
Breaking Barriers, Building Pathways
A Conversation With 2025–2026 RAMS President
Daniel Artiga, MD


A Conversation With 2025–2026 RAMS President
Daniel Artiga, MD

Michelle D. Lall, MD, MHS
SAEM President
Emory University School of Medicine
Board Liaison to:
• Bylaws Committee
• Governance Committee
• Ethics Committee

Jody A. Vogel, MD, MSc, MSW
SAEM President-Elect
Stanford University
Board Liaison to:
• RAMS Board
• Committee of Academy Leaders
• SAEM Federal Funding Committee
• Nominating Committee
• Sex and Gender in Emergency Medicine Interest Group

Pooja Agrawal, MD, MPH
Member at Large Yale Department of Emergency Medicine
Board Liaison to:
• Clerkship Directors in Emergency Medicine
• ED Administration and Clinical Operations Committee
• Grants Committee
• Behavioral and Psychological Interest Group
• Pediatric Emergency Medicine Interest Group

Bryn Mumma, MD, MAS
Member at Large
University of California, Davis
Board Liaison to:
• Academy for Women in Academic Emergency Medicine
• Research Committee
• Disaster Medicine Interest Group
• Palliative Medicine Interest Group
• Research Directors Interest Group
• Trauma Interest Group

Cassandra Bradby, MD Member at Large East Carolina University
Board Liaison to:
• Academy of Emergency Ultrasound
• Awards Committee
• Critical Care Interest Group
• Oncologic Emergencies Interest Group
• Toxicology/Addiction Medicine Interest Group

Jane H. Brice, MD, MPH Chair Member University of North Carolina at Chapel Hill School of Medicine
Board Liaison to:
• Faculty Development Committee
• Vice Chairs Interest Group

Ava E. Pierce, MD
SAEM Secretary-Treasurer
UT Southwestern Medical Center
Board Liaison to:
• Global Emergency Medicine Academy
• Finance Committee
• Program Committee
• Clinical Researchers United Exchange Interest Group
• Wilderness Medicine Interest Group

Jeffrey P. Druck, MD
Member at Large
The University of Utah
Board Liaison to:
• Academy for Diversity & Inclusion in Emergency Medicine
• Fellowship Approval Committee
• Climate Change and Health Interest Group
• Evidence-Based Healthcare & Implementation Interest Group
• Tactical and Law Enforcement Interest Group

Patricia Hernandez, MD Resident Member
Massachusetts General Hospital
Board Liaison to:
• Wellness Committee
• Innovation Interest Group
• Neurologic Emergency Medicine Interest Group,
• Telehealth Interest Group
Ryan LaFollette, MD Member at Large University of Cincinnati
Board Liaison to:
• Simulation Academy
• Education Committee
• Airway Interest Group
• Operations Interest Group
• Transmissible Infectious Diseases Interest Group

Ali S. Raja, MD, DBA, MPH
SAEM Immediate Past President
Massachusetts General Hospital/ Harvard Medical School
Board Liaison to:
• Academy of Administrators in Academic Emergency Medicine
• Workforce Committee
• Educational Research Interest Group
• Informatics, Data Science, and Artificial Intelligence Interest Group
• Quality and Patient Safety Interest Group

Nicholas M. Mohr, MD, MS Member at Large University of Iowa Carver College of Medicine
Board Liaison to:
• Academy of Emergency Medicine Pharmacists
• Academy of Geriatric Emergency Medicine
• SAEM Federal Funding Committee
• Membership Committee
• Emergency Medical Services Interest Group

Megan Schagrin, MBA, CAE, CFRE
SAEM Chief Executive Officer
Liaison to:
• SAEM Executive Committee
• Association of Academic Chairs of Emergency Medicine (AACEM)
• RAMS Board
• SAEM Foundation

Physicians Can Help End Gun Violence Against Children
Motivation: Applying Self-Determination Theory to Enhance Well-Being in Emergency Medicine
Process, Proceed: Emotional Reflection Inside and Outside the Hospital
Repellents in Wilderness Medicine: Essential Tools for Outdoor Health Management — Part 2
and Sustaining Donors of


Michelle D. Lall, MD, MHS Emory University 2025-2026 President, SAEM
It was truly a pleasure to see so many of you at SAEM25. This year’s gathering in Philadelphia was nothing short of extraordinary—a record-breaking event that reflected the incredible momentum of our community. We welcomed the largest number of attendees in SAEM’s history, and members submitted an unprecedented number of didactic sessions and scientific abstracts. The energy, engagement, and scholarly excellence on display were inspiring. Heartfelt thanks to our dedicated members and the exceptional SAEM staff for making SAEM25 our most successful annual meeting to date.
Moments like these remind us that our greatest achievements are built together. As we carry this energy forward, I plan to use this year to reflect on the strength of our SAEM community. I will be highlighting key initiatives and accomplishments to keep all members informed of our organization’s trajectory—both for the year ahead and for the future. Together, we will continue to grow stronger, more connected, and more impactful.
At SAEM, we believe that progress is driven by community—by collaboration, connection, and shared purpose. Our mission to advance academic emergency medicine through education, research, and professional development is made possible by the passion and dedication of our diverse membership. I am continually inspired by your contributions.
My own SAEM journey began as a junior faculty member when I was invited to attend a meeting of the Academy for Women in Academic Emergency Medicine (AWAEM). I found more than a professional group—I found a home. AWAEM became a space for mentorship, growth, and empowerment. It reminded me that when we feel seen and supported, we are more likely to step forward, take risks, and lead with purpose.
I am proud to share several initiatives that reflect our continued commitment to fostering a meaningful community:
• Federal Funding Committee: This new committee will strengthen SAEM’s engagement with federal
“This year’s gathering in Philadelphia was nothing short of extraordinary—a record-breaking event that reflected the incredible momentum of our community.”

“SAEM has surpassed 10,000 members—a historic milestone that speaks to the strength, inclusivity, and vibrancy of our community.”
agencies, expand funding opportunities, and keep members informed on research priorities. Many thanks to Dr. Manish Shah for serving as its inaugural chair.
• Editor-in-Chief Search for Academic Emergency Medicine: Applications open Sept. 1 for our next editor-in-chief. We are deeply grateful to Dr. Jeff Kline for nearly a decade of outstanding leadership and look forward to building on his legacy.
• Launch of the Academy for Emergency Medicine Pharmacists (AEMP): AEMP is now SAEM’s ninth academy—an important step forward in fostering interdisciplinary collaboration. Congratulations to the founding team for this achievement.
Finally, SAEM has surpassed 10,000 members—a historic milestone that speaks to the strength, inclusivity, and vibrancy of our community. If you have not yet discovered your SAEM story, know there is a place here for you. Volunteer, connect, and be part of something bigger. Together, we are shaping the future of academic emergency medicine—and we are just getting started.
ABOUT DR. LALL: Michelle D. Lall, MD, MHS, FACEP, is professor and vice chair of diversity, equity, and inclusion in the Department of Emergency Medicine at Emory University School of Medicine.
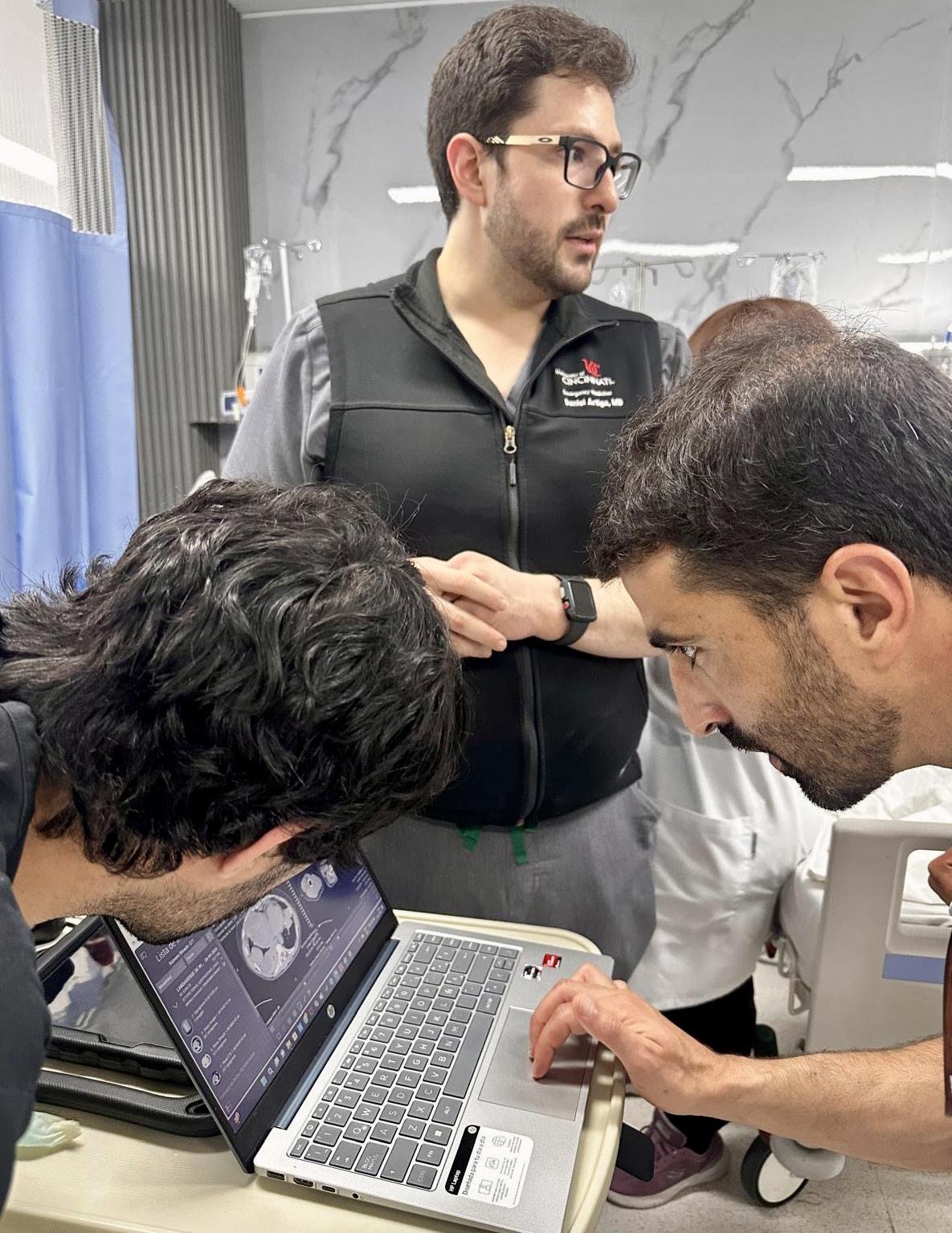
Daniel Jose Artiga, MD is a fourth-year emergency medicine resident at the University of Cincinnati and the 2025-2026 president of SAEM RAMS (Residents and Medical Students). As a first-generation Latino—and the first in his family born in the U.S., to earn a college degree, and to become a physician—he is committed to expanding access to emergency care and advancing equity, and inclusion in medicine.
Dr. Artiga earned his medical degree as a David Geffen Medical Scholar at the University of California, Los Angeles, and holds a bachelor’s degree in Molecular and Cellular Biology from Harvard University. His passion for emergency medicine was sparked by early life experiences receiving care in the emergency department, inspiring his dedication to serving resource-limited communities.
Dr. Artiga’s academic interests include ultrasound, education, and advocacy. Within SAEM RAMS, he has led initiatives such as the Ask-A-Chair educational podcast series, advocacy efforts related to unionization, social media campaigns to promote resident engagement, and the development of board review resources for emergency medicine certification. He has recently taught ultrasound to emergency medicine programs in Latin America.
Dr. Artiga plans to pursue a fellowship in ultrasound and continues to champion equitable access to care and opportunities for those underrepresented in medicine.


Your journey from receiving much of your childhood healthcare in the emergency department to leading SAEM RAMS is remarkable. How have those early experiences shaped your vision for the role emergency medicine should play—particularly in resource-limited communities— and how will that vision guide your priorities as RAMS president?
Emergency medicine (EM) was a natural fit for me because it is the only specialty that inherently serves everyone anywhere. Growing up, I experienced firsthand how the emergency department (ED) serves as a healthcare access point for those in resource-limited communities. EM directly addressed the challenges I saw around me. As RAMS president, my priorities are shaped by that foundation, even if indirectly.
While much of my current focus is on evolving issues, such as changes to the Accreditation Council for Graduate Medical Education (ACGME) requirements, American Board of Emergency Medicine (ABEM) certification, and the ResidencyCAS rollout, my broader vision ties back to equity and building pathways for underrepresented groups in medicine. Mentorship is a key part of that vision, which is how I plan to create lasting change. We're trying to expand mentorship opportunities for students and residents who may not otherwise see a path into this field. For example, we're developing initiatives and pipeline programming with SAEM’s medical student ambassadors and the Medical Student Symposium—which reflect the same kind of outreach programs that exposed me to medicine in the first place.

As a first-generation, U.S.-born Latino and a strong advocate for diversity, equity, and inclusion (DEI), what steps do you believe RAMS and the broader academic EM community should take to empower those underrepresented in medicine? What role can RAMS play in advancing that mission?
It starts with mentorship that leads to meaningful recruitment, inclusion, and ultimately representation. We need to build pathways that don't just invite underrepresented students into the field but support them through it. We also need to be intentional about our research and advocacy. We should be studying disparities in care and ensuring we’re not applying one-size-fits-all solutions to our patients. There's a dual responsibility: caring for patients from underserved communities while also lifting up members of those communities to become providers themselves.
That’s where RAMS can play a unique role: through pipeline programs, educational initiatives, and pushing forward strategies even as the national conversation around DEI evolves. The RAMS Board plans to increase awareness of resources and opportunities available to medical students and residents through SAEM groups such as the Academy for Diversity and Inclusion in Emergency Medicine (ADIEM), the Academy for Women in Academic Emergency Medicine (AWAEM), and the Social EM and Population Health interest group.

continued from Page 7
You’ve already made a significant impact through your involvement with RAMS initiatives—from the Ask-AChair podcast series to advocacy for unionization and global ultrasound education. Looking ahead, what new or continuing projects are you most excited to champion during your presidency?
Emergency medicine is undergoing major transitions across the board. One of the projects I’m most excited about is continuing to support the rollout and development of the ResidencyCAS platform. This platform doesn’t just streamline the application experience; it provides real-time data that programs can use to understand how applicants are engaging with EM, which in turn helps guide recruitment strategies.
At the same time, we’re seeing changes to ACGME program requirements and the ABEM Certifying Exam. These shifts raise important questions about how we define competency and what makes a capable emergency physician. During my presidency, I want to ensure RAMS has a voice in those conversations, particularly when it comes to protecting the things that
make EM unique: our broad skill set, adaptability, and patient-centered approach.
This is a critical period for the specialty, and being involved at this moment means helping shape the foundation for future trainees. That’s a responsibility I take seriously.
Balancing clinical duties, academic interests, and leadership responsibilities is no small feat for a resident. What motivates you to stay engaged at this level, and what advice would you give to other trainees looking to make meaningful contributions to academic emergency medicine?
I first became involved in RAMS because I was concerned about the direction of emergency medicine, particularly with the growing presence of for-profit models that stretch physicians to care more patients than they can realistically manage. It felt like the heart of what makes being a doctor special—giving thoughtful and attentive care to our patients’ needs—was being threatened by business decisions.
My motivation comes from a desire to protect the core of this specialty. If you care deeply about EM, you have to be part of the solution. National leadership roles
“If you care deeply about EM, you have to be part of the solution. Once you see the impact you can have, it’s hard not to want to be part of it.”
like those with RAMS give you a chance to help shape the future of the field in a structured, impactful way.
For other trainees, I’d say: find your people. Surround yourself with others who are just as passionate and driven. The most powerful changes often come from the work of these motivated groups. I’ve found SAEM to be the perfect venue to find these people.
You’ve been involved in teaching ultrasound to emergency medicine programs in Latin America. What have you learned from that experience, and how has it influenced your approach to global health and education in EM?
It was an extremely humbling and eye-opening experience. I went to teach in my father’s country, El Salvador, where I had never visited before. I never truly understood the conditions he lived in beyond his words. All the issues that exist in the U.S. are magnified when you go to countries that don’t have similar resources. Medical decision making is limited by access to resources. It’s not about a lack of capability. I worked with incredibly brilliant doctors who just don’t have access to the same technology or infrastructure we have here. That’s why I believe in supporting ultrasound specifically in these settings. In capable hands, point-ofcare ultrasound can give a clinician life-saving information. Providing this tool and empowering physicians to use it can have a huge impact on individual patients and healthcare systems across the world.
You’ve spoken about the importance of advocating for our specialty. In today’s rapidly evolving healthcare environment, what do you see as the biggest challenges facing EM residents—and how can RAMS help address them?
The biggest challenge facing EM residents right now is the changing foundation of our training. Every step—from applying to residency, to how we’re evaluated during training, to how we’re certified after graduation—is in flux. This matters because better training leads to better patient care. If we’re serious about delivering the best possible care, we must take our training systems seriously too. RAMS and SAEM are already stepping up to meet this moment. RAMS is working with the Council of Residency Directors in Emergency Medicine (CORD) to develop social media materials and guides for ResidencyCAS for new applicants to our specialty. We are in contact with ABEM to elucidate the resource materials they have released so far and plan to publish what we learn to our members. We co-wrote and co-signed a letter to the ACGME with our comments regarding changes to our specialty
requirements. RAMS board members attended the SAM25 Consensus Conference aimed at developing a research agenda for competency-based training.
Our goal is to make sure the voices of residents and students are included in shaping these changes from the ground up.
What have been some of the most meaningful lessons you’ve learned through your leadership roles within SAEM RAMS, and how have they shaped your growth as a physician and a leader?
For me, it’s been about chasing my passion and asking, “Who’s on this ride with me?” I’ve always been drawn to ultrasound. Through SAEM’s and the Academy for Emergency Ultrasound’s (AEUS’s) ultrasound didactics and activities, I’ve noticed similar faces showing up. These spaces allow for ideas to connect and develop in ways that don’t happen when you're working alone. You can’t have synergy in isolation. You need people who challenge and inspire you to promote growth. It’s individuals working together, learning from one another, and pushing ideas forward that produce progress.
As someone who’s contributed to educational resources like board review materials and the Ask-A-Chair podcast, what do you see as the most effective ways to support fellow residents in their academic and career development?
The most effective way to support others is by not gatekeeping. It’s easy to forget how far you’ve come since applying to medical school. You have to give advice in a way that benefits someone at their level of training but also sharing what worked for you when you were in their shoes. Share resources and opportunities. Coaching and being an excellent mentor to near-peers is the key. Organizing these efforts through an organization like RAMS and SAEM, however, is able to amplify that impact— creating structured, accessible pathways for mentorship, collaboration, and professional growth on a national scale. What’s one misconception people often have about emergency medicine trainees, and how would you like to see that narrative change?
A common misconception across the board is that EM trainees “just order tests and imaging.” That couldn’t be further from the truth. The sharpest senior emergency
physicians I’ve worked with order plenty of advanced tests or imaging, but not out of habit. It’s because they’ve thought deeply about the case. They’ve considered the patient’s risk factors, demographics, history, and physical. They have combined that information with clinical decision tools and years of clinical gestalt to guide their medical plan.
Diagnostics aren’t the end-all-be-all. Trainees are educated on the specificities and negative predictive values of the diagnostic tests we use to evaluate life-threatening disease. We pair those test characteristics with clinical judgment to develop a good plan for the patient. The best EM physicians are the ones who know how to use these tests and imaging modalities effectively, without relying on them but also using them when necessary.
If you could accomplish just one thing during your term as RAMS president that would have a lasting impact, what would it be—and why?
One lasting accomplishment I desire is improving communication between the RAMS Board and our resident and medical student community members. There’s so much incredible work happening behind the scenes. I do perceive a gap where members don’t know how much we are up to and how they can get involved themselves. I want more people to know opportunities exist and that they’re
accessible. My hope is that clearer communication not only showcases what RAMS is doing but inspires more residents and students to step up and get involved. Once you see the impact you can have, it’s hard not to want to be part of it.
Why should EM residents and medical students become involved with RAMS? What needs does the group meet or concerns does it address?
RAMS is the gateway for EM residents and medical students to shape the future of emergency medicine while also building their own careers. If you care about professional development, equity, or mentorship, RAMS is where those opportunities begin.
We meet a wide range of needs—from practical support with residency applications and post-residency job prep, to broader guidance through initiatives like the RAMS Career Roadmaps. We’ve built educational content across formats: webinars, podcasts, and toolkits on everything from contract negotiation to wellness. RAMS also leads on issues that matter deeply to trainees: improving ED learning environments, fostering DEI through partnerships with ADIEM and others, and pushing for resident wellbeing through campaigns like “Stop the Stigma.” And of course, we're also involved in national discussions with organizations such as ABEM, EMRA, CORD and ACGME.
Getting involved in RAMS means joining a community of peers who want to lead, teach, and transform the specialty.
If you weren’t in medicine, what career would you have pursued instead—and why? Some aspect of filmmaking. I really enjoy cinematography and being in control of the camera.
What’s one item you always have with you on shift—besides your pen and stethoscope?
Every shift, I wear a silver chain necklace my dad got me for my first communion with my wedding ring hanging from the necklace. They are reminders of my family and where I come from.
What’s the most unexpected skill you've picked up during residency?
The ability to sleep anywhere at any time. Residency is exhausting, but I also became a father at the start of residency. I now have a toddler and baby girl, and you have to sleep whenever they give you a chance.
What’s your guilty pleasure when you finally get a day off?
Giving undivided attention to my son and daughter. It’s easy to be preoccupied by the many issues affecting our country, our specialty, and our personal lives. I make a conscious effor t to ground myself with them and give them my focus and love whenever I have the chance.
If you could instantly master one non-medical skill or hobby, what would it be? Calisthenics. Have you ever seen someone do the “human flag?” It requires so much strength and body coordination.






The 2025 SAEM Annual Meeting, held May 13–16 in the heart of Philadelphia, was nothing short of legendary. With record-breaking attendance, the highest number of workshop, didactic, and abstract submissions in our history, and an electrifying atmosphere of collaboration and discovery, SAEM25 was a defining moment for academic emergency medicine
For four unforgettable days, our community came together to learn, lead, and celebrate everything that makes emergency medicine one of the most dynamic and essential specialties in healthcare. From sunrise sessions to evening strolls through Philly’s historic streets, SAEM25 was filled with powerful presentations, game-changing research, meaningful connections, and the unmistakable feeling of coming home.
SAEM25 raised the bar with a program packed full of hands-on workshops, thought-provoking didactics, and trailblazing research designed to elevate every attendee — from students to seasoned leaders. With something for everyone, the meeting featured:
• Deep-dive sessions in cutting-edge clinical and educational topics
• Innovative simulations and skill-building workshops
• Passion-fueled discussions led by top experts in the field
• Friendly, high-energy competitions to test knowledge and spark new ideas

Attendees left feeling energized, equipped, and inspired to take on the next chapter of their careers with renewed purpose.
At its core, SAEM25 was about connection. Whether catching up with old friends, forging new collaborations, or engaging in rich mentorship conversations, the meeting was a powerful reminder of the strength of our academic emergency medicine family.
SAEM25 provided welcoming spaces for networking, peer exchange, and reflection — proving once again that the relationships we build extend far beyond the walls of a conference center.

Dr. Peter Rosen Memorial Keynote: Charles Cairns, MD
Dr. Charles Cairns delivered a brilliant and visionary address, “Advancing Precision Emergency Medicine: Innovations in Translational Medicine and Population Health,” challenging us to reimagine emergency care through the lens of systems biology, big data, and the digital revolution. His insights into population health and translational research set a powerful tone for the week ahead.

With her keynote, “The Health Humanities: The Next Great Frontier in Emergency Medicine Education,” Dr. Kamna Balhara brought humanity to the forefront of emergency medicine. Her exploration of arts and humanities in
medical education was both moving and enlightening, underscoring how creativity and empathy can transform the way we learn, teach, and care.
The brightest minds in emergency medicine took center stage in our Plenary Sessions, presenting the top eight abstracts chosen from over 1,426 submissions. These sessions spotlighted bold ideas and groundbreaking research that will shape the future of our field:
• Treatment strategies for opioid use disorder
• Proteomic biomarkers in pulmonary embolism
• Resuscitation science and clinical decision-making
• Health systems innovation and education reform
These presentations, and others like them, were a testament to the rigor, creativity, and scientific excellence that defines our SAEM community.

At the opening ceremony, we proudly welcomed Michelle Lall, MD, MPH as the new SAEM President. A trailblazer in diversity, equity, and inclusion, Dr. Lall announced exciting new initiatives:
• Formation of the SAEM Federal Funding Committee to expand support for EM research
• Launch of the Academy of Emergency Medicine Pharmacists (AEMP) — our ninth academy!
• A national search for the next Editor-in-Chief of Academic Emergency Medicine
With Dr. Lall at the helm, the future of SAEM has never looked brighter.
continued on Page 14

• A heartfelt tribute honored the late Dr. Amy Kaji, SAEM Past President, with the 2025 Organizational Advancement Award. Her legacy will live on through the Amy H. Kaji, MD, PhD Early Investigator Awards, supporting the next generation of EM scholars.

• In a stunning gesture of support, AACEM gifted $500,000 to the SAEM Foundation, a bold investment in the future of academic emergency medicine. The gift reflects an unwavering commitment to education, research, and innovation at the highest level.
From morning education session to evening adventures, from the halls of the conference center to the cobblestone streets of Philadelphia — SAEM25 was a celebration of everything we are and everything we are becoming. It was a place to learn, to lead, to connect, and to belong.
We are grateful to each of you who joined us and contributed to this unforgettable experience. Your passion, knowledge, and energy made history. And together, we’ll keep writing the future of academic emergency medicine.
See you next year at SAEM26 in Atlanta, Georgia — where the story continues!
Claim Your SAEM25 CME
The deadline is July 31 to claim your SAEM25 continuing medical education (CME). Just follow the steps found on this webpage
Access SAEM25 Content on SOAR
Unable to attend SAEM25 in Philadelphia or missed out on some sessions at the annual meeting? Starting in August, you'll have access to all the presentations from the annual meeting anytime, anywhere through our SAEM Online Academic Resources (SOAR) webpage. Enjoy convenient online and mobile viewing of SAEM25's Advanced EM Workshops, didactics, forums, abstracts, and more!
Note: CME credits are not designated for SAEM25 content accessed through SOAR.
The SAEM Annual Meeting is the premier event for presenting original, high-quality research and educational innovations in emergency care. Mark your calendar and start preparing to submit your work as soon as submissions open!
Advanced EM Workshops
Aug. 1 – Sep. 17, 2025
Didactics
Aug. 15– Oct. 2, 2025
Year in Review for AEMP Program
Aug. 15 – Oct. 2, 2025
Keynote
Sep. 4 – Nov. 6, 2025
Abstracts
Nov. 3, 2025 – Jan. 5, 2026
Innovations
Nov. 3, 2025 – Jan. 12, 2026
IGNITE!
Nov. 3, 2025 – Jan. 12, 2026
Clinical Images
Nov. 3, 2025 – Jan. 12, 2026
SAEM awards are given each year at the SAEM Annual Meeting in recognition of exceptional contributions to emergency medicine and patient care through leadership, research, education, and compassion. Congratulations to all of our 2025 award recipients!

University of Pennsylvania Department of Emergency Medicine (PennEM)
PennEM’s proactive and research-driven approach to wellness has positioned the department as a national leader in promoting wellness, mitigating burnout, and fostering an inclusive, supportive culture.

Vik Bebarta, MD
University of Colorado
Presented to a member of SAEM who has made outstanding contributions to emergency medicine through the creation and sharing of new knowledge.

Alister Martin, MD, MPP
Massachusetts General Hospital
Honors an SAEM member who has made exceptional contributions to emergency medicine through advancing diversity and inclusion in emergency medicine.
Arnold P. Gold Foundation Humanism in Medicine Award
Theresa Hsiang-Ting Cheng, MD, JD
University of California, San Francisco Department of Emergency Medicine
- Zuckerberg San Francisco General Hospital
Given to a practicing emergency medicine physician who exemplifies compassionate, patient-centered care.

Ian B. K. Martin, MD, MBA
Medical College of Wisconsin
Honors an SAEM member who has made exceptional contributions to emergency medicine through leadership - locally, regionally, nationally or internationally, with priority given to those with demonstrated leadership within SAEM.

Luan Lawson, MD, MAEd
Virginia Commonwealth University School of Medicine
Awarded to a member of SAEM who has made outstanding contributions to emergency medicine through the teaching of others and the improvement of pedagogy.


Judy Linden, MD
Boston University Chobanian and Avedisian School of Medicine, Boston Medical Center
Recognizes an SAEM member who has made significant contributions to the advancement of women in academic emergency medicine.
Nicholas Jouriles, MD
Northeast Ohio Emergency Medicine; US Acute Care Solutions; Summa Health System
Honors an SAEM member who has mentored the career advancement of other SAEM members.

Megan L. Ranney, MD, MPH
Yale School of Public Health and Yale School of Medicine
Junaid A. Razzak, MBBS, PhD
Weill Cornell Medicine
Honors an SAEM member who has made exceptional contributions to addressing public health challenges through interdisciplinary leadership in innovation – locally, regionally, nationally, internationally.

Nour Al Jalbout, MD
Massachusetts General Hospital
Mary R. C. Haas, MD, MHPE University of Michigan
Christopher E. San Miguel, MD, MEd
The Ohio State University


Honors an SAEM member, within eight years of their first faculty appointment who has made outstanding contributions to emergency medicine through the teaching of others.

Todd Florin, MD, MSCE
Ann & Robert H. Lurie Children's Hospital of Chicago
Tony Rosen, MD, MPH
Weill Cornell Medicine / NewYorkPresbyterian Hospital
Recognizes those SAEM members who have demonstrated commitment and achievement in research during the mid-stage of their academic career.

Ryan A. Coute, DO University of Alabama at Birmingham
Ari B. Friedman, MD, PhD University of Pennsylvania
Felipe Teran, MD, MSCE
Weill Cornell Medicine



Alex Koyfman, MD
UT Southwestern Medical Center / Parkland Health and Hospital System
Manpreet Singh, MD, MBE
Harbor-UCLA Medical Center
Honors an SAEM member who has made outstanding contributions to the online learning community of emergency medicine through innovative and engaging FOAMed content.

Sarah Aly, DO Yale University
Established in honor of former SAEM President Dr. Amy Kaji, this award supports early-career EM scholars committed to research by funding their attendance at the SAEM Annual Meeting to foster professional growth and development.
Priya Arumuganathan, MD University of Pennsylvania
Richmond Malabanan Castillo, MD, MA, MS Children's National Hospital
Amir J. Mansour, MD Yale University
Wendy W. Sun, MD Yale University
Presented to EM fellows in any subspecialty for outstanding dedication to education and impactful research through significant contributions, presentations, and publications.

Konnor Davis
University of California, Irvine School of Medicine
Honors a medical student or practicing emergency medicine resident taking a leading role in their student interest group or residency program and making an impact on the local, regional, national, or international level through their efforts.
RAMS Excellence in Research Award

David Gordon
Sidney Kimmel Medical College, Thomas Jefferson University
Awarded to annually to a senior emergency medicine resident or student who has demonstrated exceptional promise and early accomplishment in the creation of new knowledge.
RAMS Resident Education/Innovation Award

Patricia Hernández, MD
Massachusetts General Hospital
Given to underrepresented medical students who demonstrate a strong commitment to and leadership skills in emergency medicine.
RAMS Excellence in Education Award

Michael DiGaetano, MD
Rutgers Robert Wood Johnson Medical School
Given annually to a senior emergency medicine resident who has demonstrated exceptional aptitude and passion for teaching during residency.
RAMS Medical Student Education Award


Rana M. Barghout
Weill Cornell Medicine
Given to a senior medical student who has demonstrated excellence in the specialty of emergency medicine.
SAEM Annual Meeting | May 18–21, 2026 Atlanta Marriott Marquis
Get ready for a next-level annual meeting experience in the heart of Atlanta, Georgia! Here’s what’s in store at the stunning Atlanta Marriott Marquis:
• Spacious, modern meeting rooms for seamless learning and networking
• Expansive common areas perfect for casual conversations and impromptu meetups
• Friendly, expert hotel staff who know how to support large-scale events
• On-site Starbucks—mobile orders ready in just 6 minutes
• Tons of nearby restaurants and eateries within walking distance
• Clean, welcoming city vibe with city ambassadors ready to guide you
Mark your calendars now. You won’t want to miss it!

SONOGAMES® CHAMPIONS
UConn Emergency Medicine

DODGEBALL CHAMPIONS
UT Southwestern

SIMULATION ACADEMY SIMWARS CHAMPIONS
Massachusetts General Hospital

• American Board of Emergency Medicine (ABEM)
• American College of Emergency Physicians (ACEP)
• ApolloMD
• ARS Pharmaceuticals Operations, Inc.
• AstraZeneca
• AstraZeneca
• B Braun Medical Inc
• Brault
• BRC
• Butterfly Network
• Ceribell
• Cleo Health
• CyrenCare, Inc.
Bingo! Tiles Sponsors
• American College of Emergency Physicians (ACEP)
• ApolloMD
• Brault
• B Braun Medical Inc
• The Guthrie Clinic
• Geisinger Health System
• Natus Medical
• Purdue Pharma LP
• SERB Pharmaceuticals
• TEAMhealth
• Vituity
Childcare Area
• Brown Emergency Medicine
• Medical College of Wisconsin
• The Ohio State University Wexner Medical Center
• University of Cincinnati Medical Center/College of Medicine
• University of North Carolina Hospitals Chapel Hill
• Stanford University Department of Emergency Medicine
• Rush University Medical Center
• Diasorin
• EchoNous
• Emergency Care Partners
• Emergency Medicine Foundation
• Emergency Medicine Specialists
• Emergent Medical Associates
• EMrecruits
• GE Healthcare
• Geisinger Health System
• The Guthrie Clinic
• HCA Healthcare
• Liaison - ResidencyCAS
• Locum Physicians United
• Mayo Clinic & Mayo Clinic Health System
• Medical College of Wisconsin
• Medlytix
• Mindray North America
• Natus Medical
• ODBMed
• Orthoscan
• Penn State Health
• Permanente Medicine
• PGY1 Financial Solutions Corp
• Purdue Pharma LP
• QuidelOrtho
• Radiometer Medical
• Safer Medical LLC
• Sandhills Emergency Physicians
• Sayvant
• SERB Pharmaceuticals
• SonoSim, Inc.
• TEAMHealth
• U.S. Bank Private Wealth Management
• Ubuntu Med
• University of Maryland Emergency Medicine Associates
• UPMC Emergency Medicine
• US Acute Care Solutions
• Vituity
• Washington University School of Medicine
• WestJem
• Zeto, Inc.
In-Kind Commercial Supporters
• AMBU
• B Braun Medical Inc
• GE Healthcare
• Mindray North America
• Philips Point of Care Ultrasound
• Sonosim
• Sonosite
• Verathon
Luncheon with Chairs
• Emergency Medicine Residents' Association (EMRA)
Consensus Conference
• Association of Academic Chairs of Emergency Medicine (AACEM)
• CORD Council of Emergency Medicine Residency Directors
• Stanford University Department of Emergency Medicine
• American Board of Emergency Medicine (ABEM)
• Diasorin
Philadelphia Hunt
• US Acute Care Solutions
RAMS Party
• The Ohio State University Wexner Medical Center
• Stanford University Department of Emergency Medicine
• Medical College of Wisconsin
Residency/ Fellowship Fair
• Vituity
• TEAMhealth
• Stanford University Department of Emergency Medicine
• Gilead Sciences
• AstraZeneca
• Zeto, Inc.
• Butterfly Network
• Echonous
• GE Healthcare
• Mindray North America
• Philips Point of Care Ultrasound
• Sonosite
• Sonosim
• B Braun Medical Inc
Volunteer Event
• Providers Clinical Support System-Opioid Response Network (PCSS - ORN)

By Brian Kenny, DO, MBA, MBe; Mina Attaalla, DO; Puja Singh, MD; and Anthony Rosania, MD, on behalf of the SAEM Vice Chairs Interest Group
Ensuring optimal patient care and staff satisfaction in emergency medicine requires more than clinical expertise—it demands active, visible leadership. One effective strategy to foster this kind of leadership is daily administrative rounding. This simple yet impactful practice involves department leaders regularly visiting the emergency department to observe operations, engage with staff, and address concerns in real time.
This approach, rooted in Lean Management, is often referred to as “going to the Gemba”—a Japanese term meaning to visit the “front lines” to understand the current state of operations and address conflicts. Although frequently overlooked in favor of formal reports and metrics, daily rounding provides a wide range of tangible benefits. It also serves as a real-time sensing mechanism to ensure operational interventions are not only implemented but effective.
Daily rounding offers staff a consistent opportunity to voice concerns, share ideas, and receive real-time feedback. The visibility of leadership through rounding communicates that employees are valued and heard.
Sara Berg, writing for the American Medical Association, describes how addressing small problems—or

“Daily administrative rounding in the emergency department is a low-cost, high-impact strategy that strengthens communication, improves team and patient experiences, and supports a culture of accountability.”
“pebbles”—in real time can reduce physician burnout and increase team morale. Left unaddressed, these issues are often managed through workarounds or become part of normalized deviance, which may create resistance to change.
Administrative rounding allows leaders to identify these issues, understand them, and develop timely interventions. This visibility and responsiveness from leadership communicates that staff are valued and heard, fostering a sense of connection and support. Over time, this kind of engagement contributes
to better teamwork, improved job satisfaction, and lower turnover rates.
Rounding allows leaders to directly observe safety risks, communication breakdowns, or inefficiencies that might otherwise go unnoticed. Immediate action can then be taken to address concerns before they escalate. For example, rounding may identify recurring delays in triage or malfunctioning equipment.
Timely interventions support a culture of continuous improvement
and reduce the risk of adverse events. Without active engagement, minor problems may go unnoticed, leading to latent safety risks. Rounding also allows administrators to reinforce new processes through positive feedback and checklist validation.
Rounding improves communication between frontline staff and administration by providing a direct,

“Too often, small problems—the aforementioned ‘pebbles’—are accepted as part of the norm, introducing risk and undermining larger quality improvement efforts.”
ADMINISTRATION
continued from Page 21
unfiltered channel of information. This reduces distortion from the “telephone game” effect that often accompanies multilayered communication chains.
This transparency builds trust, accelerates problem-solving, and fosters an environment in which staff members feel empowered and involved in decision-making. When staff understand the rationale behind new initiatives and have a voice in their development, they are more likely to support and implement them.
Daily rounding enables leaders to identify and address issues immediately. This real-time troubleshooting enhances departmental agility and supports smoother operations and improved patient throughput.
Too often, small problems—the aforementioned “pebbles”—are accepted as part of the norm. Not only does this introduce risk, but it also creates an environment where larger quality improvement efforts fail due to a lack of buy-in. Engaging with staff and promptly removing these “pebbles” allows leaders to “celebrate small wins,” a critical component of building sustainable change.
Additionally, this process allows staff to observe and learn from administrators who model systemsbased practices and effective communication strategies.
Patients and families take notice when leaders are present and engaged. When administrators interact directly
with patients, it reinforces that the patient experience matters. This personal attention can improve patient satisfaction, especially when feedback leads to measurable improvements.
In one study by Borinski and colleagues, patient satisfaction scores increased by up to 20% following the implementation of regular administrative rounding. Rounding should intentionally include patients waiting in hallway beds or those admitted and awaiting inpatient placement. Despite best efforts, patients boarding in the emergency department associate their experience with the emergency team—making these interactions critical touchpoints.
Although rounding is largely observational and interpersonal, it complements data analytics by adding context to performance metrics. It can uncover the underlying causes of trends seen in reports and surface systemic issues.
Combining the qualitative insights from rounding with quantitative data creates a more complete picture for strategic planning and resource allocation. Rounding may also identify opportunities to collect data not captured by the electronic health record or other reporting tools. When planned intentionally, rounding can include mechanisms for capturing this real-time, experiential data.
Daily administrative rounding in the emergency department is a low-cost, high-impact strategy that strengthens communication, improves team and patient experiences, and supports a culture of accountability.
Consistent leadership presence reinforces expectations for high standards and ensures that policies and best practices are followed. In a complex, fast-paced environment like emergency medicine, these daily check-ins help leaders stay connected to the front lines and foster continuous improvement.

Dr. Rosania is the vice chair for clinical operations and the chief of the division of operations, quality and informatics at Rutgers New Jersey Medical School. In addition to emergency medicine, he is board certified in clinical informatics and healthcare administration, leadership and management.

Dr. Singh is the fellow in healthcare operations, quality and leadership at Rutgers New Jersey Medical School and an attending physician at University Hospital in Newark, New Jersey. She completed residency at Mount Sinai Morningside-West in 2024 and is currently pursuing a Master of Business Administration while completing her fellowship.


Dr. Kenny is an assistant fellowship director and assistant medical director at Rutgers New Jersey Medical School. He is also an assistant professor there.
Dr. Attaalla is the emergency department medical director of quality at University Hospital, where he leads quality improvement and patient safety initiatives for the department of emergency medicine. He is also an associate professor at Rutgers University, where he teaches and mentors residents and medical students in emergency medicine, simulation medicine, point-of-care ultrasound, emergency critical care and evidencebased emergency medicine.

By Alicia Pycraft, PharmD, on behalf of the SAEM Academy of Emergency Medicine Pharmacists
Penicillin allergies are the most commonly reported drug allergies, with approximately 10% of patients worldwide claiming to be allergic. However, studies show that 95% of these individuals do not have an IgE-meditated hypersensitivity and can tolerate penicillins safely. In many cases, symptoms of viral illness—such as rash or fever—are misinterpreted as allergic reactions, leading to inaccurate labeling in childhood.
Mislabeling patients with penicillin allergies can significantly affect clinical outcomes, as beta-lactams
are often first-line therapies for many infections. Patients labeled as allergic are frequently prescribed second-line or broader-spectrum antibiotics, which contributes to antimicrobial resistance.
Documented penicillin allergies have been associated with increased risks of healthcare-associated infections, surgical site infections, prolonged hospital stays, higher antibiotic costs, and increased readmission rates
Although many patients are incorrectly labeled as allergic, penicillin remains the leading cause
of drug-induced anaphylaxis in the United States among those with true allergic reactions. Therefore, careful evaluation of reported penicillin allergies is essential to ensure safe and effective antimicrobial therapy.
When evaluating a reported penicillin allergy, it is critical to distinguish low-risk histories from true immune-mediated hypersensitivity. Low-risk histories may include gastrointestinal upset, a family history of penicillin allergy, pruritus without rash, or remote, unknown

“Approximately 95 percent of individuals who report a penicillin allergy do not have an immunoglobulin E-mediated hypersensitivity and can safely tolerate penicillins.”
reactions without IgE-mediated features. Clinical decision-making tools, such as the PEN-FAST score, can assist in identifying low-risk patients.
Clinically significant hypersensitivity reactions are immune-mediated and best understood through the Gell and Coombs classification system, which categorizes reactions into four types:
• Type I is immediate and IgEmediated. Re-exposure to the allergen leads to rapid-onset symptoms such as urticaria, bronchospasm, hypotension, and potentially life-threatening anaphylaxis. Notably, these reactions tend to diminish over time with approximately 80% of affected individuals developing tolerance within 10 years.
• Type II involves antibodymediated cytotoxicity, which can manifest as hemolytic anemia, thrombocytopenia, or neutropenia, typically within hours to days of exposure.
• Type III is caused by immune complex formation and deposition in tissues, leading to complement activation and inflammation. These reactions generally emerge one to three weeks after exposure and may present as serum sickness–like syndromes, vasculitis, or immune complex–mediated arthritis.
• Type IV is a delayed, T-cell–mediated response that can appear days to weeks after drug administration. Reactions range from mild maculopapular eruptions to severe cutaneous
adverse reactions, including Stevens-Johnson syndrome, toxic epidermal necrolysis, drug reaction with eosinophilia and systemic symptoms, and acute generalized exanthematous pustulosis. This category also includes isolated organ involvement, such as acute interstitial nephritis or drug-induced liver injury.
Accurately identifying the type of hypersensitivity reaction is crucial for diagnosis, risk assessment, and determining whether rechallenge, desensitization, or alternative antibiotics are appropriate.
A detailed allergy history is vital to classifying the reaction type and

“By conducting a thorough allergy history and applying appropriate delabeling strategies, emergency clinicians can promote antibiotic stewardship and expand access to effective beta-lactam treatment options.”
ASK THE PHARMACIST
continued from Page 25
ensuring patients receive optimal antimicrobial therapy. When assessing penicillin allergies, consider asking the following questions:
• What is the name of the medication?
• How was the medication administered?
• How long ago did the reaction occur?
• What were the signs and symptoms?
• How long after taking the medication did symptoms start?
• When in the course of therapy did the reaction occur?
• What other medications were being taken at the time?
• Why was the medication prescribed?
• What treatment was required to manage the symptoms?
• Had the patient taken this medication or a cross-reacting medication before?
• Has the patient taken the same or similar medications since the reaction?
Several strategies are available for penicillin allergy delabeling, depending on the nature and severity of the reaction. For patients with a history of anaphylaxis or a recent reaction suggestive of IgE mediation (e.g., immediate-onset urticaria), skin testing is recommended.
For adult patients with low-risk allergy histories and pediatric patients with benign cutaneous drug reactions, a direct oral amoxicillin challenge is preferred. This involves administering a full dose of amoxicillin, followed by 30 to 60 minutes of observation. If no reaction occurs, the allergy label can be removed from the medical record.
Skin testing and oral challenges are contraindicated in patients with histories suggestive of type II, III, or IV hypersensitivity.
Beta-lactam antibiotics contain a core beta-lactam ring and up to three variable side chains (R1, R2, R3). Cross-reactivity between penicillins and cephalosporins is primarily due to structural similarities in the R1 side chain. The estimated cross-reactivity rate is approximately 2% to 8% for first-generation cephalosporins and less than 1% for later generations and carbapenems.
Recent evidence shows that true immunologic cross-reactivity is much lower than previously believed. Historically, it was recommended that patients with penicillin allergies be skin tested prior to receiving cephalosporins due to cross-reactivity risk. A 2022 practice parameter update published in the Journal of Allergy and Clinical Immunology supports a simplified approach:
Patients with an unverified, nonanaphylactic penicillin allergy may receive any cephalosporin without prior testing. Even patients with a documented history of IgE-mediated anaphylaxis may safely receive a noncross-reactive cephalosporin (e.g.,
cefazolin, ceftriaxone, or cefepime) without testing. Carbapenems may also be used safely in patients with prior penicillin or cephalosporin allergies, regardless of the severity of the reaction.
However, patients with a history of type II through IV hypersensitivity reactions should not be re-exposed to any beta-lactam agents without consultation with an immunologist. In these high-risk cases, alternative antimicrobials should be chosen based on the infection source and local susceptibility patterns. If no safe alternative exists, rapid desensitization may be required.
Penicillin allergies are frequently reported, but most patients do not have true immune-mediated hypersensitivity. Mislabeling leads to unnecessary use of second-line antibiotics and contributes to poorer outcomes. Emergency clinicians can improve antibiotic stewardship and patient safety by taking thorough allergy histories and applying evidence-based delabeling strategies. This enables broader use of effective beta-lactam agents and reduces the risks associated with inappropriate antibiotic selection

Dr. Pycraft is an emergency medicine clinical pharmacy specialist at the University of Maryland Medical Center in Baltimore, Maryland. She currently serves on the communications committee for the Academy of Emergency Medicine Pharmacists.

By Nathan Lewis, MD; Ambika Anand, MD, MEHP; Carrie Maupin, MD; and Danielle Nesbit, DO, on behalf of the SAEM Clerkship Directors in Emergency Medicine academy
Did you hear the news? Emergency medicine is back to being a popular specialty! According to the most recently published 2025 National Resident Matching Program (NRMP) data, the number of applicants is rising, and unfilled positions are declining. For many, this feels like a return to form for a specialty long considered a competitive and popular choice. But while the latest numbers bring some optimism, they tell an incomplete story. To fully understand the current landscape,
it’s important to examine the broader trends that led to this point.
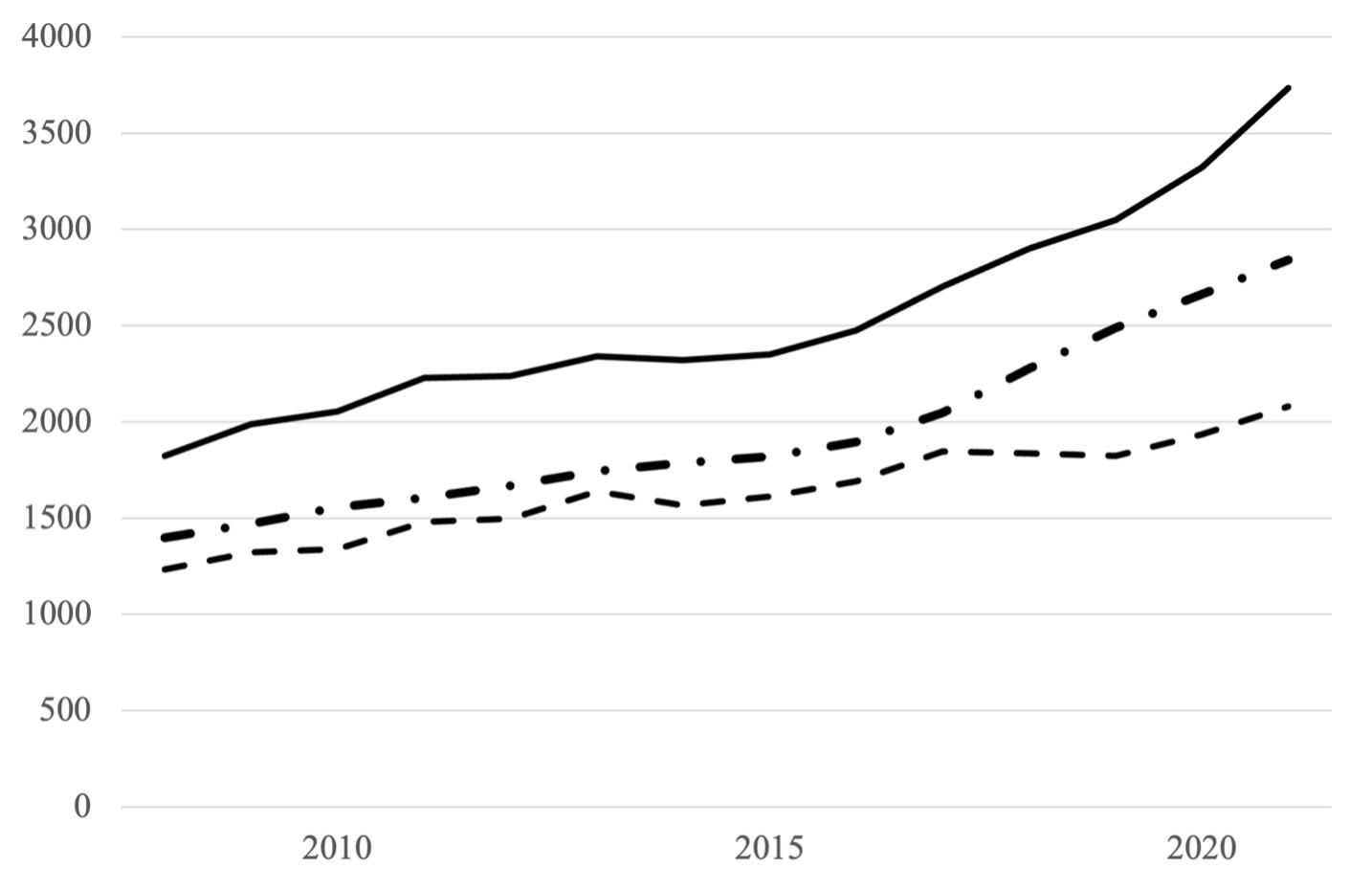
The Setup: Decades of Growth Data from the NRMP’s Results and Data and Charting Outcomes reports offer valuable insight. One of the most consistent patterns in the emergency medicine match has been growth—significant growth. In 2025, the number of available postgraduate year one (PGY-1) training positions offered by categorical emergency medicine
programs has roughly doubled since 2009 and more than tripled since the start of the 2000s. That growth has not been linear. A steeper increase in the number of positions offered annually began in 2017.
Although detailed data on all applicants is unavailable prior to 2008, trends since then show that the growth in applicants roughly mirrored the growth in available positions. Applicant numbers increased steadily from 2008 to 2016, then surged beginning in 2017.
“The applicant pool has diversified, with more Doctor of Osteopathic Medicine graduates and international medical graduates matching into emergency medicine.”
(Figure 1) This rise in both applicants and applications contributed to the perception of emergency medicine as a highly competitive specialty. For a field historically dominated by an allopathic match majority and an unfilled rate well under 1%, it is easy to see why.
Despite this rapid expansion, most applicant groups continued to match successfully. Over the past 10 years, the proportion of U.S. Doctor of Medicine (MD) seniors applying to and matching in emergency medicine has remained steady—and even increased
slightly in the past five years. The same trend holds true for Doctor of Osteopathic Medicine (DO) senior applicants. (Figure 2) Additionally, the percentage of total matches accounted for by international medical graduates (IMGs) has steadily risen over the past five years, including the period prior to the 2023 Match.
The Crash: A Sudden Shift
Although 2023 is remembered as the year emergency medicine saw a striking number of unfilled programs nationwide, the decline in applicants did not happen overnight. It began in 2021 and was already reflected in the
2022 Match. That year, the percentage of unfilled positions reached 7.5%, surpassing the previous all-time high of 6.8% in 1990. Then in 2023, the rate of unfilled positions exceeded 18%. (Figure 3)
In this unprecedented year, the total number of applicants fell short of the number of available training positions, and the unfilled rate climbed to nearly three times the previous record. This was a significant disruption for a specialty typically ranked among
continued on Page 31
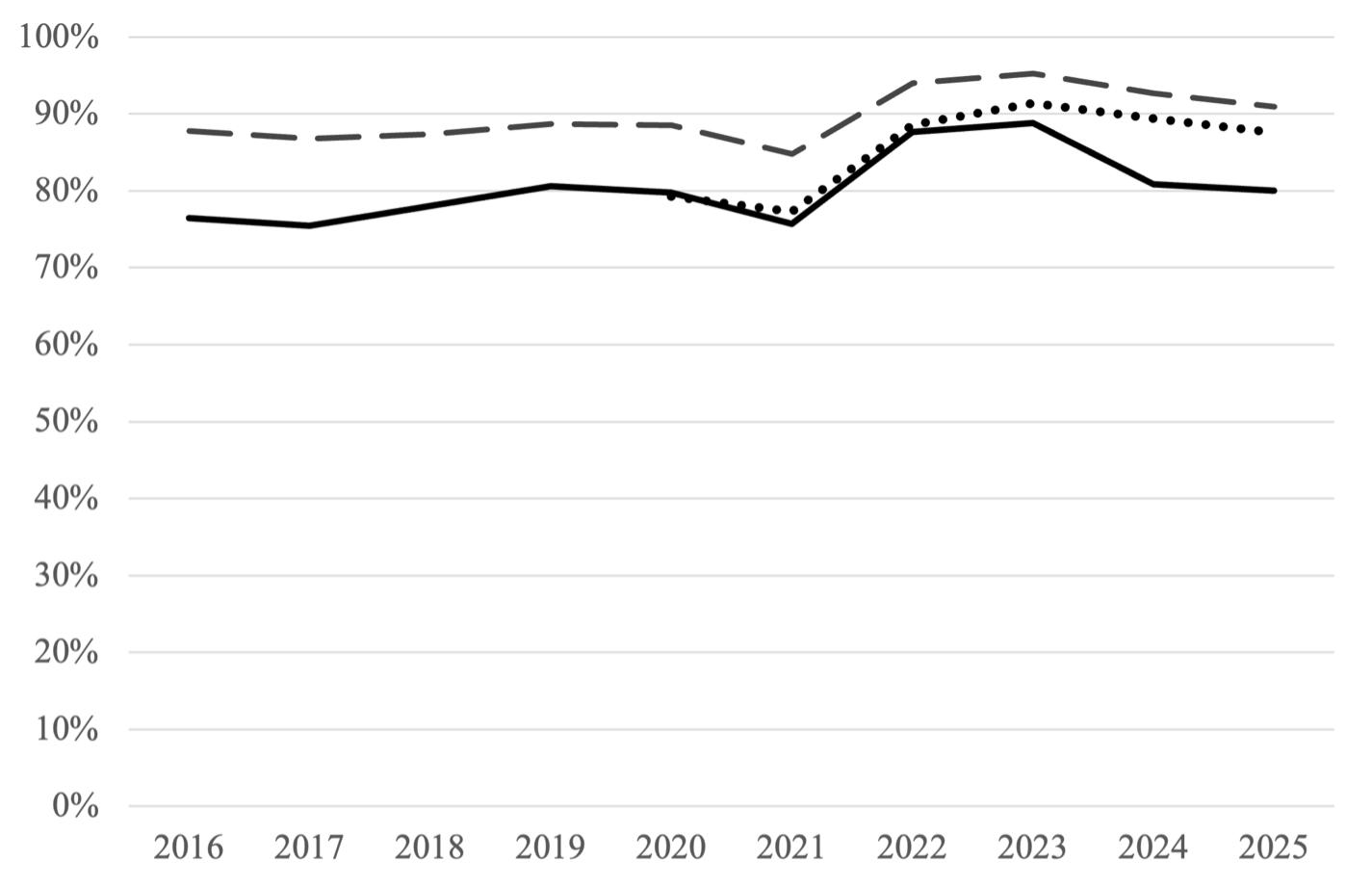
Figure 2. Percentage of MD senior applicants (dashed line), DO senior applicants (dotted line; data unavailable prior to 2020), and all applicants (solid line) applying to emergency medicine who successfully match into EM from 2016 to 2025.
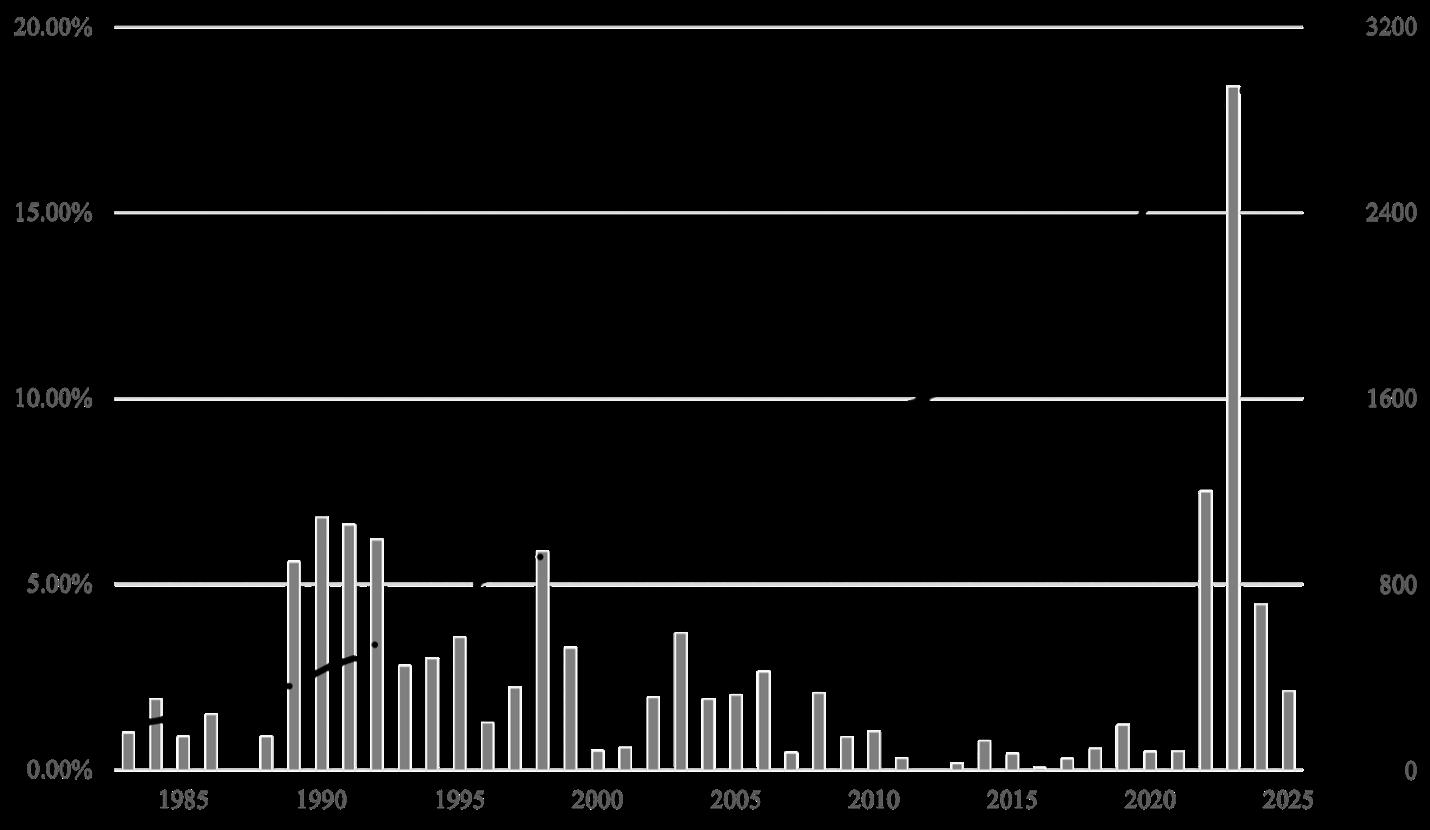
3. Number of offered PGY-1 training positions (dash-dotted line, right axis) overlaid on percentage of unfilled PGY-1 training positions (vertical bars, left axis) from 1983 to 2025.
“In 2023, the rate of unfilled positions exceeded 18%—a significant disruption for a specialty typically ranked among the top three or four in categorical match volume.”
CAREER CORNER
continued from Page 29
the top three or four in categorical specialties with the highest volume of matches.
Much speculation has emerged about the factors contributing to the 2023 Match outcome. Regardless of cause, students, medical schools, and program directors approached the 2024 cycle with anticipation and cautious optimism. The result was a clear rebound. Not only did emergency medicine overcome its applicant deficit, but the total number of applicants also returned to near-2021 levels.
However, the composition of the applicant pool shifted. Proportionally more DOs and IMGs matched into emergency medicine than in previous years.
Another notable change is in the number of applicants who preferred emergency medicine—meaning it was either the only specialty to which they applied or the top-ranked specialty in a dual-application strategy. Across Charting Outcomes reports released by the National Resident Matching Program (NRMP) from 2007 to 2024, although the number of preferred emergency medicine applicants grew, it did so at a slower rate than the total applicant pool. In 2014, preferred EM applicants accounted for 91% of the entire applicant pool; in 2024, that figure fell to 83%. Further, the ratio of preferred applicants to available positions has declined—from 1.3 to 1 in 2007 to just under 1 to 1 in 2024.
This suggests that more applicants may now be considering emergency medicine as a backup option.
This year, the number of PGY-1 training positions again increased— though at a slower pace than in recent years—to a new high of 3,068. Applications also rose to 3,753, roughly equal to the 2021 total. Of those applicants, 40% were MD seniors and 33% were DO seniors. Among those who matched into emergency medicine, 46% were MD seniors, 36% were DO seniors, and 15% were IMGs. Just over 2% of positions went unfilled—half the unfilled rate in 2024. The NRMP has not yet released data on preferred specialties for 2025, and it remains to be seen whether these trends will continue.
The data from the 2025 Match indicate a second consecutive year of recovery for emergency medicine, with rising applicant numbers and fewer unfilled positions. However, this recovery tells only part of the story. The applicant pool has diversified, with more DOs and IMGs matching into emergency medicine. There also appears to be an increase in applicants ranking emergency medicine as an alternative to their first-choice specialty. Though still a minority, this trend may have long-term implications for program recruitment.
Is this good news for students? Absolutely. Emergency medicine has never been more welcoming to a broad and diverse group of applicants. The specialty’s growth over the past four decades underscores its resilience and enduring importance to the healthcare system.




Dr. Lewis is an associate professor at the Virginia Commonwealth University School of Medicine, where he serves as emergency medicine clerkship director and assistant residency program director.
Dr. Anand is an assistant professor at the Virginia Commonwealth University School of Medicine, where she serves as associate program director for the medical education fellowship.
Dr. Maupin is a second-year medical education fellow and clinical instructor in the Virginia Commonwealth University Department of Emergency Medicine.
Dr. Nesbit is a first-year medical education fellow and clinical instructor in the Virginia Commonwealth University Department of Emergency Medicine.

By Jacob Garrell, MD; Michael Sherman, MD; and Peter Hou, MD on behalf of the SAEM Critical Care Interest Group
If you have worked in a U.S. emergency department (ED), you are likely familiar with the growing challenge of ED boarding. Prior to the COVID-19 pandemic, ED patient volumes had increased more than 30% over the previous decade. From 2006 to 2014, the number of annual ED visits for critically ill patients rose from 2.8 million to 5.2 million.
The American College of Emergency Physicians (ACEP) defines boarding as the time after a patient has been admitted but before they are transferred from the ED. As hospital crowding worsens, critically
ill patients are increasingly boarding in the ED while awaiting intensive care unit (ICU) beds. These patients face unique risks, and the problem is intensifying as demand for critical care grows.
For ICU-level patients, the duration of ED boarding varies widely depending on institutional capacity and mitigation strategies. Multiple studies have shown that boarding beyond six hours is associated with increased mortality, with some reporting a 1.5% increase in risk of death for each additional hour a critically ill patient remains in the ED.
Recognizing this concern, the Society of Critical Care Medicine and ACEP formed the Emergency Department–Critical Care Medicine (ED-CCM) Boarding Task Force in 2017. Their findings revealed that ED boarding contributes to higher mortality, longer ICU stays, and increased ventilator use. The task force recommended action in three main areas: ED-based solutions, hospital-level strategies, and the development of resuscitation care units (RCUs).

continued from Page 33
One promising and broadly applicable solution is the implementation of a standardized handoff tool for ICU boarders. Transitions of care during ED shift changes are known risk points for medical error. Tools such as I-PASS have already demonstrated improvements in communication and patient safety in pediatric emergency settings and may serve as a model for similar handoff standardization. Applying a similar structure to ICU boarder handoffs between ED teams could reduce errors, boost efficiency, and improve outcomes. Regardless of whether an ED uses acuity cohorting, RCUs, or traditional layouts, handoff represents a common vulnerability—and an opportunity for improvement.
Research into existing handoff practices for ICU patients in adult EDs has revealed significant gaps
“Transitions of care during emergency department shift changes are known risk points for medical errors.”
in critical information. For example, documentation of code status, contingency plans, and completed interventions is often incomplete at the time of handoff These gaps underscore the need for structured approaches to mitigate the potential impact of ED boarding.
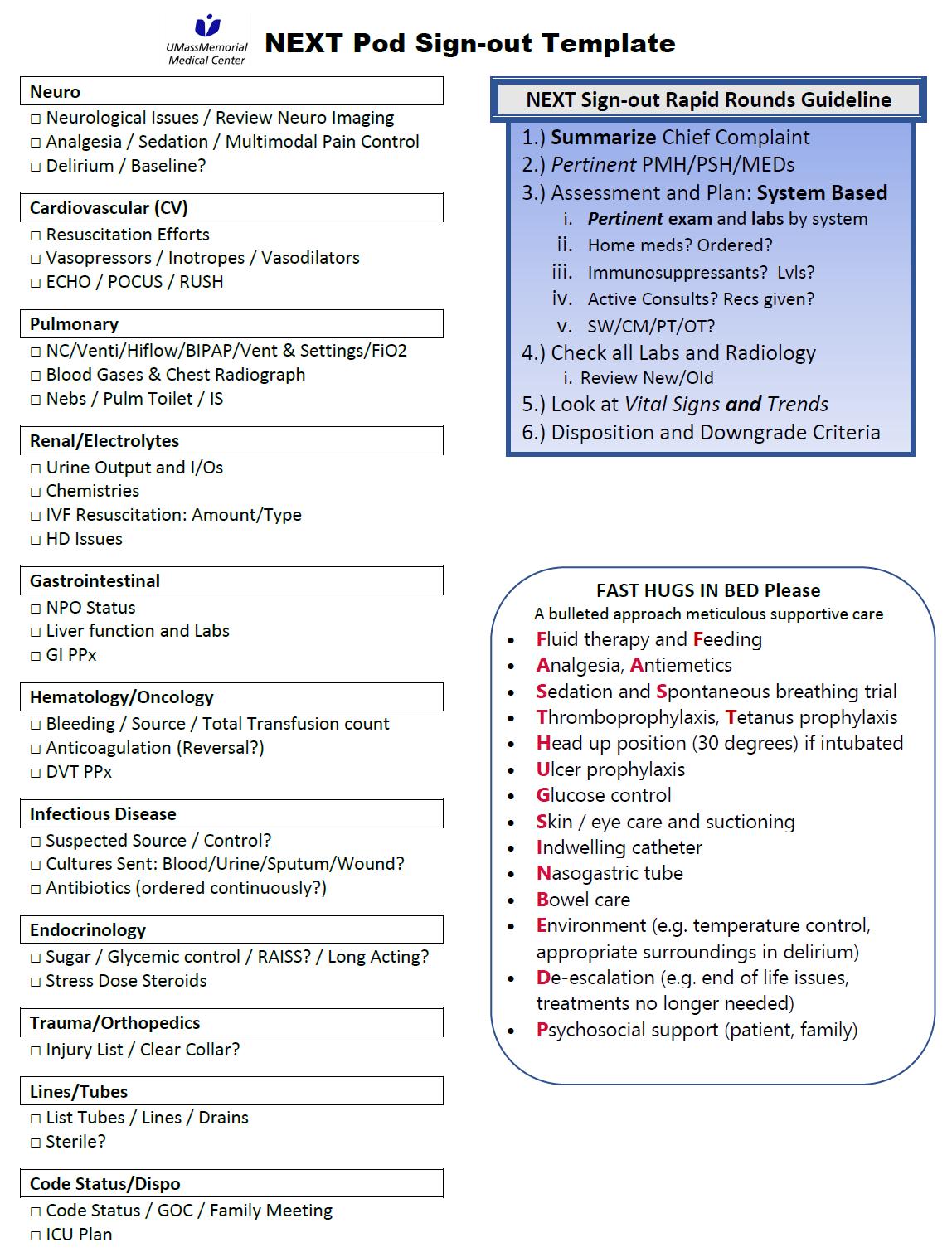
At UMass Memorial Medical Center’s University Campus in Worcester, Massachusetts—an urban tertiary care center that serves approximately 90,000 patients annually—critically ill patients frequently board in the ED due to high patient volumes and acuity.
To address the specific needs of this patient population, the hospital created a dedicated 9-bed RCU, known locally as the NEXT Pod. The unit is staffed by an attending physician and resident, with a low nurse-to-patient ratio. It routinely manages ICU-level patients awaiting transfer to inpatient critical care. It admits approximately 20 new highacuity patients daily, in addition to those transferred from other areas of the ED. ICU boarding times in the NEXT Pod vary, often exceeding 24 hours and spanning multiple ED shifts.
“Improving communication during the handoff of our most vulnerable patients is not just a quality improvement initiative—it is a frontline strategy to reduce morbidity and mortality in the emergency department.”
To reduce errors and improve care transitions in this complex environment, a multidisciplinary quality improvement team developed a rapid, systems-based ICU-style signout tool tailored for ED use. Designed by emergency medicine and EM/ critical care-trained physicians, the tool draws from traditional ICU rounds, incorporating structured systemby-system prompts and reminders for best practices—such as deep vein thrombosis prophylaxis, timely antibiotic administration, continuation of critical home medications, and ventilator settings.
For ease of access, the tool was laminated and posted at computer workstations. Despite its formal nature, the tool was built for emergency department, with the goal of completing a flexible and rapid sign-out within 30 minutes.
The handoff tool was launched in fall 2024. Its impact was assessed using a de-identified survey based on the Feasibility of Intervention Measure (FIM) framework. The survey evaluated providers’ perceptions of:
• The existing handoff process
• The utility and usability of the new tool
• Integration with current ED workflows
• Provider comfort in managing ICUlevel patients
The survey also included an openended response section for additional feedback.
Results were largely positive. Nearly 93% of respondents agreed that the standard ED handoff process omitted important elements of care, especially
for the most complex patients. All respondents agreed that the new tool had the potential to reduce perceived errors in patient care. A salient finding was how feasible is a standardized handoff in an already chaotic setting. Notably, 78.5% of participants reported feeling more comfortable managing and signing out critically ill patients after using the tool.
The open-ended responses offered valuable insights beyond what was captured in the structured survey questions. Participants consistently expressed appreciation for the tool’s organized format and its alignment with expectations commonly seen in intensive care unit settings. However, a key concern also emerged: while the idea of standardization was widely supported, its successful implementation depends on having sufficient time, staffing, and, in some cases, adjustments to existing workflows. Several respondents noted that the handoff process added to their time burden and suggested that protected time or formal integration into shift schedules would be necessary to ensure consistent use.
Although this pilot study involved a small sample size, the early results suggest that a structured ICU-style sign-out tool adapted for emergency medicine can enhance care continuity, patient safety, and provider confidence during transitions of care from the ED to the ICU.
As ED boarding continues to worsen in the post-COVID landscape— particularly for ICU-level patients— low-cost, scalable interventions such as this may hold promise for both
academic and community settings. Further research involving larger sample sizes, longitudinal tracking, and potential integration with electronic medical records could help validate and refine the approach.
Improving communication during the handoff of our most vulnerable patients is not just a quality improvement initiative—it is a frontline strategy to reduce morbidity and mortality in the emergency department

Dr. Garrell is a postgraduate year three emergency medicine resident at the University of Massachusetts in Worcester with a growing interest in the care of critically ill patients in both emergency department and intensive care unit settings. He plans to pursue a fellowship in critical care medicine at Brigham and Women’s Hospital.

Dr. Sherman is dual boardcertified in emergency medicine and critical care medicine and practices at Boston Medical Center. With experience working across multiple emergency department–intensive care unit and resuscitation care unit settings, his research focuses on resuscitation and ED-ICU operations. He has led numerous quality improvement initiatives and developed clinical practice guidelines at the intersection of emergency and critical care medicine.

Dr. Hou is dual board-certified in emergency medicine and critical care medicine. He practices at Brigham and Women’s Hospital and is an assistant professor of emergency medicine at Harvard Medical School. His research focuses on sepsis, acute respiratory distress syndrome, and COVID-19.

By Diana M. Bongiorno, MD, MPH; Jennifer Love, MD, MSCR; Joe-Ann Moser, MD, MS; Richelle J. Cooper, MD, MSHS; and Amy Zeidan, MD, on behalf of the SAEM Academy for Women in Academic Emergency Medicine
Despite notable advancements, women in academic emergency medicine (EM) continue to face challenges related to pay equity, promotion, scholarly activity, and parental leave policies. A growing body of research is helping to better understand these persistent gender equity issues within the EM workforce.
To highlight key developments, members of the SAEM Academy for Women in Academic Emergency Medicine (AWAEM) Research Committee conducted a literature
review of 2024 PubMed-indexed publications relevant to gender equity in EM. The committee reached a consensus on five top articles that provide timely insight. These studies cover a range of topics, including salaries of new EM residency graduates, chief resident selection, family-friendly policies, attrition rates, and women’s professional development programs.
Together, these articles offer evidence to guide the development and implementation of strategies for members of the Society for
Academic Emergency Medicine (SAEM) to promote gender equity within their departments.
Association of Gender and Personal Choices with Salaries of New Emergency Medicine
Graduates
Fiona E. Gallahue et al.
Methods: The authors sent a survey to over 2,000 graduating EM residents in 2019 that included questions about their demographics, perspectives on factors influencing their first job post-training, and base

“Compared to White men, women residents from underrepresented in medicine groups were half as likely to be chief residents.”
salary and characteristics of their first job. Quantile regression was used to analyze salary differences by gender while controlling for demographic, training, and first job characteristics.
Key Results: Among 258 graduating EM residents with completed surveys, the median first job salary was $30,000 higher for men versus women, even after adjusting for other factors. Women placed more importance on parental leave policy, proximity to family, and location/ setting in the job search, and less importance on salary, compared to men.
Limitations: A key limitation is the representativeness of the sample given only ~12% response rate among 2019 graduating EM residents.
Jennifer W. Tsai et al.
Methods: The authors analyzed data collected by the Association of American Medical College on EM graduates from 2017-2018. Binomial regression was used to analyze the relative risk of sex, and intersection of sex and racial and ethnic identity, on serving as chief resident, adjusting for USMLE Step 2 CK scores and clustering within residency programs.
Key Results: Compared to White men, women residents from underrepresented in medicine groups were half as likely to be chief residents. White women were significantly more likely to be chief
residents, relative to White men.
Limitations: The authors did not have data on residents who may have been selected for, but declined, the chief resident position, or on factors such as residency evaluations and test scores that may have influenced selection. Additionally, analyses could not account for the different ways in which chief residents are selected at different programs.
Consensus-Driven Recommendations to Support Physician Pregnancy, Adoption, Surrogacy, Parental Leave, and Lactation in Emergency Medicine
Michelle D. Lall et al.
“Among 258 graduating was $30,000 higher

graduating EM residents with completed surveys, the median first job salary higher for men versus women, even after adjusting for other factors.”
AWARENESS
continued from Page 37
Methods: The steps involved in developing consensus recommendations included: 1) a working group of members from the ACEP Well-Being Committee and SAEM AWAEM completing a literature review of parental leave and related policies, including relevant laws and national standards, and drafting initial recommendations; 2) recruiting 33 stakeholders from 11 national EM groups to participate in a consensus process that involved contributing additional recommendations and 3 rounds of voting to reach consensus; 3) incorporating feedback from focus groups and an open public comment period.
Key Results: This group developed 17 consensus-driven recommendations to assist departments with implementing family-friendly policies, including related to miscarriage, prepartum and peripartum periods, parental leave, and lactation.
Limitations: The consensus process involved a group of stakeholders which may not be representative of the EM workforce. The group did not consider the feasibility of implementing these recommendations as part of the consensus process and did not come to a consensus to make recommendations on fertility treatment, secondary parental leave, scheduling upon return to work, or childcare.
Rates of Emergency Medicine Residency Graduates by Gender
Nikita A. Salker et al.
Methods: The authors gathered lists of EM graduates from classes pre1990 to 2010 from 21 EM residency programs established before 2005.
In 2020, they collected data from state licensing board websites and other public websites (e.g. hospital websites, social media), including on state license status and hospital privileges. “Attrition” was defined as not currently working clinically in EM or an EM subspecialty.
Key Results: Among 3,725 EM physicians in the workforce at least 10-30 years following residency, attrition rate from clinical EM did not significantly differ by gender.
Limitations: It is possible that individuals may have been misclassified, as the authors did not contact individuals in the “attrition” group to ensure accurate classification. Graduates of programs included in this study may not be representative of the EM workforce, and trends among physicians graduating residency 10-30 years prior may not be the same as trends among more recent graduates.
Women's Professional Development Programs for Emergency Physicians: A Scoping Review
Stacey Frisch et al.
Methods: The authors conducted a systematic search of peer-reviewed literature related to women’s professional development groups for EM physicians. They extracted data on program leadership and objectives, funding sources, educational activities, meeting themes, and barriers encountered from the included studies.
Key Results: Data from 11 studies of 10 professional development groups for women in EM suggest these groups can have an important role in increasing mentorship, recognition, community, job satisfaction, and well-being. The authors summarize strategies to overcome potential
challenges related to facilitating attendance, ensuring sustainability, obtaining funding, and measuring impact.
Limitations: Some of the included studies were missing data on program characteristics of interest. The included programs were largely in academic institutions, limiting generalizability.





Dr. Bongiorno is a chief resident in the Harvard Affiliated Emergency Medicine Residency at Mass General Brigham. In July, she will begin a research fellowship in the National Clinician Scholars Program at the University of Pennsylvania. Dr. Love is an assistant professor of emergency medicine at the Icahn School of Medicine at Mount Sinai. She also serves as the vice president of education for the Academy for Women in Academic Emergency Medicine.
Dr. Moser is an assistant professor and assistant residency program director at the University of Wisconsin–Madison. She also serves as co-chair of the Academy for Women in Academic Emergency Medicine Research Committee.
Dr. Cooper is a professor of emergency medicine and vice chair of research at the UCLA Department of Emergency Medicine. She is also executive deputy editor at Annals of Emergency Medicine.
Dr. Zeidan is an associate professor of emergency medicine at Emory University School of Medicine and adjunct professor at Emory Rollins School of Public Health. She is the medical director of the Grady Medical-Legal Partnership and co-director of the Georgia Human Rights Clinic. She is also the outgoing president of the Academy for Women in Academic Emergency Medicine.

By Rana Barghout; Joshua Lachs; and Tony Rosen, MD, MPH
Case 1: A 47-year-old man with a medical history of hypertension, hyperlipidemia, and tobacco use presents with crushing substernal chest pain, nausea, shortness of breath, and diaphoresis. An electrocardiogram (EKG) performed in triage reveals ST-segment elevations consistent with an inferior wall acute myocardial infarction. His pain is worsening, he is bradycardic, and he expresses a desire to leave the emergency department (ED), saying, “My brother died in this hospital.”
Case 2: Another 47-year-old man with no significant medical history presents with a single episode of sharp, non-exertional, nonreproducible chest pain, worsened by movement. His lung exam and EKG are normal. While awaiting troponin results, he reports feeling reassured by the normal workup thus far, feels
better, and says he wants to “get out of the ED.”
On a busy shift in a crowded ED, physicians often encounter patients who refuse further workup or treatment and wish to leave against medical advice (AMA). Approaching these situations is inherently challenging, as it requires balancing the duty to provide care with the ethical obligation to respect patient autonomy.
In many cases, patients refuse treatment due to misunderstanding or miscommunication. Ideally, patients can be persuaded—without coercion—to accept the necessary care. Emergency physicians may achieve this by identifying and addressing the patient’s underlying concerns. This often requires building trust through attentive listening, empathy, and meeting basic needs (such as
offering a blanket or a glass of water). Physicians should explain medical concerns in clear, easily understandable terms. Negotiation and compromise may also help; patients might accept a partial workup or agree to the first steps of a treatment plan in exchange for a promise to reassess afterward. However, some patients remain firm in their decision to leave the ED despite our concerns. In these situations, physicians must evaluate whether the patient has the capacity to make the decision to leave AMA. The standard criteria for assessing decision-making capacity include the ability to:
• Understand relevant information.
• Appreciate the situation and its consequences.
• Reason through options.
• Communicate a choice.
“The threshold of decision-making capacity required to refuse treatment increases in proportion to the risk and complexity of the decision.”
A patient who meets all four criteria at the time of evaluation should be allowed to leave AMA. A patient who lacks any of these components does not have the capacity to refuse care and should not be permitted to leave. For their safety, it may be necessary to involve hospital security or administer sedatives, if appropriate, to continue medical workup and treatment.
This approach—standard across emergency medicine and other medical specialties—suggests that the same criteria should be used to assess both patients described above. Yet, many emergency physicians would feel differently about discharging these patients AMA, despite their similar age and presenting complaint.
This contrast underscores a key but underemphasized concept in emergency medicine: the “sliding scale” of capacity, as described by medical ethicists. According to this framework, the threshold of decisionmaking capacity required to refuse (or accept) treatment increases in proportion to the risk of refusal and complexity of the decision. In the examples provided, the likelihood of a poor outcome after leaving the ED is vastly different for the two patients. For the patient experiencing a STEMI and bradycardia, the capacity threshold to refuse intervention is substantially higher than for the patient with benign chest pain.
So how should emergency physicians apply the sliding scale in practice? We suggest three strategies:
1. Consider risk and gather more information, when possible, to accurately assess it.
2. Spend more time evaluating capacity in cases involving higher medical risk or complex decisions.
3. Consult a specialist for a second opinion when a patient’s capacity remains uncertain.
Understanding the medical risk associated with leaving AMA is essential to evaluating capacity. Before allowing a patient to sign out AMA, clinicians should attempt to obtain additional context through further history-taking or a more thorough chart review. Although information is often limited, risk assessment amid uncertainty is a core skill in emergency medicine.
Physicians should also devote more time to assessing the capacity of patients at higher medical risk or facing complex decisions. These patients must clearly possess all four elements of decision-making capacity and meet the heightened threshold dictated by the risk associated with the decision.
While assessing capacity falls within the scope of emergency medicine and does not typically require psychiatric or ethics consultation, seeking a second opinion may be appropriate in uncertain or high-risk cases. For example, in Case 1, where the stakes are especially high, a specialist consultation can provide added clarity. Before consulting, however, physicians should make a final effort to ethically persuade the patient. This could involve active listening, offering small compromises (such as agreeing to one more test), or simply continuing to provide comfort and build rapport. If these efforts fail, a consultant may not only offer a fresh perspective but
also reinforce the seriousness of the situation to the patient. In some cases, the act of calling in a specialist—along with the wait involved—can prompt a patient to reconsider leaving.
In the midst of a busy ED shift, one of the best outcomes is hearing a consultant say, “I’ve convinced them to stay for the workup and treatment.”
As physicians, we are ethically bound both to respect a capacitated patient’s right to make an unsafe decision and to protect a noncapacitated patient from harm. Navigating this tension can be challenging in time-pressured, lifethreatening emergencies. Keeping the “sliding scale” framework in mind and applying these practical strategies can help emergency physicians make ethically sound decisions when patients seek to leave AMA.


Rana Barghout is a fourth-year medical student at Weill Cornell Medicine pursuing a career in emergency medicine. Her research focuses on refusal of care, capacity assessment, and agitation management among older adults in emergency department settings.
Josh Lachs is a research assistant in the Department of Emergency Medicine at Weill Cornell.
Dr. Rosen is an associate professor of emergency medicine at Weill Cornell Medicine and an emergency physician practicing at NewYorkPresbyterian Hospital

By Joel Cox, PhD
Whenever Billy Pilgrim encounters death in Kurt Vonnegut’s 1969 novel Slaughterhouse-Five, he recites the same cynical epitaph: “So it goes.” The phrase functions both as a way of rationalizing death—of making it make sense—and as a startling reminder of how frequently death occurs in the novel, which centers on the end of World War II.
While shadowing in the emergency department (ED) as part of my graduate studies in health care ethics, I found that death was often met with a similarly stoic response.
At least two patients died the night I shadowed. It was my first time in the ED—and also the first for one of the trauma nurses. A motor vehicle accident and a gunshot wound—two
unfortunately common incidents in St. Louis, where the hospital is located—punctuated the night and were part of a steady stream of trauma patients wheeled into the bays and later taken to the floor.
One image that has stayed with me is of two clinicians wheeling a patient with an open thoracotomy through the ED, one of them manually pumping the patient’s heart with his hand. I didn’t see the patient die, but the extreme nature of the intervention—combined with the later confirmation of his death—deeply rattled me, as well as the new trauma nurse, who broke down in tears. One of her colleagues explained quietly that it had been her “first death.”
Later, during a brief pause between events, the attending physician took a moment to chart and said
something she would repeat several times throughout the night: “We are rarely bored.”
To me, as an ethics graduate student, that seemed like an understatement. At first, I took it as a kind of dark humor common in medicine—a way to diffuse the tension for clinicians who encounter death on a scale few of us can imagine. But on further reflection, I now see the phrase as something closer to Vonnegut’s “So it goes.”
“We are rarely bored” served to rationalize the experience of the clinicians in the ED that night. It also underscored the connection among them—as members of one team. Most of all, it gave voice to a situation in which most people, including myself, would have no words at all.

“How does one make sense of watching someone die after receiving brutally invasive, though necessary, care—only to watch those same clinicians, still covered in blood, march down the hall to save someone else.”
How does one make sense of watching someone die after receiving brutally invasive, though necessary, care—only to watch those same clinicians, still covered in blood, march down the hall to save someone else?
“We are rarely bored” doesn’t do justice to the experience, but it was something to say. And it seemed to help the team move on with their shift.
In my estimation, that phrase served three purposes:
1. It provided language for a situation where words are often elusive.
2. It fostered unity among clinicians, reinforcing their shared experience.
(“We” as a team are rarely bored.),
3. Its repetition served as a quiet reminder—like “So it goes”—that there is too much death occurring.
All three of those functions are necessary to sustain the work of emergency care. Clinicians need a way to make sense of what they witness, a feeling of comradery, and a reminder that what they are experiencing is not normal—and should not be normalized.
Of course, a phrase like “We are rarely bored” is no substitute for emotional or psychological care for clinicians, nor for institutional change where needed. But sayings like this do serve an important role in the practice of emergency care. That night, I saw how the attending physician’s words reflected not only her experience but also exemplified her leadership and quiet expertise.
I left the hospital wondering how the team processes death on such a
scale. I think part of the answer lies in the words clinicians use to fill the silences left by tragedy. When many words feel inadequate for the reality of death in the ED, sometimes only a few words—like “We are rarely bored”—can begin to encapsulate what they’ve witnessed.
So it goes in the ED.

Dr. Cox is a doctoral student at Saint Louis University studying healthcare ethics and philosophy.

By Surriya Colleen Ahmad, MD, on behalf of the SAEM Academy for Geriatric Emergency Medicine
“Group mind.” In improvisational comedy, we use this phrase to describe a state of harmony among performers—a collective flow in which everyone is listening, responding, and building something together. It’s not about one person being funny or standing out; it’s about co-creating a moment, often from nothing, through trust and presence.
Over the years, I’ve realized that group mind isn’t just for the stage. It’s the same force at work in a trauma bay—when an emergency medicine team instinctively moves together, anticipating each other’s
actions, aligned toward a single goal: saving a life. For me, improvisational comedy and emergency medicine are deeply intertwined. The skills I learned through improv have shaped how I practice medicine—and how I live my life.
I first discovered improv in 2011 during my senior year at Emory University in Atlanta, Georgia. I was on the pre-med track, buried in science coursework, when I took a chance on an improv class with Automatic Improv in Midtown. It felt rebellious. It felt freeing. And it opened up a whole new part of myself. I became more outgoing,
a better communicator, and more comfortable with uncertainty—skills that would prove invaluable later in medicine. I even saw my MyersBriggs personality type shift over time.
When I returned to my hometown of Louisville, Kentucky, for medical school, I worried that I’d have to put all of that aside. But I came to understand that building a life in medicine didn’t mean giving up everything else. It meant finding ways to integrate my passions. I joined a local short-form team, Improv Anonymous, and performed regularly—often on Wednesday
“Emergency medicine often feels like improvised medicine—thinking on your feet, adapting to new information, managing the unexpected.”
nights—while navigating medical school.
As I entered my clinical years, the overlap between improv and medicine became even clearer. Improv improved my bedside manner. I listened more actively, responded more empathetically, and felt more grounded in the moment. Likewise, my clinical experiences informed my improv work, giving me new insights into human emotion, resilience, and vulnerability. Looking back, I realize I’ve done improv in every city I’ve lived in—including a two-day workshop in Madrid, Spain, when I studied abroad between college and medical school. Eventually, I chose to pursue a combined emergency medicine/ internal medicine residency at SUNY Downstate Health Sciences University and Kings County Hospital in Brooklyn, New York. That decision, too, was inspired by my improv training. Emergency medicine often feels like improvised medicine—thinking on your feet, adapting to new information, managing the unexpected. After residency, I completed a geriatric emergency medicine fellowship at NewYork-Presbyterian/Weill Cornell Medical Center. I continued performing and studying improv, completing the Upright Citizens Brigade and Magnet Theater training programs in New York City.
During my fellowship, I became interested in the intersection of improvisational comedy and aging— specifically, how improv could be used to reduce loneliness and social isolation in older adults. Previous studies have shown that improv can improve quality of life for people with Alzheimer’s disease and enhance social connection more broadly.
On Feb. 19, 2025, I had the opportunity to bring these two worlds together. Alongside two fellow improvisers, I led an improv session for residents at the Cobble Hill Health Center in Brooklyn. My goal was to use improv as a tool to foster connection, encourage expression, boost mood, and promote communication—while simply having fun.
We began with introductions and a brief history of improv, tracing its roots back to Viola Spolin, who developed improvisational exercises in Chicago in the 1930s as part of theater education. I reminded participants that none of us wakes up with a script. Every day, we’re improvising in some form.
We opened with a simple mindfulness exercise: deep breaths, followed by an “ahhh.” Then we passed a sound and movement around the circle, following the lead of the person before us. From there, we moved into games designed to spark self-expression. We played “The Awesome Game,” where each person shared something they had done that day, followed by an enthusiastic group response of “Awesome!”
We also adapted the classic improv game “Five Things” into a gratitude version, where participants listed five things they love or are thankful for. Next, we performed “One Voice Interview,” a favorite short-form game where two people speak in perfect unison to answer questions as one character.
The highlight of the day came during our final activity: the “Chair Dance Party.” I created a playlist of familiar songs from the 1960s and ’70s. Residents took turns being the
“chair dance leader,” demonstrating a simple move for the group to copy. When one resident, who typically uses a wheelchair, appeared so energized that she nearly stood up to dance—it felt like witnessing a miracle.
My long-term goal is twofold: to explore whether improvisational comedy can measurably reduce loneliness in older adults, and to create performance opportunities for and by older adults—spaces where they can be seen, heard, and celebrated.
Improvisational comedy has brought me joy, purpose, and resilience. It has made me a better doctor, a more present human being, and a stronger advocate for older adults. I’m committed to continuing this work— and to encouraging others in medicine to find their own form of creative expression, whatever it may be.
Special thanks to Paula Dirkes for sharing her extensive expertise and experience working with older adults.

Dr. Ahmad is a physician in geriatric emergency medicine and internal medicine who divides her time between New York City and Louisville, Kentucky. She began her improv training in Atlanta with Automatic Improv and has since performed with teams in Louisville and New York. She is a graduate of the Upright Citizens Brigade and Magnet Theater conservatory programs and is a member of the improvisational comedy teams Goat Party (@goatpartyimprov) and Halalrious, an all-Muslim improv group. Dr. Ahmad serves as secretary on the executive committee of SAEM’s Academy of Geriatric Emergency Medicine (GEMA). She is passionate about physician wellness and improving the emergency department experience for older adults.

By Milana Boukhman Trounce, MD, MBA
As emergency physicians, we routinely care for patients suffering the downstream effects of their environments. From asthma flares during wildfire season to viral outbreaks amplified by crowded spaces, the emergency department is a mirror of society’s air. Yet for too long, the quality of that air—indoors— has been overlooked in clinical practice and public health policy.
It’s time to change that. Clean indoor air is emerging as a foundational determinant of health— akin to clean water—and emergency medicine has a critical role in advancing this next frontier.
Just as clean water infrastructure reshaped global health by controlling cholera, typhoid, and countless other
waterborne diseases, we now face a parallel opportunity—and obligation— with the air we breathe indoors. People spend more than 90 percent of their time inside. During wildfires, most exposure to outdoor air pollution doesn’t happen outdoors— it happens indoors, through leaky building envelopes and inadequate filtration.
In our clinical practice, we see the toll: surging respiratory complaints, exacerbated chronic disease, and preventable admissions. Yet indoor air remains unmonitored and unregulated in most buildings. This is a public health blind spot we can no longer afford.
A growing body of evidence is reshaping our understanding of respiratory virus transmission. For decades, viruses like influenza
were considered primarily dropletspread. But research now confirms that influenza, RSV, and others can transmit via fine aerosol particles that remain suspended in the air and travel beyond 6 feet.
The COVID-19 pandemic was driven by this airborne route— explaining its rapid and widespread transmission indoors, even without close contact. This insight has lasting relevance. Clean indoor air isn’t just about COVID-19; it has the potential to reduce the burden of seasonal respiratory infections and build long-term resilience— potentially decreasing emergency department visits during annual viral surges.
For emergency medicine, the implications are clear. We manage febrile patients in crowded, often under-ventilated settings. Airborne transmission isn’t theoretical—it

directly impacts both patient care and clinician safety.
At Stanford’s BioSecurity and Pandemic Resilience program, we advocate for a precision emergency medicine model—anticipating risk upstream, not just responding downstream. Clean indoor air fits squarely within this framework. By improving ventilation and filtration, we can reduce exposure to pathogens, fine particulates, and CO₂ buildup, thereby improving clinical outcomes and community resilience.
This isn’t just about protecting against the next pandemic or the next wildfire season. It’s about preventing everyday harms from “normal” air: the kind that increases absenteeism, worsens cardiovascular and pulmonary conditions, and impairs cognition—even in otherwise healthy individuals.
Stanford Forum on Clean Indoor Air
In March 2025, the Stanford Department of Emergency Medicine
co-led a national roundtable on indoor air quality (IAQ), hosted in partnership with Professor Lidia Morawska, co-chair of the World Health Organization’s Air Quality Advisory Committee.
Together, we convened experts across medicine, science, and government to explore performancebased IAQ standards that are both scientifically rigorous and practically achievable.
What made this event unique was that it was rooted in clinical relevance. Emergency physicians helped frame the agenda—not as advocates, but as front-line providers grappling with the real-world consequences of poor indoor air. From the perspective of the ED, we asked: How can we reduce preventable suffering linked to indoor air? How can we define and implement “clean” in a way that’s measurable and meaningful?
Consensus emerged around several key ideas:
• Performance-based standards are essential. Just as we monitor water quality, we need to measure IAQ based on outcomes—CO₂, PM2.5, and air exchange rates—not just design specs.
• Monitoring is foundational. Without real-time data on IAQ, we can’t make informed decisions about health risks in clinical, residential, or public settings.
• Clean indoor air is clinically relevant. It belongs in our differentials, our discharge planning, and our thinking about prevention.
Emergency medicine sits at the intersection of acute care, public health, and disaster response. We are the first to see patterns—of worsening COPD during fire season, of viral surges in poorly ventilated long-term care facilities, of fatigue and confusion in children exposed to CO₂rich classrooms.
Recognizing the role of indoor air empowers us to intervene more effectively. It informs patient education (“crack a window,” “use a
HEPA filter,” “avoid recirculated air when sick”), shapes facility design, and supports clinician safety. We don’t need to wait for a new building code to act—we can start with awareness, measurement, and small, evidencebased improvements in our clinical environments.
As medicine evolves, so too must our understanding of environmental exposures. Just as we now screen for social determinants of health, we must begin to consider physical determinants—like the air patients live, work, and heal in.
Emergency medicine has always adapted rapidly to emerging threats. The challenge of indoor air is no different. It’s time we see it not as an engineering issue or a facilities problem, but as a clinical parameter we can influence.
Clean indoor air should be treated the way we treat clean water: as a baseline infrastructure requirement for health. We don’t wait for waterborne illness to act—we monitor, regulate, and safeguard water quality because the risk is invisible but consequential. Indoor air deserves the same vigilance.
We already take proactive measures in other areas of emergency and disaster medicine—securing medications to prevent overdose, locking up firearms to reduce accidental injury, creating surge protocols to anticipate crises before they overwhelm. Clean indoor air is no different: it is a preventable hazard and a resilience multiplier.
Clean indoor air is the next chapter. Emergency medicine should help write it.

Dr. Boukhman Trounce is a clinical professor of emergency medicine at Stanford, where she leads the biosecurity and pandemic resilience program. She has taught hundreds of Stanford students and emergency medicine residents through this program over the past decade. Dr. Boukhman Trounce is a fellow of Stanford’s Center for Innovation in Global Health.
By Eve Ameen, MD and Fahmida Patwari, MD
In the winter of 2024, I spent two weeks rotating in the emergency department (ED) of a tertiary care hospital in Mwanza, Tanzania, a medium-sized city on the shores of Lake Victoria. As anyone who has participated in a global health elective can attest, the experience was profoundly rewarding as a young doctor, both personally and professionally. I was especially struck by the contrast in medical practice and clinical decision-making compared with what I had grown accustomed to during residency training at a large, urban, academic hospital in New York City.
In the United States, I’ve become used to a system where advanced diagnostics and rigorous protocols govern clinical decisions. In Tanzania, by contrast, I saw how
clinicians navigate similar scenarios with limited resources, relying more on clinical judgment and cultural context. I was particularly impressed by the approach to brain death — specifically two cases interpreted and managed very differently in each setting.
The first case, during my medical intensive care unit (MICU) rotation in New York, involved a previously healthy woman in her 50s who was found unresponsive at work. She arrived at the emergency department, was promptly intubated, and a computed tomography (CT) scan revealed a large subarachnoid hemorrhage. Upon admission to the MICU, she was declared clinically brain dead by the neurology team. However, per hospital policy, she could not be formally pronounced
dead without a confirmatory study — either an apnea test or a nuclear brain scan. Neither was feasible due to her hemodynamic instability and the logistical impossibility of transporting her out of the unit.
Despite repeated family meetings with palliative care, neurology, neurosurgery and the MICU team, her family could not accept the devastating prognosis and requested continued aggressive interventions. As a result, she remained in the MICU on full life support for weeks as her condition visibly deteriorated. Skin breakdown and early decomposition occurred — a deeply distressing experience for both staff and family. Eventually, she coded and died, but only after weeks of unnecessarily prolonging a life that had already ended.

“In the United States, our protocols reflect a fear of legal repercussions and a reliance on technology — sometimes to the point of paralysis. Death is often medicalized and delayed; families, providers and institutions struggle with ambiguity and liability.”
In contrast, while in the emergency department in Mwanza, I witnessed the management of a young man in his 20s who had suffered a motorcycle accident while unhelmeted — a common occurrence in a region where traffic rules are lax and torrential rainfall is frequent. He arrived already intubated by paramedics, obtunded and without meaningful neurological activity. He was placed on one of the department’s two functioning ventilators. Shortly after his arrival, the on-call neurosurgeon performed a bedside brain death exam and declared the patient dead based on clinical findings alone. No imaging was obtained. His clinical management was swift, definitive and culturally appropriate. His body was immediately released to the family for funeral arrangements.
These two cases reflect more than just differences in resources
— they highlight a broader tension between systemic rigidity and clinical pragmatism, particularly in how we frame and approach death. In New York, our protocols reflect a fear of legal repercussions and a reliance on technology — sometimes to the point of paralysis. Death is often medicalized and delayed; families, providers and institutions struggle with ambiguity and liability. In Mwanza, limited resources necessitate decisive clinical judgment, with trust placed in the clinician over the machine. Death was treated more as a fact of life — not any less tragic, but less obscured by machinery and policy.
These experiences challenged my assumptions about what good care looks like. While I value the thoroughness of American medicine, I came to respect the decisiveness and humanity embedded in Tanzanian
practice. As I continue my training, I hope to carry forward a more nuanced view of clinical decision-making — one that honors both scientific rigor and the reality of the moment

Dr. Ameen is a PGY-3 in emergency medicine at Mount Sinai Morningside-West in New York City. She has a strong interest in global health and, in addition to attending a global health elective in Tanzania in November 2024, serves as the resident director of the global health pathway, which increases education and discussion of global health topics across the Mount Sinai health system.

Dr. Patwari graduated from Downstate College of Medicine in 2022 and is currently a PGY-3 in emergency medicine at Mount Sinai Morningside-West. She is interested in global emergency care, burden of disease and resource limitations within health systems.

By Abdoulie Gaye, DO
Like the average emergency physician, my day shifts often begin with an essential, common procedure: making a cup of coffee. That didn’t change when I arrived at Edward Francis Small Teaching Hospital (EFSTH) in Banjul, The Gambia. As I stepped into a small café across from the hospital on my first morning, an elderly woman followed behind me, gently speaking in Mandinka and holding out a prescription slip. She asked for help purchasing her medication. “How much?” I inquired. “One hundred
and fifty dalasis,” she replied—about two U.S. dollars at the time. I helped without much thought and then began my shift.
Days later, that brief exchange resurfaced in my mind—not just as an act of kindness, but as a glimpse into the broader realities of healthcare in The Gambia.
The Gambia is the smallest country on mainland Africa. It remains one of the world’s poorest nations. Nearly one-third of its population survives on less than $1.25 a day, according to United Nations data. Access to acute and emergency care is
limited, and infrastructure is strained. EFSTH is one of only two emergency departments in the entire country. Inside, the overcrowded emergency ward reflects the weight of that burden: critically ill patients lie on mattresses beside standard hospital beds, resources are stretched thin, and essential imaging technologies such as computed tomography (CT), magnetic resonance imaging (MRI), and even ultrasound are scarce or altogether absent.
X-ray imaging is the only consistently available modality. Patients requiring a CT scan must be transported—often at great

cost and delay—to a private clinic about 20 minutes away. Advanced imaging options like MRI are entirely inaccessible. In this context, pointof-care ultrasound (POCUS) has the potential to be a diagnostic game changer.
POCUS: Revolutionizing Diagnostic Care in Low-Resource Settings
Point-of-care ultrasound has revolutionized clinical care worldwide over the past decade. In low-income countries, it fills a critical gap where conventional radiology services are lacking. The World Health Organization estimates that two-thirds of the global population lacks access to basic diagnostic imaging and explicitly recommends ultrasound as a
tool to address this disparity. Studies across low- and middle-income countries (LMICs) consistently show that bedside ultrasound significantly alters diagnosis and management in acute care settings.
Despite its promise, the use of POCUS in The Gambia remains limited. Even at tertiary centers like EFSTH, patients may wait hours or days for a formal ultrasound—often without success. POCUS offers a real-time, accessible solution—one that can expedite diagnosis and management when time is of the essence.
To illustrate the impact of POCUS in this setting, consider the following cases from my time in The Gambia:
Case 1: A Missed Hernia, Caught in Time

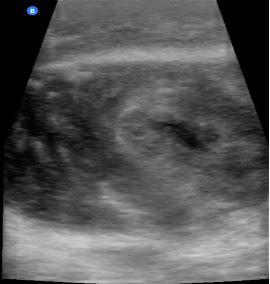
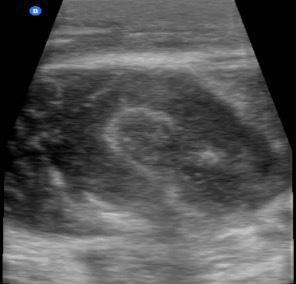
A 38-year-old man presented with a painful lower abdominal mass that had gradually enlarged over three weeks. He was otherwise healthy and hemodynamically stable but had a rapid heartbeat (tachycardic). The mass, located just above the pubic bone and extending into the left
on Page 53
“Point-of-care
resource-limited
“Without ultrasound delayed or missed complications
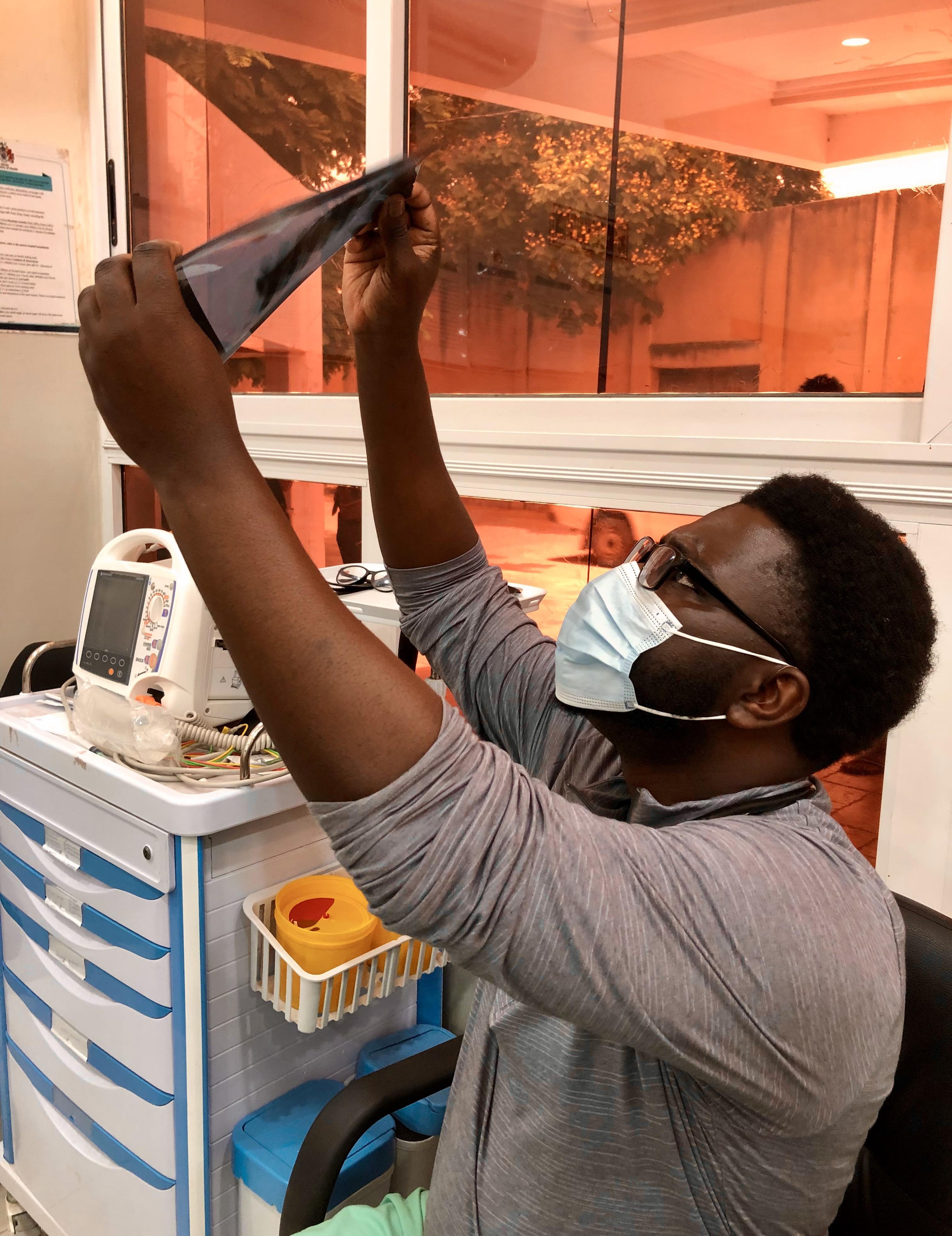
continued from Page 51
groin area, measured roughly 5 by 6 centimeters. It was tender but showed no redness of the skin. Clinical concerns included possibilities such as an abdominal wall abscess, incarcerated hernia, or neoplastic lesion.
Given the absence of timely formal imaging, the surgical team requested that I perform a bedside ultrasound. A focused POCUS exam revealed loops of bowel within the mass, actively moving—findings consistent with an incarcerated abdominal wall hernia. The patient was promptly scheduled for surgical repair the same day, averting potential complications such as strangulation or perforation.



In another case, a 26-year-old man with a history of peptic ulcer disease returned to the emergency department with worsening pain in the upper middle abdomen (epigastric pain). He had been seen two days earlier with similar symptoms and was treated symptomatically due to a presumed ulcer flare. At that time, diagnostic imaging was considered but unavailable. On this return visit, his rapid heartbeat and localized tenderness raised new concerns. POCUS was performed at the bedside: gallbladder
“Point-of-care ultrasound is more than a diagnostic aid—it’s a clinical equalizer in resource-limited environments where every minute and every decision counts.” ultrasound
at
the bedside, diagnoses may be missed altogether, potentially leading to serious complications such as tissue death or systemic infection.”
findings were unremarkable, but a scan of the pancreas revealed fluid around the gland and enlargement— features consistent with acute pancreatitis. The patient was admitted for appropriate management.
Without ultrasound at the bedside, this diagnosis might have been delayed or missed altogether, potentially leading to serious complications such as tissue death (necrosis) or systemic infection (sepsis).
In resource-limited environments like The Gambia, POCUS is more than a diagnostic aid—it’s a clinical equalizer. Its ability to provide immediate, actionable information at the bedside is invaluable in settings where every minute and every decision counts.
To fully realize the potential of POCUS in The Gambia, sustained investment is needed—not only in devices but also in clinician training, mentorship, and systems integration. Building local capacity will help ensure continuity, reduce diagnostic delays, and ultimately improve patient outcomes.
In conclusion, these cases underscore how point-of-care ultrasound can transform emergency care in the most resource-constrained settings. When integrated thoughtfully and supported sustainably, POCUS has the power to bridge the gap between limited resources and high-quality care.

Dr. Gaye is a third-year emergency medicine resident at Cleveland Clinic Akron General in Akron, Ohio.

By Loraine Ochoa
Digital health, also known as telehealth, was established in the 1960s with the introduction of the first electronic medical record system, PROMIS, by Dr. Lawrence L. Weed. Over the years, continuous advancements in technology have led to the development of wearable devices, remote monitoring systems and telemedicine platforms. The COVID-19 pandemic in 2020 accelerated the adoption of telehealth services. This shift emphasized the importance of digital health in providing accessible and sustainable health care.
Shortly thereafter, in 2021, the health care industry began adapting to the metaverse phenomenon. The metaverse is a persistent, shared virtual world where users can interact with each other and their surroundings in a more immersive and collaborative way than in traditional online environments. It involves creating and exploring real-time digital environments that mimic or extend real-world spaces, often using artificial intelligence, augmented reality (AR) and virtual reality (VR). AR enhances human perception or adds new functions to real-world environments through digital stimuli, whereas VR creates
a fully simulated environment separate from physical reality. While the metaverse is often associated with entertainment and gaming, its potential has expanded to influence economic, cultural and, more recently, health care industries.
With its immersive and interactive capabilities, the metaverse has begun to redefine emergency medicine by overcoming geographical barriers and enhancing the efficiency and speed of medical interventions. Although research on the metaverse in emergency medicine is still limited, studies
“The metaverse is influencing various aspects of emergency medicine — from creating real-time simulations for clinical training to supporting triage in disaster scenarios and aiding treatment and administrative processes.”
have identified its application in four key domains: education, prehospital and disaster medicine, diagnosis and treatment, and administrative affairs.
Simulated training environments using AR provide valuable tools for training emergency responders, allowing them to refine their skills without realworld consequences in high-pressure scenarios. Procedures such as central line insertion, airway management and ultrasound interpretation are commonly practiced using AR. Both AR and VR are also employed in cardiopulmonary resuscitation (CPR) training and pediatric septic shock simulations, offering trainees a level of realism and immersion not achievable with traditional methods. In critical care education, VR-based training for conditions like diabetic ketoacidosis and status epilepticus has been shown to improve response times and team coordination during emergencies.
The use of AR-enabled smart glasses during mass casualty incidents has enhanced triage decision-making and accelerated care delivery. VR simulations allow medical providers to regularly train for chaotic and infrequent events such as mass disasters, creating realistic scenarios while reducing the cost of otherwise resource-intensive training. VR has also been used in prehospital settings to assess CPR quality during ambulance transport. These studies have shown, for example, that compression depth is often reduced during speed bumps or abrupt stops.
AR-based assistive tools have been used in complex pediatric emergencies to aid in size estimation and accurate drug dosage calculations (for example, amiodarone). AR smart glasses have also assisted in assessing brain concussions through cephalic accelerometry. VR interventions have been explored for treating conditions such as schizophrenia and autism. In pediatric emergency departments, VR has been used to alleviate needlerelated pain and anxiety.
This domain remains underexplored, with only four studies identified to date. However, VR-based programs have been used to evaluate emergency medicine applicants, providing deeper insights compared with traditional interviews. Additionally, VR simulations of emergency departments have been employed to study patient flow, quality of care and safety in overcrowded conditions.
While the metaverse presents promising advancements in emergency medicine, it also raises legal and ethical concerns. Key issues include patient privacy and data security, with potential risks such as data breaches and unauthorized access in virtual health care environments. Another major concern is the ambiguous allocation of responsibility for adverse events involving metaverse technologies. This highlights the need for clear legal
and accountability frameworks.
To address these challenges, proposed strategies include:
• Enforcing strong cybersecurity protocols in virtual health care systems
• Ensuring clear communication during informed consent processes in metaverse-based interventions
• Fostering collaboration between health care providers and legal experts to develop standards for liability and accountability
Conclusion
The metaverse is influencing various aspects of emergency medicine — from creating real-time simulations for clinical training to supporting triage in disaster scenarios and aiding treatment and administrative processes. As these technologies continue to evolve, they will bring new opportunities and innovations to the field. However, it is equally important to acknowledge the limitations and risks associated with metaverse use in patient care. To fully realize its potential, the medical community must work toward establishing standardized regulations and guidelines that ensure safety, privacy and accountability.

Ochoa is a fourth-year medical student at Robert Wood Johnson Medical School in New Jersey. She served as a medical student ambassador at this year's SAEM annual conference.

By Christopher Awad, MD, MBA; Michael Makutonin; Moira Smith, MD, MPH; Joshua Joseph, MD, MS, MBE; Adrian D. Haimovich, MD, PhD; and Arwen Declan, MD, PhD on behalf of the SAEM Informatics, Data Science & Artificial Intelligence Interest Group
Let me guess—you were on shift, ordering antibiotics for a septic patient, when the alert popped up for the fifth time, forcing you to confirm something you already confirmed three screens ago. You sighed dramatically, clicked through it, and thought, “There has to be a better way.”
Welcome to the possibility of informatics.
Whether you are tech-curious, workflow-frustrated, or genuinely excited about SlicerDicer, clinical informatics (CI) might just be your calling. But how do you turn that interest into a fellowship application? What are programs looking for? And,
most importantly, do you really have to learn to code?
Fear not. This article breaks down the realities—and myths—of applying to CI fellowships. We've gathered wisdom from leaders of the SAEM Informatics, Data Science & Artificial Intelligence Interest Group and borrowed insights from an Emergency Medicine Residents’ Association (EMRA) panel — so let’s dive in.
Why Fellowship?
First, let's address the elephant in the server room: Do you need a CI fellowship to work in informatics?
Now that the CI practice pathway is closing, if you’re aiming to
lead operational change at the institutional level, yes—fellowship is highly recommended. A CI fellowship provides a degree (often an MPH or MS) and more; it includes structured exposure to workflows, leadership training, and a deep dive into how healthcare technology is developed, deployed, and governed. As Dr. Moira Smith says: “Informatics opened up a lot of doors... it was empowering to find ways to solve operational problems instead of throwing your hands up.”
Spoiler: It’s not a GitHub portfolio, a black hoodie, or a Python terminal.
“Understanding how people use systems is more valuable than writing the next machine-learning algorithm from scratch. Your main superpower is asking the right questions—and building solutions people will actually use.” — Dr. Adrian D. Haimovich
Programs want:
• Commitment
• Curiosity
• Collaboration
• Experience in quality improvement or informatics
“We want people who are interested in solving problems, not just smart people taking a break,” said Dr. Jeff Nielson.
You don’t need a formal program at your residency site to start building your informatics street cred. Start small, whether your residency site has a CI fellowship or not:
• Attend an informatics interest group meeting or an American Medical Informatics Association (AMIA) webinar
• Identify a small, annoying workflow problem and propose a fix
• Build a dot phrase—a shortcut text expansion commonly used in electronic health records
• Volunteer on a quality improvement committee
Pro tip: Don’t open with, “I want to use AI to revolutionize clinical care.” Instead, try, “Can we auto-populate the chief complaint field to avoid thirty redundant clicks?” Start with problems you’ve seen—and better yet, bring a solution. The experience and satisfaction you get solving small problems will help you tackle the big ones.
“There’s always someone doing informatics at your hospital,” one EMRA panelist noted. “You just have to find them.”

So... Do I Need to Learn to Code?
Nope. Not at first. Coding helps, sure—but most informaticists are not full-time developers.
Dr. Haimovich gave us the golden ratio: “Informatics is 20% technical and 80% sociology.” Translation? Understanding how people use systems is more valuable than writing the next machine-learning algorithm from scratch.
Sure, learn basic SQL. But remember—your main superpower is asking the right questions—and building solutions people will actually use. Do not worry about coding: informatics, like emergency medicine, is a team sport, and thinking about clinical problems you’ve experienced is already a huge contribution.
The Shape of a Career in Informatics Myth: Informatics careers are onesize-fits-all.
Fellowship opens multiple doors: operations, education, startups, research. Dr. Smith noted that flexibility is the field’s biggest strength—all her co-fellows’ career paths varied dramatically.
You can be the builder, the visionary, the translator between clinical and technology teams. You can stay rooted in emergency medicine or expand into enterprise leadership. The point is: there’s room to shape your path.
Why Informatics Now?
Generative AI. Machine learning. Predictive models. Large language models that summarize patient charts faster than a seasoned intern.
We’re at a critical moment. And as Dr. Haimovich said, “Whether right or wrong, it’s coming.”
“A clinical Health or workflows, leadership

informatics fellowship provides a degree—often a Master of Public or Master of Science—and more; it includes structured exposure to leadership
training,
and a deep dive into how healthcare technology is developed, deployed, and governed.” — Dr. Moira Smith
continued from Page 57
That’s why it’s more important than ever for clinicians to lead this evolution—to guide it ethically, thoughtfully, and with patients at the center. Informatics is how we ensure that the tools being built for us are also built with us.
Final Takeaways (i.e. Your Fellowship To-Do List):
• Join SAEM’s Informatics, Data Science & Artificial Intelligence Interest Group
• Visit AMIA webinars
• Find a small workflow issue and solve it
• Find an informatician at your institution
• Document your work—even small projects count
• Look for opportunities to learn basic SQL or electronic health record (EHR) data structures (optional but helpful)
And if you’re feeling overwhelmed, just remember:
“Informatics empowers you to fix the future — not just live in it.” (Anon)
Now go forth and click wisely. Your fellowship application is waiting.

Clinical informatics fellowships vary widely in emphasis and opportunities. We sat down with Dr. Jeff Nielson, program director of the Kettering Health (Soin) Clinical Informatics Fellowship, Dayton, Ohio, to learn what makes his program unique.
Dr. Nielson explained that the current fellowship model offers a significant degree of flexibility, allowing fellows to develop individual areas of expertise while still covering the full breadth of the core clinical informatics curriculum. He emphasized his enjoyment in customizing learning experiences to match each fellow’s unique interests.
Dr. Nielson was also particularly enthusiastic about the program’s on-site masseuse, available to fellows for one appointment per week. Equally important to him is the appeal of Dayton itself, which he described as a beautiful city with a low cost of living, a familyfriendly environment, and a rich cultural scene.





Dr. Awad is a resident and researcher in the department of emergency medicine at The Ohio State University. He leads data and technology projects that help evolve our understanding of patients, providers, and the complex relationships within healthcare networks.
Dr. Makutonin is a resident and researcher at Yale, where he has led data science projects on decision support, patient boarding, and other fixable issues. He is passionate about using data science research to inform and solve clinical problems.
Dr. Smith is the assistant emergency medicine informatics director at the University of Virginia. Her work focuses on data analytics and reporting, quality improvement, electronic health record usability and workflow, and clinical decision support.
Dr. Joseph is an assistant professor of emergency medicine at Harvard Medical School and the medical director for enterprise emergency medicine analytics at Mass General Brigham. His research focuses on leveraging artificial intelligence to improve operations and triage.
Dr. Haimovich is assistant professor of emergency medicine at Harvard Medical School and director of geriatric emergency medicine at Beth Israel Deaconess Medical Center.
Dr. Declan is the assistant research director at Prisma Health Upstate and clinical assistant professor at the University of South Carolina School of Medicine - Greenville & Clemson University.

By Nicholas Stark, MD, MBA, Joe Gannett, MD, Moira E. Smith, MD, MPH, and Brandon
Allen, MD, on behalf of the SAEM Innovation Interest Group, the SAEM ED Administration and Clinical Operations Committee, and the SAEM Informatics, Data Science, & AI Interest Group
At SAEM25 in Philadelphia, a packed audience gathered for a dynamic didactic session, “The Future Is Now: Impacts of AI on Emergency Department Operations.” Cosponsored by the SAEM Innovation Interest Group, the ED Administration and Clinical Operations Committee, and the Informatics, Data Science & AI Interest Group, the panel brought together leaders at the forefront of clinical operations and artificial intelligence integration into emergency care.
Panelists included Dr. Joe Gannett, hospital flow lead at LA General; Dr.
Ben Slovis, chief medical information officer at Temple University; Dr. Alan Cherney, emergency department medical director at Jefferson Health; and Rebecca Urban, vice president of operations at Jefferson Health. Their insights went beyond hype into the operational realities, pitfalls, and potential of AI tools as they pertain to operations and flow.
Opening the session, the panel focused on a foundational question: What does success in ED operations actually mean — and what should AI be building toward?
“For me, it's about quality, safety and efficiency. We're here to take better care of more patients — and AI should make that easier,” said Dr. Gannett.
The panelists emphasized that AI should be building toward a future where burdensome clerical tasks are minimized, workflows are streamlined, and frontline teams are freed to focus on patient care. They painted a clear picture of AI’s emerging role as a strategic co-pilot in clinical operations.
For example, Dr. Cherney and Urban shared how predictive models
“Artificial intelligence should be building toward a future where burdensome clerical tasks are minimized, workflows are streamlined, and frontline teams are freed to focus on patient care.”
at Jefferson Health have directly improved patient flow and transitional care, including cutting multi-hour ED transfer delays by nearly half. These models allowed them to simulate the real-time impact of new staffing or discharge strategies before implementation, providing powerful foresight for operational decisions. Those wins weren’t theoretical — they translated into safer, faster care and stronger business cases for investing in additional staff and tools.
“We were already on the cusp of scaling a solid transfer process,” Urban said. “But the modeling helped push it over the edge by showing it could work — and that it was working.”
Even at institutions where AI has gained traction, the road has been
anything but linear. Panelists shared candid reflections on early missteps and resistance.
Dr. Slovis described efforts at Temple to evaluate diabetes management algorithms, which initially met strong resistance from clinicians confident in their own workflows. “But when the data showed significant outcome improvements — especially among the loudest critics — that changed the conversation,” he noted.
This tension between clinical autonomy and algorithmic guidance remains a real barrier. The panelists reinforced that AI must be framed not as a verdict, but as supportive infrastructure offering recommendations, not commands.
As AI tools are integrated, they don’t just optimize throughput — they reshape the way people work. Dr. Gannett emphasized that AI cannot succeed without thoughtful change management and recognition of how tools alter team dynamics.
“People need to trust that these tools won’t replace them,” he said. “They need to know where the data is coming from and what the end goal is.”
Engaging frontline staff — nurses, techs, residents and attendings — is essential. Dr. Cherney noted the importance of removing emotion from
“No matter how advanced the algorithm, utility. Garbage in, garbage out remains

continued from Page 61
contentious discussions by using data to drive consensus. “Once you take out the emotion and just show what the numbers say, it’s easier to build buy-in,” he said.
If there’s one recurring truth about AI, it’s this: garbage in, garbage out. No matter how advanced the algorithm, flawed or inconsistent data will derail its utility. Dr. Slovis and others spoke candidly about the foundational role of data integrity and the operational risk of building AI on unstable ground.
At Temple, something as seemingly straightforward as “onset time” revealed deep cracks. Multiple versions of the same variable existed in the electronic health record, inconsistently documented and poorly understood by end users. “We thought we had solid data,” Slovis said. “But we realized we didn’t even know which variable was actually being used in practice.”
This challenge isn’t unique to any one system — it’s widespread and largely unaddressed by formal standards. While regulatory discussions are increasing, there is still no universal framework guiding how health systems should define, validate and monitor the data feeding AI models. The panel underscored the urgent need for governance structures that mirror the rigor of clinical quality improvement programs.
How do we move forward? The path includes robust AI governance structures with multidisciplinary representation, clinician-in-the-loop oversight to validate model inputs and outputs, and relentless attention to terminology, validation and stakeholder alignment.
When it comes to securing resources, panelists stressed the importance of telling the right story to the right audience.
Gannett urged physicians to model the operational impact of new resources — whether a second CT scanner or a new analyst — then show how it pays off in both patient care and system efficiency. “That kind of proof — local, real and financially clear — is how you win over leadership,” he said.
Urban added that crossdepartmental alignment adds strength to the case: “When the same message comes from multiple areas — ED, hospital medicine and more — it stops being an ‘ED project’ and becomes an enterprise priority.”
The session ended with a forwardlooking discussion: Where is AI in emergency medicine going in the next five years?
Panelists agreed on several themes:
• Ambient AI — which runs in the background without active input — can help capture clinical encounters in real time, ultimately reducing aftershift charting and allowing clinicians to stay focused on patient care.
• Locally trained models will improve relevance, reduce bias and enhance trust.
• Advanced natural language processing will turn free text into structured data, making predictive tools both more precise and userfriendly.
• AI-driven video and sensor systems may help prevent workplace violence and detect clinical deterioration earlier.
algorithm, flawed or inconsistent data will derail its a fundamental truth for artificial intelligence.”
• Equity-focused applications, such as real-time interpretation and literacy-aware communication tools, could reshape how we connect with underserved patients.
To help get there, panelists recommended that clinical leaders:
• Start small. Prove impact, then scale.
• Build governance that spans clinical, technical and equity perspectives.
• Don’t chase shiny tools — solve real problems.
Above all, don’t sit on the sidelines. AI is arriving in emergency departments whether we’re ready or not. The opportunity — and responsibility — lies in shaping it for the better.
Disclosure: AI was utilized to review audio transcripts and guide structure development for this article. Article content was largely created and heavily revised by the authors.

Dr. Stark serves as chair of emergency medicine and director of the Acute Care Innovation Center at Mercy Medical Center Merced. He is also assistant director of the UCSF Acute Care Innovation Center and co-founder of the Emergency Medicine Innovation Collaborative.

Dr. Gannett is assistant medical director of patient flow at LA General and co-director of both the Health System Leader Fellowship and the Health Administration Scholars Program, leading hospital-wide efforts to improve capacity, throughput and care coordination.

Dr. Smith is assistant emergency medicine informatics director and director of digital clinical workflows at the University of Virginia. Her work focuses on data analytics and reporting, quality improvement, electronic health record usability and workflow, and clinical decision support.
Dr. Allen is an associate professor of emergency medicine at UF Health, serving as administrative fellowship director and medical director of the Clinical Decision Unit and Chest Pain Center. His interests include clinical decision-making and quality improvement. He also holds an affiliate role in psychiatry and cardiology.

By Hannah Mishkin, MD, MS; Wan-Tsu Wendy Chang, MD; Lindsay MacConaghy, MD; Neha Raukar, MD, MS; Wendy Sun, MD; and Laura Walker, MD, MBA, on behalf of the Academy for Women in Academic Emergency Medicine
Academic emergency medicine is no stranger to the challenges of time scarcity, unpaid labor, and persistent gender disparities. Women in medicine, in particular, are often held back by invisible work and institutional inertia, resulting in slower promotions, fewer opportunities, and disproportionate burdens. But a new tool has emerged that may help level the playing field.
At SAEM 2025, several sessions focused on the use of artificial intelligence (AI) in emergency medicine. If you missed the AWAEM/Informatics co-sponsored didactic, this article summarizes key
applications for career development. Specifically, it explores how large language models (LLMs) can reduce inefficiencies, support leadership development, and mitigate disparities in academic emergency medicine. As these tools grow in capability, they offer both practical advantages and ethical considerations that academic leaders must now address.
The Problem: Gender Inequity and Invisible Labor
Research shows that women in academic medicine are promoted more slowly than men. The reasons are multifaceted: childcare
responsibilities, caregiving demands, and a disproportionate load of "invisible" work—committee service, mentoring, curriculum development, and event planning—much of which goes unrewarded in promotion metrics.
Women are also less likely to receive institutional mentorship and sponsorship and more likely to invest in external coaching. Timeintensive tasks like writing letters of recommendation, drafting promotion packets, and planning departmental events siphon energy from scholarly activities and leadership opportunities.

“Artificial intelligence is not a silver bullet, but for academic emergency medicine—and especially for women disproportionately burdened by invisible labor—large language models can be a lever for equity.”
LLMs are AI systems trained on vast text datasets, capable of generating human-like content in response to natural language prompts. In academic settings, they can serve as digital administrative assistants, streamlining repetitive tasks and freeing up time for high-impact work. They can also act as digital executive coaches, decreasing barriers to access and facilitating self-reflection.
The evolution of AI—from foundational theory in the 1950s, through machine learning and deep
learning in the 1980s and 2010s, to today’s generative AI—has finally produced tools accessible enough for busy clinicians and educators to use in their daily workflow.
Practical Strategies: Using AI to Reclaim Time
1. Administrative and Educational Tasks
• Email drafting: AI can generate concise, professional emails in seconds—ideal for coordinating shifts, meetings or follow-ups.
• Document creation: LLMs draft objectives, evaluations, and program materials using structured prompts and templates.
• Real-time teaching: Tools like Perplexity summarize current literature at the bedside, aiding evidence-based teaching on the fly.
• Difficult conversations: Simulated dialogues help faculty prepare scripts for professionalism feedback or resident coaching.
• Lecture prep: LLMs assist in creating outlines, slides, and learning objectives—offering a launchpad, not a final product.

• Data handling: AI scripts (e.g., in Python or R) expedite data cleaning and formatting, though human oversight remains crucial.
• Journal selection: LLMs suggest target journals and help draft cover letters, reducing submission friction.
• Writing support: While LLMs should never write manuscripts, they help with grammar, tone, and formatting— always with careful review and appropriate disclosure.
3. Career Development
• Evaluations and letters: AI assists with peer and trainee evaluations and can help draft tailored, accomplishment-based recommendation letters.
• Bias reduction: Omit gender and pronouns to prevent perpetuating gendered language patterns common in AI-generated text.
• Post-processing: Tools like Grammarly or Hemingway enhance the clarity and polish of AI-generated drafts.
4. Personal and Operational Support
• Task management: AI helps with daily planning, prioritization and even wellness check-ins.
• Mentorship documentation: Automate tracking of meetings, goals, and action items.
• Policy drafts: Draft contracts or policy outlines. (Caution: AI tools are not substitutes for legal counsel.)
Best Practices for Prompting AI Treat LLMs as intelligent assistants that thrive on clarity. According to Microsoft’s best practices, an effective prompt includes:
• Persona: Define the AI’s role (e.g., “You are a program director…”).
• Objective: State the task clearly.
• Audience: Indicate who will read or use the output.
• Context: Provide background or relevant text.
• Boundaries: Limit length, tone and format expectations.
Always review, refine, and personalize AI outputs—and be cautious about entering confidential or proprietary data, especially in public versions.
Ethics, Equity and Evolving Norms As AI becomes ubiquitous, institutions must develop clear policies around privacy, disclosure, and appropriate use. The line between assistance and authorship is increasingly blurry— should AI assistance be disclosed in letters of recommendation? What about research manuscripts?
Bias remains a risk. Both humanand AI-generated text may reflect gender and cultural stereotypes. We must be proactive in mitigating bias, particularly when drafting evaluations and narratives that influence careers.
The reliance on templated, AIgenerated language may also dilute the value of traditional academic artifacts like letters of recommendation. As these tools proliferate, academia must reconsider how best to signal excellence and potential in ways that are human, authentic and equitable.
1. Clarify institutional guidelines: Understand your institution’s policy on AI and LLM use—especially regarding sensitive data.
2. Refine your prompts: Practice crafting detailed, effective prompts tailored to your academic needs.
3. Vet and personalize: Always factcheck and adjust AI output to suit your tone, audience and context.
4. Advocate for policy development: Encourage your department or institution to create ethical, clear policies around AI use.
5. Invest in education: Organize training sessions to help faculty and staff use AI tools effectively and responsibly.
AI is not a silver bullet, but for academic emergency medicine— and especially for women disproportionately burdened by invisible labor—LLMs can be a lever for equity. When used thoughtfully, these tools help reclaim time,
accelerate career advancement, and shift focus back to the work that matters most: mentoring, leading, discovering and caring.
Disclosure: The authors utilized AI-based tools to help refine the language and structure of this article. We have no financial interests or affiliations with any of these services.



Dr. Mishkin is the emergency medicine residency program director at Reading Hospital, Tower Health, in West Reading, Pennsylvania. Her academic areas of focus include innovation in medical education and administration, and diversity, equity, and inclusion.
Dr. Chang is an associate professor of emergency medicine at the University of Maryland. Her professional focus is on medical education and the management of neurologic emergencies.
Dr. MacConaghy is an assistant professor of emergency medicine at Geisinger Commonwealth School of Medicine and serves as the assistant residency program director at Guthrie Robert Packer Hospital in Sayre, Pennsylvania. Her professional focus includes advancing medical education and residency training.



Dr. Raukar is an associate professor and vice chair for academic advancement and faculty development at Mayo Clinic Rochester. Her research emphasizes life-threatening injuries in athletes, innovations in emergency medicine, and faculty and leadership development.
Dr. Sun is an administration fellow at Yale School of Medicine. She has a passion for clinical operations, patient quality and safety, and health innovation.
Dr. Walker is an assistant professor of emergency medicine at Mayo Clinic. She is a leader in emergency medicine and hospital operations, focusing on health systems, equity, and quality improvement. Her research focuses on improving healthcare systems and promoting effective management practices within emergency medicine.

By Jeremy Brown, MD
In the past, we took a close look at the NIH study sections. These are committees that review all the proposals for funding, and are made up entirely of non-NIH experts. These reviewers usually come from universities, though occasionally they may be drawn from industry or patient or disease advocacy organizations. As a reminder, there are a couple of hundred standing study sections, who membership is publicly available, and they review most of the investigator-initiated proposals. The Center for Scientific Review (CSR) convenes most of these study sections, and reviews about three-quarters of all the proposals submitted to the NIH –
about 66,000 per year. In addition, there are Special Emphasis Panels (SEPs), which review applications on special topics.
Many of these SEPs were convened by the twenty-three NIH Institutes rather than by the Center for Scientific Review. So, for example, all neurological clinical trials that were submitted to the National Institute for Neurological Disorders and Stroke (NINDS) were reviewed by a study section convened by that Institute, rather than by the CSR. Other than that, these study sections are identical to those convened by the CSR; they are made up of outside expert peer reviewers, who have no conflicts of interest and who produce detailed summary statements.
In March of this year, the NIH announced that in the future, only the CSR would convene study sections. Most of the employees of the various institutes who were involved in setting up the special panels have been transferred to the CSR, from where they will continue their work. By centralizing all reviews at the CSR alone, the NIH predicted savings of over $60 million per year.
What does this mean for those of you submitting grant proposals? Is there anything different that you need to do, or might expect from the review? The only difference is what happens behind the scenes; for investigators, there will be the same high quality peer reviews, and the changes at NIH will likely be

invisible. It is possible that a very small number of sections may be combined or eliminated, and the experts at the CSR will continue to guide any reviewer with questions about where to submit a proposal.
When you submit a proposal to the NIH you can (and should) request that it be reviewed by a particular study section, one that seems to you to be the best scientific fit. In addition, you can always request that a reviewer with appropriate expertise be added to the existing section as an ad hoc member (but you cannot request a specific named individual).
This ensures that your proposal receives the most appropriate review, and wherever possible, the CSR will honor your request.
One easy way to find out which study section might be the best fit for your proposal is to use the Matchmaker function on the NIH RePorter website. Just type in your abstract, or some key terms from your work, and Matchmaker will suggest the best program official, institute and study section to review your proposal. It really is as simple as that.

Dr. Brown is the director of the Office of Emergency Care Research (OECR) where he leads efforts to coordinate emergency care research funding opportunities across NIH. Additionally, Jeremy is the primary contact for the NINDS Exploratory and Efficacy FOAs and serves as NIH's representative in government-wide efforts to improve emergency care throughout the country. He is also the medical officer for the SIREN emergency care research network which is supported by both NINDS and NHLBI. Email: Jeremy.brown@nih.gov

By Patricia Brock, MD, MS; John Stroh, MD; Sarah Dendy, MD; Jasmine King, MA; David Robinson, MD, MS; Aiham Qdaisat, MD, MS, MPH; and Monica K. Wattana, MD, on behalf of the SAEM Oncologic Emergencies Interest Group
Patients with cancer frequently present to the emergency department (ED) for various reasons, ranging from complications of their illness to side effects from treatment to acute oncologic crises. In 2019, cancer-related visits accounted for 5.4% of all ED encounters. Similar rates of ED presentation have been observed for chronic kidney disease (3.5%), cerebrovascular disease, including strokes (3.7%), congestive heart failure (4%), and
other common chronic conditions like diabetes (6%). Recognizing the high frequency and unique needs of these patient groups, specialized ED designations have emerged to optimize care delivery by concentrating necessary resources and standardizing evidence-based protocols. Stroke centers, dialysisaccess facilities, and comprehensive heart attack centers exemplify how these designations have improved outcomes and standardized
emergency care. Building on these successful models, we propose creating an Oncologic Emergency Department Accreditation (OEDA) process to better address the needs of a growing population of cancer patients requiring acute care.
The development of a patientpopulation-specific accreditation within emergency medicine is not unprecedented. Recognizing the complex needs of older adults,
“Ultimately, the rising number of cancer-related emergency department visits highlights a critical need for tailored, standardized care for this vulnerable population.”
leaders in the field created the Geriatric Emergency Department Accreditation (GEDA), which has led to improved patient outcomes, enhanced safety, and increased satisfaction among patients and providers, resulting in cost savings. Similarly, cancer patients presenting to the ED have distinct needs requiring specialized care pathways, additional staff training, and systemic approaches that an OEDA framework could provide. Such an initiative would not only improve patient outcomes but also bridge a critical gap in our current emergency care system.
Establishing an OEDA requires careful planning and adherence to specific standards to ensure optimal management of cancer patients. Key components would include developing detailed standard operating procedures (SOPs) tailored to common oncologic emergencies, such as neutropenic fever, spinal cord compression, and tumor lysis syndrome. Protocols for addressing palliative care needs—including endof-life issues and severe pain crises— must also be incorporated. Metrics for tracking oncology-specific ED outcomes, such as time to pain relief, patient satisfaction, and adherence to recommended protocols, should be established. Integration of these protocols into existing workflows and electronic health record (EHR) systems would ensure seamless patient management. Accreditation could also address specific facility upgrades required to manage oncology patients, such as accommodations for negative or positive pressure rooms, anterooms, processing equipment and supplies, interfacility transport, and blood bank capabilities. Management dashboards and regular protocol reviews based
on current research and frontline feedback would ensure continuous quality improvement.
Education and training would be an essential pillar of OEDA. Physicians, nurses, and ED staff have expressed a growing need for more specialized education in managing oncologic emergencies, including febrile neutropenia, tumor lysis syndrome, immune therapy side effects, and complications of cancer treatments. Training should also encompass acute oncologic crises and palliative care emergencies. Accreditation should require a structured educational component with a set number of continuing medical education (CME) hours, refresher courses, and updated didactic sessions to ensure healthcare professionals stay abreast of the latest practices and innovations in oncologic emergency care. This comprehensive approach ensures not only the attainment of certification but also sustains high-quality emergency care for oncology patients.
Ultimately, the rising number of cancer-related ED visits highlights a critical need for tailored, standardized care for this vulnerable population. Previous specialized ED designations have demonstrated the power of accreditation to improve outcomes through focused education, protocol standardization, and resource alignment. An OEDA would provide EDs with tools to enhance care quality and efficiency for patients with cancer, addressing complex presentations such as neutropenic fever, immunotherapy side effects, and endof-life crises. As cancer prevalence rises alongside an aging population, OEDA represents a proactive and dynamic strategy to meet a growing and critical healthcare need.







Dr. Brock is professor and deputy chair, department of emergency medicine, and executive medical director of inpatient medical operations at The University of Texas MD Anderson Cancer Center in Houston, Texas.
Dr. Stroh is associate professor, department of emergency medicine, at The University of Texas MD Anderson Cancer Center in Houston, Texas.
Dr. Dendy is assistant professor, department of emergency medicine, at The University of Texas MD Anderson Cancer Center in Houston, Texas.
Jasmine King is a third-year medical student at The Ohio State College of Medicine in Columbus, Ohio.
Dr. Robinson is professor of emergency medicine at The University of Texas Health Science Center at Houston and professor of emergency medicine at MD Anderson Cancer Center.
Dr. Qdaisat is assistant professor, department of emergency medicine, at The University of Texas MD Anderson Cancer Center in Houston, Texas.
Dr. Wattana is associate professor and director of education, oncologic emergency medicine fellowship program director, at The University of Texas MD Anderson Cancer Center in Houston, Texas.

By Kenneth N. Appel, DO; David Arbona, MD; and Esteban Casasola, MD
Introduction
Capnography is a noninvasive technique utilized to measure carbon dioxide (CO2) levels during respiration, providing continuous and real-time data regarding a patient’s ventilatory status. This method employs an infrared beam to analyze exhaled air, producing a waveform referred to as capnography, which reflects the dynamic process of respiration.
Furthermore, capnography indirectly estimates the partial pressure of carbon dioxide (PaCO2) in the blood. Such estimations are crucial in critical care and emergency settings where direct measurement of PaCO2 through arterial blood gas (ABG) analysis may not be immediately available.
Monitoring end-tidal carbon dioxide (EtCO2) helps health care
professionals detect changes in PaCO2 levels, identifying issues like hypoventilation, hyperventilation, or ventilation-perfusion mismatches. Although it does not replace the accuracy of ABG measurements, capnography provides a noninvasive, real-time approach for ongoing assessment, making it a valuable complement to other diagnostic tools.
The respiratory process, as monitored by capnography, is categorized into four distinct phases, each providing crucial insight into the dynamics of gas exchange, ventilation efficiency, and overall respiratory function. These phases are as follows:
• Phase 1 – Baseline (No CO2): This phase begins with the initial part of exhalation and reflects the
air coming from the anatomical dead space, such as the trachea and bronchi. This air does not participate in gas exchange within the alveoli and therefore contains negligible or no measurable CO2 On capnography, this phase is represented by a flat baseline, as CO2 levels remain at or near zero.
• Phase 2 – Expiratory Upstroke (Mixing of Gases): As exhalation continues, air from the anatomical dead space begins to mix with CO2-rich alveolar gas. This results in a rapid rise in CO2 levels, which is depicted as a steep upward slope on the capnography. The transition from dead space air to alveolar gas is a critical indicator of effective gas exchange. Factors such as airway obstructions or ventilation-perfusion mismatches can alter the shape or slope of this phase, providing diagnostic
information about the patient’s respiratory status.
• Phase 3 – Alveolar Plateau (Stable CO2 Levels): This phase represents the consistent expulsion of CO2 from the alveoli. As the alveolar gas is exhaled, the capnography reaches a near-horizontal plateau, indicating stable CO2 levels. The end-tidal CO2 (EtCO2), which occurs at the end of this phase, is the maximum concentration of CO2 during the respiratory cycle and is used as a critical marker of ventilation, perfusion, and metabolic function. EtCO2 levels are particularly valuable in assessing the adequacy of ventilation and identifying changes in respiratory or circulatory status.
• Phase 4 – Inspiratory Downstroke (CO2 Clearance): During inhalation, fresh atmospheric air with negligible CO2 enters the lungs, causing a rapid decline in measured CO2 levels. This phase is marked by a sharp downward slope on the capnography as the waveform returns to the baseline established in Phase 1. The steepness of the downstroke can also indicate the efficiency of CO2 clearance and airway dynamics.
Each of these phases provides valuable diagnostic information about respiratory and metabolic processes. By analyzing the shape, slope, and characteristics of the capnography, health care providers can detect abnormalities such as airway obstructions, ventilation-perfusion mismatches, hypoventilation, and hyperventilation. This four-phase framework allows clinicians to monitor and optimize patient care, ensuring effective gas exchange and ventilation during critical interventions. The role of capnography in improving patient safety and outcomes cannot be overstated, making it an essential tool in the emergency department.
The application of capnography extends far beyond simple monitoring. Capnography is widely used in various clinical settings, including anesthesia,
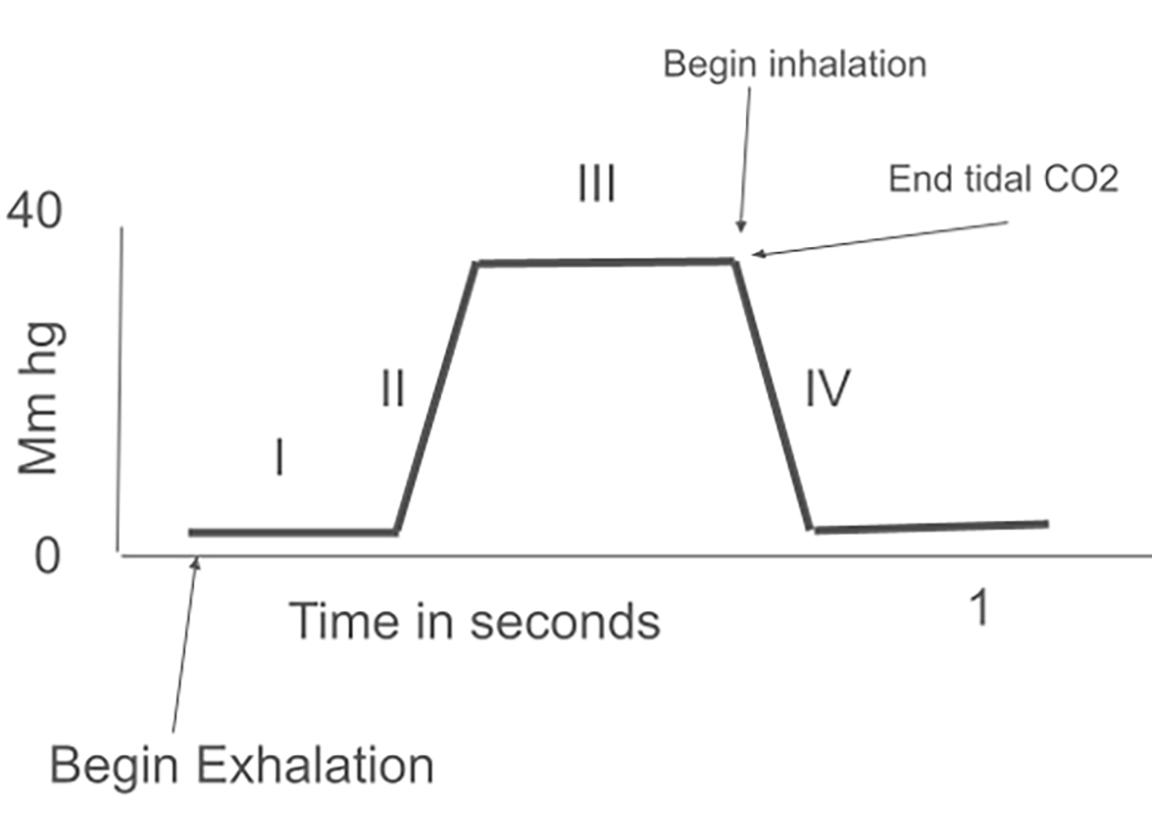
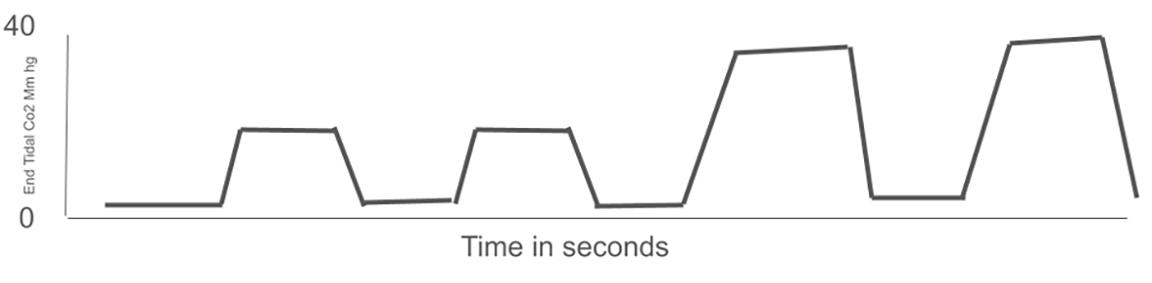
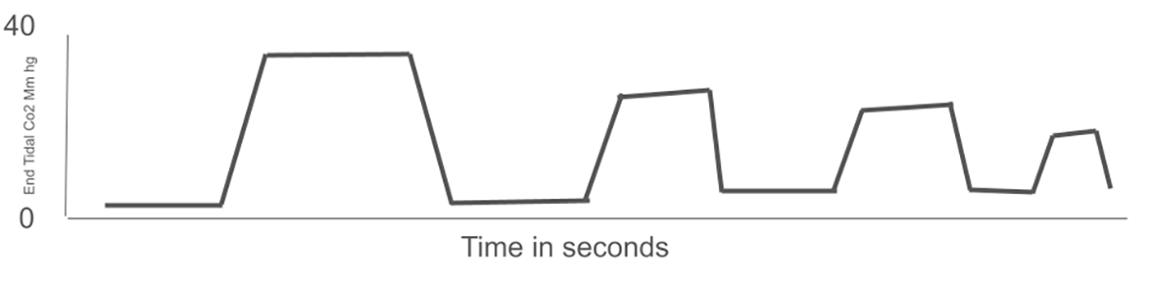
“Capnography offers real-time data on the patient’s ventilation-perfusion status, with a sudden absence of carbon dioxide indicating potential endotracheal tube displacement.”

PREHOSPITAL EM continued from Page 73
intensive care, and emergency medicine, due to its ability to offer continuous, real-time, noninvasive insights into respiratory function. In emergency medicine, it is crucial for evaluating the effectiveness of cardiopulmonary resuscitation (CPR), identifying airway obstructions, and monitoring patients experiencing respiratory distress.
During resuscitation, a significant increase in EtCO2 can indicate the return of spontaneous circulation (ROSC), allowing anticipation of a pulse at the subsequent pulse check. Additionally, capnography can demonstrate decreasing EtCO2 levels during CPR, suggesting ineffective compressions and signaling the need to replace the person performing the compressions.
Capnography can be employed as a decision-making tool at the 20-minute mark to determine whether to continue CPR or cease resuscitative efforts based on EtCO2 readings. Capnography offers real-time data on the patient’s ventilation-perfusion status, with a sudden absence of CO2 indicating potential endotracheal tube displacement, which can be rectified promptly to prevent patient deterioration, particularly in pediatric cases. In cases of refractory cardiac arrest, EtCO2 levels can inform the decision to initiate extracorporeal membrane oxygenation (ECMO).
EtCO2 levels have demonstrated a significant correlation with cardiac output during instances of cardiac
“End-tidal carbon dioxide levels have demonstrated a significant correlation with cardiac output during instances of cardiac arrest, which may signal return of spontaneous circulation.”
“By providing continuous, real-time feedback on the patient’s ventilatory status, capnography enhances the effectiveness of resuscitative measures, ensures appropriate interventions, and aids in critical decision-making processes.”
arrest, which may signal ROSC. This correlation exists because EtCO2 serves as an indirect measurement of the efficiency of pulmonary blood flow, which in turn reflects cardiac function. During cardiac arrest, monitoring EtCO2 can provide valuable information about the effectiveness of chest compressions and the likelihood of ROSC. Furthermore, capnography’s use during CPR is supported by conclusive evidence of correct endotracheal tube placement and its potential for predicting patient survival post-cardiac arrest.
As seen in the figures above, higher EtCO2 levels typically indicate better perfusion (Figure 2), while lower levels may suggest inadequate blood flow (Figure 3). A study of 737 cases of out-of-hospital intubated cardiac arrest patients showed that after 20 minutes of advanced cardiac life support (ACLS), EtCO2 values exceeding 14.3 mmHg accurately predicted ROSC. Another study involving 150 patients experiencing cardiac arrest with pulseless electrical activity (PEA) demonstrated that an EtCO2 value of 10 or less after 20 minutes of ACLS was an accurate predictor of death. Therefore, continuous management of EtCO2 is a crucial component in the management and resuscitation efforts during cardiac emergencies.
Capnography offers significant advantages; however, it has certain limitations during resuscitation. A study involving 575 patients using capnography indicated that the initial presenting rhythm, the cause of the
cardiac arrest, whether bystander CPR was initiated, and the duration from cardiac arrest to the setting of capnography all influenced the capnography values, which in turn affected its prognostic value. This study demonstrated a statistically significant increase in CO2 levels among cardiac arrest patients with a respiratory cause, as opposed to those with a primary cardiac cause.
For patients with cardiac arrest due to pulmonary embolism, occlusion of the pulmonary vasculature results in an increase in physiological dead space and thus shows a low EtCO2 in relation to the PaCO2 Furthermore, specific ACLS medications can also influence EtCO2 levels. Adrenaline may temporarily decrease EtCO2 levels. This can potentially indicate suboptimal CPR quality.
EtCO2 may rise briefly after sodium bicarbonate administration due to increased CO2 production. EtCO2 levels are also affected by ventilation, hypothermia, vasoconstriction, asphyxia duration, and CPR timing. All these variables can influence EtCO2 levels and can be mistaken for ROSC.
In summary, while the use of capnography in cardiac arrest scenarios presents certain challenges, its benefits in monitoring and guiding resuscitation efforts are substantial. In the emergency room, integrating capnography into the monitoring of a cardiac arrest patient is relatively straightforward. However, clinicians must be cognizant of potential pitfalls when utilizing capnography. While EtCO2 monitoring can provide essential feedback in a cardiac arrest
situation, it is important to interpret the results in context, considering other clinical signs and monitoring tools. It is important to remember that EtCO2 values during resuscitation are not absolute indicators of prognosis and should be used as one piece of the puzzle rather than the sole determinant.
Despite these challenges, capnography serves as a valuable diagnostic tool in the resuscitation of cardiac arrest patients. By providing continuous, real-time feedback on the patient’s ventilatory status, capnography enhances the effectiveness of resuscitative measures, ensures appropriate interventions, and aids in critical decision-making processes.



Dr. Appel is a second-year resident at the HCA Florida Brandon emergency medicine residency program.
Dr. Casasola is a first-year resident at the HCA Florida Brandon emergency medicine residency program.
Dr. Arbona is a member of the core faculty and the emergency medical services director at the HCA Florida Brandon emergency medicine residency program.

By Taylor Giller, MD and Irfan Husain, MD, MPH
Emergency medical services (EMS) respond to a nursing home for an elderly man found unresponsive and pulseless, with bystander cardiopulmonary resuscitation (CPR) already in progress. Upon arrival, the EMS team initiates high-quality chest compressions, ventilatory support, and advanced cardiovascular life support (ACLS) interventions. The patient remains in pulseless electrical activity (PEA) despite multiple resuscitation cycles. Midway through resuscitation, a sharp rise in end-tidal carbon dioxide (EtCO₂) from 20 mmHg to 35 mmHg is noted, raising suspicion for impending return of spontaneous circulation (ROSC). However, the
next pulse check reveals continued pulselessness and persistent PEA. Following local protocol, EMS consults medical direction and is advised to transport the patient to the nearest hospital due to the elevated EtCO₂. In the emergency department, ACLS efforts continue. During a pulse check, point-ofcare ultrasound (POCUS) reveals organized cardiac activity, prompting initiation of an epinephrine infusion. An arterial line confirms a perfusing blood pressure, and the patient is stabilized and admitted to the intensive care unit for ongoing management.
This case illustrates pseudopulseless electrical activity
(pseudo-PEA), a critical but often misinterpreted condition in which cardiac activity is present without a palpable pulse. It underscores the importance of differentiating true PEA from pseudo-PEA in the field and raises the question of how prehospital POCUS could enhance EMS decision-making, potentially influencing transport decisions and resuscitation strategies.
The prehospital setting presents distinct challenges, including limited diagnostic clarity and limited ability to confirm clinical suspicions with advanced tools. EMS providers often arrive with minimal

“This case illustrates pseudo-pulseless electrical activity, a critical but often misinterpreted condition in which cardiac activity is present without a palpable pulse.”
information, relying primarily on history, physical examination, and vital signs—tools that lack the diagnostic depth available in hospitals.
In select clinical scenarios, POCUS may help bridge this gap. Advances in portability and durability have made ultrasound increasingly viable in the field. Its use is more common in EMS systems that routinely incorporate physicians, such as those in Europe, Australia, and Canada. Although implementation in the United States is growing, it remains relatively rare.
A 2014 survey of EMS systems in the United States and Canada found that 4.1% were using ultrasound, with 21.7% considering adoption. The The Focused Assessment with Sonography for Trauma (FAST) exam and assessment of PEA arrest were the most common current and anticipated applications. A more recent analysis of the U.S. National Emergency Medical Services Information System
database from 2018 to 2021 showed an increase in POCUS use from 5.2 to 38.9 evaluations per million EMS activations, with participating agencies growing from 11 to 54. In that study, ultrasound was performed primarily by paramedics. POCUS use in cardiac arrests, trauma, and respiratory cases accounted for 70.1% of all exams.
The potential applications of prehospital POCUS are extensive. In cases of out-of-hospital cardiac arrest (OCHA), it can help differentiate between true PEA and pseudo-PEA, thereby guiding resuscitation efforts and informing decisions about field termination of resuscitation. POCUS may also be used to confirm endotracheal tube placement after intubation.
Additionally, POCUS can assist in evaluating fluid status in patients with respiratory distress, helping distinguish between congestive heart failure (CHF) and conditions such as chronic obstructive pulmonary disease (COPD) or asthma exacerbations. This distinction can prevent inappropriate fluid administration and worsening symptoms.
In trauma scenarios, prehospital FAST exams can identify clinically significant intra-abdominal bleeding, allowing for targeted blood product administration and expedited surgical intervention. Other potential applications include identification of obstetric emergencies, detection of long bone fractures, and emerging exploration of transcranial ultrasound for stroke diagnosis in the field.

continued on Page 79
“If successfully integrated, point-of-care ultrasound could become tool in prehospital care—enhancing diagnostic capabilities, management, and ultimately improving survival and

“The central question is whether prehospital ultrasound— despite its costs and training demands—can meaningfully influence care decisions, transport destinations, and time to definitive treatment.”
PREHOSPITAL EM
continued from Page 77
A primary concern regarding the introduction of POCUS in the prehospital environment is the training required, as prehospital providers traditionally do not receive formal ultrasound education. Critics argue that implementation may be timeconsuming and costly, with ongoing training necessary to maintain proficiency.
Several studies have examined the feasibility of training paramedics to use ultrasound. For example, the Prehospital Assessment with UltraSound for Emergencies (PAUSE) protocol, implemented in an urban EMS system in California, demonstrated that firefighterparamedics could accurately assess for pericardial effusion, pneumothorax, and cardiac activity after a single twohour training session. The duration was intentionally selected to align with existing training modules.
Additional research has shown that both civilian and military medics, regardless of prior experience,
become a transformative capabilities, optimizing field recovery rates.”
developed sufficient ultrasound proficiency after a one-day training course.
Another concern is whether paramedics can interpret ultrasound images with the same accuracy as physicians. A study in Minnesota addressed this by evaluating paramedic-performed FAST exams, showing 100% agreement between paramedic interpretations and physician overreads after a six-hour training session.
While initial training appears feasible, maintaining competency is a challenge—particularly for providers who use ultrasound infrequently. To date, no studies have established the most effective model for continuing medical education (CME) in prehospital ultrasound. Developing structured training and re-training programs will be critical for ensuring skill retention and patient safety.
Several challenges remain. Acquiring ultrasound equipment involves a significant one-time expense, along with maintenance and software updates. Training and education barriers persist, and some argue that identifying pathology may not always result in actionable changes in the prehospital setting.
For example, while POCUS may detect a pneumothorax or cardiac tamponade, definitive treatment may fall outside the scope of practice for many EMS providers. As such, the central question is whether prehospital ultrasound—despite its costs and training demands—can meaningfully influence care decisions,
transport destinations, and time to definitive treatment.
While already well-established in emergency and critical care settings, POCUS holds promise to improve prehospital care by enhancing diagnostic precision and guiding more targeted field interventions. However, significant barriers must be addressed. Although numerous observational studies describe prehospital POCUS use, no largescale interventional trials have been conducted to date.
Given its potential, further research is needed to evaluate the feasibility, accuracy, and impact of POCUS on patient-centered outcomes. If successfully integrated, POCUS could become a transformative tool in prehospital care—enhancing diagnostic capabilities, optimizing field management, and ultimately improving survival and recovery rates.


Dr. Giller is a rising third-year emergency medicine resident at Emory University School of Medicine in Atlanta, Georgia. She plans to pursue an emergency medical services fellowship after residency.
Dr. Husain is an assistant professor of emergency medicine at Emory University School of Medicine. He also serves as the associate medical director for Sandy Springs Fire Department and MetroAtlanta Ambulance Service.

By Dakota Burke, MD; Charlie Ryan, MD; and Julian Campillo Luna, MD, MHS, on behalf of the SAEM EMS Interest Group
Over the past two decades, the use of point-of-care ultrasound (POCUS) has steadily increased in emergency medical services (EMS), particularly in helicopter EMS (HEMS). In 2014, only 4% of North American EMS units used POCUS. By 2021, however, 75% of European HEMS units had routine access to the technology. Despite this growth, limited research has explored procedural applications, specifically ultrasound-guided intravenous (IV) access in HEMS.
The primary uses of ultrasound in HEMS have centered around predesignated protocols, such as the extended Focused Assessment with Sonography for Trauma (eFAST), Rapid Ultrasound for Shock and Hypotension (RUSH) exams, echocardiography, lung ultrasound, and obstetric assessments—similar to applications now commonly seen in ground-based EMS units.
Additional research is underway into the use of POCUS to identify various forms of shock
Although research on POCUS utility in HEMS remains limited, many providers find it increasingly valuable. POCUS can augment clinical decision-making, evaluate treatment response, improve triage, and potentially enhance patient outcomes. In fact, several studies support these benefits.
Research has demonstrated that HEMS providers can accurately perform the eFAST exam with high specificity. A retrospective case series found that the use of eFAST by a trained HEMS unit altered clinical management in a subset of trauma patients. Case reports have described POCUS use by flight physicians to identify types of shock, including obstructive
shock. Other studies have shown that HEMS providers can effectively identify pneumothorax with a high degree of accuracy and specificity. Importantly, providers are also able to reliably interpret negative thoracic ultrasound findings, which may help prevent unnecessary and potentially risky prehospital procedures
As ultrasound technology becomes more available, training improves, and proficiency grows, new procedural uses for prehospital POCUS are emerging. Beyond diagnostics, POCUS offers procedural advantages—particularly in vascular access, an area of increasing interest in prehospital care. One notable application is ultrasound-guided peripheral intravenous (USGPIV) access.
HEMS teams typically include flight nurses, paramedics, and physicians,
“Point-of-care ultrasound can augment clinical decision-making, evaluate treatment response, improve triage, and potentially enhance patient outcomes.”
all of whom often need to establish peripheral venous access quickly and accurately. In difficult access scenarios or time-sensitive cases, intraosseous (IO) access is frequently used. While IO access is effective and generally safe, it is not without complications, and not all patients are candidates. USGPIV placement offers a less invasive alternative.
In hospital emergency departments, ultrasound has long been used to guide peripheral IV (PIV) placement, especially in patients with difficult access. Studies have shown that USGPIV use can triple first-pass success rates. In prehospital settings, the results have varied, but overall, success rates tend to generally improve with ultrasound guidance.
To date, no published studies have examined USGPIV use specifically in the HEMS environment, likely due to the slow integration of ultrasound into flight units. However, research involving non-physician providers— including technicians, paramedics, nurses, and military corpsmen—has shown that USGPIV is a learnable skill across a range of medical professionals, not only physicians. These findings suggest that HEMS providers are also well-positioned to adopt this skill.
When training providers in USGPIV in the HEMS setting, it is important to recognize that providers may have varying levels of experience with ultrasound. As ultrasound technology becomes more available in the prehospital environment, aeromedical providers are gradually building competency in its use.
As with other ultrasound applications, comprehensive training
is essential. Providers must be taught the relevant indications and contraindications, how to operate the equipment, relevant anatomy, how to differentiate veins from arteries, how to identify surrounding structures, and proper procedural techniques.
Although adding ultrasound guidance to PIV placement is a technical skill, it is relatively straightforward to learn. With focused instruction and repeated practice, providers can become proficient. Once mastered, USGPIV can be integrated into the broad clinical toolkit of aeromedical personnel, offering a valuable option for establishing vascular access in patients with difficult veins—without resorting to intraosseous (IO) or central line placement.
As with any new procedure, there are challenges to implementation. These include limited access to qualified instructors, clinical simulators, appropriate equipment, and consistent opportunities for hands-on practice. The unique environment of HEMS also presents additional obstacles. Performing USGPIV requires time to set up equipment, prepare the patient, and complete the procedure—all of which may be difficult in the context of short transport times or urgent clinical scenarios.
Therefore, training must also emphasize appropriate patient selection. Teaching providers how to determine when USGPIV is feasible and beneficial is key to ensuring its effective and practical use in the HEMS setting.
Despite these challenges, the growing availability of ultrasound
and improved provider competency make USGPIV a logical next step in prehospital care. With comprehensive training, HEMS providers can expand their capabilities and improve vascular access options for critically ill patients. However, before widespread adoption can occur, more research is needed.
Future investigations should examine:
• Time required to achieve proficiency
• Procedure duration versus transport time
• In-flight application and feasibility
• Provider willingness to apply skills in real-time
• Impacts on clinical outcomes
As HEMS continues to evolve, incorporating ultrasound-guided vascular access may significantly enhance patient care in the prehospital environment.


Dr. Burke is a second-year resident at the University of Michigan.
Dr. Ryan is a second-year resident at the University of Michigan.

Dr. Campillo Luna is a fourthyear resident at the University of Michigan.

By Kristina Awan, MD
I still remember the pit in my stomach. I walked into the designated quiet space in the middle of a loud, busy ED waiting room with social work to tell a woman I’d never met that her 27-year-old husband had died for an unknown reason.
EMS reported that she found him passed out at home—so many unanswered questions. I don’t see a history of dysrhythmias or substance use in his chart; he seems healthy. None of this makes sense.
Okay, it’s finished. She knows that he died and took it way better than I would have. but I’m struggling with the fact that the patient’s death didn’t affect me as much as his wife’s reaction did. I wanted her to know that he didn’t die alone, but I started to choke up and wanted to maintain a brave face.
“I walked into the designated quiet space in the middle of a loud, busy emergency department waiting room to tell a woman I’d never met that her 27-year-old husband had died.”
How is this a normal part of my job? Can I do this forever? Why wasn’t I sad when I called the time of death? It’s hard to explain, but I can actively feel the emotional, soft side of my personality harden. But I know this is necessary. I have other patients I need to disposition so I can get home to my husband and hug him a little tighter tonight

Dr. Awan is a third-year emergency medicine resident at the University of Rochester in New York. She will pursue a fellowship in addiction medicine at the University at Buffalo following her residency. Her clinical focus is rooted in harm reduction, advocacy, and improving access to comprehensive care for vulnerable populations.

By Lindsay Maguire, MD and Adrienne Malik, MD, on behalf of the SAEM Research Committee
Psychiatric and behavioral health emergencies are common in the emergency department, yet the field remains under-researched. This is not due to lack of clinical importance— nearly one in eight ED visits involves a mental health concern—but rather a host of ethical and logistical challenges that make research in this area particularly complex.
Still, ethically sound, high-quality studies are feasible and must be undertaken. This article outlines practical methods and best practices for conducting research on psychiatric and behavioral emergencies while
respecting patients’ rights, autonomy and safety.
The foundation of any research endeavor—especially in the ethically sensitive context of psychiatric emergencies—is selecting a question that is both clinically meaningful and ethically appropriate. A well-crafted research question must respect patient dignity and autonomy while addressing real-world care gaps.
Ask yourself:
• Does this question arise from a clinical need that cannot be answered by other means?
• Could answering this question improve outcomes, reduce harm or inform policy for high-risk populations?
• Are there less invasive ways to answer the question (such as chart review or observational studies)?
Avoid questions that:
• Require exposing participants to unnecessary risk
• Involve vulnerable populations without direct benefit or safeguards

continued from Page 83
• Focus solely on academic interest without potential patient impact
Ethical research begins with asking questions that aim to improve care without compromising patient welfare.

Ethical example: Among patients presenting to the ED with suicidal ideation, does the use of a brief safety planning intervention reduce 30-day return visits compared to usual care?

Unethical example: How do patients with active psychosis respond to different communication styles during acute agitation?
(Raises concerns about consent, coercion and benefit.)
Consulting with ethicists, institutional review boards and
community stakeholders early on can help ensure your question aligns with the principles of autonomy, beneficence and justice.
Reconsider How and When Consent Happens
Informed consent is the central ethical hurdle in emergency psychiatry trials. Patients may be acutely psychotic, intoxicated or suicidal—raising concerns about their ability to understand and consent to a proposed intervention. Decision-making capacity may fluctuate, especially in cases of psychosis or delirium. Not all patients in crisis lack capacity, and including only those who can consent may introduce bias.
The Food and Drug Administration allows for exceptions from informed consent in life-threatening situations (such as research on cardiac arrest or traumatic brain injury), but psychiatric emergencies are
usually not life-threatening once emergency care has been sought. Blanket waivers of informed consent are rarely requested but may be appropriate when the intervention poses minimal risk.
When such waivers cannot be obtained and a patient lacks decision-making capacity, alternate consent methods may be used:
• Substituted consent from a surrogate decision-maker
• Deferred consent, where recruitment begins before full capacity is regained and formal consent is obtained later
In some cases, consent may be implied if the intervention is likely to help and unlikely to cause harm.
Given the acuity and vulnerability of this population, psychiatric ED research should be as low-risk and minimally intrusive as possible.
“Psychiatric and behavioral health emergencies are common in the emergency department, yet the field remains underresearched due to a host of ethical and logistical challenges that make research in this area particularly complex.”
Choose the least invasive method to answer the research question. Retrospective chart reviews, observational cohort studies and comparative effectiveness research using standard treatments can protect patients who may not fully understand the risks and benefits of experimental interventions.
Some questions require clinical trials. In these cases, patient safety must remain the top priority. If an intervention poses more than minimal risk, and the alternative to not participating is not life-threatening, patients must be stable enough to engage in the consent process.
For such trials:
• Begin with a small pilot study enrolling only patients who can provide consent
• If safety is confirmed, consent waivers may be reasonable for larger studies assessing effectiveness and generalizability
When studying patients unable to consent—such as those experiencing acute psychosis or drug overdose— only interventions that introduce minimal risk may be ethically justified.

Ethical example: Among patients presenting obtunded after an intentional toxic ingestion, does early psychotherapy reduce the need for psychiatric hospitalization? (Intervention is non-invasive and unlikely to cause harm.)

Unethical example: Does a new drug with an unknown adverse effect profile lead to faster sedation in acute sympathomimetic toxidrome than IM midazolam? (Harms of the
new drug are unknown and testing without consent is unethical.)
Mental health patients in the ED often belong to historically underserved populations, including those who are unhoused, uninsured or impacted by structural racism. Ethical research demands equitable inclusion in order to ensure generalizability.
Whenever possible, ensure study protocols:
• Do not inadvertently exclude patients based on language, housing or insurance status
• Include translated consent materials and culturally competent communication
• Collect and report demographic data to monitor for enrollment disparities
Support Follow-Up and Participant Safety
Planning for follow-up is difficult but necessary. Patients experiencing psychiatric emergencies may lack stable housing, transportation, phone access or social support. Consider flexible, low-burden follow-up approaches:
• Short digital surveys, phone calls, text messages or telehealth visits
• Follow-up through outpatient providers or care navigators
• Ethical, non-coercive compensation that participants can reasonably access
If research encounters reveal ongoing distress, suicidality or unmet behavioral health needs, ensure your protocol includes a plan to connect participants with appropriate services.
Conducting ethical research in emergency psychiatry is not only possible—it is essential. As EDs face growing volumes of mental health crises, we must build an evidence base to guide compassionate, effective and equitable care. By embedding ethical safeguards into every step of study design— from consent models to community engagement—emergency physicians and researchers can lead the way in generating data that serves those who need it most.

Dr. Maguire is an assistant professor of emergency medicine at the University of Kansas Medical Center. She completed a research fellowship at Orlando Health in Orlando, Florida. She is the associate director of clinical trials at KUMC and leads multiple funded and unfunded research efforts, focusing on emergency psychiatry. She is a member of the SAEM research and grants committees.

Dr. Malik is an associate professor of emergency medicine at the University of Kansas Medical Center. She serves as the director of research training for the University of Kansas emergency medicine residency and oversees the quarterly research workshop. Dr. Malik is the institutional principal investigator for multiple industry-funded clinical studies, the NIH SIREN network, and her own investigator-initiated studies. She has been a member of the UKMC institutional review board for four years and is an elected member of the University of Kansas School of Medicine research committee. Dr. Malik serves as a regular peer reviewer for multiple emergency medicine journals and is a member of the SAEM research and grants committees.

By Layla S. Abubshait, MD, on behalf of the SAEM Social Emergency Medicine and Population Health Interest Group
Introduction
Picture this: an elderly Bengalispeaking woman arrives in your emergency department (ED) with chest pain, her son insisting on translating despite the availability of professional interpreters. Beyond the immediate medical concern lies a complex web of social and cultural factors that could significantly impact her care. This scenario—one of many we use in our curriculum at Jefferson Einstein Montgomery Hospital—illustrates why teaching emergency medicine residents about social determinants of health (SDoH)
isn't just important; it's crucial.
EDs are often the first point of contact for individuals facing not only acute medical crises but also the harsh realities of SDoH. As emergency physicians, we're adept at addressing immediate medical needs—but are we adequately prepared to tackle the underlying social factors that contribute to poor health outcomes? Recognizing this critical gap, our emergency medicine program at Jefferson Einstein Montgomery Hospital developed a team-based learning
curriculum to equip residents with the tools to identify and address SDoH comprehensively. This article highlights our approach, key findings, and the importance of integrating SDoH into emergency medicine training.
Background
Social determinants of health— factors such as socioeconomic status, education, housing, and access to care—profoundly impact a patient’s well-being. These factors can influence everything from chronic disease management to
LEP (Limited English Proficiency)
An 85-year-old Bengali-speaking woman presents to the ED with chest pain and cough, accompanied by her son who insists on translating despite the offer of professional interpretation services. During the historytaking, the son answers most questions and doesn't fully translate all inquiries to the patient. Initial tests are ordered, including a chest X-ray which reveals an opacity and pleural effusion suggestive of a possible malignancy. A follow-up CT scan confirms the presence of what appears to be a malignancy. Upon receiving this news, the son becomes distressed and expresses his desire not to inform his mother of the results, claiming she wouldn't want to know or undergo treatment.
access to preventive care, ultimately driving individuals to seek emergency care. Traditional medical training often focuses on treating symptoms, but a more holistic approach requires understanding and addressing the root causes. By integrating SDoH into emergency medicine, we can enhance residents' ability to provide immediate care and foster preventive strategies to mitigate future emergencies.
Our curriculum employed a multifaceted approach, incorporating a variety of educational strategies to engage residents and promote active learning. Key components included:
• Foundational knowledge: We started with lectures led by faculty experienced in SDoH, providing residents with a framework for understanding the impact of social factors on health.
• Immersive simulation: Residents participated in SPENT, a web-based simulation challenging them to survive on a minimal wage. This experience provided firsthand insight into the difficult choices patients face regarding housing, transportation, and healthcare access.
• Real-world application through case scenarios: Working in teams, residents tackled clinical case scenarios that highlighted the impact of SDoH, such as food insecurity or housing instability.
• This case highlights the critical importance of language access in healthcare, as the elderly Bengali-speaking patient's limited English proficiency (LEP) significantly impacts her care quality and outcomes.
• This scenario emphasizes the need for patient-centered care that respects cultural diversity while ensuring LEP patients are fully involved in their healthcare decisions, potentially using professional interpreters and multilingual resources.
• Discuss how training providers and staff in cultural competencies can improve patient outcome
• Discuss the importance of having certified medical interpreters or video/audio remote interpreting services
• Encourage translating written educational materials in commonly spoken languages

These scenarios encouraged holistic care, addressing underlying social determinants alongside medical needs. For example, a case involving a patient with limited English proficiency underscored the importance of language access and cultural competency in healthcare (see Table 1).
• Debriefing and reflection: Debriefing sessions allowed residents to reflect on challenges, strategies, and lessons learned—fostering a patientcentered mindset.
• Community engagement: We connected residents with community experts and resources, including social workers and shelter managers,
to provide insights into available support services.
To evaluate the effectiveness of our curriculum, we conducted pre- and post-curriculum surveys assessing residents’ knowledge, attitudes, and skills related to SDoH. Our findings revealed significant improvements in residents’ understanding and application of SDoH concepts. Specifically, residents demonstrated a marked increase in their ability to recognize the impact of SDoH on patients’ physical health, mental well-being, and quality of life. Notably,
continued on Page 89


“Teaching emergency medicine residents about social determinants of health isn’t just important—it’s crucial.”
continued from Page 87
there was a substantial gain in awareness of community resources related to SDoH.
Discussion
Our experience demonstrates the potential of a dedicated SDoH curriculum to enhance emergency medicine residents' ability to provide comprehensive and equitable care. By bridging the gap between theoretical knowledge and practical application— through lectures, simulations like SPENT, case scenarios, and community engagement—our program empowers residents to address the complex interplay between social factors and health outcomes in emergency settings. The substantial improvements observed in residents’ understanding and familiarity with local SDoH-related
resources underscore the curriculum’s effectiveness.
However, it’s important to acknowledge the limitations of our study. The small sample size—16 residents from a single institution— limits the generalizability of our findings to other emergency medicine programs with different demographics or resource availability. While the preand post-curriculum surveys revealed significant improvements in residents’ self-reported knowledge and attitudes, further research is needed to assess the long-term impact of this training on clinical practice and patient outcomes. For example, future studies could track residents’ documentation of SDoH in patient charts, referral rates to community resources, and utilization of interpreter services.
Conclusion
Integrating SDoH into emergency medicine training is not just about
enhancing clinical skills—it’s about fostering a commitment to social justice and health equity. As emergency physicians, we have a responsibility to advocate for our patients’ well-being, both inside and outside the hospital walls. By embracing a more holistic approach to care, we can make a meaningful difference in the lives of our patients and build a stronger, healthier community
Dr. Abubshait is a boardcertified emergency medicine physician and associate program director at Jefferson Einstein Montgomery Hospital. A dedicated medical educator and cultural competency leader, she specializes in patient advocacy and bridging cultural gaps in emergency care. Fluent in five languages, Dr. Abubshait has published extensively on care for patients with limited English proficiency and the social determinants of health in emergency medicine.

By Ricardo Soubelet, DO and Mark Rivera-Morales, MD
Imagine this scenario: a patient is brought into your emergency department (ED) after falling off his bike onto the left side of his chest, landing on a large rock. He presents with tachypnea, shortness of breath, and severe pain in the left lateral chest. Auscultation reveals decreased breath sounds on the left; ultrasound shows no lung sliding on that side, and an AP chest X-ray confirms your suspicion: a large leftsided pneumothorax with associated fractures of ribs 4–8. The patient is hemodynamically stable but requires intervention.
What’s your next move? Chest tube.
Chest tube placement is widely recognized as one of the most painful procedures performed in emergency medicine (EM). Despite this, analgesia strategies often remain suboptimal—typically involving a rushed combination of local anesthetic injection, systemic opioids, and, in some cases, procedural sedation. The use of systemic opioids and sedatives can be problematic in unstable, hypoxic, or elderly patients. A growing
number of EM physicians are now asking a simple question: Can we do better?
Enter the Serratus Anterior Plane Block
The serratus anterior plane block (SAPB) is an ultrasound (US)-guided regional anesthesia technique that’s gaining momentum for its ability to provide targeted, reliable analgesia to the anterior and lateral chest wall. Originally popularized in thoracic surgery and postoperative pain management, SAPB is now finding applications in the ED for procedures

“Chest tube placement is widely recognized as one of the most painful procedures performed in emergency medicine, yet analgesia strategies often remain suboptimal.”
such as tube thoracostomy, rib fractures, and blunt chest trauma.
SAPB is a US-guided fascial plane block that involves the injection of anesthetic into either the superficial or deep fascial plane of the serratus anterior muscle. It provides analgesia by blocking the lateral cutaneous branches of the intercostal nerves (T2–T9). When guided by ultrasound, the technique is relatively easy to learn and perform—especially for today’s EM clinicians who are already
experienced with ultrasound-guided procedures.
Unlike intercostal nerve blocks, SAPB covers a broader dermatomal range and offers a longer duration of analgesia—typically lasting 6 to 12 hours, but potentially up to 24 hours depending on the anesthetic used. This makes it particularly useful not only for pain control during the procedure, but also for managing post-procedural pain.
A growing body of literature suggests meaningful reductions in pain scores and opioid use following SAPB. In small clinical studies and
case reports, patients undergoing chest tube placement with SAPB have shown improved comfort, better spirometry performance, and, in many cases, a preference for this approach over sedation.
SAPB is also applicable for both adult and pediatric patients, as well as those with elevated body mass index (BMI), due to the relatively shallow depth of the nerve block. It has been used successfully in cases of isolated rib fractures, prior to chest tube or pigtail catheter placement, complex
“The serratus anterior plane block is regional anesthesia technique that reliable analgesia to the anterior and

lacerations of the chest wall, and even for shingles-related pain—thanks to its ability to block multiple dermatomes without interfering with overlying lesions.
Image A: Shows the lateral decubitus positioning and dermatome distribution of the serratus anterior plane nerve block. Note that the typical chest tube placement (4th–5th intercostal space) lies roughly in the middle of the anesthetized area.
Image B: Demonstrates the correct setup for a successful serratus anterior plane block. The black star indicates the probe marker orientation, which corresponds to the probe marker on the ultrasound screen shown on the left. The needle is inserted on the opposite side of the probe marker and therefore appears on the right side of the screen. The block is performed using an inplane approach, allowing dynamic visualization of the entire needle length.
Image C: An actual ultrasound image of the serratus anterior plane block in progress. The muscles and fascial planes are clearly identified. The needle is approaching in an in-plane fashion from the top right of the image. The rib and pleura are visible in the bottom left, providing confidence that these critical structures are safely out of reach with proper visualization. The anesthetic appears as a hypoechoic fluid collection in the anterior fascial plane of the serratus anterior muscle. This is a high-volume block, typically using a total of 30 mL of diluted anesthetic. Always calculate
is an ultrasound-guided that provides targeted, and lateral chest wall.”
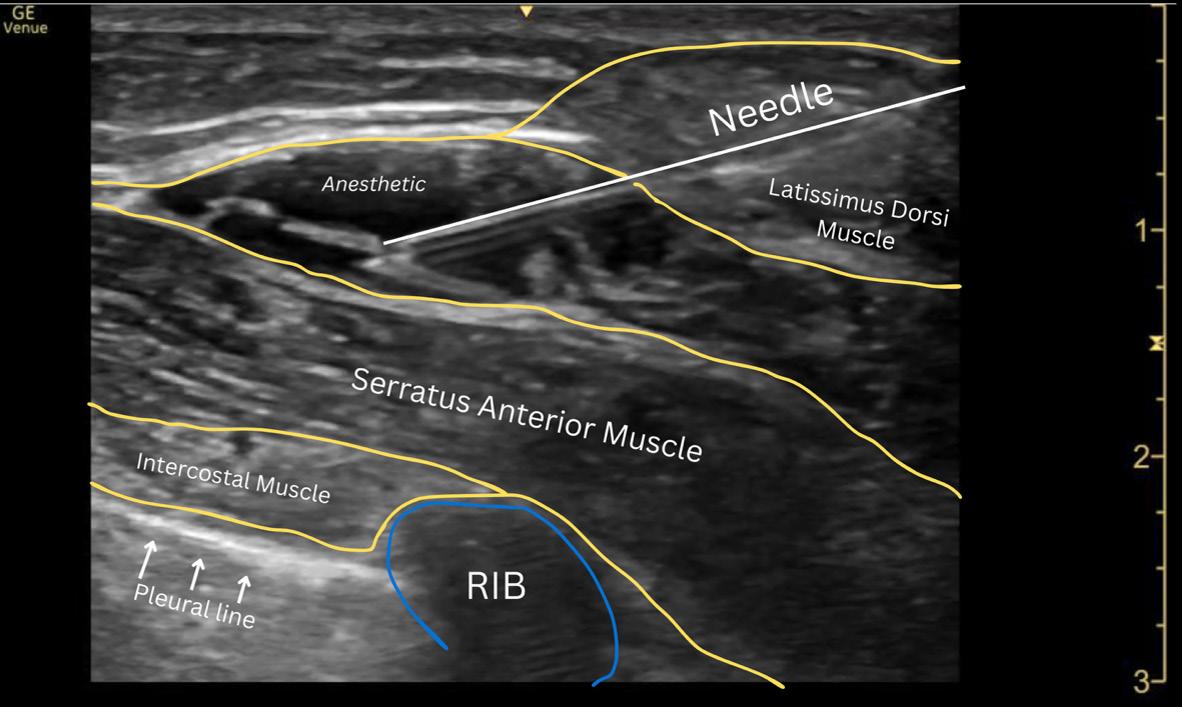
the toxic dose of your chosen anesthetic beforehand and dilute with normal saline as needed to reach approximately 30 mL total volume.
SAPB is particularly useful for patients in whom sedation poses high risks or is contraindicated—such as those with respiratory compromise, altered mental status, or traumainduced hemodynamic instability. By preserving airway reflexes and cognitive function, SAPB avoids the risks associated with systemic medications while still delivering effective pain relief.
The safety profile is also favorable. When performed under ultrasound guidance, complications such as local anesthetic toxicity, bleeding, or pneumothorax are rare. Most existing data—from thoracic trauma and perioperative settings—report no major adverse events.
While SAPB is not yet widely adopted as a first-line strategy for ED chest tube analgesia, it is rapidly gaining recognition. It represents a procedural innovation that aligns with the values of modern emergency medicine: efficient, ultrasound-driven, patient-centered care.
It’s important to acknowledge that most of the current evidence supporting SAPB comes from thoracic surgery, trauma, and postoperative
settings. High-quality trials focused specifically on chest tube placement in the ED are still limited. Nonetheless, the available evidence is both promising and growing.
As regional anesthesia continues to expand in EM, the serratus anterior plane block deserves a place in the conversation. It won’t eliminate the need for procedural sedation in all cases, but it could significantly reduce our reliance on it—especially in critical patients where every decision counts.
In the hands of ultrasound-trained emergency physicians, SAPB offers a safe, effective, and accessible tool to improve pain control during one of the ED’s most uncomfortable and highstakes interventions.
Is it time to make SAPB part of the standard chest tube protocol?


Dr. Soubelet is a PGY-2 emergency medicine resident at HCA Florida Kendall Hospital. Dr. Rivera-Morales is emergency medicine residency and AEMUS fellowship core faculty at HCA Florida Kendall Hospital.

By Nazaret Colón-Fernández, MD; Moises Moreno, DO, FACEP, Nicole Aviles, MD, FACEP
Point-of-care ultrasound (POCUS) has emerged as a valuable diagnostic tool across a variety of clinical settings. Its role in identifying deep vein thrombosis (DVT) and clot in transit (CIT) in patients presenting with atypical symptoms—such as back pain—has gained increasing attention. This article explores the utility of POCUS in diagnosing DVT and CIT in a patient who initially presented with back pain.
Case presentation
An 80-year-old woman with a medical history of atrial fibrillation, hypertension, dementia, bipolar disorder, gastritis, and hyperthyroidism presented to the
emergency department with aching lumbar back pain that had persisted for two days. She also reported constipation, fatigue, decreased appetite, and lower abdominal pain. Recently, she had been treated for a reported urinary tract infection.
On evaluation, the patient exhibited tachycardia and mild hypoxia. Electrocardiogram showed atrial fibrillation with a rapid ventricular response. Effective management required identifying potential systemic triggers contributing to her presentation. Alongside blood and urine tests, POCUS was performed to assess cardiac function and evaluate other possible cardiac causes of
the arrhythmia before initiating pharmaceutical treatment.
Point-of-care ultrasound revealed a clot in the right atrium moving toward the right ventricle (Figure 1).
A thorough search for the clot’s source included assessment of both legs for signs of DVT. Although no swelling or redness was present, POCUS identified a thrombus in the femoral vein characterized by vessel non-compressibility (Figure 2).
These POCUS findings prompted changes in the patient’s management. Additional blood tests were ordered to assess cardiac dysfunction using troponin and

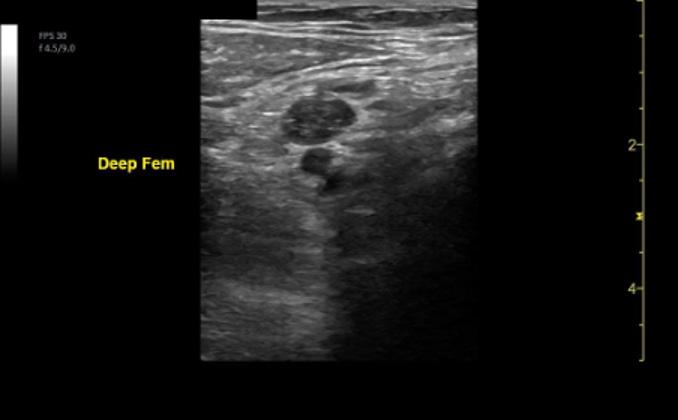
“Point-of-care ultrasound enables clinicians to quickly identify non-compressible veins—an indication of thrombus presence—minimizing the need for more invasive and time-consuming procedures.”
pro–brain natriuretic peptide (proBNP) levels. Computed tomography angiography (CTA) of the chest was performed as well. Elevated troponin and pro-BNP levels indicated possible right heart strain, which was confirmed by the CTA. Based on this information, interventional radiology was consulted to perform thrombectomy, successfully removing a significant clot burden and improving the patient’s hemodynamic status.
POCUS is especially valuable in emergency settings because it is portable, user-friendly, and provides immediate results. When diagnosing DVT, POCUS enables clinicians to quickly identify non-compressible veins—an indication of thrombus presence. Trained emergency physicians can perform this bedside evaluation, minimizing the need for more invasive and time-consuming procedures.
Detecting clot in transit via POCUS is
critical because of the high risk for pulmonary embolism. Visualization of the inferior vena cava and right heart chambers can reveal mobile thrombi, enabling immediate intervention. In this case, identifying CIT was pivotal in altering the patient’s management.
Traditional imaging for diagnosing DVT and CIT—such as duplex ultrasound performed by radiology and CTA—requires specialized equipment and personnel, often causing delays. In contrast, POCUS allows clinicians to conduct examinations at the bedside, facilitating rapid diagnosis and timely treatment decisions. This is especially important in emergency care, where every moment counts.
POCUS serves as a valuable diagnostic tool for detecting DVT and CIT in patients with atypical symptoms, such as back pain. Its ability to provide rapid, accurate, and noninvasive diagnosis makes it an essential resource in emergency medicine. This case highlights the
critical role POCUS plays in the prompt identification and management of thromboembolic events, ultimately improving patient outcomes



Dr. Colón-Fernández is an EUS fellow at HCA Florida Kendall Hospital.
Dr. Moreno is ultrasound fellowship program director and ultrasound director at HCA Florida Kendall Hospital. He is core faculty at HCA Florida Kendall Hospital.
Dr. Aviles is ultrasound fellowship associate program director and ultrasound director at HCA Florida Kendall Hospital. She is associate program director of the KRMC emergency medicine residency and core faculty at HCA Florida Kendall Hospital.

By Jessica Manrique, MD; Nicole Irizarry del Valle, MD; and Nicole Aviles, MD, on behalf of the SAEM Academy of Emergency Ultrasound
The Case
A five-year-old boy with no significant past medical history presented to the emergency department after referral from urgent care for a possible left elbow fracture. The patient had fallen at a park the previous day, landing directly on his left elbow. He had been given ibuprofen before arrival. There was no reported loss of consciousness, head trauma, or other injuries. On initial evaluation, the patient had no additional complaints.
Plain radiographs of the elbow revealed joint effusion with both
anterior and posterior fat pad signs (see Figure 1). No obvious fracture line, dislocation, subluxation, radiopaque foreign bodies, or abnormal osseous lesions were identified. Despite the lack of a visible fracture, the fat pad signs raised concern for an occult injury.
Introduction
Supracondylar humerus fractures are the most common type of elbow fracture in children. They typically occur after a fall onto an outstretched hand (FOOSH) or with elbow hyperextension. Displaced fractures, such as Gartland types
II–IV, are generally apparent on plain radiographs and typically require urgent orthopedic consultation, closed reduction, and surgical pinning.
In contrast, type I supracondylar fractures are nondisplaced and may be radiographically occult. When X-rays appear normal but clinical suspicion remains high, clinicians should look for subtle signs such as the presence of a posterior fat pad. Even when these signs are absent, point-of-care ultrasound (POCUS) can serve as a valuable tool to identify occult injuries.

Using a linear probe, place the patient’s elbow in 90 degrees and scan in both longitudinal and transverse views. Start at the proximal arm and scan toward the olecranon fossa. In a normal elbow evaluated via ultrasound, the humeral line, triceps muscle, and olecranon fossa can be identified (Figure 2). The fascial line within the olecranon fossa is typically flat and positioned slightly below the surrounding bony landmarks.
When an occult supracondylar fracture is present, the posterior fat pad appears elevated above the bony contours—often due to an effusion or lipohemarthrosis (Figure 3). In some cases, an obvious cortical deformity may also be visible as a step-off in the humeral cortex.
Ultrasound is increasingly recognized as a helpful adjunct for evaluating pediatric elbow injuries, especially when plain radiographs are inconclusive or appear normal. Scanning in both transverse and longitudinal planes can help detect subtle signs of fracture, such as elevation of the posterior fat pad.



“When X-rays appear normal but clinical suspicion remains high, clinicians should look for subtle signs such as the presence of a posterior fat pad.”
continued from Page 97
While ultrasound is not yet standard practice in all settings for these injuries, it holds promise for minimizing unnecessary imaging, reducing overtreatment, and improving patient comfort. Still, when clinical suspicion remains high despite inconclusive imaging, placing the arm in a splint remains the safest course of action while awaiting orthopedic evaluation.
A bedside POCUS of the elbow was performed to further evaluate the radiographic findings. The ultrasound demonstrated elevation and irregularity of the posterior fat pad, consistent with an occult supracondylar fracture. The patient was placed in a long posterior arm splint and discharged with instructions to follow up with pediatric orthopedics on an outpatient basis.
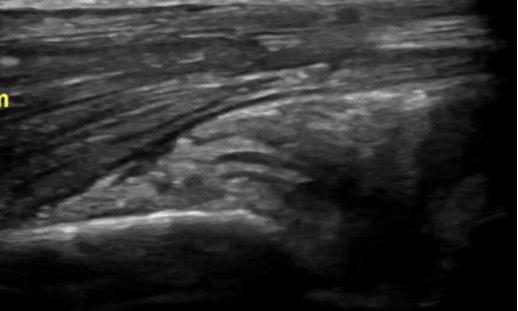
This case highlights the utility of point-of-care ultrasound in diagnosing an occult supracondylar fracture in a pediatric patient with normal-appearing X-rays. Emergency clinicians should consider bedside

ultrasound as a valuable diagnostic adjunct when managing pediatric elbow trauma with subtle clinical or radiographic findings



Dr. Manrique is a second-year emergency medicine resident at HCA Florida Kendall Hospital in Miami, Florida.
Dr. Irizarry is emergency medicine faculty at HCA Florida Kendall Hospital. She completed a pediatric emergency medicine fellowship and has an interest in qualitative and improvement projects for the pediatric population.
Dr. Aviles is ultrasound fellowship associate program director and ultrasound director at HCA Florida Kendall Hospital. She is associate program director of the KRMC emergency medicine residency and core faculty at HCA Florida Kendall Hospital.

By Jessica Pelletier, DO; Faith Ibu, MD; and Mary Ellen Lyon, MD
Emergency medicine is expanding in low- and middle-income countries, while U.S. residents increasingly pursue global health. Yet international medical graduates (IMGs) remain underrepresented in U.S. emergency medicine programs. Although one in four U.S. medical residents are IMGs, emergency medicine programs accept far fewer compared with other specialties, such as pediatrics and internal medicine. The U.S. remains a top destination for IMGs seeking training in established emergency medicine settings, and evidence is growing about the benefits they bring both to U.S. programs and to the health systems in their home countries. Incorporating IMGs enriches training for U.S. residents and equips
graduates to strengthen healthcare abroad.
IMGs face numerous hurdles to matching into emergency medicine. In 2024, the categorical emergency medicine match rate for non-U.S. IMGs was only 35%, compared with 67% for U.S. IMGs, 89% for U.S. DO seniors and 93% for U.S. MD seniors. IMGs often need higher Step 2 scores, stronger grades and more competitive CVs to be considered This population must apply to many more residency programs to increase their chances of matching, which presents a significant financial burden for applicants from low- and middle-income countries. Educational Commission for Foreign Medical Graduates (ECFMG)
certification is also required, and this process is costly
In today’s political environment, H-1B visa denial rates have skyrocketed, and J-1 visas for international students are being unexpectedly revoked. One rarely discussed but insurmountable challenge for IMG applicants is the inability to obtain a standardized letter of evaluation (SLOE) — yet the expectation is that IMGs have at least two, compared to one for their U.S. MD peers
Originally developed in 1995 as the Standardized Letter of Recommendation (SLOR), the SLOE was renamed in 2014 and transitioned to an electronic format (eSLOE) in 2016. The SLOE has
“Surely we can do better than to send regrets to such students because they lack internships and Standardized Letters of Evaluation we did not allow them to obtain.”
become a unique component of the emergency medicine application process compared with other specialties. Unlike a typical letter of recommendation, which is mainly subjective, the SLOE aims to objectively assess the applicant’s performance compared with peers and clearly identify strengths and weaknesses. While not perfect, and with some variability in how institutions use its rating scales, the eSLOE is thought to be less biased than previous versions.
To obtain a SLOE, an applicant must apply for an audition rotation — also called an acting internship, sub-internship or “sub-I” — at a given emergency medicine residency program. Most programs use the Visiting Student Learning Opportunities (VSLO) system Only current medical students are eligible to apply through VSLO, which automatically excludes non-U.S. IMG applicants who have already graduated Another challenge is that a medical school must participate in VSLO to send students for rotations listed in the database. Currently, no new international institutions are being allowed to join the VSLO database. Most programs require applicants to use VSLO to apply for emergency medicine rotations No published data exist on how many programs accept rotators outside VSLO. In November 2024, outreach to the Council of Emergency Medicine Residency Directors (CORD) listserv and individual programs yielded only one response indicating flexibility. These challenges significantly limit opportunities for non-U.S. IMGs to rotate at academic institutions and obtain SLOEs. Given these constraints, expecting non-U.S. IMGs to secure two
or more SLOEs to remain competitive presents a substantial challenge.
Because program directors typically consider the SLOE the most important part of the emergency medicine residency application, the inability for many non-U.S. IMGs to obtain one acts as a direct barrier to matching. As a result, programs may miss out on outstanding applicants. Moreover, when IMGs cannot interact with the specialty and U.S. healthcare system before residency, those who do match face significant disadvantages integrating into a new system and may be perceived as less competent than peers. Taking on an IMG resident can be seen as a “gamble,” since many American institutions are unfamiliar with the quality of their medical training. However, many resourcelimited settings have yet to develop emergency medicine as a specialty, and they will not be able to do so without EM-trained physicians. We live in an increasingly global community with an imperative to improve healthcare both in and outside the U.S. Without offering education, how can this be accomplished?
International medical graduates are a valuable but underutilized resource in U.S. emergency medicine residency programs. Their diverse experiences enrich training environments and align with the growing global health focus in emergency medicine. Despite exceptional talent and perseverance, many IMGs face systemic barriers, such as limited access to internships and SLOEs, that hinder their ability to match. A highly qualified emergency medicine educator from a lowresource setting known to the authors recently failed to match despite strong credentials — a missed opportunity for the specialty. Surely we can do better
than to send regrets to such students because they lack internships and SLOEs we did not allow them to obtain.
The authors propose that programs be willing to review applications from international medical students and graduates and offer promising candidates opportunities to rotate in their systems. By formally allowing IMGs to apply for subinternship rotations, programs can provide essential SLOEs and, more importantly, foster direct, personal evaluations of students’ clinical skills, professionalism and adaptability — attributes often difficult to assess through paper credentials alone.

Dr. Pelletier is an assistant professor of emergency medicine and associate program director at the University of MissouriColumbia. She serves as the medical director for Techies Without Borders, a global nonprofit organization dedicated to using technology solutions to create continuing education accessibility for healthcare workers in limited-resource settings.

Dr. Ibu is a third-year emergency medicine resident at the University of Missouri-Columbia. An international medical graduate, she earned her medical degree from the College of Medicine at the University of Lagos, Nigeria. Her interests include emergency medical services, global health, and medical education. She serves as an ECHO coordinator for Techies Without Borders.

Dr. Lyon is an emergency physician and global health educator with Seed Global Health at Makerere University College of Health Sciences in Kampala, Uganda. Her work focuses on capacity building in emergency care and medical education in resource-limited settings.

By Megan Schultz, MD, MA, and Sehr Khan, MD
(This article is written from Dr. Schultz’s perspective; both authors contributed to its development.)
My patient was 15 years old, shot in the upper leg. He was obviously in pain, but the bleeding was controlled, and his vital signs were stable. After completing the trauma assessment and speaking with police, I ordered imaging and moved on. There were more patients to see, and a kid with a gunshot wound is not uncommon at our pediatric trauma center. Just another summer shift in the emergency department.
Then the call came from the radiology technician — the bullets
on his X-ray didn’t match the history and exam. The patient had reported being shot once, with one entry wound visible in the trauma bay. But the films were clear: several bullets tracked up the extremity into the pelvis. I raced to the bedside — what had I missed? — and there was my patient, sitting up calmly, normal sinus rhythm on the monitor.
I asked him again, “How many times were you shot? How many gun blasts did you hear?” He paused, then said, “This time? Just once.”
It took me longer than it should have to understand that this child had been shot before, that he was
calm because this was not his first gunshot wound, that our X-rays had found a chronology of bullets — a childhood filled with bullets. That this summer day of violence was not just uncommon for me as an emergency physician but common for him as a young Black boy in Milwaukee.
In 2020, deaths due to firearms surpassed all other causes of death for American children. On average, seven children die from a gunshot wound every day in the United States. Gun violence is especially devastating for the Black community: although Black youth represent only 14% of the youth population, they
“Firearm injuries, as the leading cause of childhood death, deserve the same public health framework as motor vehicle crashes, with injury documentation, tracking, and research advocacy at the federal level.”
account for nearly 50% of firearmrelated deaths.
Repeat gunshot wounds in childhood, like in my patient, offer a harrowing look into how pervasive gun violence is in America. A single gunshot wound, if survived, has lifelong effects. Studies of both children and adults who suffer gunshot wounds demonstrate increased rates of post-traumatic stress disorder, unemployment, substance use, and mental health disorders over their lifetimes. What about our patients who are shot more than once? What about those who live in fear of being shot, survive being shot, and then are shot again? Nearly one-fourth of patients who survive a gunshot wound at age 24 or younger will be shot again at least once within the next ten years. This level of recurrent injury is staggering. When patients return to the emergency department with another bullet wound, it’s not just another statistic. It’s a warning we cannot ignore; it’s a call to action for us to break the cycle of gun violence through prevention, policy, and trauma-informed care that sees the whole person, not just the injury.
What can we as emergency physicians do about gun violence in our communities? How do we advocate for our patients? One key tactic is fighting for evidence. For decades, the National Highway Traffic Safety Administration has maintained a database and provided leadership in the fight against motor vehicle crash-related deaths. Its efforts have informed legislative activities, trauma research, and public safety messaging. Firearm injuries, as the
leading cause of childhood death, deserve the same public health framework, with injury documentation, tracking, and research advocacy at the federal level. Dissemination of data that is state- and community-specific is invaluable for local intervention strategies.
Gun safety legislation is another evidence-based way to curb gun violence among children. Child access prevention laws hold gun owners liable if a child accesses a firearm, with the strictest laws associated with the lowest pediatric gun deaths. Universal background checks, which identify, for example, those with felony or domestic abuse convictions, require federal and local law enforcement to screen any individual purchasing a firearm. These have been linked with lower pediatric firearm mortality rates. “Red flag” laws allow the temporary removal of a gun if a person is deemed at imminent risk of injury to themselves or others. Implementation of red flag laws in Indiana and Connecticut showed a decrease in suicide deaths. As emergency physicians, we need to stay connected to our elected officials and serve as community resources for evidence-based policy decisionmaking that impacts the safety and well-being of children.
Secure storage prevents pediatric firearm deaths that occur both unintentionally and by suicide. Secure storage means a firearm is unloaded and locked, with ammunition stored and locked in a separate location. The vast majority of children under 12 who die by gunshot are shot in their own homes. Emergency departments
can collaborate with law enforcement agencies to provide free cable trigger locks, lockboxes, and safestorage information to parents and guardians. This practical intervention is especially important in a time of pediatric behavioral health crises and increased need for mental health care.
Pediatric injuries and deaths due to firearms demonstrate the current failure of our society to protect the most vulnerable. My 15-year-old patient, who has already survived multiple shootings, is not just a statistic but a real-world example of a trauma survivor who deserves to thrive as he reaches adulthood. He is our call to action to break the cycle of gun violence through prevention and policy. As emergency physicians, we can fight for evidence, use it to inform effective legislation and better public health strategies, and form community partnerships to keep our children safe.

Dr. Khan is an emergency medicine physician at Froedtert Hospital and an assistant professor in emergency medicine at the Medical College of Wisconsin. She is an advocate for gun violence prevention and for providing trauma-informed care to victims of gun violence.

Dr. Schultz is a pediatric emergency medicine physician at Children’s Wisconsin and an associate professor of pediatrics at the Medical College of Wisconsin. She has been a gun violence prevention advocate since working as a high school teacher in Baltimore, when one of her students sustained a life-altering gunshot wound.

By Saadia Akhtar, MD; Al’ai Alvarez, MD; Amanda J. Deutsch, MD; Rita Manfredi, MD; Christine R. Stehman, MD; and Maia Winkel, MD, on behalf of the SAEM Wellness Committee
Throughout training, emergency medicine (EM) physicians learn clinical skills to provide highquality patient care. This process begins before medical school and continues through residency, with a relatively clear, stepwise career progression. While medical schools understandably prioritize building a strong knowledge base critical for patient care, the importance of personal and professional well-being is often overlooked.
Over the past 20-plus years, burnout and moral injury in medicine—particularly among EM physicians—have continued to rise. These trends correlate with increased professional frustration, career dissatisfaction, and negative impacts on both personal relationships and practice longevity. Despite concerted efforts to address barriers to physician wellbeing, burnout and moral injury
remain pervasive. One persistent challenge is that many EM physicians lack tools to align career development with personal needs and motivations. This disconnect can hinder career satisfaction, growth, and the ability to navigate transitions effectively.
Self-determination theory (SDT) is a psychological framework that explores how sources of motivation affect the fulfillment of three core
psychological needs: autonomy, belonging, and competence—the “ABCs” of motivation. By understanding this relationship, individuals can better identify and influence goal setting and achievement. In short, SDT suggests we are more likely to reach our goals when we combine internal motivation with methods that support autonomy, connection, and mastery.
Recognizing the benefits of SDT in EM can help physicians shift from external pressures to an internal locus of motivation, a concept known as autonomous motivation. Focusing on intrinsic goals and values improves wellbeing, performance, learning, engagement, enthusiasm, and satisfaction—both at work and at home. Autonomous motivation is driven by personal values and interests rather than by external rewards or institutional demands. SDTbased approaches have also been shown to reduce symptoms of burnout, such as cynicism, emotional exhaustion, and inefficacy, as well as lower stress, anxiety, and depression
SDT is especially relevant in the daily realities of EM practice. Consider times when you’ve ordered numerous tests in accordance with institutional standards and repeatedly reassessed a patient, ensuring your recommendations for critical care and admission were clear. Despite your thorough work, a patient might still respond with dissatisfaction—perhaps even demanding to leave against medical advice, saying, “You’ve done nothing for me.” These common yet disheartening encounters can demoralize the entire care team and create a disconnect between effort and outcome, leading to moral distress or moral injury
In moments like these, applying the ABCs of SDT can help reframe the experience. By reconnecting with your values—your sense of belonging to your team, and your competence as a trained professional—you can shift your perspective. Instead of focusing on frustration, you can find reassurance in knowing you provided appropriate, compassionate care. This mindset shift fosters self-compassion and clarity while maintaining empathy for the patient.
In sum, using SDT to guide goal setting and decision making can help physicians:
1. Create better learning environments by promoting autonomy
2. Increase workplace motivation and satisfaction

Self-Determination Theory (SDT )
sed on
25 presentat
tar, Alvarez , Deuts
y 14, 2025
Type of Motivation + Suf ficiency of Psychologic al Needs Met
Achievement of Goals/ Pursuits Why Use SDT ? How to use SDT ? Improved Well-Being and Decreased Burnout Enhances learning environments (improved volitional learning, deep study, info absorption)
Improves workplace motivation/satisfaction (teamwork behaviors, support autonomy in others, better engagement)
Encourages long-term health and fitness behaviors (decreased stress, increased satisfaction with life)
Supports mental well-being (decreased burnout & stress levels)

“Despite your with dissatisfaction—perhaps
advice,

thorough work, a patient
dissatisfaction—perhaps even
advice, saying,
?
might still respond
demanding to leave against
'You’ve done nothing for me.”
al you want to achieve are going to achieve the goal.
Goals/Pursuits
Anything
do with your day of f
to lose weight
cus on in your career hing learners
l Identity Formation
Formation: Intersection of t), Belonging (Feel), etency (Think)
You Motivated?
working on this goal?
Autonomous
(Internal)
ased punishment /reward
3. Which Psychological Need Is Being Met?
continued from Page 105
3. Encourage lasting health and fitness habits
4. Support mental well-being through meaningful relationships By understanding and applying the ABCs of SDT, EM physicians can more clearly identify and pursue personal and professional goals at every stage of their careers—aligning their actions with what truly matters.
Dif fe
ectives
Providing rationale, freedom
Avoid ex ternal rewards
Minimize controlling words
Teaching Learners is a fine balance between allows autonomy and providing supervision.


Dr. Akhtar is a professor of emergency medicine and medical education and senior associate dean for trainee well-being and resilience in graduate medical education at Icahn School of Medicine at Mount Sinai.
Dr. Alvarez is a clinical associate professor and director of wellbeing at Stanford Emergency Medicine.

nishments
punishments (guilt /shame)
reward, action aligns with
u are
nally identify with rule
s with core values/norm
interest , play, curiosity
onomously Motivated y to be achieved
Belonging : Feel Like Par t Of A Team
B C D
rk done
Provide/seek positive & constructive feedback Suppor t skills development




Dr. Deutsch is a clinical assistant professor and director of well-being in the department of emergency medicine at Thomas Jefferson University.
Dr. Manfredi is a clinical professor of emergency medicine at George Washington University School of Medicine and Health Sciences.
Dr. Stehman is a visiting clinical associate professor at the University of Illinois College of Medicine at Peoria and OSF Healthcare.
Dr. Winkel is a clinical instructor and physician wellness fellow at Stanford Emergency Medicine.

By McKenzie Warshel, DO Med; Kirlos N. Haroun, MD; Kamna Balhara, MD, MA; Rodney Omron, MD, MPH; and Neda Gould, PhD
This is a story a colleague entrusted to me—one he has carried for years and gave me permission to share. Details have been altered to protect the patient’s privacy.
It was his very first day as an emergency medicine attending. Already overwhelmed by a busy morning, he encountered a case that seemed straightforward: a 45-year-old woman with numerous comorbidities arrived with a displaced tracheostomy tube. She was breathing comfortably and even joking with her mother at the bedside. Her trach size was atypical,
prompting a call to respiratory therapy and a precautionary chest X-ray.
Her mother stated, “My daughter hates hospitals. Can we just fix this and go home?”
He reassured her: “Of course. We’ll get this taken care of and get her home soon.”
While waiting, the patient developed mild shortness of breath. A bedside cardiac ultrasound— performed out of an abundance of caution—revealed an unexpected pericardial effusion. She remained
stable and showed no signs of distress or chest pain. Cardiology was consulted and recommended admission but didn’t feel urgent pericardiocentesis was necessary.
The trach was replaced. The patient again asked, “Can I go home now?”
He gently insisted, “We need to admit you. We don’t know where this fluid is coming from.”
Though frustrated, she agreed.
An hour later, she rapidly decompensated into cardiac tamponade. Unfamiliar with

“When an adverse event or unexpected outcome occurs, the patient is the first victim—but clinicians can become the second. This is known as second victim syndrome.”
the department layout, my colleague struggled to locate the pericardiocentesis kit.
Cardiopulmonary resuscitation (CPR) was initiated. It took 30 minutes to retrieve the necessary equipment. After 45 minutes, 200 cc of pericardial fluid was drained—but her pulse never returned.
Years later, he still asks himself, “Should I have pushed harder? Should I have had the needle ready? Did I do right by that patient?” And perhaps most painfully: “Did I keep my promise to her mother?”
Despite the weight of these questions, he had to finish his shift— moving on to the next patient, doing his best to care for each one that followed.
As healthcare professionals, we expect perfection from ourselves, but mistakes, bad outcomes, and missed diagnoses will happen. These events affect us—whether we want them to or not.
This story reflects something many in emergency medicine quietly endure: the emotional toll of clinical work. When an adverse event or unexpected outcome occurs, the patient is the first victim—but clinicians can become the second. This is known as second victim syndrome (SVS).
SVS describes the psychological aftermath providers may experience after involvement in a traumatic clinical event. It can provoke guilt, anxiety, and self-doubt—sometimes leading to burnout, isolation, or symptoms resembling post-traumatic stress disorder.
Studies estimate that up to 50% of healthcare professionals will experience SVS. Emergency medicine, with its high acuity and unpredictable pace, is particularly vulnerable. One study found that 30% of clinicians involved in an adverse event reported
long-lasting emotional distress, and 7% considered leaving medicine. Ideally, healthcare systems would provide the time and support needed to process these experiences. But with staffing shortages, growing patient volumes, and administrative burdens, there’s little space for reflection. Yet these unresolved emotions don’t just disappear—they follow us from room to room, subtly affecting the care we provide.
There is no one-size-fits-all approach to healing, but we offer two interventions to create space for reflection—tools, not solutions, that may help with SVS.
On-Shift
To address the emotional residue clinicians carry between patient encounters, Dr. Gould proposed ALL-
“Sometimes, thing we this reminder:

“Studies estimate that up to 50 percent of healthcare professionals will experience second victim syndrome, and emergency medicine is particularly vulnerable.”
continued from Page 109
CLEAR. ALL-CLEAR is a simple mental reset on shift. It’s not therapy or a substitute for deeper processing, but in the few seconds you have between rooms, it can help you refocus for the next patient.
• A: Accept that the event occurred. Not resignation—but acknowledgment that it happened.
• L: Label the emotion. Name what you’re feeling: sadness, frustration, anger, guilt.
• L: Learn from the moment. If there’s insight, hold onto it. If not, know that deeper reflection can come later.
• —: This is a space for a deep breath or mindful moment. This can be tailored to the amount of time you have—even five seconds.
• CLEAR: Clear your mind. Make space to be fully present for the next patient.
Off-Shift Connection: A Night of Reflection (NOR)
While ALL-CLEAR works in the moment, we also recognized the need
“Sometimes, the most powerful we can offer each other is reminder: you are not alone.”
for dedicated time to process the emotional challenges of clinical work. That’s why we created A Night of Reflection (NOR).
NOR is a communal gathering of residents and faculty, designed to foster connection, healing, and vulnerability. NOR is solely focused on emotions and experiences of clinicians—not as a morbidity and mortality (M&M) conference or clinical decision analysis.
We began the event by setting expectations about confidentiality and safety, opening with a facilitated discussion of thematically relevant artwork. This low-stakes approach allowed people to engage emotionally with the topic of SVS without having to speak right away.
Following this, we formed small groups with a mix of residents and faculty. Using guided prompts, participants shared personal experiences of challenging patient encounters. No one was obligated to share personal stories, but many did—finding strength in the presence of peers and mentors who simply listened without judgment. Many felt relief from shame, guilt, and self-doubt once they realized they were not alone.
We closed the evening with a guided meditation led by a licensed psychologist, followed by a largegroup debrief. The psychologist introduced the ALL-CLEAR tool as a take-home strategy—a bridge between the reflection created that night and real-world practice.
A Final Reminder
We share these two interventions—
ALL-CLEAR and A Night of Reflection— not as answers, but as invitations: to pause, acknowledge what we carry, and remember that behind every decision is a human being doing their best. Sometimes, the most powerful thing we can offer each other is this reminder: you are not alone




Dr. Warshel is a combined emergency medicine and anesthesia critical care medicine resident at Johns Hopkins Hospital.
Dr. Haroun is clinical faculty of emergency medicine at Johns Hopkins Hospital.
Dr. Balhara is associate professor of emergency medicine at Johns Hopkins Hospital.
Dr. Omron is assistant professor of emergency medicine at Johns Hopkins Hospital.
Dr. Gould is associate professor of clinical psychiatry and behavioral sciences at Johns Hopkins Hospital.

By Negin Ceraolo, MD, MS, and Kevin Watkins, MD, on behalf of the SAEM Wilderness Medicine Interest Group
In Part I, we discussed synthetic repellents and their effectiveness. While chemical repellents such as DEET (N,N-diethyl-meta-toluamide) are widely used and effective, there has been growing interest in natural alternatives. Many people seek natural insect repellents that are both effective and gentle on the skin. Fortunately, the FDA has approved several natural ingredients for use in insect repellents. Part II explores some of the most popular FDA-
approved natural insect repellents and their benefits.
One of the most popular natural insect repellents approved by the FDA is oil of lemon eucalyptus (OLE). Derived from the leaves of the Eucalyptus citriodora tree, OLE contains a compound called p-menthane-3,8-diol (PMD), which is responsible for its insect-repelling
properties. OLE has been shown to be effective in repelling mosquitoes and other biting insects, providing protection similar to that of DEET. The FDA has classified OLE as a biopesticide, and it is the only plantbased repellent that has received registration from the Environmental Protection Agency (EPA) for use as an insect repellent. Studies show OLE can provide up to six hours of protection against mosquitoes when applied correctly.

“Natural insect repellents offer an excellent way to enjoy outdoor activities while reducing the risk of insect-borne diseases.”
Benefits:
• Natural and plant-based alternative to chemical repellents
• Effective against a wide range of mosquitoes and other insects
• Has a fresh, citrus-like scent, which many people find more pleasant than synthetic repellents
Citronella Oil
Citronella oil is another natural ingredient commonly used in insect repellents. Derived from the leaves and stems of lemongrass (Cymbopogon nardus), citronella has a strong citrus-like scent that mosquitoes and other insects find unpleasant. It works by masking the scents that attract insects, such as carbon dioxide and body odors. Although it is not as long-lasting as DEET, citronella is effective for short periods—usually 30 to 60 minutes— and can be found in sprays, candles, and diffusers.
Benefits:
• Non-toxic and safe for use around children and pets
• Plant-based and environmentally friendly
• Easy to apply and available in various forms (sprays, lotions, candles)
Lavender Oil
Lavender oil is known for its soothing properties as well as its ability to repel insects, particularly mosquitoes. The oil contains compounds such as linalool and linalyl acetate, which have insect-repelling effects. Lavender oil disrupts sensory receptors in insects, making them avoid treated areas. While it may not provide as long-lasting protection as DEET, it can repel mosquitoes effectively for a few hours.
Benefits:
• Safe and gentle for people with sensitive skin
• Calming fragrance that can promote relaxation
• Safe for use around children and pets, making it ideal for families
Peppermint Oil
Peppermint oil is effective against mosquitoes, ants, and other insects. Its active compounds, including menthol, have insect-repelling properties. The strong menthol scent confuses and repels insects, making peppermint oil a popular choice for personal use. It can be applied directly to the skin when diluted with a carrier oil or used in sprays. Peppermint oil is often included in natural insect repellent formulations because it is both effective and refreshing.
Benefits:
• Refreshing scent that many find pleasant

“Oil of lemon eucalyptus is the only plant-based repellent that has received registration from the Environmental Protection Agency for use as an insect repellent.”
continued from Page 113
• Provides a cooling sensation while repelling insects
• Helps soothe itching from insect bites
Neem Oil
Neem oil, derived from the seeds of the neem tree (Azadirachta indica), has long been used in traditional medicine for its antifungal, antibacterial, and insect-repelling properties. Though less well-known than other oils, neem oil has gained popularity as a natural alternative repellent. It contains compounds such as azadirachtin that interfere with insects’ ability to reproduce and feed, making it effective against mosquitoes and ticks.
Benefits:
• Provides long-lasting protection
• Non-toxic and safe for use on skin
• Has antifungal and antibacterial properties that may reduce skin irritation after insect bites
Tea Tree Oil
Tea tree oil, derived from the leaves of the Melaleuca alternifolia tree, is well known for its antibacterial and antifungal properties. It also repels mosquitoes. Compounds such as terpinen-4-ol act as natural insect deterrents by disrupting insects' ability to sense human body odors, making it harder for them to locate their target.
Benefits:
• Often used to soothe insect bites and reduce inflammation
• Gentle alternative for sensitive skin when diluted properly
• Has a fresh, medicinal scent that complements other essential oils in natural repellent blends
Natural insect repellents are popular among those seeking alternatives to traditional chemical repellents. While the FDA has approved several plant-based ingredients—including oil of lemon eucalyptus, citronella, lavender, peppermint, neem, and tea tree oils—it is important to understand that not all natural repellents are equally effective or long-lasting. Some require more frequent application than chemical-based options. Before using any insect repellent, natural or synthetic, follow product instructions carefully and test on a small skin area to check for allergic reactions. Natural repellents offer an excellent way to enjoy outdoor activities while reducing the risk of insect-borne diseases.
1. Follow instructions: Always read and follow the manufacturer's guidelines when applying insect repellents. Overuse or incorrect application can cause skin irritation or reduce effectiveness.
2. Apply to exposed skin and clothing: Repellents should be applied to exposed skin, especially areas not covered by clothing. Products like permethrin should be applied to clothing for longer-lasting protection.
3. Reapply as needed: Some repellents, particularly those with lower active ingredient concentrations, require reapplication after several hours, depending on activity and environment.
4. Avoid contact with eyes and mouth:
When applying repellent to the face, use your hands and avoid sensitive areas such as eyes, mouth, and mucous membranes.
5. Consider your environment: In areas with high insect populations or disease risk, take extra precautions such as wearing long sleeves, pants, and head nets, especially when combined with repellent use.
In conclusion, insect repellents are an essential tool in wilderness medicine, providing a critical line of defense against the discomfort and health risks posed by insect bites. By understanding the different types of repellents available and the specific risks posed by various insects, outdoor enthusiasts and medical professionals can make informed decisions to protect themselves and others. Whether camping in the backcountry or exploring remote wilderness areas, insect repellents remain an integral part of wilderness safety and health management.


Dr. Ceraolo is an emergency medicine resident physician currently training at Cleveland Clinic Akron General Medical Center. Her interests during residency include prehospital care, wilderness medicine, research, advocacy, and global health medicine.
Dr. Watkins is core faculty at Cleveland Clinic Akron General, where he serves as director of wilderness medicine and is ultrasound faculty. He is also vice chair of the Society for Academic Emergency Medicine wilderness medicine interest group and a Wilderness Life Support for Medical Professionals instructor
SAEMF proudly recognizes its Enduring and Sustaining donors for their commitment to advancing academic emergency medicine. Through their support of the Annual Alliance, these dedicated individuals are helping drive innovation in research and education, and shaping the future of emergency care.




























































Every donor makes a meaningful impact—together, Annual Alliance supporters enable SAEMF to award over $1 million each year in research and education grants. We look forward to honoring our Advocates, Mentors, Young Professionals, and RAMS donors in future issues. Learn more about becoming an Annual Alliance donor and see the full 2025 Annual Alliance Donor list. Contact Julie Wolfe, Senior Manager of Development, for more information about SAEMF’s work and ways to get involved.

Successful Grant Writing Workshop Draws High Participation and Engagement
The Research Committee is pleased to share that the SAEM25 Grant Writing Workshop was a great success, with a high number of participants and an especially engaged audience—including many from the Academic Research Mentoring and Education Development (ARMED) program. Special thanks go to Dr. Brandon Maughan for organizing and leading the workshop, and to SAEM staff for their essential support at the door and behind the scenes, helping to ensure all technical aspects ran smoothly. Thank you to everyone who participated and contributed to a productive and collaborative session!

Upcoming Webinar: Exploring Loneliness and Social Isolation in Older Adults
We invite you to join the next webinar in the Geriatric Mental Health and Wellness Collaborative Series, hosted by the Aging, Geriatric, and Emergency Medicine Interest Group and the Behavioral and Psychological Interest Group. The webinar, titled "Loneliness and Social Isolation," will take place Thursday, Aug. 14, at 6 p.m. CT. Click here to register.
This session will provide a space to explore and discuss the impact of loneliness and social isolation on older adults, along with strategies to address and reduce these issues.
In the meantime, feel free to revisit or share the recording of our previous webinar, “Altered Mental Status, Delirium and Geriatric Agitation in the Emergency Department,” with your colleagues. We look forward to your participation!
Accepting
The Clerkship Directors in Emergency Medicine (CDEM) Career Development & Mentorship Committee has launched a new mentorship program to support the growth of academic emergency medicine educators. Open to all CDEM and SAEM Education Committee, and fellow members, the program pairs participants based on shared interests, goals, and expertise to foster meaningful, long-term connections. Structured yet flexible, the program is built on four pillars:
• Career Development: Support in academic promotion, scholarship, and leadership.
• Educational Leadership: Exchange of best practices across UME and GME.
• Meaningful Relationships: Mentoring that goes beyond career advice.
• Community Building: Strengthening collaboration within CDEM and SAEM.
To be considered, qualified applicants must complete the official form by September 5, 2025. To access it, log into your SAEM account using the “Login” button in the top-right corner. After logging in, you’ll be redirected back to this page, and the application link will appear at the top.
The Simulation Academy hosted its virtual Fellows Forum in April, spotlighting research by simulation fellows and early career simulationists. A judging panel recognized two presenters for outstanding work:
• Dr. Kevin Hon (New York University): Emergency Medicine Resident-Led Clinical Event Debriefing: Impact on Behaviors and Wellness
• Dr. Nora McNulty (Vanderbilt University): Effectiveness of Self-Directed Rapid Cycle Deliberate Practice Simulation in Cardiac Arrest Management
Designed to support early career faculty and fellows (within two years of training), these rapid grants fund projects for forum presentation. This year’s awardees all presented at the Fellow Forum, with Dr. Stewart receiving additional recognition for excellence.
• Dr. Katherine Stewart (Brown University): Narrative vs. Scientific Priming Literature on Resident Attitudes in Verbal De-Escalation Simulation
• Dr. Alaa Aldalati (University of Kansas): SimulationBased Debriefing to Support Launch of KU-Wesley EM Residency
• Dr. Victoria Zhou (University of Vermont): Resuscitation Leadership Curriculum for Emergency Medicine Residents
ARMED MedEd Scholarship
Awarded annually to support simulation faculty in educational scholarship, this year’s recipient is Dr. Mariju Baluyot, associate director for pediatric emergency medicine simulation at Riley Hospital for Children. Her project focuses on in-situ simulation to enhance interprofessional communication during pediatric resuscitations.
Novice Research Grant
Jointly awarded by the SAEM Foundation and Simulation Academy, this competitive grant went to Dr. John Gaillard and Dr. Dominique Gelmann (Wake Forest University) for Using Simulation to Improve Extracorporeal Cardiopulmonary Resuscitation in the Emergency Department
SAEM Reports provides your group with a platform to highlight key activities and initiatives, increase visibility, and engage potential new members from across the SAEM community. By contributing updates, you help showcase the valuable work of your academy and strengthen connections that can support its continued growth. Here’s how to submit:
1. Click the appropriate link below for your group and bookmark it:
• Committees
• Academies
• Interest Groups
2. Find your group in the alphabetized list.
3. Provide your name, email, and date submitted
4. Insert up to 3 announcements of no more than 150 words each by the stated deadline
2025 Simulation Academy Awards
Over 45 nominations from 31 institutions were submitted this year. Award recipients include:
• Early Career Educator: Dr. Michelle Hughes
• Distinguished Educator: Dr. Christopher Strothers
• Simulation Innovation: Dr. Laura Weber
• Simulation Research: Dr. Rebekah Cole
• Change Agent: Dr. Stephanie Stapleton
• Trainee of the Year: Dr. Taylor Cesarz
• Travel Scholarship: Dr. Danier Ong, Dr. Katherine Stewart
“Submit
The Early Career Subcommittee hosted an Instagram contest to showcase creative simulation efforts (view the winning videos on the SAEM Simulation Academy Instagram page.):
• Most Creative: Dr. Audrey Bethel (East Valley Emergency Medicine Residency)
• Most Popular: Dr. Colleen Donovan (Robert Wood Johnson Medical School)
The Simulation Academy congratulates all recipients and celebrates their contributions to simulation-based education in emergency medicine.


Rahul Sharma, MD, the Barbara and Stephen Friedman Professor and chair of emergency medicine at Weill Cornell Medicine, and emergency physician-in-chief at NewYork-Presbyterian/Weill Cornell Medical Center, has received the 2025 Roger Schenke Award from the American Association for Physician Leadership. The award recognizes individuals who have made significant contributions to leadership education, management training and professional development in health care. Sharma was honored for his work in telemedicine and virtual care. He founded Weill Cornell Medicine’s Center for Virtual Care, a national leader in training and curriculum development in telemedicine. He also spearheaded the “Doctoring in the Digital Age” curriculum, which trains first-year residents and fellows in providing high-quality virtual care.

Ana Pineda, MD, has been appointed the first chair of the newly independent Department of Emergency Medicine at HCA Florida Kendall Hospital, effective January 2025. Her two-year appointment follows the department’s separation from internal medicine and marks a significant milestone for the institution. A member of the hospital’s first emergency medicine residency graduating class in 2019, Dr. Pineda also completed the inaugural Emergency Medicine Administration and Operations Fellowship in 2020. Her combined clinical and administrative experience positions her to lead the department into its next chapter.

Stephanie Carreiro, MD, PhD, has been promoted to vice chair of research in the Department of Emergency Medicine at UMass Chan Medical School. A nationally recognized leader in medical toxicology and co-director of the ACMT Antidote Institute, Carreiro has secured extensive federal and industry funding. Her visionary research and commitment to mentorship are helping shape the future of emergency medicine.




Jason Wilson, MD, PhD, professor and chair of emergency medicine at the University of South Florida Morsani College of Medicine, has appointed three vice chairs during the department’s inaugural year. Roland C. Merchant, MD, MPH, ScD, joined the faculty as vice chair of research and assistant dean of faculty development. David Wein, MD, MBA, was appointed vice chair of clinical operations. Haru Okuda, MD, was named vice chair of academic affairs.

Lauren Maloney, MD, clinical assistant professor of emergency medicine and adjunct assistant professor of biomedical engineering at Stony Brook University, has received the Young Academic Inventor’s Award from the Stony Brook University Chapter of the National Academy of Inventors. She is the first physician to receive the award, which recognized her invention of a motion-adaptive training system to improve prehospital ultrasound education for paramedics.

Cassandra Bradby, MD, has been promoted to associate professor of emergency medicine with tenure at the Brody School of Medicine at East Carolina University. A graduate of Meharry Medical College and SUNY Downstate Medical Center, Bradby is the emergency medicine residency program director for ECU Health Medical Center. In 2025, she received the ECU ScholarTeacher Award, a university-wide honor recognizing excellence in the integration of teaching and research. She is widely known for her commitment to mentorship, clinical education, and academic leadership.

Allegheny General Hospital’s Emergency Medicine Residency Program marks its 43rd anniversary this June. Founded in 1982, the program has become a national leader in emergency medicine training and innovation. It also gained visibility as the real-life setting for the acclaimed medical drama The Pitt
Dr. Emily Jean Lucid, a University of Texas Medical Branch graduate, led the program during its formative years, shaping a culture of compassionate, high-performance care. AGH was an early adopter of point-of-care ultrasound in the emergency department and played a key role in advancing therapeutic hypothermia after cardiac arrest.
Among its founding figures is Dr. Dietrich Jehle, now chair of emergency medicine at UTMB. Alumni from the program hold leadership roles nationwide, including with SAEM, and remain active in academic emergency medicine.
The milestone celebrates a legacy of excellence in clinical care, education and mentorship that continues to influence the specialty today.

SAEM Launches Federal Funding Committee to Advance Research and Agency Engagement
SAEM has established a new Federal Funding Committee to strengthen research and support academic emergency medicine. The committee will build relationships with federal agencies, promote funding opportunities, and keep members informed on policy and research updates. Applications for the new committee closed on June 15, 2025.
AEMP Becomes SAEM’s Ninth Academy!
SAEM proudly welcomes the Academy of Emergency Medicine Pharmacists Academy of Emergency Medicine Pharmacists (AEMP) as its ninth academy. Approved by the SAEM Board of Directors at SAEM25, AEMP evolved from a thriving interest group and shared vision to advance EM pharmacy through research, education, and multidisciplinary collaboration. AEMP strengthens ties between EM pharmacists and SAEM’s academic community, providing a professional home that supports leadership, innovation, and excellence in practice. We look forward to the vital contributions AEMP will bring to our shared mission of improving emergency care.
Ready to Match? Connect With Top Programs at the Virtual RFF!
Meet online with top residency and fellowship programs from across the country — ready to share insights and guide you through the application process. The fair is free and open to all residents and medical students. View the updated list of participating programs and sign up today to meet with as many as you'd like!
Residency and Fellowship Programs: Recruit Top Candidates — All in One Place! Connect with hundreds of qualified candidates in this streamlined, cost-effective virtual fair. Showcase your program and evaluate fit efficiently. Space is limited — register your program today!
Apply for These Educational Courses By July 31!
Boost your skills and leadership in emergency medicine with these specialized educational programs. Whether you’re focused on research, leadership, or administration, these opportunities provide expert training, mentorship, and career development to advance your career in emergency medicine.
• Advanced Research Methodology Evaluation and Design (ARMED): For junior faculty, fellows, and senior residents. Gain essential skills in research design and grant writing through interactive workshops and monthly webinars. Scholarships available.
• Chair Development Program (CDP): For new and aspiring academic EM chairs. Receive leadership training through in-person and virtual sessions led by seasoned professionals. Scholarships available.
Academic Emergency Medicine invites submissions for a 2026 special issue focused on advancing emergency care for older adults. We welcome original research, reviews, case studies, and clinical guidelines on topics such as:
• Innovative models of geriatric ED care
• Polypharmacy and multimorbidity
• Risk stratification and screening tools
• Age-friendly health systems and the 4Ms
• Delirium, dementia, falls, and elder mistreatment
Submission deadline is October 31, 2025. For inquiries contact Elyssa. grogan@nyulangone.org. Find full details and submission instructions here
A special issue of AEM Education and Training (AEM E&T) highlighting proceedings from SAEM24 in Phoenix, is now available. The issue includes conceptually based white papers authored by members of SAEM academies, committees, and interest groups. These papers present innovative ideas and approaches relevant to medical education and training.
AEM Education and Training (AEM E&T) is seeking submissions for a special SAEM25 Proceedings issue, to be published in early 2026. We invite manuscripts and conceptually based white papers from SAEM academies, committees, and interest groups. Papers should focus on innovative ideas and concepts unique to their areas of expertise, with an emphasis on education and training in emergency medicine. Submit by September 1, 2025.
A variety of insightful webinars are scheduled in the coming months—be sure to mark your calendar and check back often as new sessions are added. Visit the SAEM Webinar Library to explore the full lineup of live and recorded presentations on important topics in academic emergency medicine.
The SAEM Foundation (SAEMF), in partnership with SAEM, provides grants to national and international universities and medical schools to help fund innovative research and education initiatives in the field of emergency medicine. In order for a project to be eligible for funding, it must fit into the scope of one of the grant categories listed below, and must support the mission of SAEM and the SAEMF. Grants below are accepting applications. Apply by 5 p.m. CT on August 1, 2025.
• Research Training Grant (RTG)$300,000
• Research Large Project Grant (LPG)$150,000
• Education Research Training Grant (ERG) - $100,000
• SAEMF Emerging Infectious Disease and Preparedness Grant - Up to $100,000
• SAEMF/ED Benchmarking Alliance Clinical Operations Research Grant$50,000
• SAEMF ARMED Pilot Grant - $25,000
• SAEMF ARMED MedEd Pilot Grant$25,000
• Education Project Grant (EPG) - $20,000
• Geriatric Emergency Medicine Research Catalyst Grant, Supported by Michelle Blanda, MD - $10,000
• SAEMF/Clerkship Directors in Emergency Medicine (CDEM) Innovations in Undergraduate Emergency Medicine Education Grant - $8,000
• MTF/SAEMF Toxicology Research Grant - $20,000
• SAEMF/Academy of Emergency Ultrasound (AEUS) Research Grant$10,000
• SAEMF/Global Emergency Medicine Academy (GEMA) Research Pilot Grant - $10,000
• SAEMF/Academy for Women in Academic Emergency Medicine (AWAEM) Research Grant - $10,000
• SAEMF/Simulation Academy Novice Research Grant - $5,000
• SAEMF/Academy for Diversity and Inclusion in Emergency Medicine (ADIEM) Research Grant - $6,000
• SAEMF/Resident and Medical Students (RAMS) Research Grant$2,500 - $5,000
• The Ali and Danielle Raja RAMS Medical Student Research Grant - Grant of $2,500 plus scholarship to defray costs of participation as a Medical Student Ambassador at the SAEM’s Annual Meeting
• The David E. Wilcox, MD, FACEP Endowed Scholarship - Scholarship: $1,250 Bestowed upon the highest scoring RAMS Resident and RAMS Medical Student Research Grant recipients annually
Not all categories are offered every year. Visit saem.org/grants for more info.
Whether you’re just getting started or looking to expand your impact, these curated resources will support your success in research. Explore study types and research methodologies, discover writing and funding opportunities, find your research niche, learn how develop a research question and design a study, and more!
This curriculum is designed for medical students rotating through pediatric emergency departments. Developed as a supplement to the original CDEM curriculum, it emphasizes core pediatric topics essential for clinical practice. Topics range from trauma and respiratory conditions to gastrointestinal, neurological, and endocrine emergencies.
This evolving repository introduces foundational AI concepts, highlights practical applications, and provides curated resources to help educators integrate AI into teaching, learning, and assessment. Sections include definitions, implications for medical education, ethical considerations, basics of working with large language models (LLMs), prompt engineering, and real-world examples such as journal clubs, communication practice, chalk talks, teaching materials, and letters of recommendation.
This digital guide is designed to empower women navigating the complexities of academic emergency medicine. Spanning professional development, mentoring, promotion, recruitment/support, grant writing, scholarship development, wellness, and gender-specific needs, it serves as a compass, providing insights and strategies to overcome challenges and seize opportunities.
This 5-module curriculum is designed to help emergency medicine physicians build confidence and skills in clinical teaching. Perfect for faculty development or individual learning, this evidence-based toolkit includes videos, activities, and curated resources to support effective teaching while managing patient care.
This comprehensive digital guide empowers academic emergency medicine physicians with essential strategies for tackling critical issues in today’s health care landscape. From optimizing telehealth in emergency medicine to implementing effective emergency department observation units, this toolkit offers invaluable insights to mitigate the impact of boarding on patient experience.

For early-career educators interested in academic publishing, few opportunities are as hands-on and high-impact as the Academic Emergency Medicine Education and Training (AEM E&T) Fellow Editor-in-Training Program.
Launched to mentor medical education fellows in peer review, editing, and scholarly publishing, the program offers a one-year appointment to the journal’s editorial board. For the 2024–2025 term, Neelou Tabatabai, DO (UNC Health Southeastern), and Ivan Zvonar, MD (University of Washington), were selected from a competitive national pool.
The experience gave both physicians a front-row seat to the editorial process—and helped them grow as educators, scholars, and future mentors.
“When I started, I had never done a peer review,” said Dr. Tabatabai. “It felt intimidating, but with guidance from Dr. Esther Chen, I learned it’s not about having all the answers—it’s about contributing meaningfully to the conversation.”
Through repeated reviews, feedback, and mentorship from Dr. Chen, Tabatabai gained confidence and developed a deeper understanding of how thoughtful critique can improve both a manuscript and the reviewer’s own writing. During her fellowship year, she submitted her first commentary to AEM E&T and was selected to present at the 2025 SAEM Annual Meeting.
Dr. Zvonar also entered the program with a hunger to learn the nuances of academic medicine. “There’s a
hidden curriculum in academic writing—skills we’re not taught in medical school or residency,” he said. “This fellowship filled in those gaps.”
He highlighted three key takeaways from the experience: insight into the editorial process, the value of strong mentorship, and the importance of joining a community of practice. “You start to recognize authors you’ve read and admired, and suddenly you’re reviewing their work or sitting in meetings with them. It’s humbling—and motivating,” he said.
Both fellows credited Dr. Chen, who serves as decision editor at AEM E&T and leads the program, as instrumental to their growth. “Her mentorship sets the tone,” Zvonar said. “She challenges you, encourages you, and helps you see yourself as a contributor to the field.”
The fellowship also fosters a sense of community. “Academic writing can feel solitary,” said Tabatabai, “but this experience reminded me that collaboration and mentorship are at the heart of impactful scholarship.”
The program not only prepares fellows to review and write more effectively—it also empowers them to pursue academic careers with confidence and purpose. “It changed how I see academic writing,” Tabatabai said. “What once felt intimidating now feels like an essential, fulfilling part of my career.”
Applications for the 2026–2027 Fellow Editor-inTraining term will open in December 2025. All applicants must be current fellows in emergency medicine education with a strong interest in scholarship.
As Zvonar put it: “Fellowship education is like a choose-your-own-adventure novel. This one opened doors I didn’t even know existed—and I’m better for it.”

POST YOUR OPEN JOBS IN FRONT OF OUR
Accepting ads for our “Now Hiring” section!
Deadline for the next issue of SAEM Pulse is August 1.
For specs and pricing, visit the SAEM Pulse advertising webpage.

Check companies advertising jobs on SAEM’s EM Job Link against your LinkedIn contacts. Leverage professional connections for more information about the company or request a referral.

(1T32HL160513 | NIH / National Heart, Lung, and Blood Institute)
Advance your career through a 2- or 3-year NIH-funded fellowship at the Icahn School of Medicine at Mount Sinai, preparing early-career clinicians and scientists for independent research careers in emergency care. Tracks in clinical and health services research available. Application Deadline: July 1, 2026
Program Highlights
• Extensive Research Experience: Work on individual and collaborative projects with progressive independence in acute cardiac, pulmonary, hematologic, and traumatic conditions.
• Outstanding Mentorship: 30+ interdisciplinary mentors from Emergency Medicine, Cardiology, Pulmonary, Hematology, and more.
• Structured Didactics: Formal training in research methods, biostatistics, ethics, disparities, and community engagement.
• Degree Opportunity: Earn a Master of Science in Clinical Research.
• Career Development: Workshops on grant writing, leadership, academic advancement, and wellness.
• Collaborative Culture: Supportive environment emphasizing multidisciplinary teamwork and mutual respect.
Eligibility
• Physicians: EM residency graduates, surgery residents (3+ years), or current fellows in cardiology, pulmonary, critical care, hematology, or pediatric EM.
• Other Clinicians: Doctoral-level nurses, pharmacists, social workers with emergency care research interest.
• Non-Clinicians: Doctorates in biostatistics, epidemiology, health services research, or related fields.
Applicants must be U.S. citizens or permanent residents with a doctoral degree. Prior NIH R/P/K awardees are ineligible.
Application Deadline: July 1, 2026
Submit the following via our online application portal:
• CV (with contact info)
• Personal Statement (2 pages)
• 3 Letters of Recommendation (incl. 1 from program director/supervisor)
• Medical/Professional Diploma
• USMLE/In-Service Scores (for MDs)
Contact Us:
• Phone: 212-824-8057
• Email: ERTP@mountsinai.org
Program Leadership:
Lynne D. Richardson, MD, FACEP, program director
Alex Manini, MD, MS, associate program director
Cindy Clesca, MA, program administrator


Mount Sinai Emergency Care Research Fellowship, One Gustave L. Levy Place, Box 1620, New York, NY 10029


About Us: Penn State Health is a multi-hospital health system serving patients and communities across central Pennsylvania. We are the only medical facility in Pennsylvania to be accredited as a Level I pediatric trauma center and Level I adult trauma center. The system includes Penn State Health Milton S. Hershey Medical Center, Penn State Health Children’s Hospital and Penn State Cancer Institute based in Hershey, Pa.; Penn State Health Hampden Medical Center in Enola, Pa.; Penn State Health Holy Spirit Medical Center in Camp Hill, Pa.; Penn State Health Lancaster Medical Center in Lancaster, Pa.; Penn State Health St. Joseph Medical Center in Reading, Pa.; Pennsylvania Psychiatric Institute, a specialty provider of inpatient and outpatient behavioral health services, in Harrisburg, Pa.; and 2,450+ physicians and direct care providers at 225 outpatient practices. Additionally, the system jointly operates various healthcare providers, including Penn State Health Rehabilitation Hospital, Hershey Outpatient Surgery Center and Hershey Endoscopy Center.
We foster a collaborative environment rich with diversity, share a passion for patient care, and have a space for those who share our spark of innovative research interests. Our health system is expanding and we have opportunities in both academic hospital as well community hospital settings.

Benefit highlights include:
• Competitive salary with sign-on bonus
• Comprehensive benefits and retirement package
• Relocation assistance & CME allowance
• Attractive neighborhoods in scenic central Pennsylvania



May 18-21, 2026 | Atlanta Marriott Marquis