the field
• Ongoing involvement in the ICECAP and BOOST trials
• The Neurologic EM IG plans to host several neuro-related sessions at SAEM24

Member-at-Large, 2023-2024 SAEM Board of Directors
Director of Medical Student Education, Associate Professor of Emergency Medicine
Johns Hopkins University School of Medicine
Dr. Jung is SAEM Board Liaison for the following SAEM groups:
President: Joseph House, MD
Mission
Founded in 2008 as the inaugural
Academy of SAEM, the Clerkship Directors in Emergency Medicine (CDEM) is the national organization representing undergraduate medical education in Emergency Medicine. CDEM members are medical student educators who are committed to enhancing medical student education within our specialty. The mission of CDEM is to advance undergraduate medical education in EM, and to serve as a unified voice for EM clerkship directors and other undergraduate educators on the national level. (Full statement.)
• Development and maintenance of three widely used national curricula for medical students in emergency medicine (EM), providing offerings for M3 students, M4 students, and students on pediatric EM rotations. The M3 curriculum was comprehensively updated this year by the Curriculum and Assessment Committee.
• Unveiled a new version of the M4 exam on SAEM Tests, which is an online platform containing national standardized exams for students in EM clerkships, used by medical schools across the country. The SAEM Test development process includes rigorous question writing and revision, statistical analysis, and continuous quality improvement.
• Development and maintenance of a directory of scholarships for students from groups that are underrepresented in medicine to pursue away rotations in EM
• Development and maintenance of a clerkship directory that allows all students to locate and contact institutions offering EM rotations
• Continued support of the annual SAEM Clerkship Directors Bootcamp
• Hosting a preconference session on Multiple Choice Item Writing for aspiring test developers at SAEM24
• Conferring “Academy Awards” for Clerkship Director of the Year, Clerkship Coordinator of the Year, Educational Innovations, and Distinguished Educator, and others
• Sponsoring several education abstracts at the national meeting
continued on Page 8
• Supporting a scholarship for a member to attend ARMED MedEd
• Planning an Academy-wide needs assessment survey to optimally align CDEM offerings with what members want most
• Planning an updated “State of the Clerkship” survey to evaluate the landscape of undergraduate medical education in EM
Chair: Chris Carpenter, MD
Overview
The SAEM GRACE program addresses the best practices for the care of the most common chief complaints that can be seen on the tracking board of any emergency department in the country, based upon research and expert consensus. These guidelines are designed with de-implementation as a guiding principle to reasonably reduce wasteful testing, provide explicit criteria to reduce foreseeable risk, and define sensible and prudent medical care. The first GRACE guideline was published in 2021, with new topics tackled annually by the group.
• GRACE represents emergency medicine’s first clinical practice guidelines based on the rigorous Grading of Recommendations, Assessment, Development, and Evaluations (GRADE) methodology
• GRACE guidelines now cover three crucial EM topics (chest pain, abdominal pain, and dizziness) with two more coming (substance use disorders and syncope), supported on a foundation of original systematic reviews and listed by ECRI (Emergency Care Research Institute) as trustworthy guidelines).
• GRACE citations:
• GRACE-1 has been cited 17 times with an AltMetric of 282. Learn more about GRACE-1 from this SGEM podcast
• GRACE-2 has been cited eight times with an AltMetric of 101. Learn more
from this SGEM podcast.
• GRACE-3 has been cited 12 times with an AltMetric of 618 which is number seven in the history of Academic Emergency Medicine. Learn more from this SGEM podcast
• GRACE has developed an internal SAEM systematic review subcommittee to facilitate creation of foundational systematic reviews and has had its latest work accepted in abstract form to SAEM2024.
• GRACE continues to expand the GRADE meta-science by contributing insightful commentaries that outline the challenges inherent to applying the rigorous GRADE methodology in the world of emergency medicine.
Chair: James Paxton, MD
The SAEM Research Committee serves as a resource for finding funding opportunities and for preparing materials that are helpful to all of SAEM’s members in improving their research skills. The Research Committee is responsible for organizing the annual Grant Writing Workshop for submitting specialized didactic sessions for SAEM’s annual meeting, and for other research-related objectives as required.
• Under the strong leadership of subcommittee chair Layne Dylla, MD, we have continued to grow and develop the Research Learning Series, an invaluable archived resource for junior researchers to learn about research topics. Some highlights from this year’s offerings include talks about research career and program development, metaanalysis and randomized controlled trial methodology, and three “Talk with a Biostatistician” sessions covering key topics in data analysis.
• Finished first in the SAEM Foundation Challenge annual fundraising competition for committees, with over $13,000 raised
• Sponsored 31 didactics for SAEM24, a new record for the committee
• Continued to provide assistance to the ARMED and ARMED MedEd programs
• Submitted multiple joint SAEM-ACEP
responses to federal funding agency Requests for Information (RFIs), representing the common interests of all EM researchers
• Working to increase the number of emergency care investigators participating in NIH study sections, with nearly 50 candidates forwarded to NIH over the last four years
• Under the leadership of subcommittee chair Samuel Lam, MD, have successfully re-envisioned the process for administering the annual SAEM Consensus Conference. From the application process through the planning stages to the final exectution of the conference itself, we have made the process more streamlined and supportive for leaders and participants, ensuring scientific rigor at every step.
• Have prioritized efforts to promote diversity among EM researchers, including collaboration with other relevant groups
• Under the leadership of subcommittee chair Joshua Lupton, MD, MPH, MPhil, have continued efforts to draw attention to SAEM members who have demonstrated excellence in research, including podcasts, Pulse articles, webinars, and other media.
Chairs: Josh Baugh, MD, Elizabeth Temin, MD, MPH
This new interest group was formed this year by merging groups with common interests into a single unified front. Members of the previous ED Crowding, Clinical Directors, and Advanced Practice Providers interest groups now have a common home to work towards advancing the science of care delivery. This interest group works in close collaboration with the ED Clinical Operations Committee of SAEM.
• Hosted Operations Journal Club, for members to learn about important topics in ED operations and emerging evidence about care delivery systems
• Hosted open forms to discuss departmental initiatives around advance practice providers and the impact of operational factors on care quality
• Sponsored several didactics for the annual meeting
• Increased recruitment efforts for junior members (students/residents/fellows) to support learning and engagement with ED operations topics
Pediatric Emergency Medicine Interest Group
Chair: Jennifer Mitzman, MD
Overview
This interest group is dedicated to improving pediatric emergency care through the advancement of science and education.
• Hosted a “best of” session at the annual meeting, in which the most impactful pediatric emergency medicine abstracts were presented orally
• Conferred awards for top contributors to pediatric emergency care
• Sponsored several didactics for the annual meeting



Michael Wade, MD, is a pediatric emergency medicine physician at Phoenix Children's Hospital. Following his service as an Army medic, Dr. Wade decided to further pursue his true calling by continuing to provide care for individuals in emergency situations. Upon completing his medical degree at Howard University College of Medicine in Washington, D.C., he sought additional training at Phoenix Children's through a pediatric residency and a pediatric urgent care fellowship. Phoenix Children's has become a significant professional environment for him, fostering a sense of belonging. Dr. Wade values his colleagues as much as the diverse patient population he serves. Currently, Dr. Wade addresses all issues that arise in both emergency care and urgent care settings. Additionally, he actively works towards educating families, empowering them to make well-informed medical decisions.
Dr. Wade is affiliated with the American Academy of Pediatrics and the Society for Academic Emergency Medicine, where he assumes a leadership role as one of three chairs for the SAEM Medical Student Ambassador program.
Additionally, Dr. Wade has been recognized as a Gold Humanism Honor Society Inductee, an honor reserved for medical students, residents, and faculty who are exemplars of compassionate patient care and serve as role models, mentors, and leaders in the field of medicine.
In his free time, Dr. Wade enjoys competing in mud runs and adventure races and has successfully completed numerous races across multiple states. As a native of Arizona, he also finds enjoyment in attending Phoenix Suns and Arizona Diamondbacks games.


How and why did you become involved with the Medical Student Ambassador (MSA) program and how long have you been involved with the program?
I became involved with SAEM in 2018 when I was selected as a Medical Student Ambassador. At the time, I was a third-year medical student preparing for my residency application cycle. When I received the invitation to volunteer at SAEM18 I saw an opportunity to bolster my application while providing a service to an organization that greatly interested me. The experience helped solidify my future career in emergency medicine as well as in academia.
What is your current role with the MSA program and how long have you held that role?
Presently, I serve as an SAEM program committee member and co-chair of the MSA program, alongside Zeinab ShafieKhorassani and Hamza Ijaz. These roles extend beyond the planning of the annual meeting to include recruiting, orienting, and guiding the Medical Student Ambassadors (MSAs) in keeping the annual meeting functioning as seamlessly as possible throughout the week. My involvement began in 2019 as a program committee member, and I subsequently took on the role of co-chair of the MSA program in 2022.
In a nutshell, what are the primary responsibilities of a Medical Student Ambassador?
In essence, Medical Student Ambassadors act as a jack-of-all trades during the meetings. Their primary responsibilities center around the various sessions, including oral presentations, poster
presentations, abstracts, and workshops. Within these sessions, their duties include ensuring the presence of speakers, resolving any IT or AV issues before the sessions commence. Additionally, they track the attendance at each session, enabling us to adjust room sizes for future meetings based on the observed turnout and the nature of activities within each session.
There are many benefits to medical students of being an MSA, but what, in your opinion, are the top 3-4?
The primary benefits of medical students serving as MSAs include professional networking, access to educational content, and opportunities for fostering personal relationships. The extent of networking success largely depends on the effort invested by each student. With unrestricted access to the entire annual meeting, MSAs have the chance to meet individuals from just about every major emergency medicine (EM) program across the United States.
Furthermore, access to the meeting can be used as a platform for learning about or expanding upon topics presented by leading minds in the specialty. This extends beyond the sessions they are assigned to, as students can utilize their “downtime” to participate in additional sessions, enriching their understanding of specific topics.
Finally, MSAs have the opportunity to build meaningful relationships within the program committee, at the residency fair, with meeting presenters, and among fellow MSAs. This
continued on Page 12

Michael Wade’s children Logan and Olivia enjoying the seemingly never-ending swimming season at their home.
continued from Page 11
happens through candid conversations with and support from others who have gone through or are going through similar experiences.
Walk me through a typical day for an MSA at the SAEM Annual Meeting.
Typically, our days start early, around 7:30 am with a briefing over breakfast, setting the tone for the day ahead. This early start might seem challenging for many of us, but for medical students accustomed to early clinical rotations, this is sleeping in! After breakfast, the MSAs head out to their assigned, morning block sessions, putting out all the fires that inevitably arise in such a large meeting.
Lunchtime provides a break, during which we encourage students to reconvene in the MSA room for guest lectures from one of our esteemed colleagues from across the country. These sessions cover a range of topics, including CVs, applications, away rotations, interviews, and everything in between. The afternoon wraps up with students returning to their assigned sessions for the remainder of the day.
Between scheduled assignments, students often have several blocks of free time. With full access to the annual meeting, this time allows them to explore various lectures, presentations, workshops, or simply unwind with a nap — a welcome break from patient rounds. Evenings are free for leisure, fostering opportunities for students to get together in groups, organize social activities, and explore the city.
What makes this program so special and why is a program like this so important?
While numerous organizations have tried to implement similar
programs to gain exposure and cultivate interest, SAEM has been able to knock this out of the park! In fact, for SAEM24 we experienced the single largest MSA applicant pool since the program began. This diverse group ranges from undergraduates to medical school graduates from across the United States and extending globally to Canada, France, and the United Kingdom.
Although my personal involvement in this program spans only a few years, the extensive groundwork laid by those who came before me has helped build it into the successful program it is today. The robust interest alone shows how big an impact this program has on our future colleagues in emergency medicine and beyond. In addition to engaging future leaders in academic emergency medicine, this program has continued to expand the impact of the SAEM annual meeting on medicine as a whole.
As you mentioned, this year’s Medical Student Application pool is SAEM’s largest ever. Aside from the tangible benefits of participation, what do you believe is the primary appeal to medical students of a program such as this?
As a previous MSA myself and currently serving as a co-chair of the program, I can tell you that what drew me into the program was networking. As a medical student, I came from a medical school without an EM residency, which left me with limited access to academic mentors in my preferred specialty. Many students share similar sentiments as well as a desire to become more involved in national organizations such as SAEM. The select few that are afforded the opportunity to serve as MSAs typically apply to the program with the goal of gaining unique experiences that can help them on their journey through medicine.

Please share one of the highlights/most memorable experiences you’ve had so far as a leader of the MSA program.
Without a doubt, the most memorable experiences I have had revolve around conversations with former MSAs who attest to successfully matching into their preferred programs due to their experiences as an MSA. Many of them shared with me that the opportunities to interact with program directors, attendings, residents, and fellow medical students from various schools provided them with one-on-one conversations they never thought possible.
Many have found new friendships with fellow MSAs who have offered support during interview season. Whether providing a couch to crash on or sharing critical details about specific programs, these friendships have contributed to their interview success. These invaluable connections and experiences have helped numerous medical students achieve their dreams—an impact that far exceeds any expectations I could have envisioned for the program.
How do you feel Phoenix will rate as an SAEM Annual Meeting location and what are you most looking forward to at SAEM24?
Being an Arizona native, I have to say that SAEM24 will undoubtedly be the best one yet! Sure, sure, some may complain about the heat, but it is a dry heat after all! Whether you enjoy the gorgeous sunsets from your air-conditioned hotel room, catch a Phoenix Suns playoff game (fingers crossed), or venture on a "warm" hike to Piestewa Peak just a few miles away, everyone attending in Phoenix this year is in for a great time. Personally, what excites me the most is not having to live out of a suitcase for an entire week!
Favorite “after hours” hotspot(s):
Finding one of the many “speakeasies” hidden in the downtown Phoenix or Old Town Scottsdale areas.
Here are a few to try within walking distance of our Sheraton Downtown host hotel:
• Barcoa Agaveria
• Melinda’s Alley
• Pigtails
• Rough Rider
• Little Rituals
• Bitter & Twisted Cocktail Parlour
• Trophy Room
Best place for tacos and margaritas:
Chico Malo or Centrico
Favorite place to “take a hike”/enjoy the great outdoors:
Piestewa Peak or South Mountain where you might be lucky enough to see the saguaro cactus blossoms
Most epic view/Instagrammable spot in Phoenix:
Any rooftop bar at sunset.
Here are four in the metro Phoenix area you might want to try:
• Floor 13 Rooftop Bar
• From the Rooftop
• Eden Rooftop Bar
• Bar Smith
Outdoor patio(s) to “dine” for:
Pizzeria Bianco
Favorite place to have fun with the family:
Phoenix Zoo
Footprint Center to watch the Phoenix Suns or Phoenix Mercury
Chase Field to watch the Arizona Diamondbacks
Attraction to add to an “Only in Phoenix” bucket list:
With Arizona’s rich and cultural history of both Indigenous and Mexican heritage, visiting places like the Heard Museum can help you explore the unique background of Phoenix and Arizona as a whole. Additionally, a short, two-hour drive can take you up to the unique and gorgeous red rocks of Sedona, Ariz

A Message From Ryan LaFollette, MD, SAEM24 Program Committee Chair
Whether you're an experienced professional or just starting out on your EM journey, the SAEM Annual Meeting is designed to meet your specific needs. Building on the tremendous success of SAEM23, SAEM24 is poised to exceed expectations once again. We’ve planned a robust educational lineup featuring diverse workshops on specialized topics, enriching didactic sessions, groundbreaking research, and forums tailored to every stage of your career. Our two keynote speakers will inspire innovative ideas and fuel your pursuit of excellence. Popular gamified experiential learning competitions such as SimWARs and Sonogames combine intellectual stimulation and friendly competition for participants and spectators alike.
For our residents and medical students, the SAEM Annual Meeting also connects you with peers, leaders, and others who can help you take your career to the next level. Check out the article “SAEM24: Top 10 Reasons Residents and Med Students Should Be There!” in this special SAEM24
preview section of this issue of SAEM Pulse for all the “Don’t Miss”details!
SAEM24 is a distinctive hub for networking and collaboration that is unmatched by any other event. At the SAEM Annual Meeting, EM professionals across all career stages convene, forming connections that not only shape their personal and professional paths but also contribute to the collective growth of the specialty. Our attendees tell is there’s nothing quite like it when it comes to building meaningful mentoring relationships, building productive collaborative alliances, and fostering a tight-knit emergency medicine community.
Prioritizing
For our SAEM family we provide free, licensed childcare services, ensuring you can fully engage in the meeting knowing your little ones are being well cared for. (Register by March 12 if you’re interested!) Plus, our private, well-equipped family/lactation room caters to the needs of both baby and parent.
The Best of Phoenix at Your Doorstep Nestled in the heart of a rejuvenated downtown, the Sheraton Downtown Phoenix host hotel places you steps away from vibrant a culinary scene, iconic sports venues, hidden entertainment and cultural gems, and natural wonders like Camelback Mountain and the Grand Canyon.
The Countdown Has Begun!
Join us May 14-17, 2024, in the Valley of the Sun, for another extraordinary educational experience. We’re counting the days until your arrival and the chance to showcase all we have in store for you at SAEM24—where learning, networking, and innovation converge!
Register by March 12 to secure your early bird discount!
Abstracts present research data, including study background and methodology, research limitations and results, and the conclusions/significance of the study. Abstract session lengths vary depending on the presentation type: plenary (15 minutes), full oral (12 minutes), lightning oral (7 minutes), ePoster (5 minutes).
The SAEM24 Program Committee is pleased to announce the top eight abstracts selected to be presented during a special plenary session to be held immediately following the keynote addresses on Wednesday and Thursday. These eight abstracts were chosen as the best from among a record 1,395 submissions
Wednesday, May 15, 10:00 AM – 11:00 AM MT
Following the Dr. Peter Rosen Memorial Keynote.
1. Visualization of Occult Ventricular Fibrillation by Echocardiography During Cardiac Arrest: A Multicenter Trial
Romolo Gaspari, Josie Acuna, Jacob Baxter, Drew Clare, John DeAngelis, Timothy Gleeson, Powell Graham, John Hipskind, Ryan Joseph, Monica Kapoor, Tobias Kummer, Margaret Lewis, Stephanie Midgley, Robert Lindsay, Offdan Narvaez-Guerra, Jason Nomura, Mark Scheatzle, Nikolai Schnittke, Michael Secko, Trent She, Zachary Soucy, Jeffrey Stowell, Rebecca Theophanous, Jordan Tozer, Tyler Yates, Andrew Balk
2. Pharmacy Density As a Community Level Predictor of Heart Failure Medication Nonadherence: A Geospatial Analysis
Madeline Woodson, Matthew Durthaler, Karlee Waugh, Robert Ehrman, Nicholas Harrison
3. Implementation of Artificial Intelligence-Informed RiskDriven Emergency Department Triage Decreased Length of Stay for High-Risk Chest Pain
Jeremiah Hinson, Richard Taylor, Benjamin Steinhart, Christopher Chmura, Inessa Cohen, Haipeng Xue, Scott Levin
4. Emergency Department Utilization by Youth Before and After Firearm Injury
Samaa Kemal, Rebecca Cash, Kenneth Michelson, Elizabeth Alpern, Margaret Samuels-Kalow

Robert Neumar, MD, PhD, chair of emergency medicine at the University of Michigan, will deliver the SAEM24 Dr. Peter Rosen Memorial Keynote, "Emergency Medicine Research: Past, Present, and Future," on Wednesday, May 15, 2024.
Dr. Neumar is well-regarded for his contributions and advocacy for federally funded research in emergency care. With over 30 years of cardiac arrest resuscitation research, he has mentored medical students, doctoral candidates, post-doctoral fellows, and NIH K-award recipients. A leading advocate for federally funded emergency care research, Dr. Neumar served as the inaugural co-chair of the ACEP/ SAEM Task Force on Emergency Care Research. His other pivotal contributions include organizing NIH Roundtables, establishing the first NIH K12 program dedicated to emergency care research in 2011, and founding the NIH Office of Emergency Care Research.
Dr. Neumar formerly led the ACEP Research Committee, ACEP Scientific Review Subcommittee, and ACEP EM Research Section. Currently, he cochairs the AACEM Research Workgroup, playing a key role in developing the Emergency Medicine Research: 2030 Strategic Goals.
Dr. Neumar's significant contributions to the field have earned him several accolades, including the ACEP Award for Outstanding Contribution in Research, the SAEM John Marx Leadership Award, and his election to the prestigious National Academy of Medicine.
In his keynote address, Dr. Neumar will explore the evolution of emergency medicine as a specialty. Focusing on the pivotal role of research in driving advancements and enhancing patient care, he will trace the specialty’s growth over the past few decades, assess the present condition of our research enterprise, and articulate a vision for the future.
The aim of the keynote is to emphasize the crucial need for the entire specialty to steadfastly commit to fulfilling the research mission and to underscore the significance of proactively investing in a sustainable and diverse pipeline of emergency medicine clinician-scientists.
Anticipated as a pivotal moment during SAEM24's opening session, Dr. Neumar's address is expected to inspire and energize the next generation, encouraging them to actively engage in shaping the future of emergency care by fostering innovative knowledge creation for continuous improvement in patient outcomes.

Holly Caretta-Weyer, MD, MHPE, a prominent figure in competencybased medical education, is set to deliver the SAEM24 Education Keynote “Patient-Focused and Learner-Centered: The Promise of Competency-Based Medical Education,” on May 16, 2024, at the SAEM Annual Meeting in Phoenix, Ariz. Dr. Caretta-Weyer is the associate residency program director and director of evaluation and assessment for the Stanford University Emergency Medicine Residency Program. She also serves as the implementation lead for Entrustable Professional Activities/Competency-Based Medical Education (EPA/CBME) at the Stanford University School of Medicine.
While completing a Medical Education Scholarship Fellowship at Oregon Health & Science University (OHSU), Dr. Caretta-Weyer contributed to the Association of American Medical Colleges (AAMC) Core Entrustable Professional Activities for Entering Residency pilot team and played a key role in the OHSU undergraduate medical education entrustment committee. She is actively involved in the national AAMC Core EPA Pilot, focusing on programmatic assessment, entrustment decisions, and the transition from undergraduate to graduate medical education.
Dr. Caretta-Weyer is the principal investigator of a $1.3 million American Medical Association (AMA) Reimagining Residency Grant, aiming to implement competency-based education and redesign assessment in emergency medicine training. As a visiting scholar with the American Board of Medical Specialties (ABMS), she examines summative entrustment decisionmaking. Additionally, she is a member of the International Competency-Based Medical Education Collaborators (ICBME), contributing to global research on CBME.
Recently elected as the inaugural chair of the CBME Task Force for Emergency Medicine, her impactful work earned her the title of International Medical Educator of the Year by the Royal College of Physicians and Surgeons of Canada in 2022.
The keynote address will emphasize the significance of Competency-Based Medical Education (CBME) in the context of emergency medicine and underscore the need for collaboration within the specialty to overcome challenges in the implementation of CBME. In her presentation, Dr. Caretta-Weyer will articulate a shared mental model of the fundamental elements of competency-based medical education, discuss challenges in its implementation, and explore avenues for research, innovation, and adoption in this field.
Thursday, May 16, 10:00 AM – 11:00 AM MT
5. Author Visibility in Video Presentations: Impact on Knowledge Retention and Satisfaction in Medical Education
Priya Patel
6. Resident Scholarly Activity and Productivity Outcomes Before and After Implementing a Structured Research Program
Sydney Krispin, Eric Kontowicz, Brett Faine, Michael Takacs, Karisa Harland, J. Priyanka Vakkalanka, Kelli Wallace, Andrew Nugent, Nicholas Mohr
7. Home vs Away Rotation Differences in the Standardized Letters of Evaluation 2.0
Aman Pandey, Cullen Hegarty, Sharon Bord, Katarzyna Gore, Thomas Beardsley, Sara Krzyzaniak, Sandra Monteiro, Al'ai Alvarez, Teresa Davis, Melissa Parsons, Michael Gottlieb, Alexandra Mannix
8. Simulation-Based Mastery Learning Improves Resident Ability to Perform Emergency Cricothyrotomy
Dana Loke, Andrew Rogers, Morgan McCarthy, Maren Leibowitz, Elizabeth Stulpin, David Salzman
Tuesday, May 14, 8:00 AM – 5:00 PM MT
The SAEM24 Consensus Conference is dedicated to the critical task of establishing a sustainable and diverse pipeline of federally funded clinicianscientists in the field of emergency medicine. The primary goal is to collaboratively develop a comprehensive toolkit, addressing barriers and implementing strategies at various career levels, from undergraduates to mid-career faculty. By fostering diversity and sustainability, the conference aims to propel emergency medicine research towards achieving or surpassing its strategic goals for the year 2030. It is an opportunity for participants to actively contribute to shaping the future of emergency medicine.
Advanced EM Workshop Day
Tuesday, May 14

Advanced EM Workshops are intensive educational sessions that focus on techniques, skills, and practical aspects of the specialty. This year’s Advanced EM Workshop Day offerings includes 16 half- and full-day sessions that cover specialized areas in emergency medicine and strengthen knowledge and skills in specific topic areas. Add any workshop when you register for SAEM24
Full-Day Workshops, 8:00 AM – 5:00 PM MT
• World Health Organization Basic Emergency Care Training of the Trainers Course
• Grant Writing Workshop
• SAEM24 Consensus Conference: Creating a Diverse and Sustainable Emergency Medicine Investigator Pathway
Half-Day Morning Workshops, 8:00 AM – 12:00 PM MT
• Be The Best Teacher: Clinical Teaching Educational Bootcamp
• Breaking Bias: Cultivating Inclusive Learning Environments in MedEd
• Clerkship Director Bootcamp: Best Practices and Expert Insights
• From ChatGPT to the ED: Leveraging the Potential of Large Language Models in EM
• Figuring Out the Fiberscope: A Practical Training Session for Emergency Physicians
• The Art of Writing Effective Multiple-Choice Questions (by invite only)
Half-Day Afternoon Workshops, 1:00 PM – 5:00 PM MT
• Present Like a Pro: Crafting Compelling and Captivating Talks
• Stepping Up Your Procedure Game: Ultrasound-Guided Nerve Blocks and Arthrocentesis
• Wellness Tools That Drive Change and Promote a Healthier Work Environment
• Elevate Your Scholarly Pursuits: A Medical Education Research Bootcamp
• Breaking the Glass Ceiling: Networking Best Practices That Empower Women in Academic EM
• Bringing the Outside In: Integrating Wilderness and Resource-Limited Medicine into Your Practice and Curriculum
• Simulation Workshop in Facilitation and Teaching: Empower Learners with Effective Debriefing and Feedback
Didactics
SAEM didactics feature instructional presentations in various formats, from traditional lectures to flipped classrooms and small group discussions. These sessions aim to impart knowledge and skills, creating a dynamic learning environment. SAEM24 offers 140 innovative sessions covering diverse topics like administration, career development, education methodologies, clinical practices, and research advancements.
Wednesday May 15, 8:00 AM – 5:20 PM MT
View Wednesday’s Didactics
Thursday, May 16, 8:00 AM – 5:20 PM MT
View Thursday’s Didactics
Friday, May 17, 8:00 AM – 12:50 PM MT
View Friday’s Didactics
Wednesday, May 15, 11:00 AM - 1:00 PM MT
Friday, May 17, 11:00 AM - 1:00 PM MT
In this dynamic, fast-paced event, speakers take the stage for five minutes, backed by 20 auto-advancing slides that keep the energy high. The topics are diverse and captivating, ranging from disaster relief experiences to exploring the impact of machine learning in emergency medicine. Judges select a “Best of IGNITE!” winner in each session, while the audience gets a say with the “Audience Choice Award” based on live polling. With no restrictions on topics, IGNITE! promises a stimulating showcase of insights and challenges from speakers across the country and all levels of training. Don’t miss this unique blend of excitement and innovation in EM!
May 15-17, 2024
At the Clinical Images Exhibit, emergency medicine comes to life in stunning highdefinition visuals. Featuring EM cases selected for their educational merit, relevance to emergency medicine, and quality, each image is a puzzle waiting to be solved. Attendees are invited to review selected submissions, analyze case notes, and engage in a diagnostic challenge before uncovering the answers. This interactive exhibit not only highlights the practical aspects of emergency medicine, but also offers a dynamic learning experience.
Certain SAEM24 events and activities require separate registrations. Don't miss your chance! If you're interested in joining any of these popular SAEM Annual Meeting offerings, make sure to sign up before they fill up!
• AACEM Annual Reception and Dinner
• AWAEM and ADIEM Luncheon
• Program Officer Event
• ADIEM LGBTQIA+ Mixer
Wednesday, May 15, 12:00 PM - 3:30 PM MT
Thursday, May 16, 11:00 AM - 4:30 PM MT (tabletop)
Thursday, May 17, 8:00 AM - 9:50 AM MT
Innovations serves as a platform to showcase advancements in both undergraduate and graduate medical education, along with nonclinical areas like faculty development, wellness strategies, operational excellence, and patient care innovations. This event provides a unique space for creative exploration where participants can present visionary ideas through dynamic oral presentations or engaging tabletop/ hands-on demonstrations.
This year’s edition of Innovations will feature innovations in novel themes, including the intersection of machine learning/artificial intelligence with medical education, sustainable practices to reduce waste in healthcare settings, advancements in reproductive health and education, and solutions addressing the unique challenges of rural health. Join us at Innovations to be part of the transformative dialogue shaping the future of medical education and healthcare.
Tuesday, May 14, 8:00 AM – 5:00 PM MT
SAEM Leadership Forum focuses on core leadership subjects, emphasizing experiential learning and practical application. Led by recognized experts boasting extensive leadership backgrounds, the event covers diverse topics such as wellness, successful leadership strategies, increasing visibility, and conflict management. It’s a comprehensive platform for aspiring leaders seeking tangible insights and skills to elevate their leadership capabilities.
Thursday, May 16, 8:00 AM – 3:00 PM MT
Chief Resident Forum is the preeminent training ground for the next generation of emergency medicine leaders. It provides
aspiring chief residents with a balance of leadership training and practical insights for managing residency programs. The event facilitates networking among future chief residents from across the nation, offering a platform to share best practices. EM educational leaders share their experiences during engaging sessions designed to prepare future chief residents for the challenges of their roles and develop their leadership skills mindfully. The Chief Resident Forum is a long-standing tradition and serves as a crucial preparation for navigating the complexities of leading residency programs and building careers in academic emergency medicine.
Thursday, May 16, 8:00 AM – 3:00 PM MT

Medical Student Symposium is led by EM thought leaders and covers vital topics such as clerkships, away rotations, personal statements, interviews, and the match process. Tailored for applicants from allopathic, osteopathic, international, and military backgrounds, this day-long event offers unique insights into individual EM programs. Engage in discussions, pose questions, and gain valuable knowledge during lunch with EM program and clerkship directors. This symposium is your essential guide to navigating the intricate path to an EM residency.
SAEM RAMS Phoenix Hunt
Tuesday, May 14, 6:00 PM to 9:00 PM MT
SAEM RAMS Phoenix Hunt brings residency teams of three together to explore Phoenix’s iconic landmarks while tackling unique challenges linked to patient care, education, and professional development with a focus on content related to biological sex, gender, and diversity. The culmination of this quest-like adventure includes complimentary food and drinks and networking opportunities with fellow programs and stakeholders in academic emergency medicine. Prizes will be awarded to the team with the best time, team name, and social media picture.
Interested in Participating?
If you are signing as a team of three, please register as a TEAM; If you are an individual looking to join a team, please register as an INDIVIDUAL. RAMS Hunt Registration
Wednesday, May 15, 1:00 PM to 5:20 PM MT

Simulation Academy SimWars, the premier national simulation competition for emergency medicine residents, offers a unique learning experience. Teams of clinical providers compete in simulation-based challenges, showcasing various aspects of patient care before an engaged audience. Rooted in experiential learning, teams participate in immersive scenarios that demand mental, physical, and emotional involvement. Beyond the competition, SimWars fosters a collaborative community of practice, allowing observers and instructors to glean insights from diverse decision-making processes and practice variations. The event’s innovative group-learning format, coupled with individual skill assessment, cultivates global knowledge and skill enhancement.
Thursday, May 16, 6:00 PM to 8:00 PM MT

Dodgeball brings emergency medicine residency teams from across the country together for an epic showdown. Join us as we transform a standard ballroom into an extraordinary dodgeball court, with bleachers, hot dogs, cold brews, and exuberant fans! Whether you’re a seasoned dodgeball pro, a newcomer to the game, or a spectator, don’t miss this opportunity to watch EM’s best “dodgers” duck, dip, and dive in this thrilling face-off for the right to call themselves dodgeball champs!
Interested in Participating?
Registration is required to participate in Dodgeball at SAEM24. This popular event typically fills quickly, so be sure to register as soon as possible.
Taking place May 14-17, 2024, SAEM24 will be held in Phoenix, Arizona. With more than 1,000 educational sessions, presentation opportunities, and valuable networking, you won’t want to miss this essential event. These links will help you navigate the general information you need to know.
• Pricing and Registration
• Schedule-at-a-Glance
• SAEM24 FAQs
• Accessibility
• For International Travelers
Friday, May 17, 8:00 AM to 1:00 PM MT

SonoGames® is a national ultrasound competition in which emergency medicine (EM) residents demonstrate their mad skills and knowledge of point-of-care ultrasound in an exciting and educational display of expertise and camaraderie. Experience the exhilarating winner-takes-all showdown as teams of over 300 emergency medicine residents in crazy costumes engage in a no-holds-barred battle in front of a captivated audience. Don’t miss the thrilling spectacle as they demonstrate their mastery of “SonoSkills” in their quest to be crowned “SonoChamps” and claim the coveted “SonoCup.”
Interested in Participating?
Each residency program is allowed a single team made of three residents. Only one person from each team should register for SonoGames®

All of the following events take place inside the SAEM24 exhibit hall.
Tuesday, May 14
5:00 PM - 6:00 PM MT Kickoff Party
Wednesday, May 15
7:00 AM - 9:00 AM MT
Exhibit Hall Open
11:00 AM - 4:00 PM MT
Exhibit Hall Open
5:30 PM - 7:30 PM MT
Opening Reception
Thursday, May 16
7:00 AM - 1:00 PM MT
Exhibit Hall Open
View the SAEM24 Exhibitor Prospectus for details, including information about add-ons and sponsorship opportunities to increase your visibility and maximize your exhibitor experience. Contact exhibitors@saem.org or call Bill Schmitt, manager, exhibits and sponsorships, at (847) 257-7224.
3,800 (+4) Reasons Why You Should Exhibit at SAEM24!
The SAEM Annual Meeting is the ultimate gathering of emergency medicine's brightest minds! Be part this premiere event as we welcome 3,800+ thought leaders, innovators, and early adopters to SAEM24. Reserve your exhibit space today!
1. Unparalleled Exposure: Connect with 3,800+ influential minds, from prestigious medical schools and teaching institutions, all eager to explore cutting-edge research, educational content, and the latest innovations.
2. Academic Excellence: SAEM is the academic powerhouse of emergency medicine, leading the way in research, education, and professional development. Our 8,400+ members, including department chairs, residents, fellows, researchers, and educators, are influential leaders shaping the future of emergency medicine worldwide.
3. Premier Networking: Engage with decision-makers and influencers who publish scholarly articles, serve on governing bodies, and act as role models for the next generation of emergency medicine practitioners. The SAEM Annual Meeting is where academic emergency medicine gathers to learn, connect, and advance the specialty.
4. Proven Growth: The SAEM Annual Meeting has steadily grown each year, now attracting over 3,800 attendees. This premier venue is where professionals seek highquality research, education, and innovations in products and services. Don't miss the opportunity to be part of this thriving community!
Wednesday, May 15, 3:30 PM to 5:20 PM MT
Experience the dynamic synergy of Speed Mentoring, where resident and medical student mentees are strategically matched into small groups of 5-10 attendees who share common interests. You’ll engage in rapid, 10-minute mentoring sessions that offer a unique platform to kickstart valuable connections. This event not only provides an avenue to establish mentoring relationships with professionals nationwide but also encourages networking and socialization among fellow residents and medical students.
Mentors needed!
If you are interested in serving as a mentor for this event, sign up when you register for the annual meeting.
Thursday, May 16, 11:00 AM to 11:50 AM MT
Speed Mentoring for Medical Educators offers faculty members an opportunity to engage in concise yet insightful discussions with seasoned mentors who possess significant expertise and experience in medical education. This unique event allows participants to explore potential mentoring relationships, ultimately helping them identify a medical education mentor whose experience and personality aligns with their professional interests, desired career trajectory, and individual personality traits.
Mentors needed!
If you are interested in serving as a mentor for this event, sign up when you register for the annual meeting.
This spring, at SAEM24 in Phoenix, Ariz., we will take a moment to honor and remember our SAEM friends and colleagues who have departed in the past year. We invite submissions of names for the individuals who have passed away since April 1, 2023, to be included in an "In Memoriam" video tribute showcased during the SAEM24 opening session. Please contribute your "In Memoriam" submissions, including the individual's name, institution, and a photo, to Stacey Roseen at sroseen@saem.org by April 3, 2024.
Experience the full benefits of the SAEM24 annual meeting by entrusting the care of your child(ren) (infant through age 12) to Jovie's team of professionals. You can enjoy and participate in the event with peace of mind, knowing that your child(ren) are being well cared for through our onsite childcare/day camp. Reserve your spot by March 12 to ensure a worry-free experience for both you and your little ones.
Thursday, May 16, 3:00 PM to 5:00 PM MT

Explore dozens of residency and fellowship programs from across the nation, all conveniently gathered under one roof at the 2024 SAEM Residency & Fellowship Fair (RFF). Engage with representatives coveted programs who are eager to talk to you about their programs and provide invaluable insights to guide you through the application process. Connect with current residents and fellows to ask questions and gain valuable advice and encouragement to navigate the next steps in your career journey. This event is free for residents and medical students registered for SAEM24, so be sure to take full advantage of this opportunity to visit as many programs as your schedule permits!
The SAEM Residency & Fellowship Fair (RFF) provides a streamlined, cost-effective recruitment opportunity, reaching hundreds of potential candidates in a single event, saving you valuable time and resources. The fair encourages interactive discussions for candidates to ask questions, gain program insights, and make informed decisions, helping you assess their suitability more clearly. Choose from THREE cost-effective options: 1.) our live event at SAEM24 on May 16, 2024, 2.) our virtual event, July 22-25, 2024, or 3.) opt for both and save! Learn more and register your program today!
The SAEM Annual Meeting offers a unique and enriching experience for emergency medicine residents and medical students. Here are several compelling reasons that underscore the value of attending:

1. Networking Opportunities:
SAEM meetings gather professionals, educators, and researchers in the field of emergency medicine. Attending allows residents and medical students to connect with experienced individuals, mentors, and potential collaborators.
2. Learning and Education:
The SAEM annual meeting provides a platform for the latest research, advancements, and best practices in academic emergency medicine. Attendees have access to a diverse range of educational sessions, workshops, and didactics that can enhance their knowledge and skills.
3. Exposure to Research and Innovation:
The annual meeting showcases cutting-edge research and innovations in emergency medicine. This exposure can inspire residents and students, offering insights into potential areas of interest for research projects or career paths.
4. Career Development:
SAEM meetings include events and activities that offer career development, mentorship, and advice for navigating the challenges of academic emergency medicine.
5. Access to Experts:
The event brings together experts and thought leaders in emergency medicine. Attending provides an opportunity to interact with these professionals, ask questions, and gain insights that might not be easily accessible elsewhere.
6. Stay Informed about Industry Trends:
SAEM meetings cover the latest trends, policies, and changes in the field of emergency medicine. Staying informed about these developments is crucial for those planning to build a career in this dynamic and evolving specialty.
7. Fellowship and Residency Programs:
The annual meeting is an excellent opportunity to learn about different emergency medicine fellowship and residency programs. Residents and medical students can explore options, gather information, and make informed decisions about their future training.
8. Collaboration Opportunities:
SAEM meetings provide a collaborative environment where residents and students can interact with peers from other institutions. This fosters the exchange of ideas, collaboration on projects, and the building of professional relationships.
9. Inspiration and Motivation:
Being surrounded by passionate individuals in the field is inspiring! The meeting can motivate residents and students by showcasing the impact they can have within academic emergency medicine.
10. For the Fun of It!
Renowned for its exciting atmosphere, contagious energy, and lively camaraderie, the SAEM Annual Meeting guarantees an extraordinary, unforgettable, and fun experience for residents and medical students.
• Medical Student Symposium
• Chief Resident Leadership Forum
• Speed Mentoring
• Residency and Fellowship Fair
• AWAEM and ADIEM Luncheon
• Cocktails with Chairs
• Dodgeball
• Simulation Academy SimWars
• SonoGames®
• SAEM RAMS Hunt
• Advanced EM Workshops
• Didactics
• Clinical Images Exhibit
• IGNITE!
• Innovations
• Dr. Peter Rosen Memorial Keynote
• Education Keynote Pro Tip
When you spot the RAMS head icon next to a listing in the SAEM24 Program Planner, you'll know that it's an event you’ll find value in attending as a resident and/or medical student.
Thursday, May 16, 10:00 PM MT

When it comes to throwing unforgettable parties, SAEM's residents and medical students (RAMS) are in a league of their own. And this time, we're taking the celebration to the extraordinary setting of The Duce in Phoenix!
Housed in a revitalized historic warehouse within the former speakeasy district of Phoenix, The Duce oozes with character. Picture this: you with your elbows on the actual bar transplanted from the iconic The Black Orchid nightclub in Chicago where Rat Pack legends like Sammy Davis Jr. and Frank Sinatra once partied. It’s old-school cool with a modern twist!
The Duce has all the ingredients for an unforgettable night on the town: an open bar, an inviting dancefloor, and live music all set in a space with loads of industrial-chic and just the right touch of vintage allure. There’s no cover charge and all SAEM24 attendees are invited, so step with us into this playground for the senses, where nostalgia meets cutting-edge entertainment, and let your inner child run wild.
Accepting VIP Table Reservations
Everyone is invited to the party, but our special VIP tables for faculty and residents are limited and go fast, so if you’re interested you should reserve a table real soon! Questions? Contact Bill Schmitt at wschmitt@saem.org or 847-257-7224.
Wednesday, May 15, Noon MT
AstraZeneca
Title: Management of FXa Inhibitor-Related LifeThreatening or Uncontrolled Bleeding
Speaker: Lionel Picot-Vierra, PharmD, Medical Science Liaison AstraZeneca Pharmaceuticals LP Inflammatix
Title: Revolutionizing the Diagnosis of Acute Infection and Sepsis with Cutting-Edge Host Response Diagnostics
Speaker: TBD
Thursday, May 16 at Noon MT
Abbott
Title: Evaluation and Management of Traumatic Brain Injury with Blood Biomarkers
Speaker: TBD


PHOENIX, AZ • MAY 14-17

By Elina Kurkurina, MPH, and Tehreem Rehman, MD, MPH, MBA, on behalf of the SAEM Administration and Clinical Operations Committee
It is widely acknowledged that diversity, equity, and inclusion within health care teams is vital for the well-being of patients, trainees, and practicing clinicians. Despite this recognition, there is a persistent underrepresentation of physicians from diverse racial and ethnic backgrounds in medicine. The 2022 Physician Specialty Data Report by the Association of American Medical Colleges reveals that only 6.1% of emergency physicians identify as Hispanic, 4.9% as Black or African
American, and 0.4% as American Indian or Native Alaskan. This is in contrast to the respective 19.1%, 13.6%, and 1.3% of the U.S. population identifying with these backgrounds. Establishing a diverse and inclusive environment in emergency departments can improve patient outcomes, satisfaction, and the learning environment for trainees.
Workforce Diversity Can Improve Patient Satisfaction and Health
Racial and socioeconomic disparities continue to exist in the processes and outcomes of emergency department
care. From triage to treatment, minority and low-income patients face a higher likelihood of experiencing queue jumps, being placed in hallways, and leaving the facility before receiving attention from a health care provider, in contrast to white patients with equivalent acuity ratings. Likewise, when it comes to black patients experiencing undifferentiated abdominal pain, there is a lower likelihood of them receiving narcotic pain management compared to their white counterparts.
Pediatric emergency departments also exhibit disparities, with black

“Establishing a diverse and inclusive environment in emergency departments can improve patient outcomes, satisfaction, and the learning environment for trainees.”
children receiving suboptimal pain reduction compared to white children. Patients with limited English proficiency experience higher rates of diagnostic testing, stress testing, and increased admission rates upon returning to the ED within seven days. Black male patients facing a ST-segment Elevated Myocardial Infarction have lower odds of receiving timely door-to-balloon care. Diverse workforce representation, particularly among primary care physicians, has been shown to contribute to improved patient outcomes and reduced mortality differences between racial groups.
Having a diverse workforce can expand access to high-quality, culturally sensitive
care for racial, ethnic, and linguistic minorities, leading to improved patient outcomes. Prior research indicates that racial and ethnic minority primary care physicians tend to serve a higher proportion of minority, low-income, uninsured, and historically underserved patients. Additionally, a recent study found that a 10% increase in the representation of Black primary care physicians was linked to a 1.2% decrease in all-cause mortality differences between Black and white patients. Patients treated by racially concordant physicians have reported higher satisfaction compared to those treated by racially disconcordant physicians. These findings underscore the importance of a diverse workforce, providing patients with more choices for accessible and preference-aligned care.
While there is a lack of similar research on racial bias among emergency medicine physicians, it is essential to recognize that emergency medicine residents and recent graduates are not exempt from racial bias Given the limited representation of emergency physicians from racial or ethnic minorities, actively recruiting a diverse workforce becomes crucial to mitigating implicit bias and enhancing patient outcomes, as well as the overall performance of the department on critical process and outcome measures. Consequently, it is imperative for emergency department

“Having a diverse workforce can expand access to high-quality, culturally sensitive care for racial, ethnic, and linguistic minorities, leading to improved patient outcomes.”
ADMINISTRATION
continued from Page 25
leaders to prioritize investments in the development, recruitment, and retention of a diverse workforce.
The development, recruitment, and retention of a diverse emergency medicine workforce should start early in the educational process. Students often emphasize the positive impact of acting internships, elective rotations, and core clerkships on their specialty interests and career choices. Collaboration between emergency department leaders and clerkship directors is essential to establish an
environment that prioritizes diversity, equity, and inclusion, to mitigate assessment bias. Clerkship grades, more subjective and susceptible to bias compared to pre-clinical years, can be influenced by racial bias, as observed in standardized assessments like the emergency medicine standardized letter of evaluation “rank against peers” and “grade” sections.
Historically, the training environment has not been conducive for minority students, who have faced implicit bias, microaggressions, and mistreatment throughout their training. To address this, measures such as the use of grading committees, broadening access to question banks, providing implicit bias training for students and faculty, recruiting diverse staff, and maintaining
a commitment to ongoing quality improvement have been proven effective in minimizing grading disparities for minority students during clinical rotations.
Recruiting and retaining diverse faculty members are crucial for addressing the “leaky pipeline” in medical education, allowing students to benefit from mentorship, advising, and opportunities. However, recruiting a diverse faculty alone is not enough. Medical students closely observe interactions among faculty members for cues regarding acceptable professional behavior. One study revealed that female students, minority students, and those identifying as lesbian, gay, or bisexual reported
“Diverse teams play a pivotal role in enhancing the delivery of equitable care in the emergency department, ultimately resulting in improved patient outcomes and satisfaction.”
witnessing instances lacking respect for diversity among faculty members. Such actions, including inappropriate humor and discriminatory remarks, can significantly impact the learning environment and subsequently influence students’ performance on assessments.
These issues also extend to emergency medicine trainees, attendings, and faculty members. Junior emergency medicine residents emphasize the importance of authenticity and representation when evaluating potential residency programs; yet, fewer than half of emergency medicine training programs employ at least two strategies aimed at recruiting a diverse class of residents. Racial disparities also persist in faculty promotions, with only 7% of associate professors and less than 6% of full professors in emergency medicine being minorities. Recognizing the contributions of diverse team members, particularly those from historically marginalized backgrounds, to improving care delivery is crucial. Traditionally, such efforts are relegated to service or volunteer work without adequate inclusion in promotion advancement processes, protected time, or resources.
Diverse teams play a pivotal role in enhancing the delivery of equitable care in the emergency department. By improving the training environment, there is an opportunity to boost workforce diversity, ultimately resulting in improved patient outcomes and satisfaction. Additionally, shared experiences among team members can foster empathy, particularly among physicians from historically marginalized backgrounds who often have to navigate challenging situations and discrimination regularly and may develop higher emotional IQ as a result.
Moreover, different lived experiences foster a diversity of thought and innovation, aspects that are not adequately captured by existing standardized tests. This lack of
representation in assessments can exacerbate disparities within the physician workforce. Importantly, these diverse perspectives become increasingly vital in the context of growing health care provider burnout, offering unique insights and solutions to address the challenges faced in the healthcare environment.
Considerable efforts have been made by minorities in medical leadership, offering a valuable template for effectively increasing diversity in workforce recruitment and retention. This, in turn, can lead to tangible improvements in equity and the quality of care delivered in the emergency department. Ultimately, the onus for ensuring equitable care should not solely rest on providers from historically marginalized backgrounds. To address this, we suggest adapting existing quality measure frameworks for emergency department leaders. Below are some examples that can serve as a guide in this endeavor.
In alignment with the White Coats 4 Black Lives Hospital Report Card, emergency department leaders have the opportunity to make a commitment to collecting, monitoring, and reporting disparities data. These metrics should encompass various aspects, such as the implementation of bias mitigation policies for clerkship grading, allocation of residency curricula time dedicated to examining racial disparities in emergency care, existence of bias reporting mechanisms for physicians, staff, and trainees, and the percent of representation of assistant, associate, and full professors from underrepresented groups in medicine.
These reports should be closely correlated with the performance on measures and processes that are known to exhibit racial disparities. These include queue jumps, hallway placement, departures against medical advice, pain management, and door-to-balloon time. The goal is to create a comprehensive and transparent approach to addressing disparities within the emergency
department and fostering an environment committed to equity.
Emergency department leaders dedicated to addressing disparities in their departments should collaborate with colleagues at every stage of the process. This collaboration should involve partnering with clerkship directors, residency program directors, nursing leadership, social work, and case management to comprehensively address these issues. To guide these efforts, leaders can adopt a roadmap, similar to Mount Sinai’s, to align priorities and establish shared goals.
Furthermore, a reporting dashboard can be instituted and shared with team members. This tool aims to generate actionable data, fostering accountability among all team members for supporting diverse teams. Ultimately, the objective is to enhance care delivery in emergency departments by continuously monitoring progress and addressing disparities proactively

Elina Kurkurina is a secondyear medical student in the Healthcare Management and Organizational Leadership concentration at the Frank H. Netter MD School of Medicine at Quinnipiac University. She holds an MPH degree in Social and Behavioral Sciences from the Yale School of Public Health.

Dr. Rehman is an assistant professor and assistant medical director in the department of emergency medicine at Mount Sinai Hospital. She has a nationally recognized and published track record in work on clinical operations, social drivers of health, quality improvement, transitions of care, informatics, and reimbursement policy.

By Casey M Clements, MD, PhD, on behalf of the on behalf of the SAEM Consultation Services Committee and the SAEM ED Administration and Clinical Operations Committee
In the early history of emergency medicine (EM), the term "emergency room" aptly described the practice of emergency care in hospitals. A nurse, a doctor trained in any specialty, and a few medications constituted the resources available for treating emergencies. Quality evidence for emergency care was lacking, and patients received the best efforts of those who preceded and founded our specialty. Patients often sought care through their family doctors, delaying access to emergency rooms, for better or worse. This scenario is a far cry from the practice of emergency medicine in
“Now, more than ever, it is evident that emergency department operations are inextricably linked to the success of academic missions in education and research.”
the third decade of the 21st century.
Fortunately, EM has evolved. "emergency rooms" transformed into emergency departments (EDs), staffed with EM residency-trained physicians providing evidence-based
care to improve patient outcomes. The public now recognizes the value that emergency medicine adds to their care, leading to frequent utilization of EDs. Throughout the initial 40 years of our specialty, EM adapted and established operational practices that serve our
patients while also furthering education and research that advance the field of EM. Until recently, we had relatively stable models for administration of departments with most changes centered around growth and efficiency to accommodate more patients.
However, these past few years have presented unprecedented challenges to EM. While it is tempting to attribute these changes solely to COVID-19, health care delivery is complex. The pandemic may have initiated alterations in health care, but its impact extends beyond the treatment of a pandemic virus. Undoubtedly, the pandemic posed challenges that disproportionately affected EDs, thrusting them into the frontline and the headlines. The ED assumed a central role in health care for the first time in our specialty's history, briefly hailed as “health care heroes.” What was not immediately apparent was the fundamental changes occurring within health care and the public.
Health care delivery systems have experienced significant strain in recent years. Many staff left health care during the pandemic or took lucrative temporary positions. Patient access to health care has become more challenging. The disease burden of chronic illness management and conditions of isolation, such as mental health and chemical use disorders, has risen. Patient trust in reliable health care has eroded. Health care financing has undergone significant fluctuations, transitioning from a scenario marked by private insurers and Medicare, along with a substantial number of uninsured patients. It then shifted to increased Medicaid coverage and temporary government funding during the pandemic. Subsequently, there was a return to Medicaid cuts, accompanied by a resurgence in the number of uninsured patients. The net result is that EDs have been tasked with doing much more with much less. While EDs struggled through this new reality, education and research priorities have often suffered.
Now, more than ever, it is evident that ED operations are inextricably linked to the success of academic missions in education and research. Teaching at the bedside to students, residents, and fellows depends on the volume and acuity of patients in a conducive clinical environment. The challenge is apparent: how can we train the next generation of emergency physicians when our time
To address the challenges and changes of emergency care in 2024 and beyond, SAEM has launched the Operations Consultation. Developed over several years by experts in ED operations, SAEM’s newest consultation service is tailored to meet the needs of any academic ED. These expert consultations are customized to the specific needs of the department, including:
• Data use/analysis
• Matching capacity and demand –volume, acuity, & complexity
• Physician retention
• Schedule optimization
• Incentive plans, reimbursement, and workload analysis in academic centers
• Throughput/patient flow optimization
• Alignment with groups outside of the ED
Here's how it works:
• Change management
• Learner integration strategies
• Clinical research integration strategies
• Managing patient experience in an academic setting
• Meeting publicly reported quality metric goals
• Workforce optimization
• Physician/nursing alignment and integration
• And more!
1. Any interested department can request a consultation by sending an email to dray@saem.org.
2. SAEM will then send a brief form to determine the department's needs, how they can help, and the costs of consultation.
3. The Society will assemble a customized consultant team to address the focus of that ED.
4. The SAEM consultation team will virtually meet with the client ED to understand the current state, organizational outline, and available data.
5. This will prepare the consultation team for a 2-day on-site consultation to review processes, interact with frontline staff and ancillary leadership, and model tabletop patient tracers to better understand the issues and potential solutions.
6. At the end of the second day, the team, along with ED leadership, will conduct a high-level debrief with findings and discuss possible solutions.
7. After the consultation visit, findings and suggestions will be delivered in writing to the ED and their institution on behalf of SAEM.
Learn More!
and space are occupied with boarding patients? How can we screen patients for research studies when they wait for hours to be triaged and roomed? A higher rate of patients leaving without being seen is detrimental to both patient care and the academic mission.
Emergency medicine has been through a lot recently. It is time to work together to move academic EM in the right direction and advance emergency care to meet the new reality of health care in 2024. SAEM Operations Consultation Services is one new option to help move academic EM in the right direction

Dr. Clements is a consultant physician and associate professor of emergency medicine at the Mayo Clinic in Rochester, Minnesota. Having served as clinical practice chair for the department of emergency medicine for several years, he now works in quality improvement, including large-scale interdepartmental and interdisciplinary practice improvements.

By Michael Stone, MD; Michael J DeFilippo, DO; Shriman Balasubramanian, DO; and Gabriela Galli, MD
Out-of-hospital cardiac arrest (OHCA) poses a significant public health challenge, both in the United States and globally, impacting hundreds of thousands annually with an overall survival rate of less than 10%. Cardiac arrest care witnessed substantial advancements in the 1960s to 1980s through the standardization of CPR and prehospital defibrillation. Since then, progress has primarily focused on other elements of the chain of survival. Public education regarding automated external defibrillator (AED) use and bystander cardiopulmonary resuscitation (CPR) has enhanced outcomes by prompting
“Out-of-hospital cardiac arrest poses a significant public health challenge, both in the United States and globally, impacting hundreds of thousands annually with an overall survival rate of less than 10%.”
bystanders to initiate CPR before EMS arrival. In-hospital care saw the widespread adoption of percutaneous
coronary intervention in the 1990s, leading to improved outcomes for post-arrest patients with durable return

of spontaneous circulation. However, novel treatment modalities were limited until the emergence of extracorporeal cardiopulmonary resuscitation (ECPR) in resuscitation paradigms over the past decade.
ECPR's growth began in the 1990s, employing veno-arterial extracorporeal membrane oxygenation (VA-ECMO) as a bridge to definitive care, typically percutaneous coronary intervention (PCI). Initially used for refractory in-hospital cardiac arrest in large academic medical centers, ECPR has gradually expanded to encompass broader cardiac arrest populations. Initial retrospective analysis of its application in out-of-hospital cardiac arrest (OHCA) during the 2000s yielded mixed results with no clear benefit. Nevertheless, over the following decade, its utilization grew, and mid-2010s analyses indicated improved outcomes in OHCA patients with a primary cardiac etiology.
These positive findings prompted the collection of prospective data on ECPR's use for OHCA. The first randomized control trial (RCT) in the United States, focused on refractory ventricular fibrillation/tachycardia OHCA. The results were promising, revealing an impressive 43% rate of neurologically-intact survival to hospital discharge. International RCTs in Prague (Belohlavek et al., 2022) and the Netherlands (Suverein et al., 2023) explored different patient populations but failed to demonstrate a significant
survival benefit. They attempted to broaden included patient populations by considering all refractory OHCA of presumed cardiac origin regardless of initial rhythm (Prague) and whether the initial ventricular rhythm had to be sustained or not (Netherlands).
Despite the initial mixed results, critical analysis of the data revealed crucial trends toward benefit. Optimal outcomes were observed with a shorter time to extracorporeal membrane oxygenation (ECMO) flow and in patients with refractory shockable rhythms. In the United States, several new academic prehospital ECPR programs have emerged, incorporating these lessons into their protocols. Some prehospital entities directly cannulate in the field, while others prioritize transport to ECMOcapable centers for specific indications, such as refractory ventricular fibrillation.
The future trajectory of cardiac arrest care relies on robust, generalizable data. Ongoing pragmatic studies hold the potential to usher in a new standard of care, potentially saving lives within a specific population of OHCA patients. ECPR, in particular, holds promise as a bridge between prehospital CPR and definitive cardiac care. The evolution and future of ECPR are particularly exciting, with advancements pointing towards broader accessibility in both in and out of hospital settings. Additionally, the development of more portable ECMO machines looks to extend its life-saving
potential to prehospital environments. As we await more conclusive findings, the emphasis remains on generating data that can bring about lasting and meaningful changes in patient care.




Dr. Stone is a fourth-year emergency medicine resident at NewYork-Presbyterian Columbia & Cornell. He is a former emergency medical technician (EMT).
Dr. DeFilippo is a chief resident in emergency medicine at NewYork-Presbyterian Columbia & Cornell and former paramedic. He is currently the resident member of the SAEM Board of Directors.
Dr. Balasubramanian is a third-year emergency medicine resident at NewYorkPresbyterian Columbia & Cornell. He is a former EMT from Poughkeepsie, NY.
Dr. Galli is a second-year emergency medicine resident at NewYork-Presbyterian Columbia & Cornell. He is a former paramedic.

By Dave Tillman, MD, on behalf of the SAEM Clerkship Directors in Emergency Medicine academy
Our team has been diving into the world of away rotations, giving advice to our home students, and sifting through applications from eager visitors. As I mull over the whole process, I'm caught between seeing the perks and potential downsides of sending our students on these adventures. Spoiler alert: I'm “pro” away rotation, but with a cautious eye, because, as Tolkien wisely said, "advice is a dangerous gift… and all courses may run ill." As I navigate the coming months from my students' point of view, here are a few thoughts:
Benefits of Away Rotations
Diversity of Learning Opportunities
Away rotations immerse our medical
students in diverse medical practice settings, patient populations, and health care systems. These rotations are like crash courses in adaptability and flexibility — crucial skills vital for our students’ future careers. Plus, let's not forget that the whole experience can be a blast!
With virtual interviews becoming the norm, away rotations can provide a unique window of opportunity for students to explore a program, city, or health system to see if it aligns with their expectations. The way they perceive faculty and learner interactions during this period can significantly

influence their rank lists. Additionally, away rotations provide students with an opportunity to showcase their own qualities that may not be readily evident on their ERAS applications.
While our local Standardized Letters of Evaluation (SLOEs) strive to fairly evaluate our students, an away SLOE serves as a crucial second opinion from an independent evaluator. In emergency medicine (EM), away rotations hold more weight than in any other specialty. This secondary SLOE provides an opportunity for students to demonstrate their career trajectory and enhance their overall narrative.
Visiting Student Learning Opportunities (VSLO) costs for away rotations are manageable, but the overall financial burden extends beyond application fees. The most recent away rotation cost estimate I encountered (in 2016) was approximately $1,000 per rotation. It's essential to consider whether


recommending away rotations carries a different weight for students with financial safety nets in comparison to those without. Despite the overall decrease in application costs attributed to virtual interviews, the financial impact of away rotations that is felt by over 50% of medical students with parents in the top quintile of wealth, is likely different from that experienced by some of their peers.
The time invested in away electives means less time for fulfilling graduation requirements. Committing to away rotations may inadvertently push students into a pseudo-commitment to a specific specialty early in the season, potentially limiting their exploration of other options. Finally, consider how our students are managing an increasingly complex ERAS cycle during this high-stakes away month.
Statistically, students participating in away rotations receive SLOEs with lower ratings compared to their home ratings. Given how savvy program directors (PDs) and review committees are, this may not be a significant issue, but it's definitely a source of stress for our students.
In conclusion, despite the associated costs and considerations, I’d say away rotations are beneficial for students, particularly in this age of virtual interviews, which reduce costs and in-person exposure. Never mind that away rotation are “standard” in the minds of PDs. If there were a magic wand to redesign the system, it might look different; however, as wisely stated by Tolkien, "all we have to decide is what to do with the time that is given us."

Dr. Tillman is director of medical student education in the department of emergency medicine at the University of Wisconsin. He has a passion for advising students and helping them reach their best. He has led educational initiatives and courses throughout all phases of medical school. He serves as a member-at-large on the executive committee of the Clerkship Directors in Emergency Medicine (CDEM).
Clerkship Directors in Emergency Medicine (CDEM) represents the interests of undergraduate medical educators in emergency medicine. It serves as a unified voice for EM clerkship directors and medical student educators and provides a forum for them to communicate, share ideas, and generate solutions to common problems. For more information, visit the CDEM webpage Membership in SAEM's academies and interest groups is free. To participate in one more groups: 1.) log into SAEM.org; 2.) click “My Participation” in the upper navigation bar; and 3) click “Update (+/-) Academies or Interest Groups.”

By Emily Wang, Ella Grann, and Kyle Denison Martin, DO, MPH, on behalf of the SAEM Climate Change & Health Interest Group
Climate change is altering the course of aquatic ecosystems and introducing new diagnostic concerns across the United States. The consequences of fossil fuel consumption, overfishing, and other anthropomorphic effects have exacerbated climate change, creating conditions conducive for unopposed growth of organisms. Warmer waters, altered salinity levels, and excess nutrient runoff are some of the many factors fueling the expansion of organisms in new, unexpected regions.
Among the many public health risks are water-borne bacterial infections like Vibrio Vulnificus and Harmful Algal Blooms (HABs), in addition to an uptick in Atlantic sea nettles,
sharks, and stingrays. In the United States, Northeastern coastal regions in particular face distinct challenges as modeled by recent studies. Florida and California will also face new aquatic threats in the decades to come.
This article serves as an overview on the diagnosis, treatment, and prevention of these aquatic threats to increase awareness amongst health care providers as cases are expected to rise with climate change.
Vibrio Vulnificus
V. Vulnificus is a bacterium that can be transmitted through the consumption of raw seafood, particularly oysters, or exposure of open wounds to
contaminated waters, such as swimming in infested waters. During the summer of 2022, the New England coast reported two deaths due to wound infections and one due to consumption. Alarmingly, V. vulnificus infections account for 95% of seafoodrelated deaths in some reports, with wound infections having an 18% mortality rate. The geographical expansion of reported V. vulnificus infections is also concerning, with the northern boundary stretching from Georgia to Connecticut since the 1980s.
Timely diagnostic confirmation is paramount for initiating appropriate treatment. This entails sending samples

“V. Vulnificus infections account for 95% of seafood-related deaths in some reports, with wound infections having an 18% mortality rate.”
of stool, blood, and/or wound tissue for analysis. In milder instances of foodrelated gastroenteritis, the illness tends to be self-limiting and can be effectively managed with supportive care. However, wound infections can vary from mild cellulitis to severe tissue damage and potentially fatal outcomes such as necrotizing infections and bacteremia. More serious cases require administering a third-generation cephalosporin in combination with doxycycline or a fluoroquinolone. Pediatric cases often benefit from trimethoprimsulfamethoxazole with an aminoglycoside to mitigate side effects. Tetanus vaccination should be administered when indicated. Failure to promptly address acute infections, particularly those related to wounds, may necessitate more invasive interventions such as fluid
drainage, surgical debridement, or, in extreme scenarios, amputation.
Prevention of V. vulnificus infections entails avoiding the consumption of raw shellfish, ensuring thoroughly cooked seafood, promptly bandaging open wounds, refraining from swimming with cuts, and diligently cleaning wounds that may have been exposed to contaminated waters.
Harmful Algal Blooms (HABs) are characterized by the vibrant overgrowth of bacteria in freshwater bodies, presenting significant health risks through direct contact or ingestion of contaminated water and aquatic organisms, notably shellfish.
Domoic acid and saxitoxin are two neurotoxins produced by HABs and
accumulate within shellfish feeding on the algae. Symptoms of toxin poisoning range from gastrointestinal (GI) distress to confusion, paralysis, coma, and, in severe cases, death. Skin, eye, nose, and respiratory irritation may also be found.
In cases of toxin exposure, activated charcoal may be administered within the first hour to mitigate absorption, while atropine has demonstrated efficacy in addressing saxitoxin exposure. However, there is currently no standardized treatment for HAB toxin infections, underscoring the importance of avoiding further exposure. Additional recommendations include promptly washing exposed skin and eyes and cleaning contaminated clothing.

“In cases of toxin exposure [from Harmful Algal Blooms], activated charcoal may be administered within the first hour to mitigate absorption, while atropine has demonstrated efficacy in addressing saxitoxin exposure.”
CLIMATE CHANGE
continued from Page 35
To minimize risk of infection, individuals should avoid drinking water while swimming or consuming shellfish from affected areas. Authorities may impose restrictions on certain freshwater systems if HAB infections pose a significant risk, as evidenced by past bans on shellfish harvesting in regions like the Gulf of Mexico and Narragansett Bay due to elevated concentrations of toxins in shellfish populations.
Atlantic sea nettles (Chrysaora
quinquecirrha) are jellyfish characterized by their distinctive yellow-orange bell and long tentacles. They inhabit temperate waters, including oceans, bays, and brackish waters. In 2021, the Rhode Island Department of Environmental Management reported a significant increase in the Atlantic sea nettle population within salt ponds, prompting warnings to swimmers and temporary beach closures.
The venom from sea nettle stings induces a burning pain on the skin at lower concentrations. However, at higher concentrations, the venom can lead to more severe systemic reactions, including hepatic, cardiovascular,
respiratory, and renal injuries.
Treatment for sea nettle stings involves thorough irrigation of the affected area with seawater. Some studies suggest applying baking soda to the wound site to alleviate pain and inhibit nematocyst discharge. Additionally, hot water immersion (40-45°C) or hot packs can help reduce pain and swelling. Patients with localized urticaria may benefit from topical steroids or oral antihistamines. While anaphylaxis is rare, patients exhibiting signs should receive immediate intramuscular epinephrine and be closely monitored in a healthcare setting.
“Patients often cannot identify the type of shark that attacked them, but the approach to treatment remains consistent for all shark bites. In cases of significant bleeding, applying pressure is crucial, and surgery may be necessary.”
Notably, traditional treatments for other jellyfish stings, such as using vinegar to remove stingers, are not recommended as they may trigger further nematocyst release. Similarly, urinating on the sting site has been disproven as a treatment and can exacerbate pain.
In general, jellyfish stings can be prevented by wearing wet suits, being cautious of swimming locations, and using lotions designed to protect against stings.
Numerous shark species are endangered, resulting in no overall increase in shark populations. Nonetheless, rising ocean temperatures have prompted many shark species to migrate northward as their habitats become unsuitably warm. As a consequence, sightings of Great White Sharks, once primarily confined to Southern California, have occurred along the northern California coast. Since the 1950s, shark attacks have escalated, reaching a peak in 2015 with nearly one hundred incidents recorded. Although shark attacks are uncommon, healthcare providers and swimmers should maintain vigilance.
Shark attacks can result in a spectrum of injuries, ranging from mild to fatal. Patients often cannot identify the type of shark that attacked them, but the approach to treatment remains consistent for all shark bites. In cases of significant bleeding, applying pressure is crucial, and surgery may be necessary. Thoroughly cleaning the wound area is essential to prevent infection. For deep or extensive wounds, antibiotics may be prescribed, typically a third-generation cephalosporin in combination with doxycycline or a fluoroquinolone.
Prevention strategies for shark attacks include monitoring swimming areas closely, avoiding swimming in areas known for shark activity (especially if currently bleeding or menstruating), swimming in groups, limiting swimming
to daylight hours, and refraining from wearing shiny jewelry.
For a more comprehensive understanding of shark bite types and treatments, healthcare professionals can refer to resources such as “Summer of the Sharks: Managing Shark Bites in the ED.”
Stingrays pose a threat to humans through contact with their venomous tails, commonly resulting in stings on the legs or feet. While these attacks are typically not severe, allergic reactions can present as respiratory issues, itchiness, and vomiting. Similar to shark bites, patients should monitor for signs of infection following a sting.
Instances of stingray-related incidents, such as the seventy-eight cases reported in a single day in 2018 at Huntington Beach, California, underscore the need for heightened awareness and precautionary measures. Furthermore, recent sightings of large Roughtail Stingrays in unexpected regions, like the Long Island Sound, highlight the shifting distribution patterns of these marine creatures and encourage greater work to mitigate human-stingray encounters.
In all cases, meticulous cleaning of the infection site is essential, accompanied by the application of localized pressure if bleeding occurs. Soaking the affected area in hot water (40-45°C) can alleviate pain, and any embedded pieces of the stingray spine should be carefully removed. Depending on the severity, antibiotics or a tetanus shot may be warranted. Antibiotic coverage should account for possible Vibrio infection (see above).
Preventive measures against stingray attacks include wearing protective footwear and exercising caution in areas known for high stingray activity.
The United States is poised to experience heightened marine-related threats due
to the influence of climate change. Recognizing these potential hazards can assist healthcare providers, public health workers, and policymakers in their endeavors to mitigate adverse impacts on human health. Maintaining vigilant oversight, promoting education, and enforcing preventive measures are imperative strategies for addressing the escalating health risks posed by marine organisms in the context of climate change.

Emily Wang is a second-year medical student at the Warren Alpert Medical School (AMS) at Brown University. She is passionate about climate change and sustainability in medicine and currently leads planetary health initiatives and interests groups at AMS.

Ella Grann is a student in the science research program at Rye Neck High School with prior research experience in cardiovascular health. She is interested in the intersection between environmental science and public health, which has inspired her research on harmful algal blooms and ocean acidification.

Dr. Martin is an assistant professor of emergency medicine at the Warren Alpert Medical School of Brown University. His research interests include global emergency medicine education and curriculum development, innovative approaches to noncommunicable disease management in low- and middle-Income countries, and climate change and health. He serves as vice chair of the SAEM Climate Change & Health Interest Group.

By Emelia Potter, DO; Alexander Bracey, MD; and Gregory P. Wu, MD, on behalf of the SAEM Critical Care Interest Group and the SAEM Airway Interest Group
Airway management is a cornerstone of emergency medicine. Emergency medicine physicians must proficiently handle various techniques, including rapid and delayed sequence intubation, managing difficult airways, and emergent surgical interventions. In the current era, where hospital systems and intensive care units grapple with congestion and overwhelming patient loads, emergency medicine physicians must also oversee the continuation of mechanical ventilation. With this, the skill of ventilator liberation via extubation has emerged as a necessary addition to our skillset, despite not being typically associated with emergency medicine. While intubation generally leads to
admission in intensive care settings— beds that are in high demand and short supply—safe extubation in the emergency department offers a means for expedited patient disposition or even discharge. Patients suitable for emergency department (ED) extubation typically include those requiring shortterm airway protection for procedural sedation, imaging, or due to intoxication or agitation. Patients transitioning to palliative care deserve special consideration for extubation, despite often having critical diseases.
While criteria for extubation are similar to those established for intensive care unit (ICU) patients, important differences exist for those undergoing consideration
for ED extubation. Arguably the single most important parameter is that of success. While most ICU physicians cite an acceptable 15% reintubation rate, this would be deemed unacceptable in most EDs. Therefore, careful patient selection is paramount. Moreover, several small studies have demonstrated the feasibility and safety of ED extubation.
One notable study by Weingart et al., sought to establish the safety of ED extubation through a retrospective, observational study of 50 trauma patients. All were extubated by trauma and critical care specialists familiar with the procedure. None of the patients in the study required unplanned
“Emergency Department extubations play a crucial role in expediting patient discharges following intubation, effectively optimizing bed turnover rates, and contributing to the efficient utilization of available resources.”
reintubation, and none experienced post-extubation stridor. One limitation of this study is the use of critical caretrained physicians. Another retrospective, single-center study by Nwakanma and Wright assessed the need for reintubation in trauma patients determined to be candidates for extubation by emergency physicians without critical care fellowship training. Of these 50 patients, again, none required reintubation, and eight were able to discharge from the department. Similar findings were noted by Haas et al., in another retrospective study that included 202 ED-ICU patients. The emergency physician performing extubation was not critical care fellowship-trained in most cases.
There has been subsequent development of protocols specifically tailored for emergency department extubation. These protocols delineate inclusion criteria, list necessary equipment, and detail post-procedural monitoring, all with the overarching goal of minimizing patient harm. The first step is to assess whether a patient is ready for a spontaneous breathing trial. Criteria vary, but typically include:
• Resolution of the primary insult that required intubation, e.g. a patient intubated for intoxication who has since metabolized the toxin and is now more sober.
• Minimal oxygen requirements, as demonstrated by an SPO2 ≥92% with an FIO2 ≤ 50% and a PEEP of 5cm H2O.
• Clinical team has determined that any previously administered paralytics are no longer in effect.
• Hemodynamic stability, generally defined as no or minimal vasopressor requirements (e.g., <0.1mcg/kg/min of norepinephrine or equivalent) and no active cardiac ischemia.
• No imminent intervention that intubation and mechanical ventilation would be optimal, e.g. patient is going to the operating room.
• A cuff leak is present.
Once these criteria are met, the next step is to perform a spontaneous awakening trial and spontaneous breathing trial. A spontaneous awakening trial is a complete cessation of continuous sedative and analgesic infusions to see if patent awakens and follows commands. If a patient


CRITICAL CARE EM continued from Page 39
becomes agitated and does not meet other outlined extubation criteria, sedation and analgesics are resumed at half the previous dose. A spontaneous breathing trial involves placing the patient on a pressure support ventilation with an inspiratory support of 3-5cm H2O and PEEP of 5cm H2O. A spontaneous breathing trial is generally considered successful if the following are met:
• Patient maintained SPO2 ≥92%.
• Adequate spontaneous minute ventilation, typically 5-12L/min with a respiratory rate <30 breaths per minute.
• No signs of respiratory distress, e.g. nasal flaring, accessory muscle use, agitation.
The rapid shallow breathing index (RSBI) can be evaluated as well but should be reviewed in conjunction with other clinical indicators of patient readiness. RSBI is calculated as respiratory rate in minutes divided by tidal volume in liters. A RSBI <105 typically predicts successful extubation in ICU literature. A lower RSBI target of <80-90 is reasonable to decrease the risk of a false positive that could result in re-intubation; however, this may delay some ventilator liberations.
The final assessment is whether a patient can protect their airway if extubated. The ability to lift the head off the bed is one such assessment to ensure maintenance of airway patency and capacity to clear secretions. Next, suction the endotracheal tube and oropharynx, elevate the head of bed, and deflate of the endotracheal tube cuff. The endotracheal tube and any orogastric tube are then removed as the patient coughs. Repeat oral suctioning and apply supplemental oxygen.
The emergency department physician must also be aware of potential post-extubation complications. Postextubation hypoxemia can result from de-recruitment secondary to atelectasis or increases in airway resistance. Noninvasive ventilation may be employed if concerns for respiratory distress arise, often averting the need for reintubation. Stridor resulting from airway edema may also be present in the post-extubation period. In general, endotracheal tube provocation of laryngeal edema is typically within 36 hours of intubation. Assessing for a cuff leak may help predict risk for post-extubation stridor, however, even low risk patients may develop stridor. Management includes nebulized epinephrine, heliox, glucocorticoids, and reintubation if needed. Although there is no infallible predictor of extubation success, risk stratification and preparation for potential complications can limit the possibility of poor patient outcomes.
Another type of patient suitable for ED ventilator liberation is the compassionate extubation, sometimes termed “terminal” extubation. These are intended for patients at the end of life whom no longer seek restorative care, but instead have the goal of extubation being a natural and dignified death. Compassionate extubation should be adapted to each patient’s unique
situation and timing coordinated with the patient’s loved ones. In general, the procedure is:
• Confirm resuscitation status and desire for compassionate extubation with the patient or surrogate decision maker in the event the patient is incapacitated, with the expected outcome of death.
• Ensure that an adequate time has passed since the last dose of paralytics so that the patient is not under neuromuscular blockade. Stop continuous IV anesthetics.
• Suction the patient above the glottis. The endotracheal tube cuff is then deflated and removed along with any OG tube.
• Place the patient on humidified oxygen by nasal cannula, titrated for comfort not a SpO2 goal.
Palliative measures should subsequently commence. The use of scopolamine transdermal patches has been shown to reduce the “death rattle” and thereby reduce bystander distress as the patient’s final moments. A fan blowing in the face can reduce dyspnea as well as morphine intravenous boluses of 1-2mg every hour as needed. Continuous infusion of opioids may be beneficial in situations of difficult to control pain or when frequent doses are needed. Frequent reassessment and reassurance can help the patient’s loved ones through the dying process.
Extubation elevates the critical care capabilities of emergency physicians and contributes significantly to resource optimization. While careful patient selection is essential, ED extubations are safe and can be performed by those even without additional critical care training. This resourceconscious approach is pivotal in the contemporary health care landscape by improving ICU resource utilization. Emergency department extubations play a crucial role in expediting patient discharges following intubation, effectively optimizing bed turnover rates, and contributing to the efficient utilization of available resources.


Dr. Potter is a third-year emergency medicine resident at Oklahoma State University. She has interests in critical care, trauma, and mechanical circulatory support.
Dr. Bracey is an emergency physician at Albany Medical College. He is the fellowship director of the Resuscitation and Emergency Critical Care program and assistant program director for the EM residency. His interests include managing critically ill ED patients, advanced ECG interpretation, airway management, and advanced vascular access techniques. He is the current SAEM Airway Interest Group Chair.
Dr. Wu is an associate professor of Emergency Medicine and Internal Medicine at Albany Medical College. He is an emergency physician and medical intensivist. He is the Critical Care clerkship director and the Resuscitation and Emergency Critical Care associate fellowship director. He is the current SAEM Critical Care Interest Group Chair.


By Catrina Cropano, MD; Elyse Lavine, MD; Eric Legome, MD; Michael Redlener, MD; and Samuel E Sondheim, MD, MBA, on behalf of the SAEM Disaster Medicine Interest Group
The emergency department (ED) boarding crisis has become a significant challenge in health care systems globally, straining resources and compromising patient care effectiveness and efficiency. Boarding times have reached all-time highs nationwide, according to data from the Emergency Department Benchmarking Alliance. Our two comprehensive academic centers at Mount Sinai, with a combined volume of over 135,000 patient visits in 2023, are no exception, as 2023 boarding rates soared 195% and 326% from prepandemic levels.
Boarding refers to patients admitted to the hospital but receiving inpatient services in the ED due to a lack of inpatient bed availability. The boarding crisis has arisen from insufficient inpatient bed availability and increased ED utilization with heightened clinical acuity. Consequences of boarding
include compromised safety and quality of care, higher rates of morbidity and mortality, extended hospital length of stay, increased staff burnout, and overall escalated costs to the health care system. Prior literature has established that boarding is associated with worse clinical outcomes. National organizations, including the American College of Emergency Physicians (ACEP), have dedicated significant efforts to address this issue, with ACEP's website focusing on sharing boarding stories and the Fall 2023 summit concentrating on ED boarding. Most recently, the Agency for Healthcare Research and Quality (AHRQ) announced the development of a national boarding task force to address this pressing issue. While the boarding crisis will likely take years to solve, there are efforts and workflows that can help improve patient experience and care.
While immediate solutions may not be evident to local and national leaders, ED leaders must act to mitigate the situation for patients. ED leadership at Mount Sinai’s two NYC hospitals devised contingency surge plans to respond to the unprecedented boarding challenge. These surge operational plans are intended for deployment during high crowding and boarding times and include triggers for activation, mechanisms for distribution, and requests from other services in a tiered structure based on census. Since many needs during high crowding and boarding times are beyond the control of the ED, the surge plans primarily concentrate on alerting support services about pre-established responses. These responses aim to address needs arising from crowding, and these needs fall within the respective responsibilities of the support services.
Triggers developed for activating surge plans differ between our two Mount Sinai sites but include overall patient volume, patient volume in acute ED areas, the number of critical care patients, the number of admitted boarders, and National Emergency Department Overcrowding Scale (NEDOCS) score. When meeting activation criteria, an email notification is distributed early in the morning and again in the early afternoon to provide ample time for ancillary and clinical services to respond to respective requests depending on surge level.
Our surge escalation pathways have multiple tiers but always involve collaboration with additional clinical and ancillary services. Partnering with case management and social work early in care for anticipated admissions can often be helpful to screen for potential obstacles to discharge, expedite additional ancillary service evaluations (such as physical therapy), and possibly decrease length of stay. With expeditious evaluations from support services in the ED, a significant percentage of boarders are eligible for discharge directly from the ED. We have seen up to 20% of boarders never reach an inpatient floor, with their care completed in the ED, though this may be partially due to the extended boarding length as well. Similarly, security is essential to maintaining our visitor policy, which may be adjusted or limited during high census times to ensure adequate space for patients, though prioritizing visitor access remains a priority. Furthermore, engineering is requested to prioritize work order requests from the ED.
Collaboration and communication with other clinical services are key. ED requests to inpatient medicine and surgery services include prioritizing ED rounding first and confirming a frontline provider assigned to every patient in our electronic health record (Epic) to enhance communication. Additional
escalations for higher census include requests for additional afternoon rounding on ED boarders and ultimately an inpatient medicine boarder team stationed in the ED during predefined crisis level volumes. Subspecialists may be asked to expedite consultations with the goal of recommendations in less than one hour. Developing a surge plan that relies on other clinical services requires partnerships to understand their respective capabilities to combat boarding, knowing that at times their own service line demands may overtake their ability to fulfill all ED requests. Additional helpful partnerships inside and outside the institution may include connections with local skilled nursing and rehabilitation facilities and hospital-at-home programs.
Increased patient boarding is inversely proportional to patient comfort and satisfaction. Hence, surge plan activations include collaboration from environmental services to ensure cleanliness and appropriate linen resources, food, and nutrition to increase the quantity of food deliveries, and transport to increase the supply of wheelchairs and beds and dedicate additional efforts to transporting and prioritizing ED patient transports for studies and to the inpatient units when assigned. Patient relations availability to proactively improve patient comfort and reactively address patient concerns in real-time has been particularly beneficial, with one of our sites maintaining a full-time patient experience coordinator dedicated to the ED.
Departmental leaders play a crucial role in maintaining efficient patient care within their own departments. Hence, surge plans request regular rounding by leaders from environmental services, transport, nutrition, laboratory, radiology, and engineering. By physically being present in the department, leaders can observe firsthand the challenges that each of their respective departments can help address.
The emergency department boarding crisis is a multifaceted issue that demands urgent attention and comprehensive solutions. While escalation pathways won't solve the crisis immediately, they are a mitigation strategy to improve operational efficiency, patient safety, and patient experience as much as possible. As the demand for emergency services rises in EDs constrained by census, staffing, and infrastructure, proactive measures are essential to ensure that the ED functions as intended — as a vital resource for acute care rather than a bottleneck in the health care delivery system

Dr. Cropano is an assistant professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the assistant medical director for the Mount Sinai West Emergency department. catrina.cropano@mountsinai.org

Dr. Lavine is an assistant professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the interim medical director for the Mount Sinai Morningside Emergency Department. Elyse.Lavine@mountsinai.org

Dr. Legome is a professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the chair of emergency medicine for Mount Sinai Morningside and West Hospitals. eric.legome@mountsinai.org

Dr. Redlener is an associate professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the Medical Director for the Mount Sinai West Emergency Department. He can be reached at michael. redlener@mountsinai.org

Dr. Sondheim is an Assistant Professor in the department of emergency medicine at the Icahn School of Medicine at Mount Sinai and serves as the Assistant Medical Director for the Mount Sinai Morningside Emergency Department. He can be reached at samuel.sondheim@mountsinai.org

By Parker Miller, MD, MAUB; Sarah Kaelin, MD, ScM; Ryan Hoopes, MD; and Lance Shaull, MD, on behalf of the SAEM Education Committee
Introduction
Rapid atrial fibrillation, defined as a heart rate exceeding 110 beats per minute, is frequently encountered in emergency departments. Despite attempts to address underlying causes, the condition often persists, prompting consideration of rate control interventions. In such situations, emergency providers commonly resort to intravenous (IV) diltiazem or IV metoprolol, sparking ongoing debates on the preferred agent for effective management.
IV diltiazem, a non-dihydropyridine calcium-channel blocker, operates
“The American College of Cardiology cautions against co-administration of these medications within 6 hours, citing a higher risk of adverse events such as hypotension and bradycardia.”
by slowing AV-nodal conduction and extending the refractory period of the AV node. For rapid atrial fibrillation, it is administered at a dose of 0.25 mg/ kg delivered over 2 minutes. After 15
minutes, the rate is reassessed, and if atrial fibrillation with a rate exceeding 110 beats per minute persists, patients may receive an additional dose of IV diltiazem, typically up to a maximum of two doses.
IV metoprolol, a beta-blocker, blocks sympathetic activity in the AV node, slowing the ventricular rate. It is given at a dose of 2.5-5 mg, with reassessment and subsequent redosing every 5 minutes if the heart rate remains above 110 beats per minute (to a maximum of 3 doses).
The American College of Cardiology cautions against co-administration of these medications within 6 hours, citing a higher risk of adverse events such as hypotension and bradycardia. To better understand the differences in efficacy of the two medications, this article summarizes a systematic review and meta-analysis published in the Indian Heart Journal, examining the efficacy and safety of IV metoprolol compared to IV diltiazem for rate control in atrial fibrillation.
This analysis by Sharda et al., included three randomized control trials (RCTs) and eleven retrospective studies. Notably, all RCTs excluded patients with heart failure, an area of ongoing debate in emergency department rate control not covered in this review. None of the studies demonstrated a difference in rates of bradycardia or hypotension. The included RCTs are summarized below.
The three highlighted RCTs provide insights into the comparative effectiveness of IV diltiazem and IV metoprolol. Fromm et al., found that 50% of the diltiazem group and 11% of the metoprolol group achieved a heart rate less than 100 beats per minute at ten minutes, with the gap widening to 95% versus 46% at 30 minutes. Demircan et al., observed that 90% of the diltiazem group and 80% of the metoprolol group had a successful rate reduction to less than 100 beats per minute at 20 minutes. Memis et al., reported that 37 out of 50 patients in the diltiazem group achieved rate control after the first dose, compared

to 18 out of 50 in the metoprolol group. After a second dose, rates increased to 46 out of 50 and 26 out of 50, respectively.
Overall, the scarcity of available RCT data on such a common problem in the emergency department is striking. Additionally, none of these studies discuss safety profiles of either of these medications in cases with heart failure, despite the frequency with which these conditions present together. These results (and Sharda et al’s., overall findings when retrospective analyses were included) favor the selection of diltiazem as the preferred agent over metoprolol for rate control in the emergent setting, but more work needs to be done to reinforce this conclusion and better understand how these medications affect patients with additional cardiac comorbidities.
“The three highlighted RCTs provide insights into the comparative effectiveness of IV diltiazem and IV metoprolol, revealing significant differences in achieving heart rate control at various time points.”




Dr. Miller is a third-year resident at Boston Medical Center with a strong interest in resident education and evidence-based medicine. After residency, he hopes to go on to complete an ultrasound fellowship.
Dr. Kaelin is an emergency medicine resident at Boston Medical Center. She is a graduate of the primary carepopulation medicine program at Brown University.
Dr. Hoopes is an EM resident at Boston Medical Center. He chose emergency medicine for the breadth and diversity it provides, both in patient population and clinical presentation. Outside of medicine, Ryan enjoys all the EM cliches, including skiing, hiking/camping, and photography.

Dr. Shaull is a fourth-year EM resident at Boston Medical Center. Outside of residency, he works with Hippo Education as a recurrent guest expert on Urgent Care RAP. His academic interests include rural medicine, addiction medicine, high-frequency ED utilization, and toxicology

By Jeremy Simon, MD, PhD
An 85-year-old male is brought into the hospital after being found unresponsive by emergency medical services (EMS). On arrival, his blood pressure is 110/60, heart rate is 80, respiratory rate is 10, and oxygen saturation on non-rebreather mask (NRB) is 100%. A quick review of the electronic medical record reveals that the patient had been hospitalized a few months ago for pneumonia and had since had multiple admissions for falls. On the last admission, it was noted that the social worker had encouraged him to move into a nursing home, but the patient had declined.
“Attempts of suicide with a DNR or DNI (do not intubate) present a unique ethical dilemma unique to emergency medicine.”
During the initial evaluation, two pills, identified as lorazepam, were discovered in the patient's mouth, prompting preparations for an urgent intubation due to the patient's precarious mental and respiratory status. However, at this juncture, the police, who routinely respond to EMS
calls in this city, arrived with papers they deemed important, found on the dining room table. One document was a Physician Orders for Life-Sustaining Treatment (POLST) form, directing that the patient not be intubated or resuscitated, and the other was a one-page suicide note. The emergency
“When the law is unclear, one's response to these cases must be guided by ethics, providing arguments in both directions.”
department (ED) team was uncertain how to proceed. On the one hand, the patient had a do-not-resuscitate (DNR) order; on the other hand, they felt that they would be abetting a suicide if they failed to resuscitate and were very uncomfortable with this.
Attempts of suicide with a DNR or DNI (do not intubate) present a unique ethical dilemma unique to emergency medicine. Since resuscitation and DNR forms are generally regulated by state law, some might look to the law to resolve the issue. However, most states do not explicitly address the matter, and those that do take different approaches. California takes the clearest position, stating that “If there is suspicion that a patient's cardiorespiratory arrest is not part of a natural or expected death (e.g., attempted suicide or possibly suffering harm by another), then resuscitation shall be attempted despite the presence of a CDCR 7465 stating no attempt at resuscitation” (Cal. Code Regs. tit. 15 § 3999.241). New Mexico seems to address only EMS, stating, “If there is any question about the validity of an EMS DNR order, or there is evidence of an attempted homicide or suicide, initiate resuscitation until such time that the questions have been answered” (N.M. Code R. § 7.27.6.9), implying, though not explicitly stating, that a DNR should not be respected in the case of attempted suicide. Texas has a similar rule (25 Tex. Admin. Code §157.25 (2010)). While both states recommend consultation with a physician, neither instructs the physician on how to respond if suicide is suspected. (Note that this may not represent an exhaustive report of state laws relevant to this matter.)
When the law is unclear, one's response to these cases must be guided by ethics, providing arguments in both directions. On one hand, respecting the patient’s autonomy may necessitate refraining from resuscitation. Whether or not the patient had capacity at the time of the attempted suicide, he had capacity when the POLST was filled out. At that point, the patient made a decision that under no circumstances did he want
to be intubated or resuscitated. That autonomous decision did not exclude suicide attempts, so one could argue that it should be honored. Furthermore, some cases of suicide can be rational and not solely the result of acute emotional distress or treatable depression. Autonomy would also advocate for not resuscitating these patients. Finally, when the law does not explicitly reference attempted suicide, the DNR is presumably still active. In that case, one can also draw support from the law’s status (in a democracy) as representing the will of the people to honor the DNR.
On the other hand, the prevailing assumption is that suicide is not chosen rationally or autonomously and is generally considered undesirable. This perspective is not solely from a moral or religious standpoint anymore but stems from a societal perspective. The Joint Commission even includes suicide prevention as one of its patient safety goals. Furthermore, it may not be reasonable to assume that when the patient filled out the POLST form, he was taking into account the possibility of acting irrationally at some point. He may well have been solely considering natural death. Given the uncertainty inherent in the emergency department setting and our strong bias, and even obligation, to prevent suicide in at least most cases, there is a compelling argument that acting in the patient’s best interests requires us to intubate and/or resuscitate as needed, superseding concerns about respecting the patient’s autonomy.
Ultimately, there is no definitive, general ethical response to an attempted suicide with a DNR. Responses to these cases will be shaped by both one’s understanding of the specific case and one’s attitude towards suicide. Most individuals would choose to resuscitate a young patient with no significant chronic medical issues. Some cases, however, may be less clear. For instance, in this case, one would be more inclined to resuscitate if there is a belief that the suicide attempt was driven by depression related to the potential loss of independence, rather than being a

truly autonomous statement about the patient's desire to live independently. Similarly, those who strongly believe that suicide is never rational or acceptable would likely be inclined to resuscitate in all such cases, while those who view suicide as a legitimate option might be less certain. All these factors can reasonably contribute to one’s ethical analysis of the case.
Note that, while there is no single correct ethical response, there may be a correct legal response. Making an error in this regard could expose one to charges of battery (if treatment was administered inappropriately) or wrongful death if it was inappropriately withheld. Therefore, it is crucial, as in many similar issues, to be aware of what, if anything, local laws stipulate on the matter.

Dr. Simon is a professor of emergency medicine at the Columbia University Medical Center, in addition to serving as faculty associate at the Columbia Center for Clinical Medical Ethics. Dr. Simon is also a senior research associate for the department of philosophy at the University of Johannesburg.

By Zachary Davidson, MD; Jeffery Ho, MD; and Jean Tersteeg, RN
Another cold night in Minneapolis, and there are 12 patients slumbering in the triage waiting room at our safety-net hospital. The evening unfolded with patients initially presenting various chief complaints, having their normal vitals taken, and now comfortably fast asleep among the benches and chairs. Many are homeless; we recognize them as 'regulars,' glad to provide momentary comforts.
In the era of emergency department (ED) boarding, we know we can only offer this support for a few more hours, as morning is approaching and soon more patients will enter triage with
medical complaints, all deserving rapid assessments for acute issues.
The shelters are full amidst the frigid weather, and we've already dealt with several severe cases of frostbite this week — the ultimate adverse event, although we know our accrediting organizations won't include this as a quality measure, despite it being as common as sepsis in winter here in the Upper Midwest. If these patients seek a safe, warm place to stay, they will find it, and we are happy to provide it.
At 4:30 a.m., an astute nurse noted that some patients in our triage waiting
area were starting to awaken. Between her offering of juice and blankets, the RN determined that many patients did not remember their original medical complaint and were more concerned about how to get to where they now wanted to go.
Our team offered these 12 patients the choice to either remain in triage to await


“In the era of emergency department (ED) boarding, we know we can only offer this support for a few more hours, as morning approaches and more patients enter triage with medical complaints, all deserving rapid assessments for acute issues.”
being seen by a provider or receive a complimentary bus token, good for a single ride to their destination of choice. Nine patients opted for the bus token, while the remaining three adults were eventually seen, evaluated by a provider, and discharged. No complaints were received from those who opted for the token, and no adverse outcomes were documented.

In this “convenience sample” of overnight patients in our ED Triage, nine patients opted for a bus token over eventual medical care. The association suggests it may be more desired for
patients with unstable housing to receive transport to be “first in line at a definitive shelter rather than awaiting care for a medical problem they deem no longer significant. We found this to be a mutually beneficial solution as it provided a simple, immediate, temperature-controlled solution to our homeless patients, and we could now dedicate staff resources to meet the next patient walking in the door.
Although our ED has free transit tokens, they are not available everywhere. We call on Minnesota state and local Twin Cities leaders to provide our emergency departments with resources for them to care for their communities effectively and address their social determinants of health, which, in our emergency medicine patient population, are as pertinent as the medical or surgical history we learned in medical school.

Dr. Davidson is a PGY-5 combined emergency-internal medicine resident at Hennepin Healthcare. His interests include medical education, quality improvement (QI), and primary care. He was the recipient of Hennepin Healthcare’s Excellence in Primary Care award in 2021 and 2023.

Dr. Ho is a professor of emergency medicine at the University of Minnesota Medical School. He is board certified in emergency medicine and is an examiner for the American Board of Emergency Medicine. He is considered a national and international expert in areas where medicine and law enforcement intersect.

Jean Tersteeg, RN is an emergency department nurse at Hennepin Healthcare, program coordinator for HQ Med Ed, and a member of the Minnesota Disaster Medical Assistance Team. In addition to local service, she continues to be called to national deployments rendering aid to patients in need.

By Amanda Fawcett on behalf of the SAEM Academy of Geriatric Emergency Medicine
In August 2020, months after the pandemic shut down the world and changed the health care landscape, I received my first white coat. It symbolized the community of healing, compassion, and service I had long aspired to join. I took an abbreviated medical student oath, pledging to represent a larger community, dedicated to improving the health and well-being of patients and society. I committed to acting in my patient’s best interest and adhering to the well-known principle of "do no harm."
Later in my medical school journey, I spent two weeks in the emergency department as part of a brief elective
— long enough for me to confirm that this was how I wanted to spend the next forty years of my life, but brief enough that I left feeling like I knew even less than when I started. My first patient was a woman in her late sixties with a productive cough and a history of worsening shortness of breath over several days. She was accompanied by her daughter, who rolled her eyes when my patient mentioned using a walker at home, stating, “She is supposed to, but she leaves it in the corner because she thinks it slows her down.” I delivered what I believed to be a thorough and well-thought-out case to my attending, concluding confidently, “I believe this patient requires admission for the
treatment of her likely pneumonia.” My attending, however, tilted her head at me and responded, “Does she?”
Geriatric emergency medicine requires a departure from a “onesize-fits-all” approach, necessitating consideration of the patient’s support network and a careful weighing of the benefits of inpatient treatment with the risks of delirium, deconditioning, and nosocomial infections, as exemplified by the aforementioned patient. Despite older adults comprising up to 20% of emergency department visits, geriatric emergency medicine is frequently an undervalued subspecialty within emergency medicine. It is crucial to
“Geriatric emergency medicine requires a departure from a 'one-sizefits-all' approach, necessitating consideration of the patient’s support network and a careful weighing of the benefits of inpatient treatment with the risks of delirium, deconditioning, and nosocomial infections.”
cultivate an interest in geriatric emergency medicine early in a medical student’s career, emphasizing the complexities involved in caring for this patient population, irrespective of their intention to pursue a geriatrics fellowship. This objective can be achieved through various means, three of which are delineated below:
We are all too familiar with the adage, "Children are not just little adults!" However, a similar approach can be applied in caring for older adults, who face their own challenges and unique pathologies. Even when dealing with younger, less medically complex patients, prompt medical students to contemplate, "How would your differential change if this were a geriatric patient? What additional workup might you order?" Encourage them to assess whether admission is genuinely in the best interest of the patient or if there is adequate support for outpatient treatment. Remind them to reflect on the commitment made when they received their first white coat, pledging to treat the patient holistically, considering their environment and social support.
Most medical schools include a mandatory interprofessional collaboration component in their curriculum. The multidisciplinary care of older adults in the acute setting provides an ideal opportunity for students to brainstorm how to engage their interprofessional colleagues effectively in patient care. Pharmacists and pharmacy technologists can assist in reducing polypharmacy,
social workers can coordinate home health efforts, physical therapists can collaborate with patients to minimize their risk of falls, and dietitians can conduct nutritional assessments. If you need information about the resources available to the older adults you are caring for, ask whether your medical student knows! They likely completed rotations through the neurology service or a recent physical medicine and rehabilitation elective and may be aware of services that could benefit your patients. If they lack this information, reach out to your physician colleagues for assistance.
Medical students are eager to assist but often feel uncertain about how to contribute and may be apprehensive about being in the way of the residents and attendings managing a busy emergency department. Additionally, medical students typically have more time available and can use this additional time to develop a deeper understanding of a patient’s baseline cognitive function (Are they really “as sharp as a tack” or just good at hiding it?), reasons they are (or are not) taking their medication, how they navigate their home environment (whether their walker functions more as a table than a mobility aid), and who constitutes their support network. It is vital for any physician, regardless of their stage of training or years into their career, to understand how the specific older adult in front of them behaves and interacts with their environment, moving beyond preconceived expectations of how we expect them to.
With the aging population, medical students and emerging emergency

medicine physicians must grasp the intricacies of geriatric emergency medicine. This practice encompasses everything the field of medicine represents to a bright-eyed medical student eager to make a difference. Geriatric emergency medicine provides an opportunity for medical students to improve communication skills, develop a nuanced understanding of polypharmacy and complex medical conditions, and deliver comprehensive care by considering the social and functional aspects of an older adult’s life.

Amanda Fawcett is a fourthyear medical student at The Ohio State University College of Medicine in Columbus, Ohio. She will begin her emergency medicine residency in July of 2024. Her interests outside of geriatric emergency medicine include point-ofcare ultrasound and EMS.
The Academy of Geriatric Emergency Medicine (AGEM) works to improve the clinical care of older patients, prepare trainees to care for older patients, and advance the geriatric EM research agenda. Joining AGEM is free! Just log into your member profile. Click “My Account” in the upper right navigation bar. Click the “Update (+/-) Academies and Interest Groups” button on the left side. Select the box next to the academy you wish to join. Click “save.”

By Alvaro Uribe, Anna Dobbins, MPH, on behalf of the SAEM Global Emergency Medicine Academy
Despite having some of the greatest need for emergency care, the lack of emergency medicine training programs in low- and middle-income countries (LMICs) is an often-overlooked health inequity. To address this, the first emergency medicine residency program (EMRP) in Rwanda was established at the University Teaching Hospital of Kigali (KUTH) in August 2015. Nine years later, the program has transformed emergency medicine in Rwanda, saving lives and building a generation of skilled, experienced, and motivated emergency medicine (EM) physicians.
The EMRP (officially a Master of Medicine in Emergency Medicine & Critical Care) is a four-year experience, consisting of weekly didactics, medical
simulation, quarterly assessments, clinical rotations, research, and individual international mentorship. In order to graduate, residents must complete a comprehensive written exam, objective structured clinical exams (OSCEs), case simulation assessment, and a publishable medical dissertation.
The didactic curriculum covers seven EM and critical care modules each year with a peer-to-peer learning approach, allowing senior residents to gain experience in medical teaching. The program also includes guest lectures featuring faculty from all over the globe, including the United States, UK, Tanzania, Kenya, and Uganda.
In addition to didactic sessions, the
EMRP addresses the research gap in East Africa through a researchbased curriculum intended to foster the development of medical research and cultivate qualified knowledgeable researchers. Residents are expected to complete a research methods course during their first year, a quality improvement plan during their second year, and a publishable medical dissertation by their final year.
The impact of the EMRP has been substantial. A study by Adam Aluisio, MD, of Brown University, found that in-hospital mortality decreased by 43% after the program was established. Dr. Aluisio attributes some of this impact to the program being the only de novo specialty in the Rwandan health system.
“Despite having some of the greatest need for emergency care, the lack of emergency medicine training programs in low- and middle-income countries is an often-overlooked health inequity.”
Since the program was established in 2015, a total of 24 EM physicians have graduated. Of those who have graduated, 16 physicians remain in Rwanda.
Through the EMRP, more than 50 scientific abstracts and manuscripts have been published in peer-reviewed journals. Dr. Kamunga Badibanga Laurent Gamy, a graduate of the EMRP, received the Best Poster Award at the 2022 African Conference of Emergency Medicine (AfCEM) in Accra, Ghana for his dissertation work.
In an SAEM Pulse article by Destry Jensen, MPH, Dr. Laurent details the experience of paving the way as a trainee in the de novo EM training program. Dr. Laurent describes a sense of consistent pressure to define the EM specialty within the hospital and how this pressure helped shape him into a holistically reliable, flexible, and more prepared physician.
Other graduates from the EMRP are having lasting impacts across communities in Rwanda. Dr. Joseph Birahamire (EM '21) is currently steering an initiative with the Rwanda Emergency Care Association (RECA) to strengthen trauma care at district hospitals across the country. Dr. Birhamine provides instruction on pediatric trauma, geriatric trauma, and trauma in pregnant women while simultaneously evaluating course quality and changes in patient outcomes at hospitals that receive training. There are currently eight district hospitals and more than 200 health providers participating in this initiative.

Dr. Pascal Mugemangando (EM ‘21), a junior faculty and EM clinical consultant at KUTH, and Dr. François Régis Twagirumukiz (EM ‘21) joined the core faculty of the EMRP after graduation. Dr. Mugemangango is a World Health Organization/International Committee of the Red Cross (WHO/ICRC) Basic Emergency Care (BEC) Master Trainer and served as head of department in the ED at Kibuye Referral Hospital for two years before returning to KUTH. Dr. Twagirumukiza leads several research initiatives, accreditation activities, and continues to give back to the field, teaching both undergraduates and residents in emergency medicine and critical care.
There are currently 20 trainees enrolled in the EMRP with KUTH expecting to welcome its largest cohort of additional trainees in 2024. Current trainees are dedicated to generating impactful thesis projects across various topics such as assessing blunt abdominal trauma patient outcomes with operative versus nonoperative management, assessing door-to-electrocardiogram time and outcomes in patients with undifferentiated cardiorespiratory symptoms, and many more. One trainee notes: “[Heart attacks] are currently increasing [in the] ED. I hope my thesis will contribute to the awareness of heart attacks and lead to the development of a national guideline in Rwanda.”
Since its inception, the EMRP in Rwanda has transformed emergency
care throughout the country. The program has reduced patient mortality and built a future generation of skilled emergency medicine physicians. It is a prime example of a successful EM training program in an LMIC.
As the EMRP continues to expand, larger cohorts of physicians emerge to pave the way and develop emergency systems. The future is bright for emergency medicine in Rwanda.

Alvaro Uribe is a Brown University student (2026) concentrating in biochemistry and public health. In the Summer of 2023, he engaged himself with and developed a flame for executing trauma medicine training in Rwanda. Alvaro Uribe is a current intern at The Warren Alpert Medical School Global Emergency Medicine program, where he is passionate about expanding his knowledge and study of global public health interventions.

Anna Dobbins graduated with a Master of Public Health from the University of Nevada, Reno in 2022. Anna now serves as the Rwanda Research Fellow within the department of emergency medicine at Brown University, building research capacity among emergency medicine residents at the University Teaching Hospital of Kigali.
The Global Emergency Medicine Academy (GEMA) focuses on improvement of the worldwide delivery of emergency medical care. Membership in SAEM's academies and interest groups is free. To participate in one more groups: 1.) log into SAEM.org; 2.) click “My Participation” in the upper navigation bar; and 3) click “Update (+/-) Academies or Interest Groups.”

By Habab A. Iraqi, MBBS; Charlotte Roy, MD, MPH; and Mallika Manyapu, MD, MPH, on behalf of the GEMA Humanitarian Task Force
Sudan has a long history of coups d’état and military rule, which has stood in opposition to the persistent struggle of the Sudanese people to establish a democratic political order. In 2019, a transitional government emerged following the coup that deposed President Omar al-Bashir, raising hopes for democracy. However, since April 2023, the power struggle between the Sudanese Armed Forces (SAF) and the Rapid Support Forces (RSF) has escalated into a large-scale conflict, driving a worsening humanitarian crisis. Sudan is not merely a country on the brink of collapse; it is in a free fall that has devastated public services, including, and especially, health care.
Even before the most recent conflict, Sudan faced a humanitarian
catastrophe due to protracted political unrest and economic strain, with 15.8 million people needing humanitarian aid as of November 2022, according to the United Nations Office for the Coordination of Humanitarian Affairs (OCHA). Now, due to the deepening conflict, nearly 25 million people, over half of Sudan’s population, are in need. Sudan is grappling with the largest internal displacement crisis globally, with more than 6 million internally displaced Sudanese and 1.4 million seeking refuge abroad. Approximately half of those forced to flee are children. At the same time, humanitarian efforts face intense violence and movement restrictions, making it difficult for relief to reach vulnerable communities.
The conflict has destroyed Sudan’s public infrastructure, especially in the health sector. Continuous attacks, looting, and occupation of medical facilities have led to severe staffing, financial, and medical supply shortages. In conflict-affected areas, 70-80% of health facilities are closed or inoperable. The RSF’s control over key health institutions, such as the National Public Health Laboratory, the Central Blood Bank, and the National Medical Supplies Fund, has depleted medical supplies and blood reserves, resulting in a loss of an estimated $700 million for the health care system. This will have a significant impact on a system that was already chronically underfunded and facing severe financial limits as a result of economic decline in 2023.
“Sudan is not merely a country on the brink of collapse; it is in a free fall that has devastated public services, including, and especially, health care.”
Already crippled by severe resource limitations, the health care system is also facing increased stress as a result of civilian displacement and infectious disease outbreaks. For instance, according to UN OCHA, in September 2023 a cholera outbreak was detected in Gedaref state and subsequently expanded to eleven cities. As of January 2024, nearly 10,000 suspected cases of cholera have been reported, with 275 related deaths. More than 3 million people are estimated to be at risk.
Already crippled by resource limitations, the health care system faces added stress from civilian displacement and infectious disease outbreaks. According to UN OCHA, a cholera outbreak in Gedaref state in September 2023 expanded to eleven cities, resulting in nearly 10,000 suspected cases and 275 related deaths as of January 2024. More than 3 million people are estimated to be at risk.
Meanwhile, UNHCR teams in Sudan’s White Nile state reported that over 1,200 refugee children under the age of five died in nine camps between May 15 and September 14 as a result of a suspected measles outbreak and severe malnutrition. Additionally, outbreaks of Dengue and malaria have been reported in other parts of the country, reflecting an escalating epidemic risk attributed to massive displacement, overcrowded camps, inadequate clean water and sanitation, shortages of medicines and medical supplies, and disruptions in vaccination programs.
The crisis has spilled into neighboring countries, affecting South Sudan and Chad. Humanitarian partners across the border in South Sudan report a surge in measles cases and high rates of malnutrition among Sudanese children seeking refuge. In Chad, hospital admissions for malnourished children have increased by 56% since the conflict’s onset — a reflection of the catastrophic situation that has forced many to flee Darfur.
Food shortages remain critical, with
18 million Sudanese experiencing severe food insecurity between October 2023 and January 2024. Parts of Sudan are at a high risk of slipping into catastrophic hunger conditions unless humanitarian organizations, such as the World Food Program, can expand access and regularly deliver food assistance to people trapped in conflict hotspots.
Sudan is also experiencing the world’s largest child displacement crisis and is on the brink of the world’s worst education crisis, according to UNICEF Since April 2023, around 19 million children have been deprived of completing their education. If the war continues, no Sudanese child will be able to return to school in the months to come, exposing them to immediate and long-term threats such as displacement, recruitment into armed groups, and sexual violence.
Amid the conflict, medical professionals, facilities, and ambulances, protected under international humanitarian law, are targeted. The acceptance of civilian collateral damage has led to the targeting of hospitals and failure to prioritize medical treatment for civilians during hostilities. The room that used to be a supply closet now serves as a tiny hospital. Premature infants sleep in incubators powered by generators in a disused storage area that escaped shelling.
In this era of global conflicts, hospitals have stopped providing medical care and are converted into battlefields, opening the door to issues that will persist long after the last bullet is fired. The systematic targeting of health care systems cannot become routine. As long as these attacks continue to infuriate us, we will not become desensitized to them. Action, not complacency, must follow fury. The imperative is glaringly obvious: even as a multitude of tragedies unfold across the globe, the world cannot turn a blind eye to the suffering of the Sudanese people.
As emergency physicians, we must work together. Emergency physicians, even from abroad, can contribute through research, knowledge sharing, and clinical support. Advocacy for humanitarian
assistance within Sudan and across borders is crucial to prevent more deaths. Eessential supplies like medicines for the treatment of cholera and malnutrition, reproductive health kits, and tents for mobile health clinics are urgently needed.
We must use our platform to raise awareness about the struggles of Sudanese emergency physicians and exert pressure the international community through social media campaigns is vital. Applying pressure on the international community through social media campaigns holds the potential to shape government policies.
Humanitarian workers must be allowed to carry out their work without restriction, and attacks on health care cannot be tolerated

Dr. Roy is an assistant professor of emergency medicine at the University of Southern California. She completed a fellowship in Global Emergency Medicine at Columbia University and has worked for Doctors Without Borders in Ethiopia, Democratic Republic of Congo, and Central African Republic.

Dr. Iraqi is a Sudanese emergency medicine intern. She has served in global health organizations since medical school. Current affiliations include SAEM, IFEM and EUSEM. Her research interests involve humanitarian healthcare, global health policy, and pediatric emergency medicine.

Dr. Mallika is an emergency medicine physician and current Global Emergency Medicine fellow at George Washington University. She has worked in various settings such as India, Jamaica, Ukraine, Tanzania, and Uganda. Her global health interests include humanitarian response and education/training in low resource settings.

By Christian Rose, MD; Joshua W. Joseph MD, MS, MBE; Diane Kuhn, MD, PhD; David G. Beiser, MD, MS; Moira Smith, MD, MPH; David Kim, MD, PhD;
and Arwen
Declan, MD, PhD,
on behalf of the SAEM Informatics, Data Science, and Artificial Intelligence Interest Group
Emergency physicians (EPs) are consistently tasked with anticipating the future, whether in the short term (patient physiology and responses to interventions) or the long term (changes in clinical practice). We integrate our experience, knowledge, and risk assessments to construct future-oriented, predictive mental models. Unsurprisingly, we now foresee an impending paradigm shift stemming from recent developments
in data-centric artificial intelligence (AI). Conversations around large language models and image recognition algorithms are sparking interest and optimism. Given that the potentials of generative AI are matched by perils, we must consider the many possible impacts AI will have on emergency medicine. As we engage in forecasting with both enthusiasm and cautious trepidation, we develop mental models to help shape a future in which AI
enhances safety, privacy, and the human relationships that underpin highquality care.
Several factors make this an opportune moment for emergency physicians to consider the use of emerging AI technologies. First, the Health Information Technology for Economic Clinical Health (HITECH) Act, by offering financial incentives for electronic health
“We integrate our experience, knowledge, and risk assessments to construct future-oriented, predictive mental models. Unsurprisingly, we now foresee an impending paradigm shift stemming from recent developments in data-centric artificial intelligence.”
record (EHR) use, has prompted the adoption of electronic records in clinical practice by health systems and physician practices. While hospital systems are not yet fully interconnected, modern EHRs nevertheless contain the data needed to build robust, high-quality algorithms. Secondly, available AI methods have experienced significant expansion and improvement. Compared to the rulebased algorithms relied upon by most common emergency department (ED) decision instruments, newer methods, like the “transformer” architectures underlying large language models such as GPT-4, can process enormous amounts of data and can demonstrate adaptability across a wide range of tasks. These methods produce flexible and detailed outputs, including interpretations of medical data and summaries of clinical text. The modern “foundation models” exhibit such flexibility that they can be generalized to new use cases without requiring a unique model for each case. Finally, advancements in computing hardware enable the training and deployment of these large and complex models.
We believe that well-designed applications of AI can support patient care across various settings, from prehospital care, to the ED, to largescale public health applications. In the prehospital setting, the first stage of triage might involve AI bots collecting data through natural language communication with patients to assess the complexity and acuity of their questions or complaints. The process could be linked to primary or urgent care scheduling, potentially diverting some low-acuity cases away from overburdened EDs. Similarly, emergency medical services (EMS) teams may use real-time resource modeling to optimally route ambulances Additionally, AI has the potential to optimize and automate patient registration and triage, improving patient

flow in the ED. Given that AI-driven predictive tools can analyze complex clinical data, they may also enhance the speed and accuracy of ED diagnosis and management. Consequently, AI has the potential to reduce waiting times, alleviate ED crowding, and enhance the overall quality of care. Finally, AI analysis of population level data can offer insights into public health trends and system-wide operational efficiency. By streamlining the many workflows relevant to emergency care, AI may allow EPs to focus more on delivering high quality emergency care for patients who need it.
Despite the reasons for optimism, EPs must address potential risks posed by AI, including impacts on professional satisfaction, equity, and privacy.
Electronic Health Records (EHRs), once envisioned as time-saving technologies to improve clinical efficiency and care, have ironically become a significant source of physician burnout. Similarly, an excessive focus on data and computation, without careful clinical design, risks further alienating EPs. AI models may overlook the nuances of human communication and the larger context of a patient’s health determinants. Furthermore, recommendation systems require careful design to capture the variety of patient needs and preferences. Thus, the
ultimate authority and responsibility must rest with physicians.
Importantly, the expanding role of AI in medicine has the potential to exacerbate health inequities. When a model is trained on biased data, its outputs can reproduce and amplify those biases. Moreover, the performance of AI models may not be uniform across patient race, ethnicity, gender, and socioeconomic status. Careful optimization of model performance across patient subgroups and vulnerable populations is necessary, and it is imperative that the scope and limitations of models be communicated clearly. Ensuring the effective use of AI in emergency care requires optimizing the quality and representativeness of training data, reducing biases in model performance, and incorporating a diverse range of perspectives.
Further, AI introduces significant privacy concerns. The data that form the basis of AI systems re derived from individuals whose right to data autonomy must be protected. Patients disclose highly sensitive information to their physicians with the explicit expectation of privacy.
“We believe intelligence settings, department,

believe that well-designed applications of artificial intelligence can support patient care across various settings, from prehospital care, to the emergency department, to large-scale public health applications.”
continued from Page 57
However, in current practice, patient data and physician intellectual property are often extracted and used under unclear contracts and dubious consent processes. Without careful regulation and monitoring, there is a risk of a digital reprise of Henrietta Lacks: patient information exploited for the benefit of others without the patient’s consent. The vast troves of data used by modern AI systems introduce intrinsic privacy risks, as sensitive and personal health information is collected, stored, analyzed, and transformed. The potential for data breaches further threatens confidentiality and trust. Modern AI models, capable of drawing inferences across several data sources, can re-identify individual data. In contrast, to the previous generation of predictive models, de-identification must be ensured both during training (data input) and inference (response output). Navigating this delicate balance between capability and privacy demands advanced technological safeguards, stringent ethical guidelines, and robust legal frameworks.
Emergency medicine is optimally poised to navigate the complexities and promise of artificial intelligence with insight and foresight. Our field revolves around making rapid, high-stakes decisions with incomplete information, requiring constant adaptation to evolving scenarios with agility and precision. The longstanding commitment of emergency medicine to advancing equity, enhancing operational efficiencies, and prioritizing patient-centric care uniquely equips us to integrate the latest technological innovations while safeguarding quality, safety, and privacy.
To best serve our patients, emergency physicians must be at the forefront of shaping, developing, and applying AI technologies. We cannot merely be consumers; instead, we must be collaborators, innovators, and advocates. This approach aligns with the long-established practice in medicine. Previous paradigm-shifting discoveries, which also required us to expand our academic horizons, did not entail sacrificing human-centric approaches. Instead, we successfully merged the two. This uniquely positions EPs to integrate AI into the hospital setting in ways that do not compromise quality of care.
The Society for Academic Emergency Medicine (SAEM) plays a pivotal role in supporting this initiative. It represents a quest for knowledge that aligns with patient-focused, quality-driven clinical practices. The upcoming SAEM Annual Meeting in Phoenix, Ariz. will provide an important forum to discuss and navigate the complexities of AI in our field. This dialogue will help bridge current practices with future innovations, ensuring that our approach to AI is informed by same rigorous, patientcentered ethos that guides clinical decisions.
The integration of AI into emergency medicine requires us to leverage expertise in clinical decision-making, ethics, and systems-based practice. This ensures that AI implementations enhance the patient-physician relationship and improve quality of care. As clinician informaticians and academic emergency physicians, our interest in and pursuit of new technological advances should mirror our patientcentered and evidence-based approach to medicine. Knowing that what we do matters means we have a responsibility to our patients. Therefore, any future implementation of AI must be carefully crafted to support equity, quality, and patient-centered care.

Dr. Rose is an assistant professor of emergency medicine at Stanford University focusing on the intersection of clinical practice and informatics to elevate patient care and promote a human-centered approach. Dual-boarded in emergency medicine and clinical informatics, his work leverages technology within health care to transform health outcomes through information systems.

Dr. Joseph is an assistant professor of emergency medicine at Harvard Medical School and the medical director for enterprise emergency medicine analytics at Mass General Brigham. His research focuses on leveraging AI to improve operations and triage.


Dr. Kuhn is an assistant professor of emergency medicine at the Indiana University School of Medicine. Her research focuses on value-based care including patient experience, artificial intelligence, and informatics.
Dr. Beiser is an associate professor and board certified informaticist at the University of Chicago. His focus is research informatics as well as the development and implementation of patient-facing digital health tools.

Dr. Smith is a clinical informatics fellow at the University of Virginia (UVA) Health System. After Informatics fellowship, she will be an assistant professor at UVA. Her work focuses on data analytics and reporting, quality improvement, EHR usability and workflow optimization, and clinical decision support.


Dr. Kim is assistant professor of emergency medicine at Stanford University. His lab studies the physiology and clinical trajectories of emergency department patients using machine learning.
Dr. Declan is the assistant research director at Prisma Health Upstate and clinical assistant professor at the University of South Carolina School of Medicine-Greenville and Clemson University. She applies informatics methods to improve patient care and support the clinician workforce.

By Jeremy Brown, MD
Currently, every NIH Study Sectionreviewed grant application is scored based on five separate domains or criteria: Significance, Investigator, Innovation, Approach, and Environment. For the purposes of this discussion, we will focus on the review of a clinical trial, as opposed to a basic or laboratory research proposal, and how these criteria might be scored.
Significance: Is the trial likely to advance the field or improve patient care? Is the scientific rationale and the necessity for a clinical trial wellsupported by preliminary data, clinical or preclinical studies, or information in the literature or knowledge of biological mechanisms?
Investigator: Are the principal investigators (PI) and their collaborators well-suited to the project? Do they possess an ongoing record of
accomplishments in their field? If there are multiple principal investigators, have they clarified their respective roles and contributions to the project?
Innovation: A project will receive a favorable score if it is likely to improve patient care in an important way (not merely by reducing a white cell count but by reducing hospitalization days for pneumonia). Reviewers also look for novel theoretical concepts, approaches, or methodologies, though these are less likely to be relevant to a clinical trial.
Approach: Recognizing that every study has weaknesses, how does this one address them? Has the PI addressed potential problems and outlined alternative strategies? Has the PI ensured the study will enroll patients in a fair and equitable manner? This criterion also includes the statistical plan, and often with a statistician reviewing, so it is essential that the plan
is easy to follow and replicable.
Environment: The last criterion asks whether proposed sites have the capability and capacity to conduct the trial. Additionally, are there plans to add or drop enrollment centers as necessary? Given that nearly all clinical trials occur at multiple sites, has the PI presented evidence that each site can enroll the proposed numbers, adhere to the protocol, and collect and transmit data accurately and in a timely fashion?
These five criteria have formed the basic rubric for scoring proposals for many years. However, as part of an initiative to improve and simplify the review process, starting in 2025, the NIH will reduce them to just three. Two will receive numerical criterion scores, and one will be evaluated for sufficiency. All three factors will then be considered in arriving at the overall score. The breakdown is as follows:
Current NIH Scoring Criterion
Significance
Innovation
Approach
Investigator
Environment
1. Factor 1 assesses the importance of the research, combining the previous criteria of significance and innovation.
2. Factor 2 evaluates the rigor and feasibility, essentially incorporating
New NIH Scoring Criterion Begins in 2025
Factor 1: Importance
Factor 2: Rigor and Feasibility
Factor 3: Expertise and Resources
Will be scored as “appropriate” or that additional expertise or resources are needed
what was formerly termed the "approach."
3. Factor 3 now scores the expertise and resources, encompassing evaluations previously included under

the investigator and environment. This will be scored as either "appropriate" or indicating a need for additional expertise or resources. Each of these three new criteria includes several important factors that are clearly outlined in the specific funding opportunity announcement. Therefore, read them carefully and ensure that any proposal submitted in 2025 is responsive to these criteria.

Dr. Brown is the director of the Office of Emergency Care Research (OECR) where he leads efforts to coordinate emergency care research funding opportunities across NIH. Additionally, Jeremy is the primary contact for the NINDS Exploratory and Efficacy FOAs and serves as NIH's representative in government-wide efforts to improve emergency care throughout the country. He is also the medical officer for the SIREN emergency care research network which is supported by both NINDS and NHLBI. Jeremy.brown@nih.gov

By Emily A Cloessner, MD, MSPH; Katherine Dickerson Mayes, MD, PhD; Carly D. Eastin, MD; and Keith Marill, MD, MS, on behalf of the SAEM Research Committee and SAEM RAMS
Journal club is a time-honored tradition in resident medical education yet lacks a standardized implementation method. When operating on autopilot, the journal club faces the risk of becoming an additional monotonous requirement for faculty and residents. However, with careful planning, journal club can evolve into an engaging forum that encourages discussion, sparks intellectual curiosity, and nurtures social bonds within your residency program. Here are three
suggestions, derived from conversations with colleagues nationwide, to revitalize your journal club:
Adding a social component into journal club stimulates participation. Crafting the event to be family-friendly not only fosters connections within the residency but also includes the loved ones of residents, who are impacted by their
training. Colleagues suggest scheduling the journal club prior to a casual departmental social event. Alternatively, hosting the journal club at a faculty member's home, a restaurant, a park, or another mixed-use area, where space allows for work as well as family attendance, socializing, and a shared meal, has proven effective. Some even combined a journal club meeting with their residency book club, selecting articles relevant to the book's themes.

Regardless of your chosen approach, emphasize two key components: stepping out of the hospital environment and planning the event to include both socializing and learning.
Reformat: Revitalize Discussion Dynamics through Reformatting Presenting multiple papers in a dry, factual manner poses the risk of a lackluster discussion. However, various alternatives exist to the traditional format. For instance, toxicology departments often adopt a "historical" format, exploring articles on the treatment of the same condition over the years. This approach reveals evolving best practices and highlights the growth of knowledge in the field. Given the emergency department's intersection with other hospital departments, journal club provides an opportunity for interdisciplinary collaboration with other Graduate Medical Education (GME) programs at your hospital. Residents and faculty from different specialties can discuss landmark trials that affect patients requiring multidisciplinary care. Introducing opposing papers in a debate
format adds vibrancy to the discussion, culminating in the selection of a winner at the evening's end.
Journal club offers a prime opportunity to familiarize residents with the research process at your institution. Invite a staff statistician to elucidate the intricacies of designing and testing a particularly complex study. Engage someone from the Institutional Review Board (IRB) to explain the approvals process for the presented articles. Are your faculty currently conducting interesting studies? Invite them to share insights not only into their articles but also into the entire research process, from funding to presentation, along with the challenges they encountered. When utilized in this manner, journal club demystifies research for junior researchers and shows residents how to begin their projects at your institution.
If your institution's journal club has been lacking in liveliness, consider
“Adding a social component into journal club stimulates participation. Crafting the event to be family-friendly not only fosters connections within the residency but also includes the loved ones of residents, who are impacted by their training.”
implementing one of these suggestions to infuse interdisciplinary learning, mentorship, and wellness into this time-honored academic tradition. We would love to hear any success stories stemming from their implementation!



Dr. Cloessner is a PGY-3 and incoming chief resident at the Washington University in Saint Louis. She is also a memberat-large on the RAMS board of SAEM and serves as RAMS liaison to the SAEM Research Committee.
Dr. Dickerson Mayes is a chief resident at the Harvard Affiliated Emergency Medicine Residency at Mass General Brigham. Her research focuses on social determinants of health and traumatic brain injury.
Dr. Eastin is an associate professor of emergency medicine at the University of Arkansas for Medical Sciences in Little Rock, Ark., where she leads the residency journal club. She is also the chair of the SAEM Evidence Based Healthcare and Implementation Interest Group

Dr. Marill is a core faculty member for the Harvard Affiliated Emergency Medicine Residency (HAEMR) and associate professor of Emergency Medicine at Harvard Medical School. He has provided faculty direction for the HAEMR journal club since 2003.

By Joshua Lupton, MD, MPH, MPhil, on behalf of the SAEM Research Committee
Project: System Dynamics Modeling to Promote Health Equity in Management of Agitation
Awarding Organization: National Institute of Mental Health


Ambrose Wong, MD, MSEd, MHS
Is assistant professor in the department of emergency medicine at Yale School of Medicine and director of simulation research and fellowship director at the Yale Center for Healthcare Simulation. Dr. Wong is immediate past president of the SAEM Simulation Academy and is an active member of the SAEM Research Committee.
Rebekah Heckmann, MD, MPH, MPA
Is an assistant professor in the department of emergency medicine at Yale School of Medicine and a research scientist at the Yale Center for Outcomes Research and Evaluation. She is also the associate medical director of the Project ASSERT Program as well as core faculty in the Yale Program in Addiction Medicine.
Tell us about your R01 project and what you are hoping to find.
Dr. Wong: It’s an exciting project that will be a marriage between Dr. Heckmann and her team’s expertise in system dynamics modeling with our team’s focus on patient-centeredness for managing symptoms of patient agitation that can lead to aggressive and violent behavior. We are hoping to involve patients, clinicians, and administrators in mathematical modeling through a process called participatory group model building so that we can create data-driven interventions that have input from the actual people impacted by the problem. We hope that this process can also alleviate some of the disparities that we have seen in how agitation is managed, especially around use of sedation and physical restraints.

Dr. Heckmann: Our approach also addresses patient advocacy and staff safety as related issues within one unifying systems model and recognizes that both issues need to be addressed for any potential interventions to be effective. Another aspect of this project that we’re really excited about is that our group will not be prescribing specific workplace interventions to study sites but, rather, will facilitate evidence-based decision making by empowering study participants to modify factors over which they have control to make decisions for themselves, promoting a level of sustainability that is often not possible with more traditional methods of intervention design and testing.
Your R01 award is a multiple principal investigator (MPI) award, can you talk about applying as MPI?
Dr. Wong: The MPI aspect to this grant is one of the most exciting and rewarding aspects of our work. I attribute a big part of our success to an amazing peerbased mentorship and collaboration that Rebekah and I have established
over the past several years. It creates a collaborative and multidisciplinary culture to our research. We each bring our own network of collaborators and experts from different institutions and backgrounds, which makes the science more innovative and unique. Rebekah and I also have different but complementary leadership and working styles which makes the grant preparation and scientific process so much smoother and more fun.
Dr. Heckmann: I completely agree with Ambrose! Our unique strengths have absolutely made us better prepared to lead team science and have equipped us to address important topics that neither of us might be prepared to research individually. Practically speaking, as a junior investigator, it has been a joy to navigate through the setbacks and successes of academic life with a research partner; and, as Ambrose mentioned, the MPI approach has allowed us to develop a community of senior investigators, peer collaborators, and students where mentorship and sponsorship can happen in real time.
What prior grants did you each receive before your R01 award and how did these impact your success at receiving an R01?
Dr. Wong: I was very fortunate to have received an institutional KL2/CTSA award from Yale Center for Clinical Investigation as well as a K23 from the National Institute of Mental Health. Having experience working with the program officers at NIMH was instrumental to understand the institute’s funding priorities and interests. I also received an R21 from NIMHD focusing on disparities in agitation. This grant helped us establish key preliminary data to feed into this R01.
Dr. Heckmann: When I first arrived at Yale, my primary mentor appointed me as a co-investigator on a CDC grant for which I was able to use system dynamics (SD) modeling to assess harm reduction efforts. That project, in turn, introduced me to another longstanding research partner, Dr. Nasim

“We each bring our own network of collaborators and experts from different institutions and backgrounds, which makes the science more innovative and unique. We have different but complementary leadership and working styles which makes the grant preparation and scientific process so much smoother and more fun.”
continued from Page 65
Sabounchi, and to colleagues at the Connecticut Department of Public Health (DPH), where I would receive funds for my first project as a principal investigator. Years later, Dr. Sabounchi and I are currently MPIs for a NIDAfunded R61 grant focused on using SD to evaluate telehealth interventions; and the preliminary work that our modeling group has produced directly contributed to our success in securing this R01.
How did you each initially develop an interest in research?
Dr. Wong: My background was originally in health care simulation. I completed a simulation fellowship at NYU and became interested in applications for patient safety and care quality. During my fellow project using live actor-based simulation scenarios to train staff for managing agitation symptoms, I became increasingly aware that more rigorous science was needed to better care for these patients from marginalized backgrounds suffering from stigmatizing conditions like substance use disorders and psychosis.
Dr. Heckmann: I have long felt that a lack of perfect data is not an acceptable reason for failing to design and advocate for the most evidence-based health policy and protocols possible, and I completed a health policy research and translation fellowship at Brigham & Women’s Hospital with the goal of learning how to translate research findings into practical policy recommendations. Since that time, I’ve been fascinated by the process of wrangling disparate datasets using quantitative social science methods, including system dynamics modeling, to promote the adoption of effective public health interventions.
How has SAEM impacted your path to an R01?
Dr. Wong: SAEM has been a tremendous resource and community of practice for emergency care research. Examples include the research committee, which supports didactics at the annual meeting focused on extramural funding and liaises directly with federal agencies to advocate for emergency physician scientists to serve on study sections. Through SAEM, I have also had the opportunity to make connections with other early career investigators and K-awardees to share resources and create lasting friendships.
Dr. Heckmann: In addition to everything that Ambrose mentioned, we have also both benefited tremendously from being mentored by faculty who have gained leadership experience through their involvement with SAEM, like Dr. Pooja Agarwal.
What piece of advice would you give a medical student or resident interested in pursuing a career as a physicianscientist?
Dr. Wong: Mentorship from NIH funded investigators has been key to successfully obtaining research funding. Many of the biggest names in emergency care research are SAEM members. I have found senior researchers in emergency medicine to be gracious and generous with their time and advice when I approach them for mentorship. We are very lucky to belong to a supportive community of practice for early career scientists.
Dr. Heckmann: After you’ve found a mentor, if possible, you should seek out a sponsor who will actively provide you with opportunities to grow. Your mentor and sponsor might be the same person, or your mentor might be able to point you in the direction of someone who can sponsor you. Also, I highly recommend
finding a research buddy! Whether you choose to pursue an MPI award or not, you will have a relationship with someone who understands you, can hold you accountable for your own goals and team goals, and who supports you.
What has been the most challenging aspect of your work as a physicianscientist?
Dr. Wong: I would say time management and learning skills to be a supportive but effective manager of a research team to be an ongoing challenge! Our vice chair of faculty affairs, Dr. Basmah Safdar, has introduced me to the use of professional coaches and faculty development coursework to learning management skills. I have found them to be immensely helpful as I move towards the next stage of my academic career.
Dr. Heckmann: I also sometimes struggle to determine which tasks truly require my attention and which I should delegate. When you’re just starting out and don’t have a research team, it is also easy to be derailed by the urgent administrative tasks of the day and lose sight of less urgent but often more important longterm goals like writing papers and building a cohesive research portfolio. Engaging in team science has certainly allowed me to observe and learn from my peers and mentors who have faced the same challenges in their careers.

Dr. Lupton is an assistant professor in the department of emergency medicine at Oregon Health & Science University and a member of the SAEM Research Committee.

By Jordi Garcia-Diaz on behalf of the SAEM Sex and Gender in Emergency Medicine Interest Group
Alcohol consumption by men surpasses that of women in terms of volume (19.0 vs 6.7 liters of pure alcohol per year), frequency (3.1 vs 2.7 days per week), and the percentage of individuals who drink annually (68% of men vs 64% of women). Moreover, high-risk drinking is more prevalent in men than in women (16.4% vs 9%). Given these gender-based disparities in alcohol consumption, research has tended to focus on the effects of alcohol more specifically in relation to men. However, over the past several years, there has been a narrowing of the gender alcoholuse gap. For this reason, it is critical to highlight the alcohol-related risks that women face.
A composite of national surveys analyzing alcohol use trends in the early 21st century revealed a 6% increase in the number of adult women who drink, while adult men decreased by 0.2% Additionally, the number of adult women reporting binge drinking rose by 14%, whereas men experienced only a 0.5% increase. As the rate of risky drinking behavior among women rises, it is crucial to acknowledge various studies indicating that the effects of alcohol on women may be significantly more devastating when compared to men. This discrepancy may arise because, even when consuming similar amounts of alcohol as males, females are found to have higher blood alcohol
levels (BALs). These elevated BALs are believed to stem primarily from sexspecific lower levels of gastric alcohol dehydrogenase. The resulting higher BALs expose female patients’ organ systems to greater amounts of the toxic metabolite of alcohol, acetaldehyde, leading to organ dysfunction. Studies also suggest that higher levels of estrogen could exacerbate complications of alcohol use disorder (AUD), such as liver disease.
Moreover, studies examining cirrhosis, one of the most prevalent complications of alcohol-related liver disease, have discovered that, despite consuming fewer drinks per day and for shorter
“A composite of national surveys analyzing alcohol use trends in the early 21st century revealed a 6% increase in the number of adult women who drink, while adult men decreased by 0.2%. Additionally, the number of adult women reporting binge drinking rose by 14%, whereas men experienced only a 0.5% increase.”
durations, females exhibit increased levels of biomarkers indicative of hepatic dysfunction (i.e., alanine aminotransferase (ALT) and aspartate aminotransferase (AST)) when compared to males.
When examining changes in brain matter, women with AUD were observed to have smaller volumes of gray matter and white matter, along with larger sulci and ventricles compared to controls These alterations were more pronounced in women compared to men with AUD. In summary, these findings imply that females are more sensitive to the neurotoxic effects of alcohol.
Alcohol additionally heightens the risk of breast cancer, the most prevalent oncological disease in women. Women who moderately consume alcohol (defined as 1-2 standard drinks per day) are identified to have a 30-50% increased likelihood of developing breast cancer This is believed to result from alcohol’s association with elevated levels of circulating estrogen.
These female-specific alcohol-related effects have taken a toll on our healthcare system and are especially reflected in the emergency department (ED). A 2018 publication by White et. al details that women suffering from the acute and chronic effects of alcohol seeking out ED care increased 70%, compared to 58% among men What may be the most disturbing statistic is that over the course of recent years, mortality has increased by 136% for females suffering from AUD when compared to males at 93% This trend continues for our youngest females aged 16-20, where deaths associated with accidental injuries and overdoses increased, while staying constant for males.
These female-specific alcohol-related effects have placed a strain on our health care system, notably evident in the emergency department (ED). A 2018

publication by White et al. details a 70% increase in women seeking ED care for the acute and chronic effects of alcohol, compared to a 58% increase among men. Perhaps the most alarming statistic is the recent surge in mortality rates, with a 136% increase for females suffering from AUD compared to a 93% increase in males. This trend persists among our youngest females aged 16-20, where deaths associated with accidental injuries and overdoses have risen, while remaining constant for males.
Continued research on the gender and sex-specific effects of alcohol consumption is undoubtedly necessary.
However, it is essential that we identify the factors driving increased alcohol consumption among women and consider potentially impactful ED-based interventions

Dr. Garcia-Diaz is a PGY-3 emergency medicine resident at the University of Alabama at Birmingham (UAB). He will be beginning a research fellowship at UAB in 2024.

By Michelle Hughes, MD; Stephanie Cohen, DO; Tiffany Moadel, MD; and Sara Hock, MD, on behalf of the SAEM Simulation Academy
Physicians encounter both summative and formative assessments throughout their education and training. Simulationbased medical education is firmly established as a standard component of residency training, with more than 90% of emergency medicine residency programs incorporating this educational modality[1]. It is also widely accepted in undergraduate medical student education[2]. While data exists to demonstrate the benefits of simulation as an assessment tool in the realms of skills assessment and clinical practice improvement[3,4,5], it is essential to clearly understand the definitions and nuances of formative and summative assessments in relation to simulation and their evolving use within the emergency medicine specialty.
Formative-based simulation experiences can be considered for learning purposes exclusively; this assessment type involves no grades and is considered low or no-stakes. It frequently occurs throughout an entire training period at regular intervals and includes immediate debriefing and feedback to enhance knowledge retention among learners[6]. Most commonly, the format comprises a recurring simulation curriculum with high-fidelity mannequin-based cases, often associated with procedural skills and task trainers. Formative assessment requires a significant level of expertise and commitment from faculty facilitating recurring education, providing timely and detailed feedback; this is precisely what is believed to make those learning
encounters engaging and impactful. Skillful facilitators play a crucial role in this environment to ensure the psychological safety of the learners by promoting respectful discourse around simulated experiences. It has also been demonstrated that self and peer assessments foster reflection, promote learning, and lead to skill retention even in these lower-stake environments[7]
Conversely, summative assessment is an evaluative assessment well-suited for evaluating knowledge and core content, commonly employed in preclinical medical education[7]. Summative assessment typically carries high stakes for the learner, contributing to a course grade, graduation eligibility, and, in some instances, board certification[6]
Traditional summative-based simulation in medical education has involved Objective
Structured Clinical Examinations (OSCE) conducted in medical school; a significant number of U.S.-based medical schools mandate a standardized patient or OSCE-based final exam[8]. The previously required USMLE Step 2 CS for allopathic medical students has been discontinued without a replacement, placing the responsibility of clinical skill assessment solely with individual medical schools[9]. Given the high-stakes nature of summative-based assessment, ensuring quality assurance, score reliability, and the validity of decisions and inferences made on scores is vital [10]. Despite good intentions, learners in high-stakes summative environments are much less
likely to experience psychological safety due to the stress associated with the assessment outcomes[11]
When choosing between formative and summative-based assessments, it is crucial to identify the assessment's purpose, the skills being assessed, and to recognize the differences in planning and execution required for each. Both summative and formative assessments in simulation play a role. As medical education progresses, it is essential to recognize the goals and objectives of each simulation-based curricular element to facilitate learner growth in nurturing, psychologically safe environments, and to enable practice and assessment with higher-stakes trials. Each educator bears the responsibility of ensuring
1. National Growth in Simulation Training within Emergency Medicine Residency Programs, 2003-2008
2. The History of Simulation in Medical Education and Possible Future Directions
3. The Use of Simulation for Emergency Medicine Resident Assessment
4. Review of Mannequin-based High-Fidelity Simulation in Emergency Medicine
5. Assessment of Clinical Skills Using Simulator Technologies
6. Debriefing as Formative Assessment: Closing Performance Gaps in Medical Education
7. Assessment in Medical Education: What are we trying to achieve?
8. AAMC Curriculum Reports: “SP/OSCE Required Final Examinations”
9. AMA: “USMLE Step 2 CS canceled: What it means for medical students”
10. Summative Assessment in Medicine: The Promise of Simulation for Highstakes Evaluation
11. Psychological Safe Environment: A Concept Analysis
“Simulation-based medical education is firmly established as a standard component of residency training, with more than 90% of emergency medicine residency programs incorporating this educational modality.”
the appropriate type of assessment is used and that the overall methods and objectives are transparent to all participants.

Dr. Hughes is an assistant professor of emergency medicine at the University of Wisconsin School of Medicine and Public Health. She serves as the director of medical simulation for the Emergency Department Residency and Simulation Fellowship Program Director. She is also the faculty lead for faculty and advanced practice provider simulation education. Dr. Hughes is the current secretary on the SAEM Simulation Academy and immediate past secretary for the International Meeting on Simulation in Healthcare (IMSH) EM section.

Dr. Cohen is an assistant professor of emergency medicine at the University of Central Florida College of Medicine. She serves as the simulation director for the emergency medicine residency and program director of the simulation fellowship. She is the current vice president of membership for the SAEM Simulation Academy.

Dr. Moadel is an assistant professor of emergency medicine at the Zucker School of Medicine at Hofstra/Northwell. She also serves as the director of the medical simulation fellowship within the Northwell Health Emergency Medicine Service Line and director of medical student simulation for the North Shore-LIJ Emergency Medicine Residency Program. Dr. Moadel currently serves as the treasurer for the SAEM Simulation Academy.

Dr. Hock is an associate professor of emergency medicine at Rush University and the current director of emergency medicine simulation, as well as the program director of the simulation fellowship. She is the director of assessment at Rush Medical College. She is the current president of the SAEM Simulation Academy.
The Simulation Academy focuses on the development and use of simulation in emergency medicine education, research, and patient care. Membership in SAEM's academies and interest groups is free. To participate in one more groups: 1.) log into SAEM.org; 2.) click “My Participation” in the upper navigation bar; and 3) click “Update (+/-) Academies or Interest Groups.”

By Natalie Strokes, DO, MS; Lauren Westafer, DO, MPH, MS; Bill Soares, MD, MS; and Elizabeth Schoenfeld, MD, MS, on behalf of the Social EM and Population Health Interest Group
The Case
Your next patient is a 33-year-old female with a forearm abscess and cellulitis. She has endured a 10-hour wait in your waiting room due to current capacity challenges. Upon examination, she appears restless, anxious, sweaty, with notable goosebumps. Vital signs reveal a heart rate of 110 and a temperature of 100.2. She explains that she attempted to manage the abscess at home with warm compresses, but it has worsened over the past three days. She discloses injecting heroin/fentanyl into that area about 5 days ago. She mentions experiencing pain all over, along with recent nausea and diarrhea. Notably,
her medical record indicates a similar presentation a year ago when she left against medical advice (AMA) despite being tachycardic and febrile at that time.
The Discussion
In addition to treating her cellulitis, what additional care does she require? What resources does your emergency department (ED) have to increase the likelihood that she stays for her needed antibiotics? How can you reduce her risk of bacterial endocarditis and overall improve her health while decreasing mortality? Managing patients with opioid use disorder (OUD) can be challenging. These patients can be
medically, socially, and emotionally complex, often with priorities misaligned with the health care team. Despite this, the health risks they face are clear: ED patients presenting with a nonfatal opioid overdose have a 1-year mortality of 5.5%, comparable to patients admitted for NSTEMI. Those in withdrawal, presenting with injectionrelated infections or opioid withdrawal alone, are frequently offered marginally effective treatment, increasing their likelihood of leaving AMA and hindering future access to medical care during episodes of illness or withdrawal. The burden of OUD-related infections is substantial, with OUD-related infections

Start buprenorphine or provide prescription
Dose methadone in the ED for withdrawal (20mg or 30mg)
Link to methadone clinic (i.e. sealed last dose letter and instructions for follow-up)
Dispense intranasal Naloxone
Dispense needles
Dispense supplies to clean skin and keep injection supplies clean (alcohol wipes, sterile water)
Inquire about injection techniques and educate about safest options
NA – all clinicians can do this at this time
NA – all clinicians can do this at this time
Provide list of local methadone clinics
Prescribe intranasal Naloxone
Provide list of local resources (i.e. for syringe access*)
NA – all clinicians can do this at this time
NA – all clinicians can do this at this time
NA-Not Applicable. *Some states may not allow syringe distribution at this time
costing the U.S. health care system over $700 million in 2012 alone, excluding indirect costs and lives lost. If current trends persist, the U.S. could lose more than a quarter of a million lives to intravenous drug use (IVDU)-infective endocarditis alone between 2020 and 2030, in addition to lives lost to overdose and other infections.
When caring for OUD patients, clinicians can reduce the likelihood of patients leaving AMA by prioritizing the alleviation of suffering—treating withdrawal. Adequate withdrawal treatment increases the likelihood that patients will stay for antibiotics, admission, and other necessary aspects
of care while fostering trust in health care providers. The simplest approach is to manage pain and withdrawal with opioid agonists (morphine, hydromorphone, methadone) or a partial agonist like buprenorphine, depending on clinical circumstances. Regardless of local ED follow-up pathways, administering buprenorphine or methadone are reasonable and legal options that do not require additional licensing or protocols. Emergency medicine guidelines are clear that opioid agonists should be the first-line treatment for withdrawal, with “comfort” medications such as
• Avoid using alone. If an overdose occurs, having someone present can provide assistance.
• Exercise caution if it's been a while since your last use. The risk of overdose is higher in such situations.
• Avoid mixing substances. Overdoses frequently result from combining heroin or painkillers with other drugs such as benzodiazepines, methadone, antidepressants, or alcohol.
• Perform a tester shot to ensure a new batch is not excessively potent.
• Develop an overdose plan. Stay prepared with naloxone and keep a phone handy for potential 911 calls.
• Don't hesitate to call 911. If you suspect someone is overdosing, calling 911 is crucial. The law provides substantial protection from prosecution in such cases.
• Use new equipment — never share. Many communities offer free, anonymous distribution of syringes and drug use paraphernalia.
• Never lick needles, always use sterile water, and dispose of cotton after each use.
“ED patients presenting mortality of 5.5%, comparable

presenting with a nonfatal opioid overdose have a 1-year comparable to patients admitted for NSTEMI.”
continued from Page 73
ondansetron, clonidine, loperamide, and lorazepam as supplementary, albeit less effective options.
Federal law allows for the treatment of opioid withdrawal in the emergency department with buprenorphine or methadone. Distribution of harm reduction supplies, including syringes, is regulated by state law. More information about your state laws regarding harm reduction supplies is available here.
Once patients are comfortable enough for conversation, clinicians can provide harm reduction education and supplies, depending on availability. Harm reduction not only makes drug use safer, reducing morbidity and mortality, but also facilitates open and non-judgmental conversations about drug use. Engaging patients in such discussions may increase trust, making it easier to provide necessary supplies and care. Clinicians can mitigate stigma by directly offering supplies, saying, “We have new needles; do you know anyone who might benefit from them?” allowing patients to accept supplies for others if they prefer not to discuss their own use. Many OUD patients have been conditioned by
previous medical experiences to tell clinicians, I’m never going to use again!”, a learned behavior that may discourage clinicians from offering harm reduction resources.
Harm reduction is an evidence-based approach that is critical to engaging with people who use drugs and equipping them with life-saving tools and information to create positive change in their lives and potentially save their lives.
As emergency physicians, we take pride in our ability to provide treatment and perform lifesaving procedures with 24/7/365 availability. In the face of the ongoing opioid epidemic and the alarming rate of lives lost, our skills and availability can contribute to providing lifesaving treatments in this context. Emergency physicians are often the first doctors OUD patients encounter after an overdose and perhaps the only ones seen in years when seeking care for an infection. To prevent future morbidity and mortality, addressing barriers to care, especially the fear of withdrawal, is crucial. We must use available resources to assist patients with OUD in any way possible.
You prescribe methadone to your patient, initiating at a dose of 20 mg based on her recent usage patterns. She begins to feel better, allowing for the collection of labs, initiation of antibiotics, and ultrasound examination of her abscess. As she
• Initiation and Rapid Titration of Methadone in an Acute Care Setting for the Treatment of Opioid Use Disorder: A Case Report
• Guidelines for the Psychosocially Assisted Pharmacological Treatment of Opioid Dependence
• Safety of Rapid Inpatient Methadone Initiation Protocol: A Retrospective Cohort Study
• SHOUT Guideline: Inpatient Management of Opioid Use Disorder: Methadone
• American Society of Addiction Medicine National Practice Guideline for the Use of Medications in the Treatment of Addiction Involving Opioid Use
• Recommendations for Methadone Induction, Titration, & Stabilization in the Treatment of Opioid Use Disorder
becomes calmer, you discuss harm reduction, and she reveals access to new needles but occasional needle reuse. Further discussion reveals that although she uses alcohol wipes, she habitually licks the needle before injection. You inquire about her knowledge regarding bacteria in the mouth, and she realizes that her mouth might be the origin of her current infection, despite her efforts to keep her skin clean. Your ultrasound confirms a deep, intramuscular abscess, and you are relieved that she is calm, comfortable, and willing to stay for continued care.
Funding for this initiative was made possible (in part) by grant no. 1H79TI086770 from SAMHSA. The views expressed in written conference materials or publications and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services; nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.

Dr. Schoenfeld is a practicing emergency physician and the vice chair of research in the department of emergency medicine at UMass ChanBaystate where she also serves as research faculty in the Department of Healthcare Delivery and Population Health.

Dr. Strokes is an instructor in emergency medicine at UMass Chan - Baystate. She is currently a health equity fellow at Baystate and is simultaneously pursuing her Master of Public Health (MPH) at UMass-Amherst, both of which will be completed this summer. She is passionate about minimizing disparities within emergency medicine while providing high-quality care for patients.


Dr. Westafer is an assistant professor of emergency nedicine at UMass ChenBaystate
Dr. Soares is an assistant professor of emergency medicine at UMass ChenBaystate

By Tony Fabiano, MD
As emergency physicians, our adaptability, innovative mindset, and comfort with uncertainty have played a pivotal role in the growth and success of our specialty. These attributes not only prepare us for excellence in the emergency department (ED) but also extend our expertise beyond the traditional emergency department setting, uniquely positioning us for the expanding domain of telehealth.
Telehealth’s potential in emergency medicine goes beyond virtual urgent care, remote triage, e-consults, and providing critical emergency medicine
expertise to remote and underserved areas. More profoundly, it represents our role in shaping an increasingly digital and decentralized health care model, causing ripples across all specialties.
On the ground floor of the house of medicine, we face the repercussions of inaccessible health care daily. We witness the consequences when patients cannot access the care they need, leading them to our emergency departments when their primary care physician is unavailable, requiring a squad when transportation is an issue, and turning to us when they have nowhere else to go. What if, as
emergency physicians, we could pivot from being the last line of defense to becoming proactive architects in a more accessible and efficient health care system?
Telehealth is not just a tool; it’s a gateway to crafting the future of health care, enhancing both patient and provider experiences. However, this evolution demands visionary leadership — leaders who are innovative, adaptable, capable of highstakes decision-making, and adept at fostering cross-specialty collaboration. Emergency physicians embody these qualities, and with looming workforce

“Telehealth's potential in emergency medicine goes beyond virtual urgent care, remote triage, e-consults, and providing critical emergency medicine expertise to remote and underserved areas. More profoundly, it represents our role in shaping an increasingly digital and decentralized health care model, causing ripples across all specialties.”
challenges in our specialty, the call to action to embrace telehealth becomes even more critical. We must adapt swiftly, using telehealth not only to extend our reach but also to alleviate pressures on our physical emergency departments.
As health care institutions establish their “digital front doors” to adapt to this decentralized health care paradigm, our active participation is non-negotiable. If we, as emergency physicians, do not lead this transformation, other specialties might sideline our crucial role in this new era of health care. Every medical specialty will be influenced by these changes, making it incumbent upon us to lead, ensuring our specialty’s central position in the health care system’s future.
For those at institutions where telehealth is still nascent, the path to integration may seem formidable; however, numerous resources are available. The SAEM Telehealth Interest Group, the AMA Telehealth Implementation Playbook, and the National Consortium of Telehealth Resource Centers provide comprehensive guidance, from practical implementation tactics to insights on the intricacies of virtual care. For those at institutions with established telehealth programs, this is your opportunity to dive in. Join initiatives, absorb knowledge from colleagues, and emerge as a leader in telehealth. The future of emergency medicine, and our ability to adapt to and
remain at the forefront of health care innovation, depends on our proactive embrace and leadership of these digital transformations.

Dr. Fabiano is a PGY-4 at the University of Cincinnati. He will be starting a virtual care and innovation fellowship at Thomas Jefferson University in July. He believes in leadership and advocacy through entrepreneurship and plans to leverage telehealth to drive innovations in patient care over the coming decades.

By Joseph Pare, MD, MHS; Erika Constantine, MD; and Kristin Dwyer, MD, MPH, on behalf of the SAEM Academy of Emergency Ultrasound
Trauma center verification falls under the purview of the American College of Surgeons’ (ACS) Verification, Review, and Consultation (VRC) Program. This program evaluates hospitals’ resources, structures, and processes to ensure compliance with published guidelines for injured patient care, last updated in 2022 as “Resources for the Optimal Care of the Injured Patient.” Trauma site verification, active at 578 U.S. trauma sites, has demonstrated an association with reduced mortality. The VRC type I standards are “critical standards that directly impact patient care.” Failure to meet these standards results in the denial of trauma center verification.
As per the most recent VRC guidelines, medical imaging standards generally fall under the radiology department’s jurisdiction. However, we wish to highlight a new type I
“Under the new guidelines, functioning ultrasound machines and qualified medical professionals must be available 24/7 to perform POCUS within 15 minutes. This requirement may pose challenges for many level I, II, and III trauma centers.”
standard that focuses on point-of-care ultrasound (POCUS) accessibility within 15 minutes at level I, II, and III trauma centers. The guidelines explicitly state that accessibility implies the availability of necessary human resources and equipment. We want to examine critical aspects because ensuring
rapid access to POCUS necessitates a well-established workflow that relies on several interconnected elements. Notably, the guidelines make no distinction between pediatric and adult trauma centers, meaning pediatric facilities must also adhere to these standards.
“Trauma site verification, active at 578 U.S. trauma sites, has demonstrated an association with reduced mortality. The VRC type I standards are 'critical standards that directly impact patient care.' Failure to meet these standards results in the denial of trauma center verification.”
Under the new guidelines, functioning ultrasound machines and qualified medical professionals must be available 24/7 to perform POCUS within 15 minutes. This requirement may pose challenges for many level I, II, and III trauma centers. Historically, 20% of emergency medicine residency programs (2009) and 23% of pediatric emergency medicine (PEM) fellowships (2021) reported lacking a structured ultrasound curriculum. With emergency physicians having a median age of approximately 50 years and the PEM workforce averaging 19.6 years postmedical school, a substantial number of actively practicing physicians were trained when POCUS was not an integral part of their education. Given the current composition of the emergency medicine (EM) and PEM workforce, it is likely that numerous physicians at trauma centers may lack the credentials or skills required for POCUS as stipulated by the updated 2022 VRC guidelines. To meet these revised guidelines, facilities must devise plans to ensure the availability of POCUSqualified physicians and workflows for performing appropriate trauma-related ultrasounds.
The guidelines do not stipulate the types of POCUS exams required at trauma sites. However, we advocate for proficiency in performing and interpreting extended focused assessment with sonography in trauma (EFAST) and procedural guidance as a minimum requirement. While there is controversy about the utility of EFAST in the pediatric population, due to poor sensitivity
for detecting intra-abdominal injury, it continues to show promise as an adjunct to the physical exam in trauma cases involving children. POCUS is most valuable when patients, regardless of age, are too unstable to travel, but its importance is not limited to unstable patients, as even in the hemodynamically stable patient, it can identify early signs of life-threatening injuries.
Though not directly addressed in the guidelines, performing ultrasounds that guide management requires a workflow solution for image storage and documentation in the patient chart. When medical decision-making relies on POCUS, recorded, documented, and discoverable images are crucial, and should be part of the patient record. The practice of “phantom” or “ghost” scanning, in which an ultrasound is performed but not recorded and documented, is unacceptable due to legal and billing implications.
POCUS skills are now imperative for managing injured patients at accredited trauma centers and can no longer be considered optional, based on ACS recommendations. Although the VRC does not establish a specific standard of care, the ability to conduct POCUS studies at level I, II, and III centers will directly influence site verification. We emphasize these updated standards. While some surgical colleagues may possess training and credentials for POCUS, ensuring timely availability to patients necessitates the presence of qualified and experienced emergency
medicine physicians, along with the associated systems. The evaluation of POCUS capabilities will be assessed at site visits commencing September 2023 and beyond.

Dr. Pare is director of ultrasound research in the department of emergency medicine at the Warren Alpert Medical School of Brown University. His area of academic interest is cardiopulmonary ultrasound and the use of artificial intelligence for point of care ultrasound. @BrownUltrasound

Dr. Constantine is a pediatric emergency medicine physician at Hasbro Children’s Hospital and director of pediatric emergency ultrasound in the department of emergency medicine at the Warren Alpert Medical School of Brown University. Her academic interests include ultrasound education and ultrasound use in resource-limited settings.
@BrownUltrasound

Dr. Dwyer completed her residency at Boston Medical Center and ultrasound fellowship at Brigham while obtaining an MPH in quantitative methods at Harvard. She joined Brown in 2016, where she is an associate professor and serves as the director of the emergency ultrasound division and fellowship. @BrownUltrasound
The Academy of Emergency Ultrasound is an international forum bringing together clinician sonologists with the common goal of advancing patient care and safety through the use of bedside ultrasound. Joining AEUS is free! Just log in to your member profile. Click “My Account” in the upper right navigation bar. Click the “Update (+/-) Academies and Interest Groups” button on the left side. Select the box next to the academy you wish to join. Click “save.”

By Jace Morganstein, MD, MS and Elizabeth Yetter, MD, MHPE
Ovarian hyperstimulation syndrome (OHSS) is a recognized complication of assisted reproductive technology (ART) that leads to a considerable number of emergency department visits annually and is a significant contributor to ascites and dyspnea While OHSS typically manifests with mild symptoms, it can progress to an acute, life-threatening condition with complications such as hypotension, pulmonary edema, and severe electrolyte abnormalities. This article presents a case where a patient undergoing fertility treatment, presenting with ascites and dyspnea, was diagnosed with severe hyperkalemia as a complication of OHSS.
A 40-year-old female with a history of polycystic ovarian syndrome presented to the emergency department with one day of shortness of breath and abdominal distention. She had recently completed a course of clomiphene and follitropin therapy for fertility treatment and underwent ovum retrieval six days prior. Two days earlier, she had an outpatient paracentesis for ascites, with 1.2L removed and symptomatic improvement but presented to the emergency department with the return of worsening symptoms. She denied any prior liver, cardiac, or renal comorbidities. Review of systems was
negative for chest pain, cough, vaginal bleeding, and fever.
Initial vital signs were a blood pressure of 129/102 mmHg, a heart rate of 89 beats/minute, a respiratory rate of 14 breaths/minute, and an oxygen saturation of 98% on room air. She was afebrile. Physical exam revealed an uncomfortable, diaphoretic woman with a distended, non-tender abdomen. No lower extremity edema or jugular venous distension was appreciated.
Initial laboratory testing revealed hemoconcentration with a hematocrit of 62.1%, hyponatremia of 128 mmol/L, and notably, hyperkalemia with a
“Emergency point-of-care ultrasound examinations of the abdomen and chest were performed, revealing significant ascites and pleural effusions, along with markedly enlarged ovaries consistent with severe ovarian hyperstimulation syndrome.”
potassium of 9.1 mmol/L, confirmed by whole blood potassium sampling. An EKG showed peaked T waves, with no QRS prolongation.
Emergency point-of-care ultrasound (POCUS) examinations of the abdomen and chest were performed. Chest sonography revealed mild bilateral pleural effusions, noted by a positive spine sign at the lung bases. FAST exam of the abdomen revealed significant ascites in the right and left upper quadrants (Figure 1). No pericardial effusion was noted on the subxiphoid view. The pelvic view revealed further intraperitoneal free fluid and grossly enlarged, polycystic ovaries consistent with severe OHSS (Figure 2).
The patient received immediate treatment with 2g of calcium gluconate, insulin, and dextrose. Continuous telemetry monitoring was initiated, and her potassium down-trended to 5.7 mmol/L on repeat sampling. She was admitted to internal medicine with gynecology as a consulting service and transferred to the floors in stable condition. On the first day of hospitalization, telemetry monitoring showed no events, and she was started on sodium-zirconium cyclosilicate for potassium excretion. On the second day, abdominal distention worsened but did not cause hemodynamic instability or worsening shortness of breath. Gynecology recommended outpatient follow-up with the patient’s fertility clinic for paracentesis. Repeat chemistry on that day showed a potassium of 4.1 mmol/L, and the EKG showed normal sinus rhythm without peaked T waves or QRS prolongation. The patient was deemed stable for discharge and instructed to complete outpatient followup at her fertility clinic.
Ovarian hyperstimulation syndrome (OHSS) primarily affects patients undergoing fertility treatment via assisted reproductive technology (ART), although


non-iatrogenic causes may also be implicated. Mild OHSS is estimated to occur in 20-30% of all in-vitro fertilization cycles During ART cycles, exogenous gonadotropin is administered to stimulate ovarian follicle development, Following the completion of the gonadotropin course, human chorionic gonadotropin
(hCG) is administered to finalize follicular maturation and luteinization of ovarian granulosa cells. In OHSS cases, the administration of hCG and subsequent follicular maturation lead to the secretion

“While hyperkalemia is an uncommon consequence of ovarian hyperstimulation syndrome, this case highlights its importance as a complication that should be considered when evaluating patients with the condition.”
ULTRASOUND CASE REPORT
continued from Page 81
of vasoactive substances, thereby increasing capillary permeability.
Vascular Endothelial Growth Factor (VEGF) is the primary vasoactive substance released by granulosa cells after hCG administration. VEGF exerts a potent influence on vascular permeability, causing disruption of the capillary endothelium and resulting in capillary leakage. This, in turn, leads to the development of ascites, pleural effusions, and pulmonary edema. In instances of severe OHSS, this pronounced capillary leak can give rise to significant electrolyte abnormalities, including hyponatremia and hyperkalemia, as observed in this case.
Similar to other pathologies leading to third-spacing, severe OHSS can induce hyperkalemia by impairing the renal processes that regulate potassium homeostasis. As capillary leak intensifies and intravascular volume diminishes, there is a reduced delivery of sodium and water to the distal nephron and cortical collecting duct in the renal collection system. This reduced delivery of sodium and water, in turn, leads to decreased potassium excretion via the BK channels in the cortical collecting duct. Consequently, potassium excretion in the urine is diminished.
The Renin-Angiotensin-Aldosterone system is concomitantly activated as intravascular volume is depleted. While Aldosterone typically acts to increase potassium reabsorption from the distal nephron, the heightened mineralocorticoid activity does not adequately compensate for the absence of potassium secretion in the CCD. This process, ultimately resulting in potassium retention, contributes to the hyperkalemia sometimes observed in OHSS. Emergency physicians should be mindful of this potentially fatal complication when treating a patient with OHSS and treat accordingly.
In diagnosing OHSS, a supporting patient history is crucial, given that the condition typically arises in the context of a recent ART cycle. However, obtaining such a history may not always be feasible, especially in severe cases. Emergency medicine physicians can benefit from point-of-care ultrasound (POCUS) to arrive at an accurate diagnosis. Ultrasonographic findings indicative of OHSS include significantly enlarged ovaries containing multiple follicles and cysts, typically enlarged up to 10 cm in diameter. Notably, there have been reports of ovaries measuring 12-25 cm in diameter, posing a risk for rupture, hemorrhage, or torsion
In severe OHSS cases, ultrasound findings may include intra-abdominal and pelvic free fluid, along with pleural or pericardial effusions. These findings suggest to the emergency medicine physician that OHSS may be the underlying cause of the patient’s presentation.
OHSS is a complication of ART that can present in its severe form as a lifethreatening condition. Our patient initially presented with normal vital signs but was later discovered to have significant hyperkalemia, along with pleural effusions and marked ascites. A prompt bedside ultrasound examination confirmed the reaccumulation of ascites, pleural effusions, and markedly enlarged ovaries consistent with OHSS. This underscores the critical role of sonographic examination when evaluating a patient with ascites and shortness of breath.
While hyperkalemia is an uncommon consequence of OHSS, this case highlights its importance as a complication that should be considered when evaluating patients with the condition.
Ovarian hyperstimulation syndrome (OHSS) is not a common presentation in the emergency department. While patients with OHSS can sometimes
be managed on an outpatient basis, more severe cases necessitate inpatient treatment. In rare instances, OHSS can lead to acutely life-threatening complications, including severe hypotension, abdominal compartment syndrome, acute respiratory distress syndrome, and, as observed in our case, severe electrolyte abnormalities
It is crucial for the emergency medicine physician to be vigilant, identify, and promptly treat these severe manifestations of the disease. Additionally, the more common presenting signs and symptoms of OHSS, such as peripheral edema, abdominal distention, and shortness of breath, can masquerade as numerous other disease processes routinely encountered in emergency medicine, including heart failure, liver failure, renal failure, and sepsis. A supporting history may not always be available in patients with severe presentations, and POCUS can aid in arriving at the diagnosis.
Abdominal ultrasonography will reveal enlarged, polycystic ovaries, ascites, and possibly pleural or pericardial effusions. Armed with this information, emergency physicians can effectively manage the disease and coordinate appropriate gynecologic care.


Dr. Morganstein is an attending physician at Hunterdon Medical Center where he practices emergency medicine and urgent care.
Dr. Yetter is an assistant professor of emergency medicine and serves as the ultrasound division director at Mount Sinai Morningside and Mount Sinai West in New York City. elizabeth.yetter@mountsinai.org

By Josie Valenzuela, MD
It’s July again, and your site’s residency director has asked you to give the ultrasound IV workshop for the interns. Piece of cake, you think. But wait! The workshop is next week. All 18 interns will need to practice, and you have the night shift for three of those days. What will you do for the phantoms? A quick internet search shows a dizzying number of options. Good news! I researched and tested them, so you don’t have to. Let’s discuss.
For IV phantoms, the vessels are the star of the show. Your model should emphasize haptic feedback and psychomotor coordination between the needle and the probe, allowing the learner to trace the needle tip into
the vessel itself. Many articles will recommend using modeling balloons, but these have two core disadvantages. First, we know from Michael Wittig’s 2010 Journal of Emergency Medicine paper that vessels greater than 4mm in diameter, or around 3/16 inch, are the most likely to be successfully cannulated. An ideal phantom will have vessels around this size. With a modeling balloon, the amount of pressure with which you fill the balloon will determine its diameter; getting a specific diameter is difficult. The second disadvantage of modeling balloons is that, unlike a real vein, they give a hard “pop” on needle entry into the vessel. Training with modeling balloons may engender learners to expect a “pop” that does not exist in real life. Better to create a tract in your phantom that does not have a hard wall. Next, for vessel
placement, remember that vessels less than 1.6 cm in depth are the most likely to be cannulated (Nova Panebianco, Academic Emergency Medicine, 2009), and vessels less than 1.2 cm deep are more likely to stay cannulated (J. Matthew Fields, American Journal of Emergency Medicine, 2014). With all this in mind, I use 3/16 inch outer diameter silicone tubing (amazon.com, $8.99 for 10 feet) to create the tracts for vessels and place them between 0.5 and 1.5 cm deep. Then I fill the tracts with plain water as gel-filled tracts cause shadows from air bubbles.
Once you have vessels, you need tissue. The main choice here is whether to use food or synthetic gel. Food choices include chicken, tofu, SPAM, and food gelatin. I agree in part with
“Your model should emphasize haptic feedback and psychomotor coordination between the needle and the probe, allowing the learner to trace the needle tip into the vessel itself.”
Lauren Selame’s 2021 paper in The Journal of Vascular Access, which compares do-it-yourself ultrasound vascular phantoms head-to-head. Of the food options, all except SPAM give a good sonographic appearance. Chicken and tofu have the advantage of not creating sonographic “tracks.” Here is where my experience differs from Dr. Selame’s evaluators. The downside of using food is it’s messy and hard to work with, plus it’s perishable, so you will need to prepare the phantoms within a few days of using them. You also need to store them in the fridge. Chicken in particular poses difficulty with tract creation, requiring the use of modeling balloons. Food gelatin turned my kitchen into a sticky nightmare. Tofu required the use of modeling balloons and disintegrated quickly under repeated use. What you gain in sonographic appearance from these options, you lose in the hassle of preparation and storage, poor vessel penetration haptics, and perishability. Overall, I recommend skipping food options and using synthetic gel. It is stable at room temperature, easy to work with, and reusable. You can prepare multiple phantoms weeks or months in advance and in bulk. You can place vessels tracts precisely and easily. While early models, like Richard Amini’s 2015 World Journal of Emergency Medicine recipe, used ballistics gel, which is firmer than normal tissue, medical phantom gel is now available to purchase online by the pound (humimic. com, $35.98 per pound). Each trainer requires about 0.7 pounds of gel. This gel is marginally more expensive, but much softer, giving more realistic haptic feedback. The #2 gel is just the right level of softest without falling apart too easily. Finally, you need a mold for your gel. Most articles recommend using a plastic food container to shape the gel. This has two disadvantages: First, you can’t heat the plastic in the oven, so you must pour hot gel into the container and immediately cool it, which causes bubbles and mess. Second, the plastic cracks on repeated
use. A substantial improvement is a silicone baking mold. Mini loaf pans (amazon.com, 4 for $9.99) are ideal. They are long and narrow like an arm, but not so deep that they require a lot of gel to fill. You can use a simple hole punch (amazon.com, $19.99) to determine where the vessels go, then insert your silicone tubing into the mold. You can crisscross or layer the tubing to create more challenging trainers. The whole mold can then go into the oven. I put six molds on a half sheet, one on the top rack, and one on the bottom, to prepare a dozen phantoms at the same time. Be sure to make the hole slightly smaller than the silicone tubing to prevent gel leakage. I use a 1/8 inch hole punch and thread 3/16 inch outer diameter silicone tubing.
For cheap and reusable vascular phantoms that can be made quickly to scale, use a soft synthetic medical phantom gel, silicone mini loaf pans, and 3/16 inch outer diameter silicone tubing. Create the mold by using a hole puncher to place 1/8 inch holes no further than 1.5 cm from the surface. Thread the tubing through the holes. Break the gel into small pieces and fill your molds, then bake for two hours in an oven. Cool, remove silicone tubing, place the gel in a fresh loaf pan without holes, and fill with water. The cost comes out to around $35 per trainer. For the price of one CAE Blue Phantom vascular trainer, you can make 18 of these, one for each intern to perfect their IV skills.

Dr. Valenzuela is an assistant clinical professor in the department of emergency medicine for University of Arizona, Phoenix, and Creighton University. She serves as assistant emergency ultrasound director for Valleywise Health in Phoenix, Arizona. josephine_valenzuela@dmgaz.org





By Anisa Heravian, MD and Erica Olsen, MD
Telehealth has assumed a growing role in health care delivery within the acute care setting, accelerated by the global COVID-19 pandemic. However, its widespread integration into medical education curricula has remained limited thus far. In this SAEM Pulse contribution, we describe the development of a pioneering telehealth-based virtual curriculum for first-year medical students, address implementation challenges, and outline future steps in this innovative area of medical education.
Background: Disruption Brings
Innovation
The COVID-19 global pandemic upended traditional clinical and
educational models in health care systems. On March 17, 2020, in response to the escalating cases in the United States, the Association of American Medical Colleges recommended that medical schools temporarily halt in-person clinical rotations for medical students In light of this, educators began exploring alternative methods for clinical teaching, including involving students in the telehealth environment. Prior to the pandemic, telehealth education for medical students had been increasing in frequency and exposure during both pre-clinical and clinical years. While telemedicine in the acute care setting, specifically the emergency department (ED), presented an innovative approach
to patient management, there was limited reporting on telehealth education for medical students in the ED setting. This article describes the creation of a novel telehealth-based virtual curriculum for first-year medical students.
Clerkship Design and Implementation: An Overview
The emergency department clerkship rotation was a component of a general clerkship course for pre-clinical medical students, lasting six weeks. The clerkship comprised virtual didactic/ small group sessions and virtual clinical shifts. Students were assigned to telehealth shifts, collaborating oneon-one with emergency attending providers. Two distinct virtual programs
“As telehealth becomes increasingly integral to health care delivery, introducing it early in training through clerkships like ours will be crucial.”
were staffed, including virtual urgent care and virtual triage, where students observed triage care for patients treated in person in the emergency department (ED). The rotation aimed to increase student awareness and understanding of telehealth’s role in patient care, provide insights into its contextual relevance within the overall health system, and foster communication and professionalism skills. Formal virtual conference orientation, technical and logistical training, and detailed workflow processes for maintaining discretion and patient privacy during telehealth encounters were provided. Additionally, students received weekly core content topics related to medical management in a virtual setting.
Students provided self-report feedback to the medical school during the midpoint of the clerkship and completed pre and post-clerkship surveys. Additional sessions were offered if students felt they lacked sufficient patient experiences on their shifts, and real-time feedback was encouraged.
During the pilot phase of the clerkship, nine students were enrolled, and all successfully completed the program, participating in both pre- and postsurvey assessments on telehealth (100% response rate). In the pre-clerkship survey, none of the participants had prior telehealth experience. However, two out of nine (22%) indicated a good understanding of telehealth, while only one out of nine (11%) felt that telehealth was easily accessible. Following the telehealth rotation, all participants in the clerkship (100%) found the experience valuable and unanimously agreed on the importance of telehealth in emergency medicine. Six out of nine students (67%) expressed a preference for telehealth to be mandatory in the curriculum, with the remaining three being neutral. In the post-survey results, stable perceptions were observed, with two out of seven respondents (22%) stating that they did not believe telehealth to be easily accessible for patients.
Although the small sample size and the single-site nature of our pilot study restrict the generalizability of our findings, our primary focus in this program is to explore the feasibility of a novel approach to medical education in the ED setting. Moreover, despite our efforts to ensure respondent anonymity and clarify that survey participation would not impact students’ evaluations, there exists the potential for response or favorability biases in the self-reporting nature of the participants’ responses.
In our effort to introduce a pilot telehealth clerkship rotation for medical students in the ED, we observed that participants were generally satisfied with the clerkship and acknowledged the importance of telehealth in emergency medicine. Given the rapidly evolving landscape of medical education and clinical care, exacerbated by the global pandemic, telehealth education programs in the ED setting offer a valuable platform for medical students to develop early familiarity and exposure to this distinctive clinical environment and workflow.
Notably, our telehealth clerkship, which centered on a comprehensive telehealth experience, originated in response to the COVID-19 pandemic. The broader clinical and educational constraints imposed during the pandemic allowed this clerkship to complement and facilitate a reimagining of the educational experience within the limitations of reduced in-person clinical opportunities. These observations may have implications for approaches to telehealth education for emergency providers beyond the global pandemic.
While our project primarily aimed to capture students’ self-reports of their clinical experience, the one-on-one nature of telehealth ED clerkships may provide more uninterrupted, face-toface teaching opportunities compared to the physical emergency department. Additionally, involving medical students early in their training in telehealth clinical settings allows them to develop technical familiarity and comfort with the modality,
enhancing their professional awareness of subtle yet crucial features of telehealth encounters. This includes considerations such as the perceived importance of establishing professional home environments and considering factors like lighting, dress code, and eye contact.
Moreover, these clinical encounters offer students an intimate view into a patient’s living quarters and situation. This exposure adds context to the practical implementation and operationalization of treatment recommendations. During the COVID-19 pandemic, students observed poignant instances where patients were instructed to self-isolate if COVID positive, shedding light on the formidable challenges confronting individuals residing in compact living spaces with multiple family members. Firsthand exposure such as this provides students with a direct understanding of the challenges and barriers encountered by patients.
As telehealth becomes increasingly integral to health care delivery, introducing it early in training through clerkships like ours will be crucial. Future work focusing on tailoring telehealth experiences into existing medical student and trainee curricula can explore ways to optimize and create a comprehensive training program adaptable to various clinical innovations in the acute care setting.

Dr. Heravian is assistant professor of emergency medicine and the associate director of adult telemedicine for the department of emergency medicine at Columbia University Irving Medical center in New York City.

Dr. Olsen is assistant professor of emergency medicine and director of telemedicine for the department of emergency medicine at Columbia University Irving Medical center in New York City.

By Ashley C. Rider MD MEHP; Shubhi G. Goli, MD; and Mia L. Karamatsu, MD, on behalf of the SAEM Academy of Women in Academic Emergency Medicine and the SAEM Wellness Committee
It was my first conference since the birth of my baby. Not only was I dreading leaving the baby, I was stressed about managing lactation demands while traveling. Juggling pouring breast milk into storage bags amidst turbulence was tricky but resulted in only a little bit of spilled milk to cry over. Exhausted, I arrived at my hotel room at 1 a.m. ready to transfer the milk to the fridge, only to discover that the fridge was the same temperature as the room.
This incident was just the first of many lactation hiccups that would unfold during the trip.
The arrival of a baby is a life-changing experience, and for parents in academic emergency medicine (AEM), it can also be career changing. The demands of childcare often interfere with professional pursuits, particularly in the first year of an infant’s life. Female faculty with children tend to have fewer publications, slower career advancement, and lower career satisfaction. While participation in professional conferences is crucial for career development and promotion, for lactating individuals, it requires an entirely new set of planning and logistics beyond the usual packing and presentation preparation. With careful
forethought, advice from others in our specialty, and recommendations from other female professionals, managing lactation while traveling can become less daunting. Efforts to improve these experiences are a step in the right direction for gender equity in AEM career development.
• Be honest about your readiness to leave your baby. There will be other conferences. It is okay to say no. Alternatively, if you have the support, consider bringing your baby.
“Juggling pouring breast milk into storage bags amidst turbulence was tricky but resulted in only a little bit of spilled milk to cry over.”
• Maintain a pumping schedule to ensure consistent milk output. Increase nursing frequency upon return.
• Ensure an adequate supply of stored milk or formula for the baby for the duration of your trip.
• Reserve a hotel room with a mini-fridge that has a freezer for ice packs and/or milk storage, ensuring it maintains the recommended temperature of 40° F
• If possible, book the conference hotel to facilitate easier pumping in your room. Otherwise, contact conference coordinators to identify designated lactation areas.
• Most airlines do not count bags containing pumping supplies and breast milk towards your carryon allowance. Verify your airline’s guidelines for pump parts and milk carry-on regulations.
Continuing our commitment to a family-friendly atmosphere at the SAEM Annual Meeting, we are delighted to reintroduce our complimentary, private family/lactation room tailored to meet the needs of both parents and babies. Operating during regular meeting hours, the SAEM24 Family Room is equipped with essential amenities, including a refrigerator for milk storage, wipes, sanitizer, burp cloths, a changing table, comfy chairs, water, and snacks. Moreover, for parents bringing their little ones, we offer complimentary licensed onsite childcare/day camp services. This ensures that you can actively engage in the meeting, knowing that your children are well taken care of. Don't miss out! You must register for childcare by March 12 to take advantage of this parentfriendly offering!
• Frozen ice packs are ideal for TSA screening. Although milk is exempt from TSA quantity limits, it may be subject to testing, so allocate extra time to get through security.
• Familiarize yourself with the Friendly Airports for Mothers (FAM) Act, which mandates designated non-bathroom pumping spaces at most airports.
• While shipping options such as Milk Stork exist to avoid carrying milk on the airplane, they can be expensive.
• Stay hydrated and eat enough food to maintain your milk supply. Bring a water bottle and snacks.
• Block adequate time before commitments for pumping to avoid feeling rushed.
• If you find yourself in a conference planning role, this article discusses best practices for including lactation support



Dr. Rider is a clinical assistant professor of emergency medicine at Stanford University and assistant program director for the EM Residency Program.
Dr. Goli is a pediatric emergency medicine fellow at Stanford University.
Dr. Karamatsu is a clinical assistant professor of emergency medicine and pediatrics at Stanford University.
Pumping-friendly
Extra pump parts
Chargers or batteries
Extra pump
Pump carry bag
Milk storage bottles or bags
Cooler
Ice packs
Wipes for on-the-go cleaning
Liquid soap
Mat or towel for drying parts
Pumping bras
Mik pads
Nursing cover
Snacks
Water bottle or other drinks
Hand sanitizer
Milk "encouragers" (photos, supplements)


By Julie Tondt, MD, on behalf of the SAEM Wellness Committee
The alarm clock rings, waking the baby before I can turn it off. I briefly long for the days of quiet moments before an emergency department shift as I try to feed and rock the baby back to sleep, only to be interrupted by the dogs who have decided now is a good time to start barking. Since the house is now awake for the day, I climb Mount Unfolded Laundry to find a clean pair of scrubs, finish getting myself and the baby ready, and trek downstairs where I hope for, but do not find, any remaining coffee. The nanny arrives, I give our baby one more hug, and leave for the day changing roles from parent to physician.
In brief moments between patient care, tasks, and challenges on shift, I
find myself thinking about my child. “Are there enough clean bottles at home?”
“Does the nanny know the special song for nap time?” The shift moves quickly, I sign out, and finally get back home to relieve the nanny, leaving the weight of the day outside. My husband returns home, the bedtime routine marches on, and we give up our aspirations for a clean house. As I set my alarm clock for another shift, I find myself wondering how everyone else seems to be great at being a parent and a physician while I find myself barely holding everything together as a new attending and parent. A few years later, I now have a toddler, and I have gained an appreciation for the importance of taking time for self-care while navigating life as an EM
physician and parent. Although I am by no means a parenting expert, here are a few tips and pieces of advice, from one EM parent to another, that have had a positive impact on my own life.
According to a 2019 article published by Gade and Yeo work-life integration is an approach that focuses on coordinating different aspects of our personal and professional

“According to a 2019 article published by Gade and Yeo, work-life integration is an approach that focuses on coordinating different aspects of our personal and professional lives. This differs from the approach of work-life balance that views these as two separate areas of our lives.”
lives. This differs from the approach of work-life balance that views these as two separate areas of our lives. Trying to achieve work-life balance may seem challenging, if not impossible, as this approach arguably does not consider the complexity and often necessary overlap of our professional and personal lives. As an EM physician and parent, you are likely already applying the concepts of work-life integration into your day as you continuously move between different tasks, roles, and responsibilities. Leading a virtual work meeting in the morning, picking up your child from daycare in the afternoon, and leaving for a clinical shift in the evening are a few examples of the way our professional and personal lives blend throughout the day.
As a new parent and attending, I often found myself thinking, “I’ll do that later” when it came to investing time in different aspects of my own life and frequently getting to the end of the day after caring for patients and my child and not having any time left for myself. Although I was initially reluctant to add yet another schedule to a seemingly endless list of calendars, I found that writing in time for self-care made it much more likely to be a routine part of my day. Truly use this time, even if you can only afford a few minutes, to focus on your mental and physical health and well-being. Taking a much-needed nap, revisiting an old hobby, exercising, or enjoying the rest of your coffee in the quiet of your car before going inside the house are a few of the many ways you can utilize the time to focus on taking care of

In the second year of the pandemic and several hours away
from the support of family (aside from my husband), I had a baby, graduated from residency, and started my fellowship all within a few weeks. Although I was excited for this new chapter in my personal and professional life, I also at times felt stressed, isolated, and overwhelmed. Parent guilt is real, and I often felt torn between wanting to soak up every moment with my newborn and, after years of training, working toward achieving my professional goals as an EM physician. One key aspect to integrating the roles of being an EM physician and parent was to identify and build a support system. I spoke with colleagues who were also physician parents and learned that I was not alone in my experiences. I gained valuable insight and advice from others who had navigated similar situations, such as finding reliable and affordable childcare. Participating in community events, joining local social media parenting groups, and volunteering for school or extracurricular activities are a few ways to get to know others and expand your support system outside of your parent colleagues.
Early on as a parent, I often tried to find time in the day for bigger activities, such as taking my child to the zoo or amusement park, often at the expense of time I should have used to focus on aspects of self-care, such as getting enough sleep between shifts. I later understood that what was most meaningful to my child was time together, not necessarily the type of activity. In an already full personal and professional schedule, embracing the small moments can have a big impact. There are several ways to incorporate wellness activities with your child into your day: take a silly dance break, attempt a craft, go for a walk, make a meal together. These small, but special, activities can connect you with your child and help you decompress after a busy EM shift.
As emergency physicians, we take care of anyone, anywhere, anytime. The boundaries between physician, parent, and individual can easily become hazy as we try to take care of everyone and everything all the time. Listening to a meeting on the way to daycare dropoff, charting with an infant in our lap, or cheering on the sidelines of a soccer game in our scrubs after a difficult shift are a few places you may find an EM physician parent. Although at times difficult, learning to set personal and professional boundaries in an important aspect of integrating life as an EM physician and parent. Creating a schedule, prioritizing tasks, utilizing your support system, and communicating your boundaries are a few ways to integrate your roles as an EM physician and parent, while also leaving time for you to focus on your own mental health and well-being.
Emergency Medicine is an exciting and rewarding specialty that can also be emotionally and physically demanding. As EM physicians, we lead our team through the controlled chaos of the department as we care for complex and critically ill patients. While the workload of being a parent is not always visible to others, we are truly working a second shift when we arrive home from the hospital. Let us take the time to remember that we are at best equipped to take care of others when we have invested time to care for ourselves.

Julie Tondt, MD is an assistant professor of emergency medicine at Penn State Hershey Medical Center. She completed her emergency medicine residency and a fellowship in medical education at Eastern Virginia Medical School. tondtjm@gmail.com

By Amanda Deutsch, MD; Vytas Karalius, MD; Joselyn Miller, DO; Marla Doehring, MD; and Al’ai Alvarez, MD, on behalf of the SAEM Wellness Committee
I still recall a co-resident sharing her experience about a patient who had become extremely violent toward her. The co-resident screamed, and that action saved both an attending and a nurse from being choked and hit in the head. I cried as she shared her experience, her voice cracking with emotion. It was a stark reminder to all of us, of our humanness and our vulnerability as emergency physicians. We pursued a career in medicine to help others. In our early medical school training, instructors emphasized the importance of positioning ourselves
between the patient and the door as a safety precaution, enabling for a quick exit if threatened. However, as training progressed, these safety reminders dwindled. As an intern, I often found myself in rooms with patients angrily demanding their preferred pain medications. As my skills and confidence grew, I began asserting my boundaries. When patients raised their voices or used profanity, I calmly informed them that I would resume care after they calmed down. Internally, I frequently questioned this approach: Was it correct to say I would return
later? What was my obligation to the patient and myself in a setting where I felt attacked or concerned for my safety? Was it wrong to feel entitled to a secure work environment as an emergency physician?
The Joint Commission defines workplace violence as “an act or threat occurring at the workplace that can include verbal, nonverbal, written, or physical aggression.” This broad definition

“In a 2022 ACEP poll, 66% of emergency physicians reported experiencing assault in their last year of work, with 55% facing physical assault and 79% witnessing an assault. Notably, this poll also revealed an increasing trend in violence: 85% of emergency physicians observed a rise in violence in the emergency department (ED), indicating a significant increase from the 2018 poll results.”
encompasses behaviors ranging from threatening and intimidating to harassing and humiliating, including racial slurs, microaggressions, and physical actions. Unfortunately, at the outset of our training, many of us internalized and accepted such incidents as part of the job. Rarely did we question this norm; instead, we quickly moved on to the next patient.
In a 2022 ACEP poll, 66% of emergency physicians reported experiencing assault in their last year of work, with 55% facing physical assault and 79% witnessing an assault. Notably, this poll also revealed an increasing trend in violence: 85% of emergency physicians observed a rise in violence in the emergency department (ED), indicating a significant increase from the 2018 poll results. Additionally, in 2018, health care workers comprised 73% of all nonfatal workplace injuries and illnesses resulting from violence.
In a profession dedicated to combating violence against our patients, it’s equally important for us to expect more for ourselves and actively prevent the
encounter in our daily work. This violence may manifest in seemingly minor acts or in more overtly horrific events that leave an indelible impact on all of us. The essential out-of-hospital mental assessment, “Is the scene safe?” is a question we must also apply to every patient encounter. If the scene is unsafe, it’s not just acceptable but imperative to learn to protect ourselves and act in our best interest against all forms of workplace violence.
In emergency medicine, we often encounter patients on their worst days, including those with delirium, acute mental health crises, or acute intoxication. Each situation necessitates a unique approach, distinct from handling behavior that arises from causes other than medical conditions. Regardless of the underlying cause of a patient’s behavior, our personal safety is as crucial as patient care, and we deserve a safe working environment. It is critical to ensure that an adequate number of trained staff and necessary equipment are in place before approaching a violent or potentially violent patient. Employing verbal de-escalation techniques and clear behavioral boundaries at the outset of the patient encounter can be beneficial. Using phrases like “You can’t speak to your nurse like that” or “We don’t allow patients to use those words with their care providers” are effective strategies for addressing verbal abuse.

Patients who have decision-making capacity and are not acutely ill should be given the choice to either conclude their ED visit after a medical screening exam or comply with basic behavioral norms. Hospitals have flags in patient charts
to identify those at risk of violent behavior, prompting health care teams to be extra vigilant. Additionally, “behavior contracts” establish boundaries for patients with a history of abusive behavior. These measures are pivotal as we work together to enhance workplace safety for frontline health care workers.
In 2022, Congress passed the Safety from Violence for Healthcare Employees (SAVE) Act, criminalizing violence against health care workers. This legislation, combined with initiatives from the Joint Commission on Workplace Violence, facilitates the creation and implementation of protective measures. The following are straightforward strategies we can employ to educate faculty and colleagues on addressing workplace violence and ensuring their safety in our ED:
1. Understanding the Prevalence and Nature of Workplace Violence. Insights can be gained from our nursing colleagues, particularly in emergency, psychiatric, and medical-surgical areas, who frequently face violence, mainly from patients but also from co-workers. Being aware of the frequency and various forms of such violence is crucial in equipping health care professionals to anticipate and manage potential incidents.
2. Recognize Risk Factors and Protective Strategies. It is critical to recognize risk factors, including mental health disorders, substance abuse, and environmental influences. Similarly, adopting protective strategies such as having a telephone on hand, learning effective de-escalation techniques, undergoing self-defense training, and minimizing interactions with potential perpetrators can be beneficial.

“Behavior contracts” establish boundaries for patients with a history of abusive behavior. These measures are pivotal as we work together to enhance workplace safety for frontline health care workers.”
WELLNESS IN THE WORKPLACE continued from Page 93
Employ Prevention and Harm Minimization Strategies. Effective measures include implementing prevention strategies that heighten barriers against patient-initiated violence and taking action post-assault to support the affected health care professional. This includes screening for weapons in the ED.
4. Develop a Zero Tolerance for Violence. Developing a culture in the ED that supports respect, open communication, employee involvement, and an effective training program can help prevent workplace violence in health care environments.
5. Ensure Organizational and Social Support. Health care workers exposed to violence anticipate both organizational and social support. Ensuring a safe, open communication environment for colleagues to share through the availability of hospital therapy is an important tool. Essential measures include training programs to enhance response skills towards violence and the implementation of workplace violence legislation.
6. Develop Comprehensive Violence Prevention Programs. Crucial elements include evidence-based risk assessment, prevention, management, education, and training, with ongoing adjustments. Strong leadership is critical to the program’s success.
Workplace Violence Resources
• ACEP Workplace Violence & Mental Health
• Joint Commission Workplace Violence Prevention
• ACEP ED Violence Poll
• Poll: ED Violence is on the Rise
• Workplace Violence in Healthcare 2018 Fact Sheet
• Notice of Behavioral Standards at Stanford Medicine
• Workplace Violence in Healthcare Settings: Risk Factors, Implications, Collaborative Preventive Measures
• Interventions to Prevent Aggression Against Doctors: A Systematic Review
• Congress SAVE Act
• Workplace Violence in Healthcare Settings: Risk Factors and Protective Strategies
• Workplace Violence in Hospitals: Safe Havens No More
• A Qualitative System Model for Effects of Workplace Violence & Clinician Burnout on Agitation Management in the ED
For the most up-to-date list of resources, please visit SAEM24 Safety First or scan the QR code.

With rising violence in emergency medicine, taking immediate action is critical to foster a safer workplace. We must rigorously implement comprehensive violence prevention programs, embrace the principles of the SAVE Act, and cultivate a zerotolerance culture for violence. Our commitment must go beyond words and acknowledgments, proactively ensuring a safe and respectful environment for all health care professionals. This is a fundamental right, as we, too, are just as human as our patients





Dr. Deutsch is the director of wellness at Thomas Jefferson Emergency Medicine and the 2024-2025 chair of the SAEM Wellness Committee. @amandajdeutsch
Dr. Karalius is a medical education fellow and clinical instructor at Stanford University. @VytasKaralius
Dr. Miller is an emergency medicine resident at The University of Connecticut.
Dr. Doehring is associate professor of clinical emergency medicine at Indiana University.
Dr. Alvarez, MD, is director of Well-Being at Stanford Emergency Medicine and the 2023-2024 chair of the SAEM Wellness Committee. @alvarezzzy

By Kevin Watkins, MD, on behalf of the SAEM Wilderness Medicine Interest Group
The final subgroup of cardiotoxic plants are the sodium/calcium channel blockers, consisting solely of yews (Taxus spp.). There are numerous species of these evergreen trees worldwide, with the Canada yew (T. canadensis) in the northeast and Pacific yew (T. brevifolia), best known as the source of paclitaxel, prevalent along the west coast.
Yew ingestions are generally uncommon, predominantly accidental, and result in minimal or no toxicity. The majority of involve children ingesting a small number of leaves or consuming the fruit. Lethal ingestions are mainly associated with suicidal intent, with
reported lethal adult doses around 50 grams. An instance exists of an admitted psychiatric patient who took their own life by ingesting yew leaves from hospital grounds.
Yews encompass various taxine alkaloids throughout the entire plant, excluding the fruit pulp, with taxine B being the primary agent. These cardioselective toxins block both Na and Ca channels, disrupting the NaK-ATPase. The toxidrome combines cardiac glycosides and calcium channel blockers. Symptoms usually begin with gastrointestinal disturbance within and hour and progressing to cardiac effects. Patients may experience
decreased cardiac output, bradycardias or QRS widening, potentially leading to ventricular arrhythmias or pulseless electrical activity. The EKG may exhibit the Brugada pattern, and seizures can occur alongside QRS widening. Fatal ingestions typically result in death within 2-5 hours.
There are no specific antidotes and treatment is supportive. Autopsies have revealed yew leaves in the stomach, but rapid gastric absorption raises uncertainty about the efficacy of gastric decontamination. Atropine may be considered for bradycardias and AV blocks, though it is generally ineffective for high-degree AV blocks.


Credit: Mykola Swarnyk (Wikimedia)
Sodium bicarbonate may aid in narrowing widened QRS complexes, and drips may enhance the success of antiarrhythmic agents. High-dose lidocaine appears more effective against ventricular arrhythmias than amiodarone. Pacing may be used, though capture is not always successful. Pressors are
commonly needed for cardiogenic shock. Although some reports have claimed success with digoxin Fab fragments, it remains unclear whether they were truly beneficial, and other studies have found yew toxicity to be refractory to this treatment. Due to the high molecular weight, hydrophobic nature, high protein binding, and large volume of distribution of taxine B, dialysis is not effective. Lipid emulsion has also been proposed; however, most cases have not shown benefit. Extracorporeal life support has been successfully employed in refractory cases.
To summarize, cardiotoxic plants can be categorized into cardiac glycosides, sodium channel openers, and sodium/ calcium channel blockers. All can induce digoxin-like toxicity, though the latter two groups present slight variations in toxidromes. Sodium channel openers are more prone to cause neurological symptoms, while sodium/calcium
channel blockers are inclined to induce cardiogenic shock. Cardiac glycosides typically result in elevated serum digoxin levels and respond to digoxin Fab fragments, whereas the latter two groups often do not.

Dr. Watkins is an assistant professor of emergency medicine at Northeast Ohio Medical University and core faculty at the Cleveland Clinic Akron emergency medicine residency program, where he serves as division head of wilderness medicine. He enjoys teaching with the track and elective as well as the local Wilderness Life Support for the Medical Professional (WLS:MP) program and Cuyahoga Valley Wilderness Medicine Conference. He is a member of the SAEM Wilderness Medicine Interest Group. @kwat2122
Join the Annual Alliance and Enjoy SAEM24 As Never Before!
When you become a 2024 Annual Alliance donor, you not only contribute to advancements in emergency care but also unlock exclusive benefits that express our deepest thanks for your commitment. Some of the benefits most valued by Annual Alliance members are those they receive at the SAEM Annual Meeting, such as:
• Recognition on the prestigious Donor Wall
• Exclusive invitation to SAEMF’s Coffee and Networking Event
• VIP Lounge Access
• Sedan transportation from the airport
Annual Alliance Benefits
(Recognition varies by donor level, click on image!)
A gift of any amount will lead to donor recognition. Your support is not only a donation, it is an investment in the future of emergency care. Check out the SAEMF Impact Report to learn more about how your donation can make a significant impact.
























As we continue to strengthen and diversify the financial support necessary to elevate research and education grants funding, we see even more generosity from SAEM members who have accepted the invitation to become Annual Alliance Enduring Donors. Together with the strength of our endowment — and our entire cadre of Annual Alliance Donors — our Enduring Donors are positioning us to make the biggest leap forward in research funding in our foundation’s history.
We are grateful to the following Enduring Donors who are leading the way to a stronger specialty through their generous giving.























Please join us in saluting the generosity and visionary spirit of philanthropy of our Annual Alliance Donors!
On behalf of the SAEMF Board of Trustees and our grantees, we extend gratitude to our Sustaining Donors who have made a significant gift to ensure more and larger grants are possible in the future.



































Please join us in saluting the generosity and visionary spirit of philanthropy of our Annual Alliance Donors!
Annual Alliance Advocate Donors provide a three-year commitment that is essential to sustaining our grant funding and education programs year-after-year. Many of these generous donors have stepped up this year to increase their commitment to help address challenges facing emergency medicine that are highlighted in our SAEMF Donor Guide
Can we count on you to become an ally for EM research?
• James G. Adams, MD
• Bo D. Burns, DO
• Danielle Campagne, MD
• Chad M. Cannon, MD
• Christopher Robert Carpenter, MD, MSc
• Jeffrey M. Caterino, MD, MPH
• Douglas M. Char, MD
• Ted A. Christopher, MD
• Carl Chudnofsky, MD and Keck School of Medicine of the University of Southern California
• James E. Colletti, MD
• Ted Corbin, MD, MPP
• John DeAngelis, MD, FAEMUS
• Jeff Druck, MD
• Petra Duran-Gehring, MD
• Robert Eisenstein, MD
• Marie-Carmelle Elie, MD
• Prasanthi (Prasha) Govindarajan, MD, MAS
• Erik P. Hess, MD
• Christy Hopkins, MD, MPH, MBA
• Ula Hwang, MD, MPH
• Nicholas J. Jouriles, MD
• Stephanie Kayden, MD, MPH
• Kevin Kotkowski, MD, MBA
• Michael Lozano Jr., MD, MSHI
• Timothy J. Mader, MD in honor of Dr. James Irving Raymond
• Chadwick Miller, MD
• Joseph B. Miller, MD, MS
• James R. Miner, MD
• Bryn Mumma, MD, MAS
• Marquita S. Norman, MD, MBA
• Brian J. O’Neil, MD
• Arthur M. Pancioli, MD
• Peter S. Pang, MD
• Samuel J. Prater, MD
• Robert W. Schafermeyer, MD
• David C. Seaberg, MD
• Peter E. Sokolove, MD
• Mary E. Tanski, MD, MBA
• Terry L. Vanden Hoek, MD
• Scott G. Weiner, MD, MPH
• David W. Wright, MD
• Richard D. Zane, MD
• James M. Ziadeh, MD
As of March 4, 2024
The Annual Alliance’s Mentor Donors generously support our work through a gift of $1,000. Join this group of donors in their support of developing the pathway of future EM researchers and educators by donating today!
• Mike Baumann, MD
• Julianna Jung, MD, MEd
• Nathan Kuppermann, MD, MPH
• Eric L. Legome, MD
• Adrienne N. Malik, MD
• Robert W. Neumar, MD, PhD
Thank you to ALL of our Annual Alliance Donors. Without your support, SAEMF could not make such a significant impact on EM’s future. See the full list of donors.















SAEMF is grateful to these SAEMF Legacy Society Donors who are strengthening the resources available for tomorrow’s emergency medicine (EM) researchers and educators through their legacy giving. Each of these Donors has generously supported SAEMF throughout their careers, and now they have shared that they have made thoughtful, visionary planned gifts by including SAEMF in their estate plans. Through the Legacy Society, you, too, can solidify future support of this organization that’s been so important to you during your career. If you are interested in learning more about legacy giving or the Legacy Society, please let us know. We will coordinate time for you to visit with one of your fellow members who has already made this decision. It may be easier than you think to make such a gift.
Several longtime SAEM members have already included the SAEMF in their estate plans. If you are one of these donors, please let us know by completing the SAEMF Legacy Society Declaration of Intent and returning it to foundation@saem.org so that we can recognize your generosity.
You can Name a grant in honor of someone who has made a difference in your career or in the field. Email Julie Wolfe for details.
Your gift of any amount counts toward participation in the Chairs Challenge (if made before March 22nd), Vice Chairs' Challenge (if made before the end of the AACEM Retreat), and the Academy, Committee, Interest Group Challenge (if made before August 31st). Give once and you are done!
It’s easy to become a Mentor level donor with an annual monthly gift of just $100 (March - December 31, 2024). Pledge that same monthly gift for three years and you’ll be our newest Advocate donor.
Join now to take advantage of 2024 recognition benefits. Your gift will help fund future researchers, educators, and leaders.
You can play a vital role in ensuring greater investments in EM research and education by joining the growing number of SAEM member donors who support the Annual Alliance or become Legacy Society donors each year. An annual gift today or a planned gift for the future will help make more funding available for the SAEMF’s grantees. Donors share why they support SAEMF:

“We have so many aspiring researchers and so many questions that could improve emergency care delivery to our patients and I would like to see these come together. I like to support young researchers who are looking to kick start their research careers and SAEMF has given me the opportunity to do it.”
- Prasanthi Govindarajan, MD, MAS, Annual Alliance Donor

“Reading the stories of those who have been awarded grants and the amazing work that they are doing influenced me to donate.”
- Michelle D. Lall, MD, MHS, Annual Alliance Donor

“At each point of my career, from medical student, to resident, to faculty, SAEM has been instrumental in my professional development. The organization has given so much to me - it felt right to give back.”
- Christopher Bennett, MD, MA, Annual Alliance Donor
Introducing Your 2024-2025 Leaders! Elections are over, the results have been tabulated, and SAEM is pleased to announce the results of recent leadership elections for SAEM, SAEM Academies, Association of Academic Chairs of Emergency Medicine (AACEM), SAEM Foundation (SAEMF), and Residents and Medical Students (RAMS). Thank you to everyone who took the time to vote and congratulations to this year's winners. The 2024-2025 leadership will take office at SAEM24 in Phoenix, Ariz.
Western
There’s Still Time to Register for the March 7-8 Western Regional!
Join us for the 2024 SAEM Western Regional Meeting, hosted by the University of Southern California Keck School of Medicine at the Hyatt Regency Long Beach Hotel on March 7-8, 2024. Themed “Compassion in Critical Times,” this event offers top-tier emergency medicine (EM) research and education for EM physicians. Program highlights include interactive workshops, dedicated tracks, abstract presentations, plenary sessions, and a new Speakers Forum. Don’t miss this enriching experience for academic EM professionals at all career stages. Learn more and register today!

New Englanders, NERDS24 is April 3!
Registration is open for NERDS24, the 27th Annual SAEM New England Regional Meeting, regional meeting, to be held April 3 at the Hogan Campus Center, College of the Holy Cross, Worcester, Mass. The meeting will feature a poster
session, lightning orals, plenary orals, and innovations.
Celebrate Match Day With SAEM and RAMS!
Match Day is right around the corner and we invite all medical students to join SAEM and RAMS as we celebrate this significant milestone in your professional lives. On Friday, March 15 — the big day — be sure to connect with SAEM on social media. Throughout the day we'll be featuring congratulatory videos from residency program directors and chairs across the country, offering their words of wisdom and welcome to all the medical students who have matched.

Share Your Good News for a Chance to Win! Use #RAMSMatch and tag @SAEMonline and @SAEM_RAMS and you'll automatically be entered into a drawing to win a stethoscope or trauma shears.
Attention Academic EM Department Chairs: It’s Almost Time for the Chairs’ Challenge
Each year, the AACEM/AAAEM Annual Retreat in March kicks off this important challenge that raises vital funds to help strengthen the pipeline of emergency medicine (EM) researchers who will advance this specialty in the future. Since 2019, you and generous AACEM members have raised over $410,423 to support your own researchers and educators through SAEMF’s grants. Last
year alone, you raised over $145,598! The Challenge has resulted in a vibrant annual grant funding campaign which has led to SAEMF awarding nearly $1 million back to your departments. In 2024 we hope to turn the challenge map green by achieving 100% participation from AACEM Chairs in each state. Browse the SAEMF Donor Guide to learn about SAEMF’s impact, our researchers and the work they are doing, and how you can join your colleagues in supporting a bold vision for EM research. Then donate today to be one of our first 2024 Chairs’ Challenge donors! No need to wait until the retreat; donate $1,000 today at www.saem.org/donate or by emailing Julie Wolfe at jwolfe@saem.org to pledge.
In this new section we’ll be featuring the wide range of resources SAEM provides members to help them further advance their career in academic EM.
Educational Offerings Guide Highlights SAEM Resources for Each Phase of Your Career
SAEM provides an extensive range of programs and resources tailored to every stage of your academic emergency medicine career. Explore our diverse range of courses, training programs, virtual and live learning experiences, academy and interest group initiatives, and curated curricula. Our Educational Offerings By Career Level Guide simplifies your search, providing a user-friendly, easy-to-navigate overview of the learning opportunities available to you at every phase of your professional journey.
The CDEM M4 Curriculum was developed to encompass the most common conditions encountered by fourth-year students during their elective clinical rotations in the emergency department (ED). It aims to encapsulate the key medical scenarios typical in ED settings. The content is regularly reviewed and updated by subject matter experts every two to three years to ensure its relevance and accuracy.
Tailored to medical students participating in EM rotations, the curriculum aids in comprehending the fundamental core content essential to this field.

SAEM's Global Emergency Medicine Academy (GEMA) focuses on improving the global delivery of emergency care through research, education, and mentorship. GEMA provides resources
for students, residents, fellows, and others interested in global health careers, including:
• Trainee Info
• Short Courses
• Resource Library
• Research
• Books
• Travel Tips
• And More!
Academic Career Guide: Direction for Navigating Your Professional Pathway
The SAEM Academic Career Guide is a comprehensive manual for students, residents, fellows, and early career physicians who are interested in pursuing a career in academic emergency medicine. It offers essential tips and strategies for securing future EM positions such as department chair, residency program director, clerkship director, or dean.
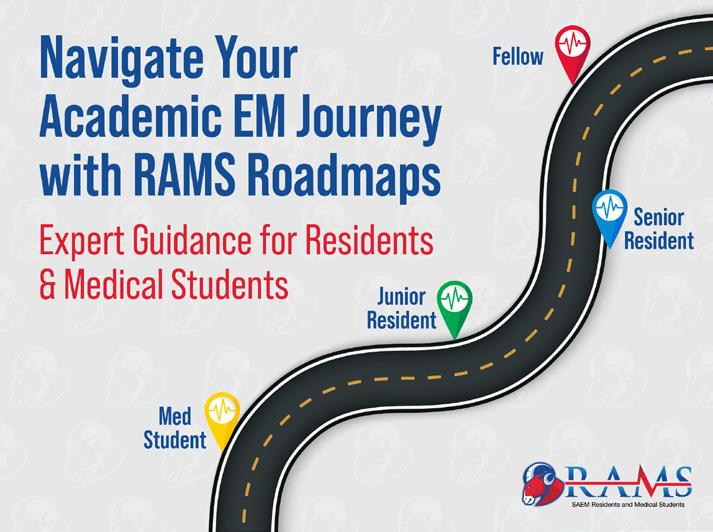
RAMS Roadmaps: Supporting Young EM Physicians on Their Career Journeys
RAMS Roadmaps guides young physicians through each career stage: senior medical student, junior resident, senior resident, and fellow. With 16 detailed Roadmaps covering topics such as administration, ultrasound, health policy, and more, RAMS Roadmaps equips aspiring EM physicians with the structure, instruction, and resources they need to take confident steps on their path to a gratifying and successful career in academic emergency medicine.

Surriya
Ahmad, MD
NewYork-Presbyterian/Weill Cornell
Geriatric Emergency Medicine Fellowship
Completed in 2022
What advice would you give to someone who is on the fence about doing a fellowship? What do you see as the cost-benefit?
It is a wonderful opportunity to focus on and develop a career niche within the field of Emergency Medicine and create the opportunity for career longevity, including the opportunity to further explore routes of administration, education, and research, while also practicing as a clinical Emergency Medicine attending.
What was the most career-enhancing, or eye-opening thing, you gained from the fellowship?
The opportunity to meet and work with leaders in the field of Geriatric Emergency Medicine, and to explore all the career paths available to me. I completed a residency in Emergency Medicine and Internal Medicine, and during the year I realized that although paths are available, we must also at times carve our own unique paths and make our career decisions our own, and if we follow our passions, and what we are most interested in, we can’t go wrong. Individuals, especially early in training are continually evolving.
Learn More!
Nurturing Diversity, Equity, and Inclusion in EM: The SAEM DEI Resource Library
Are you in need of an article on a justice, diversity, equity, or inclusion (JEDI)-related topic but don’t know where to start? Have you been tasked with planning a Journal Club and seeking a topic? Are you interested in sharing outstanding resources related to JEDI topics with the broader emergency medicine (EM) community? You’re in luck with the SAEM Diversity, Equity, and Inclusion (DEI) Resource Library!
SAEM’s DEI Resource Library is a free, online resource available to all SAEM members. Designed as an online repository for DEIrelated articles and other resources, the library currently contains many resources for wide use. The library was developed with the goal of supporting emergency physicians interested in learning more about eliminating health disparities and achieving health equity. Resources are divided into eight topic areas, including the history of discrimination in America; pipeline programs for learners across the educational continuum; evidence of inequities in patient care; evidence of exclusion in academic medicine; recruiting diverse faculty; advocacy for public health; diversity, equity, and inclusion curricula (including SAEM’s DEI Curriculum); and provider wellbeing/ caring for ourselves in the face of inequities.
Members can browse by topic with easy access to a wide range of resources, including articles, recommended books, editorials, videos, podcasts, diverse educational images, suggested websites, and more.
Members are encouraged to contribute to the DEI resource library when they discover a resource with potential utility for our community. Material submissions are brief and should include contact information, a link to or copy of the material, and the suggested category for optimal placement. Submissions, along with the tables of contents for relevant journals, undergo monthly review by the Resources and Products Subcommittee of the Equity and Inclusion Committee. We welcome not only your submissions but also your participation in our subcommittee, feedback on this resource, and suggestions regarding on how we can enhance its usefulness. Inquiries and feedback can be directed to tania.strout@ mainehealth.org
We envision this resource as a living repository that is useful in educational sessions, including journal clubs, brief DEI-focused educational interventions, or longer didactic sessions. Some materials, such as links to medical image libraries that focus on diverse skin tones, can assist in creating your own educational slides or other supporting material. Podcasts and other resources may offer valuable perspectives as you nurture your own DEI knowledge and inspire others in your sphere of influence to do the same. This also provides and opportunity to amplify your scholarly writing in this area, so please consider submitting your own publications to broaden their reach and utility. The SAEM DEI Library serves as a resource for all our members, be sure to check it out when planning your next academic event!
Submitted by Tania D. Strout, PhD, RN, MS, on behalf of the SAEM Equity & Inclusion Committee and Cassandra Bradby, MD, on behalf of the SAEM Academy for Diversity and Inclusion in Emergency Medicine.
AEUS Innovation Grant Provides Funding for Sonography
Throughout my residency, I have been enamored with ultrasound and its diagnostic utility in clinical practice. However, discussions with recently graduated colleagues have left me disheartened to learn that point-of-care ultrasound (POCUS) may be limited in its use. One contributing factor to this limitation is the often unstructured and expensive post-residency education that is accessible to providers. Additionally, there is a clear desire for increased POCUS education availability in various specialties.
As an education chief at Harbor-UCLA, I have experienced the amount of time needed to develop a curriculum and expand knowledge. Currently, individuals interested in learning ultrasound must act as their own curriculum coordinators and invest more time finding resources than benefiting from them. Considering this, I began to think of ways to reduce this opportunity cost and began conceptualizing what would eventually become the Sonography Education App.
What if we could develop an application that allowed both novice and experienced sonographers an opportunity to maintain and develop their skills? Modeled after Duolingo, this application would enable users to customize their education and follow pathways to enhance skills in their desired ultrasound areas. Employing spaced repetition, quality improvement elements, and designer graphics, it would not only demonstrate how to acquire and interpret images and assess quality, but also make the learning experience enjoyable.
In 2022 I had the opportunity to share this proposal with the Academy of Emergency Ultrasound and was honored to be selected to receive the AEUS Innovation Grant. This grant provided the initial funding necessary to launch the project and host our lessons on a learning management system.
While progress has been made in creating lesson content for the application, there have been some delays in coding. Our project has evolved into SonoNavigator, and we are finalizing introductory ultrasound lessons covering the basics of ultrasound, artifacts, echocardiography, biliary, musculoskeletal, and vascular ultrasound. By the end of this introductory session, we hope that users will be prepared to use POCUS to address various clinical questions.
In the coming months, we will collaborate closely with no-code application development to release and beta-test a live version of SonoNavigator. As we go live, we aim to gauge interest and success, and guide future development by collecting statistics from users, including their reported improvements in ultrasound. We are already planning our next steps, and with our modular development approach, we anticipate not only releasing intermediate and advanced curriculums in the future but also providing just-in-time education on additional procedural scans such as the RUSH exam, FAST exam, and various others that build upon the knowledge acquired in previous lessons.
I am exicited and inspired by the team of fellow residents and faculty who have joined me on this project to expand and grow education within the ultrasound community. With success, our goal is to continue expanding and providing education not only to other specialties but also to communities across the globe that may benefit from ultrasound education.
Submitted by Jonathan Warren, MD, Harbor-UCLA Department of Emergency Medicine. @jonthewookie; Jonwarren.w@gmail.com
Hopkins
The Department of Emergency Medicine at Johns Hopkins University, under the leadership of Dr. Bhakti Hansoti, associate professor of emergency medicine, has been designated a Pan American Health Organization/World Health Organization (PAHO/WHO) Collaborating Centre for Emergency, Critical and Operative Care. This is the first emergency medicine-led PAHO/WHO collaborating center and it will be supporting the work on the latest WHO resolution that was recently approved at the World Health Assembly.
Yiadom

Maame Yaa “Maya” A.B. Yiadom, MD, MPH, MSCI, associate professor of emergency medicine at Stanford University has received a $3.5 million NIH R01 National Heart Lung and Blood Institute Grant for her team’s study “Using Predictive Modeling for Acute Coronary Syndrome Screening to Improve Timely Diagnosis and Mortality for STEMI.” The grant will support the development of artificial intelligence (AI) for enhancing early diagnosis of ST-segment elevation myocardial infarction (STEMI) upon patients’ arrival in the emergency department (ED). The envisioned AI system will integrate into the electronic medical record to screen patient data during registration. Its purpose is to assist staff in minimizing instances of overlooked STEMIs. Congratulations to Dr. Yiadom and her team.
Dr. Alex Manini Is Named Director of New Mount Sinai Center for Research on Emerging Substances, Poisoning, Overdose, and New Discoveries

Alex Manini, MD, MS, a professor of emergency medicine at the Icahn School of Medicine at Mount Sinai, has been appointed the director of the new Mount Sinai Center for Research on Emerging Substances, Poisoning, Overdose, and New Discoveries (RESPOND). Founded in 2023 by Dr. Manini, MD, RESPOND was designed to bridge gaps between basic and translational science, clinical research, and clinical care in substance use disorder research. RESPOND embraces interdisciplinary approaches to advance knowledge and understanding of overdose, poisonings, and substance use disorders.

Creagh Boulger, MD, professor of emergency medicine in the Department of Emergency Medicine at Ohio State Wexner Medical Center, is the department’s new vice chair of education. Dr. Boulger is also the ultrasound fellowship director and associate ultrasound director at Ohio State University. She is a nationally recognized medical educator who utilizes gamification and gaming techniques in events such as SAEM SonoGames and SonoSlam.

Betty Chang, MD, MHA, assistant professor of emergency medicine at the Columbia University Medical Center (CUMC), has been announced senior director of social emergency medicine and health equity for the CUMC Department of Emergency Medicine. Dr. Chang is a past secretarytreasurer of the American College of Emergency Physicians (ACEP) Social Emergency Medicine Section, chair of the Departmental Social EM Committee, an inductee of the Columbia University Irving Medical Center (CUIMC) Academy of Community and Public Service, and the recipient of numerous awards including the 2022 CUIMC Physician of the Year Award and New York ACEP Unsung Hero Award.
Dr. Marc Probst Promoted to Associate Professor of Emergency

Marc Probst, MD, MS, has been promoted to associate professor of emergency medicine (tenure track) at Columbia University Vagelos College of Physicians & Surgeons. Dr. Probst presently serves as the director of general emergency medicine research. He is the recipient of a National Heart, Lung, and Blood Institute (NHLBI) independent K23 career development grant, and an R01 grant for his syncope research. His numerous awards include the SAEM Research Achievement Award for Oral Abstracts and the New York American College of Emergency Physicians (NY ACEP) Outstanding Researcher Award for Established Faculty. In addition, Dr. Probst is a frequent Top 50 peer reviewer for Annals of Emergency Medicine.
continued from Page 107
Danielle Campagne Appointed Chief of EM at UCSF Fresno and Vice Chair of EM at UCSF School of Medicine

Danielle Campagne, MD, professor in clinical emergency medicine, has been named chief of emergency medicine at UCSF Fresno and vice chair of emergency medicine at the UCSF School of Medicine. Dr. Campagne served as interim chief since August 2022. Prior to becoming interim chief, she served as vice chief since 2017. She joined UCSF Fresno as a health sciences clinical instructor in emergency medicine in 2008. She became an assistant health sciences clinical professor in 2010 and an associate professor in 2016. In addition, Dr. Campagne was the program director of the UCSF Fresno Department of Emergency Medicine Wilderness Medicine Fellowship from 2013-2015 and has served as medical director for both American Ambulance and the Department of Emergency Medicine’s Physician Assistant Residency Program since 2019 and 2018, respectively.

Neha Raukar, MD, MS, is the recipient of the 2023 Distinguished Emergency Medicine Clinician Award from the Mayo Clinic Department of Emergency Medicine. The award recognizes the emergency medicine consultant who makes outstanding contributions in patient care and embodies Mayo’s primary value that the needs of the patient come first.
Dr. Raukar is an associate professor and vice chair for academic advancement and faculty development in the department of emergency medicine at Mayo Clinic, Rochester. Previously she was director for the Division of Sports Medicine in the department of emergency medicine at Brown University. Dr. Raukar is an educator and a grant funded researcher in sports and emergency medicine and has served on national committees creating policies to ensure the health and safety of athletes from the youth to Olympic level. Dr. Raukar was co-director for SAEM’s 2022 Consensus Conference, “Diversity, Equity, and Inclusion: Developing a Research Agenda for Addressing Racism in Emergency Medicine.”
Dr. Devjani Das Accepted into the Columbia Vagelos College of Physicians and Surgeons
Virginia Apgar Academy of Medical Educators

Devjani Das, MD, was selected as a member of the Virginia Apgar Academy of Medical Educators, an elite group of advanced educators at Columbia University Vagelos College of Physicians and Surgeons (VP&S). Dr. Das is an associate professor of emergency medicine and serves as the director of the emergency ultrasound division and director of the emergency medicine clerkship at Columbia University VP&S. She is a past president of SAEM Academy of Women in Academic Emergency Medicine (AWAEM) and incoming chair of the New York American College of Emergency Physicians (NY ACEP) Education Committee.
Virginia Apgar Academy of Medical Educators

Christopher Tedeschi, MD, was selected as a member of the 2023 Virginia Apgar Academy of Medical Educators, an elite group of advanced educators at Columbia University Vagelos College of Physicians and Surgeons (VP&S). Dr. Tedeschi is an associate professor of emergency medicine and serves as the director of emergency preparedness for the Columbia University Department of Emergency Medicine.

Laura Walker, MD, MBA, has been promoted to the position of associate professor in the department of emergency medicine at Mayo Clinic. Dr. Walker has held multiple leadership positions at Mayo focusing on systems improvement and is currently leading digital transformation for the department of emergency medicine. She works toward elevating women EM leaders in all aspects of health care through her work as a member of the executive committee for the SAEM Academy for Women in Academic Emergency Medicine.

Benjamin J. Sandefur, MD, MHPE, a medical educator concentrating on emergency airway management and electrocardiography, has been promoted to associate professor in the department of emergency medicine at Mayo Clinic. Recognized for his clinical and educational contributions, Dr. Sandefur has received numerous awards, including the SAEM Clerkship Directors in Emergency Medicine Young Educator of the Year Award, the Mayo Fellows’ Association Emergency Medicine Teacher of the Year Award, and the Distinguished Emergency Medicine Clinician Award at Mayo Clinic. Dr. Sandefur is an oral board examiner for the American Board of Emergency Medicine and contributes significantly to the emergency airway management literature.

Casey Clements, MD, PhD, has been promoted to associate professor in the department of emergency medicine at Mayo Clinic, Rochester. Dr. Clements serves the Mayo Clinic Staff Safety Officer, leading environmental health and safety for the Mayo Clinic Enterprise and an operational occupational safety team based in Rochester, Minn. In this capacity he is responsible for an integrated safety management system and its many programs working throughout Mayo Clinic on staff injury prevention, mitigation, and response. He also chairs the Complex Behavior Committee for both the Rochester practice and the Mayo Enterprise which spearheads efforts of violence prevention, mitigation, and response.

Tom P. Aufderheide, MD, MS, professor of emergency medicine and director of the NIH-funded Resuscitation Research Center in the department of emergency medicine at the Medical College of Wisconsin, received the Council on Cardiopulmonary, Critical Care, Perioperative, and Resuscitation (3CPR) Distinguished Achievement Award at American Heart Association Scientific Sessions in Philadelphia. The Distinguished Achievement Award is the highest award granted by the Council and recognizes individuals who have made major professional contributions over a continuing period, and who have made substantial professional contributions to the field represented by the council, including contributions to new knowledge, teaching and/or clinical care, and professional leadership in national or international organizations.

Rebekah Cole, PhD, MEd, director of research in the department of military and emergency medicine at the Uniformed Services University, received a twoyear, $841,343 award from the Military Operational Medicine Research Program (Defense Health Program) for her medical education research project, “Modalities of Mindfulness-Based Mental Strength and Resilience Training: Comparison of Conventional vs. Virtual Reality.” Dr. Cole is a current participant in the ARMED MedEd program. “I really appreciate how ARMED MedEd equipped me with the tools I needed to apply for this award. My career is in a completely different place than it was last year at this time.”

Katherine Heilpern, MD, has been announced by Yale New Haven Health as the new president of Yale New Haven Hospital, the Health System’s flagship hospital, effective March 11.
Dr. Heilpern is joining the health system from New York-Presbyterian (NYP), where she led the Weill Cornell Division during the apex of COVID-19 infections in New York City. Just prior to the pandemic, Dr. Heilpern led the teams that developed the strategy, operations and staffing of the NYP David H. Koch Ambulatory Care Center. She then led the teams in the strategy, construction and operations of the Alexandra Cohen Hospital for Women and Newborns that opened in 2020.
Dr. Heilpern was recruited to NYP from Emory University School of Medicine and Emory Healthcare, where she practiced emergency medicine and served on the faculty for 22 years, including 12 years as chair of the Department of Emergency Medicine.
Dr. Heilpern is a former president for the Society for Academic Emergency Medicine (SAEM). She has a long history of national service to the medical profession, serving on boards and in leadership roles with SAEM, AACEM, ACEP, and the National Academy of Medicine.
Dr. Heilpern is the recipient of numerous awards and honors, including the SAEM John Marx Leadership Award, AWAEM Outstanding Department of Emergency Medicine award, Crain’s New York Notable Women in Healthcare, and the Emory School of Medicine Alumni Association Distinguished Medical Achievement Award.
Accepting ads for our “Now Hiring” section!
Deadline for the next issue of SAEM Pulse is April 1.
For specs and pricing, visit the SAEM Pulse advertising webpage.


Employers, are your recruiting efforts effective?
Specific targeted career websites, like EM Job Link, deliver the most highly qualified talent and have the best return on investment. Our candidates are made up of the specific professionals you want to reach. If you want the best and brightest candidates, you need to go where they job search – EM Job Link. Along with posting your jobs in front of qualified candidates at EM Job Link, you can search our resume bank for talent as well. Post today or speak to an expert who can help create a customized recruiting solution to get you great candidates.












Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pa.




The University of California San Francisco, Department of Emergency Medicine is recruiting for a full-time faculty member to serve as the Medical Director of our new Urgent Care based on the Mission Bay campus, opening in Fall of 2024. We seek individuals who meet the following criteria: emergency medicine faculty with administrative leadership experience and/or advanced administrative training (e.g., administrative fellowship training, MBA, MPP) and outstanding clinical and interpersonal skills. Rank, step and series will be commensurate with qualifications. Board certification in Emergency Medicine is required. All applicants should excel in bedside teaching and have a strong ethic of service to their patients and profession.
The Department of Emergency Medicine provides comprehensive emergency services to a large local and referral population at multiple academic hospitals across the San Francisco Bay Area, including UCSF Medical Center at Parnassus Heights, Zuckerberg San Francisco General Hospital, and the UCSF Benioff Children’s Hospitals in San Francisco and Oakland. The Department of Emergency Medicine hosts a fully accredited 4-year Emergency Medicine residency program and multiple fellowship programs. This opportunity will involve clinical work at both the UCSF Parnassus ED campus and the new Urgent Care at the Mission Bay campus, and the Urgent Care Medical Director will work closely with the emergency medicine leadership team at Parnassus.
The University of California, San Francisco (UCSF) is one of the nation’s top five medical schools and demonstrates excellence in basic science and clinical research, global health sciences, policy, advocacy, and medical education scholarship. The San Francisco Bay Area is well-known for its great food, mild climate, beautiful scenery, vibrant cultural environment, and its outdoor recreational activities.
PLEASE APPLY ONLINE AT: https://aprecruit.ucsf.edu/apply/JPF04867
UCSF seeks candidates whose experience, teaching, research, and community service has prepared them to contribute to our commitment to diversity and excellence. UCSF is an Equal Opportunity/Affirmative Action Employer. The University undertakes affirmative action to assure equal employment opportunity for underrepresented minorities and women, for persons with disabilities, and for covered veterans. All qualified applicants are encouraged to apply, including minorities and women. For additional information, please visit our website at http://emergency.ucsf.edu/
Check companies advertising jobs on SAEM’s EM Job Link against your LinkedIn contacts. Leverage professional connections for more information about the company or request a referral.

■ Physician-led group on the local, regional and national levels
■ Professional development, mentoring and leadership opportunities
■ Robust support for clinician wellness
■ Flexible, equitable scheduling that supports work-life balance
■ Full-time, part-time, per diem and ENVOY Ambassador Team options
RESIDENCY PROGRAM DIRECTOR
Centerpoint Medical Center
Kansas City, MO
RESIDENCY PROGRAM DIRECTOR
HCA Florida Lawnwood Hospital Fort Pierce, FL
EMS PHYSICIAN
Trinity Health Ann Arbor Hospital Ann Arbor, MI
CORE FACULTY OPPORTUNITIES
HCA Florida Lawnwood Hospital Fort Pierce, FL
PEDIATRIC EM PHYSICIAN
Medical City Dallas Dallas, TX
RESEARCH DIRECTOR
Morristown Medical Center Morristown, NJ
EMS PHYSICIAN
TriStar Skyline Medical Center Nashville, TN
ULTRASOUND PHYSICIAN
TriStar Skyline Medical Center Nashville, TN

